Boston Scientific CRMU22814 L300, L301, L321, L310, L311, L331, L200, L201, L221, L210, L211, L231, L100, L101, L121, L110, L111, L131, U225, U226, U228, U125, U128 User Manual
Boston Scientific Corporation L300, L301, L321, L310, L311, L331, L200, L201, L221, L210, L211, L231, L100, L101, L121, L110, L111, L131, U225, U226, U228, U125, U128
User Manual
PHYSICIAN’S TECHNICAL MANUAL
VALITUDE™, VALITUDE™X4,
INTUA™,INVIVE
™
CARDIAC RESYNCHRONIZATION THERAPY
PACEMAKER
Model U125, U128, V272, V273, V172, V173
CAUTION: Federal law (USA)
restricts this device to sale by
or on the order of a physician
trained or experienced in
device implant and follow-up
procedures.
Table of Contents
Additional Information..................................................................................................................... 1
Device Description.......................................................................................................................... 1
Related Information ........................................................................................................................ 3
Indications and Usage .................................................................................................................... 4
Contraindications............................................................................................................................ 4
Warnings ........................................................................................................................................ 5
Precautions..................................................................................................................................... 7
Supplemental Precautionary Information ..................................................................................... 20
Post-Therapy Pulse Generator Follow Up .......................................................................... 20
Minimizing Pacemaker/S-ICD Interaction ........................................................................... 21
Transcutaneous Electrical Nerve Stimulation (TENS)......................................................... 23
Electrocautery and Radio Frequency (RF) Ablation............................................................ 24
Ionizing Radiation................................................................................................................ 26
Elevated Pressures ............................................................................................................. 27
Potential Adverse Events ............................................................................................................. 28
Mechanical Specifications ............................................................................................................ 31
Items Included in Package ........................................................................................................... 34
Symbols on Packaging ................................................................................................................. 34
Characteristics as Shipped........................................................................................................... 38
X-Ray Identifier............................................................................................................................. 39
Federal Communications Commission (FCC) .............................................................................. 41
Pulse Generator Longevity........................................................................................................... 42
Warranty Information .................................................................................................................... 46
Product Reliability......................................................................................................................... 46
Patient Counseling Information ....................................................................................................47
Patient Handbook................................................................................................................ 48
Lead Connections......................................................................................................................... 48
Implanting the Pulse Generator.................................................................................................... 52
Step A: Check Equipment ................................................................................................ 52
Step B: Interrogate and Check the Pulse Generator ........................................................ 52
Step C: Implant the Lead System..................................................................................... 53
Step D: Take Baseline Measurements ............................................................................. 54
Step E: Form the Implantation Pocket.............................................................................. 57
Step F: Connect the Leads to the Pulse Generator.......................................................... 58
Step G: Evaluate Lead Signals......................................................................................... 62
Step H: Program the Pulse Generator.............................................................................. 63
Step I: Implant the Pulse Generator ................................................................................. 64
Step J: Complete and Return the Implantation Form ....................................................... 65
Bidirectional Torque Wrench......................................................................................................... 66
Follow Up Testing ......................................................................................................................... 68
Predischarge Follow Up ...................................................................................................... 68
Routine Follow Up............................................................................................................... 68
Explantation.................................................................................................................................. 69
ADDITIONAL INFORMATION
For additional reference information, go to www.bostonscientific.com/ifu.
DEVICE DESCRIPTION
This manual contains information about the VALITUDE, INTUA, and INVIVE families of cardiac
resynchronization therapy pacemakers (CRT-Ps) (specific models are listed in "Mechanical Specifications"
on page 31).
NOTE: Specific features discussed in this manual may not apply to all models. References to names of
non-quadripolar devices also apply to the corresponding quadripolar devices. References to “ICD” include all
types of ICDs (e.g., ICD, CRT-D, S-ICD).
Therapies
These pulse generators provide a variety of therapies, including:
• Cardiac Resynchronization Therapy (CRT), which treats heart failure by resynchronizing ventricular
contractions through biventricular electrical stimulation
• Bradycardia pacing, including adaptive rate pacing, to detect and treat bradyarrhythmias
Leads
The pulse generator has independently programmable outputs and accepts one or more of the following
leads, depending on the model:
•OneIS-1
1unipolar or bipolar atrial lead
• One IS-1 unipolar or bipolar right ventricular lead
• One LV-1 unipolar or bipolar left ventricular lead
1. IS-1 refers to the international standard ISO 5841-3:2013.
1
• One IS-1 unipolar or bipolar left ventricular lead
• One compatible IS42quadripolar left ventricular lead3
The pulse generator and the leads constitute the implantable portion of the pulse generator system.
PRM System
These pulse generators can be used only with the ZOOM LATITUDE Programming System, which is the
external portion of the pulse generator system and includes:
• Model 3120 Programmer/Recorder/Monitor (PRM)
• Model 3140 ZOOM Wireless Transmitter
• Model 2869 ZOOMVIEW Software Application
• Model 6577 Accessory Telemetry Wand
You can use the PRM system to do the following:
• Interrogate the pulse generator
• Program the pulse generator to provide a variety of therapy options
• Access the pulse generator’s diagnostic features
• Perform noninvasive diagnostic testing
• Access therapy history data
• Store a 12 second trace of the ECG/EGM display from any screen
• Access an interactive Demonstration Mode or Patient Data Mode without the presence of a pulse
generator
• Print patient data including pulse generator therapy options and therapy history data
2. IS4 refers to the international standard ISO 27186:2010.
3. Compatibility with St. Jude Quartet IS4 lead has been demonstrated through chronic in-vivo animal GLP testing.
2
• Save patient data
You can program the pulse generator using two methods: automatically using Indications-Based Programming
(IBP) or manually.
RELATED INFORMATION
Refer to the lead’s instruction manual for implant information, general warnings and precautions, indications,
contraindications, and technical specifications. Read this material carefully for implant procedure instructions
specific to the chosen lead configurations.
Refer to the PRM system Operator’s Manual or ZOOM Wireless Transmitter Reference Guide for specific
information about the PRM or ZOOM Wireless Transmitter such as setup, maintenance, and handling.
LATITUDE NXT is a remote monitoring system that provides pulse generator data for clinicians. These pulse
generators are designed to be LATITUDE NXT enabled; availability varies by region.
LATITUDE NXT is available for the following devices: VALITUDE, INTUA, INVIVE.
• Physicians/Clinicians—LATITUDE NXT enables you to periodically monitor both patient and device
status remotely and automatically. The LATITUDE NXT system provides patient data that can be used
as part of the clinical evaluation of the patient.
• Patients—A key component of the system is the LATITUDE Communicator, an easy-to-use, in-home
monitoring device. The Communicator automatically reads implanted device data from a compatible
Boston Scientific pulse generator at times scheduled by the physician. The Communicator sends this
data to the LATITUDE NXT secure server through a standard analog telephone line or over a cellular data
network. The LATITUDE NXT server displays the patient data on the LATITUDE NXT Web site, which is
readily accessible over the Internet to authorized physicians and clinicians.
Refer to the LATITUDE NXT Clinician Manual for more information.
3
INTENDED AUDIENCE
This literature is intended for use by professionals trained or experienced in device implant and/or follow-up
procedures.
INDICATIONS AND USAGE
Boston Scientific cardiac resynchronization therapy pacemakers (CRT-Ps) are indicated for patients with
moderate to severe heart failure (NYHA Class III/IV) including left ventricular dysfunction (EF ≤35%) and
QRS duration ≥120 ms and remain symptomatic despite stable optimal pharmacological therapy (OPT)
for heart failure.
Atrial tracking modes are also indicated for patients who may benefit from maintenance of AV synchrony.
Adaptive-rate pacing is indicated for patients exhibiting chronotropic incompetence and who would benefitfrom
increased pacing rates concurrent with increases in physical activity.
CONTRAINDICATIONS
These Boston Scientific pulse generators have the following contraindications:
• This device is contraindicated in patients who have a separate implanted cardioverter defibrillator (ICD)
with transvenous leads.
• Unipolar pacing or use of the Respiratory Sensor with a Subcutaneous Implantable Cardioverter
Defibrillator (S-ICD) is contraindicated because it may cause inappropriate therapy or inhibition of
appropriate S-ICD therapy.
• Single-chamber atrial pacing is contraindicated in patients with impaired AV nodal conduction.
• Atrial tracking modes are contraindicated in patients with chronic refractory atrial tachyarrhythmias (atrial
fibrillation or flutter), which might trigger ventricular pacing.
