Layout 7 Spectrum Organ Nyp Transplant Brochure
User Manual: Spectrum Organ
Open the PDF directly: View PDF ![]() .
.
Page Count: 28
Organ Transplant Program
NewYork-Presbyterian Hospital
HEART
INTESTINAL AND MULTIVISCERAL
KIDNEY
LIVER
LUNG
PANCREAS
Managing the spectrum
of organ failure
and transplantation

Leadership in Organ Transplantation
The comprehensive transplant services at NewYork-Presbyterian
Hospital support longstanding programs in heart, liver, lung, kid-
ney, and pancreatic transplantation, and most recently, intestinal
and multivisceral transplantation. Ranking first in the nation in
the number of solid organ transplants performed each year,
NewYork-Presbyterian physicians treat adults and children with
the most complex and challenging problems. These include many
patients referred from centers across the U.S. and internationally,
including multi-organ transplant recipients. The center’s out-
comes are excellent in each program.
NewYork-Presbyterian Hospital has made important contribu-
tions to increasing the pool of available donor organs through
innovative approaches in organ selection, preservation, immune
protocols, and improved monitoring of graft status. Its faculty
are also dedicated to the study of ethics and public policy related
to transplantation, and the study of long-term health in donors
and recipients.
The Hospital’s faculty have a distinguished history of advancing
standards of care and survival rates by employing innovative
surgical techniques and by applying basic scientific research in
immunosuppression to the clinical setting. Additionally, cardiac
and liver patients benefit from the invention and perfection of
life-sustaining cardiac and liver devices that extend and improve
the lives of patients awaiting organ transplantation.
Moreover, the program recognizes the complexity of how out-
comes are affected by the myriad factors impacting donors’ and
recipients’ health. When performing transplantation as an imme-
diate lifesaving event, some disparities between donor and recip-
ient are to be expected. In all cases, however, the clinicians strive
to maximize patients’ health prior to transplantation, minimize
donors’ medical issues, and, based on clinical experience, to best
match donor organs with the most appropriate recipients.
Looking to the future of organ transplantation at NewYork-
Presbyterian, Manikkam Suthanthiran, MD, says, “An important
goal is to provide individualized treatment for each transplant
recipient. With the use of molecular diagnostic approaches, we
plan to minimize immunosuppressive drug therapy and offer
personalized medicine to our patients. Our ultimate goal is to
altogether eliminate the need for immunosuppressive drugs.”
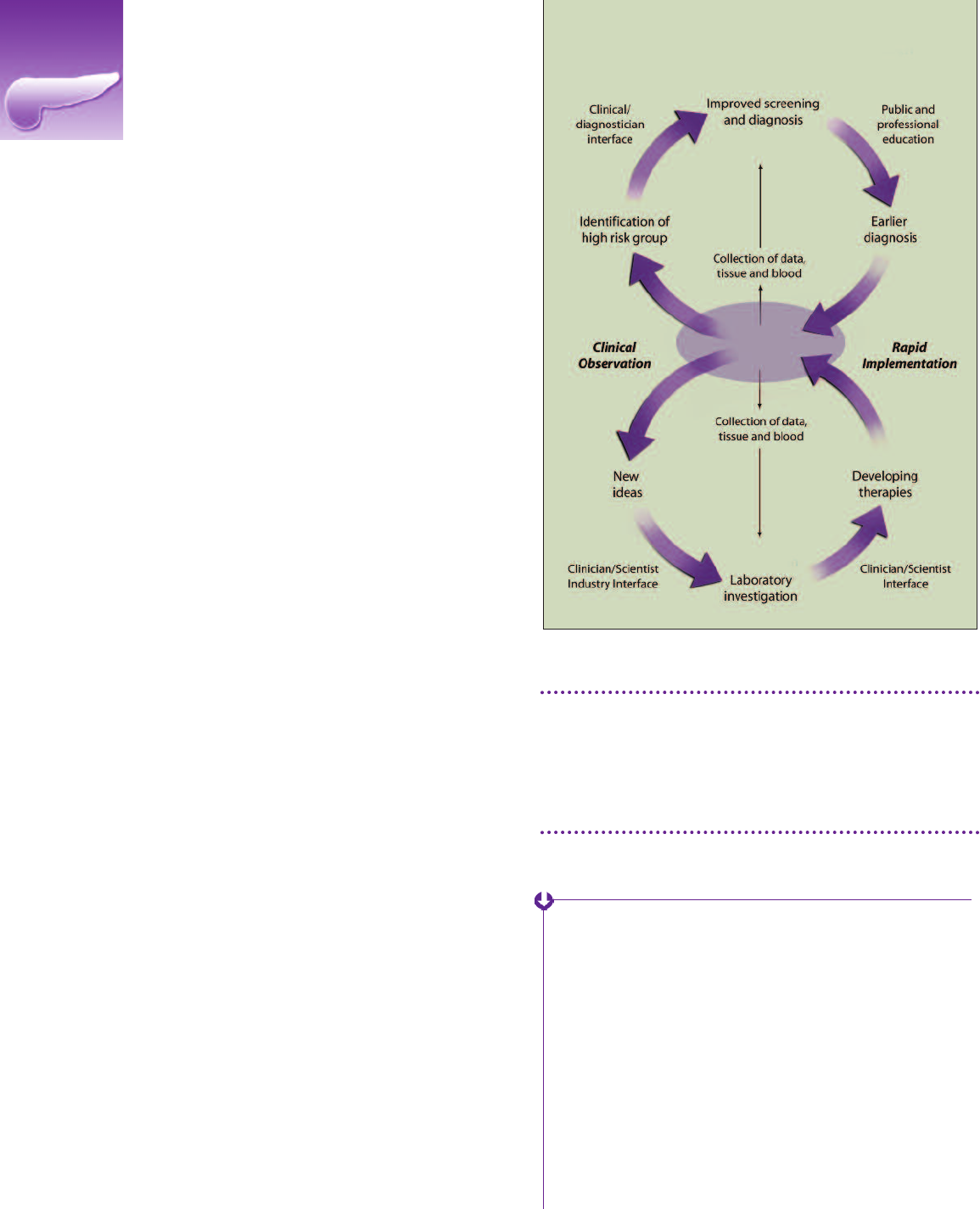
Transplant Initiative
At NewYork-Presbyterian Hospital/Columbia University Medical
Center, a major transplant initiative has been launched to drive
the growth of both clinical and research aspects of transplanta-
tion. This multi-year undertaking will involve medicine, pathology,
and surgery in both adults and children.
Although the Hospital is already a national leader in clinical
transplantation with respect to volume and patient outcomes,
this initiative will further leverage the diverse expertise of its
transplant scientists and clinicians. The goal: new discoveries in
patient care and deeper understanding of the biology of
transplantation. “Formalizing and further integrating the com-
munity of transplant professionals will better position NewYork-
Presbyterian/Columbia to carry out larger research initiatives
both in the laboratory and in patient care,” according to Jean C.
Emond, MD. “The objective is to have a full-spectrum center
dedicated to transplantation – one at the leading edge of discov-
ery and delivery of care – a center of excellence for translational
research, new creativity in medical and surgical care, and the
achievement of groundbreaking outcomes.”
With its commitment to excellence in every facet of organ trans-
plantation, patients and their primary care physicians can expect
the Hospital to provide the highest level of care at every stage of
transplantation and beyond.
Jean C. Emond, MD
Vice Chair and Director of Transplantation,
NewYork-Presbyterian Hospital/
Columbia Medical Center
Thomas S. Zimmer Professor of Surgery,
Columbia University College of Physicians
and Surgeons
Manikkam Suthanthiran, MD
Chief, Department of Transplantation
Medicine, NewYork-Presbyterian Hospital/
Weill Cornell Medical Center
Chief, Division of Nephrology and
Hypertension, and Stanton Griffis
Distinguished Professor of Medicine,
Weill Cornell Medical College
NewYork-Presbyterian Hospital
Comprehensive Capabilities for Adult Organ Transplantation
Heart Failure and Transplantation 2
Intestinal and Multivisceral Transplantation 6
Kidney Transplantation 8
Liver Transplantation 12
Lung Transplantation 16
Pancreas Transplantation 20
Heart Failure and Transplantation
The heart failure and transplantation program at NewYork-Presbyterian Hospital is the
largest and most active heart transplant program in the nation. In 2007, the program
