Bravo Marine Heating System Bh 0133 Users Manual
2015-02-02
: Bravo Bravo-Bravo-Marine-Heating-System-Bh-0133-Users-Manual-484987 bravo-bravo-marine-heating-system-bh-0133-users-manual-484987 bravo pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 74

Live life well.
2008
Provider Manual
Texas
BH-0133 Revised January 2008
1
TABLE OF CONTENTS
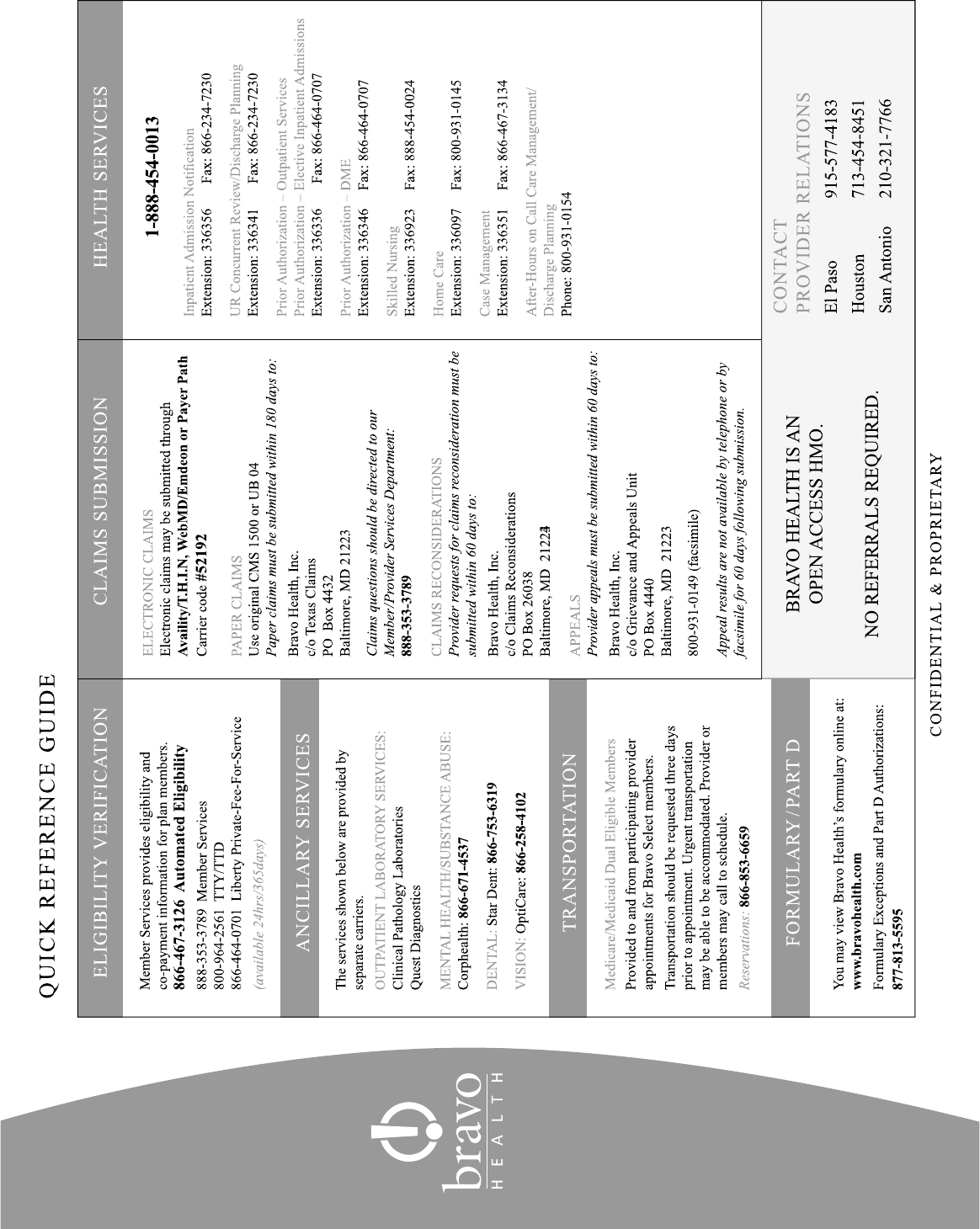
QUICK REFERENCE GUIDE .........................................................................................................................................................4
MEMBER INFORMATION ............................................................................................................................................................ 6
Member Eligibility .................................................................................................................................................................6
Eligibility Verification............................................................................................................................................................6
Member Hold Harmless..........................................................................................................................................................8
Member Confidentiality .........................................................................................................................................................8
Member Rights and Responsibilities ......................................................................................................................................9
Advance Medical Directives...................................................................................................................................................13
Benefits and Services..............................................................................................................................................................13
PROVIDER INFORMATION ..........................................................................................................................................................13
Role of the Primary Care Physician (PCP).............................................................................................................................13
Role of the Specialist Physician .............................................................................................................................................14
Communication between Providers........................................................................................................................................14
Provider Marketing Guidelines...............................................................................................................................................14
PROVIDER CREDENTIALING AND PARTICIPATION ........................................................................................................... 15
PROVIDER & ALLIED HEALTH PRACTITIONERS CREDENTIALING CRITERIA ........................................................ 15
Required Information .............................................................................................................................................................15
Credentials Criteria................................................................................................................................................................. 16
Additional Requirements........................................................................................................................................................19
Initial Credentialing Office Site Reviews...............................................................................................................................19
Provider Re-Credentialing......................................................................................................................................................20
Practitioner’s Rights ...............................................................................................................................................................20
PROVIDERS DESIGNATED AS PRIMARY CARE PHYSICIANS............................................................................................21
CHANGES IN ADMINISTRATIVE, MEDICAL AND/OR REIMBURSEMENT POLICIES..................................................21
NOTIFICATION REQUIREMENTS FOR PROVIDERS............................................................................................................. 21
CLOSING PATIENT PANELS......................................................................................................................................................... 22
PROVIDER ACCESS AND AVAILABILITY STANDARDS ....................................................................................................... 22
CLAIMS SUBMISSION ................................................................................................................................................................... 23
Professional Claims ................................................................................................................................................................23
Institutional Claims.................................................................................................................................................................24
Participating Provider Claim Reconsideration Process .......................................................................................................... 25
Claim Adjustment Reason Codes ...........................................................................................................................................26
NATIONAL PROVIDER IDENTIFIER (NPI)................................................................................................................................ 31
HIERARCHICAL CONDITION CATEGORIES (HCC) .............................................................................................................. 33
SAMPLE EXPLANATION OF BENEFITS (EOB) STATEMENT AND PAYMENT CHECK ................................................34
2
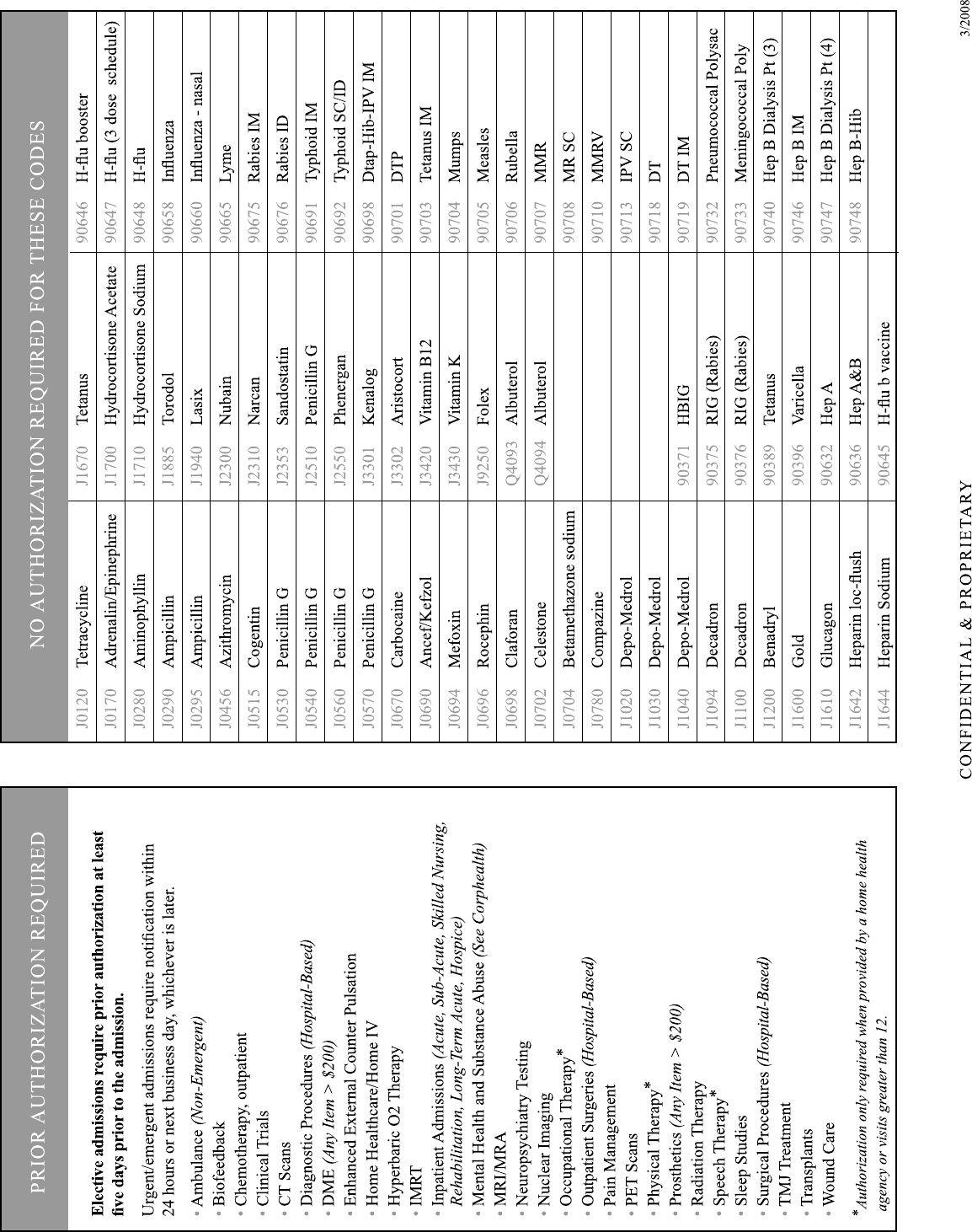
PRIOR AUTHORIZATION ............................................................................................................................................................. 35
General Rules .........................................................................................................................................................................35
Authorization Rules by Place of Service ................................................................................................................................36
In Office ................................................................................................................................................................... 36
Inpatient....................................................................................................................................................................37
Outpatient.................................................................................................................................................................38
Ambulatory Surgery Center .....................................................................................................................................40
Home Health Services..............................................................................................................................................40
Preventive Care ........................................................................................................................................................41
Health and Wellness.................................................................................................................................................42
Medicines and Injectibles.........................................................................................................................................43
Prior Authorization Request Form ...........................................................................................................................45
QUALITY IMPROVEMENT............................................................................................................................................................ 46
Quality Improvement Program...............................................................................................................................................46
Healthcare Effectiveness Data and Information Set ...............................................................................................................47
ON-SITE ASSESSMENTS ................................................................................................................................................................48
Office Standards .....................................................................................................................................................................48
Medical Record Review .........................................................................................................................................................48
HEALTH SERVICES ........................................................................................................................................................................ 50
Goals.......................................................................................................................................................................................50
Clinical Review Guidelines .................................................................................................................................................... 50
Prospective Review Process ...................................................................................................................................................51
Decision Time Frames............................................................................................................................................................ 51
Concurrent Review.................................................................................................................................................................53
Retrospective Review.............................................................................................................................................................53
Referrals to Non- Contracted Providers.................................................................................................................................. 53
Ambulatory Services ..............................................................................................................................................................53
Discharge Planning.................................................................................................................................................................54
Case Management...................................................................................................................................................................55
Skilled Nursing Care .............................................................................................................................................................. 55
Emergency Services ...............................................................................................................................................................55
Decision Time Frames............................................................................................................................................................ 56
DENIALS.............................................................................................................................................................................................56
Rendering Denials ..................................................................................................................................................................56
Notification of Denials ...........................................................................................................................................................56
CONTINUITY OF CARE..................................................................................................................................................................57
CLINICAL PRACTICE GUIDELINES ..........................................................................................................................................58
Congestive Heart Failure........................................................................................................................................................58
CHF Pharmacological Treatment Options..............................................................................................................................59
Heart Failure Disease Classification....................................................................................................................................... 60
Diabetes ..................................................................................................................................................................................61
Coronary and Other Vascular Disease.................................................................................................................................... 62
COPD .....................................................................................................................................................................................64
PHARMACEUTICAL MANAGEMENT ........................................................................................................................................ 65
Step Therapy........................................................................................................................................................................... 65
Prior Authorization.................................................................................................................................................................66
ALTERNATIVE DISPUTE RESOLUTION ...................................................................................................................................67
ADULT PREVENTION AND SCREENING GUIDELINES......................................................................................................... 71

3
Dear Valued Provider and Staff:
I would like to extend a warm welcome and thank you for participating with Bravo
Health’s network of Participating Providers. We value our relationship with all of our
Providers and are committed to working with you to meet the needs of your Bravo Health
patients.
For more than ten years we have been focusing on serving the healthcare needs of people
with Medicare. We will continue to serve the Medicare market and, in doing so, will
continue to seek ways to bring the benefits and services our Members need to live life well.
Thank you for continued participation with Bravo Health.
Sincerely,
Pat Feyen
Senior Vice President and Executive Director
Bravo Health Texas, Inc.
4
5
6
MEMBER ELIGIBILITY
Anyone who meets the following criteria is eligible to enroll in one of Bravo Health’s HMO Benefit Plans.
• Must be enrolled in Medicare, both Part A and Part B.
• Must reside in one of the following Counties:
• Bexar
• El Paso
• Harris
• Must not have End Stage Renal Disease (ESRD) at time of enrollment.
To enroll in one of Bravo Health’s Private Fee-For-Service (PFFS) Benefit Plans, the Member must
• Be enrolled in Medicare Part A and Part B
• Reside in one of the following Counties:
• Atascosa
• Bexar
• Brazoria
• Chambers
• El Paso
• Fort Bend
• Galveston
• Guadalupe
• Harris
• Jasper
• Jefferson
• Liberty
• Medina
• Montgomery
• Orange
• Must not have End Stage Renal Disease (ESRD) at the time of enrollment
ELIGIBILITY VERIFICATION
All Participating Providers are responsible for verifying a Member’s eligibility at each and every visit.
Please note that Membership data is subject to change. CMS retroactively terminates Members for various
reasons. When this occurs, the Bravo Health claim recovery unit will request a refund from the Provider. The
Provider must then contact CMS eligibility to determine the Member’s actual benefit coverage for the date of
service in question.

7
You can verify HMO (Bravo Classic, Bravo Healthy Heart, Bravo Gold or Bravo Select) Member eligibility in
three ways:
o Online through Emdeon or other office management software
o By calling Provider services at 1-888-353-3789
o Through our Interactive Voice Response (IVR) System at 1-866-467-3126 The IVR
System is available 24 hours a day, 7 days a week.
To verify Private-Fee-For-Service (Bravo Liberty) Member eligibility:
o Call 1-866-464-0701
Classic
RXBIN 610014
RXPCN MEDDPRIME
RXGrp ELDERHLTH
Issuer 80840 Processor = PAID
ID 99999999 G/BF/BNF $0/$35/$70
Name SAMPLE A SAMPLE
PCP Name SAMPLE SAMPLE
PCP Phone 999-999-9999
PCP $0 Specialist $35 Emergency Room $50
Behavioral Health (Corphealth): 866-671-4537
H4528001
8
MEMBER HOLD HARMLESS
Participating Providers are prohibited from balance billing Bravo Health Members including, but not
limited to, situations involving non-payment by Bravo Health, insolvency of Bravo Health, or Bravo
Health’s breach of its Agreement. Provider shall not bill, charge, collect a deposit from, seek
compensation or reimbursement from, or have any recourse against Members or persons, other than
Bravo Health, acting on behalf of Members for Covered Services provided pursuant to the contracted
Provider’s Agreement. The Provider is not, however, prohibited from collecting co-payments, co-
insurances or deductibles for non-covered services in accordance with the terms of the applicable
Member’s Benefit Plan.
In the event a Provider refers a Member to a non-Participating Provider without pre-approval, or
provides Excluded Services to Member, Provider must inform the Member in advance, in writing: (i)
of the service(s) to be provided; (ii) that Bravo Health will not pay for or be liable for said services;
and (iii) that Member will be financially liable for such services. In the event the Provider does not
comply with the requirements of this section, Provider shall be required to hold the Member harmless
as described above.
MEMBER CONFIDENTIALITY
At Bravo Health, we know Bravo Health Members’ privacy is extremely important to them, and we
respect their right to privacy when it comes to their personal information and health care. We are
committed to protecting our Member’s personal information. Bravo Health does not give out any
Member information to anyone without obtaining consent from an authorized person(s), unless we are
permitted to do so by law. Because you are a valued Provider to Bravo Health, we want you to know
the steps we have taken to protect Bravo Health’s Members’ privacy. This includes how we gather
and use their personal information. Bravo Health’s privacy practices apply to all of Bravo Health’s
past, present and future Members.
When a Member joins a Bravo Health Medicare Advantage plan, the Member agrees to give Bravo
Health access to Protected Health Information. Protected Health Information (“PHI”), as defined by
the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”), is information created or
received by a health care Provider, health plan, employer or health care clearinghouse, that: (i) relates
to the past, present, or future physical or mental health or condition of an individual, the provision of
health care to the individual, or the past, present or future payment for provision of health care to the
individual; (ii) identifies the individual, or with respect to which there is a reasonable basis to believe
the information can be used to identify the individual; and (iii) is transmitted or maintained in an
electronic medium, or in any form or medium. Access to PHI allows Bravo Health to work with
Providers, like yourself, to decide whether a service is a Covered Service and pay your clean claims
for Covered Services using the Members’ medical records. Medical records and claims are generally
used to review treatment and to do quality assurance activities. It also allows Bravo Health to look at
how care is delivered and carry out programs to improve the quality of care Bravo Health’s Members
receive. This information also helps Bravo Health manage the treatment of diseases to improve Bravo
Health’s Members’ quality of life.
9
Bravo Health’s Members have additional rights over their health information. They have the right to:
• Send Bravo Health a written request to see or get a copy of information that we have about
them, or amend their personal information that they believe is incomplete or inaccurate. If we
did not create the information, we will refer Bravo Health’s Member to the source, such as
you.
• Request that we communicate with them about medical matters using reasonable alternative
means or at an alternative address, if communications to their home address could endanger
them.
• Receive an accounting of Bravo Health’s disclosures of their medical information, except
when those disclosures are for treatment, payment or health care operations, or the law
otherwise restricts the accounting.
MEMBER RIGHTS AND RESPONSIBILITIES
Bravo Health Members have the following rights:
The right to be treated with dignity and respect
Members have the right to be treated with dignity, respect, and fairness at all times. Bravo Health must
obey laws against discrimination that protect Members from unfair treatment. These laws say that
Bravo Health cannot discriminate against Members (treat Members unfairly) because of a person’s
race, disability, religion, sex, sexual orientation, health, ethnicity, creed, age, or national origin. If
Members need help with communication, such as help from a language interpreter, they should be
directed to call Member Services. Member Services can also help Members in filing complaints about
access (such as wheel chair access). Members can also call the Office of Civil rights at 1-800-368-
1019 or TTY/TDD 1-800-537-7697 or the Office for Civil Rights in their area.
The right to the privacy of medical records and personal health information
There are federal and state laws that protect the privacy of Member medical records and personal
health information. Bravo Health keeps Members’ personal health information private as protected
under these laws. Any personal information that a Member gives Bravo Health when they enroll in our
plans is protected. Bravo Health staff will make sure that unauthorized people do not see or change
Member records. Generally, we will get written permission from the Member (or from someone the
Member has given legal authority to make decisions on their behalf) before we can give Member
health information to anyone who is not providing the Member’s medical care. There are exceptions
allowed or required by law, such as release of health information to government agencies that are
checking on quality of care.
The laws that protect Member privacy give them rights related to getting information and controlling
how their health information is used. Bravo Health is required to provide Members with a notice that
tells them about these rights and explains how Bravo Health protects the privacy of their health
information. For example, Members have the right to look at their medical records, and to get copies
of the records (there may be a fee charged for making copies). Members also have the right to ask plan
Providers to make additions or corrections to their medical records (if Members ask plan Providers to
do this, they will review Members request and figure out whether the changes are appropriate).
Members have the right to know how their health information has been given out and used for non-
routine purposes. If Members have questions or concerns about privacy of their personal information
and medical records, they should be directed to call Member Services. Bravo Health will release a
10
Member’s information, including prescription drug event data, to Medicare, which may release it for
research and other purposes that follow all applicable Federal statutes and regulations.
The right to see Participating Providers, get covered services, and get prescriptions filled within a
reasonable period of time
Members will get most or all of their health care from Participating Providers, that is, from doctors and
other health Providers who are part of Bravo Health. Members have the right to choose a Participating
Provider (Bravo Health will tell Members which doctors are accepting new patients). Members have
the right to go to a women’s health specialist (such as a gynecologist) without a referral. Members
have the right to timely access to their Providers and to see specialists when care from a specialist is
needed. Members also have the right to timely access to their prescriptions at any network pharmacy.
“Timely access” means that Members can get appointments and services within a reasonable amount
of time. The Evidence of Coverage explains how Members access Participating Providers to get the
care and services they need. It also explains their rights to get care for a medical emergency and
urgently needed care.
The right to know treatment choices and participate in decisions about their health care
Members have the right to get full information from their Providers when they go for medical care,
and the right to participate fully in treatment planning and decisions about their health care. Bravo
Health Providers must explain things in a way that Members can understand. Members have the right
to know about all of the treatment choices that are recommended for their condition including all
appropriate and medically necessary treatment options, no matter what they cost or whether they are
covered by Bravo Health. This includes the right to know about the different Medication Management
Treatment Programs Bravo Health offers and in which Members may participate. Members have the
right to be told about any risks involved in their care. Members must be told in advance if any
proposed medical care or treatment is part of a research experiment, and be given the choice of
refusing experimental treatments.
Members have the right to receive a detailed explanation from Bravo Health if they believe that a plan
Provider has denied care that they believe they are entitled to receive or care they believe they should
continue to receive. In these cases, Members must request an initial decision. “Initial decisions” are
discussed in the Members’ Evidence of Coverage.
Members have the right to refuse treatment. This includes the right to leave a hospital or other medical
facility, even if their doctor advises them not to leave. This includes the right to stop taking their
medication. If Members refuse treatment, they accept responsibility for what happens as a result of
refusing treatment.
The right to use advance directives (such as a living will or a power of attorney)
Members have the right to ask someone such as a family member or friend to help them with decisions
about their health care. Sometimes, people become unable to make health care decisions for
themselves due to accidents or serious illness. If a Member wants to, he/she can use a special form to
give someone they trust the legal authority to make decisions for them if they ever become unable to
make decisions for themselves. Members also have the right to give their doctors written instructions
about how they want them to handle their medical care if they become unable to make decisions for
themselves. The legal documents that Members can use to give their directions in advance in these
situations are called “advance directives.” There are different types of advance directives and
different names for them. Documents called “living will” and “power of attorney for health care”
are examples of advance directives.
11
If Members decide that they want to have an advance directive, there are several ways to get this type
of legal form. Members can get a form from their lawyer, from a social worker, from Bravo Health, or
from some office supply stores. Members can sometimes get advance directive forms from
organizations that give people information about Medicare. Regardless of where they get this form,
keep in mind that it is a legal document. Members should consider having a lawyer help them prepare
it. It is important to sign this form and keep a copy at home. Members should give a copy of the form
to their doctor and to the person they name on the form as the one to make decisions for them if they
can’t. Members may want to give copies to close friends or family Members as well.
If Members know ahead of time that they are going to be hospitalized, and they have signed an
advance directive, take should a copy with them to the hospital. If Members are admitted to the
hospital, the hospital will ask them whether they have signed an advance directive form and whether
they have it with them. If Members have not signed an advance directive form, the hospital has forms
available and will ask if the Member wants to sign one.
Remember, it is a Member’s choice whether he/she wants to fill out an advance directive (including
whether they want to sign one if they are in the hospital). According to law, no one can deny them care
or discriminate against them based on whether or not they have signed an advance directive. If
Members have signed an advance directive, and they believe that a doctor or hospital has not followed
the instructions in it, Members may file a complaint with their State’s Board of Medicine.
The right to make complaints
Members have the right to make a complaint if they have concerns or problems related to their
coverage or care. “Appeals” and “grievances” are the two different types of complaints Members can
make. If Members make a complaint, Bravo Health must treat them fairly, i.e., not discriminate against
Members, because they made a complaint. Members have the right to get a summary of information
about the appeals and grievances that have been filed with Bravo Health in the past. To get this
information, Members should be directed to call Member Services.
The right to get information about their health care coverage and cost
The Evidence of Coverage tells Members what medical services are covered and what they have to
pay. If they need more information, they should be directed to call Member Services. Members have
the right to an explanation from Bravo Health about any bills they may get for services not covered by
Bravo Health. Bravo Health must tell Members in writing why Bravo Health will not pay for or allow
them to get a service, and how they can file an appeal to ask Bravo Health to change this decision.
Staff should inform Members on how to file an appeal, if asked and should direct Members to review
their Evidence of Coverage for more information about filing an appeal.
The right to get information about Bravo Health, plan Providers, drug coverage, and costs
Members have the right to get information from us about our plan and operations. This includes
information about our financial condition, the services we provide, about our health care Providers and
their qualifications, and about how Bravo Health compares to other health plans. Members have the
right to find out from us how we pay our doctors. To get any of this information, Members should be
directed to call Member Services. Members have the right to get information from us about their Part
D prescription coverage. This includes information about our financial condition and about our
network pharmacies. To get any of this information, staff should direct Members to call Member
Services.

12
How to get more information about Members rights
Members have the right to receive information about their rights and responsibilities and if Members
have questions or concerns about their rights and protections, they should be directed to call Member
Services. Members can also get free help and information from their State Health Assistance Insurance
Program (SHIP). In addition, the Medicare program has written a booklet called Members Medicare
Rights and Protections. To get a free copy, Members should be directed to call 1-800-MEDICARE
(1-800-633-4227). TTY is 1-877-486-2048. Members can call 24 hours a day, 7 days a week. Or,
Members can visit www.medicare.gov on the web to order this booklet or print it directly from their
computer.
What can Members do if they think they have been treated unfairly or their rights are not being
respected?
If Members think they have been treated unfairly or their rights have not been respected, there are
options for what they can do.