• Asynchronous pacing is contraindicated in the presence (or likelihood) of competition between paced
and intrinsic rhythms.
4
WARNINGS
General
• Labeling knowledge. Read this manual thoroughly before implantation to avoid damage to the pulse
generator and/or lead. Such damage can result in patient injury or death.
• For single patient use only. Do not reuse, reprocess, or resterilize. Reuse, reprocessing, or
resterilization may compromise the structural integrity of the device and/or lead to device failure which, in
turn, may result in patient injury, illness, or death. Reuse, reprocessing, or resterilization may also create
a risk of contamination of the device and/or cause patient infection or cross-infection, including, but not
limited to, the transmission of infectious disease(s) from one patient to another. Contamination of the
device may lead to injury, illness, or death of the patient.
• Backup defibrillation protection. Always have external defibrillation equipment available during
implant and electrophysiologic testing. If not terminated in a timely fashion, an induced ventricular
tachyarrhythmia can result in the patient’s death.
• Separate pulse generator. Using multiple pulse generators could cause pulse generator interaction,
resulting in patient injury or a lack of therapy delivery. Test each system individually and in combination to
help prevent undesirable interactions ("Minimizing Pacemaker/S-ICD Interaction" on page 21).
• Safety Core operation. In response to applicable nonrecoverable or repeat fault conditions, the pulse
generator will switch irreversibly to Safety Core operation. Safety Core pacing is unipolar, which may
interact with an ICD ("Minimizing Pacemaker/S-ICD Interaction" on page 21).
Handling
• Do not kink leads. Do not kink, twist, or braid the lead with other leads as doing so could cause lead
insulation abrasion damage or conductor damage.
5
• Handling the lead without Connector Tool. For leads that require the use of a Connector Tool, use
caution handling the lead terminal when the Connector Tool is not present on the lead. Do not directly
contact the lead terminal with any surgical instruments or electrical connections such as PSA (alligator)
clips, ECG connections, forceps, hemostats, and clamps. This could damage the lead terminal, possibly
compromising the sealing integrity and result in loss of therapy or inappropriate therapy, such as a
short within the header.
• Handling the terminal while tunneling. Do not contact any other portion of the IS4–LLLL lead terminal,
other than the terminal pin, even when the lead cap is in place.
Programming and Device Operations
• Atrial tracking modes. Do not use atrial tracking modes in patients with chronic refractory atrial
tachyarrhythmias. Tracking of atrial arrhythmias could result in ventricular tachyarrhythmias.
• Atrial-only modes. Do not use atrial-only modes in patients with heart failure because such modes do
not provide CRT.
• Lead Safety Switch. Lead Safety Switch should be programmed Off for patients with an ICD. Unipolar
pacing due to Lead Safety Switch is contraindicated for patients with an ICD.
• RAAT testing. Unipolar pacing due to RAAT is contraindicated and should be programmed off for patients
with an ICD. The RAAT feature performs automatic threshold testing in a unipolar pacing configuration.
• Ventricular sensing. Left ventricular lead dislodgement to a position near the atria can result in atrial
oversensing and left ventricular pacing inhibition.
• Sensitivity settings and EMI. If programmed to a fixed atrial Sensitivity value of 0.15 mV, or a fixed
sensitivity value of 2.0 mV or less in a unipolar lead configuration in any chamber, the pulse generator
may be more susceptible to electromagnetic interference. This increased susceptibility should be taken
into consideration when determining the follow-up schedule for patients requiring such a setting.
6
Post-Implant
• Protected environments. Advise patients to seek medical guidance before entering environments that
could adversely affect the operation of the active implantable medical device, including areas protected
by a warning notice that prevents entry by patients who have a pulse generator.
• Magnetic Resonance Imaging (MRI) exposure. Do not expose a patient to MRI scanning. Strong
magnetic fields may damage the pulse generator and/or lead system, possibly resulting in injury to
or death of the patient.
•Diathermy.Do not subject a patient with an implanted pulse generator and/or lead to diathermy since
diathermy may cause fibrillation, burning of the myocardium, and irreversible damage to the pulse
generator because of induced currents.
PRECAUTIONS
Clinical Considerations
• STAT PACE. STAT PACE will initiate unipolar pacing. Unipolar pacing due to STAT PACE may cause
inappropriate therapy or inhibition of appropriate S-ICD therapy.
• Pacemaker-mediated tachycardia (PMT). Programming minimum PVARP less than retrograde V–A
conduction may increase the likelihood of a PMT.
• Rate Adaptive Pacing in Heart Failure Patients. The clinical benefit of Rate Adaptive Pacing in heart
failure patients has not been studied. Rate Adaptive Pacing should be used with medical discretion if the
patient develops an indication such as chronotropic incompetence. Patients with heart failure may have
hemodynamic compromise at rapid sensor-driven rates, and the physician may wish to program less
aggressive rate adaptive parameters in accordance with patient condition. Rate Adaptive Pacing may be
helpful for heart failure patients with coexisting bradyarrhythmic conditions. It is not recommended for
patients who exhibit only heart failure-induced chronotropic incompetency.
7
Sterilization and Storage
• If package is damaged. The blister trays and contents are sterilized with ethylene oxide gas before
final packaging. When the pulse generator and/or lead is received, it is sterile provided the container is
intact. If the packaging is wet, punctured, opened, or otherwise damaged, return the pulse generator
and/or lead to Boston Scientific.
• If device is dropped. Do not implant a device which has been dropped while outside of its intact shelf
package. Do not implant a device which has been dropped from a height of more than 24 inches (61 cm)
while within its intact shelf package. Sterility, integrity and/or function cannot be guaranteed under these
conditions and the device should be returned to Boston Scientific for inspection.
• Storage temperature and equilibration. Recommended storage temperatures are 0°C–50°C
(32°F–122°F). Allow the device to reach a proper temperature before using telemetry communication
capabilities, programming or implanting the device because temperature extremes may affect initial
device function.
•Devicestorage.Store the pulse generator in a clean area away from magnets, kits containing magnets,
and sources of EMI to avoid device damage.
•Usebydate.Implant the pulse generator and/or lead before or on the USE BY date on the package
label because this date reflects a validated shelf life. For example, if the date is January 1, do not
implant on or after January 2.
Implantation
• Expected benefits. Determine whether the expected device benefits provided by programmable options
outweigh the possibility of more rapid battery depletion.
• Evaluate patient for surgery. There may be additional factors regarding the patient’s overall health
and medical condition that, while not related to device function or purpose, could render the patient a
poor candidate for implantation of this system. Cardiac health advocacy groups may have published
guidelines that may be helpful in conducting this evaluation.
8
• Lead compatibility. Prior to implantation, confirm the lead-to-pulse generator compatibility. Using
incompatible leads and pulse generators can damage the connector and/or result in potential adverse
consequences, such as undersensing of cardiac activity or failure to deliver necessary therapy.
• Telemetry wand. Make sure a sterile telemetry wand is available should loss of ZIP telemetry occur.
Verify that the wand can easily be connected to the programmer and is within reach of the pulse generator.
• Line-powered equipment. Exercise extreme caution if testing leads using line-powered equipment
because leakage current exceeding 10 µA can induce ventricular fibrillation. Ensure that any line-powered
equipment is within specifications.
• Replacement device. Implanting a replacement device in a subcutaneous pocket that previously housed
a larger device may result in pocket air entrapment, migration, erosion, or insufficient grounding between
the device and tissue. Irrigating the pocket with sterile saline solution decreases the possibility of
pocket air entrapment and insufficient grounding. Suturing the device in place reduces the possibility of
migration and erosion.
• Do not bend the lead near the lead-header interface. Insert the lead terminal straight into the lead
port. Do not bend the lead near the lead-header interface. Improper insertion can cause insulation
or connector damage.
• Absence of a lead. The absence of a lead or plug in a lead port may affect device performance. If a
lead is not used, be sure to properly insert a plug in the unused port, and then tighten the setscrew
onto the plug.
• Dual chamber device without a functional RV lead. If a dual-chamber device is programmed to
AAI(R), ensure that a functional RV lead is present. In the absence of a functional RV lead, programming
to AAI(R) may result in undersensing or oversensing.
9
• Electrode connections. Do not insert a lead into the pulse generator connector without taking the
following precautions to ensure proper lead insertion:
• Insert the torque wrench into the preslit depression of the seal plug before inserting the lead into the
port, to release any trapped fluid or air.
• Visually verify that the setscrew is sufficiently retracted to allow insertion. Use the torque wrench
to loosen the setscrew if necessary.
• Fully insert each lead into its lead port and then tighten the setscrew onto the terminal pin.