celebrated its 2000th transplant — a milestone no other U.S. hospital has achieved.
Overview
The program consistently treats patients with significant co-
morbidities and high risks, including those with cardiac amyloi-
dosis, diabetes-related end-stage organ damage, and HIV.
Despite taking on these high-risk patients, the program’s survival
rates have consistently met or exceeded the national average
since its inception in 1977. UNOS ranked NewYork-Presbyterian
Hospital’s heart transplantation program number one in 2006
and 2007, and the program continues to lead the nation in both
transplant volume and outcomes today.
Patients with end-stage cardiac disease receive state-of-the-art
care at both campuses of the Hospital.
The Center for Advanced Cardiac Care at NewYork-Presbyter-
ian/Columbia has evolved from what was the very first U.S.
program devoted solely to the treatment of congestive heart
failure. Today it offers the full range of medical and surgical
treatments for heart failure, including established as well as
late generation investigational LVADs.
The Mechanical Circulatory Support Program at NewYork-
Presbyterian/Columbia stands as a clear leader in the implan-
tation, development, and study of left ventricular assist
devices, both as bridge-to-transplantation and as destination
therapy. The program is committed to improving LVAD tech-
nology and to extending the availability of LVADs to under-
served patient populations (including small adults and
children). The latest devices, which are much smaller and
more comfortable than earlier predecessors, are now being
placed for longer-term use with excellent results.
The Perkin Center for Heart Failure at the Ronald O. Perelman
Heart Institute of NewYork-Presbyterian Hospital/Weill Cornell
Medical Center is dedicated to medical and surgical manage-
ment of heart failure. It offers special expertise in treating pa-
tients with pulmonary hypertension and right heart failure.
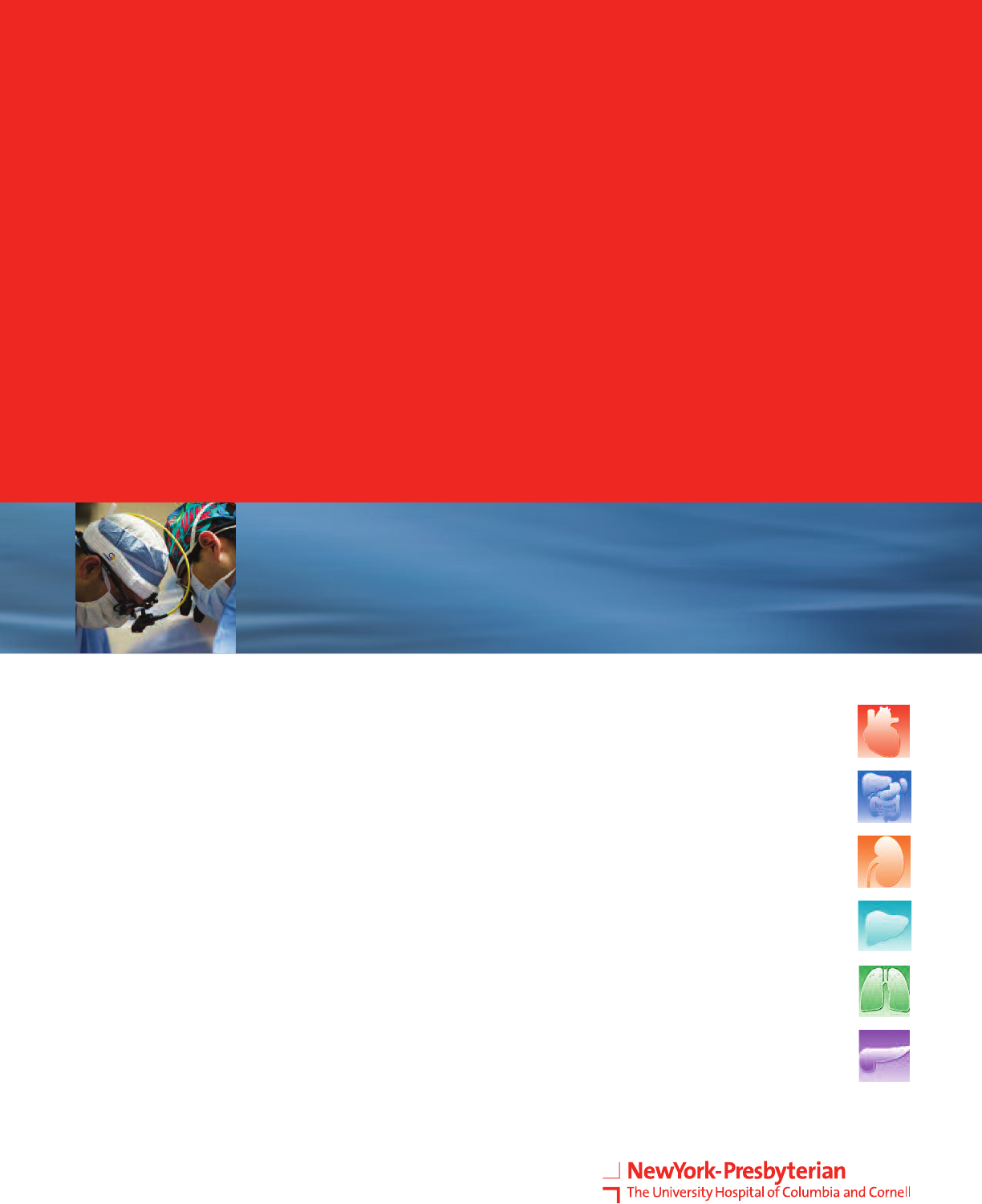
Ren´e Perez
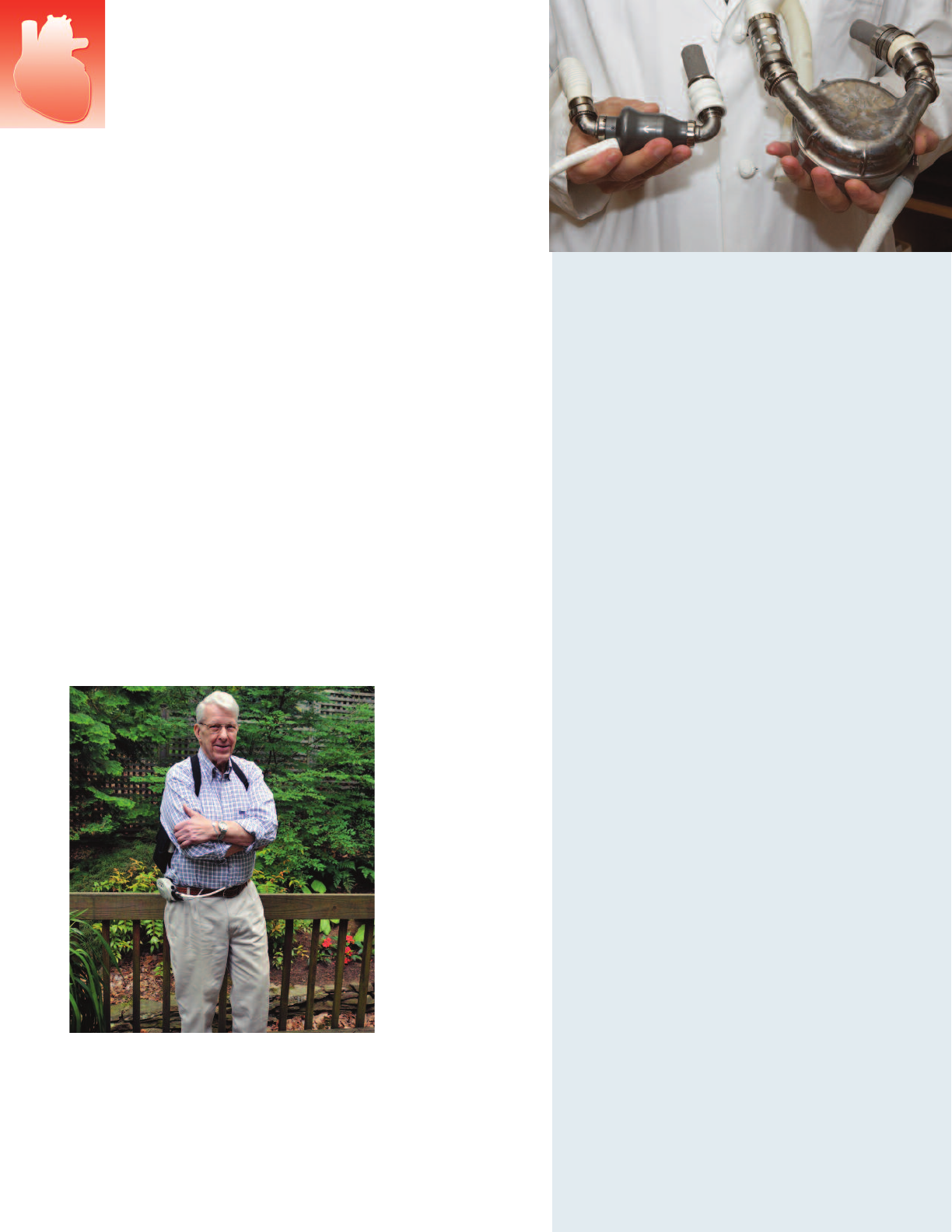
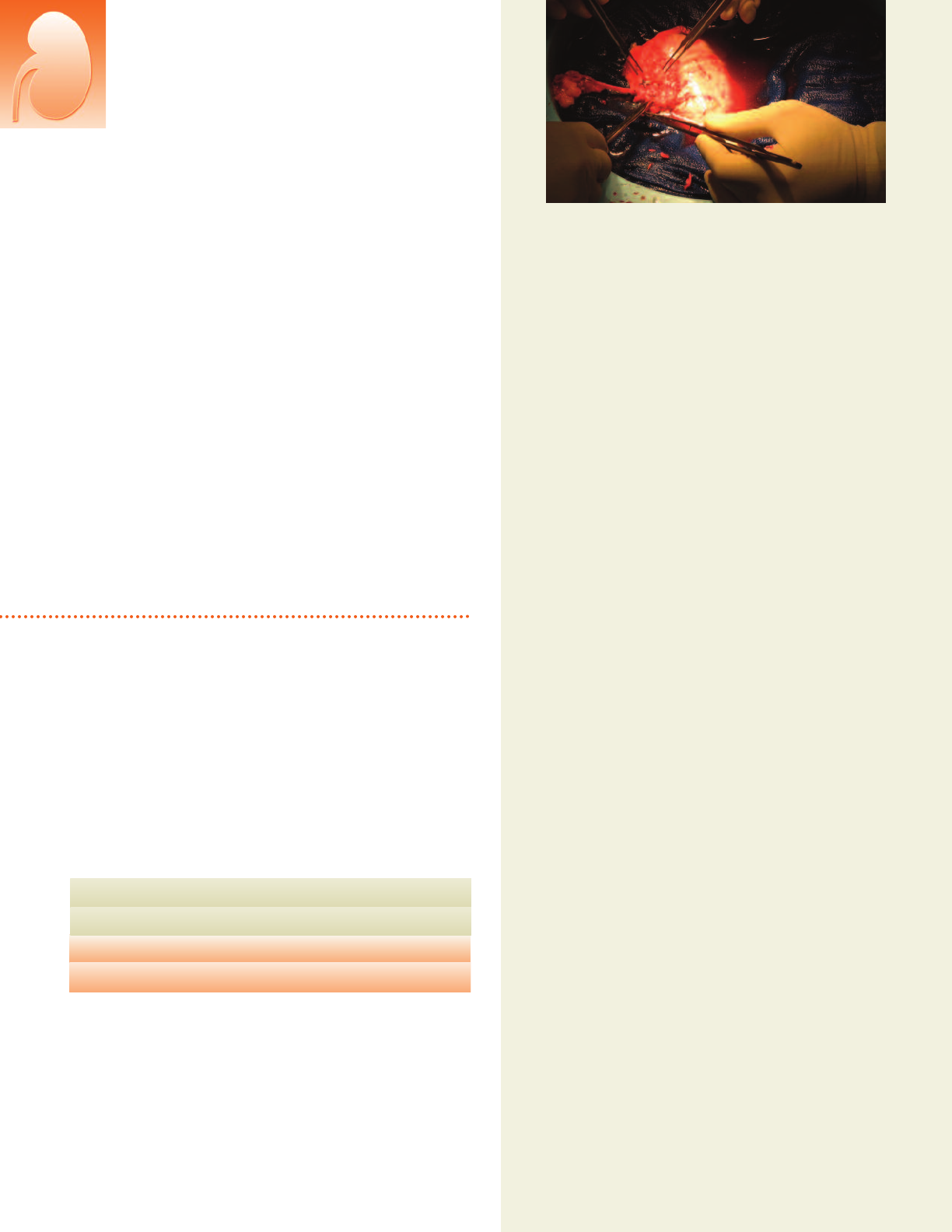
Surgeons performing a heart transplant
at NewYork-Presbyterian Hospital.
▲
2 Heart Transplantation
Innovations
Innovation is the driving force behind the heart failure and trans-
plantation program, with physician-researchers making daily
advances in medical therapies, surgical techniques, immunologic
therapies, imaging methods, and device development.
The program’s long history of innovation encompasses many
milestones, including:
the first mechanical bridge-to-transplantation using intra-
aortic balloon pumps, in the 1970's;
the first pediatric heart transplant, in 1984;
the development of minimally invasive and hybrid (surgical-
catheter based) cardiac procedures;
the development of third-generation LVAD technologies;
the improvement of immunosuppressant regimens;
the creation of a gene-based blood test to replace heart
biopsies to detect rejection after transplantation;
the implementation of extended criteria organ transplantation
to improve access to transplantation; and
the use of gene therapy in the treatment of heart failure.
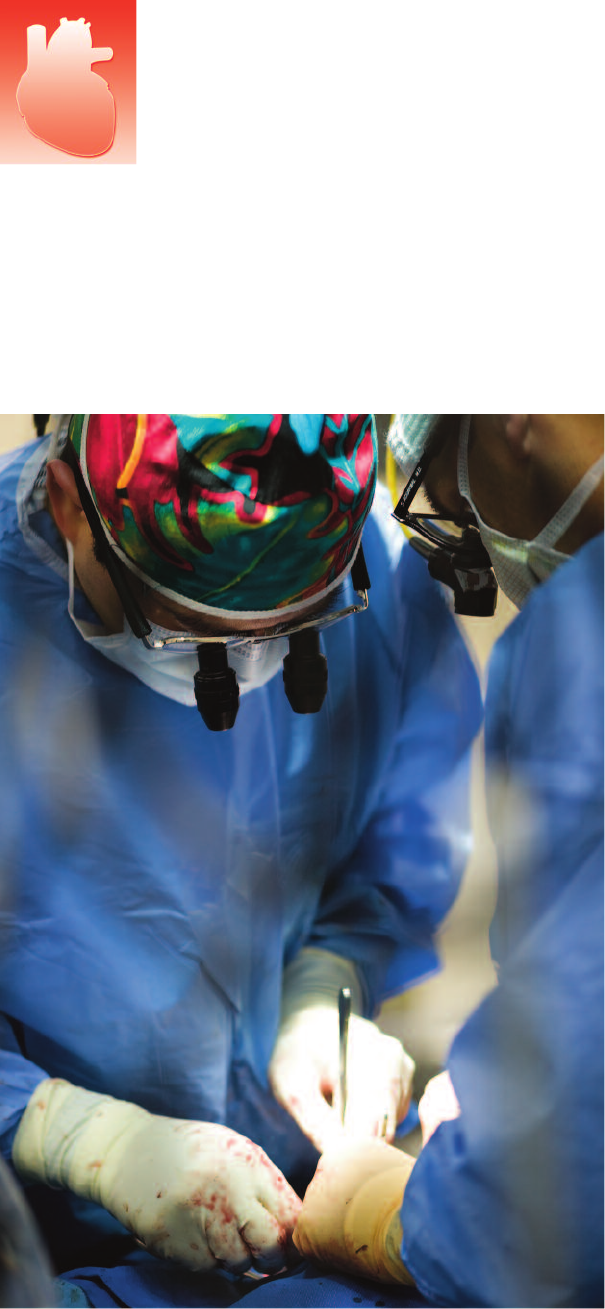
Implantation of LVAD.
▲
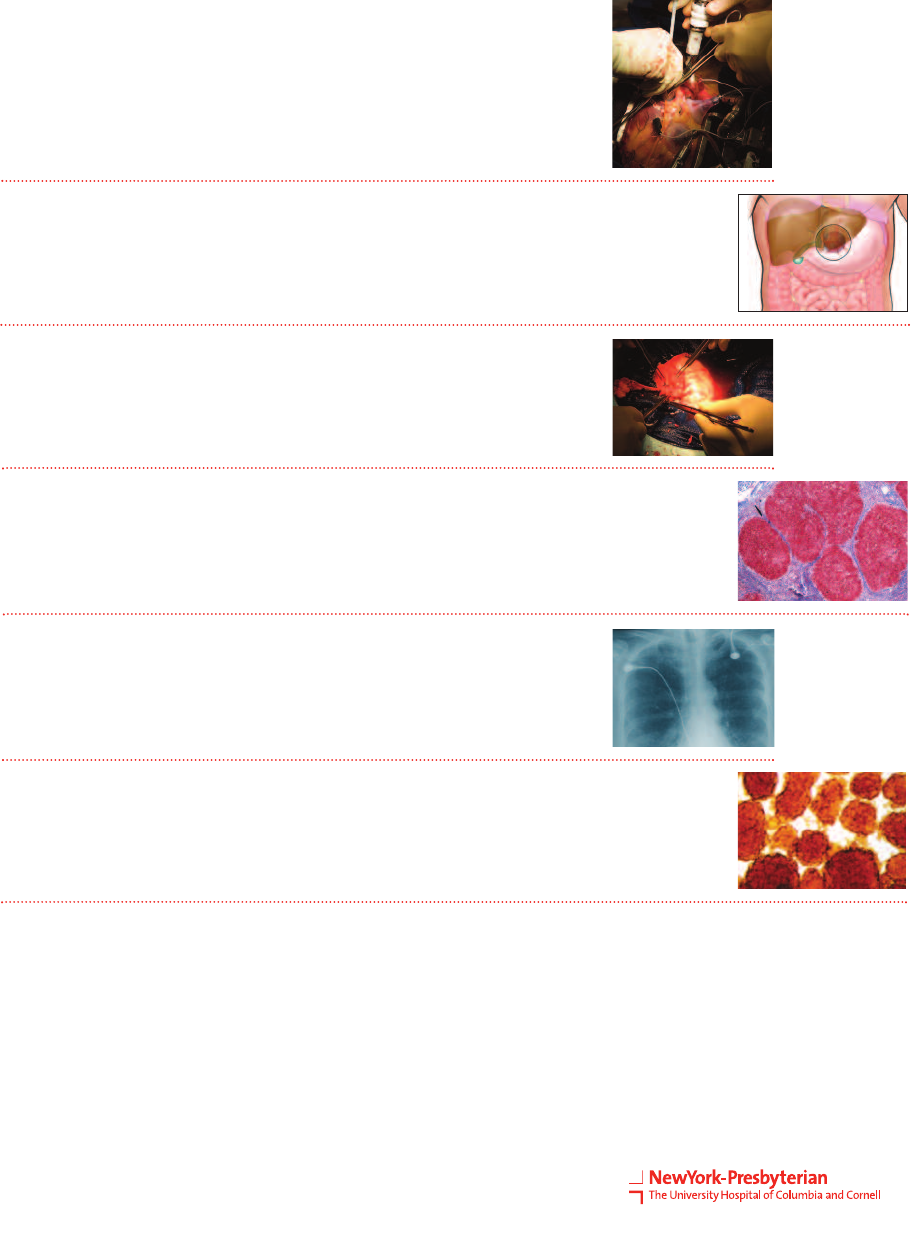
Ultrasound of the heart (axial
section) showing left ventricular
hypertrophy.
Inclusion Criteria
Patients with end-stage cardiac
disease and a life expectancy
of less than one year will be
considered for transplantation.
These patients will have one of
the following:
NYHA Class III or IV CHF re-
fractory to maximal medical
therapy. Objective data
would include a reduced left
ventricular ejection fraction
and a reduced functional ca-
pacity with maximal oxygen
consumption <10 ml/kg/min;
Inoperable coronary artery
disease with intractable
anginal symptoms;
Malignant ventricular ar-
rhythmias unresponsive to
medical or surgical therapy.
Eligibility for
Transplantation
© ISM/Phototake
Inclusion Criteria for
LVAD Implantation
Transplant candidate;
NYHA Class III or IV CHF
refractory to maximal medical
therapy;
Patients dependent on
intravenous inotropic support;
PCW or LAP >20, systolic
BP<80, CI<2.0;
Systolic BP<60.
Ren´e Perez
▲
Heart
3
Research
On the cutting edge:
Researchers at NewYork-Presbyterian/Columbia are currently
conducting a study on the SERCA-2 gene, which is critical
for proper contraction of the heart muscle. Intracoronary
injections of the gene may restore cardiac function and output
in patients with severe heart failure.
One arm of the SCCOR grant (see sidebar) is investigating the
combination of stem cell therapy in conjunction with LVADs to
facilitate recovery of the native heart.
Columbia and Weill Cornell researchers are studying the
etiologies of heart failure and pulmonary hypertension, and
are working to develop targeted therapies based on their
discoveries.
Cardiac transplantation researchers at NewYork-Presbyterian/
Columbia developed a non-invasive blood test to detect organ
rejection after heart transplantation. The team is now applying
similar genetic techniques to better define the phenotypes of
heart failure and develop an approach that will be applicable
to pulmonary hypertension.