• If Members think they have been treated unfairly due to their race, color, national origin,
disability, age, or religion, we must encourage them to let us know immediately. They can also
call the Office for Civil Rights in their area.
• For any other kind of concerns or problem related to their Medicare rights and protections
described in this section, Members should be encouraged to call Member Services. Members
can also get help from their SHIP.
Bravo Health Members have the following responsibilities:
Along with rights Members have responsibilities by being a Member of Bravo Health. Members are
responsible for the following:
a. To become familiar with their Bravo Health coverage and the rules they must follow to get care as a
Member. Members can use their Bravo Health Evidence of Coverage and other information that we
provide them to learn about their coverage, what we have to pay, and the rules they need to follow.
Members should always be encouraged to call Member Services if they have any questions or
complaints.
b. To advise Bravo Health if the Member has other insurance coverage
c. To notify Providers when seeking care (unless it is an emergency) that Member is enrolled with
Bravo Health and present their plan enrollment card to the Provider.
d. To give their doctors and other Providers the information they need to care for the Member, and to
follow the treatment plans and instructions that they and their doctors agree upon. Members must be
encouraged to ask their doctors and other Providers questions whenever they have them.
e. To act in a way that supports the care given to other patients and helps the smooth running of their
doctor’s office, hospitals, and other offices.
f. To pay their plan premiums and any co-payments they may have for the covered services they
receive. Members must also meet their other financial responsibilities that are described in their
Evidence of Coverage.
g. To let Bravo Health know if they have any questions, concerns, problems, or suggestions regarding
their rights, responsibilities, coverage and Bravo Health operations.
13
h. To notify Bravo Health Member Services and their Providers of any address and phone number
changes as soon as possible.
i. To use their Bravo Health plan only to access services, medications and other benefits for
themselves.
ADVANCE MEDICAL DIRECTIVES
All Providers, contracted directly or indirectly with Bravo Health, may be informed by the Member
that Member has executed, changed or revoked an advance directive. At the time service is provided
the Provider should ask the Member to provide a copy of the advance directive to be included in
his/her medical record.
If the PCP and/or treating Provider, cannot, as a matter of conscience, fulfill the Member’s written
advance directive he/she must advise the Member and Bravo Health. Bravo Health and the PCP
and/or treating Provider will arrange a transfer of care.
Participating Providers may not condition the provision of care or otherwise discriminate against an
individual based on whether the individual has executed an advance directive. However, nothing in
The Patient Self-Determination Act precludes the right under state law of a Provider to refuse to
comply with an advance directive as a matter of conscience.
BENEFITS AND SERVICES
All Bravo Health Members receive the benefits and services as defined in their Evidence of Coverage
(EOC). Each month, Bravo Health sends Participating Primary Care Physicians a list of his/her
active Members. The name of the Plan in which the Member enrolled will be listed on the roster.
Recently terminated Members may appear on the list.
Bravo Health encourages its Members to call their Primary Care Physician to schedule appointments.
However, if a Bravo Health Member calls or comes to your office for an unscheduled non-emergent
appointment, please attempt to accommodate the Member and explain to them your office policy
regarding appointments. If this problem persists, please contact Bravo Health.
THE ROLE OF THE PRIMARY CARE PHYSICIAN (“PCP”)
Each Bravo Health Member must select a Bravo Health Participating Primary Care Physician (“PCP”)
at the time of enrollment. The Primary Care Physician is responsible for managing all the health care
needs of a Bravo Health Member as follows:
• Manage the health care needs of Bravo Health Members who have chosen them as their Primary
Care Physician;
• Ensure that Member receives treatment as frequently as is necessary based on the Member’s
condition;
• Develop an Individual Treatment Plan for each Member;
• Submit accurately and timely encounter information for clinical care coordination;
• Comply with Bravo Health’s pre-authorization procedures;
• Refer to Bravo Health Participating Providers;
14
• Comply with Bravo Health’s Quality Management and Utilization Management programs;
• Use appropriate designated ancillary services;
• Comply with emergency care procedures;
• Comply with Bravo Health access and availability standards as outlined in this manual including
after-hours care;
• Bill Bravo Health on the CMS 1500 claim form or electronically in accordance with Bravo Health
billing procedures;
• When billing ensure that coding is specific enough to capture to acuity and complexity of a
Member’s condition and ensure that the codes submitted are supported by proper documentation
in the medical record;
• Comply with Preventive Screening and Clinical Guidelines;
• Adhere to Bravo Health’s medical record standards as outlined on page 49 of this manual.
THE ROLE OF THE SPECIALIST PHYSICIAN
• Provide specialty services;
• Collaborate with Bravo Health Primary Care Physician to enhance continuity of health care and
appropriate treatment;
• Provide consultative and follow-up reports to the referring physician in a timely manner;
• Comply with access and availability standards as outlined in this manual including after-hours
care;
• Comply with Bravo Health’s pre-authorization process;
• Comply with Bravo Health’s Quality Management and Utilization Management programs;
• Bill Bravo Health on the CMS 1500 claim form in accordance with Bravo Health’s billing
procedures;
• When billing ensure that coding is specific enough to capture to acuity and complexity of a
Member’s condition and ensure that the codes submitted are supported by proper documentation
in the medical record;
• Refer to Bravo Health Participating Providers only;
• Submit encounter information to Bravo Health accurately and timely;
• Adhere to Bravo Health’s medical record standards as outlined on page 49 of this manual.
COMMUNICATION BETWEEN PROVIDERS
• PCP should provide Specialist Physician with relevant clinical information regarding the
Member’s care.
• Specialist Physician must provide PCP with information about his/her visit with the Member
in a timely manner.
• PCP must document in the Member’s chart his/her review of any reports, labs or diagnostic
tests received from a Specialist Physician.
PROVIDER MARKETING GUIDELINES
Bravo Health Participating Providers must adhere to the following guidelines with regard to any marketing activities:
• Ensure that any marketing activities are approved in advance by Bravo Health to ensure compliance
with CMS guidelines;
• Ensure that any letters, events, health fairs, etc. are reported to and cleared in advance by Bravo
Health;
• Ensure that any gifts or promotional items are cleared with Bravo Health in advance;
15
• Providers may make available and/or distribute Bravo Health marketing materials and display posters
in accordance with and subject to Medicare Marketing Guidelines;
• Providers may not make available, accept or distribute plan enrollment applications or offer
inducements to enroll in a specific plan; and
• Providers may not offer anything of value to induce a prospective Member to select them as their
Provider.
PROVIDER CREDENTIALING AND PARTICIPATION
Providers must be credentialed by Bravo Health according to the following guidelines:
Provider Status Procedure
New to plan, not
previously credentialed
Practicing in a solo practice Requires a signed contract and
initial credentialing which may
include a site visit depending upon
Provider’s specialty*
New to plan, not
previously credentialed
Joining a contracted group
practice
Requires initial credentialing;
however, a site visit is not be
required regardless of specialty.
Already contracted and
credentialed
Leaving a group practice to
begin a solo practice
Does not require credentialing;
however a new contract is required
and a new office location may
require a site visit depending upon
Provider’s Specialty*
Already contracted and
credentialed
Leaving a group practice to
join another contracted
group practice
Does not require credentialing and
no site visit is required regardless of
specialty.
Already contracted and
credentialed
Leaving a group practice to
join a non-contracted group
practice
The Provider’s participation is
terminated unless non-contracted
group signs a contract with Bravo
Health.
* Primary Care and OB/GYN offices require site visits
PROVIDER & ALLIED HEALTH PRACTITIONERS CREDENTIALING CRITERIA
REQUIRED INFORMATION
1) Completed Bravo Health, Texas Standard or CAQH application with a signed and dated Bravo Health
Certification and Attestation form.
a) If you answer yes to any of the questions, supply all additional information.
b) If you answer yes to the malpractice history question, please supply for each case:
1. Date of alleged malpractice
2. A brief description of the nature of the case and alleged malpractice
3. A statement describing your role in the case
4. Current status of case, including any settlement amount
16
2) Current and complete professional liability information on the application and provide a copy of your
current malpractice insurance face sheet.
3) Current and complete hospital affiliation information on the application and a copy of your current
appointment or reappointment letter.
4) If no hospital privileges and your specialty warrants hospital privileges, a letter from you detailing your
coverage arrangements and a letter from the physician who will admit for you.
5) Five years of work history (month/year format) documented on the application or on current curriculum
vitae with any gaps of more than 6 months explained and gaps of one year or more explained in writing.
6) A signed and dated Provider Agreement. Upon acceptance, an executed copy will be returned to you for
your files.
7) Completed and signed W-9 form.
8) Bravo Health conducts an office site visit at Primary Care and OB/GYN offices. This requirement is
waived for new physicians joining an existing practice.
All applications for participation with Bravo Health will be reviewed by the designated Bravo Health
Medical Director and Physician Advisory Credentialing Committee (PACC). Applications will be
reviewed on an individual basis
The criteria stated below are the minimum standards, and meeting these criteria is not sufficient in and
of itself for acceptance. Bravo Health maintains the right to limit the Provider network according to its
needs. The credentials process is a vital part of the Bravo Health Quality Assessment program and is an
essential tool to assure that the care delivered is of optimal quality using the resources available.
All information submitted to Bravo Health for both the initial credentialing and re-credentialing
processes will be considered by the PACC prior to making a decision regarding acceptance, denial, or
termination.
CREDENTIALS CRITERIA
1. Physicians must have obtained a Doctor of Medicine, Doctor of Osteopathy, Doctor of Medical
Dentistry, or Doctor of Dental Surgery, degree from a medical school accredited by one of the
following: the Liaison Committee on Medical Education (or have obtained a certificate from the
Educational Council for Foreign Medical Graduates-ECFMG), the American Osteopathic
Association (AOA) or the American Board of Oral and Maxillofacial Surgery (ABOMS). Allied
Health Professionals must have graduated from an approved professional degree program for the
specialty they are applying for participation.
2. Physicians must have completed a full residency training program accredited by one of the agencies
listed below in the specialty designated as the individual’s principal type of practice: American
Osteopathic Association (AOA) or the American Dental Association Commission on Dental
Accreditation or the American Medical Association (AMA).
3. Physicians and Allied Health Professionals must have and maintain a current and unrestricted license
to practice medicine granted by each State where he or she has an office listing with Bravo Health.
Any Provider whose license is in a probationary status is not eligible for Membership.
17
4. Physicians credentialed for participation with Bravo Health that are not board certified must have
completed an approved residency training program with the following exception noted below.
If not board certified, the credentialing staff will verify the physician’s residency. Residencies will
be verified through the AMA or AOA physician master profile for the specialty being requested or
by writing the residency program itself. For podiatrists, the residency will be verified by writing the
residency program itself. Board certification and residency verifications are completed within 180
days of being presented to the PACC.
Exception: If a physician is not board certified but has completed internship/residency training
prior to January 1, 1980 AND has ten year’s of experience in his/her trained specialty, then the
physician may be credentialed and listed in that designated specialty and is considered to be
“grandfathered.”
5. For physician listings in Bravo Health provider directories:
• Upon initial credentialing, if a physician is board certified in his/her primary specialty and has
the appropriate fellowship training or board certification in his/her subspecialty, then the
physician may be credentialed and listed in both the primary specialty and the subspecialty.
• Upon initial credentialing, if a physician is not board certified in his/her primary specialty, then
he/she may not be listed in his/her subspecialty. The physician will be credentialed and listed
only in his/her primary specialty for which he/she has the appropriate residency training as
outlined in # 4 above.
If the physician’s designated specialty includes the provision of services in a hospital setting, then:
a. The physician must demonstrate active privileges at a state licensed acute-care hospital that is
currently contracted with Bravo Health or part of the evolving network; or
b. The physician must provide to Bravo Health a written explanation as to why he/she does not have
hospital privileges and an acceptable method of hospitalizing Members. Both the applicant and the
Bravo Health contracted admitting physician must submit documentation of the arrangement; and
c. If the physician does not have hospital privileges due to any reason other than a strictly voluntary
relinquishment by the physician, the physician’s application will be reviewed by a Bravo Health Medical
Director and forwarded for review to the PACC.
6. Primary care physicians must have coverage arrangements with a Bravo Health Participating
physician to assure that services are available on a twenty-four-hour-a-day, seven-days-a-week basis.
7. Practitioners must disclose for Bravo Health Credentialing Committee review all claims or suits
alleging malpractice that have been filed against him or her or appealed or settled by the physician or
his or her insurance carrier in the past five (5) years.
8. Practitioners who currently or have ever been excluded from Medicare and/or Medicaid participation
is not eligible for participation with Bravo Health. If a physician is accepted into Bravo Health and
then is excluded from Medicare and/or Medicaid participation, that physician will be terminated.
18
9. Practitioners must hold and maintain a current federal narcotics license. It must include all DEA
schedules that the physician prescribes. It is recommended that this license include all of the
following DEA Schedules: 2, 2N, 3, 3N, 4, and 5. Pathologists and diagnostic radiologists may be
exempted from this criterion.
10. Physicians must have and maintain malpractice insurance of at least $1,000,000 per incident and
$3,000,000 aggregate, or minimum amounts according to community standards
11. Physicians must meet Bravo Health standards for medical office certification and medical record
assessment (if applicable to their specialty).
12. Physicians must demonstrate professional growth and development through continuing education
demonstrated by obtaining 50 hours of Category I AMA recognized Continuing Medical Education
(CME) credits every two years. A current AMA Physician’s Recognition Award will satisfy this
criterion.
This requirement will be waived:
• In any year a physician becomes board certified or re-certified; or
• If the physician is in his/her first year of practice.
13. Allied Health practitioners must demonstrate professional growth and development through
continuing education units at the time of re-credentialing.
14. If any practitioner is indicted for a felony or a crime including moral turpitude, dishonesty or false
statement or other acts, that practitioner will be suspended and may be terminated if the outcome is a
conviction.
15. a. Physicians must exhibit understanding of and agree to Bravo Health policies relative to the
provision of health care services, including ancillary services and adherence to the HMO’s
utilization, cost containment and quality assessment policies.
b. Physicians must agree to cooperate with and/or respond to Bravo Health investigations of
Member complaints, quality activities and/or satisfaction surveys or samplings.
c. Physicians and Allied Health Professionals must agree to Bravo Health administrative protocols.
16. Physicians/Allied Health Practitioners must recognize that information from the National
Practitioner Data Bank (NPDB) and confirmation of the validity of the practitioners board
preparedness or certification, State License, Federal DEA Certificate and malpractice insurance
information must be forthcoming and will be considered prior to credentialing.
19
ADDITIONAL REQUIREMENTS
If the applicant is accepted for participation in Bravo Health the following additional requirements will
apply:
1. The physician or allied health professional must continually maintain and comply with all Bravo
Health policies and procedures.
2. According to the Provider’s Contract, physicians or oral surgeons must notify Bravo Health in
writing within five (5) days of any changes in his or her status relative to the established credentials
criteria or any other matter that could potentially affect a continued contractual relationship with
Bravo Health, such as significant or prolonged illness, leave of absence, suspension or modification
of privileges, any change in physical or mental health status that affects practitioner’s ability to
practice or any other action that materially changes the practitioner’s ability to provide service to
Members.
3. A physician or oral surgeon who maintains more than one office after acceptance must have all
offices participate for the purpose of providing health care to patients.
4. If the relationship between the physician or oral surgeon and Bravo Health should be terminated at
any point for any reason other than a voluntary termination, a one-year period will elapse prior to
eligibility for reapplication. Upon reapplication, all the circumstances of the termination/resignation
must be revealed and will be considered.
INITIAL CREDENTIALING OFFICE SITE REVIEWS
1. Provider Relations staff shall conduct initial credentialing office site reviews using the Office Site
Evaluation Form.
2. The Office Site Evaluation Form is divided into the following sections:
a. Physical Appearance and Accessibility
b. Patient Safety and Risk Management
c. Medical Record Keeping and Storage
d. Appointment Availability
3. Each section of the Office Site Evaluation Form addresses a review topic with questions to be
answered “YES”, “NO”, or N/A (not applicable). Each answer is scored and scores are added to
generate an overall score for the office site.
4. Results of the office site review shall be reported directly to the reviewed office site. Objective
findings and recommendations for improvement of deficiencies shall be included in the report.
5. Any office site scoring below 80% will be given thirty (30) days in which to submit and ninety (90)
days to complete a corrective action plan for identified deficiencies. Upon completion of the
corrective action plan, a repeat office site review will be performed.
20
6. The completed Office Site Evaluation Form will be placed in the practitioner’s Credentialing file
prior to review by the PACC.
Member Complaint or Quality of Care Concern
1. In response to a Member complaint and/or Quality Improvement office site or a quality of care
concern relating to office site issues, Provider Relations staff shall conduct an office site review
using the same Office Site Evaluation Form and procedures as at initial credentialing or a different
data tool depending on the substance of the complaint.
2. Results of office site review will be evaluated, along with the complaint or quality of care concern,
by the Provider Advisory Credentialing, Committee.
PROVIDER RE-CREDENTIALING
All Participating Providers must adhere to the re-credentialing requirements established by Bravo Health.
The standard states that Providers must be formally re-credentialed every three (3) years. It is imperative
that Providers complete the re-credentialing process in order remain in good standing and continue to treat
Bravo Health Members. Non-compliance with the re-credentialing process in advance of the Provider’s due
date for re-credentialing will result in termination from the Bravo Health Provider network.
PRACTITIONER’S RIGHTS
The practitioner has the right to review information submitted to Bravo Health in support of his or her
credentialing/re-credentialing application except for peer review information that is confidential, protected
and restricted under State and Federal Peer Review Laws.
The practitioner will be notified in the event that information obtained from other sources varies
substantially from that provided by the physician and he or she will be given the opportunity to clarify
and/or correct this information prior to the finalization of the credentialing/re-credentialing process.
The practitioner has the right, upon request, to be informed of the status of their credentialing or re-
credentialing application. The practitioner can contact their Provider Recruiter or the Bravo Health
Credentialing Department at 866-442-7499 to make such a request.
Bravo Health Texas, Inc. conducts its credentialing and re-credentialing processes in a non-discriminatory
manner and does not base its decisions for applicant participation solely on an applicant’s race,
ethnic/national identity, gender, age, and sexual orientation or the types of procedures or types of patients
the practitioner specializes in. All decisions are based in the aforementioned criteria.
Bravo Health Texas, Inc., upon written request from a health care Provider that is applying to be
credentialed or a physician who is already credentialed, shall disclose the relevant credentialing criteria
outlined above.
Bravo Health Texas, Inc. will not exclude from credentialing or terminate a health care Provider who has a
practice that includes a substantial number of patients with expensive medical conditions.
21
PROVIDERS DESIGNATED AS PRIMARY CARE PHYSICIANS (PCPs)
Bravo Health recognizes the following physician types as PCPs:
• Family Practice
• General Practice
• Geriatric Medicine
• Internal Medicine
Bravo Health also recognizes Infectious Disease physicians as a PCP for Members who may require a
specialized physician to manage their specific healthcare needs.
CHANGES IN ADMINISTRATIVE, MEDICAL AND/OR REIMBURSEMENT POLICIES
From time to time, Bravo Health may amend, alter or clarify its policies. Examples of this include, but are
not limited to, regulatory changes, changes in medical standards and modification of Covered Services.
Specific Bravo Health policies and procedures may be obtained by calling our Provider Services
Department.
Bravo Health will communicate changes to the Provider Manual through the use of a variety of methods
including but not limited to:
• Annual Provider Manual Updates
• Letter
• Facsimile
• E-Mail
• Provider Newsletters
Providers are responsible for the review and inclusion of policy updates in the Provider Manual and for
complying with these changes upon receipt of these notices.
NOTIFICATION REQUIREMENTS FOR PROVIDERS
Participating Providers must provide written notice to Bravo Health 60 days in advance of any changes to
their practice or, if advance notice is not possible, as soon as possible thereafter.
These changes should be communicated to the Bravo Health Provider Data Maintenance Department
via facsimile at 1-866-234-9418 or by e-mail to PDM@BravoHealth.com.
The following is a list of changes that must be reported to Bravo Health:
• Practice address
• Billing address
• Fax or telephone number
• Hospital affiliation
• Tax Identification Number
• Practice name
• Providers joining or leaving the practice (including retirement or death)
• Practice Mergers and/or acquisitions
• Adding or closing a practice location
22
CLOSING PATIENT PANELS
When a Participating Primary Care Physician elects to stop accepting new patients, the Provider’s patient
panel is considered closed.
If a Participating Primary Care Physician closes his or her patient panel, the decision to stop accepting new
patients must apply to all patients regardless of insurance coverage. Providers may not discriminate against
Bravo Health Members by closing the patient panels for Bravo Health Members only, nor may they
discriminate among Bravo Health Members by closing their panel to certain product lines.
Providers who decide that they will no longer accept any new patients must notify Bravo Health’s Network
Management Department, in writing, at least 60 days before the date on which the patient panel will be
closed.
PROVIDER ACCESS AND AVAILABILITY STANDARDS
A Primary Care Physician (PCP) must have their primary office open to receive Bravo Health Members
five (5) days and for at least 20 hours per week. The PCP must ensure that coverage is available 24
hours a day, seven days a week. PCP offices must be able to schedule appointments for Bravo Health
Members at least two (2) months in advance of the appointment. A PCP must arrange for coverage during
absences with a Bravo Health Participating Provider in an appropriate specialty which is documented on the
Provider Application and agreed upon in the Provider Agreement.
Primary Care Access Standards
Appointment Type Access Standard
Urgent Within 24 hours
Non-Urgent/Non-Emergent Within 48 hours
Routine and Preventative Within 4 weeks
On-Call Response (After Hours) Within 30 minutes for emergency
Waiting Time in Office 30 minutes or less
Specialist Access Standards
Appointment Type Access Standard
Urgent Within 24 hours
Non-Urgent/Non-Emergent Within 48 hours
Elective Within 4 weeks
High Index of Suspicion of Malignancy Less than one (1) week
After-hours Access Standards
All Participating Providers must return telephone calls related to medical issues. Emergency calls must be
returned within 30 minutes of the receipt of the telephone call. Non-emergency calls should be returned
within a 24 hour time period. A reliable 24 hours a day, 7 days a week answering service with a beeper or
paging system and on-call coverage arranged with another Participating Provider of the same specialty is
preferred.
Behavioral Health Access Standards
Appointment Type Access Standard
Emergency Within 6 hours of the referral
Urgent/Symptomatic Within 48 hours of the referral
23
Routine Within 4 weeks of the referral
Availability Standards
PCPs OB/GYNs Behavioral Health Providers
1 Provider for every 500 Members 1 Provider for every 2500
Members
1 Provider within 20 miles/minutes to
Member
1 Provider within 20 miles to
Member
1 Provider within 20 miles to
Member
1 Provider within 30 miles/minutes to
Member
1 Provider within 30 minutes to
Member
1 Provider within 30 minutes to
Member
CLAIMS SUBMISSION
While Bravo Health prefers electronic submission of claims, both electronic and paper claims are accepted.
Please see quick reference guide for details (page 3).
Bravo Health pays Clean Claims according to contractual requirements and CMS guidelines. A Clean
Claim is defined as:
A claim for a Covered Service that has no defect or impropriety. A defect or impropriety includes,
without limitation, lack of data fields required by Bravo Health or substantiating documentation, or
a particular circumstance requiring special handling or treatment, which prevents timely payment
from being made on the claim. The term Clean Claim shall not include a claim from a Provider that
is under investigation for fraud or abuse regarding that claim. The term shall be consistent with the
Clean Claim definition set forth in applicable federal or state law, including lack of required
substantiating documentation for non-Participating Providers and suppliers, or particular
circumstances requiring special treatment that prevents timely payment from being made on the
claim. If additional substantiating documentation involves a source outside of Bravo Health, the
claim is not considered clean.
The following standard CMS-required data elements must be present for a claim to be considered a Clean
Claim. This applies to both electronic and paper claims:
Professional Claims
• Patient name
• Patient demographic information
• Member identification number
• Rendering Provider name
• Payee name and address
• Provider signature
• Explanation of Benefits from the primary carrier when Bravo Health is the secondary payor
• If the services were not rendered in an office or home setting, list the name and address of the
facility where services were rendered in Box 32
• Provider federal tax identification number
• Date of service
• All appropriate diagnosis codes (ICD9-CM codes)
• Procedure code for each service rendered (CPT-4 or HCPCS Codes)
• All appropriate modifiers for each service rendered
• Amount billed for each procedure
24
• Place of service code
• NPI number
• Type of service
• Days and units
• Anesthesia time in minutes
• Include the following information for all injectible drugs:
1. Average Wholesale Price (AWP) reimbursed Providers - the National Drug Code (NDC)
Number and the NDC unit(s) associated with each drug.
2. Average Sale Price (ASP) reimbursed Providers – the applicable HCPCS code and HCPCS
unit(s).
Institutional Claims
• Bill type
• Revenue codes and HCPCS codes
• Patient status code
• DRG code
• All appropriate diagnostic codes
• All appropriate diagnosis codes (ICD9-CM codes)
• Detailed billing for all pharmacy related revenue codes. The detailed billing should include the
name of the drug, the National Drug Code (NDC) number and the units associated with each
drug.
• Skilled nursing facilities should include a description of charges, for example, bed level, blood
glucose draw/stick, occupational/physical/speech therapy and radiology. Specific CPT-4 Codes
are also required based on the services rendered.
• NPI Number
Claims must be submitted with all required information within 180 days of the date on which the
service was rendered. All claims submitted after the 180-day period will be denied for untimely filing.
For claims questions, please contact Provider Services at 1-888-353-3789. A Provider Service
Representative will be able to answer your questions concerning eligibility, benefits and claims. If a
claim needs to be reprocessed for any reason, the Provider Service Representative will work with the
Claims Department to handle these cases.
Providers who are being paid under capitation and expect no additional payments still must submit
claims in order to capture encounter data as required per your Bravo Health Provider Agreement. This
encounter data should be submitted to Bravo Health’s Claims Department.
If a Provider provides services that require prior authorization, without obtaining prior authorization, the
claim for those services will be denied.
If appropriate, Providers must include the following additional attachments to their claim
submission:
• If Bravo Health is the secondary payer, the primary payer’s Explanation of Payment
• For Institutional Claims a itemized bill for pharmacy charges or claims exceeding stop loss thresholds.
25
PARTICIPATING PROVIDER CLAIM RECONSIDERATION PROCESS
As a Participating Provider, you have the right to initiate a Claim Reconsideration Request and seek to have
Bravo Health review its claim adjudication decisions. You have sixty (60) days from the date you received
Bravo Health’s claim denial or claim adjustment notice to request a review of our administrative decisions.
Your Claim Reconsideration Request must be in writing and include the following information:
1. The name of the Member, the Member’s date of birth, and the Member’s Bravo Health identification
number;
2. Provider name and address;
3. A copy of the specific claim and our payment adjustment or denial notice;
4. An explanation of the specific service and dates of service for which payment was adjusted or denied
and, using applicable Provider Agreement provisions, your rationale for requesting a
reconsideration.
