025d12e9 Bad1 42a4 866b 690fab076ab7
14A0A5F1-B501-4756-9C4F-9C78148Ae9Da 14a0a5f1-b501-4756-9c4f-9c78148ae9da 14a0a5f1-b501-4756-9c4f-9c78148ae9da 3 2017 pdf 258413772373414384
604C9C77-56Ee-406B-9Da4-8782Cd88Edb4 604c9c77-56ee-406b-9da4-8782cd88edb4 604c9c77-56ee-406b-9da4-8782cd88edb4 3 2017 pdf 258413772373414384
2017-03-27
: Pdf 025D12E9-Bad1-42A4-866B-690Fab076Ab7 025d12e9-bad1-42a4-866b-690fab076ab7 3 2017 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 20

Improving the Value of
Primary Total Knee Arthroplasty:
the ATTUNE® Knee System
David A. Fisher, M.D.
Professor David Parkin

Page 2 of 20
Improving the Value of
Primary Total Knee Arthroplasty:
the ATTUNE® Knee System
David A. Fisher, M.D.
David A. Fisher, M.D.*, is a board certified and fellowship trained orthopaedic surgeon who
specializes in primary and revision knee replacement. He currently serves as Director of the Total
Joint Center of Excellence at OrthoIndy Hospital, Indianapolis, Indiana. In addition, he is an Assistant
Clinical Professor of Orthopaedic Surgery at the Indiana University School of Medicine.
Professor David Parkin
Professor David Parkin is an experienced health economist whose previous roles include serving in
academia as well as Chief Economist in one of the regions of the United Kingdom’s National Health
Service (NHS). He is currently a Senior Visiting Fellow at the Office of Health Economics, a non-
government entity in the U.K., and is an Honorary Visiting Professor at City, University of London.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 3 of 20
Improving the Value of
Primary Total Knee Arthroplasty:
the ATTUNE® Knee System
EXECUTIVE SUMMARY
TABLE OF CONTENTS
Total Knee Arthroplasty (TKA) is a successful and
common procedure that provides pain relief and
improved function in patients with osteoarthritis of
the knee. Despite the globally reported success of
this procedure, studies have shown that up to 20%
of patients are dissatisfied with the results of their
TKA. Given the increasing incidence in osteoarthritis
worldwide, changing patient demographics, and the
corresponding demand for TKAs, there is a need for
meaningful innovation that continues to raise the bar to
improve quality outcomes and meet the expectations of
all stakeholders in a cost-constrained environment.
The ATTUNE® Knee System was designed to help
address some of these shortcomings and improve
patient outcomes. Early clinical results with the ATTUNE
Knee provide insights into how this knee implant could
help provide value as demonstrated by survivorship,
improved patient reported outcomes scores and
reduced secondary procedures for complications such
as patellofemoral pain. Additionally, real world evidence
from one study that included a sample of U.S. hospitals
has shown that those patients treated with the ATTUNE
Knee experienced a shorter length of stay, and a higher
percentage of those patients with the ATTUNE Knee
were discharged directly home, compared to another
leading knee system. These outcomes may bring
benefits to clinicians, patients, providers, and payors.
The purpose of this report is to summarize the burden
of osteoarthritis, primary TKA as a treatment option for
those patients, approaches for evaluating TKA from a
clinical and health economic perspective, and assess the
available data on the primary ATTUNE Knee.
1 Osteoarthritis and Total Knee Arthroplasty
1.1 The Burden of Disease: Knee Osteoarthritis
1.2 Primary Total Knee Arthroplasty: A Surgical Treatment
1.3 Assessment of Outcomes
1.4 Measuring Patient Reported Outcomes (PROMS)
1.5 The Economics of Total Knee Arthroplasty
1.6 Barriers to Referral for Treatment
2 The ATTUNE Knee System
2.1 Improving the Performance of Total Knee Arthroplasty
2.2 Total Knee Arthroplasty Outcomes Using the ATTUNE Knee
2.3 Economic Benefits of the ATTUNE Knee
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 4 of 20
1 OSTEOARTHRITIS AND TOTAL KNEE ARTHROPLASTY
1.1 The Burden of Disease: Knee Osteoarthritis
Osteoarthritis of the knee is one of the five leading causes
of disability among non-institutionalized adults in the
United States.1 According to the Centers for Disease
Control and Prevention, osteoarthritis affects 13.9% of
adults over 25 years of age, and 33.6% of those over 65.
In the United Kingdom, it is estimated that 18.2%
of those over age 45 have knee osteoarthritis.4 Patients
with knee osteoarthritis generally experience pain,
swelling, and unpredictable buckling of the knee; about
80% of patients have difficulties with mobility, including
25% who cannot perform major activities of daily living,
such as dressing themselves.46
The direct health care costs of nonsurgical management
of knee osteoarthritis, which include medication,
physical therapy, and pain center visits, are relatively
low, but there are large indirect costs in the form of lost
earnings, reduced work productivity, and disability benefit
payments.41,58 In addition, there are personal health costs
in terms of decreased activity level, increasing weight
and obesity with related health conditions, and chronic
pain management concerns including potential narcotic
abuse. Interventions that alleviate the burden associated
with osteoarthritis are therefore valued across multiple
stakeholders.
In patients whose knees have become excessively worn
or degenerated due to osteoarthritis, a Total Knee
Arthroplasty (TKA) to replace the damaged bone and
cartilage is a viable option. Modern TKA can be traced
back to the 1970s when John Insall implanted the first
total condylar knee system.33 Despite limited offerings
with this and other early TKA implants and instruments,
with strict indications and careful surgical technique, the
potential success of this operation became evident as
durable pain relief and improved function were benefits
patients could enjoy. With the hope of providing better
solutions for patients with knee osteoarthritis, newer
implants were needed to deal with the wide variety of
human knee anatomy as well as more complex primary
procedures and revision TKAs. This led to much research
into implant and instrumentation design in an attempt to
improve outcomes. By 1990, much of this work had come
to fruition, and the results of total knee arthroplasty now
demonstrate long-term survivorship. In a recent report
from the Australian Orthopaedic Association National
Joint Replacement Registry (AOANJRR), the durability of
total knee implants including more than 350,000 implants
showed 93.5% implant survivorship at 12 years,
meaning 93.5% of these implants were still functioning
well at 12 years.5
The long-term effectiveness of TKA means that morbidity
is reduced and as a result, so is the indirect cost burden.
