SET 10 Appendix E 1
User Manual: SET-10
Open the PDF directly: View PDF ![]() .
.
Page Count: 45

©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
1
American Academy of Neurology
Multiple Sclerosis
Quality Measurement Set
Approved by the Multiple Sclerosis Quality Measurement Development Work Group on February 12,
2015, by the AAN Quality and Safety Subcommittee on February 20, 2015; by the AAN Practice
Committee on March 10, 2015; and by the AANI Board of Directors on March 24, 2015.
This measurement set was endorsed by the American Association of Neuroscience Nurses
on March 13, 2015.

©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
2
Disclaimer
Performance Measures (Measures) and related data specifications developed by the American Academy
of Neurology (AAN) are intended to facilitate quality improvement activities by providers.
AAN Measures: 1) are not clinical guidelines and do not establish a standard of medical care, and have
not been tested for all potential applications; 2) are not continually updated and may not reflect the most
recent information; and 3) are subject to review and may be revised or rescinded at any time by the AAN.
The measures, while copyrighted, can be reproduced and distributed, without modification, for
noncommercial purposes (e.g., use by health care providers in connection with their practices); they must
not be altered without prior written approval from the AAN. Commercial use is defined as the sale,
license, or distribution of the measures for commercial gain, or incorporation of the measures into a
product or service that is sold, licensed, or distributed for commercial gain. Commercial uses of the
measures require a license agreement between the user and the AAN. Neither the AAN nor its members
are responsible for any use of the measures.
AAN Measures and related data specifications do not mandate any particular course of medical care and
are not intended to substitute for the independent professional judgment of the treating provider, as the
information does not account for individual variation among patients. In all cases, the selected course of
action should be considered by the treating provider in the context of treating the individual patient. Use
of the information is voluntary. AAN provides this information on an “as is” basis, and makes no
warranty, expressed or implied, regarding the information. AAN specifically disclaims any warranties of
merchantability or fitness for a particular use or purpose. AAN assumes no responsibility for any injury or
damage to persons or property arising out of or related to any use of this information or for any errors or
omissions.
©2014 American Academy of Neurology. All rights reserved.
Limited proprietary coding is contained in the measure specifications for convenience. Users of the
proprietary coding sets should obtain all necessary licenses from the owners of these code sets. The AAN
and its members disclaim all liability for use or accuracy of any Current Procedural Terminology (CPT®)
or other coding contained in the specifications. ICD-10 copyright 2012 International Health Terminology
Standards Development Organization
CPT ® is a registered trademark of the American Medical Association and is copyright 2012. CPT®
codes contained in the Measure specifications are copyright 2004-2013 American Medical Association.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
3
Table of Contents
Page
Work Group Members
4
Improving Outcomes for Patients with Multiple Sclerosis (MS)
5
Clinical Evidence Base
6
Definitions and Abbreviations
6
Desired Outcomes
7
Work Group Recommendations
7
Other Potential Measures
8
Intended Care Audience, Settings, and Patient Population
9
Measure Harmonization
9
Technical Specifications Overview
9
Measure Exceptions
10
Testing and Implementation of the Measurement Set
10
Multiple Sclerosis Measurement Set
1. Multiple Sclerosis (MS) Diagnosis
11
2. Comparison MRI Within 24 Months of MS Diagnosis
14
3. Current MS Disability Scale Score
17
4. Fall Risk Screening for Patients with MS
20
5. Bladder Infections for Patients with MS
23
6. Exercise and Appropriate Physical Activity Counseling for Patients with MS
26
7. Fatigue Outcome for Patients with MS
29
8. Cognitive Impairment Testing for Patients with MS
32
9. Clinical Depression Screening for Patients with MS
35
10. Depression Outcome for Patients with MS
38
11. Maintained or Improved Baseline Quality of Life for Patients with MS
41
Contact Information
44
References
44
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
4
Multiple Sclerosis Work Group Members
Co-Chairs
Christopher Bever, MD, MBA, FAAN
Alexander Rae-Grant, MD, FRCP(C)
American Academy of Neurology
Barbara Giesser, MD, FAAN
Douglas Jeffery, MD, PhD
Mitch Wallin, MD, MPH
Mary Alissa Willis, MD
American Academy of Physical Medicine and
Rehabilitation
K. Rao Poduri, MD, FAA PMR
American Association of Neuroscience Nurses
Patricia Pagnotta, MSN, ARNP, CNRN, MSCN
American Association of Nurse Practitioners
Carrie Sammarco, DrNP, FNP-C, MSCN
American Occupational Therapy Association
Virgil Mathiowetz, PhD, OTR/L, FAOTA
American Physical Therapy Association
Amy Yorke, PT, PhD, NCS
American Psychiatric Association
Melanie Schwarz, MD
American Society of Neurorehabiltation
Victor Mark, MD
Anthem
Ronald Koenig, MD, FAAN
National Academy of Neuropsychology
John DeLuca, PhD
Consortium of Multiple Sclerosis Centers
June Halper, MSN, APN-C, MSCN, FAAN
Multiple Sclerosis Association of America
Cindy Richman
Multiple Sclerosis Foundation
Annette Okai, MD
National Multiple Sclerosis Society
Nicholas LaRocca, PhD
National Multiple Sclerosis Society – Midwest
Chapter
William MacNally, MHA, FACHE
Work Group Facilitators
Eric Cheng, MD, MS, FAAN
Michael Phipps, MD, MHS
Amy Sanders, MD, MS
American Academy of Neurology Staff
Amy Bennett, JD
Gina Gjorvad
Erin Hagen
Becky Schierman, MPH
Declined
Aetna, American Academy of Family
Physicians, American Academy of
Ophthalmology, American Chronic Pain
Association, American Congress of
Rehabilitation Medicine, American Pain
Society, American Psychological Association,
Cigna, First Coast Service Options, Health Net,
Highmark, Humana, Paralyzed Veterans of
America, United Healthcare

©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
5
Improving Outcomes for Patients with Multiple Sclerosis (MS)
Purpose of Measurement Set
In 2014, the American Academy of Neurology (AAN) formed a multi-disciplinary Multiple Sclerosis
Work Group (Work Group) to review existing guidelines and evidence, gaps in care and to develop a
measurement set for multiple sclerosis (MS) to promote quality improvement and drive improved
outcomes for patients with MS.
The AAN develops quality measures based on the belief that neurologists should play a major role in
selecting and creating performance measures that will drive performance improvement and possibly be
used in accountability programs. The AAN formed the Work Group with representatives from
professional associations, patient advocacy organizations, and payers to ensure measures developed
include input from all members of the healthcare team. All members of the Work Group were required to
disclose relationships with industry and other entities to avoid actual, potential, or perceived conflicts of
interest.
Topic Importance
It is estimated that MS affects about 400,000 Americans and is the leading cause of disability among
young adults.
1
,
2
The disorder generally worsens over time, leading to irreversible functional disability
with symptoms including visual or sensory disturbances, loss of strength, tremor, ambulatory problems,
loss of bladder/bowel control, fatigue, spasticity, cognitive impairment and sexual dysfunction. Further,
the number of people with MS worldwide is approximately 2.3 to 2.5 million.
3
,
4
MS is not a “reportable”
disease in the United States, which makes it difficult to determine an accurate number of individuals who
have MS.
5
There are twice as many women with MS as men with MS overall.3 Geographic differences in
the prevalence of MS in the United States have been noted.
6
80% of patients present with an initial episode of neurological symptoms, which can either represent a
clinically isolated syndrome or multiple sclerosis depending on clinical and magnetic resonance imaging
(MRI) factors. Of these those who have white-matter abnormalities on MRI, the chance of a second attack
subsequently occurring increases from 50% at 2 years to 82% at 20 years.
7
Progression to the secondary
progressive phase starts at varying age but averages about 40 years of age.7
Compston notes that death is attributable to MS in two-thirds of cases and to increased infection risks and
complications in others.7 The median time to death is around 30 years from disease onset, which
represents a reduction in life expectancy of 5-10 years.7
The cost of MS is rapidly rising given the advances of in therapies. A review of the cost burden of MS
indicated the mean cost for patients with MS ranged from $8,528-$54,244 per year and direct costs,
including hospitalization, outpatient care and pharmaceuticals, ranged from $6,144-$34,511 in 2011
dollars.
8
Prescription drugs and indirect costs, such as disease-related absences from work, were the
biggest single cost drivers of MS representing an average of 50% and 23% of total costs.8 This high cost
burden review did not include newer, more costly therapies.8
Opportunities for Improvement
Additional data on opportunities for improvement and gaps in care specific to the MS measures can be
located in the quality measurement set that follows. Treatment use remains uneven, and treatment of MS
is much debated due to the fact available treatments are expensive and do not always meet routine
standards for cost-effectiveness.8
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
6
Clinical Evidence Base
The MS Work Group reviewed existing literature and consulted MS clinical practice guidelines including:
1. Assessment and Management of Psychiatric Disorders in Individuals with MS: Report of the
Guideline Development Subcommittee of the American Academy of Neurology.
9
2. Evidence report: the efficacy and safety of mitoxantrone (Novantrone) in the treatment of
multiple sclerosis.
10
3. Neutralizing antibodies to interferon beta: Assessment of their clinical and radiographic impact:
An evidence report.
11
4. Evidence-based guideline update: plasmapheresis in neurologic disorders.
12
5. Evidence-based guideline: clinical evaluation and treatment of transverse myelitis.
13
6. Practice parameter: The usefulness of evoked potentials in identifying clinically silent lesions in
patients with suspected multiple sclerosis (an evidence-based review): Report of the Quality
Standards Subcommittee of the American Academy of Neurology.
14
7. Evidence-based guideline: Complementary and alternative medicine in multiple sclerosis.
15
8. Multiple sclerosis: management of multiple sclerosis in primary and secondary care.
16
9. Nursing management of the patient with multiple sclerosis.
17
10. EFNS guidelines on the use of anti-interferon beta antibody measurements in multiple sclerosis.
18
11. EFNS guidelines on acute relapses of multiple sclerosis.
19
12. Fingolimod for the treatment of highly active relapsing-remitting multiple sclerosis.
20
13. Consortium of MS Centers MRI Protocol for the Diagnosis and Follow-up of MS 2009 Revised
Guidelines.
21
14. The importance of quality-of-life assessment in the management of patients with multiple
sclerosis Recommendations from the Middle East MS Advisory Group.
