National Vision And Hearing Screening Protocols C 542 Nov09
User Manual: C 542
Open the PDF directly: View PDF ![]() .
.
Page Count: 35
- Contents
- Introduction
- Programme Summary
- Hearing Screening
- Screening Technique – Screening Audiometry
- Screening Technique: Threshold Audiometry
- Screening Technique: Tympanometry
- Vision Screening
- Screening Technique: Parr Letter-Matching Charts or Sheridan Gardner Charts
- Screening Technique: Snellen Vision Chart
- Colour Vision: Ishihara Pseudoisochromatic Plate
National Vision and Hearing
Screening Protocols

Ministry of Health. 2009. National Vision and Hearing Screening Protocols.
Wellington: Ministry of Health.
Published in November 2009 by the
Ministry of Health
PO Box 5013, Wellington, New Zealand
ISBN 978-0-478-33938-3 (online)
HP 4969
This document is available on the Ministry of Health’s website:
http://www.moh.govt.nz

Contents
Introduction 1
Programme Summary 2
The programme 2
Cohort groups 2
Test environments/locations 3
Competencies 3
Test equipment 3
Quality requirements 4
Hearing Screening 5
Who to screen and which screening methods to use 5
Consent 6
Setting for hearing screening 6
Equipment needed for hearing screening 7
Hygiene protocols for hearing screening 8
After the screening test 9
Funding for services 9
Screening Technique – Screening Audiometry 10
Referral pathways 11
Screening Technique: Threshold Audiometry 13
Referral pathways 14
Screening Technique: Tympanometry 15
Referral pathways 16
Vision Screening 18
Who to screen and which screening methods to use 18
Consent 19
Setting for vision screening 19
Equipment needed for vision screening 20
After the screening 21
Subsidies for glasses/spectacles and eye exams 22
Screening Technique: Parr Letter-Matching Charts or Sheridan
Gardner Charts 23
Referral pathways 24
Screening Technique: Snellen Vision Chart 26
Referral pathways 26
Colour Vision: Ishihara Pseudoisochromatic Plate 30
National Vision and Hearing Screening Protocols iii

List of Tables
Table 1: Risk factors for hearing related developmental/learning difficulties 12
List of Figures
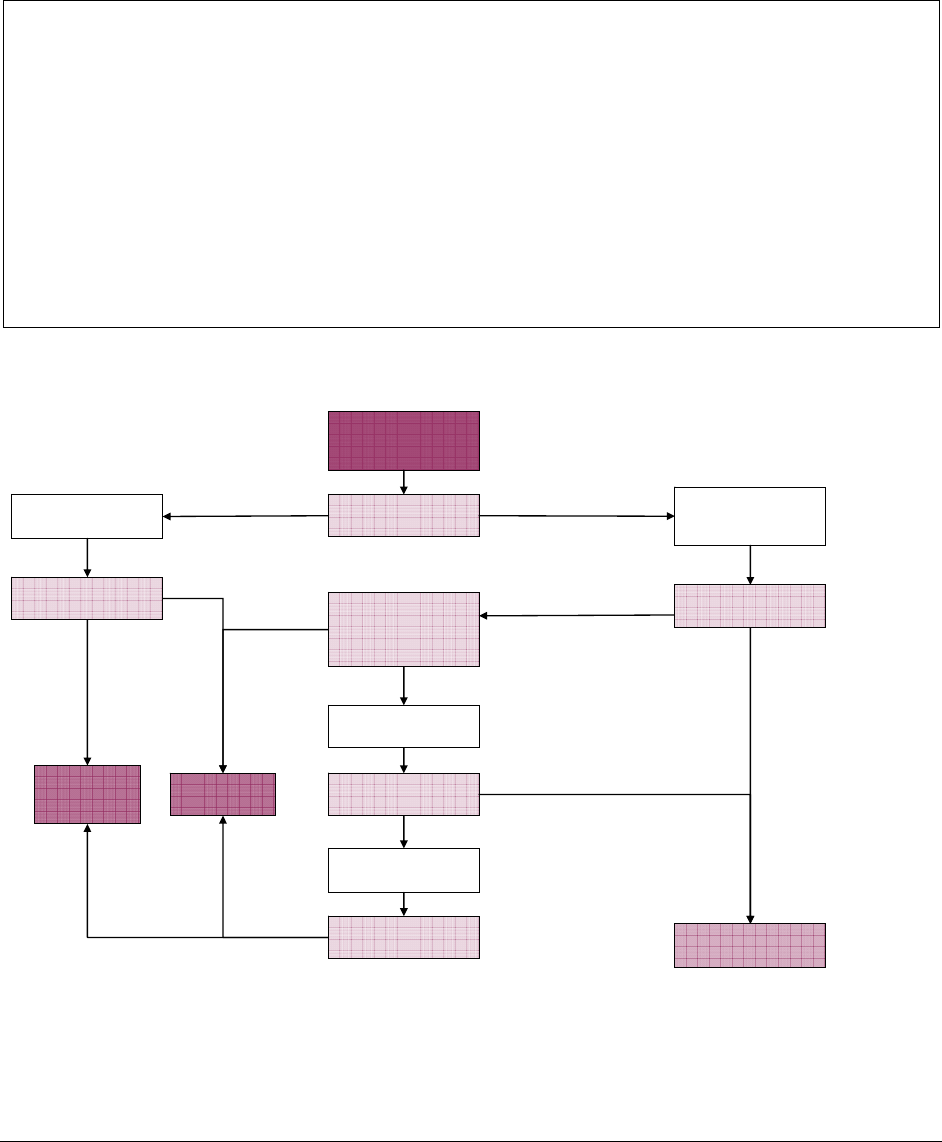
Figure 1: Screening audiometry clinical pathway and referral criteria 12
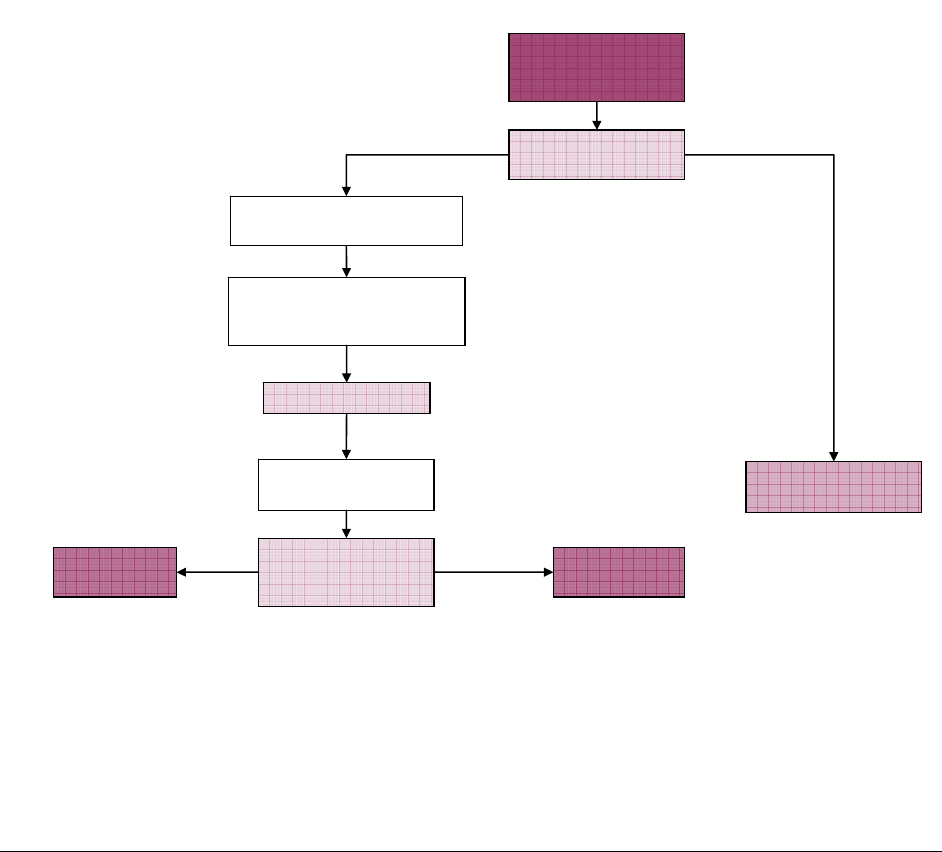
Figure 2: Threshold audiometry clinical pathway and referral criteria 14
Figure 3: Vision screening clinical pathway and referral at four years old 25
Figure 4: Vision screening clinical pathway and referral at five years and older 29
iv National Vision and Hearing Screening Protocols