However, in the short term, TKA is more expensive than
nonsurgical management, leading to increases in overall
short-term medical costs. For example, in the U.S. nearly
800,000 knee procedures are performed annually,2 at a
cost of over $24.8 billion.6
The increased economic burden needs to be weighed
against the cost of not undertaking the procedure – to
both payors and patients alike.
1.2 Primary Total Knee Arthroplasty: A Surgical Treatment
1.3 Outcomes Assessment
There are different ways to measure outcomes after TKA.
Outcomes related to the procedure and associated health
care services include readmissions, reoperations, and
revision surgery rates that can be measured over time.
Patient reported outcomes include patient satisfaction,
improvements in knee function, return to productive
employment and improvements in quality of life.
In general, outcomes of TKA have improved over the past
50 years. National joint implant registries have been in
place for many years in the U.K., Australia, New Zealand
and, more recently, the U.S. These registries track the
performance of specific total joint implants in the different
countries. Failure of an implant is reported as a revision,
and implant survivorship curves are used to describe the
The expansion in the number of total knee procedures is
projected to increase for the next 20 years as longevity
increases, patients seek earlier remedy from arthritic
conditions, and access to care improves. This increase in
numbers of procedures and the attendant costs will put
increasing financial stress on health care systems.38
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 5 of 20
success in terms of the number of implants remaining in
service over time. The good longevity of contemporary
TKA has been reported in all joint registries with 10-year
revision rates of 4-5% (or 95% implant survivorship).9,11
Revision rates, however, may vary among different implant
types, with some implants performing better than others.
Differences between patient age groups have also been
noted with younger patients (under 55 years of age)
having a fivefold increased risk of revision in the first 10
years compared with older patients (over 80 years).36
This difference may be due to increased activity levels of
younger patients leading to wear and loosening of the
implants, or to higher expectations in the younger group,
which could lead to greater dissatisfaction and more
revision procedures.
Patient reported outcomes show improved patient
satisfaction, function and quality of life after TKA.60
Yet, 10-20% of total knee replacement patients may be
dissatisfied with their procedure.18 Issues that remain
for these patients include ongoing pain or discomfort,
stiffness, crepitation (noise or vibration with movement),
and difficulty squatting, kneeling, or negotiating stairs.19,
47,59,61 Research has been conducted to help identify
patient risk factors for complications and poor clinical
results. Patient factors that may contribute to a higher risk
of poor outcomes include a history of depression or mental
illness, morbid obesity, diabetes and chronic narcotic
use.34,35 Furthermore, some of these risk factors are
potentially modifiable conditions, and efforts are underway
to try to improve outcomes by optimizing comorbid
conditions prior to surgery. Some of these programs
include smoking cessation, weight loss for morbid obesity,
improved diabetes management, narcotic cessation, and
pre-operative physical therapy to improve muscle strength
and coordination.17,64 While the hope is that better
outcomes or at least lower episodic costs can be obtained
in these patients, the evidence is not complete.
TKA is a highly technical procedure, requiring surgical skills
to obtain adequate bone preparation and implant fixation,
but also soft tissue balancing to replicate knee function.
With such a major surgical procedure, patient and surgeon
satisfaction are linked. For the surgeon, the ability to
implant the device efficiently and reproducibly is extremely
important. Achieving optimal harmony of implant
positioning/alignment and soft tissue balance during
the procedure can affect the long-term satisfaction for
the patient and is part of the art of TKA.30 Furthermore,
the longevity of the reconstructed knee may be directly
related to the design and quality of initial fixation. Patient
satisfaction and outcome are at least partly determined by
specific implant design features including sizing options,
implant kinematics (how the implants track relative to
the native knee), the patellofemoral articulation, as well
as surgical techniques of implant rotation, soft tissue
balancing and alignment.
Improving patients’ health or preventing its decline is of
course the major aim of any health care intervention,
and an important feature of modern health service
provision is the ability to measure such improvements
via validated tools.
In 2006, the U.S. Food & Drug Administration stated,“The
use of PRO instruments is part of a general movement
toward the idea that the patient, properly queried, is the
best source of information about how he or she feels.”12
It is important to recognize that the objective of PROMs is
to measure patients’ perceptions of their health, not their
experiences of health care delivery. Health care delivery
surveys measure patients’ experience of, or satisfaction
with, the care that they receive, including such factors as
whether they are treated with respect and compassion,
they have a comfortable environment for their care,
and they are provided with enough information about
their care. While these are important quality measures in
their own right, and while PROMs may be influenced by
patients’ experience of health care delivery, the two are
separate and measured in different ways.
PROMs are validated questionnaires that ask patients to
assess their own health and their quality of life as a result
of their health, usually capturing changes over time –
especially pre- and post-intervention at specified time
points. The responses to the different questions are usually
processed to generate either a “profile” of health – a
combined summary of the responses that gives a picture of
health in different dimensions – or a number that gives an
overall score. There are many thousands of such PROMs
1.4 Measuring Patient Reported Outcomes
While objective physiological and functional measures
can tell us much about the effectiveness of health care
interventions, an important test is patients’ perceptions
of their health. This has led to the establishment of
Patient Reported Outcome Measures (PROMs) as a
key factor in evaluating the effectiveness and cost-
effectiveness of health care technologies.13
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 6 of 20
available in multiple languages. Some of them are related
to a particular condition, treatment or symptom, and are
generally known as condition-specific or disease-specific
measures. Others are intended to be applicable,
in principle, to any condition and are usually called
generic measures.
The specialty of orthopaedics has been a leader in the
development and adoption of PROMs. The main generic
measures used to measure a person’s state of health with
knee problems are the EQ-5D and the SF-36.22,63 As
well as generating a “profile” in five and 12 dimensions
respectively, these enable a score to be calculated that
can be interpreted as the value of a patient’s health state
relative to best and worst possible health states.
