3752 Hcsw Literaturereview
User Manual: 3752
Open the PDF directly: View PDF ![]() .
.
Page Count: 56
The Development of the Clinical
Healthcare Support Worker Role:
A Review of the Evidence

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence 1
Contents
Page
1. Introduction .............................................................................................................................2
2. The literature review .............................................................................................................2
3. Presentation of the literature .............................................................................................3
4. Denitions of HCSWs ............................................................................................................4
5. Evolution of the HCSW role ................................................................................................6
6. Rationale for the introduction of HCSWs .......................................................................8
7. Scottish Policy Context ...................................................................................................... 11
8. Number of HCSWs ............................................................................................................... 13
9. Characteristics of HCSWs .................................................................................................. 14
10. Education to prepare for and develop the HCSW role ........................................... 17
i) Types of education provided - formal and informal ............................................ 17
ii) Education and training needs .................................................................................... 18
iii) Format of training carried out................................................................................... 19
iv) Evaluation of the training and education provided .......................................... 19
v) Case studies – local training courses ....................................................................... 20
vi) Challenges in undertaking education ................................................................... 22
vii) Conclusion on education and training evidence in the literature .............. 23
11. Competencies and core standards ............................................................................... 24
12. Supervision of HCSWs........................................................................................................ 25
13. Mentorship of HCSWs ....................................................................................................... 26
14. Relationships with other healthcare workers ........................................................... 27
15. Boundary disputes and professional identity ........................................................... 29
16. Roles and scopes of practice ........................................................................................... 30
i) Classication of and types of roles ............................................................................ 30
ii) Critique of HCSW roles .................................................................................................. 30
iii) Guidance on HCSW roles ............................................................................................ 32
17. Tasks conducted by HCSWs ............................................................................................. 33
18. HCSW job descriptions ...................................................................................................... 34
19. Regulation .............................................................................................................................. 35
i) Government policy ......................................................................................................... 35
ii) Professional and regulatory bodies ......................................................................... 36
20. The impact of HCSWs ......................................................................................................... 37
i) Benets of HCSWs .......................................................................................................... 38
21. Stakeholders’ insights into HCSW education and the role ................................... 40
i) Views of HCSWs ................................................................................................................ 40
ii) Views of managers on the role................................................................................... 41
iii) Views of registered practitioners on the role ...................................................... 41
iv) Views of service users on the role ............................................................................ 42
22. Development into registered roles ............................................................................... 43
23. The role of the Assistant Practitioner .......................................................................... 45
24. Future developments ........................................................................................................ 46
25. Limitations of the literature ............................................................................................. 46
26. Conclusion ............................................................................................................................. 47
i) Recommendations for the development of HCSWs ........................................... 48
ii) Areas for further research ............................................................................................ 49
Appendix 1 – Examples of professional organisations’ descriptions ....................... 50
of HCSWs
References ...................................................................................................................................... 50

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 2
1. Introduction
There is currently a major focus
on the Healthcare Support
Worker (HCSW) agenda for a
number of reasons including role
development, regulation issues, skill
mix considerations, cost pressures,
new methods of service delivery,
recruitment and retention issues.
Against this background of interest in the Clinical HCSW
role a narrative literature review was undertaken with the
aims of:
- placing the role in context
- identifying evidence around the role
- identifying best practice around the role
- identifying developments and intelligence around
the role
2. The literature review
The literature was located by a combination of a personal electronic literature
search backed up by a search carried out by the Health Management Library.
The personal literature search was conducted via the
Knowledge Network using the following databases:
Medline; All Evidence Based Medicine Reviews; British
Nursing Index, ERIC, CINAHL (Computerised Index of
Allied Health Literature). No time limit was placed on
the search but the most informative and relevant papers
appeared from the year 2000 onwards. The review was
devoted to Clinical Healthcare Support Workers.
An overview of the literature reveals that:
- The majority of evidence and published papers
are from the UK (Centre for Allied Health Evidence
(CAHE) 2006)
- In terms of sector and professions:
- The majority of the literature is from the acute
hospital sector (Bosley and Dale 2008, CAHE
2006)
- Within the hospital sector the literature is
drawn from across a number of professions
and emanates originally from the Healthcare
Assistant (HCA) role but is now recognising and
reecting the respective dierent levels within
the HCSW structure
This is not a systematic review but analysis of the
literature leads to condence that it is a comprehensive
overview of evidence around the HCSW agenda due to:
- the same themes emerging throughout the
literature
- a cross check of the original personal search by the
search from the Health Management Library
As this is a narrative review the literature has not
been subjected to the rigorous selection procedures
associated with the methodology of a systematic
review. Therefore the quality of the literature cannot be
guaranteed to the same degree as that which appears
in a systematic review. However the majority of the
evidence presented here has been published in peer
reviewed journals which provides a degree of assurance
as to its validity.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 3
3. Presentation of the literature
The literature is drawn from the year 2000 onwards with the earlier papers
addressing the healthcare assistant (HCA) agenda.
The research into the HCA role is largely transferable
to the grades of HCSWs that have evolved from this
original role. The literature has been grouped into the
main themes identied below and within each theme
the evidence is presented in chronological order with the
earliest rst to reect progression over time as the HCA
role has evolved into that now commonly recognised
under the generic HCSW heading.
The topics and themes identied from the literature are:
-Denitions of HCSWs
-Evolution of the HCSW Role
-Number of HCSWs
-Characteristics of HCSWs
-Education and training provided for
HCSW development
-Supervision of HCSWs
-Mentorship of HCSWs in training
-Relationships with other healthcare
workers
-Boundary disputes and professional
identity
-Roles and scopes of practice
-Tasks conducted by HCSWs
-Job descriptions
-Regulation
-The impact of HCSWs
-Views of HCSWs on education and the role
-Views of managers on the role
-Views of registered practitioners on the
role
-Service users’ views on the role
-Development into registered roles
-Future developments
-The Assistant Practitioner Role

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 4
4. Denitions of HCSWs
There are a number of approaches to dening what a HCSW is.
A systematic review (CAHE 2006) into the role of
rehabilitation support workers, which looked at support
workers in all settings, concluded that there was little
agreement in the literature to what constitutes the
denition of a support worker.
This is partly explained by reference to Nancarrow
et al. (2005) who stated that “… the titles and roles
of support workers vary according to the service and
the setting in which the provider is employed”. This is
illustrated by a range of job titles including rehabilitation
assistants, support workers, healthcare assistants,
community rehabilitation team therapists, healthcare
support workers, rehabilitation support workers, care
practitioners, care assistants, therapy assistants (for
physiotherapy, occupational therapy, podiatry), technical
instructors.
The number of job titles associated with HCSW roles
was illustrated by a scoping exercise in Wales (Health
Professions Wales (HPW) 2004) which identied over 260
individual job titles associated with this type of role.
Notwithstanding the diversity in job titles a common
factor relating to all HCSWs is their professional status
in being unregistered. This has implications for the
accountability of their actions and the requirement
that they are supervised by registered healthcare
professionals.
The emergence of a career framework in health (Skills
for Health 2005) and Scottish Credit and Qualication’s
Framework (SCQF) (www.sqa.org.uk) provide a means
of mapping and dening the hierarchical levels which sit
under the umbrella term of HCSW.
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 5
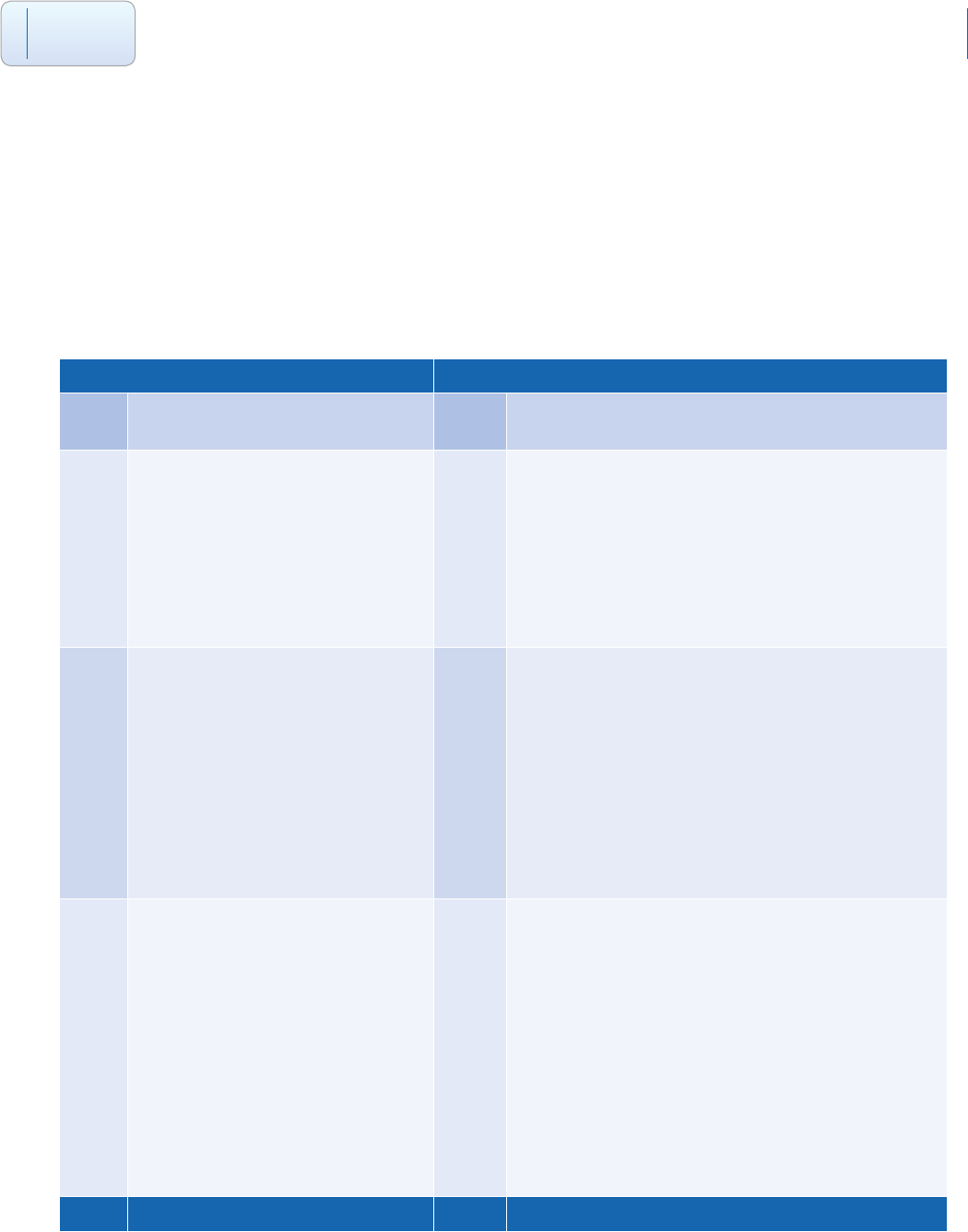
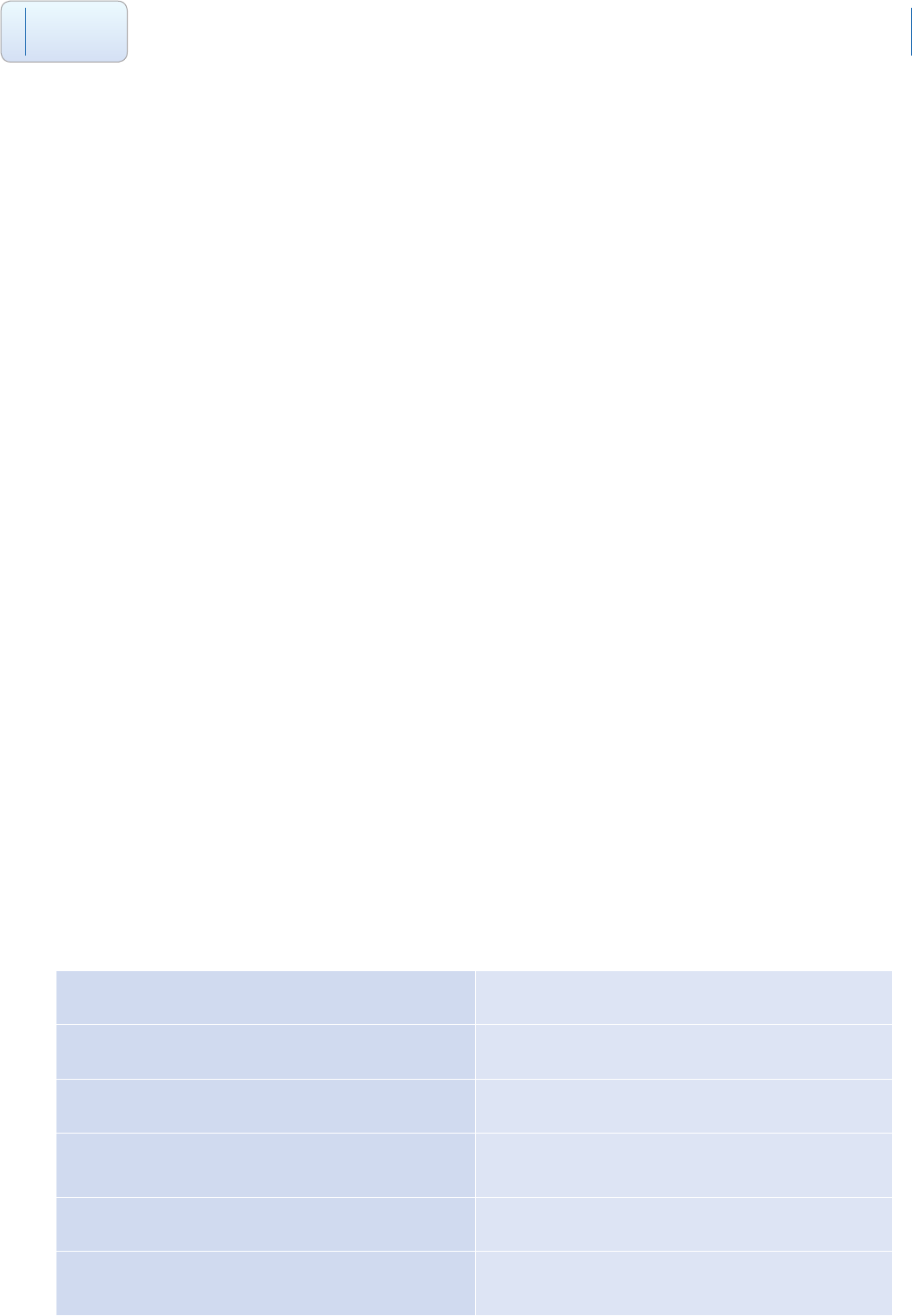
Table 1 - Mapping of HCSW roles to Career Level Framework and SCQF Level Framework
Career Framework Qualication’s Framework
Level Description SCQF
Level
Description
2Support Worker
Frequently have the job title of
healthcare assistant/technician.
They are probably studying for, or
have attained, a national vocational
qualication (NVQ) at level 2.
6Healthcare Support Worker
The HCSW has the awareness and ability to address the
basic care needs of individual patients/clients under the
direction and supervision of healthcare professionals.
They support the multidisciplinary team in the delivery
of high quality care. The HCSW will possess, or have
the opportunity to attain within an agreed timeframe,
education at SCQF level 6.
3Senior Healthcare Assistants/
Technicians
Have a higher level of responsibility
than support workers. They are
probably studying for, or have attained
through an assessment of prior
experiential learning, a level 3 NVQ.
7Senior Healthcare Support Worker
The Senior HCSW can evidence previous experience and/
or consolidation of practice as a HCSW or can evidence
an appropriate level of knowledge. They will have the
understanding and ability to deliver delegated care under
the direction and supervision of healthcare professionals
and support the multidisciplinary team in the delivery of
high quality care. The Senior HCSW will possess, or have
the opportunity to attain within an agreed timeframe,
education at SCQF level 7.
4Assistant practitioners/
associate practitioners
Probably studying for a foundation
degree/BTEC higher or higher national
diploma.Their responsibilities will
include delivering protocol-based
clinical care that had previously been
in the remit of registered professionals,
under the direction and
supervision of a state registered
practitioner.
8Assistant Practitioner
The Assistant Practitioner can evidence previous
experience and consolidation of practice as a Senior
HCSW and/or has the appropriate skills and knowledge
and demonstrates the depth of understanding and ability
required to participate in the planning and carrying out
of holistic, protocol based care under the direction and
supervision of healthcare professionals. They will assist
and support the multidisciplinary team in the delivery of
high quality care. The Assistant Practitioner will possess
or have the opportunity to attain within an agreed
timeframe, education at SCQF level 8.
Source Skills for Health (2005) NHS Education for Scotland (2010)
The reference to Agenda for Change (AfC) bands (DH
1999) is another way of categorising the respective
HCSW levels. Typically a healthcare support worker will
be a band 2, a senior HCSW (sometimes referred to as
an Associate Practitioner) a band 3 and an Assistant
Practitioner a band 4.
Most recently the Scottish Government (2010) has
clearly dened a Healthcare Support Worker in relation
to induction standards and codes. The comprehensive
denition can be found at http://www.hcswtoolkit.nes.
scot.nhs.uk/resources/standards-and-codes
Individual professional organisations also describe and
dene HCSWs in relation to the particular context which
they operate in. Examples are provided in Appendix 1.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 6
5. Evolution of the HCSW role
In terms of chronology, the role of a HCSW has evolved from that of a
healthcare assistant (HCA).
The term HCA is still used interchangeably and
synonymously with that of a HCSW and some support
sta are still referred to as HCAs. In this respect it is
helpful to recognise the characteristics of a HCA.
Bosley and Dale (2008) note that “a healthcare assistant
is the title ocially applied to sta working at National
Vocational Qualication (NVQ) level 2 or 3 in healthcare,
which equates to GCSE and A level respectively. HCAs
may be recruited from among existing unqualied
support sta, and in hospitals they commonly engage in
nursing duties and direct patient care, such as bathing,
monitoring, and observing patients, and talking to and
reassuring patients and their relatives”.
