Presentation SMCI 2018 2019 FULL Benefit Guide With Notices
User Manual:
Open the PDF directly: View PDF ![]() .
.
Page Count: 28
The following descriptions of available benefit
elections options, are purely informational and
have been provided to you for illustrative purposes
only. Payment of benefits will vary from claim to
claim within a particular benefit option and will be
paid at the sole discretion of the applicable
insurance provider for each benefit option. The
terms and conditions of each applicable policy or
certificate of coverage will provide specific details
and will govern in all matters relating to each
particular benefit option described in this
summary. In no case will any information in this
summary amend, modify, expand, enhance,
improve or otherwise change any term, condition
or element of the policies or certificates of
coverage that govern the benefit options described
in this summary.
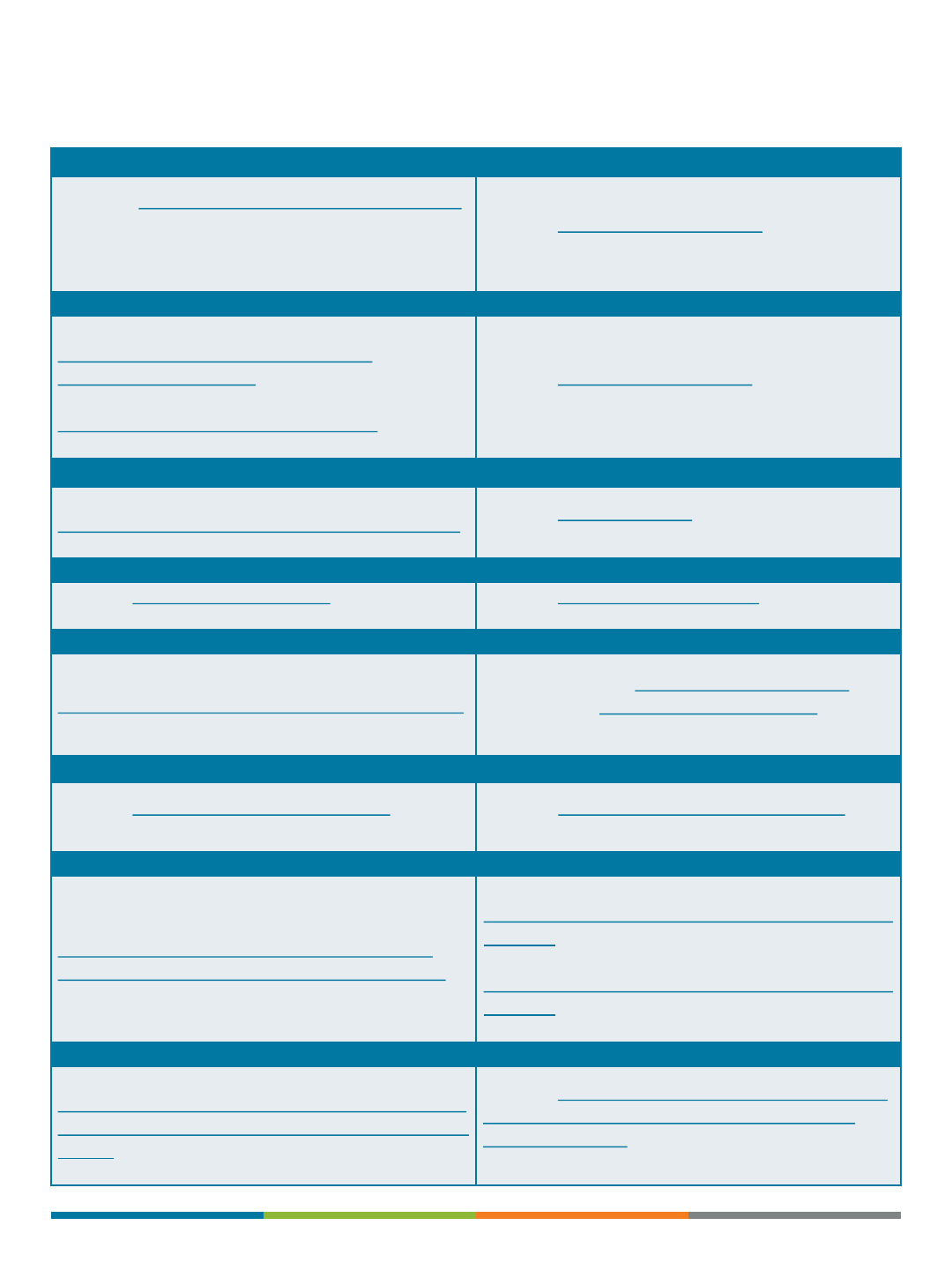
TABLE OF CONTENTS
Presented by:
Additional Contact:
Tammie J. King, RHU, REBC
TJKing@OneDigital.com
803-227-8639 ext. 102
Carol Iverson
Civerson@OneDigital.com
803-227-8639 ext. 103
Enrollment and Eligibility 03
Medical Plans 04
Dental Plan 06
Vision Plan 08
Life Insurance 10
Disability Insurance 12
Special Benefits –FSA 14
Required Notices 16
Confidentiality Notice 22
2
Offering a comprehensive and competitive benefits package is one way we recognize your
contribution to the success of the organization and our role in helping you and your family
to be healthy, feel secure and maintain work/life balance. This enrollment guide has been
designed to provide you with information about the benefit choices available to you.
Remember, open enrollment is your only opportunity each year to make changes to your
elections, unless you or your family members experience an eligible "change in status."
ENROLLMENT AND ELIGIBILITY
How to Enroll in the Plans
Read your materials and make sure you
understand all of the options available.
•Locate your enrollment/change forms or
log on to your benefit administration
system.
•Fill out any necessary personal
information.
•Make your benefit choices.
•If you have questions or concerns,
please contact your HR department.
Whom Can You Add to Your Plan?
Eligible:
•Legally married spouse
•Natural or adopted children up to age
26, regardless of student and marital
status
•Children under your legal guardianship
•Stepchildren
•Children under a qualified medical child
support order
•Disabled children 19 years or older
•Children placed in your physical custody
for adoption
Ineligible:
•Divorced or legally separated spouse
•Common law spouse, even if recognized
by your state
•Domestic partners, unless your
employer states otherwise
•Foster children
•Sisters, brothers, parents or in-laws,
grandchildren, etc.
