1600 Chap1600
User Manual: 1600
Open the PDF directly: View PDF ![]() .
.
Page Count: 149 [warning: Documents this large are best viewed by clicking the View PDF Link!]
- 1600 Table of Contents
- 1600, CHAPTER OVERVIEW
- 1610, COMPONENTS OF ALTCS CASE MANAGEMENT
- 1620, CASE MANAGER STANDARDS
- 1620-A INITIAL CONTACT/VISIT STANDARD
- 1620-B, NEEDS ASSESSMENT/CARE PLANNING STANDARD
- 620-C, COST EFFECTIVENESS STUDY STANDARD
- 1620-D , PLACEMENT/SERVICE PLANNING
- 1620-E, SERVICE PLAN MONITORING AND REASSESSMENT STANDARD
- 1620-F, TRIBAL FEE-FOR-SERVICE STANDARDS
- 1620-G, BEHAVIORAL HEALTH STANDARD
- 1620-H, TRANSITIONAL PROGRAM STANDARD
- 1620-I, HIGH COST BEHAVIORAL HEALTH REINSURANCE STANDARD
- 1620-J, OUT-OF-STATE PLACEMENT STANDARD
- 1620-K, SKILLED NURSING NEED STANDARD
- 1620-L, CASE FILE DOCUMENTATION STANDARD
- 1620-M, CONTRACTOR CHANGE STANDARD
- 1620-N, SERVICE CLOSURE STANDARD
- 1620, ABUSE/NEGLECT REPORTING STANDARD
- EXHIBIT 1620-1 CASE MANAGEMENT (CM) TIMEFRAMES
- EXHIBIT 1620-2 ARIZONA LONG TERM CARE SYSTEM (ALTCS) MEMBER CHANGE REPORT HARD COPY EXAMPLE ONLY – CHANGES MUST BE REPORTED ELECTRONICALLY
- EXHIBIT 1620-3 UNIFORM ASSESSMENT TOOL AND GUIDELINES
- EXHIBIT 1620-4 ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
- EXHIBIT 1620-5 RESERVED
- EXHIBIT 1620-6 HIGH COST BEHAVIORAL HEALTH REINSURANCE FORM
- EXHIBIT 1620-7 FEE-FOR-SERVICE (FFS) OUT-OF-STATE NURSING FACILITY PLACEMENT REQUEST FORM
- EXHIBIT 1620-8 CONTRACTOR CHANGE REQUEST FORM
- EXHIBIT 1620-9 ARIZONA LONG TERM CARE SYSTEM (ALTCS) ENROLLMENT TRANSITION INFORMATION (ETI) FORM
- EXHIBIT 1620-10 RESERVED
- EXHIBIT 1620-11 SAMPLE CRITICAL SERVICE GAP REPORT FORM
- EXHIBIT 1620-12 SPOUSE ATTENDANT CARE ACKNOWLEDGEMENT OF UNDERSTANDING FORM
- EXHIBIT 1620-13 ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM ALTCS MEMBER SERVICE PLAN
- EXHIBIT 1620-14 AHCCCS/ARIZONA LONG TERM CARE SYSTEM (ALTCS) MEMBER CONTINGENCY/BACK-UP PLAN
- EXHIBIT 1620-15, ASSISTED LIVING FACILITY (ALF) RESIDENCY AGREEMENT
- EXHIBIT1620-16, ASSISTED LIVING FACILITY (ALF) FINANCIAL CHANGE AGREEMENT
- EXHIBIT 1620-17, HOME AND COMMUNITY BASED SERVICE (HCBS) MEMBER NEEDS ASSESSMENT
- AMPM 1630, ADMINISTRATIVE STANDARDS
- EXHIBIT 1630-1, ATTENDANT CARE GUIDELINES
- 1640, TARGETED CASE MANAGEMENT STANDARDS
CHAPTER 1600
CASE MANAGEMENT
1600 CHAPTER OVERVIEW ...........................................................................
1600-1
1610 COMPONENTS OF ALTCS CASE MANAGEMENT ...............................
1610-1
1620 CASE MANAGER STANDARDS ..............................................................
1620-1
1620-A INITIAL CONTACT/VISIT STANDARD ................................................
1620-1
1620-B NEEDS ASSESSMENT/CARE PLANNING STANDARD ..........................
1620-3
1620-C COST EFFECTIVENESS STUDY STANDARD ........................................
1620-7
1620-D PLACEMENT/SERVICE PLANNING STANDARD ..................................
1620-14
1620-E SERVICE PLAN MONITORING AND REASSESSMENT STANDARD .......
1620-26
1620-F TRIBAL FEE-FOR-SERVICE STANDARD ............................................
1620-33
1620-G BEHAVIORAL HEALTH STANDARD ...................................................
1620-34
1620-H TRANSITIONAL PROGRAM STANDARD .............................................
1620-37
1620-I HIGH COST BEHAVIORAL HEALTH REINSURANCE STANDARD .........
1620-39
1620-J OUT-OF-STATE PLACEMENT STANDARD .........................................
1620-41
1620-K SKILLED NURSING NEED STANDARD ...............................................
1620-43
1620-L CASE FILE DOCUMENTATION STANDARD ........................................
1620-45
1620-M CONTRACTOR CHANGE STANDARD .................................................
1620-49
1620-N SERVICE CLOSURE STANDARD .........................................................
1620-53
1620-O ABUSE/NEGLECT REPORTING STANDARD ........................................
1620-56
EXHIBIT 1620-1 CASE MANAGEMENT (CM) TIMEFRAMES
EXHIBIT 1620-2 ALTCS MEMBER CHANGE REPORT
EXHIBIT 1620-3 UNIFORM ASSESSMENT TOOL AND GUIDELINES
EXHIBIT 1620-4 ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
EXHIBIT 1620-5 RESERVED
EXHIBIT 1620-6 HIGH COST BEHAVIORAL HEALTH REINSURANCE FORM
EXHIBIT 1620-7 FEE-FOR-SERVICE (FFS) OUT-OF-STATE NURSING
FACILITY PLACEMENT REQUEST FORM
EXHIBIT 1620-8 CONTRACTOR CHANGE REQUEST FORM

CHAPTER 1600
CASE MANAGEMENT
1620 CASE MANAGER STANDARDS (CONTINUED)……..………………………….
EXHIBIT 1620-9 ALTCS ENROLLMENT TRANSITION INFORMATION (ETI) FORM
EXHIBIT1620-10 RESERVED
EXHIBIT 1620-11 SAMPLE CRITICAL SERVICE GAP REPORT FORM
EXHIBIT 1620-12 SPOUSE ATTENDANT CARE ACKNOWLEDGEMENT OF
UNDERSTANDING FORM
EXHIBIT 1620-13 ALTCS MEMBER SERVICE PLAN
EXHIBIT 1620-14 AHCCCS/ALTCS MEMBER CONTINGENCY/BACK-UP PLAN
EXHIBIT 1620-15 ASSISTED LIVING FACILITY (ALF) RESIDENCY AGREEMENT
EXHIBIT 1620-16 ASSISTED LIVING FACILITY (ALF) FINANCIAL CHANGE
AGREEMENT
EXHIBIT 1620-17 HOME AND COMMUNITY BASED SERVICE (HCBS) MEMBER
NEEDS ASSESSMENT
1630 ADMINISTRATIVE STANDARDS .............................................................
1630-1
A. CASE MANAGER QUALIFICATIONS .....................................................................
1630-1
B. CASE MANAGEMENT PROCEDURES/TECHNICAL ................................................
1630-1
C. TRAINING ...........................................................................................................
1630-1
D. CASELOAD MANAGEMENT .................................................................................
1630-4
E. ACCESSIBILITY...................................................................................................
1630-5
F. TIME MANAGEMENT ..........................................................................................
1630-6
G. CONFLICT OF INTEREST ......................................................................................
1630-6
H. SUPERVISION .....................................................................................................
1630-6
I. INTER-DEPARTMENTAL COOPERATION ..............................................................
1630-7
J. REPORTING REQUIREMENTS ..............................................................................
1630-7
EXHIBIT 1630-1 ATTENDANT CARE GUIDELINES
1640 TARGETED CASE MANAGEMENT STANDARDS ....................................
1640-1
CHAPTER 1600
CASE MANAGEMENT
POLICY 1600
CHAPTER OVERVIEW
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1600-1
AHCCCS MEDICAL POLICY MANUAL
1600 CHAPTER OVERVIEW
REVISION DATES: 01/01/16, 05/01/12, 04/01/11, 01/01/11, 10/01/04
INITIAL
EFFECTIVE DATE: 02/14/1996
Chapter 1600 provides process and administrative standards for Arizona Long Term Care
System (ALTCS) and targeted case management. These standards must be included in
policies and procedures developed by Contractors for case management of their enrolled
members. Standards set forth in this chapter may be exceeded in order to meet the needs
of enrolled members.
For the purpose of this chapter, the following definitions apply:
1. Contractor(s) – unless otherwise specified, means Contractors for ALTCS
managed care members, Tribal Contractors for ALTCS Fee-For-Service (FFS)
members and the Targeted Case Management Contractor for acute care
members with developmental disabilities.
a. Tribal case management for on-reservation FFS members may be
provided by the Tribal government through an Inter-Governmental
Agreement (IGA) with AHCCCS or, if there is no IGA between AHCCCS
and a Tribal government, case management is provided through a special
Tribal case management Contractor.
b. Contractors and the Targeted Case Management Contractor have formal
contracts with AHCCCS.
2. Managed Risk Agreement - A document that the case manager must develop
with the member which outlines risks to the member’s safety and well-being as
a result of choices or decisions made by the member. Alternatives offered to the
member and the member’s choices with regard to placement and services must
be documented. The managed risk agreement, signed by the member or
guardian must be kept in the member’s case file.
3. Member(s) – those individuals who are eligible for ALTCS or targeted case
management and are enrolled with a Contractor.
a. Eligible individuals who are Elderly and/or have a Physical Disability
(E/PD) and are enrolled with a Program Contractor.
b. Eligible individuals who have a developmental disability and are enrolled
with the Arizona Department of Economic Security/Division of
Developmental Disabilities (ADES/DDD).
CHAPTER 1600
CASE MANAGEMENT
POLICY 1600
CHAPTER OVERVIEW
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1600-2
AHCCCS MEDICAL POLICY MANUAL
c. Eligible E/PD individuals who are Native American and living on a
reservation (or lived on a reservation immediately prior to placement in an
institutional facility that is located off-reservation) and are enrolled in the
ALTCS FFS program and receive ALTCS services through a Tribal
Contractor.
d. Eligible individuals with developmental disability who qualify financially
for the Title XIX and Title XXI acute care programs, but do not meet the
functional requirements of the ALTCS program, may receive targeted case
management services through ADES/DDD. These members receive their
acute care services through an AHCCCS acute care Contractor.
(i) Service Plan – for ALTCS, a uniform system of tracking member
services, date ranges and units of services authorized by the ALTCS
Contractor. It does not specifically refer to the CA165 screen in the
Client Assessment and Tracking System (CATS), except for ALTCS
Tribal Contractors
Information regarding other ALTCS topics, such as acute care services, provider
qualifications and FFS quality and utilization management is also included in this
manual. Refer to the Manual Table of Contents for guidance.
Refer to the AHCCCS FFS Provider Manual and the Encounter Reporting User Manual
for complete information regarding claims and encounter reporting procedures for
covered services, the provider registration process, and rate determination methodologies
used for ALTCS services, required financial reporting for nursing facilities and general
billing information. Both of these manuals are available from the AHCCCS Web site at
www.azahcccs.govH.
Refer to the Eligibility Manual, available from the AHCCCS web site at
www.azahcccs.gov for information on the financial and medical eligibility determination
processes for ALTCS members.
Forms requiring a member’s signature are available in Spanish. Refer to Appendix K,
Select ALTCS Case Management Forms in Spanish, for these forms.
CHAPTER 1600
CASE MANAGEMENT
POLICY 1610
COMPONENTS OF ALTCS CASE MANAGEMENT
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1610-1
AHCCCS MEDICAL POLICY MANUAL
1610 COMPONENTS OF ALTCS CASE MANAGEMENT
REVISION DATES: 01/01/16, 05/01/12, 05/01/10, 02/01/05, 10/01/04
REVIEW DATES: 10/01/13, 01/01/11
INITIAL
EFFECTIVE DATE: 02/14/1996
Description
Case management is the process through which appropriate and cost effective medical,
medically related social and behavioral health supports and services are identified,
planned, obtained and monitored for individuals eligible for Arizona Long Term Care
System (ALTCS) services. Each individual enrolled as an ALTCS member must receive
case management services as specified in the chapter and provided by a qualified case
manager.
The process involves a review of the ALTCS member’s strengths and needs by the
member, his/her family or representative and the case manager. The review should result
in a mutually agreed upon, appropriate and cost effective service plan that meets the
medical, functional, social and behavioral health needs of the member in the most
integrated and least restrictive setting. The case manager must foster a person-centered
approach and maximize member/family self-determination while promoting the values of
dignity, independence, individuality, privacy and choice. Case management begins with a
respect for the member’s preferences, interests, needs, culture, language and belief
system.
Amount, Duration and Scope
ALTCS case management components include the following:
1. Service planning and coordination to identify services that will effectively meet
the member’s needs in the most cost effective manner and to develop and
maintain the member’s service plan. Development of the service plan must be
coordinated with the member and/or member’s family/representative to ensure
mutually agreed upon approaches to meet the member’s needs within the scope
and limitations of the program, including cost effectiveness. Service planning
and coordination also includes ensuring members/representatives know how to
report the unavailability of or other problems with services and that these issues
will be addressed as quickly as possible when they are reported.
2. Brokering of services to obtain and integrate all ALTCS services to be provided
to the member, as well as other aspects of the member’s care, in accordance
with the service plan. If certain services are unavailable, the case manager may
CHAPTER 1600
CASE MANAGEMENT
POLICY 1610
COMPONENTS OF ALTCS CASE MANAGEMENT
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1610-2
AHCCCS MEDICAL POLICY MANUAL
substitute combinations of other services, within cost effectiveness standards, in
order to meet the member’s needs until the case manager is able to obtain such
services for the member. The case manager must also consider and integrate
non-ALTCS covered community resources/services as appropriate based on the
member’s needs.
3. Facilitation/Advocacy to resolve issues which impede the member’s progress
and access to needed services (both ALTCS and non-ALTCS covered services)
and to ensure that services are provided that are beneficial for the member. The
case manager will assist the member in maintaining or progressing toward
his/her highest functional level through the coordination of all services.
4. Monitoring and reassessment of services provided to ALTCS members and
modifying/reviewing member service plans and goals as necessary based on
changes in the member’s condition.
5. Gatekeeping to assess and determine the need for, and cost effectiveness of,
ALTCS services for assigned members. This includes assessing the member’s
placement and the services being received and taking necessary action to ensure
that services and placement are appropriate to meet the member’s needs.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-1
AHCCCS MEDICAL POLICY MANUAL
1620 CASE MANAGER STANDARDS
1620-A INITIAL CONTACT/VISIT STANDARD
REVISION DATES: 01/01/16, 05/01/12, 01/01/11, 10/01/07, 09/01/05, 02/01/05, 10/01/04
REVIEW DATES: 10/01/13, 03/01/13
INITIAL
EFFECTIVE DATE: 02/14/1996
1. Within seven business days of a new member’s enrollment, the assigned case
manager, or designee, must initiate contact with the member or member
representative. If the member resides in a nursing facility or other residential
setting, the case manager, or designee, will contact the facility to inform the
facility of the member’s enrollment. Initial contact may be made via telephone,
a face-to-face visit or by letter, if the case manager is unable to contact the
member by other approaches.
An on-site visit to initiate service planning must be completed by the case
manager within 12 business days of the member’s enrollment. If information
obtained during the initial contact or from the Pre-Admission Screening Tool
completed by AHCCCS during the eligibility determination indicates the
member has more immediate needs for services, the on-site visit should be
completed as soon as possible.
The on-site visit must be conducted at the member’s place of residence in order
to develop the member’s service plan. Confirmation of the scheduled on-site
visit is recommended prior to the meeting.
The member must be present for, and be included in, the on-site visit. The
member representative must be contacted for care planning, including
establishing service needs and setting goals, if the member is unable to
participate due to cognitive impairment, the member is a minor child and/or the
member has a legal guardian.
Refer to Exhibit 1620-1 for a chart of Case Management Timeframes.
2. If the case manager is unable to locate/contact a member via telephone, visit
or letter, or through information from the member’s relatives, neighbors or
others, another letter requesting that the member contact the case manager
should be left at, or sent to, the member’s residence. If there is no contact
within 30 calendar days from the member’s date of enrollment, the case must
be referred to the member’s Arizona Long Term Care Services (ALTCS)
eligibility worker, via the electronic Member Change Report (MCR) process,

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-2
AHCCCS MEDICAL POLICY MANUAL
for potential loss of contact. A hard copy of the MCR may be found in Exhibit
1620-2.
Only when AHCCCS Division of Member Services staff are also unable to
contact the member or representative, will the process of disenrolling the
member be initiated.
3. All contact attempted and made with, or regarding, an ALTCS member must
be documented in the member’s case file.
The case manager is responsible for explaining the member’s rights and
responsibilities under the ALTCS program to the member or member
representative, including the procedures for filing a grievance and/or an appeal. A
copy of these rights and responsibilities must also be provided in writing
(generally via the Member Handbook). The member or member representative
must sign and date a statement indicating that they have received the member
rights and responsibilities in writing, that these rights and responsibilities have
been explained to them and that they clearly understand them.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-3
AHCCCS MEDICAL POLICY MANUAL
1620-B NEEDS ASSESSMENT/CARE PLANNING STANDARD
REVISION DATES: 01/01/16, 03/01/13, 05/01/12, 01/01/11, 05/07/10, 10/01/07, 10/01/06,
09/01/05,
02/01/05, 10/01/04
INITIAL
EFFECTIVE DATE: 02/14/1996
1. Case managers are expected to use a person-centered approach regarding the
member assessment and needs, taking into account not only Arizona Long Term
Care System (ALTCS) covered services, but also other needed community
resources as applicable. Case managers are expected to:
a. Respect the member and the member’s rights
b. Support the member to have a meaningful role in planning and directing
their own supports and services to the maximum extent possible.
c. Provide adequate information and teaching to support the member
representative to make informed decisions and choices.
d. Be available to answer questions and address issues raised by the member
or representative, including between regularly scheduled review visits.
e. Provide a continuum of service options that supports the expectations and
agreements established through the planning process
f. Educate the member/family on how to report unavailability or other
problems with service delivery to the Contractor in order that unmet
service needs can be addressed as quickly as possible. See also subsections
1620-D and 1620-E in this policy regarding specific requirements.
g. Facilitate access to non-ALTCS supports and services available
throughout the community
h. Advocate for the member and/or family/significant others as the need
occurs
i. Allow the member/family to identify their role in interacting with the
system, including the extent to which the family/informal support system
will provide uncompensated care
j. Provide members with flexible and creative service delivery options
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-4
AHCCCS MEDICAL POLICY MANUAL
k. Educate members about member directed options for delivery of
designated services (see Chapter 1300 of this manual for more details).
Review these options, at least annually, with members living in their own
homes.
l. Educate members on their option to choose their spouse as their paid
attendant caregiver and the need to consider how that choice may impact
eligibility for other publicly funded programs.
m. Provide necessary information to providers about any changes in
member’s goals, functioning and/or eligibility to assist the provider in
planning, delivering and monitoring services,
n. Provide coordination across all facets of the service system in order to
determine the efficient use of resources and minimize any negative impact
on the member,
o. Assist members to identify their independent living goals and provide
them with information about local resources that may help them transition
to greater self-sufficiency in the areas of housing, education and
employment, and
p. Refer member cases, via electronic Member Change Report (MCR), to the
AHCCCS Division of Member Services for a medical eligibility re-
assessment if a member is assessed to no longer require an institutional
level of care. See the AHCCCS ALTCS Member Change Report Guide
for MCR instructions.
2. The involvement of the member and member’s family in strengths/needs
identification as well as decision making is a basic tenet of ALTCS case
management practice. Anyone can be involved in the planning the meetings at
the member’s or member representative’s request. The member, family, and/or
significant others partner with the case manager in the development of the plan
and the case manager is generally the facilitator.
3. The case manager must complete a Uniform Assessment Tool (UAT) based on
information from the strengths/needs assessment to determine the member’s
current Level of Care. The UAT and guidelines for completion can be found in
Exhibit 1620-3.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-5
AHCCCS MEDICAL POLICY MANUAL
4. Care planning is based on:
a. Face-to-face discussion with the member and/or member representative
that includes a systematic approach to the assessment of the member’s
strengths and needs in at least the following areas:
i. Functional abilities
ii. Medical conditions
iii. Behavioral health
iv. Social/environmental/cultural factors, and
v. Existing support system.
The case manager shall use the HCBS Needs Tool (HNT) found in Exhibit
1620-17 to determine the amount of service hours a member needs when
Attendant Care, Personal Care, Homemaker, Habilitation and/or Respite
services will be authorized for the member.
b. Recommendations of the member’s Primary Care Provider (PCP)
c. Input from ALTCS service providers, as applicable, and
d. Preadmission Screening (PAS), as appropriate.
5. The case manager will assist the member to identify meaningful and
measureable goals for him/herself. Goals should be built on the member’s
strengths and include steps that the member will take to achieve the goal(s).
Goals are written to outline clear expectations about what is to be achieved
through the service delivery and care coordination processes.
6. Member goals must:
a. Be member specific
b. Be measurable
c. Specify a plan of action/interventions to be used to meet the goals
d. Include a timeframe for the attainment of the desired outcome, and
e. Be reviewed at each assessment visit and progress must be documented.
Progress means information regarding potential barriers, changes that need
to be made to the goal and/or plan of action, and, if the goal has been met
but will be continued, the reason(s) for this.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-6
AHCCCS MEDICAL POLICY MANUAL
7. For members who have been receiving Home and Community Based Services
(HCBS) during the Prior Period Coverage (PPC) timeframe (as defined in
Chapter 100 of this Manual), a retrospective assessment must occur to
determine whether those services were:
a. Medically necessary
b. Cost effective, and
c. Provided by a registered AHCCCS provider.
If all three of these criteria are met, the services are eligible for reimbursement
by the ALTCS Contractor, or, for Fee-For-Service (FFS) members, the
AHCCCS Administration, as specified in the separate care/service plan.
A separate care/service plan must be developed and documented to indicate
those services that will be retroactively approved based on this assessment. If
any of the services provided during the PPC are not approved by the ALTCS
Contractor or, for FFS members, the AHCCCS Administration, the member
must be provided written notice of this decision and given an opportunity to file
an appeal. Refer to Arizona Administrative Code 9 A.A.C., Chapter 34, for
more detailed information on this requirement.
Assisted Living Facilities are encouraged to bill/accept Medicaid payment for
services for members who are eligible in the PPC but they are not required by
regulations to do so. If the facility chooses to, or is required by contract to bill
the Contractor, they must accept the Medicaid payment as full payment and are
not permitted to bill the member or family for the difference between the
Medicaid and private pay rate. The facility must refund private payments made
by the member or family, less the amount of room and board assigned by the
Contractor, prior to billing the Contractor for Medicaid reimbursement.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-7
AHCCCS MEDICAL POLICY MANUAL
1620-C COST EFFECTIVENESS STUDY STANDARD
REVISION DATES: 01/01/16, 03/01/13, 05/01/12, 04/01/12, 07/01/11, 02/01/11, 01/01/11,
10/01/07, 10/01/06, 07/01/06, 01/01/06, 09/01/05, 02/01/05, 10/01/04
INITIAL
EFFECTIVE DATE: 02/14/1996
Services provided under Title XIX must be cost effective whether the placement is in an
institutional facility or a Home and Community Based (HCB) setting. Placement in a
HCB setting is considered appropriate if the cost of Home and Community Based
Services (HCBS) for a specific member does not exceed 100% of the net cost of
institutional care for that member, is the least restrictive setting and HCBS will meet the
member’s needs.
1. A Cost Effectiveness Study (CES) must be completed for all Arizona Long
Term Care System (ALTCS) members who are Elderly and/or Physical
Disabilities (E/PD) in a HCB setting and for those E/PD members currently
placed in an institutional setting who have discharge potential according to the
timeframes outlined in Exhibit 1620-1.
2. The Contractor’s Annual Case Management Plan must describe a process used
by the Contractor that evaluates the net cost of institutional care that meets the
requirements of this policy. This process must include:
a. Calculation on institutional costs stratified for levels of care and
specialized needs.
b. Annual re-assessment and adjustment of the institutional rates based upon
changes in costs associated with the assessed levels of care and specialized
needs.
c. Implementation of processes consistent with this policy, for determination
and evaluation of CES for each member and processes for resolution of
cases where the net HCBS cost exceeds the net cost of institutional care.
3. A CES must be completed for members with developmental under the following
circumstances:
a. Every three months for a member whose service costs exceed 80% of the
cost of the appropriate institutional setting for the member,

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-8
AHCCCS MEDICAL POLICY MANUAL
b. When the service costs of a member whose service costs previously
exceeded 80% of the cost of the appropriate institutional setting are
subsequently reduced to below 80%, and/or
c. When discharge is contemplated for any member residing in an
Intermediate Care Facility (ICF).
The net cost of institutional care for each member takes into consideration the
specific member’s assessed Level of Care, the institutional rate appropriate for
that Level of Care and the amount of the specific member’s “CES Share of
Cost.”
If the member has needs that would necessitate a specialized rate in an
institutional setting (for example, Alzheimer’s or behavioral unit, residential
treatment center, extensive respiratory care), this cost must be used in
calculating the cost effectiveness of HCBS.
The “CES Share of Cost” is the amount the Division of Member Services/
Arizona Long Term Care System (DMS/ALTCS) eligibility has determined,
based on the member’s income and expenses, that s/he would have to pay
monthly IF s/he was placed in a nursing home.
The net Medicaid cost of institutional care is calculated by subtracting the
monthly CES Share of Cost amount for the member from the monthly nursing
facility cost based on the specific member’s level of care or other needs. The
result is called the Net Institutional Cost.
If the member has been assessed by the DMS/ALTCS unit, to have an actual
Share of Cost that must be paid in HCBS, that amount is deducted from the total
monthly cost of the HCB services the member needs. The result is called the
“Net HCBS Cost.”
If the Net HCBS Cost is more than the Net Institutional Cost, then home care
services at that level are not “cost effective” and cannot be provided unless the
HCBS costs are expected to decrease to less than the cost of institutional care
within six months of the current CES date. At that time, the member must be
issued a Notice of Action (NOA) that explains any decision to not provide
services at the level requested/needed by the member/representative and given
an opportunity to file an appeal if s/he does not agree with the decision.
The portion of HCB services that are cost effective can be provided if the
member/representative still desires HCBS placement and is willing to accept
that level of services and to assume the potential risks of remaining at home
without all the care that has been assessed as needed. The case manager must
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-9
AHCCCS MEDICAL POLICY MANUAL
complete a managed risk agreement with the member/representative to
document this situation.
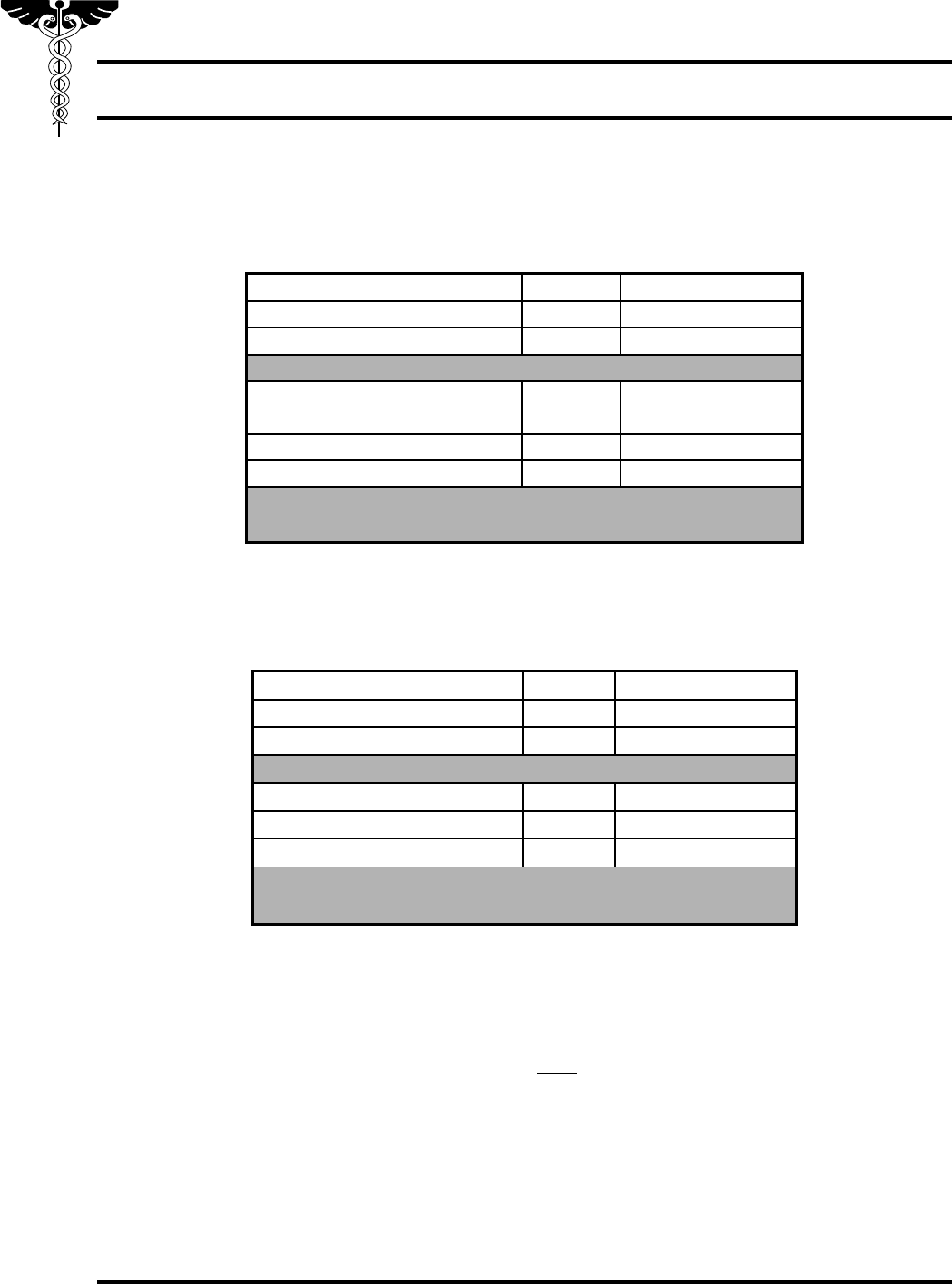
Example of CES>100%
Total Nursing Home Cost
$4920.10
CES Share of Cost
–
$ 726.90
Net Institutional Cost
=
$4193.20
SERVICES MEMBER NEEDS
40 hours of Attendant Care
per week
$2924.00
12 Nursing visits per month
+
$1341.60
Net HCBS Cost
=
$4265.60
$4265.60 DIVIDED BY $4193.20 = 102%
REQUESTED HCB SERVICES ARE NOT COST EFFECTIVE
If the member in the previous example requested all the services that could cost
effectively be provided, the case manager should determine which services are
priorities for the member and recalculate the CES. For example:
Total Nursing Home Cost
$4920.10
CES Share of Cost
–
$ 726.90
Net Institutional Cost
=
$4193.20
SERVICES THAT CAN COST EFFECTIVELY BE PROVIDED
40 hours of Attendant Care
$2924.00
11 Nursing visits per month
+
$1144.00
Net Home Services Cost
=
$4068.00
$4068.00 DIVIDED BY $4193.20 = $4193.20 = 97%
REQUESTED HCB SERVICES ARE COST EFFECTIVE
Existing HCBS units cannot be reduced if there is an increased cost of services
incurred to fill a service gap (for example, if personal care and homemaker services
are provided to substitute for a gap in attendant care services).
4. When the cost of HCBS exceeds 80% of the cost of institutional care:
a. Contractor case managers must provide written justification of services to
their administration for approval.
b. Tribal Contractor case managers must provide written justification of
services to the AHCCCS Division of Fee-for-Service Management
(DFSM) as a request for approval.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-10
AHCCCS MEDICAL POLICY MANUAL
5. When the cost of HCBS exceeds 100% of the cost of institutional care, but the
cost is expected to drop below 100% within the next six months because of an
anticipated change in the member’s needs:
a. A Contractor’s administration may approve the HCBS costs. Justification
and the approval must be documented in the case file.
b. Tribal Contractor case managers must provide written justification of
services to the DFSM Unit as a request for approval.
6. If the cost of HCBS is expected to exceed 100% of net institutional cost for
more than six months the case manager must advise the member of the cost
effectiveness limitations of the program and discuss other options. The case
manager must either reduce or not initiate any Title XIX service costs in excess
of 100%. Contractors may review individual cases with the appropriate
AHCCCS unit (DHCM or DFSM) before the decision to deny or reduce
services is made. A NOA must be issued to the member regarding any decision
to deny, reduce, limit or terminate requested services.
If the member chooses to remain in his/her own home even though the
Contractor cannot provide all of the services which have been assessed as
medically necessary (including those ordered by the member’s Primary Care
Provider [PCP]), a managed risk agreement/contract should be written. This
agreement should document the services the Contractor can cost effectively
provide, the placement/service options offered to the member, the member’s
choices with regard to those options, the risks associated with potential gaps in
service and any plans the member has to address those risks (for example,
volunteer services or paying privately for services). The member’s or member
representative’s signature on the agreement documents his/her
acknowledgement of the service limitations and risks.
The cost of HCBS services that will be retroactively approved during prior
period coverage enrollment cannot exceed 100% of the cost of
institutionalization for that member.
The CES must be updated when there is a change in placement to HCBS or
there is a change in services that would potentially place the member’s costs at
greater than 80% of institutional cost.
7. A CES may be completed indicating “NONE” for HCBS services needed under
the following circumstances:
a. Members residing in nursing facility who have no potential for HCBS
placement (Placement/Reason code: Q/05). Documentation in the