To place the HCA role in historical context Thornley
(2000) outlined the range of titles which the equivalent
of healthcare assistants were referred to: generic support
worker; clinical support worker; healthcare support
worker; care team assistant; nursing assistant; ward
assistant; theatre assistant; community care worker;
home carer; scientic helper; doctors’ assistant; and even
‘bed maker’.
i) Origins of Support Workers
The history of support workers and healthcare assistants
in nursing is outlined by Kessler et al. (2010). Nursing
assistants can be traced back to the Crimean War and
in modern times the main impetus was the recognition
of the nursing auxiliary role in 1955. The support
worker role progressively developed until the formal
introduction of the HCA role alongside the NHS and
Community Care Act 1990. The Act introduced the
HCA role as a local grade for newly created Trusts to
complement the existing nursing auxiliary role. Similarly
the history of the introduction of support workers in
midwifery and the AHP professions are outlined in the all
Wales scoping report (HPW 2004).
The midwifery support worker has been slower to
emerge in comparison to the nursing equivalent
because of dierences in midwifery education and the
way midwives practice. In terms of education it was
not possible to introduce the maternity care assistant
role as a part replacement for a student contribution
as happened in nursing in the early 1990s. At this point
diploma level nurse education was introduced meaning
student nurses became supernumerary and the role
of support worker accordingly assumed a greater
signicance at this level of care. Also the midwife enjoys
an autonomous role demonstrating their expertise in
care delivery which also limits the potential contribution
of students and support workers. However reported
shortages in registered midwives and associated
diculties in delivering maternity services has seen a rise
in the number of maternity care assistants in a number of
NHS trusts in Wales (HPW 2004).
There have also been variations in the adoption
of support workers across the AHP professions.
Physiotherapy (formerly remedial gymnastics) and
occupational therapy (OT) support workers can be traced
back to 1948 when they were known as “aides” and
took on more of a housekeeping role than be engaged
in direct contact with patients. In physiotherapy there

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 7
was a shortage in qualied sta in the 1960s with
an increase in the delivery of services for the elderly
meaning that support workers were employed to ll
this gap. Subsequently there has also been an increase
in the “technical instructor” grade to coincide with the
expansion of services and shortfalls in qualied sta.
Ellis and Connell (2001) estimated that physiotherapy
assistants constituted around 20% of the physiotherapy
workforce.
In OT the “technician” grade has been well established
with skilled tradesmen such as joiners and carpenters
employed in workshops producing aids to help daily
living activities.
Radiography has a history of employing support sta
known as “dark room technicians”. This role has been
subsequently developed into a wider “helper’s” role
which also incorporates associated nursing, clerical and
portering duties. Increasing demand for radiography
services and predicted shortages of qualied
radiographers has led to the emergence of the assistant
practitioner role in the last ten years throughout the UK.
In other professions such as Speech and Language
Therapy (SLT) and health visiting the introduction of
support workers are more recent in comparison. However
traditionally these professional groups have had close
relationships with other support sta such as nursery
nurses and education support sta. The scoping report
also notes the development of more comprehensive
pre-school screening programmes has prompted the
introduction of support sta in audiology and orthoptics.
Podiatry (Farndon and Nancarrow 2003) and dietetics
(Le Cornu and Halliday 2008) are identied as the latest
adopters of support workers. The number of podiatry
workers in Wales is described as small (HPW 2004) and
dietetic support workers were rst introduced in the
late 1990s to counter increasing levels of malnutrition in
hospitals (Le Cornu and Halliday 2008).
ii) The emergence of support workers in
other areas
As well as HCSWs operating in nursing, midwifery and
the allied health professions the literature conrms
the breadth of other areas and clinical specialties
which employ support workers. These include nursing
homes (Baldwin et al. 2003, Fitzpatrick and Roberts
2004), intermediate care (spanning health and social
care, Nancarrow 2005), older people (Field and Smith
2003), rehabilitation (Galloway and Smith 2005) and
mental health (Torjesen 2009). In addition there is the
emergence of a generic support worker identied in a
systematic review of the support worker literature (CAHE
2006). This type of support worker is characterised as one
who can work across dierent professional boundaries.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 8
6. Rationale for the introduction of HCSWs
A review of the literature identies a combination of international, national
and local drivers behind the introduction of HCSWs.
i) International drivers
Bosley and Dale (2008) observe a number of common
themes/factors across developed countries causing
pressure on both primary and secondary healthcare
systems. Briey these include: an ageing population;
more sophisticated medical treatments resulting form
technological and pharmaceutical advances; increasing
costs of delivering healthcare; increasing patient
expectations; shortages of skilled, qualied healthcare
sta.
One solution to these pressures is role development
which changes traditional boundaries between sta
groups by extending, delegating, substituting existing
roles or introducing new ones. Thus nurses may take on
tasks that were the exclusive territory of doctors and
similarly support workers will be utilised for some tasks
that were the responsibility of nurses.
Other factors identied in an international context
include increases in chronic disease, growth of day
surgery and the subsequent expansion of primary
and community care and the continued reduction in
the length of hospital stay. The combination of these
challenges drives the need for the creation of a exible
healthcare workforce (CAHE 2006).
ii) National drivers
The particular circumstances of the British healthcare
system are noted as being a factor in the development
of HCSWs. An international systematic review conducted
across all types of support workers revealed that more
than half of the papers located originated from the UK
signifying the interest in this type of healthcare worker
(CAHE 2006). This predominance of British based papers
is attributed to stang pressures in the NHS and the
particular developing needs of the population.
The British context is also addressed by Wakeeld et al.
(2009) who identify a range of workforce changes related
to the emergence of assistant practitioners (table 2).
Although the majority of these changes are identied
as being peculiar to the British healthcare system it is
recognised that some have their origins in European
legislation, for example the European Working Time
Directive (EWTD) which limits the working hours of
medical sta.
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 9
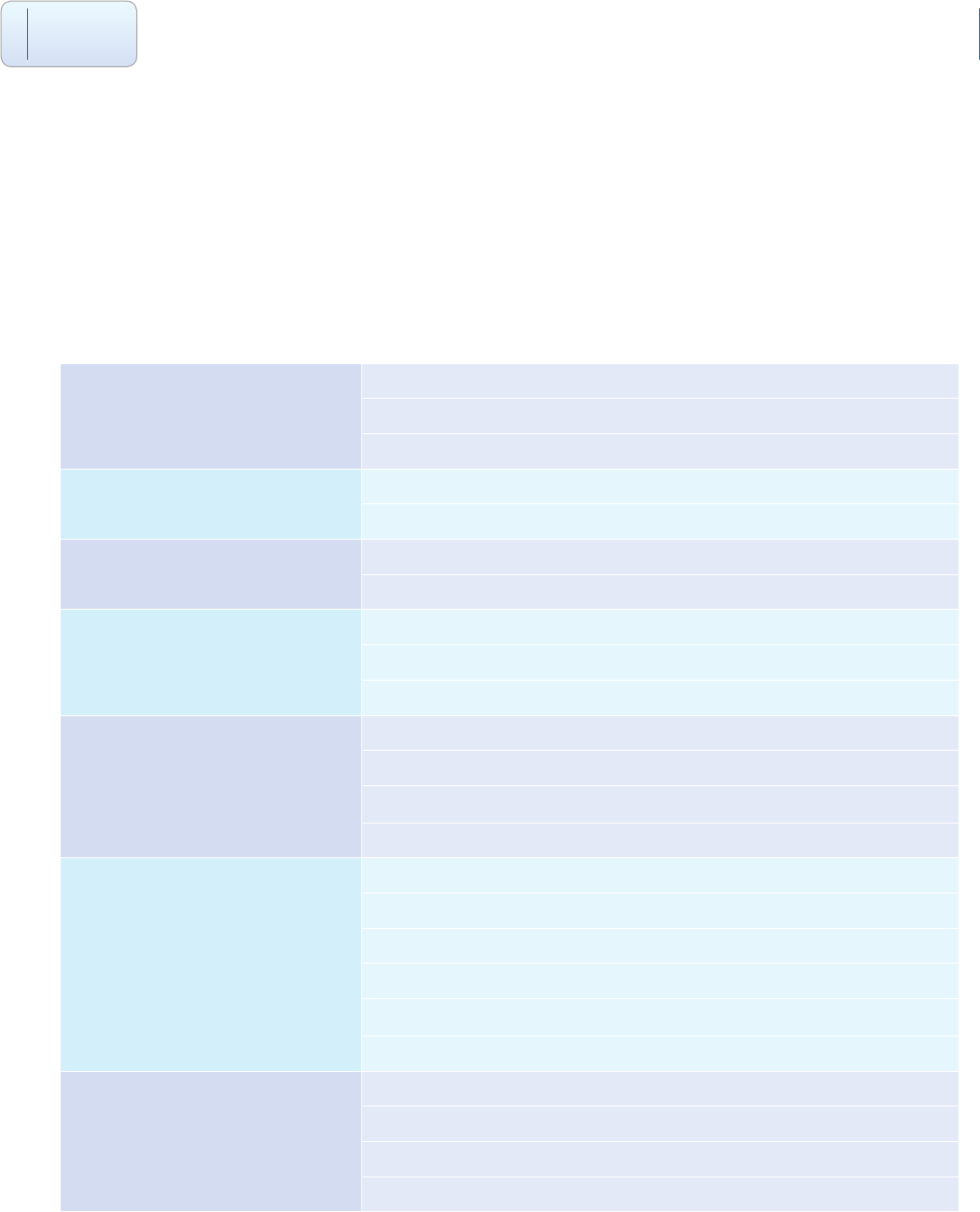
Table 2 - Major Factors Driving Workforce Changes within the UK
1. Employment policies European working time directive 2009
Improving working lives document
Age diversity legislation 2006
2. Restructuring the workforce Gershon report
Requirement for improvements in productive time
3. Regulatory frameworks Professional regulation
Support sta regulation
4. Workforce preparation Modernising medical careers framework
Knowledge and skills framework
Life long learning
5. HR management, workforce
pay and rewards
Agenda for Change
Introduction of the electronic sta record system in the NHS
Workforce changes (for example ageing workforce and retirement trends)
Workforce shortages in diagnostic services
6. Commissioning of services Commissioning a patient-led NHS
Payment by results framework
Practice-based commissioning frameworks
Reduced nancial growth for the NHS from 2008 onwards
Growth of the independent sector as a provider of NHS services
Current nancial pressures within healthcare
7. Patient populations Demographic changes
Chronic disease management
National service frameworks
Clinical eectiveness and clinical governance
Source: Wakeeld et al. (2009), p287
At a high level the practical reasons for the introduction of HCSWs are identied by NHS Education for Scotland
(2010).
1 relief/substitute: releasing professionals from non-core activities and taking on work
previously the remit of registered practitioners
2 co-producer: providing complementary and distinctive capabilities
3 apprentice: providing a stepping stone into qualied work.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 10
iii) Local drivers
While the literature provides an overview of national
and international drivers for the introduction of HCSWs
a good example of local needs is provided by McGowan
and Campbell (2010a). They report on the running of a
pilot course to develop nursing assistant practitioners
(APs) for a chemotherapy unit. Local drivers which were
cited included: an increase in chemotherapy workload
placing increased demands on chemotherapy nurses;
signicant amounts of workload in the chemotherapy
unit resulting from supportive care; recruitment and
retention diculties with qualied chemotherapy
nurses. These local drivers contributed to a regional
review of chemotherapy services which identied
new and improved ways of working. The new ways
of working included introducing the supporting
role of AP to address diculties with recruiting and
retaining registered nursing sta for chemotherapy
administration and supportive care (e.g. care of central
lines, venepuncture, cannulation, managing blood
transfusions).
Likewise Ellis and Connell (2001) report a combination of
national and local catalysts prompting the introduction
of physiotherapy support workers. National drivers
were a shortage in qualied sta and increasing service
demands from the growing elderly population. Local
drivers, perceived to have more eect, were identied
as changes in rehabilitation services, recruitment of new
supervisory sta, alterations in funding of posts and the
existence of national or specic locally initiated assistants’
training schemes.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 11
7. Scottish Policy Context
The emphasis on the development of healthcare support workers in Scotland
in recent times is documented throughout the literature.
Dunlop (2004) identies government and NHS policies
as being a particular stimulus driving HCSW career
development. The Scottish Executive Health Department
(SEHD) published Learning Together in 1999 which
outlined a training and education strategy for all NHS
sta in Scotland, both registered and unregistered.
The clear message from the strategy was that all sta
regardless of status should have the opportunity to
develop themselves as part of the modernisation of the
NHS in Scotland. Learning Together required all health
boards to ensure that all sta had an annual personal
development plan meeting with their manager, and that
access to learning and development opportunities were
improved.
At the same time the Department of Health (1999) issued
UK-wide proposals for Agenda for Change. This was the
new pay grading stucture in the NHS which covered all
sta except for doctors, dentists and senior managers.
Agenda for Change, which was implemented in October
2004, equates pay to the knowledge and skills required
to undertake a particular NHS post. The Agenda for
Change agreement has three components which made
up a package of new terms and conditions of service,
these were
- Terms and conditions
- Job evaluation (to establish pay band for post)
- NHS Knowledge and Skills Framework (NHS KSF)
The consequence of the introduction of NHS KSF strand
of Agenda for Change was the requirement for all NHS
employees to have an annual joint development review
with their manager. The output is an agreed personal
development plan to develop the skills and knowledge
for their particular job as well as for future career
development.
The impetus toward HCSW development was continued
by the Scottish Executive with the publication of Caring
for Scotland (SEHD 2001), a strategy for nursing and
midwifery (Cowie 2002). The strategy gave directors
of nursing a number of responsibilities toward HCSWs
including ensuring that all support workers in their
organisations undertook training by 2005 to maintain
standards of practice.
HCSWs came under further scrutiny with a consultation
exercise around their regulation. The Consultation on the
Regulation of Health Care Support Sta and Social Care
Support Sta in Scotland (SEHD 2004) was undertaken
from May to August 2004. The outcomes of the
consultation are summarised by Birch and Martin (2009).
Briey the responses indicated backing for the regulation
of support workers. Respondents on the whole felt that
support workers should be responsible for their own
practice and this would be dictated by their level of
training and scope of practice. The regulation of HCSWs is
further discussed in section 19.
More recent Scottish NHS policy directives Delivering
Care, Enabling Health (SEHD 2006) and Better Health,
Better Care (Scottish Government Health Directorates
(SGHD) 2007) have armed the drive to develop
the NHSScotland workforce. Factors such as role
development and changing demographics, for example
an ageing workforce, have led to an increased focus on
non-registered sta playing a more prominent role in the
delivery of healthcare.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 12
The development of the workforce emerged as a key
part of a stakeholder consultation exercise subsequently
held to identify the drivers required to implement
Better Health, Better Care. The actions resulting from
the consultation were accordingly outlined in a Force
for Improvement (Scottish Government 2009). Three
particular core challenges were identied in relation to
developing the workforce: ensuring a quality workforce;
delivering best value across the workforce; working
toward an integrated workforce. The role of health care
support workers was recognised as having contributed
to a more widely skilled workforce which has resulted
in increased service capacity. Moving forward, multi-
disciplinary education and training will be required for
all sta to demonstrate core competencies related to
the patient safety and quality improvement agendas.
The KSF, NHS Careers Framework and Scottish Credit
and Qualications Framework (SCQF 2009) provide the
context for the development and delivery of education
and training for the existing and future HCSW workforce
(NES 2010).
Aside from government policy a range of NHS
workforce development initiatives has given HCSWs
the opportunity to develop professionally. The NHS
Knowledge and Skills Framework (NHS KSF), the long-
term strand of Agenda for Change which facilitates the
individual personal development process, was agreed
in 2004 (SEHD 2004). The NHS KSF, through mechanisms
such as a joint development review (JDR) and personal
development plan (PDP), allows HCSWs to identify areas
for personal development which will aid their career
progression. Similarly the career level framework (Skills
for Health 2005), as previously discussed, has put in
place a structure which identies three distinct levels for
HCSWs to operate at. As such it provides a framework for
HCSWs to progress their careers.
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 13
8. Number of HCSWs
The number of HCSWs are considerable. Different denitions of what a HCSW
is and does result in a variety of estimates as to their numbers.
Bosley and Dale (2008) report on a 2005 study which
estimated the number of HCAs employed across dierent
NHS settings in England at 39,522 along with a further
128,325 nursing auxiliaries or assistants.
More recently Kessler et al. (2010) discuss various
approaches to dening the support worker role which
results in dierent estimates as to their number. For
example in dening support workers as those who
support clinical sta, classied as those who provide
support to doctors and nurses, scientic, therapeutic and
technical sta, ambulance sta in England in 2008 there
were 284,000 full time equivalent (FTE) a signicant rise
from the equivalent gure of 220,000 (FTE) in 1998.
These examples illustrate, as with the attempt to capture
a universal denition of HCSWs, that there is no denitive
answer but it is apparent they constitute a signicant
proportion of the NHS workforce and are growing in
number.
In terms of coverage of nursing assistant practitioners
in England, Spilsbury et al. (2009) estimated their
distribution from a 2007 survey of Nurse Directors.
Of those trusts which responded (143/168), forty-six
per cent (n=66) of Trusts had introduced assistant
practitioners and 22% (n=31) were planning to
implement them before 2009. The authors identied
a wide variation in the numbers of APs between
Strategic Health Authorities, Trusts and clinical areas.
The remaining responding trusts (n=46) were resistant
to introducing the role. Reasons given for this reluctance
included no perceived need for the role, lack of evidence
of eectiveness, nancial constraints and professional
and patient safety concerns.
In Scotland it is possible to identify the numbers of
sta in A4C bands 2, 3 and 4 as constituting the HCSW
workforce. At September 2009, for those working in
primary and secondary care, this amounts to 24,341 sta.