Your request should be sent to the following address:
Bravo Health
Claim Reconsideration Team
P. O. Box 26038
Baltimore, MD 21224
Bravo Health will review your request and respond within 60 days of receipt of the request. If our original
claim adjudication decision is reversed, in whole or in part, the claim will be reprocessed and paid within 60
days. If our original claim adjudication decision is upheld, we will respond in writing and include a reason
for the reconsideration denial. If you disagree with the outcome of the claim reconsideration process, or for
any dispute other than claim reconsideration, you may pursue dispute resolution as described on page 67 of
this Manual and in your Agreement with us.
You do have the right, in most instances, to file an appeal on behalf of a Bravo Health Member provided
the Member has specifically authorized you to act on his/her behalf. A copy of the Member’s written
authorization must accompany the appeal.
26
Claim Adjustment Reason Codes-Texas
Code Description Denial Language
3 SERVICE NOT AUTHORIZED There is no authorization on file for these services.
7
SKILLED NURSING DAYS BENEFIT
EXHAUSTED
This claim exceeds the maximum of 100 days per benefit period in a Medicare certified skilled nursing
facility.
8 PREDATES ELIGIBILITY WITH PLAN This service was rendered prior to the Member's effective date with Bravo Health.
9 POSTDATES ELIGIBILITY W/PLAN This service was rendered after the Member's Bravo Health coverage ended.
14 PATIENT ENROLLED IN HOSPICE Please submit this claim to Medicare. The patient is enrolled in Hospice.
15 DME RENTAL FOR 15 MOS. ONLY
Rental for durable medical equipment is capped at 15 months. No additional benefits are available for
this equipment.
16 MEDICAL RECORDS REQUIRED Please resubmit this claim with medical records.
17 INVALID PROCEDURE CODE The procedure code billed is not valid. Please resubmit this claim with a valid code.
18 INVALID DIAGNOSIS CODE Please resubmit this claim with a valid ICD9 diagnosis code.
19 INVALID PLACE OF SERVICE Please resubmit this claim with a valid place of service e code.
21 CORRECTION TO PRIOR CLAIM This claim represents a correction to a prior claim.
22 FILING TIME LIMIT EXPIRED
All claims for participating Providers must be submitted within 180 days of the date of service. This
claim was submitted after the filing deadline.
25 AUTH EXPIRED This service was rendered after the expiration date of the authorization.
32 SUBMITTED W/O NDC NUMBERS Please resubmit this claim with National Drug Code number(s).
33 SUBMITTED W/O DETAIL
Please resubmit this claim with a detailed bill showing the charges and specific services for each date
of service.
35 SUBMITTED W/O CPT CODES Please resubmit with a valid CPT4 code.
36 INCLUDED IN PER DIEM Reimbursement for this service is included in the per diem payment.
37 INCLUDED IN BASE RATE Reimbursement for this service is included in the base rate.
38 SUBMITTED W/O HCPCS CODE Please resubmit this claim with HCPCS codes.
39 MISSING DATE OF SERVICE Please resubmit with dates of service.
60 ANESTHESIA TIME UNITS This line item represents the payment of the anesthesia time units.
61 MISSING ANESTHESIA TIME UNITS
The claim was submitted without anesthesia time or anesthesia time units. Please resubmit the claim
to indicate the length of time the patient was anesthetized.
63 DISCONTINUED PROCEDURE CODE The procedure code billed has been discontinued. Please resubmit with a current procedure code.
72 SKILLED AT DIFFERENT LEVEL
The skill level billed is different than the skill level that was authorized. This claim has been
processed according to the level authorized.
76 MISSING NUMBER OF UNITS Please resubmit with the number of units specified.
82 INCORRECT PLACE OF SERVICE Please resubmit with the correct place of service.
91 MISSING DIAGNOSIS Please resubmit with appropriate diagnosis codes.
102 BILL WITH CPT ANESTHESIA CODES Anesthesia claims must be submitted with ASA codes. Please resubmit this claim with ASA codes.
103 PREDATES AUTHORIZATION DATES This service was rendered before the effective date of the authorization.
27
Claim Adjustment Reason Codes-Texas (cont.)
104 PAID AT PER DIEM RATE The payment for this service is included in the per diem rate.
105 PREVIOUSLY PAID
This claim has been previously processed. Please review your records and contact our Provider
Service Team for assistance.
109 SUBMITTED W/O SERVICE UNITS Please resubmit this claim with the units field completed.
110 MILEAGE INCLUDED IN BASE RATE The mileage is included in the base rate and is not separately reimbursable.
114 POST DATES AUTHORIZATION DATES This service was rendered after the expiration date of the authorization.
118 UR DENIED HOSPITAL DAYS These hospital days have been denied by our Health Services Department.
120 PATIENT CONVENIENCE ITEM Patient convenience items are not covered under this benefit plan.
123 DENTAL COPAY/PATIENT LIABILITY This is a Member co-payment amount.
124 EXCEEDS AUTHORIZATION This service exceeds the number of services authorized.
127 NOT ELIG ON DATE OF SERVICE This patient was not a Bravo Health Member on the date of service.
128 SUBMIT TO SENIOR PARTNERS Please resubmit this claim to Senior Partners because the service date is within their coverage period.
130 PROVIDE DETAIL SERVICE DATES Please resubmit this claim with a detailed bill showing each separate date of service.
132 AUTH FOR DIFFERENT PROVIDER The authorization on file for this service was issued to a different Provider.
134 ER VISIT W/IN 72 HRS OF ADMIT
Emergency Room visits within 72 hours of an inpatient admission cannot be billed and reimbursed
separately.
135 ITEMIZED BILL REQUESTED Please resubmit with an itemized bill.
136 SUBMITTED W/O MODIFIER Please resubmit with appropriate modifier(s)
137 SUBMIT WITH NDC NUMBERS Please resubmit with National Drug Code (NDC) numbers.
139 NO CHARGE BILLED Please resubmit with billed charges for each service.
140 NOT COVERED SELF ADMIN RX Self administered drugs are not covered services under this plan.
141 NOT COVERED EXPERIMENTAL Experimental treatments are not covered services under this plan.
142 NOT COVERED ACUPUNCTURE Acupuncture is not a covered service under this plan.
143 NOT COVERED COSMETIC Cosmetic services are not covered services under this plan.
144 NOT COVERED CUSTODIAL CARE Custodial services are not covered services under this plan.
145 NOT COVERED HOMEMAKER SVC Homemaker services are not covered services under this plan.
147 NOT COVERED DELIVERED MEAL Delivered meals are not covered services under this plan.
148 NOT COVERED NATUROPATH SVC Naturopath services are not covered services under this plan.
149 NOT COVERED FULL TIME NURSING Full time nursing services are not covered services under this plan.
150 NOT COVERED ORTHOPEDIC SHOES Orthopedic shoes are not covered items under this plan.
151 NOT COVERED FOOT SUPPORT Foot supports are not covered items under this plan.
153 NOT COVERED PRIVATE DUTY NURSE Private Duty Nursing is not a covered service under this plan.
154 NOT COVERED PRIVATE ROOM Private Room charges are not covered under this plan.
155 NOT COVERED CHARGE BY RELATIVE Services rendered by a patient's relative are not covered services under this plan.
157 NOT COVERED SEX CHANGE Services related to a sex change are not covered services under this plan.
158 NOT COVERED STERILIZ. REVERSAL Services related to sterilization reversal are not covered services under this plan.
159 NOT COVERED NON RX CONTRACEPT Non prescription contraceptives are not covered under this plan.
28
Claim Adjustment Reason Codes-Texas (cont.)
160 NOT COVERED OBESITY Services related to the treatment of obesity are not covered under this plan.
161 NOT COVERED RADIAL KERATOTOMY Radial Keratotomy is not a covered service under this plan.
162 NOT COVERED LOW VISION AID/SVC Services and equipment related to low vision aids are not covered services under this plan.
164 NOT COVERED ROUTINE CHIROPRACT Routine chiropractic services are not covered services under this plan.
165 NOT COVERED ER FOR ROUTINE SVC
Emergency services are services needed immediately due to sudden illness or injury. Since the
services received do not meet these requirements, the services are not covered under the Plan.
166 NOT COVERED HEALTH EDUCATION Health Education services are not covered services under this plan.
167 NOT MEDICALLY NECESSARY
The service requested was reviewed by our Medical Director. The Medical documentation received
does not support the need for this service.
168 PAID AT DRG RATE This claim was paid at the DRG rate.
171 NOT COVERED BLOOD FIRST 3 UNIT The first three units of blood are not covered services under this plan.
174 DUPLICATE OF CLAIM IN REVIEW This claim is a duplicate of a claim that is currently in process.
175 PREVIOUSLY DENIED
This claim has been denied. Please review your records and contact our Provider Service Team for
assistance.
176 SUBMITTED W/O ADA CODE Please resubmit this claim with American Dental Association Codes.
177 MULTIPLE SURGERY DEDUCTION Standard multiple surgery rules have been applied to this service.
180 INAPPROPRIATE MODIFIER
This modifier is not appropriate for this procedure code. Please resubmit this claim with appropriate
codes.
181 MULT PROC BILLED W/O MODIFIER Please resubmit with this claim with appropriate modifiers.
186
PREVIOUSLY APPLIED TO
DEDUCTIBLE The approved amount for this service was previously applied to the Member's deductible.
193 PREVIOUSLY APPLIED TO COPAYMENT The approved amount for this service was previously applied to the Member's co-payment.
200 INCLUDED IN DRG RATE Payment for this service is included in the DRG rate.
204 PAID AT CASE RATE Reimbursement for this claim is made at the case rate.
205 INCLUDED IN CASE RATE Payment for this service is included in the case rate.
206 INCLUDED IN ASC RATE Payment for this service is included in the ASC rate.
216
SUBMIT CLAIM TO MENTAL HEALTH
VENDOR Please submit this claim to the Behavioral Health Vendor.
217 INVALID NDC NUMBER Please resubmit with a valid National Drug Code (NDC) number. The number submitted is not valid.
221 PD AT STOPLOSS RATE This claim was reimbursed according to the contracted stop-loss rate.
222 INCLUDED IN STOPLOSS RATE Reimbursement for this service is included in the contracted stop-loss rate.
223 SUBMIT CLAIM WITH INVOICE Please resubmit this claim with the appropriate invoice.
224 OVERTURNED APPEAL This claim represents a change to a prior claim based on an appeal decision.
230 CUSTOMER SERVICE AUTH ISSUE This claim was reprocessed as the result of a customer service case.
231 SUBMIT WITH CORRECT POS Please resubmit this claim with a corrected place of service.
233 CUSTOMER SERVICE CLAIMS ISSUE This claim was reprocessed as the result of a customer service case.
234 RETRO REVIEW IN PROCESS
Our Health Services Department has requested Medical Records on this admission. When the
decision has been rendered, the claim will be processed in accordance with the decision.
29
Claim Adjustment Reason Codes-Texas (cont.)
251 DN TO OBSERVATION RATE This claim is processed as an observation stay.
252 RESUBMIT AS OBSERVATION
This stay was authorized as observation. Please resubmit this claims as an observation claim
255 IACD SERVICES - BILL MEDICARE
This claim is the responsibility of Original Medicare. Please bill this claim directly to Medicare with
the appropriate codes.
256 REBILL WITH CPT CODES Please resubmit this claim with CPT4 codes.
267 PRIMARY CARRIER PAYMENT This amount represents the payment made by the primary carrier.
268 EOB REQUESTED Please resubmit with an Explanation of Benefits from the primary insurance carrier.
270 INCORRECT BILL TYPE Please resubmit with a corrected Bill Type.
275 MISSING DRG Please resubmit this claim with the appropriate DRG code.
279 QUARTERLY MAXIMUM REACHED
The quarterly dental maximum has been met. No additional dental benefits are available for this
quarter.
281 NON QUEST LAB PROVIDER
Laboratory services must be provided by Quest Laboratory unless the services have been pre
authorized.
288 ITEMIZED BILL NOT= TO CHARGES
Please resubmit a corrected claim. The total on the itemized bill does not equal the total of the billed
charges for these items.
302 UNLISTED PROCEDURE Please resubmit this claim with medical records to support the unlisted procedure code.
305 DN GRADED TO SKILLED NURSING This claim is processed as a skilled nursing claim.
306 DN GRADED TO TELEMETRY This claim is processed as a telemetry stay.
308 NEED VALID ANESTHESIA CODE Anesthesia claims must be submitted with ASA codes. Please resubmit this claim with ASA codes.
310 DN GRADED TO MED/SURG DAY This claim is processed as a medical/surgical stay.
311 DN GRADED TO SUBACUTE This claim is processed as a sub-acute stay.
312 INCLUDED IN INPATIENT PER DIEM Reimbursement for this service is included in the inpatient per diem payment.
402
TRANSPORTATION MAXIMUM
REACHED
The maximum benefit of 12 routine transportation roundtrips to plan-approved locations for covered
health care services has been provided and no additional benefits are available.
404 MEDICAL NUTRITION THERAPY Medical nutrition therapy must be approved in advance of the therapy.
405 SMOKING CESSATION PROGRAM Smoking cessation counseling programs require prior authorization.
450 GLASSES ONE PAIR EVERY 2 YEARS
One pair of eye glasses is a covered benefit every two years. This pair of glasses exceeds the benefit
maximum.
451 HEARING AID MAXIMUM REACHED The maximum benefit for hearing aids has been provided and no additional benefits are available.
452 ROUTINE PODIATRY MAX REACHED
The maximum benefit for routine podiatry services of 4 visits every calendar year has been reached
and no additional benefits are available.
505 BILL WITH SPECIFIC DATES Please resubmit this claim with specific dates of service.
560 INCORRECT NUMBER OF UNITS Please submit with the correct number of units.
574 UNIT COST < $1,000 The item billed is less than $1,000 and no separate reimbursement is due.
612 INCORRECT DISCHARGE DATE This claim was submitted with an incorrect discharge date. Please resubmit with a correct date.
615 DRG GROUPER DISCREPANCY
The DRG listed on the claim does not match the DRG derived from the claim. Please resubmit with
correct information.
30
Claim Adjustment Reason Codes-Texas (cont.)
619 SUBMIT OPERATIVE NOTES Please resubmit this claim with operative notes.
620 SUBMIT TO DAVIS VISION Please submit this claim to Davis Vision.
620 SUBMIT TO DAVIS VISION Please submit this claim to Davis Vision.
621 CONVERTED TO ASA CODE
The procedure code for this service was converted to an ASA code for pricing. Please submit all future
claims with ASA codes.
624 NDC # DOES NOT MATCH RX NAME
This NDC number submitted with this claim is not valid for the drug name listed on the claim. Please
resubmit with the correct code and name.
702 REBILL USING MEDICARE G CODES Please resubmit with the appropriate HCPCS codes.
706 SUBMIT WITH CMG This is an acute rehab admit. Please resubmit claim with the appropriate case mix group code.
707 PAID AT CMG This claim was reimbursed according to the CMS case mix group.
708 INCLUDED IN CMG Reimbursement for this service in included in the CMG
810 SUBMIT TO DENTAL HEALTH VENDOR Please submit this claim to the Dental Health Vendor.
812 NON PAR PROVIDER TIMELY FILING
All claims for non participating Providers must be submitted by 12/31 of the year following the year of
service, or by 12/31 of the second year for care rendered during the last 3 months of the year.
813 INPATIENT COPAYMENTS APPLY The inpatient hospital co-pay applies to these inpatient hospital days.
814 INPATIENT DAYS EXHAUSTED Inpatient hospital days have been exhausted.
855 CONTACT HEALTH SERVICES Please contact our Health Services Department to discuss the Member's treatment.
877 NOT INCLUDED IN DENTAL BENEFIT This service is not covered under the Member's dental benefit.
900 INCLUDED IN APC PRICE Reimbursement for this service is included in the APC reimbursement.
999 ADJUSTMENT This is an adjustment of a previously processed claim.
#C SYSTEM-CAPITATED SERVICE Reimbursement for this claim is included in the capitation payment.
C CAPITATED SERVICE Reimbursement for this claim is included in the capitation payment.
CG CLAIMSGUARD ADJUSTMENT
This claim has been reimbursed according to Medicare and Correct Coding Initiative rules. If you
disagree with this reimbursement, we will review the claim with additional supporting documentation.

31
NATIONAL PROVIDER IDENTIFIER (NPI)
Why the National Provider Identifier?
Providers utilize, in many situations, a different provider identification number for every health plan
they are submitting claims to.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) mandated that the Secretary
of Health and Human Services adopt a standard unique identifier for health care providers called the
National Provider Identifier.
The unique Health Identifier for Health Care Providers rule was published January 23, 2004, with an
effective date of May 23, 2008.
The National Provider Identifier Number
The rule establishes a standard nationally assigned “non intelligent” Provider identifier required to be
used in all electronic health care transactions.
This number will be a 10 digit numeric unique identifier, with an International Standard Organization
(ISO) check digit in the 10th position.
This check digit acts the same way your checking account numbers allow banking institutions to verify
your account number.
A Provider will have one number only and the Provider will use this number for every health plan they
submit electronic transactions too. Once a Provider is enumerated with an NPI this number will not
change ever. The NPI remains with the Provider regardless of job or location change.
Who will have responsibility of issuing the NPI?
The National Provider System (Fox Systems, Inc.) has the sole responsibility for issuing all NPI’s to
every provider in the country. This system is a comprehensive, uniform system for identifying and
uniquely enumerating health care providers at the national level. The Department of Health and Human
Services (DHHS) will have overall responsibility for oversight and management of the system.
How can a Provider apply for an NPI?
There are several methods that a Provider can apply for a NPI number;
1. Phone: 1-800-465-3203
TTY: 1-800-692-2326
2. E-mail: customerservice@npienumerator.com
3. Mail: NPI Enumerator
P.O. Box 6059
Fargo. ND 58108-6059
32
NOTE: If a Provider wishes to obtain a copy of the NPI application form they must call to obtain an
application form. No e-mail or mail requests for applications will be accepted.
Reminder to Providers: A Provider may apply for an NPI using only one of the ways described above.
Make sure that the Provider has a correct Social Security Number (SSN) and Federal employee
identification number when applying.
How do I bill with an NPI number?
The NPI number should be placed in the following boxes on the appropriate claim form:
CMS 1500
Place the NPI in Block 24J
UB92
Place the NPI in Block 56
Additional questions on how to bill an NPI number?
• Refer to: www.cms.gov
• Medicare Claims Processing Manual
o Chapter 26
o Completing and Processing Form CMS 1500 Data Set
33
THE IMPORTANCE OF HIERARCHICAL CONDITION CATEGORIES (HCC)
Effective January 1, 2004, CMS implemented a risk adjustment model in which reimbursement to Medicare
Advantage organizations such as Bravo Health is based on hospital inpatient, hospital outpatient, and
office-based Provider encounter data. This model predicts health cost expenditures by calculating the
disease burden of the population. A Member’s risk is measured by assessing the diagnostic characteristics
(ICD-9) of the Member, rather than assessing what treatments (CPT) they have received.
Provider must document the Member’s conditions and diseases accurately using ICD-9 codes and extend to
the fifth digit where appropriate. This is particularly true for high-risk conditions where co-morbidities
make a significant difference in risk scoring. Diabetes is a perfect example of where ICD-9 code 250 is not
enough to establish the extent of diabetic complications such as neuropathy, blindness and vascular disease.
Chronic conditions must be documented at least once a year to ensure correct risk stratification of the
Member.
Ensure that all diagnosis codes are transferred to the CMS 1500 claim form when billing. For complicated
cases, this may require additional CMS 1500 forms to document more than four diagnoses.
It is important that you document the diagnosis clearly and update the Member’s problem list with each
encounter. Even visits for minor conditions in patients with persistent conditions should be first coded with
the conditions for which the patient is seen and second with accurate co-morbid codes for persistent
conditions like diabetes and CHF. This will ensure that we capture accurate information on your patients
annually. The Member’s name should be recorded on each page of the medical record and the physician
should sign and date each entry.
To meet CMS requirements and to initiate the risk adjustment chart and case management review process,
Bravo Health requires your cooperation in providing access to office medical records. On a regular basis,
you will receive written notification from Bravo Health requesting a chart audit. Please be assured that we
will conduct these audits efficiently and professionally with minimal disruption to your office workflow. In
addition, our certified coders or nurse coders will be glad to come to your office to work with you and/or
your staff to resolve any coding issues that may arise.
34
Sample Explanation of Benefits Statement
Bravo Health Texas, Inc. P8790028002
7551 Callaghan Road, Suite 310 San Antonio, TX 78229
Forwarding Service Requested
TEST
1 0. 3840 SP 0.370 Date: 06/29/2006
liiiiiiiiiiiiiiiiiiiiillillillillillillilliillillillillillillI
Vendor 9370
Get Well Medical Care, P.A. Voucher Number: 64687
PO BOX 3012 Check ID: P6041
San Antonio, TX 78229-1234 Check Number: 058522
Explanation of Payment
Member ID: 449999999 Option: BSEL Provider Acct. No. AB-458518
Member Name: SMITH, JOHN Claim Number: 205062201700120 Provider Name: William Physician
From Date of
Service
To Date of
Service
Service
Code
Billed
Amount
Allowed
Amount
Copay
Coinsurance
Deductible Adjustment Interest Payment Reason
Code
05/13/2008 05/13/2008 99213 253.00 94.49 25.00 0.00 0.00 0.00 69.49
253.00 94.49 25.00 0.00 0.00 0.00 69.49 Claims Totals
Vendor Totals 253.00 94.49 25.00 0.00 0.00 0.00 69.49
Remark Code Explanation
***IF APPLICABLE IMPORTANT INFORMATION REGARDING APPEAL RIGHTS IS ATTACHED***
Sample Bravo Health Payment Check
Bravo Health Texas, Inc. 65-320 CHECK NO.: 0058522
7551 Callaghan Road, Suite 310
San Antonio, TX 78229
AMOUNT
*******69.49
PAY Sixty Nine & 49/100 dollars
TO THE Get Well Medical Care, P.A.
ORDER OF PO BOX 3012
San Antonio, TX 78229-1234
Wachovia Bank N.A.
Philadel
p
hia, PA 19102
35
PRIOR AUTHORIZATION - GENERAL RULES
The following table outlines the general Bravo Health prior authorization and care direction procedures:
Ambulance (Place of Service 41)
No Authorization Required for "911" ambulance service
Only Medicare covered ambulance services. Routine Ambulance NOT COVERED
Behavioral Health Inpatient & Outpatient
Pennsylvania & Mid-Atlantic Contact CompCare : 1-800-541-3647
Texas Contact Corphealth : 1-866-671-4537
Chiropractic
The only codes covered to chiropractic care are: 98940, 98941, 98942, 98943
Clinical Trials
Must Notify Plan (Original Medicare Plan pays for clinical trials with 20% coinsurance to the
Member)
Dental
Pennsylvania & Mid-Atlantic Contact Doral Dental : 1-800-341-8478
Texas Contact StarDent : 1-866-753-6319
Laboratory
Lab services provided by any lab other than those listed below require pre-authorization except for
certain procedures that can be performed in outpatient settings. See appropriate place of service guide
for a list of codes.
Philadelphia & Mid-Atlantic MUST use Quest Labs
Pittsburgh Can use participating hospitals and Quest Labs
Texas Can use Clinical Pathology Lab (CPL) or Quest Labs
Lab services performed at skilled nursing and long term care facilities do not require pre-
authorization.
Non-Participating Providers
NON PARTICIPATING
PROVIDERS
(All non-Participating providers require prior authorization
except Chiropractor, Radiologist and Anesthesiologist, or ER)
Podiatry
Routine Refer to specific plan benefits
Non-Routine Refer to Medicare Coverage Guidelines
Professional Services
Modifier 26 professional component does not require an authorization for Participating or Non
Participating Providers.
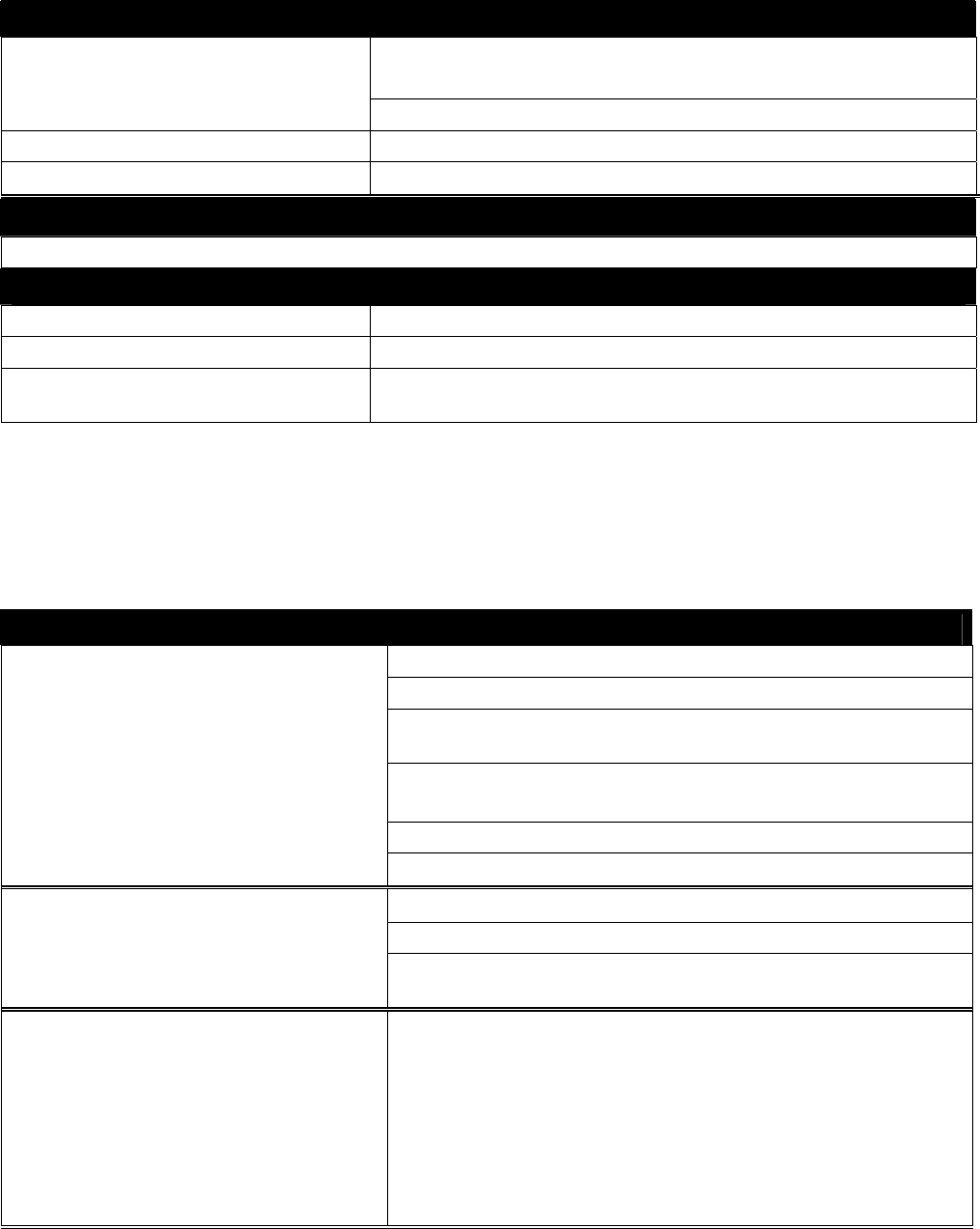
36
Radiology Authorization
Bravo: Contact NIA at 1-800-642-2804 for all procedures
requiring authorization
Pennsylvania Senior Partners: Contact 215-606-6336
Mid-Atlantic & Texas Contact: 1-888-454-0013
All Regions Requests may be faxed to: 1-866-464-0707
Transportation
Benefits vary according to plan. See Quick Reference Guide and Benefit Grid for details.