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-11
AHCCCS MEDICAL POLICY MANUAL
member’s case notes is required to justify the lack of discharge potential
and that the nursing facility is the most appropriate placement.
b. Members receiving only hospice services (Placement/Reason code: 10).
NOTE: Members receiving other Long Term Care (LTC) services in
combination with hospice must have a CES completed in
accordance with other CES policy explained in this section.
c. Members residing in a nursing facility because the cost of HCBS would
exceed 100% of institutional costs (Placement/Reason code: Q/01) or
d. Members with Acute Care Only status (Placement/Reason code: D/04,
D/11 or D/12).
8. CES data must be entered into the Client Assessment Tracking System (CATS)
system within ten business days of the date the action took place (for example,
initial on-site visit to determine service needs, placement changes or significant
increase in cost of services). Refer to the AHCCCS Contractors Operations
Manual (ACOM), Chapter 400, Policy 411, for information on the codes and
procedures for entering CES data into the CATS system (CA160 screen).
If the initial CES entered in the CATS system also reflects the assessment of the
cost effectiveness of HCBS services provided in the PPC, a comment to that
effect must be added to the case file, or system notes if comments are entered in
CATS. If the services entered on the initial CES do not reflect those provided
during the PPC, a separate hard copy CES must be completed to demonstrate
that PPC services were cost effective and this CES must be maintained in the
case file.
Refer to the AHCCCS Contractor Operations Manual, Chapter 400, Policy 411,
for information on the codes and procedures for entering CES data into the
CATS system (CA160 screen).
9. HCBS which must be included in the CES include:
a. Adult day health
b. Attendant care, including when provided through a member directed
option. See Chapter 1300 of this manual for information on member
directed options. If the member chooses to utilize his or her spouse as the
paid caregiver of these services, the spouse shall not be authorized for
more than 40 hours of services in a seven day period. Refer to Policy 1240
for more information on this limitation.
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-12
AHCCCS MEDICAL POLICY MANUAL
c. Habilitation, including when provided through a member directed option.
See Chapter 1300 of this manual for information on member directed
options.
d. Home health nurse
e. Home health aide
f. Home delivered meals
g. Homemaker, including when provided through a member directed option.
See Chapter 1300 of this manual for information on member directed
options.
h. Personal care, including when provided through a member directed option.
See Chapter 1300 of this manual for information on member directed
options.
i. Respite, if provided in a repeated pattern, such as weekly.
j. Regularly scheduled medically necessary transportation when the round
trip mileage exceeds 100 miles. These costs do not need to be included if
similar costs would be incurred while in a nursing facility. For example, if
dialysis transportation costs for an HCBS member would be essentially the
same as if the member were in an institutional setting; these costs would
not be included on the CES.
k. Emergency alert systems
l. Non-customized Durable Medical Equipment (DME) included in the
nursing facility per diem and having a value exceeding $300, regardless of
purchase or rental (for example, standard wheelchairs, walkers, hospital
beds). DME items covered under other insurance may be omitted from the
CES until the Contractor assumes responsibility for partial or full
payment.
m. Partial care (supervised, therapeutic and medical day programs)
n. Behavioral management (behavioral health personal assistance, family
support and peer support)
o. Psychosocial rehabilitation (living skills training, health promotion, pre-
job training, education and development, job coaching and employment
support)
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-13
AHCCCS MEDICAL POLICY MANUAL
p. Assisted living facilities, and
q. Behavioral health alternative residential settings.
10. Services which are not to be included in a CES include:
a. Hospice services
b. Customized DME items
c. Physical, speech, occupational and/or respiratory therapies
d. Medical supplies and pharmaceuticals
e. Behavioral health services which are not listed above, and
f. Home modification
g. Community Transition Services
h. Member and/or DCW Training, authorized as part of a member directed
service option.
If the member only receives ALTCS-covered HCBS that are provided by another funding
source (Medicare, Children’s Rehabilitative Services, tribal entities), s/he may still be in
an HCBS placement and therefore must have a CES completed. The CES should be
completed indicating the services received, but with no unit cost paid by the Contractor.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-14
AHCCCS MEDICAL POLICY MANUAL
1620-D PLACEMENT/SERVICE PLANNING STANDARD
REVISION DATES: 01/01/16, 03/01/13, 05/01/12, 02/01/11, 01/01/11, 05/07/10, 03/01/10,
02/01/09, 10/01/07, 05/01/06, 01/01/06, 09/01/05, 02/01/05, 10/01/04
INITIAL
EFFECTIVE DATE: 02/14/1996
The case manager is responsible for facilitating placement/services based primarily on
the member’s choice. Additional input in the decision-making may come from the
member’s guardian/family/significant other, the case manager’s assessment, the Pre-
Assessment Screening, the members Primary Care Provider (PCP) and/or other service
providers.
A guiding principle of the Arizona Long Term Care System (ALTCS) program is that
members are placed and/or maintained in the most integrated/least restrictive setting.
This needs to be the placement goal for ALTCS members as long as cost effectiveness
standards can be met in the Home and Community Based (HCB) setting.
1. After the needs assessment is completed, the case manager must discuss the cost
effectiveness and availability of needed services with the member and/or
member representative.
2. In determining the most appropriate service placement for the member, the case
manager and the member and/or the member representative should discuss the
following issues as applicable:
a. The member’s placement choice
b. Services necessary to meet the member’s needs in the most integrated
setting. See Chapter 1200H of this manual for information about the
following types of services available:
i. Home and Community Based Services (HCBS)
ii. Institutional services
iii. Acute care services, and
iv. Behavioral health services.
c. The member’s interest in and ability to direct their own supports and
services. If the member is unable to direct his/her own supports and
services, a legal guardian or Individual Representative may be appointed
who can choose to direct the member’s care. Member directed options for
service delivery of designated services are outlined in Chapter 1300 of this
manual.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-15
AHCCCS MEDICAL POLICY MANUAL
d. The availability of HCBS in the member’s community
e. Cost effectiveness of the member’s placement/service choice
f. Covered services which are associated with care in a nursing facility
compared to services provided in the member’s home or another HCB
setting as defined in Chapter 1200.
g. The risks that may be associated with representative member’s choices
and decisions regarding services, placements, caregivers, which would
require a managed risk agreement signed by the member/guardian to
document the situation
NOTE: Should a member or a member’s guardian refuse to sign the
managed risk agreement, the agreement should be place in the
case file with documentation of the refusal.
h. The member’s Share of Cost (SOC) responsibility. The SOC is the amount
of the member’s income that s/he must pay towards the cost of long term
care services. The amount of the member’s SOC is determined and
communicated to the member by the local ALTCS Eligibility office.
i. The member’s Room and Board (R & B) responsibility. Since AHCCCS
does not cover R & B in an HCB alternative residential setting, this
portion of the cost of the care in these settings must be paid by the
member or other source (such as the member’s family). The monthly R &
B amount is determined by and communicated to the member by the
ALTCS Contractor. See Assisted Living Facility Residency Agreement
and Assisted Living Facility Member Financial Change Agreement in
Exhibits 1620-15 and 1620-16. The Change Agreement should be used to
update the R&B amount whenever the member’s income or facility rate
changes.
3. Any member who lives in his/her own home must be allowed to remain in
his/her own home as long as HCBS are cost effective. Members cannot be
required to enter an alternative residential placement/setting that is “more” cost
effective. Refer to Chapter 100 of this Manual for a definition of “own home”.
4. Members must be informed that they have the choice to select their spouse to be
their paid caregiver for medically necessary and cost effective services
(provided the spouse meets all the qualifications as specified in the attendant
care section of Policy 1240 of this Manual) not to exceed 40 hours in a seven
day period. The case manager must inform and be available to discuss with
member and spouse the financial impact that this choice could have on the

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-16
AHCCCS MEDICAL POLICY MANUAL
eligibility of their household for publicly funded programs, including AHCCCS.
The “Spouse Attendant Care Acknowledgement of Understanding” Form
(Exhibit 1620-12) must be signed by the member and spouse prior to the
authorization of the member’s spouse as the paid caregiver. The case manager
must be available to assist member/spouse with this decision but is not expected
to contact the applicable agencies for the member to determine the impact of the
change in the spouse’s income on eligibility for programs.
5. Upon the member’s or member representative’s agreement to the service plan,
the case manager is responsible for coordinating the services with appropriate
providers.
NOTE: A provider’s compliance with the U.S. Department of Labor, Fair
Labor Standards Act, has no bearing on a member’s assessed needs
and corresponding authorized services and service hours.
Placement within an appropriate setting and/or all services to meet the
member’s needs must be provided as soon as possible. A decision regarding the
provision of services requested must be made within 14 calendar days following
the receipt of the request/order (three business days if the member’s life, health
or ability to attain, maintain or regain maximum function would otherwise be
jeopardized). Refer to Title 42 of the Code of Federal Regulations (42 C.F.R.)
438.210 for more information.
Services determined to be medically necessary for a newly enrolled member
must be provided to the member within 30 calendar days of the member’s
enrollment. Services for an existing member must be provided within 14
calendar days following the determination that the services are medically
necessary and cost effective.
Contractors shall develop a standardized system for verifying and documenting
the delivery of services with the member or representative after authorization.
6. The case manager must ensure that the member or representative understands
that some long term care services (such as home health nurse, home health aide
or Durable Medical Equipment [DME]) must be prescribed by the PCP. A
decision about the medical necessity of these services cannot be made until the
PCP writes an order for them. All orders for medical services must include the
frequency, duration and scope of the service(s) required, when applicable.
7. If an ALTCS member does not have a PCP or wishes to change PCP, it is the
case manager or designee’s responsibility to coordinate the effort to obtain a
PCP or to change the PCP.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-17
AHCCCS MEDICAL POLICY MANUAL
8. The case manager must also verify that the needed services are available in the
member’s community. If a service is not currently available, the case manager
must substitute a combination of other services in order to meet the member’s
needs until such time as the desired service becomes available (for example, a
combination of personal care or home health aide and homemaker services may
substitute for attendant care). A temporary alternative placement may be needed
if services cannot be provided to safely meet the member’s needs.
9. The case manager is responsible for developing a written service plan (Exhibit
1620-13) that reflects services that will be authorized. It must be noted for each
ALTCS covered service whether the frequency/quantity of the service has
changed since the previous service plan. Every effort must be made to ensure
the member or representative understands the service plan. The member or
representative must indicate whether they agree or disagree with each service
authorization and sign the service plan at initial development, when there are
changes in services and at the time of each service review. If the member is
physically unable to sign, the case manager must document how the member
communicated his/her agreement/disagreement. If the member is unable to
participate due to cognitive limitations and there is no representative, the case
manager must leave the service plan unsigned and document the circumstances.
The case manager must provide a copy of the service plan to the member or
representative and maintain a copy in the case file.
10. If the member disagrees with the assessment and/or authorization of placement/
services (including the amount and/or frequency of a service), the case manager
must provide the member with a NOA that explains the member’s right to file
an appeal regarding the placement or service plan determination. Refer to
Arizona Administrative Code, Title 9, Chapter 34 (9 A.A.C. 34) and the
AHCCCS Contractors Operations Manual (ACOM) Policy 414 for additional
information.
11. The AHCCCS/ALTCS Member Contingency/Back-Up Plan (found in Exhibit
1620-14) must also be completed for those members who will receive any of the
following critical services in their own home:
a. Attendant care, including spouse attendant care, Agency with Choice and
Self-Directed Attendant Care
b. Personal care, including Agency with Choice
c. Homemaker, including Agency with Choice and/or
d. In-home respite.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-18
AHCCCS MEDICAL POLICY MANUAL
The term “critical services” is inclusive of tasks such as bathing, toileting,
dressing, feeding, transferring to or from bed or wheelchair, and assistance with
similar daily activities.
A gap in critical services is defined as the difference between the number of
hours of direct care worker critical service scheduled in each member’s HCBS
care plan and the hours of the scheduled type of critical service that are actually
delivered to the member.
The following situations are not considered gaps:
a. The member is not available to receive the service when the caregiver
arrives at the member’s home at the scheduled time,
b. The member refuses the caregiver when s/he arrives at the member’s
home, unless the caregiver’s ability to accomplish the assigned duties is
significantly impaired by the caregiver’s condition or state (for example,
drug and/or alcohol intoxication),
c. The member refuses services,
d. The provider agency or case manager is able to find an alternative
caregiver for the scheduled service when the regular caregiver becomes
unavailable,
e. The member and regular caregiver agree in advance to reschedule all or
part of a scheduled service, and/or
f. The caregiver refuses to go or return to an unsafe or threatening
environment at the member’s residence.
The contingency plan must include information about actions that the
member and/or representative should take to report any gaps and what
resources are available to the member, including on-call back-up
caregivers and the member’s informal support system, to resolve
unforeseeable gaps (e.g., regular caregiver illness, resignation without
notice, transportation failure, etc.) within two hours. The informal
support system must not be considered the primary source of
assistance in the event of a gap, unless this is the member’s/family’s
choice. An out-of-home placement in a Nursing Facility (NF) or Assisted
Living Facility (ALF) should be the last resort in addressing gaps.
The contingency plan must include the telephone numbers for the toll-free
AHCCCS line and provider and/or contractor that will be responded to
promptly 24 hours per day, seven days per week. The member or member

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-19
AHCCCS MEDICAL POLICY MANUAL
representative must also be provided the Critical Service Gap Report Form
(Exhibit 1620-11), which can be mailed to the Contractor as an alternative
to calling in the service gap. The member or member representative should
be encouraged to call the toll-free AHCCCS line and provider and/or
Contractor rather than mailing the Critical Service Gap Report form so
that the service gap can be responded to more timely.
In those instances where an unforeseeable gap in critical services occurs, it
is the responsibility of the Contractor to ensure that critical services are
provided within two hours of the report of the gap. If the provider agency
or case manager is able to contact the member or representative before the
scheduled service to advise him/her that the regular caregiver will be
unavailable, the member or representative may choose to receive the
service from a back-up substitute caregiver, at an alternative time from the
regular caregiver or from an alternate caregiver from the member’s
informal support system. The member or representative has the final
say in how (informal versus paid caregiver) and when care to replace
a scheduled caregiver who is unavailable will be delivered.
The member or member representative must receive a response from the
provider acknowledging the gap which provides a detailed explanation as
to:
i. The reason for the gap, and
ii. The alternative plan to resolve the particular gap. .
iii. The alternative plan to resolve any possible future gaps.
12. The written contingency plan for members receiving those critical services
described above must include a Member Service Preference Level from one of
the four categories shown below:
a. Needs service within two hours
b. Needs service today
c. Needs service within 48 hours, or
d. Can wait until the next scheduled service date.
Member Service Preference Levels must be developed in cooperation with the
member and/or representative and are based on the most critical in-home service
that is authorized for the member. The Member Service Preference Level will
indicate how quickly the member chooses to have a service gap filled if the
scheduled caregiver of that critical service is not available. The member or
representative must be given the final say about how (informal versus paid

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-20
AHCCCS MEDICAL POLICY MANUAL
caregiver) and when care to replace a scheduled caregiver who is unavailable
will be delivered.
The case manager should assist the member or representative in determining the
member’s Service Preference Level by discussing the member’s caregiving
needs associated with his/her Activities of Daily Living (ADL) and Instrumental
Activities of Daily Living (IADL, such as housekeeping, meal preparation and
grocery shopping), abilities and cognitive, behavioral and medical status. The
case manager should ensure the member or representative has considered all
appropriate factors in deciding the member’s Service Preference Level. The
member/representative is not required to take into account the presence of an
informal support system when determining the Service Preference Level.
The case manager must document the Member Service Preference Level chosen
in the case file. This documentation must clearly indicate the member’s or
representative’s involvement in contingency planning.
A member or representative can change the Service Preference Level from a
previously determined Service Preference Level at the time of the service gap,
depending on the circumstances at the time. The provider agency or Contractor
must discuss the current circumstances with the member or representative at the
time the gap is reported to determine if there is a change in the Service
Preference Level. The plan to resolve the service gap must address the
member’s choice at the time the gap is reported.
The contingency plan must be discussed with the member/representative at least
quarterly. A copy of the contingency plan must be given to the member when
developed and at the time of each review visit. The member/representative may
change the member Service Preference Level and his/her choices for how
service gaps will be addressed at any time.
13. Members who reside in “own home” settings should be encouraged, and
assisted as indicated, by the case manager to have a disaster/emergency plan for
their household that considers the special needs of the member. Informational
materials are available at the Federal Emergency Management Agency’s
(FEMA) website at www.fema.gov or www.ready.gov.
14. Members who reside in out-of-home residential placements must be regularly
assessed to determine if they are in the most integrated setting possible for their
needs. Members should be allowed or encouraged to change to a less restrictive
placement, as long as needed services are available and cost effective in that
setting.
15. If the member will be admitted to a nursing facility, the case manager must
ensure and document that a Pre-Admission Screening and Resident Review
(PASRR) Level I screening and Level II evaluation, if indicated, have been

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-21
AHCCCS MEDICAL POLICY MANUAL
completed prior to admission. See Chapter 1200 of this manual for more
information.
16. If the member does not intend to pursue receiving HCBS or institutional
services, the member needs to be encouraged to withdraw from the ALTCS
program voluntarily and seek services through an AHCCCS acute care
Contractor or other programs.
If the member refuses long term care services that have been offered or refuses
to allow the case manager to conduct a review visit in accordance with the
required timeframes and locations, but does not wish to withdraw from the
ALTCS program, the case must be referred for an evaluation of Acute Care
Only eligibility via the electronic Member Change Report (MCR) process. The
member/representative must be advised that s/he could be disenrolled from the
ALTCS program depending on his/her income. The electronic MCR and
documentation that further describes the circumstances of the member’s refusal
to accept ALTCS services should be sent to the AHCCCS/Division of Health
Care Management (DHCM) Medical Management (MM) Unit.
Refer to Exhibit 1620-2 for a hard copy of the MCR form. Exhibit 1620-2 also
provides guidelines on circumstances for which an MCR is needed and Exhibit
1620-4 describes and gives examples of member situations for which an Acute
Care Only “D” placement is appropriate.
17. The service plan must include the date range and units for each service
authorized in the member’s case file according to the Contractor’s system for
tracking service authorizations. Tribal Contractor case manager must enter those
services authorized for the member on the CA165/Service Plan in the CATS
system.
18. Service plans for members residing in an Uinstitutional setting must include the
following types of services, as appropriate based on the member’s needs:
a. Nursing facility services. The service plan must indicate the Level of Care
(Level I, II, or III) based on the Uniform Assessment Tool or other
contractor method for determining specialty care (for example, behavior
management, wandering/ dementia or sub-acute).
b. Hospital admissions (acute and psychiatric)
c. Bed hold or therapeutic leave days (refer to Chapter 100 of this manual for
definitions and limitations)
d. Services in an uncertified nursing facility

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-22
AHCCCS MEDICAL POLICY MANUAL
e. DME outside the institutional facility per diem (item/items with a value
exceeding $300 regardless if rented, purchased or repaired). This
requirement is waived for ALTCS/DDD members.
f. Hospice services
g. Therapies (occupational, physical and speech)
h. Medically necessary non-emergency transportation (required for Tribal
Contractors only)
i. Behavioral health services (only those provided by behavioral health
independent billers – see definition in the Glossary of the Behavioral
Health Services Guide)
j. Title XIX covered services as noted above if provided by other funding
sources, for example, Medicare, Tribes, Children’s Rehabilitative
Services, other insurance sources.
20. Service plans for members residing in an UHCB setting must include the
following types of services, as appropriate, based on the member’s needs:
a. Adult day health or group respite
b. Hospital admissions (acute and psychiatric)
c. Attendant care – including when provided through a member directed
option. One or more service code modifiers must be used to distinguish
the type of Attendant Care when /if provided as follows:
i. by the member’s spouse (U3)
ii. by family living with the member (U5)
iii. by family not living with the member (U4)
iv. as Self Directed Attendant Care (U2)
v. as Agency with Choice (U7)
d. DME outside the institutional facility per diem (item/items with a value
exceeding $300 regardless if rented, purchased or repaired). This
requirement is waived for ALTCS/DDD members.
e. Emergency alert systems
f. Medical supplies that have a monthly cost in excess of $100.00 (required
for Tribal Contractors only)

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-23
AHCCCS MEDICAL POLICY MANUAL
g. Habilitation, including when provided through a member directed option.
The U7 service code modifier must be used to designate when the service
is provided as Agency with Choice
h. Home delivered meals
i. Home health aide
j. Community Transition Services that will be authorized in order to
transition the Nursing Facility (NF) member to HCBS “Own Home”.
Refer to Policy 1240 of this manual for definitions and limitations. This
service may be authorized while the member is still in an institutional
placement.
k. Homemaker, including when provided through a member directed option.
The U7 service code modifier must be used to designate when the service
is provided as Agency with Choice
l. Hospice
m. Personal care, including when provided through a member directed option.
The U7 service code modifier must be used to designate when the service
is provided as Agency with Choice
n. Respite care, including nursing facility respite
o. Therapies (occupational, physical, speech, and/or respiratory)
p. Behavioral health services (only those that are authorized with Healthcare
Common Practice Coding System [HCPCS] codes)
q. Medically necessary non-emergency transportation when the round trip
mileage exceeds 100 miles (required for Tribal Contractors only)
r. Home modifications
s. Assisted Living Facility services
t. Community Transition Services that have been authorized in order to
transition a NF member to HCBS “Own Home”. Refer to Policy 1240 of
this manual for definitions and limitations.
u. Member and/or DCW Training, authorized as part of a member directed
service option
v. Behavioral health alternative residential facility services, and
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-24
AHCCCS MEDICAL POLICY MANUAL
w. Title XIX covered services as noted above, if provided by other funding
sources, for example, Medicare, Tribes, Children’s Rehabilitative
Services, other insurance sources.
21. Service plans for members designated as “Acute Care Only (ACO)” must
include the following types of services, as appropriate, based on the member’s
needs:
a. DME (this requirement is waived for ALTCS DDD members).
b. Medically necessary non-emergency transportation when the round trip
mileage exceeds 100 miles (required for Tribal Contractors only)
c. Rehabilitative therapies (physical, occupational and speech), and
d. Behavioral health services.
Members who are enrolled as “ACO” due to financial reasons (such as a
transfer of resources) are eligible to receive all medically necessary behavioral
health services as listed in Chapter 300, Policy 310 of this manual, including
those typically considered as HCBS.
22. Refer to Chapter 1200 for descriptions of the amount, duration and scope of
ALTCS services and settings, including information about restrictions on the
combination of services.
23. The CA161/Placement Maintenance screen in the Client Assessment Tracking
System (CATS) system must be updated with the following information within
ten days of the initial visit:
a. ID number of case manager currently assigned to the case
b. Date of last case management review visit with the member
c. Placement code(s) and begin/end dates since enrollment
d. Residence code that corresponds with each Placement
e. Placement Reason code that corresponds with each Placement, and
f. Behavioral health code that reflects member’s current status
Refer to the AHCCCS Contractors Operations Manual (ACOM), Chapter 400,
Policy 411, for information on the codes and procedures for entering the above
data into the CATS system.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-25
AHCCCS MEDICAL POLICY MANUAL
24. The CA162/Community First Choice screen in the Client Assessment Tracking
System (CATS) must be entered with the following member information within
ten business days of the service visit and updated at least annually:
a. Agency With Choice indicator
b. Self-Directed Attendant Care indicator
c. Employment Status
d. Educational Level
e. Level of Care
f. Incontinence Status
g. Whether member receives any Antipsychotic Medications
h. Major Diagnosis (at least one but up to three diagnoses).
Refer to the AHCCCS Contractors Operation Manual (ACOM), Chapter 400,
Policy 411, for information on the codes and procedures for entering the above
data into the CATS system.
25. Contractors are not required to enter service authorizations on the
CA165/Service Plan in the CATS system. Tribal Contractors are required to
enter this information on the CA165/Service Plan within five business days of
the initiation of the service(s) authorized.
Refer to the AHCCCS Contractors Operations Manual, Chapter 400, Policy 411, for
information on the codes and procedures for entering service plan data into the CATS
system.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-26
AHCCCS MEDICAL POLICY MANUAL
1620-E SERVICE PLAN MONITORING AND REASSESSMENT STANDARD
REVISION DATES: 01/01/16, 03/01/13, 05/01/12, 01/01/11, 02/01/09, 10/01/07, 09/01/05,
02/01/05, 10/01/04
INITIAL
EFFECTIVE DATE: 02/14/1996
1. Case managers are responsible for ongoing monitoring of the services and
placement of each member assigned to their caseload in order to assess the
continued suitability and cost effectiveness of the services and placement in
meeting the member’s needs as well as the quality of the care delivered by the
member’s service providers.
2. Member placement and services must be reviewed , with the member present,
within the following timeframe:
a. At least every 180 days for a member in an institutional setting (this
includes members receiving hospice services and those in uncertified
institutional settings)
b. At least every 90 days for a member receiving Home and Community
Based Services (HCBS)
c. At least every 90 days for a community-based member receiving acute
care services only and living in an HCBS setting. Acute care service
monitoring for these members may be conducted on-site, via telephone or
by certified letter. However, an on-site visit with the member must be
completed at least once a year. Acute Care Only members residing in a
non-contracted or uncertified institutional setting must have an on-site
visit at least every 180 days, and
d. At least every 180 days for DDD members 12 years or older residing in a
group home, unless the member is medically involved or Seriously
Mentally Ill/Severely Emotionally Disturbed (SMI/SED). If medically
involved or SMI/SED, on-site visits must be made at least every 90 days.
Refer to Exhibit 1620-1 for a chart on Case Management Timeframes.
Contractors may develop standards for more frequent monitoring visits of
specific types of members/placements at their discretion but may not determine
members to need less frequent visits.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-27
AHCCCS MEDICAL POLICY MANUAL
Case managers must attend nursing facility care conferences on a periodic basis
to discuss the member’s needs and services jointly with the member, care
providers and the family. At a minimum, case managers must consult with
facility staff during 180-day visits to assess changes in member Level of Care.
3. Review visits are to be conducted where the member receives services,
including service settings both inside and outside of the member’s home as
described below. At a minimum, case managers must conduct review visits
with a member in his or her home at least once annually in order to evaluate the
living environment, identify potential barriers to quality care, and assess for
unmet needs. If a member receives services outside of the home, at a minimum,
a review visit must be conducted at one of the member’s service setting
locations. At the election of the member or member’s representative, remaining
visits may be conducted at an alternate location that is not a service setting. The
location of each review visit, whether at a service setting location or an alternate
site, must be determined by the member or member’s representative and not for
the convenience of the case manager or providers. The choice of location by the
member/representative must be documented in the case management file.
If a case manager is unable to conduct a review visit as specified above due to
the refusal by the member and/or the member’s representative to comply with
these provisions, services cannot be evaluated for medical necessity and
therefore, will not be authorized. A NOA must then be issued to the member
setting forth the reasons for the denial/discontinuance of services.
4. Members must be able to contact their case manager, or designee between the
regularly scheduled visits to ask questions, discuss changes/needs and/or to
request a meeting with the case manager. The case manager must respond
promptly to the questions and/or requests.
5. Case managers must be able to assess/identify a problem or situation as urgent
or as a potential emergency and take appropriate action. More frequent case
monitoring is required when the case manager is notified of an urgent/emergent
need or change of condition which will require revisions to the existing service
plan.
An emergency visit is required when the situation is urgent and cannot be
handled over the telephone or when the case manager has reason to believe that
the member’s well-being is endangered.
6. Case managers must conduct an on-site review within ten business days
following a member’s change of placement type (for example, from HCBS to an
institutional setting, own home to assisted living facility or institutional setting
to HCBS) or from the date the case manager is made aware of such a change.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-28
AHCCCS MEDICAL POLICY MANUAL
This review must be conducted to ensure that appropriate services are in place
and that the member agrees with the service plan as authorized.
Whenever possible, discharge to a member’s own home should be delayed until
adequate services can be arranged. In-home services must be initiated within ten
business days following a member’s discharge to HCBS.
7. If the case manager is unable to contact an enrolled member to schedule a visit,
a letter must be sent to the member or representative requesting contact by a
specific date (ten business days from the date of the letter is the suggested
timeframe). If no response is received by the designated date, the case manager
must send an electronic Member Change Report, indicating loss of contact, to
the local Arizona Long Term Care System (ALTCS) Eligibility office for
possible disenrollment from the ALTCS program.
NOTE – Disenrollment will not occur if the local office is able to make contact
with the member or representative and confirm that the member does
not wish to withdraw from the ALTCS program.
8. The case manager must meet with the member and/or representative, according
to the established standards, in order to:
a. Discuss the type, amount and providers of authorized services. If any
issues are reported or discovered, the case manager must take and
document action taken to resolve these as quickly as possible. The
Contractor administration must also be advised of member grievances and
provider issues for purposes of tracking/ trending.
b. Assess the member’s current functional, medical, behavioral and social
strengths and needs, including any changes to the member’s informal
support system. If the member is assessed to no longer need an
institutional level of care, the case manager must refer the case for a
medical eligibility Pre-Admission Screening (PAS) reassessment via the
electronic Member Change Report process.
The case manager shall use the HCBS Needs Tool (HNT) found in Exhibit
1620-17 to review the service hours a member needs when Attendant
Care, Personal Care, Homemaker, Habilitation and/or Respite services
will be authorized for the member. The HNT must also reflect care that is
provided and agreed to by the member’s informal support system. This
tool must be reviewed at each 90-day service review.
The Uniform Assessment Tool (UAT), used to determine the Level of
Care for EPD members, must be updated at least annually, more often as
indicated by a change in member condition. Depending on contractual

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-29
AHCCCS MEDICAL POLICY MANUAL
requirements, it may also be updated as requested for nursing facility
authorizations.
Case managers must review the UAT every 180 days for nursing facility
EPD members, comparing it with facility documentation such as the
Minimum Data Set (MDS) to determine changes in Level of Care.
Changes in Level of Care must be communicated to the nursing facility.
A copy of the UAT may be found in Exhibit 1620-3.
c. Assess the continued appropriateness of the member’s current placement
and services, including whether the member is residing in the setting of
his/her choice and whether there are any goals that need to be developed
and/or risks to manage related to the member’s service or placement
decisions.
d. Assess the cost effectiveness of services provided and/or requested
e. Discuss the member’s perception of his/her progress toward established
goals
f. Identify any barriers to the achievement of the member’s goals
g. Develop new goals as needed
h. Review service delivery options available to the member, including
member directed options, on at least an annual basis
i. Review and document, at least annually, the member’s continued choice
of his or her spouse as paid caregiver. Documentation shall include the
member’s signature on the “Spouse Attendant Care Acknowledgement of
Understanding Form” (Exhibit 1620-12) and,
j. Review, at least annually, the Contractor’s (or the Administration’s for
members enrolled with a Tribal Contractor) member handbook to ensure
members/ representatives are familiar with the contents, especially as
related to covered services and their rights/responsibilities.
8. The member representative must be involved for the above if the member is
unable to participate due to a cognitive impairment, if the member is a minor
child and/or if the member has a legal guardian.
If the member is not capable of making his/her own decisions, but does not have
a legal representative or member representative available, the case manager
must refer the case to the Public Fiduciary or other available resource. If a
guardian/fiduciary is not available, the reason must be documented in the file.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-30
AHCCCS MEDICAL POLICY MANUAL
9. Members who reside in an out-of-home residential setting must be regularly
assessed to determine if it is possible to safely meet the member’s needs in a
more integrated setting. Community Transition Services (CTS) may be used to
assist Nursing Facility (NF) members with discharge to an HCBS “Own Home”
setting (see Policy 1240 of this manual for definitions and limitations related to
CTS).
10. The case manager must complete a written service plan (Exhibit 1620-13) at the
time of the initial visit, when there are any changes in services, and at the time
of each review visit (every 90 or 180 days). The member or representative must
indicate whether they agree or disagree with each service authorization and sign
the service plan each time. The member must be given a copy of each signed
service plan.
11. The case manager must review, with the member and/or representative, the
Contractor’s process for immediately reporting any unplanned gaps in service
delivery at the time of each service review for each HCBS member receiving
“critical” services.
12. The member’s HCB service providers must be contacted at least annually to
discuss their assessment of the member’s needs and status. Contact should be
made as soon as possible to address problems or issues identified by the
member/representative or case manager. This should include providers of such
services as personal or attendant care, home delivered meals, homemaker,
therapy, etc.
If the member is receiving skilled nursing care from a home health agency,
contact is required with the service provider more frequently (see Standard XI,
Skilled Nursing Need, in this Chapter).
For members receiving behavioral health services, the case manager may need
to make contact with the service provider quarterly in order to complete the
behavioral health consultation.
13. The case manager is responsible for coordinating physician’s orders for those
medical services requiring a physician’s order (see HChapter 1200 of this Manual
for more information on which services require an order from the member’s
Primary Care Provider (PCP)).
If the case manager and PCP or attending physician disagree regarding the need
for a change in level of care, placement or physician’s orders for medical
services, the case manager may refer the case to the Contractor’s Medical
Director (or the AHCCCS Medical Director for members enrolled with a Tribal
Contractor) for review. The Medical Director is responsible for reviewing the
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-31
AHCCCS MEDICAL POLICY MANUAL
case, discussing it with the PCP and/or attending physician if necessary, and
making a determination in order to resolve the issue.
14. If the case manager determines during the reassessment process that changes in
placement or services are indicated, this must be discussed with the member
and/or representative prior to the initiation of any changes. This is especially
critical if the changes result in a reduction or termination of services.
15. The member or member representative must be notified in writing of any denial,
reduction, termination or suspension of services, when the member or
representative has indicated, on the service plan, that s/he disagrees with the
type, amount, or frequency of services to be authorized. Refer to Arizona
Administrative Code 9 A.A.C. 34 and the AHCCCS Contractors Operations
Manual (ACOM) policy 414 for more detailed information and specific time
frames.
All grievances and requests for hearings and appeals of members enrolled with
a Tribal Contractor are addressed directly to AHCCCS Administration, Office
of Administrative Legal Services. A managed care member’s request for
hearing and/or appeal is initiated through the member’s Program Contractor.
16. The case manager must be aware of the following regarding members eligible to
receive hospice services:
a. Members may elect to receive hospice services. These services may be
covered by private insurance or Medicare, if the member has Part A, or by
ALTCS if no other payer source is available.
b. The Medicare hospice benefit is divided into two 90-day election periods.
Thereafter, the member may continue to receive hospice benefits in 60-
day increments. A physician must recertify hospice eligibility at the
beginning or each election period.
c. The member has the right to revoke the election of Medicare hospice care
at any time during the election period and resume ALTCS coverage;
however, any remaining days of coverage are then forfeited for that
election period.
A member may also at any time again elect to receive Medicare hospice
coverage for any other hospice election periods for which they are eligible.
The hospice agency is responsible for providing covered services to meet
the needs of the member related to the member’s hospice-qualifying
condition. Medicaid services provided to members receiving Medicare
hospice services that are duplicative of Medicare hospice benefits (i.e.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-32
AHCCCS MEDICAL POLICY MANUAL
Home Health Aide, Personal Care and Homemaker Services) will not be
covered. Attendant care is not considered a duplicative service. If the
hospice agency is unable or unwilling to provide or cover medically
necessary services related to the hospice diagnosis, the services must be
provided by the Contractor. The Contractor may report such cases to
Arizona Department of Health Services (ADHS) as the hospice licensing
agency in Arizona. Refer to Chapter 1200H, Policy 1250, for additional
information regarding hospice services.
17. All nursing facilities that participate in AHCCCS are dually certified as
Medicare and Medicaid facilities. Therefore, beds in these nursing facilities may
not be designated as Medicare-only. An ALTCS member may not be asked to
leave a Medicaid-participating nursing facility after his/her Medicare benefit
days have been exhausted.
18. In most cases, members must receive a written 30-day advance notice before
discharge from a nursing facility as outlined in Code of Federal Regulations 42
C.F.R. 483.12. Exceptions may be made when the health and/or safety of the
member or other residents is/are endangered.
ALTCS Contractors set their own rules regarding advance notice of discharge of
members who reside in assisted living facilities in their contracts with those
facilities.
19. Case managers are responsible for using the electronic Member Change Report
(MCR) process to notify AHCCCS of a variety of changes in the member’s
status. Refer to Exhibit 1620-2 for a hard copy of the MCR form and more
information on the circumstances for using this form. Instructions for
completing the electronic MCR can be found in the AHCCCS Contractor
Operations Manual (ACOM), Chapter 400, Policy 411 available on the
AHCCCS Website. The hard copy form should only be used when an electronic
version is not possible (for example when member is no longer enrolled with the
Contractor).
20. The case manager is responsible for updating information in the Client
Assessment Tracking System (CATS) within 14 business days of the
reassessment.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-33
AHCCCS MEDICAL POLICY MANUAL
1620-F TRIBAL FEE-FOR-SERVICE STANDARDS
REVISION DATE: 07/01/12 (RELOCATED FROM CHAPTER 1200, CHAPTER OVERVIEW)
REVIEW DATE: 01/01/16, 03/01/13
In addition to all other Arizona Long Term Care System (ALTCS) case management
standards, the following standards also apply for members who are enrolled with a Tribal
Fee-For-Service (FFS) contractor:
1. For the following services, the tribal case manager must assist in obtaining the
documentation and must coordinate with the Division of Fee-For-Service
Management (DFSM) Care Management Systems Unit (CMSU) for approval
prior to the tribal case manager entering the service authorization on the
CA165/Service Plan;
a. Specialty rates for facilities (nursing facilities and alternative residential
settings) and above level of care facility rates, and
b. Home Modifications (refer to Exhibit 1240-4 in Chapter 1200 of this
Manual).
2. For the following services, the tribal case manager must obtain medical review
by the DFSM CMSU Unit before the tribal case manager provides authorization
and enters the service authorization on the CA165/Service Plan:
a. Durable Medical Equipment (DME), when the cost exceeds $500 (items
between $300 and $499 must be authorized by the FFS case manager and
included on the CA165/Service Plan).
b. Medically necessary incontinence supplies (e.g., diapers and Chux). This
does not include catheters, ostomy supplies, etc. and
c. Specialty beds and wound care treatments.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-34
AHCCCS MEDICAL POLICY MANUAL
1620-G BEHAVIORAL HEALTH STANDARD
REVISION DATES: 01/01/16, 10/01/13, 05/01/12, 10/01/11, 01/01/11, 10/01/07, 09/01/06,
09/01/05, 02/01/05, 10/01/04
REVIEW DATE: 03/01/13
INITIAL
EFFECTIVE DATE: 02/14/1996
In addition to all other Arizona Long Term Care System (ALTCS) case management
standards, the following standards also apply to members who need or receive behavioral
health services:
1. Direct referral for a behavioral health evaluation may be made by the member
or by any health care professional in coordination with the case manager and
Primary Care Provider (PCP).
2. Requests for behavioral health services made by the member or member
representative must be assessed for appropriateness within three business days
of the request. If it is determined that services are needed, the referral for
evaluation must be made within one business day.
3. Behavioral health services which have been determined to be medically
necessary by a qualified behavioral health professional (as defined in Arizona
Administrative Code 9 A.A.C.10) may be provided.
4. The case manager must ensure there is communication with the PCP and
behavioral health providers involved in the member’s care and that care is
coordinated with other agencies and involved parties.
5. The case manager must ensure the timely involvement of a behavioral health
professional to assess, develop a care plan and preserve the current placement if
possible when a member in a non-behavioral health setting presents with
difficult to manage behaviors (new or existing). Refer to the “Policy for
Management of Acute Behavioral Health Situations” found in Appendix H of
this manual for more detailed information on that process.
6. Information from the Pre-Admission Screening and Resident Review (PASRR)
Level II Evaluation for determination of mental illness (completed by the
Arizona Department of Health Services when indicated by PASRR Level I
screening) regarding a member’s need for specialized services must be
incorporated into the member’s service plan. AHCCCS registered Nursing
Facilities (NFs) must complete Level I PASRR screening, or verify that a