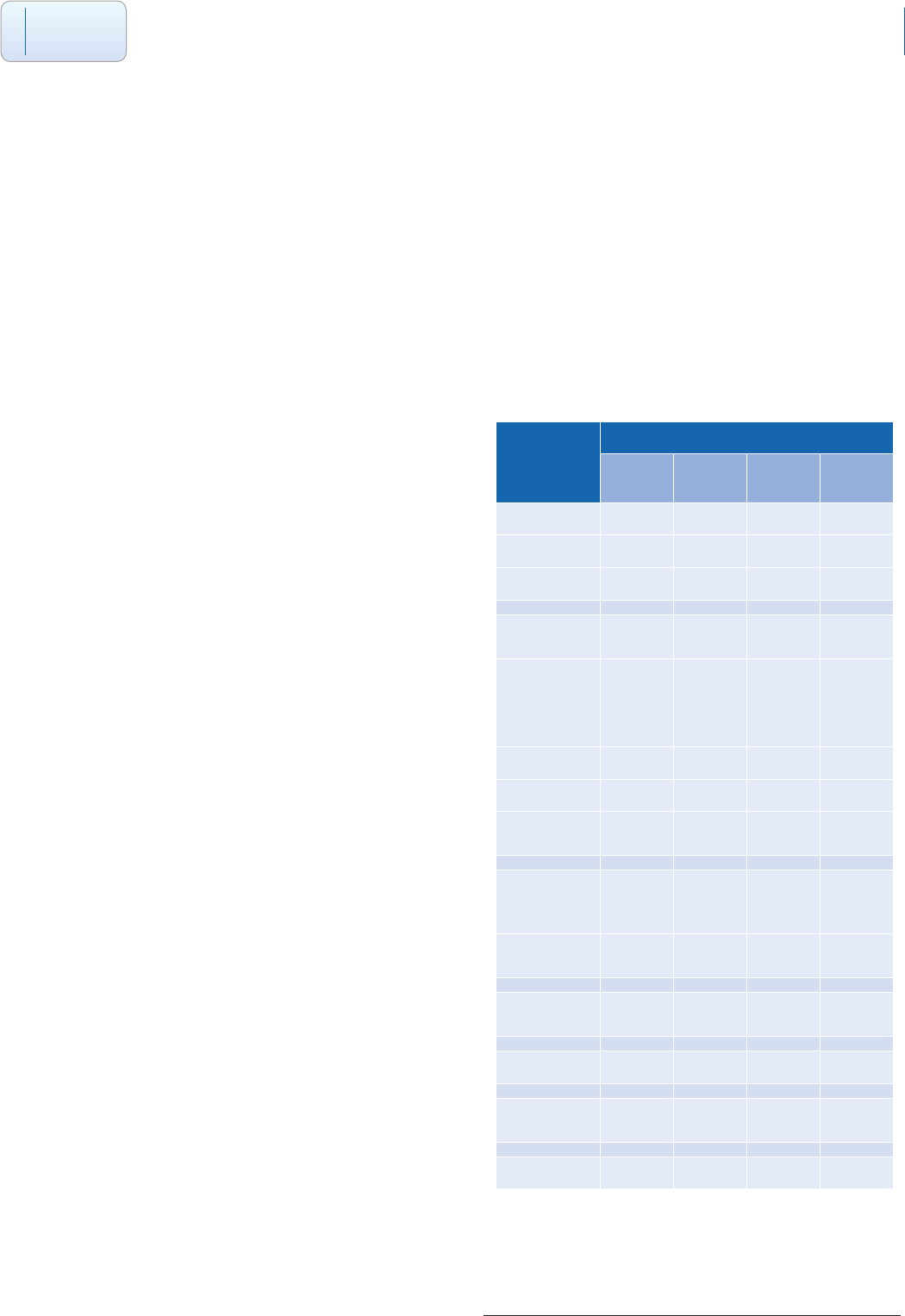
Table 3 - Information Services Division (ISD)
Workforce Statistics (headcount, September 2009)
A4C Bands
2 3 4 Total
Nursing 12878 5254 470 18602
Midwifery 302 42 69 413
AHPs 267 1233 504 2004
Other
Therapeutic
Clinical
Psychology
and
Counselling
9 42 51
Optometry 3 3
Pharmacy 314 40 360 714
Play
specialists 3 58 61
Personal
and Social
Care
Health
promotion 11 11
Healthcare
Science 692 887 178 1757
Total 14462 7501 1653 23616
Primary
Care 1 725 2
24341
Note: Excludes social services, tertiary sector
1 Figure for primary care is drawn from NHS Scotland, National Primary Care, Workforce Planning Survey (December 2009)
and relates to an estimated gure for HCAs and phlebotomists
2 In comparison Bosley and Dale (2008) report an estimate of 6,700 HCAs in 8,451 general practices in England.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 14
9. Characteristics of HCSWs
Demographic, personal and work based characteristics
The literature provides a consistent prole of HCSWs across a number of
occupations.
Thornley (2000) carried out a survey of HCAs and nursing
auxiliaries and states the “outstanding characteristics of
these workers is their maturity and experience”. Similarly
Kessler et al. (2010) summarised the HCSW workforce
in their study as tending to be “mature women with
partners and children”. These characteristics and qualities
are reected across a number of studies.
i) Age
Thornley (2000) discovered that the great majority of
HCAs are aged over 30, with nearly half aged over 40.
Similarly, the great majority of Nursing Auxiliaries (NAs)
are aged over 30, with 60 per cent of this workforce
aged over 40 and fully a third aged 50 or over. Similarly
Ellis and Connell (2001) established in a study of
physiotherapy assistants that most were over 35 (13/16).
More recently Benson and Smith (2006) in an evaluation
of trainee APs (n=50) in Greater Manchester found an
average age of 40 years ranging from 23 to 56 years. The
majority (60%) of radiography trainee APs in a Scottish
study (Colthart et al. 2010b) were aged over 40. Leach
and Wilton (2009) in an evaluation of trainee APs in ve
clinical areas note that all but one had undertaken their
study and training as mature students. The average age
of support workers in Kessler at al’s 2010 study was 42.6.
Outside the secondary sector a Scottish survey of
HCAs and Phlebotomists in primary care found that
49% (309/630) were aged 45 and over. (NHS Scotland,
National Primary Care, Workforce Planning Survey 2009).
ii) Sex
The HCSW workforce are predominately female in line
with the NHS workforce as a whole. Eighty two percent
of trainee APs in the Greater Manchester evaluation
were female (Benson and Smith 2006). Equally the
majority (26/31) of radiography trainee APs in a Scottish
educational programme were female (Colthart et al.
2010b). In a study of physiotherapy assistants all 18 were
women (Ellis and Connell 2001). Kessler et al. (2010)
found that across four English acute trusts females
accounted for between 84% to 95% of all nursing
support workers.
iii) Ethnicity
There is limited data on the ethnicity of the HCSW
workforce. Ninety percent of trainee APs in NHS North
West gave their ethnicity as White British (Benson and
Smith 2006). More recently Kessler et al. (2010) have
provided valuable data. In a survey of four acute trusts
they found a signicant variation in the proportion
declaring themselves as Black and Minority Ethnic (BME)
depending on the respective geographic location of the
trust: South 24%; Midlands 17%; North 10%; London
43%.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 15
iv) Dependants
The age and sex prole of the HCSW workforce is
reected in those that they care for. Benson and Smith
(2006) reported that over half (54%) of the trainee AP
respondents to their evaluation of their educational
programmes had dependants ranging from pre-school
children and school children to elderly or sick relatives.
Responsibility for dependants is also referred to in
the context of providing transferable caring skills (see
experience below). Kessler at al. (2010) report that
typically around 75% of HCSWs in their study have a
partner and children.
v) Experience
Studies identify both formal job experience and informal
caring experience as being key characteristics of the
HCSW workforce.
In terms of formal job experience Thornley (2000)
identied that around half of HCAs have over ve years
experience and nearly a third had between 10 and
28 years experience. Similarly the average length of
employment as a NA was 12 years with over a quarter
having worked between 19 and 31 or more years in the
job. Ellis and Connell’s (2001) study of physiotherapy
assistants revealed they had 5.6 years average service
in this role. Trainee radiography assistant practitioners
had on average 12.9 years service in the NHS (range 3 to
30 years) (Colthart et al. 2010b). In a study of four acute
trusts Kessler et al. (2010) found that the average length
of service of support workers was 9 years. At the lower
end around a quarter had less than 2 years experience
in the role and at the other end around a third had more
than 10 years experience.
In relation to less formal caring experience Thornley
(2000) points to the fact that as a mature workforce
“many recognize their ‘informal’ caring experience at
home (e.g. care of children, the elderly and/or disabled)
as an important part of their ability to cope with the role
of HCA”.
vi) Career history
Kessler et al. (2010) looked at nursing HCSWs’ broader
career histories encompassing both areas of previous
employment and most recent area of employment prior
to becoming a support worker. In relation to all previous
employment experience not surprisingly common areas
were social care and healthcare with between a third and
a half having worked there. Other areas of signicant
previous employment were retail (just less than 50% in
most trusts) and manufacturing and leisure at around
25% each respectively. Interestingly a signicant
proportion of around a third had been full-time unpaid
domestic carers at some point.
Similarly in terms of most recent employment prior to
embarking on a support worker role the most common
areas were social care and healthcare in that order with
between 43% and 62% of support workers across the
trusts coming from these two areas. This leads Kessler et
al. (2010) to conclude that few other occupations oer a
“springboard” directly into the support worker role. They
also found that a small proportion (maximum of 5% in
any trust) became a support worker directly from a full-
time domestic caring role.
vii) Working patterns
There was some variation in the proportions of HCSWs
working part-time. Ellis and Connell (2001) found that all
but one of the physiotherapy assistants (17/18) in their
study worked part-time. Kessler at al. (2010) revealed
that around a quarter of support workers across four
trusts worked part-time (dened as less than 29 hours
per week). Studies of trainee assistant practitioners
reect the fact that most work full-time, for example 94%
(Benson and Smith 2006) and 75% (Colthart et al. 2010b)
respectively.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 16
viii) Comparison with nurses
Kessler et al. (2010), as part of their study, compared
a number of characteristics of the healthcare support
workforce with that of nurses. A number of interesting
ndings emerged from this comparison.
-Age: nurses (38.4) were on average younger than
HCSWs (42.6)
-Years of service: both groups had on average 9
years service
-Support workers are much less likely to have BME
backgrounds than nurses
-A majority of support workers, typically around
three quarters, have a partner and children. Nurses
are as likely to have a partner but less likely to have
children.
-Support workers were signicantly more likely to
work part-time than nurses, a nding which might
be related to their greater childcare responsibilities
-A noteworthy minority of support workers, around
one third, is the sole or main income earner. Nurses
are more likely to assume primary earner status
than support workers.
-Support workers were more likely than nurses
to have a connection to the local community.
For example a considerable and much higher
proportion of support workers than nurses had
attended a local primary school. This suggests that
support workers are more rmly embedded in the
local community than their nursing colleagues.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 17
10. Education to prepare for and develop the HCSW role
The literature identies both formal and informal mechanisms for educating
the HCSW workforce. Formal education takes the form of external accredited
qualications. Informal education is characterised as in-house training such as
shadowing, on-the-job learning and short courses.
i) Types of education provided - formal and informal
a) Formal education
Formal education will follow a set structure and cover
identied skills and competencies which will be
assessed on completion of the programme. Successful
completion of the programme will result in attainment
of a recognised, accredited qualication. A number
of dierent types of formal qualications have been
undertaken across the HCSW workforce.
Typically the primary type of qualication introduced
has been a National Vocational Qualication (NVQ).
Keeney, Hasson and McKenna (2005a) describe NVQs as
“statements of competence in employment, and their
purpose is to provide access to work-based training
and facilitate the attainment of national occupational
standards”. NVQs provided both a formal recognition
of HCAs’ experiential learning and also the means for
their potential progress into registered nurse training. In
Scotland the equivalent to NVQs are Scottish Vocational
Qualications (see www.sqa.org.uk for the range of SVQs
available).
Similarly foundation degrees (Selfe at al. 2008), which
were launched in 2001 around the same time as the
introduction of the assistant practitioner, have become
a recognised qualication, particularly for that grade of
HCSW.
The introduction of foundation degrees in Greater
Manchester for NHS North West is charted in a case
study (Kilgannon 2007). Foundation degrees were seen
as a good solution to the need to provide education for
APs as their delivery would allow support workers to be
retained in the workforce during their training. It was also
recognised that previous methods of training had had
either a competency or knowledge-based approach. The
foundation degree oered an opportunity to develop
these together in an integrated way within the work
context.
In Scotland a suite of Higher National Certicates (HNCs)
have been developed for the AHP HCSW workforce.
HNCs are currently oered in Radiography, Speech and
Language Therapy, Physiotherapy and Occupational
Therapy (see www.sqa.org.uk). The qualications are
designed to support all levels from support worker to
preparing individuals to become assistant practitioners.
The dierent levels of formal education required for
the respective grades of HCSWs in terms of the Scottish
Credit and Qualications Framework (SCQF) are outlined
in table 1 (see p3). Briey a HCSW requires to be educated
to SCQF level 6, a senior HCSW to level 7 and an Assistant
Practitioner to level 8 (see also NES 2010, p14-15).
In relation to developing support workers and assistants
into assistant practitioner roles the provision of
education in radiography demonstrates the range of
dierent qualications utilised. Education provision
to develop Assistant Practitioners began as early as
2001 with a two year pilot course at the University of
Leeds (Whyke 2003). Radiography support workers
undertook an access course for a year and then joined
undergraduate radiography students in their rst year
of studies. Ten support workers started and successfully
completed the course. On completion of their studies
they were awarded a Certicate of Education in
Radiography Studies (Cert. HE). Subsequently seven
trainees took up posts as Assistant Practitioners and three
resigned to become student radiographers by joining
the second year of the radiography undergraduate
course. Similarly a distance learning course for Assistant
Practitioners has been run by Anglia Ruskin University
since 2002 (Winnard, Kittle 2008). A NES scoping exercise
(NES 2004) identied courses at ve other HEIs including
Robert Gordon University as well as NVQ Level 3
Diagnostic and Therapeutic support delivered by further
education institutions.
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 18
The accounts of the development of individual
educational solutions for the introduction of Assistant
Practitioners are described by a number of authors. These
involved work-placed learning in combination with a
NVQ (Betts et al. 2003), a Higher Certicate in Education
(Forsyth et al. 2003) and a Diploma in Higher Education
(Hodgson et al. 2005). Alternatively a foundation degree
programme may be undertaken (Shaw 2005).
b) Informal education
Keeney, Hasson and McKenna (2005b) discuss informal
training alongside the formal component. They
characterise the content, delivery and duration of
informal training programmes as being based on the
requirements of individual healthcare settings. Trainees
receive no formal academic credit for completing such
courses and many healthcare settings provide training at
their own cost.
The provision of informal training is not quantied in the
literature but a survey of 387 Allied Health Profession
HCSWs and Assistant Practitioners in Scotland, carried
out as part of the market research for the validation
of the HNC in Speech and Language Therapy (2008),
demonstrated that the predominant mode of education
was in-service (80%, 310/387) followed by SVQ (18%,
70/387) and HNC (9%, 35/387). Other education was cited
by 30% (115/387).
ii) Education and training needs
A review of core training requirements for support
workers is presented in detail in a systematic review
(CAHE 2006). This review specically addressed the
question of what training was required by support
workers in community rehabilitation but the generic
evidence is drawn from across the entire HCSW literature.
The 15 core training requirements identied are drawn
from 18 studies (Table 14, page 67) and reproduced
in table 4 below. In discussing the documented core
requirements the authors note that a number of them
relate to aspects such as occupational health and safety,
care skills, communication skills, professional issues,
etc. These reect the desire to provide safe, eective,
ecient, patient centred and equitable healthcare.
The systematic review (CAHE 2006) concluded that
while a variety of training programmes exist for support
workers, the core training requirements include
aspects of occupational health and safety, care skills,
communications skills and professional issues. The wide
variety of training models reected the variability of the
roles these support workers undertook in diverse and
changeable working environments.
Table 4 – Core Training Requirements for Support Workers
Organisational
structure
Communication First aid Anatomy/
physiology
Infection control
OHS/manual
handling
Professional issues Care principles Recording/
reporting
Admin/
Clerical
House keeping/
maintenance
Care skills Study skills Team work Community/
culture
Source: CAHE (2006), Table 14, page 67

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 19
In a British context there is a paper which addressed
the training needs of HCSWs. Moseley et al. (2007) ran
a scoping study which aimed to estimate how many
support workers need further training and which
competencies the training should target. Their Welsh
study surveyed all the support workers and their
managers at work on a given day in four NHS Trusts,
two independent sector healthcare organizations and
in social care. The study was designed as a self-report
questionnaire survey using as its basis 32 descriptors
from the NHS Knowledge and Skills Framework levels
1 and 2. An overall response rate of 77% was achieved
covering 117 respondents (82 support workers and 35
managers).
Thirty-ve per cent of respondents thought that HCSWs
were ‘unable’ to perform six or more of the 32 descriptors
used, whilst on the criterion of being ‘less than able’, the
gure was 64%. Support workers and their managers
agreed closely on where the diculties lay in achieving
KSF competencies. Those diculties lay in two particular
areas - biomedical/ physiological knowledge and data-
handling.
The main relevance of the study to clinical practice is that
there should be a greater concentration on the more
scientic areas of expertise and a similar emphasis is
needed for those who train mentors or supervisors. These
implications will become more important over time as
scientic knowledge about medicine and healthcare
increases.
iii) Format of training carried out
The training programmes identied (n=28) were
analysed in terms of their format and method of
delivery (CAHE 2006). Programmes were delivered by
a combination of theoretical teaching and practical
experience. The particular methods, duration and setting
for each respective programme are summarised (table
15, Training Models for Support Workers, p69).
iv) Evaluation of the training and
education provided
A recurring theme in the literature relates to historic
decits in education and training provided for HCSWs.
Keeney et al. (2005b) in reviewing the relevant literature
identied three problems with vocational training
programmes for HCAs. Firstly no consistency in their
duration, secondly questions over who is responsible for
and pays for the training and nally a lack of consensus
on the content of the training. Taking all these into
account they agreed with White (2002) who stated that
there was no consensus on the best way of providing
minimum standards of training to HCAs.
This echoes the ndings of Ramprogus and O’Brien
(2002) (cited in Keeney, Hasson, McKenna, 2005a) who
surveyed 200 HCAs in NHS trusts and found that there
were some short courses on anatomy and physiology,
communication skills and personal care but in general
there was a lack of organized and systematic education
and training.
In terms of allied health professions a lack of access
to appropriate training for support workers has been
identied in occupational therapy (Nancarrow and
Mackey 2005) and similarly a lack of provision of training
for dietetic support workers (Le Cornu and Halliday
2008). Similarly Leach and Wilton (2008), reporting on
an evaluation of assistant practitioner training across
a variety of professions, noted diculties relating to
workplace learning in terms of logistical problems in
providing radiography placements.