• Do not suture directly over lead. Do not suture directly over the lead body, as this may cause structural
damage. Use the suture sleeve to secure the lead proximal to the venous entry site to prevent lead
movement.
• Diaphragmatic stimulation. Patients should be tested for diaphragmatic stimulation by pacing the LV
lead through the pulse generator at 7.5 V and adjusting the lead configurations and lead position as
necessary. PSA testing at higher outputs (e.g., 10.0 V) may also be considered to better characterize
stimulation margins. The probability of diaphragmatic stimulation increases when a pacing system
includes an LV lead because of this lead’s proximity to the phrenic nerve.
Device Programming
• Device communication. Use only the designated PRM and software application to communicate
with this pulse generator.
• STAT PACE settings. When a pulse generator is programmed to STAT PACE settings, it will continue to
pace at the high-energy STAT PACE values if it is not reprogrammed. The use of STAT PACE parameters
will likely decrease device longevity.
10
• Biventricular pacing therapy. This device is intended to provide biventricular pacing therapy.
Programming the device to provide RV-only pacing, or programming the RV pace amplitude below the
pacing threshold (resulting in LV-only pacing), is not intended for the treatment of heart failure. The
clinical effects of LV-only or RV-only pacing for the treatment of heart failure have not been established.
• Pacing and sensing margins. Consider lead maturation in your choice of Pacing Amplitude, pacing
Pulse Width, and Sensitivity settings.
• An acute Pacing Threshold greater than 1.5 V or a chronic Pacing Threshold greater than 3 V can
result in loss of capture because thresholds may increase over time.
• An R-Wave Amplitude less than 5 mV or a P-Wave Amplitude less than 2 mV can result in
undersensing because the sensed amplitude may decrease after implantation.
• Pacing Lead Impedance should be greater than the programmed Low Impedance Limit and less
than 2000 Ω(or the programmed High Impedance Limit).
• Lead impedance values and Lead Safety Switch. If properly functioning leads with stable measured
impedance values near the programmed impedance limits are used, consider programming Lead
Safety Switch Off or changing the impedance limits to avoid undesirable switching to a Unipolar Lead
Configuration.
• Proper programming of the lead configuration. If the Lead Configuration is programmed to Bipolar
when a unipolar lead is implanted, pacing will not occur.
• Programming for supraventricular tachyarrhythmias (SVTs). Determine if the device and
programmable options are appropriate for patients with SVTs because SVTs can initiate unwanted
device therapy.
• AV Delay. To ensure a high percentage of biventricular pacing, the programmed AV Delay setting
must be less than the patient’s intrinsic PR interval.
• Adaptive-rate pacing. Rate Adaptive Pacing should be used with care in patients who are unable to
tolerate increased pacing rates.
11
• Ventricular refractory periods (VRPs) in adaptive-rate pacing. Adaptive-rate pacing is not limited by
refractory periods. A long refractory period programmed in combination with a high MSR can result in
asynchronous pacing during refractory periods since the combination can cause a very small sensing
window or none at all. Use Dynamic AV Delay or Dynamic PVARP to optimize sensing windows. If you
are programming a fixed AV Delay, consider the sensing outcomes.
• MTR/MSR programming. The pulse generator’s MTR and MSR should be programmed to a rate lower
than a concomitant S-ICD’s lowest tachycardia detection zone.
• Atrial Tachy Response (ATR). ATR should be programmed to On if the patient has a history of atrial
tachyarrhythmias. The delivery of CRT is compromised because AV synchrony is disrupted if the ATR
mode switch occurs.
• Threshold test. During a manual LV Threshold test, RV Backup Pacing is unavailable.
• Left ventricular pacing only. The clinical effect of LV pacing alone for heart failure patients has not
been studied.
• Atrial oversensing. Take care to ensure that artifacts from the ventricles are not present on the atrial
channel, or atrial oversensing may result. If ventricular artifacts are present in the atrial channel, the
atrial lead may need to be repositioned to minimize its interaction.
• ATR entry count. Exercise care when programming the Entry Count to low values in conjunction with
a short ATR Duration. This combination allows mode switching with very few fast atrial beats. For
example, if the Entry Count was programmed to 2 and the ATR Duration to 0, ATR mode switching could
occur on 2 fast atrial intervals. In these instances, a short series of premature atrial events could cause
the device to mode switch.
• ATR exit count. Exercise care when programming the Exit Count to low values. For example, if the
Exit Count was programmed to 2, a few cycles of atrial undersensing could cause termination of mode
switching.
12
• Proper programming without an atrial lead. If an atrial lead is not implanted (port is plugged instead),
or an atrial lead is abandoned but remains connected to the header, device programming should be
consistent with the number and type of leads actually in use.
• Atrial sensing programmed to Off. When atrial sensing is programmed to Off in a DDI(R) or DDD(R)
mode, any atrial pacing that occurs will be asynchronous. Additionally, features that require atrial sensing
may not function as expected.
• High atrial rates. Sensing high atrial rates may impact device longevity. Therefore, the Atrial Sense
lead configuration will be seeded to Off when programming from an atrial sensing mode to a non-atrial
sensing mode.
• Cross-chamber artifacts. Sensitivity adjustments associated with Smart Blanking may not be sufficient
to inhibit detection of cross-chamber artifacts if the cross-chamber artifacts are too large. Consider other
factors that impact the size/amplitude of cross-chamber artifacts including lead-placement, pacing output,
and programmed Sensitivity settings.
• Sensor signal artifacts. If Respiratory Sensor signal artifacts are observed on EGMs, and the leads
are otherwise shown to be performing appropriately, consider programming the sensor to Off to prevent
oversensing.
• Single pass VDD leads. When a single pass VDD lead is used with a dual-chamber device, the atrial
electrodes may not be in contact with the atrial wall. In this case, the measured depolarization signal has
a relatively low Amplitude and could require a more sensitive setting.
• Left ventricular lead configuration. Proper programming of the LV coronary venous Lead Configuration
is essential for proper LV lead function. Program the Lead Configuration in accordance with the number
of electrodes on the LV lead; otherwise, erratic LV sensing, loss of LV pacing, or ineffective LV pacing
might occur.
• Quadripolar pacing configuration. When an LVRing4>>RV pacing configuration is programmed with
an IS4-LLLL lead, the LV tip may be used as the anode rather than the RV ring. When programming to
this configuration, evaluate the pacing threshold and ensure no extracardiac stimulation is present.
13
• Left Ventricular Protection Period (LVPP). Use of a long LVPP reduces the maximum LV pacing
rate and may inhibit CRT at higher pacing rates.
• Sensing adjustment. Following any Sensitivity parameter adjustment or any modification of the sensing
lead, always verify appropriate sensing. Programming Sensitivity to the highest value (lowest sensitivity)
may result in undersensing of cardiac activity. Likewise, programming to the lowest value (highest
sensitivity) may result in oversensing of non-cardiac signals.
• Sensitivity in unipolar lead configuration. The amplitude and prevalence of myopotential noise is
increased in unipolar lead configurations, as compared to bipolar lead configurations. For patients with a
unipolar lead configuration and myopotential oversensing during activity involving the pectoral muscles,
the programming of Fixed Sensitivity is recommended.
• Use of Patient Triggered Monitor. Use care when using Patient Triggered Monitor, because the
following conditions will exist while it is enabled:
• All other magnet features, including asynchronous pacing, are disabled. The Magnet feature will
not indicate magnet position.
• Device longevity is impacted. To help reduce the longevity impact, PTM only allows storage of one
episode, and PTM is automatically disabled after 60 days if data storage was never triggered.
• Once the EGM is stored (or 60 days elapses), PTM is disabled and the device Magnet Response
automatically will be set to Pace Async. However, if a magnet is used, the pulse generator will
not revert to asynchronous operation until the magnet is removed for 3 seconds and placed on
the device again.
14
Environmental and Medical Therapy Hazards
• Avoid electromagnetic interference (EMI). Advise patients to avoid sources of EMI. The pulse
generator may inhibit pacing due to oversensing, or may switch to asynchronous pacing at the
programmed pacing rate or at the magnet rate in the presence of EMI.
Moving away from the source of the EMI or turning off the source usually allows the pulse generator
to return to normal operation.