National Vision and Hearing Screening Protocols 1
Introduction
The National Vision and Hearing Screening Protocols (National Protocols) describe the
best practice requirements for Vision Hearing Technicians (VHTs) who are delivering
the National Vision and Hearing Screening Programme.
The National Protocols provide an outline of the screening process, but are not a
training manual. Personnel delivering this screening programme need to have attained
or be working towards the NZQA National Certificate in Community Support Services
(Vision and Hearing Screening) (Level 3) and comply with national competencies (refer
to page 3).
This document should be read in conjunction with the appropriate National Service
Specifications, which the Ministry of Health uses to purchase Vision Hearing Screening
services from District Health Boards.
This document is in two sections:
Hearing screening protocols (pages 5–17)
Vision screening protocols (pages 18–35)
If you have any questions or queries about the National Vision and Hearing Screening
Programme or this document, please contact the Well Child team at the Ministry of
Health (well_child@moh.govt.nz).

Programme Summary
The programme
Mass screening of a defined cohort of children (4 and 11 years old) to identify
prevalent, undetected hearing problems and some undetected vision problems
requiring further assessment and/or treatment.
Targeted and follow up screening of groups at high risk and/or who have missed
earlier screening events.
Screening carried out by qualified personnel using appropriate equipment/tools in
specified environments.
Referrals to appropriate agencies using identified pass/fail criteria for screening.
Documentation of results and reporting of statistical information.
Cohort groups
3 years
At individual DHB’s discretion, targeted tympanometry screening of groups at high-
risk of harm from glue ear.
4 years (B4 School Check)
Distance visual acuity screening used to detect children likely to have amblyopia.
Screening audiometry (and tympanometry if required).
New entrants and Year 1 children (5- and 6-year-olds)
Catch up screening for children who have not had B4 School Check screening as
above, or need follow up tests from B4 School Check.
Year 7 (11-year-olds)
Distance visual acuity screening to detect children with myopia or other conditions
causing reduced acuity.
Ishihara colour vision screening for boys.
Children in special circumstances and migrant children
Screening audiometry/threshold audiometry depending on the age/ability of the child.
Distance visual acuity screening to identify children with possible amblyopia
depending on the age/ability of the child.
2 National Vision and Hearing Screening Protocols

Test environments/locations
Registered pre-school/early childhood education centres and kohanga reo.
Community venues including churches, marae and community halls.
State/private primary schools.
State/private intermediate schools.
Defined clinic settings.
All environments are to comply with National Protocol requirements for light and
sound levels or the VHT must make arrangements to use the environments at times
when compliance is achievable.
Competencies
Personnel who provide vision and hearing screening services must have attained or be
working towards the National Certificate in Community Support Services (Vision and
Hearing Screening) (Level 3) and:
be employed for a minimum of 16 hours per week for vision and hearing screening
work
receive ongoing professional development relevant to the screening processes
specified in the National Protocols and attend the annual Training Seminar (at least
biennially)
have a biennial review/assessment of their competence
have completed training in the Ministry of Education’s ENROL database and the
Ministry of Health’s B4 School Check database.
Where personnel provide either vision screening or hearing screening alone, they still
must meet the above employment/experience/review/training requirements.
Registered nurses and other health professionals carrying out vision and hearing
screening do not need to be dedicated to vision and hearing screening for 16 hours per
week but must meet all other competency requirements.
Test equipment
Calibrated (annually) screening audiometer (0.5 kHz to 6 kHz @ 0–100 dB
presentation range) fitted with noise-attenuating audiocups.
Calibrated (annually) screening tympanometer (+200–-400 daPa range).
Parr letter-matching chart (with and without confusion bars) or an equivalent
Sheridan Gardner chart.
Snellen-ratio letter chart.
Ishihara pseudoisochromatic plates for colour deficiency (24-plate edition).
Black eye patch (tie-on or elasticised).
Hand-held eye occluder (Denver model or similar).
National Vision and Hearing Screening Protocols 3

Sound level meter.
Light level meter (illuminance meter, lux meter).
Alcohol wipes, handrub and Milton solution.
Quality requirements
Standard consent process prior to screening.
Standard format for feedback of screening results to parent/caregiver of each child
post-screening.
Standard format of recording results onto the relevant national database to enable
national reporting.
Ministry of Health requirements as specified in the relevant National Service
Specification and the National Protocols.
4 National Vision and Hearing Screening Protocols

Hearing Screening
The hearing screen of four year olds is part of an overall framework of hearing
screening and Well Child/Tamariki Ora hearing surveillance. This screen follows
Universal Newborn Hearing Screening (UNBHS) shortly after birth and the intervening
Well Child/Tamariki Ora checks.
The screening protocol is designed to identify hearing loss that is likely to interfere with
normal speech, language development and learning, and to find children with persistent
middle ear disorder that also causes a significant hearing loss. This screen is also
designed to target, detect and refer children where there are hearing-related
developmental/learning difficulties (referred to as risk factors), so that appropriate
intervention can be provided prior to or early in a child’s primary education.
If the child’s hearing loss has already been confirmed as part of UNBHS or other Well
Child/Tamariki Ora surveillance and the child is already under the care of an
audiologist/wearing hearing aids, etc, it is not necessary to carry out screening
audiometry.
Who to screen and which screening methods to use
Pre-school children (4-year-olds) B4 School Check
Pre-school screening is carried out in early childhood education centres or clinic
settings. Screening audiometry and tympanometry (if required) are the screening tests
to be administered. The results and outcomes (ie, pass, refer or re-screen) from this
screen must be recorded in the B4 School Check database. If it becomes possible, the
results will be transferred into the Ministry of Education’s ENROL database.
New Entrants and Year 1 children (5- and 6-year-olds)
This screening is to capture the cohort of children who have not been screened as
preschoolers or who need a follow-up test as a result of earlier screening. The same
screening methods should be used as described above.
Older school-aged children on request and children new to New Zealand
In situations where there is concern about hearing from parents, teachers, and others in
an older primary school aged child, a threshold audiometric test may be requested.
Children that are new to the country also require screening unless there is already a
documented hearing loss and the child is receiving care. In these situations the screen
should be a full audiogram from 500 Hz to 6000 Hz. People requesting a screen should
be informed that screening is not a full diagnostic hearing assessment, and a child
should be referred to their GP/ear nurse/audiologist if there are any concerns. The
results and outcomes (ie, pass, refer or re-screen) from this screen must be recorded in
the ENROL database.
National Vision and Hearing Screening Protocols 5

Consent
Although VHTs are still covered by Section 125 of the Health Act (1956), most regions
have now implemented a consent process to encourage parents to make informed
choices about their child’s health. In addition, the recording of results in the national B4
School Check database requires the informed consent of parents. Therefore, all
services delivering vision and hearing screening should implement an opt-off consent
process. Section 125 should only be used in exceptional circumstances where the
school or health services have concerns for a child’s welfare.
The consent process should include information for parents about what their child is
being screened for and questions about whether the child is already under the care of
an audiologist or ear, nose and throat specialist and/or has grommets or a hearing aid.
Setting for hearing screening
It is important that the VHT obtains a suitable room for hearing screening. Inappropriate
conditions may compromise the validity of screening. A range of setting may be used
for hearing screening, according to local availability. The conditions discussed below
apply to community settings, as well as clinic settings.
Type of room
The room in which the hearing screening takes place must:
be quiet and free of distractions
have soft furnishings and floor coverings to absorb noise.
In a school or preschool, the most suitable room is usually the school library or an
office.
Minimise ambient noise
The degree of ambient noise in the room in which the hearing screening will take place
must be less than 50 dB. Check the ambient noise with a sound level meter at the
beginning of the screening session and at any other time you consider it necessary.
Alternatively the screener (who must have normal hearing) can check that they are able
to hear the test tones at 10 dB.
If the noise level exceeds 50 dB, speak to the staff and ask for noise levels to be
reduced. Use a standalone sound-absorbing screen and approved noise attenuating
headset cups in noisier environments to achieve the required noise attenuation. If
appropriate background levels cannot be obtained do not continue with the testing as
the results are likely to be invalid.
6 National Vision and Hearing Screening Protocols