Where vocational qualications have been put in place
there has been some criticism of their operation. Agnew
(2001) (cited in Keeney, Hasson and McKenna (2005a))
criticised the NVQ system for a lack of time for support
and assessment in the workplace and because of an
open-ended structure which allowed the lack of xed
deadlines to lead to non-completion. Nancarrow and
Mackey (2005), in an evaluation of training for OT APs,
reported concerns about the consistency of the quality of
NVQ training and assessment.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 20
Understanding of vocational qualications may also be
an issue. Nancarrow and Mackey (2005) observed that
the qualied supervising OTs had little understanding of
the content of NVQs and did not confer the same value
to vocational qualications as university qualications.
In eect the OTs perceived university qualications to
equate to a level of clinical skills and competence which
was not implied by the vocational qualications achieved
by the assistant practitioners.
The diculties noted above by a variety of authors
are neatly summed up in the conclusion of a scoping
exercise in Wales (HPW 2004, p253) which examined
training and development opportunities. The ndings,
covering 14,445 HCSWs, concluded that:
“the existing provision of training and development
opportunities for support sta in the NHS in Wales,
varies considerably in quality, quantity and level of
provision, with diversity across the dierent healthcare
professions within individual Trusts and Local Health
Boards. There is a lack of accredited training directly
linked to role competencies and measurable against
national standards, for example the Knowledge and
Skills Framework or National Occupational Standards.
Transferable credit is, therefore, very limited”.
v) Case studies – local training courses
There are a number of individual accounts in the
literature which describe training courses developed to
provide a local solution to an identied training need
for HCSWs. These case studies are valuable in learning
from the experience of those who have devised and
implemented training and education programmes to
prepare HCSWs for practice.
McCready and Macdonald (2002) describe the setting
up of a course which was designed to meet perceived
knowledge and skills gaps for HCAs working with cancer
patients. The course was accredited by a local university
and attracted 12 credits at level one. The course was
delivered over ten weeks and consisted of 90 hours
taught time and private study with an additional 50
hours for assignments. There were no formal entry
requirements other than basic literacy skills and a desire
to undertake the course. In terms of content the course
consisted of ten stand alone units ranging from biology
and life history of cancer to general causes, cancer
prevention and screening. The course was underpinned
by the need to improve communication skills and related
the content to psychosocial factors and holistic caring.
In terms of outcomes a small scale evaluation reported
positive feedback from the HCAs on improvements in the
care they were delivering and their knowledge of cancer
care.
Field and Smith (2003) report on a short course aimed at
educating and supporting HCAs involved in the care of
older people. The authors identied a need to provide a
basic care course for HCAs after characterising existing
training as “fragmented”. The course focused on elements
of essential care and interestingly the content was in
part inuenced by user involvement. Focus groups of
recent patients were conducted and they prioritised
privacy, dignity and communication as being their most
valued components in the delivery of basic care. The
course consisted of 30 hours of taught theory and private
study. The course leaders were in the process of seeking
accreditation for the course at the time of publication of
the paper.
The course was routinely evaluated by questionnaires
but the authors recognised the need to go further than
this and were planning to evaluate the impact of the
course on clinical practice. This was to be done by a
combination of methods, primarily observation by the
course leaders of the HCAs in their clinical areas against
the key aims and learning outcomes of the course. This
would be supplemented by feedback from the HCAs’
themselves by questionnaires and focus groups as well
as the observations of nursing and interprofessional
colleagues.
Arblaster et al. (2004) illustrate the benets of a three
staged education programme in developing HCSWs
and outline several factors which have contributed
to its success. The rst phase is the “Essence of Care”
programme which is a mandatory induction course for
all new HCSWs. The programme is of seven day’s duration
and covers areas such as principles of self-care and food
and nutrition. The rst phase is assessed by means of a
competency based workbook which must be successfully
completed within six months of nishing this rst phase.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 21
Having successfully completed the rst phase all HCSWs
are required to undertake the second stage which is a
NVQ in Care level 2. The third and nal phase is the NVQ
in Care Level 3 which is open to those who have passed
the level 2 qualication and meet a variety of criteria
including that they are in or intend to apply for a senior
HCSW role. Attainment of the level 3 qualication allows
the support worker to apply for senior HCSW roles, nurse
training or NVQ assessor training.
A number of factors are identied which have ensured
the programme has achieved its aim of developing
support workers into senior HCSWs. These factors relate
to both support for the individual and support for the
educational programme system.
In terms of supporting the individual, study skills training
is provided at two points on the programme. This is
rstly after the initial “Essence of Care” course and prior
to undertaking the NVQ. In preparation for NVQ study
it covers areas such as learning styles and reective
practice. Having completed the level 3 qualication
additional study skills training was introduced for those
going on to university based nurse training following
feedback from participants that there was a large
academic gap between NVQs and university study. The
second study skills course lasts for two days and covers
topics such as critical appraisal, presentation skills,
referencing and writing and formatting essays.
The educational system has been supported by a
dedicated team of four registered nurses and senior
HCSWs as peripatetic NVQ assessors. Initially the amount
of NVQ participants was limited by the number of work
based assessors available. Traditionally this function had
been carried out by registered nurses but pressure of
work had constrained their ability to carry out this role. A
solution of training senior HCSWs as assessors who had
completed the programme themselves was identied as
a means of getting round this obstacle. The success of
this solution can be gauged by the fact that prior to the
introduction of HCSWs as assessors 12 support workers
a year were completing the course and this number rose
to 45 per year after the change. A personal account of a
HCSW becoming a NVQ assessor for this programme is
given by Muddiman (2010).
McGloin and Knowles (2005) report on an evaluation of
a progressive, tiered course to train critical care (CCA)
assistants. The 18 month course consisted of: a two
week orientation programme, a ten week foundation
programme which covered the trust’s own support
worker competencies; a one year NVQ level 3 care course
and the trust’s advanced support worker competencies;
nally a twelve week course adapted from the operating
department’s NVQ level 3 units and the trust’s CCA
competencies completed by a nal assessment case
study and MCQ.
The CCA role was initiated in a what was described as a
“hurried” manner following the successful attainment
of funding to support the training. The training was
implemented immediately on receipt of funding and
this had implications for the introduction of the CCA
role in the department. The evaluation reports that
the implementation of the CCA role was met with
“trepidation” among the intensive care nurses that
would be working alongside these assistants. There
was a feeling that the role had been introduced too
quickly without sucient consultation with relevant
nursing sta. The authors surmise that if the nurses had
been more involved in determining the role this would
have led to less worry and concern. The evaluation also
revealed concerns from registered nursing sta relating
to their own code of professional conduct and the CCAs’
quality of patient care, accountability and responsibilities.
The ndings lead McGloin and Knowles to recommend a
number of prerequisites for the successful introduction
of the CCA’s role: a clear denition of the role from
the outset; the deployment of dedicated practice
development sta to develop the role; the use of
appropriate change management techniques to ensure
that all appropriate sta contributing to the training are
fully consulted and involved.
Rehabilitation support workers were the recipients of a
short two day course detailed by Galloway and Smith
(2005). The course was aimed at the particular needs
of those working in the rehabilitation environment
which crosses the health, social services, voluntary and
independent sectors. As such the course was run under
the auspices of a Primary Care Trust (PCT). In common
with Field and Smith (cited above) a focus group

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 22
was employed to identify the education and training
requirements for the course. The focus group identied
the need to provide a portfolio of interdisciplinary
educational provision to meet the needs of a diverse
workforce with opportunities for academic credit
and award. The education should provide career
development and access to other CPD opportunities.
The course was attended by healthcare assistants,
rehabilitation support workers and occupational therapy
and physiotherapy technical instructors. Learning
outcomes focused on both generic and rehabilitation
specic issues: principles of rehabilitation; principles
of client centred care; current issues in rehabilitation
practice; review current practice through reection and
identify areas for development.
An evaluation highlighted the strength of the training as
the value placed on all support worker roles in the PCT.
Similarly participants were able to learn from colleagues.
The course demonstrated partnership working between
the PCT and university which has enabled the integration
of theory, research and clinical practice. Future plans to
develop the course included the introduction of work
based learning and experiential leaning.
The literature also reports on the development of
pilot courses which add to the body of evidence
surrounding education and training for HCSWs. One such
example of this was a national training course for HCAs
commissioned by the Department of Health and Children
in Ireland (Keeney S, Hasson F, McKenna HP, 2005a).
The training culminated in the award of a Healthcare
Support Certicate and was composed of eight modules
(three mandatory modules, two elective modules related
to a specialist working area, a communication module, a
general studies module and a work experience module).
The course lasted six months and was initiated by one
week’s intensive training followed by one day a week
for the remainder of the time. In addition there was a
clinical placement which required an additional 20 days
over the six month period. The training was delivered by
classroom teaching of both theory and practical skills
which were then assessed in a clinical setting.
An evaluation identied a number of recurring themes
which led the authors to make six observations on the
future running of the course. The evaluation concluded
that on the positive side the course increased knowledge
and condence, improved understanding, provided
greater awareness of patient-focused care. However all
participants thought the course duration was too short
for the amount of work involved.
Most recently McGowan and Campbell (2010b) describe
the rationale and operation of a pilot course to enable
support workers to become assistant practitioners in
a chemotherapy unit in Edinburgh. The course was
delivered by a variety of modules from a combination
of a further education college and a higher education
institution.
An independent evaluation identied four particular
challenges that emerged over the course of the pilot:
more support required in the clinical area to achieve
clinical competencies and complete a practice workbook;
lack of understanding of the assistant practitioner role;
the need for the education to be pitched at the right
SCQF level; the academic diculties encountered when
moving from level 7 based education to level 8. In all
these instances solutions were identied to meet these
challenges.
vi) Challenges in undertaking
education
Benson and Smith (2006) report on the main challenges
faced by TAPs (n = 50) as they completed their two
years on a Foundation Degree programme. The most
commonly identied problems were a lack of time to
complete their studies against a backdrop of work and
domestic commitments (42/50) and their diculty in
gaining understanding of their role in their working
environment (37/50). Less frequently cited concerns
included lack of resources (13/50) and problems with
placements (13/50).
The nancial challenge was highlighted by Leach
and Wilton (2008) who identied the need to earn
while learning was seen as paramount by assistant
practitioners undertaking foundation degrees to prepare
them for this role.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 23
McGowan and Campbell (2010) identied a number of
aspects for development following the initial running
of a pilot course to train APs to work in a chemotherapy
unit. Firstly the recruitment of future participants should
become more formal and that potential candidates
should be able to demonstrate capabilities in a band
3 post. In terms of the course content, a number of
areas were identied which would enhance its value
for example covering aspects of psychology to enable
APs to be able to support patients and have a greater
understanding of the impact of bad news and issues
surrounding death. Academic and clinical support for
trainee APs (TAPs) emerged as an important issue in
the evaluation of the course and it was recommended
that a policy should be drawn up to identify mentors’
commitment when supporting and training APs, ensure
equity of support and monitor mentors’ additional
workload burdens. Finally the course was recognised
as being potentially transferable to other clinical areas
and this could be achieved in partnership with an HEI in
developing a core generic content for the AP role and
adding specialised units for individual areas of nursing
such as intensive care and mental health nursing.
vii) Conclusion on HCSW education
and training evidence in the
literature
A review of education and training over time for HCAs
and HCSWs is characterised by Bosley and Dale (2008) as
“neither statutory nor standardised”. This has led to calls
in the literature for the introduction of more organised
training formerly for HCAs and latterly for HCSWs
(Keeney, Hasson, McKenna 2005a). This has included a
recent call for the introduction of mandatory training for
all HCSWs by the RCN (Sprinks 2009).
Whilst acknowledging the diculties associated with
training and education for the support workforce, on
the positive side Keeney, Hasson, McKenna (2005a)
concluded that educational courses are feasible for HCAs
and where they have been implemented they have
helped achieve an increase in knowledge, condence
and skills. This positive impact of training was echoed in
a systematic review (CAHE 2006) which noted evidence
of support workers knowledge and care skills having
improved on completion of training programmes.
Indirect benets of participation in training programmes
were positive sta recruitment and clearer denition of
roles.
In order to optimise the eectiveness of education
provided evidence in the literature highlights that
training programmes need to identify and address local
barriers to uptake (such as nance constraints, cultural
issues, career ladders) for them to succeed (CAHE 2006).
In this respect experience and knowledge gained from
accounts of designing and running local training courses
is valuable.
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 24
11. Competencies and core standards
Closely related to identifying training and education needs have been
exercises and projects setting out the competencies required for HCSWs.
The identied competencies are comprehensively
summarised by the CAHE review (2006, p56). The
summary conveniently divides the competencies into
generic (table 11), allied health professions (table 12) and
healthcare/nursing assistants (table 13).
The authors note that the common core competencies
reected in the literature are related to occupational
health and safety, communication, administration,
commitment to life long learning and professional
issues (such as ethical conduct, dignity and patient
condentiality).
Competencies for support workers who work within
specic disciplines reect the unique requirements of
those disciplines. The generic and discipline specic
competencies required by the local setting in which
support workers are employed are likely to dier
according to service type, sta levels, etc.
An illustration of core competencies are provided by
Keeney, Hasson and McKenna (2005b) who identied
these for a pilot training programme in Ireland for
healthcare assistants across care settings and client
populations:
Taking the initiative Listening eectively
Problem solving Communicating orally and in writing
Being numerate and literate Working eectively in group situations
Taking responsibility for one’s learning
and progress
Having information and communication technology
skills
Sourcing and organising information eectively Understanding health and safety issues
Applying theoretical knowledge in
practical contexts
Reecting on and evaluating the quality of own
learning and achievement
More recently Skills for Health (2009) launched core
standards for Assistant Practitioners. These are not
mandatory standards but considered best practice and
cover the deployment and management of APs as well as
their recruitment, education and training, competencies
and development (Sprinks 2009).
The need to identify the competencies HCSWs require
to practice and how best to ensure they gain these is
identied as a research gap by Lizarondo et al. (2010).
Related to this is the need to devise an educational
programme which incorporates a skills escalation
framework which will allow HCSWs to develop their
careers.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 25
12. Supervision of HCSWs
The non-registered status of HCSWs has implications for their clinical
supervision.
The onus on registered sta to supervise support workers
is illustrated by the College of Radiographer’s Scopes of
Practice for Assistant Practitioners (CoR 2007a, b):
“An Assistant Practitioner performs protocol-limited
clinical tasks under the direction and supervision of a
state registered practitioner.”
Nancarrow and Mackey (2005) identied supervision as
one of the key themes to emerge from their evaluation
of OT assistant practitioner training. All participants in
the evaluation, including service users, recognised the
importance of supervision for assistant practitioners.
Supervision was categorised as both formal and informal
in nature. Formal supervision related to ensuring the
competence of the assistant practitioner, supporting
their clinical role and providing pastoral support. Such
formal supervision should be on a regular basis with
an indentied member of sta. Informal supervision
was characterised as being more ad-hoc in response
to immediate needs such as a day-to-day problem
arising. This type of supervision may be carried out on a
interprofessional basis by dierent levels of sta.
An important observation in relation to supervision was
a lack of experience of this role by the OTs being asked to
carry this out. In practice this led some to over supervise
(being over controlling) and others to under supervise
(not wanting to supervise). Closely associated with
supervision were issues of professional responsibility (the
question of the accountability of non-registered sta in
comparison to HPC registered sta) and the competence
of non-registered sta who have undertaken vocational
qualications. In this respect only OTs who had been
involved in actual NVQ training recognised and valued
the qualications as an indicator of the competence of
that particular assistant practitioner.
Nancarrow et al. (2005) investigated the operation
of support workers in intermediate care in England.
Intermediate care encompasses community based
care delivered through a combination of primary care
trusts and social services. As such this type of care is
very diverse given the type of environment it operates
in. Typical roles identied for support workers were
multidisciplinary working, meeting rehabilitation needs,
providing personal care and enablement.
The study covered 794 support workers and identied
three models of supervision. Firstly by means of a mentor
who may be a registered practitioner. Little detail was
given however on who the mentor was and how the
mentoring process worked in practice. The second
mechanism was by team supervision from members
of the multi-disciplinary team. Typically this type of
supervision was carried out by attendance at regular
(mostly monthly) meetings or contacting an appropriate
member of sta. Finally direct formal or informal
supervision through the line manager or team leader was
reported.
The authors concluded that the variations in supervision
may necessitate the need for a good practice model for
support workers. This might involve gaining a consensus
as to what constitutes ‘appropriate’ supervision for
support workers in dierent types of settings.
A systematic review (CAHE 2006) investigated
supervision in the context of methods of service
delivery. A review of the way services were delivered by
support workers in 47 studies revealed that most are
underpinned by supervision and explicit task delegation
as opposed to independent working where the support
workers practice individually.
The systematic review concluded that “while there was
consensus for supervision of the support sta, there was
little consensus on how much supervision was required
and the most eective methods of supervision”. Similarly
an important nding from the literature were concerns
expressed by qualied practitioners for training in
supervision and delegation to enable them to carry out
these tasks eectively.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 26
13. Mentorship of HCSWs
The need to support HCSWs, typically in the form of mentorship, is
acknowledged in the literature.
Colthart et al. (2010a) investigated the experience of
radiographers acting as mentors on an educational
programme to prepare support workers to become APs.
The programmes employed a combination of academic
and workplace learning (two days per week) and as such
mentors were integral to the successful operation of
the programmes. The mentors identied personal and
professional development benets for themselves in
undertaking this role. However there was some tensions
identied in providing mentoring time for both TAPs and
radiography undergraduates. The mentors identied the
provision of protected time and better knowledge of the
theoretical teaching the TAPs were receiving at college as
a means of improving their ability to carry out this role.
Leach and Wilton (2009), in an evaluation of AP roles,
reported that the assistant practitioners discussed
the importance of having a champion for their role.
This champion would support their development and
encourage the growth of new skills and competencies.
McGowan and Campbell (2010b) describe the
development of a pilot course to train assistant
practitioners for a chemotherapy unit. One of the
issues to emerge from the evaluation was diculties
encountered in providing adequate mentorship support.
Initially each trainee AP was assigned their own named
clinical mentor, who as a registered nurse (RN), took on
this role in addition to their normal clinical workload.
However this arrangement did not function well in
practice and as a result an appropriately trained RN was
employed to carry out the mentoring function for the
four trainee APs in their respective clinical areas. This
experience led the authors to recommend that a policy
should be developed to identify mentors’ commitment
when supporting and training APs, ensure equity of
support and monitor mentors’ additional workload
burdens

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 27
14. Relationships with other healthcare workers
The participation of HCSWs in multi-disciplinary teams raises the question of
their relationships with those they work in these team based environments.