Vision
Pennsylvania Contact Davis Vision : 1-800-584-3140
Texas Contact OptiCare : 1-866-258-4102
Mid-Atlantic Use Advantica Network – Contact Bravo Health for Customer
Service
PRIOR AUTHORIZATION RULES BY PLACE OF SERVICE
The following tables list outlines the Bravo Health authorization procedures by place of service. Services
listed in the tables require authorization as noted.
In Office (Place of Service 11,32,33)
DURABLE MEDICAL EQUIPMENT Diabetic Shoes
Diabetic Supplies (initial set up only)
DME Purchase (All Medicare Approved) >$200 Per Line
Item
All Prosthetics except mastectomy bras, colostomy
supplies, indwelling Foley catheters
Rentals (All)
Repairs & Maintenance (All)
EDUCATION Diabetic Education Training (Except Senior Partners)
Dialysis Self Training
Nutritional Education Classes (97802-97804) Diabetes and
Renal
LABORATORY Labs (ALL) except these labs performed in Physician's
Office:
81000, 81002, 81003, 81007, 81025, 82010, 82270, 82272,
82570, 82947, 82962, 83026, 83036, 83721, 84478, 84520,
84703, 85013, 85014, 85108, 85610, 87449, 87804, 87880
Providers will be reimbursed for the lab draw (36415) for all
other labs tests not listed above.
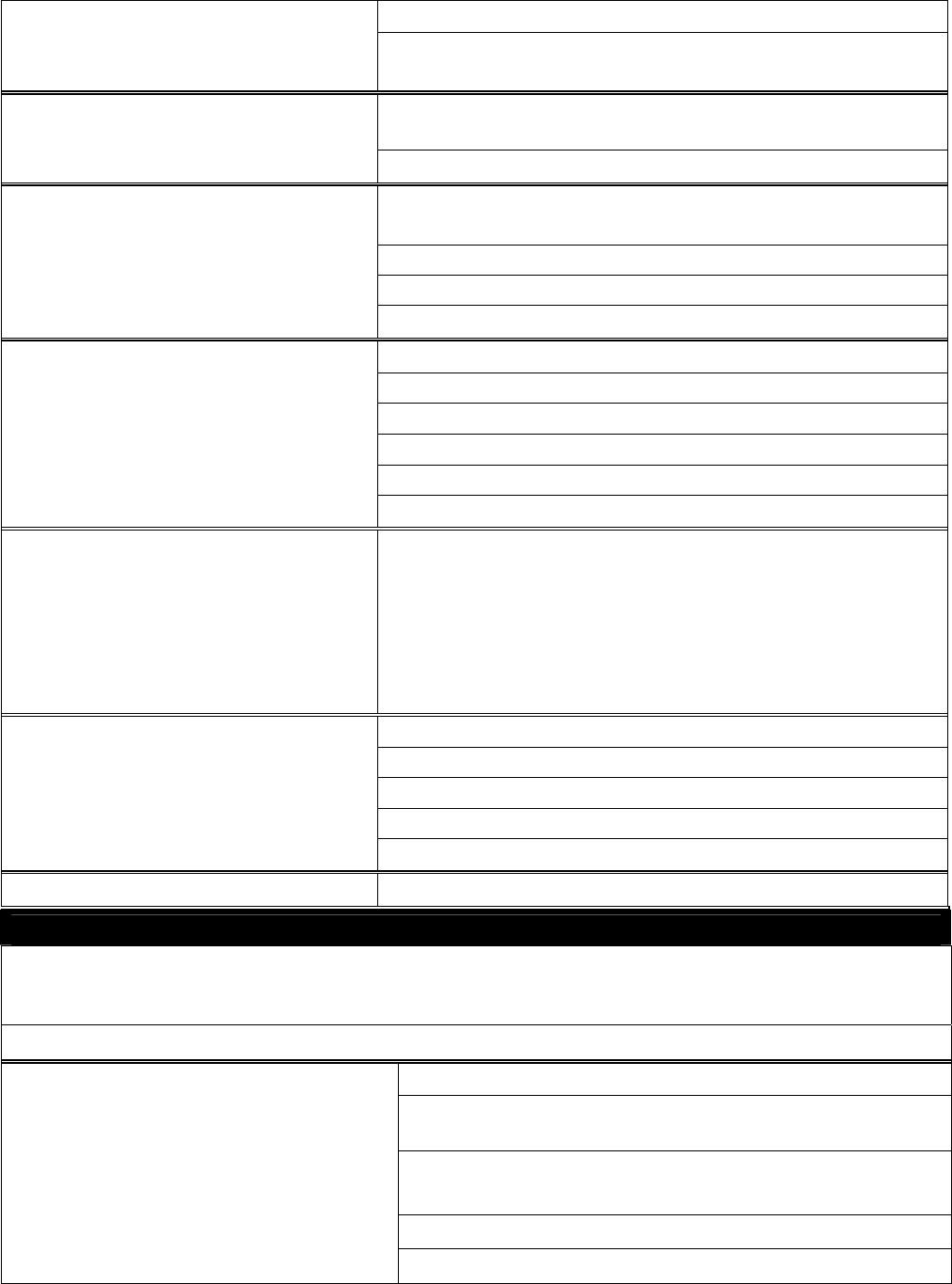
37
MEDICATIONS AND INJECTIBLES Infusion Therapy (except exclusion list) *see pages 43-44
Injectibles (except Flu, Pneumococcal, Tetanus and
Hepatitis B) *see attachment pages 43-44
IMMUNIZATIONS (except Influenza,
Tetanus, Hepatitis B and Pneumovax)
Immunizations for Travel
Enhanced External Counter Pulsation (ECP) G0166 (limited
to 35 visits per 12 month period)
Hyperbaric Oxygen Therapy
Interventional Radiology
OUT-PATIENT SERVICES
Thoracic Stress Echo
RADIOLOGY CT Scans
MRA
MRI
ALL Nuclear Medicine including Nuclear Cardiology
PET Scans
Stress Echo
RADIATION THERAPY Intensity-Modulated Radiation Therapy (IMRT) - Prior
authorization is required only for elective admission. A
course of therapy occurring as part of an inpatient
confinement that has met medical necessity criteria and been
authorized does not require separate authorization.
Cardiac Rehabilitation
Occupational Therapy (after 1st 12 visits)
Physical Therapy (after 1st 12 visits)
THERAPY /REHABILITATION
Pulmonary Rehabilitation
Speech Therapy (except initial evaluation)
Inpatient (Place of Service 21,31,51,61)
Note: Emergency and urgent admissions do not require prior authorization. Medical necessity criteria will be
applied after facility’s notification to Bravo Health. Authorization for claims payment will only be granted to
those meeting medical necessity criteria.
The following services do require authorization as outlined below:
Diabetic Supplies (initial set up only)
DME Purchase (All Medicare Approved) >$200 Per Line
Item
All Prosthetics except mastectomy bras, colostomy
supplies, indwelling Foley catheters
Rentals (All)
DURABLE MEDICAL EQUIPMENT
Repairs & Maintenance (All)
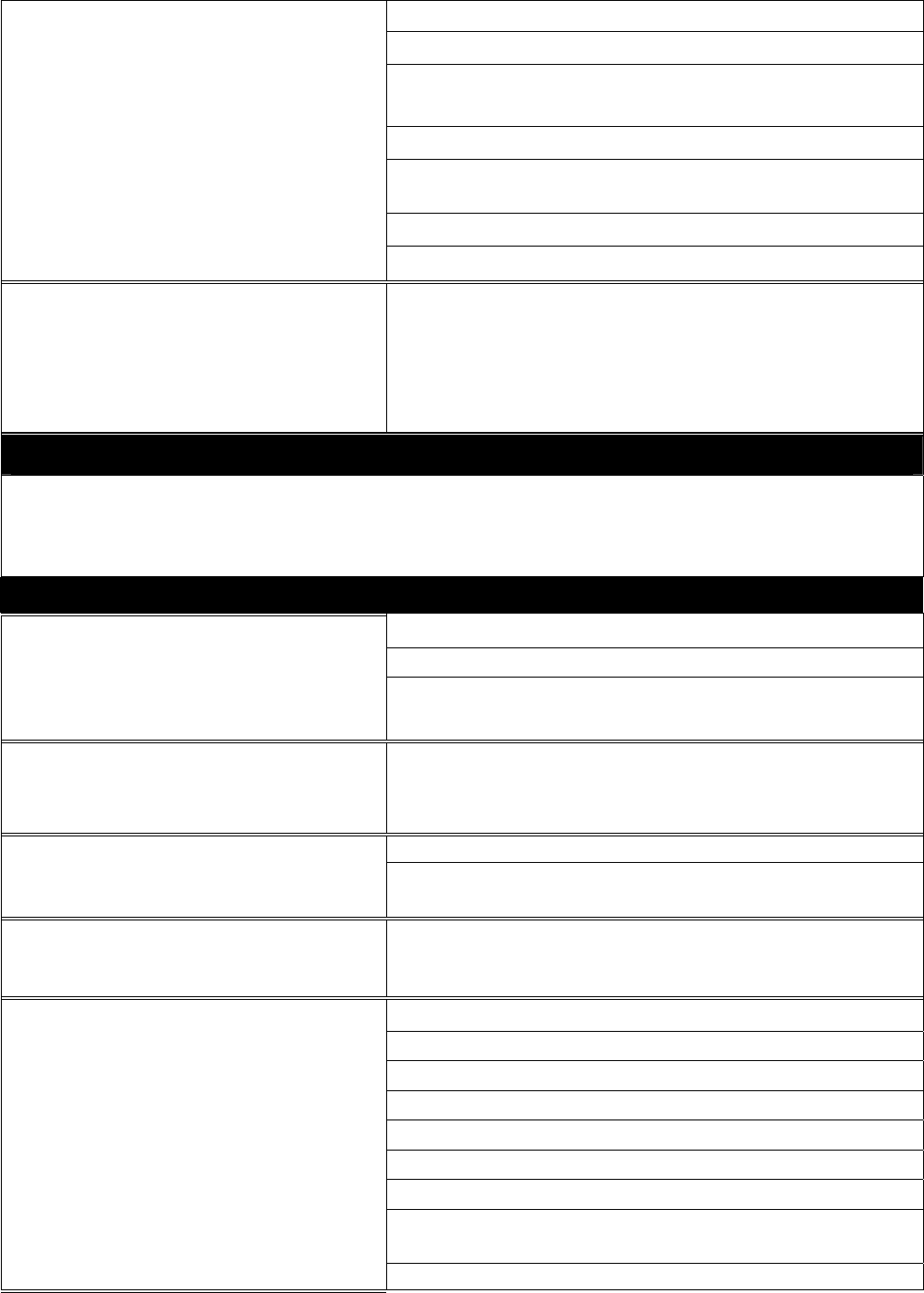
38
Acute Hospital Admissions (All)
Acute Rehab Admissions (All)
Behavioral Health Hospital Admissions (CompCare or
Corphealth) *See Behavioral Health
Elective Admissions (All)
Long Term Acute Care Hospital Admissions (LTACH)
(All)
Skilled Nursing Admissions (All)
INPATIENT SERVICES
Sub acute Admission (All)
RADIATION THERAPY
Intensity-Modulated Radiation Therapy (IMRT) - Prior
authorization is required only for elective admission. A
course of therapy occurring as part of an inpatient
confinement that has met medical necessity criteria and
been authorized does not require separate authorization.
Emergency Room/Urgent Care (Place of Service 20&23)
No Authorizations are required
Outpatient Hospital (Place of Service 22)
Diabetic Education Training (Except Senior Partners)
Dialysis Self Training
EDUCATION
Nutritional Education Classes (97802-97804) Diabetes
and Renal
LABORATORY Labs (ALL) except these labs that may be performed in
Physician's Office: 85018, 82947, 82962, 81000, 81002,
81003, 81005, 86308, 86403-86406
Infusion Therapy (except exclusion list) *see pages 43-44 MEDICATIONS AND INJECTIBLES
Injectibles (except Influenza, Pneumococcal, Tetanus and
Hepatitis B) *see attachment
IMMUNIZATIONS (except
Influenza, Tetanus, Hepatitis B and
Pneumovax) Immunizations for Travel
Allergy Testing (95004-95199)
Audiologic Function Test (92551-92597)
Blood Transfusions
Bronchoscopy
Cardiac Catheterization
OUTPATIENT SERVICES
Chemotherapy (includes all IM, SQ, and IV injections)
Colonoscopy, Diagnostic
Enhanced External Counter Pulsation (ECP) G0166
(limited to 35 visits per 12 month period)
Electroencephalogram (EEG) w/ video monitoring 48 hrs
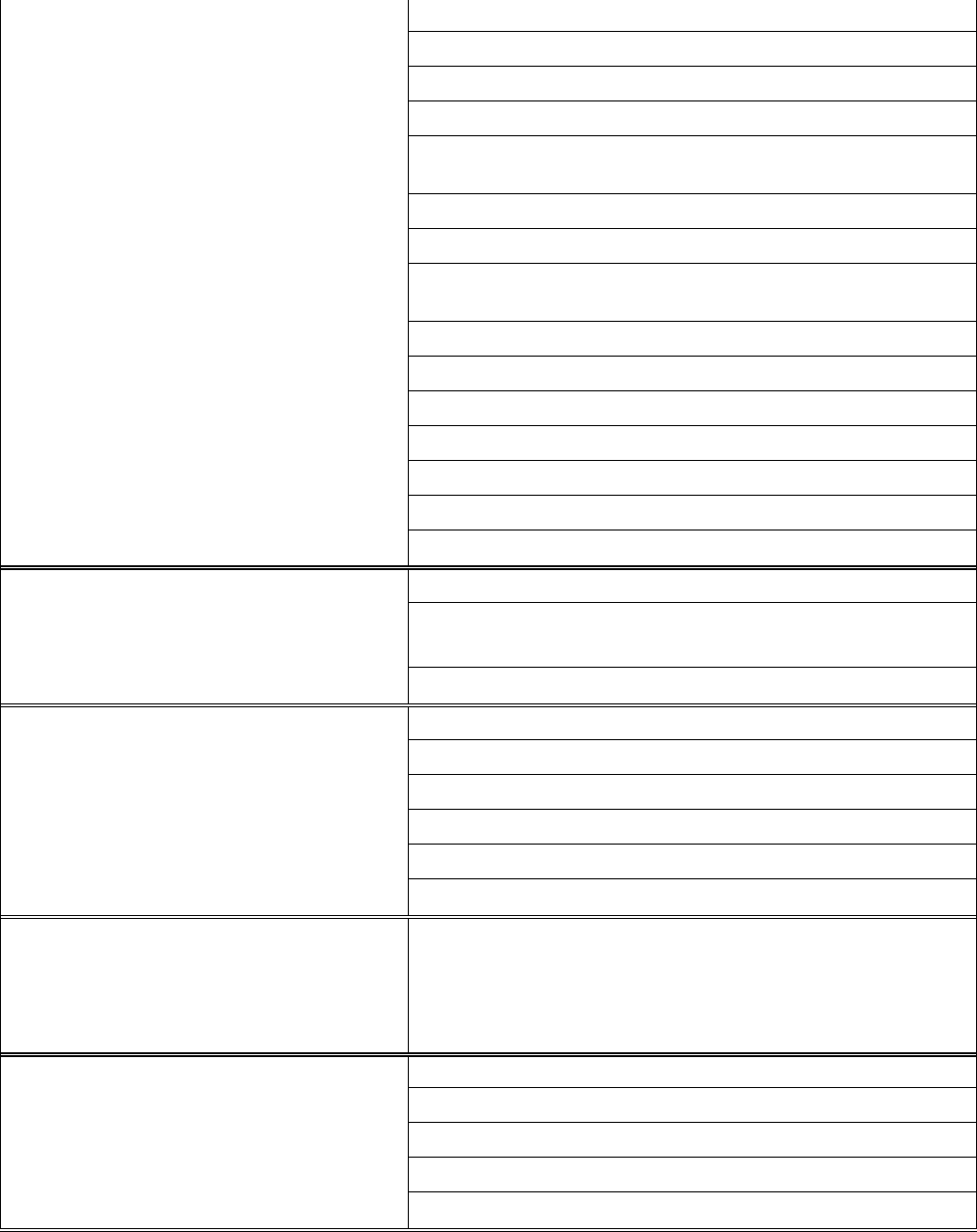
39
Endoscopy Procedures
Gastroenterology (91000-91299)
Hyperbaric Oxygen Therapy
Interventional Radiology
Intracardiac Electrophysiological Procedures (93600-
93668)
Neurological Testing (95812-96120)
Out-Patient Therapy *see therapy for auth rule
Pain Management Epidural 64400-64530 (ASC approval
after 3rd inject) *Performed by Anesthesiologist
Pulmonary Testing (94010-94799)
Regulated Space (Maryland only)
Sleep Studies
Surgery
Thoracic Stress Echo
Vestibular Function Test (92531-92548)
Wound Management
Hearing Exams
Non-Participating Providers except Anesthesiologists
*Refer to Pain Management
PROFESSIONAL SERVICES
Non-Participating except chiropractors
CT Scans
MRA
MRI
ALL Nuclear Medicine including Nuclear Cardiology
PET Scans
RADIOLOGY
Stress Echo
RADIATION THERAPY Intensity-Modulated Radiation Therapy (IMRT) - Prior
authorization is required only for elective admission. A
course of therapy occurring as part of an inpatient
confinement that has met medical necessity criteria and
been authorized does not require separate authorization.
Cardiac Rehabilitation
Occupational Therapy (after 1st 12 visits)
Physical Therapy (after 1st 12 visits)
Pulmonary Rehabilitation
THERAPY /REHABILITATION
Speech Therapy (except evaluation)
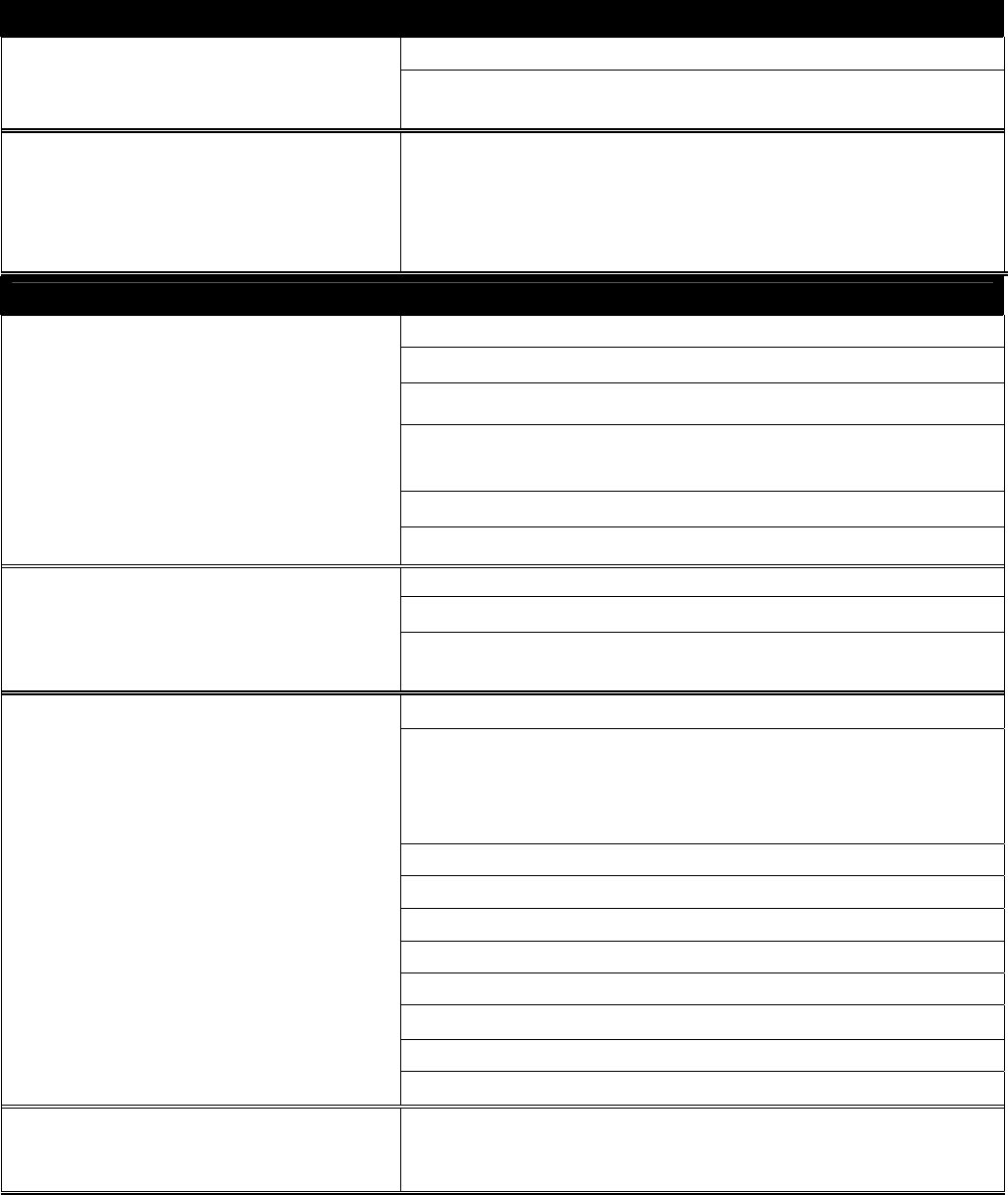
40
Ambulatory Surgery Center (Place of Service 24)
Interventional Radiology
OUTPATIENT SERVICES
Pain Management Epidural 64400-64530 (ASC approval
after 3rd inject) *Performed by Anesthesiologist
RADIATION THERAPY Intensity-Modulated Radiation Therapy (IMRT) - Prior
authorization is required only for elective admission. A
course of therapy occurring as part of an inpatient
confinement that has met medical necessity criteria and been
authorized does not require separate authorization.
Home Health Services (Place of Service 12)
Diabetic Shoes
Diabetic Supplies (initial set up only required)
purchase ( Medicare Approved) >$200 Per Line Item
Prosthetics except mastectomy bras, colostomy supplies,
indwelling Foley catheters
Rentals
DURABLE MEDICAL
EQUIPMENT
Repairs & Maintenance
Diabetic Education Training
Dialysis Self Training
EDUCATION
Nutritional Education Classes (97802-97804) Diabetes and
Renal
HOME HEALTH SERVICES Aide
Primary Care Physicians (PCPs) may see
Members in their home without prior
authorization
Dialysis in Home
Infusion
Nurse
Occupational Therapy
Physical Therapy
Specialist Physician Home Visits (except Podiatry)
Speech Therapy
Wound Management
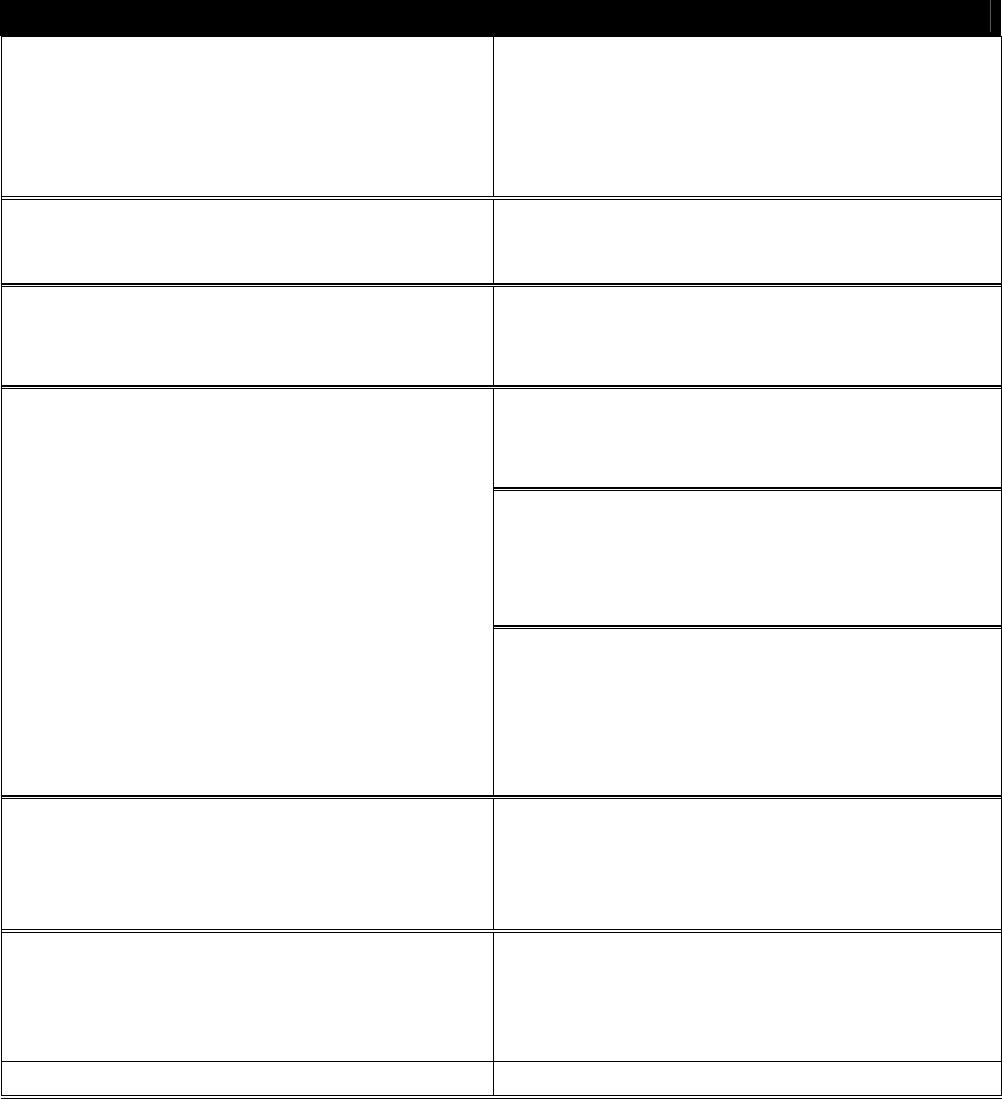
41
PREVENTIVE CARE
The following Preventive Health Care Services DO NOT require authorization:
Preventive Care
Abdominal Aortic Aneurysm Ultrasound: A
one-time screening ultrasound for people at risk
(like people who have smoked).