The most widely used condition-specific PROMs for knee
osteoarthritis are the Oxford Knee Score (OKS)44 and the
Knee injury and Osteoarthritis Outcome Score (KOOS).56
The OKS has 12 questions, each of which generates a
score between zero and four. These are added together
to give an overall score between zero, meaning as severe
knee arthritis as possible, to 48, representing no knee
problems at all. KOOS by contrast does not calculate an
overall score, but generates scores from zero (extreme
symptoms) to 100 (no symptoms) in five subscales: pain,
other symptoms, daily living, sport and recreation, and
knee related quality of life. It is an extension of another
widely used measure, the Western Ontario and McMaster
University Osteoarthritis Index (WOMAC),16 which is
applicable to both hip and knee problems; a WOMAC
score can be derived from the KOOS questionnaire.
PKIP has four subscales (Confidence, Stability, Modify
Activities and Satisfaction), each of which generates
a score from zero to 10, where higher scores indicate
better knee function, and an overall score which ranges
from zero to 100. This has been shown in initial studies
to perform well in terms of key psychometric criteria
such as reliability, validity and responsiveness, which may
help discriminate the impact of different implant designs
and surgical techniques.25 It is important to note that
“satisfaction” here refers to the implant, which enables
a proper assessment of the procedure itself, rather than
more general patient satisfaction with the care that they
receive, which will be influenced by the environment in
which care is provided.
PROMs have many uses, but assessing the results of
a health care intervention usually requires changes in
health to assess outcome measures. Typically, this requires
patients to complete PROMs questionnaires both before
and after the intervention. For TKA, this may be referred
to as pre-operative and post-operative health states, or
baseline and follow-up. It is important to ensure that these
assessments are carried out at times that will properly
reflect the period over which improvements will be realized
and that there are further assessments for possible longer
term effects. For example, a common post-operative
PROMs assessment for TKA is six months, but, in some
cases, the follow-up will also be at one year or longer,
enabling a profile of changes over time to be assessed.
PROMs are widely used in clinical trials, but are also
increasingly used routinely in practice, for example in
joint registries. Since 2009 the National Health Service
(NHS) in England has required all health care providers,
both publicly and privately owned, to collect specified
PROMs for all patients funded by the NHS.13 PROMs are
collected before and after undergoing surgery for four
elective procedures, including hip and knee replacements.
Around 250,000 patients are invited each year to complete
questionnaires, which include both the EQ-5D and
the OKS, and the response rates are good: on average
95% of knee replacement patients complete the pre-
operative and 75% the post-operative questionnaire. In
New Zealand, TKA patients are also invited to complete
OKS questionnaires and their data have established that
each one-unit drop in the OKS at six months predicts a
9.9% increase in revision rates over two years,57 which
demonstrates the importance of PROMs data from a wider
health care perspective.
The English PROMs data are especially useful for examining
the overall effects of TKA in real world practice, rather
than in the experimental conditions required by clinical
trials. Averaging over all NHS providers in England in 2014-
2015,8 93.2% of knee replacement patients had improved
health specific to their condition, measured by the OKS,
and 80.5% had improved health more generally, measured
by the EQ-5D. The average PROMs scores for primary
knee replacement patients pre-operatively were 19/48
according to the OKS and 0.425 for the EQ-5D index.
At six months post-operative, primary knee replacement
patients reported OKS scores of 35 and EQ-5D index scores
of 0.739. The measured outcome of TKAs in the NHS
in England was therefore an average improvement per
patient of 16 in the OKS and 0.315 in the EQ-5D index.
The Patient’s Knee Implant Performance (PKIP) is a
relatively newer condition-specific PROM that has been
specifically developed to assess the functional status of
a patient’s knee from their own perspective, before and
after TKA.40 It was developed to address gaps in
other common PROMs by assessing a patient’s
satisfaction with their implant, which represents an
innovative approach to better understand the nuances
involved in outcomes for TKA patients.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 7 of 20
Within the hospital, there are fixed costs, and costs
associated with the surgical procedure itself, including
operating room staff, physicians, implants, and disposable
items to perform the procedure. There are also costs of
providing nursing care and therapy after surgery. Upon
discharge, patients usually continue rehabilitation that
can last for weeks or months, with the attendant costs
of ongoing treatments. Some of these patients require
placement in skilled nursing facilities or rehabilitation units.
Post discharge costs are a significant portion (up to 50%)7
of the overall episode of care. Bozic et al. found that up
to 35% of the episodic costs were related to care after
discharge.20 Unpredictable events such as complications
and readmissions can also add considerably to the
episode of care costs.
In many countries, a global evaluation of the episode of
care is a major focus. The mandatory bundled payment
initiatives in the U.S. are one example. These involve a 90-
day window of time where all associated costs are included
with the procedure. This process creates incentives for
hospital systems to better manage patient care following
total joint replacement procedures. Hospitals must manage
the total costs for a given procedure, including post-acute
care. Any complications and/or readmissions will greatly
increase chances of the hospital exceeding this fixed price
and therefore owing a penalty payment back to Medicare
(CMS). This puts additional risk on the providing hospital
but allows the payor, e.g., Medicare, better forecasting of
the cost of care to a given population.
In the NHS in England, health care providers are
reimbursed by health care commissioners under the
“Payment by Results” system. Each patient treated is
assigned to a Healthcare Resource Group (HRG), similar
to the Diagnosis Related Group (DRG) classification found
in the U.S. and other countries’ health care systems, for
which there is a “tariff” payment covering all inpatient
services. Knee replacements are one of a few procedures
that are reimbursed using a “Best Practice Tariff,” which
offers a much larger payment to providers who provide a
high standard of performance, such as minimum average
improvements in PROMs scores and good data provision,
including rates of registration with the National Joint
Registry (NJR). They also attract a special additional tariff
for post discharge rehabilitation care that follows a defined
clinical pathway, including specified numbers of nurse,
physiotherapist and occupational therapy appointments,
and consultant-led clinic visits.
With the growing population of patients needing TKAs,
it is critically important to minimize the total cost of this
procedure, subject to maintaining quality of care.
