A603e89f 7e12 449d 8c9d 28616061f601
2017-09-26
: Pdf A603E89F-7E12-449D-8C9D-28616061F601 a603e89f-7e12-449d-8c9d-28616061f601 9 2017 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 2
Case Study:
Staging Bridge™ Occlusion Balloon Mid-Case
Sumit Verma, MD, FACC, Heart Rhythm Center, Baptist Hospital, Pensacola, Florida
Background:
SVC tears during lead extraction are very rare, occurring in less than 0.5%
of procedures. The Bridge Occlusion Balloon was designed to provide
hemostasis in the rare event of a SVC tear, allowing time for surgical repair
and increasing survivability. Dozens of rescues have been supported utilizing
this novel device.1
One of several recommendations for deploying Bridge prophylactically is
for high-risk cases.2 When Bridge is staged in the IVC, it can support rapid
deployment and minimize blood loss. At the onset, some cases may not
appear high risk. Yet, case diculty may increase intra-procedure, and
prophylactic deployment may be considered. This case description details
a lead extraction case performed by Dr. Sumit Verma. Bridge was deployed
mid-case when the perception of risk increased.
Case Description
• Procedure performed in a surgical OR suite with cardiovascular surgeon and
perfusionist on stand by.
• Standard lead extraction protocol (central and arterial lines, femoral vein
and arterial access, intraoperative TEE, blood products in the room).
• Bridge™ Prep Kit was used. A 0.035” super-sti guidewire was advanced
through a 6F peel away sheath from the left femoral vein to the right IJ.
A 12F introducer sheath was on the wire outside of the body in case of
emergent Bridge deployment. The bottom end of the guidewire was
clamped to the drape to maintain position throughout the procedure.
• A 60 cc syringe was lled with contrast and saline mix (per the IFU, 12
cc contrast & 48 cc saline). Bridge™ Occlusion Balloon was immediately
available.
• Temporary pacer was also inserted through the left femoral vein.
• The generator was then removed and access to the left subclavian vein
was secured.
• To create a traction platform, LLD EZ™ locking devices were deployed in
the lumen of each lead and sutures were tied to the insulation.
• In order to minimize the lead-to-sheath gap, a 12F GlideLight™ laser
sheath with a VisiSheath was selected. The sheath was advanced over the
RV lead.
• Signicant lead-on-lead and lead-to-wall binding was encountered at the
innominate/SVC junction and progression stalled.
• Before upsizing to a 14F GlideLight™ laser sheath, Bridge was advanced
into the anatomy as a precaution.
• The 14F laser sheath was advanced from the SVC to the tricuspid valve, at
which point systolic blood pressure dropped from 120 mm to 70 mm and
remained low despite releasing the traction on the lead and immediate
infusion of vasopressors.
• Bridge was deployed, and diagnostics were investigated. TEE showed no
eusion and no tamponade. No hemothorax was seen uoroscopically.
• Once the surgeon was in the room, the balloon was deated and an
angiogram was performed from the right arm. No extravasation was seen.
• The extraction continued and the RV and RA lead were successfully
removed.
Patient and Device History
• 89-year-old male with a dual-chamber
pacemaker implanted in 2009 for atrial brillation
and complete heart block.
• Patient underwent generator change three
weeks prior and developed a pacer site infection,
necessitating extraction of the system.
• No prior CABG or open heart surgery. Previous
atrial utter RFA.
Figure 1. Practicing Bridge
ination prior to an
emergent situation helps
refresh the team on the
workow.