Examples of potential EMI sources are:
• Electrical power sources, arc welding or resistance welding equipment, and robotic jacks
• High voltage power distribution lines
• Electrical smelting furnaces
• Large RF transmitters such as radar
• Radio transmitters, including those used to control toys
• Electronic surveillance (antitheft) devices
• An alternator on a car that is running
• Medical treatments and diagnostic tests in which an electrical current is passed through the body,
such as TENS, electrocautery, electrolysis/thermolysis, electrodiagnostic testing, electromyography,
or nerve conduction studies
• Any externally applied device that uses an automatic lead detection alarm system (e.g., an EKG
machine)
Hospital and Medical Environments
• Mechanical ventilators. During mechanical ventilation, respiration-based trending may be misleading;
therefore, the Respiratory Sensor should be programmed to Off.
15
• Conducted electrical current. Any medical equipment, treatment, therapy, or diagnostic test that
introduces electrical current into the patient has the potential to interfere with pulse generator function.
• External patient monitors (e.g., respiratory monitors, surface ECG monitors, hemodynamic
monitors) may interfere with the pulse generator’s impedance-based diagnostics (e.g., Respiratory
Rate trend). To resolve suspected interactions with Respiratory Sensor-based diagnostics,
deactivate the pulse generator’s Respiratory Sensor by programming it to Off.
• Medical therapies, treatments, and diagnostic tests that use conducted electrical current (e.g.,
TENS, electrocautery, electrolysis/thermolysis, electrodiagnostic testing, electromyography, or
nerve conduction studies) may interfere with or damage the pulse generator. Program the device
to Electrocautery Protection Mode prior to the treatment, and monitor device performance during
the treatment. After the treatment, verify pulse generator function ("Post-Therapy Pulse Generator
Follow Up" on page 20).
•Internaldefibrillation. Do not use internal defibrillation paddles or catheters unless the pulse generator
is disconnected from the leads because the leads may shunt energy. This could result in injury to the
patient and damage to the implanted system.
16
• External defibrillation. Itcantakeupto15secondsforsensingto recover after an external shock is
delivered. In non-emergency situations, for pacemaker dependent patients, consider programming the
pulse generator to an asynchronous pacing mode and programming the Respiratory Sensor to Off prior to
performing external cardioversion or defibrillation.
External defibrillation or cardioversion can damage the pulse generator. To help prevent damage to the
pulse generator, consider the following:
• Avoid placing a pad (or paddle) directly over the pulse generator. Position the pads (or paddles)
as far from the pulse generator as possible.
• Position the pads (or paddles) in a posterior-anterior orientation when the device is implanted in
the right pectoral region or an anterior-apex orientation when the device is implanted in the left
pectoral region.
• Set energy output of external defibrillation equipment as low as clinically acceptable.
Following external cardioversion or defibrillation, verify pulse generator function ("Post-Therapy Pulse
Generator Follow Up" on page 20).
• Lithotripsy. Extracorporeal shock wave lithotripsy (ESWL) may cause electromagnetic interference with
or damage to the pulse generator. If ESWL is medically necessary, consider the following to minimize the
potential for encountering interaction:
• Focus the ESWL beam at least 15 cm (6 in) away from the pulse generator.
• Depending on the pacing needs of the patient, program the Brady Mode to a non-rate-responsive
VVI or VOO mode.
• Ultrasound energy. Therapeutic ultrasound (e.g., lithotripsy) energy may damage the pulse generator. If
therapeutic ultrasound energy must be used, avoid focusing near the pulse generator site. Diagnostic
ultrasound (e.g., echocardiography) is not known to be harmful to the pulse generator.
17
• Electrical interference. Electrical interference or “noise” from devices such as electrocautery and
monitoring equipment may interfere with establishing or maintaining telemetry for interrogating or
programming the device. In the presence of such interference, move the programmer away from
electrical devices, and ensure that the wand cord and cables are not crossing one another. If telemetry is
cancelled as a result of interference, the device should be re-interrogated prior to evaluating information
from pulse generator memory.
• Radio frequency (RF) interference. RF signals from devices that operate at frequencies near that of
the pulse generator may interrupt ZIP telemetry while interrogating or programming the pulse generator.
This RF interference can be reduced by increasing the distance between the interfering device and
the PRM and pulse generator. Examples of devices that may cause interference in the 916.5 MHz
frequency band include:
• Cordless phone handsets or base stations
• Certain patient monitoring systems
• Central line guidewire insertion. Use caution when inserting guidewires for placement of other types
of central venous catheter systems such as PIC lines or Hickman catheters in locations where pulse
generator leads may be encountered. Insertion of such guidewires into veins containing leads could
result in the leads being damaged or dislodged.
Home and Occupational Environments
• Home appliances. Home appliances that are in good working order and properly grounded do not
usually produce enough EMI to interfere with pulse generator operation. There have been reports of
pulse generator disturbances caused by electric hand tools or electric razors used directly over the
pulse generator implant site.
18
• Magnetic fields. Advise patients that extended exposure to strong (greater than 10 gauss or 1 mTesla)
magnetic fields may trigger the magnet feature. Examples of magnetic sources include:
• Industrial transformers and motors
• MRI scanners
• Large stereo speakers
• Telephone receivers if held within 1.27 cm (0.5 inches) of the pulse generator
• Magnetic wands such as those used for airport security and in the Bingo game
• Electronic Article Surveillance (EAS) and Security Systems. Advise patients to avoid lingering near
or leaning against antitheft and security gates or tag readers that include radio frequency identification
(RFID) equipment. These systems may be found at the entrances and exits of stores, in public libraries,
and in point-of-entry access control systems. These systems are unlikely to affect cardiac device function
when patients walk through them at a normal pace. If the patient is near an electronic antitheft, security,
or entry control system and experiences symptoms, they should promptly move away from nearby
equipment and inform their doctor.
• Cellular phones. Advise patients to hold cellular phones to the ear opposite the side of the implanted
device. Patients should not carry a cellular phone that is turned on in a breast pocket or on a belt within
15 cm (6 inches) of the implanted device since some cellular phones may cause the pulse generator to
deliver inappropriate therapy or inhibit appropriate therapy.
Follow-up Testing
• Pacing threshold testing. If the patient’s condition or drug regimen has changed or device parameters
have been reprogrammed, consider performing a pacing threshold test to confirm adequate margins
for pace capture.
19
• Follow-up considerations for patients leaving the country. Pulse generator follow-up considerations
should be made in advance for patients who plan to travel or relocate post-implant to a country other than
the country in which their device was implanted. Regulatory approval status for devices and associated
programmer software configurations varies by country; certain countries may not have approval or
capability to follow specific products.
Contact Boston Scientific, using the information on the back cover, for help in determining feasibility of
device follow-up in the patient’s destination country.
Explant and Disposal
• Incineration. Be sure that the pulse generator is removed before cremation. Cremation and incineration
temperatures might cause the pulse generator to explode.
• Device handling. Before explanting, cleaning, or shipping the device, complete the following actions to
prevent overwriting of important therapy history data:
• Program the pulse generator Brady Mode to Off
• Program Ventricular Tachy EGM Storage to Off
Clean and disinfect the device using standard biohazard handling techniques.
SUPPLEMENTAL PRECAUTIONARY INFORMATION
Post-Therapy Pulse Generator Follow Up
Following any surgery or medical procedure with the potential to affect pulse generator function, you should
perform a thorough follow-up, which may include the following:
• Interrogating the pulse generator with a programmer
• Reviewing clinical events and fault codes
• Reviewing the Arrhythmia Logbook, including stored electrograms (EGMs)
20
• Reviewing real-time EGMs
• Testing the leads (threshold, amplitude, and impedance)
• Reviewing respiratory sensor-based diagnostics
• Verifying battery status
• Programming any permanent brady parameter to a new value and then reprogramming it back to the
desired value
• Saving all patient data
• Verifying the appropriate final programming prior to allowing the patient to leave the clinic
Minimizing Pacemaker/S-ICD Interaction
These pulse generators are compatible for use with a Subcutaneous Implantable Cardioverter Defibrillator
(S-ICD) when implanted with bipolar leads and programmed to a bipolar pacing configuration.
A pacemaker can interact with an S-ICD in the following ways:
• If during a tachyarrhythmia the pacemaker is not inhibited and the pacing pulses are detected by the
rate-sensing circuit of the S-ICD, the S-ICD could interpret the pacing pulses as a normal rhythm. The
S-ICD would not detect the arrhythmia and therefore would not deliver therapy.
• Pacemaker failure to sense or to capture could result in two independent signals (intrinsic and pacing
pulses) to the S-ICD. This could cause the S-ICD’s rate measurement to be faster than the actual heart
rate. As a result, the S-ICD could deliver unnecessary therapy.
• If the S-ICD counts both the pacing pulses and the resultant ventricular depolarizations, the S-ICD’s rate
measurement would be faster than the actual heart rate. This could result in unnecessary S-ICD therapy.