Spilsbury and Meyer (2004) undertook a case study
which examined the relationship of HCAs and registered
nursing sta in an English acute hospital. The interactions
between the HCAs and nursing sta are characterised
under the headings of the use, misuse and non-use of
HCAs.
Firstly in terms of use, the HCA job descriptions noted
three main areas of work: direct care, housekeeping
and clerical duties. In practice the majority of HCA work
activity came under the heading of direct care with in
contrast RNs tending to move away from direct bedside
care to activities such as paperwork and discharge
planning. These types of typical work activity were
perceived by both HCAs and RNs as having implications
for patient care, safety and nursing teamwork.
The misuse of HCAs is described as situations where HCAs
were used in ways that were beyond the expectations
of formal policies and was described by the authors
of being an “exploitation of the HCA role”. This may
have occurred because of increased workload or
under-stang. An example of this was asking HCAs to
undertake blood glucose monitoring without providing
training for this particular task, as required by local policy.
Non-use of HCAs was exemplied by RNs preventing
HCAs from putting their skills and experience into
practice. The authors identied four particular ways RNs
restricted HCAs;
1 the use of credentials such as the title nurse to
dierentiate between the role of nurse and HCA
2 the work which RNs permitted HCAs did not
take account of their skills, experience and
qualications e.g. a trained dietician working
as an HCA not being allowed to give dietary
advice, HCAs who had previously worked as
phlebotomists with healthcare agency services
but were told that they could not take blood as
part of their current role.
3 RNs outwardly restricting HCA’s involvement in
certain perceived higher level tasks which were
reported as being the nurse’s job e.g. wound
dressings
4 RNs ignoring the HCAs’ knowledge of the
organization and local community that they had
gained through experience. Whilst RNs may have
recognized this experience they chose not to use
it practice. For example RNs not involving HCAs
in discussions about patient care and discharges.
The case study illustrates the need for HCAs to be
employed in the most eective manner if their
contribution to patient care is to be maximised.
Keeney, Hasson, McKenna (2005b) in reviewing
the literature on HCAs (in their study of managers’
perceptions of HCAs) observe that integration within and
acceptance by the healthcare team was a major issue
which has prompted much controversy and discussion.
Evidence suggests that the introduction of HCAs has
been met with scepticism by a number of qualied sta
who regard them as a cheaper alternative which have
encroached on their role and territory.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 28
More recently there has been a debate on the ratio of
registered sta to non-registered sta. Sprinks (2009)
reports that the RCN suggests that the benchmark
ratio in an acute setting should be around 65 per cent
registered sta to 35 per cent non-registered. Ideal ratios
depend on a number of factors, including geographical
location, the number of elective admissions and the type
of ward. It is clear that the ratio of non-registered sta to
registered sta has risen over recent times. For example
in the NHS in England in 1998 there were the equivalent
of 10.5 band ve or six equivalent nurses for every one
HCA. By 2008 the respective gure was 6.6 nurses to
each HCA, a rise of over 40% in the proportions of HCAs
(Gainsbury 2009).
The ratio of registered to non-registered sta is part of a
wider deliberation on ideal skill mixes. The interest in skill
mix is usually linked to the dual outcomes of patient care
and cost to determine which is the optimal combination
of sta for both of these factors.
The evidence on using dierent grades of nursing sta
(skill mix) has been systematically reviewed by the
National Nursing Research Unit at King’s College London
(NNRU 2009). The volume of evidence is small and mostly
originates from the USA. Given the dearth of literature
in this area it was concluded that the limited evidence
available does not support the UK introducing a nurse
in a direct care-giving role below that of the Band 5
registered nurse. Further the success of initiatives to
formalise the training of Band 4 assistant practitioners
is likely to depend on clear role boundaries and strong
leadership.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 29
15. Boundary disputes and professional identity
The relationships between registered and non-registered staff has resulted
in debates in the literature about boundaries and professional identity. A
number of papers have addressed this subject area.
Nancarrow and Mackey (2005) identied a lack of a clear
career direction for qualied occupational therapists,
creating uncertainty about which aspects of their job
they should be ‘giving away’ to assistants. This resulted
in a need to clarify career structures and accountability
relationships between existing and new sta members
and ensure that appropriate training is available to
support sta in their new roles.
Bosley and Dale (2008) provide a detailed overview of
the literature in this area in relation to nursing. They
observe that nurses may experience uncertainty as
they themselves are asked to take on tasks previously
undertaken by medical sta and in turn see their
traditional domain “encroached” upon by HCAs. Nurses
dierentiate themselves from HCAs in a number of ways:
by professional qualications and their accountability
as registered healthcare professionals; their level of
knowledge; their emphasis on patent-centred, holistic
care in comparison to their perceptions of HCAs
undertaking a task oriented approach. There is evidence
of nurses sensing a loss of relationships with patients
and attempting to protect their identity by restricting
the roles of HCAs. Equally HCAs may choose to withhold
patient and other information from nurses in an attempt
to increase their inuence. This leads to the conclusion
that neither of these situations are conducive to eective
teamwork or patient care.
Leach and Wilton (2009) carried out an evaluation of
sixteen APs in a number of occupations in an English
Strategic Health Authority (SHA). The APs reported
initially encountering fear from registered sta that their
professional roles were being eroded. This prompted the
authors to observe that this echoes “the reluctance of
some registered sta to either let go skills that they had
thought belonged solely to them or the fear of letting
unregistered sta practice these skills without direct
supervision”.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 30
16. Roles and scopes of practice
i) Classication of and types of roles
The CAHE systematic review (2006) neatly summarises
the range of activities carried out by HCSWs in terms of
direct and indirect roles. Charting these roles over time
as HCAs have evolved into HCSWs, the review notes that
typical activities of housekeeping, hotel, clerical and
general care duties have changed somewhat to support
workers concentrating more on basic care duties and
non-nursing duties.
A number of factors are identied by the review in
explaining the variety and diversity of roles undertaken
by HCSWs. These factors include the attitudes and
beliefs of the qualied health professional with whom
the support worker will work, lack of clarity of their own
role by the qualied health professional, the perceived
training of the support worker and the local needs of the
health service where the support worker is employed.
In addition personal and contextual factors such as
experience, responsibility and stang will play a part in
dening the HCSW role.
A full tabular description and analysis of the direct and
indirect roles of HCSWs is presented in the review. Direct
roles (table 6, p33) are summarised as combination
of general hygiene, portering and assistance in the
administration of clinical services. Indirect roles (table
7, p37) are typically a combination of administrative
duties, housekeeping and maintenance of workplace and
equipment.
More recently a systematic review of allied health
assistants charted their roles and responsibilities
(Lizarondo et al. 2010). The review classies these under
the headings of clinical and non-clinical duties. Typical
clinical duties include preparing patients for treatment,
providing patients with physical and social support,
patient education. Non- clinical duties encompass
areas such as administration, stock ordering, recording
statistics, housekeeping and cleaning. The review
observes that many of the clinical duties mirror those of
registered AHPs.
The reference to boundary disputes in the literature
point to the need for a clear denition of HCSWs’ roles.
However the evidence drawn from the literature suggests
that this is not the case in practice. The Welsh scoping
study (HPW 2004, p12) referred to previously noted that
“while the use of support sta in some professions may
have a long history and in others may constitute a large
proportion of the workforce, this does not necessarily
mean the roles are well dened. On the contrary”.
ii) Critique of HCSW roles
The literature reects the variation in HCSWs’ roles across
professions and also reveals a number of recurring
themes.
Thornley (2000) examined the roles of nursing auxiliaries
(equated to a lower grade HCSW) and HCAs. This study
concluded that “that the boundaries between so-called
‘ancillary’ work and ‘nursing’ work continue to be highly
blurred and uid, with both the traditional grade of NA
and the ‘new’ grade of HCA engaging widely in ‘nursing’
duties, and with job titles used almost interchangeably in
most Trusts”.
Ellis and Connell (2001) looked at the roles of
physiotherapy assistants and concluded that there was
variation in the scope of activities of the 18 assistants
across one English NHS region. Supervisors in the study
were of the opinion that the assistant’s role equated
more to that of a junior physiotherapist in elderly care
and rehabilitation. The supervisors viewed the assistants
as undertaking new roles in the community in that they
were extending the availability of physiotherapy care.
Finally there was evidence in outpatient departments of
assistants undertaking new, extended roles and tasks, for
example electrotherapy.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 31
Baldwin et al. (2003) considered the evidence across all
sectors in the process of examining the roles of support
workers in nursing homes. The authors concluded
that the majority of the support worker role focussed
on direct patient care activities but that a lack of role
clarication was apparent. This was evident in dierences
of opinion between support workers and RNs over the
role of support workers in the care process. Support
workers regarded their role as similar to RNs whereas
nurses saw them as providing “basic nursing care”.
Keeney et al. (2005b) in reviewing the literature around
this theme identied a number of interesting ndings
from research that had been carried out in relation
to HCA roles. These include a UK study (Anderson
1996) which reported diculty among qualied sta
in accepting their need to alter roles as a result of the
introduction of HCAs. This study identied the lack of
a clear distinction between the activities that lie within
and outside the domain of qualied sta. Previous to this
Harper (1986) had concluded that with the increased
number of HCAs in the UK, nurses would drift away
from direct patient care to indirect supervisory roles. He
warned that caution was needed as more nursing time
could be spent on the supervision of HCAs, leaving little
time for other professional interventions. Keeney et al.
also cited a number of other similar reports which they
feel demonstrated concerns that HCAs were undertaking
nursing activities which should only be performed by
nurses (Dolt 1998, NHS Executive 1998, Snell 1998).
Hancock et al. (2005) also present a comprehensive
overview of the literature in this area in setting the
context for their research into role development of HCAs
(see also Hancock and Campbell 2006). The study was
small in scale but a noteworthy aspect of this research
was the inclusion of patient’s views. In practical terms
the study revealed that HCAs were taking on roles
normally associated with nursing such as taking blood
and dressing wounds. However organizational and local
culture appeared important in dictating the boundaries
of the HCA’s role.
The authors address the particular question of
delineation in relation to HCA and nursing roles. The
study found that after the HCAs had completed a
development course their role was not well dened and
variations existed. Although changes were detected
in the HCA roles the majority of registered sta were
reluctant to delegate core ‘nursing’ activities for a
variety of reasons: role transition, uncertainty about
role boundaries, fear of losing part(s) of their role and
concerns about responsibility.
In analysing the reasons for this reluctance the authors
identied cultural competence and trust as being key as
to why certain HCAs were able to develop their role more
than others. Cultural competence relates to the beliefs,
values, norms and practices of a group which guide its
thinking, decision making and action. It is encapsulated
in the phrase “the way we do things around here’. In
reality this meant that “HCAs practised according to
local agreement, with signicant variation between
wards/departments about what constituted acceptable
practice”. This is put forward as an explanation for the
change or absence of change in HCAs roles.
Similarly trust was identied as being pivotal to the HCA
role and was aected by their relationship with their
colleagues. Although the HCA may have demonstrated
cultural competence in terms of awareness of their own
role and how it tted into the team there was also the
issue of trust to be considered. The authors refer to
Rogers (1983) who suggested that the need for power
over others is based on a lack of trust, and that until trust
is established, those in power will always feel it is their
obligation to control. This may explain the reluctance of
some RNs and Midwives to allow HCAs to develop their
roles.
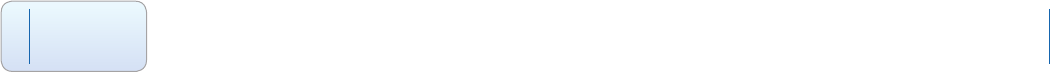
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 32
These ndings have implications for the content of
educational programmes in that they must take account
of context. It is not enough to assume knowledge
acquired via an educational programme is independent
of the personal, interpersonal and organizational context
that it will operate in. With this in mind the authors put
forward recommendations to improve the environment
that HCAs develop their roles in on completion of their
educational programme. These recommendations
include provisos that: explicit policies in relation to roles
of the HCA should be formalized in discussion with HCAs
and their colleagues; and that a consistent, formalized,
open approach to role transition is required at both local
and organizational levels in order that role changes are
successful.
A number of recent studies have specically looked at the
introduction of assistant practitioners into the workforce
and their role. Spilsbury et al. (2009) mapped the roles
of assistant practitioners across acute trusts in England
by canvassing the opinions of directors of nursing. They
found that APs were mostly being employed in medical
and surgical wards. A recurring theme in their research
however was uncertainty on a number of levels as to the
role of assistant practitioners and this extended to other
HCSWs. In particular there was a need for role clarication
between bands 2, 3 and 4 support workers. This was
apparent in hospitals where APs have been introduced
as there was uncertainty between the roles of bands 3
and 4. Equally in hospitals where there was no APs the
directors of nursing were of the opinion that the existing
bands 2 and 3 were already operating in extended roles
and so there was no need to introduce band 4 APs. This
also prompts the question of whether such bands 3 and
4 are being undervalued and underpaid.
Continuing the investigation of APs, Wakeeld et al.
(2010) examined the job descriptions of 27 AP roles
in three acute trusts in England. They examined the
job descriptions against a framework that categorised
their clinical roles in terms of their emphasis on how
independent or dependent the role was. This is in the
context that AP roles should deliver protocol based care
which would have previously been the responsibility of
registered practitioners and that such care should be
under the direct supervision of a registered practitioner.
The study found that there were instances where APs
were expected to go beyond delivering protocol based
care and act independently. This contradiction leads to
uncertainty as to where the AP role ts into the nursing
workforce. This uncertainty is exacerbated by the Skills
for Health (2008) career framework descriptors which
recommend that level 4 practitioners (i.e. assistant
practitioners) should “develop self-directed working
practices” and “make judgements requiring comparison
of options”.
The study concludes that “it still not clear what managers
and workforce planners want from the AP role as it
does not have a clearly dened position in the clinical
hierarchy despite being located at level 4 on the SfH
(2008) Framework.”
Confusion over the role of APs is echoed in McGowan
and Campbell’s (2010b) account of the introduction of a
pilot scheme to introduce APs in a chemotherapy unit.
One of the main ndings from the evaluation was that
nursing sta were confused about the AP role and their
level of responsibilities. The pilot scheme’s solution was
for the trainee AP’s mentor to give nursing sta verbal
and written updates on their progress including the
clinical competencies they had achieved. Looking at the
wider picture the authors believe that there is a need for
the roles of newly qualied sta nurse, APs and nursing
assistants to be clearly dierentiated.
iii) Guidance on HCSW roles
The need to remove ambiguity from HCSW roles and
has led to the emergence of guidance documents. The
aim of these documents is to specify the types of roles
that HCSWs can undertake and in so doing introduce a
degree of uniformity. Examples of these include setting
out role parameters for the three levels of HCSWs (NES
2010) and scopes of practice produced by professional
organisations (see for example College of Radiographers
2007a, b) which outline acceptable and equally
importantly unacceptable roles for radiography APs.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 33
17. Tasks conducted by HCSWs
At a micro level Bosley and Dale (2008) summarise the constituent tasks which
HCAs incorporate into their roles in both the secondary and primary care
sectors.
In a hospital setting these include practical nursing care
such as bathing and emotional support. In some cases
the literature reects the feeling that HCAs are able to
build up closer relationships with patients than nurses
and perceive their role to be similar with the exception
of drug administration, paperwork and professional
accountability. There is also evidence in the literature of
HCAs going beyond what would be generally deemed to
be the boundaries of their levels of responsibility. Tasks
identied in this context include: undertaking systematic
observations and electrocardiogram tracings; monitoring
blood glucose levels without supervision; taking blood
and dressing wounds; administering drugs while
unsupervised; running clinics without a nurse. Further
the HCA role has been found to encompass teaching
nursing students and newly qualied nurses and
communicating with doctors about patients. In general
practice HCAs have been trained to undertake clinical
procedures such as blood pressure and new patient
checks, health promotion, urinalysis, weight and height
recording, ordering supplies, equipment sterilisation and
phlebotomy.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 34
18. HCSW job descriptions
A number of studies have specically examined HCSW job descriptions.
The Welsh scoping study (HPW 2004) identied 103 job
descriptions, most commonly in nursing, occupational
therapy, physiotherapy and speech and language
therapy. The job descriptions were analysed to identify
common tasks, roles and skills across the professions.
The analysis revealed a number of generic and specic
skills. Generic skills were summarised under the headings
of: team working; care delivery (direct/indirect, clinical
skills); supporting trained sta; assisting with care
delivery; health and safety/patient safety; equipment/
stock maintenance; record keeping; administration and
communication.
Specic skills were associated with the HCSW displaying
more autonomy and assuming greater levels of
responsibility. These types of skills included: carrying a
caseload under supervision; patient/client assessment;
teaching new sta and/or patients; client group skills;
supervision of new and other sta.
Benson and Smith (2006) investigated the drawing up
of job descriptions in the “Delivering the Workforce”
project to develop the assistant practitioner role in
Greater Manchester. Their research revealed varying
progress across respective pilot sites in the project in
drawing up job descriptions. This meant that as some
trainee assistant practitioners neared completion of their
training there was the possibility of no job description
being in place for them as they took up their duties. In
reality job descriptions should denitely be in place at
this stage. This has implications in ensuring that there is a
clearly dened role for the AP which has been identied
elsewhere in the literature as being important for the
ecient functioning of the post (CAHE 2006). A clearly
documented denition of roles is essential to avoid
confusion among other healthcare professionals as to the
boundaries of respective team members’ duties.
Wakeeld et al. specically examined the job descriptions
of assistant practitioners in two related studies. The rst
study (2009) analysed the job descriptions of 16 AP posts
in an acute hospital trust in England. The aim of the
study was to compare the content of the job descriptions
against the policy vision of the posts as being assistive in
nature. Assistive essentially means that “APs are expected
to undertake those tasks specically designed to assist
and support the work of the registered practitioner
under whose direct supervision they are managed”. As
such the AP is not expected to act autonomously or
independently. Analysis of the job descriptions revealed
that only one post was truly assistive with the remainder
being classied across a framework encompassing
various elements of supportive, substitutive and
autonomous practice. This situation leads the authors
to conclude that this has the potential to lead to role
confusion, role conict and exploitation around the
AP role. In reality this could lead to role substitution,
reassignment and delegation which is not what the AP
role was intended for.