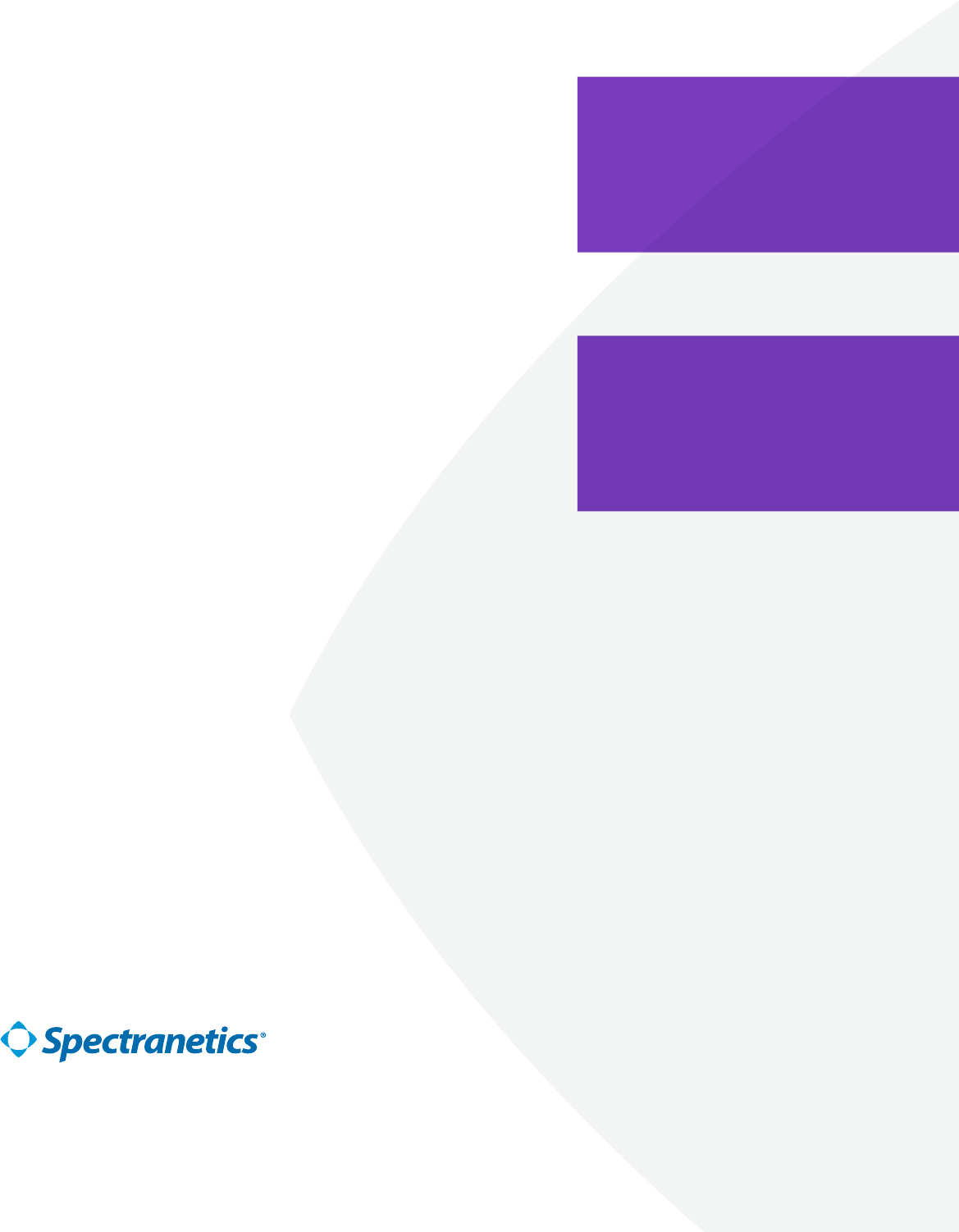
Figure 2. Determining
placement in the SVC
for potential ination
beforehand. Bridge can then
be stationed in the IVC.
Figure 3. Bridge inated after
blood pressure dropped.
Diagnostics determined
no SVC tear. Bridge was
deated and the extraction
completed successfully.
Implanted Leads: Implant Date
Guidant 4087 (RA lead) 2009
Guidant 4088 (RV lead) 2009
Indication for Extraction
Pocket Infection (Class I)
Always Reaching Farther
©2017 Spectranetics. All Rights Reserved. Approved for External Distribution. D038018-00 072017
References
1. SPNC Post Market Surveillance, 2017. Data on File.
2. Wilko BL, Kennergren C, Love CJ, Kutalek SP, Epstein LM, Carrillo R, Bridge to Surgery: Best Practice
Protocol Derived From Early Clinical Experience with the Bridge Occlusion Balloon., Heart Rhythm (2017),
doi: 10.1016/j.hrthm.2017.07.008.”