22
Definitions and Abbreviations in the Measurement Set
The Work Group utilized the following definitions and abbreviations in the measurement set:
Consult: to ask the advice or opinion of (Merriam-Webster
23
)
Counsel: to advise seriously and formally after consultation (Merriam-Webster
24
)
Educate: to give someone information or training about something (Merriam-Webster
25
)
Refer: to send or direct for diagnosis or treatment (Merriam-Webster
26
)
Screen: to test or examine for the presence of something (Merriam-Webster
27
)
Below is a list of acronyms utilized in this document. The AAN has a Quality Improvement Glossary,
which provides more in depth explanations and is available at aan.com/practice/quality-measures/quality-
resources.
ACO: Accountable Care Organization
ADL: Activities of Daily Living
CMS: Centers for Medicare & Medicaid Services
DMT: Disease Modifying Therapy
MS: Multiple Sclerosis
NQF: National Quality Forum
PQRS: Physician Quality Reporting System
QOL: Quality of Life
Desired Outcomes
The Work Group reviewed desired outcomes for patients with MS and identified the following:
• Confirmation of MS diagnosis as soon as possible
• Reduce mortality directly related to MS
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
7
• Reduce MS progression
• Reduce MS exacerbation frequency
• Maintain or increase existing cognitive and physical functioning levels
• Reduce affective symptoms in patient population, which include, but are not limited to emotional
lability, depression, and anxiety
• Reduce falls
• Improve adherence to Disease Modifying Therapy (DMT)
• Increase patients engagement in treatment decision process
• Increase patients acting on received MS education and incorporating information into treatment
• Improve quality of care from a coordinated treatment team
• Address all patient needs and engage all patients on a personal level
• Increase patient satisfaction with care provided
• Reduce caregiver burden
• Decrease rates of comorbidities (i.e., HTN, Diabetes, Smoking Obesity)
• Increase Quality of Life ratings
• Reduce hospitalizations
• Decrease complications of MS:
• Pressure Ulcers
• Fatigue
• Spasticity
• Pain and Headache
• Sexual Dysfunction
• Bowel and Urinary Dysfunction
Work Group Recommendations
The Work Group recommended the following measures be developed.
Multiple Sclerosis Measurement Set
1. Multiple Sclerosis (MS) Diagnosis
2. Comparison MRI Within 24 Months of MS Diagnosis
3. Current MS Disability Scale Score
4. Fall Risk Screening for Patients with MS
5. Bladder Infections for Patients with MS
6. Exercise and Appropriate Physical Activity Counseling for Patients with MS
7. Fatigue Outcome for Patients with MS
8. Cognitive Impairment Testing for Patients with MS
9. Clinical Depression Screening for Patients with MS
10. Depression Outcome for Patients with MS
11. Maintained or Improved Baseline Quality of Life for Patients with MS
Other Potential Measures
It is impossible for one quality measurement set to address all MS quality of care issues. At the
beginning of this project, it was determined the scope would be limited. Neuromyelitis Optica (NMO)
and Clinically Isolated Syndrome (CIS) measures were excluded from project scope.
The Work Group evaluated possible MS relapse measures. Development of a relapse measure was
deemed to be of high importance given the fact that reduction of the number of relapses is considered to
be one of the most important desired outcomes for a patient with MS. However, potential measure drafts
were noted to be potentially cost inefficient, difficult or impossible to measure, difficult or impossible for
a practitioner to act upon. Possible relapse measures discussed included:
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
8
The percentage of patients with multiple sclerosis who demonstrate a response to treatment at
twelve months defined by a reduction of new lesion formation and active lesions on MRI from
prior MRI in measurement period.
Percentage of patients with multiple sclerosis who did not require steroids or inpatient treatment
during a 12-month period.
Percentage of patients with multiple sclerosis who demonstrate a response to treatment at twelve
months defined by maintenance or improvement of Expanded Disability Scale Score (EDSS).
Percentage of patients with relapsing or secondary progressive MS with relapses in a given
population during a 12-month period. (Such a measure would be useful for comparisons of
different MS centers.)
Percentage of patients with MS with defined relapses affecting function offered treatment for
their relapses/number of patients with defined relapses.
Percentage of patients with multiple sclerosis who reported relapses.
The Work Group also considered a treatment complication – spasticity measure. A lack of adequate
outcome scale prevented further development of such a measure. Lack of uniformity in documenting
spasticity evaluation and an electronic health record (EHR) variability exacerbated spasticity measure
development (i.e., most spasticity evaluations are recorded in an EHR as free form text, which would
result in a manual chart review.)
The Work Group discussed development of a measure related to DMT, but was unable to locate published
data supporting a treatment gap in care. There were also concerns that a denominator cannot be readily
identified using administrative data with limitations in ICD coding. The Work Group developed measure
concepts to address mobility and visual deficits, but did not approve these concepts for further
development following the in person meeting.
The Work Group approved pain assessment and fall follow-up plan documented measures for public
comment. These measures were withdrawn following public comment. The pain assessment measure was
withdrawn due to concern that it unnecessarily duplicates existing measures. The Work Group encourages
individuals to consider National Quality Forum (NQF) endorsed measure #0420 and adopted into
Physician Quality Reporting System (PQRS) measure #131. The fall follow-up measure was withdrawn
due to potential difficulty locating follow-up plan documentation. Locating follow-up plan documentation
would potentially require burdensome chart review, as the information would not be easily accessed in an
EHR.
Intended Care Audience, Settings, and Patient Population
The AAN encourages use of these measures by physicians, other health care professionals, and the health
care systems, where appropriate, to achieve improved performance and as steps towards optimized
clinical outcomes for patients with MS. The Work Group included adolescent populations for select
measures where appropriate and supported by the evidence.
Not all AAN measures are appropriate for accountability programs, and the MS Work Group has
designated appropriate measures use in the measure descriptions that follow. The following is a summary
of measures recommended for use in accountability programs.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
9
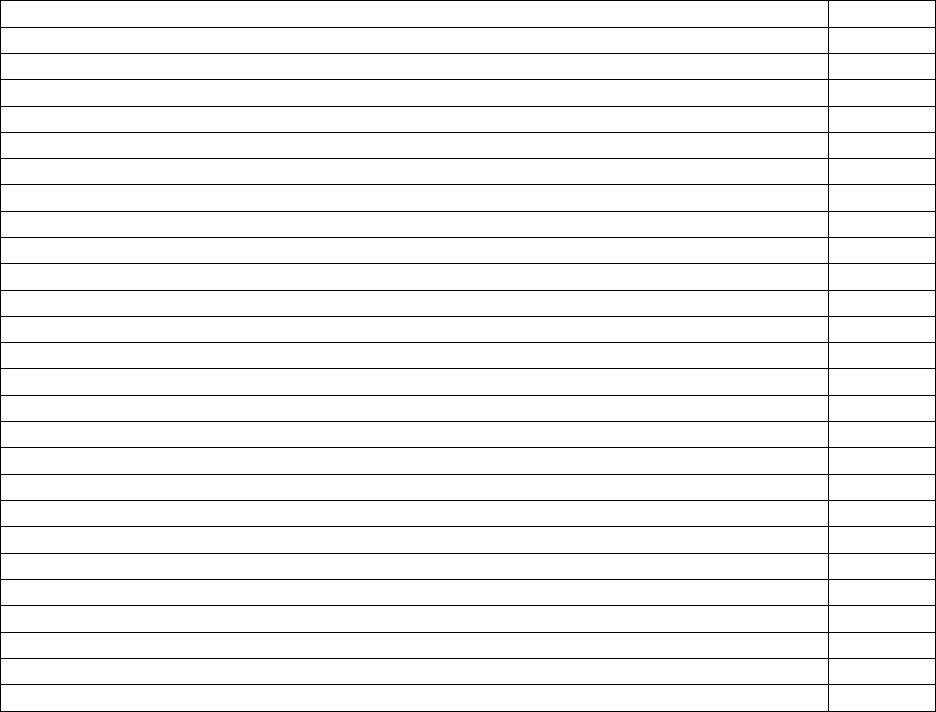
Multiple Sclerosis Measurement Set
Recommended for
Accountability Programs
1. Multiple Sclerosis (MS) Diagnosis
No
2. Comparison MRI Within 24 Months of MS Diagnosis
No
3. Current MS Disability Scale Score
Yes
4. Fall Risk Screening for Patients with MS
Yes
5. Bladder Infections for Patients with MS
Yes
For System or Health Plans Only
6. Exercise and Appropriate Physical Activity Counseling for
Patients with MS
Yes
7. Fatigue Outcome for Patients with MS
Yes
For System or Health Plans Only
8. Cognitive Impairment Testing for Patients with MS
Yes
For System or Health Plans Only
9. Clinical Depression Screening for Patients with MS
Yes
10. Depression Outcome for Patients with MS
Yes
For System or Health Plans Only
11. Maintained or Improved Baseline Quality of Life for Patients
with MS
Yes
For System or Health Plans Only
Measure Harmonization
The MS Work Group searched for existing performance measures operating with a denominator of
patients with MS, and did not locate any. Cheng et al. created a list of quality indicators specific to MS
that was reviewed by the Work Group.
28
Efforts were made to unify denominator statements when
possible to ease data collection. Multiple measure sets exist that have potential implications for patients
with MS such as depression, urinary function, etc. Details on how these existing measures were
harmonized are included in the specific measure specifications that follow below.
Technical Specifications Overview
The AAN develops technical specifications for measures that may include:
Electronic Health Record (EHR) Data
Electronic Administrative Data (Claims)
Chart Review (for select measures where EHR data cannot be gathered)
Registry
Administrative claims specifications are provided for MS measures when applicable. The AAN is in the
process of creating code value sets and the logic required for electronic capture of the quality measures
with EHRs, when possible. A listing of the quality data model elements, code value sets, and measure
logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made available at
a later date. These technical specifications will be updated as warranted.
The measurement set includes measures that require the use of validated screening tools. The Work
Group discussed and determined that multiple tools should be offered to allow providers to determine
which tool best meets their individual practice needs. Tools may be subject to copyright and require
licensing fees.

©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
10
Measure Exceptions
A denominator exclusion is a factor supported by the clinical evidence that removes a patient from
inclusion in the measure population. For example, if the denominator indicates the measure is for all
patients aged 0 to 18 years of age, a patient who is 19 years of age is excluded.
A denominator exception is a condition that should remove the patient, procedure or unit of measurement
from the denominator only if the numerator criteria are not met. The AAN includes three possible types
of exceptions for reasons why a patient should not be included in a measure denominator: medical (e.g.,
contraindication), patient (e.g., declination or religious belief), or system (e.g., resource limitation)
reasons. For each measure, there must be a clear rationale to permit an exception for a medical, patient, or
system reason. The Work Group provided explicit exceptions when applicable for ease of use in
eMeasure development.