Currect Clinical Trials:
HeartMate®II: For advanced-stage heart
failure patients: This multicenter trial, led
by NewYork-Presbyterian/Columbia,
found that recipients of the device as
bridge-to-transplantation achieved over
90% survival;
SCCOR: $17 million NIH grant to investi-
gate the most significant challenges asso-
ciated with LVAD therapy – infection,
coagulation, and neurological events;
COPS: Cardiac Output Prognosis Study:
noninvasively measuring cardiac output to
achieve better risk-stratification and iden-
tify patients best suited for transplantation
or LVAD therapies;
Rapamycin vs Neoral: Evaluation of
therapy in preserving kidney function after
cardiac transplant surgery;
NIH RO1 Grant: Erythropoietin in dias-
tolic heart failure;
NIH RO1 Grant: Oxidized LDL in heart
failure;
Assessment of Endothelial Dysfunction in
heart failure with venous biopsies;
CARGO: Genomic profiling to detect allo-
graft rejection after heart transplantation;
CUPID: First gene therapy trial in heart
failure.
Richard Stowe received a HeartMate II in 2006. He feels
completely normal and mobile, and has been able to
eliminate or reduce many of his heart medications. Echo-
cardiography in April 2009 revealed dramatic improve-
ment: his left ventricle is perfectly normal in size, his
ejection fraction has increased from 5-10% to 40%, and
the other chambers of his heart continue to improve.
▲
Comparison of larger LVAD to newer,
smaller device.
▲
Charles Manley
4 Heart Transplantation
Jada Fabrizio
Patient Care
The surgeons and cardiologists at NewYork-Presbyterian Hospital
have a long and distinguished history of advancing standards of
care and the survival rates of patients by using innovative surgical
techniques, by applying basic scientific research in immunosup-
pression to the clinical setting, and by inventing and perfect-
ing life-sustaining cardiac assist devices that prolong life during
the wait for organ availability. Underpinning all their efforts is a
solid foundation of collaborative, multidisciplinary cooperation.
High-risk surgeries, such as coronary bypass surgery with mitral
valve repair, are routinely performed to restore ventricular func-
tion and improve cardiac function sufficiently to avoid transplan-
tation. Where possible, catheter-based techniques are now
replacing open surgeries, or they are employed in conjunction
with traditional surgical techniques in new “hybrid” procedures,
to provide patients with the least invasive, least traumatic, most
effective solutions.
Use of the newest ventricular assist devices now produces fewer
complications and less bleeding than older versions, making
them suitable for patients in earlier stages of disease. The physi-
cians’ expertise in choosing the best therapeutic window for VAD
implantation benefits many patients, who may now receive opti-
mal support before transplantation with smaller, quiet, comfort-
able devices.
For patients who require transplant surgery, protocols are in place
to ensure rapid and seamless coordination of care between the
two transplant centers of the Hospital. Alternate waiting list
strategies for heart transplantation are helping to maximize the
use of extended donor organs. As a result, waiting times to
transplantation are lower at the Hospital than at other centers in
the region, and the ability to transplant sooner translates into
better post-transplant outcomes.
The heart transplant program has implemented extended criteria
protocols for both organ donors and transplant recipients. Today,
extended donor organs are routinely utilized, and may be offered
to patients over age 65 or those formerly considered too com-
promised to undergo transplantation. These extended criteria
protocols are significantly widening the availability of organs and
providing the option of transplantation to patients who would
otherwise be denied treatment, with superior results.
Outcomes
The Hospital currently performs over 100 heart transplant surger-
ies each year, making it the largest U.S. heart transplant program
by volume. UNOS ranked this program first in the nation in 2006
and 2007. One of 12 high-performing transplant centers in the
nation, the Hospital's heart transplant program is part of the
Health Resources Services Administration (HRSA) Transplant Cen-
ter Growth and Management Best Practices Study.
Heart Failure and Transplantation
NewYork-Presbyterian Hospital/
Columbia University Medical Center
Presbyterian Hospital Building, Room 1262
622 West 168th Street
New York, NY 10032
Cardiac Transplant Center: 212.305.7600
Emergency referrals and transfers: 800.NYP.STAT
The use of extended donor and extended recipient criteria permits
transplantation for patients who might never receive a transplant otherwise,
providing more options to improve patients’ quality of life.
“
“
— Ulrich P. Jorde, MD, Assistant Professor of Clinical Medicine
Division of Cardiology, NewYork-Presbyterian Hospital/Columbia University Medical Center.
For the most current data regarding heart transplant
outcomes, please visit www.ustransplant.org.
01 234
Standard 221 150 93 33
High Risk 37 24 17 5
Year 0 1 2 3 4
Year
1.00
0.75
0.50
0.00
0.25
Kaplan-Meier actuarial analysis comparing the survival of
high-risk and standard list recipients at NewYork-Presbyterian/
Columbia, post-transplant (p>0.05).
Source: NewYork-Presbyterian Heart Transplantation Program data, 2007
Heart
5
Intestinal and Multivisceral Transplantation
Intestinal and multivisceral transplantation have become a standard of care in adults
and children with intestinal failure or certain abdominal tumors.
6 Intestinal and Multivisceral Transplantation
▲
Overview
Approximately 200 patients worldwide currently undergo intes-
tinal and multivisceral transplantation each year, the majority of
which take place in the United States. NewYork-Presbyterian
Hospital/Columbia University Medical Center is among the few
U.S. transplantation centers with the expertise to offer this rare
clinical service.
Intestinal grafts are classified as one of the following types:
Isolated intestinal transplantation for patients with intestinal
failure but who have a functioning liver;
Combined liver and intestinal transplantation, for patients
with liver and intestinal failure but normal stomach and
pancreas; and
Multivisceral transplantation including the stomach, liver,
pancreas, and intestine.
Because allograft rejection remains a serious risk, intestinal trans-
plantation has largely been reserved for life-threatening condi-
tions associated with total parenteral nutrition and liver failure.
As advances in surgical technique, immunosuppressant drugs,
and post-operative monitoring have significantly improved
survival, earlier transplantation (before liver failure) has become a
viable option. Approximately 70% of multivisceral transplant
recipients now survive at one year.
Physicians should refer patients with short bowel syndrome for
evaluation at the Center for Liver Disease and Transplantation as
early as possible, and before the development of liver failure due
to total parenteral nutrition (TPN).
Research
A high priority of intestinal and multivisceral transplant research
is expansion of the indications for transplantation to patients
with tumors. The Hospital’s research plans include trials investi-
gating oncological indications for transplant, as well as studies
on induction of tolerance after transplantation.
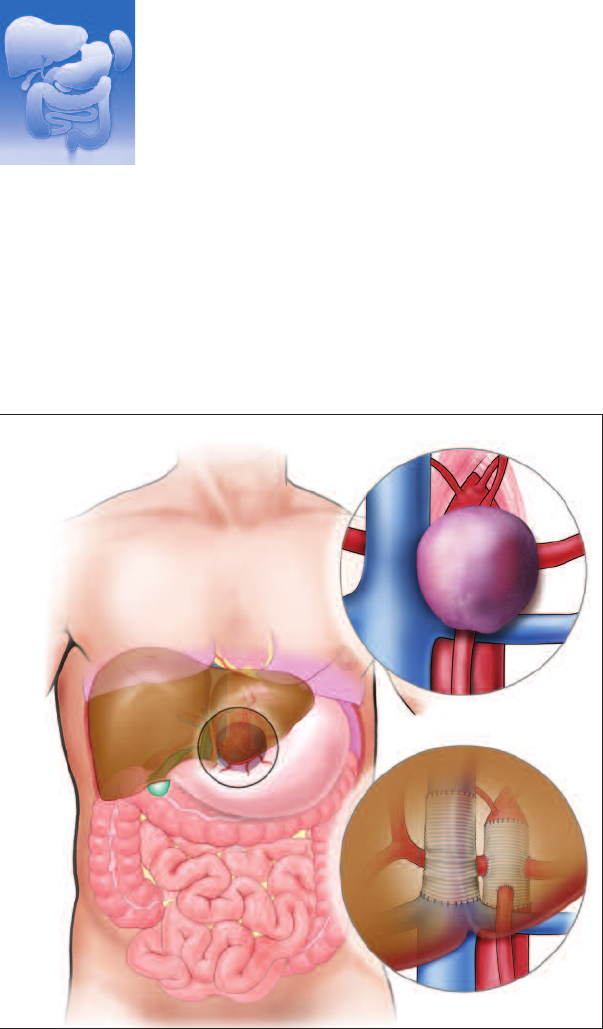
Advances in multivisceral transplantation now allow unprecedented
procedures like the one illustrated above.
Figure 1: A lemon-sized tumor, attached to the main arteries and wedged
behind several organs, was considered unresectable by other
institutions.
Figure 2: At NewYork-Presbyterian Hospital, surgeons successfully
removed the patient’s liver, pancreas, spleen, stomach, small intestine,
and two-thirds of the large intestine.
Figure 3: After excising the tumor safely, the team reconstructed the
blood vessels and performed auto-transplantation to reattach the
patient’s organs. In a very similar procedure, surgeons successfully
excised a deeply embedded tumor from a pediatric patient at NewYork-
Presbyterian Morgan Stanley Children’s Hospital.
2
1
3
Nancy Heim

▲
Innovations
Autotransplantation for Ex Vivo Tumor Resection
Columbia transplant surgeons at NewYork-Presbyterian have
established a new method of performing ex vivo tumor resection
for tumors involving the blood vessels that supply the major ab-
dominal organs. Because of their inaccessibility and their location
in or near the major vessels, such tumors are considered inopera-
ble by most centers. The option of autotransplantation allows
surgeons to remove the intestine, liver, or other abdominal organs
as required in order to access the tumor resection. After excising
the tumor, they reconstruct the blood vessel and then reimplant
the patient’s native organs. Patients undergoing autotransplanta-
tion need no immunosuppressant medications following surgery,
and outcomes have been excellent.
Abdominal Wall Transplantation
Abdominal wall transplantation is the reconstruction and closure
of the abdominal compartment, which may be necessary after
extensive abdominal resections, repeated laparotomies, tumor
resection, wound infections or enterocutaneous fistulae. Abdo-
minal wall transplantation may also be required to close the
abdomen after small-bowel and multivisceral transplantation.
NewYork-Presbyterian is one of the few centers in the country
with experience performing this novel technique.
Intestinal and Multivisceral Transplantation
Outcomes
Worldwide, the one-year survival rate for isolated intestinal trans-
plantation is over 77%. Increased survival rates are associated
with surgeons’ experience in intestinal and multivisceral trans-
plantation, patient volumes greater than 10 cases per year, and
immunosuppression protocols that include induction therapy.*
*Source: 2003 Report of the International Intestine Transplant Registry
Indications for referral and evaluation
Short bowel syndrome caused by mesenteric vascular
thrombosis;
Crohn’s disease;
Trauma;
Volvulus;
Functional disorders such as chronic intestinal pseudo-
obstruction;
Multiple or extensive desmoid tumors, including
Gardener’s syndrome, which necessitate extensive
intestinal removal.
Closure of the abdomen through
abdominal wall transplantation.
Autotransplantation can also be used in place of traditional transplantation
for some patients, precluding the need for a donor organ. This could
save lives and make lifelong post-transplant immunosuppression unnecessary.
—Jean C. Emond, MD, Vice Chair and Director of Transplantation,
NewYork-Presbyterian Hospital/Columbia University Medical Center
“
“
7
Intestinal and Multivisceral Transplantation
NewYork-Presbyterian Hospital/
Columbia University Medical Center
Presbyterian Hospital Building, 14th floor
622 West 168th Street
New York, NY 10032
Phone: 877.LIVER.MD
Emergency referrals and transfers: 800.NYP.STAT

Kidney Transplantation
Kidney transplantation is the optimal therapy for patients with end-stage renal disease,
affording them healthy and productive lives free from dialysis.
8 Kidney Transplantation
Preparation of a donor kidney
before transplantation.
▲
Overview
The kidney transplantation programs at both NewYork-Presbyter-
ian/Columbia and NewYork-Presbyterian/Weill Cornell are the
oldest in the region and the largest in the nation. NewYork-
Presbyterian/Weill Cornell works in conjunction with the Rogosin
Institute, one of the top comprehensive renal centers in the na-
tion. The multidisciplinary transplant team is composed of sur-
geons, nephrologists, social workers, financial coordinators, and
other specialists, who rely routinely on the expertise of an unpar-
alleled pathology unit at the Hospital, as well as its blood bank
and apheresis unit.
Both programs are committed to increasing access to transplan-
tation and returning patients to active lives. Living donor
transplantation is done whenever possible in order to perform
transplantation before patients require dialysis.
For those patients on the UNOS waiting list for a deceased
donor organ, the renal transplantation programs use a highly ef-
fective method of managing their waiting lists. This aggressive
approach ensures that those patients at the top of the list are
ready to be transplanted as soon as a kidney is available. This ap-
proach is complemented by comprehensive protocols to evaluate
all potential organs, including those in the ‘extended criteria’
category. These strategies have reduced the waiting time for
deceased donor organs by an average of four years, reducing
the number of patient deaths while on the waiting list and sig-
nificantly improving outcomes after transplantation.
For patients with other co-morbidities, the programs offer com-
prehensive medical and surgical care in every field. Diabetic pa-
tients with end-stage renal failure may receive pancreatic
transplantation, either simultaneously with the kidney or in a
separate procedure following kidney transplantation. Patients
with advanced cardiac or liver disease may be candidates for
combined heart-kidney or liver-kidney transplantation.
Jada Fabrizio
Innovations
Established in 1961 and 1969, respectively, the kidney transplant
programs at NewYork-Presbyterian/Weill Cornell and NewYork-
Presbyterian/Columbia have a long history of innovation. Both
are dedicated to providing every possible opportunity for trans-
plantation, and to overcoming the most significant challenges in
kidney transplantation. They have developed innovative strate-
gies to increase access to transplantation not only for average
patients, but for people with difficult problems, and those with
immunologic incompatibilities. The programs are national lead-
ers in developing creative approaches including:
ABO incompatible transplantation;
Transplantation across positive cross-match;
Desensitization of HLA antibodies in deceased donor opera-
tions; and
Paired exchanges, including both simple and complex ex-
changes, and transplants involving both compatible and
incompatible live donors.
NewYork-Presbyterian/Columbia is a national leader in the per-
formance of multiple paired living donor kidney transplantation,
a revolutionary approach that may dramatically improve the op-
portunity for patients in need of kidney transplants to find a
compatible donor.
NewYork-Presbyterian/Weill Cornell was a pioneer in developing
the Never Ending Altruistic Donation (NEAD), in which one altru-
istic (or “non-directed”) living kidney donor, willing to donate to
any patient awaiting transplantation, can begin a chain of kid-
ney transplants that otherwise would not be possible.
At NewYork-Presbyterian/Weill Cornell, physician scientists were
the first to develop gene-expression-based assays to non-inva-
sively detect organ rejection after kidney transplantation (pub-
lished in 2001). Using biomarkers available in simple urine tests,
this unique program allows for individualizing and minimizing
the amount of immunosuppressive therapy that patients require.
Donor kidney ready for transplantation
at NewYork-Presbyterian Hospital.
▲
Kidney
The renal transplantation programs offer
patients with end-stage kidney disease four
transplant alternatives.
■
Compatible live donor transplants: The gold standard of
kidney transplant procedures. A kidney from a perfectly
matched sibling donor can function for an average of 35
years, while less perfectly matched kidneys function for 20
years on average.