Discussion with Dr. Verma
Prophylactic Deployment Mid-Case
Just looking at the demographics, this patient may not have appeared high
risk. Normally, I would not expect this case to give me any trouble. Yet, as
heavy lead-on-lead and lead-to-wall binding was encountered and greater
traction force was required, the case became higher risk in my mind. The
balloon was inserted as a precaution to support a quick deployment and limit
any potential blood loss.
When the blood pressure dropped and we inated Bridge, it was impressive
to see everyone in the room was composed. We were prepared and felt we
had the situation under control. Bridge has changed the dynamic of the
room—from panic to calm.
In the future, I plan to prophylactically inate Bridge when I feel case diculty
has increased intra-procedure. We have surgical backup that is immediately
available, yet often not in the room. Bridge provides time to stabilize the
patient and transition to surgery.
Patient Prep
Prepping every patient undergoing extraction with a guidewire and
introducer sheath has become our standard. This is part of Bridge Best
Practice Protocol.2 In this case, additional time was required to insert the
guidewire because the right femoral vein was occluded. The guidewire was
alternately placed through the left femoral vein to the right IJ. Also, the
patient had signicant binding in the vessel, and a JR4 catheter was required
to guide the wire past the heart. Trying to place a wire and the balloon in an
emergent situation, instead of beforehand, may have been impossible in this
patient.
It is important for operators to understand that there may be unforeseen
patient characteristics that add time to deployment. It is imperative to
be prepared beforehand. The more you can prepare for immediate
deployment, the better o you are.
Pre-Huddle Timeout
We incorporate Bridge into our pre-case timeout. We know exactly where it
is, and it is always immediately available. Then we decide whether the case is
high-risk and if we want to stage Bridge in the IVC.
Prior to this case, I had prophylactically inated the balloon in order to
become familiar with the device and the workow. It is important for our
team to practice the workow on a regular basis. Dierent extractors and
support sta all need to be familiar with the balloon, patient prep and steps
for deployment.
“There was no tear in this case,
but had there been a tear, we
would have been prepared to
save the patient.”
-- Sumit Verma, MD, FACC
Important Safety Information
Indications for Use
The Bridge Occlusion Balloon Catheter is indicated for use for temporary vessel
occlusion of the superior vena cava in applications including perioperative
occlusion and emergency control of hemorrhage.
Any use for procedures other than those indicated in these instructions is not
recommended
Contraindications
None Known
Warnings
Lead extraction should be performed at institutions with cardiothoracic surgical
capabilities by physicians knowledgeable in the techniques and devices for
lead or catheter removal. Complication prevention and management protocols
should be in place and routinely practiced. It is strongly suggested that the
recommendations for lead management of the Heart Rhythm Society (HRS) and
European Heart Rhythm Association (EHRA) be followed for best results.
Prior to initiating the lead extraction procedure, a Bridge Occlusion Balloon
Catheter compatible guidewire should be placed through a venous access
site and across the length of the superior vena cava. Attempting to place a
compatible guidewire after a venous tear occurs may:
• result in an inability to traverse the superior vena cava with the guidewire
• result in the guidewire exiting the vasculature at the tear site
• result in an inability to place the Bridge Occlusion Balloon Catheter
• delay or prevent the ability to achieve occlusion
Do not position the Bridge Occlusion Balloon Catheter in a manner that would
obstruct the right atrium. Obstruction of the atrium could lead to arrhythmias
and/or hemodynamic compromise. Failure to observe recommended ination
techniques may result in the formation of contrast crystals which could prevent
deation.
Do not over-inate the Bridge Occlusion Balloon Catheter after fully occluding
the vessel. Over ination may result in damage to the vessel, rupture of the
balloon, or introduction of air emboli.
Do not exceed the Maximum Ination Volume. Over ination may result in
damage to the vessel, rupture of the balloon, or introduction of air emboli.
Occlusion of the superior vena cava beyond 30 minutes is not recommended as
this may increase the risk of adverse physiologic or neurologic complications.
Do not resterilize or reuse this device, as these actions can compromise device
performance or increase the risk of cross-contamination due to inappropriate
reprocessing.
Reuse of this single use device could lead to serious patient injury or death and
voids manufacturer warranties
Refer to the IFU for additional information.
Case study and discussion provided, reviewed, and approved
by Dr. Sumit Verma, MD FACC 07/2017
“Bridge allows us to perform
the extraction procedure with
more control over potential
complications.”
-- Sumit Verma, MD, FACC