The second paper (Wakeeld et al. 2010) widened
the study by adding another 11 AP job descriptions
from a further two acute trusts to the original 16 job
descriptions. The extended study conrmed similar
ndings to the rst in terms of classifying the additional
job descriptions as assistive, supportive, substitutive and
autonomous. The authors highlight the contradiction
from Skills for Health level 4 career framework descriptors
(Skills for Health 2008) which call for APs to “develop self-
directed work practices” and “make judgements requiring
comparison of options”. In eect these desired actions
go beyond assisting or helping and being self-directed
and making judgements are associated with registered
practitioner roles.
The crossover of practices from registered practitioners
to non-registered sta such as APs has the potential
to lead to blurring of role boundaries. One way of
countering role blurring is to draw up “robust, clear
and publicly-dened job descriptors” (cited by Rolfe et
al. 1999). However in this study Wakeeld et al. (2010)
conclude that “job descriptions did not clearly dene APs’
scope of practice. This led to confusion about what they
could, should and/or did undertake as part of their role”.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 35
19. Regulation
Regulation of HCAs and HCSWs is a subject which has recurred over time in
the literature.
Hopkin (2008) identies a number of aspects which
characterise regulation. Essentially regulation entails
being on a professional register which brings with it
professional accountability. In eect any member of the
healthcare workforce has a duty of care to their patients
but it is only those who are professionally regulated who
are held professionally accountable. Regulation also has
many facets other than being on a professional register.
These facets include having standards for practice and
education which include standards of entry to the
register, a code of ethical conduct, titles that are clearly
understood by all and an agreed denition of roles and
functions. Most importantly entry to a professional
register requires evidence of tness to practice in relation
to health, character and training.
There has been an ongoing debate in the literature
regarding the regulation of HCAs and now HCSWs and
it has gained increased attention over recent times
(O’Dowd 2009, Blakemore 2009). The purposes for
professionally led regulation are outlined clearly by the
RCN (2007) as: public protection; education; safety of
the individual; competence; performance management;
quality assurance; setting standards. Arguments in
setting the case for and against regulation have been
well rehearsed in the literature. Briey the arguments
for are that HCSWs are in direct contact with patients
and regulation will provide patient safety and public
protection (Hopkin 2008). Equally regulation will protect
individual HCSWs by providing standards, education,
professional development, dening their scope of
practice and giving value and recognition to their role.
Conversely regulation is undesirable (Youg 2008)
because it in itself will not provide protection for patients
as evidenced by a number of high prole medical
scandals (e.g. Shipman, Allit) where patients were
harmed by regulated healthcare professionals who had
already proved their knowledge and competence to
practice. Patient safety depends on any number of other
factors such as trustworthiness of the individual involved
which will not necessarily be picked up in the regulation
process. Also in a nursing context the regulation of
HCSWs may lead to the mistaken belief that they are
suciently qualied to replace nurses. Essentially
the question is posed - “is it safer for the public to be
cared for by a number of HCAs who are led, monitored
and supervised by nurses, or by HCAs, who, following
regulation, are perceived by many to have the ability
and authority to decide what nursing care is needed by
patients?” The author believes that in scally challenging
times the opportunity to replace nurses with regulated
HCAs would be too tempting with an overall increase
in the number of the latter at the expense of the former
based on the justication of regulation.
i) Government policy
The background to policy developments in the
regulation of HCSWs are outlined in depth by Birch and
Martin (2009). The debate on regulation has also been
conducted by government. Two parallel consultations
were held in 2004 seeking views on the regulation of
support workers by the Department of Health in England
(which also covered Wales) and the Scottish Executive.
Both consultations resulted in a consensus for regulation.
In Scotland there was a strong majority (90%) and in
England a subsequent white paper resulting from the
consultation intimated that those who responded to
the consultation were in favour of regulation for some
types of support workers but not necessarily all of this
occupational group.
As a consequence of the consultations and consideration
by the Review of Non-medical Regulation (Foster Review
2005), Scotland was chosen to pilot a project for the four
home nations which addressed minimum standards
for HCSWs. The standards contained three elements:
induction standards for healthcare support workers; a
code of conduct for healthcare support workers; a code
of practice for NHS Scotland employers. The pilot was
conducted on a voluntary basis over two years in three
health boards and an independent sector hospital. The
ndings are detailed by QIS (2008) and Birch and Martin
(2009). As a result of the pilot induction standards for
HCSWs are to become mandatory in Scotland from
December 2010.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 36
ii) Professional and regulatory bodies
The Royal College of Nursing (RCN) is clear in its
support for regulation (RCN 2007). Prior to this the RCN
had allowed HCAs with a level 3 NVQ to join the RCN
register (Hancock et al. 2006). The RCN’s commitment
to regulation was recently reiterated by its general
secretary Peter Carter who thinks that it would rectify
the “fragmented approach” to training across the NHS
(Sprinks 2009). The RCN would initially like to see
APs regulated rst in a staged process for all HCSWs
(RCN 2007) but others caution against this single level
approach.
Adams (2010), in arguing the case for regulation as
head of nursing at UNISON, notes that there too many
variations in the roles and responsibilities of HCAs to base
regulation on a job title (or equally a pay band) alone.
As such all HCAs should be regulated. UNISON currently
favours HPC to be the body responsible for regulation
(Santry 2010).
The issue of regulation has prompted recent comment
from the Nursing and Midwifery Council (NMC) that
they are in favour of such a process and accordingly
they commissioned research from the National Nursing
Research Unit (NNRU) to explore the matter further
(Santry 2010). The NNRU subsequently published a
scoping report (Griths and Robinson 2010) which
summarised the evidence surrounding a number of
aspects of regulating HCSWs. Interestingly the authors
conclude that there is a “strong” case for regulation
despite being unable to nd unequivocal evidence that a
lack of regulation for HCSWs poses a risk to patient safety.
The rationale for regulation is that the current situation
allows individuals who have been previously dismissed
from healthcare posts for misconduct to be re-employed
as support workers. Also it is evident that HCSWs are
currently undertaking clinical tasks that they are not
trained for which poses a potential risk to patients.
The report goes on to note that regulation will have
implications for the standardisation of training.
The current unregulated status of HCSWs has attracted
recent comment in the literature. Bosley and Dale
(2008) recognise the positive aspect of regulation in
that it would standardise training but on the downside
the formality and increased responsibility associated
with it may deter some from going down the route of
developing HCAs. Spilsbury et al. (2009), in a survey
of acute trusts in England, found that some had not
introduced the assistant practitioner role due to concerns
over patient safety related to the unregulated status of
this group. Wakeeld et al. (2010) point out the pitfalls
of the current situation for APs in that they are caught
between two stools. One stool is the unregulated one
and the other is regulated by registration and legislation.
Having analysed their job descriptions and noted that
in some cases the APs are involved in substitutive and
autonomous nursing tasks, this could leave them in an
exposed situation if something were to go wrong. In this
case there would be no clear directives to guide their
actions and give them subsequent protection.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 37
20. The impact of HCSWs
One of the reasons cited for the non-introduction of assistant practitioner
roles across some trusts in England was a lack of evidence for their
effectiveness (Spilsbury et al. 2009).
Having identied the outcome measure the review
summarises the eects identied by them in the
literature. However there is a health warning given as
to the quality of the research. Most of the evidence
emanates from qualitative research which is limited
by methodological deciencies. Further the nature
of qualitative research restricts the generalisability
of its ndings. In addition empirical evidence based
on sound outcome measures is described as “scant”.
Notwithstanding these deciencies the review
summarises the evidence as mostly positive across all
outcome measures and stakeholder groups (table 10,
p52).
An example of study contained in the CAHE review is
research by Hancock et al. (2005). This was a small scale
qualitative study which aimed to evaluate the impact of
a HCA Development Programme on care delivery. With
this in mind participants in the study included patients
themselves. In undertaking the study the authors
concurred with the general feeling that “there is a lack of
comprehensive evidence regarding their role in terms of
their contribution to, and impact on, patients and other
members of the healthcare team”. The study ndings in
relation to patient care concluded that completion of the
programme had resulted in a more holistic approach to
care.
Similarly Betts et al. (2003) describe how the introduction
of Radiography Assistant Practitioners enabled them
to sta a chest room which they had previously had
diculty in operating due to a diculty in recruiting
radiographers. The Assistant Practitioners helped spread
the workload in their department and in doing so
reduced stress and pressure for other sta and improved
the overall service for patients.
Bosley and Dale (2008) concur with this view and report
that “despite very limited evidence of the impact or
eectiveness of HCAs, the role is being advanced in
general practice”. Recognition of the need to evaluate
the impact of HCSW roles has led to the initiation of a
programme of research, which is currently underway,
funded by the Department of Health (Spilsbury and Atkin
2009).
A review of the literature suggests there is some limited
evidence of impact and that which does exist is of
questionable quality and value. The systematic review
of rehabilitation support workers (CAHE 2006), which
was broadened to look at all support workers, sought to
identify rstly outcome measures by which eectiveness
could be measured and secondly what evidence exists by
virtue of these outcome measures.
Outcome measures identied in the review were
categorised as relating to (a) patients, (b) individual(s)
providing healthcare and (c) other stakeholders with
an interest but not directly involved in patient care e.g.
funders, managers and the community. Typical outcome
measures for patients were satisfaction, communication
and quality of living measures. For those providing the
healthcare, measures included eciency, knowledge
and skills and job satisfaction. Measures for the other
stakeholders related to costs, quality of care, safety and
recruitment and retention.
In summary the outcome measures reported in studies
related to either evaluation of services provided by the
support worker or evaluation of training programmes for
them.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 38
A small scale study of the impact of associate and
assistant practitioner roles is reported by Leach and
Wilton (2009). This study was conducted in an English
strategic health authority across a number of occupations
in both acute and primary care. The views of APs and
managers were sought by questionnaire and interview.
The study reports the perceptions of participants and as
such anecdotal evidence is presented. Identied impacts
cited were benets to patient care, service improvement,
cost eectiveness and personal benets for the APs. The
anecdotal nature of the ndings is acknowledged by the
authors who highlight the need to substantiate these
with hard evidence.
The perceptions of the impact of the Assistant
Practitioner role on practice is presented by radiography
mentors and APs themselves in an evaluation of an
educational programme. The APs mainly saw their
role as an enabling one in freeing up radiographers to
undertake more specialised examinations (Colthart et
al. 2010b). This recognizes their role in the radiography
four tier model (DH 2003) and their contribution to
the radiography team. The four tier model was a new
model of service delivery within radiography initiated
in 1999. The model has four levels that represent
escalating competencies and responsibilities within a
multidisciplinary team. The rst level is the assistant
practitioner which progresses into the levels of
practitioner, advanced practitioner and consultant
practitioner.
Assistant Practitioners in diagnostic imaging undertake
the non-complex radiography procedures as laid down
by their scope of practice (CoR 2007a). This should enable
radiographers to expand their own role within radiology
services, providing a more ecient clinical diagnostic
pathway for the patient, including reduced waiting times.
In radiotherapy, more generic impacts were identied,
like maintaining capacity by providing cover for sickness
absences.
Similarly mentors (Colthart et al. 2010a) oered their
perceptions of the impact of the APs in aspects of
their radiography department’s operations. The largest
positive eect was observed in teamworking with 15
out of 22 mentors noting a benecial outcome from the
presence of trainee APs. Similarly half of the mentors
(n =11) felt the programme had been benecial for
the patient’s experience in their department. On the
downside some mentors reported a negative impact on
the speed of service delivery but not on the quality of
practice.
i) Benets of HCSWs
The literature identies a range of benets for employing
HCSWs but most of these are anecdotal given the lack of
robust evidence of the impact of the roles at the present
time. For example Leach and Wilton (2008) evaluated
the introduction of associate and assistant practitioner
roles in a strategic health authority in England. The
evaluation included the views of both the APs (n =16)
and managers (n=6). Perceived benets identied from
the establishment of these HCSW posts are categorised
under a number of headings: patient care; service
improvement and team benets; cost benets; personal
benets.
In terms of patient care the APs felt that they contributed
positively to the patient experience and delivery of care
in a number of areas: by providing continuity of care;
by being able to spend more time with patients which
allowed them to communicate, explain procedures and
answer their questions; by observing if changes in care
were needed by being the member of sta who was
most in regular contact with patients. Other indirect
benets of the AP role for patient care included freeing
up registered sta to take on more complex clinical
procedures and in helping to shorten or prevent hospital
admissions.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 39
Service improvements cited included observing the
processes and procedures used and identifying changes
to transform the care provided to patients. Examples
include:
-in a Radiography department APs have reorganised
the use of rooms to ensure that all paperwork is
completed and patients are fully prepped to allow
them to go straight in to the X-ray room once it is
free, ensuring there are no gaps in service delivery.
-an incontinence assessment tool has been
developed by an AP, which, since its introduction
has cut the number of catherisations and has been
noted in an infection control audit.
Team benets relate to the role of the AP and how they
interact with other members of sta. APs have been
noted as supporting band 2 and 3 sta. In some cases
this has been formalised in job descriptions thus: “APs
help to train new band three assistants and assist in
the management of their workload, helping practically
when required”. Such supervision frees up registered
from performing this type of task. In practical terms
examples were cited of APs signing o competencies
for radiography students and catheterisation for junior
doctors. Looking forward, all the APs would like to
become mentors for trainee APs and some would like to
progress to become NVQ assessors.
Other associated benets for members of their teams
related to freeing up time for registered sta. This
allowed such sta to take on more complex clinical
cases as previously mentioned and also enabled them to
spend more time on assessing, planning and evaluating
their clinical work. More free time also allowed some
registered sta to able to attend courses. APs were also
seen as a resource in covering for sick leave and in so
doing helping to keep waiting lists down.
Reference was also made to cost savings by respondents
to the evaluation (both APs and managers) but these
nancial benets are not backed up by any hard
evidence and are purely based on subjective personal
opinions. For example the manger of a breast screening
unit observed that “I can have two APs for the price of
one mammographer” without any economic appraisal
of the relative merits or costs in changing the skill
mix in this way. In this respect Lizarondo et al. (2010)
note that the cost eectiveness of alternate workforce
models which incorporate HCSWs have not been widely
investigated to date. Therefore research is required with
cost eectiveness as a central outcome measure to
evaluate the impact of HCSWs in the workforce.
Personal benets for the APs are summarised as being
greater job satisfaction and enhanced self-esteem. The
APs were glad to have had a second chance at education
and were proud to have changed the attitudes of
registered sta towards them. In some cases the positive
experience of becoming an AP had translated into their
personal life.
McGowan and Campbell (2010a), in their evaluation
of introducing the AP role into a chemotherapy unit,
summarise the benets of the AP role outlined in the
literature. These benets described validate some of
those identied by Leach and Wilton (2008 above). In
particular in enabling registered nurses to perform more
complex procedures and assessments and to use their
skills and knowledge more appropriately and eectively;
facilitating continuity of care. In addition oering AP
development opportunities may oer career progression
to non-registered sta and in so doing facilitate sta
retention. Career advancement may also encourage APs
to consider studying to become a registered professional
(cited from Macleod and Clark 2007).

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 40
21. Stakeholders’ insights into HCSW education and the role
i) Views of HCSWs
A number of studies have reported on HCSWs’ own
experiences and perceptions. These studies tend to
concentrate on the views of HCSWs in evaluations of
education programmes to prepare them for the role
rather than investigations into the role itself.
An example of this is Keeney, Hasson and McKenna
(2005a) who report the views of 22 HCAs in Ireland who
were undertaking a national training course. Semi-
structured interviews with the trainees revealed positive
changes as a result of attendance on the course. Benets
cited by the trainees included more condence in their
ability to undertake delegated duties and improvement
in their knowledge and care skills.
Similarly Hancock et al (2006) sought the views of
HCAs on two particular aspects of their development.
Firstly the impact (outcomes) of their attendance on
an education programme to develop their role and
secondly the preparedness of HCAs to undertake the
programme and the new developed HCA role they
would be undertaking. The outcomes indicated positive
changes to the HCAs’ role, which included skill and
knowledge development, increased condence and
initiative and a more holistic approach to care. Secondly
there was a range of opinion from the HCAs on their role
development with both favourable and unfavourable
views expressed. Similarly not all HCAs interviewed (2/12)
were willing to enter an educational programme to assist
their role development.
Another account of student experiences is reported in a
case study describing the piloting of a training course for
assistant practitioners in a chemotherapy unit (McGowan
and Campbell, 2010). Initially students felt apprehensive
on beginning the course but developed condence
in their clinical practice ability as it progressed. Other
issues highlighted by the TAPs included the workload
associated with the course. There was also anxiety
expressed in moving from a further education college
to a higher education college for one of the units.
Associated with this was the dierence in moving
from SCQF level 7 to level 8 education in terms of a
perceived “step up”. Finally the TAPs stressed the need for
formalised clinical and educational support and that this
must be clearly outlined at the outset for both students
and those supporting them.
In terms of views on the particular HCSW role, Dranseld
(2006) gives an anecdotal, personal account of his four
years as a radiography Assistant Practitioner. Initially
he reports there was reservation from some sta and
a degree of uncertainty as to his responsibilities and
boundaries due to a lack of clear guidelines. However
with time the role became more accepted and his
responsibilities were claried and extended, particularly
in the last year of his account.
Most recently Kessler et al. (2010) present an informative
summary of HCAs attitudes to their role. This was a
comprehensive two year study commissioned by the
National Institute for Health Research (NIHR) which
used a mixed methods approach to explore a variety of
aspects of the HCA role in England. The HCAs included
in the study demonstrated disaection with their
banding (band 2) and their associated pay, qualications
and tasks. In eect they felt they were undervalued for
their qualications and were able to carry out more
advanced tasks than they were being paid for. In some
cases this lead to entrenchment into Band 2 roles
and a reluctance to take on more advanced tasks and
duties. Other diculties were encountered in HCAs’
relations with nurses and other healthcare professional
groupings. On the positive side the HCAs enjoyed their
jobs and in particular the patient centred aspect of it
which gave them intrinsic rewards in caring for others.
The enjoyment of their jobs manifested itself in the
HCAs expressing job satisfaction and low intentions to
leave the role. The study also identied an emotional
dimension to the HCA role. Firstly in the HCAs managing
their own emotions (e.g. dealing with death) and also
dealing with others’ emotions (e.g. patients and their
relatives).

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 41
ii) Views of managers on the role
Mackey and Nancarrow (2004) evaluated the
introduction of assistant practitioners in occupational
therapy among a range of stakeholders including
managers. These new roles were viewed as a challenge in
that a degree of innovation and exibility was required
to introduce them but these elements were restricted by
the need to adhere to clinical governance. The managers
identied a range of factors which were seen as helpful
in implementing the AP role: having a ‘champion’ for the
role at the management level, an innovative and exible
environment for service delivery, willingness of managers
and clinicians to try new ideas and learn from their
mistakes, and a team attitude that embraces ‘modern’
ways of working.