■
Paired donor exchanges: Offer the benefits inherent in
finding a compatible live donor, compared to waiting for
a deceased donor. Paired donor exchanges have been
performed at NewYork-Presbyterian Hospital since 2004.
Several three-way exchanges (requiring six simultaneous
operations), one four-way exchange, and a six-way ex-
change have also been successfully performed.
■
Incompatible live donors: An option if the donor and re-
cipient are either blood-group incompatible or incompatible
due to antibodies against the transplant antigens. To accept
a kidney from an incompatible donor, the recipient’s blood
must be repeatedly “cleansed” of mismatched antibodies
through plasmapheresis.
■
Deceased donor procedures: Reserved for those patients
who do not have any willing or medically suitable live
donors. Deceased donor kidneys have a good chance of
maintaining their function for 10 years post-transplant.
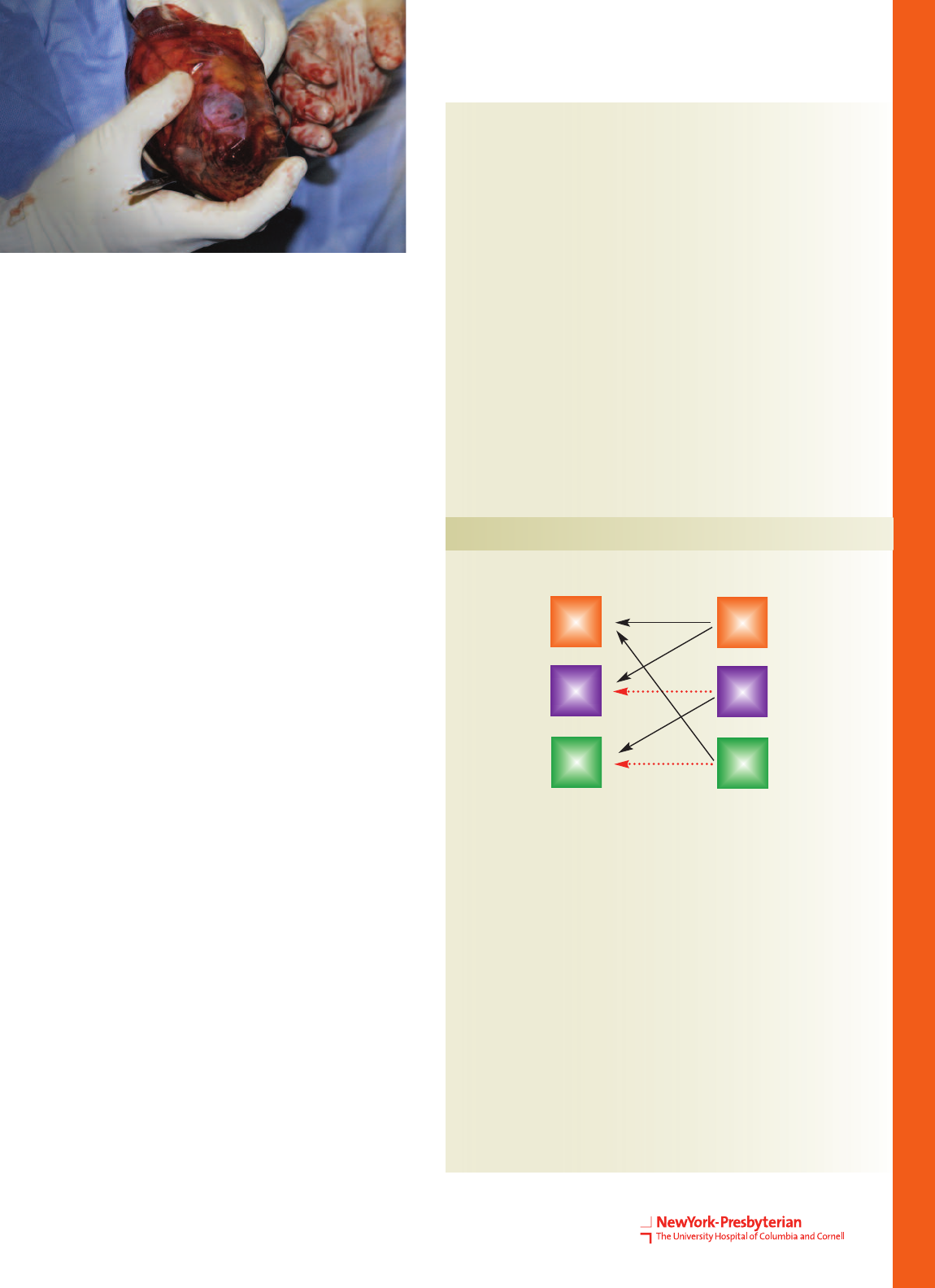
A donor-recipient pair that was compatible with one another
(patient 3) participated in a paired kidney exchange in order to
facilitate the transplantation of two other recipients who had
incompatible donors (patients 1 and 2).
OAB
AB A
AO
Spouse
Recipient 1
Recipient 2
Recipient 3
Friend
Spouse
X
Altruistic Unbalanced Paired Kidney Exchange
Recipients Donors
Jada Fabrizio
9
10 Kidney Transplantation
Research
A major area of research focuses on overcoming immunologic
incompatibilities in transplant recipients. In particular, the pro-
grams are researching ways to optimize paired kidney exchanges
and to improve immunosuppressant protocols. Continued re-
search is underway to perform both donor and transplant opera-
tions through minimally invasive techniques. At this time all
donor operations are done laparoscopically. In recipients, smaller
surgical incisions and laparoscopic operations are undergoing
preclinical testing. Other research efforts include:
investigations of live donor risk;
research to further reduce the already low risk of hemorrhagic
complications in donors;
ways to expand the profile of suitable donors; and
improving immunosuppression regimens.
Patient Care
Together, the two campuses perform over 450 kidney
transplants per year. Trials of most new therapeutic op-
tions are available to NewYork-Presbyterian Hospital's
patients due to their high volume and superb academic
and research facilities.
Aggressive extended criteria protocols enable surgeons
on both campuses to safely use more organs than ever
for transplantation. These protocols are highly success-
ful, especially among older recipients and those doing
poorly on dialysis.
The programs are leaders in coordinating “donor
swaps” to maximize the availability of compatible donor
kidneys. Both centers actively encourage altruistic live
organ donation and are prepared to perform multiple
simultaneous donor and recipient operations.
Where compatible donors are not available, the pro-
grams are among the few worldwide to offer incompati-
ble kidney transplantation. They use the latest
immunologic strategies to cleanse mismatched antibod-
ies from recipients' blood, allowing the transplantation
of kidneys into recipients who would normally reject the
graft. Long-term survival among incompatible recipients
is equivalent to that for compatible transplants.
After transplantation, 90% of patients at NewYork-
Presbyterian Hospital are able to avoid steroid use, as
part of a highly successful steroid avoidance protocol in
place since 2001. Molecular-based techniques, which are
under continued research, now provide patients at both
campuses with highly personalized immunosuppressant
therapy in order to reduce or eliminate the use of steroids
after transplantation. Over 700 transplanted patients re-
main completely free of steroid medications post-trans-
plant, with an average rejection rate of just six percent.
Incompatible Transplants and Paired Exchanges
Since the programs established their comprehensive incompatible
renal transplant programs, over 90 patients have received kidney
transplants when they did not have a compatible live donor, via
ABO blood group incompatible transplants, transplants across a
positive crossmatch, or paired kidney exchanges.
Transplant Rate While on Waitlist
NewYork-Presbyterian OPO Region U.S.
Kidney
Columbia University
Deceased
Donors Only
Kidney
Weill Cornell
Deceased
Donors Only
0.41* 0.36* 0.19 0.20 0.20
0.23* 0.23* 0.12 0.13 0.14
0.37* 0.34* 0.19 0.19 0.20
0.25* 0.16* 0.12 0.12 0.14
*Statistically higher compared to U.S.
Patients at NewYork-Presbyterian Hospital are significantly more likely to
receive a kidney transplant while on the waitlist than patients at other
hospitals regionally and nationally.
Suturing the anastomosis during
kidney transplant surgery.
▲
7/06-6/07 7/07-6/08 7/07-6/08 7/07-6/08 7/07-6/08
Source: SRTR Center and OPO Specific Reports, January 2009
Kidney
Partners in Care
Numerous specialty programs provide additional services to en-
sure the comprehensive depth and breadth of care:
A program with the Columbia University Department of Obstet-
rics and Gynecology provides women with specialized care in
fertility and pregnancy after kidney transplantation.
A program with the Columbia University Department of Derma-
tology specializes in treating skin cancer and other dermatologic
diseases in transplant patients.
The Live Donor Programs at both campuses are dedicated to the
health and well-being of potential live donors. These programs
advocate solely for donors and act completely independently of
the needs of recipients.
The program at NewYork-Presbyterian/Weill Cornell works in
seamless conjunction with the Rogosin Institute, one of the top
comprehensive renal disease programs in the nation. Transplant
operations take place in a dedicated transplant facility, while
patients receive medical care at the Rogosin Institute.
At NewYork-Presbyterian/Columbia, patients receive pre- and
post-surgical care at the Beverly and Arthur Shorin Comprehen-
sive Outpatient Transplant Center.
Outcomes
Since U.S. News & World Report began ranking nephrology,
NewYork-Presbyterian Hospital has been ranked in the top ten in
the nation every year. Even with a large volume of complex
cases, its programs’ outcomes surpass the national average.
The challenges of immunologic incompatibility have been mitigated by our ability
to perform multiple exchanges or incompatible transplants with antibody
removal techniques, so that patients who were otherwise relegated to
the waitlist are now receiving transplants far more quickly than ever before.
“
“
— Lloyd E. Ratner, MD, Director, Kidney & Pancreas Transplantation,
NewYork-Presbyterian Hospital/Columbia University Medical Center
For the most current data regarding renal transplant out-
comes, please visit www.ustransplant.org.
Source: SRTR Center and OPO Specific Reports, January 2009
Valerie Beckford, left,
received a kidney
from friend and
co-worker Jeanette
Martinez, right.
▲
0 20 40 60 80 100
Observed
Expected
Patient Survival Rate
96.95
95.64
Observed
Expected
94.33
92.25
%
NewYork-Presbyterian/Weill Cornell
1-year
3-years
0 20 40 60 80 100
Observed
Expected
Patient Survival Rate
96.67
96.40
Observed
Expected
91.18
91.42
%
NewYork-Presbyterian/Columbia
1-year
3-years
11
Kidney Transplantation
NewYork-Presbyterian Hospital/
Columbia University Medical Center
Presbyterian Hospital Building, 12th Floor
622 West 168th Street
New York, NY 10032
Phone: 212.305.6469
NewYork-Presbyterian Hospital/
Weill Cornell Medical Center
525 East 68th Street
New York, NY 10065
Phone: 212.517.3099
Emergency referrals and transfers: 800.NYP.STAT
Liver Disease and Transplantation
For patients with advanced organ failure, the Center for Liver Disease and
Transplantation provides comprehensive treatment including medical, radiologic,
and surgical care for the most complex and serious diseases.
12 Liver Transplantation
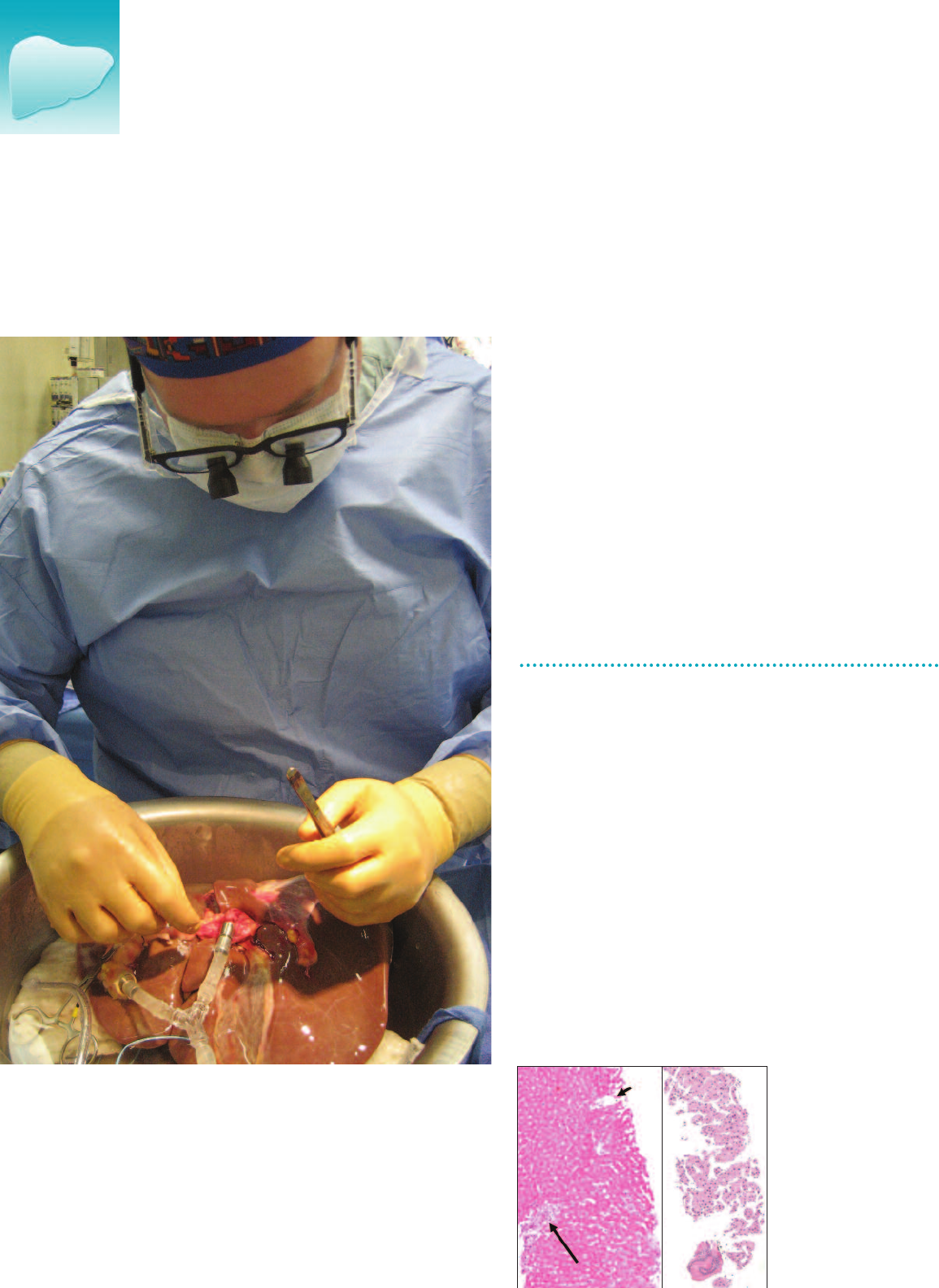
Examination of a donor liver that
was stored with machine preser-
vation.
▲
Overview
Protocols for early intervention and prevention of decompensation
are highly effective in treating many patients. Transplantation serv-
ices are available for patients in whom all other efforts fail.
The Center for Liver Disease and Transplantation (CLDT) performed
its 1000th transplant in 2008. The center’s outcomes consistently
meet or exceed the expected national average.