Testing and Implementation of the Measurement Set
The MS measures in this set are being made available without any prior testing. The AAN encourages
testing of this measurement set for feasibility and reliability by organizations or individuals positioned to
do so. Any testing data gathered will be considered during future measurement set updates. Select
measures will be beta tested once the set has been released, prior to submission to the National Quality
Forum for possible endorsement. All readers are encouraged to read the AAN Statement on Comparing
Outcomes of Patients available in the AAN measurement manual. (https://www.aan.com/practice/quality-
measures/about-quality-measures/)
This measure set includes outcome measures which are intended to be applied at the system or
accountable care organization level. Use of these measures to compare providers or practices would
require the application of a valid risk adjustment methodology which does not exist for MS populations.
These measures may be used for accountability at the system or accountable care organization level if the
MS populations being compared are similar in demographics, socioeconomic status and the prevalence of
comorbid conditions. These measures may also be used for internal, non-publicly reported quality
improvement for a patient population that is not subject to significant change, as risk adjustment or
stratification would not be required.
The AAN encourages a minimum sample size of 20 for use in public reporting programs to reduce
likelihood of error. The number 20 reflects current CMS sample requirements for Physician Compare.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
11
Multiple Sclerosis (MS) Diagnosis
Measure Description
Percentage of patients who received a new diagnosis of multiple sclerosis in the past 12 months who
fulfilled international criteria.*
Measure Components
Numerator
Statement
Patients who received a new diagnosis of multiple sclerosis in the past 12
months who fulfilled international criteria.*
Definitions:
*International criteria is use of the either the 2005 or 2010 revised McDonald
criteria.1,2 These criteria facilitate the diagnosis of MS, but do not protect
against misdiagnosis. Additional diagnostic evaluation may be needed, and
this must be tailored to each patient’s clinical situation.
Denominator
Statement
All patients with a new diagnosis of MS in the past 12 months.
Denominator
Exclusions
Excluding other neuroimmunological syndromes including
Neuromyelitis Optica,
Clinically Isolated Syndrome,
Radiologically Isolated Syndrome, and
Acute Disseminated Encephalomyelitis.
Denominator
Exceptions
None
Supporting Guideline
& Other References
“A proportion of patients with nonspecific symptoms and nonspecific MRI
findings are referred to secondary and tertiary MS centers in the developed
world for a second opinion and do not in fact have MS.”1 Use of international
diagnostic criteria allows for a more rapid diagnosis of MS in some instances
and clarify and simplify the diagnostic process in many instances with fewer
MRI examinations.1, 2
Measure Importance
Relationship to
Desired Outcome
Desired outcome is to confirm diagnosis of MS in line with the most recent
internationally recognized criteria for the diagnosis. It is recognized that
excluding MS mimics is a key aspect of diagnosis which is not addressed by
this measure.3 Intention is to increase early diagnosis and treatment for
patients with MS and reduce costs of harms from delayed diagnosis of MS.
Patients meeting international diagnostic criteria for relapsing MS and
secondary progressive MS with relapses are potential candidate for disease
modifying therapy (DMT). It is anticipated that if measured, there is a
likelihood to reduce prescriptions and costs for patients not meeting DMT use
criteria who otherwise might be offered these treatments.
Opportunity for
Improvement
Diagnostic errors are common in MS.4,5 Misdiagnosis is a significant
contributor to patient harm.6 Increasing awareness and adherence to
international diagnostic criteria for MS is desired. A need to reduce the
population of patients using DMT who do not have MS by international
criteria exists. The measure does not require confirmation of diagnosis
through a second opinion or physician referral, but is intended to confirm
diagnosis only within the first twelve months of diagnosis or a referral to a
specialist.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
12
National Quality
Strategy Domains
☐ Patient and Family Engagement
☒ Patient Safety
☒Care Coordination
☐ Population/Public Health
☒ Efficient Use of Healthcare Resources
☐ Clinical Process/Effectiveness
Exception
Justification
Not Applicable
Harmonization with
Existing Measures
There are currently no other comparable measures in national measurement
programs or endorsed by the National Quality Forum.
Measure Designation
Measure Purpose
(Check all that apply)
☒ Quality improvement
☐Accountability
Type of Measure
(Check all that apply)
☐Process
☒ Outcome
☐ Structure
Level of
Measurement (Check
all that apply)
☒ Individual Provider
☒ Practice
Care Setting (Check
all that apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source (Check
all that apply)
☐ Electronic health record (EHR) data
☒Administrative Data/Claims
☒ Chart Review
☒ Registry
References
1 Polman CH, Reingold SC, Banwell B, et al. Diagnostic Criteria for Multiple Sclerosis: 2010 Revisions to the
McDonald Criteria. Ann Neurol 2011; 69:292-302.
2 Polman CH, Reingold SC, Edan, G, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the
“McDonald Criteria”. Annals of Neurology 2005; 58(6):840-846.
3 Miller DH, Weinshenker BG, Filippi M, et al. Differential diagnosis of suspected multiple sclerosis: a
consensus approach. Mult Scler 2008; 14:1157-1174.
4 Solomon AJ and Weinshenker BG. Misdiagnosis of Multiple Sclerosis: Frequency, Causes, Effects, and
Prevention. Curr Neurol Neurosci Rep 2013; 13:403.
5 Carmosino MJ, Brousseau KM, Arciniegas DB, et al. Initial Evaluations for Multiple Sclerosis in a University
Multiple Sclerosis Center. Arch Neurol 2005; 62:585-590.
6 El-Kareh R. Making Clinical Diagnoses: How Measureable Is the Process? National Quality Measures
Clearinghouse. May 5, 2014. Available at: http://www.qualitymeasures.ahrq.gov/expert/expert-
commentary.aspx?f=rss&id=47927
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
13
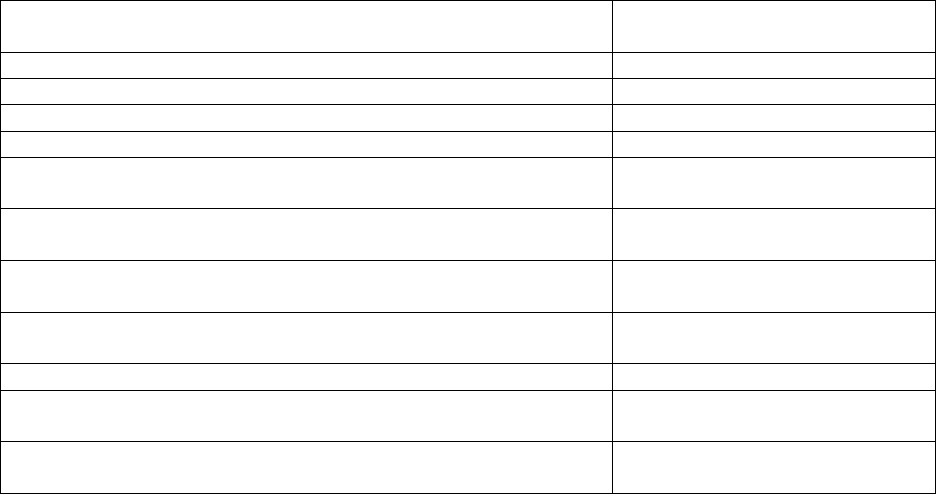
Denominator
(Eligible Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New
Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-
Established Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient
Consultation-New or Established Patient)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
14
Comparison MRI Within 24 Months of MS Diagnosis
Measure Description
Percentage of patients with MS who had an MRI with and without gadolinium within 24 months of
diagnosis compared with a baseline MRI.
Measure Components
Numerator
Statement
Patients with MS who had an MRI with and without gadolinium within 24 months
of diagnosis compared with a baseline MRI.
Denominator
Statement
All patients with a diagnosis of MS within the past 24 months.
Denominator
Exceptions
Patient has clinically evident disease activity.
Patient declines referral to MRI of brain and/or spinal cord for personal,
medical, or system reasons (i.e., claustrophobia).
Patient meets MRI exclusions (i.e., any trauma or surgery which may have
left ferromagnetic material in the body, ferromagnetic implants or
pacemakers; and inability to lie still for 1 hour or more).
Supporting
Guideline &
Other
References
The following evidence statements are quoted verbatim from the referenced
clinical guidelines:
“A brain MRI with gadolinium …for the following of MS patients to
assess subclinical disease activity should be CONSIDERED every 1 to 2
years.”1,2
Measure Importance
Relationship to
Desired
Outcome
The desired outcomes in MS patients are to prevent clinical relapses and to prevent
long term impairment and disability. Clinically apparent relapses are not fully
predictive of long term disability and prevention of relapses does not fully prevent
long term disability so more sensitive predictors of long term disability have been
sought. Disease activity that is seen on MRI, but not clinically evident, is
predictive of disability progression early in the disease course. Therefore, MRI is
being used as a sensitive biomarker of disease activity to judge long term
prognosis and to help guide the use of disease modifying therapies.
Opportunity for
Improvement
Prior to the recognition that MRI is more sensitive to MS disease activity than
monitoring of clinical symptoms, monitoring response to therapy was based
primarily on clinical symptoms. Because of this, many MS providers continue to
rely primarily on clinical evaluation to drive decision making in MS patients and
do not monitor MRI activity on a regular basis. Increasing the use of MRI
monitoring could lead to patients being moved to more effective therapies which
would reduce long term impairment and disability.
National Quality
Strategy
Domains
☐ Patient and Family Engagement
☐ Patient Safety
☐Care Coordination
☒ Population/Public Health
☐ Efficient Use of Healthcare Resources
☒ Clinical Process/Effectiveness
Exception
Justification
Exception provided for patients who have clinically evident disease
activity to reduce unnecessary MRI testing.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
15
Exception for patient declinations need as patients need to be willing to
undergo a MRI.
Exception for MRI exclusions necessary to avoid harm to patients.
Harmonization
with Existing
Measures
There are currently no other comparable measures in national measurement
programs or endorsed by the National Quality Forum.
Measure Designation
Measure
Purpose (check
all that apply)
☒ Quality improvement
☐ Accountability
Type of
Measure (check
all that apply)
☒ Process
☐ Outcome
☐ Structure
Level of
Measurement
(check all that
apply)
☒ Individual Provider
☒ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☐Electronic health record (EHR) data
☒ Administrative Data/Claims
☒Chart Review
☒ Registry
References
1 Consortium of Multiple Sclerosis Centers. Consortium of MS Centers MRI Protocol for the Diagnosis and
Follow-up of MS 2009 Revised Guidelines.
2 Simon JH, Li D, Traboulsee A, et al. Standardized MR imaging protocol for multiple sclerosis. Consortium of
MS Centers consensus guidelines. AJNR Am J Neuroradiol. 2006;27:455-461.
Additional Supporting References (Literature):
Bagnato F, Tancredi A, Richert N, et al. Contrast-enhanced magnetic resonance activity in relapsing-
remitting multiple sclerosis. Mult Scler 2000; 6: 43-49.