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-35
AHCCCS MEDICAL POLICY MANUAL
screening has been conducted, in order to identify mental illness and/or an
intellectual disability prior to initial admission of individuals to a NF bed that is
Medicaid certified or dually certified for Medicaid/Medicare. (See additional
information related to PASRR in Chapter 1200, Policy 1220 of this Manual)
7. Behavioral health appointments must be provided within the following
timeframes:
a. Within 24 hours of referral for emergency appointments, or
b. Within 30 days of referral for routine appointments.
8. Case management for a member receiving behavioral health services must be
provided in consultation/collaboration with a qualified behavioral health
professional in those cases where the case manager does not meet the
qualifications of a behavioral health professional (as defined in 9 A.A.C. 10).
The consultation does not have to be with the provider of behavioral health
services. It may be with the Contractor’s behavioral health coordinator or other
qualified designee.
9. The ALTCS case manager must make contact with the behavioral health
professional prior to the initial behavioral health consultation for all members
receiving/needing behavioral health services. Quarterly discussions between the
ALTCS case manager and the behavioral health professional are required
thereafter as long as the member continues to receive/need behavioral health
services.
10. Initial and quarterly discussions are not required for members who are stable on
psychotropic medications and/or are not receiving any behavioral health
services other than medication management.
11. The case manager must document the content and results of the initial and
quarterly discussions with the behavioral health professional. The discussion
must be a communication between the case manager and a behavioral health
professional about the member’s status and plan of treatment. It must not simply
be a report from the provider that has been received by the case manager and
put in the case file.
12. As part of the service plan monitoring, the case manager must review the
psychotropic medications being taken by the member. Only those medications
used to modify behavioral health symptoms need to be included in this special
monitoring. Examples of medication uses that do not require this monitoring are
sedative hypnotics when used to treat insomnia or on an as needed basis prior to
a procedure, anti-anxiety medications used for muscle spasms and
anticonvulsants used to treat a seizure disorder.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-36
AHCCCS MEDICAL POLICY MANUAL
Documentation of the medication review must be clearly evident in the member
case file. The review must take place at each reassessment and include the
purpose of the medication, the effectiveness of the medication and any adverse
side effects that may have occurred. Any concerns noted (for example,
medication appears to be ineffective, adverse side effects are present, multiple
medications apparently prescribed for the same diagnosis) must be discussed
with the behavioral health consultant and/or prescribing practitioner. Case notes
must reflect this discussion and a plan of action to address these issues.
13. Case managers are responsible for identifying, assisting with and monitoring the
special needs and requirements related to members who are unable or unwilling
to consent to treatment (i.e. petitioning, court ordered treatment and judicial
review). Case file documentation must reflect this activity.
14. The behavioral health code that reflects the member’s current behavioral health
status must be updated at the time of each review visit on the CA161/Placement
Maintenance screen in Client Assessment Tracking System (CATS). Refer to
the AHCCCS Contractors Operations Manual (ACOM), Chapter 400, Policy
411, for a list and description of these codes.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-37
AHCCCS MEDICAL POLICY MANUAL
1620-H TRANSITIONAL PROGRAM STANDARD
REVISION DATES: 05/01/12, 04/01/12, 10/01/11, 10/01/07, 09/01/06, 09/01/05, 02/01/05,
10/01/04
REVIEW DATE: 01/01/16, 03/01/13
INITIAL
EFFECTIVE DATE: 02/14/1996
The Arizona Long Term Care System (ALTCS) Transitional program is a program for
currently eligible Arizona Long Term Care System ALTCS members who have improved
either medically, functionally or both, to the extent that they are no longer at immediate
risk of institutionalization at a Nursing Facility (NF) or Intermediate Care Facility (ICF)
for persons with Intellectual Disabilities level of care. These members continue to require
some long term care services, but at a lower level of care. The ALTCS Transitional
program allows those members who meet the lower level of care, as determined by the
Pre-Admission Screening (PAS), to continue to receive all ALTCS covered services that
are medically necessary. NF and ICF services are excluded, since reassessment has
determined that institutional services are not medically necessary.
In addition to all other ALTCS case management standards, the following standards also
apply to Transitional program members:
1. The case manager, upon being notified of the change of a member to the
Transitional program, must discuss the change in level of care with the member
or representative to ensure understanding of the change.
2. The case manager must ensure that the member in a Home and Community
Based (HCB) setting meeting transitional criteria continues to receive all
covered Home and Community Based Services (HCBS) as necessary.
3. While institutional services are no longer considered medically necessary for
transitional eligible members, a short-term stay in a NF or ICF is available.
ALTCS Transitional program members whose medical condition temporarily
worsens to the extent that NF services are medically necessary may receive up
to 90 continuous days of care at any one admission.
4. The case manager must ensure that the member, or the representative of a
member, already residing in a NF or ICF who becomes eligible for the
Transitional program., understands that discharge from the NF or ICF is
necessary within 90 days from the Transitional program effective date. The case
manager must work with the member or representative towards HCBS
placement as soon as possible.
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-38
AHCCCS MEDICAL POLICY MANUAL
5. A PAS reassessment must be requested, via electronic Member Change Report
(MCR), within 45 days of institutional admission, for any Transitional program
member who has had a deterioration of condition and who is expected to need NF
or ICF services for greater than 90 continuous days. A PAS reassessment is not
needed if a Transitional program member will remain in or return to a HCB setting
within 90 days.
The case manager must follow up on the MCR with the local ALTCS office after the PAS
reassessment has been requested if there has been no response by the 60th day following
admission. Alternate placement options may need to be explored in case the member
continues to meet the transitional program criteria.
Case file documentation must demonstrate that the case manager has taken appropriate and
timely action either to pursue discharge to a HCB setting or facilitate a PAS reassessment as
indicated.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-39
AHCCCS MEDICAL POLICY MANUAL
1620-I HIGH COST BEHAVIORAL HEALTH REINSURANCE STANDARD
REVISION DATES: 01/01/16, 10/01/13, 03/01/13, 05/01/12, 01/01/11, 10/01/07, 09/01/05,
02/01/05, 10/01/04
INITIAL
EFFECTIVE DATE: 2/14/1996
The Arizona Long Term Care System (ALTCS) program for high cost behavioral health
reinsurance is specifically designed to provide supplemental payment for members who are
elderly and/or have physical disabilities, enrolled with ALTCS Contractors (as specified by
contract), and who meet all of the following criteria:
1. Have significant behavioral problems or a history of these behaviors which have
been documented as difficult to manage,
2. Require a specialized service regimen for the management of his/her behavioral
challenges,
3. Would be inappropriate for placement in a locked Alzheimer’s or dementia unit,
and
4. Behavioral health reinsurance was approved by AHCCCS prior to October 1, 2007
and the case was active on September 30, 2007.
A member’s temporary absence from the approved placement (e.g. for hospitalization) will
not impact the continuation of the approval upon the member’s return. However, a
previously approved reinsurance case where the member has been terminated for the
circumstances described below cannot be reapproved at a later date.
1. Contractor’s activity to transfer the member to a lower level of care.
2. AHCCCS determines through the review process at renewal that the member no
longer meets the criteria.
In addition to all other ALTCS case management standards, the following standards also
apply to members covered under the ALTCS reinsurance program for high cost
behavioral health:
1. A request for renewal of a reinsurance authorization must be submitted to the
AHCCCS/Division of Health Care Management (DHCM)/ALTCS Unit using
the form found in Exhibit 1620-6, within ten business days prior to the
expiration of the current approval. Additional provider documentation that
supports the member’s behaviors and need for intervention must also be
submitted.
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-40
AHCCCS MEDICAL POLICY MANUAL
AHCCCS will provide the Contractor with written verification of authorization
or denial. Authorization will be granted for the member’s current placement and
setting only. If there is a subsequent change of placement or setting, information
and documentation to describe the reason for the change must be submitted as a
new reinsurance request. Contractors must also notify AHCCCS when a
reinsurance member is disenrolled from ALTCS, transferred to another
Contractor and/or discharged from a specialized treatment setting.
2. The service plans for E/PDmembers who receive specialized services covered
under the High Cost Behavioral Health Reinsurance program must be
coordinated with the member’s Primary Care Provider (PCP) and the
Contractor’s Medical Director.
3. Covered services may be provided in the member’s own home, in a Home
Community Based (HCB) approved alternative residential setting, an
unclassified health care institution licensed by the Arizona Department of
Health Services or a nursing facility that is licensed to provide behavioral health
services.
4. All institutional and Home Community Based Services (HCBS) described in
Chapter 1200 of this Manual, including non-emergency transportation, are
included in the High Cost Behavioral Health Reinsurance program. Behavioral
health services, except as noted below, are also covered. The following services
are excluded from behavioral health reinsurance coverage under this program as
they are included as a part of regular reinsurance:
a. Individual and group behavioral health counseling
b. Acute care hospitalization, including psychiatric hospitalization
c. Durable medical equipment and medical supplies
d. Pharmaceuticals
e. Physician services, and
f. Therapies, including physical therapy, occupational therapy, speech
therapy and respiratory therapy.
Refer to the Encounter Reporting User Manual and the AHCCCS
Reinsurance Claims Processing Manual for information regarding
reporting and payment issues. These manuals are available on the
AHCCCS Web site at HUwww.azahcccs.govUH

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-41
AHCCCS MEDICAL POLICY MANUAL
1620-J OUT-OF-STATE PLACEMENT STANDARD
REVISION DATES: 01/01/16, 05/01/12, 01/01/11, 10/01/07, 01/01/06, 09/01/05, 02/01/05,
10/01/04
REVIEW DATE: 03/01/13
INITIAL
EFFECTIVE DATE: 02/14/1996
Out-of-state services are covered as provided for under Code of Federal Regulations 42
C.F.R., Part 431, Subpart B. This includes services that, as determined on the basis of
medical advice, are more readily available in other states and services needed due to a
medical emergency. Services furnished to AHCCCS members outside the United States
(as defined in Chapter 300) are not covered.
This section of the manual is intended to address the standards related to the long term
placement of members in out-of-state settings. It does not apply to situations in which the
member is temporarily absent from the State.
Out-of-state placements may be approved in licensed/certified residential-type settings
only (for example, nursing facilities, residential treatment centers, group homes).
Personal residences outside of the State of Arizona are not approved placements. Out-of-
state facility providers must be registered with AHCCCS.
Written authorization from AHCCCS is required prior to the placement of an Arizona
Long Term Care System (ALTCS) member in an out-of-state placement.
In addition to all other ALTCS case management standards, the following standards also
apply when the Contractor seeks an out-of-state placement:
1. A request for out-of-state placement must be submitted to AHCCCS when it is
determined that an ALTCS member’s need for services cannot be met by
existing providers within the State of Arizona.
2. Tribal Contractors requesting out-of-state placement approval for members
being placed in one of the nursing facilities in Utah or New Mexico must submit
a written request to the AHCCCSDHCM MM Unit using the form found in
Exhibit 1620-7.
3. Contractors requesting out-of-state placement approval must submit a written
request to the AHCCCSDHCM MM Unit. The request must include at least the
following information:
a. Member name and AHCCCS ID#

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-42
AHCCCS MEDICAL POLICY MANUAL
b. Name/location of facility where the Contractor intends to place the
member, include the facility’s AHCCCS provider ID#
c. Description of the member’s medical/behavioral condition that
necessitates this placement
d. Description of facility’s program(s) that makes this placement appropriate
for the member
e. Information about other in-state placement options ruled out for the
member, and
f. Plan for member’s return to an Arizona placement
4. When justified, AHCCCS approvals are generally given for six month intervals.
The case manager must submit appropriate documentation to request a renewal
if the out-of-state placement is expected to continue beyond the initial approval
time period. Requests for renewals must be submitted prior to the expiration of
the previous approval.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-43
AHCCCS MEDICAL POLICY MANUAL
1620-K SKILLED NURSING NEED STANDARD
REVISION DATES: 05/01/12, 01/01/11, 10/01/07, 09/01/05, 02/01/05, 10/01/04
REVIEW DATE: 01/01/16, 03/01/13
INITIAL
EFFECTIVE DATE: 02/14/1996
The case manager is responsible for ensuring that a member who has skilled nursing
needs is provided with the monitoring and care necessary to meet his/her individual
needs.
A. NON-INSTITUTIONAL SETTINGS
1. The member’s initial needs assessment must be conducted by an AHCCCS
registered home health agency if the member is at risk of compromising his/her
skin integrity (for example, the member is bed bound, quadriplegic) or if the
member has a history of medical instability (for example, frequent seizures,
unstable diabetes, Chronic Obstructive Pulmonary Disease [COPD]). If a
registered home health provider is not available, an independent registered nurse
may conduct the assessment for skilled nursing needs. Thereafter, the member
will be monitored for skilled nursing needs, by the home health agency or
independent registered nurse, within established timeframes and as otherwise
necessary. Department of Economic Security/Division of Developmental
Disabilities (DES/DDD) may utilize its district nurses in performing these
assessments and making recommendations to the Primary Care Provider (PCP)
for continued monitoring.
2. A member who has skilled nursing needs (for example, pressure ulcers, surgical
wounds, tube feedings, pain management and/or tracheotomy) must be referred
to a home health agency for the initial assessment and the ongoing provision of
skilled nursing care as well as monitoring determined necessary by the
assessment. An independent registered nurse may provide these services if an
AHCCCS registered home health agency is not available.
3. The case file must contain documentation from the initial nursing assessment.
In addition there must be evidence of quarterly consultations with the provider
of the skilled nursing care and documentation of the member’s condition and
progress until the member no longer requires skilled nursing care.
4. If the member or member representative refuses skilled nursing care, the case
manager must inform the member or representative of the possible risks of
refusing such care. The case manager must utilize a managed risk agreement to
document the reason given for refusing the recommended care and that the

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-44
AHCCCS MEDICAL POLICY MANUAL
member or representative has been informed of the risks. The member or
representative should sign this agreement. The member’s PCP must also be
informed of the refusal.
B. INSTITUTIONAL SETTINGS
1. The facility is responsible for providing appropriate care to meet the needs of
each member who is at risk of compromising his/her skin integrity (for example,
the member being bed bound, quadriplegic, or having a history of medical
instability such as frequent seizures, unstable diabetes, COPD) and members
who require skilled nursing for other conditions such as pressure ulcers, surgical
wounds, and/or pain management.
Every six months, the case manager must consult with the appropriate facility staff and
review treatment record and other Level of Care documentation related to the member’s
condition and progress. The member’s progress related to the specific skilled nursing
need(s) including compliance with prescribed treatments, must then be documented in the
case management file.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-45
AHCCCS MEDICAL POLICY MANUAL
1620-L CASE FILE DOCUMENTATION STANDARD
REVISION DATES: 01/01/16, 03/01/13, 05/01/12, 01/01/11, 10/01/07, 10/01/06, 09/01/05,
02/01/05, 10/01/04
INITIAL
EFFECTIVE DATE: 02/14/1996
1. Case file documentation must be complete and comprehensive. It may be
written by hand or typewritten. Each case file page should indicate the
member’s name and AHCCCS identification number. Each entry made by the
case manager must be signed and dated. If electronic records are utilized, the
Contractor must ensure the integrity of the documentation. AHCCCS may
request that documentation kept in an electronic system be printed out for
purposes of a case file review.
2. Contractors must adhere to the confidentiality standards under the Health
Insurance Portability and Accountability Act (HIPAA).
3. Case files must be kept secured.
4. Contractors are expected to maintain a uniform tracking system for
documenting the begin and end dates of those services listed in the
Placement/Service Planning Standard section of this chapter, as applicable, in
each member’s chart. This documentation is inclusive of renewal of services
and the number of units authorized for services.
5. Tribal Contractors must show authorization of services on the CA165/Service
Plan.
6. Case files must include, at a minimum:
a. Member demographic information, including residence address and
telephone number, and the emergency contact person and his/her
telephone number
b. Identification of the member’s Primary Care Provider (PCP)
c. Uniform Assessment Tool (UAT), completed at least annually
d. Information from 90/180 day on-site assessments that addresses at least
the following:

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-46
AHCCCS MEDICAL POLICY MANUAL
i. Member’s current medical/functional/behavioral health status,
including strengths and needs
ii. The appropriateness of member’s current placement/services in
meeting his/her needs, including the discharge potential of
residentially placed member
iii. The cost effectiveness of Arizona Long Term Care System (ALTCS)
services being provided
iv. Identification of family/informal support system or community
resources and their availability and willingness to assist the member
as uncompensated caregivers, including barriers to assistance
v. Identification of service issues and/or unmet needs, an action plan to
address them and documentation of timely follow-up and resolution
vi. Member-specific goals that will allow the member to gain functional
skills or maintain/increase their current functioning level. Goals must
be evaluated for appropriateness at each review with progress
towards each goal documented and adjustments to goals/services
made as necessary. Documentation should reflect member
involvement in the development of goals
vii. Member’s ability to participate in the review and/or who has been
designated for the case manager to discuss service needs and goals
with if the member is unable to participate, and
viii. Environmental and/or other special needs.
e. Information from the initial on-site assessment that includes all items
listed in 4 above, as well as, for those members with HCBS services
already in place at the time of enrollment, an assessment of the medical
necessity and cost effectiveness of those services and a care/service plan
that indicates which Prior Period Coverage (PPC) services will be
retroactively authorized by the Contractor.
f. Copies of the member’s Cost Effectiveness Studies (CES), placement
history and service plans/authorizations. The service plan must be signed
by the member or member representative at each service review visit
(every 90 or 180 days) and a copy kept in the file.
g. A copy of the HCBS Needs Tool (HNT) completed for all members
receiving Attendant Care, Personal Care, Homemaker, Habilitation and/or
Respite services that indicates how the service hours were assessed and
which portions of care, if any, are provided by the member’s informal
support system.
h. A copy of the contingency plan and other documentation that indicates the
member/representative has been advised regarding how to report
unplanned gaps in authorized “critical” services.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-47
AHCCCS MEDICAL POLICY MANUAL
i. A copy of the “Spouse Attendant Care Acknowledgement of
Understanding” Form (Exhibit 1620-12) signed by any member choosing
to have his or her spouse as the paid caregiver, both before that service
arrangement is initiated and annually to indicate the member’s continued
choice for this option.
j. Copies of Agency with Choice (AWC) or Self Directed Attendant Care
(SDAC) related forms requiring case manager signature for all members
choosing a member directed option, including the AWC Individual
Representative form. Member directed forms can be found in Chapter
1300 of this manual.
k. A copy of the managed risk agreement, if indicated for the member, that
identifies potential risks associated with service and/or placement
decisions the member has made
l. Copies of current Client Assessment Tracking System (CATS) screens
(CA160, CA161, CA165) for Tribal Contractors. CATS screens or
comparable forms for Contractors.
m. Notices of Action sent to the member regarding denial or changes of
services (discontinuance, termination, reduction or suspension)
n. Member-specific correspondence
o. Physician’s orders for medical services and equipment
p. Documentation that a Pre-Admission Screening and Resident Review
(PASRR) Level I screening and PASRR Level II evaluation, if applicable,
have been completed for members in nursing facility placements and that
copies are in the facility chart. A copy of the PASRR Level II evaluation,
if applicable, must also be retained in the case manager’s file.
q. Provider evaluations/assessments and/or progress reports (for example,
home health, therapy, behavioral health)
r. Case notes including documentation of the type of contact made with the
member and/or all other persons who may be involved with the member’s
care (e.g. providers). Case notes should also include notifications of
services not provided as scheduled (e.g. hospitalization, vacation, or
respite outside of the home).
s. Documentation of the initial and quarterly consultation/collaboration with
a qualified behavioral health professional, if applicable, and

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-48
AHCCCS MEDICAL POLICY MANUAL
t. Other documentation as required by the Contractor.
7. ALTCS member file information must be maintained by the Contractor for a
minimum of five years.
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-49
AHCCCS MEDICAL POLICY MANUAL
1620-M CONTRACTOR CHANGE STANDARD
REVISION DATES: 01/01/16, 05/01/12, 01/01/11, 07/01/08, 10/01/07, 09/01/05, 02/01/05,
10/01/04
REVIEW DATE: 03/01/13
INITIAL
EFFECTIVE DATE: 02/14/1996
For purposes of this section, the term “Elderly and/or have Physical Disabilities (E/PD)
Contractor” refers to all Contractors, but not the Arizona Department of Economic
Security/Division of Developmental Disabilities (DES/DDD).
Members may be transferred between E/PD Contractors or between an E/PD Contractor
and DES/DDD. Transfers between E/PD Contractors are generally as a result of the
member moving out of one Contractor’s service area into another’s. Transfers between an
E/PD Contractor and DES/DDD are the result of a change in DDD eligibility, as
determined by DES/DDD. The service area of DES/DDD includes the entire state. When
a DDD eligible member moves from one area of the state to another, a change of
Contractors does not occur; there is just a change of DES/DDD case managers.
1. The case manager is responsible for the transition of and discharge planning for
members transferred to another Contractor. Refer to Chapter 500H, Policy 520, of
this manual regarding member transitions for further information on standards
set forth for the transition of Arizona Long Term Care System (ALTCS)
members.
2. A change of E/PD Contractors due to member movement to another service area
or member choice where multiple Contractors are available may be initiated by:
a. The E/PD member or his/her representative
b. The current Contractor, or
c. AHCCCS Administration.
3. The case manager is responsible for initiating action when the request is made
by the member or member representative. Case managers must not assume, or
allow the member to assume, that a change of Contractor is automatic.
4. E/PD case managers are responsible for explaining that there may be service
limitations and exclusions when the member moves into another Contractor’s
service area.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-50
AHCCCS MEDICAL POLICY MANUAL
Refer to the AHCCCS Contractor Operations Manual (ACOM) Policy 403 for
more information on these conditions and changes of Contractor.
5. For transfers within or into Maricopa County, the E/PD member must make a
choice of Contractors before any change can be processed. The member will be
given a choice of Contractors by the local ALTCS office upon notice (from
either the member/representative or the case manager) that the member intends
to move or has moved to Maricopa County.
6. Tribal members are considered to have on-reservation status even though they
are admitted to a nursing facility or alternative residential setting within a
Contractor area of service off the reservation. Tribal members who move to own
home HCBS settings off reservation will be transitioned to the Contractor
serving that area.
7. Case managers must discuss the potential transfer of a member with the
Transition Coordinator or case manager of the potential receiving Contractor to
ascertain availability of services in that area. This information will assist the
member/family with planning. A list of current Transition Coordinators for the
Contractors is available from the AHCCCS Division of Health Care
Management/Case Management Unit.
8. The Contractor Change Request (PCCR) form (found in Exhibit 1620-8) is used
for all member transfers. In some cases, as noted below, the transfer will first
require the receiving Contractor’s agreement to accept enrollment of the
member. In others because of a change in the county of fiscal responsibility or
reservation status, the relinquishing and receiving Contractor only need to agree
on the effective date of the transfer that will occur.
a. E/PD members who move from any setting to Home and Community
Based Services (HCBS) own home in another Contractor’s service area
will have a change of fiscal county and therefore Contractor. The
relinquishing and receiving Contractor must agree to the effective date of
transfer.
NOTE: Refer to Chapter 100 of this Manual for definition of “Own
Home”.
b. Native American members who move from any setting type to HCBS own
home in another Tribal Contractor’s service area/reservation will have a
change of reservation status and therefore Tribal Contractor. This applies
when the Tribal Contractor enrolled E/PD member will reside on a
different reservation than where s/he lived at enrollment (for example, A
Navajo Nation member who will now reside on the Tohono O’Odham

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-51
AHCCCS MEDICAL POLICY MANUAL
reservation in his/her “own home” should be enrolled with Tohono
O’Odham Nation). The relinquishing and receiving Tribal Contractors
must agree to the effective date of transfer.
c. Native American E/PD members who are enrolled with an E/PD
Contractor who move to HCBS own home on the reservation will have a
change of reservation status and therefore will be enrolled with the Tribal
Contractor responsible for case managing that reservation. The
relinquishing and receiving Tribal Contractors must agree to the effective
date of transfer.
d. E/PD Tribal members who move from a Tribal Contractor’s
reservation/service are (HCBS or institutional setting) to HCBS own home
off-reservation within an E/PD Contractor’s area of service will have a
change of reservation status and therefore Contractor. The sending and
receiving Contractors must agree to the effective date of transfer.
e. Transfers of E/PD members who move from any setting to an institutional
or alternative residential setting in another E/PD Contractor’s service area
will require the receiving Contractor to agree to the transfer. The sending
and receiving Contractors must agree to the effective date of transfer.
f. Transfers of E/PD members in Maricopa County for whom medical
continuity of care is cited by the member’s Primary Care Provider (PCP)
as the reason for a change of Contractors must be reviewed and approved
by the Medical Directors of both Program Contractors before the
relinquishing Contractor can submit the PCCR. The sending and receiving
Contractors must agree to the effective date of transfer.
g. Transfers of E/PD members who are minor children that are moved/placed
out of the service area where their parents reside to another service area
will require the receiving Contractor to agree to the transfer. The sending
and receiving Contractors must agree to the effective date of transfer.
9. DES/DDD must notify AHCCCS (via electronic Member Change Report) if a
DDD member no longer meets the DDD eligibility criteria. AHCCCS would
need to complete a PAS assessment to determine if the member meets ALTCS
eligibility criteria as an E/PD member. If the member is determined to be E/PD,
DES/DDD must coordinate the transition to an E/PD Contractor through the
PCCR. Both sending and receiving Contractors must agree to the effective date
of transfer.
10. The relinquishing case manager must provide adequate member information
(case documentation and/or medical records) to the receiving Contractor to

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-52
AHCCCS MEDICAL POLICY MANUAL
assure continuity of care. The ALTCS Enrollment Transition Information (ETI)
form (found in Exhibit 1620-9) is used for this purpose.
11. The potential receiving Contractor is responsible for reviewing the request and
notifying the relinquishing Contractor within ten business days of the request
for transfer decision.
The current/relinquishing Contractor must notify the member’s case manager
and the member within seven days of receiving decision notification from the
potential receiving Contractor. The relinquishing Contractor must arrange and
pay for transporting the member, if necessary.
12. If a change of Contractor is agreed to by both Contractors, a scanned copy of
the completed/signed PCCR form, or at least the information listed below must
be sent via secure email to the AHCCCS PCCR mailbox (pccr@azahcccs.gov).
a. Member’s Name
b. Member ID#
c. Address and county of member’s new residence
d. Phone number of member or representative (this is needed to allow
AHCCCS eligibility to confirm the new residence before processing the
transfer)
e. Effective date of transfer to new Contractor.
13. If the potential receiving Contractor denies the request for enrollment change,
the relinquishing Contractor may request a review by AHCCCS after both
receiving and relinquishing Contractors representatives have discussed the
request and have not been able to come to agreement.
AHCCCS will notify the relinquishing Contractor of its decision. The
Contractor will be responsible for informing the member of that decision.
14. Both the relinquishing and receiving Contractions are responsible for ensuring a
safe transition for the member.
15. The CA161 (Placement Screen) and service plan must be updated to reflect any
changes in placement, services and/or Contractor enrollment dates.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-53
AHCCCS MEDICAL POLICY MANUAL
1620-N SERVICE CLOSURE STANDARD
REVISION DATES: 01/01/16, 05/01/12, 01/01/11, 01/01/10, 10/01/07, 09/01/05, 02/01/05,
10/01/04
REVIEW DATE: 03/01/13
INITIAL
EFFECTIVE DATE: 02/14/1996
1. Closure of a member’s service(s) may occur for several different reasons. The
following is a list of the most common reasons. This list is not meant to be all-
inclusive:
a. The member is no longer Arizona Long Term Care System (ALTCS)-
eligible, as determined by AHCCCS/Division of Member Services/Field
Operations Administration (DMS/FOA)
b. The member dies
c. The case manager and/or physician determine that a service is no longer
necessary
d. The member or representative requests discontinuance of the service(s) or
refuses services.
e. The member moves out of the Contractor service area
f. The member leaves the Contractor service area temporarily and the
Contractor is unable to continue services
g. For Elderly and/or have Physical Disabilities (E/PD) members in
Maricopa County only – the member’s Contractor has been changed due
to member request, and/or
h. Contact has been lost with the member.
2. Case managers are required to provide community referral information on
available services and resources to meet the needs of members who are no longer
eligible for ALTCS.
3. If the member has been determined ineligible for ALTCS, the member or member
representative will be informed of this action and the reason(s), in writing, by
DMS/FOA. This notification will provide information about the member’s rights
regarding that decision.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-54
AHCCCS MEDICAL POLICY MANUAL
4. If a service is closed because the ALTCS Contractor has determined that it is no
longer medically necessary, the member must be given a NOA regarding the plan
to discontinue the service that contains information about his/her rights with
regards to that decision.
A NOA is not required if the member/representative agrees with the closure of a
service on the service plan (Exhibit 1620-13).
Refer to Arizona Administrative Code 9 A.A.C. 34 for specific information and
timeframes about written member notices. The AHCCCS Contractor Operations
Manual (ACOM) policy 414 provides additional guidelines on and examples of
Notices of Action.
5. When the member’s enrollment will be changed to another Contractor, the case
manager must coordinate a transfer between the Contractors. Refer to Standard
XIII, Contractor Change, in this Chapter, as well as to HChapter 500H of this manual
for more detailed information.
6. The case manager is responsible for notification of and coordination with service
providers to assure a thorough discharge planning process.
7. If a member is disenrolled from ALTCS, but remains eligible for AHCCCS acute
care benefits, the case manager must direct the member to the AHCCCS website
for information regarding available acute care health plans and encourage the
member to convey their choice of health plans to the AHCCCS Communication
Center at 1-800-962-6690.
8. Case notes must be updated to reflect service closure activity, including, but not
limited to:
a. Reason for the closure
b. Member’s status at the time of the closure, and
c. Referrals to community resources if the member is no longer ALTCS
eligible.
9. The case manager must update placement history (CA161) and service plan
information in the case file and Clients Assessment Tracking System (CATS),
as applicable. When a service is closed, the end date and service units must be
adjusted accordingly.
10. A member who is disenrolling from ALTCS will generally remain enrolled
through at least the end of the month in which the eligibility is terminated. If the

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-55
AHCCCS MEDICAL POLICY MANUAL
member voluntarily withdraws and wants ALTCS benefits to stop immediately,
the disenrollment will be effective with the processing of the withdrawal by
DMS/FOA.
11. The member continues to be the responsibility of the Contractor until the
disenrollment is processed by ALTCS and appears on the Contractor’s
roster. Members are eligible to receive medically necessary services through
their disenrollment date.
12. When the reason for termination is the member’s death, the case manager must
end date the service authorization(s) with the actual date of death.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-56
AHCCCS MEDICAL POLICY MANUAL
1620-O ABUSE/NEGLECT REPORTING STANDARD
REVISION DATES: 05/01/12, 01/01/11, 10/01/07, 09/01/05, 02/01/05, 10/01/04
REVIEW DATE: 01/01/16, 03/01/13
INITIAL
EFFECTIVE DATE: 02/14/1996
1. Suspected cases of abuse neglect and/or exploitation must be reported to the
appropriate authorities by the case manager. Case managers are responsible for
identifying the agency in their area that handles these issues for adults and/or
children, as applicable.
2. Adult abuse includes:
a. Intentional infliction of physical harm
b. Injury caused by negligent acts or omissions (including pressure sores and
dehydration)
c. Unreasonable confinement
d. Sexual abuse or sexual assault,
e. Neglect (a pattern of conduct without the person’s informed consent
resulting in deprivation of food, water, medication, medical services,
shelter, cooling, heating or other services necessary to maintain minimum
physical or mental health), and/or
f. Exploitation (the illegal or improper use of vulnerable adult or his
resources for another’s profit or advantage).
3. Vulnerable adult is defined as an individual who is 18 years of age or older who
is unable to protect himself/herself from abuse, neglect or exploitation by others
because of a mental or physical impairment. Vulnerable adult includes an
incapacitated person (defined in Arizona Revised Statute A.R.S. 14-5101 as any
person who is impaired by reason of mental illness, mental deficiency, mental
disorder, physical illness or disability, chronic use of drugs, chronic intoxication
or other cause, except minority, to the extent that he lacks sufficient
understanding or capacity to make or communicate responsible decisions
concerning his person).

CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-57
AHCCCS MEDICAL POLICY MANUAL
4. Child abuse includes:
a. The infliction or allowing of physical injury including that which results
from permitting a child to enter or remain in a dangerous environment or
setting
b. Impairment of bodily function or disfigurement
c. Infliction of or allowing another person to cause serious emotional harm,
d. Inflicting or allowing sexual abuse and/or sexual exploitation, including
incest, molestation and child prostitution to occur and
e. Unreasonable confinement.
5. Adult Protective Services (APS) – a program within the Arizona Department of
Economic Security, which is governed by A.R.S. §§46-451 through 46-459 and
14.5310.01, to protect vulnerable adults from abuse or neglect.
APS workers also serve as a part of Arizona’s Ombudsman Program to act as an
advocate, investigate reports of abuse, neglect or exploitation and assist in
problem resolution for individuals residing in long term care facilities.
6. Department of Child Safety (DCS) – a department which functions to ensure the
safety of children. A.R.S. Title 8 Chapter 10 (§§8-800 through 8-819) requires
that the agency investigate reports of suspected child abuse, neglect, and/or
abandonment.
The program also assists parents/caregivers in receiving available services
which will help improve family relationships and strengthen their ability to
provide good child care. If this is not possible, alternative solutions and
placement are sought.
7. For Tribal members – the APS and CPS programs do not have jurisdiction on
the reservations to intervene in cases of abuse, neglect or exploitation. Case
managers must determine which Tribal program is responsible for handling
these issues in their area.
8. Documentation related to the suspected abuse, neglect or exploitation, including
the reporting of such, must be kept in a file, separate from the member’s case
file, that is designated as confidential. The confidentiality of this information is
protected under A.R.S. §§36-441, 36-445.01 through 445.02, 36-2401 through
2404, 36-2917, and 42 Code of Federal Regulations C.F.R. 431 Subpart F.
CHAPTER 1600
CASE MANAGEMENT
POLICY 1620
CASE MANAGER STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1620-58
AHCCCS MEDICAL POLICY MANUAL
9. Member quality of care issues must be reported to and a resolution coordinated
with the Contractor’s Quality Management Unit and/or AHCCCS/Division of
Health Care Management/Clinical Quality Management Unit. Refer to Chapter
900H, Policy 960, of this manual for more information on the Contractor’s
responsibilities related to these issues.
EXHIBIT 1620-1
CASE MANAGEMENT (CM) TIMEFRAMES
4BEXHIBIT 1620-1
CASE MANAGEMENT (CM) TIMEFRAMES
Revision Date: 01/01/16, 05/01/12, 01/01/11
INITIAL CONTACT/VISIT
TIMEFRAME
Initial Contact (CM or designee)
Within seven business days of enrollment
Initial on-site visit
Within 12 business days of enrollment
Initial service start-up
Within 30 days of enrollment
CASE FILE UPDATES
TIMEFRAME
Initial Cost Effective Study (CES)
Prior to placement/services
Initial CES, when services in place at
enrollment
Within 12 business days of enrollment
CES update
Prior to placement change to HCBS and
annually for all HCBS members, and when
there is a change in the member’s condition,
authorized services, or rates.
CES when no discharge potential
No updates required, CES will reflect “NONE”
CATS ENTRIES
TIMEFRAMES
CES/CA160
Within ten business days of date of action
Placement/CA161
Within ten business days of date of action
Service Plan/CA165 (Tribal only)
Within five business days of date of action
REASSESSMENT VISITS
(Includes service plan review and signature)
TIMEFRAMES
HCBS member
At least every 90 days
Nursing Facility (NF) member
At least every 180 days
Acute Care Only members –
may be phone contact but on-site visit required
at least once a year
At least every 90 days for home based
members
At least every 180 days for institutionalized
members*
Developmentally Disabled (DD) members 12
years or older residing in a group home, unless
the member is medically involved or Seriously
Mentally Ill/Severely Emotionally Disabled
(SMI/SED)
At least every 180 days*
*The “Next Review Date” on the CA161/Placement Maintenance screen in Client Assessment Tracking System
(CATS) will be calculated at 90 days for these members.
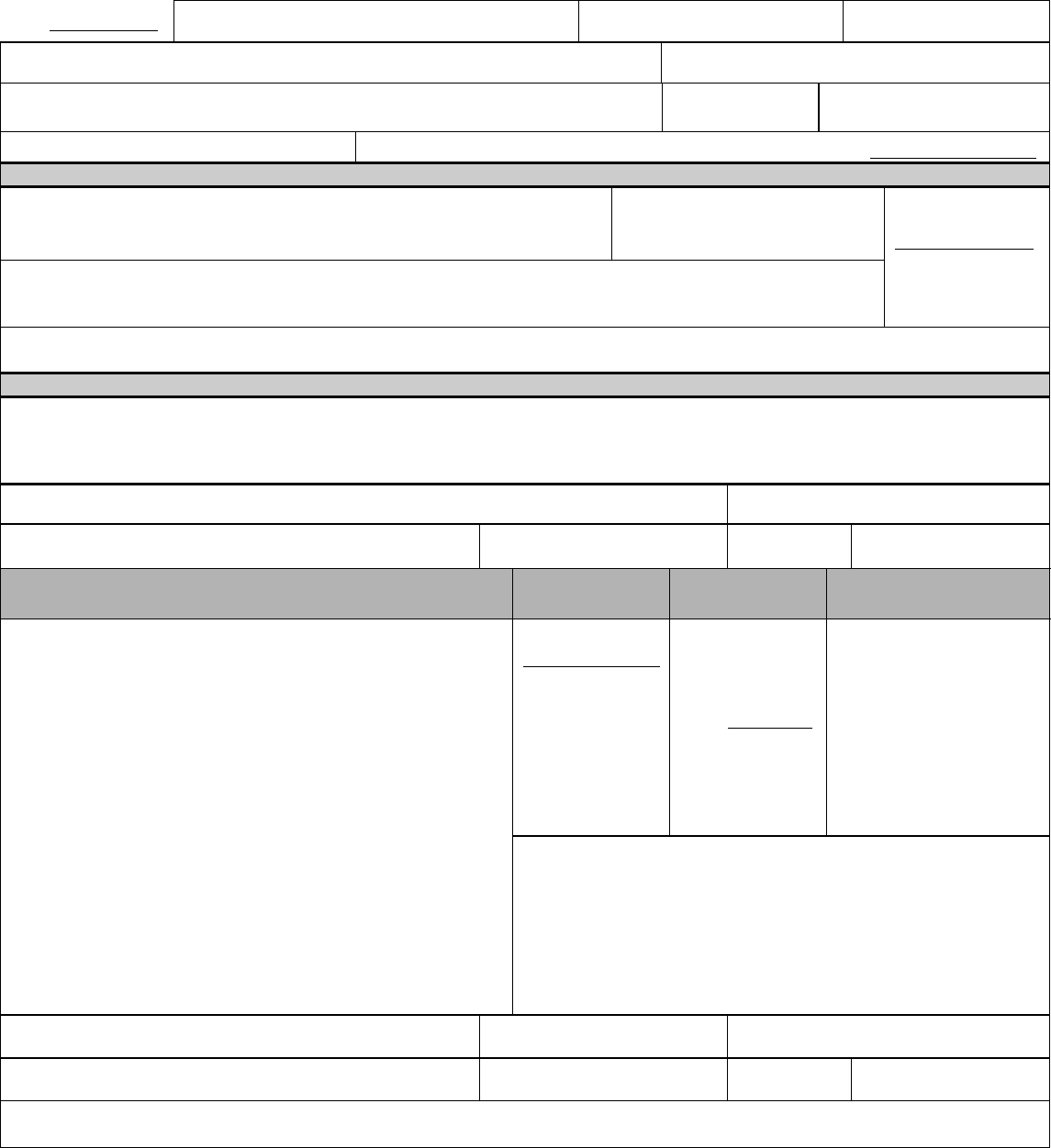
EXHIBIT 1620-2
ARIZONA LONG TERM CARE SYSTEM (ALTCS) MEMBER CHANGE REPORT
Date / /
ALTCS Contractor:
Reported By:
Phone #:
MEMBER NAME:
AHCCCS ID:
Sent To:
❑ ALTCS Local Office ❑ DHCM ❑ Medical QC Supervisor
DOB:
Customer #:
Verification Attached? ❑ YES ❑ NO
Verification Type: ❑ DE-130 ❑ Case Notes ❑ Other: ___
PART I - DEMOGRAPHIC/MISCELLANEOUS (SEND DE-701 TO ALTCS LOCAL OFFICE)
❑ Address Change:
❑ Residential ❑ Move to Home in Different Fiscal County
❑ Mailing ❑ Move Out of State
For: ❑ Representative
❑ Member
Effective Date:
/ /
❑ Name
❑ Sex
❑ DOB
❑ Phone #
❑ SSN
❑ DOD
❑ Other:
Explain Change:
PART II - PLACEMENT/LIVING ARRANGEMENT (SEND DE-701 TO ALTCS LOCAL OFFICE)
FROM: (previous residence) Enter facility name (if applicable), address and phone number. TO: (new residence) Check living
arrangement. (Abbreviations in parentheses are used by the ALTCS local offices). Effective date: Indicate effective date of change.
Length of Stay: Indicate length of stay and if temporary, enter date. Facility Status: Check facility Status (if applicable). Enter facility
name (if applicable), address, phone number. Enter comments.
FROM:
Phone: ( )
Address:
City:
State:
Zip Code:
TO: LIVING ARRANGEMENT
EFFECTIVE
DATE:
LENGTH OF
STAY:
FACILITY STATUS:
❑ NF/ICF
❑ Home
/ /
❑ Permanent
❑ Medicare Certified
❑ Not Medicare Certified
❑ Adult Foster Care Home *
❑ Assisted Living Home *
❑ Temporary
Until: / /
❑ Licensed
❑ Assisted Living Center *
❑
❑ Unknown
❑ Unlicensed
❑ Behavioral Health Residential
❑ Behavioral Health Supportive Home
❑ Contracted with PC
❑ Not Contracted with PC
❑ DD Group Home/Adult Developmental
Home
NOTE TO LOCAL OFFICE:
❑ Child Developmental Foster Home/Large Group Setting
To change from Acute to LTC call the Technical Service Center
in addition to entering the change in ACE.
❑ Alternative Acute Living Arrangement
❑ Loss of Contact
❑ Other _____________________________________
*If not registered with AHCCCS or licensed by ADHS or OBHL,
use Alternative Acute Living Arrangement.
Facility Name:
Provider ID:
Phone: ( )
Address:
City:
State:
Zip Code:
Comments:
DE-701 Revision Date: 01/01/16, 10/01/13, 01/01/12, 01/01/11, 10/07, 7/04 Review Date: 05/01/2012
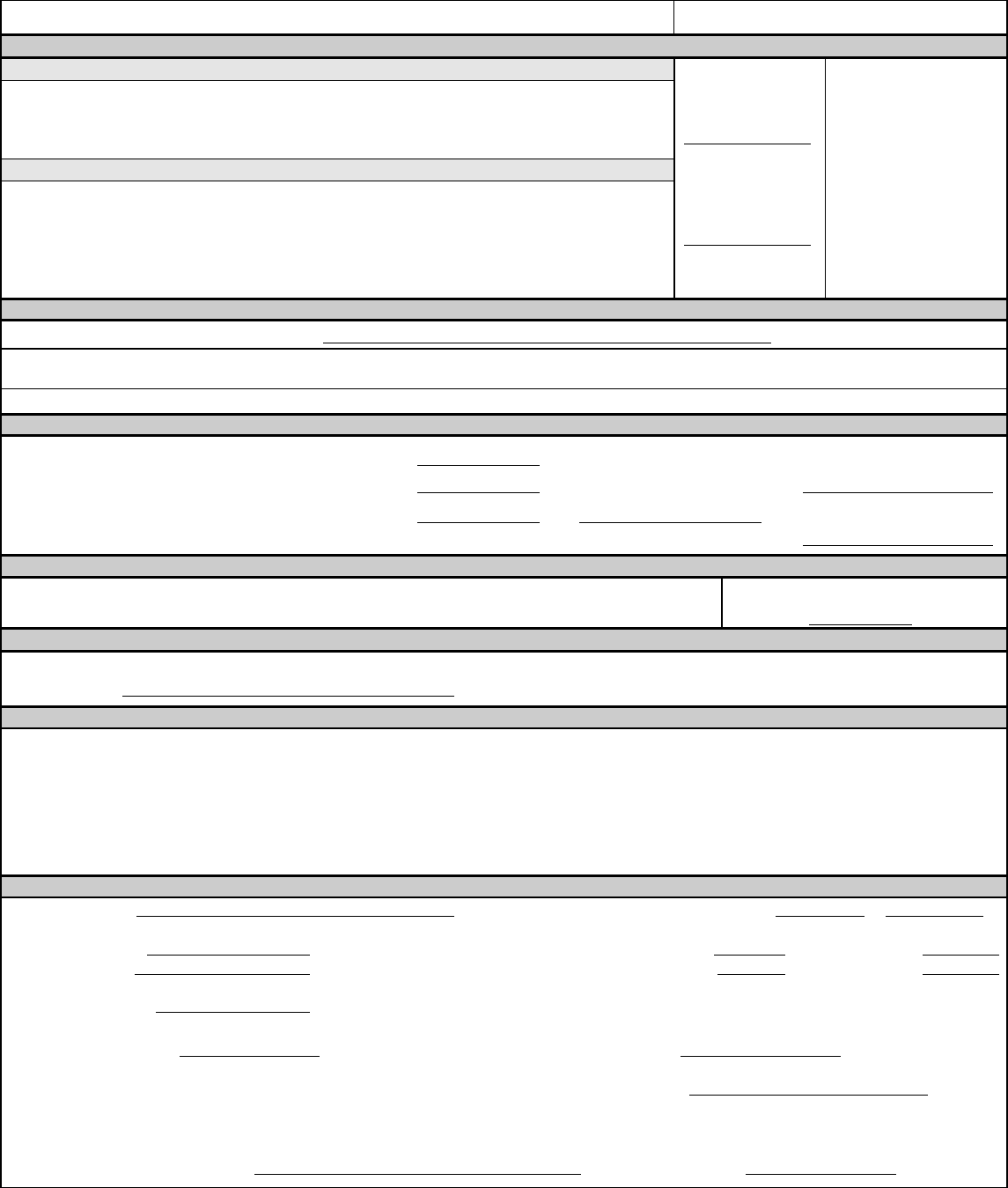
EXHIBIT 1620-2
ARIZONA LONG TERM CARE SYSTEM (ALTCS) MEMBER CHANGE REPORT
MEMBER NAME:
AHCCCS ID:
PART III - CLIENT STATUS
SEND THE DE-701 TO THE ALTCS LOCAL OFFICE TO REPORT THE FOLLOWING CHANGES:
Comments:
Member requests voluntary withdrawal from ALTCS (DE-130 attached)
Change Contract Type from LTC to Acute for retroactive period (refusing services)
Temporarily Absent from Arizona Returned to Arizona
Tribal Enrollment Change – DHCM was contacted On-Reservation Off-Reservation
Date From:
/ /
SEND THE DE-701 TO DHCM FOR THE FOLLOWING CHANGES:
From LTC to Acute– (Attach case notes)
Services not available Temporarily out of service area
Refusing Services (DE-130 not signed)
From Acute to LTC
Services are available No longer out of service area
No longer Refusing Services
Date To:
/ /
PART IV - CHANGE PC WITHIN MARICOPA COUNTY (SEND DE-701 TO ALTCS LOCAL OFFICE)
Member Requests Enrollment Change to: ( Contractor)
REASON:
Erroneous Information/Error Family Continuity Lack of Choice Continuity of Placement
COMMENTS:
PART V - MEDICARE/OTHER HEALTH INSURANCE (SEND DE-701 TO ALTCS LOCAL OFFICE)
Medicare Part A YES NO
Effective Date: / /
Medicare Number:
Medicare Part B YES NO
Effective Date: / / Disenrollment Date:
Other Insurance YES NO
Effective Date: / /
/ /
Policy Number:
INSURANCE CARRIER:
PART - SHARE OF COST (SEND DE-701 TO ALTCS LOCAL OFFICE)
Reduce Share of Cost Due to Death of Member
Effective: Month/Year
/
Other (Specify):
PART VII - INCOME/RESOURCE CHANGE (SEND DE-701 TO ALTCS LOCAL OFFICE)
Income Resources
Explain the change:
Source or Type:
PART VIII - VENTILATOR STATUS CHANGE/PAS REASSESSMENT REQUEST (SEE FORM INSTRUCTIONS)
Ventilator Dependent Non-Ventilator Dependent Effective date: ___________________
PAS Reassessment Request – Check Reason for Assessment and provide comment
Improvement in functional abilities or medical condition to the extent that the member may no longer be medically eligible. Explain the change
in comments.
Transitional member now in NF; expected to exceed 90 days: (Complete Part II)
Other (Explain):
Comments:
RESPONSE - (COMPLETED BY AHCCCS EMPLOYEE)
Refer to Part(s)
Change Completed
Date Completed / /
Effective Date / /
Member no longer eligible
Effective Date / /
Contract Type Change from to
Begin date ____________ End date ___________
SOC increased to $ Effective Date: / /
SOC decreased to $ Effective Date: / /
Income Changed
Resources Changed
Failed PAS
Other Reason
Member still eligible
Passed PAS Reassessment
Member eligible for acute care only
Effective Date / /
ALTCS Acute care
Health Plan
DHCM has determined LTC status should continue
No Action Taken (see comments)
Comments:
Signature of AHCCCS Staff Person
Date Returned / /
DE-701 Revision Date: 01/01/16, 10/01/13, 01/01/12, 01/01/11, 10/07, 7/04 Review Date: 05/01/2012
EXHIBIT 1620-2
ARIZONA LONG TERM CARE SYSTEM (ALTCS) MEMBER CHANGE REPORT
GUIDELINES ON WHEN TO USE A MEMBER CHANGE REPORT FORM
Revision Date: 01/01/16, 10/01/13, 01/01/12, 01/01/11, 10/07, 7/04 Review Date: 05/01/2012 1
An electronic Member Change Report (MCR) should be sent to AHCCCS to report or request the
following:
To report a change in the member’s demographic data (for example, address, marital status,
name change, etc.).
To report a change in the member’s financial status (or that of his/her household) which may
affect their Arizona Long Term Care System (ALTCS) eligibility, including the initiation of
the member’s spouse as the paid caregiver.
To report a change in an ALTCS member’s placement.
To report a change in the member’s DDD status and request a Pre-Admission Screening
(PAS) reassessment.
To report the closure of a member’s service plan for reasons other that financial or medical
eligibility (for example, the member dies, moves out of the state, or voluntarily withdraws
from the program).
To initiate a Contractor change for a member who is Elderly and/or has Physical Disabilities
(E/PD) when the member moves into another Contractor’s service area in a Home and
Community Based (HCB) setting (does not include alternative residential settings).
To request a PAS reassessment when the case manager thinks the member no longer meets
medical eligibility criteria for either the ALTCS or Transitional programs.
To request a PAS reassessment if a Transitional eligible member has a deterioration of
condition and will be/has been admitted to a nursing home or Intermediate Care Facility
(ICF) and is expected to stay more than 90 continuous days (this request must be sent within
45 days of admission to the institutional setting).
To request an Acute Care Only determination for a member who has received no Long
Term Care (LTC) services for a full calendar month because s/he refuses ALTCS covered
services but s/he has not signed a Voluntary Withdrawal. “Refusing” includes being
unwilling or unavailable to receive services offered or covered by the Contractor (examples:
members is not home whenever provider comes to deliver care, member unwilling to move
out of non-contracted alternative residential setting or member temporarily out of
contractor’s service area). This determination could result in the member being disenrolled
from ALTCS if his/her income exceeds 100% of the Federal Benefit Rate.
To request a change in a member’s status from Acute Care Only back to full LTC when the
member begins to accept LTC services.
To request a change in Contract Type when a member has received no LTC services for a
full calendar month, due to no LTC service provider being available. This change will not
cause a member to be disenrolled.
EXHIBIT 1620-2
ARIZONA LONG TERM CARE SYSTEM (ALTCS) MEMBER CHANGE REPORT
GUIDELINES ON WHEN TO USE A MEMBER CHANGE REPORT FORM
Revision Date: 01/01/16, 10/01/13, 01/01/12, 01/01/11, 10/07, 7/04 Review Date: 05/01/2012 2
To inform ALTCS when a member is temporarily out-of-state (>30 days).
For Maricopa County E/PD members only – to report the member’s request to change
Contractors and the need for an enrollment choice.
To report loss of contact with the member.
NOTE – Members who are temporarily out of the Contractor’s service area
including out of state, may be provided with LTC services if these are available, in the
member’s best interests and are approved by the contractor. No AHCCCS services may
be provided while a member is outside of the United States.
A hard copy MCR may be needed if, at the time of submission, the member is no longer enrolled
with the Contractor that is attempting to send the report.
EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
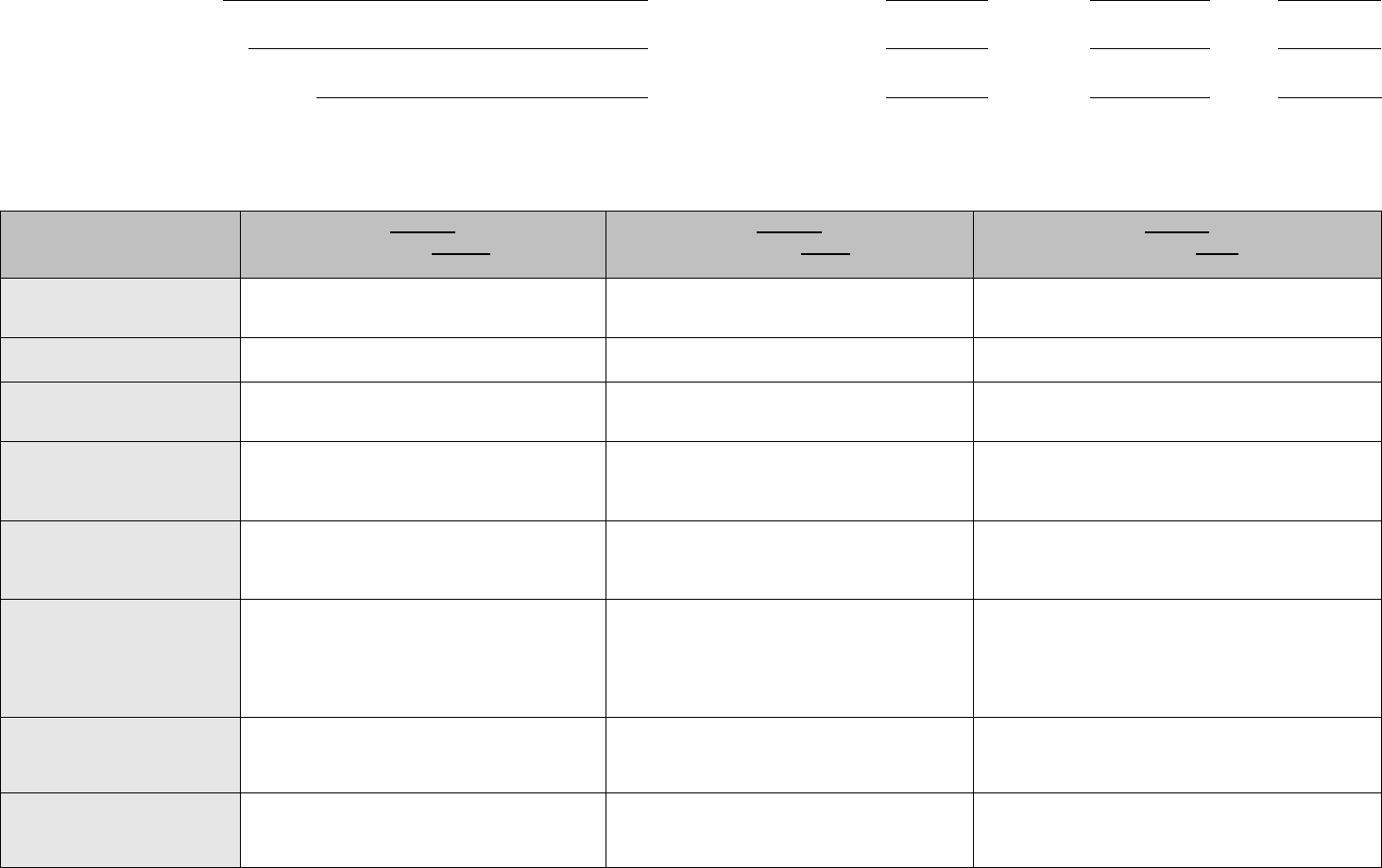
EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
Revision Date: 01/01/16
MEMBER NAME:
REVIEW DATE:
CLASS
CM:
DETERMINED CLASS:
REVIEW DATE:
CLASS
CM:
DATE CLASS DETERMINED:
REVIEW DATE:
CLASS
CM:
Acuity determinations are based on this UAT matrix which describes characteristics of clients in each level. Information will be gathered through assessment of the client,
interview with nursing facility staff, and medical record review, with particular attention to documentation regarding the past 30 days and updates within the MDS. If the CM is
uncertain regarding client’s level of care, he/she will review case with their manager.
CLASS 1
CLIENT HAS THREE OR
MORE OF THE FOLLOWING
CLASS 2
CLIENT HAS FOUR OR
MORE OF THE FOLLOWING:
CLASS 3
CLIENT HAS FIVE OR
MORE OF THE FOLLOWING:
BATHING, DRESSING,
GROOMING
Independent or may participate in care, but
requires assistance with bathing, dressing, and/or
grooming.
Requires moderate assistance with bathing,
dressing, and/or grooming.
Requires maximum assistance with bathing, dressing,
and grooming.
FEEDING/
EATING
Independent or requires minimum set
up/prompting assistance with feeding/eating.
Requires moderate assistance with feeding/eating.
Requires maximum assistance with feeding/eating (for
example, tube feeding).
MOBILITY
Independent or requires minimum or stand by
assistance to move from one location to another
with or without assistive devices.
Requires moderate assistance to move from one
location to another with or without assistive
devices.
Requires maximum assistance to move from one
location to another with or without assistive devices.
TRANSFERRING
Can transfer to some or all surfaces
independently. Requires the assistance of no
more than one person to transfer from one surface
to another with or without assistive devices.
Requires hands-on physical guidance or assistance
of one person for all transfers with or without
assistive devices. The client may participate by
being able to bear weight and pivot.
Requires assistance of two or more people to be
physically lifted or moved from one surface to another
with or without assistive devices.
BOWEL/
BLADDER
Continent or occasionally incontinent (less than
seven times per week) of bowel and/or bladder or
may be continent at times with a training program.
Moderately (daily but some control) incontinent of
bowel and/or bladder
Totally incontinent of bowel and/or bladder, receives
scheduled toileting on a daily basis to avoid
incontinence and/or receives care of a catheter or
ostomy.
ORIENTATION/
BEHAVIOR
Requires no intervention or requires minimum
staff intervention for episodes of confusion,
memory deficits, impaired judgment, or agitation.
May require temporary (24 hours or less)
restraints to control a behavioral or medical
problem and restraints for personal safety.
Requires moderate staff intervention. May have
periodic emotional or mental disturbances,
including combativeness.
Requires maximum staff intervention. May be
disoriented, confused, combative, withdrawn, or
depressed. May need restraints (physical/chemical) for
personal safety or protection of others.
MEDICAL CONDITIONS
Stable, with no or some routine nursing/medical
monitoring and care.
Conditions require more frequent monitoring to
maintain stability (for example, unstable
hypertension needing frequent assessment and
medication adjustment).
Conditions require intense professional intervention to
maintain stability (for example, unstable diabetes, come,
terminal medical condition).
MEDICAL/
NURSING
TREATMENTS
None or routine, such as range of motion and
injections, as well as routine medication
administration and routine catheter care.
6BANYTHING MORE WOULD COUNT UNDER CLS 2
Skilled nursing treatment in addition to routine
medication administration. (Such as a treatment for
skin condition.)
Relatively complex, with more than one professional or
technical treatment, such as IV therapy, tube or parenteral
feeding, care of recent wound, care of infected or stage 4
decubitus, deep suctioning or an extensive rehab regime.
For ADLs: Minimum means some or less than half of the task, moderate means approximately one-half to less than three-quarters of the task, and maximum means extensive or
approximately three-quarters of the task or more.
EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
GUIDELINES FOR THE USE OF THE UNIFORM ASSESSMENT TOOL
Revision Date: 01/01/16 1
I. PURPOSE
The purpose of the Uniform Assessment Tool (UAT) is to assess the acuity of Nursing Facility
(NF) residents. The UAT will also be used on HCBS members when determining the institutional
rate to use when developing a Cost Effectiveness Study.
The use of the UAT is not intended to impact how Contractors determine authorizations for
specialty levels of care (for example, wandering dementia and medical sub-acute).
II. DEFINITIONS
The following definitions apply for most situations. Exceptions are noted within this document and
on the UAT.
1. Minimum = means less than half the task.
2. Moderate = means approximately 50% to less than 75% of the task.
3. Maximum = means extensive or approximately 75% of the task or more.
III. ASSESSMENT CATEGORIES
The following information is for the purpose of assisting the case manager in completing the UAT.
The information that follows is not intended to be all-inclusive. Case managers should consult with
their supervisor/manager when a Characteristic does not clearly fall within a specific level.
The UAT is made up of eight Characteristics:
1. Bathing/Dressing/Grooming
2. Feeding/Eating
3. Mobility
4. Transferring
5. Bowel/Bladder
6. Orientation/Behavior
7. Medical Condition
8. Medical/Nursing Treatment
Each Characteristic is assessed for one of three acuity levels. The cumulative levels determined for
each Characteristic will determine the overall Class level for the member (Class 1, Class 2 or Class 3).
A single UAT form is designed to allow the case manager to document up to four assessments. The
case manager shall document the assessment-related date in the box associated with a Characteristic’s
determined acuity. When the eight Characteristics are assessed, determine the Class level as
summarized on the UAT. Finally, document, at the top of the tool, the review date, Class and the case
manager’s initials. The first assessment is documented in the upper left corner. Subsequent assessments
would be documented in the upper right corner.

EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
GUIDELINES FOR THE USE OF THE UNIFORM ASSESSMENT TOOL
Revision Date: 01/01/16 2
A. BATHING/DRESSING/GROOMING
Bathing - the process of washing, rinsing and toweling the body or body parts and transferring in/out
of the tub or shower. This includes the ability to get the bath water and/or equipment, whether this is
in bed, tub, shower, or sink. Use of assistive devices such as tub/shower chair, pedal/knee controlled
faucets, or long-handled brushes does not disqualify the client from being independent. If the client
has a problem getting to and from the bathroom to bathe, that should be reflected in the Mobility
section and should not affect the score for bathing.
Assessment Considerations:
1. When taking a bath/shower, can the person get their own towel, washcloth, soap, and run the
water?
2. Can the person tell if the water is too hot or too cold?
3. Is the person able to get in and out of the shower or tub by themselves?
4. Does the person need a bath bench, shower seat or hand held shower to assist with bathing?
5. What kind of problems does the person have with bathing him/herself?
Minimum = the client requires up to minimal supervision, verbal cueing, assistance in and/or out of
the shower, and may need assistance with washing back or lower extremities.
Moderate = the client requires step by step cueing with the entire bathing process, one person assist
getting in and out of the tub/shower, and/or hands-on assistance with approximately 50% to 75% of
the bathing process.
Maximum = the client is dependent on others for assistance with approximately 75% or more of the
bathing process or requires assistance of two or more persons to get in and out of shower/tub or
requires the use of a Hoyer lift.
Dressing - dressing includes laying out, putting on and fastening of clothing and footwear. Use of
assistive devices such as reachers, sock pullers, shoe horns, Velcro fasteners does not disqualify the
client from being independent.
Assessment Considerations:
1. Can the person choose their own clothes, get them from the closet or drawer, put them on and
button the buttons, fasten/close the zipper or tie their shoes?
2. If someone lays out the clothes, can the person put them on?
3. Does the person have assistive devices to assist in dressing, such as reachers, sock pullers,
shoe horns, Velcro fasteners?
4. How does the person get dressed if help is needed?
Minimum = the client may need some supervision or reminding (for example, laying out clothes,
giving advice or being available.

EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
GUIDELINES FOR THE USE OF THE UNIFORM ASSESSMENT TOOL
Revision Date: 01/01/16 3
Moderate = the client required hands-on physical assistance of another person or supervision with
approximately 50% to 75% of the dressing activities.
Maximum = the client needs assistance with dressing approximately 75% or more of the time.
Grooming - grooming activities include combing hair, shaving, brushing teeth, washing hands/face,
nail care and/or menses care. Obtaining the water and supplies necessary to complete the task are
included in grooming.
Assessment Considerations:
1. Can the person run the sink water and wash their face, comb their hair and brush their teeth?
Minimum = the client needs up to minimal supervision or reminding (for example, setting up
grooming implements, giving advise, being available, menses care.
Moderate = the client requires some physical assistance or supervision or step by step cueing with
approximately 50% to 75% of their grooming activities.
Maximum = the client is dependent on others for assistance with approximately 75% or more of their
grooming activities.
B. EATING/FEEDING
Eating/Feeding – the process of getting nourishment by any means from a receptacle (dish, plate,
cup, glass, bottle, etc.) into the body. Use of mechanical aids such as modified utensils or plate
guards does not disqualify the client from being independent.
Assessment considerations:
1. Can the person effectively get food and beverages into his/her mouth?
2. Can the person cut his/her own meat?
3. Does the person use any mechanical aids to assist with eating?
4. Is the person receiving an intravenous or tube feeding as a means of total nutrition?
5. Does the person need cueing or supervision to ensure an adequate intake?
Minimum = client requires some supervision, reminding, set-up or cutting, including alteration of
food (for example, pureeing) or hands-on assistance with less than half of the meal task.
Moderate = client requires hands-on physical assistance, cueing or reminding with approximately
50% to 75% of the meal task, but can participate physically.
Maximum = client requires hands-on physical assistance with approximately 75% or more of the
meal task or is totally dependent for nutritional needs (for example, tube feeding or TPN).

EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
GUIDELINES FOR THE USE OF THE UNIFORM ASSESSMENT TOOL
Revision Date: 01/01/16 4
C. MOBILITY
Mobility – the extent of the client’s purposeful movement within their residence. The use of assistive
devices such as a wheelchair, walker or quad cane does not disqualify the person from being
independent.
Assessment Considerations:
1. Can the person purposely move about in his/her current environment independently?
2. Does the person have an unstable gait or balance?
3. Could the person avoid an obstacle in his/her path?
4. Does the person use any assistive devices such as a cane, walker, wheelchair or handrails?
5. Is the person unsafe without the assistance of another person in ambulating?
Minimum = approximately 50% or less of the time the client requires supervision, standby or
hands-on assistance by one person for safety, including adjustment of assistive devices or restraints.
Moderate = approximately 50% to 75% of the time the client requires supervision, standby
assistance or hands-on assistance of one person, including adjustment of assistive devices or
restraints.
Maximum = approximately 75% or more of the time the client requires hands-on assistance of one or
more persons or may be totally dependent on others for mobility (for example, cannot self-propel
wheelchair).
D. TRANSFERRING
Transferring – the client’s ability to move horizontally and/or vertically between the bed, chair,
wheelchair, commode, etc.
Assessment Considerations:
1. Can the person move horizontally or vertically between the bed, chair, wheelchair or
commode independently?
2. Does the person display any weakness or unsteady balance, which would require assistance
when transferring?
3. Does the person use any mechanical devices such as a walker, cane, handrails or wheelchair
to assist with transfers?
4. Can the person physically participate in the transfer by pivoting, holding on, or bracing
themselves to assist the caregiver?
Minimum = can transfer to some or all surfaces independently. If needed, the assistance of no more
than one person to transfer from one surface to another with or without assistive devices. The client
may require some supervision or reminding or standby assistance for safety.
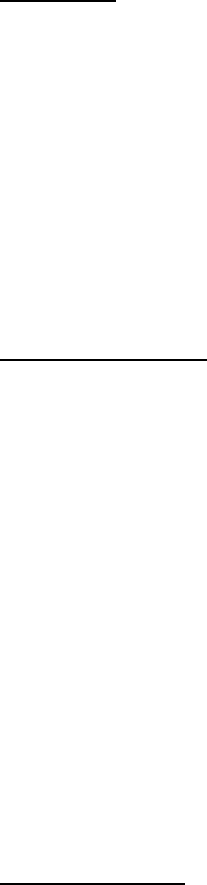
EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
GUIDELINES FOR THE USE OF THE UNIFORM ASSESSMENT TOOL
Revision Date: 01/01/16 5
Moderate = the client requires hands-on physical guidance or assistance of one person for all
transfers. The client may participate by being able to bear weight and pivot.
Maximum = the client requires assistance of two or more people to be physically lifted or moved.
E. BOWEL/BLADDER CONTINENCE
Continence – the ability to voluntarily control the discharge of body waste from bladder or bowel.
Incontinence means the involuntary loss of bowel and bladder contents. Stress incontinence means
the inability to prevent escape of small amounts of bowel/bladder contents during certain activities
such as coughing, lifting or laughing.
Those who willfully toilet in inappropriate places will not necessarily be assessed as being
incontinent. These behaviors may be assessed in other parts of this instrument (for example,
Behaviors). Those who receive dialysis and do not urinate will be rated as continent of bladder.
Clients who have no voluntary control secondary to physiological conditions and rely upon dilatation,
indwelling catheters, intermittent catheterization, ostomies, condom catheters or placed urinals for
evacuation should be rated as totally incontinent in the applicable function.
Bladder Continence – the ability of the client to voluntarily control the discharge of body wastes
from the bladder. A client with a Foley catheter or ostomy will be scored maximum.
Assessment Considerations:
1. Does the person have any episodes of incontinence?
2. Can the person “hold their urine” until they get to the toilet?
3. Does the person have accidents when they sneeze or cough?
4. How frequently does the person have accidents – once or twice a week, every day, once a
month?
Minimum = the client may be incontinent less than seven times a week.
Moderate = the client may be frequently incontinent or incontinent daily, but some control is present
(for example, daytime, or if toileted frequently).
Maximum = the client is totally incontinent of bladder, receives scheduled toileting on daily basis to
avoid bladder incontinence and/or receives care of a catheter or ostomy.
Bowel Continence - the ability of the client to voluntarily control the discharge of body wastes from
the bowel. A client with an ostomy will be scored maximum.
Assessment Considerations:
1. Does the person have bowel accidents?
2. Does the person ever soil their clothing?

EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
GUIDELINES FOR THE USE OF THE UNIFORM ASSESSMENT TOOL
Revision Date: 01/01/16 6
3. How often does the person accidents?
Minimum = the client may be continent less than seven times per week.
Moderate = the client may be frequently incontinent (seven times or more per week) or incontinent
daily, but some control is present.
Maximum = the client has no voluntary control of bowel and/or receives care of an ostomy.
F. ORIENTATION/BEHAVIOR
Behavior – identify the presence of certain behaviors that may reflect the level of an individual’s
emotional functioning and need for intervention. Behaviors should be assessed based on the last 90
days (with particular attention to the past 30 days), or since the last review. Documentation should
include frequency and type of behavior and if there has been or will be a request for mental health
services.
Wandering is defined as moving about with no rational purpose and with a tendency to go beyond
physical parameters of the environment in a manner that may jeopardize safety of self or others.
Repeated behaviors that cause injury to self (for example, biting scratching, picking behaviors;
putting inappropriate objects into the ear, mouth or nose; head slapping or banging) or others (for
example, physically attacking another person, throwing objects, punching, biting, pushing, pinching,
pulling hair and physically threatening behavior).
Other repeated behaviors that interferes with the activities of others or the individuals own activities:
for example, putting on or removing clothes inappropriately, stubbornness, sexual behavior
inappropriate to time, place or person, excessive crying or screaming, persistent pestering or teasing;
constantly demanding attention and urinating or defecating in inappropriate places, or threats and or
attempts to take one’s own life.
Minimum = requires staff intervention less than 50% of the time for episodes of confusion, memory
defects, impaired judgment, or agitation. May require temporary (24 hours or less) restraints to
control a behavioral or medical problem and restraints for personal safety.
Moderate = requires staff intervention approximately 50% to 75% of the time for episodes of
confusion, memory defects, impaired judgment, or agitation. May have periodic emotional or mental
disturbances, including combativeness.
Maximum = requires staff intervention approximately 75% or more of the time. May be disoriented,
confused, combative, withdrawn, or depressed. May need restraints (physical/chemical) for personal
safety or protection of others.

EXHIBIT 1620-3
UNIFORM ASSESSMENT TOOL AND GUIDELINES
GUIDELINES FOR THE USE OF THE UNIFORM ASSESSMENT TOOL
Revision Date: 01/01/16 7
G. MEDICAL CONDITION
Medical Condition – refers to the degree of stability of health care needs that may require nursing
and/or medical monitoring of treatment(s) and/or therapy to restore and/or maintain function. This
does not include maintenance regimens (monthly weights and blood pressure checks).
Minimum = stable, with routine nursing/medical monitoring and care.
Moderate = conditions require more frequent professional monitoring to maintain stability (for
example, unstable hypertension needing frequent assessment and medication adjustment).
Maximum = conditions require intense professional intervention to maintain stability (for example,
unstable diabetes, coma, terminal medical conditions).
H. MEDICAL/NURSING TREATMENTS
Medical/Nursing Treatments – refers to level of nursing and/or medical care that is required to
perform medical assistance and interventions with current health care needs.
Minimum = Routine treatments, such as range of motion and injections, as well as routine
medication administration and routine catheter care. Anything more would be considered at least
“moderate”.
Moderate = Skilled nursing treatment in addition to routine medication administration (for example,
treatment of stage one to three pressure ulcer, tube feeding).
Maximum = Relatively complex, with more than one professional or technical treatment, such as IV
therapy, tube or parenteral feeding, care of recent wound, care of infected or stage 4 pressure ulcer,
deep suctioning or an extensive rehab regimen.
EXHIBIT 1620-4
ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
EXHIBIT 1620-4
ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
Revision Date: 01/01/16, 01/01/11 1
A. Members should be placed in a “D” placement in the following situations:
1. The member has refused both institutional and/or Home and Community Based
(HCB) services but does not wish to withdraw from the program. “Refused” includes
circumstances where the member/representative is unavailable or unwilling to receive
services offered by the Contractor.
2. The member receives no Long Term Care (LTC) services because a provider for the
service(s) requested/needed is not available in the member’s area.
3. The member resides in an Alternative Residential Setting that is not contracted with
the member’s Contractor, or in Maricopa County is not contracted with any available
Contractors and s/he does not want to move.
4. The member resides in an Alternative Residential Setting that is not registered with
AHCCCS and s/he does not want to move.
5. The member is not eligible for full LTC benefits due to an uncompensated transfer of
resources/property. A member under these circumstances will be approved by
AHCCCS as Acute Care Only (ACO) at the time of enrollment.
6. The member receives no services, has signed a Voluntary Discontinuance and is
pending disenrollment.
7. The member resides in an uncertified nursing facility.
8. The member and/or member’s guardian refuses to comply with the review visit
requirements.
B. “D” placements are generally for a full calendar month only. See exceptions to this rule in
case examples #5, #7 and #9-10 to follow.
C. If HCB services are provided to the member for any portion of a month, that member should
be in an “H” placement code for the entire calendar month.
D. “Q” placement begin and end dates however, must match the actual date of admission and/or
discharge. This is because member Share of Cost is assessed based on date of admission
and/or discharge.
E. Placements do not need to be changed to “D” when a member is hospitalized and not
receiving LTC services for a full calendar month. The placement code should remain the same
as it was prior to hospitalization until it is known what placement member will be discharged
to.
F. Member Change Reports (MCR) should be submitted electronically for changes of member
status from LTC to ACO as well as ACO back to LTC.
EXHIBIT 1620-4
ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
Revision Date: 01/01/16, 01/01/11 2
G. MCRs are sent electronically after at least one full calendar month has passed in which no
LTC services were provided.
H. MCRs for changes from LTC to ACO must be sent electronically with adequate information
to describe the reason for the change.
I. Members whose income is greater than 100% of the current Federal Benefit Rate will not be
eligible for ALTCS if/when they refuse LTC services. Case managers should advise members
who refuse LTC services of the possibility of disenrollment
J. MCRs sent must indicate the effective date(s) of ACO (at least the begin date of this status)
and the reason for change (Refusing Home and Community Based Services [HCBS] or
Services Not Available).
K. The “D” placement code dates on CA161/Placement Maintenance must match the dates
indicate on the MCR.
L. AHCCCS capitates E/PD Contractors at a lower rate for all days that any member is in a “D”
placement. AHCCCS will recoup funds for all members in “D” placement for whom the E/PD
Contractor has received full LTC capitation.
CASE EXAMPLES:
1. Member enrolls on 4/03. Case manager conducts on-site visit and HCBS begin on 4/17.
“H” placement begins on the date LTC services begin following initial contact.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
Z
1
11
4/03
4/16
H
1
13
4/17
2. Member enrolled on 1/15with HCBS in place. Member stops receiving HCBS on 5/25.
Member begins to receive HCBS again on 6/19. This member’s placement will remain
“H” since the member received LTC services at home in both May and June.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
H
1
13
1/15
EXHIBIT 1620-4
ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
Revision Date: 01/01/16, 01/01/11 3
3. Member enrolled on 1/15with HCBS in place. Member stops receiving HCBS on 5/25. As
of 6/30, the member is still not receiving any LTC services. Case manager should change
placement code to “D” beginning 6/01and send MCR indicating change from full LTC to
ACO effective 6/01with no end date.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
H
1
13
1/15
5/31
D
1
12
6/01
4. Member enrolled on 1/15 with HCBS in place. Member stops receiving HCBS on 5/25.
As of 6/30, the member is still not receiving any LTC services. Case manager should
change placement code to “D” beginning 6/010 and send MCR indicating ACO effective
6/01 with no end date.
Member then begins to receive HCBS on 7/20. Case manager should change placement
code to “H” beginning 7/01and send another MCR indicating change from ACO back to
full LTC effective 7/01.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
H
1
13
1/15
5/31
D
1
12
6/01
6/30
H
1
13
7/01
5. New member enrolls on 7/13with no services in place. Case manager completes on-site
assessment on 7/20 and member declines any LTC service. Member should be in a “Z”
placement beginning 7/13. After 30 days, the member’s placement code should be changed
to “D” if no LTC services have begun. If the member has still not received LTC services
by the end of the calendar month, case manager should send MCR indicating change from
full LTC to ACO effective 8/13 (the 31st day after enrollment) with no end date.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
Z
1
11
7/13
8/12
D
1
12
8/13
EXHIBIT 1620-4
ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
Revision Date: 01/01/16, 01/01/11 4
6. New member enrolls on 7/13with no services in place. Case manager completes on-site
assessment on 7/20 and member begins to receive HCBS on 8/26. This member’s
placement can be changed to “H” beginning on the 1st of August since LTC HCBS services
were provided within the month of August.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
Z
1
11
7/13
7/31
H
1
13
8/01
7. New member enrolls on 7/13with no services in place. Case manager completes on-site
assessment on 7/20and member declines any LTC service. Member should be in a “Z”
placement beginning 7/13. After 30 days, the member’s placement code should be changed
to “D” if no LTC services begun. If the member has still not received LTC services by the
end of the calendar month case manager should send MCR indicating change from full
LTC to ACO effective 8/13(the 31st day after enrollment) with no end date.
Member then begins to receive HCBS on 9/13. Case manager should change placement
code to “H” beginning 9/01and send MCR indicating change from ACO back to full LTC
effective 9/01.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
Z
1
11
7/13
8/12
D
1
12
8/13
8/31
H
1
13
9/01
8. Member enrolled 5/13residing in an ALF that is not contracted with the Contractor. As
long as the ALF is licensed by ADHS and registered with AHCCCS, the member will be
enrolled as full LTC benefits even though it is not contracted. If the facility is not
contracted with another PC in the area, or there is no other PC in the area, and the member
refuses to move, an MCR should be sent indicating a change from LTC to ACO (refusing
LTC services) effective 5/13.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
D
*1
12
5/13
*Residence code(s) for Assisted Living Facilities (B, 5, 9, etc.) can not be combined with “D” placement so
must use (1) as
above.
EXHIBIT 1620-4
ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
Revision Date: 01/01/16, 01/01/11 5
9. Member enrolled 5/13 residing in an ALF that is not contracted with the Contractor. As
long as the ALF is licensed by ADHS and registered with AHCCCS, the member will be
enrolled as full LTC benefits even though it is not contracted. If the facility is not
contracted with another PC in the area, or there is no other PC in the area, and the member
refuses to move, an MCR should be sent indicating a change from LTC to ACO (refusing
LTC services) effective 5/13.
Member moves to a nursing facility on 6/17. MCR should be sent requesting a change from
ACO to full LTC status effective 6/17. Unlike when HCBS are provided in the calendar
month the “Q” placement does not begin at the first of that month but rather on the actual
date of admission. This is because member share of cost is assessed based on date of
admission and/or discharge.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
D
1*
12
5/13
6/16
Q
2
01
6/17
*Residence code(s) for Assisted Living Facilities (B, 5, 9, etc.) can not be combined with “D” placement so
must use (1) as
above.
10. Member enrolls on 3/19in a nursing facility placed and leaves AMA on 8/11. Case
manager is unable to locate the member until 9/09 and member agrees to HCBS that begin
on 9/18. As long as the member receives HCB services in the calendar month, the “H”
placement may begin on the 1st of that month. An MCR is needed to change the member’s
status to ACO and then back to full LTC effective 9/01 to match the placement.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
Q
2
01
3/19
8/10
D
1
12
8/11
8/31
H
1
13
9/01
EXHIBIT 1620-4
ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
Revision Date: 01/01/16, 01/01/11 6
11. Member who has been residing in a nursing facility placement leaves the facility before
HCB services are in place on 2/13. Case manager becomes aware of discharge and visits
member to set up home services on 2/16. HCB services begin on 2/18. Since member will
receive LTC services during the entire calendar month the “H” placement may begin on
2/14immediately after “Q” placement ends even though home services did not begin right
away.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
Q
2
01
3/19
2/13
H
1
13
2/14
12. Member enrolls on 4/12with ACO status due to an uncompensated transfer status will end
10/31. Regardless of member’s residence type, placement must be “D” during this time
period. Member begins receiving HCBS services on 11/03. As long as the member
receives HCB services in the calendar month the “H” placement may begin on the 1st of
that month. No MCR is necessary because the change from ACO status to full LTC status
has already been processed by the eligibility office with the end of the transfer period.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
D
1
12
4/12
10/31
H
1
13
11/01
13. Member enrolls on 4/12with ACO status due to an uncompensated transfer, status will end
10/31. Regardless of member’s residence type, placement must be “D” during this time
period. Member is admitted to a NF on 11/05. Unlike when HCBS are provided in the
calendar month, the “Q” placement does not begin at the first of the month but rather on the
actual date of admission. This is because member Share of Cost is assessed based on date
of admission and/or discharge.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
D
1
12
4/12
11/04
Q
2
03
11/05
EXHIBIT 1620-4
ACUTE CARE ONLY “D” PLACEMENT GUIDELINES
Revision Date: 01/01/16, 01/01/11 7
14. Member enrolls on 4/12with ACO status due to an uncompensated transfer, status will end
10/31. Regardless of member’s residence type, placement must be “D” during this time
period. Member begins to receive HCB services on 12/09. Since AHCCCS would not be
aware of the continuation of Acute Care status after the end of the transfer period on 10/31,
an MCR needs to be sent requesting a change from full LTC status to ACO status through
11/30.
CA 161 SCREEN:
P
LACEMENT
CODE
R
ESIDENCE
CODE
P
LACEMENT
REASON
P
LACEMENT
BEGIN DATE
P
LACEMENT
END DATE
D
1
12
4/12
11/30
H
1
13
12/01
15. Member and/or member’s guardian refuses to allow the Case manager to conduct the
required on-site visit, the Case manager should change the placement code to “D” on the
30th day following the due date of the last Case manager’s review. The Case manager
must send an MCR indicating change from full LTC to ACO with no end date.
EXHIBIT 1620-5
RESERVED
EXHIBIT 1620-6
HIGH COST BEHAVIORAL HEALTH REINSURANCE FORM
Revision Date: 01/01/16, 04/01/12, 01/01/11 Reviewed 10/01/13 1
EXHIBIT 1620-6
DIVISION OF HEALTH CARE MANAGEMENT
HIGH COST BH REINSURANCE REQUEST FORM
PAGE 1 OF 3
REQUEST/NOTIFICATION TYPE
MEMBER NAME:
AHCCCS #:
RENEWAL AUTHORIZATION
PLACEMENT CHANGE
EFFECTIVE DATE:
REASON:
TERMINATION
EFFECTIVE DATE:
REASON:
CONTRACTOR CHANGE
NEW CONTRACTOR:
EFFECTIVE DATE:
OTHER
SIGNATURE: ___________________________________ Date: _________________________
CONTRACTOR NAME: ___________________________________________________
Revision Date: 01/01/16, 04/01/12, 01/01/11 Reviewed 10/01/13 2
EXHIBIT 1620-6
DIVISION OF HEALTH CARE MANAGEMENT
HIGH COST BH REINSURANCE REQUEST FORM
PAGE 2 OF 3
MEMBER DEMOGRAPHIC INFORMATION
MEMBER NAME:
AHCCCS #:
FACILITY NAME AND TYPE:
DOB:
PLACEMENT DATE:
DAILY RATE:
DIAGNOSES
Include Psychiatric and Medical, as relevant:
CURRENT BEHAVIORAL ISSUES
Describe member’s current behaviors and the frequency and intensity of those behaviors;
FACILITY PROGRAMMING DESCRIPTION
Explain programs and activities at the facility specific to this member that assist this member in
managing inappropriate behaviors:
BEHAVIORAL TREATMENT PLAN
56B
Explain/describe behavioral and chemical interventions in place to actively manage member’s current
behavioral issues:
Revision Date: 01/01/16, 04/01/12, 01/01/11 Reviewed 10/01/13 3
EXHIBIT 1620-6
DIVISION OF HEALTH CARE MANAGEMENT
HIGH COST BH REINSURANCE REQUEST FORM
PAGE 3 OF 3
MEMBER NAME:
AHCCCS #:
PLACEMENT HISTORY
Explain why this member cannot live in a non-behavioral living arrangement and include specific
information (including dates) regarding reason (s) previous placement(s) were unsuccessful
RE-EVALUATION OF PLACEMENT
Results of periodic re-evaluation of the member’s ability to function with a lower level of
intervention than provided under current treatment plan (not just attempts at placement change).
Explain any discharge plans:
DOCUMENTATION TO INCLUDE
Behavioral Treatment Plan
Psychotropic Medication Record
Psychiatric or psychological evaluation reports
Nursing notes with behavioral issues highlighted
Facility staff notes with behavioral issues highlighted
Any other information in the member’s records that support the need for a high-cost
behavioral treatment program and specialized placement
SIGNATURE: ________________________________________ DATE: ___________________
CONTRACTOR NAME:____________________________________________________
EXHIBIT 1620-7
FEE-FOR-SERVICE (FFS) OUT-OF-STATE NURSING FACILITY
PLACEMENT REQUEST FORM
EXHIBIT 1620-7
FEE-FOR-SERVICE (FFS) OUT-OF-STATE NURSING FACILITY
PLACEMENT REQUEST FORM
Revision Date: 01/01/16, 01/01/11 Review Date: 05/01/12 Initial Effective Date 04/01/2004
SECTION A: TO BE COMPLETED BY THE CASE MANAGER
Member Name:
Tribal Contractor:
AHCCCS ID #:
Date of Birth:
Current Residence/Placement:
Diagnosis/Condition necessitating this placement:
Distance from NF to nearest family:
Level of involvement by family:
Description of facility’s program(s) that makes this placement appropriate for the member:
Information about AZ NFs ruled out for this member:
Plan for member’s return to AZ placement:
Indicate requested nursing facility:
San Juan Manor
806 W. Maple
Farmington, NM 87401
Provider ID # 841826
Four Corners Care Ctr
818 North 400 West
Blanding, UT 84511
Provider ID# 161406
Bloomfield Nursing
803 Hacienda Lane
Bloomfield, NM 87413
Provider ID# 825316
Red Rocks Care Ctr.
3720 Church Rock Rd.
Gallup, NM 87301
Provider ID# 820632
PCP Name:
AHCCCS Provider ID:
Case Manager:
Date:
SECTION B. TO BE COMPLETED BY AHCCCS
Comments:
Approved
Signature
Date
(Name and Title)
Denied
Signature
Date
(AHCCCS Medical Director or designee)
EXHIBIT 1620-8
CONTRACTOR CHANGE REQUEST FORM
EXHIBIT 1620-8
CONTRACTOR CHANGE REQUEST
Revision Date: 01/01/16, 10/00
Member/Recipient’s Name:
AHCCCS ID #:
50BI. CURRENT CONTRACTOR INFORMATION
Person Requesting Change:
Phone #:
Contractor Name:
Fiscal County Name:
Fiscal County #:
Provider ID #:
Transfer: ❑ Approved ❑ Denied
Date:
Reason:
❑ Member/Recipient Leaving Service Area
❑ Member/Recipient Resides Out of Service Area
❑ Within Service Area for Medical Continuity of Care
❑ Family Request
❑ Other – Specify:
Comments/Current Medical Condition:
(Attach Medical Release, Current Plan of Care and Other
Necessary Information)
Authorized Signature:
Title:
Date:
34BII. RECEIVING CONTRACTOR INFORMATION
Contractor Name:
Fiscal County Name
Fiscal County Number:
Provider ID #:
Transfer: ❑ Approved ❑ Denied
Effective Enrollment Date:
Authorized Signature
Title
Date
If approved, complete member/recipient information below and send this form to the AHCCCS Administration. If
request denied, return form to originator.
35BIII. MEMBER/RECIPIENT INFORMATION
Is this a change in Contractors within Maricopa County? ❑ YES ❑ NO
Is the change due to a move to a new county of fiscal responsibility? ❑ YES ❑ NO
Has the member/recipient physically moved to a new county of fiscal responsibility? ❑ YES ❑ NO
If YES, provide the new address below.
Effective Date of the Move:
Residential Address:
Facility Name (if applicable)
Phone #:
Street
City
State
Zip
Mailing Address
(if different):
Street
City
State
Zip
Type of Placement: ❑ Home & Community Based – Specify:
❑ Nursing Home ❑ Other – Specify:
36BIV. AHCCCS CONTRACTOR CHANGE REQUEST COORDINATOR USE ONLY
❑ Local Office Contacted:
51BNAME:
Date:
Initials:
❑ Local Office Changes Made:
Date:
Initials:
❑ MFIS Referral Completed
Date:
Initials:
❑ Enrollment Effective Date Adjusted in PMMIS
Date:
Initials:
Comments:
DE-621 WHITE – Coordinator CANARY – Current Contractor PINK – Receiving Contractor
EXHIBIT 1620-9
ARIZONA LONG TERM CARE SYSTEM (ALTCS)
ENROLLMENT TRANSITION INFORMATION (ETI) FORM
EXHIBIT 1620-9
ARIZONA LONG TERM CARE SYSTEM (ALTCS)
ENROLLMENT TRANSITION INFORMATION (ETI) FORM
Revision Date: 01/01/16, 10/01/11, 02/01/11, 10/01/10, 07/01/08, 10/01/07, 12/01/06
Reviewed Date: 05/01/12
ALTCS ETI FORM, Page 1
Sending PC:
Receiving PC:
Transition Date:
Rate Code:
Member Name:
DOB:
AHCCCS ID:
M or F (circle one)
Primary Language Spoken:
Contact Person / Relationship:
indicate if Guardian, POA, etc.
Contact Person Phone #:
PRIMARY HEALTH INSURANCE
Medicare #:
Part A B D (circle all that apply)
Medicare Advantage -PDP:
SNP?
YES
NO
PDP:
Other:
MEMBER LOCATION
Current Address:
Phone Number:
Facility Name (if applicable):
Type of Facility:
Skilled Nursing Facility
Assisted Living Facility
Behavioral Health
Admission Date:
Specialty Unit:
Level of Care:
ALF Room and Board Amount:
MEDICAL INFORMATION
Diagnoses:
PCP Name:
PCP Phone #:
Specialists (Including out of area)
Name:
Type:
Phone #:
Name:
Type:
Phone #:
Scheduled appointments/procedures:
Special Medications/Treatments:
CRS Services:
Pending Physicians orders not yet completed:
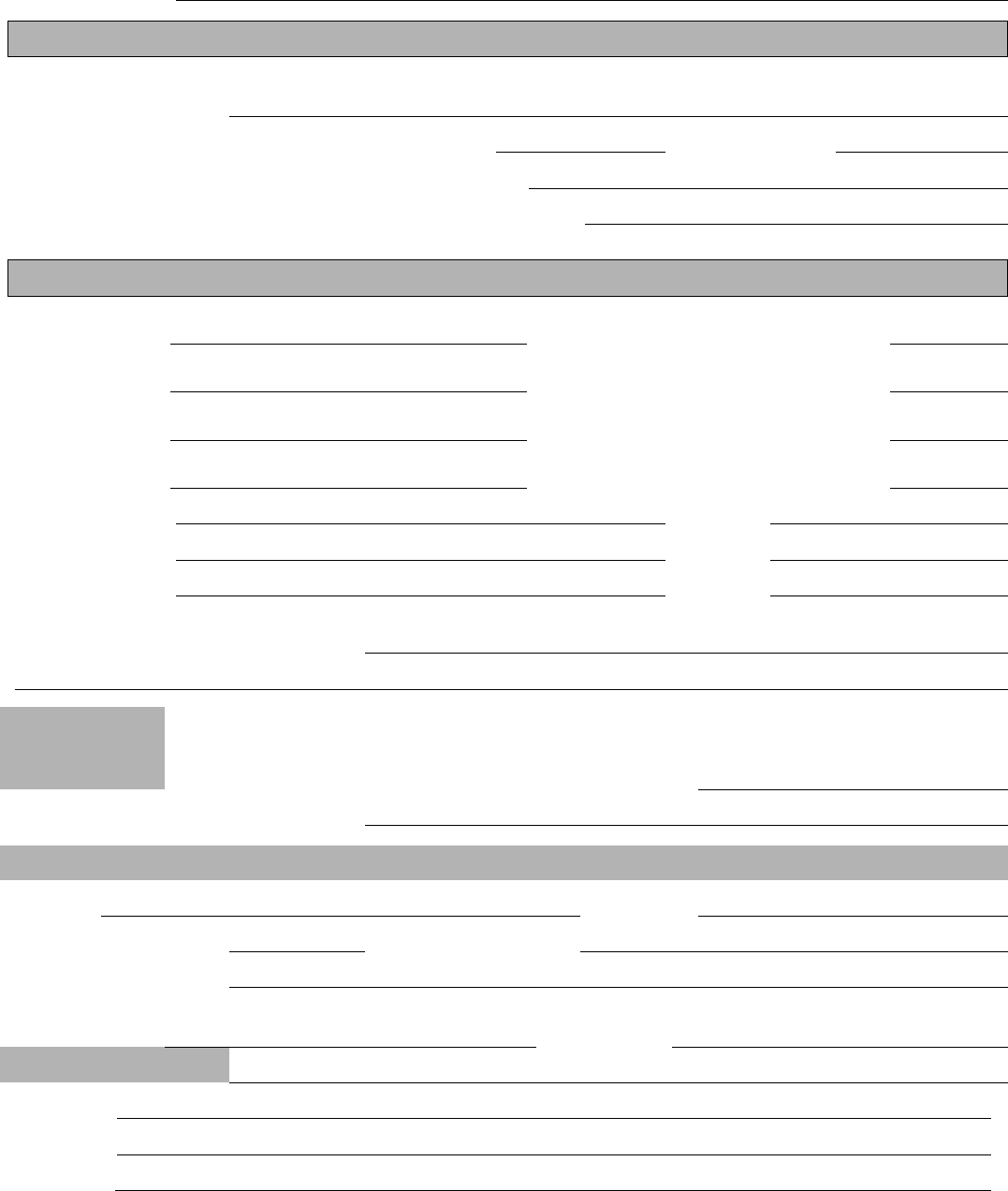
EXHIBIT 1620-9
ARIZONA LONG TERM CARE SYSTEM (ALTCS)
ENROLLMENT TRANSITION INFORMATION (ETI) FORM
Revision Date: 01/01/16, 10/01/11, 02/01/11, 10/01/10, 07/01/08, 10/01/07, 12/01/06
Reviewed Date: 05/01/12
ALTCS ETI FORM, Page 2
Member Name:
DIALYSIS
Site Name and
Address:
Days: M T W Th F Sat Sun Time:
Phone Number:
Transportation Provided by:
Assistance and/or Type of Transportation Required:
DME/SUPPLIES (see attached information for additional details on DME/Supplies as needed)
DME:
Rented?
Owned?
Provider:
DME:
Rented?
Owned?
Provider:
DME:
Rented?
Owned?
Provider:
DME:
Rented?
Owned?
Provider:
Supplies Needed:
Provider:
Supplies Needed:
Provider:
Supplies Needed:
Provider:
Pending Issues requiring follow-up:
PENDING
GRIEVANCE?
Yes No
Expected
Resolution
Date:
What is nature of grievance?
HOSPITALIZED MEMBERS (complete if member is hospitalized on date form is completed)
Hospital:
Phone:
Admission Date:
Admitting Diagnosis:
Inpatient Treatments:
Expected
Discharge Date:
D/C To:
OTHER COMMENTS:
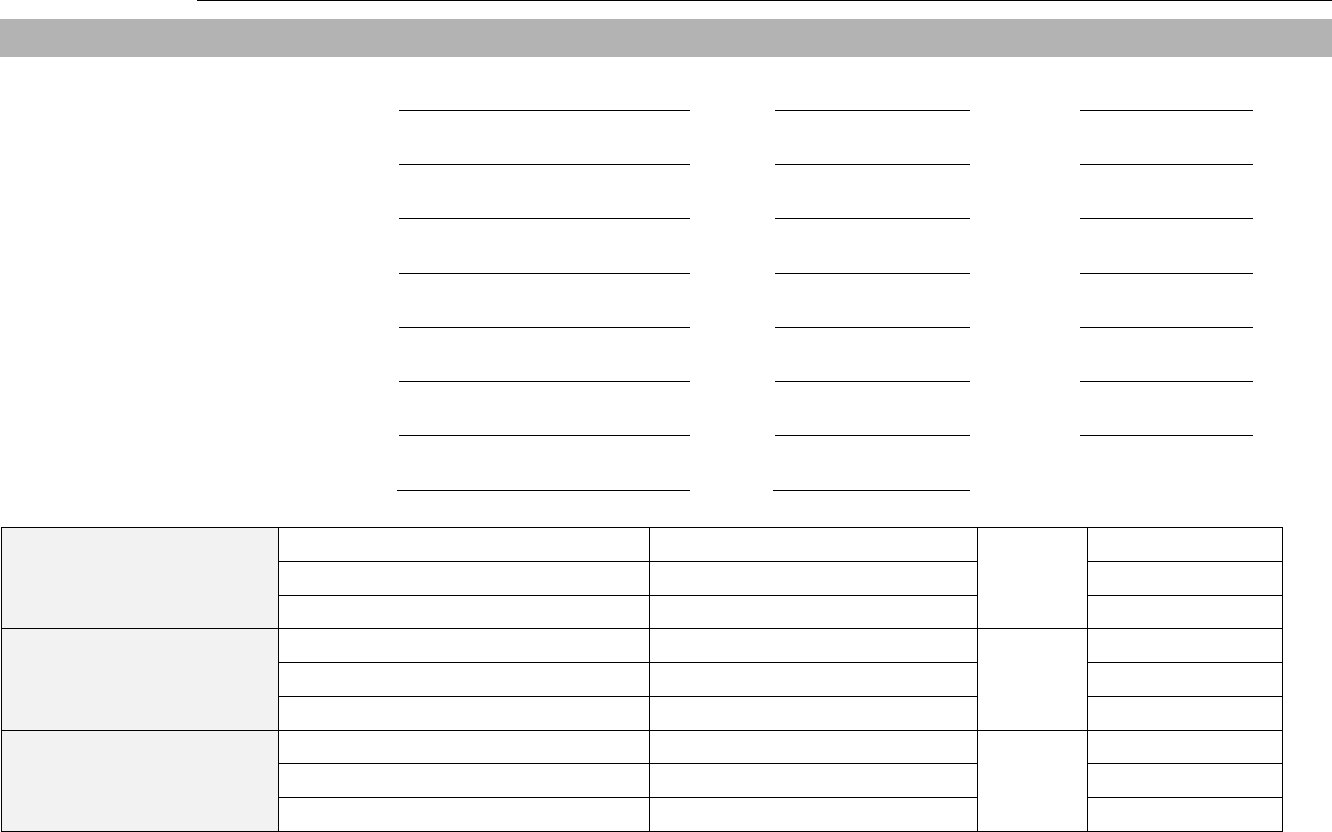
EXHIBIT 1620-9
ARIZONA LONG TERM CARE SYSTEM (ALTCS)
ENROLLMENT TRANSITION INFORMATION (ETI) FORM
Revision Date: 01/01/16, 10/01/11, 02/01/11, 10/01/10, 07/01/08, 10/01/07, 12/01/06
Reviewed Date: 05/01/12
ALTCS ETI FORM, Page 3
MEMBER NAME:
HCBS SERVICES (Check all that apply or attach Service Authorizations for details)
Adult Day Health
Provider:
Phone#:
Frequency:
Attendant Care
Provider:
Phone#:
Frequency:
Home Delivered Meals
Provider:
Phone#:
Frequency:
Homemaker
Provider:
Phone#:
Frequency:
Personal Care
Provider:
Phone#:
Frequency:
Respite
Provider:
Phone#:
Frequency:
Other ___________
Provider:
Phone#:
Frequency:
Emergency Alert
Provider
Phone#:
HOME HEALTH NURSING
Provider:
Frequency:
Phone#:
Payer Source:
HOME HEALTH AIDE
Provider:
Frequency:
Phone#:
Payer Source
HOSPICE
Provider:
Frequency:
Phone#:
Payer Source:
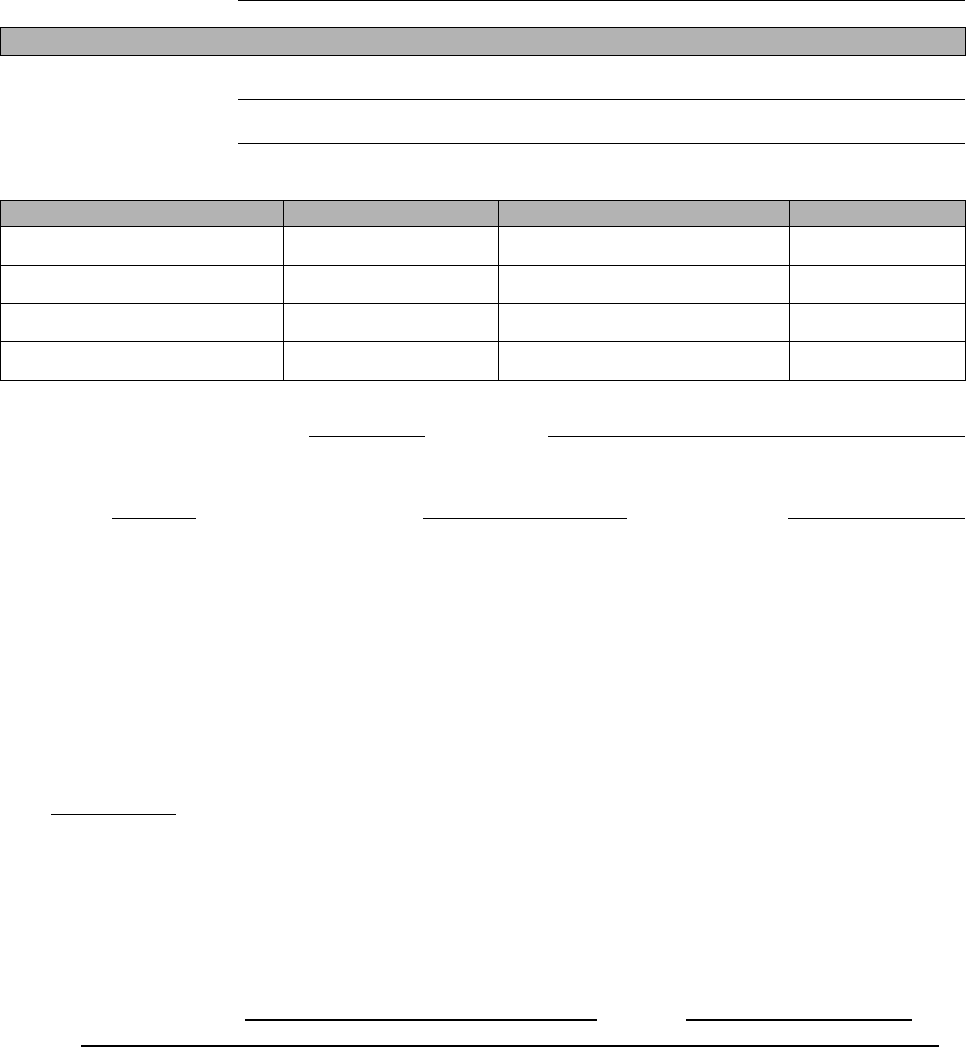
EXHIBIT 1620-9
ARIZONA LONG TERM CARE SYSTEM (ALTCS)
ENROLLMENT TRANSITION INFORMATION (ETI) FORM
Revision Date: 01/01/16, 10/01/11, 02/01/11, 10/01/10, 07/01/08, 10/01/07, 12/01/06
Reviewed Date: 05/01/12
ALTCS ETI FORM, Page 4
MEMBER NAME:
BEHAVIORAL HEALTH
BH Diagnosis:
BH Medications:
BH SERVICES/PROVIDERS:
SERVICE
PROVIDER
PHONE #
FREQUENCY
Last Date of Judicial Review:
Outcome:
COT
Name on Court
Order:
Expiration
Date:
REQUIRED ATTACHMENTS AND OTHER TRANSITIONING INFORMATION:
Last CM Assessment
CM Summary
Last Quarterly Behavioral Health
Consult, if applicable
Advanced Directives (Living wills, Powers of
Attorney, etc.), if applicable
List of Medications
EPSDT Forms, if applicable
Contingency Plan, if member
receiving critical services
Out-Pt Adult Physical Therapy
Service. The number of visits
received for current contract year
___________
Respite Hours Utilized
Inpatient Days Utilized
Guardian/Conservatorship or Power of Attorney, if
applicable
Lifetime use of Community Transition Service
(CTS) Benefit Community Transition Service
Date: _________
CASE MANAGER NAME: ________________________________ PHONE: ____________________
DATE: ______________________________________________________________________________
EXHIBIT 1620-10
RESERVED
EXHIBIT 1620-11
SAMPLE CRITICAL SERVICE GAP REPORT FORM