Change in Status
Generally, you may enroll in the plan, or make
changes to your benefits, when you are first
eligible. However, you can make changes/enroll
during the plan year if you experience a change in
status. As with a new enrollee, you must submit
your paperwork within 30 days of the change or
you will be considered a late enrollee and you may
not be eligible to enroll.
Examples of changes in status:
•You get married, divorced or legally separated
•You have a baby or adopt a child
•You or your spouse takes an unpaid leave of
absence
•You or your spouse has a change in employment
status
•Your spouse dies
•You become eligible for or lose Medicaid
coverage
•Significant increase or decrease in plan benefits
or cost
Open Enrollment is the only
chance to make changes,
unless you experience a
“change in status.”
3

The benefit plan information shown in this guide is illustrative only. To the extent the benefit plan information summarized herein differs from the
underlying plan details specified in the insurance documents that govern the terms and conditions of the plans of insurance described in this
guide, the underlying insurance documents will govern in all cases.
Medical Plans
4

5

The benefit plan information shown in this guide is illustrative only. To the extent the benefit plan information summarized herein differs from the
underlying plan details specified in the insurance documents that govern the terms and conditions of the plans of insurance described in this
guide, the underlying insurance documents will govern in all cases.
Dental Plan
6
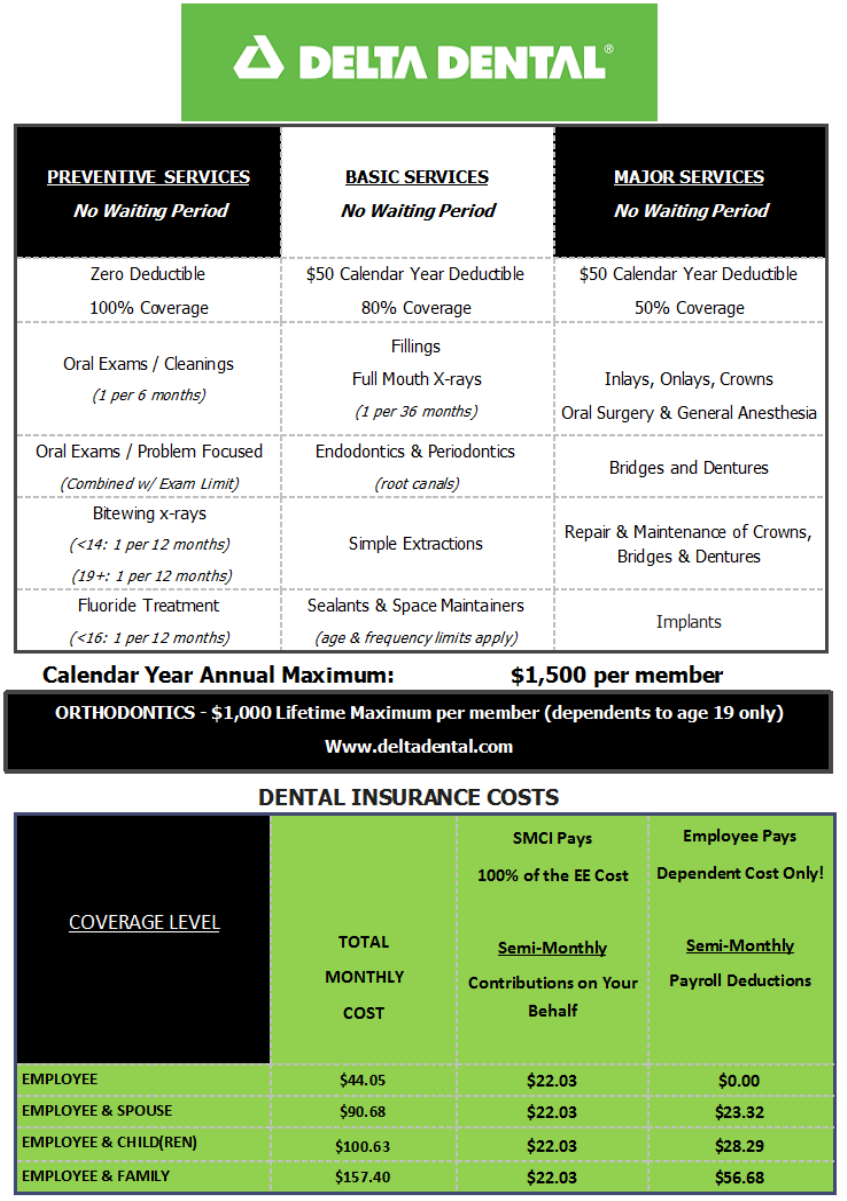
7

The benefit plan information shown in this guide is illustrative only. To the extent the benefit plan information summarized herein differs from the
underlying plan details specified in the insurance documents that govern the terms and conditions of the plans of insurance described in this
guide, the underlying insurance documents will govern in all cases.
Vision Plan
8

9

The benefit plan information shown in this guide is illustrative only. To the extent the benefit plan information summarized herein differs from the
underlying plan details specified in the insurance documents that govern the terms and conditions of the plans of insurance described in this
guide, the underlying insurance documents will govern in all cases.