Keeney, Hasson, McKenna (2005b) surveyed healthcare
managers in Ireland on their attitudes to a national
training course and their willingness to employ HCAs
who had completed the course. The training course
contained core units and elective units relating to their
particular area of practice. Most of the respondents
(n=70) indicated a willingness to employ HCAs and
identied additional content they would like added
to the training. This related to mental health, health
promotion, care of the elderly, challenging behaviour
skills and training in the management and prevention
of violence. Managers thought it important to have
explicit standard entry criteria for the course. In terms of
the role of the HCA, most managers saw it as supporting
nurses and midwives but a small number felt that it could
encroach on these professional groups. The authors note
that perceptions of encroachment has the potential for
role confusion, role strain and role conict.
Leach and Wilton (2008), in an evaluation of associate
and assistant practitioner roles, sought the views of
mangers as to developing these roles. The principal
advice was the need for good communication with all
members of the department and the importance of prior
planning. This involves examining carefully what the
department’s service needs are and drawing up a clear
job description. Managers also identied the need for
them to support the APs in a number of ways. Primarily
in the role as champion as many of the APs indicated
that they would not have undertaken the foundation
degree without the prompting and support of their
mangers. The manager also had an important role to play
in allaying the fears of other members of sta who felt
threatened by this new role.
iii) Views of registered practitioners on
the role
There literature frequently makes reference to the
attitudes of registered sta to HCSWs (CAHE 2006).
The following references are illustrative of the views of
healthcare professionals to the HCSW role.
Mackey (2004) examined the views of occupational
therapists to extending the role of support workers. A
series of focus groups were held across a community
trust in England with 36 participants taking part. The
main factors identied as being of importance in
extending the support role were the need to: increase
role clarity; lessen role threat; review organizational
eectiveness; ensure clear delegation and design and
implement responsive training programmes. In addition
the author noted that many of the OT support workers
had completed or were in the process of attaining a NVQ.
However not all qualied occupational therapists were
aware of the content, assessment and knowledge base of
this type of qualication.
Alcorn and Topping (2009) specically addressed
the question of registered nurses’ attitudes toward
healthcare assistants. They employed a survey method
which received responses from 148 RNs working in the
surgical directorate of an English NHS trust.
The study revealed that most RNs indicated they
delegated tasks to HCAs and recognised that they
themselves remained accountable for the action of those
HCAs. The majority of RNs did not perceive their role and
the role of the HCA as the same. More than half of the
respondents felt that HCAs should be held accountable
for their actions if adequately trained and prepared
and were in favour of registration for HCAs. Expansion
of the HCA workforce was perceived by a minority as a
strategy to replace RNs and a cost-cutting exercise. Most
respondents agreed that patient care was enhanced via
investment in the development of HCAs. The authors

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 42
The study revealed that in general, patients could not
easily identify HCAs and in so doing dierentiate them
from registered nursing sta. Notwithstanding this
diculty however it appeared that patients in general
were able to relate better to HCAs than nurses. Further
it emerged that HCAs appeared better equipped than
nurses in dealing with patients in certain circumstances,
for example when patients were upset or confused.
However patients in other types of situations still
preferred to interact with a nurse rather than an HCA.
The research revealed that when patients were able to
distinguish between HCAs and registered nurses they
reported a more positive care experience. This leads
to the conclusion that it is important to help patients
recognise HCAs and educate them as to their role so they
are better informed about what member of a ward team
to approach in a given situation. In this respect dierent
types and colours of uniforms will not in themselves
educate patients and the onus is on sta to introduce
themselves and their particular role and responsibilities
to patients.
conclude that the role of RNs in developing HCAs has
implications for their own training needs in ensuring that
they are adequately equipped to supervise and delegate
work to HCAs.
Kessler et al. (2010) investigated the views of registered
nurses toward support workers. The study concluded that
in general nurses valued the support workers but there
was some ambiguity around certain role boundaries
reecting this recurring theme in the wider literature.
iv) Views of service users on the role
A small number of studies have sought the views of
service users on their interactions with HCSWs. Mackey
and Nancarrow (2004), in their evaluation of OT assistant
practitioners, included the views of a limited number
of patients. The study revealed that patients could not
dierentiate between qualied and unqualied members
of sta. Further to this patients had no concerns about
sta members having formal qualications as long
as that member of sta was properly trained to do
their job. There was a lack of understanding of the OT
AP role among patients who did however value the
ability of such workers to spend more time with them
on a regular basis. One area noted as important by all
stakeholders to the evaluation, including service users,
was the supervision of APs, both formal and informal.
Interestingly the APs themselves and their managers put
forward the theory that APs are able to identify more
easily with patients than registered sta as they tend to
come from a similar background and do not use technical
or complicated language.
More recently Kessler et al. (2010), in their study of HCAs
in English acute hospitals (in medical and surgical wards),
investigated the views of former patients by focus groups
(n=94) and questionnaires (n=1651) in two separate
phases of their study. The project identied three
particular research questions in relation to the impact
of HCAs from the patient perspective, namely whether
patients could tell the dierence between HCAs and
nurses; whether patients developed a dierent type of
relationship with HCAs and nurses; and if so, whether this
dierence mattered to patients.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 43
22. Development into registered roles
There is an appetite for a section of HCSWs to develop themselves further
into registered healthcare professionals.
category who had recent academic study experience.
In contrast younger students with little academic
experience were signicantly less likely to successfully
complete the course. This has implications as the
typical prole of a HCSW is a mature female who lacks
formal qualications and academic experience. This
suggests that putting systems in place to support the
learning of HCSWs is important particularly for those
with no recent academic experience. In terms of the
content of pre-registration nursing courses biological
science was found to be most problematical for
students to grasp ahead of any other theoretical
teaching. Finally research into pre-registration nursing
courses has highlighted the support required by
older learners. This is particularly in relation to their
domestic commitments as for example they would
appreciate clinical placements nearer home. This is
directly relevant to HCSWs who are likely to fall into
this category of type of learner.
Hibbert (2006) undertook a qualitative study to
investigate the factors that affect HCAs progressing
to nurse training. Semi-structured interviews were
held with all 28 strategic health authorities (SHAs)
in England. The main factors identied as hindering
HCAs progressing were: a lack of denition of the
HCA role and the level they should be operating at;
lack of nancial support; low numbers of HCAs being
able to access secondments into nurse training which
are regarded as being the only viable affordable
training option especially for mature HCAs; a lack of
recognition of HCAs existing knowledge (e.g. NVQs)
which is then duplicated during nurse training thus
lengthening it unnecessarily; a perception from
the SHAs that HCAs lacked condence in pursuing
academic studies, for example academic writing,
completing assessments and in some particular
subjects e.g. physiology (related to this was a
perception that HCAs were concerned about studying
in groups of young learners).
Thornley (2000) in a survey of HCAs reported that 52%
were interested in undertaking registered nursing
training. McGloin and Knowles (2005) report on a training
programme for critical care assistants of which, on
completion of, all six went on to pre-registration nurse
training. A survey of AHP HCSWs in Scotland revealed
that 58% (207/357) would like to train as a qualied AHP
(NES 2008). Similarly a quarter (8/31) of radiography
APs in Scotland would like to train in time to become
radiographers (NES 2009). Kessler et al. (2010) surveyed
HCAs and found that across four acute trusts between
26% to 40% of them expressed ambitions to become
registered nurses.
There a number of challenges identied in the
literature associated with HCSWs training to become
registered professionals. Thornley (2000) sought the
opinions of HCAs and the main factor which would
impact on them undertaking such training was
related to nancial considerations. On the positive
side the ability to undertake training “on the job”
while maintaining employment would mean that
their salaries would be protected. This is particularly
important for HCAs who receive low incomes and
would not be able to sacrice these to train full-time.
Gould et al. (2004), in the absence of hard evidence
derived from the experience of HCAs undertaking
pre-registration nursing programmes, identied
a range of indicators associated with successful
completion of pre-registration courses by nursing
students. These indicators were predicted as being
potentially transferable to HCAs for them to be
successful in completing equivalent courses. A
number of studies were reviewed to provide an
insight into the type of individual most likely to attain
registration and the support they may require to
do so. Age and education were identied as being
predictive factors in a study of four pre-registration
diploma nursing cohorts at the same university
(evidence cited from Kevern et al. 1999). Those most
likely to be successful were mature women with
previous care experience and particularly those in this

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 44
These barriers led Hibbert to make a series of
recommendations to counter them: rstly to create a
clear denition of the HCA role; secondly to evaluate
nancial support for HCAs undertaking nurse training;
thirdly to establish transparent systems to improve
access to opportunities (e.g. secondments) to undertake
nurse training; fourthly HEIs should oer APEL for all
HCAs.
Kessler at al. (2010) found an association between length
of service as an HCA and desire to become a registered
nurse. Those who were newer to the role (e.g. 2 years or
less) were more likely to want to become a nurse than
those with lengthy periods of service (e.g. 10 years or
more). Similarly for those HCAs who held the desire
to pursue a nursing career this ambition progressively
diminished over time with a signicant drop after 10
years service. Reasons identied for not wanting to
become a nurse included: enjoyment of current HCA
role; exposure to the downsides of nursing from working
alongside registered sta; a perception of being too
old to begin studying; lack of condence in being able
to undertake a nursing role with the responsibilities it
entails; domestic pressures.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 45
23. The role of the Assistant Practitioner
Interest in the Assistant Practitioner role has intensied in recent times as
the futures shape of NHS workforce is examined and debated particularly in
relation to the nursing component (RCN 2009).
Briey the scoping exercise found that there was no
common denition of APs and summarised the impact
of the role that was evident this far. A total of over 60 AP
roles were identied across England working in dierent
service areas and associated with dierent professional
roles. There were variations in entry qualications
required to enter the role. The authors identied two
particular problems in relation to the operation of the AP
role in practice. Firstly in some regions it was reported
that senior sta were not completely comfortable with
APs and are not sure how they should be used and what
value to attach to their qualications. Secondly there was
feedback from some registered practitioners that they
felt APs “diluted” their own professional qualications.
The scoping report notes that the role has been
formalised faster in some parts of England than others
with dierent emphasis on foundation degrees as an
entry requirement. In practice the role itself diers in
terms of its breadth. Given all this, the authors conclude
that APs are still work in progress with lack of evidence as
to the best approach for developing the role.
In order to develop the AP role, Skills for Health (2009)
published a nationally transferable roles template which
includes both common core competencies and role
specic competencies.
The emergence of the assistant practitioner role has
attracted a number of papers dedicated to its particular
development (Nancarrow and Mackey 2005; Spilsbury et
al. 2009; Benson and Smith 2006; Leach and Wilton 2008,
2009; McGowan and Campbell 2010a, b).
A useful summary of the experience of introducing
the AP role over six years in NHS North West has been
recently published (Mullen 2010). There are now over
2000 APs embedded and operating in this SHA and
evaluations highlight four key characteristics that need to
be present in an organization to help ensure the smooth
introduction of the role. These are: a supportive team
with strong role awareness; consistent support from
management; clarity of role; regular clear communication
within the organization.
The interest in APs is illustrated by a scoping exercise
commissioned by Skills for Health which examined the
role in depth across England (Mackinnon and Kearney
2009). The scoping exercise was a result of concerns from
Skills for Health regarding variations in the role which led
to it setting up a task group to develop core standards
for APs in England. The report investigated the education
and training of APs, assessed their job descriptions and
identied the services and professions they support. The
scoping was carried out by a combination of interviews
with workforce leads in all England’s 10 SHAs, assessment
of AP job descriptions and a review of regional reports
recounting the particular development of APs in that
area.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 46
24. Future developments
As well as considering the past experience of HCSWs, the literature also looks
forward in considering what the future will hold for this fast developing group
of NHS staff. The following gives an indication of issues that are emerging
around the HCSW agenda.
Bosley and Dale (2008) report that more support sta will
be required to relieve nurses of routine healthcare tasks.
They suggest that up to an additional 74,000 HCAs will
be required over the next 20 years.
In terms of regulation Sprinks (2009) reports that
the Department of Health has no plans to introduce
standards for HCSW training, but is developing education
and training for NHS sta in ve key job roles, including
acute nursing support workers and maternity support
workers.
Unison has been consulting key stakeholders to develop
a national support worker induction programme and
proposals for mandatory training (Adams 2010). Unison
represents around 100,000 HCAs and is particularly active
in advancing their agenda.
Similarly Unison is drafting its own set of HCA core
competencies and specialist extras for areas including
acute and mental health which it will present at its HCA
conference in September 2010 (Clover 2010).
On the career front Spilsbury et al. (2009) identify a
plateau eect for some kinds of HCSWs, in this case
assistant practitioners, as there may be a lack of further
opportunities for such individuals to continue their
development unless they undertake training as a
registered professional.
25. Limitations of the literature
In considering the evidence presented one should be aware of the limitations
of the literature.
Kessler et al. (2010) summarised these thus:
“The literature on support roles in health provides insights
into these issues: on the personal characteristics of support
workers; on the malleability of roles; on their degraded
nature; and on the ambiguity of nurses’ attitudes towards
them. This literature has, however, been fractured, focusing
on discrete issues and lacking an integrated analytical
framework; it has also been uneven in terms of the issues
covered and in the forms of investigation”.
Similarly the scale and type of studies from which the
evidence is drawn has attracted criticism from Lizarondo
et al. (2010). These are typically small-scale, quality
improvement (case study) projects rather than larger
multi-centre projects from which more transferable
evidence can be drawn. The authors call for a mix of both
approaches as each can provide valuable evidence.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 47
26. Conclusion
A review of the HCA and HCSW literature presents a number of clear
messages relevant to supporting education and training for these groups of
healthcare staff. The main messages to emerge are as follows:
Denitions
-There is no universal denition of a HCSW and
various approaches have been used to categorise this
workforce. This lack of consensus has implications as
summarised thus:
“the lack of suitable and uniform denition
prohibits clear identication of the role played
by support workers, their boundaries for tasks
undertaken and prevents rigorous measurement
of their service performance” (CAHE 2006).
Workforce numbers
-The dierent denitions of the HCSW workforce makes
it dicult in establishing their precise numbers but it
is clear they are a substantial and growing element of
the NHS workforce.
Characteristics of the HCSW workforce
-The literature paints a fairly consistent picture of
HCSWs’ demographics, work backgrounds and
employment patterns. The demographics and caring
commitment demonstrated by a large proportion of
the HCSW workforce has implications for arranging
and supporting their training and education.
Education and training for HCSWs
-The literature points to reliance on informal training
for HCAs in earlier time periods with the introduction
of formal qualications for HCSWs in more recent
times. Historically the education and training has been
criticised for its lack of uniformity and consistency.
-A number of individual cases studies are presented
which point to a number of lessons when considering
the design of HCSW training. These lessons include:
the value of consulting stakeholders and service users
in their design; the need to equip participants with
study skills; the importance of establishing and having
support systems in place e.g. dedicated mentors.
Roles of HCSWs
-A recurring theme in the literature is the exploration
of the roles of HCSWs. The investigation has included
studies of job descriptions in an attempt to clarify
what tasks and duties HCSWs undertake. The
exploration of HCSWs roles reveals a number of
related issues which impact on how these sta and
their registered colleagues interact and work. These
issues include blurring of roles between professional
groups, boundary disputes and concerns over
professional identity.
-The literature reects variation and confusion
over HCSW roles which has consequences for the
registered sta they work with. The clear implication
from this is that HCSW roles should be clearly dened
and just as importantly clearly understood.
Regulation of HCSWs
-The literature embraces the long standing debate
over the regulation of HCSWs outlining the rationale
and benets of moving in this direction. A consensus
seems to have emerged from professional bodies
in favour of such regulation. The move towards
regulation has implications for standardising HCSW
training and education.
Impact of HCSWs
-There is limited evidence regarding the impact of
HCSWs on a variety of outcomes including clinical
practice. However this has been recognised and is
currently the focus of a Department of Health funded
project in England for the assistant practitioner
role. The evidence which does exists tends to be
of debatable quality and anecdotal in nature. That
said however a number of benets resulting from
the employment of HCSWs are put forward. The
establishment of robust evidence as to the value of
HCSWs will be important in consolidating these roles
and maximising their potential.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 48
Stakeholders’ views on HCSW roles
-The operation of HCSWs roles in multi-disciplinary
teams is reected in the range of insights to the
role provided in the literature. The views of HCSWs
themselves, their managers, mentors, supervisors,
registered sta colleagues and service users are
all presented. In terms of HCSWs themselves, their
views have been largely gathered in relation to their
experience of training and education rather than
on the role per se. However collectively all these
stakeholder insights are helpful in dening the role
and in the context of education and training in
identifying means of supporting those undertaking
such development.
Development into registered roles
-The literature suggests that a proportion of HCSWs
have aspirations to develop their careers and also
identies barriers and enablers to them successfully
attaining registered status.
Differentiation of HCSW roles in the literature
-The development of HCSWs on three career levels
is beginning to be reected in the literature. This is
evidenced by the number of more recent papers
dedicated to examining the assistant practitioner role.
This complements the existing body of evidence on
HCAs and support workers and gives a fuller picture
of these respective HCSW roles and the relationship
between them.
i) Recommendations for development
of HCSWs
The systematic review (CAHE 2006), referred to
throughout, conveniently summarises in the form of ten
recommendations a number of the ndings and themes
echoed in this current literature review:
1There is little doubt regarding the value of support
workers in healthcare. There is historical and growing
positive evidence for utilising support workers in
healthcare.
2Utilisation of support workers should be
underpinned by clear denition of their roles and
allocation of duties. Delegation of specic tasks to
support workers should be documented to avoid
confusion among other healthcare professionals.
3Support workers can be utilised in a mixture of both
direct and indirect roles. The process underpinning
the composites of direct and indirect roles of the
support worker will be inuenced by local factors.
4Service delivery models involving support workers
should be underpinned by supervision and specic
task delegation. Such a framework provides exibility
for local health services.
5Support workers need to be supervised, especially
during direct roles. As the literature does not shed
any light on the framework for supervision, this
provides the opportunity for local health services to
develop geographic specic supervision models for
support workers.