Venue organisation
Prior to visiting an early childhood centre or school you should:
notify the venue of your intended visit and asked to plan quiet activities for when
hearing screening is being carried out
obtain the list of children requiring screening, eg, ENROL, preschool attendance lists
ensure the consent process with parents has been completed.
Frequency of visits
Venues should be visited at least three times each year to ensure that all children are
screened and re-screens can be done in a timely fashion. This may not always be
possible in very small remote rural areas. In these cases, serial testing could be carried
out in a scheduled clinic setting.
Service promotion
Wherever possible, VHTs should take the opportunity to promote understanding of the
screening programme. It is important that parents and teachers appreciate the
limitations of screening services. Speaking to school staff during morning tea/lunch
breaks or at staff meetings is recommended. Information pamphlets or posters in the
school are also encouraged.
Information for educators to help them understand vision and hearing screening is
currently being developed. VHTs will be notified when this information is available for
use. This information will be available online at the Ministry of Health website, and
VHTs can print copies for distribution to preschool and school teachers, principals and
other educators.
Equipment needed for hearing screening
To screen a child’s hearing you need:
an audiometer, tympanometer and ancillary equipment
an appropriate chair and a table or desk on which to set up the audiometer and
paperwork
a set of record sheets
a sound level meter
headphones
pegs and a container
a chair for the child being screened.
Audiometers and tympanometers need to be calibrated regularly. A basic calibration
shall be performed at least yearly by an independently audited laboratory with full
traceability to National Standards (IANZ). Headphones are calibrated to a particular
audiometer and so are not interchangeable.
National Vision and Hearing Screening Protocols 7

Hygiene protocols for hearing screening
Audiometry
Hearing screen involving the placement of ear phones onto a child’s ears. (NOTE:
Audiometry should not be performed on children with discharging ears, or where the ear
or surrounding skin is inflamed or broken.) These children need referral to the GP or
ear nurse.
Procedures
Back at base – Check earphones regularly. If cleaning is required, carefully remove
rubber cushions from earphones and wipe with warm soapy water. Ensure cushions
are totally dry before replacing. (NOTE: If earphone cushions become cracked or
porous they must be replaced to maintain hygiene).
Tympanometry
Middle-ear screens involving the placement of rubber tip at the opening of ear canal.
(NOTE: Tympanometry is not performed on children with discharging ears, or where the
skin is broken or inflamed).
Procedures
During screening – Change to a clean, unused rubber tip between each child screened.
Back at base – Ensure all used tips are wiped clean and any debris (eg, ear wax)
removed, then place in the dish of Milton solution. The tips should be totally submerged
in the solution so that all surfaces are covered. After soaking period, (manufacturer’s
recommendation) the tips should be left to drain onto clean absorbent tissue. When
dry, they should be stored in their covered containers.
Personnel
Where VHTs have cuts or abrasions of the skin that may be susceptible to infection (ie,
to the hands) it is advisable to wear disposable plastic gloves. Regular hand washing
during screening is recommended. Where there is no access to a hand-basin, a topical
antibacterial solution handrub or similar is suitable.
Suggested cleaning products
Milton solution tablets are acceptable for cleaning tympanometer tips (or similar
antiseptic solution). The solution must be mixed according to the manufacturer’s
recommendations. The solution must be changed daily.
Alcohol swabs: 2 ply – medium grade (saturated with 70% isopropyl alcohol) in sterile
individual packages.
Handrub: Microshield handrub (containing chlorhexidine gluconate 0.5% w/v in 70% v/v
ethanol) or similar.
8 National Vision and Hearing Screening Protocols

After the screening test
Notification to parents
Parents should be notified after every screen by using the nationally consistent parent
feedback form.
Pass and refer brochures for hearing screening are currently being developed. These
will be distributed to VHTs for use with all four and five year olds screened.
Follow up
Local records must be kept of all children who have been screened including:
those who have passed
those requiring a re-screen
those who have been referred.
Parents/GPs/audiologists/ear nurses are asked to inform the referrer of their findings
and proposed treatments. This information is recorded for future reference.
If no feedback information has been received from the referral, a follow-up letter or
phone call to the family may be required to see if any action has been taken. If this is
unsuccessful then the case should be referred to the Public Health Nurse Services or
Community Health Team to initiate a home visit. This information must be recorded for
future reference.
Where a child has already been assessed and determined as needing hearing aids or
another assistive device (eg, hearing aids, cochlear implants, FM systems) but is not
wearing them, or where a child failed to attend a Hospital audiology clinic appointment,
the school’s nurse/public health nurse should be informed. No further screening is
warranted.
Preschool and school recording systems
There are two national databases for recording hearing results:
Ministry of Education’s ENROL database
Ministry of Health’s B4 School Check National Information System.
The entry of hearing screening results is required to meet the national reporting
requirements for hearing screening, including the B4 School Check. The default system
for entering the hearing screening results is the B4 School Check database. Transfer of
results to the ENROL system will be done centrally.
Funding for services
Parents of children under 18 who are eligible for health services with hearing problems
are not asked to pay for audiological services, habilitation services or assistive devices.
These costs are funded by the Ministry of Health and the Ministry of Education.
National Vision and Hearing Screening Protocols 9

Screening Technique – Screening Audiometry
The procedure for screening audiometry is based on the American Speech-Language-
Hearing Association screening guidelines (ASHA 1997). The technique relies on a
conditioned response to sound. The screen is difficult for children under three years of
age. The success of the screen will depend upon achieving the conditioned response
and this is described below.
The screen consists of presenting a tone at 40 dB at 1000 Hz initially, then reducing the
level decibel level and screening across a range of frequencies.
Preparing the child for screening audiometry
Bring the child close to the audiometer (child must be no more than 30 cm from the
headphones) and explain to the child that you will be playing a simple game. Tell the
child that you will be making some sounds or beeps with the machine.
Leave the headphones on the desk with earphones facing toward child. Demonstrate
with a 1000 Hz tone at 100 dB. Continue to explain to the child that to play the game
the child must drop a peg into the container each time there is a beep. Demonstrate by
dropping a peg into the container at the sound of a tone.
Present another 1000 Hz tone and drop another peg into the container, repeat this
several times waiting between each beep so that the child understands that they must
wait for the sound. Get the child to demonstrate dropping the peg at the sound of the
tone. Ensure the child repeats this several times to show they thoroughly understand
the task.
If the child is unable to sit still and participate, then they are not ready to be screened
and will need to be put on a re-screen schedule. If there is concern, they should be
referred to an audiologist for other screening techniques that are more appropriate for
the child’s developmental age.
Procedure for screening audiometry
IMPORTANT! Reduce the intensity level of the tone from 100 dB to 40 dB; the starting
level for screening is 40 dB. Failure to reduce the sound level may cause pain or
discomfort to the child.
Place the headphones on the child and present a 1000Hz tone at 40 dB in the right ear.
If the child responds decrease the level to 20 dB and test at 1000, 2000 and 4000 Hz.
Then adjust the audiometer to 30 dB and administer the 500 Hz tone. If the child
responds to all these tones, then test the left ear in the same way starting with the
500 Hz tone at 30 dB. Then reduce the intensity to 20 dB and continue with the left ear
at 20 dB at 1000, 2000 and 4000 Hz. If the child hears all frequencies the result is a
pass. Record the results and no further action is required.
10 National Vision and Hearing Screening Protocols