Review Date: 01/01/16 Revision Date: 05/01/12, 05/07/10, 08/16/05
LOGO AND ADDRESS OF CONTRACTOR HERE
[Must use Times New Roman and 14 point font]
CRITICAL SERVICE GAP REPORT FORM
All ALTCS members have the right to receive all critical services in their care plan to help with
bathing, dressing, toileting, feeding, transferring to or from your bed or wheelchair and other
similar daily activities. If you do not receive your critical services as specified in your care plan,
you should report this as quickly as possible. You should immediately call the AHCCCS,
provider agency or Contractor at the phone numbers listed on the Contingency Plan Form your
case manager filled out with you. You may also call your case manager. You have the right to
receive these critical services from a back-up substitute caregiver within two hours of you
reporting the gap.
In addition, you can mail this form to us at the address listed above telling us the services you
have not received. As your Contractor, we will respond to you either by telephone or by the
mail. You will be told the reason for the delay and how it will be fixed now and in the future if
it happens again. Please fill in the following:
Your Name:________________________________________________________________
AHCCCS ID Number (if available)______________________________________________
Date of Birth:_______________________________________________________________
Date(s) you did not receive your services:_________________________________________
Critical Service(s) not received:_________________________________________________
Comments:_________________________________________________________________
__________________________________________________________________________
*Exhibit 1620-11 is also available in Spanish. See Appendix K, Select ALTCS Case Management Forms in Spanish.
EXHIBIT 1620-12
SPOUSE ATTENDANT CARE ACKNOWLEDGEMENT OF UNDERSTANDING FORM
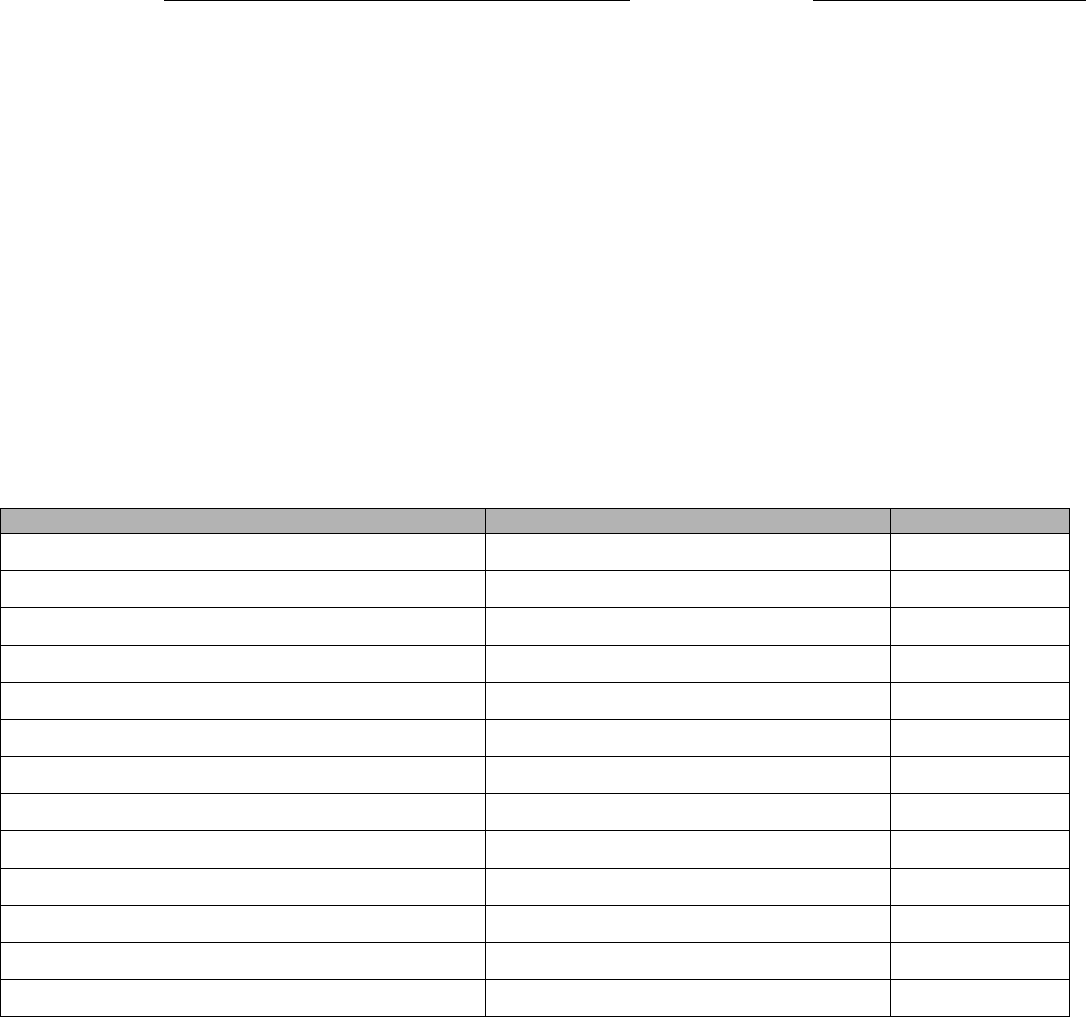
EXHIBIT 1620-12
SPOUSE ATTENDANT CARE ACKNOWLEDGEMENT OF UNDERSTANDING
Review Date: 01/01/16 Initial Effective Date: 10/01/2007
MEMBER NAME:
AHCCCS ID#:
We, the people who have signed on the next page, choose to have Arizona Long Term Care System (ALTCS)
pay _____________(the spouse) for ______________’s (the member’s) care. We know and agree that:
The ALTCS Case Manager will decide the number of hours that will be paid for _________________’s
(the member’s) care;
All services will be medically necessary and cost effective; and
We cannot have more than 40 hours of Attendant Care (or similar services) in a seven day period.
We know and agree that if _________________ (the spouse) is paid for giving care:
There will be an increase in the earned income of ________________________ (the spouse);
The extra income could cause us to lose benefits from other publicly funded programs; and
This change in benefits could affect us and/or others in our household.
Publicly funded programs may include but are not limited to the following:
BENEFIT TYPE
AGENCY RESPONSIBLE
PHONE NUMBER
AHCCCS, ALTCS and/or KidsCare eligibility
AHCCCS
Supplemental Security Income (SSI)
Social Security Administration
Medicare Part D Low Income Subsidy
Social Security Administration
Food Stamps
Arizona Department of Economic Security
Temporary Assistance to Needy Families (TANF)
Arizona Department of Economic Security
General Assistance
Arizona Department of Economic Security
Housing and Urban Development (HUD) Housing
Local Housing Authority
Social Security Disability
Social Security Administration
Qualified Medicare Beneficiary (QMB)
AHCCCS
Specified Low-Income Medicare Beneficiary (SLMB)
AHCCCS
Qualified Individual – 1 (QI-1)
AHCCCS
Other:
Other:
Page 1 of 2
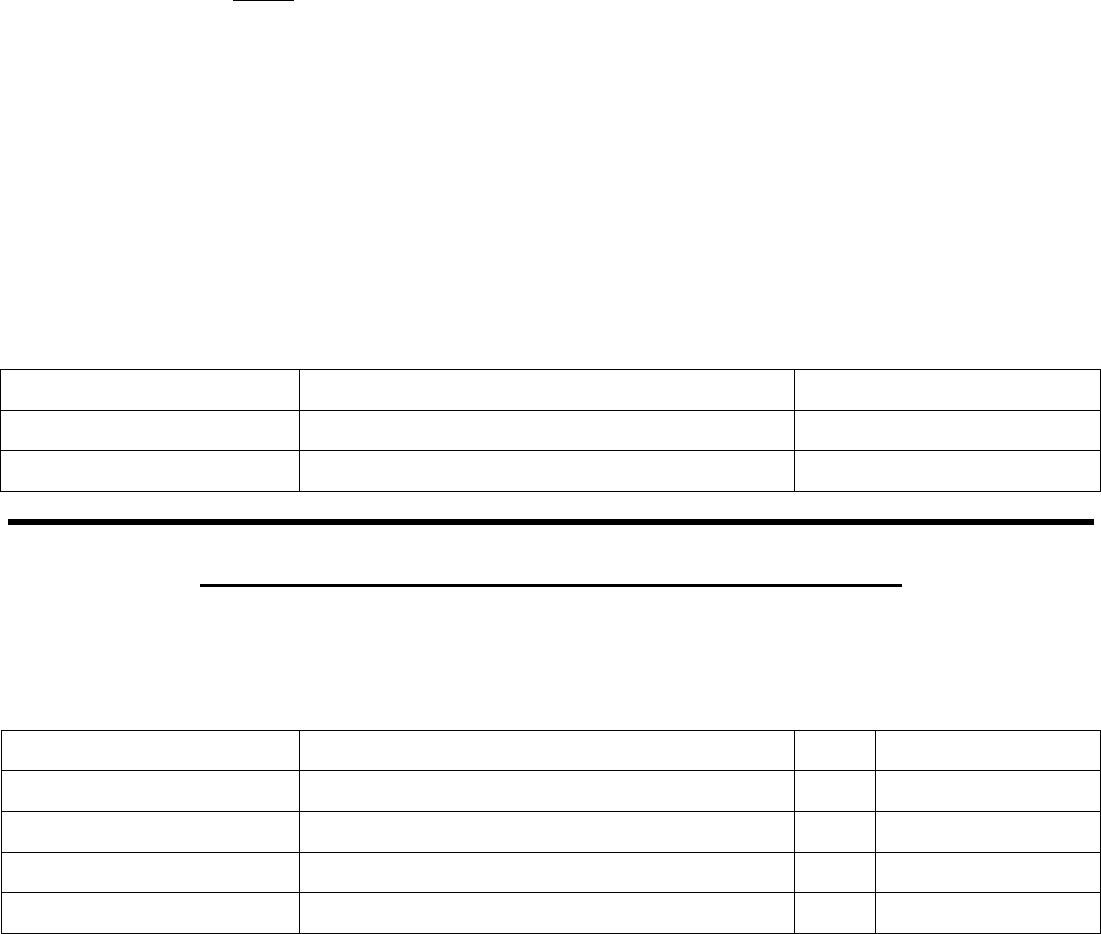
EXHIBIT 1620-12
SPOUSE ATTENDANT CARE ACKNOWLEDGEMENT OF UNDERSTANDING
Review Date: 01/01/16 Initial Effective Date: 10/01/2007
We know it is up to us to get in touch with any agencies from whom anyone in our household receives benefits.
We will:
Talk about how a change in the income for __________________________ (the spouse) may affect
those benefits;
Talk about this before making a decision to pay ________________ (the spouse) for care; and
Tell any agency from whom we currently receive benefits of the change in income if/when we decide to
pay ________________ (the spouse) for care.
We understand that some or all of our publicly funded benefits could be stopped or reduced. This depends on
the amount of income ____________________ (the spouse) receives as an ALTCS paid caregiver. We will ask
_________________________’s (the member’s) ALTCS case manager for assistance if we need it.
We also know:
We can change our minds about paying ________________ (the spouse) for care at any time;
We can decide that __________________ (the member) should receive other ALTCS services; and
These services must be medically necessary and cost effective.
Signature of Member:
Date:
Signature of Spouse:
Date:
Signature of Case Manager:
Date:
ANNUAL REVIEW OF CHOICE FOR SPOUSE ATTENDANT CARE
My spouse has been my paid ALTCS caregiver. I wish to continue with that plan. I know that there are other
agencies and caregivers who could provide my care. I know that by choosing my spouse, I only get up to 40
hours of Attendant Care (or similar services) per week.
Signature of Member:
Date:
Signature of Member:
Date:
Signature of Member:
Date:
Signature of Member:
Date:
Signature of Member:
Date:
cc: Member
Case file
*Exhibit 1620-12 is also available in Spanish. See Appendix K, Select ALTCS Case Management Forms in Spanish.
Page 2 of 2
EXHIBIT 1620-13
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM
ALTCS MEMBER SERVICE PLAN
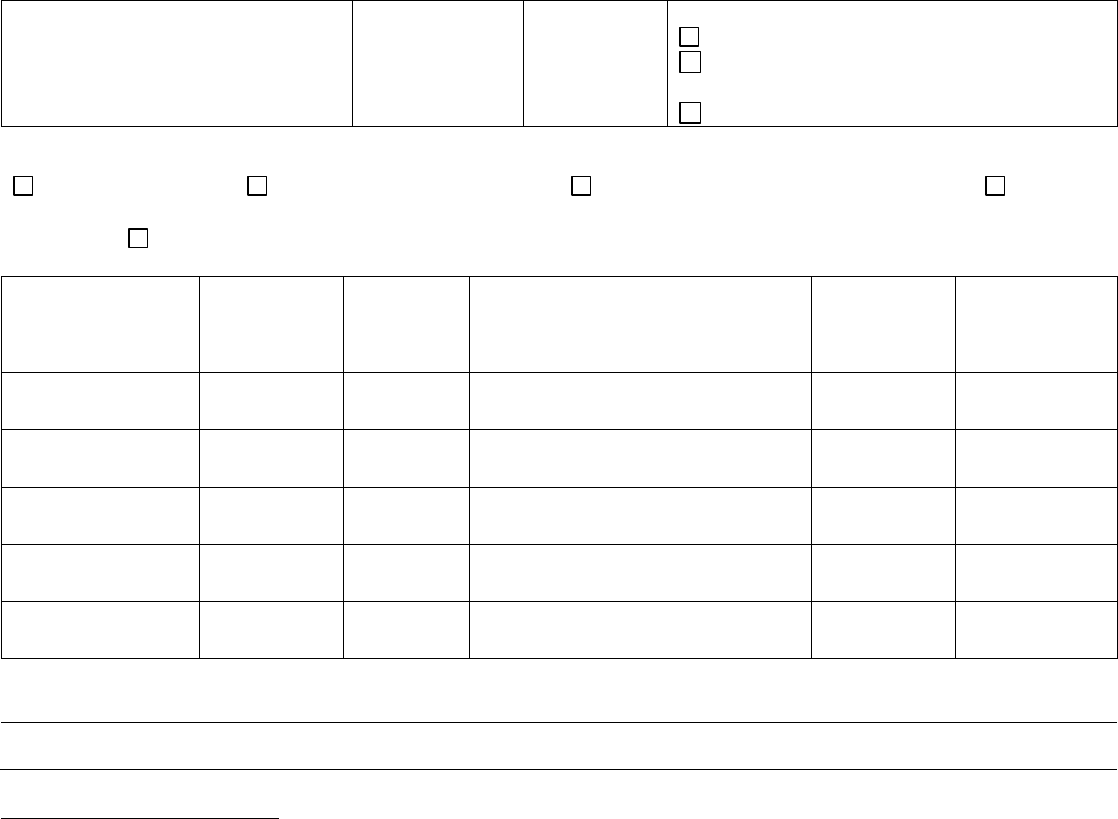
EXHIBIT 1620-13
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM
ALTCS MEMBER SERVICE PLAN
Revised: 01/01/16, 03/01/13 Initial Effective Date: 02/01/2009
Member’s Name:
AHCCCS ID#:
Date:
Next Review Date: check one
Not to exceed 90 days (HCBS)
Not to exceed 180 days
(Nursing Facility or DDD Group Home)
Annual (Acute Care Only)
I choose the following service model: (Check “N/A” for members not receiving Attendant Care, Personal Care, Homemaker, or Habilitation)
TRADITIONAL
AGENCY WITH CHOICE
SELF-DIRECTED ATTENDANT CARE
N/A
INDEPENDENT PROVIDER (DDD or FFS members)
Service & Provider
Service
Frequency in
place prior to
this assessment
Service
Frequency
currently
assessed
Service Change
Start/End
Date
Member/
Representative
None New Increase
Reduce Terminate Suspend
Agree
Disagree
None New Increase
Reduce Terminate Suspend
Agree
Disagree
None New Increase
Reduce Terminate Suspend
Agree
Disagree
None New Increase
Reduce Terminate Suspend
Agree
Disagree
None New Increase
Reduce Terminate Suspend
Agree
Disagree
Comments:
Service Plan Acknowledgement: My service plan has been reviewed with me by my case manager. I know what services I
will be getting and how often. All changes in the services I was getting have been explained to me. I have marked my
agreement and/or disagreement with each service above. I know that any reductions, terminations or suspensions
(stopping for a set time frame) of my current services will begin no earlier than 10 days from the date of this plan. I know
that I can ask for this to be sooner.
If I do not agree with some or all of the services that have been authorized in this plan, I have noted that above. I know
that my case manager will send me a letter that tells me why the service(s) I asked for was denied, reduced, suspended or
terminated. That letter will tell me how to appeal the decision that has been made about my services. The letter will also
tell me how I can receive continued services.
Page 1 of 2
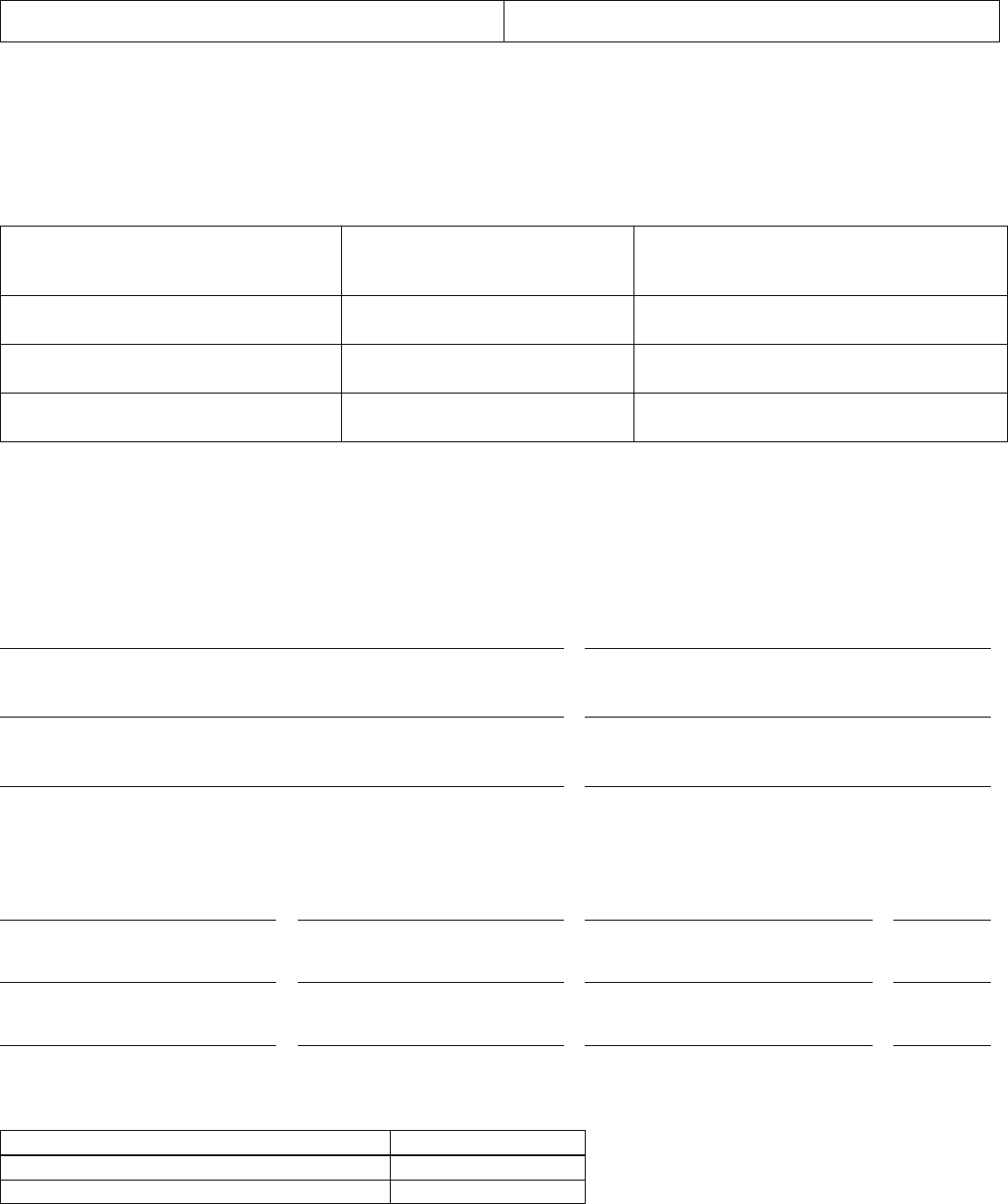
EXHIBIT 1620-13
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM
ALTCS MEMBER SERVICE PLAN
Revised: 01/01/16, 03/01/13 Initial Effective Date: 02/01/2009
Member’s Name:
AHCCCS ID#:
My case manager has told me how the appeal process works. I know how I can appeal service changes I do not agree
with. I know that I can change my mind later about services I agree with today. I know that if I change my mind before
the changes go into effect, I will get a letter that tells me the reason my services changed. The letter will also tell me about
my appeal rights, including how to receive continued services.
Case manager: Please list all non-ALTCS funded services provided by payer source (i.e. Medicare). Attach a separate
page if more lines are needed. Please do not include informal/natural supports, as they are listed on the HNT.
Non-ALTCS Funded Service
Responsible Party/Payer Source
Approximate Service Frequency
(example: daily, weekly, monthly)
I know that I can ask for another service planning meeting to go over my needs and any changes to this plan that are
needed. I can contact my case manager ___________________________ at (____) _____-_____. I also know that I can
contact my case manager at any time to discuss any questions, issues, and/or concerns that I may have regarding my
services. My case manager will contact me within 3 working days. Once I have talked with my case manager, s/he will
give me a decision about that request within 14 days. If the case manager is not able to make a decision about my request
within 14 days, s/he will send me a letter to let me know more time is needed to make a decision.
Member/Legal Representative Signature
Date
Individual Representative Signature (Agency with Choice only)
Date
Case Manager Signature
Date
Other Attendees: (Attendees please note that by signing below, you are saying you participated in today’s service
planning meeting and not attesting to whether or not you are in agreement/disagreement with this service plan)
Name
Signature
Name of Agency/Relationship
Date
Name
Signature
Name of Agency/Relationship
Date
Name
Signature
Name of Agency/Relationship
Date
Case Managers: Please document when the service plan was sent to the Member, Individual Representative and/or the
Legal Representative.
Name
Date
*Exhibit 1620-13 is also available in Spanish. See Appendix K, Select ALTCS Case Management Forms in Spanish.
Page 2 of 2
EXHIBIT 1620-14
AHCCCS/ARIZONA LONG TERM CARE SYSTEM (ALTCS)
MEMBER CONTINGENCY/BACK-UP PLAN
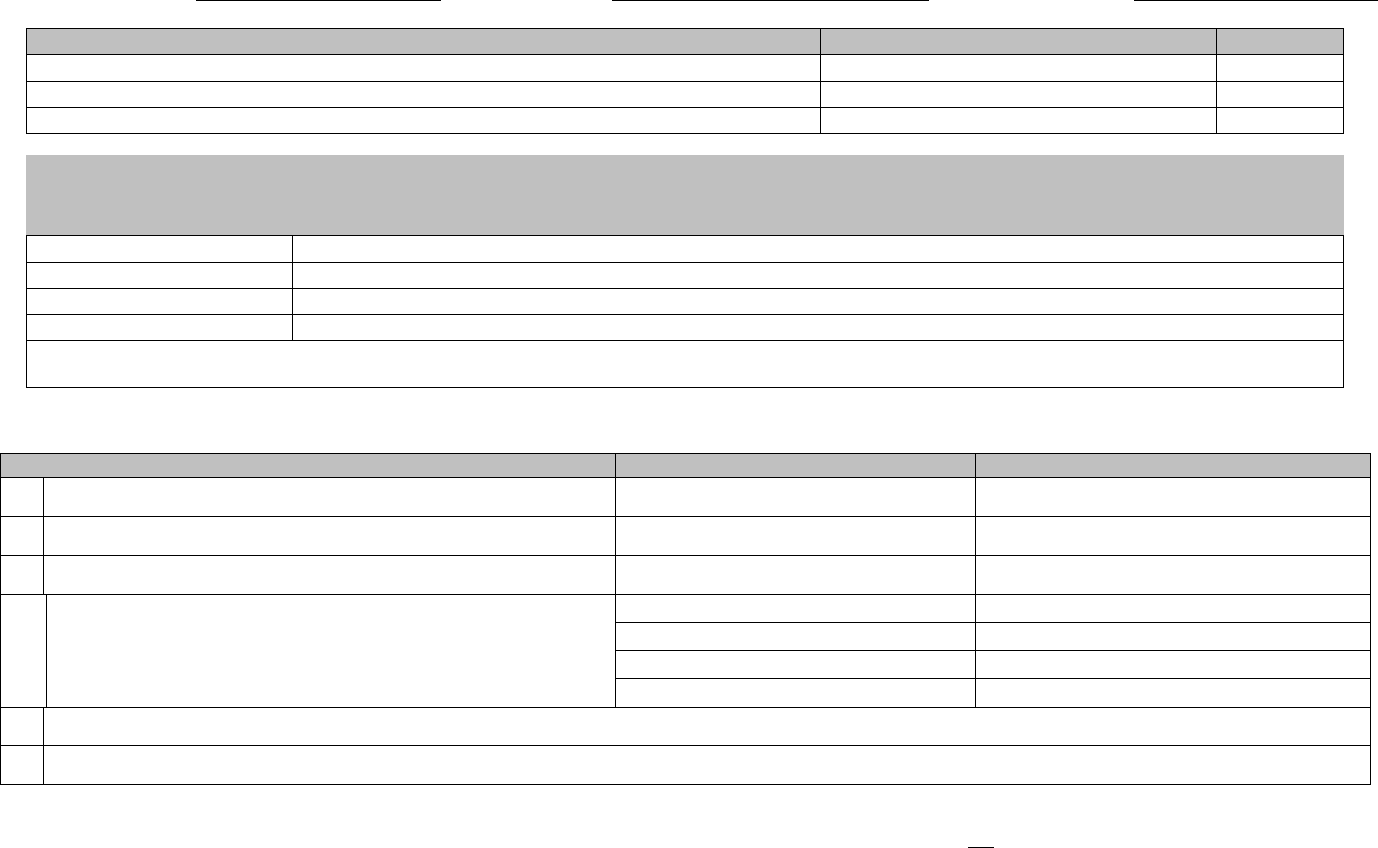
Review Date: 01/01/16 Page 1 of 2
EXHIBIT 1620-14
AHCCCS/ARIZONA LONG TERM CARE SYSTEM (ALTCS) MEMBER CONTINGENCY/BACK-UP PLAN
MEMBER NAME:
AHCCCS ID#:
DATE OF PLAN:
IN-HOME SERVICES PROVIDED BY ALTCS
FREQUENCY
PROVIDER
1)
2)
3)
MEMBER SERVICE PREFERENCE LEVEL – based on member’s choice for how quickly a replacement caregiver will be needed if the scheduled
caregiver becomes unavailable. Members must be informed that they have the right to a back-up caregiver within 2 hours if they choose. Circle
member’s choice:
1
Needs services within 2 hours.
2
Needs services today.
3
Needs services within 48 hours.
4
Can wait until next scheduled visit by provider.
Member has been advised that s/he may change the Member Service Preference Level and also his/her back-up plan, as indicated below, at any time,
including at the time of a gap*
Case Manager Initial and Date
If my ALTCS caregiver does not show up to provide services as scheduled, my back-up plan is as follows (check all that apply):
BACK-UP PLAN
NAME
PHONE NUMBER
I will contact AHCCCS.
AHCCCS
1-800-218-7509
I will contact my provider agency.
I will contact my case manager.
I prefer to have family or friends provide my care instead of
another ALTCS provider/caregiver.
1)
2)
3)
4)
I can wait until the next scheduled visit from my provider agency to receive authorized care.
Other:
* A gap in critical services is defined as the difference between the number of hours of critical service scheduled in each individual’s care plan and the hours
of the scheduled type of critical service that are actually delivered to the individual. The following situations are not considered gaps:
The member is not available to receive the service when the caregiver arrives at the member’s home as scheduled.
The member refuses the caregiver when s/he arrives, unless the caregiver is not able to do the assigned duties.
The member refuses services.
The member’s home is seen as unsafe by the agency/caregiver, so the caregiver refuses to go there.
Review Date: 01/01/16 Page 2 of 2
AHCCCS/ALTCS MEMBER CONTINGENCY/BACK-UP PLAN – CONT’D
MEMBER NAME:
AHCCCS ID#:
I understand that I have the right to receive all the services in my care plan to help me with bathing, toileting, dressing, feeding, transferring to or from my bed and
wheelchair, and other similar daily activities as needed. These services (Attendant Care, Personal Care, Homemaker and Respite) are called “critical services.” I
understand that my health plan must make sure that I receive these critical services without delays. I understand that if I do not receive my critical services on time
I can call AHCCCS to report the problem so they can assist in replacing my caregiver as soon as possible. I may also call my provider agency or case manager for
help. If there is a delay and I do not receive these services on time, my health plan must provide a back-up caregiver within 2 hours of the time they are notified of
the gap, unless I specify otherwise at the time of the gap. I understand I also have the right to file a written complaint about the failure to provide such services as
scheduled.
I understand that in order to receive services I must be available and willing to accept the scheduled services. If I choose not to accept the services I understand I
must tell my case manager this. This plan has been reviewed with me and I agree with it. I will keep a copy of this plan.
Please have member/representative sign here at time of initial plan development:
Member/Representative Signature:
Date:
Relationship to Member:
QUARTERLY VISIT
This plan was reviewed with me by the case manager during my quarterly service review. My signature below indicates I still agree with this plan and no changes
are needed. I understand that I may change my Member Service Preference Level at any time, including at the time a gap may occur. My case manager and I will
fill out a new Contingency Plan form if I have changes to my plan, but at least once a year.
Please have member/representative sign here to indicate continued agreement with plan at the time of each 90 day service assessment. If the
member/representative wishes to make changes to the information in this plan, a new plan must be written. A new plan is required at least once a year.
Date of Review:
Member/Representative Signature:
Date of Review:
Member/Representative Signature:
Date of Review:
Member/Representative Signature:
cc: Member/Representative
Case File
*Exhibit 1620-14 is also available in Spanish. See Appendix K, Select ALTCS Case Management Forms in Spanish.
Review Date: 01/01/16
AHCCCS/ALTCS CONTINGENCY PLAN
INSTRUCTIONS
All ALTCS Contractors must use this standardized form. It may be altered in the ways listed below without
AHCCCS approval. All other changes to the form must be prior approved by AHCCCS.
1. Contractor letterhead may be added.
2. Terms such as “case manager” and “health plan” may be changed to terms more commonly used by the
Contractor.
3. Contractor-specific member ID numbers may be added.
This form must be completed by the case manager for all Home and Community Based Service (HCBS)
members who receive one or more of the following ALTCS services:
1. Attendant Care
2. Personal Care
3. Homemaker
4. In-home Respite
The member must be advised of his/her right to have a back-up on-call caregiver provided in the event an
unforeseeable gap occurs.
The member must be advised of his/her right to change a previously designated Member Service Preference
Level at any time, including at the time a gap occurs. The case manager must initial and date the statement
on the first page indicating this was done at the time the plan was developed.
The member should designate the back-up plan for how the member chooses to have his/her needs met in
the event the regular caregiver is not available as scheduled. More than one option can be chosen.
The member/representative should not indicate “I can wait until the next scheduled visit from my provider
agency to receive authorized care” in the back-up plan unless the designated Member Service Preference
Level is 4 (can wait until next scheduled visit by provider).
If the member indicates s/he wants family or friends to provide unpaid back-up care for some or all of the
time that the ALTCS provider was scheduled to be there, the names of those individuals should be listed.
The selection of this informal support system as the back-up plan must be the member’s choice and
not assumed simply because those individuals live in the home and/or appear to be available.
The phone number for the AHCCCS toll-free phone line must be listed. The name and phone number(s) of
the member’s provider agency must be listed, including the after-hours number. The case manager’s name
and phone number(s) should also be included. The Contractor’s after-hours phone number should be
included on this form or made available to members when they call the case manager’s phone number.
The member or representative must sign the completed form indicating it has been reviewed with him/her
and that s/he is in agreement with it. A copy of the signed plan must be given to the member/representative.
This form must be signed upon initial completion as well as at each 90-day service review if there are
no changes to the plan. If there are changes to any part of the plan, a new plan must be written, signed and
a copy left with the member/representative. A new plan must be written at least once a year.
*Exhibit 1620-14 is also available in Spanish. See Appendix K, Select ALTCS Case Management Forms in Spanish.
EXHIBIT 1620-15
ASSISTED LIVING FACILITY (ALF) RESIDENCY AGREEMENT
EXHIBIT 1620-15
ASSISTED LIVING FACILITY (ALF) RESIDENCY AGREEMENT
Review Date: 01/01/16 Revision Date: 03/01/2013, 01/01/2011 1
1. _____________________________________, an approved Assisted Living Facility (hereinafter “ALF”), and
(Name of ALF)
______________________, an Arizona Long Term Care System / ALTCS Member (hereinafter “Resident”),
(Resident’s Name)
agree to the placement of Resident, by _________________________ (hereinafter “Contractor”), represented
herein (Contractor)
by _______________________ (hereinafter “Case Manager”) in ALF effective ____________________ .
(Case Manager) (Date of Placement)
The Contractor will pay ALF based on the Contracted Rate for the Authorized Care Level minus Resident’s
Room
and Board cost as described below.
For ALTCS Fee For Service (FFS) only: AHCCCS will pay ALF $_________________ per day minus
(Daily Rate)
Resident’s Room and Board cost as described below.
2. ALF and Resident further agree to the following terms and conditions of this placement. Resident shall pay
the ALF for Room and Board. Resident agrees to pay ALF the pro-rated Room and Board amount of
$________ per day from _______________ to ______________________.
(Admit Date) (End of 1st partial month)
Thereafter Resident agrees to pay the amount of $_________ per month. The Room and Board amount that
the Case Manager enters in the Contractor’s service authorization system, if different from the amount on this
form, supercedes the amount in this Residency Agreement. The Resident must pay the monthly Room and
Board to ALF on or before the 10th of each month effective ____________________.
(1st Full month)
If Resident’s Room and Board payment is not made by the 10th of the month, ALF will send Resident a notice
of delinquency of payment. If the payment is not made within two weeks of the date of such notice, Case
Manager must be informed by ALF so that Resident and/or other responsible party will receive a 14-day
notice, from the facility, to make other living arrangements.
The Room and Board amount is subject to change as the Resident’s income amount changes and will be Initial
adjusted in accordance with program guidelines. Anytime the Resident, other responsible party or ALF
becomes aware of a change in the amount of the Resident’s income, immediate notification to the Contractor
Case Manager and AHCCCS Eligibility Worker is required.
EXHIBIT 1620-15
ASSISTED LIVING FACILITY (ALF) RESIDENCY AGREEMENT
Review Date: 01/01/16 Revision Date: 03/01/2013, 01/01/2011 2
3. ALF agrees to comply with the Arizona Administrative Code Title 9, Chapter 10, Article 8, Assisted Living
Facility as appropriate.
4. ALF shall be paid by Contractor and Resident for the Date of Placement but not the date of discharge. For partial
months and care level changes, payment from Contractor and Resident as appropriate shall be pro-rated to
reflect changes on a daily basis.
5. During Resident’s temporary absence (of greater than 24 hours), ALF is not entitled to any payment from the
Contractor. ALF shall notify the Case Manager of any absences within one working day. Resident remains
obligated to pay ALF the Resident’s Room and Board amount during any and all temporary absences.
6. No gifts will be accepted by the ALF from the Resident except nominal gifts during the holidays or for
birthdays.
7. This placement may be terminated upon Contractor being provided with a written request from either ALF or the
Resident. Contractor shall have 30 days from the date of the request to make other placement arrangements for
the Resident. Except when R9-10-807 (F) applies.
8. Within 30 days after the date of termination of residency, the ALF shall refund any Room and Board prepaid by
Resident for the date of discharge and any and all days thereafter.
9. ALF has not and will not pay any referral fees for placement at said ALF (42 USC § 1320a-7b and 42 CFR Part
1001).
10. Neither ALF nor any other party on behalf of the ALF can charge for the development of resident care plans.
11. Residents residing in Assisted Living Facilities may have to share a room. If the Resident chooses a private
room, there may be a charge, unless the facility does not have semi-private rooms as an option.
12. Resident/representative is not to be charged for transportation of Resident to medical appointments. If
applicable, ALF may arrange transportation with the Contractor.
13. All medically necessary durable medical equipment is provided by the PC. Resident/representative is not to be
charged a rental fee for any medical necessary equipment. The ALF shall contact the PC to obtain this
equipment.
14. No ALF licensee, staff or their family members may act as a representative, agent, surrogate, health care
power of attorney, power of attorney, guardian, or conservator of a Resident who is not a relative. [R9-10-
803(G)(1)].
EXHIBIT 1620-15
ASSISTED LIVING FACILITY (ALF) RESIDENCY AGREEMENT
Review Date: 01/01/16 Revision Date: 03/01/2013, 01/01/2011 3
15. ALF may, with the Resident’s or Resident’s representative’s written permission, administer personal funds
that do not exceed $500.00 per month. If ALF administers such funds, ALF must keep receipts for
expenditures and give a written accounting to the Resident or __________________________, Resident’s
representative, every three months.
16. ALF may enter into an agreement with Resident/representative to provide non-covered services, however, the
Case Manager must review the agreement to ascertain that the service is not covered by ALTCS.
17. ALF shall refund to Resident any deposits (including security deposits) paid prior to ALTCS enrollment
(inclusive of Prior Period Coverage), within 30 days of ALTCS enrollment, unless such deposits (or a portion
thereof) are necessary to remedy default in the payment of rent or repair damages to the premises exclusive of
ordinary wear and tear.
ALF AND RESIDENT AGREE TO ABIDE BY THE TERMS AND CONDITIONS AS OUTLINED IN THIS RESIDENCY
AGREEMENT:
Member or Representative______________________________________ Date______/_______/_______
ALF Sponsor/Manager_________________________________________ Date______/_______/_______
Case Manager_________________________________________________ Date______/_______/_______
*Exhibit 1620-15 is also available in Spanish. See Appendix K, Select ALTCS Case Management Forms in Spanish.
EXHIBIT 1620-16
ASSISTED LIVING FACILITY (ALF) FINANCIAL CHANGE AGREEMENT
EXHIBIT 1620-16
ASSISTED LIVING FACILITY (ALF) MEMBER FINANCIAL CHANGE AGREEMENT
Review Date: 01/01/16 Revision Date: 01/01/2011
FACILITY NAME:_______________________________ PC NAME:__________________________
MEMBER NAME:______________________________ AHCCCS ID:_______________________
THE FOLLOWING BILLING/MEMBER LOC CHANGE(S) HAVE OCCURRED
Rate: Effective:
I. Facility Reimbursement: LOC_____ $____________ ____________________
II. Level of Care (LOC) Changed to: _____ $____________ ____________________
III. Member Room & Board Responsibility $____________ ____________________
I HAVE READ AND AGREE WITH THE ABOVE CHANGES.
FACILITY REPRESENTATIVE:
Printed _____________________________________________ Title: __________________________
Signature ___________________________________________ Date: _________________________
MEMBER / REPRESENTATIVE: (ONLY REQUIRED FOR CHANGES IN ROOM & BOARD)
Printed ______________________________________________ Relationship: __________________
Signature ____________________________________________ Date: ________________________
CASE MANAGER:
Printed _______________________________________________
Signature _____________________________________________ Date: _______________________
A SIGNED COPY MUST BE PROVIDED TO THE CONTRACTOR’S CASE MANAGER
FOR THE MEMBER’S FILE.
*Exhibit 1620-16 is also available in Spanish. See Appendix K, Select ALTCS Case Management Forms in Spanish.
EXHIBIT 1620-17
HOME AND COMMUNITY BASED SERVICE (HCBS) MEMBER NEEDS ASSESSMENT
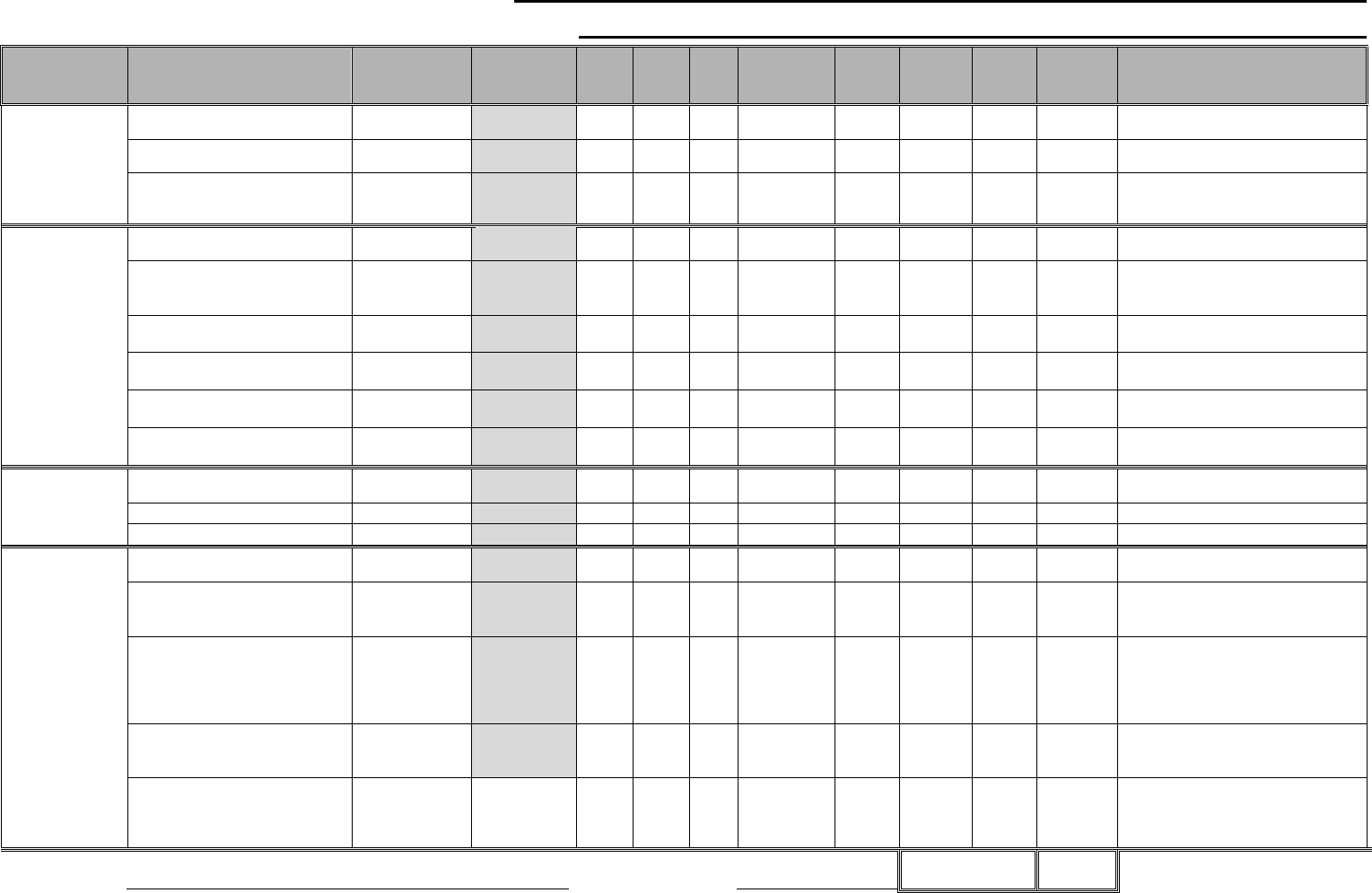
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
Exhibit 1620-17
HCBS MEMBER NEEDS ASSESSMENT
This tool is to be used as a guide and is not intended to replace professional experience. If there are questions or comments about a specific task, please review with your supervisor.
This tool is to be used anytime a member is requesting Attendant Care, Personal Care, or Homemaker Services.
Living Situation: o Lives Alone o Lives with Family o Lives with Non-family
Supervision Need: o Wandering Risk o Confused/Disoriented at risk to themselves o Unable to call for help, even with lifeline o NA
Name/ Relationship of Informal Supports that will be assisting with care:
Tasks completed by Informal Supports must be marked "IFS" on the spreadsheet below in the appropriate space to clearly identify when IFS is being provided. Ensuring member’s needs are met.
If lives with others, indicate Days/Hours others are not available to assist member:
TASK
DESCRIPTION
APPROX
TIME
TASKS PER
DAY
MON
TUE
WE
D
THU
FRI
SAT
SUN
TOTAL
COMMENTS
(WHO IS PROVIDING CARE/
WHY> <TIME NEEDED)
HOUSEKEEPING
AND
CLEANING
Independent:
No assistance needed.
0
min/day
Lives with others:
Cleaning member's area only.
1-60
min/week
Without Support:
Member lives alone.
Consider the size of the home.
1-120
min/week
LAUNDRY
Folding and
Putting Away
Laundry is
included.
Independent:
No assistance needed.
0
min/week
Washer & dryer are on site,
inside the member's home,
garage, or yard.
1-30
min/week
Washer is on site but clothes are
line dried.
1-60
min/week
Laundry is done in Apartment
Laundry Facility
1-90
min/week
Laundry facility is off site, such as
community Laundromat facility.
1-120
min/week
Incontinence Episodes –
Soiled Clothes and Linens
1-10
min/week
SHOPPING
Including
medication
pick-up
Independent:
No assistance needed.
0
min/day
Pick-up with Family Shopping
1-5 min/week
Lives alone.
1-90 min/week
MEAL PREP &
CLEAN UP
In general,
should not
exceed 75
minutes per day
Includes
blenderizing or
pureeing but not
cutting up food
Independent:
No assistance needed.
0
min/day
Breakfast:
If member eats same meal with
others:
1-15 min/day
1-5 min/day
Lunch:
If member eats same meal with
others:
If HDM is in place, please note this
on this line for the appropriate day.
1-20 min/day
1-5 min/day
Dinner:
If member eats same meal with
others:
1-40 min/day
1-5 min/day
Alternative Meal Schedule or
snacks: Ex: Diabetic with multiple
small meals/snack per day
requiring prep.
1-10 min/meal
Member Name:
AHCCCS ID:
Page 1 Total:
Page
1 of 4
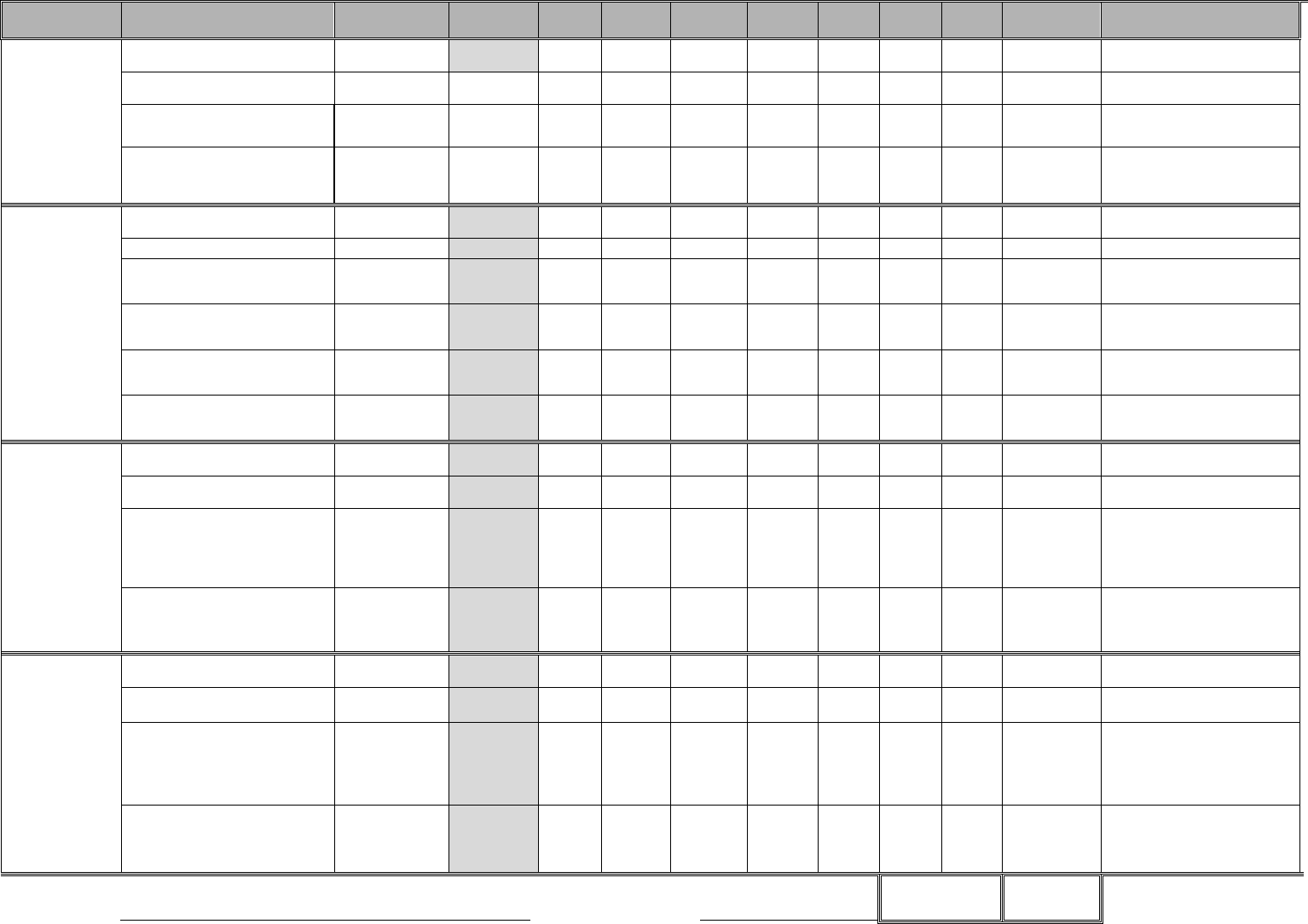
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
TASK
DESCRIPTION
APPROX
TIME
TASKS PER
DAY
MON
TUE
WED
THU
FRI
SAT
SUN
TOTAL
COMMENTS
(WHO IS PROVIDING CARE)
EATING &
FEEDING
Enter number of
meals eaten per
day requiring
assistance, then
enter the time
per meal
Independent:
No assistance needed
0
min/day
Minimum: Meal set up, cutting food, or
cueing /reminders.
1-10
min/meal
Moderate: As above plus hands-on
assist, cueing, or supervision for 50-
75% of meal.
1-15
min/meal
Maximum: Hands-on assist with
75%+ of meal, bringing food to
mouth or totally feeding member.
Constant supervision and cueing.
1-30
min/meal
BATHING
As needed per
week. In
general not to
exceed 45
transfers
including in
bath time.
Independent:
No assistance needed
0
min/day
Sponge bath:
1-5min/day
Minimum: Some supervision, cueing,
or set-up. Assist with getting in & out
of tub. Help with back or lower body.
1-15
min/day
Moderate: Step-by-step cueing or
supervision. Hands-on assist with 50-
75% of the bathing process.
1-30
min/day
Moderate: Step-by-step cueing or
supervision. Hands-on assist with 50-
75% of the bath process.
1-30
min/day
Maximum: 75%+ with bathing process.
One or more assist. Hoyer needed /
bed-baths.
1-45
min/day
DRESSING AND
GROOMING AM
Independent:
No assistance needed
0
min/day
Minimum: Some supervision,
reminding, selecting clothes.
1-10
min/day
Moderate: Supervision or hands-
on with 50-75% of dressing
activity. Regular asst. with
buttons, shoes & socks, fixing hair
or brushing teeth.
1-15
min/day
Maximum: Hands-on with 75%+
of dressing and grooming tasks.
Complete assist with dressing
includes transfer if needed.
1-20
min/day
DRESSING AND
GROOMING PM
Independent:
No assistance needed
0
min/day
Minimum: Some supervision,
reminding, selecting clothes.
1-10
min/day
Moderate: Supervision or hands-
on with 50-75% of dressing
activity. Regular asst. with
buttons, shoes & socks, or
brushing teeth.
1-15
min/day
Maximum: Hands-on with 75% of
dressing and grooming tasks.
Complete assist with dressing
includes transfer if needed.
1-20
min/day
Member Name:
AHCCCS
ID:
Page 2 Total:
Page 2 of 4
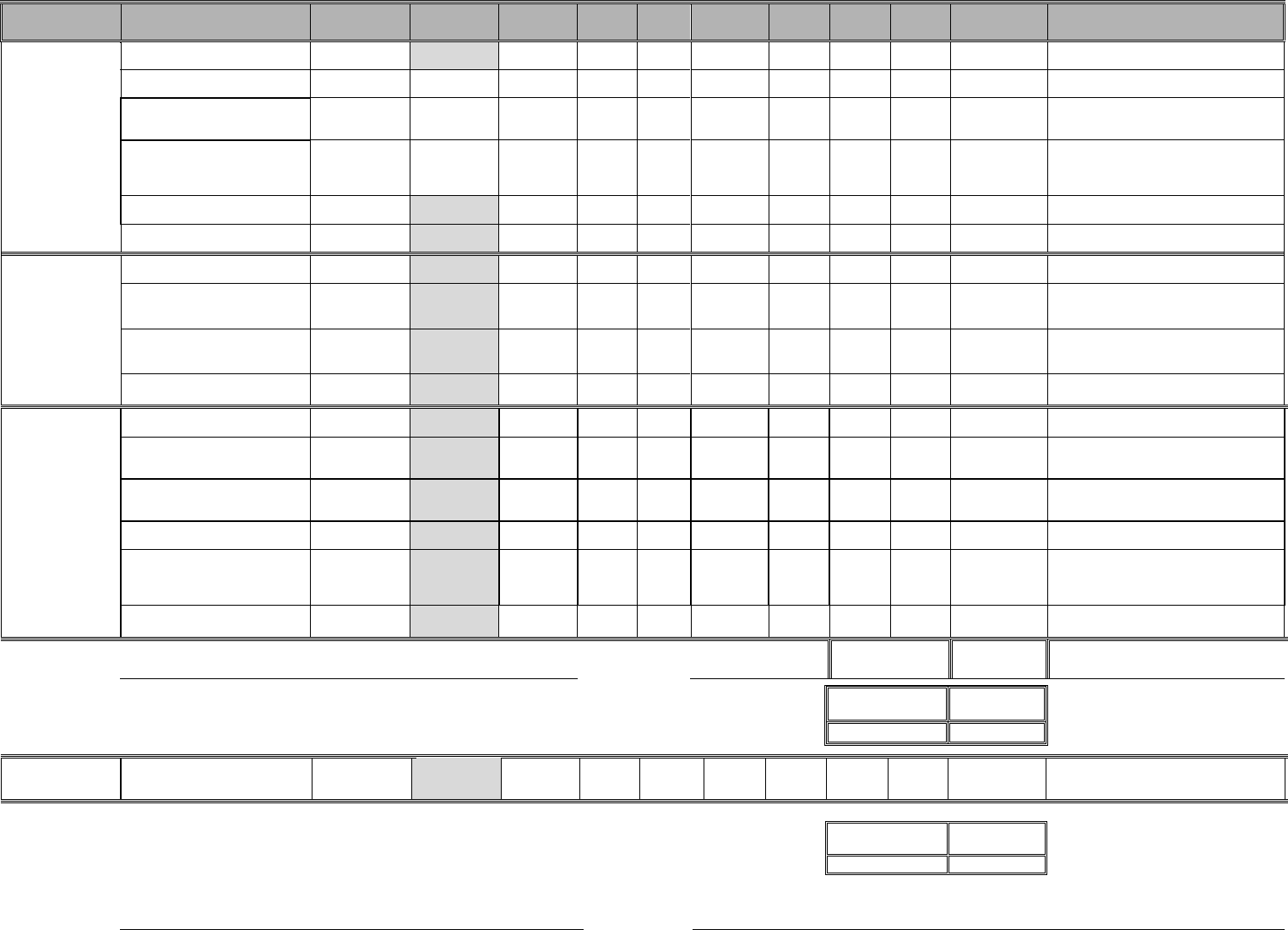
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
TASK
DESCRIPTION
APPROX
TIME
TASKS PER
DAY
MON
TUE
WED
THU
FRI
SAT
SUN
TOTAL
COMMENTS
(WHO IS PROVIDING CARE)
TOILETING
Independent:
No assistance needed
0 min/event
Minimum: Stand-by assist,
supervision, reminders
1-5 min/event
Moderate: 50-70% assist with
clothing, diapers, post-toilet
hygiene or equipment
1-10
min/event
Maximum: Total assist with
clothing, briefs, entire toileting
process. Includes episodes of
incontinence.
1-15
min/event
Catheter: Pouring out bag and
cleaning bag or other supplies.
1-15 min/day
Ostomy: Pouring out and cleaning
bag
1-15 min/day
MOBILITY
Independent: No assistance needed
with/without assistive devices
0 min/day
Minimum: Some supervision,
stand-by, or reminders for safety.
Adjusting devices or restraints
1-10 min/day
Moderate: Needs hands-on assist.
One-person assist with/without
assistive devices
1-15 min/day
Maximum: One or more person
assist, totally dependent.
1-30 min/day
TRANSFERRING
Includes bathing
and Toileting
Transfers
Independent: No assistance needed
with/without assistive devices
0 min/day
Minimum: Some supervision,
stand-by, or reminders for safety.
Adjusting devices or restraints.
1-10 min/day
Moderate: Needs hands-on assist.
One-person assist with/without
assistive devices.
1-15 min/day
Maximum: One or more person
assist, totally dependent.
1-30 min/day
Bed Bound: Frequent turning &
repositioning in the bed. Outside
caregiver 20-40 min/day. Live-in
caregiver 60-90 min/day.
20-40 min/day
60-90 min/day
Hoyer: If hoyer time assessed no
transfer time in other areas.
1-20
min/event
Member Name
AHCCCS ID:
Page 3 Total:
Total minutes
w/o Supervision:
Total Hours:
GENERAL
SUPERVISION
Supervision is based on need, and
can be provided based on member
need identified on Page 1.
X Time/Day
Total minutes
with Supervision:
Total Hours:
Member Name:
AHCCCS ID:
Page 3 of 4
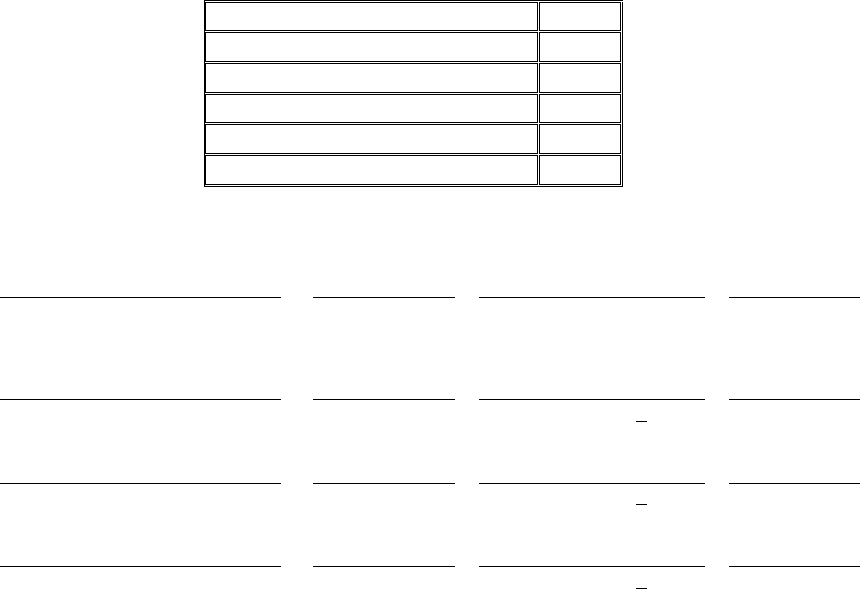
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
ATTENDANT CARE-PERSONAL CARE- HOMEMAKER
WORKSHEET SUMMARY
TOTAL PAID HOURS INDENTIFIED
Page 1 Total Minutes:
0
Page 2 Total Minutes:
0
Page 3 Total Minutes:
0
Supervision (if Applicable)
0
Total Minutes
0
Total Hours
0.00
Case Manager Signature
Original Date
Supervisor Signature >20 hrs
Original Date
Case Manager Signature
1st Review Date
Supervisor Signature >20 hrs
1st Review Date
Case Manager Signature
2nd Review Date
Supervisor Signature >20 hrs
2nd Review Date
Case Manager Signature
3rd Review Date
Supervisor Signature >20 hrs
3rd Review Date
Page 4 of 4
1
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
HCBS NEEDS TOOL (HNT) INSTRUCTIONS
HCBS NEEDS TOOL GUIDELINES:
Attendant Care, Personal Care, and Homemaker services are intended to augment and support
the existing informal care and community services being provided to allow the member to
remain in a home setting.
The HCBS Needs Tool (HNT) is intended to evaluate the member’s functional care needs and
which of those needs will be met by informal support system and which parts will be provided
by the formal paid caregiver.
Prior to authorizing Attendant Care, Personal Care or Homemaker services, the case manager
must complete the Contractor’s assessment tool, the HNT, the Uniform Assessment Tool (UAT)
and the service plan.
The HNT must be completed with direct involvement of the member and/or representative.
Discussion must take place about what care is needed, the average amount of time it takes to
complete that care for the member and the availability of informal supports and community
services to meet those needs. Discussion should include stressors the informal caregivers may be
experiencing in providing care and the supports that can be provided through community
resources as well as Arizona Long Term Care System (ALTCS) services.
Times shown on the HNT are only guidelines that reflect approximate the time frame that it takes
to complete tasks based on general and reasonable expectations in homecare provision. Time
for each category must be based on the evaluation of the member’s individual needs and
informal supports available.
Time above the suggested amount in any category may be assessed but the case manager must
provide an explanation for the amount of time needed to complete that task for the member.
There must be adequate case file documentation to support the assessment and hours authorized.
There must be consistency between the Contractor’s assessment tool, the HNT, the UAT and the
service plan.
After the member’s needs are assessed, the Cost Effectiveness Study (CES) must be calculated to
determine what can be provided within the ALTCS cost effectiveness standards. Services whose
costs are at or below 100% of the cost of institutionalization or those that are expected to be at
this level within 6 months may be authorized.