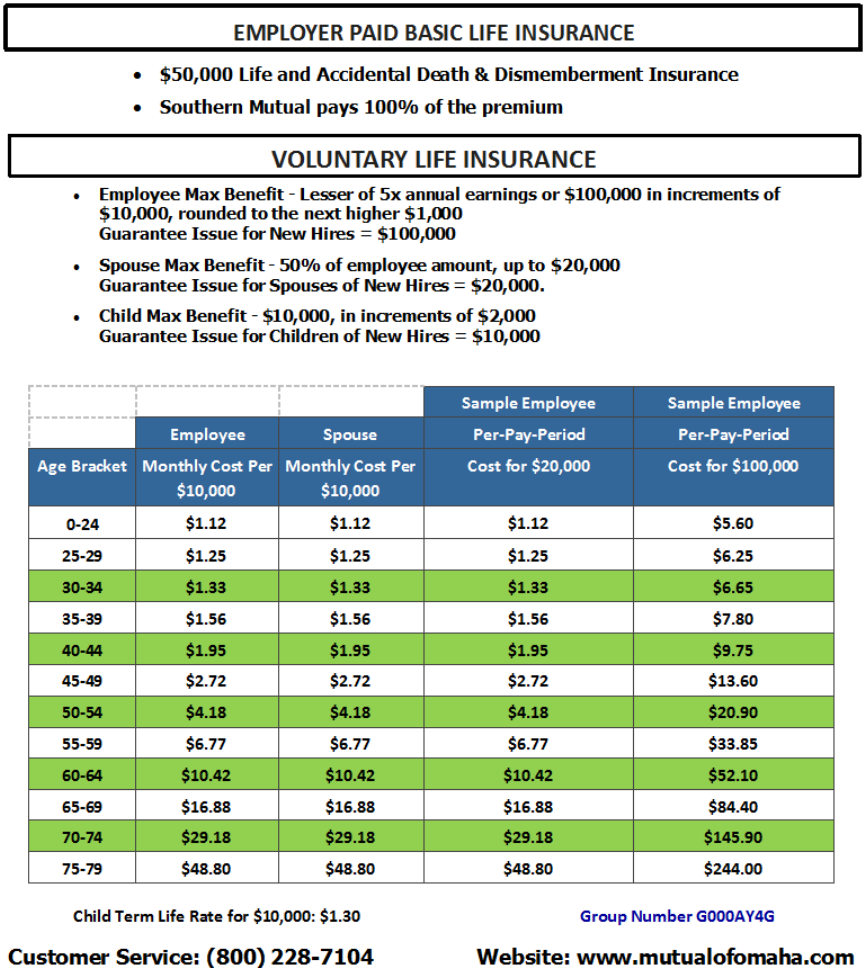
Life / AD&D Plans
10
11

The benefit plan information shown in this guide is illustrative only. To the extent the benefit plan information summarized herein differs from the
underlying plan details specified in the insurance documents that govern the terms and conditions of the plans of insurance described in this
guide, the underlying insurance documents will govern in all cases.
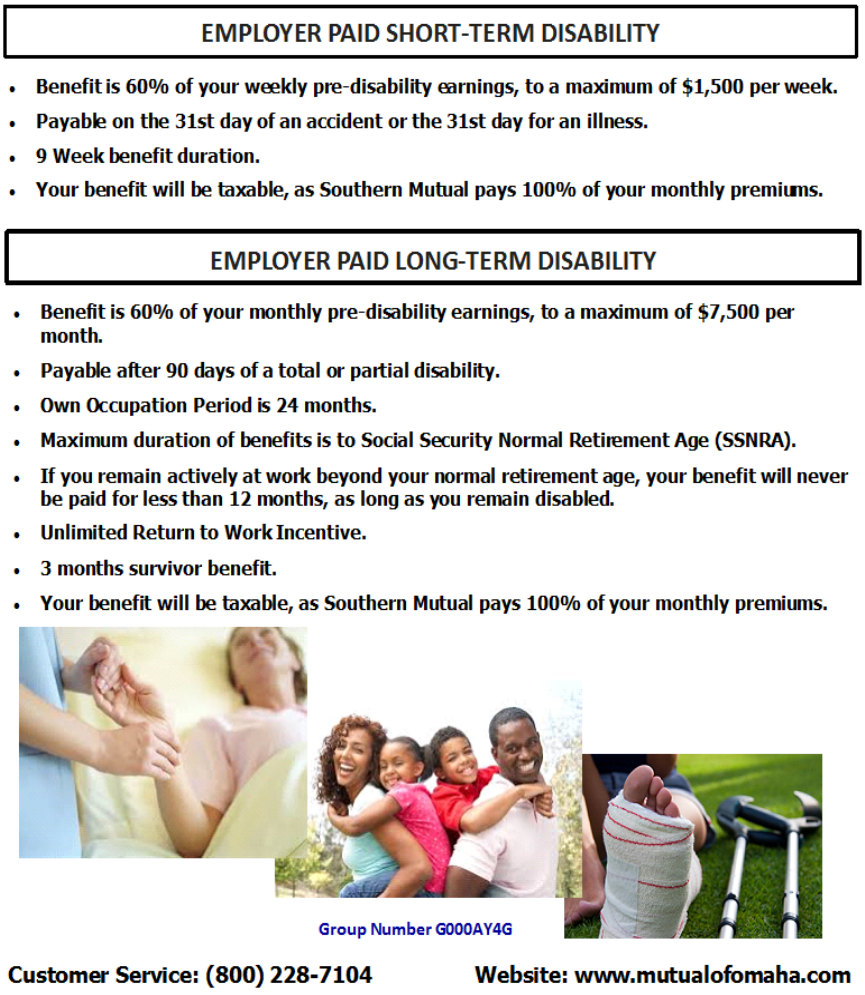
Disability Plans
12
13

The benefit plan information shown in this guide is illustrative only. To the extent the benefit plan information summarized herein differs from the
underlying plan details specified in the insurance documents that govern the terms and conditions of the plans of insurance described in this
guide, the underlying insurance documents will govern in all cases.