Rio J, Rovira A, Tintore M, et al. Evaluating the response to glatiramer acetate in relapsing-remitting
multiple sclerosis patients. Mult Scl 2014; Epub ahead of print, pubmed no 34622350.
Bermel RA, You X, Foulds P, et al. Predictors of long-term outcome in patients treated with interferon-
beta. Ann Neurol 2013; 73: 95-103.
Durelli L, Barbero P, Bergui M et al. MRI activity and neutralizing antibodies as predictors of response
to interferon-beta treatment in multiple sclerosis. J Neurol Neurosurg Psych 2008; 79: 646-651.
Grimaldi LM, Prosperini L, Vittello G, et al. MRI-based analysis of the natalizumab therapeutic
window. Mult Scler 2012; 18: 1337-1339.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
16
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
17
Current MS Disability Scale Score
Measure Description
Percentage of patients with MS who have a MS disability scale score* documented in the medical
record in the past 12 months.
Measure Components
Numerator
Statement
Patients with MS who have a MS disability scale score* documented in the
medical record in the past 12 months.
*MS disability scale score is defined as the score obtained from administering one
of the following:
Patient Determined Disease Steps (PDDS)1,
At least 2 measures of MS Functional Composite (MSFC)2,
Kurtzke Expanded Disability Status Scale (EDSS)3,4,
European Database on MS Grading System (EDMUS-GS)5,6,
Functional Independence Measure (FIM)7,
Guy’s Neurological Disability Scale (GNDS)8,
Neurological Rating Scale from the Scripps Clinic,9
MS Rating Scale, Revised (MSRS-S).10
Appropriate instruments from the NIH Toolbox (i.e. if the patient’s
primary impairment is motor, motor function would be assessed).11
Appropriate instruments from the PROMIS12 or NeuroQOL.13
Denominator
Statement
All patients with a diagnosis of MS.
Denominator
Exceptions
Patient declines to self-report and declines neurological examination.
Patient is unable to participate in neurological examination (i.e., advanced
stage dementia, profound psychosis, neurodevelopmental disorder, brain
injury encephalopathy, or hydrocephalus.)
Supporting
Guideline &
Other
References
Following evidence statements are quoted verbatim from the referenced clinical
guidelines:
“Ensure all people with MS have a comprehensive review of all aspects of
their care at least once a year.”14
“Tailor the comprehensive review to the needs of the person with MS
assessing: MS symptoms… MS disease course…”14
Measure Importance
Relationship to
Desired
Outcome
It is anticipated that by monitoring disease progression, clinicians will be able to
offer timely interventions, thereby reducing MS progression.
The annual relapse rate and Expanded Disability Status Scale (EDSS) progression
are the most commonly used clinical endpoints in disease modifying therapy
trials.3,4 A disability measure should be part of any annual assessment. The relapse
rate and disability progression are also important objective determinants for
changing MS therapy.1 Additionally, these morbidity endpoints are used in the
EDMUS database, Canadian MS Databases (BC and Ontario), NY State MS
Consortium, and NARCOMS.5,6,15
Opportunity for
Improvement
Not all patients in clinical practice have an annual validated MS scale
measurement. Clinicians cannot detect disability progression unless there is
regular assessment and comparison of assessment scores.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
18
National
Quality Strategy
Domains
☐ Patient and Family Engagement
☐ Patient Safety
☐Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☒ Clinical Process/Effectiveness
Exception
Justification
Patients need to be willing to undergo a standardized neurological examination for
most of the MS performance scales scores to be valid.
Harmonization
with Existing
Measures
There are currently no other comparable measures in national measurement
programs or endorsed by the National Quality Forum.
Measure Designation
Measure
Purpose (Check
all that apply)
☒ Quality improvement
☒ Accountability
Type of
Measure (Check
all that apply)
☒ Process
☐ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☒ Individual Provider
☒ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒ Administrative Data/Claims
☐ Chart Review
☒ Registry
References
1 Learmonth YC, Motl RW, Sandroff BM, et al. Validation of patient determined disease steps (PDDS) scale
scores in persons with multiple sclerosis. BMC Neurology 2013;13:37.
2 Cutter GR, Baier ML, Rudick RA, et al. Development of a multiple sclerosis functional composite as a clinical
trial outcome measure. Brain 1999; 122: 871–882
3 Kurtzke JF. Origin of DSS: to present the plan. Mult Scler 2007; 13:120-123.
4 Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS).
Neurology. 1983 Nov;33(11):1444-52.
5 Grimaud J, Amato MP, and Confavreux C. Design of a European multicenter study dedicated to the evaluation
of the EDMUS System: EVALUED. Mult Scler 1999; 5: 234-238.
6 Amato MP, Grimaud J, Achiti I, et. Al. European validation of a standardized clinical description of multiple
sclerosis. J Neurol 2004; 251: 1472-1480.
7 Ottenbacher KJ, Hsu Y, Granger CV, et al. The reliability of the Functional Independence Measure: a
quantitative review. Arch Phys Med Rehabil 1996;77:1226-32.
8 Sharrack B, Hughes RA. The Guy’s Neurological Disability Scale (GNDS): a new disability measure for
multiple sclerosis. Mult Scler. 199;5(4)223-233.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
19
9 Sipe JC, Knobler RL, Braheny SL, et al. A neurologic rating scale (NRS) for use in multiple sclerosis.
Neurology 1984;34:1368-1372.
10 Wicks P, Vaughan TE, and Massagli MP. The multiple sclerosis rating scale, revised (MSRS-R): Development,
refinement, and psychometric validation using an online community, Health and Quality of Life Outcomes.
2010;10:70.
11 Hodes RJ, Insel TR, Landis SC. On behalf of the NIH Blueprint for Neuroscience Research. The NIH Toolbox:
Setting a standard for biomedical research. Neurology 2013;80(S3):S1-S92. All NIH Toolbox-related materials
are ©2012 Northwestern University and the National Institutes of Health.
12 Cella D, Riley W, Stone A, et al. Initial Adult Health Item Banks and First Wave Testing of the Patient-
Reported Outcomes Measurement Information System (PROMIS) Network: 2005-2008. J Clin Epidemiol.
2010; 63(11):1179-1194.
13 Gershon RC, Lai JS, Bode R, et al. Neuro-QOL: quality of life item banks for adults with neurological
disorders: item development and calibrations based upon clinical and general population testing. Qual Life
Res. 2012; 21(3):475-486.
14 National Institute for Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis in
primary and secondary care. NICE Clinical Guideline 186. October 2014.
15 Vollmer TL, Ni W, Stanton S, Hadjimichael O. The NARCOMS patient registry: A resource for investigators.
Int J MS Care 1999; 1:12-15.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
20
Fall Risk Screening for Patients with MS
Measure Description
Percentage of patients with MS who were screened for fall risk in past 12 months.
Measure Components
Numerator
Statement
Patients with MS who were screened for fall risk in past 12 months.
Definitions:
*Fall Risk Screen is not further defined, and is at provider’s discretion to allow for
flexibility to meet practice needs. The screen may include use of a validated
instrument or patient interview.
Denominator
Statement
All patients with a diagnosis of MS.
Denominator
Exceptions
None
Supporting
Guideline &
Other
References
CMS has approved the following fall risk screening measures (See Measures
Harmonization below.):
Patients aged 65 years and older who were screened for future fall risk at
least once within 12 months. (ACO#13/NQF#0101)
Patients aged 65 years and older with a history of falls who had a risk
assessment for falls completed within 12 months. (PQRS #154)
Following evidence statements are quoted verbatim from the referenced clinical
guidelines:
“Ensure all people with MS have a comprehensive review of all aspects of
their care at least once a year.”1
“Ensure the comprehensive review is carried out by healthcare
professionals with expertise in MS and its complications. Involve
different healthcare professionals with expertise in specific areas of the
review if needed.”1
“Tailor the comprehensive review to the needs of the person with MS
assessing: MS symptoms: mobility and balance including falls.”1
Measure Importance
Relationship to
Desired
Outcome
Falls screening and subsequent management are essential to reduce the number of
future falls.
Opportunity for
Improvement
Patients with MS are at risk for falls. A recent systematic review found 30 to 63%
of patients with MS had fallen within the past year.2 Risk factors for falling include
worse disability course, progressive course, use of ambulation aids, and poorer
performance in balance tests. A recent study found 56% of patients with MS
recorded a fall in the past 3 months in their patient diary.3
Falls screening is underutilized. Matsuda 2011 reported that 58% of persons with
MS experienced a fall in the past 6 months.4 Among that group, only 51%
reported speaking to a healthcare provider about it.4 Determining whether patients
have fallen in the past year has been found to be a strong predictor of who would
fall again.5 In a comparison of fall history, questioning on fear of fall, EDSS,
Timed 25 foot walk, and computerized balance assessment, it was found that fall
history was the best predictor of future falls, and that this is the quickest and
easiest method for assessing fall risk.6
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
21
Gillespie performed a systematic review of randomized trials to reduce falls in the
general population.7 They identified 159 RCTs comprising 79,193 patients, and
determined that exercise programs and home safety interventions were effective in
reducing fall risk. 7 Multifactorial interventions that assess an individual’s risk of
falling then recommends specific treatment based on individualized risk also
reduces falling.7
The United States Preventive Services Task Force recommends exercise or
physical therapy to prevent falls in community-dwelling adults aged 65 years or
older who are at increased risk for falls. Michael, 2010.8 In its Physician Quality
Reporting System (PQRS) Measure # 155, CMS defines a fall plan of care to
include balance, strength, and gait training.9
National Quality
Strategy
Domains
☐ Patient and Family Engagement
☒ Patient Safety
☐Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☐ Clinical Process/Effectiveness
Exception
Justification
Not Applicable
Harmonization
with Existing
Measures
Existing measures (e.g., ACO Measure #13/NQF #0101, PQRS Measure #154)
focus on individuals aged 65 and older. All patients with MS should be screened
for fall risk, not just those aged 65 years and older, and as a result this measure was
developed to capture screening for this population.
Measure Designation
Measure
Purpose (Check
all that apply)
☒ Quality improvement
☒ Accountability
Type of
Measure (Check
all that apply)
☒Process
☐ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☒ Individual Provider
☒ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒Administrative Data/Claims
☐ Chart Review
☒ Registry
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
22
References
1 National Institute for Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis in
primary and secondary care. NICE Clinical Guideline 186. October 2014
2 Giannì C, Prosperini L, Jonsdottir J, Cattaneo D. A systematic review of factors associated with accidental falls
in people with multiple sclerosis: a meta-analytic approach. Clin Rehabil. 2014 Feb 25;28(7):704-716.