6It needs to be recognised health professionals who
are required to supervise also require training in
supervision and ongoing support. Expectation that
health professionals are aware of supervisory roles
and are competent in the provision of eective
supervision may lead to potential angst among
stakeholders.
7Clarications on accountability for support
workers interventions need to be established
and documented. As the literature is unclear on
the accountability of support workers and health
professionals are fearful of litigations it is imperative
such clarications are provided to all stakeholders
prior to health service provision.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 49
8Due to the nature of service delivery provided by
support workers, evaluation of outcomes specic to
the intervention provided by support workers will
be dicult. However, global measures of outcomes
from the perspective of all stakeholders are required.
This can be undertaken via multiple approaches
measuring both processes and outcome indicators at
regular intervals e.g. audit, surveys, interviews, focus
groups.
9Increasingly the historical perception of support
workers being “untrained” and “unqualied” is
becoming less prevalent. There is an expectation
that support workers are equipped with some core
competencies and depending upon the specialties
they work with, they should be equipped with
additional skills, knowledge and attitudes. The
training to secure these skills should be acquired in
the form of formal and informal training. Presence of
either of them in isolation is seen to be insucient.
While there are numerous avenues for training,
there are several barriers in accessing these training
opportunities. These barriers (such as cost of training,
lack of adequate resources to relieve support
workers to undertake training) need to be identied,
recognised and subsequently addressed for support
workers to access these training opportunities.
Additionally, an environment which supports
ongoing life long learning should also be created.
10Support workers need to be supported. Support
workers can be marginalised, mistreated and not
recognised as being integral to the team. Such
practices will lead to poor working environments
and potentially poor quality care. Support workers
need to be supported within and across the
organisation at all levels, provided with clear career
pathways and opportunities for promotions and be
consulted in decision making processes, if they are
equipped to do so.
ii) Areas for further research
The need to establish best practice in the introduction of
HCSWs roles is reected in the call for targeted research
in a number of specic areas (CAHE 2006, adapted for all
HCSWs from a review of rehabilitation support workers).
-Exploration of the growing place of HCSWs in
healthcare and especially in the community, due to
the gradual shifting of care from acute hospital setting
into community rehabilitation settings
-Identication of a uniform denition of support
workers in healthcare
-Provision of evidence of the roles and boundaries for
support workers in healthcare
-Tests of the short and long term eectiveness of
models of service delivery and outcomes of care
provided by support workers in healthcare
-A focus on uniform core competencies for HCSWs
in healthcare and the provision of a framework for
competencies for support workers who specialise in
working within specic disciplines
-Provision of evidence for innovative and eective
training models for support workers
-Specic focus on the barriers to uptake of training of
HCSWs
-Exploration of other healthcare sta’s perspective of
HCSWs, their role as supervisors and their perception
of delegating tasks to HCSWs
-Establish all stakeholders’ perspectives of support
worker involvement in healthcare and achieve a
consensus
Similarly Lizarondo et al. (2010) identify a range of
information gaps in relation to AHP support workers that
are worthy of investigation.
-How HCSWs are used to supplement, complement or
replace registered sta
-The optimal mix of HCSWs to registered sta
-The impact on outcomes of changing roles in patient
care
Finally the need to explore how registered nurses
currently delegate and supervise HCAs was highlighted
by Alcorn and Topping (2009).
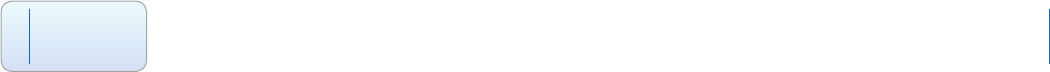
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 50
Appendix 1
Examples of professional organisations’ descriptions of HCSWs
British Dietetic Association
Dietetic Assistants work with registered dieticians
in either a community or hospital setting. A dietetic
assistant working in a hospital may, for example, be
involved in assisting patients requiring special diets to
choose from the hospital menu, collecting information
regarding patients’ intake and weight as and liaising
with the dietician regarding patients’ progress. Within
a community setting, dietetic assistants may work with
the dietician to assess the food and health needs of local
residents and assist in enabling people to eat a healthier
diet to prevent disease.
Chartered Society of Physiotherapy
The CSP refers to a support worker as one who is
“delivering or supporting the delivery of physiotherapy
under a registered physiotherapist or registered Allied
Health Professional (AHP). This includes rehabilitation
assistants, technical instructors, assistant practitioners,
generic assistants, and any of 300 dierent role titles”.
References
Adams G (2010) HCA regulation cannot be based on pay alone. Nursing Times 106(12), 30 March, 21.
Alcorn J, Topping AE (2009) Registered nurses’ attitudes towards the role of the healthcare assistant. Nursing Standard
23(42), 39-45.
Arblaster G, Streather C, Hughill L, McKenzie M, Missenden J (2004) A training programme for healthcare support workers.
Nursing Standard 18 (43) 33-37.
Baldwin J, Roberts JD, Fitzpatrick JI, While A & Cowan DT (2003) The role of the support worker in nursing homes: a
consideration of key issues. Journal of Nursing Management 11, 410–420.
Benson L, Smith L (2006) Delivering The Workforce. Evaluation Of The Introduction Of Assistant Practitioners In Seven Sites In
Greater Manchester Second Report May 2006. Centre for Public Policy and Management, University of Manchester.
Betts EA, Sorrell M, Faulkner T (2003) The Assistant Practitioner in the imaging department: A practical experience. Synergy
March, 15–17.
Birch A, Martin C (2009) Healthcare Support Workers in Scotland: Evaluation of a National Pilot of Standards and Listing in
Three NHS Boards. Scottish Government Social Research, Edinburgh
Blakemore S (2009) As healthcare assistants take on more responsibility, should they be regulated? Nursing Standard
23(44), 12-13.
Bosley S, Dale J (2008) Healthcare assistants in general practice: practical and conceptual issues of skill-mix change. British
Journal of General Practice 58, 118–124.
Acknowledgements
The literature review was conducted by Iain Colthart, Research and Information Ocer, NHS Education for Scotland

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 51
Centre for Allied Health Evidence (CAHE) (2006) Systematic Review Of The Literature On Utilisation of Support Workers In
Community Based Rehabilitation. University of South Australia, Adelaide.
Clover B (2010) Unison calls for formal HCA registration. Nursing Times 22 June.
College of Radiographers (CoR) (2007a). The Scope of Practice of Assistant Practitioners in Clinical Imaging. CoR, London.
College of Radiographers (CoR) (2007b). The Scope of Practice of Assistant Practitioners in Radiotherapy. CoR, London.
Colthart I, McBride M, Murray M. (2010a) Mentoring assistant practitioners - The radiographer’s perspective. Radiography
16(3), 223–229.
Colthart I, McBride M, Murray M. (2010b) On your wavelength; Radiography assistant practitioner training in Scotland.
British Journal of Healthcare Assistants 4(1), 1-5.
Cowie A (2002) Supporting the Development of Healthcare Support Workers In Scotland – Final Report. SEHD, Edinburgh.
Dean E (2009) Researchers caution against use of support workers in direct care. Nursing Standard 24 (12), November 25.
Department of Health (1999) Agenda for Change – Modernising the NHS Pay System. DH, London.
Department of Health (2003) Radiography Skills Mix – A report on the four-tier service delivery model. DH, London.
Dunlop GM (2004) Allied Healthcare Support Worker Role Development. Building for the Future. Report for Scottish Executive
Health Department. Queen Margaret University College, Edinburgh.
Ellis B, Connell NAD (2001) Factors determining the current use of physiotherapy assistants: Views on their future role in
the South and West UK Region. Physiotherapy 87(2), 73-82.
Farndon L, Nancarrow S (2003) Employment and career development opportunities for podiatrists and foot care assistants
in the NHS. British Journal of Podiatry 6(4), 103-108.
Field L, Smith B (2003) An essential care course for healthcare assistants. Nursing Standard 17(44), 16 July, 33-35.
Fitzpatrick JM, Roberts JD (2004) Challenges for care homes: education and training of healthcare assistants. British Journal
of Nursing 13(21), 1258-1261.
Forsyth L, Hunt K, McGowan D (2003) Assistant training – a local approach to a national initiative. Synergy December, 7-10.
Gainsbury S (2009) Risks and benets: changing the nursing skill mix. Nursing Times 22 September.
Galloway J, Smith B (2005) Meeting the education and training needs of rehabilitation support workers. International
Journal of Therapy and Rehabilitation 12(5), 195-199.
Gould D, Carr G, Kelly D, Brown P (2004) Healthcare assistants: the new registration route. Nursing Standard 18(33), 37-40.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 52
Griths and Robinson (2010) Moving forward with healthcare support workforce regulation. A scoping review: evidence,
questions, risks and options. National Nursing Research Unit, London.
Hancock H, Campbell S (2006) Developing the role of the healthcare assistant. Nursing Standard 20(49), 35-41.
Hancock H, Campbell S, Ramprogus V, Kilgour J (2005) Role development in healthcare assistants: the impact of education
on practice. Journal of Evaluation in Clinical Practice 11(5), 489-498.
Health Professions Wales (2004) Health Care Support Workers. All Wales Scoping Project Final Report.
http://www.wales.nhs.uk/sites3/Documents/484/HCSW%20All%20Wales%20Scoping%20Project%20-%20Final%20
Report%20Pages%201%20to%20155.pdf
Hibbert A (2006). The factors that aect HCA routes into nurse training. Nursing Times 102(1), 32-6.
Hodgson D, Graham L, Abraham M (2005) A work-based learning programme for Assistant Practitioners in radiotherapy.
Synergy September, 16–21.
Hopkin S (2008) Regulation: why it should be introduced. British Journal of Healthcare Assistants 2(4), 182-184.
Keeney S, Hasson F, McKenna HP (2005a) Healthcare assistants’ experiences and perceptions of participating in a training
course. Learning in Health and Social Care 4(2), 78–88.
Keeney S, Hasson F, McKenna H (2005b) Health care assistants: the views of managers of health care agencies on training
and employment. Journal of Nursing Management 13, 83–92.
Kessler I, Heron P, Dopson S, Magee H, Swain D (2010). Nature and Consequences of Support Workers in a Hospital Setting.
Final report. NIHR Service Delivery and Organisation programme.
http://www.sdo.nihr.ac.uk/projdetails.php?ref=08-1619-155
Kilgannon H (2007) Foundation Degrees: Developing the Workforce of the Future in the Health and Social Care Sector.
Foundation Degree Forward, NHS North West.
Le Cornu KA, Halliday D (2008) A study to investigate perceptions of the role of the dietetic support worker by dieticians
and dietetic support workers in the NHS. Journal of Human Nutrition and Diet 21, 373–406.
Leach C, Wilton E (2008) Evaluation of Assistant and Associate Practitioner Roles across NHS South Central, NESC Report
summary report. NHS South Central.
Leach C, Wilton E (2009) Evaluation of assistant and associate practitioner roles across NHS South Central. British Journal of
Healthcare Assistants 2(3) 97-99.
Lizarondo L, Kumar S, Hyde L, Skidmore D (2010). Allied Health Assistants and what they do: A systematic review of the
literature. Journal of Multidisciplinary Healthcare 3, 143-153.
Mackey H (2004) An extended role for support workers: the views of occupational therapists. International Journal of
Therapy and Rehabilitation 11(6), 259-66.
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 53
Mackinnon I. Kearney J (2009) Assistant Practitioners: scoping exercise. A report to Skills for Health. The Mackinnon
Partnership, London.
McCready T, Macdonald J (2002) Development of an accredited cancer care course for HCAs. Nursing Standard 16(16), 3
January, 41-42.
McGloin S, Knowles J (2005). An evaluation of the critical care assistant role within an acute NHS Trust Critical Care Unit.
Nursing in Critical Care 10(4), 210-215.
McGowan D, Campbell K (2010a) Enhancing Care: Developing the Assistant Practitioner Role. Cancer Nursing Practice 9(2),
16-20.
McGowan D, Campbell K (2010b) Training assistant practitioners to deliver clinical care in specialist services. Nursing Times
106(12), 18-20.
Muddiman B (2010) Supporting support workers. British Journal of Healthcare Assistants 4(6), 306-307.
Mullen C (2010) Core characteristics of the AP’s role—six years on. British Journal of Healthcare Assistants 4(6), 278–281.
Moseley LG, Davies M, Evans LE (2007) The training needs of health care support workers: results of a study of workers and
their managers. Journal of Clinical Nursing 16, 2280–2286.
Nancarrow S, Mackey H (2005) The introduction and evaluation of an occupational therapy assistant practitioner.
Australian Occupational Therapy Journal 52, 293–301.
Nancarrow SA, Shuttleworth P, Tongue A, Brown L (2005). Support workers in intermediate care. Health and Social Care in
the Community 13(4), 338–344.
National Nursing Research Unit (NNRU) (2009) Is there a case for the UK nursing workforce to include grades of qualied
nurse other than the registered nurse? Policy plus evidence, issues and opinions in healthcare. Issue 21, October.
NHS Education for Scotland (2004). Role development for radiographers, Assistant Practitioners and support workers: national
scoping report. NES, Edinburgh.
NHS Education for Scotland (2008). HNC Allied Health Professions: Speech and Language Therapy Support Validation Proposal
Document May 2008. NES, Edinburgh.
NHS Education for Scotland (2009) Evaluation of the Radiography Trainee Assistant Practitioner’s Programme. Higher National
Certicates in Diagnostic Imaging and Radiotherapy. Summary Report. NES, Edinburgh.
NHS Education for Scotland (2010) A Guide to Healthcare Support Worker Education and Role Development. NES, Edinburgh.
NHS Scotland (2009) National Primary Care, Workforce Planning Survey 2009. Results for Scotland. Published 15th
December.
O’Dowd A (2009). Regulation ahead. Nursing Times 105(15) 21 April Suppl., 12-13.
Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 54
Quality Improvement Scotland (2008) Working to Standard. Final Project Report – Pilot for the regulation of healthcare
support workers. QIS, Edinburgh.
RCN Policy Unit (2007). The Regulation of Healthcare Support Workers. Policy Brieng 11/2007. RCN, London.
RCN Policy Unit (2009). The Assistant Practitioner Role. A policy discussion paper. Policy Brieng 06/2009. RCN, London.
Santry C (2010) NMC ‘single minded’ about HCA regulation. Nursing Times, 19 January.
Scottish Credit and Qualication Framework (2009) The Scottish Credit and Qualication Framework, Glasgow
http://www.scqf.org.uk/TheFramework/The-Framework-Home.aspx
Scottish Executive Health Department (1999) Learning Together. SEHD, Edinburgh.
Scottish Executive Health Department (2001) Caring for Scotland: The Strategy for Nursing and Midwifery in Scotland. SEHD,
Edinburgh.
Scottish Executive Health Department (2004) The NHS Knowledge and Skills Framework (NHS KSF) and the development
review process. SEHD, Edinburgh.
Scottish Executive Health Department (2004) Consultation on the Regulation of Healthcare Support Sta and Social Care
Support Sta in Scotland. SEHD, Edinburgh.
Scottish Executive Health Department (2006) Delivering Care, Enabling Health. Harnessing the Nursing, Midwifery and Allied
Health Professions’ Contribution to Implementing Delivering for Health in Scotland. SEHD, Edinburgh.
Scottish Government (2009) A Force for Improvement: The Workforce Response to Better Health, Better Care. SG, Edinburgh
Scottish Government (2010) Healthcare Support Worker - Mandatory Induction Standards and Code of Conduct for Healthcare
Support Workers and Mandatory Code of Practice for Employers of Healthcare Support Workers CEL23 (15 June). SG, Edinburgh
Scottish Government Health Directorates (2007) Better Health, Better Care. Planning tomorrow’s workforce today. SGHD,
Edinburgh.
Selfe J, Roddam H, Cording H, Temple B Green L, Chambers A. (2008). Assistant Practitioner Foundation degree Evaluation
Project Final Report – June 2008. University of Central Lancashire (UCLAN).
Shaw A (2005) Assistant Practitioners: Their education and training. Synergy. July, 26-27.
Skills for Health (2005) The career framework for health.
http://www.skillsforhealth.org.uk/developing-your-organisations-talent/career-frameworks.aspx
Skills for Health (2008) Career Framework Descriptors. SfH, Bristol.
Skills for Health (2009) National Occupational Standards (NOS) Nationally Transferable Roles Template Assistant Practitioner.
SfH, Bristol.

Healthcare Support Workers
The Development of the Clinical Healthcare Support Worker Role: A Review of the Evidence
Back to
Contents 55
Spilsbury K, Atkin K (2009). The impact of assistant practitioners on acute NHS trusts. British Journal of Healthcare Assistants
3(10), 508-509.
Spilsbury K, Meyer J (2004) Use, misuse and non-use of health care assistants: understanding the work of health care
assistants in a hospital setting. Journal of Nursing Management 12, 411–418.
Spilsbury K, Stuttard L, Adamson J, Atkin K, Borglin G, McCaughan D, McKenna H, Wakeeld A & Carr-Hill R (2009). Mapping
the introduction of Assistant Practitioner roles in Acute NHS (Hospital) Trusts in England. Journal of Nursing Management
17, 615–626.
Sprinks J (2009) RCN urges compulsory training for every healthcare support worker. Nursing Standard 24(14), December 9,
12-13.
Torjesen I (2009) All in the mind. Nursing Times 105 (15), 21 April Supplement, 10-11.
Thornley C (2000). A question of competence? Re-evaluating the roles of the nursing auxiliary and health care assistant in
the NHS. Journal of Clinical Nursing 9(3),451–458.
Wakeeld A, Spilsbury K, Atkin K, McKenna H (2010) What work do assistant practitioners do and where do they t in the
nursing workforce? Nursing Times 106(12), 14-17.
Wakeeld A, Spilsbury K, Atkin K, McKenna H, Borglin G, Stuttard L (2009) Assistant or substitute: Exploring the t between
national policy vision and local practice realities of assistant practitioner job descriptions. Health Policy 90, 286–295.
Whyke M (2003) Assistant radiography practitioners evaluation report. University of Leeds.
Winnard Y, Kittle S (2008) Assistant practitioners in radiography. British Journal of Healthcare Assistants 2(1), 42–44.
Youg L (2008) Regulation: why it should not be introduced. British Journal of Healthcare Assistants 2(5), 243-244.
© NHS Education for Scotland 2010. You can copy or reproduce the information in this document for use within
NHSScotland and for non-commercial educational purposes. Use of this document for commercial purposes is permitted
only with the written permission of NES.