Special Benefits
14
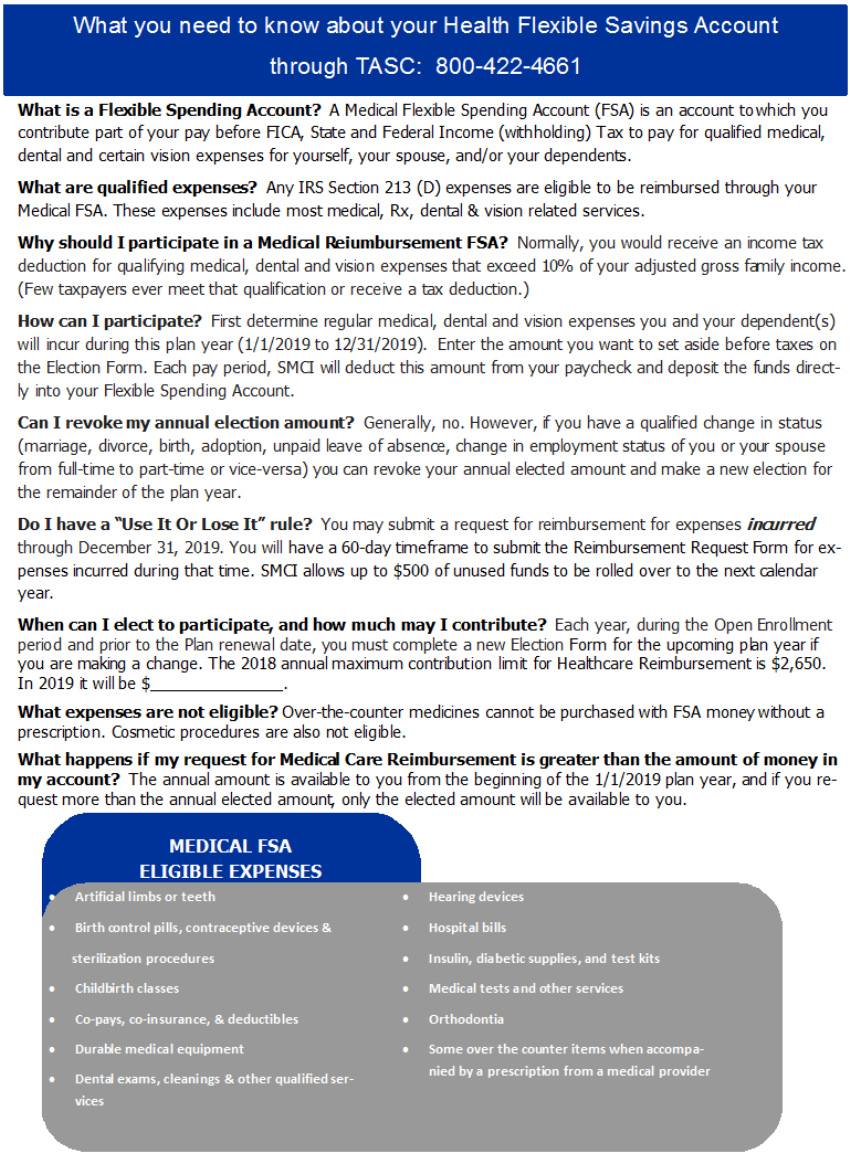
15

REQUIRED NOTICES
Newborn and Mothers’
Health Protection Act
Group health plans and health insurance issuers
generally may not, under federal law restrict
benefits for any hospital length of stay in
connection with childbirth for the mother or
newborn child to less than 48 hours following
vaginal delivery, or less than 96 hours following
a cesarean section. However, federal law
generally does not prohibit the mother’s or
newborn’s attending provider, after consulting
with the mother, from discharging the mother
or newborn earlier than 48 hours (or 96 hours
as applicable). In any case, plans and issuers
may not, under federal law, require that a
provider obtain authorization from the plan or
the issuer for prescribing a length of stay not in
excess of 48 hours (or 96 hours).
Women’s Health and
Cancer Rights Act
In October 1998, Congress enacted the Women’s
Health and Cancer Rights Act of 1998. This notice
explains some important provisions of the Act.
Please review this information carefully. As specified
in the Women’s Health and Cancer Rights Act, a plan
participant or beneficiary who elects breast
reconstruction in connection with a covered
mastectomy is also entitled to the following benefits:
1. All stages of reconstruction of the breast on which
the mastectomy has been performed: 2. Surgery and
reconstruction of the other breast to produce a
symmetrical appearance; and 3. Prostheses and
treatment of physical complications of the
mastectomy , including lymphedemas. Health plans
must provide coverage of mastectomy related
benefits in a manner to determine in consultation
with the attending physician and the patient.
Coverage for breast reconstruction and related
services may be subject to deductibles and insurance
amounts that are consistent with those that apply to
other benefits under the plan.
16

REQUIRED CHIP NOTICE
Alabama –Medicaid Arkansas –Medicaid
Website:
http://myalhipp.com/
Phone: 1
-855-692-5447
Website: http://myarhipp.com/
Phone: 1-855-MyARHIPP (855-692-7447)
Alaska –Medicaid
Colorado –Health First Colorado
(Colorado’s Medicaid Program) & Child Health
Plan Plus (CHP+)
The AK Health Insurance Premium Payment
Program
Website:
http://myakhipp.com/
Phone: 1
-866-251-4861
Email:
CustomerService@MyAKHIPP.com
Medicaid Eligibility:
http://dhss.alaska.gov/dpa/Pages/medicaid/default.aspx
Health First Colorado Website:
https://www.healthfirstcolorado.com/
Health First Colorado Member Contact Center:
1-800-221-3943/ State Relay 711
CHP+: Colorado.gov/HCPF/Child-Health-Plan-Plus
CHP+ Customer Service: 1-800-359-1991/
State Relay 711
Premium Assistance Under Medicaid and the
Children’s Health Insurance Program (CHIP)
If you or your children are eligible for Medicaid or CHIP and you’re eligible for health coverage from your
employer, your state may have a premium assistance program that can help pay for coverage, using funds
from their Medicaid or CHIP programs. If you or your children aren’t eligible for Medicaid or CHIP, you
won’t be eligible for these premium assistance programs but you may be able to buy individual insurance
coverage through the Health Insurance Marketplace. For more information, visit www.healthcare.gov.
If you or your dependents are already enrolled in Medicaid or CHIP and you live in a State listed below,
contact your State Medicaid or CHIP office to find out if premium assistance is available.
If you or your dependents are NOT currently enrolled in Medicaid or CHIP, and you think you or any of your
dependents might be eligible for either of these programs, contact your State Medicaid or CHIP office or
dial 1-877-KIDS NOW or www.insurekidsnow.gov to find out how to apply. If you qualify, ask your state if
it has a program that might help you pay the premiums for an employer-sponsored plan.
If you or your dependents are eligible for premium assistance under Medicaid or CHIP, as well as eligible
under your employer plan, your employer must allow you to enroll in your employer plan if you aren’t
already enrolled. This is called a “special enrollment” opportunity, and you must request coverage within
60 days of being determined eligible for premium assistance. If you have questions about enrolling in your
employer plan, contact the Department of Labor at www.askebsa.dol.gov or call 1-866-444-EBSA (3272).