Globally, each element of cost for the episode of care
is under review for potential cost savings by hospital
systems. Length of hospital stay and post-discharge
disposition are two areas under review by payors and
providers. Decreasing length of stay clearly reduces the
cost of inpatient care and can be done safely, with many
patients now being discharged directly home within 48
hours and, in some cases, on the day of surgery.37 The
use of skilled nursing and rehabilitation units has also
been identified as high cost items associated with 35%20
-50%7 of the episode of care cost, and efforts to minimize
the use of these facilities are underway. The benefits of
post-discharge therapy (either in home or in outpatient)
are under review and at least one paper suggests it may be
unnecessary following TKA.23 Further study of this topic
will likely be forthcoming.
1.5 The Economics of Total Knee Arthroplasty
PROMs that, like the EQ-5D and the SF-36, generate a
single score representing the value of a health state can
be used to calculate Quality Adjusted Life Years (QALYs).
QALYs are a measure that combine length and health-
related quality of life into a single score. For example, a
person who enjoys a year without any health problems
would generate one QALY; someone who had a quality
of life value of 80% would have 0.8 QALYs for that year.
If there were an intervention that would cure the second
person’s health problem, they would gain 0.2 QALYs each
year. If that improvement lasted for 10 years, they would
gain two QALYs, the equivalent of two additional life years
with no health problems.
For example, the reported gain from TKA of 0.315 in the
EQ-5D index in the NHS in England suggests that if the
improvement is maintained over 10 years, there is a gain
of over three QALYs per patient. QALYs, combined with
costs, provide the building blocks to the formal economic
analysis of a given intervention used by organizations
like the National Institute for Health and Care Excellence
(NICE), in England.
QALYs are a particularly useful measure to ensure that
procedures, like TKA, that do more to improve people’s
quality of life than reduce mortality are judged fairly in
comparison with procedures that extend life expectancy.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 8 of 20
TKA is widely accepted as a highly cost effective means
of generating improvements in patients’ quality of life.
The cost of a health care intervention can be measured
by comparison with the next best alternative way of
managing the condition that it deals with. This gives an
estimate of the additional or ”incremental” cost of the
intervention. The cost is compared with the improvements
in patient outcomes, measured as gains in QALYS, that the
intervention generates compared with the best alternative
treatment option. Dividing additional costs by QALY gains
gives a cost-effectiveness ratio, an estimate of the cost of
generating an additional QALY using that intervention.
The inverse of this, Porter’s “Value” measure, shows the
amount of improved outcome generated by each dollar
spent on the intervention.52
In the U.S., Losina et al. analyzed Medicare data using a
modelling approach comparing lifetime costs and quality
of life for patients aged 65 and over who had end-stage
knee osteoarthritis.42 They estimated a cost-effectiveness
ratio of $18,300 per QALY gained, although for high-risk
patients this was much higher, at $28,100. The cost of
TKA and post-operative quality of life both affected the
level of cost-effectiveness achieved, but no other patient-
or procedure-related factors such as revision rates were
important to this outcome.
In the U.K., Dakin et al. analyzed data from a large,
randomized trial of different knee prostheses measuring
both costs and quality of life.27 They estimated an average
cost-effectiveness ratio of £5,623 per QALY gained, using
conservative assumptions about the extent of changes
in costs and quality of life due to TKA. This ratio is well
below £20,000 per QALY gained, which is a threshold
defined by NICE below which pharmaceutical and other
interventions are, without further qualification, accepted
for funding. Moreover, although patients’ age, gender and
baseline severity, as measured by ASA (American Society
of Anesthesiologists) grade and OKS score, impacted on
cost-effectiveness, there are very few eligible patients
for whom the cost per QALY gained exceeds the NICE
threshold. Although TKA costs more for patients who had
worse pre-operative health states, the greater QALY gains
that they achieved meant that it was more cost-effective
than for patients with only moderate symptoms. This study
also examined the impact of different assumptions about
factors that affect cost-effectiveness. This included the
length of stay in hospital following
the procedure, confirming that shorter hospital stays
would improve cost-effectiveness.
In 2016, Pennington et al. compared the relative cost-
effectiveness of different implants, using data from the
U.K. National Joint Registry.48 In identifying the most cost-
effective option, they found that the main determinant
was differences between the implants in the post-
operative quality of life that they generate for patients.
For the range of implants covered, factors such as their
cost and revision rates were not so important – improving
patients’ quality of life was found to be key. Moreover,
the quality of life differences between the implants were
relatively small, further emphasizing the importance of this
as a determinant of cost-effectiveness. What may appear
to be small changes in quality of life at a single point
of time can translate into large changes in QALYs if the
improvement is sustained over a long period of time. This
study covered TKAs implanted between August 2008 and
July 2012, since then, new implants have been introduced
which may affect the conclusions.
Additional benefits may be applicable to TKA patients
whose ability to work is affected by knee problems. TKA
will enable such individuals to continue working, which
is beneficial to society. These are known as indirect costs,
by contrast to the direct costs of health care that arise
from either TKA or its alternatives. Ruiz et al. estimated
the total additional direct costs of TKA over the lifetime
of a patient in the U.S. to be on average $20,635 in 2009
dollars, offset by a reduction in lifetime indirect costs of
$39,565.58 TKA therefore generates an average societal
savings of $18,930 per patient. Most of these savings
directly benefit patients by increasing their employment
potential and earnings, but there is a wider benefit to
society of increased production and reduced disability
payments.
A number of scientific studies in countries including
the U.S., U.K., Finland and Spain, have concluded that
TKA is the most cost-effective means of managing
osteoarthritis, according to standards that are widely
accepted in developed countries.27,39,42,45,48,54,55
The evidence suggesting that TKA is highly
cost-effective in terms of improvements to patients’
quality of life applies to all relevant age groups.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 9 of 20
National professional associations for orthopaedic surgeons
and the policy bodies of national health systems emphasize
that the decision to refer a patient for TKA should only
depend on individual clinical judgements that a patient will
benefit from treatment. In particular, decisions should not
be made using “scoring tools” that identify which patients
are eligible for referral. In the U.K., for example, NICE has
issued quality guidelines that instruct health professionals,
health care providers and health care commissioners not to
use such scoring systems.10 These guidelines also attempt
to drive consistency in equity of care provided across the
NHS in the U.K.