2
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
COMPLETING THE HCBS NEEDS TOOL
TOP OF FORM – PAGE 1
LIVING SITUATION:
Select appropriate choice based on the member’s situation.
SUPERVISION NEED:
Select one or more of the choices or NA if none of the other choices apply.
Wandering Risk - Member has already been found to leave their home unsafely and/or is
unable to find their way back.
Confused/Disoriented - Member is confused and/or disoriented to the point they are
unable to perform functional activities on the HNT and in fact are at risk if they do, such
as leaving the stove on when cooking, leaving the shower running after a bath, not being
able to judge the temperature of the water for bathing, attempting to walk without
necessary assistive devices, etc.
Unable to call for help, even with lifeline - Member’s medical condition is such that even
with a lifeline system they would be unable to call for help, such as a member in a coma
or on a vent or a member with Dementia who does not understand how the system works.
If member lives alone and one of the applicable choices is selected, a discussion about an
alternative living situation should take place.Consider completing a Care Management Risk
Agreement.
NAME/RELATIONSHIP OF INFORMAL SUPPORTS:
List the individuals who are available to provide informal support.
On the worksheet enter “IFS” on the specific tasks and days for which the informal support is
present to provide the care.
Listing the IFS information is mandatory as it is always necessary to clearly document what care
is already being provided to the member in order to demonstrate what needs remain unmet.
In addition to informal supports, if the member is receiving care from another source, such
as Medicare home health or hospice, be sure to include this.
DAYS/HOURS FAMILY NOT AVAILABLE:
Make note of the time others in the household are away from the home on a regular basis for
other obligations.