If you live in one of the following states, you may be eligible for assistance paying your employer health
plan premiums. The following list of states is current as of July 31, 2018. Contact your State for more
information on eligibility –
17

REQUIRED CHIP NOTICE (CONT)
Florida –Medicaid Maine –Medicaid
Website:
http://flmedicaidtplrecovery.com/hipp/
Phone: 1
-877-357-3268
Website:
http://www.maine.gov/dhhs/ofi/public-
assistance/index.html
Phone: 1
-800-442-6003
TTY: Maine relay 711
Georgia –Medicaid Massachusetts –Medicaid and CHIP
Website:
http://dch.georgia.gov/medicaid
-
Click on Health Insurance Premium Payment
(HIPP)
Phone: 404
-656-4507
Website:
http://www.mass.gov/eohhs/gov/departments/ma
sshealth/
Phone: 1
-800-862-4840
Indiana –Medicaid Minnesota –Medicaid
Healthy Indiana Plan for low-income adults 19-64
Website: http://www.in.gov/fssa/hip/
Phone: 1-877-438-4479
All other Medicaid
Website: http://www.indianamedicaid.com
Phone 1-800-403-0864
Website:
http://mn.gov/dhs/people-we-
serve/seniors/health
-care/health-care-
programs/programs
-and-services/medical-
assistance.jsp
Phone: 1
-800-657-3739
Iowa –Medicaid Missouri –Medicaid
Website:
http://dhs.iowa.gov/ime/members/medicaid-a-to-
z/hipp
Phone: 1-888-346-9562
Website:
https://www.dss.mo.gov/mhd/participants/pages/h
ipp.htm
Phone: 573
-751-2005
Kansas –Medicaid Montana –Medicaid
Website: http://www.kdheks.gov/hcf/
Phone: 1-785-296-3512
Website:
http://dphhs.mt.gov/MontanaHealthcarePrograms/
HIPP
Phone: 1
-800-694-3084
Kentucky –Medicaid Nebraska –Medicaid
Website: http://chfs.ky.gov/dms/default.htm
Phone: 1-800-635-2570
Website:
http://www.ACCESSNebraska.ne.gov
Phone: (855) 632
-7633
Lincoln: (402) 473
-7000
Omaha: (402) 595
-1178
Louisiana –Medicaid Nevada –Medicaid
Website:
http://dhh.louisiana.gov/index.cfm/subhome/1/n/331
Phone: 1
-888-695-2447
Medicaid Website: https://dhcfp.nv.gov
Medicaid Phone: 1-800-992-0900
18
REQUIRED CHIP NOTICE (CONT)
New Hampshire –Medicaid Rhode Island –Medicaid
Website: https://www.dhhs.nh.gov/ombp/nhhpp/
Phone: 603-271-5218
Hotline: NH Medicaid Service Center at 1-888-
901-4999
Website:
http://www.eohhs.ri.gov/
Phone: 855
-697-4347
New Jersey –Medicaid and CHIP South Carolina –Medicaid
Medicaid Website:
http://
www.state.nj.us/humanservices/
dmahs
/clients/medicaid/
Medicaid Phone: 609
-631-2392 CHIP Website:
http://www.njfamilycare.org/index.html
CHIP Phone: 1
-800-701-0710
Website:
https://www.scdhhs.gov
Phone: 1
-888-549-0820
New York –Medicaid South Dakota - Medicaid
Website:
https://www.health.ny.gov/health_care/medicaid/
Phone: 1
-800-541-2831
Website:
http://dss.sd.gov
Phone: 1
-888-828-0059
North Carolina –Medicaid Texas –Medicaid
Website:
https://dma.ncdhhs.gov/
Phone: 919
-855-4100
Website:
http://gethipptexas.com/
Phone: 1
-800-440-0493
North Dakota –Medicaid Utah –Medicaid and CHIP
Website:
http://www.nd.gov/dhs/services/medicalserv/medicaid/
Phone: 1
-844-854-4825
Medicaid Website:
https://medicaid.utah.gov/
CHIP Website:
http://health.utah.gov/chip
Phone: 1
-877-543-7669
Oklahoma –Medicaid and CHIP Vermont–Medicaid
Website:
http://www.insureoklahoma.org
Phone: 1
-888-365-3742
Website:
http://www.greenmountaincare.org
Phone: 1
-800-250-8427
Oregon –Medicaid Virginia –Medicaid and CHIP
Website:
http://healthcare.oregon.gov/Pages/index.aspx
http://www.oregonhealthcare.gov/index
-es.html
Phone: 1
-800-699-9075
Medicaid Website:
http://www.coverva.org/programs_premium_assist
ance.cfm
Medicaid Phone: 1
-800-432-5924 CHIP Website:
http://www.coverva.org/programs_premium_assist
ance.cfm
CHIP Phone: 1
-855-242-8282
Pennsylvania –Medicaid Washington –Medicaid
Website:
http://www.dhs.pa.gov/provider/medicalassistance
/healthinsurancepremiumpaymenthippprogram/ind
ex.htm
Phone: 1
-800-692-7462
Website:
http://www.hca.wa.gov/free-or-low-cost-
health
-care/program-administration/premium-
payment
-program
Phone: 1
-800-562-3022 ext. 15473
19

REQUIRED CHIP NOTICE (CONT)
West Virginia –Medicaid Wyoming –Medicaid
Website:
http://mywvhipp.com/
Toll
-free phone: 1-855-MyWVHIPP
(
1-855-699-8447)
Website:
https://wyequalitycare.acs-inc.com/
Phone: 307
-777-7531
Wisconsin –Medicaid and CHIP
Website:
https://www.dhs.wisconsin.gov/publications/p1/p1
0095.pdf
Phone: 1
-800-362-3002
To see if any other states have added a premium assistance program since July 31, 2018, or for more
information on special enrollment rights, contact either:
U.S. Department of Labor
Employee Benefits Security Administration
www.dol.gov/agencies/ebsa
1-866-444-EBSA (3272)
U.S. Department of Health and Human Services
Centers for Medicare & Medicaid Services
www.cms.hhs.gov
1-877-267-2323, Menu Option 4, Ext. 61565
PAPERWORK REDUCTION ACT STATEMENT
According to the Paperwork Reduction Act of 1995 (Pub. L. 104-13) (PRA), no persons are required to
respond to a collection of information unless such collection displays a valid Office of Management and
Budget (OMB) control number. The Department notes that a Federal agency cannot conduct or sponsor a
collection of information unless it is approved by OMB under the PRA, and displays a currently valid OMB
control number, and the public is not required to respond to a collection of information unless it displays a
currently valid OMB control number. See 44 U.S.C. 3507. Also, notwithstanding any other provisions of law,
no person shall be subject to penalty for failing to comply with a collection of information if the collection of
information does not display a currently valid OMB control number. See 44 U.S.C. 3512.
The public reporting burden for this collection of information is estimated to average approximately seven
minutes per respondent. Interested parties are encouraged to send comments regarding the burden
estimate or any other aspect of this collection of information, including suggestions for reducing this
burden, to the U.S. Department of Labor, Employee Benefits Security Administration, Office of Policy and
Research, Attention: PRA Clearance Officer, 200 Constitution Avenue, N.W., Room N-5718, Washington, DC
20210 or email ebsa.opr@dol.gov and reference the OMB Control Number 1210-0137.