The center's uptown and downtown academic medical center loca-
tions are seamlessly integrated, with close collaboration among he-
patologists, gastroenterologists, hepatobiliary surgeons, diagnostic
and pathology experts, advanced practice nurses, social workers,
and patient support staff.
By improving access to transplantation, particularly in regions
such as New York that have longer waiting lists, living donor liver
transplantation may reduce patients' risk of dying by 20-40%.
In living donor liver transplantation, up to 60% of a donor's liver
may be removed for an adult transplant, and up to 20-25% for a
child recipient. The donor's liver regenerates to its original size in
several weeks, and donors return to normal activity within about
a month.
The National Living Donor Assistance Center (NLDAC), established
by the U.S. Health Resources and Services Administration (HRSA),
provides financial assistance for travel, lodging, and meals to
those who want to donate an organ and would otherwise not be
able to afford these expenses.
Living Donor Liver Transplantation
Microscopic comparison
of normal liver biopsy
(left) with hepatocellular
carcinoma (right) .
▲

Innovations
The Center for Liver Disease and Transplantation (CLDT) is com-
mitted to understanding and extending the limits of organ
transplantation in order to provide the greatest number of trans-
plants possible with a limited organ supply.
Numerous clinical trials have yielded methods to reduce the size
of tumors, and in so doing, render patients eligible for trans-
plantation. Among patients with unresectable localized cancer
who have undergone transplantation, the five-year survival rate
is 75-80%.
Living Donor Transplantation
Dr. Emond was a member of the team that pioneered living
donor liver transplantation, which is now considered one of the
most important advances in the treatment of severe liver dis-
ease. Approximately 15-20% of the center's transplant patients
currently receive a liver from a living donor.
Partial Liver Transplantation
NewYork-Presbyterian Hospital was one of the first institutions
to perform split liver transplantation. This procedure now ac-
counts for a substantial proportion of liver transplants in the
U.S., primarily in children.
Organ Preservation
The CLDT has completed a pilot study in machine perfusion to
improve organ preservation between procurement and transplan-
tation. By better protecting the donor organ and preventing dam-
age that can occur between harvesting and transplantation,
surgeons can safely use a wider range of organs with excellent
outcomes. The next step of this study involves repairing and trans-
planting organs that would otherwise have been considered un-
usable, but that are safe and effective after treatment.
Multi-Organ Transplantation
The Hospital has extensive experience in performing combined
liver-kidney transplantations. Approximately 5% of the trans-
plant volume consists of combination procedures. In the sum-
mer of 2007, one pediatric patient received five organs in a rare
multi-organ transplant operation, reflecting the Hospital’s expert
capabilities.
Transplantation for Patients with Liver and Bile Duct Cancer
The CLDT has established a new protocol to perform transplanta-
tion in patients with hilar cholangiocarcinoma. In this experi-
mental protocol, patients receive chemoradiation to eliminate
systemic malignant cells, followed by transplant. Early results
are promising, with no patients having tumor recurrence after
orthotopic liver transplantation. This compares favorably with
the recurrence rate of cholangiocarcinoma after medical or sur-
gical therapy.
Top: Cirrhotic liver stained with trichrome stain. Diffuse
scarring (excess collagen) appears blue; rounded
regenerative nodules (hepatocytes) appear red.
Bottom: In auxiliary partial orthotopic liver transplanta-
tion (APOLT), a partial donor liver provides support
while the native liver recovers.
Liver
▲
Partial Liver Transplantation for Acute Liver Failure
Patients with fulminant hepatic failure traditionally have had
limited options: timely recovery of the native liver with medical
management, or liver transplantation. Having revamped a proce-
dure that was largely abandoned in the 1980’s, transplant sur-
geons at NewYork-Presbyterian/Columbia are now able to offer
patients an important alternative. In auxiliary partial orthotopic
liver transplantation (APOLT), the surgeons resect part of the fail-
ing native liver and attach a partial donor liver to it. The donor
liver supports the patient during recovery, clearing toxins and
preventing brain injury. In the majority of patients, the native liver
recovers with this support. Immunosuppressant medication can
then be withdrawn, and the donor liver withers in most patients.
Although partial liver transplantation is particularly suited to chil-
dren because the regenerative capacity of their livers is optimal,
this technique may also be applied in young adults. In studies it
has proven highly successful, with 100% of patients surviving at
the time of this publication. Over half of patients have com-
pletely withdrawn from immunosuppression and the remainder
are in the process of withdrawal. One patient required surgical
removal of the donor liver. NewYork-Presbyterian Hospital is one
of only a few hospitals worldwide with the expertise to perform
partial liver transplantation.
13
14 Liver Transplantation
Regina Williams with her son, Paul Mladineo, who
donated part of his liver when his mother experi-
enced liver failure due to autoimmune disease.
“Paul and I are doing great. Our livers are functioning
perfectly,” says Williams.
▲
Research
Clinical innovation and scientific progress constitute the core of
the Center for Liver Disease and Transplantation’s mission. The
CLDT participates in multiple government- and industry-funded
clinical research studies at any given time. Patients at the CLDT
have the opportunity to receive treatments that are available in
few or no other centers. The Hospital is also a major center for
the study of outcomes for liver disease treatment and liver trans-
plantation.
Many of the CLDT’s 40-plus studies address hepatitis C, which is
the leading indication for transplantation and a major cause of
organ failure after transplantation.
The CLDT is a leader in the multi-center Adult to Adult Living-
donor Liver Transplant (A2ALL) study, a NIH sponsored trial to in-
vestigate the outcomes of living donor transplantation.
Current Clinical Trials:
Solid Organ Transplantation in HIV: The primary aim of
this observational trial is to evaluate the safety and efficacy
of solid organ transplantation in patients with HIV disease;
Boceprevir (SPRINT 2): A phase 3 safety and efficacy
study of boceprevir in previously untreated patients with
chronic hepatitis C genotype 1;
Telaprevir (Vertex 111): A randomized study of stopping
treatment at 24 weeks vs. continuing treatment to 48
weeks in treatment naive patients with genotype 1 hepati-
tis C who achieve an extended viral response (eRVR) while
receiving telaprevir, pegylated interferon and ribavirin;
Rimonabant (NASH): A placebo controlled trial to study
rimonabant treatment in non-diabetic and type 2 diabetic
patients with nonalcoholic steatohepatitis;
Adefovir Plus Vaccination: Determining the efficacy of
adefovir dipivoxil (ADV) and vaccination in recipients of liv-
ers testing positive for hepatitis B core antibody;
HBV Inflammatory Markers: Assessment and clinical
utility of non-invasive parameters of inflammatory activity
in chronic hepatitis B;
Gilead-0108: Double-blind, multi-center, randomized
study comparing tenofovir disoproxil fumarate, emtric-
itabine plus tenofovir disoproxil fumarate, and entecavir in
the treatment of chronic hepatitis B subjects with decom-
pensated liver disease;
Live Donor Education: Increasing liver donation through
peer-developed education: baseline survey (HRSA);
ALF Adult: A multi-center study of acute liver failure in
adults;
Liver Perfusion: Hypothermic machine preservation of
liver grafts for transplantation;
A2ALL Cohort Study: Adult-to-adult living donor liver
transplantation cohort study;
A2ALL LADR: Low accelerating dose regimen of pegy-
lated interferon and ribavirin pretransplant, to eliminate
post transplant hepatitis C virus recurrence;
ELAD: A bioartificial liver assist device for patients with
acute or chronic liver failure.

Patient Care
The Center for Liver Disease and Transplantation offers the
full spectrum of services to patients with liver disease, from con-
sultations on all forms of benign and malignant liver disease,
to antiviral therapies for hepatitis B and hepatitis C, to transplan-
tation.
Patients co-infected with hepatitis C or HIV may also receive
transplant services at the CLDT, as can patients with cancer of
the bile ducts. NewYork-Presbyterian Hospital is one of very few
institutions to provide these options.
The CLDT is committed to providing care to patients and will
work to assist them with their financial needs.
Living donor liver transplantation
▲
Our surgical team has become expert at assessing the quality and properties of different
types of organs — deceased standard criteria donor, deceased extended criteria organs,
or living donor — and can determine which patient will most benefit from each one.
“
“
— Dianne LaPointe-Rudow, DNP, Senior Transplant Coordinator and Clinical Director of the Living
Donor Liver Transplant Program, NewYork-Presbyterian Hospital/Columbia University Medical Center
For the most current data regarding liver transplant outcomes,
please visit
www.ustransplant.org.
Living Donor Recipient Criteria:
A potential live donor liver transplant recipient must:
Meet the current listing criteria for liver transplant;
Be listed with OPTN/UNOS;
Be informed of the risks/benefits, alternative treatments and
outcomes for living donor and deceased donor transplantation;
Sign consent to have potential donors evaluated for living
donation.
89
87
85
83
81
79
77
75
2007 One-Year Patient Survival at New York Transplant Centers
(percentage of patients survivng one year)
NYPH-CUMC Other Centers
Source: OPTN/SRTR 2007 Annual Report
Outcomes
The Center for Liver Disease and Transplantation has the highest
survival rate while on the waiting list, and the shortest waiting
time, in the New York State region. According to SRTR data from
2007, the Center’s waiting list mortality rate is 7%, compared
with 13% at the other four regional transplant centers. This is
even better than expected when adjusted for the severity of pa-
tients’ illness while on the waiting list.
From January 2004 to June 2006, the CLDT had a 98% survival
rate for the 267 adults, and 97% survival rate for the 43 children
on whom it performed liver transplants; the national rate was
96%. In that period, the one-year post-transplant survival rate
was 88% for adults (87% nationally) and 94% for children.
Liver
15
Liver Disease and Transplantation
NewYork-Presbyterian Hospital/
Columbia University Medical Center
Presbyterian Hospital Building, 14th floor
622 West 168th Street
New York, NY 10032
Phone: 877.LIVER.MD
NewYork-Presbyterian Hospital/
Weill Cornell Medical Center
1305 York Avenue, 4th floor
New York, NY 10065
Phone: 646.962.LIVER
Emergency referrals and transfers: 800.NYP.STAT

Lung Transplantation
Lung transplantation can prolong and dramatically improve quality of life for patients
with severe end-stage, non-malignant pulmonary disease and no alternative treatment
options. The majority of patients return to work, school, and other activities within
three to six months of surgery.
16 Lung Transplantation
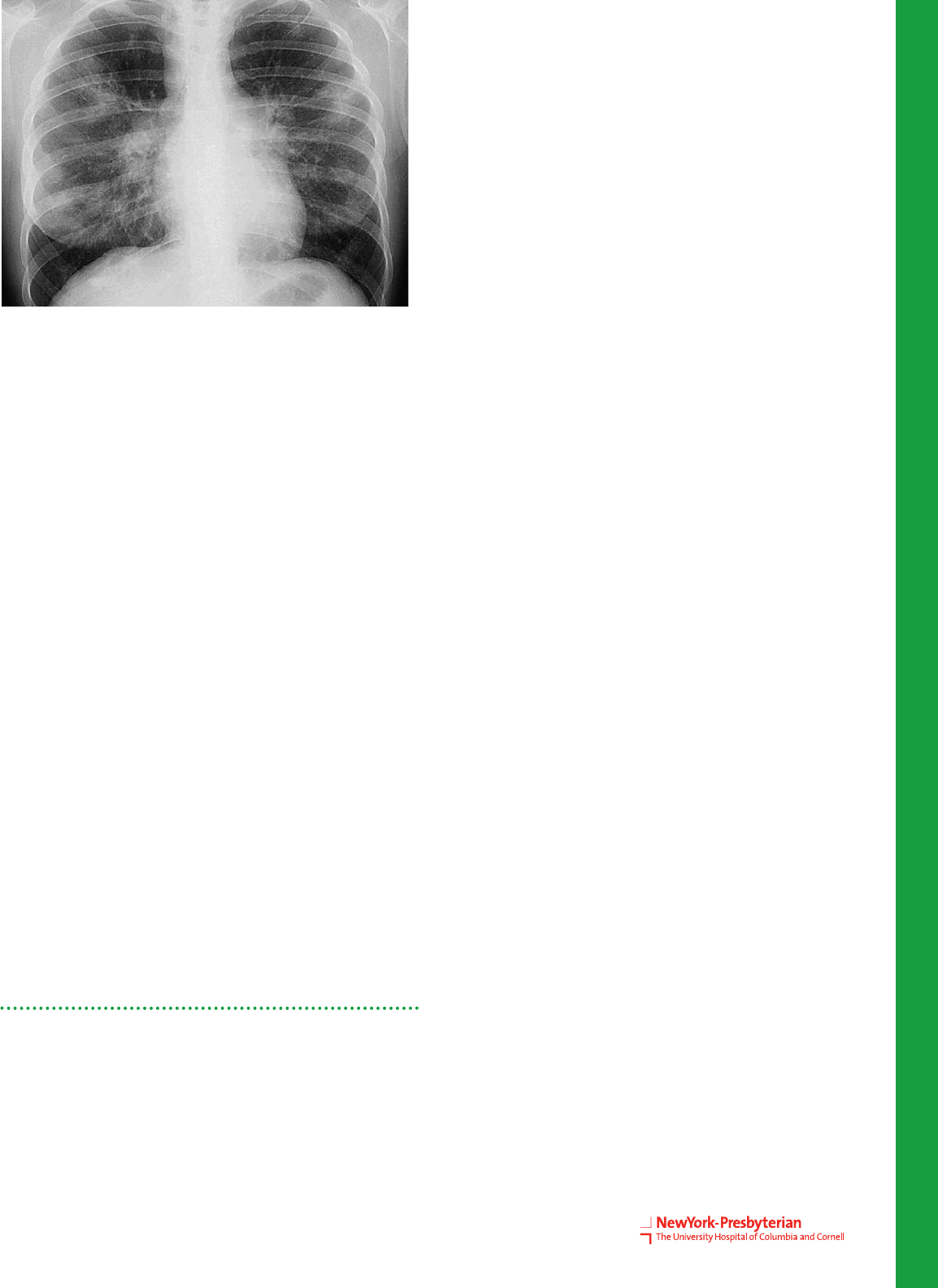
Chest X-ray showing chronic
obstructive pulmonary disease (COPD).
▲
Overview
Widely regarded as the preeminent center for lung transplanta-
tion in the New York tri-state area, the Center for Lung Disease
and Transplantation at NewYork-Presbyterian/Columbia Univer-
sity Medical Center has the highest three-year survival rate
among the U.S. News & World Report Honor Roll Hospitals. Its
patient volume has dramatically risen during the last seven years,
earning the program a position in the top five programs in the
nation in 2007.
Comprehensive, coordinated, multidisciplinary care is provided to
patients with every type of lung disease. To avoid transplantation
whenever feasible, patients are evaluated with second opinion
consultations for eligibility in the interstitial lung disease pro-
gram, the pulmonary hypertension program, adult cystic fibrosis
program, lung volume reduction program, or for eligibility in
new clinical trials. These options can effectively treat certain
conditions with less invasive alternatives, or offer therapies that
serve as a bridge to lung transplantation, delaying the need to
perform this difficult treatment option.