3
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
COMPLETING THE HCBS NEEDS TOOL
TASKS
HOUSEKEEPING/CLEANING
Housekeeping includes cleaning tasks necessary to attain and maintain sanitary living conditions
for the member.
ASSESSMENT CONSIDERATIONS
Housekeeping does not include excessive tasks such as mowing the lawn, carpet cleaning,
moving furniture, etc.
For members living alone, housekeeping may apply to the entire residence. The size of the
home may be considered if the member and/or provider are able to show that more than 2
hours per week is necessary to maintain sanitary living conditions.
For members sharing a residence, housekeeping applies only to the areas used by the
member. This area includes the member’s bedroom and one bathroom.
Case managers should staff the case with a supervisor if the member’s paid caregiver is not
maintaining the member’s living area appropriately.
TIME GUIDE: Do not write in the gray areas.
Independent: Member needs no assistance in maintaining sanitary living conditions
Time Guide: 0 min/week.
Member lives with others. Cleaning for member areas only, including the member’s
bedroom and bathroom.
Time Guide: 1 to 60 min/week.
Without Support. Member lives alone. Consider the size of the home.
Time Guide: 1 to 120 min/week.
LAUNDRY
Laundry tasks include preparing clothes to be washed, putting the clothes in the washer, putting
the clothes in the dryer or on the line, and folding/putting away the clothes, with the goal of
maintaining the member’s clothing in a clean manner and neat appearance. These tasks apply
only to member’s clothing and linens.
ASSESSMENT CONSIDERATIONS
Routine changing of bed linens is considered part of bedroom housekeeping.
Caregiver should be completing other activities in the home while the washer/dryer are in
process.
If laundry must be done at Apartment laundry complex and community laundry complex
more time can be given since the caregiver must sit and watch the clothes and cannot perform
other activities during that time.
If a member soils their clothing or bedding due to incontinence, the laundry may need to be
washed more frequently (even daily) which means a single smaller load each time versus
multiple larger loads once a week.

4
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
TIME GUIDE: Do not write in the gray areas.
Independent: No assistance needed
Time Guide: 0 min
Washer/dryer on site:
Time Guide: 1-30 min/week.
Washer is on site but clothes are line dried:
Time Guide: 1-90 min/week.
Laundry is done in apartment complex laundry room:
Laundry facility is off site such as community laundry facility:
Time Guide: 1-120 min/week.
Incontinence Episodes: Soiled clothes and Linens
Time Guide: 1-10 min/day
SHOPPING
Shopping includes grocery shopping, obtaining medications or medical supplies, and household
items for the member. Travel time and time to put away groceries is included.
ASSESSMENT CONSIDERATIONS
If the member is living with informal supports, the informal supports should obtain items for
the member at the same time that they are obtaining items for themselves or others in that
household.
If a family member or other live-in is a paid caregiver, this caregiver is expected to provide
this service efficiently and pick up items for the member at the same time they are shopping
for themselves/household and not make unnecessary extra trips. Some time may be allotted
for these caregivers in picking up items for the member while shopping for their own
household as well.
Efforts should be made to coordinate that medications may be picked up at the same
store/location where they will get their groceries and other household items.
If a caregiver must take the bus or walk to the store more time may allotted to address the
individual situation.
Multiple trips to the grocery store per week or trips to a preferred store further away are
personal preferences and are not a necessity.
Shopping for recreation in not considered a medical necessity.
TIME GUIDE: Do not write in the gray areas.
Lives with Informal Supports / Independent: 0 min/week.
Lives with paid caregivers: 1-5 min/week
Lives alone and needs outside assistance: 1-90 min/week.
MEAL PREPARATION & MEAL CLEAN-UP
Meal preparation includes meal planning, preparing the foods to be cooked or served, and
actually cooking or putting foods together. This task is inclusive of tasks associated with the
time spent putting the meal together before it is brought to the table or is served to member. This
5
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
includes blenderizing or pureeing foods. Cutting foods into appropriate size pieces for the
member to eat is part of Eating/Feeding, not Meal Preparation.
Clean-up includes storing the foods utilized/left over and the cleaning of the dishes involved in
the preparation and presentation of the food.
Alternative Meal Schedule is for members with diabetes or others that eat multiple small meals
throughout the day to maintain proper levels in their bodies for medical reasons. This can
include getting the member an apple or some cheese and crackers or other small meals to help
regulate the body. Adjust time to the appropriate levels based on the situation, for example,
cleaning or cutting up an apple may only take 2 minutes, cutting and putting together cheese and
crackers might only take 5 minutes, etc.
ASSESSMENT CONSIDERATIONS
Ask the member how many times a day s/he eats and needs assistance in the preparation and
cleanup involved with the meals. Some may only eat lunch and dinner and can manage
morning coffee on their own.
Ask the member what they normally eat for breakfast/lunch/dinner. This could give an idea
of the complexity of meals being prepared.
Does the member have any special diet / special food preparation requirements. Are they
eating the same meals as others that live in the home?
Will the member eat more often if this support is put in place? This could help the member if
there are nutritional or weight loss concerns.
If the caregiver will not be at the residence all day, meals can be prepared in advance and left
in a convenient place for the member, such as a lunch or dinner plate can be left in the fridge
and quickly micro-waved, or cold foods can also be left in the fridge or a cooler close to the
member for their convenience. If the caregiver prepares meals for the day early in the day,
time can be assigned for those meals. The feasibility of this ahead of time preparation
depends on whether the member is able to access the prepared meal and serve him/herself.
TIME GUIDE: Do not write in the gray areas.
Independent: 0 min/day.
Breakfast: 1-15 min
Breakfast with others: 1-5 min/day
Lunch: 1-20 min.
Lunch with others: 1-5 min/day
Dinner: 1-30 min.
Dinner with others: 1-5 min/day
Alternative Meal Schedule: 1-10 min per meal.

6
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
EATING/FEEDING
Eating/Feeding is the process of getting oral nourishment from a receptacle (dish, plate, cup,
glass, bottle, etc.) into the body after it is cooked or prepared for eating. This does not include
tube feeding as that is considered a skilled task not performed by a Direct Care Worker.
ASSESSMENT CONSIDERATIONS
How many meals does the member eat per day?
Time for the preparation of meals is calculated in the Meal Preparation category but cutting
foods into appropriate size pieces for the member to eat is considered part of Eating/Feeding.
TIME GUIDE: Do not write in the gray areas.
Independent. Needs no assistance in eating or feeding one’s self.
Time Guide: 0 min/meal.
Minimum. May need assistance to have meal set-up, including cutting food, opening
carton, and/or cueing.
Time Guide: 1-10 min/meal.
Moderate. As above, plus, may need hands-on physical assistance, supervision, or
cueing with 50% to 75% of the meal task, but the member is still able to participate
physically.
Time Guide: 1-15 min/meal.
Maximum. Needs hands-on physical assistance with approximately 75% or more of the
meal task. Total set-up, constant supervision, and/or continual cueing, bringing food to
mouth, or must be fed.
Time Guide: 1-30 min/meal.
BATHING
Bathing is the process of washing, rinsing, and toweling the body or body parts and transferring
in/out of the tub or shower. This includes the ability to get the bath water and/or equipment
ready for bathing in either the shower or tub or at the sink or bedside. Use of assistive devices
such as tub/shower chair, pedal/knee controlled faucets, or long–handled brushes do not
disqualify the client from being independent.
If the client has a problem getting to and from the bathroom to bathe, this should be reflected in
the mobility section and not affect the score for bathing.
Transfer time into the shower/tub is included in the bath time.
Daily bathing of the elderly is not recommended due to damage that occurs to the skin from the
water and the soap. Bathing more than once per day is a personal preference and not a necessity.
ASSESSMENT CONSIDERATIONS
How many times per week does the member bathe (member specific, as needed)?

7
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
A person may not need a full bath (bathtub, shower or bed bath) every day. If a person does
not want to be bathed daily they generally need to at least have their face, underarms and
private areas washed on a daily basis.
Sponge baths can be completed by the member or the caregiver if the member is not able to
use the sponge or wash cloth to clean himself/herself.
A bed bath is for members who are bed bound and cannot get out of the bed to be bathed in a
shower or tub.
Clean up after incontinence episodes would generally be considered under the TOILETING
section as it does not usually require a full bath. If however, the clean up does require a bath,
the frequency and time for this must be included in BATHING.
TIME GUIDE: Do not write in the gray areas.
Independent. The member is able to bathe without any supervision or assistance.
Time Guide: 0 min/day.
Sponge bath. The member does not bathe on these days but still wants to freshen up with
water and a sponge or washcloth.
Time Guide: 1-5 min/day.
Minimum. The member needs minimal supervision and set-up. Needs some cueing or
assistance getting in/out of the tub/shower. May need some assistance with washing back
and/or lower extremities.
Time Guide: 1-15 min/day.
Moderate. The member needs step-by-step cueing or supervision with the entire bathing
process or hands-on assistance with 50% to 75% of the bathing process.
Time Guide: 1-30 min/day.
Maximum. The member is dependent on others for assistance with 75% or more of the
bathing process. May require two or more person assist to get in and out of the
shower/tub or requires the use of a mechanical lift or member is only able to receive bed
baths.
Time Guide: 1-45 min/day.
DRESSING/GROOMING AM & PM
Dressing includes the laying out, taking off, putting on, and fastening of clothing and footwear.
Grooming includes oral hygiene, nail care, shaving and fixing hair.
ASSESSMENT CONSIDERATIONS
Can the member choose their own clothes, put them on, and put on socks and shoes?
If someone lays out the clothes, can the member put them on?
Does the member successfully use assistive devices in dressing, such as reachers, sock
pullers, shoehorns?
While it may be faster for a caregiver to put on a member’s clothes, if the member is still
physically able to do this activity then the member should be considered independent.
Dressing and grooming in the morning is likely to take more time than evening activity.
Not all people get changed multiple times a day. Some people get changed once in the
morning into fresh clothes and may wear and sleep in the same clothing. Examples include:
a house coat, shorts and tee-shirts, or sweat pants, etc.

8
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
For a member with Diabetes, nail care of the feet should only be completed by the member or
a medical professional.
TIME GUIDE: Do not write in the gray areas.
Complete time for the AM section and, if appropriate, give additional time in the PM section.
The time in the AM section is not expected to match the time in the PM section.
Independent. The member does not need assistance with any part of dressing, undressing,
or grooming.
Time Guide: 0 min/task.
Minimum. The member needs some supervision or reminding. Includes selecting and
laying out clothes.
Time Guide: 1-10 min/task.
Moderate. The member needs hands-on assistance by another person, or supervision with
50% to 75% of dressing/grooming activities. Regular assistance with buttons, zippers,
and buckles, socks, and shoes. Regular assistance with fixing hair and/or oral hygiene.
Time Guide: 1-15 min/task.
Maximum. The member needs hands-on assistance with 75% or more of the
dressing/grooming activities. Complete assist with dressing including transfer assist if
needed.
Time Guide: 1-20 min/task.
TOILETING
Toileting tasks include reminders, toileting schedule, the taking off and putting on of clothing
and/or diapers, post-toilet hygiene, use of equipment such as a urinal, and cleaning of a catheter
or ostomy bag.
ASSESSMENT CONSIDERATIONS
It is not healthy/safe to use suppositories or laxatives to have more than one bowel movement
per day. If this is occurring, notify the member’s PCP.
If the member is incontinent but is able to manage his/her own incontinence supplies and
change themselves, then the member is still independent.
The time to pour out the urine from a catheter bag should generally not require more than 15
minutes/day.
The time to take care of a member’s ostomy bag (even when twice a day) should generally
not require more than 15 minutes/day.
TIME GUIDE: Do not write in the gray areas.
Independent. The member does not need assistance in any part of toileting or is able to
manage own incontinence with use of briefs or pads that the member is able to change on
their own.
Time Guide: 0 min/task.
Minimum. The member needs standby assist or supervision with toileting.

9
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
Time Guide: 1-5 min/task.
Moderate. The member needs moderate assistance with clothing, diapers, post-toilet
hygiene, and/or equipment for either continent or incontinent members.
Time Guide: 1-10 min/task.
Maximum. Total assist with clothing, diapers, post-toilet hygiene and/or equipment for
either continent or incontinent members.
Time Guide: 1-15 min/task.
Catheter: The member has catheter and needs assistance to pour out the urine and clean
the bag.
Time Guide: 1-15 min/day.
Ostomy: The member has an ostomy and needs assistance to pour out the feces and clean
or change the bag.
Time Guide: 1-15 min/day.
MOBILITY
Mobility is the extent of the member’s purposeful movement within their residence. The use of
assistive devices such as a wheelchair, walker, or quad cane does not disqualify the member
from being independent, nor does it guarantee an increase in the need for assistance by another
person.
Transfer time is not counted in the mobility section but in the transfer section below.
ASSESSMENT CONSIDERATIONS
Can the member purposely move about his/her residence independently with or without the
use of assistive devices? A member that can propel themselves in a wheel chair should be
considered independent.
Is the member unsafe without the assistance of another person in ambulating?
Does the member have weakness, unstable gait or unstable balance?
TIME GUIDE: Do not write in the gray areas.
The number of times a member is assisted with mobility per day is Not counted; rather an
approximate amount of time spent per day in mobility assistance must be assessed.
Independent. The member is independent in mobility with or without assistive devices.
Time Guide: 0 min/day.
Minimum. The member needs some supervision, standby, or reminders for safety. This
may include adjusting of assistive devices or restraints
Time Guide: 1-10 min/day.
Moderate. The member needs hands-on assistance for safety. One person assist, with or
without assistive devices.
Time Guide: 1-15 min/day.
Maximum. May need one or more persons or may be totally dependent on others for
mobility.
Time Guide: 1-30 min/day.

10
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
TRANSFERRING
Transferring is the member’s ability to move horizontally and/or vertically between the bed,
chair, wheelchair, commode, etc.
ASSESSMENT CONSIDERATIONS
Is the member able to use any mechanical devices such as a walker, cane, or handrails of
wheelchair to assist with transfers?
Is the member unsafe without the assistance of another person in transferring?
Can the member physically participate in the transfer by pivoting, holding on, or bracing
themselves to assist the caregiver?
If a mechanical lift is needed, then all transfer time must be noted in the lift section and not in
the other min-max assistance sections.
TIME GUIDE: Do not write in the gray areas.
The number of times a member is transferred per day is NOT counted (except when
transferred by Lift); rather an approximate amount of time spent per day is transfer
assistance must be assessed. Independent. The member is independent in transfer with
or without assistive devices.
Time Guide: 0 min/day.
Minimum. The member needs some supervision, standby, or reminders for safety. This
may include adjusting of assistive devices or restraints
Time Guide: 1-10 min/day.
Moderate. The member needs hands-on assistance for safety. One person assist, with or
without assistive devices. The member may be able to bear weight and pivot.
Time Guide: 1-15 min/day.
Maximum. May need one or more persons or may be totally dependent on others for
transfers.
Time Guide: 1-30 min/day.
Mechanical Lift: Member requires the use of a mechanical lift. If member transferred by
Lift, time for transfer will be counted in this area only and not in any of the min-max
areas above.
Time Guide: 1-20 min/event
BED -BOUND: Requires frequent turning and repositioning in bed.
Time Guide: 20-90 min/day
GENERAL SUPERVISION
Supervision time must be considered for members who, in the first section of this tool, were
assessed, because of their disability or medical condition, to be at risk of being unsafe if they
were left alone.
ASSESSMENT CONSIDERATIONS
For those needing supervision time, the time assessed should cover the time between the
specific tasks the caregiver is performing and the time the family/IFS is available/willing to
supervise the member.

11
Revision Date: 01/01/16, 03/01/13 Initial Effective Date: 05/01/2012
For example: The member needs around the clock care due to dementia, and has a history of
unsafe behaviors, but the family is unavailable to provide this care 7 AM to 6 PM (11 hours)
Monday through Friday, totaling 55 hours per week of care. If the functional assistance adds
up to 20 hours, then the supervision need would be the remaining 35 hours.
Informal Supports (IFS) must be clearly noted on the tool if they are available and willing to
cover supervision time so it is clear that the member is receiving care and not being left
unattended.
For those receiving supervision time, the caregiver may need to assist with the self-
administration of medications (as applicable), monitoring of the member’s medical condition,
monitoring the member’s level of functioning, oversight of decision making and activities of
daily living, and documentation of the same during this supervision time.
Reminder: Only licensed medical professionals are allowed to be paid to administer or use
discretion/judgment in the dispensing of medications to another person. Family members
working as caregivers who choose to administer medications or set up med-boxes are
allowed to do so but they cannot be paid to do so.
For those receiving supervision time, the caregiver may need to attend medical appointments
with the member, if the member’s family or IFS is not able to attend. Additional time will
not be added as the member’s supervision time has already been calculated to include the
time between the functional needs and the time the family or IFS is available to supervise the
member.
TIME GUIDE
Varies upon the needs of the individual member to fill in the period of time between functional
assistance being provided and when family/IFS is able to supervise the member.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1630
ADMINISTRATIVE STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1630-1
AHCCCS MEDICAL POLICY MANUAL
1630 ADMINISTRATIVE STANDARDS
REVISION DATES: 01/01/16, 03/01/13, 05/01/12, 01/01/11, 02/01/09, 10/01/2007
INITIAL
EFFECTIVE DATE: 10/01/2004
Administrative responsibilities related to case management of enrolled members include the
following:
A. CASE MANAGER QUALIFICATIONS
Individuals hired as case managers must be either:
1. A degreed social worker
2. A licensed registered nurse, OR
3. A person with a minimum of two years’ experience in providing case
management services to persons who are elderly and/or persons with physical or
developmental disabilities.
B. CASE MANAGEMENT PROCEDURES/TECHNICAL
Contractors are responsible for maintaining case management procedures that are
reflective of AHCCCS policy, as defined in this Chapter.
Contractors may develop their own standardized forms and tools for recording
information regarding members’ needs and services. However, all Contractors must
utilize the standardized forms found in this Chapter, including, but not limited to the
Uniform Assessment Tool (Exhibit 1620-3), the Member Service Plan (Exhibit 1620-
13), the Contingency Plan (found in Exhibit 1620-14) and the HCBS Needs Tool
(Exhibit 1620-17).
Contractors will establish a mechanism to ensure that CATS data is entered
accurately and within established timeframes (ten business days of the date the action
took place).
C. TRAINING
Case managers must be provided with adequate orientation and ongoing training on
subjects relevant to the population served by the Contractor. Documentation of
training dates and staff attendance as well as copies of materials used must be
maintained.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1630
ADMINISTRATIVE STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1630-2
AHCCCS MEDICAL POLICY MANUAL
1. Contractors must ensure that there is a structure in place to provide uniform
training to all case managers. This plan should include formal training classes as
well as mentoring-type opportunities for newly hired case managers.
2. Newly hired case managers must be provided orientation and training in a
minimum of the following areas:
a. The role of the case manager in utilizing a member-centered approach to
Arizona Long Term Care System (ALTCS) case management, including
maximizing the role of the member and their family in decision-making
and service planning.
b. The principle of most integrated, least restrictive settings for member
placement.
c. Member rights and responsibilities
d. Case management responsibilities as outlined in this Chapter, including,
but not limited to service planning, contingency plans, reporting service
gaps and Notices of Action.
e. Case management procedures specific to the Contractor.
f. An overview of the AHCCCS/ALTCS program.
g. The continuum of ALTCS services, including available service delivery
options, placement settings and service restrictions/limitations.
h. The Contractor provider network by location, service type and capacity.
Included in this should be information about community resources for
non-ALTCS covered services.
i. Information on local resources for housing, education and employment
services/program that could help members gain greater self-sufficiency in
the areas.
j. Responsibilities related to monitoring for and reporting of quality of care
concerns, including, but not limited to, suspected abuse, neglect and/or
exploitation.
k. General medical information, such as symptoms, medications and
treatments for diagnostic categories common to the ALTCS population
service by the Contractor.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1630
ADMINISTRATIVE STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1630-3
AHCCCS MEDICAL POLICY MANUAL
l. General social service information, such as family dynamics, care
contracting, dealing with difficult people, risk management.
m. Behavioral health information, including identification of member’s
behavioral health needs, covered behavioral health services and how to
access those services within the Contractor’s network and the
requirements for initial and quarterly behavioral health consultations.
n. Pre-Admission Screening and Resident Review (PASRR) process
o. Early and Periodic Screening, Diagnosis and Treatment (EPSDT)
standards for members under the age of 21, and
p. ALTCS management information system Client Assessment Tracking
System (CATS) that maintains member-specific data such as Cost
Effectiveness Studies, Placement/Residence codes, behavioral health
codes, review dates and, for Tribal Contractors, service authorizations.
The level of orientation to CATS will be dependent on the level of direct
usage by the Contractor case managers.
3. In addition to review of areas covered in orientation, all case managers must
also be provided with regular ongoing training on topics relevant to the
population(s) served. The following are examples of topics that could be
covered:
a. Policy updates and new procedures,
b. Refresher training for areas found deficient through the contractor’s
internal monitoring process,
c. Interviewing skills,
d. Assessment/observation skills,
e. Cultural competency,
f. Member rights,
g. Medical/behavioral health issues, and/or
h. Medications – side effects, contraindications and poly-pharmacy issues.
4. Training may also be provided by external sources, for example:
a. Consumer advocacy groups,
CHAPTER 1600
CASE MANAGEMENT
POLICY 1630
ADMINISTRATIVE STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1630-4
AHCCCS MEDICAL POLICY MANUAL
b. Providers (for example, medical or behavioral health), and
c. Accredited training agencies.
5. The Contractor shall ensure that a staff person(s) is designated as the expert(s)
on housing, education and employment issues and resources within the
Contractor’s service area. This individual must be available to assist case
managers with up-to-date information designed to aid members in making
informed decisions about their independent living options.
D. CASELOAD MANAGEMENT
Adequate numbers of qualified and trained case managers must be provided to meet
the needs of enrolled members.
Contractors must have written protocols to ensure newly enrolled ALTCS members
are assigned to a case manager immediately upon enrollment.
MEMBERS WHO ARE ELDERLY AND/OR HAVE PHYSICAL DISABILITIES (E/PD)
Each case manager’s caseload must not exceed a weighted value of 96. The following
formula represents the maximum number of members allowable per E/PD case
manager:
1. For institutionalized members, a weighted value of 1.0 is assigned. Case
managers may have up to 96 institutionalized members (96 x 1.0 = 96).
2. For HCBS (own home) members, a weighted value of 2.2 is assigned. Case
managers may have up to 43 HCBS members (43 x 2.2 = 96 or less).
3. For assisted living facility (ALF) members, a weighted value of 1.8 is assigned.
Case managers may have up to 53 ALF members (53 x 1.8 = 96 or less).
4. For Acute Care Only (ACO) members, a weighted value of 1.0 is assigned.
Case managers may have up to 96 ACO members (96 x 1.0 = 96).

CHAPTER 1600
CASE MANAGEMENT
POLICY 1630
ADMINISTRATIVE STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1630-5
AHCCCS MEDICAL POLICY MANUAL
5. If a mixed caseload is assigned, there can be no more that a weighted value of
96. The following formula is to be used in determining a case manager’s mixed
caseload:
(# of HCBS members x 2.2)
+
(# of ALF members x 1.8)
+
(# of ACO members x 1.0)
+
(# of Nursing Facility (NF) members x 1.0)
96 or less
6. A DDD case manager’s caseload must not exceed a per District average ratio of
1:40 members, regardless of setting.
Caseload Exceptions – Contractors must receive authorization from
AHCCCS/Division of Health Care Management prior to implementing
caseloads whose values exceed those outlined above. Lower caseload sizes may
be established at the discretion of the Contractor and do not require
authorization.
The Contractor’s annual Case Management Plan must describe how caseloads
will be determined and monitored.
E. ACCESSIBILITY
Members and/or member representatives must be provided adequate information in
order to be able to contact the case manager or Contractor office for assistance,
including what to do in cases of emergencies and/or after hours.
A system of back-up case managers must be in place and members who contact an
office when their primary case manager is unavailable must be given the opportunity
to be referred to a back-up for assistance.
There must be a mechanism to ensure members, representatives and providers are
called back in a timely manner when messages are left for case managers.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1630
ADMINISTRATIVE STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1630-6
AHCCCS MEDICAL POLICY MANUAL
F. TIME MANAGEMENT
Contractors must ensure that case managers are not assigned duties unrelated to
member-specific case management for more than 15% of their time if they carry a full
caseload.
G. CONFLICT OF INTEREST
Contractors must ensure that case managers are not:
1. Related by blood or marriage to a member, or any paid caregiver of a member,
on their caseload;
2. Financially responsible for a member on their caseload,
3. Empowered to make financial or health-related decisions on behalf of a member
on their caseload,
4. In a position to financially benefit from the provision of services to a member
on their caseload,
5. Providers of ALTCS services for any member on their caseload, and
6. Individuals who have an interest in, or are employed by, a provider of ALTCS
services for any member on their caseload.
Exceptions to the above may be made under limited circumstances with prior
approval from AHCCCS. A limited circumstance may include a geographic area
where it is unavoidable to have a case manager who may also have a provider
interest.
H. SUPERVISION
A supervisor to case manager ratio must be established that is conducive to a sound
support structure for case managers. Supervisors must have adequate time to train and
review the work of newly hired case managers as well as provide support and
guidance to established case managers.
A system of internal monitoring of the case management program, to include case file
audits and reviews of the consistency of member assessments and service
authorizations, must be established and applied, at a minimum, on a quarterly basis.
Results from this monitoring including the development and implementation of
continuous improvement strategies to address identified deficiencies must be
documented and made available to AHCCCS upon request.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1630
ADMINISTRATIVE STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1630-7
AHCCCS MEDICAL POLICY MANUAL
I. INTER-DEPARTMENTAL COORDINATION
The Contractor should establish and implement mechanisms to promote coordination
and communication across disciplines and departments within their own organization,
with particular emphasis on ensuring coordinated approaches with Medical
Management (MM) and Quality Management (QM). For example, there should be
coordination of information between case management, MM and QM regarding poly-
pharmacy issues to ensure measures are taken to effectively address this issue.
The Contractor should ensure the Medical Director is available as a resource to case
management and that s/he is advised of medical management issues as needed.
J. REPORTING REQUIREMENTS
A Case Management Plan must be submitted annually to AHCCCS on or before
November 15th by all Contractors. Tribal Contractors are not required to submit a
plan. The plan must address how the Contractor will implement and monitor the case
management and administrative standards outlined in this Chapter, including
specialized caseloads.
An evaluation of the Contractor’s Case Management Plan from the previous year
must also be included in the plan, highlighting lessons learned and strategies for
improvement.
EXHIBIT 1630-1
ATTENDANT CARE GUIDELINES
EXHIBIT 1630-1
ATTENDANT CARE GUIDELINES
Review Date: 01/01/16
In developing and/or implementing an Attendant Care assessment tool or process, the following
guidelines should be used:
1. The process must assess the member’s total need for care.
2. The assessment must be done with direct involvement of the member and/or
representative.
3. There must be a discussion about what care is needed, the average amount of time
needed to complete that care and the availability of informal caregivers to assist with
that care. Consideration must be given to the stressors the informal caregivers are
under in providing care and how the provision of ALTCS services to relieve them
may increase their ability to continue with that care.
4. The assessment must allow for individual member needs. Pre-determined/maximum
time limits or task frequencies (for example, maximum of ten minutes for eating or no
more than 1x/week for laundry) cannot be established. Guides may be used as a
starting point, but the case manager must have the freedom to vary from those with
adequate justification.
5. The assessment must address the member’s need for general supervision as well as
specific tasks. If the member is not safe to be alone, this must be considered. For
example, if the member needs around the clock care due to dementia, and has a
history of unsafe behaviors, but the family is unavailable to provide this care 7 AM to
6 PM (11 hours) Monday through Friday, then the attendant care need in this case
begins at 55 hours/week.
6. There can be no differentiation or discrimination in the types of frequencies of service
authorized simply because the member’s caregiver will be a family member or other
live-in person.
7. There must be adequate case file documentation to support the assessment and hours
authorized.
8. After the member’s needs are assessed, the CES must be calculated to determine what
can be provided within the ALTCS cost effectiveness standards. Services whose costs
are at or below 100% of the cost of institutionalization or those that are expected to be
at this level within six months may be authorized.
These same guidelines, with the exception of #5, may be used in assessing a member’s need for
personal care and homemaking services.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1640
TARGETED CASE MANAGEMENT STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1640-1
AHCCCS MEDICAL POLICY MANUAL
1640 TARGETED CASE MANAGEMENT STANDARDS
REVISION DATE: 01/01/16, 01/01/01
REVIEW DATE: 03/01/13
INITIAL
EFFECTIVE DATE: 10/01/2004
Targeted Case Management (TCM) is a covered service provided by the Arizona
Department of Economic Security/Division of Developmental Disabilities (ADES/DDD)
to members with developmental disabilities who are financially eligible for the Title XIX
and Title XXI acute care programs, but do not meet the functional requirements of the
ALTCS program. ADES/DDD provides the TCM services to these members; however,
the members receive their acute care services through the AHCCCS acute care
Contractors. Members must be given a choice of available Contractors and primary care
providers registered with AHCCCS and a choice of case managers from ADES/DDD.
Members are not required to accept case management services.
Members receiving TCM may reside in any of the ADES/DDD approved settings and
may choose the type (on-site visit, telephone, letter) and frequency of case management
contact except under the following circumstances:
1. New ADES/DDD members eligible for TCM must be visited every 90 days for
the first six months. Thereafter, they may choose the frequency of contact.
2. Members receiving non-medically related services funded by the Arizona Early
Intervention Program (AzEIP) must be visited every 90 days.
3. Members residing in any licensed residential setting must be visited every 180
days.
4. Members receiving attendant care provided by the family must receive an initial
30 day visit and a visit every 90 days thereafter, and
5. Members receiving State-funded services must be seen at the time of the annual
Individual Service Plan (ISP).
Targeted case manager responsibilities include, but are not limited to, the following
components:
1. Informing the member of service options, including medical services available
from Contractors based on assessed needs.

CHAPTER 1600
CASE MANAGEMENT
POLICY 1640
TARGETED CASE MANAGEMENT STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1640-2
AHCCCS MEDICAL POLICY MANUAL
2. Coordinating and participating in the plan of care ISP meetings, including
developing, revising and monitoring of the ISP.
3. Locating, coordinating and arranging social, educational and other resources to
meet the member’s needs.
4. Providing necessary information regarding the member’s functioning level and
any changes in the member’s level of functioning to assist the provider in
planning delivering and monitoring services.
5. Providing family members, or other caregivers, the support necessary to obtain
optimal benefits from available services/resources;
6. Providing assistance to strengthen the role of family as primary caregivers,
7. Providing assistance to reunite families with children who are in an alternative
setting whenever possible,
8. Preventing costly, inappropriate and unwanted out-of-home placement, and
9. Identifying services provided by other agencies to eliminate costly duplication.
ADES/DDD administrative responsibilities include, but are not limited to, the following
components:
1. Ensuring staff are qualified and employed in sufficient numbers to meet case
management needs and responsibilities.
2. Ensuring that staff receive initial and ongoing training regarding case
management responsibilities for the TCM program.
3. Identifying new members who are eligible for TCM services and assigning case
managers.
4. Ensuring the member is informed of the assignment of the case manager, when
the case manager is changed and how the case manager can be contacted,
5. Assisting the member with requesting a new case manager from those available
if s/he is dissatisfied with the assigned case manager,
6. Informing ongoing DDD members receiving TCM of visit options and
requesting their decision on the options, and

CHAPTER 1600
CASE MANAGEMENT
POLICY 1640
TARGETED CASE MANAGEMENT STANDARDS
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM 1640-3
AHCCCS MEDICAL POLICY MANUAL
7. Following ADES/DDD prescribed timeframe guidelines for Inventory for Client
and Agency Planning (ICAP) and ISP:
a. The ICAP must be done at the initial visit, when functional limitations are
in question, and upon request from the Medical Director.
b. The ISP must be developed within 12 business days of enrollment to
ADES/DDD and TCM, and completed annually thereafter.
c. The ISP must consist of a narrative including, but not limited to:
i. Identification of member as enrolled in TCM
ii. A description of the type and frequency of contact requested or
required
iii. Identification of TCM contacts made and/or attempted
iv. Demonstration of attempts made to contact member, including
certified letter (when applicable)
v. A description of member abilities, supports and needs, and
vi. Member refusal, when applicable.
The completed ISP must be signed by the member or representative and a copy
of it sent to the member or representative within 15 business days following its
completion. The ISP may be completed by telephone if the member is not
receiving ADES/DDD funded services. When completed by telephone, the ISP
must be send to the member or representative for signature within 15 business
days of the telephone conversation.
8. Establish and maintain an internal monitoring system of the TCM program, and
make results available at the time of annual review, to include a
summary/analysis and corrective action plan, when applicable.