21
In Safety Mode, these pulse generators use a unipolar pacing and sensing configuration. Safety Mode is
compatible for use with an S-ICD because the configured parameters mitigate the potential pacemaker and
S-ICD interactions as follows:
• Sensing is AGC at 0.25 mV. The AGC sensing is able to effectively sense an intrinsic rhythm faster
than the Safety Mode LRL of 72.5 bpm. As a result, pacing is inhibited and does not interfere with
S-ICD tachyarrhythmia detection.
• When pacing is necessary, the elevated output of 5.0 V and 1.0 ms reduces the risk of not capturing.
• If double detection of the pace pulse and the resulting depolarization were to occur, it would not result
in unnecessary S-ICD therapy provided the S-ICD tachy threshold is more than twice the Safety Mode
LRL (145 ppm).
To help minimize device-device interaction of a bipolar pacemaker when an S-ICD is already implanted, follow
these precautionary measures:
• Use bipolar pacing leads with close electrode spacing in both chambers. Significant spacing between
electrodes may increase the likelihood that the S-ICD will detect the pacing pulses.
• Consider programming the pacemaker to (1) the lowest Amplitude allowable for safe capture in the
chronic state, (2) the maximum Sensitivity (the lowest programmable level) while maintaining an adequate
safety margin, and (3) the minimum cardiac rate acceptable for the patient.
In addition to the above steps, perform the following testing to assess device-device interaction:
• Use the S-ICD features, such as markers, real-time electrograms (EGMs), and/or beeping tones, to help
evaluate potential for pacemaker interaction due to oversensing by the S-ICD.
NOTE: If a single chamber pacemaker is implanted with an atrial lead, perform testing in both unipolar and
bipolar configurations.
22
• Ventricular fibrillation and all of the patient’s ventricular tachycardias should be induced while the S-ICD
is activated and the pacemaker is programmed to an asynchronous mode at maximum Amplitude and
Pulse Width. This should provide the greatest opportunity for inhibition of arrhythmia detection due to
detection of pacemaker pacing pulses. The pacemaker leads might have to be repositioned to eliminate
detection of the pacing pulses by the S-ICD.
Temporarily deactivate the patient’s S-ICD when (1) evaluating pacing and sensing thresholds, (2) when using
an external temporary pacemaker during implant, and (3) when reprogramming an implanted pacemaker.
Following any S-ICD discharge, reinterrogate the pacemaker to ensure that the S-ICD shock did not damage
the pacemaker.
If implanting an S-ICD in a patient who has a pacemaker already implanted, refer to the S-ICD manual for
implantation considerations.
Refer to the Warnings section for additional information regarding pacemaker and S-ICD interactions.
Transcutaneous Electrical Nerve Stimulation (TENS)
CAUTION: TENS involves passing electrical current through the body, and may interfere with pulse generator
function. If TENS is medically necessary, evaluate the TENS therapy settings for compatibility with the pulse
generator. The following guidelines may reduce the likelihood of interaction:
• Place the TENS electrodes as close together and as far away from the pulse generator and leads
as possible.
• Use the lowest clinically-appropriate TENS energy output.
• Consider cardiac monitoring during TENS use, especially for pacemaker-dependent patients.
Additional steps can be taken to help reduce interference during in-clinic use of TENS:
• If interference is suspected during in-clinic use, turn off the TENS unit.
• If pacing inhibition is observed, use a magnet to pace asynchronously.
23
• Do not change TENS settings until you have verified that the new settings do not interfere with pulse
generator function.
If TENS is medically necessary outside the clinical setting (at-home use), provide patients with the following
instructions:
• Do not change the TENS settings or electrode positions unless instructed to do so.
• End each TENS session by turning off the unit before removing the electrodes.
• If the patient experiences symptoms of lightheadedness, dizziness, or loss of consciousness during
TENS use, they should turn off the TENS unit and contact their physician.
Follow these steps to use the PRM to evaluate pulse generator function during TENS use:
1. Observe real-time EGMs at prescribed TENS output settings, noting when appropriate sensing or
interference occurs.
NOTE: Patient triggered monitoring may be used as an additional method to confirm device function during
TENS use.
2. When finished, turn off the TENS unit.
You should also perform a thorough follow-up evaluation of the pulse generator following TENS, to ensure that
device function has not been compromised ("Post-Therapy Pulse Generator Follow Up" on page 20).
For additional information, contact Boston Scientific using the information on the back cover.
Electrocautery and Radio Frequency (RF) Ablation
CAUTION: Electrocautery and RF ablation may induce ventricular arrhythmias and/or fibrillation, and may
cause asynchronous pacing, inhibition of pacing, and/or a reduction in pulse generator pacing output possibly
leading to loss of capture. RF ablation may also cause ventricular pacing up to the MTR and/or changes in
pacing thresholds. Additionally, exercise caution when performing any other type of cardiac ablation procedure
in patients with implanted devices.
24
If electrocautery or RF ablation is medically necessary, observe the following to minimize risk to the patient
and device:
• Depending on the pacing needs of the patient, enable the Electrocautery Protection Mode, program
to an asynchronous pacing mode, or use a magnet to switch to asynchronous pacing. An option for
patients with intrinsic rhythm is to program the Brady Mode to VVI at a rate below the intrinsic rate
to avoid competitive pacing.
• Have temporary pacing and external defibrillation equipment available.
• Avoid direct contact between the electrocautery equipment or ablation catheters and the pulse generator
and leads. RF ablation close to the lead electrode may damage the lead-tissue interface.
• Keep the path of the electrical current as far away as possible from the pulse generator and leads.
• If RF ablation and/or electrocautery is performed on tissue near the device or leads, monitor pre- and
post-measurements for sensing and pacing thresholds and impedances to determine the integrity and
stability of the system.
• For electrocautery, use a bipolar electrocautery system where possible and use short, intermittent, and
irregular bursts at the lowest feasible energy levels.
• RF ablation equipment may cause telemetry interference between the pulse generator and PRM. If
device programming changes are necessary during an RF ablation procedure, turn off the RF ablation
equipment before interrogation.
When the procedure is finished, cancel the Electrocautery Protection Mode in order to reactivate the previously
programmed therapy modes.
25
Ionizing Radiation
CAUTION: It is not possible to specify a safe radiation dosage or guarantee proper pulse generator function
following exposure to ionizing radiation. Multiple factors collectively determine the impact of radiation therapy
on an implanted pulse generator, including proximity of the pulse generator to the radiation beam, type and
energy level of the radiation beam, dose rate, total dose delivered over the life of the pulse generator, and
shielding of the pulse generator. The impact of ionizing radiation will also vary from one pulse generator to
another and may range from no changes in function to a loss of pacing.
Sources of ionizing radiation vary significantly in their potential impact on an implanted pulse generator.
Several therapeutic radiation sources are capable of interfering with or damaging an implanted pulse generator,
including those used for the treatment of cancer, such as radioactive cobalt, linear accelerators, radioactive
seeds, and betatrons.
Prior to a course of therapeutic radiation treatment, the patient’s radiation oncologist and cardiologist or
electrophysiologist should consider all patient management options, including increased follow-up and device
replacement. Other considerations include:
• Maximizing shielding of the pulse generator within the treatment field
• Determining the appropriate level of patient monitoring during treatment
Evaluate pulse generator operation during and following the course of radiation treatment to exercise as much
device functionality as possible ("Post-Therapy Pulse Generator Follow Up" on page 20). The extent, timing,
and frequency of this evaluation relative to the radiation therapy regimen are dependent upon current patient
health, and therefore should be determined by the attending cardiologist or electrophysiologist.
Many pulse generator diagnostics are performed automatically once per hour, so pulse generator evaluation
should not be concluded until pulse generator diagnostics have been updated and reviewed (at least one hour
after radiation exposure). The effects of radiation exposure on the implanted pulse generator may remain
undetected until some time following exposure. For this reason, continue to monitor pulse generator function
closely and use caution when programming a feature in the weeks or months following radiation therapy.
26
Elevated Pressures
The International Standards Organization (ISO) has not approved a standardized pressure test for implantable
pulse generators that experience hyperbaric oxygen therapy (HBOT) or SCUBA diving. However, Boston
Scientific developed a test protocol to evaluate device performance upon exposure to elevated atmospheric
pressures. The following summary of pressure testing should not be viewed as and is not an endorsement of
HBOT or SCUBA diving.