Influenza Vaccine (once a year in fall winter)
Bone Mass Measurements [Dexascan]:
Every 24 months; more often if medically
necessary
Glaucoma Test: once every 12 months)
indicated for those at high risk for glaucoma
Cardiovascular Testing: Electrocardiogram
and cardiovascular blood screenings to check
cholesterol and other blood fat (lipid) levels
Hepatitis B Vaccine: Three shots are needed for
complete protection. Indicated for those at
medium to high risk for Hepatitis B.
Medical Nutrition Therapy Services: For
Members with diabetes or kidney disease and
your doctor refers you for the service
Mammogram: once every 12 months for
Members 40 years and older)
Colorectal Screening: Fecal Occult Blood Test
once every 12 months if age 50 or older.
OR
Flexible sigmoidoscopy generally, once every
48 months if age 50 or older, for those not at
high risk, 120 months after a previous screening
colonoscopy
OR
Screening Colonoscopy generally once every
120 months (high risk every 24 months), 48
months after a previous flexible sigmoidoscopy.
No minimum age.
Pap & Pelvic Exams: Once every 24 months for
women at low risk, and once every 12 months for
women at high risk and for women of child-
bearing age who have had an exam that indicated
cancer or other abnormalities in the past three
years
Colorectal Screening: Barium Enema - once
every 48 months if age 50 or older (high risk
every 24 months) when used instead of a
sigmoidoscopy or colonoscopy.
Pneumococcal Vaccine: Generally once per
lifetime
Diabetes Screening (Fasting Plasma Glucose
Test): Member may be eligible for up to two
screenings each year
*see definition for coverage
Prostate Cancer Screening: Digital Rectal
Examination once every 12 months;
Prostate Specific Antigen (PSA) Test once every
12 months
Routine Physical Exams
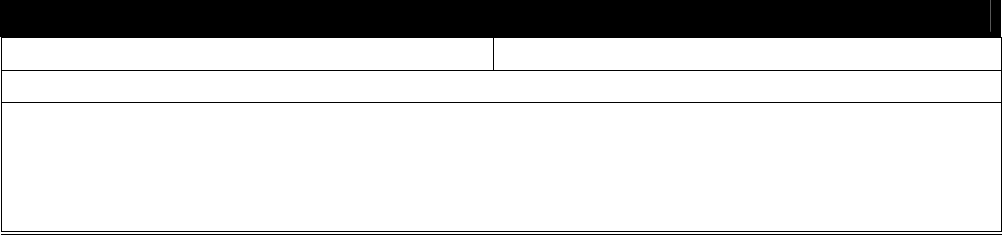
42
Health & Wellness
ForEver Fit Texas
Health Education Mailings
Smoking Cessation. Includes counseling for two cessation attempts within a 12-month period for
Members diagnosed with smoking-related illness or are taking medicines that may be affected by
stop smoking tobacco. Counseling for each cessation attempt includes up to four face-to-face visits.
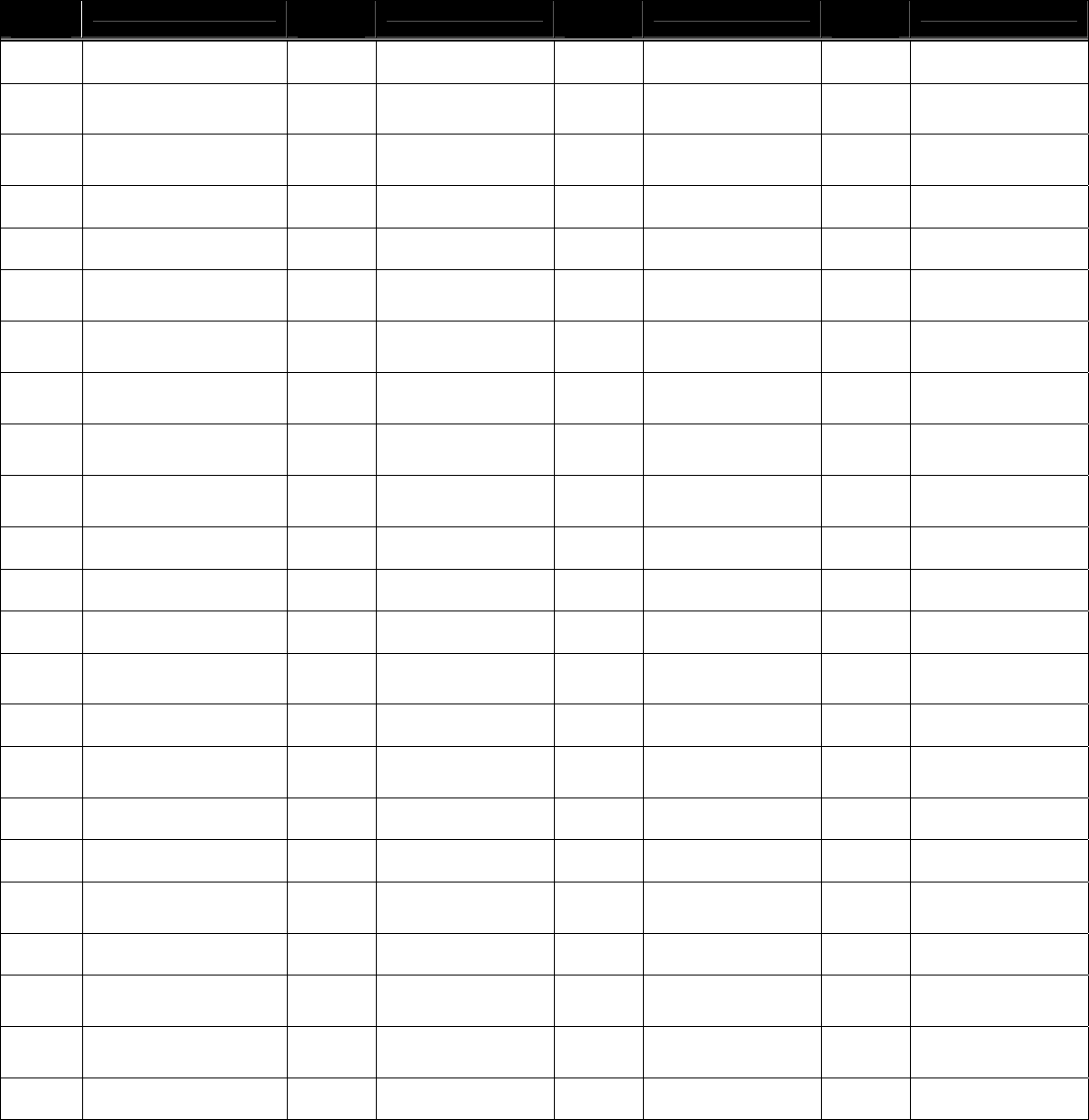
43
PRIOR AUTHORIZATION – MEDICINES AND INJECTIBLES
The following list of drugs requires authorization under the Medicare Part B Benefit:
HCPCS
Code
Short Description HCPCS
Code
Short Description HCPCS
Code
Short Description HCPCS
Code
Short Description
J0129 Abatacept, inj J0735 Clonidine
hydrochloride
Q2009 Fosphenytoin, 50 mg J9230 Mechlorethamine hcl
inj
J0130 Abciximab injection J0770 Colistimethate
sodium inj
J1458 Galsulfase, inj J7669 Metaproterenol non-
comp unit dose
J7608 Acetylcysteine inh sol u J0800 Corticotropin
injection
J1560 Gamma globulin >
10 CC inj
J7674 Methacholine
chloride, neb
J0132 Acetylcysteine injection J7631 Cromolyn sodium inh
sol u d
J1460 Gamma globulin 1
CC inj
J7505 Monoclonal
antibodies
J0135 Adalimumab injection J7330 Cultured
chondrocytes implnt
J1550 Gamma globulin 10
CC inj
Q4079 Natalizumab
injection
J0180 Agalsidase beta injection J9100 Cytarabine hcl 100
MG inj
J1470 Gamma globulin 2
CC inj
J9261 Nelarabine injection
Q4093 Albuterol inh non-comp
con (Initial auth only)
J9110 Cytarabine hcl 500
MG inj
J1480 Gamma globulin 3
CC inj
Q4087 Octagam Injection
Q4094 Albuterol inh non-comp
u d (Initial auth only)
J9098 Cytarabine liposome J1490 Gamma globulin 4
CC inj
J2357 Omalizumab
injection
J7620 Albuterol ipratrop non-
comp
J0850 Cytomegalovirus
imm IV /vial
J1500 Gamma globulin 5
CC inj
J2355 Oprelvekin injection
J9015 Aldesleukin/single use
vial
J9130 Dacarbazine 100 mg
inj
J1510 Gamma globulin 6
CC inj
Q4086 Orthovisc, inj
J0215 Alefacept J9140 Dacarbazine 200 MG
inj
J1520 Gamma globulin 7
CC inj
J9263 Oxaliplatin
J9010 Alemtuzumab injection J7513 Daclizumab,
parenteral
J1530 Gamma globulin 8
CC inj
J9265 Paclitaxel injection
J0205 Alglucerase injection J9120 Dactinomycin
actinomycin d
J1540 Gamma globulin 9
CC inj
J9264 Paclitaxel protein
bound
J0256 Alpha 1 proteinase
inhibitor
J1645 Dalteparin sodium Q4088 Gammagard Liquid
injection
J2425 Palifermin injection
J0270 Alprostadil for injection J0882 Darbepoetin alfa,
esrd use
Q4092 Gamunex injection J2469 Palonosetron HCl
J0275 Alprostadil urethral
suppos
J0881 Darbepoetin alfa,
non-esrd
J7310 Ganciclovir long act
implant
J2430 Pamidronate
disodium /30 MG
J2997 Alteplase recombinant J9150 Daunorubicin J9201 Gemcitabine HCl J2504 Pegademase bovine,
25 iu
J0207 Amifostine J9151 Daunorubicin citrate
liposom
J9300 Gemtuzumab
ozogamicin
J2503 Pegaptanib sodium
injection
J0288 Ampho b cholesteryl
sulfate
J0894 Decitabine, inj J9202 Goserelin acetate
implant
J9266 Pegaspargase/singl
dose vial
J0285 Amphotericin B J0895 Deferoxamine
mesylate inj
Q4090 HepaGam B IM
Injection
J9305 Pemetrexed injection
J0287 Amphotericin b lipid
complex
J9160 Denileukin diftitox,
300 mcg
J9225 Histrelin implant J9268 Pentostatin injection
J0289 Amphotericin b liposome
inj
J1190 Dexrazoxane HCl
injection
Q4083 Hyalgan or Supartz,
inj
J9600 Porfimer sodium
J0348 Anadulafungin injection J1162 Digoxin immune fab
(ovine)
J3470 Hyaluronidase
injection
J2783 Rasburicase
Continued on next page
44
J7198 Anti-inhibitor J0470 Dimecaprol injection J3473 Hyaluronidase,
recombinant, inj
Q4095 Reclast injection
J7197 Antithrombin iii injection J1212 Dimethyl sulfoxide
50% 50 ML
J1740 Ibandronate sodium,
inj
J2993 Reteplase injection
J7511 Antithymocyte globuln
rabbit
J9170 Docetaxel J1742 Ibutilide fumarate
injection
Q4089 Rhophylac injection
J0364 Apomorphine hcl, inj J7639 Dornase alpha inhal
sol u d
J9211 Idarubicin hcl
injection
J2794 Risperidone, long
acting
J0365 Aprotonin, 10,000 kiu J9001 Doxorubicin hcl
liposome inj
Q4080 Iloprost inhalation
solution
J9310 Rituximab cancer
treatment
J9017 Arsenic trioxide J0600 Edetate calcium
disodium inj
J1566 Immune globulin,
powder
J2820 Sargramostim
injection
J9020 Asparaginase injection J0886 Epoetin alfa, esrd on
dialysis
J1745 Infliximab injection J2941 Somatropin injection
J0475 Baclofen 10 MG injection Q4081 Epoetin alfa, for
ESRD on dialysis
J9065 Inj cladribine per 1
MG
J9320 Streptozocin
injection
J0476 Baclofen intrathecal trial J0885 Epoetin alfa, non-
esrd
J0835 Inj cosyntropin per
0.25 MG
J3030 Sumatriptan
succinate / 6 MG
J0480 Basiliximab J1325 Epoprostenol
injection
J1650 Inj enoxaparin
sodium
Q4084 Synvisc, inj
J9031 Bcg live intravesical vac J1327 Eptifibatide injection J9245 Inj melphalan
hydrochl 50 MG
J7525 Tacrolimus injection
J9035 Bevacizumab injection J1438 Etanercept injection J2260 Inj milrinone lactate /
5 MG
J7507 Tacrolimus oral per 1
MG
J0583 Bivalirudin J1430 Ethanolamine oleate
100 mg
J2850 Inj secretin synthetic
human
J3100 Tenecteplase
injection
J9040 Bleomycin sulfate
injection
J9181 Etoposide 10 MG inj J3305 Inj trimetrexate
glucoronate
Q2017 Teniposide, 50 mg
J9041 Bortezomib injection J9182 Etoposide 100 MG
inj
J7187 Inj Vonwillebrand
factor IU
J9340 Thiotepa injection
J0585 Botulinum toxin a per unit Q4085 Euflexxa, inj J9178 Inj, epirubicin hcl, 2
mg
J3240 Thyrotropin injection
J0587 Botulinum toxin type B J7194 Factor ix complex J1595 Injection glatiramer
acetate
J1655 Tinzaparin sodium
injection
J7626 Budesonide non-comp
unit dose
J7193 Factor IX non-
recombinant
J2505 Injection,
pegfilgrastim 6mg
J7682 Tobramycin non-
comp unit dose
J0594 Busulfan, inj J7195 Factor IX
recombinant
J1817 Insulin for insulin
pump use
J9350 Topotecan
J9045 Carboplatin injection J7189 Factor viia J1830 Interferon beta-1b /
.25 MG
J9355 Trastuzumab
J9050 Carmus bischl nitro inj J7190 Factor viii J7644 Ipratropium bromide
non-comp
J3285 Treprostinil injection
J0637 Caspofungin acetate J7192 Factor viii
recombinant
J9206 Irinotecan injection J3315 Triptorelin pamoate
J9055 Cetuximab injection J1440 Filgrastim 300 mcg
injection
J1945 Lepirudin J3355 Urofollitropin, 75 iu
J0725 Chorionic
gonadotropin/1000u
J1441 Filgrastim 480 mcg
injection
J1950 Leuprolide acetate
/3.75 MG
J3365 Urokinase 250,000
IU inj
J0740 Cidofovir injection Q4091 Flebogamma
injection
J9219 Leuprolide acetate
implant
J3370 Vancomycin hcl
injection
J0743 Cilastatin sodium injection J9200 Floxuridine injection J9218 Leuprolide acetate
injeciton
J3396 Verteporfin injection
J9060 Cisplatin 10 MG injection J9185 Fludarabine
phosphate inj
J9217 Leuprolide acetate
suspnsion
J1562 Vivaglobulin,
injection
J9062 Cisplatin 50 MG injection J7311 Fluocinolone
acetonide implt
J2020 Linezolid injection J3487 Zoledronic acid
J9027 Clofarabine injection J1652 Fondaparinux sodium J7504 Lymphocyte immune
globulin
45
Prior Authorization Request
Please fax to: 1-866-464-0707
Or call 1-888-454-0013, extension 336336
TX Bexar Harris El Paso
Type of Request Elective Expedited Date/Time Rec’d
Member Name ID# DOB:
PCP/Requesting Provider Office Contact Person
Phone#: Fax# e-mail:
Referring To: Specialty/Facility:
Service Requested ASC Out-Patient Hospital In -Patient Office Procedure
DME Home Health PT/OT/ST Medications
Type of Service
Medical Surgical
Service Description
Procedure Description
Date of Procedure:
Participating Provider/Facility:
Non-Participating Provider/Facility:
Reason if requesting non par
facility/Provider:
Diagnosis Codes: Procedure Codes:
Suppporting Clinical Information Attached? Yes No
(If no, was additional Information requested ?) Yes No Date Requested:
Comments:
For Office Use
Pre Cert Specialist
Medical Director Determination: Certified Not Certified
Medical Director Date
46
QUALITY IMPROVEMENT PROGRAM
Bravo Health is committed to providing access to quality healthcare for all Members in all product
lines through the continuous study, implementation and improvement of care to our Members. Quality
Improvement (QI) assumes that there is no permanent threshold for good performance. Our Members
expect and should be provided a comprehensive and therapeutic health care delivery system that is
always evolving and improving.
The Quality Improvement Department accomplishes this by integrating, analyzing, and reporting on
data from across the Plan as well as other data sources. The QI Department prioritizes quality
initiatives based on relevance to the Plan. QI works with internal Bravo Health departments to manage
plan resources in the most cost effective manner to maximize patient health outcomes. The following
is a brief overview of the QI Department’s functions.
The QI Department works on internal and external reporting of quality of care and risk management
concerns. Substantial QI/Risk Management is presented to the Quality Improvement Committee
(QIC) to formulate corrective action plans and monitor the results.
The QI Department assists Senior Management and the Medical Director in the coordination of the
Quality Improvement activities. The QIC is charged with providing oversight (identification,
prioritization, and coordination) of all quality improvement activities related to the care and service of
our Members.
The QI Department coordinates with various internal departments on mandatory Centers for Medicare
and Medicaid Services (CMS) audits such as Healthcare Plan Effectiveness Data and Information Set
(HEDIS) and The Health Outcomes Survey (HOS). QI also contributes to Bravo Health’s annual CMS
site visit and quality reviews by the Pennsylvania Department of Health.
The QI department works to maintain optimal health outcomes for our Members through annual
review of best practice standards. Preventive standards are derived from The United States Preventive
Services Task Force Standards (USPSTF), which are derived from the American Diabetes
Association, the American Cancer Society as well as other nationally recognized organizations.
Guidelines are revised and modified to reflect the latest in preventive best practices.
If you have any questions about Bravo Health’s Quality Improvement Program, or would like a
comprehensive description of The QI Program, QI Program Annual Goals, or a list of activities
towards achieving those goals, please feel free to contact Bravo Health’s Quality Improvement
Department at:
Bravo Health, Inc.
3601 O'Donnell Street
Baltimore, MD 21224
Information will be provided upon request.
47
QUALITY IMPROVEMENT PROGRAM
A. Goals
• Coordinate all quality management audits and quality improvement activities through the
QIC;
• Monitor and evaluate the quality of clinical healthcare, service quality, process
improvement, Member and Provider satisfaction, complaint/grievance resolution and
Provider network credentialing/re-credentialing;
• Monitor and evaluate Provider practice patterns, develop improvement plans as needed,
and review performance to assess whether improvements have occurred;
• Promote and monitor preventive health services;
• Identify educational needs of Members, Providers, customers, and staff, and develop
resources to meet those needs;
• Maintain accurate data to ensure QI Program integrity;
• Ensure compliance with applicable accreditation and regulatory requirements;
• Conduct an annual review of all QI actions, assessing the improvement achieved through
the initiatives of the QI Work Plan, and revising the Work Plan when necessary;
• Document and share improvements in healthcare delivery as a result of QI initiatives.
B. Quality Improvement Committee (“QIC”)
The QIC is responsible for the overall design and implementation of quality improvement activities for
the organization, as well as for the oversight of QI activities carried out by other committees and reports
these activities to the Board of Directors. The QIC ensures that all quality improvement tasks and
functions are a reflection of Membership involvement, the participation of Participating Providers, and
the compliance with all applicable regulatory and accreditation mandates.
Healthcare Effectiveness Data and Information Set (HEDIS®)
HEDIS® (a standardized data set) is developed and maintained by the National Committee for Quality
Assurance (NCQA), an accrediting body for managed care organizations. The HEDIS® measurements
enable comparison of performance across plans. The sources of HEDIS® data include administrative
data (claims/encounters) and medical record review. HEDIS® measurements include measures such as
Comprehensive Diabetes Care, Adult Access to Ambulatory and Preventive Care, Glaucoma Screening
for Older Adults, Controlling High Blood Pressure, and Breast Cancer Screening.
Plan-wide HEDIS® measures are reported annually and is a mandated activity for Health Plans
contracting with The Centers for Medicare and Medicaid Services (CMS).
All records are handled in accordance with Bravo Health’s privacy policies and in compliance with the
Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule. Only the minimum
necessary amount of information, which will be used solely for the purpose of this HEDIS® initiative,
will be requested. HEDIS® is considered a quality related health care operation activity and is
permitted by the HIPAA Privacy Rule [see 45 CFR 164.501 and 506].
Bravo Health HEDIS® results are available upon request. Contact the Health Plan’s Quality
Improvement Department.
48
ON-SITE ASSESSMENTS
On-site facility assessments are performed to assess the quality of care and services provided by
prospective or Participating Providers. Structural elements of quality care and services are evaluated.
On-site evaluations must be performed for all PCPs, OB/GYNs, and high volume Behavioral Health
Providers prior to initial credentialing and re-credentialing.
Components assessed during an on-site evaluation include, but are not limited to, the following:
Office Standards
1. Facility appearance, cleanliness
2. Access to services
3. Administrative/organizational structure
4. Policy and procedure manuals
5. Personnel
6. Confidentiality
7. Fire/safety/emergency
8. Patient care services
9. Ancillary services
10. Medical records organization and maintenance according to CMS and NCQA Medical record
documentation standards.
11. Safety and emergency procedures
12. Member-oriented educational material
13. Advance Directives and Treatment Planning
Medical Record Review
Confidentiality of Records: Participating Providers and Bravo Health agree that all Members’ medical
records shall be treated as confidential to comply with state and federal laws regarding confidentiality of
medical records. However, nothing shall limit timely dissemination of such records to authorized
Providers and consulting physicians, to governmental agencies as required and permitted by law, to
accrediting bodies, to committees of Provider and Plan concerned with the quality of care and utilization
and to Plan for purposes of administration. To the extent permitted by law, Plan shall have the right to
inspect at all reasonable times any medical records maintained by Provider pertaining to Plan’s
Members. Provider agrees to maintain all patient records pertaining to treatment of Members for a
period of ten (10) years.
Medical Records shall not be removed or transferred from Provider except in accordance with general
Provider policies, rules and regulations. Providers agree to furnish Members timely access to their own
records.
Bravo Health may audit a Provider’s medical records, for Bravo Health Members, as a component of
Bravo Health’s quality improvement, credentialing and re-credentialing processes. In accordance with
AMA guidance and NCQA guidelines, medical records must be legible with current details organized
and comprehensive in order to facilitate the assessment of the appropriateness of care rendered.
Documentation audits are performed to assure that Primary Care Physicians maintain a medical record
system that permits prompt retrieval of information. They are also performed to assure that medical
records are legible, contain accurate and comprehensive information and are readily accessible to health
care Providers. Medical record review also provides a mechanism for assessing the appropriateness and
continuity of health care services. Applicable regulations mandate medical record review by Bravo
Health.
49
Criteria (indicators) to be evaluated must include, but are not limited to, the following:
1. Demographic/personal data are noted in the record, complete patient name, date of birth, home
address and phone number, sex, marital status, insurance, and Member identification number
2. An emergency contact person’s name, address, and phone number, or that there is no contact person
is noted in the medical record
3. Each page of the medical record contains patient’s name or Bravo Health identification number
4. All entries are legible, signed and dated
5. Significant illness, medical and psychological conditions are indicated on the medical list
6. Prescribed medications, including dosage, date of initial and/or refill prescriptions are listed
7. Allergies and adverse reactions to medications are prominently noted in the record
8. Appropriate past medical history in the medical record
9. History and physical are included in the record
10. The working diagnosis are consistent with the findings
11. Treatment plans are consistent with the diagnosis and is noted on every visit note
12. There is documentation that the Member participated in the formulation of the treatment plan
13. All diagnostic and therapeutic services for which a Member was referred for are in the medical
record and there is evidence that the practitioner reviewed these reports
14. There is explicit notation in the medical record of follow-up plans related to consultation, abnormal
laboratory, and imagining study results
15. Chronic or unresolved problems from previous visits are addressed in subsequent visits
16. There is no evidence that the patient is placed at risk by a diagnostic or therapeutic procedure
17. There is evidence of patient/significant other teaching
18. There is evidence that medical care is offered in accordance to Bravo Health clinical care guidelines
19. The medical record contains appropriate notation concerning use of alcohol, cigarettes and
substance abuse
20. There is notation regarding follow-up care, calls or visits
21. The specific time of return is noted in days, weeks, months, or as needed
22. There is a separate medical record for each patient
23. The documentation is consistent with ICD-9 codes
24. Only authorized staff have access to medical records
25. Medical records are easily located and retrieved
26. Forms used for documentation are consistent in all records
27. There is a completed immunization record in accordance with the organization’s adult preventive
guidelines
28. Chart is orderly
29. Preventive screenings/services are recommended
30. There is documentation of a discussion of a living will or advance directives for patients 65 years of
age or older/or patients with life threatening conditions
31. Clinical findings/evaluations are documented
Provider must meet these requirements for medical record keeping. If opportunities for quality
improvement are identified, Bravo Health will present these opportunities and implement interventions.
50
HEALTH SERVICES
Bravo Health utilization management staff base their utilization-related decisions on the clinical needs
of its Members, the Member’s Benefit Plan, the appropriateness of care, Medicare National Coverage
Guidelines, objective, scientifically-based clinical criteria and treatment guidelines, in the context of
Provider and/or Member supplied clinical information and other such relevant information.
Bravo Health in no way rewards or offers incentives, either financially or otherwise, practitioners,
utilization reviewers, clinical care managers, physician advisers or other individuals involved in
conducting utilization review, for issuing denials of coverage or service, or inappropriately restricting
care.
If you have any further questions or comments, please feel free to contact our Provider Services
Department at 1-888-353-3789.
Goals
• To ensure that services are authorized at the appropriate level of care and are covered under the
Member’s health plan benefits.
• To monitor utilization practice patterns of Bravo Health’s Contracted Physicians, Contracted
Hospitals, and Contracted ancillary services,
• To provide a system to identify high-risk Members and ensure that appropriate care is accessed.
• To provide utilization management data for use in the process of re-credentialing Providers.