If the child does not respond at 40 dB in the right ear initially, change to the left ear and
test at 40 dB, if the child does not pass carry out tympanometry. This result is an
immediate refer.
If the child responds at 40 dB in either ear and then does not respond at 20 dB at any
frequency carry out tympanometry.
Referral pathways
Formal hearing screening as part of the New Zealand Well Child/Tamariki Ora schedule
is undertaken at four years of age as part of the B4 School Check. This screen has
three possible outcomes; a pass, re-screen or referral (a failure to meet the
performance level considered acceptable on the occasion of the screening).
Re-screens should be notified to the preschool and the parents and done as scheduled.
Pass, refer and re-screen criteria for screening audiometry
If audiometry screening levels of 30 dB at 500 Hz and 20 dB at 1000, 2000 and 4000 Hz
are obtained in both ears, record the child’s hearing test as a pass. No further action is
required.
Audiometry screening levels between 20 and 40 dB (initial screen)
If the child is unable to hear the tone presented at 20 dB in either ear at 1000, 2000 or
4000 Hz, or 30 dB at 500 Hz, they should be offered a re-screen three months later
unless there are concerns about speech/language, development or behaviour. Children
who fail the initial screen with whom there are concerns about speech/language,
development or behaviour should be referred to an audiologist.
If a child is re-screened:
– consider re-screening in a quieter location if there are concerns about ambient
noise in the initial test environment
– if the child is unable to hear the tone presented at 20 dB in either ear at 1000,
2000 or 4000 Hz, or 30 dB at 500 Hz, a tympanogram should be done
refer to audiology if the tympanogram is normal
refer to GP or ear nurse if the tympanometry is abnormal
– where a referral is made to a GP or ear nurse the child’s hearing must be
screened again to rule out an underlying sensorineural hearing loss.
Audiometry screening levels above 40 dB at any test frequency
If the child is unable to hear the tone presented at 40 dB in either ear, record the result
as refer and undertake tympanometry. If they pass tympanometry refer to an
audiologist if they fail tympanometry refer to a GP or ear nurse. Where a referral is
made to a GP or ear nurse the child’s hearing must be tested again to rule out an
underlying sensorineural hearing loss.
National Vision and Hearing Screening Protocols 11
Child unable to participate
If the child makes inconsistent responses, suggesting that the child cannot perform the
conditioned response and the child has no risk factors for developmental and language
delay (see Table 1), re-screen the child in three months’ time.
Recording of results for B4 School Check screening audiometry
The results and outcomes (ie, pass, refer or re-screen) for screening audiometry
screening must be recorded in the B4 School Check database.
Table 1: Risk factors for hearing related developmental/learning difficulties
Permanent hearing loss independent of otitis media with effusion. Provided these children have
already been identified and are being cared for they should not be part of the screening programme
but should be entered in the statistics.
Suspected or diagnosed speech and language delay.
Autism spectrum disorder or other pervasive developmental disorders.
Syndromes (eg, Down Syndrome) or craniofacial disorders that include cognitive, speech and
language delays.
Blindness or uncorrectable visual impairment.
Cleft palate with or without an associated syndrome.
Developmental delay.
Significant socioeconomic disadvantage.
Figure 1: Screening audiometry clinical pathway and referral criteria
Administer test
tones of 40dB at
1000 Hz
Do they pass
bilaterally?
Administer screening
audiometry at 4
frequencies
Do they pass
bilaterally?
Tympanometry
Do they pass
bilaterally? Are there concerns
for speech, language,
development or
behaviour?
Retest audiometry in
3 months
Do they pass
bilaterally?
Referral to
Audiology
Referral to
GP/ear
nurse
*
NFA
No
No
No
Equivocal or
no response
No
Yes
Yes
Yes
Yes
Yes
Tympanometry
Do they pass
bilaterally?
YesNo
* Where a referral is made to a GP or ear nurse the child's hearing must be screened again to rule out
an underlying sensorineural hearing loss.
12 National Vision and Hearing Screening Protocols

Screening Technique: Threshold Audiometry
A child’s parent/caregiver or teacher may occasionally have concerns about a child’s
health, development, behaviour or learning and wonder whether a hearing problem is
causing these symptoms or difficulties. Sometimes an older child will complain of
hearing difficulties or hearing-related symptoms such as tinnitus or balance problems.
Threshold audiometry can be undertaken when an older child (five years or above) is
referred with concerns about a possible hearing loss. This procedure is not a screening
test, as it identifies a child’s actual hearing thresholds. For that reason it should be
undertaken in a quiet clinic environment, preferably in a sound-proofed room. Children
under five years are likely to find threshold audiograms difficult, and few children under
four years of age will be able to complete them satisfactorily. As a rule children under
four years of age with suspected hearing difficulties should be referred to an audiologist
for audiometry.
Procedure for threshold audiometry
The screen has two steps. The first step is to get the child familiar with the screening
tone and once that is completed, the VHT should undertake the threshold
measurement.
Familiarisation is undertaken to make sure that the child is able to reliably perform the
response task. The child must be presented with a loud enough signal to evoke a clear
response.
The method used for familiarisation by VHTs is as follows:
Present a 1000-Hz tone at a 50 dB hearing level (HL). If a clear response occurs,
move to threshold measurement. If no response occurs, increase the intensity by
increments of 10 dB until a clear response is obtained.
Threshold determination
The threshold of hearing is defined as the lowest decibel hearing level at which
responses reliably occur.
The tones to be used are 1–2 second duration pure-tone stimuli at 500, 1000, 2000,
4000 and 6000 Hz.
1. Start at 50 dB (or the child’s response level if higher) and reduce intensity in 5-dB
steps until the child fails to respond.
2. After a clear threshold is identified, move to the next frequency.
3. Enter results onto ENROL system.
National Vision and Hearing Screening Protocols 13
Referral pathways
Following a parent, child or teacher initiated self-referral, the health practitioner
consulted must work within their scope of practice to ensure that the family receives a
timely high quality service.
The VHT should screen hearing and middle ear pressures in the appropriate manner
and setting for the child’s age and development and refer to a GP or audiology clinic
with the results of the threshold audiogram, tympanometry (if required) and any
relevant observations of the child.
A nurse (including an ear nurse) or GP should obtain a history, and undertake and
record audiometry and tympanometry if the equipment is available, and the
practitioner is experienced. They should undertake a clinical examination of the
external ear, ear canal and tympanic membrane and other appropriate examination
of the child, and make a referral or institute management if required.
An audiologist should obtain a history, examine the external ear, ear canal and
tympanic membrane, undertake and record an audiogram, including air and bone
conduction, measure immittance and middle ear pressures, and conduct all other
assessments necessary to determine a diagnosis. The audiologist should make a
referral or institute management if required and appropriate.
Figure 2: Threshold audiometry clinical pathway and referral criteria
Administer test
tones at 500 - 6000
Hz at 20 dB
Referral to
Audiology
NFA
Offer test tone at 50dB at
each frequency
*
Reduce amplitude by 5 dB at
each frequency until child
unable to hear tone
No
Do they pass
bilaterally?
No Yes
Tympanometry
Do they pass
tympanometry
bilaterally?
Yes Referral to
GP/ear nurse
**
Plot audiogram
* If no response occurs, increase the intensity by increments of 10 dB until a clear response is obtained.
** Where a referral is made to a GP or ear nurse, the child’s hearing must be screened again to rule out
an underlying sensorineural hearing loss.
14 National Vision and Hearing Screening Protocols