Specialized programs within or affiliated with the Center for
Lung Disease and Transplantation include:
The Jo-Ann F. LeBuhn Center for Chest Disease;
High Risk Lung Assessment Program;
Thoracic Oncology Program;
Interventional Bronchoscopy and Endobronchial Therapy
Program, for the treatment of endobronchial tumors or
tracheobronchial obstructions.
For patients who progress to end-stage lung failure, transplanta-
tion is offered when the expected survival with their native lungs
is one to two years.
ISM/Phototake
Innovations
Since 1986, lung transplant research has been dedicated to im-
proving outcomes in life-threatening lung diseases. Studies at
the Center for Lung Disease and Transplantation continue to
improve treatment options, prevent or delay the progression of
serious lung diseases, and improve the quality of life and sur-
vival for patients. These achievements have been most notable
in the areas of emphysema, idiopathic pulmonary fibrosis, pul-
monary arterial hypertension, and cystic fibrosis.
The Center has pioneered the use of minimally invasive lung
volume reduction (LVR) surgery as well as bronchoschopic LVR
for patients with emphysema. It also uses video-assisted thoracic
surgery (VATS) for both diagnostic and therapeutic interventions
for a number of chest problems that previously required large,
open surgical incisions.
Through laboratory research and participation in multi-center
clinical trials, the Center’s physicians continue to drive progress in
lung transplantation. New immunosuppressive drugs and drug
combinations are increasing the longevity of the transplanted
organ, and decreasing side effects associated with therapy. Ther-
apeutic regimens to prevent and treat infections are also being
investigated. The researchers are investigating methods for pre-
serving donor lungs for a longer period of time before they must
be transplanted into the recipient. Additionally, lung transplant
program clinical investigators are focusing on identifying specific
factors in patients that may help determine the optimal timing of
transplantation.
Understanding Rejection after Transplantation
The Lung Transplant Program is in the vanguard of addressing
the most significant risks to lung transplantation patients:
rejection of the donor organ and infections. Although medical
regimens can successfully protect patients against acute organ
rejection that occurs usually in the first year following transplant
surgery, chronic rejection slowly and steadily undermines the
health of over half of lung transplant patients during the first five
years after transplantation.
Research at NewYork-Presbyterian/Columbia has shed light on
the important role of gastro-esophageal reflux (GER) as one of
the causes of chronic lung graft dysfunction, also known as
chronic rejection.
Researchers at the Center have recently discovered the role
played by a pair of protein receptors in the immune system’s
ability to develop tolerance to a new organ. Their work is part
of an ongoing investigation into why and how transplanted
organs are rejected by the body so that new and improved
methods for protecting a transplanted lung can evolve.
The Center is testing new immunological surveillance tech-
niques to enable the diagnosis of more subtle forms of rejec-
tion earlier than ever before, which ultimately could improve
lung transplant patients’ quality and length of life.
Chest X-ray, front view,
of a 25-year-old woman
with pulmonary sarcoidosis.
▲
Lung
Main Disease Indications
For Transplantation
Interstitial Lung Disease
Cystic Fibrosis
Chronic Obstructive Pulmonary Disease
Pulmonary Hypertension and Sarcoidosis
ISM/Phototake
17
18 Lung Transplantation
Research
Current clinical studies in lung transplantation include:
The use of inhaled cyclosporine versus placebo to prevent the
development of chonic lung rejection after lung transplantation;
Comparison of a Tacrolimus/Sirolimus/Prednisone Regimen
versus Tacrolimus/Azathioprine/Prednisone Immnosuppressive
Regimen in Lung Transplantation after Lung Transplantation;
Genetic Analysis to Predict Rejection of Lung Transplants
(LARGO Study): Utilizing microarray analysis techniques to
determine peripheral blood gene expression, this study fo-
cuses on the prediction of acute rejection after lung transplan-
tation;
Lung Transplant and Hypogammaglobulinemia: Evaluating the
safety and efficacy of intravenous immunoglobulin in patients
with hypogammaglobulinemia after lung transplantation;
Role of Activated Protein C in Early Acute Respiratory Distress
Syndrome: Determining whether levels of activated protein C
after lung transplantation are associated with lung allograft
function;
Molecular Monitoring after Solid Organ Transplantation: Ex-
amining which genes are active in patients undergoing lung
transplantation;
Pathogen Discovery in Chronic Lung Disease: Analyzing the
microbes present in patients after lung transplantation;
Genetic Predictors of Primary Graft Dysfunction after Lung
Transplantation.
Indications for Referral
Chronic Obstructive Pulmonary Disease
Guideline for Referral
BODE index >5
Guidelines for Transplantation
Patients with a BODE index of 7-10;
Chronic progressive hypercapnia or hospitalization for
exacerbation associated with acute hypercapnia;
Pulmonary hypertension and/or cor pulmonale despite oxygen
therapy;
FEV1 <20% with DLCO <20% or homogeneous disease.
Idiopathic Pulmonary Fibrosis
Guidelines for Referral
Histologic or radiographic evidence of UIP irrespective of vital
capacity in patients with idiopathic disease;
Histologic evidence of fibrotic NSIP.
Guidelines for Transplantation
Histologic or radiographic evidence of UIP in idiopathic
disease or fibrotic NSIP and any of the following:
A DLCO of <39% (UIP) or <35% (NSIP) predicted;
A 10% or greater decrement in FVC or 15% decline in DLCO
during six months of follow-up;
A decrease in pulse oximetry below 88% during a 6MWT;
Honeycombing on HRCT.
Cystic Fibrosis
Guidelines for Referral
FEV1 <30 percent of predicted or rapid decline in FEV1,
particularly in young female patients;
Increasing frequency of exacerbations or exacerbation requir-
ing ICU hospitalization;
Recalcitrant and/or recurrent pneumothorax;
Recurrent hemoptysis not controlled by embolization.
Guidelines for Transplantation
Oxygen-dependent respiratory failure;
Progressive hypercapnia;
Pulmonary hypertension.
Pulmonary Arterial Hypertension
Guidelines for Referral
NYHA functional class III-IV, irrespective of therapy;
Rapidly progressive disease;
Pulmonary veno-occlusive disease and PCH;
Endarterectomy candidates.
Guidelines for Transplantation
Persisting NYHA class III or IV on medical therapy;
Failing therapy with IV epoprostenol or equivalent;
Cardiac Index <2 L/min/m2;
Right atrial pressure >15 mm Hg.
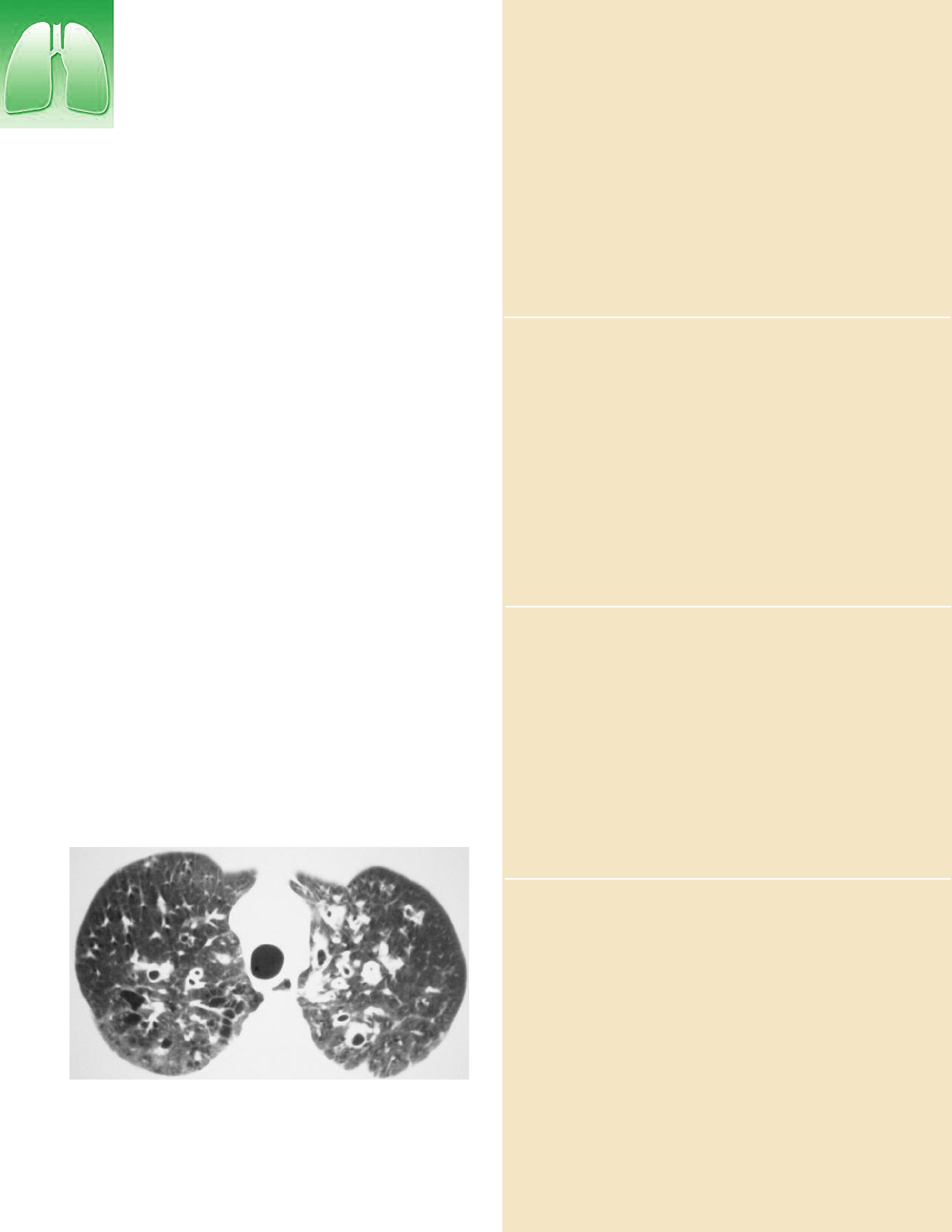
CT scan of the thorax, axial section, showing pulmonary cystic fibrosis.
Opacities that are annular (ring-like) and dispersed in parallel lines
(tram-lines) correspond to dilations of the bronchi.
▲
Reference: Orens, JB; Estenne, M; Arcasoy, S, et al. International Guidelines for the
Selection of Lung Transplant Candidates: 2006 Update – A Consensus Report from the
Pulmonary Scientific Council of the International Society for Heart and Lung
Transplantation. J Heart Lung Transplant 2006;25:745-55.
ISM/Phototake
Lung
Patient Care
Specialized multidisciplinary programs are able to provide alter-
natives to transplantation for many patients as well as help treat
other important medical problems that develop or co-exist in
patients with advanced lung disease. Some examples include
pulmonary hypertension and right heart failure, coronary artery
disease, osteoporosis, and malnutrition.
Those who do undergo lung transplantation benefit from the
breadth and depth of the Hospital’s clinical and academic
expertise and the Center’s commitment to improved outcomes:
Surgical refinements have reduced the size of the incision
required during transplantation.
Recent progress in anesthesia, surgical techniques and post-
operative care have dramatically shortened the time patients
spend in the hospital—an average of 12 to 14 days, down
from an average of 20 days.
Most transplant surgeries are now performed without using
the heart-lung bypass machine, sparing patients from associ-
ated postoperative complications.
The risk of postoperative rejection is minimized with the
newest, most advanced anti-rejection regimens.
Outcomes
The Center for Lung Disease and Transplantation at NewYork-
Presbyterian/Columbia has the highest three-year survival rate
among the U.S. News & World Report Honor Roll Hospitals.
Between July 1, 2001 and December 31, 2007, the program per-
formed 243 lung transplants, with a one-year survival rate of
92%, compared to 82% nationally, and a four-year survival rate
of 72%. The program’s 30-day survival rate for the same time
period is 98%.
Lung Transplantation
NewYork-Presbyterian Hospital/
Columbia University Medical Center
Presbyterian Hospital Building, 14th Floor
622 West 168th Street
New York, NY 10032
Phone: 212.305.7771
Emergency referrals and transfers: 800.NYP.STAT
NewYork-Presbyterian Hospital has taken a leadership
role in perfecting techniques and patient selection crite-
ria for lung transplantation in patients with cystic fibro-
sis (CF). As a result, the Hospital is home to the largest
CF lung transplant program in the New York metropoli-
tan area. Although current management strategies
reasonably control the disease into adulthood in most
pediatric patients, lung transplantation offers extended
survival in patients with advancing disease who have
severe and irreversible airflow obstruction. The Hospital
has also expanded the program to include patients
under the age of 18 years. Transplanted patients with
cystic fibrosis may now undergo subsequent transplan-
tation if their grafts fail.
Expertise in Cystic Fibrosis
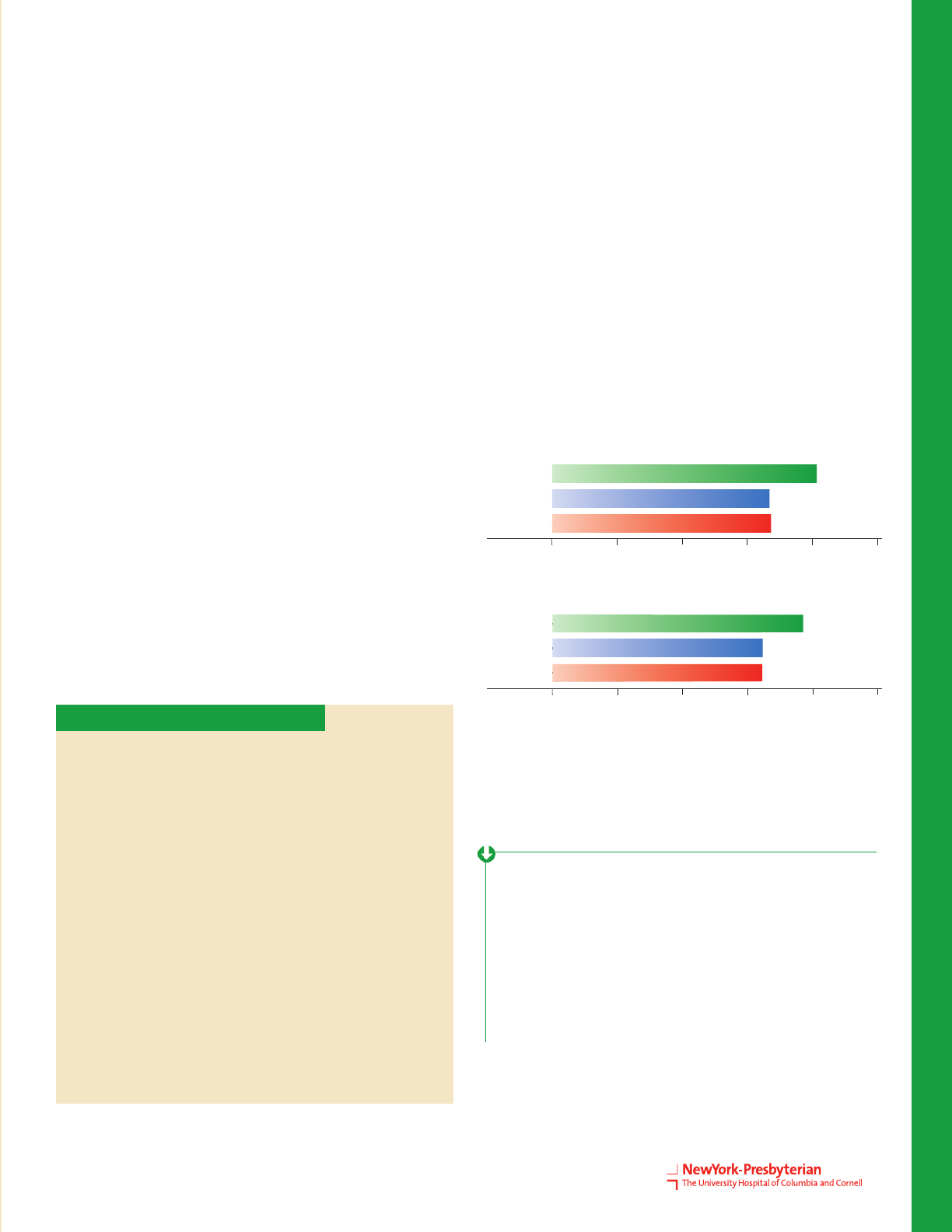
0 20 40 60 80 100
Observed
Expected
National
Patient Survival Rate
80.46
66.83
67.14
%
3 Year
0 20 40 60 80 100
Observed
Expected
National
Graft Survival Rate
77.94
64.91
64.86
%
3 Year
The exponential growth of the lung transplant program offers life-enhancing options to hundreds
of critically ill patients each year. Their quality of life is immediately improved after transplantation.