3 Nilsagård Y, Gunn H, Freeman J, et al. Falls in people with MS-an individual data meta-analysis from studies
from Australia, Sweden, United Kingdom and the United States. Mult Scler. 2014 Jun 16.;1-9.
4 Matusda, PN, Shumway-Cook A, Bamer AM, et al. Falls in multiple sclerosis. PM R 2011(7):624-632.
5 Ganz DA, Bao Y, Shekelle PG, et al. Will my patient fall? JAMA. 2007 Jan 3;297(1):77-86.
6 Cameron MH, Thielman E, Mazumder R, et al. Predicting falls in people with multiple sclerosis: fall history is
as accurate as more complex measures Mult Scler Int. 2013; 2013: Article ID 496325. 7p.
7 Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for
preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012 Sep
12;9:CD007146.
8 Michael YL, Whitlock EP, Lin JS, Fu R, O'Connor EA, Gold R; US Preventive Services Task Force. Primary
care-relevant interventions to prevent falling in older adults: a systematic evidence review for the U.S.
Preventive Services Task Force. Ann Intern Med. 2010 Dec 21;153(12):815-25.
9 Centers for Medicare & Medicaid Services. Physician Quality Reporting System Measure Codes found at:
http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/MeasuresCodes.html
Accessed on July 28, 2014.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
23
Bladder Infections for Patients with MS
Measure Description
Percentage of patients with MS who have had a bladder infection in past 12 months.
Note: Please see page 10 for further discussion of risk adjustment and stratification. Measure may be
used for accountability at the system or accountable care organization level if the MS populations being
compared are similar in demographics, socioeconomic status and the prevalence of comorbid
conditions.
Measure Components
Numerator
Statement
Patients with MS who have had a documented bladder infection in the past 12
months.
Denominator
Statement
All patients with a diagnosis of MS.
Denominator
Exceptions
Documentation of an indwelling catheter.
Documentation of diverting urostomy.
Supporting
Guideline &
Other
References
Following evidence statements are quoted verbatim from the referenced clinical
guidelines:
“Assess for infection and assist in management strategies to reduce risk of
infection, stone formation, or worsening of neurologic condition (Level
3).”1
“Ensure all people with MS have a comprehensive review of all aspects of
their care at least once a year.”1
“Tailor the comprehensive review to the needs of the person with MS
assessing: MS symptoms: … bladder, bowel and sexual function…”2
Measure Importance
Relationship to
Desired
Outcome
The desired outcome is to reduce the number of bladder infections. The measure
focuses attention on bladder infections and creates an incentive to take measures
needed to prevent them. This measure requires internal benchmarking for quality
improvement efforts, and it is anticipated in future measurement updates if the
measure is retained due to a continued gap in care that benchmarking data for
providers will be included. (e.g., bladder infection rates will be reduced by a
certain percentage rate over time.)
Opportunity for
Improvement
Bladder infections occur in up 20% of patients with MS3 and are commonly
present in patients with relapses.4 Recognition of neurogenic bladder and proper
management of bladder dysfunction can reduce the incidence of infection.
National Quality
Strategy
Domains
☐ Patient and Family Engagement
☒ Patient Safety
☐Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☐ Clinical Process/Effectiveness
Exception
Justification
Patients with indwelling catheters are likely to have chronic bacteriuria
due to bacterial colonization making implementation of the measure
difficult.
Most patients with urostomies do not have functioning bladders
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
24
Harmonization
with Existing
Measures
There are currently not comparable measures in national measurement programs or
endorsed by the National Quality Forum.
Measure Designation
Measure
Purpose (Check
all that apply)
☒ Quality improvement
☒ Accountability
Type of
Measure (Check
all that apply)
☐Process
☒ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☒ Individual Provider
☒ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒Administrative Data/Claims
☐ Chart Review
☒ Registry
References
1 American Association of Neuroscience Nurses (AANN), Association of Rehabilitation Nurses (ARN),
International Organization of Multiple Sclerosis Nurses (IOMSN). Nursing management of the patient with
multiple sclerosis. Glenview (IL): American Association of Neuroscience Nurses (AANN); 2011. 49 p.
2 National Institute for Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis in
primary and secondary care. NICE Clinical Guideline 186. October 2014.
3 Manach A, Motsko SP, Haag-Molkenteller C, et al. Epidemiology and healthcare utilization of neurogenic
bladder patients in US claims database. Neurourol Urodyn 2011; 30: 395-401.
4 Mahadeva A, Tarosescu R, Gran B. Urinary tract infections in multiple sclerosis: underdiagnosed and
undertreated? Am J Clin Exp Immunol 2014; 3: 57-67.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
25
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
26
Exercise and Appropriate Physical Activity Counseling for Patients with MS
Measure Description
Percentage of patients with MS who are counseled* on the benefits of exercise and appropriate
physical activity for patients with MS in the past 12 months.
Measure Components
Numerator
Statement
Patients with MS counseled* on the benefits of exercise and appropriate physical
activity for patients with MS in past 12 months.
*Counseled: to advise seriously and formally after consultation1
Denominator
Statement
All patients with a diagnosis of MS.
Denominator
Exceptions
None**
**All patients including those unable to exercise should be provided information
on appropriate range of motion and activity.
Supporting
Guideline &
Other References
The following evidence statements are quoted verbatim from the referenced
clinical guidelines:
“Evidence-based treatment interventions for mobility optimization
include exercise promotion (Level 1).”2
“Encourage participation in a regular pattern of exercise to improve mood
(Level 1).”2
“Encourage people with MS to exercise. Advise them that regular
exercise may have beneficial effects on their MS and does not have any
harmful effects on their MS.”3
“Ensure all people with MS have a comprehensive review of all aspects of
their care at least once a year.”3
“Tailor the comprehensive review to the needs of the person with MS
assessing: General health: …exercise…”3
Measure Importance
Relationship to
Desired
Outcome
Increased rates of physical activity and exercise improve the physical functioning
levels and quality of life for patients with MS.4
Opportunity for
Improvement
Despite known benefits of exercise and physical activity, persons with MS remain
inactive.5,6 The Work Group encourages referral to rehabilitation services,
including physical therapy, when clinically appropriate given the evidence
supporting improved outcomes for patients.7-9
National Quality
Strategy
Domains
☐ Patient and Family Engagement
☐ Patient Safety
☐Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☒ Clinical Process/Effectiveness
Exception
Justification
Not Applicable
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
27
Harmonization
with Existing
Measures
There are currently not comparable measures in national measurement
programs or endorsed by the National Quality Forum.
Measure Designation
Measure Purpose
(Check all that
apply)
☒ Quality improvement
☒ Accountability
Type of Measure
(Check all that
apply)
☒Process
☐ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☒ Individual Provider
☒ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒Administrative Data/Claims
☐ Chart Review
☒ Registry
References
1 Merriam Webster. Available at: http://www.merriam-webster.com/medical/counsel
2 American Association of Neuroscience Nurses (AANN), Association of Rehabilitation Nurses (ARN),
International Organization of Multiple Sclerosis Nurses (IOMSN). Nursing management of the patient with
multiple sclerosis. Glenview (IL): American Association of Neuroscience Nurses (AANN); 2011. 49 p.
3 National Institute for Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis in
primary and secondary care. NICE Clinical Guideline 186. October 2014.
4 American College of Sports Medicine: ACSM's Resource Manual for Guidelines for Exercise Testing and
Prescription, 6th edition edn. Baltimore, MD: Lippincott Williams & Wilkins; 2010.
5 Mayo NE, Bayley M, Duquette P, et. Al. The role of exercise in modifying outcomes for people with multiple
sclerosis: a randomized trial. BMC Neurology 2013;13:69.
6 Motl RW, McAuley E, Snook EM. Physical activity and multiple sclerosis: a meta-analysis. Mult Scler 2005;
11(4):459-463.
7 Khan F, Turner-Stokes L, Ng L, et al. Multidisciplinary rehabilitation for adults with multiple sclerosis.
Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No.: CD006036.
8 Rietberg MB, Brooks D, Uitdehaag BMJ, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane
Database of Systematic Reviews 2004, Issue 3. Art. No.: CD003980.
9 Döring A, Caspar FP, Friedemann P, et al. Exercise in multiple sclerosis – an integral component of disease
management. The EPMA Journal 2012;3:2-13.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a

©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
28
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New
Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-
New or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
29
Fatigue Outcome for Patients with MS
Measure Description
Percentage of patients with MS whose most recent score indicates results are maintained or improved
on a validated fatigue rating instrument* for patients with MS in past 12 months.
Note: Please see page 10 for further discussion of risk adjustment and stratification. Measure may be
used for accountability at the system or accountable care organization level if the MS populations being
compared are similar in demographics, socioeconomic status and the prevalence of comorbid
conditions.
Measure Components
Numerator
Statement
Patients with MS whose most recent score indicates results are maintained or
improved on a validated fatigue rating instrument* for patients with MS in past 12
months.
*Validated fatigue rating instruments include the Fatigue Severity Scale (FSS),1-3
Fatigue Impact Scale,4 MS Specific Fatigue Severity Scale,5,6 Modified Fatigue
Impact Scale,7 or Unidimensional Fatigue Impact Scale8
Denominator
Statement
All patients with a diagnosis of MS.
Denominator
Exceptions
Patients unable or declines to complete a fatigue questionnaire (i.e.,
advanced stage dementia, profound psychosis, neurodevelopmental
disorder, brain injury encephalopathy, or hydrocephalus.)
Comorbid medical condition causing fatigue (i.e., Systemic inflammatory
condition, cardiac condition, renal failure, pulmonary condition, or sleep
apnea.)
Supporting
Guideline &
Other
References
The following evidence statements are quoted verbatim from the referenced
clinical guidelines:
“Assess and offer treatment to people with MS who have fatigue for
anxiety, depression, difficulty in sleeping, and any potential medical
problems such as anaemia or thyroid disease.”9
“Explain that MS-related fatigue may be precipitated by heat, overexertion
and stress or may be related to the time of day.”9
“Nurses should be aware of and assess for secondary causes of fatigue to
include depression, medication side effects, pain, and sleep disorders
(Level 2). Nurses should educate and counsel patients regarding energy
conservation strategies, including the role of body temperature control
(Level 2). The nurse should be aware of the optimal timing of medication
administration to enhance energy level and to avoid interrupting sleep
(Level 3).”10
Measure Importance
Relationship to
Desired
Outcome
The desired outcome is to reduce or eliminate fatigue in MS patients. The measure
will provide an incentive for providers to identify and manage fatigue in MS
patients.