Screening Technique: Tympanometry
Tympanometry is not required for children with grommets
Children with patent grommets are likely to have an abnormal tympanogram. Before
the tympanometry screen, parents should be asked as part of the consent process
whether the child has grommets. If the child has grommets, no further action is
required.
Settings for tympanometry
Tympanometry screening will be carried out in the same setting as screening
audiometry and therefore must:
be quiet and free of distractions
have soft furnishings and floor coverings to absorb noise.
Equipment
A table is required to set up the equipment and paperwork, and appropriate lighting to
read results on the screen. An appropriately sized chair is also essential for health and
safety requirements.
Preparing the child for tympanometry
Follow these steps to prepare the child for the tympanometry screen.
1. Stand the child in front of you, and explain that you will be using your ‘special
camera’ to take a measurement/picture of their ears.
2. Show the child the tympanometer screen to reassure them, liken it to a small TV.
3. Tell the child they will need to stand still for just a minute while you take the
picture.
4. When you feel the child understands and is ready, begin the procedure.
Procedure for tympanometry
Follow these steps to undertake the tympanometry screen.
1. Turn the child so that their right ear is facing you.
2. Place the tympanometer probe in the child’s ear and run a screen.
If the screen result is pass, record the result. Go to step 4.
If the screen is abnormal, go to step 3.
3. Repeat the test.
If the result is a pass, record the result. Go to step 4.
If the result is abnormal, record the result including the physical volume
measure. Go to step 4.
4. Turn the child so their left ear is facing you.
National Vision and Hearing Screening Protocols 15

5. Place the tympanometer probe in the child’s ear and run a screen.
If the screen result is a pass, record the result. End of procedure.
If the screen is abnormal, go to step 6.
6. Repeat the screen.
If the result is pass, record the result. This is the end of the procedure.
If the result is abnormal, record the result including the physical volume
measure. This is the end of the procedure.
Referral pathways
Pass, refer and re-screen criteria for tympanometry screening
Children who are having tympanometry must have first had audiometry screening.
Normal audiometry (ie, bilateral pass responses) means no further screening needs to
be done. The procedures below all follow an abnormal screening test.
Tympanogram is normal
If screening test is abnormal and the tympanogram is normal, the child may have a
sensorineural hearing loss. In this situation refer the child to audiology for further
assessment.
Tympanogram result cannot be obtained
If you are unable to gain a seal (ie, there is an air leak) when trying to run a
tympanogram:
record unable on the child’s notes
contact the child’s parents to see whether the child has grommets
if the child does not have grommets, refer the child to a GP or ear nurse for further
assessment (note as a refer).
Tympanogram is abnormal
If the tympanogram shows no peak and the physical volume measure is under 0.3 ml
or over 1.5 ml, refer the child immediately to a GP/ear nurse.
If the tympanometry result shows no peak (ie, it is a flat graph), and the physical
volume measure is 0.3–1.5 ml, re-screen the child in three months’ time.
If a re-screen tympanometry result shows no peak, refer the child to a GP/ear nurse.
Children with the conditions listed in Table 1 above are at high risk for developmental
and learning difficulties, which otitis media with effusion is likely to exacerbate. If
they fail their audiogram and have an abnormal tympanogram in either ear or both
ears refer them straight away.
Always ensure after referrals for failed tympanometry that a repeat hearing screen
has been carried out, either by the screening programme or an audiologist to rule out
underlying sensorineural hearing loss.
16 National Vision and Hearing Screening Protocols

Recording of results for B4 School Check tympanometry screening
The results and outcomes (ie, pass, refer or re-screen) for tympanometry screening
must be recorded in the B4 School Check database.
National Vision and Hearing Screening Protocols 17

Vision Screening
The prevalence of visual deficits in the preschool population is estimated to be 10–15
percent (Feightner 1998). Treatment for amblyopia, the focus of the vision screening, is
most beneficial if started before the child starts school. Amblyopia can lead to
permanent vision loss in one eye if not treated early.
Who to screen and which screening methods to use
If you, a teacher or a parent/caregiver has concerns about a child’s vision or eyes,
initiate a full assessment with a ophthalmic professional.
If the child is currently under the care of an ophthalmic practitioner, a screening test is
unnecessary, whether the child wears glasses or not.
Preschool children/B4 School Check (4-year-olds)
Preschool vision screening is carried out in early childhood education centres/clinic
settings. The four metre Parr letter matching charts (WITH confusion bars) or the
equivalent four metre Sheridan Gardner letter matching charts are the screening tests
which are to be administered. The results and outcomes (ie, pass, refer or re-screen)
from this screen must be recorded in the B4 School Check database. Plans are in
place for this information to be transferred to the ENROL database for access by
educators.
Vision screening of new entrants/Year 1 children (5- and 6-year-olds)
Vision screening at this age is to capture the cohort of children who have not been
screened as preschoolers or who need a follow up screen as a result of earlier
screening. Again, the four metre Parr letter matching charts (WITH confusion bars) or
the equivalent Sheridan Gardner charts are to be used.
Year 7 children (11-year-olds)
Year 7 vision screens are carried out within the child’s first year of intermediate
schooling. The Snellen-ratio vision chart is to be used. Boys in this age group are also
examined for colour vision defects using Ishihara pseudoisochromatic plates. The
results and outcomes (ie, pass, refer or re-screen) from these screens must be
recorded in the ENROL database.
Older school-aged children on request and children new to New Zealand
In special circumstances, parents, teachers, and others may request a vision screening
for a particular child. Children new to the country also require screening. The type of
screen administered depends on the child’s age and ability – using the above screen
recommendations as a guide. People requesting a screen should be informed that
vision screening is not a full assessment, and a child should be referred to a vision
professional if there are any concerns. The results and outcomes (ie, pass, refer or
re-screen) from any additional screenings must be recorded in the ENROL database.
18 National Vision and Hearing Screening Protocols

Consent
Although VHTs are still covered by Section 125 of the Health Act (1956), most regions
have now implemented a consent process to encourage parents to make informed
choices about their child’s health. In addition, the recording of results in the national
B4 School Check database requires the informed consent of parents. Therefore, all
services delivering vision and hearing screening should implement an opt-off consent
process. Section 125 should only be used in exceptional circumstances where the
school or health services have concerns for a child’s welfare.
The consent process should include information for parents about what their child is
being screened for and questions about whether the child is already under the care of a
vision specialist and/or has glasses.
Setting for vision screening
Vision screening requires a room that is free of distractions and more than four metres
long. The room should be uniformly and brightly illuminated. It should have a light level
of at least 300 lux in the room with about 500 lux to illuminate the test chart. If you are
unsure whether the lighting is sufficient, carry out a formal light meter test.
Venue organisation
Prior to visiting an early childhood centre or school you should:
notify the venue of your intended visit and asked to plan quiet activities for when
vision screening is being carried out
obtain the list of children requiring screening, eg, ENROL, preschool attendance lists
ensure the informed consent process with parents has been completed.
Frequency of visits
Venues should be visited at least three times each year to ensure re-screens can be
achieved. It is acknowledged that this may not always be possible in very small remote
rural areas. In these cases, re-screening could be carried out in a scheduled clinic
setting.
Service promotion
Wherever possible, VHTs should take the opportunity to promote an understanding of
the screening programme. It is extremely important that parents and teachers
appreciate the limitations of the vision screening services. Speaking to school staff
during morning tea/lunch breaks or at staff meetings is recommended.
Information for educators to help them understand vision screening is currently being
developed. VHTs will be notified when this information is available for use. This
information will be available online at the Ministry of Health website, and VHTs can print
copies for distribution to preschool and school teachers, principals and other educators.
National Vision and Hearing Screening Protocols 19

Equipment needed for vision screening
For vision screening, you need:
4 m Parr charts with and without confusion bars with key card (or equivalent Sheridan
Gardner charts
4 m Snellen-ratio chart
occluding glasses or patch
retractable 5 m ruler
masking tape
light meter
chair for the child.
Hygiene protocols for vision screening
Screening involves the placement of a rigid plastic eye patch or hand-held eye occluder
over child’s eye. (NOTE: Vision screening is not performed on children with inflamed
eyes, styes, or where the surrounding skin is broken or inflamed. These children should
be booked for a re-screen at a later date).
Procedures
Option 1 – During screening – wipe rigid eye patch or hand held eye occluder with
alcohol swab after each screen. Allow to dry completely before using on a child.
Option 2 – During screening – place a clean tissue under the eye patch when it is put on
and replace the tissue between each child screened.
Back at base – Ensure eye patch and/or hand-held eye occluder is thoroughly wiped
with alcohol swab and stored in a clean container.
Personnel
Where VHTs have cuts or abrasions of the skin that may be susceptible to infection (i.e.
to the hands) it is advisable to wear disposable plastic gloves. Regular hand washing
during screening is recommended. Where there is no access to a hand-basin, a topical
antibacterial solution handrub or similar is suitable.
Suggested cleaning products
Alcohol swabs: 2 ply – medium grade (saturated with 70% isopropyl alcohol) in sterile
individual packages.
Handrub: Microshield Handrub (containing chlorhexidine gluconate 0.5% w/v in 70% v/v
ethanol) or similar.
20 National Vision and Hearing Screening Protocols