CAUTION: Elevated pressures due to HBOT or SCUBA diving may damage the pulse generator. During
laboratory testing, all pulse generators in the test sample functioned as designed when exposed to more than
1000 cycles at a pressure up to 5.0 ATA. Laboratory testing did not characterize the impact of elevated pressure
on pulse generator performance or physiological response while implanted in a human body.
Pressure for each test cycle began at ambient/room pressure, increased to a high pressure level, and then
returned to ambient pressure. Although dwell time (the amount of time under elevated pressure) may have an
impact on human physiology, testing indicated it did not impact pulse generator performance. Pressure value
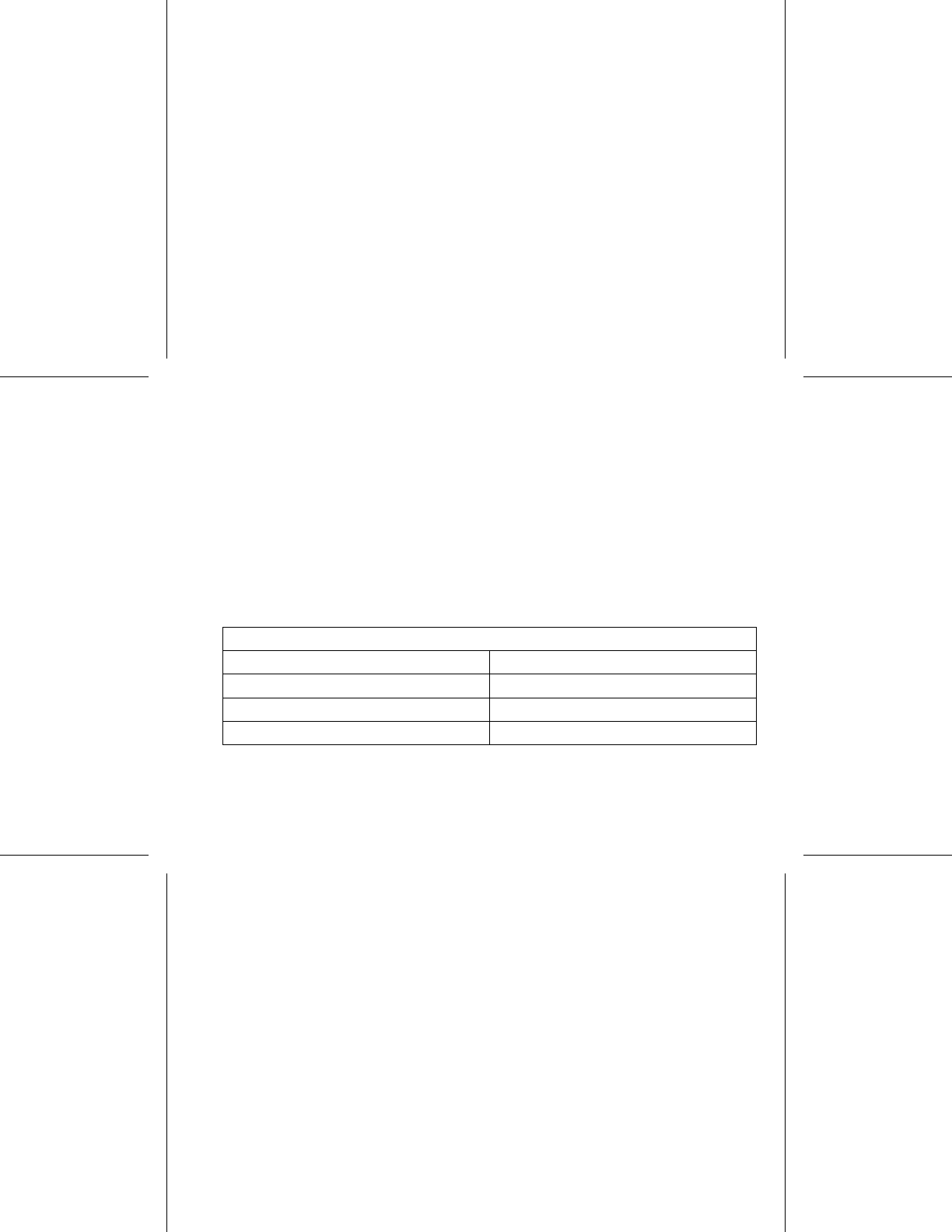
equivalencies are provided below (Table 1 on page 27).
Table 1. Pressure Value Equivalencies
Pressure value equivalencies
Atmospheres Absolute 5.0 ATA
Sea water deptha40 m (130 ft)
Pressure, absolute 72.8 psia
Pressure, gaugeb58.1 psig
27
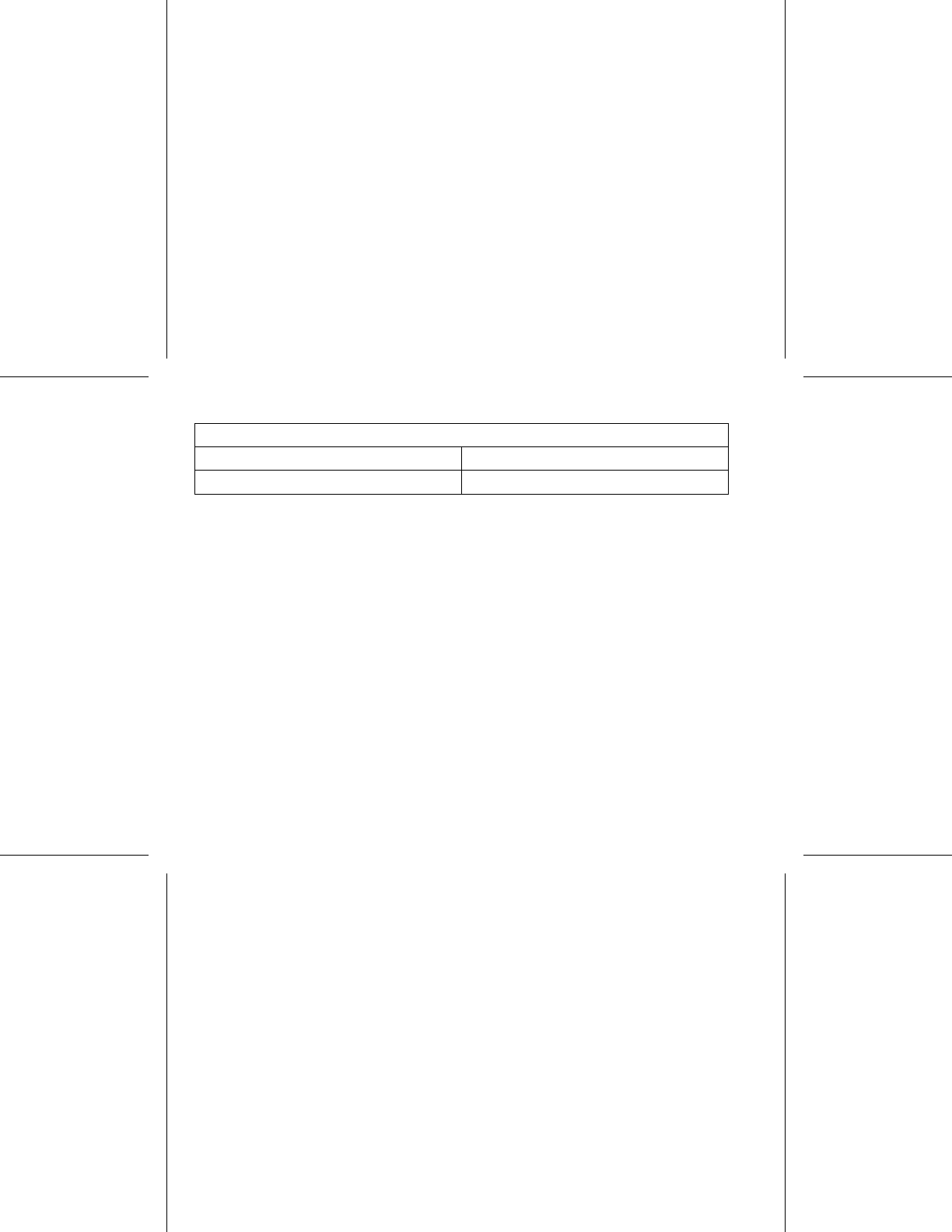
Table 1. Pressure Value Equivalencies (continued)
Pressure value equivalencies
Bar 5.0
kPa Absolute 500
a. All pressures were derived assuming sea water density of 1030 kg/m3.
b. Pressure as read on a gauge or dial (psia = psig + 14.7 psi).