• To educate patients, physicians, contracting hospitals, ancillary services, and specialty Providers
about the company’s goals for providing quality, value enhanced managed health care.
• To improve utilization of Bravo Health’s resources by identifying patterns of over and under
utilization that can be improved upon.
Clinical Review Guidelines
Bravo Health has approved the following guidelines to be used for determining medical necessity and the
appropriateness of care:
• InterQual™ Criteria Guidelines, (ISP, ISX, ISD and SAC)
• Utilization Management Policies and Procedures
• Technology Assessment
• Medicare National Coverage Decision Guidelines
• ASAM for Chemical Dependency and current literature and regulatory requirements for Mental
Health Services (MHN)
• Evidence of Coverage, consistent with the contract definition of Medical Necessity.
Utilization Review decisions approving or denying payment of a service shall be based on the medical
necessity and appropriateness of requested service, the Member’s individual circumstances, and the
appropriate contract language concerning benefits and exclusion.
All criteria utilized are available to any healthcare Provider upon written or verbal request.
51
Bravo Health and delegated utilization review entities will involve actively practicing Providers in its
development of criteria and in the development and review of procedures in applying the criteria. Clinical
criteria will be reviewed regularly and shall be modified as required to reflect current medical standards.
PROSPECTIVE REVIEW PROCESS
Bravo Health requires prospective review of non-urgent/non-emergent procedures that require the use of
a facility other than the office. InterQual™, internally developed clinical guidelines, CMS guidelines,
National Decision Coverage Guidelines and Health Plan benefits/contract and coverage guidelines are
used to help make medical necessity determinations.
Decision Time Frames
Prospective review decisions on outpatient and inpatient elective procedures will be determined and
communicated electronically or in writing to Bravo Health , the Member and the healthcare Provider
within 14 days of receipt of the request. Bravo Health or the Member may extend this period an
additional 14 days if the delay is in the best interest of the Member. If the service requested can
adversely affect the Member’s life or function, an expedited determination may be made within 3 days
of the request, or as soon as required by the health status of the Member.
Prospective Utilization Review decisions shall be communicated via telephone and/or in writing to the
requesting Provider and Member in accordance with the Standard Maximum Time Frames identified
below:
• Emergent – Authorization not required using prudent layperson standards
• Urgent – within 48 hours or as soon as the Member’s health requires
• Expedited – within 72 hours or as soon as the Member’s health requires
• Routine – within 14 days
Authorization and/or denial or alternative treatment is the end result of prospective review.
While prospective review is preferable and must occur prior to planned care (e.g., elective admissions),
situations will exist when a prospective process is not feasible (e.g., emergency admissions) and/or does
not occur.
The Provider is responsible for the prior authorization of all scheduled admissions or services. The
Provider shall obtain prior authorization for admissions/services on a prospective basis, when possible,
and in a timely manner that ensures Member’s access to medically appropriate care.
Bravo Health’s Utilization Management (UM) Department is responsible for the prospective review of
admissions/services; the authorization ensures that the Member receives the proposed treatment in the
appropriate type of facility/location. The prospective review process shall occur only after the
authorization for proposed treatment is obtained by the Provider, when indicated by the Provider
Agreement . Without the Provider’s approval, an authorization number will not be issued.
1. The clinical information regarding the Member, the severity of the Member’s illness and
the proposed plan of care are assessed and evaluated by UM. The guidelines listed above
are utilized for screening medical and surgical care for the first level review. Examples of
information needed include, but are not limited to:
52
a. Member name and identification number
b. Location of service, e.g., hospital or ambulatory surgery setting
c. Primary Care Physician name
d. Attending physician
e. Date of service
f. Diagnosis
g. Surgery, if applicable, with CPT code
h. Clinical information supporting the need for the service to be rendered
2. If the information regarding the Member, the severity of the Member’s illness, and proposed plan of
care meet the criteria for the establishment of medical necessity for inpatient care, outpatient procedure or
surgery, or other required services needing prior authorization a length of stay is assigned. This information
is entered into the Electronic Data Record and approval is communicated to the Provider and the hospital
within 2 days of the determination either via facsimile or in writing if denied.
3. If the information regarding the Member, the severity of the Member’s illness and the proposed plan of
care do not meet the criteria for the establishment of medical necessity; the attending Provider is advised
that the case will be referred to the Medical Director for review. UM Staff will advise the Provider that
he/she can contact the Medical Director for further discussion regarding the case. The Provider will also be
advised that the Medical Director will also attempt to contact him or her. If the case is approved by the
Medical Director, UM will notify the attending Provider of the authorization.
4. In the case of adverse determinations for the Member, UM will:
• Notify the PCP and/or attending Provider, Bravo Health and enrollee of the denial and the Appeal
process including time frames and methods for filing an Appeal.
• Generate a notice of adverse determination to the attending Provider and the Member within two (2)
business days of the determination or within 14 days of receipt of the request, whichever is less either
via facsimile or in writing.
5. If the prospective review does not occur prior to the procedure (e.g., the procedure was performed on an
urgent basis) a review will be conducted within twenty-four (24) hours of notification of the procedure.
6. Prospective or pre pre-service authorization is valid for ninety (90) days from the date of issuance. All
prospectively reviewed treatment, which is not begun within ninety (90) days from the date of issuance, will
require another pre-service review.
7. Pre-service review procedures will include provisions for the identification of Members with special
circumstances who may require flexibility in the application of screening criteria and for those for whom
case management services would be appropriate.
8. The information regarding the medical necessity for an approval of a prospective review request will be
accepted from any source including, but not limited to, phone, facsimile, and/or written correspondence and
can be initiated by any of the following entities: Provider, Member or authorized representative of the
Member.
53
CONCURRENT REVIEW
1. Concurrent Review is the process of continual reassessment of the medical necessity and
appropriateness of acute inpatient care during a hospital admission in order to ensure Covered Services are
being provided at the appropriate level of care. These reviews are conducted telephonically. Bravo Health
is responsible for final authorization.
2. The Concurrent Review process is performed telephonically by a licensed nurse. The Bravo Health
nurse confers with the attending Provider or other hospital staff (Case Managers, Social Workers, Discharge
Planners, etc.) regarding the acute stay and any discharge planning needs; and where appropriate, speaking
with the patient and/or family.
3. A Medical Director reviews any in-patient days that do not meet medical necessity criteria and issues a
determination. All days which do not meet medical necessity criteria, are discussed with the facility
utilization staff and attending Provider and/or PCP when appropriate or available. In those instances where
the admitting Provider does not agree with the determination, the attending is encouraged to contact Bravo
Health’s Medical Director to discuss the appropriateness of the continued hospitalization. The Medical
Director then makes a determination to approve or deny the admission or days in question.
The Hospital’s Utilization Review Department will be notified via facsimile of the daily log and/or verbally
regarding the status of the case and all denials. All determinations to deny or down grade a stay will be
followed up with a formal letter. Only a Medical Director is authorized to deny or downgrade days during
an acute stay.
RETROSPECTIVE REVIEW
Retrospective reviews are performed on all admissions to non-Participating facilities where the Member has
been admitted and discharged prior to Bravo Health’s notification. What about Participating facilities?
a. Bravo Health allows 14 days after notification for facility to provide a verbal, written or facsimile
clinical review. Bravo Health will issue a determination within 14 days of the notification based on
the clinical information provided Clinical information submitted is reviewed according to criteria
for medical necessity, and are subject to Member eligibility at the time services are rendered.
b. Retrospective review may occur for pre-authorized services in order to facilitate claims payment.
Referrals to Non-Contracted Providers
Referrals to non-Contracting Providers are approved only when the non-Contracting Providers provide
services that are not available within the network. All referrals to non-Contracting Providers must be
reviewed and authorized by Bravo Health before services are performed. There must be verification
that the Provider of service is Medicare certified. The Medical Director must review all referrals to
non-Contracted Providers. The Director of Health Services may approve non-Contracting Providers
when deemed necessary by the Medical Director.
Ambulatory Services
a. The PCP is responsible for obtaining pre-authorization for services requiring pre-authorization and
for any referral made out of network.
54
b. The Provider may make their requests via facsimile, phone or letter for pre-authorization before
scheduling the service.
c. The Medical Director reviews any request that does not meet Bravo Health’s criteria.
d. All Member requests for second opinions and recommendations for second opinions will be
provided within the network whenever the opportunity exists. Bravo Health does not require second
opinions for procedures.
e. Except for eligibility and benefit coverage denials, all denial determinations are made at the Medical
Director level.
f. Member eligibility is noted. Benefit level(s), indication of other insurance, and
limitations/exclusions are noted.
g. Prior authorization guidelines/clinical practice guidelines/medical necessity criteria are utilized as
part of the review. Guidelines will be provided to physician upon request.
h. A written description identifying the information that is collected to support decision-making is
maintained.
i. An appropriate licensed medical professional supervises all the review decisions.
j. Physician consultants from the appropriate specialty areas of medicine and surgery are utilized if the
reviewing Medical Director deems necessary.
k. Each request will be approved, denied or an alternative Covered Service may be suggested.
l. A request may be pended, in order for additional information to be obtained as requested. In these
cases, the requesting Provider will be contacted by phone or facsimile within twenty-four (24) hours
by Bravo Health to obtain the required information. If the addition al information is not received
within 14 days Bravo Health will issue a determination based on the clinical information submitted.
Discharge Planning
Discharge Planning is a critical component of the process that begins with an assessment of the patient’s
potential discharge care needs to facilitate the transition from the acute setting to the next level of care.
It includes preparation of the patient and his/her family for any discharge needs along with initiation and
coordination of arrangements for placement and/or services needed after acute care discharge. Bravo
Health’s Utilization Staff will coordinate with the acute care discharge planning team to assist in
establishing a safe and effective discharge plan. The Bravo Health Utilization Review nurse will
provide all needed discharge authorizations for services, equipment and skilled needs.
55
Case Management
Case Management is the focused arrangement of the sequence of services and resources necessary to
respond to the patient’s overall care requirements in catastrophic or complicated cases.
Case Management uses a team approach, which includes the Primary Care Physician, Specialist, Home
Health Agencies, Social Workers, family and others as appropriate. A collaborative approach is used to
assist in meeting the health care needs and community service needs of the Member on a short or long
term basis. The Primary Care Physician’s involvement in care of Members in case management is
essential to support improved Member outcomes.
The Case Management program strives to deliver access to quality care in the most cost effective
manner through appropriate utilization of all available health care resources. Members that can be
referred to Case Management include, but are not limited to, the following:
• Members discharged home from acute/sub-acute/skilled settings with specific ambulatory-sensitive
diagnosis such as DM, CHF, angina without procedure, and COPD
• Members with frequent readmissions
• Members in disease management programs to include, but not limited to, diagnosis of CHF or Diabetes
Mellitus
• Members enrolled in Special Needs Plans for Hypertension and Hyperlipidemia
• Members receiving intensive level of home health care
If you would like to refer a Bravo Health Member for Case Management services, please call 1-888-454-
0013, extension 336940.
Skilled Nursing Care
Bravo Health follows Medicare guidelines for skilled nursing care needs. All Members will be
reviewed and notified within two (2) days prior to the last covered approved day. Only the Medical
Director can deny skilled care based on medical necessity. If additional skilled services are denied, the
facility will be instructed to provide the Member and/or the authorized representative with notification
of the termination of skilled benefits.
Emergency Services
Bravo Health covers emergency services necessary to screen and stabilize Members without
preauthorization in accordance with applicable law. Bravo Health covers emergency services if a PCP
or other authorized representative acting on behalf of Bravo Health has directed the Member to the
Emergency Room.
In an emergency situation, Members sometimes self-refer without the knowledge of the Primary Care
Physician or Bravo Health. In such cases, the medical records will be reviewed retroactively. Final
determination regarding whether an emergency situation existed will be subject to review and will be
determined in accordance with applicable law.
The review is primarily used to promote high quality care, assess whether there is access to Primary
Care Physicians who are contractually obligated to provide care 24 hours a day, 7 days a week is
adequate, and increase awareness of appropriate use of costly emergency care resources.
56
Decision Time Frames
Utilization review determinations are made in a timely manner and in compliance with applicable law.
• Emergent - authorization not required in accordance with applicable law
• Urgent - within 48 hours or next business day
• Expedited – with 72 hours or as required by the health status of the Member
• Routine - within 14 days of the receipt of the request
Bravo Health recognizes the need for prompt handling of all referrals and will communicate directly
with the requesting Provider’s office all rendered decisions via telephone communication and/or
facsimile.
Denials
Efforts are made to obtain all necessary information, including pertinent clinical information from the
treating Provider to allow the Medical Director to make coverage determinations. The Medical Director
is available by telephone to the Provider to discuss determinations based on medical necessity. A denial
may occur:
a. At the time of prospective pre-service review. The process for discussion of such denials
between Bravo Health’s Medical Director and the Provider of care will be documented by
the UM department staff and processed according to the adverse decisions policy.
b. At the time of concurrent review, the health plan will notify the acute facility via facsimile or
verbally within 24 hours after receipt of all clinical information needed to render a
determination. Denial notification is sent to the facility and patient (only when in a non-
Contracting facility) in writing at the end of the admission stay. A copy of the letter is also
sent by mail to the attending Provider notifying him/her of any downgrade or denied
determination.
c. At the time of a request for authorization for a non-Covered service.
Rendering Denials
a. The Utilization Management staff can make the decision for an administrative denial based on
Covered Services, eligibility, etc.
b. Only the Medical Director makes the decision for denial based on medical necessity but he/she
can also make a decision on administrative guidelines. The Medical Director, in making the
initial decision, may elect to suggest an alternative Covered Service to the requesting Provider.
A denial notice is issued documenting the original request that was denied and the alternative
service and the process for appeal. If the Provider agrees, he/she notifies the Member.
Notification of Denials
a. The reason for each denial, including the specific utilization review criteria or benefits
provision used in the determination of the denial are included in the written notification and
sent to Members and Providers.
b. The criteria used to determine the coverage is available to the Provider and Member upon
request.
57
C. All denials for retrospective review are sent to Providers within five working days of making
the decision
CONTINUITY OF CARE
Bravo Health’s policy is to provide for continuity of and coordination of care among medical
practitioners treating the same patient, coordination between medical and behavioral care and to
minimize potential continuity problems caused when a practitioner leaves a network and has patients in
active treatment.
Any Member who is currently undergoing treatment upon the termination of a Provider for reasons
other than those associated with quality of care or a Member who is new to Bravo Health may be
allowed to continue care with their current Provider for up to 90 days from the date the enrollee is
notified by the plan of the termination or pending termination of a Contracting Provider. Members
undergoing active treatment for a chronic or acute medical condition will have access to such
discontinued Provider through the current period of active treatment for up to 90 calendar days,
whichever is shorter. Members in their second or third trimester of pregnancy have access to their
discontinued practitioner through the postpartum period. If Bravo Health terminates a Contracting
Provider for cause, Bravo Health will not be responsible for the health care services provided by the
terminated Provider to the enrollee following the date of termination.
Members with previously scheduled treatments or procedures and Members in the middle of an episode
of care may be allowed to continue care with their current Provider for up to 90 days from the date the
Member is notified by Bravo Health of the termination or pending termination of a healthcare Provider.
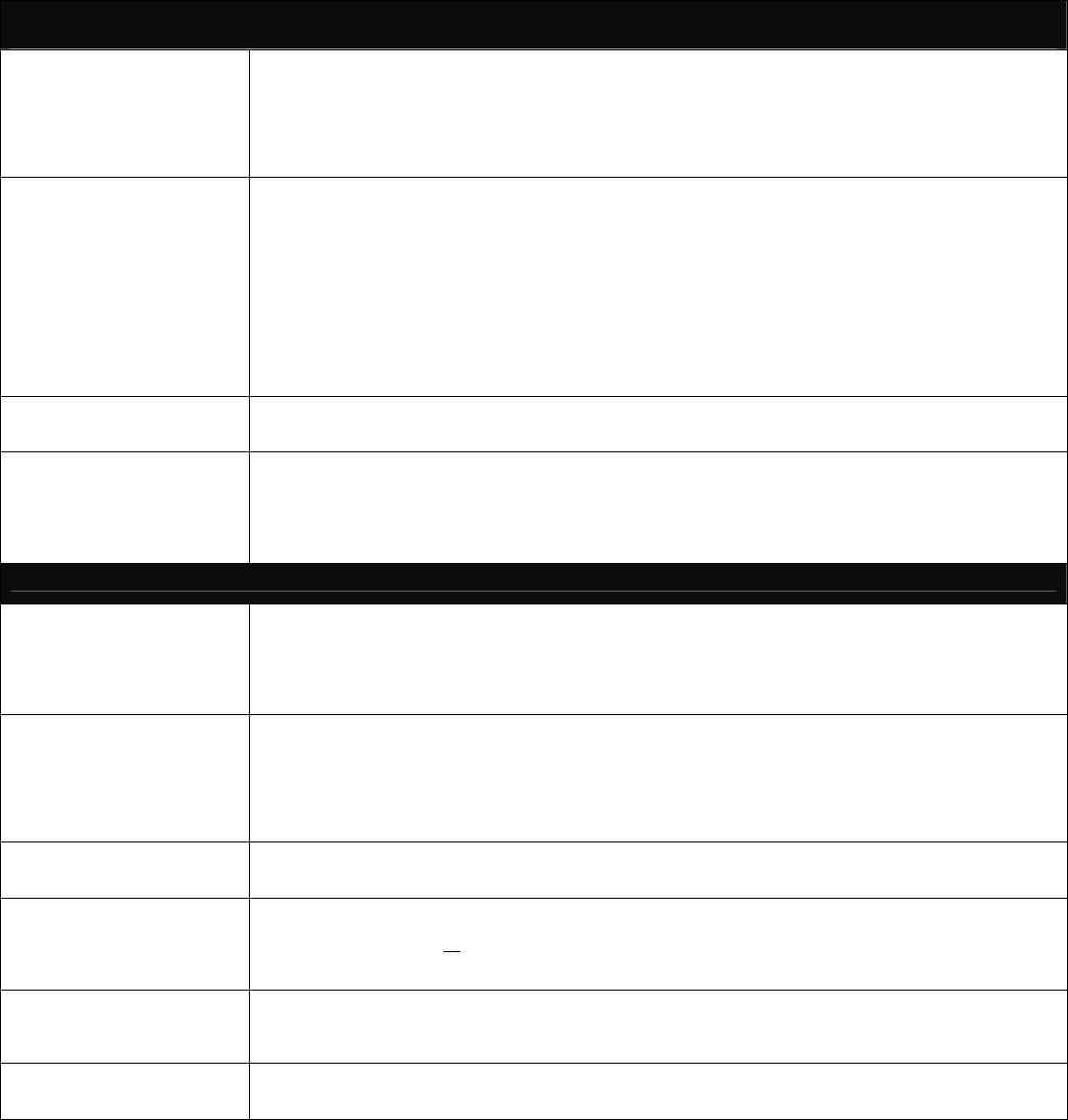
58
CLINICAL PRACTICE GUIDELINES
OUTPATIENT MANAGEMENT OF CONGESTIVE HEART FAILURE IN ADULTS
GOALS FOR DIAGNOSTIC
EVALUATION
Establish Ejection Fraction and document the Left without resulting Ventricular Dysfunction
Determine underlying cause of heart failure
Identify precipitating or aggravating correctable factors
Develop Management and Treatment Plan
Provide baseline information to monitor effects of treatment
Establish baseline NYHA classification
INITIAL EVALUATION OF
HEART FAILURE
DIAGNOSTIC TESTING
Complete History and Physical Examination
Clinical Testing
Chest X-Ray, 12-lead Electrocardiogram
Assessment of Ventricular Function
Transthoracic Doppler 2-D Echocardiography
Radionuclide ventriculography
Evaluation testing for ischemia (Stress, Nuclear Test
OR Stress Echocardiography OR Cardiac
Catheterization) Complete Blood Count, Urinalysis
Fasting Lipid Panel, (Cholesterol Triglyceride, HDL Cholesterol, LDL and LDL: HDL Ratio)
Blood Chemistry: Electrolytes, BUN, creatinine,
Glucose, Liver function test and TSH level
ADDITIONAL DIAGNOSTIC
TESTING
Consider additional diagnostic testing for evaluation of other cardiac or non-cardiac related causes in the absence of ischemia
or Valvular Heart Disease, Serum Iron and Ferritin, Endomyocardial Biopsy, Phosphorus, Magnesium, Calcium and
Albumin levels
SPECIALTY REFERRALS
Cardiac Educator – As indicated
Nutritional Counseling – As indicated
Cardiology Consult – Consider consultation during the initial evaluation and anytime during the ongoing management
of CHF as appropriate
Home Health Care – Consider home health care for outpatient monitoring
Cardiac Rehabilitation Programs – Consider rehabilitation programs to maximize functional capacity
MANAGEMENT PLAN, EDUCATION & FAMILY COUNSELING
PATIENT AND FAMILY
EDUCATION AND
COUNSELING
Nature of heart disease-Drug Adherence Regimens
Symptoms of worsening CHF-What to do if symptoms occur
Mechanisms for complicated medical regimens-Coping
Presentation measures for further progression of the disease
Accurate information concerning prognosis should be discussed in order for patients to make decisions and plans for the
future. Discuss the planning of advance directives with patients and family in the context of heart failure management
LIFESTYLE
CHANGES/HABITS
Physical Activity – Recreation, leisure and work activity as tolerated
Exercise – Establish a regular exercise program consistent with individual patient’s capabilities and clinical status.
Program should be dynamic (walking, cycling) not isometric to pervert or reserve physical including drug doses.
Sexual Activity – Discuss sexual difficulties and coping mechanisms if they occur
Smoking Cessation – Emphasis on the importance of not smoking: medications of financial assistance determine the
willingness to stop smoking and strategies for smoking cessation should be tailored to each individual
Alcohol Usage – Discourage alcohol use
DIETARY MEASURES
Sodium restriction –Define and quantify the amount of salt that is allowed in the daily diet, 3 grams or less. (Personal
food preferences, culture, income and family support should be considered)
Management of Cachexia/Management of Obesity
FLUID MANAGEMENT
Establish baseline weight
Encourage daily weights on the same scale at the same time each day
Report weight gains of > of 5+ lbs. in a week
Establish/monitor daily fluid intake limits; avoid excessive fluid intake
Instruct on fluid restriction if indicated
MEDICATION EDUCATION
Develop a patient medication schedule including drug doses
Review effects of medications on quality of life and survival
Discuss probability of side effects and what to do if they occur
Discuss availability of lower cost medications or financial assistance
IMMUNIZATIONS
Influenza (flu) –vaccine annually
Pneumococcal vaccine –initially/repeat as per CDC recommendations
**Utilization Management Committee will review Guidelines for new scientific evidence or national
standard changes prior to distribution to Providers annually.
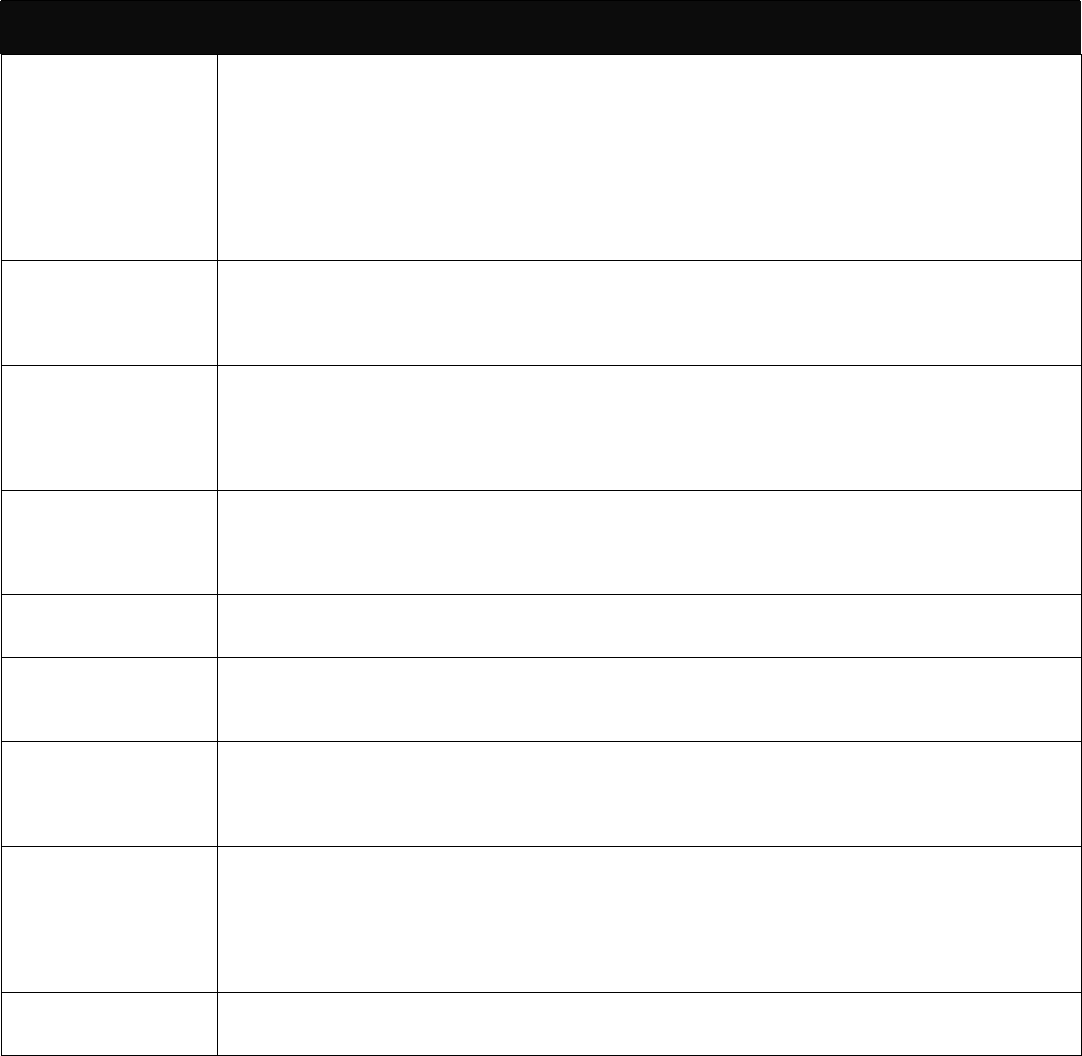
59
CHF PHARMACOLOGICAL TREATMENT OPTIONS - RECOMMENDATIONS
ACE Inhibitors
(Angiotension
Coverting Enzyme)
Need to change font to
match others
ACE Inhibitors should be prescribed for patients with left-ventricular systolic
dysfunction with EV < 40 unless contraindicated or not tolerated.
ACE Inhibitors should be continued indefinitely.
The recommended dose of ACE Inhibitors for heart failure are the larger doses used in the clinical trials
demonstrating improvement in survival.