After the screening
Notification to parents
Parents should be notified after every screen using the nationally consistent parent
feed-back form. Children who pass the screen should receive the pass brochure, while
those who are referred should receive the referral brochure and Spectacles Subsidy
brochure.
Copies of the Spectacles Subsidy can be ordered through Enable NZ (phone
0800 17 1981). Printed copies of the Spectacles Subsidy brochure are available in a
number of languages.
The pass and refer brochures are available from the Ministry of Health’s Well Child
team or the Ministry’s website (http://www.moh.govt.nz/moh.nsf/indexmh/childhealth-
b4schoolcheck-parents). These brochures are available in hardcopy in English and
online in six other languages.
Follow up
Local records must be kept of all children who have been screened including: those who
have passed, those requiring a re-screen, and those who have been referred.
Parents/ophthalmologists/optometrists/orthoptists are asked to inform the referrer of the
findings and proposed treatment. This information is recorded for future reference.
If no feedback information has been received from the referral, a follow-up letter or
phone call to the family may be required to see if any action has been taken. If this is
unsuccessful then the case should be referred to the Public Health Nurse Services or
Community Health Team to initiate a home visit. This information must be recorded for
future reference.
Where a child has already been assessed and determined as needing glasses but is not
wearing them, or where a child failed to attend a hospital eye clinic/ophthalmologist/
optometrist appointment, the school’s nurse/public health nurse should be informed. No
further screening is warranted.
Preschool and school recording systems
There is one main national database for recording vision results: The Ministry of
Health’s B4 School Check National Information System. The entry of vision screening
results is required to meet the national reporting requirements for vision screening,
including the B4 School Check. The Ministry of Health and the Ministry of Education
are developing a process for transferring vision screening data into the ENROL
database.
National Vision and Hearing Screening Protocols 21

Subsidies for glasses/spectacles and eye exams
Children with vision problems, aged 15 years and under, who are in low income families
may be able to get funding assistance for examinations, frames, lenses, eye patches
and repairs. The child will need to have an assessment by a vision assessor who is
registered as an assessor for this subsidy. The accredited vision assessor will assess a
child’s vision needs and may recommend glasses or other vision equipment. An
accredited assessor is usually an optometrist, eye specialist, or a service co-ordinator
for the Royal New Zealand Foundation of the Blind. Not all optometrists and eye
specialists are accredited vision assessors. You should have an up-to-date list of
accredited assessors.
There are brochures available for families to explain who is eligible for the subsidy. You
can view this brochure and read further information at the Ministry of Health website.
http://www.moh.govt.nz/moh.nsf/indexmh/disability-fundedservices-glasses
If the child requires a referral and their parent has a Community Services Card, advise
the parent to contact Enable New Zealand to find a vision assessor in their area (phone
0800 17 1981).
22 National Vision and Hearing Screening Protocols

Screening Technique: Parr Letter-Matching Charts or
Sheridan Gardner Charts
The screening is conducted exactly four metres from the child and at the same level as
the child’s eyes. Measure four metres from the child with the tape measure, and mark
the floor at both ends with a piece of masking tape. Note: The front legs of the child’s
chair may be ahead of the tape.
Ensure that the chart (book) and the key card match (ie, both have confusion bars),
have a matte finish to ensure the child cannot see reflections and are free from marks
such as fingerprints or pen ink. Make sure the child is not facing a window or other
bright light source that could make the chart difficult for them to see.
Remember that although the screen is done at four metres the results (eg, 6/6 or 6/12)
are written as though the test was undertaken at six metres. Do not record the results
as 4/4 etc).
Preparing the child for Parr letter-matching charts / Sheridan Gardner charts
1. Seat the child so their eyes are level with the masking tape. Note: The front legs
of the child’s chair may be ahead of the tape.
2. Ask the child to hold the key card on their lap. Explain to the child that you will be
playing a simple game.
3. Show the child a large letter shape from your book. Explain that they have to point
to the shape that is the same on their card.
4. Help the child find the letter on their card. Demonstrate that they are the same.
5. Change the letter and again help the child to find the same letter.
6. When you feel the child understands the task, show the child the eye patch and
suggest they need to be a ‘pirate’ to play the game.
7. Follow the procedure for the Parr letter-matching chart.
Procedure for Parr letter-matching charts / Sheridan Gardner charts
1. Place the eye patch over the child’s left eye.
2. Move to the four metre point. Ensure no other children are sitting between you
and the child being screened.
3. Beginning with the largest letter, show the child progressively smaller letters from
each level. Encourage the child as much as possible. Continue until the child has
difficulty identifying the letters.
4. Record the smallest letter size at which the child identified all letter shapes
correctly. Use the conversion table on the back cover of the book.
5. Place the eye patch over the child’s right eye.
6. Move to the four metre point.
National Vision and Hearing Screening Protocols 23