(OMB Control Number 1210-0137 (expires 12/31/2019).
20
HIPAA Notice
HIPAA Privacy Notices
HIPAA requires group health plans to provide a notice of current privacy practices regarding protected personal
health information (PHI) to enrolled participants. All employers must distribute HIPAA Privacy Notices if the plan is
self-funded or if the plan is fully- insured and the employer has access to PHI. If the employer maintains a benefits
website, the HIPAA Privacy Notice must be included on the website.
The HIPAA Privacy Notice must be written in plain language and must describe three things: (1) the use and
disclosures of PHI that may be made by the group health plan; (2) plan participants’ privacy rights; and (3) the group
health plan’s legal responsibilities with respect to the PHI.
The Department of Health and Human Services (HHS) has developed three different model Privacy Notices for
health plans to choose from: booklet version, layered version, and full-page version.
More information can be found at: https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/privacy-
practices-for-protected-health-information/index.html
Link to model notice: http://www.hhs.gov/sites/default/files/ocr/privacy/hipaa/nppbooklet_health_plan.pdf
Link to OneDigital’s privacy policy: https://www.onedigital.com/privacy-policy/
Model Special Enrollment Notice
The following is language that group health plans may use as a guide when crafting the special enrollment notice: If
you are declining enrollment for yourself or your dependents (including your spouse) because of other health
insurance or group health plan coverage, you may be able to enroll yourself and your dependents in this plan if you
or your dependents lose eligibility for that other coverage (or if the employer stops contributing toward your or
your dependents’ other coverage). However, you must request enrollment within the appropriate time period that
applies under the plan after you or your dependents’ other coverage ends (or after the employer stops contributing
toward the other coverage). In addition, if you have a new dependent as a result of marriage, birth, adoption, or
placement for adoption, you may be able to enroll yourself and your dependents. However, you must request
enrollment within the appropriate time period that applies under the plan after the marriage, birth, adoption, or
placement for adoption. To request special enrollment or obtain more information, contact the appropriate plan
representative.
More information can be found at: https://www.dol.gov/agencies/ebsa/about-ebsa/our-activities/resource-
center/faqs/hipaa-compliance
Link to model notice: https://www.dol.gov/sites/default/files/ebsa/about-ebsa/our-activities/resource-
center/publications/compliance-assistance-guide-appendix-c.pdf
For additional information on your employer’s privacy policy, please contact your HR department.
21

CONFIDENTIALITY NOTICE
OneDigital Health andBenefits, a division of Digital Insurance,LLCdoes not sell or share any
informationwe learn aboutour clients andunderstands you mayhave to answer sensitive
questions about your medical history, physical condition and personal health habits as
required by our insurance carrier partners.
We collect nonpublic personal information from the followingsources:
•Information from you, including data provided on applications or other forms, such as
name, address, telephone number, date of birth and Social Security number
•Information from your transactions with us and/or our partners such as policy coverage,
premium,claim, and payment history.
OneDigital Health andBenefits recognizes the importance of safeguarding the privacy
of our clients and prospective clients, and we pledge to protect the confidential
nature of your personal information. We understandourability to provide access to
affordable health insurance to businesses and individuals can only succeed with an
environment of complete trust.
In the course of business, we may disclose all or part of your customer information without
your permission to the followingpersons or entities for the following reasons:
•To an insurance carrier, agent or credit reporting agency to detect, prevent or
prosecute actual or potential criminal activity, fraud, misrepresentation,
unauthorized transactions, claims or other liabilities in connection with an
insurance transaction.
•To a medical care institution or medical professional to verify coverage or benefits,
to inform you of a medical problem of which you may or maynot be aware or to
conduct an audit that would enable us to verify treatment.
•To an insurance regulatory authority, law enforcement or other governmental
authorityto protect our interests in detecting, preventing or prosecuting actual
or potential criminal activity, fraud, misrepresentation,unauthorized
transactions, claims or other liabilities in connection with an insurance
transaction.
•To a third party, for any other disclosures requiredor permitted by law. We may disclose
all of the informationthat we collect about you, as described above.
Our practices regarding information confidentiality and security: We restrict access to
your customer informationonly to those individuals who need it to provide you with
products or services, or to otherwise service your account. In addition, we have
security measures in place to protect against the loss, misuse and/or unauthorized
alternation of the customer information underour control, includingphysical, electronic
and procedural safeguardsthat meet or exceed applicable federaland state standards.
22
Glossary of Health Coverage and Medical Terms
This glossary defines many commonly used terms, but isn’t a full list. These glossary terms and definitions are
intended to be educational and may be different from the terms and definitions in your plan or health insurance
policy. Some of these terms also might not have exactly the same meaning when used in your policy or plan, and in
any case, the policy or plan governs. (See your Summary of Benefits and Coverage for information on how to get
a copy of your policy or plan document.)
Underlined text indicates a term defined in this Glossary.
See page 6 for an example showing how deductibles, coinsurance and out-of-pocket limits work together in a real
life situation.
Allowed Amount
This is the maximum payment the plan will pay for a
covered health care service. May also be called "eligible
expense", "payment allowance", or "negotiated rate".
Copayment
Afixed amount (for example, $15) you pay for a covered
health care service, usually when you receive the service.
The amount can vary by the type of covered health care
service.
Balance Billing
When a provider bills you for the balance remaining on
the bill that your plan doesn’t cover. This amount is the
difference between the actual billed amount and the
allowed amount. For example, if the provider’s charge is
$200 and the allowed amount is $110, the provider may
bill you for the remaining $90. This happens most often
when you see an out-of-network provider (non-preferred
provider). A network provider (preferred provider) may
not bill you for covered services.
A request for a benefit (including reimbursement of a
Cost-sharing Reductions
Discounts that reduce the amount you pay for certain
services covered by an individual plan you buy through
the Marketplace. You may get a discount if your income
is below a certain level, and you choose a Silver level
health plan or if you're a member of a federally-
recognized tribe, which includes being a shareholder in an
Alaska Native Claims Settlement Act corporation.
Coinsurance
Your share of the costs
of a covered health care
service, calculated as a
percentage (for
example, 20%) of the
allowed amount for the Jane pays
20%
Her plan pays
80%
service. You generally
pay coinsurance plus (See page 6 for a detailed example.)
any deductibles you owe. (For example, if the health
insurance or plan’s allowed amount for an office visit is
$100 and you’ve met your deductible, your coinsurance
payment of 20% would be $20. The health insurance or
plan pays the rest of the allowed amount.)