Sometimes, other eligibility criteria are used that are
equally arbitrary and are opposed by national bodies.
These include a requirement that patients lose weight or
stop smoking before they can be referred for TKA; that
patients must be experiencing extreme pain or disability;
and that patients must be under a specified age. None of
these are regarded as justifiable if they do not adversely
affect the likelihood of a patient benefiting from surgery.
The NICE guidelines state if there are to be referral
thresholds, these should not be based on such criteria,
or scoring tools, but on discussions between patient
representatives, referring clinicians and surgeons.
In the U.S., global payment models reward hospitals that
show decreased complications and readmissions following
TKA. These payment models could potentially create an
adverse incentive to screen patients and forgo surgery
on individuals that have a higher risk of a complication
or readmission. The unintended consequences of these
policies in the aforementioned major TKA markets, which
are aimed at minimizing short-term costs with approaches
to rationing, may lead to problems in the access to care
for many patients who would otherwise benefit from
this procedure. Potentially, such approaches could lead to
increased overall health care direct and indirect costs
in the longer term.
1.6 Barriers to Referral for Treatment
In an effort to improve the performance of contemporary
TKA, DePuy Synthes Companies designed the ATTUNE
Knee System with university researchers and a team of
35 experienced total knee surgeons from around the
world. The team set about studying surgical workflow,
implant sizing, kinematics, patellar tracking, ligament
balancing and instrumentation issues in-depth, and new
concepts were developed and tested in laboratories
around the world. This collaboration led to over 30
peer reviewed publications, more than 60 patents and
to the development of new methods to address clinical
problems through implant and instrument design and
manufacturing.
The ATTUNE Knee is a highly versatile implant system
with options for bearing design, kinematics, patellar design
and ligament balancing techniques. The instrument system
incorporates the use of low weight composite materials
designed to allow precise bone preparation, implant
balancing and implant insertion. Primary ATTUNE Knee
implants have been implanted since 2011, with
wide availability since 2013, and are used in countries
around the world.
Additional information about the ongoing in vivo studies is
available online (see Appendix Table 1).
Factors that can influence TKA outcomes include patient
demographics, implant design and the instruments that
help surgeons implant total knee devices with greater
precision. Standard surgical instruments and tools used
to insert total knee implants have proven more than
adequate to perform high quality TKAs in most surgeons’
hands. However, there is variability in surgeon experience
and skills in performing this complex operation. Surgical