Opportunity for
Improvement
Fatigue occurs in about 80% of patients with MS reducing physical activity and
level of daily functioning.8 It is anticipated that by addressing fatigue, quality of
life will improve as individuals have decreased fatigue and increased ability to
function at work and home.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
30
National Quality
Strategy
Domains
☐ Patient and Family Engagement
☐ Patient Safety
☐Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☒ Clinical Process/Effectiveness
Exception
Justification
Fatigue is a subjective symptom that requires patient cooperation to assess.
Diseases other than MS can cause fatigue so patients with other fatigue
causing diseases are excluded from the MS measure
Harmonization
with Existing
Measures
There are currently no other comparable fatigue measures in national measurement
programs or endorsed by the National Quality Forum.
Measure Designation
Measure
Purpose (Check
all that apply)
☒ Quality improvement
☒ Accountability
Type of
Measure (Check
all that apply)
☐Process
☒ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☐ Individual Provider
☐ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒Administrative Data/Claims
☐ Chart Review
☒ Registry
References
1 Krupp LB, LaRocca NG, Nuir-Nash J, et al. The Fatigue Severity Scale: Application to Patients with Multiple
Sclerosis and Systemic Lupus Erythematosus. Arch Neurol. 1989;46(10):1121-1123.
2 Christodoulou C, MacAllister WS, Krupp LB: Psychiatry for Neurologists: Fatigue 295-306 Philadelphia:
Elsevier Science; 2003.
3 Schwartz JE, Jandorf L, Krupp LB. The measurement of fatigue: A new instrument. Journal of Psychosomatic
Research 1993; 37(7):753-762.
4 Fisk JD, Ritvo PG, Ross L, et al. Measuring the functional impact of fatigue: initial validation of the Fatigue
Impact Scale. Clin Infect Dis 1994;18(1):S79-S83.
5 Kos D., Kerckhofs E., Nagels G, et al. Assessing fatigue in multiple sclerosis: Dutch modified fatigue impact
scale. Acta Neurologica Belgica 2003;103(4):185–191.
6 Kos D, Nagels G, D’Hooghe MB, et al. A rapid screening tool for fatigue impact in multiple sclerosis. BMC
Neurology 2006, 6:27
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
31
7 Fisk JD, Pontefract A, Ritvo PG, Archibald CJ, Murray TJ. The impact of fatigue on patients with multiple
sclerosis. Can J Neurol Sci 1994; 21: 9-14.
8 Meads DM, Doward LC, McKenna SP, et al. The development and validation of the Unidimensional Fatigue
Impact Scale (U-FIS). Multiple Sclerois 2009; 15(10):1228-1238.
9 National Institute for Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis in
primary and secondary care. NICE Clinical Guideline 186. October 2014.
10 American Association of Neuroscience Nurses (AANN), Association of Rehabilitation Nurses (ARN),
International Organization of Multiple Sclerosis Nurses (IOMSN). Nursing management of the patient with
multiple sclerosis. Glenview (IL): American Association of Neuroscience Nurses (AANN); 2011. 49 p.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)

©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
32
Cognitive Impairment Testing for Patients with MS
Measure Description
Percentage of patients 18 years and older with MS who were tested* for cognitive impairment in the
past 12 months.
Measure Components
Numerator
Statement
Patients with MS aged 18 years and older were tested* for cognitive impairment at
least once in past 12 months.
Definitions:
* Tested is defined as administering either:
Brief International Assessment of Cognition for MS (BICAMS),1
Symbol Digit Modalities Test (SDMT),2
MS Neuropsychological Screening Questionnaire (MSNQ) Informant,3
Verbal fluency (phonemic and semantic),4
Paced Auditory Serial Addition Test (PASAT),3
Rao Brief Repeatable Neuropsychological Battery (BRNB),3
Minimal Assessment of Cognitive Function in MS (MACFIMS),3 or
PROMIS.5
Referral for formal neuropsychological testing where clinically appropriate
would also satisfy measure.
Denominator
Statement
All patients aged 18 years or older with a diagnosis of MS.
Denominator
Exceptions
Patient declines or is not able to participate in a cognitive assessment,
including those at end of life, comatose, or delirious.
Patient currently receiving treatment to address cognitive impairment.
Supporting
Guideline &
Other
References
Following evidence statements are quoted verbatim from the referenced clinical
guidelines:
“Assess and offer treatment to people with MS and evidence of memory
and cognitive problems for anxiety, depression, difficulty in sleeping and
fatigue.”8
“Nurses should work with the patient, care partner, and other members of
the interdisciplinary team to develop an appropriate cognitive management
program and reevaluate on an ongoing basis (Level 3). The nurse should
screen for factors that could increase cognitive problems such as
medications, sleep disturbance, inadequately treated pain, and other
untreated symptoms (Level 2). Nurses need to recognize and acknowledge
the distressing nature of cognitive deficits (Level 3). Patients should be
provided with verbal and written instructions regarding the need to reduce
distractions and implement safety measures (Level 3).”9
“Ensure all people with MS have a comprehensive review of all aspects of
their care at least once a year.”8
“Tailor the comprehensive review to the needs of the person with MS
assessing: MS symptoms: …cognitive symptoms…”8
“Be aware that the symptoms of MS can include cognitive problems,
including memory problems that the person may not immediately
recognise or associate with their MS.”8
“Talk to people with MS and their family members or carers about the
possibility that the condition might lead to cognitive problems.”8
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
33
“Consider referring people with MS and persisting memory or cognitive
problems to both an occupational therapist and a neuropsychologist to
assess and manage these symptoms.”8
Measure Importance
Relationship to
Desired
Outcome
Cognitive functioning impacts life satisfaction and health-related quality of life. It
is anticipated that if assessed on an ongoing basis, cognitive deficits may be
identified and addressed in a timely manner. Once identified, such deficits could
be treated (or patients referred to appropriate resources) and thereby improve
individuals quality of life.
Opportunity for
Improvement
43-70% of people with MS have reported cognitive impairments.7 Clinicians
cannot detect cognitive impairment unless there is regular assessment.
National Quality
Strategy
Domains
☐ Patient and Family Engagement
☐ Patient Safety
☐Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☒ Clinical Process/Effectiveness
Exception
Justification
Patients need to be willing to complete the screening tool for the screening scores
to be valid.
Harmonization
with Existing
Measures
There are no currently endorsed cognitive impairment quality measures; current
endorsed quality measures focus on dementia assessment. A measure is needed to
address the opportunity for improvement specific to the cognitive impairments
faced by the MS population.
Measure Designation
Measure
Purpose (Check
all that apply)
☒ Quality improvement
☒ Accountability for Health System or Plans only
Type of
Measure (Check
all that apply)
☒Process
☐ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☒ Individual Provider
☒ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒Administrative Data/Claims
☐ Chart Review
☒ Registry
References
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
34
1 Benedict RHB, Amato MP, Boringa J, et al. Brief International Cognitive Assessment for MS (BICAMS):
international standards for validation. BMC Neurology 2012;12:55.
2 Smith A. The symbol-digit modalities test: a neuropsychologic test of learning and other cerebral disorders. J.
Helmuth (Ed.) Learning disorders, Special Child Publications, Seattle (1968), pp. 83-91.
3 Foley FW, Benedict RHB, Gromisch ES, et al. The Need for Screening, Assessment, and Treatment for
Cognitive Dysfunction in Multiple Sclerosis. Results of a Multidisciplinary CMSC Consensus Conference,
September 24, 2010. Int J MS Care 2012;14:58–64.
4 Connick P, Kolappan M, Bak TH, et al. Verbal fluency as a rapid screening test for cognitive impairment in
progressive multiple sclerosis. J Neurol Neurosurg Psychiatry 2012;83(3):346-347.
5 Becker H, Stuifbergen A, Lee H, et al. Reliability and Validity of PROMIS Cognitive Abilities and Cognitive
Concerns Scales Among People with Multiple Sclerosis. Int J MS Care. 2014;16(1):1-8.
6 Beatty WW and Goodkin DE. Screening for Cognitive Impairment in Multiple Sclerosis: An Evaluation of the
Mini-Mental State Examination. Arch Neurol. 1990;47(3):297-301.
7 Langdon DW, Amato MP, Boringa J, et al. Recommendations for a Brief International Cognitive Assessment
for Multiple Sclerosis (BICAMS). Multiple Sclerosis Journal 2012;0(0);1-8.
8 National Institute for Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis in
primary and secondary care. NICE Clinical Guideline 186. October 2014.
9 American Association of Neuroscience Nurses (AANN), Association of Rehabilitation Nurses (ARN),
International Organization of Multiple Sclerosis Nurses (IOMSN). Nursing management of the patient with
multiple sclerosis. Glenview (IL): American Association of Neuroscience Nurses (AANN); 2011. 49 p.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
35
Clinical Depression Screening for Patients with MS
Measure Description
Percentage of patients aged 12 years and older with MS who were screened for clinical depression
using an age appropriate standardized depression screening tool* at least once in past 12 months.
Measure Components
Numerator
Statement
Patients aged 12 years and older with MS who were screened for clinical
depression using an age appropriate standardized depression screening tool* at
least once in past 12 months.
*Depression screening tool: Clinicians should consider use of validated
instruments such as the:
Beck Depression Inventory (BDI) or BDI II,
Patient Health Questionnaire (PHQ-9), (PHQ-A), or (PHQ-2),
MS Depression Rating Scale,
Center for Epidemiological Studies-Depression Revised (CESD-R),
Hospital Anxiety and Depression Scale (HADS),
General Health Questionnaire (GHQ),
2 Question Screen,
Neuro QOL Depression Bank. 1-6
Note: Currently no validated depression screening tools based on caregiver report
are known.
Denominator
Statement
All patients aged 12 years or older with a diagnosis of MS.
Denominator
Exceptions
Patients who are unable or decline to complete screening instrument.
Supporting
Guideline &
Other
References
Following evidence statements are quoted verbatim from the referenced clinical
guidelines:
“Clinicians may consider the Beck Depression Inventory and a 2-question
tool to screen for depressive disorders and the General Health
Questionnaire to screen for broadly defined emotional disturbances (Level
C).”1
“Evidence is insufficient to support/refute the use of other screening tools,
the possibility that somatic/neurovegetative symptoms affect these tools’
accuracy, or the use of diagnostic instruments or clinical evaluation
procedures for identifying psychiatric disorders in MS (Level U).”1
“Ensure all people with MS have a comprehensive review of all aspects of
their care at least once a year.”2
“Tailor the comprehensive review to the needs of the person with MS
assessing: MS symptoms:: …depression and anxiety…”2
“Mood Dysregulation: Nurses should work with the patient, care partner,
and other members of the interdisciplinary team to manage depression
appropriately (Level 2). Other roles are to assist patients and care partners
to adjust to changes involved in living with MS (Level 2); identify the
physical, emotional, spiritual, and educational needs of the patient and
family (Level 2); reinforce the importance of medication regimen and be
aware of medication side effects (Level 2); be alert to cues related to mood
changes and treatment outcomes (Level 2); and encourage participation in
a regular pattern of exercise to improve mood (Level 1).”3
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
36
Measure Importance
Relationship to
Desired Outcome
Screening is the first step to improved recognition and treatment of depression in
MS patients, and to decrease rates of affective symptoms in the MS patient
population.