OMB Control Numbers 1545-2229, 1210-0147, and 0938-1146
Glossary of Health Coverage and Medical Terms Page 1 of 6
Claim
health care expense) made by you or your health care
provider to your health insurer or plan for items or
services you think are covered.
Cost Sharing
Your share of costs for services that a plan covers that
you must pay out of your own pocket (sometimes called
“out-of-pocket costs”). Some examples of cost sharing
are copayments, deductibles, and coinsurance. Family
cost sharing is the share of cost for deductibles and out-
of-pocket costs you and your spouse and/or child(ren)
must pay out of your own pocket. Other costs, including
your premiums, penalties you may have to pay, or the
cost of care a plan doesn’t cover usually aren’t considered
cost sharing.
Appeal
A request that your health insurer or plan review a
decision that denies a benefit or payment (either in whole
or in part).
Complications of Pregnancy
Conditions due to pregnancy, labor, and delivery that
require medical care to prevent serious harm to the health
of the mother or the fetus. Morning sickness and a non-
emergency caesarean section generally aren’t
complications of pregnancy.
23
Formulary
A list of drugs your plan covers. A formulary may
include how much your share of the cost is for each drug.
Your plan may put drugs in different cost sharing levels
or tiers. For example, a formulary may include generic
drug and brand name drug tiers and different cost sharing
amounts will apply to each tier.
A complaint that you communicate to your health insurer
Habilitation Services
Health care services that help a person keep, learn or
improve skills and functioning for daily living. Examples
include therapy for a child who isn’t walking or talking at
the expected age. These services may include physical
and occupational therapy, speech-language pathology,
and other services for people with disabilities in a variety
of inpatient andor outpatient settings.
Diagnostic Test
Tests to figure out what your health problem is. For
example, an x-ray can be a diagnostic test to seeif you
have a broken bone.
A contract that requires a health insurer to pay some or
Emergency Medical Condition
An illness,injury, symptom (including severe pain), or
condition severe enough to risk serious danger to your
health if you didn’t get medical attention right away. If
you didn’t get immediate medical attention you could
reasonably expect one of the following: 1) Your health
would be put in serious danger; or 2) You would have
serious problems with your bodily functions; or 3) You
would have serious damage to any part or organof your
body.
Home Health Care
Health care services and supplies you get in your home
under your doctor’s orders. Services may be provided by
nurses, therapists, social workers, or other licensed health
care providers.Home health care usually doesn’t include
help with non-medical tasks, such as cooking, cleaning, or
driving.
Services to provide comfort and support for persons in
Hospitalization
Care in a hospital that requires admission as an inpatient
and usually requires an overnight stay. Some plans may
consider an overnight stay for observation as outpatient
care insteadof inpatient care.
Emergency Room Care / Emergency Services
Services to check for an emergency medical condition and
treat you to keep an emergency medical condition from
getting worse. These services may be provided in a
licensed hospital’s emergency room or other place that
provides care for emergency medical conditions.
Glossary of Health Coverage and Medical Terms Page 2 of 6
Hospital Outpatient Care
Care in a hospital that usually doesn’t require an
overnight stay.
Hospice Services
the last stages of a terminal illness and their families.
Emergency Medical Transportation
Ambulance services for an emergency medical
condition. Types of emergency medical transportation
may include transportation by air, land, or sea. Your
plan may not cover all types of emergency medical
transportation, or may pay less for certain types.
Health Insurance
all of your health care costs in exchange for a premium.
A health insurance contract may also be called a “policy”
or “plan”.
Durable Medical Equipment (DME)
Equipment and supplies ordered by a health care provider
for everyday or extended use. DME may include: oxygen
equipment, wheelchairs, and crutches.
Grievance
or plan.
Excluded Services
Health care services that your plan doesn’t pay for or
cover.
Deductible
An amount you could owe
during a coverage period
(usually one year) for
covered health care
services before your plan
begins to pay. An overall
deductible applies to all or
almost all covered items
and services. A plan with
an overall deductible may
Jane pays Her plan pays
100% 0%
(See page 6 for a detailed
example.)
also have separate deductibles that apply to specific
services or groups of services. A plan may also have only
separate deductibles. (For example, if your deductible is
$1000, your plan won’t pay anything until you’ve met
your $1000 deductible for covered health care services
subject to the deductible.)
24
Individual Responsibility Requirement
Sometimes called the “individual mandate”, the duty you
may have to be enrolled in health coverage that provides
minimum essential coverage. If you don’t have minimum
Minimum Essential Coverage
Health coverage that will meet the individual
responsibility requirement. Minimum essential coverage
generally includes plans, health insurance available
essential coverage, you may have to pay a penalty when through the Marketplace or other individual market
policies, Medicare, Medicaid, CHIP, TRICARE, and
certain other coverage.
you file your federal income tax return unless you qualify
for a health coverage exemption.
In-network Coinsurance
Your share (for example, 20%) of the allowed amount
for covered healthcare services. Your share is usually
lower for in-network covered services.
In-network Copayment
A fixed amount (for example, $15) you pay for covered
health care services to providers who contract with your
health insurance or plan.In-network copayments usually Network
The facilities, providers and suppliers your health insurer
or plan has contracted with to provide health care
services.
are less than out-of-network copayments.
A provider who has a contract with your health insurer or
plan. You will pay less if you see a provider in the
“participating provider.”
Orthotics and Prosthetics
Leg, arm, back and neck braces, artificial legs, arms, and
eyes, and external breast prostheses after a mastectomy.
These services include: adjustment, repairs, and
replacements required because of breakage, wear, loss, or
a change in the patient’s physical condition.
Maximum Out-of-pocket Limit
Yearly amount the federal government sets as the most
each individual or family can be required to pay in cost
sharing during the plan year for covered, in-network
services. Applies to most types of health plans and
insurance. This amount may be higher than the out-of-
pocket limits stated for your plan.
Out-of-network Copayment
Afixed amount (for example, $30) you pay for covered
health care services from providers who do not contract
with your health insurance or plan. Out-of-network
copayments usually are more than in-network
copayments.
Glossary of Health Coverage and Medical Terms Page 3 of 6
Medically Necessary
Health care services or supplies needed to prevent,
diagnose, or treat an illness, injury, condition, disease, or
its symptoms, including habilitation, and that meet
accepted standards of medicine.