“
“
— Selim M. Arcasoy, MD, FCCP, FACP, Medical Director, Lung Transplantation Program,
NewYork-Presbyterian Hospital/Columbia University Medical Center
Source: SRTR January 2009 Report.
For the most current data regarding lung transplant
outcomes, please visit www.ustransplant.org.
19
Pancreas Transplantation
Whole organ pancreas transplantation is a viable and preferred option for patients with
type 1 diabetes and end-stage renal disease.
20 Pancreas Transplantation
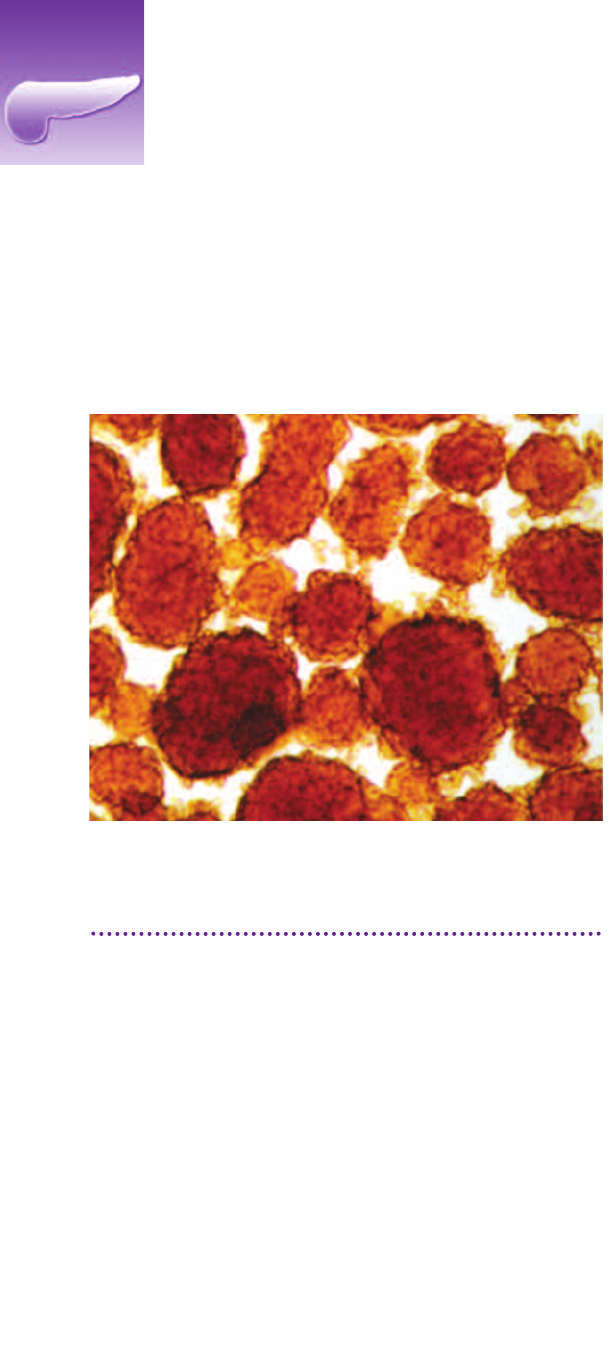
Islet cells
▲
Overview
Transplantation restores normal sugar control, allowing the
majority of type 1 diabetic patients to stop using insulin.
When performed in conjunction with renal transplantation,
pancreas transplantation protects the new kidney from the
damage caused by diabetes. In some patients, it slows the
progression or even reverses some of the secondary compli-
cations of diabetes. Overall, when successful, pancreas
transplantation is much better than insulin therapy in im-
proving quality of life, and in prevention of morbidity and
mortality.
Patients with hypoglycemic unawareness, or ‘brittle dia-
betes,’ may be appropriate candidates for pancreas trans-
plantation regardless of the need for kidney transplantation,
despite the potential complications of immunosuppression.
In such cases, pancreas transplantation can “cure” their dia-
betes and protect the native kidney.
A small subset of patients with type 2 diabetes may also be
candidates for pancreas transplantation.
During the last six years, outcomes in pancreas transplanta-
tion have improved markedly due to advancements in im-
munosuppressant regimens and the increased use of enteric
drainage of pancreatic secretions. Enteric drainage allows
the pancreas to be connected to the intestine instead of the
bladder, where pancreatic secretions can cause significant
inflammation and toxicity.
Surgeons at NewYork-Presbyterian/Weill Cornell have been
performing pancreas transplantation since 1996. Outcomes
have generally met or exceeded the national average. UNOS
approved pancreas transplantation at NewYork-Presbyter-
ian/Columbia in January 2008; it is expected that NewYork-
Presbyterian/Columbia’s premier kidney transplant program
will facilitate rapid growth of the new pancreas transplanta-
tion program, which will overlap both in its patient popula-
tion and its surgical and medical expertise.
Type 1 diabetes with renal failure
Pancreas after kidney transplantation (PAK);
Simultaneous kidney/pancreas transplantation (SPK).
Type 1 diabetes without renal failure (PTA)
Extremely brittle;
Hypoglycemic unawareness;
Progressive secondary complications despite
optimal insulin regimen.
Type 2 diabetes
Phenotypic Type 1;
•
Thin;
•
Early onset;
•
Persistent C-peptide;
Decreased insulin production.
Indications for Pancreas Transplantation
Innovations
The first successful islet cell transplantation in the tri-state area
was carried out at NewYork-Presbyterian/Weill Cornell in 2004.
Tolerance
Both centers have been conducting research to promote immuno-
logic tolerance in pancreas transplant recipients, working towards
the goal of complete freedom from immunosuppressant medica-
tions after transplantation.
Steroid Avoidance
With gene-based therapies and steroid-avoidance protocols now
in place, patients at both centers receive highly personalized im-
munosuppressant therapies that permit lower steroid doses or
steroid-free protocols.
Research
Tolerance induction to islet transplantation using primed or
non-primed UVB irradiated dendritic cells (human antigen
presenting cells) with brief peritransplant immunosuppression;
The development of a new intramuscular site for islet
transplants using an alginate scaffold impregnated with
angiogenic, antiapoptotic, and immunosuppressant factors;
Development of the use of PET techniques to visualize and eval-
uate the function and viability of pancreatic islets in humans and
in experimental models for diagnostic and prognostic use.
Pancreas
Candidates for solid organ
pancreas transplant
(but not islet)
Patients with large body habi-
tus (>180 lbs) or large insulin
requirements;
Patients with life threatening
diabetes;
Patients receiving a simultane-
ous kidney.
Candidates for islet
transplant
(but not solid organ)
Small BMI patients who do not
want invasive procedure;
Patients with life threatening
diabetes with high cardiac
risks.
21
▲
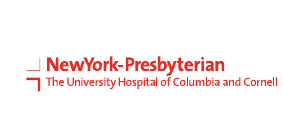
After simultaneous kidney-
pancreas transplants at
NewYork-Presbyterian/
Weill Cornell in 1999,
Glenda Daggert has no
symptoms of the diabetes
that once threatened
her life.
▲
Patient Care
The northeast region of the U.S. has been consistently under-
served as far as access to pancreas transplantation, with rela-
tively few centers serving a disproportionately large metropolitan
population. The expanding programs at NewYork-Presbyterian
Hospital now provide much-needed access to patients with dia-
betes in the New York metropolitan area, particularly those with
the most complex medical and surgical challenges. NewYork-
Presbyterian/Columbia works in close collaboration with the
Naomi Berrie Diabetes Center, the leading diabetes center in the
metropolitan area.
In addition to its transplantation options, NewYork-Presbyter-
ian/Weill Cornell offers a novel surgical alternative, an intestinal
switch operation, and both centers maintain active metabolic sur-
gery programs, which hold promise for reversing type 2
diabetes.
Pancreas transplantation can save lives, in particular for type 1
diabetics who have advanced secondary complications of diabetes
such as renal impairment.
“
—Sandip Kapur, MD, FACS, Chief, Division of Transplant Surgery,
NewYork-Presbyterian Hospital/Weill Cornell Medical Center
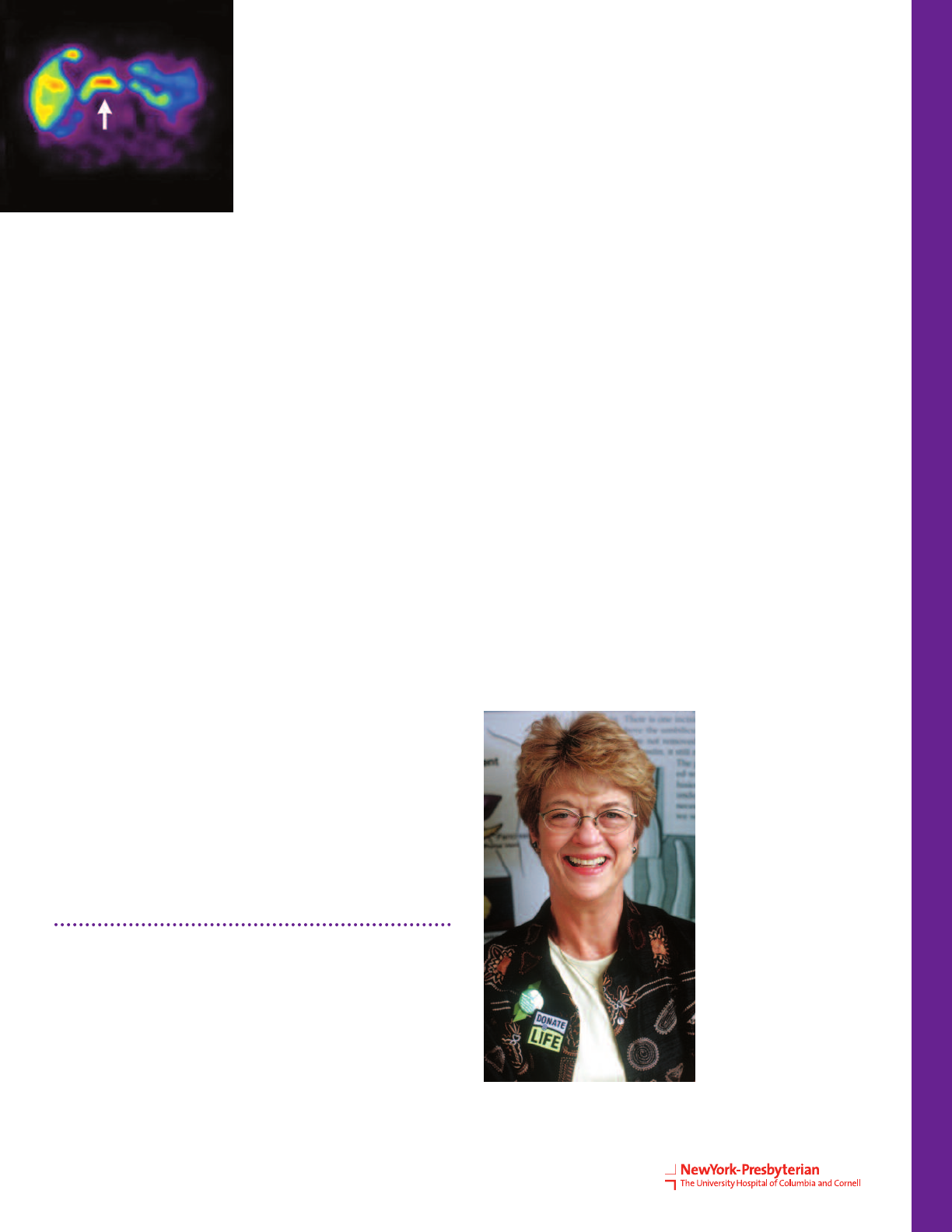
Axial view of pancreas, which is
marked by the arrow.
“
22 Pancreas Transplantation
Pancreas Transplantation
NewYork-Presbyterian Hospital/
Columbia University Medical Center
Presbyterian Hospital Building, 12th Floor
622 West 168th Street
New York, NY 10032
Phone: 212.305.6469
NewYork-Presbyterian Hospital/
Weill Cornell Medical Center
525 East 68th Street
New York, NY 10065
Phone: 212.517.3099
Emergency referrals and transfers: 800.NYP.STAT
Islet Transplantation
Transplantation of pancreatic islet cells into patients with type 1
diabetes offers the possibility of reversing the disease without
the need for major surgery. Even partial islet function in patients
with hypoglycemic unawareness, or “brittle diabetes,” can sig-
nificantly improve the management of this disease and abolish
hypoglycemic unawareness.
In this procedure, islet cells obtained from the pancreas of one or
two deceased donors are infused via catheter into the recipient’s
liver, where they act as a back-up pancreas, producing insulin
and regulating blood sugar. When this is performed with the
patient’s own cells (autotransplantation), the success is very
high, and such patients avoid developing diabetes after pancre-
atic resection. This contributes significantly to their long-term
prognosis.
Cutting-edge research at NewYork-Presbyterian/Weill Cornell has
developed a systemic gene therapy that a) eliminates the need
for immunosuppressant medications to protect islet grafts,
b) restores tolerance, and c) facilitates regeneration, in animal
models. To reduce the volume of islet cells needed for successful
transplantation, the researchers developed a novel anti-oxidant
therapy that optimizes islet isolation and improves their post-
transplant function. The program has successfully reversed dia-
betes in animal models without the use of immunosuppressants
after transplantation. Continued work on these therapies holds
considerable promise for transcending challenges to pancreatic
transplantation, and for extending the long-term durability of
islet transplantation in people.