Prior to SCUBA diving or starting an HBOT program, the patient’s attending cardiologist or electrophysiologist
should be consulted to fully understand the potential consequences relative to the patient’s specifichealth
condition. A Dive Medicine Specialist may also be consulted prior to SCUBA diving.
More frequent device follow-up may be warranted in conjunction with HBOT or SCUBA diving. Evaluate pulse
generator operation following high pressure exposure ("Post-Therapy Pulse Generator Follow Up" on page 20).
The extent, timing, and frequency of this evaluation relative to the high pressure exposure are dependent upon
current patient health, and should be determined by the attending cardiologist or electrophysiologist.
If you have additional questions, or would like more detail regarding the test protocol or test results specificto
HBOT or SCUBA diving, contact Boston Scientific using the information on the back cover.
POTENTIAL ADVERSE EVENTS
Based on the literature and on pulse generator and/or lead implant experience, the following alphabetical list
includes the possible adverse events associated with implantation of products described in this literature:
• Air embolism
• Allergic reaction
• Bleeding
• Bradycardia
28
• Cardiac tamponade
• Chronic nerve damage
• Component failure
• Conductor coil fracture
•Death
• Electrolyte imbalance/dehydration
• Elevated thresholds
•Erosion
• Excessive fibrotic tissue growth
• Extracardiac stimulation (muscle/nerve stimulation)
• Fluid accumulation
• Foreign body rejection phenomena
• Formation of hematomas or seromas
• Heart block
• Inability to pace
• Inappropriate pacing
• Incisional pain
• Incomplete lead connection with pulse generator
• Infection including endocarditis
• Lead dislodgment
• Lead fracture
• Lead insulation breakage or abrasion
• Lead perforation
29
• Lead tip deformation and/or breakage
• Local tissue reaction
• Loss of capture
• Myocardial infarction (MI)
• Myocardial necrosis
• Myocardial trauma (e.g., tissue damage, valve damage)
• Myopotential sensing
• Oversensing/undersensing
• Pacemaker-mediated tachycardia (PMT)
• Pericardial rub, effusion
• Pneumothorax
• Pulse generator migration
• Shunting current during defibrillation with internal or external paddles
• Syncope
• Tachyarrhythmias, which include acceleration of arrhythmias and early, recurrent atrial fibrillation
• Thrombosis/thromboemboli
• Valve damage
• Vasovagal response
• Venous occlusion
• Venous trauma (e.g., perforation, dissection, erosion)
• Worsening heart failure
Patients may develop psychological intolerance to a pulse generator system and may experience the following:
• Dependency
30
•Depression
• Fear of premature battery depletion
• Fear of device malfunction
Additionally, potential adverse events associated with the implantation of a coronary venous lead system
include:
• Allergic reaction to contrast media
• Breakage/failure of implant instruments
• Prolonged exposure to fluoroscopic radiation
• Renal failure from contrast media used to visualize coronary veins
MECHANICAL SPECIFICATIONS
The following mechanical specifications and material specifications apply to VALITUDE devices.
All VALITUDE models have a case electrode surface area of 35.05 cm² and all VALITUDE X4 models have
a case electrode surface area of 34.58 cm². Usable battery capacity is 1.6 Ah and residual usable battery
capacity at Explant is 0.10 Ah.
Mechanical specifications specific to each model are listed below.
31
Table 2. Mechanical Specifications - VALITUDE CRT-Ps
Model Dimensions
WxHxD(cm)
Mass (g) Volume (cm3) Connector Type
U125 4.45 x 6.13 x 0.75 30.6 16.2 RA:IS-1;RV:IS-1;
LV: IS-1
U128 4.45 x 6.17 x 0.75 33.0 17.6 RA:IS-1;RV:IS-1;
LV: IS4
VALITUDE devices include ZIP telemetry operating with a transmit frequency of 402 to 405 MHz.
Material specifications are shown below:
• Case: hermetically sealed titanium
• Header: implantation-grade polymer
• Power Supply (VALITUDE): lithium-carbon monofluoride cell; Boston Scientific; 402294
The following mechanical specifications and material specifications apply to INTUA and INVIVE devices.
All INTUA and INVIVE models have a case electrode surface area of 35.98 cm². Usable battery capacity is
1.45 Ah and residual usable battery capacity at Explant is 0.09 Ah.
Mechanical specifications specific to each model are listed below.
32
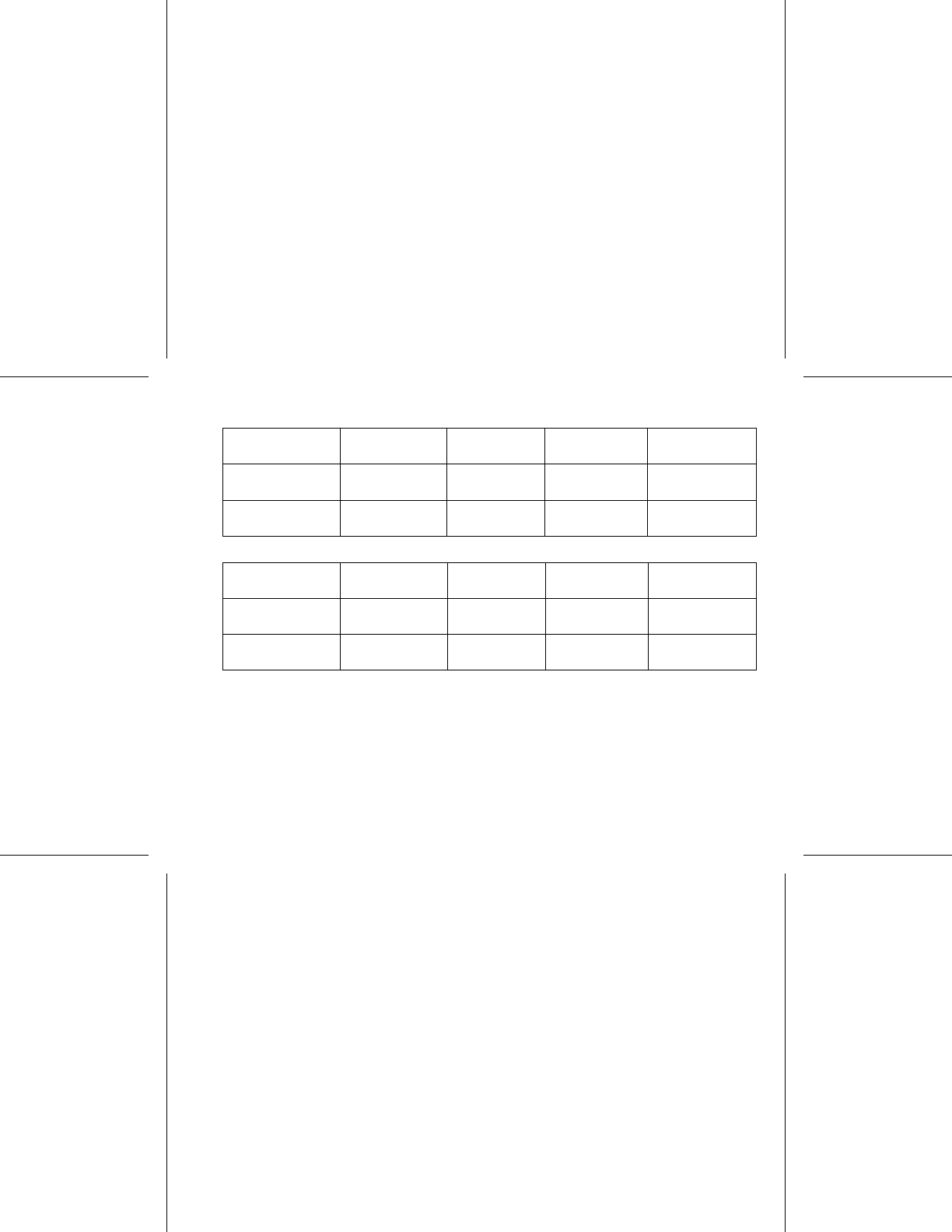
Table 3. Mechanical Specifications - INTUA CRT-Ps
Model Dimensions
WxHxD(cm)
Mass (g) Volume (cm3) Connector Type
V272 4.45 x 6.10 x 0.75 34.0 15.0 RA: IS-1, RV: IS-1,
LV: LV-1
V273 4.45 x 6.10 x 0.75 34.0 15.0 RA: IS-1, RV: IS-1,
LV: IS-1
Table 4. Mechanical Specifications - INVIVE CRT-Ps
Model Dimensions
WxHxD(cm)
Mass (g) Volume (cm3) Connector Type
V172 4.45 x 6.10 x 0.75 34.0 15.0 RA:IS-1,RV:IS-1,
LV: LV-1
V173 4.45 x 6.10 x 0.75 34.0 15.0 RA:IS-1,RV:IS-1,
LV: IS-1
INTUA and INVIVE devices include ZIP telemetry operating with a transmit frequency of 916.5 MHz.