7. Beginning with the largest letter, show the child progressively smaller letters from
each level. Show the letters in a different order from that which you showed the
child in step 3. Encourage the child as much as possible. Continue until the child
has difficulty identifying the letters.
8. Record the smallest letter size at which the child identified all letter shapes
correctly. Use the conversion table on the back cover of the book.
NB: 6/6, 6/6 is recorded when the child is shown all three 6/6 letters and can
achieve two.
9. If the child has difficulty understanding the Parr chart WITH confusion bars,
consider using the Parr chart WITHOUT confusion bars. NB: In this case a pass is
only achieved where 6/6 is achieved in both eyes. Children not achieving this
should be re-screened (6/9 both eyes) or referred (worse than 6/9 either eye) with
a note to the referrer that the Parr chart WITHOUT confusion bars was used.
Referral pathways
Pass, refer and re-screen criteria for vision screening
Four-year-old children who have a visual acuity of 6/6 in one eye and 6/9 in the other
should be re-screened within six months. This is because one eye may be improving or
one eye getting worse. A re-screen will distinguish the two possible options.
Vision is 6/9 or better in both eyes at the B4 School Check
The child’s vision screening is considered a pass.
Note the measurements of vision on the child’s records.
Take no further action.
Vision is 6/9 in one eye and 6/6 in the other at the B4 School Check
Note the measurements of vision on the child’s record.
Arrange a re-screen for three to six months’ time.
Vision is 6/12 or worse in either or both eyes at the B4 School Check
Refer the child for further assessment according to the Ministry of Health’s referral
guidelines.
On re-screen
If the child’s vision is 6/6 or better in both eyes the re-screen is considered a pass and
no further action is required. If there is no change in the child’s vision (ie, they are 6/9 in
one eye and 6/6 in the other) or their vision has become worse in either eye (ie, they are
6/9 in both eyes, or 6/12 or worse in either eye) refer the child for further assessment
according to the Ministry of Health referral guidelines.
24 National Vision and Hearing Screening Protocols
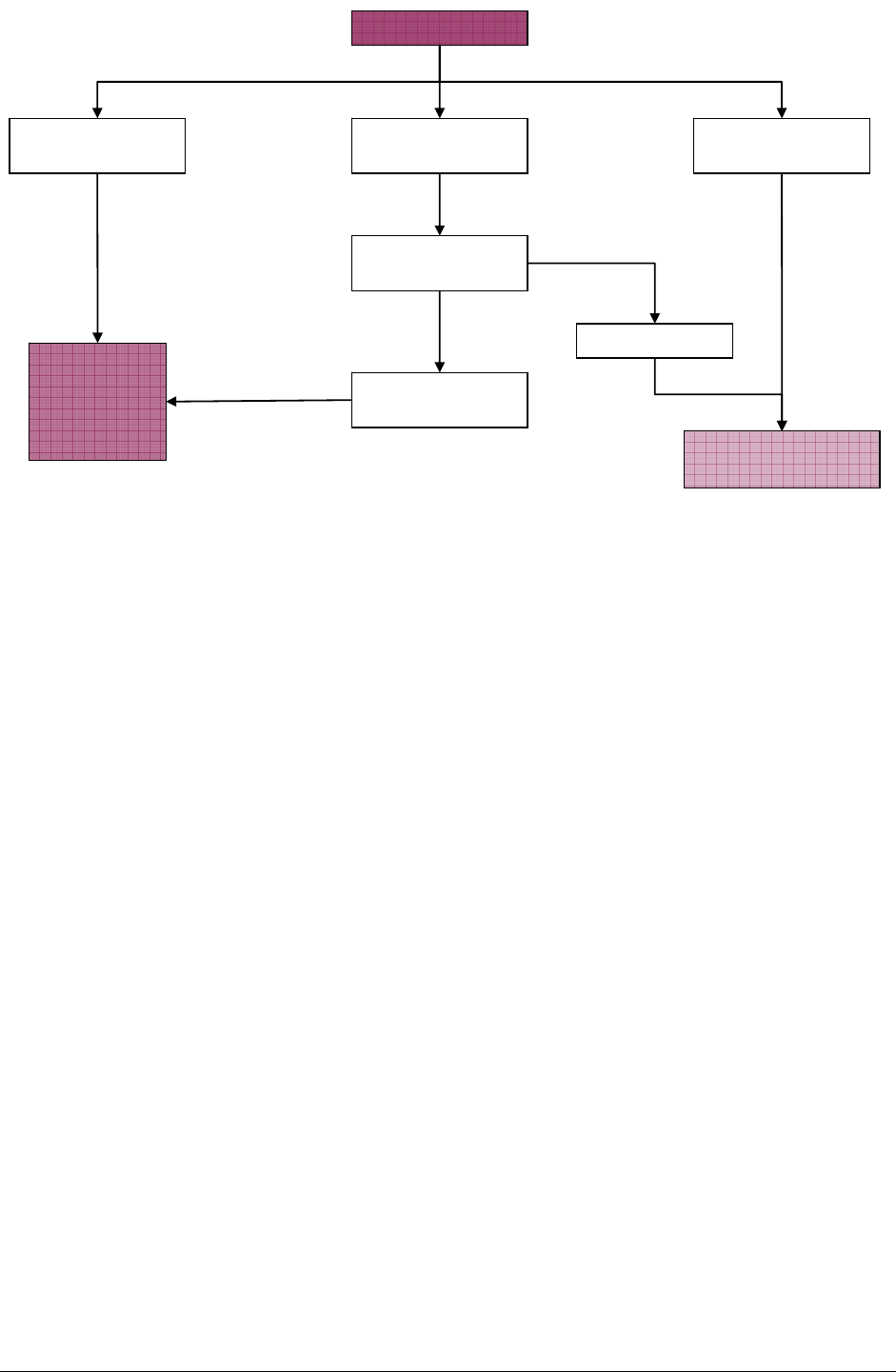
Figure 3: Vision screening clinical pathway and referral at four years old
Vision Screening
6/9 one eye and
6/6 in the other
6/12 or worse in
either eye 6/6 or 6/9 in both
eyes
Retest in 3-6
months
6/9 or worse in
either/both eyes
6/6 in both eyes
NFA
Referral for
optometric
or
ophthalmic
assessment
National Vision and Hearing Screening Protocols 25

Screening Technique: Snellen Vision Chart
The screen is conducted with the Snellen chart exactly four metres from the child and at
the same level as the child’s eyes. Measure four metres from the child with the tape
measure, and mark the floor at both ends with a piece of masking tape. Ensure that the
Snellen chart has a matte finish to ensure the child cannot see reflections. Make sure
the child is not facing a window or other bright light source that could make the chart
difficult for them to see.
Preparing the child for Snellen vision screen
1. Stand the child behind the four metre mark, with their toes on the masking tape
line.
2. Explain to the child that you will point to random letters on the chart and ask the
child to identify each letter.
3. Ensure that the child knows the names of the letters.
4. Follow the procedure for the vision chart with the Snellen Vision screen.
Procedure for Snellen vision screen
1. Place the occluder in position with the child’s right eye visible. Explain that the
child is to hold the occluder in place until asked to move it.
2. Turn the eye chart over. Beginning with the largest letter, point to progressively
smaller letters (two or three letters from each level is sufficient). Select letters
randomly. Encourage the child as much as possible. Continue until the child has
difficulty identifying the letters.
3. Record the smallest letter size at which the child identified all letters (ie, the whole
line) correctly.
4. Ask the child to turn the occluder over, so their left eye is visible.
5. Turn the eye chart over. Beginning with the largest letter, point to progressively
smaller letters (two or three letters from each level is sufficient). Select letters
randomly and in a different order from that in step 2. Encourage the child as much
as possible. Continue until the child has difficulty identifying the letters.
6. Record the smallest letter size at which the child identified all letters (ie, the whole
line) correctly.
Referral pathways
If the child is under the ongoing care of an ophthalmic practitioner (an ophthalmologist
or optometrist) and has been prescribed glasses:
the child should not usually be screened
if the child is screened, a referral is unnecessary no matter what the vision results
are, but contact the parent or caregiver to provide them with the results and to make
sure the child has had a recent vision examination.
26 National Vision and Hearing Screening Protocols

Offer referral if concerns about child’s vision
If at any stage, a teacher, parent or caregiver thinks the child has any vision or
development-related problems, it may be necessary to refer the child for a
comprehensive vision assessment (see referral guidelines). There should also be an
offer of a referral for the child’s eyes to be examined, as the screen does not cover
some aspects of vision.
Caregivers presenting to a health practitioner with concerns about their child’s
vision
A child’s caregiver or teacher may occasionally have concerns about a child’s health,
development, behaviour or learning and wonder whether a vision problem is causing
these symptoms or difficulties. Sometimes an older child will complain of vision
difficulties. Depending on the child’s age, local services and parental preferences the
initial presentation could be to a VHT, a nurse, an optometrist or a GP.
Following a parent, child or teacher initiated self-referral; the health practitioner
consulted must work within their scope of practice to ensure that the family receives a
timely high quality service as described below.
Health practitioner role
The VHT should screen visual acuity in the appropriate manner for the child’s age
and development and refer onward if required with the results of the visual acuity
screen and any relevant observations of the child.
A nurse or GP should measure and record visual acuities, undertake a clinical
examination of the eye, other appropriate examination of the child and make a
referral or institute management if required.
An optometrist should obtain a history, measure and record visual acuities, examine
the external and internal structures of the eye, assess ocular motility, fusion,
convergence, accommodation, pupil reactions, and conduct all other assessments
necessary to determine a diagnosis. The optometrist should make a referral or
institute management if required and appropriate.
Referrals
In general infants and children under three years of age with visual acuity and other
problems should be referred to an ophthalmologist for further assessment.
In certain situations access issues and parental preferences may mean that an infant
or child under three years is referred to an optometrist. Referrers should regularly
consult with the New Zealand Association of Optometrists (NZAO) about optometrists
available in their area who have appropriate training, experience and interest in
seeing younger children.
Children over three years of age with visual acuity abnormalities could be referred
either to the ophthalmologist at a hospital eye clinic or to an optometrist.
National Vision and Hearing Screening Protocols 27