Opportunity for
Improvement
MS is frequently associated with depression, and is currently under diagnosed
and treated.4,7 Evidence of under diagnosis of depression in MS patients makes
screening vital to identifying those in need of treatment.
National Quality
Strategy Domains
☐ Patient and Family Engagement
☐ Patient Safety
☒Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☐ Clinical Process/Effectiveness
Exception
Justification
Patients need to be willing to complete the screening tool for the screening
scores to be valid.
Harmonization
with Existing
Measures
Several NQF endorsed measures exist that address depression and treatment
adherence. These measures include Antidepressant Medication Management,
Child and Adolescent Major Depressive Disorders: Diagnostic Evaluation, Adult
Major Depressive Disorder: Suicide Risk Assessment, and Depression Response
at Twelve Months – Progress Towards Remission. It was determined a separate
measure assessing screening rates was required specific to the MS population
given the existing gap in care, as well as the need to use validated screening
tools specific to the MS population.
Measure Designation
Measure Purpose
(Check all that
apply)
☒ Quality improvement
☒ Accountability
Type of Measure
(Check all that
apply)
☒Process
☐ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☒ Individual Provider
☒ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒Administrative Data/Claims
☐ Chart Review
☒ Registry
References
1. Minden SL, Feinstein A, Kalb RC, et al. Evidence-based Guideline: Assessment and Management of
Psychiatric Disorders in Individuals with MS: Report of the Guideline Development Subcommittee of
the American Academy of Neurology. Neurology 2014; 82:1-8.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
37
2. National Institute for Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis
in primary and secondary care. NICE Clinical Guideline 186. October 2014.
3. American Association of Neuroscience Nurses (AANN), Association of Rehabilitation Nurses (ARN),
International Organization of Multiple Sclerosis Nurses (IOMSN). Nursing management of the patient
with multiple sclerosis. Glenview (IL): American Association of Neuroscience Nurses (AANN); 2011.
49 p.
4. Fargoso YD, Adoni T, Anacleto, et al. Recommendations on diagnosis and treatment of depression in
patients with multiple sclerosis. Pract Neurol 2014; 0:1-6.
5. Verdier-Taillerfer MH, Gourlet V, Fuhrer R, et al. Psyhometric properties of the Center for
Epidemiologic Studies- Depression scale in multiple sclerosis. Neuroepidemiology 2001; 20(4):262-267.
6. Gershon RC, Lai JS, Bode R, et al. Neuro-QOL: quality of life item banks for adults with neurological
disorders: item development and calibrations based upon clinical and general population testing. Qual
Life Res. 2012; 21(3):475-486.
7. Till C, Udler E, Ghassemi R, et al. Factors associated with emotional and behavioral outcomes in
adolescents with multiple sclerosis. Mult Scler 2012;18(8):1170-80.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
38
Depression Outcome for Patients with MS
Measure Description
Percentage of patients aged 12 years and older with MS whose most recent score indicates results are
maintained or improved on a validated depression screening instrument* for patients with MS in past
12 months.
Note: Please see page 10 for further discussion of risk adjustment and stratification. Measure may be
used for accountability at the system or accountable care organization level if the MS populations being
compared are similar in demographics, socioeconomic status and the prevalence of comorbid
conditions.
Measure Components
Numerator
Statement
Patients aged 12 years and older with MS whose most recent score indicates results
are maintained or improved on a validated depression screening instrument* for
patients with MS in past 12 months.
*Depression screening tool: Clinicians should consider use of validated
instruments such as the:
Beck Depression Inventory (BDI) or BDI II,
Patient Health Questionnaire (PHQ-9), (PHQ-A), or (PHQ-2),
MS Depression Rating Scale,
Center for Epidemiological Studies-Depression Revised (CESD-R),
Hospital Anxiety and Depression Scale (HADS),
General Health Questionnaire (GHQ),
2 Question Screen,
Neuro QOL Depression Bank. 1-6
Denominator
Statement
All patients aged 12 years or older with a diagnosis of MS.
Denominator
Exceptions
Patients who are unable or decline to complete screening instrument.
Supporting
Guideline &
Other
References
Following evidence statements are quoted verbatim from the referenced clinical
guidelines:
“Clinicians may consider the Beck Depression Inventory and a 2-question
tool to screen for depressive disorders and the General Health
Questionnaire to screen for broadly defined emotional disturbances (Level
C).”1
“Evidence is insufficient to support/refute the use of other screening tools,
the possibility that somatic/neurovegetative symptoms affect these tools’
accuracy, or the use of diagnostic instruments or clinical evaluation
procedures for identifying psychiatric disorders in MS (Level U).”1
“For individuals with MS, a 16-week program of individual T-CBT is
possibly effective and may be considered in treating depressive symptoms
(Level C).”1
“Mood Dysregulation: Nurses should work with the patient, care partner,
and other members of the interdisciplinary team to manage depression
appropriately (Level 2). Other roles are to assist patients and care partners
to adjust to changes involved in living with MS (Level 2); identify the
physical, emotional, spiritual, and educational needs of the patient and
family (Level 2); reinforce the importance of medication regimen andbe
aware of medication side effects (Level 2); be alert to cues related to mood
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
39
changes and treatment outcomes (Level 2); and encourage participation in
a regular pattern of exercise to improve mood (Level 1).”2
Measure Importance
Relationship to
Desired
Outcome
Reduction of depressive symptoms is the desired outcome for MS patients.
Opportunity for
Improvement
There is evidence of inadequate recognition and treatment of depression in MS
patients.3,4
National Quality
Strategy
Domains
☐ Patient and Family Engagement
☐ Patient Safety
☐Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☒ Clinical Process/Effectiveness
Exception
Justification
Patients need to be willing to complete the screening tool for the screening scores
to be valid.
Harmonization
with Existing
Measures
Several NQF endorsed measures exist that address depression and treatment
adherence. These measures include Antidepressant Medication Management,
Child and Adolescent Major Depressive Disorders: Diagnostic Evaluation, Adult
Major Depressive Disorder: Suicide Risk Assessment, and Depression Response at
Twelve Months – Progress Towards Remission. It was determined a separate
measure assessing screening rates was required specific to the MS population
given the existing gap in care. Efforts were made to harmonize this measure with
Depression Response at Twelve Months (MN Community Measurement); this
measure allows for clinicians to use multiple screening tools beyond the PHQ-9.
Measure Designation
Measure
Purpose (Check
all that apply)
☒ Quality improvement
☒ Accountability
Type of
Measure (Check
all that apply)
☐Process
☒ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☐ Individual Provider
☐ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒Administrative Data/Claims
☐ Chart Review
☒ Registry
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
40
References
1. Minden SL, Feinstein A, Kalb RC, et al. Evidence-based Guideline: Assessment and Management of
Psychiatric Disorders in Individuals with MS: Report of the Guideline Development Subcommittee of
the American Academy of Neurology. Neurology 2014; 82:1-8.
2. American Association of Neuroscience Nurses (AANN), Association of Rehabilitation Nurses (ARN),
International Organization of Multiple Sclerosis Nurses (IOMSN). Nursing management of the patient
with multiple sclerosis. Glenview (IL): American Association of Neuroscience Nurses (AANN); 2011.
49 p.
3. Fargoso YD, Adoni T, Anacleto, et al. Recommendations on diagnosis and treatment of depression in
patients with multiple sclerosis. Pract Neurol 2014; 0:1-6.
4. Till C, Udler E, Ghassemi R, et al. Factors associated with emotional and behavioral outcomes in
adolescents with multiple sclerosis. Mult Scler 2012;18(8):1170-80.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
41
Maintained or Improved Baseline Quality of Life for Patients with MS
Measure Description
Percentage of patients with MS whose most recent score indicates results are maintained or improved
on an age appropriate Quality of Life tool* in past 12 months.
Note: Please see page 10 for further discussion of risk adjustment and stratification. Measure may be
used for accountability at the system or accountable care organization level if the MS populations being
compared are similar in demographics, socioeconomic status and the prevalence of comorbid
conditions.
Measure Components
Numerator
Statement
Patients with MS whose most recent score indicates results are maintained or
improved on an age appropriate Quality of Life tool* in past 12 months.
*Suggested MS-specific QOL tools include the Multiple Sclerosis Impact Scale
(MSIS-29)1,2, Multiple Sclerosis Quality of Life (MS QOL-54)3, Patient-Reported
Outcome Indices for Multiple Sclerosis (PRIMUS)4,5, Multiple Sclerosis
International Quality of Life (MusiQOL)6, Functional Assessment of Multiple
Sclerosis (FAMS)7, and EuroQoL (EQ-5D)8. Alternatively, NeuroQOL or the NIH
Toolbox may be used.9,10
Denominator
Statement
All patients with a diagnosis of MS.
Denominator
Exceptions
Patients who are unable or decline to complete quality of life instrument.
Supporting
Guideline &
Other
References
Following evidence statements are quoted verbatim from the referenced clinical
guidelines:
“Use the local-language version of the multiple sclerosis international
quality of life (MusiQoL) questionnaire to assess patient QoL every12
months.”11
“Nurses should facilitate treatment and symptom management, promote
and enhance function, and support a quality of life (QOL) of adults with
MS and their family-care partners that is wellness focused (Level 3).”12
Measure Importance
Relationship to
Desired
Outcome
Improving QOL is a desired outcome for all patients with MS. MS can diminish
QOL given MS symptoms which impair a person’s ability to work and engage in
social activities.
Opportunity for
Improvement
QOL assessment is necessary as it can significantly impact adherence to
medications and affect physical rehabilitation.13 Despite the relationship between
QOL and treatment adherence, there remains a gap in treatment as clinicians fail to
address QOL.13 Measuring QOL and monitoring for maintenance or improvement
is expected to result in improved QOL assessment and prompt timely interventions
for patient identified concerns.
National Quality
Strategy
Domains
☒ Patient and Family Engagement
☐ Patient Safety
☐Care Coordination
☐ Population/Public Health
☐ Efficient Use of Healthcare Resources
☐ Clinical Process/Effectiveness
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
42
Exception
Justification
Patients need to be willing to complete the screening tool for the screening scores
to be valid.