Material specifications are shown below:
• Case: hermetically sealed titanium
• Header: implantation-grade polymer
• Power Supply (INTUA and INVIVE): lithium-manganese dioxide cell; Boston Scientific; 402125
33
ITEMS INCLUDED IN PACKAGE
The following items are included with the pulse generator:
• One torque wrench
• Product literature
NOTE: Accessories (e.g., wrenches) are intended for one-time use only. They should not be resterilized
or reused.
SYMBOLS ON PACKAGING
The following symbols may be used on packaging and labeling (Table 5 on page 34):
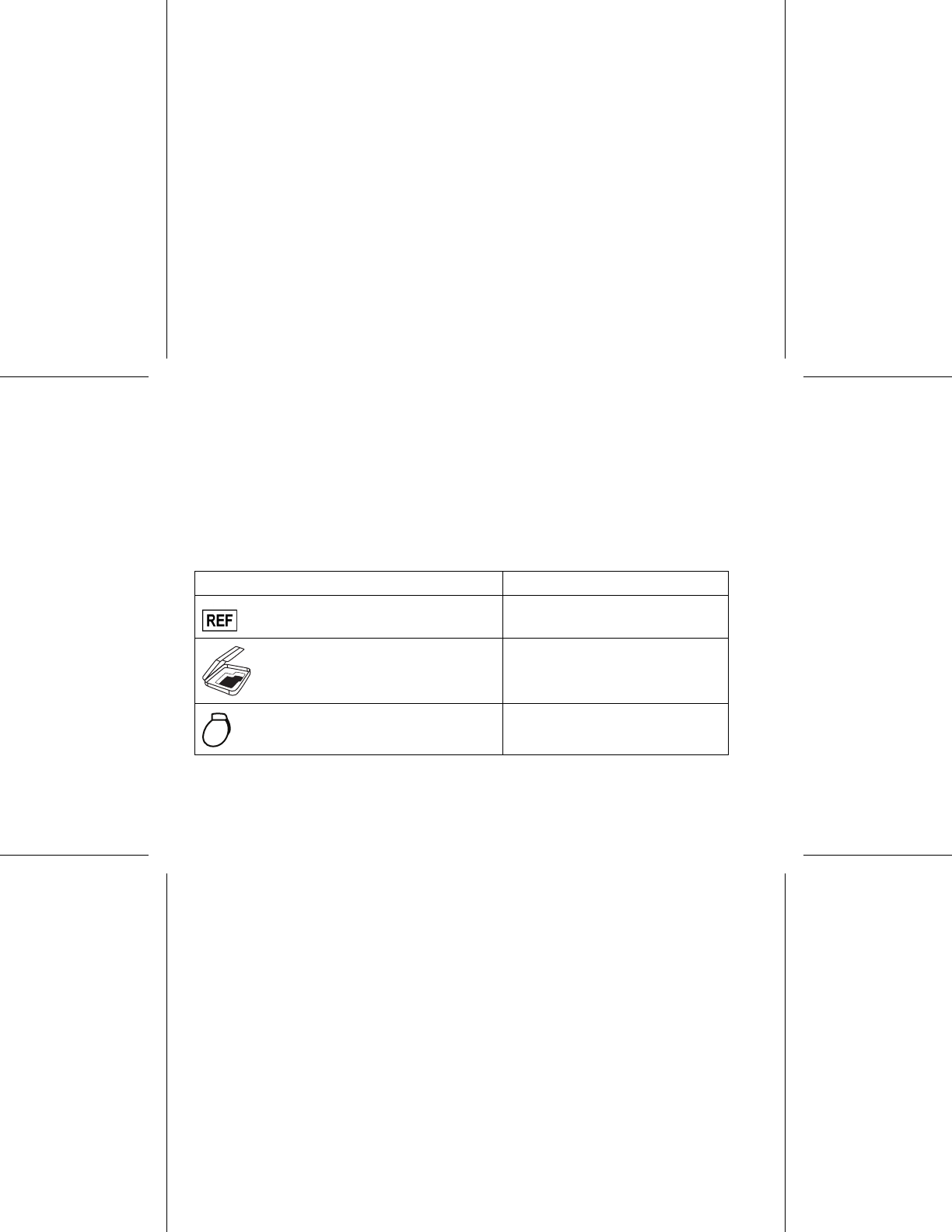
Table 5. Symbols on packaging
Symbol Description
Reference number
Package contents
Pulse generator
34
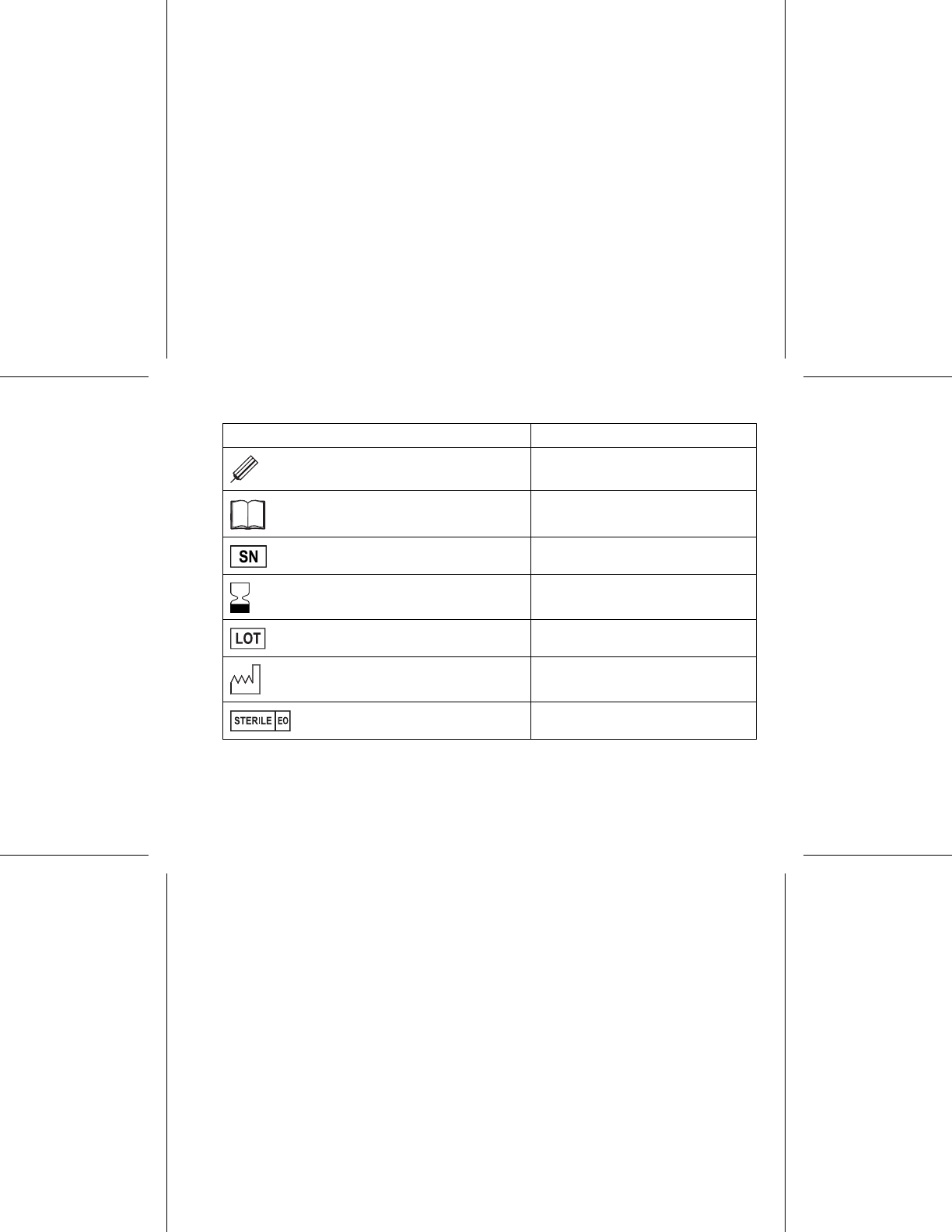
Table 5. Symbols on packaging (continued)
Symbol Description
Torque wrench
Literature enclosed
Serial number
Use by
Lot number
Date of manufacture
Sterilized using ethylene oxide
35