Contradictions to ACE Inhibitors include shock, angioneurotic edema, significant hyperkalemia (scrum
potassium >5.5mEq/1)**, symptomatic hypotension, severe renal artery stenosis, severe aortic stenosis and
pregnancy
Alternative Treatment to
ACE Inhibitors
Consider Angiotension Receptor Blockers (ARB) as alternative therapy only in ACE inhibitor – intolerant
patients due to persistent cough shock or angineurotic edema(or add to ACE if beta-blocker contraindicated)
Consider hydralazine/isosorbide dinitrate combination therapy if renal insufficiency precludes ACE/ARB
therapy.
Beta - Blockers
Data supports long acting metoprolol, carvedilol, or bisoporlol indicated for clinically stable patients with left
ventricular systolic dysfunction and mild to moderate heart failure symptoms that are on standard therapy
(which typically includes ACE Inhibitors, diuretics as needed to control fluid retention and digoxin).
Start with low doses and gradually increase.
If tolerated, beta-blockers are also indicated in the treatment of high-risk patients after an acute myocardial
infarction.
Diuretics
Consider diuretic drugs for patients with fluid overload and edema.
Patients with symptomatic heart failure should be treated with a diuretic drug, even when rendered free of
edema. Diuretic drugs should be used in conjunction with an ACE inhibitor. The dose and type of diuretic
drug may change according to fluid status, but generally will be needed indefinitely.
Digoxin
Consider digoxin in patients with symptomatic evidence of heart failure, elevated filling pressures, a third heart
sound, ventricular dilatation or depressed ejection fraction.
Useful drug in heart failure patients with atrial fibrillation with rapid ventricular rates.
Anti-Coagulants
(Warfarin)
Patients with heart failure and atrial fibrillation should be treated with Warfarin, unless contraindicated in
present systematic embolization.
Anticoagulation with Warfarin should be considered in patients with severely impaired systolic function and
high risk thromboemboli.
Aldosterone
Antagonist
Spironolactone
Considered administration of spironolactone at low dose (12.5mg to 25mg daily) for patients receiving standard
therapy who have severe heart failure caused by left ventricular dysfunction.
Patients should have a normal serum potassium level and adequate renal function.
**Monitor serum K + levels at regular intervals and after any change in dosage.
Antiarrhythmics
Not routinely recommended, but indicated in atrial fibrillation.
Due to its low incidence of proarrhythmic effects in general, amiodarone is the preferred drug when
antiarrhythmic therapy is indicated in patients with heart failure for supraventricular tachycardia not controlled
by Digoxin or beta-blocker or patients with life threatening ventricular arrhythmia that are not candidates for
implantable cardiac defibrillators.
Use of antiarrhythmic agents should not be used for the suppression of ventricular premature beats or non-
sustained ventricular tachycardia, which is either asymptomatic or perceived as palpations.
Other
Use of most calcium channel blockers is not recommended unless needed for hypertension or rapid response of atrial
fibrillation.
**Monitor Serum K+ levels on a regular basis; Consider low potassium duet and avoid foods high in potassium
Complied From:
1. Guidelines for the Evaluation and Management of Heart Failure. Report of the American College of Cardiology/American Heart Association Task Force on
Practice Guidelines (Committee on Evaluation and Management of Heart Failure). Circulation 1995; 92: 2764-84, reviewed 2005.
2. US Department of Health and Human Services. Agency for Health Care Policy and Research. Heart failure: evaluation and care of patients with left ventricular
systolic dysfunction. Rockville, The Agency 1994 (Clinical Practice Guideline No. 1) (AHCPR Publication No. 94-0612.)
3. Heart Failure Society Guidelines: A Model of Consensus and Excellence. Pharmacotherapy 20(5) 495-522, 2000
4. Institute for Clinical Systems Improvement, Inc. Health Care Guidelines; Congestive Heart Failure in Adults. November, 2000
**Utilization Management Committee will review Guidelines for new scientific evidence or national standard changes prior to
distribution to Providers annually.
60
Stage A
At high risk for heart failure,
but without structural heart
disease or symptoms of HF
Stage B
Structural heart disease,
but without signs or
symptoms of HF
Stage C
Structural heart disease
with prior or current
symptoms of HF
Stage D
Refractory HF
requiring specialized
interventions
E.g. Patients with
- hypertension
- coronary artery disease
- metabolic syndrome
- diabetes mellitus
- obesity
or
Patients
- using cardiotoxins
- with FHx CM
E.g. Patients with
- Previous MI
- LV remodeling incl.
LVH & low EF
- Asymptomatic
- Valvular disease
E.g. Patients with:
- Known structural
heart disease
- Shortness of breath
and fatigue, reduced
exercise tolerance
E.g. Patients who have
marked symptoms at rest
despite maximal medical
therapy (e.g. those who are
recurrently hospitalized or
cannot be safely discharged
from the hospital without
specialized interventions)
Structural
heart
disease
Development
of symptoms of
HF at rest
Refractory
symptoms
of HF at rest
Therapy
- Appropriate measures under
stages A,B, and C
- Decision re: appropriate level
of care
- Extraordinary Care
Heart transplant
Chronic inotropes
Permanent mechanical support
- Experimental surgery/drugs
- Hospice/end of life care
Therapy
- Treat hypertension
- Encourage smoking
cessation
- Treat lipid disorders
- Encourage regular
exercise
- Discourage alcohol intake,
illicit drug use
- Control metabolic
syndrome
-
ACE inhibition in
Therapy
- All measures under
stage A
- ACE inhibitors in
appropriate patients*
- Beta-blockers in
appropriate patients*
Therapy
- All measures under Stage A & B
- Dietary Salt Restriction
- Drugs for routine use*:
Diuretics
ACE inhibitors
Beta-blockers
Digitals
- Drugs in Selected patients*:
Aldosterone antagonisists
ARB’s,
Digitalis,
Hydralizine
Nitrates
- Devices in Selected Patients
Biventricular Pacing
Implantable defibrillator
NEW YORK HEART ASSOCIATION HEART FAILURE DISEASE CLASSIFICATION:
Class I Asymptomatic (Patients with cardiac disease but without resulting limitations of physical activity. Ordinary physical activity does not cause undo fatigue, palpitations, dyspnea, or anginal pain)
Class II Mildly symptomatic (Patients with cardiac disease resulting in slight limitation of physical activity. Comfortable at rest, ordinary physical activity results in fatigue, palpitation, dyspnea or
anginal pain)
Class III Moderately symptomatic (Patients with cardiac disease resulting in marked limitation of physical activity. Comfortable at rest, less than ordinary activity causes fatigue, palpitation, dyspnea or
anginal pain)
Class IV Severe symptoms at rest (Patients with cardiac disease resulting in an inability on any physical activity)
This table of suggested guidelines has been developed from the ACC/AHA 2005 Chronic Heart Failure Guideline Update. It is intended to provide guidance to practitioners to reduce risks associated
with CHF, increase awareness of CHF, and to optimize disease management. It contains guidelines only and should never supersede clinical judgment. The practitioner, in conjunction with the patient or
responsible party, should decide whether these or other recommended services should be performed more frequently, less frequently, or not at all. As with all services provided to Bravo Health
Members, the clinical judgment and the discussion around it should be documented in the medical record. *ACC/AHA full text guideline available at; http://circ.ahajournals.org/cgi/reprint/112/12/e154
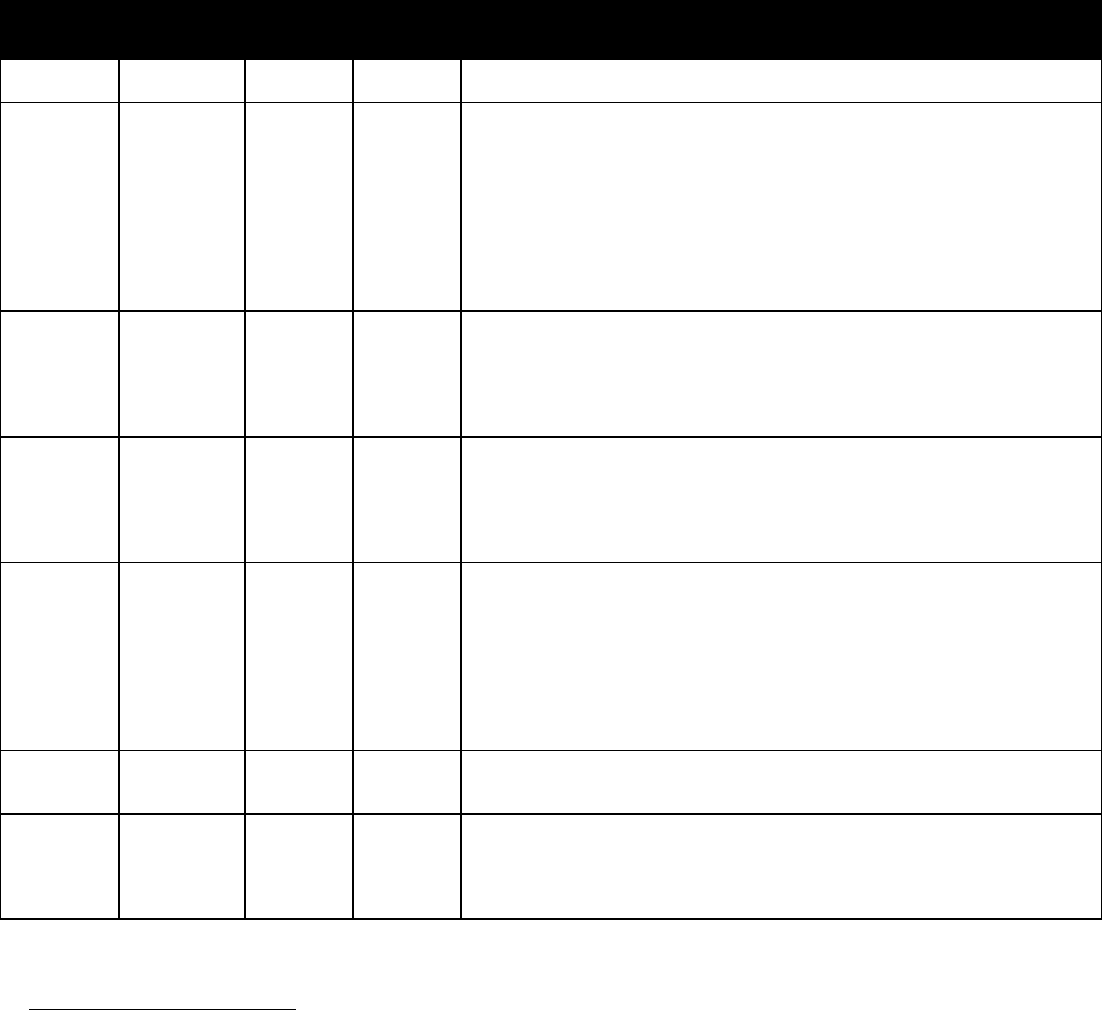
61
OUTPATIENT MANAGEMENT OF DIABETES
Aspect of
Care
Monitor Frequency Target
Outcome
Recommendations
Glycemic
Control
Fix font so
they all
match
HbA1c Quarterly
or
Semi-
Annual
<7% Target hemoglobin A1c (A1C) should be individualized. A reasonable goal for A1C
in relatively healthy adults with good functional status is 7% or lower. For frail, older
adults, persons with life expectancy of less than 5 years, and others in whom the risks
of intensive glycemic control appear to outweigh the benefits, a less stringent
treatment goal may be appropriate.
Obtain A1C test quarterly in persons whose therapy has changed or who are not
meeting glycemic goals. Obtain A1C test at least twice yearly if at goal and who have
stable glycemic control. Use of Point of Care Testing for A1C allows for timely
decisions on therapy changes when needed.
Lipids LDL Annual <100 mg/dl
Lifestyle modification focusing on the reduction of fat and cholesterol intake, weight
loss (if indicated), and increased physical activity has been shown to improve the
lipid profile in persons with diabetes. In persons without overt CVD over the age of
40 years, statin therapy to achieve an LDL reduction of 30-40% regardless of
baseline LDL is recommended. In persons with overt CVD, all persons should
receive statin therapy to achieve an LDL reduction of 30-40%.
Retinopathy Dilated-eye
examination
by an
Eye-Care
Specialist
Annual Adults with type 1 diabetes should have an initial dilated and comprehensive eye
exam performed by an eye care specialist within three to five years after the onset of
diabetes. Persons with type 2 diabetes should have an initial dilated and
comprehensive eye exam shortly after the diagnosis of diabetes. Subsequent dilated
comprehensive eye examinations for persons with type 1 and type 2 diabetes should
be performed annually.
Nephropathy Micro-
albumin
Serum
Creatinine
Annual
Perform an annual test for the presence of microalbuminuria in persons with type 1
diabetes with diabetes duration of ≥ 5 years and in all persons with type 2 diabetes
starting at diagnosis. In persons with any degree of CKD, protein intake should be
limited to RDA (0.8g/kg) to reduce the risk of nephropathy.
Serum Creatinine should be measured at least annually for the estimation of
glomerular filtration rate in all adults with diabetes regardless of the degree of urine
albumin excretion. The serum creatinine alone should not be used as a measure of
kidney function but instead used to estimate GFR and stage the level of CKD.
Hypertension Blood
Pressure
Each visit . If patient has hypertension, then the target blood pressure should be less than 130/80
if it is tolerated. Because older adults may have reduced tolerance for blood pressure
reduction, hypertension should be treated gradually to avoid complications.
Foot Care Foot exam Annual All persons with diabetes should receive an annual foot examination to identify high-
risk foot conditions. This examination should include assessment of protective
sensation, foot structure and biomechanics, vascular status, and skin integrity.
Persons with neuropathy should have a visual inspection of their feet every office
visit by a health care professional.
This table of suggested guidelines has been developed from the American Diabetes Association: 2007 Standards of Medical Care
in Diabetes:
Diabetes Care 29: S4-S42, 2006. It is intended to provide guidance to practitioners to reduce risks associated with diabetes,
increase awareness of diabetes, and to optimize disease management. It contains guidelines only and should never supersede
clinical judgment. The practitioner in conjunction with the patient should decide whether these or other recommended services
should be performed more or less frequently. Clinical judgment and discussion should be documented in the medical record
Utilization Management Committee will review Guidelines for new scientific evidence or national standard changes prior to
distribution to Providers annually. 9/27/2007
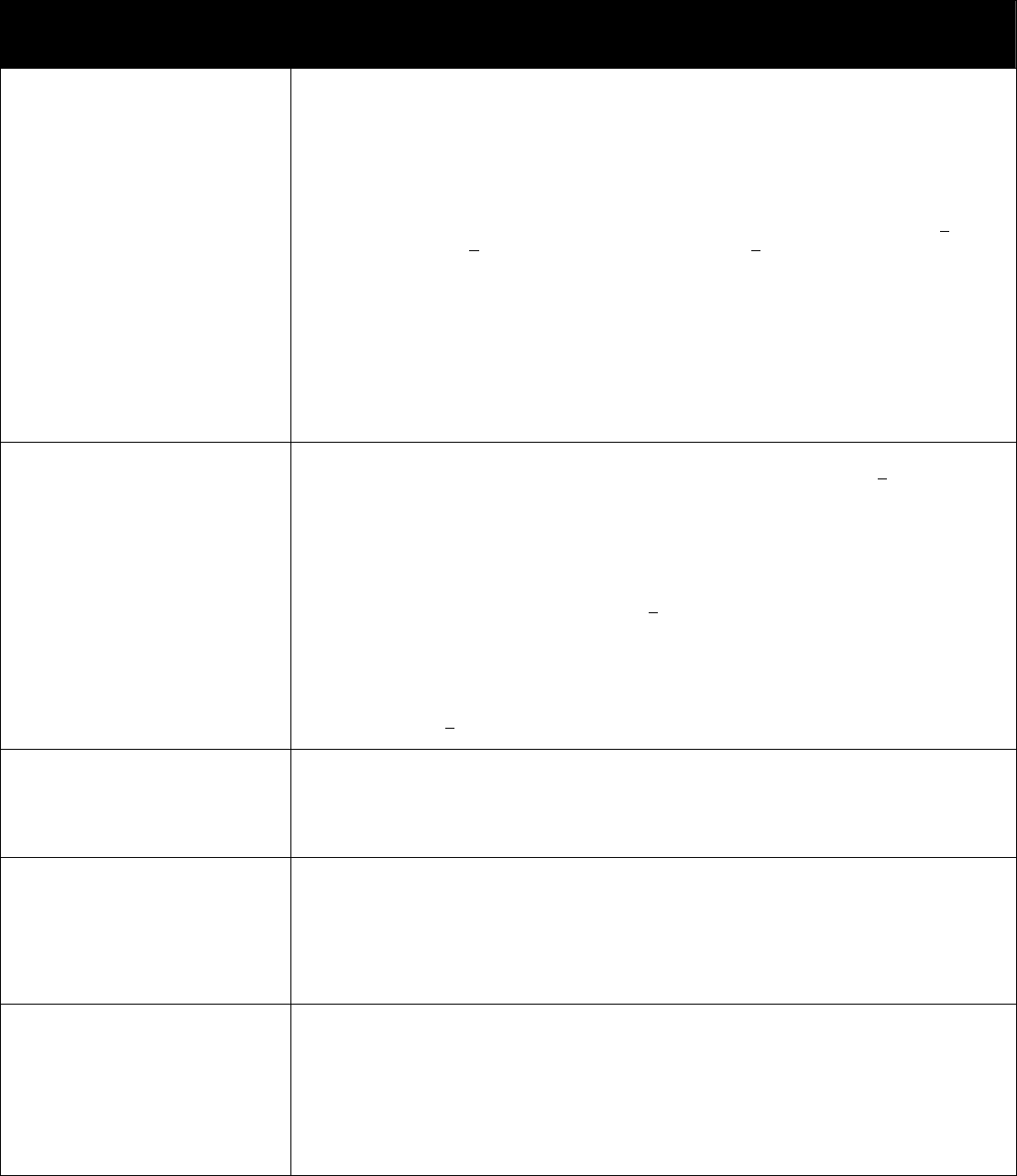
62
OUTPATIENT MANAGEMENT OF
CORONARY AND OTHER VASCULAR DISEASE
Antiplatelet Agents/
Anticoagulants
Start aspirin 75 to 162 mg/d and continue indefinitely in all patients unless contraindicated.
Gastrointestinal side effects are dose-dependent. Since the benefits of aspirin have been measured at
doses as low as 81 mg. enteric-coated 81 mg tablets are reasonable and almost always tolerated.
For patients undergoing CABG, aspirin should be started with in 48 hours after surgery to reduce
saphenous vein graft closure. Dosing regimens ranging from 100 to 325 mg/d appear to be
efficacious. Doses higher than 162 mg/d can be continued for up to 1 year.
Start and continue clopidogrel 75mg/d in combination with aspirin for up to 12 months in patients
after acute coronary syndrome or percutaneous coronary intervention with stent placement (>1 month
for bare metal stent, >3 months for sirolimus-eluting stent, and >6 months for paclitaxel-eluting
stent).
Patients who have undergone percutaneous coronary intervention with stent placement should
initially receive higher-dose aspirin at 325mg/d for 1 month for bare metal stent, 3 months for
sirolimus-eluting stent, and 6 months for paclitaxel-eluting stent
Manage Warfarin to international normalized ratio= 2.0to 3.0 for paroxysmal or chronic atrial
fibrillation or flutter, and in post myocardial infarction patients when clinically indicated (e.g., atrial
fibrillation, left ventricular thrombus).
Use of Warfarin in conjunction with aspirin and/or clopidogrel is associated with increased risk of
bleeding and should be monitored closely.
Patients with true aspirin allergy (laryngospasm, anaphylaxis) should receive Clopidogrel.
Renin-Angiotensin-
Aldosterone System
Blockers
ACE Inhibitors
Start and continue indefinitely in all patients with left ventricular ejection fraction <40% and in those
with hypertension, diabetes, or chronic kidney disease, unless contraindicated.
Among lower-risk patients with normal left ventricular ejection fraction in whom cardiovascular risk
factors are well controlled and revascularization has been performed, use of ACE inhibitors may be
considered optional.
Angiotensin receptor blockers
• Use in patients who are intolerant of ACE inhibitors and have heart failure or have had a myocardial
infarction with left ventricular ejection fraction <40%.
• Consider in other patients who are ACE inhibitor intolerant.
Aldosterone Blockade
Use in post-myocardial infarction patients, without significant renal dysfunction (creatinine
<2.5mg/dl in men, <2.0mg/dl in women) or hyperkalemia (Potassium should be <5.0MEq/L), who
are already receiving therapeutic doses of an ACE inhibitor and Beta-Blocker, have a left ventricular
ejection fraction <40%, and have either diabetes or heart failure.
Refer to the Clinical Practice Guideline for the Outpatient Management of CHF in Adults.
B-blockers
Goal:
All patients post MI
Start and continue indefinitely in all patients who have had myocardial infarction, acute coronary
syndrome, or left ventricular dysfunction with or without heart failure symptoms, unless
contraindicated.
Consider chronic therapy for all other patients with coronary or other vascular disease or diabetes
unless contraindicated.
Blood Pressure
Goal:
<140/90 mm Hg or
<130/80 mm Hg if
Diabetes or Renal Insufficiency
Identify and treat reversible causes.
Accurate BP measurements with appropriate size cuff at every visit.
Advocate & monitor lifestyle changes (weight control, physical activity, alcohol moderation, if
moderate sodium restriction, emphases on fruits/vegetables and low-fat dairy products)
Pharmacological management goals. All patients on optimal dose of drug therapy for insufficiency
adequate hypertension control. (see Seventh Report of the Joint National Committee on Prevention,
Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7).
Cigarette Smoking
Goal:
Complete Cessation
ASK – Identify use of all tobacco products at every visit.
ADVISE – Strongly urge and educate users on the importance of quitting at every visit.
ASSESS – Determine the patient’s willingness to quit.
ASSIST – Counsel the patient and help to develop quit plan and set quit date.
Prescribe pharmacotherapies found to be effective (unless contraindicated);
Combination treatment with sustained release bupropin and nicotine withdrawal products has been
shown to be the most effective.
ARRANGE – Follow up soon after quit date.
AVOIDANCE-- of exposure to environmental tobacco smoke at work and home.
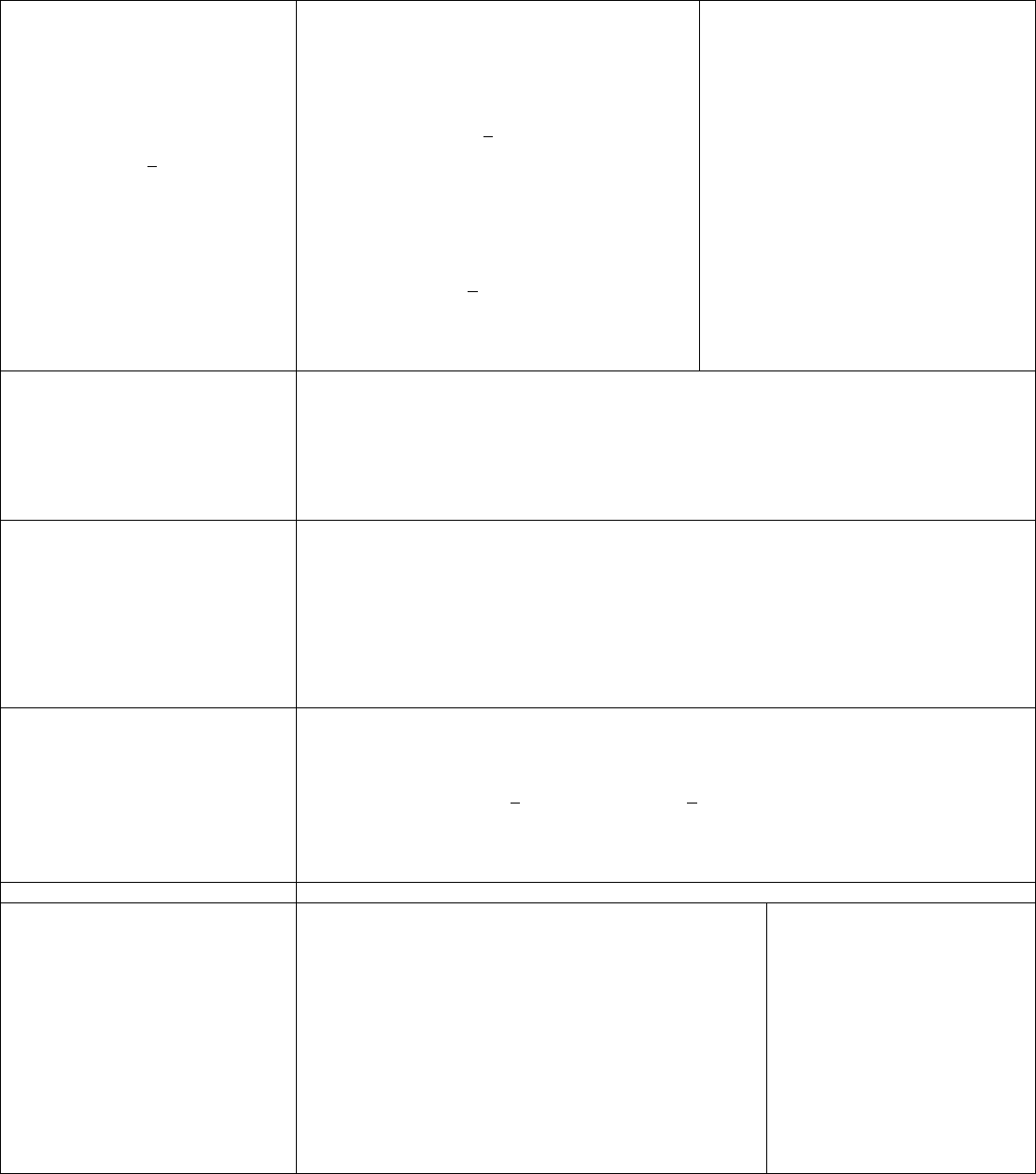
63
Cholesterol
Primary Goal:
LDL-C<100 mg/dL
If triglycerides are >200 mg/dL, non –
HDL-C should be <130 mg/dL
Intensive cholesterol-lowering therapy can
significantly reduce the risk of major coronary
events, strokes and total mortality.
LDL-C should be <100mg/dL
Further reduction of LDL-C to <70 mg/dL is
reasonable.
If baseline LDL-C is >100/dL, initiate LDL-
lowering drug therapy.
If on-treatment LDL-C is >100 mg/dL, intensify
LDL-lowering therapy (may LDL-lowering drug
combination).
If triglycerides are >200 mg/dL, non-HDL-C
should be <130mg/dL and further reduction of non-
HDL-C to <100mg/dL is reasonable.
If triglycerides are >500mg/dL, therapeutic options
to prevent pancreatitis are fibrate or niacin before
LDL-lowering therapy; and treat LDL-C to goal
after triglyceride-lowering therapy.