efficiency can lower aggregate costs, improve outcomes
by reducing complications, and improve operating room
productivity. One study conducted at Duke University in
the U.S. showed that a surgical team dedicated to total
2 THE ATTUNE KNEE SYSTEM
2.1 Improving the Performance of Total Knee Arthroplasty
The evidence strategy for the ATTUNE Knee represents
the largest clinical program in DePuy Synthes’ history and
has been designed to extensively focus on measuring the
extent to which the ATTUNE Knee is meeting the unmet
needs of TKA patients and other key stakeholders.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System

Page 10 of 20
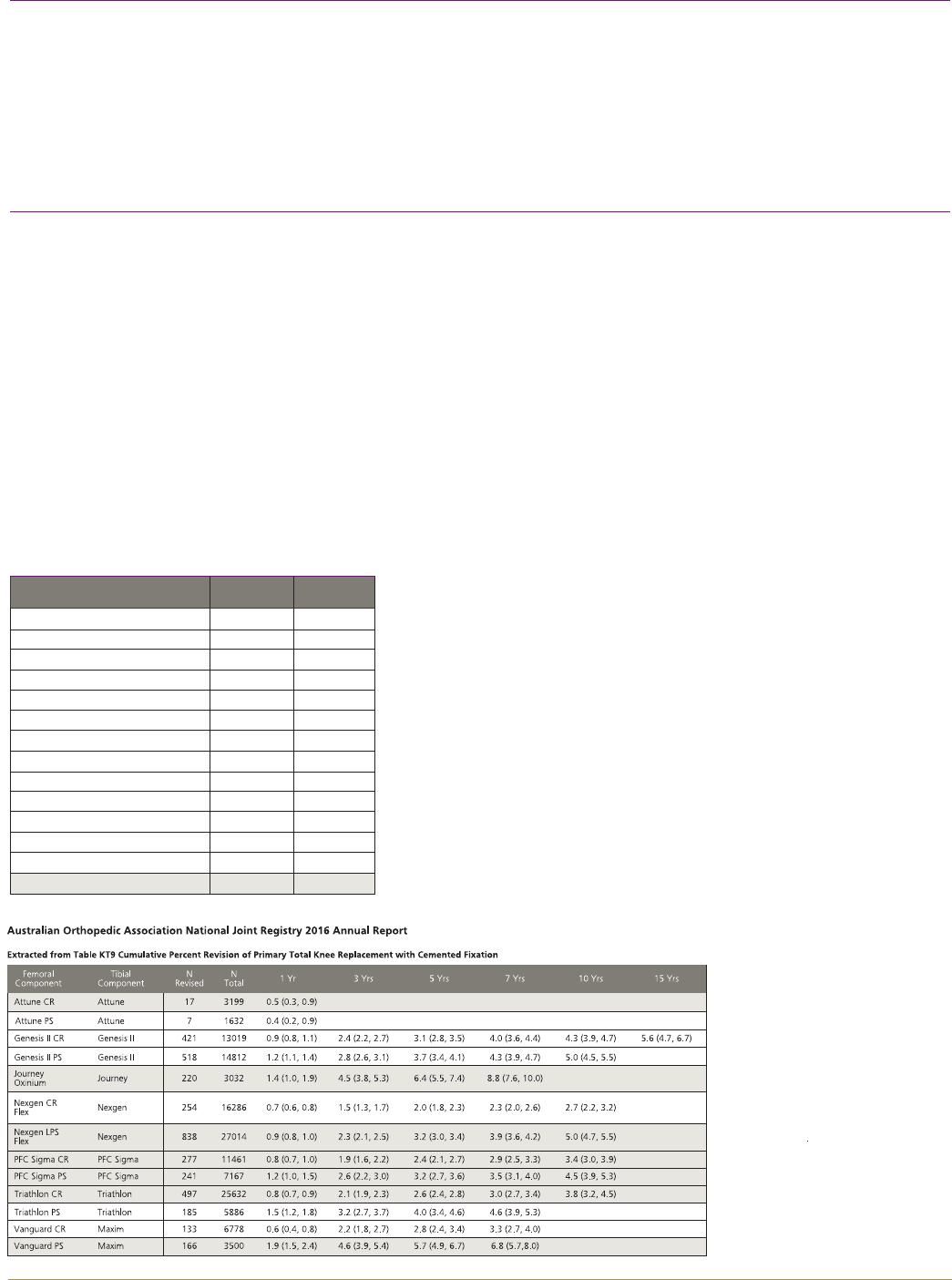
National total joint registries offer the opportunity to
track implant-specific performance by means of patient
reported outcomes, reoperations, and revisions. Sweden,
New Zealand, Australia and the United Kingdom are some
of the countries that have national registries. Per the
2016 published report from the National Joint Registry
for England, Wales, Northern Ireland and the Isle of
Man (NJR),3 the three-year cumulative percent revision
rate for over 4,000 patients receiving the ATTUNE Knee
was 1.39% (NJR Table 3.28), which compares favorably
to the class of cemented implants, which had a 1.50%
cumulative percentage probability of revision (NJR Table
3.24). ATTUNE Knee survivorship data is also available
in the 2016 published report from the National Joint
Replacement Registry from Australia (AOANJRR).5 Per the
2016 AOANJRR, in which 4,831 ATTUNE Knees are being
tracked, the ATTUNE Knee estimated cumulative percent
revision was 0.5% (ATTUNE Cruciate Retaining), 0.4%
(ATTUNE Posterior Stabilized) at one year.6 This compares
favorably to the overall class of cemented total knee
arthroplasty (TKA) at one year, which has an estimated
cumulative percent revision of 1.0% (Tables KT9 and
KT22).5
While the science behind implant design has improved,
the evidence of improvement lies in patient perception and
function. Performance measures such as pain relief and
improved function are issues patients can relate to their
knee through the various measurement tools previously
described. With these tools, knee function and pain
can be assessed pre- and post-operatively. Furthermore,
improvements can be tracked to compare outcomes
between different hospitals, surgeons, and implants.
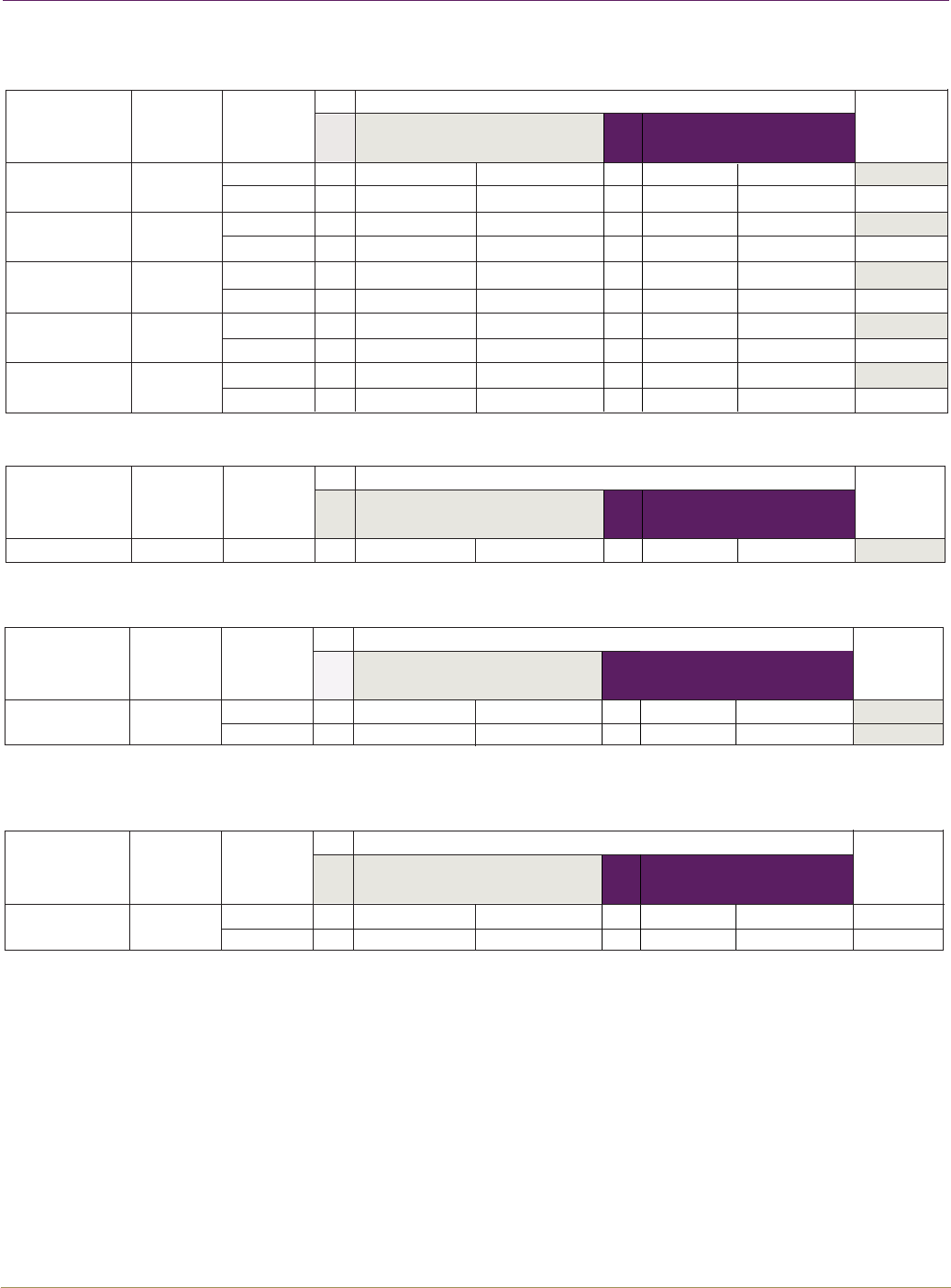
As described on the next page, a number of independent
single-center studies and company-sponsored multi-
center studies of the ATTUNE Knee have reported an
improvement in patient outcomes compared with
other knee implants. A prospective multi-center study
by Hamilton et al. compared 926 patients receiving an
ATTUNE Knee with a similar group of 845 patients who
received knee implants of other designs.31 Knee function
and patient satisfaction scores were collected using four
PROMs: KOOS, OKS, PKIP, and EQ-5D. Figure 1 shows that
at one-year post-operative, the ATTUNE Knee patients had
statistically better scores in most of these.