Harmonization
with Existing
Measures
Existing endorsed measures assess quality of life as a process measure for a select
group of individuals and are not generalizable to the MS population. (e.g.,
receiving dialysis, (Assessment of Health-related Quality of Life
http://www.qualityforum.org/QPS/0260) family receiving hospice
(http://www.qualityforum.org/QPS/0208))
Measure Designation
Measure
Purpose (Check
all that apply)
☒ Quality improvement
☒ Accountability
Type of
Measure (Check
all that apply)
☐Process
☒ Outcome
☐ Structure
Level of
Measurement
(Check all that
apply)
☐ Individual Provider
☐ Practice
☒ System or Health Plan
Care Setting
(Check all that
apply)
☒ Outpatient
☐ Inpatient
☐ Emergency Departments and Urgent Care
Data Source
(Check all that
apply)
☒ Electronic health record (EHR) data
☒Administrative Data/Claims
☐ Chart Review
☒ Registry
References
1 Hobart J, Lamping D, Fitzpatrick R, et al. The Multiple Sclerosis Impact Scale (MSIS-29) A new patient-based
outcome measure. Brain 2001;124(5):962-973.
2 Multiple Sclerosis Impact Scale (MSIS-29) Available online at:
http://www.biomedcentral.com/content/supplementary/1471-2377-8-2-s1.doc Accessed on July 28, 2014.
3 Vickery BG. Multiple Sclerosis Quality of Life (MSQOL)-54 Instrument. Available online at:
http://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/MSQOL54_995.pdf
Accessed on July 28, 2014.
4 Doward LC, McKenna SP, Meads DM, et al. The development of Patient Reported Outcome Indices for
Multiple Sclerosis (PRIMUS). Mult Scler 2009;15:1092–102.
5 McKenna SP, Doward LC, Twiss J, et al. International Development of the Patient-Reported Outcome Indices
for Multiple Sclerosis (PRIMUS). Value in Health 2010; 13(8):946-951.
6 Simeoni MC, Auquier P, Fernandez O, et al. Validation of the Multiple Sclerosis International Quality of Life
questionnaire. Multiple Sclerosis 2008;14(2):219-230.
7 Cella DF, Dineen K, Arnason B, et al. Validation of the functional assessment of multiple sclerosis quality of
life instrument. Neurology 1996;47(1):129-139.
8 Putzki N, Fischer J, Gottwald K., et al.Quality of Life in 1000 patients with early relapsing-remitting multiple
sclerosis. European Journal of Neurology 2009;16:713-720.
9 Gershon RC, Lai JS, Bode R, et al. Neuro-QOL: quality of life item banks for adults with neurological
disorders: item development and calibrations based upon clinical and general population testing. Qual Life
Res. 2012; 21(3):475-486.
10 Hodes RJ, Insel TR, Landis SC. On behalf of the NIH Blueprint for Neuroscience Research. The NIH Toolbox:
Setting a standard for biomedical research. Neurology 2013;80(S3):S1-S92. All NIH Toolbox-related materials
are ©2012 Northwestern University and the National Institutes of Health.
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
43
11 Al-Tahan ARM, Al-Jumah MA, Bohlega S, et al. The importance of quality-of-life assessment in the
management of patients with multiple sclerosis Recommendations from the Middle East MS Advisory Group.
Neurosciences 2011; 16(2):109-113.
12 American Association of Neuroscience Nurses (AANN), Association of Rehabilitation Nurses (ARN),
International Organization of Multiple Sclerosis Nurses (IOMSN). Nursing management of the patient with
multiple sclerosis. Glenview (IL): American Association of Neuroscience Nurses (AANN); 2011. 49 p.
13 Zwibel HL and Smrtka J. Improving Quality of Life in Multiple Sclerosis: An Unmet Need. Am J Manag Care.
2011;17:S139-S145.
Technical Specifications: Electronic Health Record (EHR) Data
The AAN is in the process of creating code value sets and the logic required for electronic capture of
the quality measures with EHRs. A listing of the quality data model elements, code value sets, and
measure logic (through the CMS Measure Authoring Tool) for each of the MS measures will be made
available at a later date.
Technical Specifications: Administrative Data (Claims)
Administrative claims data collection requires users to identify the eligible population (denominator)
and numerator using codes recorded on claims or billing forms (electronic or paper). Users report a
rate based on all patients in a given practice for whom data are available and who meet the eligible
population/ denominator criteria.
Denominator
(Eligible
Population)
ICD-9 Code
ICD-10 Code
340 Multiple Sclerosis
G35 Multiple Sclerosis
Disseminated multiple sclerosis
Generalized multiple sclerosis
Multiple sclerosis NOS
Multiple sclerosis of brain stem
Multiple sclerosis of cord
AND
CPT E/M Service Code:
99201, 99202, 99203, 99204, 99205 (Office or other outpatient visit-New Patient);
99211, 99212, 99213, 99214, 99215 (Office or other outpatient visit-Established
Patient);
99241, 99242, 99243, 99244, 99245 (Office or Other Outpatient Consultation-New
or Established Patient);
97001 (Physical therapy evaluation);
97002 ( Physical therapy re-evaluation);
97003 (Occupational therapy evaluation);
97004 (Occupational therapy re-evaluation)
©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
44
Contact Information
For more information about quality measures please contact:
American Academy of Neurology
201 Chicago Avenue
Minneapolis, MN 55415
Phone: (612) 928-6100
Fax: 612-454-2744
quality@aan.com
1
Kantarci O, and Wingerchuk D. Epidemiology and natural history of multiple sclerosis: new insights. Current
Opinion in Neurology 2006;19:248-254
2
Zwibel H and Smrtka J. Improving Quality of Life in MS: an Unmet Need. American Journal of Managed Care
2011;17:S139-145.
3
Multiple Sclerosis International Federation. Atlas of MS 2013. 2013 28p.
4
World Health Organization. Neurological disorders: a public health approach. 2007.
5
National Multiple Sclerosis Society. Challenges of epidemiological studies website.
6
Noonan CW, Williamson DM, Henry JP, Indian R, Lynch SG, Neuberger JS, et al. The prevalence of multiple
sclerosis in 3 US communities. Prev Chronic Dis 2010;7(1):A12. Available at:
http://www.cdc.gov/pcd/issues/2010/jan/08_0241.htm. Accessed March 11, 2014.
7
Compston A, Coles A. Multiple sclerosis. Lancet 2008; 372: 1502-1517.
8
Adelman G., Rane SG, Villa KF. The cost burden of multiple sclerosis in the United States: a systematic review of
the literature. Journal of Medical Economics 2013; 16(5):639-647.
9
Minden SL, Feinstein A, Kalb RC, et al. Evidence-based Guideline: Assessment and Management of Psychiatric
Disorders in Individuals with MS: Report of the Guideline Development Subcommittee of the American Academy
of Neurology. Neurology 2014; 82:1-8.
10
Marriott JJ, Miyasaki JM, Gronseth G, O'Connor PW, Therapeutics and Technology Assessment Subcommittee of
the American Academy of Neurology. Evidence report: the efficacy and safety of mitoxantrone (Novantrone) in the
treatment of multiple sclerosis: Report of the Therapeutics and Technology Assessment Subcommittee of the
American Academy of Neurology. Neurology. 2010;74(18):1463-1470.
11
Neutralizing antibodies to interferon beta: Assessment of their clinical and radiographic impact: An evidence
report. Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of
Neurology. Neurology. 2007;68:977-984.
12
Cortese I, Chaudhry V, So YT, Cantor F, Cornblath DR, Rae-Grant A. Evidence-based guideline update:
Plasmapheresis in neurologic disorders: report of the Therapeutics and Technology Assessment Subcommittee of the
American Academy of Neurology. Neurology. 2011;76(3):294-300.
13
Scott TF, Frohman EM, De Seze J, Gronseth GS, Weinshenker BG. Evidence-based guideline: clinical evaluation
and treatment of transverse myelitis: report of the Therapeutics and Technology Assessment Subcommittee of the
American Academy of Neurology. Neurology. 2011 Dec 13;77(24):2128-34.
14
Practice parameter: The usefulness of evoked potentials in identifying clinically silent lesions in patients with
suspected multiple sclerosis (an evidence-based review): Report of the Quality Standards Subcommittee of the
American Academy of Neurology. Neurology. 2000 54;1720-1725.
15
Yadav V, Bever CT, Bowen J, et al. Summary of evidence-based guideline: Complementary and alternative
medicine in multiple sclerosis. Report of the Guideline Development Subcommittee of the American Academy of
Neurology. Neurology 2014; 82(12):1083-1092.
16
National Institute for Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis in primary
and secondary care. NICE Clinical Guideline 186. October 2014.
17
American Association of Neuroscience Nurses (AANN), Association of Rehabilitation Nurses (ARN),
International Organization of Multiple Sclerosis Nurses (IOMSN). Nursing management of the patient with multiple
sclerosis. Glenview (IL): American Association of Neuroscience Nurses (AANN); 2011. 49 p.

©2014. American Academy of Neurology. All Rights Reserved.
CPT Copyright 2004-2013 American Medical Association.
45
18
Soelberg Sørensen P, Deisenhammer F, Duda P, et al. Use of anti-interferon beta antibody measurements in
multiple sclerosis. In: Gilhus NE, Barnes MP, Brainin M, editor(s). European handbook of neurological
management. 2nd ed. Vol. 1. Oxford (UK): Wiley-Blackwell; 2011. p. 64-74.
19
Sellebjerg F, Barnes D, Filippini G, et al. Acute relapses of multiple sclerosis. In: Gilhus NE, Barnes MP, Brainin
M, editor(s). European handbook of neurological management. 2nd ed. Vol. 1. Oxford (UK): Wiley-Blackwell;
2011. p. 410-419.
20
National Institute for Health and Clinical Excellence (NICE). Fingolimod for the treatment of highly active
relapsing-remitting multiple sclerosis. London (UK): National Institute for Health and Clinical Excellence (NICE);
2012 Apr. 55 p. (Technology appraisal guidance; no. 254).
21
Consortium of Multiple Sclerosis Centers. Consortium of MS Centers MRI Protocol for the Diagnosis and
Follow-up of MS 2009 Revised Guidelines.
22
Al-Tahan ARM, Al-Jumah MA, Bohlega S, et al. The importance of quality-of-life assessment in the
management of patients with multiple sclerosis Recommendations from the Middle East MS Advisory Group.
Neurosciences 2011; 16(2):109-113.
23
http://www.merriam-webster.com/medical/consult
24
http://www.merriam-webster.com/medical/counsel
25
http://www.merriam-webster.com/dictionary/educate
26
http://www.merriam-webster.com/medical/refer
27
http://www.merriam-webster.com/medical/screen
28
Cheng EM, Crandall CJ, Bever CT, et al. Quality indicators for multiple sclerosis. Multiple Sclerosis
2010:16(8):970-980.