Out-of-network Coinsurance
Your share (for example, 40%) of the allowed amount
for covered health care services to providers who don’t
contract with your health insurance or plan. Out-of-
network coinsurance usually costs you more than in-
network coinsurance.
Network Provider (Preferred Provider)
plan who has agreed to provide services to members of a
network. Also called “preferred provider” or
Marketplace
A marketplace for health insurance where individuals,
families and small businesses can learn about their plan
options; compare plans based on costs, benefits and other
important features; apply for and receive financial help
with premiums and cost sharing based on income; and
choose a plan and enroll in coverage. Also known as an
“Exchange”. The Marketplace is run by the state in some
states and by the federal government in others. In some
states, the Marketplace also helps eligible consumers
enroll in other programs, including Medicaid and the
Children’s Health Insurance Program (CHIP). Available
online, by phone, and in-person.
Minimum Value Standard
A basic standard to measure the percent of permitted
costs the plan covers. If you’re offered an employer plan
that pays for at least 60% of the total allowed costs of
benefits, the plan offers minimum value and you may not
qualify for premium tax credits and cost sharing
reductions to buy a plan from the Marketplace.
25
Premium
The amount that must be paid for your health insurance
or plan. You andor your employer usually pay it
monthly, quarterly, or yearly.
Financial help that lowers your taxes to help you and
this help if you get health insurance through the
Out-of-pocket Limit
The most you could
pay during a coverage
period (usually one year)
for your share of the
costs of covered
services. After you
meet this limit the
Prescription Drug Coverage
Coverage under a plan that helps pay for prescription
drugs. If the plan’s formulary uses “tiers” (levels),
prescription drugs are grouped together by type or cost.
The amount you'll pay in cost sharing will be different
Jane pays
0%
Her plan pays
100%
plan will usually pay
100% of the
for each "tier" of covered prescription drugs.
(See page 6 for a detailed example.)
allowed amount. This limit helps you plan for health
care costs. This limit never includes your premium,
balance-billed charges or health care your plan doesn’t
cover. Some plans don’t count all of your copayments,
deductibles, coinsurance payments, out-of-network
payments, or other expenses toward this limit.
Preventive Care (Preventive Service)
Routine health care, including screenings, check-ups, and
patient counseling, to prevent or discover illness,disease,
or other health problems.
A physician, including an M.D. (Medical Doctor) or
Plan
Health coverage issued to you directly (individual plan)
or through an employer, union or other group sponsor
(employer group plan) that provides coverage for certain
health care costs. Also called "health insurance plan",
"policy", "health insurance policy" or "health
insurance".
Primary Care Provider
A physician, including an M.D. (Medical Doctor) or
D.O. (Doctor of Osteopathic Medicine), nurse
practitioner, clinical nurse specialist, or physician
assistant, as allowed under state law and the terms of the
plan, who provides, coordinates, or helps you access a
range of health care services.
An individual or facility that provides health care services.
chiropractor, physician assistant, hospital, surgical center,
plan may require the provider to be licensed, certified, or
Glossary of Health Coverage and Medical Terms Page 4 of 6
Provider
Some examples of a provider include a doctor, nurse,
skilled nursing facility, and rehabilitation center. The
accredited as required by state law.
Preauthorization
A decision by your health insurer or plan that a health
care service, treatment plan, prescription drug or durable
medical equipment (DME) is medically necessary.
Sometimes called prior authorization, prior approval or
precertification. Your health insurance or plan may
require preauthorization for certain services before you
receive them, except in an emergency. Preauthorization
isn’t a promise your health insurance or plan will cover
the cost.
Primary Care Physician
D.O. (Doctor of Osteopathic Medicine), who provides
or coordinates a range of health care services for you.
Physician Services
Health care services a licensed medical physician,
including an M.D. (Medical Doctor) or D.O. (Doctor of
Osteopathic Medicine), provides or coordinates.
Prescription Drugs
Drugs and medications that by law require a prescription.
PremiumTax Credits
your family pay for private health insurance. You can get
Marketplace and your income is below a certain level.
Advance payments of the tax credit can be used right
away to lower your monthly premium costs.
Out-of-network Provider (Non-Preferred
Provider)
A provider who doesn’t have a contract with your plan to
provide services. If your plan covers out-of-network
services, you’ll usually pay more to see an out-of-network
provider than a preferred provider. Your policy will
explain what those costs may be. May also be called
“non-preferred” or “non-particiapting” instead of “out-
of-network provider”.
26
Reconstructive Surgery
Surgery and follow-up treatment needed to correct or
improve a part of the body because of birth defects,
accidents, injuries, or medical conditions.
Urgent Care
Care for an illness,injury, or condition serious enough
that a reasonable person would seek care right away, but
not so severe as to require emergency room care.
Rehabilitation Services
Health care services that help a person keep, get back, or
improve skills and functioning for daily living that have
beenlost or impaired because a person was sick, hurt, or
disabled. These services may include physical and
occupational therapy, speech-language pathology, and
psychiatric rehabilitation services in a variety of inpatient
andor outpatient settings.
Skilled Nursing Care
Services performed or supervised by licensed nurses in
your home or in a nursing home. Skilled nursing care is
not the same as “skilled care services”, which are services
performed by therapists or technicians (rather than
licensed nurses) in your home or in a nursing home.
Specialty Drug
A type of prescription drug that, in general, requires
special handling or ongoing monitoring and assessment
by a health care professional, or is relatively difficult to
dispense. Generally, specialty drugs are the most
expensive drugs on a formulary.
Glossary of Health Coverage and Medical Terms Page 5 of 6
Specialist
Aprovider focusing on a specific area of medicine or a
group of patients to diagnose, manage, prevent, or treat
certain types of symptoms and conditions.
Screening
A type of preventive care that includes tests or exams to
detect the presence of something, usually performed
when you have no symptoms, signs, or prevailing medical
history of a disease or condition.
Referral
A written order from your primary care provider for you
to see a specialist or get certain health care services. In
many health maintenance organizations (HMOs), you
needto get a referral before you can get health care
services from anyone except your primary care provider.
If you don’t get a referral first, the plan may not pay for
the services.
UCR (Usual, Customary and Reasonable)
The amount paid for a medical service in a geographic
area based on what providers in the area usually charge
for the same or similar medical service. The UCR
amount sometimes is used to determine the allowed
amount.
27