2.2 Total Knee Arthroplasty Outcomes Using the ATTUNE Knee
joint replacement improved the performance of those
procedures, improved on time starts, and increased
the number of cases by 29%.14 Attempts to improve
performance through professional education and training
are ongoing to ensure consistency in surgical process.
More training may be useful, potentially focusing on
surgeons who perform fewer cases than the academics
who typically publish.
If the performance of a higher quality knee reconstruction
led to shorter surgery time, shorter length of stay in
hospital, reduced utilization of skilled nursing facilities,
reduced time of recovery, higher patient satisfaction, fewer
complications and revisions, and lower overall costs of
care, it would be a significant improvement to the current
standard of care, which would benefit all stakeholders.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 11 of 20
ATTUNE Knee
N
Figure 1. Patient reported outcome measures including condition specific (KOOS, PKIP, OKS) and generic (EQ5D) comparing the ATTUNE Knee and other knee systems,
p-values less than 0.01 are highlighted and considered statistically significant.31
KOOS
PKIP
Scale
Scale
Timing
Timing
(Covariate
Adjusted)
p-value for
Means
(Covariate
Adjusted)
p-value for
Means
N
N
NN
Leading Knee Brands
Leading Knee Brands
ATTUNE Knee
ATTUNE Knee
0-100
0-100
Min. 1yr.
Min. 1yr.
<0.0001
88.1 ± 13.5
74.4 ± 18.0
(38.4 ± 19.2)
(45.7 ± 21.5)
751
746
746
729
85.1 ± 15.7
71.3 ± 19.1
(35.0 ± 20.0)
(43.6 ± 21.9)
674 363
752 746
674 362
752 746
674 363
744 727
655 349
750 746
674 363
Unadjusted Mean ± SD, (Change from Pre-op Baseline)
Unadjusted Mean ± SD, (Change from Pre-op Baseline)
Min. 2yr. 0.0945
90.0 ± 13.587.6 ± 14.9 (37.0 ± 20.6) (37.3 ± 19.0)
Min. 1yr. 0.0001
87.2 ± 14.6
89.4 ± 14.5
84.6 ± 16.9 (38.6 ± 20.5) (42.8 ± 19.4)
Min. 2yr. 0.1599
87.6 ± 15.6 (41.1 ± 20.7) (42.9 ± 19.0)
Min. 1yr. 0.0016
80.9 ± 14.678.5 ± 16.9 (30.4 ± 22.5) (33.6 ± 21.2)
Min. 2yr. 0.1552
84.1 ± 14.982.5 ± 15.5 (33.8 ± 21.8) (35.6 ± 20.6)
Min. 1yr. 0.0013
59.9 ± 28.2
55.5 ± 30.4 (37.1 ± 31.1) (42.3 ± 29.7)
Min. 2yr. 0.2081
63.8 ± 28.4
61.2 ± 29.3 (42.9 ± 31.5) (45.1 ± 28.1)
Min. 1yr. 0.0034
73.2 ± 21.9
70.0 ± 23.3 (45.0 ± 25.8) (48.7 ± 25.6)
Min. 2yr. 0.0694
78.3 ± 21.2
74.9 ± 22.9 (49.7 ± 26.3) (52.2 ± 24.8)
0-100
0-100
0-100
0-100
Activities of
Daily Living
Overall
Pain
Symptoms
Function in Sport/
Recreation
Quality of
Life
EQ5D-3L
OKS
Scale
Scale
Timing
Timing
(Covariate
Adjusted)
p-value for
Means
(Covariate
Adjusted)
p-value for
Means
N
NN
Leading Knee Brands
Leading Knee Brands
-1-1
0-48
Min. 1yr.
Min. 1yr.
0.0109
0.9 ± 0.2
41.4 ± 6.4
(0.3 ± 0.3)
(18.4 ± 8.6)
746
750
746
742
0.8 ± 0.2
40.2 ± 7.4
(0.3 ± 0.3)
(17.1 ± 8.8)
672
672
362
362
Unadjusted Mean ± SD, (Change from Pre-op Baseline)
Unadjusted Mean ± SD, (Change from Pre-op Baseline)
Min. 2yr.
Min. 2yr.
0.7594
0.9 ± 0.2
42.3 ± 6.4
0.9 ± 0.2
41.4 ± 6.8
(0.3 ± 0.3)
(18.1 ± 9.1)
(0.3 ± 0.3)
(18.0 ± 8.9)
Overall
Score
Overall
Score
0.0032
ATTUNE Knee
0.0002
0.2033
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System

Page 12 of 20
Another presentation combined data from the Hamilton,
et al. study with an additional study on ATTUNE TKAs,
cumulatively totalling 2,370 ATTUNE Knees and 845 knees
from other leading knee systems performed
by surgeons from around the world. This analysis
assessed the outcomes of early “learning curve” defined
as the first 10 ATTUNE Knee cases, compared to
subsequent procedures. Average operating time improved
after the first 10 cases. Additionally, when the first 10
ATTUNE TKAs by an individual surgeon (learning curve
cases) were compared to later ATTUNE TKA cases,
there was no impact on the rate of intra-operative
complications, nor was there an impact on PROMs. These
results may be useful evidence for institutions when
considering adoption of a new product.21
Patellofemoral complications are one of the problems
encountered in TKA patients. Some patients may hear
noise as a grinding or clunking sound when moving their
knee from extension to flexion. This situation is caused by
the entrapment of soft tissue between the components
and can be associated with pain and impair certain
activities. Symptoms usually begin within 12 months
of surgery and have been reported in up to 18% of
patients after TKA.26 Patellofemoral complications have
been a cause of revision surgery in approximately 6% to
11.6%5,28,51 of revisions. Furthermore, patellofemoral
complications, especially crepitus and clunk, are more
common in posterior stabilized (PS) implants.