At NewYork-Presbyterian/Columbia, a team has been conducting
islet transplantation research since 1976. It is one of ten regional
islet resource centers in the U.S. that isolate and transplant islet
cells to treat type 1 diabetes as part of a limited FDA protocol.
At this time, the team is investigating a new method of islet cell
transplantation by impregnating islets into pretreated, non-reac-
tive scaffolds, along with agents to attract blood vessels and
repel rejecting cells. When the treated scaffolds are placed into
abdominal muscles and injected with pancreatic islets, experi-
mentally induced diabetes is reversed in animal models. Both
centers will perform autotransplantation for patients undergoing
pancreatic resection for pancreatitis as part of a broad program
in islet transplantation.
Three types of whole organ pancreas transplantation:
Pancreas transplantation alone as a cure for type 1 diabetes;
Pancreas transplantation combined with kidney transplantation;
Pancreas transplant following live-donor kidney transplantation.
PATIENT
CARE
PEDIATRIC KIDNEY TRANSPLANTATION
NewYork-Presbyterian
Morgan Stanley Children’s Hospital
3959 Broadway, Suite 701
New York, NY 10032
Please call: 866.697.7755
NewYork-Presbyterian
Komansky Center for Children's Health
525 East 68th Street
New York, NY 10065
Please call: 646.962.4324
PEDIATRIC LIVER AND INTESTINAL REHABILITATION
AND TRANSPLANT PROGRAM
NewYork-Presbyterian
Morgan Stanley Children’s Hospital
3959 Broadway – 7th Floor
New York, NY 10032
Please call: 866.697.7755
PEDIATRIC CARDIAC TRANSPLANT PROGRAM
NewYork-Presbyterian
Morgan Stanley Children’s Hospital
3959 Broadway – 2 North
New York, NY 10032
Please call: 866.697.7755
PEDIATRIC LUNG TRANSPLANT PROGRAM
NewYork-Presbyterian
Morgan Stanley Children’s Hospital
3959 Broadway, Suite 701
New York, NY 10032
Please call: 866.697.7755
International Physicians and Patients
Please visit www.nyp.org/international
Each year, thousands of patients from all over the world travel to
NewYork-Presbyterian Hospital.
Our International Services staff provides personalized attention and
makes international patients and their families feel comfortable during
their stay with us. Our managers, coordinators and financial counselors
speak many languages and assist patients with a variety of details such
as scheduling physician appointments, escorting patients to procedures,
requesting second medical opinions, providing information about lodg-
ing and other medical and non-medical services. The first step to learn-
ing more about our services at NewYork-Presbyterian Hospital is to
contact our International Services Office at:
INTERNATIONAL SERVICES
NewYork-Presbyterian Hospital/Columbia University Medical Center
177 Fort Washington Avenue
Milstein Hospital Building 9 Central
New York, NY 10032
Phone: +1 212.305.4900
Fax: +1 212.342.5393
E-mail: internationalservices@nyp.org
NewYork-Presbyterian Hospital/Weill Cornell Medical Center
525 East 68th Street
Greenberg Pavilion 1-503
New York, NY 10065
Phone: +1 212.746.4455
Fax: +1 212.746.4777
E-mail: internationalservices@nyp.org
NewYork-Presbyterian
Pediatric Transplantation Programs
23
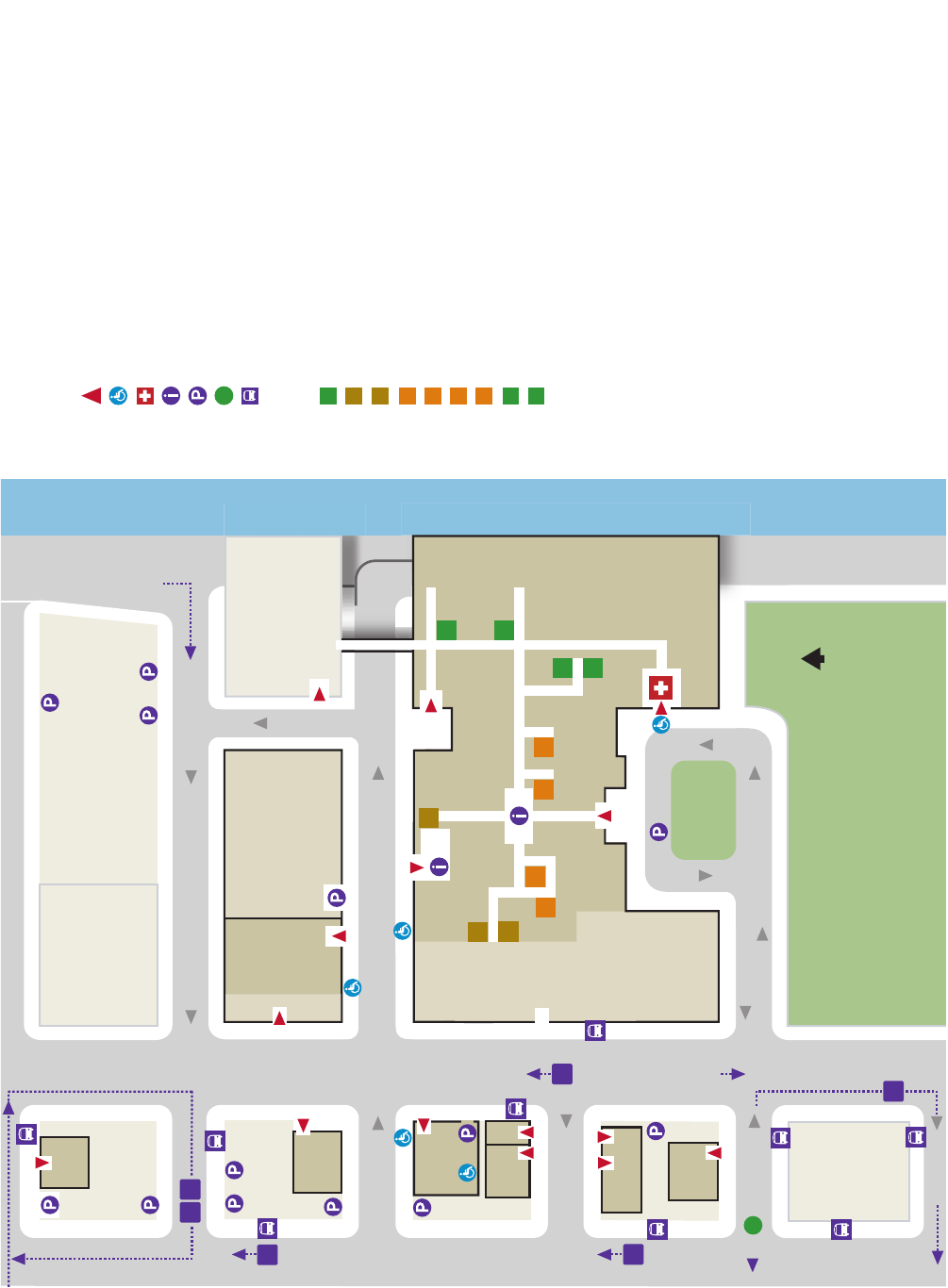
NewYork-Presbyterian Hospital/Weill Cornell Medical Center
6
Visitor's Entrance
Accessible Entrance
Emergency
Information Desk
Visitor Parking
Subway Entrance
Bus
Elevators
K Wing & F Wing, oors 2-9
Greenberg Pavilion
M Wing
N Wing
Payson Pavilion
Starr Pavilion, J Corridor & L Corridor
Whitney Pavilion
Hospital information:
212.746.5454
Legend
reviRtsaE reviRtsaE
Helmsley
Medical
Tower
505
520
1305
411
450
449
525
530
535
Weill
Cornell
Medical
College
Greenberg
Pavilion
NewYork-Presbyterian
Annex
Weill
Greenberg
Center
Stich
Building
Valet
Drop-o
Emergency
Starr
Pavilion
Memorial
Sloan
Kettering
Cancer
Center
Rockefeller
University
E 71st St
evirDRDF
E 69th St
E 70th St
E70tht
S
E8
6tht
S
E8
6tht
S
E 67th St
su
b
n
wotnw
o
d/nw
otpu
subnwotpu
6
N
1315
F
K
H
G
M
P
ST
N
W
M
N
G
G
H
P
F
ST
K
K
W
Additional Medical Oces
Weill Cornell Medical Assoc. Eastside
201 East 80th Street
Weill Cornell Medical Assoc. Westside
12 West 72nd Street
Iris Cantor Women’s Health Center
425 East 61st Street
Weill Cornell Imaging
416 East 55th Street
425 East 61st Street, 9th Floor
520 East 70th Street, lobby level
1305 York Avenue, 3rd Floor
FDR Exit
subnwotpu
E 72nd St
428
M15
M72 M30
M31
M15
M66
1320
to
Medical
Oces
at NewYork-Presbyterian
440
Baker Pavilion / F Wing, oors 9-24
First Avenue
Valet
First Avenue
York Avenue York Avenue
Sotheby’s
Baker Pavilion / F Wing, oors 9-23
Hospital
for
Special
Surgery
Oxford
Medical
Oces
Kips Bay
Medical
Oces
Phipps
House
Medical
Oces
1300
445
Olin
Hall
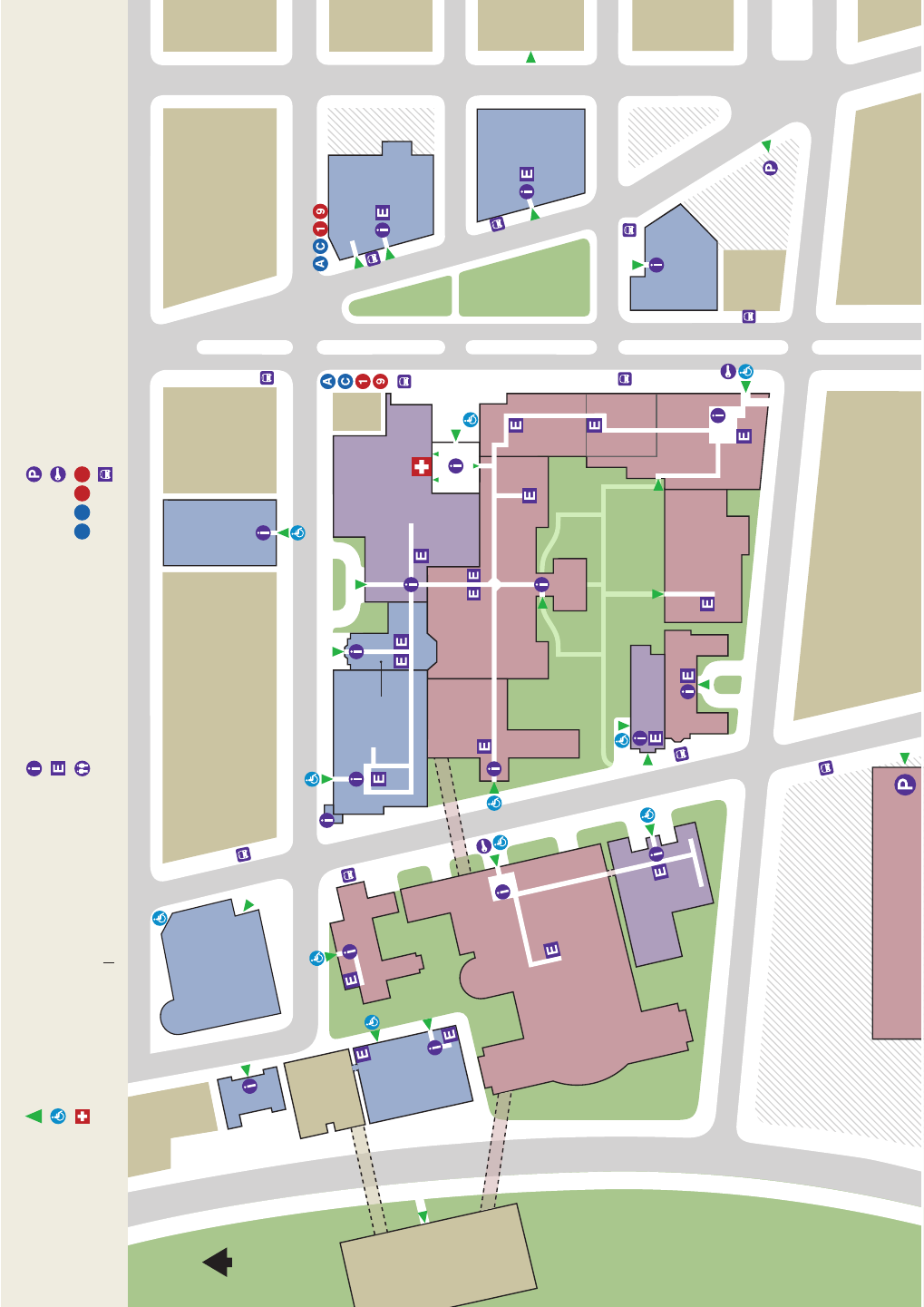
Fort Washington Garage
Broadway
Chapel
Service Building
NY State
Psychiatric
Institute
RiversideDrive
Milstein
HospitalBuilding
Herbert
Irving
Pavilion
HammerHealth
SciencesCenter
W 168th St
NeurologicalInstitute
Columbia
Pediatric
DentalClinic
Mailman
School
ofPublic
Health
NYSPI-
Kolb
Research
Bldg.
Harkness
Pavilion
College of
Physicians
and Surgeons
Black
Building
FortWashingtonAve(IrvingCancerCenterWay)
Armory
School of
Nursing
W 168th St
Broadway
W 168th St
W 167th St
W 166th St
St.NicholasAve
St.NicholasAve
Tower
Morgan Stanley
Children’s
Hospital
NYPH
The Garden
NYC
Dept of
Health
ACN
Clinic
Urgent
Care
Presbyterian Building
Broadway Entrance
Emergency
Broadway
Subway
Subway
Irving Cancer
Research Center
Mitchel
Square
Park
Audubon Ave
Lasker
Biomedical
Research
Building
AIM
Russ Berrie Medical
Science Pavilion
Central
Audubon Ave
Bard
Hall
Vanderbilt Clinic
Presbyterian
Building
Presbyterian
Building
HavenAve
W165thStW165thStW165thSt
Eye Institute
Eye Institute
Research
Annex
Emergency/
Emérgencia
School of
Dental and
Oral Surgery
Audubon
Ballroom
Building
Vanderbilt Clinic
North
St.NicholasAv
N
Visitor's Entrance | Entrada de las Visitas
Accessible Entrance | Entrada Accesible
Emergency | Emergéncia
Visitor Parking | Estacionamiento para las Visitas
Valet Parking | Estacionamiento Atendido
Subway Entrance | Subterráneo
Bus | Autobus
A9
1C
Information Desk | Información
Elevator | Elevadores
Restrooms | Baños
Legend
NewYork-Presbyterian Hospital/Columbia University Medical Center
Hospital Information 212.305.2500
NON-PROFIT ORG.
U. S. POSTAGE
PAID
NEW YORK, NY
PERMIT NO. 1043
New York residents may enroll in the Donate Life Registry to give legal consent for the recovery of organs and
tissues for transplantation and research. Contact the New York Organ Donor Network at www.donatelifeny.org.
333 East 38th Street
New York, NY 10016