Refer to NCEP III guidelines for details
The treatment of elevated LDL-C involves
therapeutic lifestyle changes (TLC) and Drug
therapy.
Essential features of TLC are:
Reduced intake of saturated fats (<7% of
total calories) and cholesterol (<200
mg/day)
Increased intake of soluble fiber
>10g/day and plant stanols/sterols
(2g/day)
Increase consumption of omega-3 fatty
acids in the form of fish or in caspsule
form (1g/d).
Weight reduction/management
Increased physical activity
HMG CoA reductase inhibitors (statins)
Diabetes
Goal:
HbA1c <7%
Screen all CAD patients for diabetes: type 1 DM increases CAD risk three-to-ten fold
Type 2 DM increases CAD risk two fold in men and four in women.
Initiate lifestyle and pharmacotherapy to achieve near-normal HbA1c.
Begin vigorous modification of other risk factors (e.g., physical activity, weight management, blood
pressure control, and cholesterol management as recommended above).
Coordinate diabetic care with patient’s primary care physician or endocrinologist.
Refer to the Clinical Practice Guideline for Diabetes Care.
Physical Activity
Goal:
At least 30 minutes
7days/week
(minimum 5 days)
Exercise training improves exercise tolerance, symptoms, psychological well-being, lipid profiles and
cardiac outcomes.
To guide exercise prescription, assess risk preferable with exercise tolerance test.
For all patient , encourage of 30-60 minutes of moderate-intensity aerobic activity, such as brisk
walking, supplemented by an increase in daily lifestyle activities (household work, gardening).
Encourage resistance training 2 days per week
For moderate-to high risk patients, recommend medically supervised “Cardiac Rehab” programs.
Physicians and patients are sometimes concerned about the safety of exercise training in patients with
CAD although there is clearly a very low rate of serious cardiac events during cardiac rehabilitation.
Weight Management
Goal:
BMI 18.5 to 24.9kg/m2
Waist circumference:
Men <40 inches
Women < 35 inches
Assess body mass index and/or waist circumference on each visit and consistently encourage weight
maintenance/reduction through an appropriate balance of physical activity, caloric intake, and formal
behavioral programs when indicated to maintain/achieve a body mass index between 18.5 and 24.9
kg/m2.
If waist circumference is >35 inches in women and >40 inches in men, initiated lifestyle changes and
consider treatment strategies for metabolic syndrome as indicated.
The initial goal of weight loss therapy should be to reduce body weight by approximately 10% from
baseline. With success, further weight loss can bet attempted if indicated through further assessment.
gardening).
Influenza Vaccine Patients with cardiovascular disease should have an influenza vaccination annually.
Education
Goal:
Improve patient
Knowledge &
Enhanced outcome
• Assess patients’ baseline understanding.
Elicit their desire for information.
Use ancillary personal and professional patient education
programs.
Involve family Members.
Invest time to improve functional capacity and survival.
Incorporate patient specific information including prognosis,
treatment plan, physical activity including limitations,
resumption of occupation and sexual activities.
Emphasize risk factor reductions.
Discuss accessing the emergency medical system.
Develop action plans for aspirin and sublingual nitroglycerin
including any contraindications.
Category I risk factors
Identify and treat aggressively
Hypertension
Smoking
Diabetes
Sedentary lifestyle
Hyperlipidemia
Obesity
Category II risk factors
Menopausal complications
Obesity
Stress
Depression
This table of suggested guidelines has been developed from the AHA/ACC Secondary Prevention for Patients with Coronary and Other Vascular Disease revised 2005 clinical guidelines. It
is intended to provide guidance to practitioners to reduce risks associated with CAD, increase awareness of CAD and to optimize disease management. It contains guidelines only and should never
supersede clinical judgment. The practitioner, in conjunction with the patient or responsible party, should decide whether these or other recommended services should be performed more
frequently, less frequently, or not at all. As with all services provided to Bravo Health Members, the clinical judgment and the discussion around it should be documented in the medical record.
64
OUTPATIENT MANAGEMENT OF COPD
ASPECT OF CARE MONITOR RECOMMENDATIONS
Screening It is important to obtain a thorough history to screen
for risk factors especially cigarette smoking,
occupational exposure, and outdoor/indoor pollution.
The most important risk factor for COPD is cigarette
smoking.
At initial assessment and periodically determine risk
factors and causes of exacerbations. Initiate and
monitor cigarette and smoking cessation
Diagnosis
Symptoms:
Chronic cough throughout the day
Any pattern of sputum production
Dyspnea that is progressive, persistent, worse on
exercise, worse during respiratory infections
Repeated episodes of acute bronchitis
History of exposure to tobacco smoke , occupational
dusts and chemicals
Smoke from home cooking and heating fuel
The diagnosis should be confirmed by spirometry if
patient has symptoms.
At initial assessment and annually. According to the
GOLD standards, spirometry can be used to monitor
disease progression but to be reliable the intervals
between measurements must be at least 12 months
apart.
Additional tests for the assessment of a patient with
Stages II-IV: Bronchodilator Reversibility Testing,
CXR, ABG
Classification by Severity:
Stage 0: At Risk
Chronic cough and sputum production
Lung function is normal
Avoidance of risk factors
Annual Influenza Vaccine
Stage 1 Mild COPD FEV1>=80% FEV1/FVC<70%
Mild airflow limitation, and usually, but not always,
chronic cough and sputum production.
Short Acting Bronchodilator when needed
Albuterol, terbutaline, metaproterenol,
ipratropium (Tier 1)
Proventil HFA, Ventolin HFA, Atrovent HFA
(Tier 2)
Stage 2 Moderate COPD FEV1/FVC < 70%
50%<=FEV1<80% predicted
Worsening airflow limitation, and usually the
progression of symptoms, with shortness of breath,
developing on exertion.
Continue short acting Bronchodilators as needed
Add treatment with one or more long acting
bronchodilators
Servent, Spiriva (Tier 2)
Pulmonary Rehabilitation
Stage 3 Severe COPD FEV1/FVC < 70%
30%<=FEV1<50% predicted
Further worsening of airflow limitation, increased
shortness of breath, and repeated exacerbations which
have an impact on patients’ quality of life.
Short and long acting bronchodilators
Pulmonary Rehabilitation
Inhaled Glucocorticosteroids if repeated exacerbations
Asmanex, Flovent HFA, Pulmicort (Tier 2)
Combo w/ long-acting bronchodilator: Advair
(Tier 2)
Stage 4 Very Severe COPD FEV1/FVC < 70%
FEV1<30% predicted or FEV1<50% predicted plus
chronic respiratory failure
Severe airflow limitation, quality of life is very
appreciably impaired, and exacerbations may be life
threatening
Add long term care oxygen
Initiate oxygen therapy for patients with Stage IV:
Very Severe COPD if:
1. PaO2 is < or = 55mm Hg or SaO2 is < or = 88%
with or without hypercapnia or 2. PaO2 is between
55mm Hg and 60 mm Hg or SaO2 is 89%, if there is
evidence of pulmonary hypertension, peripheral
edema, suggesting CHF or polycythemia
Patient Education/Prevention of Complications Patient education is an effective way to accomplish
smoking cessation, improve knowledge of disease
and associated signs and symptoms, and improve
responses to acute exacerbations.
How to assess severity of an exacerbation:
PaO2 < 60mmHg and/or SaO2 < 90% with or without
PaCO2 >50mmHg when breathing room air indicates
respiratory failure
PaO2 < 50 and PaCO2 >70 and pH<7.30 suggest a life
threatening episode that needs close monitoring or
critical management:
Smoking cessation (all stages COPD)
Yearly Influenza vaccination (all stages COPD)
Pneumococcal Vaccine:
One dose for persons under 65 who have chronic
disorders of the pulmonary systems.
One dose for unvaccinated persons age 65 and older.
One dose revaccination for persons age 65 and older
if they received the vaccine greater than or equal to 5
years previously and were less than 65 years at time
of primary vaccination.
Increase bronchodilator therapy
Consider antibiotic therapy for bacterial infection
Consider corticosteroids if no improvement in
symptoms; Administer O2 as needed;, Increase social
support; Improve exercise tolerance
Indications for Hospital Admissions:
Insufficient home support; newly occurring
arrhythmias; significant co-morbidities; onset of new
physical signs (cyanosis, peripheral edema); failure of
exacerbation to respond to initial medical treatment;
severe background COPD; marked increase in
intensity of symptoms such as development of resting
dyspnea
This table of suggested guidelines has been developed from the American Diabetes Association: 2007 Standards of Medical Care in Diabetes: Diabetes Care 29: S4-S42, 2006. It is intended to
provide guidance to practitioners to reduce risks associated with diabetes, increase awareness of diabetes, and to optimize disease management. It contains guidelines only and should never supersede
clinical judgment. The practitioner in conjunction with the patient should decide whether these or other recommended services should be performed more or less frequently. Clinical judgment and
discussion should be documented in the medical record **Utilization Management Committee will review Guidelines for new scientific evidence or national standard changes prior to distribution to
Providers annually.

65
PHARMACEUTICAL MANAGEMENT
Bravo Health provides a pharmacy benefit to all of our Members. This benefit consists of a three-tier
formulary with a fourth tier for specialty injectible medications. All prescriptions require the Member to
pay a co-payment based on the medication’s formulary status. Our formulary can be found on line at
www.bravohealth.com. Click on Providers, then Provider Forms and Information. You may also
request a printed copy of the formulary by contacting our Provider Services Department at 1-888-353-
3789.
Bravo Health’s formulary requires that some medications require prior authorization before they can be
dispensed. Please call 1-800-753-2851 for prior authorization. The formulary lists these medications
with the designation ‘PA.’ If you would like a copy of the criteria that Bravo Health uses to determine
coverage status for these medications, please visit our website. You may also request a printed copy of
these criteria by contacting our Provider Services Department.
Step Therapy
Bravo Health requires step therapy on the following 2 classes: Proton Pump Inhibitors and Lipid
lowering agents. The first line therapy for the proton pump inhibitor class will be either generic
Omeprazole or Zegerid. If you require any other medications for your Members in this class, prior
authorization will be required. For the lipid lowering class, first line medications are; Lovastatin,
Simvastatin, and Pravastatin. If you require any other medications in this class for your patients, they
will require prior authorization.
As always, remember to prescribe generics to our Members. Generic medications offer the lowest co-
payments and don’t require you to fill out any paperwork or receive callbacks from the retail pharmacies
asking you to switch to a formulary medication. If you do prescribe a brand name drug that has a
generic equivalent, the pharmacy will automatically switch the drug to the generic medication. If the
Member requires the brand name drug due to a medical failure or allergic reactions to a generic
medication, you must contact Bravo Health to seek prior authorization for the brand name medication.
66
PART D PHARMACY PRIOR AUTHORIZATION
The following drugs DO NOT require prior authorization under the Part D benefit:
Accuneb Cellcept Fosamax 40mg Myobloc Rebetol Testoderm
Actimmune Cerezyme Inj Foscarnet Inj Nebupent Rebetron Testred
Actiq Ciprofloxacin Inj Gabitril Neoral Rebif Thalomid
Actonel 30mg Cis Platin Inj Gammar Nicotine Patch Regranex Tobi
Acyclovir inj Cladribine Inj Gammimune N Nicotrol Relenza Tracleer
Adderall/Adderrall
XR Cognex Gangiclovir Inj
Nitroglycerin
Inj Remicaid Triseonx Inj
Alupent Nebulizer Concerta Genotropin Norditropin Reminyl Ultracet
Amevive Copaxone Gleevec Ofloxacin Inj Restatis Ultram
Amphotericin B Inj Copegus Halotestin Orthoclone Retin A Venoglobulin
Anabolic Steroids Delatestryl Hepsera Oxandrin Ribavirin Vfend
Anadrol Depo Testosterone Humatrope Oxycodone SR Ritalin/SR/LA Vfend Inj
Androgel Desoxyn Humira Panretin Roferon Vidaza
Anzemet Dexedrine Infergen Pegasys Saizen Vitraset
Apokyn Diflucan 150mg Tab Intron A Peg-Intron Sandimmune Winstrol
Arava Dobutamine Inj Iressa Penlac Sandoglobulin Xifaxin
Atrovent Amp Dopamine Inj Kepivance Pentamidine Inj Sensipar Xolair
Avastin Doxycycline Inj Kineret Prograf Skelid 200mg Xoponex
Avelox Inj DuoNeb Kytril Prolastine Inj Somavert Zavesca
Avonex Elidel Lotrenox Protonix Inj Stadol NS Zelnorm
Balcofen Inj Emend Lunesta Protopic Straterra Zenapax
BCG Vaccine Enbrel Metadate CD Protropin Symlin Zithromax Inj
Betaseron Erbitux
Methotrexate
(MTX) Provigil Tamiflu Zofran
Botox Farbazyme Inj Methylin ER Pulmicort Resp. Tarceva Zyvox
Brethine Amp Fludarabine Inj Metronidazole Inj Pulmozyme Targretin Gel
Byetta Focalin Mucomyst Rapamune Tazorac Cream
Camptosar Inj Forteo Myfortic Raptiva Testim
67
ALTERNATIVE DISPUTE RESOLUTION
1. Binding Arbitration.
Except as otherwise provided in the Agreement, the Parties agree that any controversy or claim
including, but not limited to, any alleged class actions, arising out of or relating to the Agreement or the
breach thereof, whether involving a claim in tort, contract or otherwise, that cannot be resolved by
informal means, shall be settled by final and binding arbitration as its exclusive remedy. A party
aggrieved by the alleged failure, neglect, or refusal of another to arbitrate under the Agreement for
arbitration may petition the applicable United States District Court of Texas for an order directing that
such arbitration proceed in the manner provided for in the Agreement. The Parties expressly agree,
however, that the right of either party to terminate the Agreement pursuant to the Agreement and Bravo
Health’s right to withdraw from a service area is absolute and shall not be subject to arbitration. All
arbitration proceedings shall take place in the applicable State in which Provider is to provide Covered
Services under the Agreement.
2. Rules for Arbitration.
The Parties agree to adopt the Rules of Procedure for Arbitration (“Rules”) and the Code of Ethics for
Arbitrators (“Code”) of the American Health Lawyers Association Alternative Dispute Resolution
Service (collectively referred to as “AHLA”). The AHLA Rules and Code for Arbitration shall apply to
any arbitration under the Agreement unless otherwise specifically stated or supplemented in the
Agreement. In the event of any conflict between the AHLA Rules and Code for Arbitration and the
Agreement, the provisions of this language and the Agreement shall control.
3. Demands for Arbitration and Selection of Arbitrators.
The demand for arbitration shall be in writing and shall be served in the manner prescribed in Section
7.9 of the Agreement. The demand for arbitration shall set forth a detailed statement of the issue and
facts supporting the arbitration demand, shall specify the matters to be arbitrated, including
identification of the Section or Article of the Agreement in dispute, and shall identify the name and
address of the Arbitrator chosen by the Party making such demand. The other Party to the dispute shall
appoint an Arbitrator, shall give written notice of such appointment in accordance with Section 7.9 to
the other Party, and shall specify the name and address of such Arbitrator within forty-five (45) calendar
days after receipt of the demand,. If such Party fails to appoint an Arbitrator and notify the other Party
as herein provided within such forty-five (45) calendar day period, the Party making the arbitration
demand shall have the right to apply to the Chief Judge of the United States District Court of Texas for
the appointment of an Arbitrator. Each Arbitrator must have a minimum of ten (10) years of legal
experience or professional experience in the healthcare industry.
4. Procedure for Selection of Third Arbitrator.
The two (2) Arbitrators appointed or selected as set forth in Section 6.4 shall appoint a third Arbitrator
as soon as practicable, or if they do not do so within forty-five (45) calendar days after notice is given to
the Parties of the appointment of the second Arbitrator, any Party may apply to the Chief Judge of the
United States District Court of Texas for the appointment of an Arbitrator. After the appointment of the
third Arbitrator, the Arbitrators shall hold a preliminary conference with the Parties within thirty (30)
days to define and narrow the issues and claims to be arbitrated. The arbitrator may, at the preliminary
conference, establish the extent of and schedule for the production of documents and other information,
identify the form of evidence to be presented, and limit discovery.
68
5. Scheduling and Timing of Arbitration.
The arbitrators must begin the formal arbitration hearing within one hundred-twenty (120) days of the
date the last arbitrator is appointed. The arbitration hearing must be completed within sixty (60) days
following the close of discovery. The parties and arbitrators shall use their best efforts to ensure that the
arbitration hearing proceeds in a timely fashion without unnecessary delay (“unnecessary delay” is
defined as a period of time that exceeds five (5) consecutive business days). The Parties must ascertain
the ability of each arbitrator to comply with this scheduling requirement as a condition of his/her
selection as an arbitrator. If the arbitration hearing is not begun within this period, either Party shall
have the right to file suit, a motion, a petition, or otherwise commence a legal proceeding in the United
States District Court of Texas and shall have the right to refuse to participate further in any arbitration
proceeding related to the same dispute.
6. Discovery.
In any such arbitration proceeding, each Party thereto shall have access to the relevant books and
records of the other Party and the power to call any employee, agent or officer of any other Party for
testimony and shall have all other rights to discovery afforded under the Federal Rules of Civil
Procedure, as well as the rules or laws applicable to the Federal District Court proceedings in Texas, all
of which shall be fully enforceable by the arbitrators or, if they fail to effect such enforcement, by the
United States District Court of Texas. Any discovery by the Parties to the arbitration shall be performed
within a discovery period to be defined and limited by the arbitrators, but in no event shall such
discovery period exceed ninety (90) calendar days following the preliminary conference, unless an
extension is mutually agreed upon in writing by the Parties.
The parties agree that each will be limited to a maximum of twenty-five (25) (including subparts)
written interrogatories and/or written document requests and/or written requests for admissions.
Responses to written discovery are due within thirty (30) days of service. Upon motion by the
aggrieved party, the arbitrators may enter any appropriate orders for non-compliance with discovery
requests against the other party up to, and including, preclusion of the presentation of certain evidence
not produced in a timely fashion. The parties may agree to reasonable extensions to respond to the
other’s discovery requests so long as the extension does not extend the overall discovery period beyond
ninety (90) calendar days following the preliminary conference.
Each party will be limited to no more than five (5) party opponent depositions and the parties agree to
make requested employees available for deposition within forty-five (45) days of such a request. If
either party believes a deposition has been requested in bad faith or for the purposes of harassment,
delay or otherwise, either party may move for an appropriate protective order and the arbitrators shall
rule on such protective order. Either party may also move for additional depositions or deponents
should the issues reasonably require and the arbitrators shall rule on such request.
The arbitrators shall strictly enforce these discovery limits. With respect to any motions to extend or
expand discovery, the arbitrators shall not agree to do so unless, the requesting party has shown good
cause as to why the additional or expanded discovery is necessary.
On motion by either Party and for good cause shown, the arbitrators shall have the power to enter and
impose any appropriate protective orders limiting use and disclosure of any information submitted
during, or related to, the arbitration. In addition, the arbitrators shall abide by any protective orders
agreed upon by the Parties.
69
7. Evidence.
Any arbitration pursuant to this Section shall be conducted by the Arbitrators under the guidance of the
Federal Rules of Evidence. The Arbitrators, however, shall not be required to conform strictly to such
Rules in conducting any such arbitration. The Arbitrators shall conduct such evidentiary or other
hearings as they deem necessary or appropriate and thereafter shall make their determination within ten
(10) days of any evidentiary hearing or motion.
The parties may offer such non-duplicative evidence as is relevant and material to the dispute and shall
produce such evidence as the arbitrators may deem necessary to an understanding and determination of
the dispute. An arbitrator or other person authorized by law to subpoena witnesses or documents may
do so upon the request of a Party or upon the arbitrators’ own motion.
The arbitrators shall be the judges for the duplicative nature, relevance and materiality of the evidence
offered and, as noted above, the Federal Rules of Evidence shall serve as guidance; however, strict
conformity is not necessary. The arbitrators should refuse to allow the introduction of any evidence that
the arbitrators believe would result in the disclosure of confidential information which is privileged
under any applicable statute or under applicable law, including, but not limited to, information subject
to: (a) a peer review privilege; (b) a patient-physician privilege; (c) an attorney-client privilege; or (d)
any business proprietary or trade secret privilege. All evidence shall be taken in the presence of the
arbitrators and all of the Parties and the Parties’ counsel and other authorized representatives, except
where a Party is absent after due notice has been given or has waived the right to be present.
8. Judgment and Award of Arbitrators.
The arbitrators shall render their decision and award upon the concurrence of at least two (2) of their
number. Such decision and award shall be in writing and shall be signed by all three (3) arbitrators.
Thereafter, counterpart copies thereof shall be delivered to each of the Parties simultaneously. In
rendering such decision and award, the arbitrators shall not add to, subtract from, or otherwise modify
the provisions of the Agreement or any agreement entered into pursuant hereto. The arbitrators shall
have the power to grant and award only legal remedies in the form of monetary damages as provided by
Texas law, except that the arbitrators shall not have the power to award punitive or exemplary damages.
As used herein, punitive or exemplary damages include, but are not limited to, multiple damage awards
and any award of attorneys’ fees, regardless of whether these types of damages are based on statute or
common law. Notwithstanding the above, in the event that either Party wishes to obtain injunctive
relief, such as a permanent or temporary restraining order, such Party may initiate an action for such
relief in a court of competent jurisdiction in the State of Texas. The decision of the court with respect to
the requested injunctive relief shall be subject to appeal only as allowed under applicable state or federal
law. However, the courts shall not have the authority to review or grant any requests or demands for
damages.
The judgment and award of the arbitrators shall be accompanied by detailed written findings of fact and
conclusions of law. At any time within one year after the award is made, any party to the arbitration
may apply to the United States District Court of Texas for an order confirming the award.
70
9. Confidentiality of Arbitration.
Except in connection with the enforcement of such award or as otherwise may be required by law, all
aspects of such arbitration proceeding will be held in strict confidence by the Parties and arbitrators and
shall not be disclosed to any third party without the prior written consent of the disclosing Party. The
parties agree that a breach of the terms of this confidentiality requirement will cause immediate and
irreparable harm to the disclosing party. As such, in addition to any other rights or remedies available at
law or in equity, the disclosing party is entitled to injunctive relief to restrain or enjoin such breach
without the need to prove actual damages.
Within sixty (60) days of the date of the decision and award of the arbitrators, the Parties agree to return
and/or destroy and provide certification of destruction of any confidential materials provided by the
other party during arbitration process. The arbitrators will also return and/or destroy and provide
certification of destruction of any confidential materials provided to them by the Parties during the
arbitration process. The Parties and their respective counsel are permitted to keep their own
confidential materials along with any attorney client privileged communications or attorney work
products.
10. Fees and Transcript of Arbitration.
The fees and expenses of each arbitrator and all other costs and expenses incurred in the arbitration,
including reasonable attorneys’ fees shall become due as specified in the arbitration award. The
arbitration award shall not include any punitive, exemplary, or other non-economic damage component.
A full and complete record and transcript of the arbitration proceeding shall be maintained. If either
Party desires a copy of the record and transcript, that Party shall bear the fees and expenses for the
record and transcript. If both Parties desire a copy then such fees and expenses will be equally shared
between the Parties.
11. Limitation of Other Proceedings.
Each Party agrees that it will not file, nor will it cause any other individual or entity to file, any suit,
motion, and petition or otherwise commence any legal proceeding which must be submitted to
arbitration pursuant to the Agreement. Upon the entry of an order dismissing or staying any such action
or proceeding in a court, the Party that filed such action or proceeding shall promptly pay to the other
Party the attorney’s fees, costs, and expenses incurred by such other Party prior to the entry of such
order.
71
Bravo Health Adult Prevention and Screening Guidelines - 2008
This chart of suggested services has been adapted from the U.S. Preventive Services Task Force Recommendations, American Diabetes Association, and American Medical Association by Bravo
Health Clinicians. It is intended to provide guidance to practitioners in selecting appropriate prevention and screening services for Bravo Health Members. It contains guidelines only and should never
supersede clinical judgment. The practitioner in conjunction with the patient or responsible party should decide whether these or other recommended services should be performed more frequently,
less frequently, or not at all. As with all services provided to Bravo Health Members, the clinical judgment and the discussion around it should be documented in the medical record. (March 17, 2006)
Females Only
Males Only
Health
Maintenance
Frequency Health Maintenance Frequency
Pelvic exam and
pap smear
At least every three years up to age 70. Prostate Cancer screening
• Digital rectal screening
• PSA
Case – by - Case basis
Case – by - Case basis
Breast examination Yearly Abdominal Aortic Aneurysm
• Abdominal ultrasonography
Screening for men aged 65-75
years who have ever smoked
Mammography Every 1-2 for women age 40 and older
Yearly for women age 50 and older
Osteoporosis Routine screening beginning at age 65. Screening for women with increased
risk for osteoporotic fractures beginning at age 60
Health Maintenance
Frequency
Physical Assessment Within 30 days of enrollment & yearly
Height & Weight Yearly
Blood Pressure Each visit and at least yearly
Lipid Profile Initial assessment & periodically
Thyroid screening Initial assessment & periodically
Diabetes screening Initial assessment & every 3 years. Earlier for high risk
patients at the discretion of the physician
Obesity screening (BMI) Initial assessment & yearly
Screening for Depression Periodically according to patient’s needs
Hearing screening Periodically according to patient’s needs
Vision screening Periodically according to patient’s needs
Glaucoma screening Periodically according to patient’s needs
Colon Cancer screening
• Colonoscopy
• Fecal Occult Blood
Every 10 years
Yearly
Aspirin use for the prevention of
cardiovascular events
Discuss with adults who are at increased risk for
cardiovascular disease (men>40 years and post-menopausal
women). Discussions should address both the potential
benefits and harms of aspirin therapy
PPD Periodically according to patient’s needs
Discussion and Counseling
(All Members)
Frequency
Diet Initial assessment and yearly for obese adults
(BMI>=30)
Exercise Initial assessment and periodically
Physical Activity At least yearly
Tobacco Use At least yearly
Alcohol use At least yearly
Dental health
At least yearly
Fall Prevention At least yearly
Vehicle Safety At least yearly
Safe Sexual Practice At least yearly
Immunization Frequency
Influenza Yearly
Pneumococcal vaccine One dose for persons under 65 who have chronic
disorders of cardiovascular or pulmonary systems,
diabetes, renal dysfunction, or immunosuppression.
One dose for nursing home residents
One dose for person age 65 and older
One dose revaccination for persons age 65 and older
if 5 years or more have past since the last dose
Tetanus-diphtheria booster Every 10 years
72

Bravo Health
7551 Callaghan Road, Suite 310
San Antonio, TX 78229
Provider Services: 1-800-291-0396 Sales Inquiries: 1-866-790-9079
TTY: 1-800-964-2591 (for the hearing impaired)
www.bravohealth.com