28 National Vision and Hearing Screening Protocols
Children failing a formal visual acuity screening
Formal vision screening as part of the New Zealand Well Child/Tamariki Ora schedule is
undertaken at four years of age as part of the B4School check and at 11 years of age.
This screen has three possible outcomes; a pass, re-screen or referral (a failure to meet
the performance level considered acceptable on the occasion of the screening).
Re-screens should be notified to the preschool and the parents and done as scheduled.
A four-year-old child who is referred from the vision screen with a visual acuity of 6/12 in
either eye or a five- or an 11-year-old who is referred at 6/9 in either eye should receive
further professional investigation.
There are three possible referral scenarios.
1 A four- or five-year-old child who has distance vision that is equally reduced in
each eye or with less than or equal to two lines difference in the vision between
the eyes could be referred to either an optometrist or an ophthalmologist,
depending on practitioner availability or parental preference.
2 A four- or five-year-old child who has a difference in distance visual acuity
between the eyes greater than two lines can be referred to either an optometrist or
an ophthalmologist, depending on practitioner availability and parental
preference.1,2
If a four- or five-year-old child with greater than two lines difference between the
visual acuity in each eye is referred to an optometrist, referrers should consult with
NZAO about optometrists available in their area who have appropriate training,
experience and interest in seeing younger children.
3 An 11-year-old child who has distance vision that is equally reduced in each eye or
where there is a difference in distance visual acuity of greater than two lines
between the eyes can be referred to an optometrist.
The ophthalmologist at the hospital eye clinic or the optometrist to whom the child is
referred should acknowledge receipt of the referral, and inform both the referrer and the
child’s GP of the outcome of the referral.
1 In the opinion of the Royal Australasian and New Zealand College of Ophthalmologists these children
should in general be referred to an ophthalmologist except if there are access issues or in line with
parental preference.
2 In the opinion of the New Zealand Association of Optometrists these children should be generally
referred to an optometrist except where there is a parental preference to see an ophthalmologist.
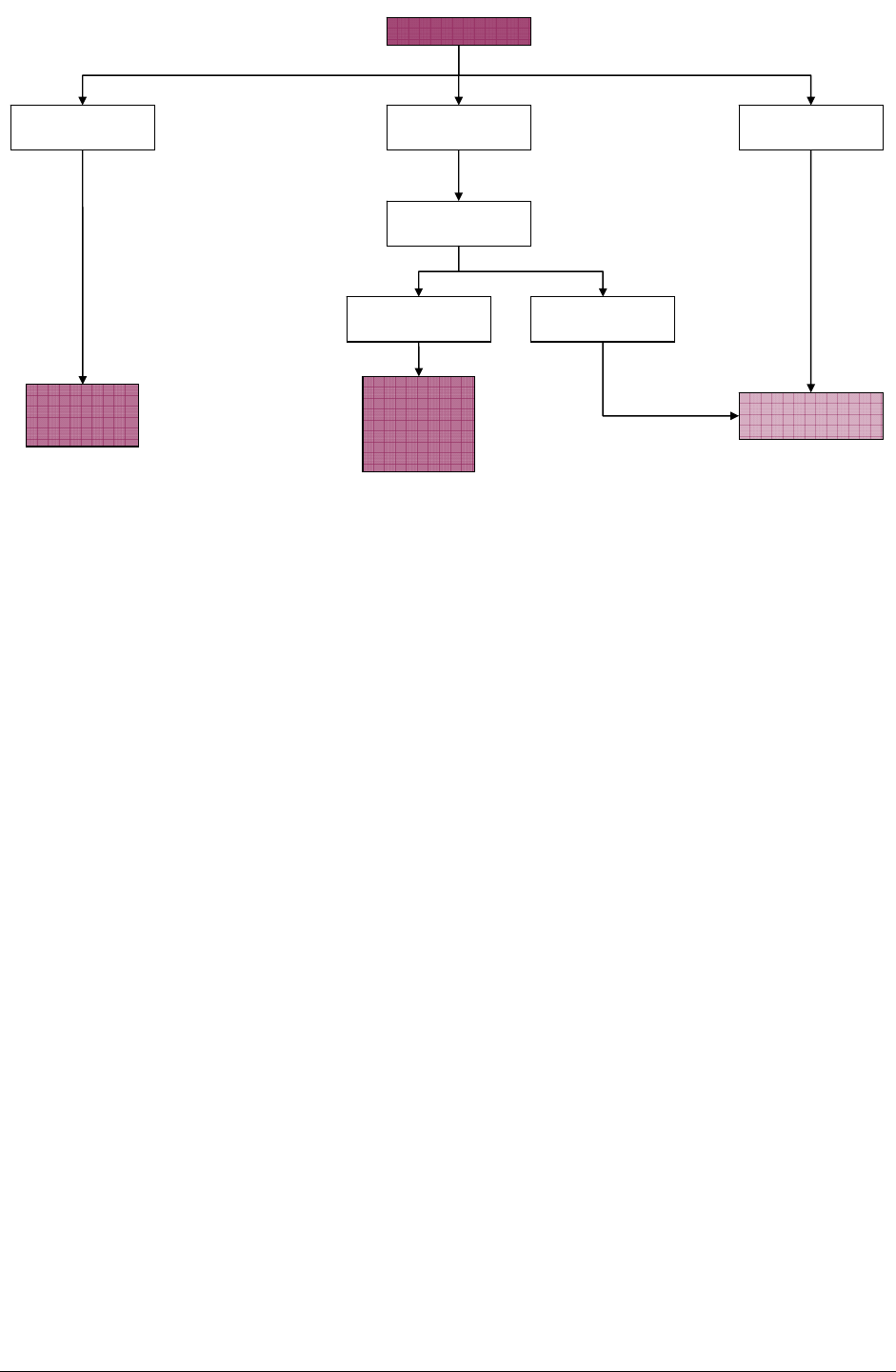
Figure 4: Vision screening clinical pathway and referral at five years and older
Vision Screening
6/9 in one eye and
6/6 in the other
6/9 or worse in
either/both eyes 6/6 in both eyes
NFA
Referral for
ophthalmic
assessment
Retest within 12
months
6/9 in either/both
eyes 6/6 in both eyes
Parent
notified with
option of
referral to
optometrist
National Vision and Hearing Screening Protocols 29

Colour Vision: Ishihara Pseudoisochromatic Plate
Conditions
Illuminate with indirect daylight (do not use in direct sun). The light level must be
500–600 lux. The plate must be held about 75 cm (30”) with the child’s line of sight
perpendicular to the page (if the test is held at a normal reading distance the visibility of
the numbers is reduced and the test is more difficult because the coloured dots making
up the numbers are more obvious). Make sure that no other child can see the
screening or overhear the responses of the child you are screening.
Equipment
This screening uses the 24-plate edition of the Ishihara Test for Colour Deficiency. The
Ishihara books must be replaced at least every seven years.
Procedure
Explain that you will be flipping through the pages of the book and asking the child to
either identify the number or numbers on each page or to let you know if there is no
number (some pages have no numbers). Reassure the child that there is no ‘trick’. The
order of the plates may be jumbled to eliminate learning effects.
Presentation
Make sure the child can identify the number on plate one correctly. Vision of better than
6/60 is required for this plate. Continue to present each of the test plates two through
17 (in the 24-plate edition), allowing approximately three seconds each plate and count
the number of plates misread. Do not count as a fail if a child has self-corrected.
Where a single plate has two numbers on it, an error on either one or both numbers
counts as a single error. Note the number of failed plates.
Ishihara colour vision screen (Ishihara pseudoisochromatic plate)
On the 24-plate edition if three or less errors are made, record as ‘Colour Vision: Pass’
on the child’s records. The word normal is not used, as this is a screening test result
only and is not a full colour vision assessment by an optometrist.
On the 24-plate edition if more than three errors are made on the number plates
(2 to 17) then a colour vision defect is almost certain to be present. Record as ‘Colour
Vision: Defect’. The number of errors made on Ishihara is not a reliable estimate of the
severity of any colour vision defect.
No referral is warranted, unless further diagnosis is required. The child and parents
should be informed so they can discuss career options. Also if a colour vision defect is
present then some educational methods, which use colour coding, can be
compromised. There are no re-screen criteria for colour vision screening. A defect
result warrants a notification to the parent.
30 National Vision and Hearing Screening Protocols

National Vision and Hearing Screening Protocols 31
Recording of Ishihara colour vision
The results of this screen must be recorded in the Ministry of Education’s ENROL
database.