1) In a prospective study by Toomey et al.,62 patellofemoral
symptoms were specifically evaluated by patients and
investigators. At one and two years, the cumulative
incidence of symptomatic crepitus in patients with ATTUNE
PS Knee implants was significantly less than that of the
non-ATTUNE Knees, primarily the SIGMA PS Knee design,
(0.78% versus 2.53% at one year, and 1.21% versus
3.14% at two years). Furthermore, the risk of patellar
symptoms increased fourfold for patients achieving more
than 110 degrees of flexion with non-ATTUNE Knee
systems, while there was no increased risk in the ATTUNE
Knee patients with over 110 degrees of knee flexion.2
2) Martin et al.43 reported a single institution study
that compared the incidence of crepitus for subjects
implanted with the ATTUNE PS Total Knee (N=728) and
subjects implanted the SIGMA PS Total Knee (N=1165).
The results showed significantly less symptomatic
patellofemoral crepitus at both minimum one and
minimum two years post-operatively for the ATTUNE
Knee versus the SIGMA Knee design (0.14 versus 2.7%,
p<0.001 at minimum one year and 0.33% versus 2.3%,
p<0.001 at minimum two years).
3) Ranawat et al.53 compared 100 each of the ATTUNE
PS Knee with the SIGMA PS Knee. While not statistically
significant, the incidence of symptomatic crepitus at two
years was 1.0% for the ATTUNE Knee cohort compared
to 4.1% for the SIGMA Knee cohort. Their results also
demonstrated a statistically significant reduction in anterior
knee pain at two years post-operative (12.5% for the
ATTUNE Knee cohort versus 25.8% for the SIGMA Knee
cohort, p =0.02).
4) Another study by Indelli et al.32 also compared 100
patients each with the ATTUNE Fixed Bearing Knee and the
SIGMA Fixed Bearing PS Knee. The ATTUNE Knee group
had significantly less anterior knee pain (2% versus 9%),
higher flexion (123 degrees versus 115 degrees, p=0.009)
and more patients with over 130 degrees of flexion (37%
versus 16%, p=0.0008). Two patients in the SIGMA Knee
group required surgery for patellar clunk and there were
no revisions in the ATTUNE Knee cohort. The ATTUNE Knee
patients experienced a statistically significant (p=0.007)
reduction in the incidence of symptomatic crepitus (1%)
compared to the SIGMA Knee patients (5%).
The ATTUNE Knee was designed to improve the
patellofemoral articulation. The trochlear design of
the PS implant has a reduced thickness of the anterior
implant flange, and an altered box configuration that was
specifically designed to maintain patellar contact through
deep flexion and avoid entrapment of soft tissue as the
patellar implant slides over the box. The native patella has
a dome whose apex is closer to the medial edge of the
bone and, in a similar fashion, the ATTUNE Knee patellar
implants restore the dome to a medial position on the
patella. The patellar implant is available in a medialized
dome or medialized anatomic configuration. While each
is designed to restore the dome of the patella to the
original position on the patella, the anatomic version has
facets which can increase the contact area of the patellar
implant on the femoral component throughout the range
of motion. In addition to the above clinical studies which
demonstrated fewer patellofemoral complications, a
comparative, kinematic study in the U.S. of both patellar
component designs showed that study subjects with
medialized anatomic geometry achieved greater patellar
flexion (the angular orientation of the patella relative to
Four independent studies32,43,53,62 have
demonstrated fewer patellofemoral complications
and one biplanar fluoroscopy study15 demonstrated
improved patellofemoral biomechanics in the ATTUNE
Knee, compared to other knee systems, primarily
the well-performing SIGMA® Knee. This data
suggests that certain design features, including the
modified trochlear groove and corresponding patellar
articulation, may lead to fewer reoperations for
patellar symptoms in ATTUNE Knee patients compared
to primarily SIGMA Knee patients.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 13 of 20
the femur) than those with the medialized dome during
lunge activity, and demonstrated patellofemoral kinematics
closer to that of the native knee.15 The anatomic patellar
design also has more polyethylene proximally which may
prevent ingrowth of the fibrous tissue meniscus that
eventually encircles most domed implants.
Recovery from TKA is a process that takes time. Most
patients will experience improvement in knee function
for up to 12 months following surgery; however, the
most rapid phase of this recovery is in the first six weeks,
when about 80% of recovery has occurred. This acute
recovery phase is mainly related to the soft tissue healing
and remodelling that occurs following the procedure.
Recovery rates vary between patients but, in general,
TKA patients will continue to have startup stiffness,
discomfort, difficulty sleeping through the night, and
weakness going up and down stairs for six to 12 weeks.
Efforts to enhance early recovery from TKA have included
pre-operative exercises, less invasive surgical approaches,
aggressive physical therapy pathways, pain management
protocols and educational efforts to help prepare patients
for the recovery phase of their treatment. While some of
these have been shown to reduce length of hospital stay
and made the recovery more tolerable for many patients,
surgical pathways and implant design may also contribute
to the speed of recovery.
While length of stay, rehabilitation time, and return of
function are multifactorial, implant design and surgical
technique may be contributing factors. The ATTUNE Knee
was designed to allow surgeons to provide stability and
anatomical reconstruction of the arthritic knee. With 14
primary femoral sizes, 10 tibial sizes, and one millimeter
increments in polyethylene thickness, the options to size
and balance the knee have been enhanced with the
ATTUNE Knee from other available systems. Improving
component stability was one way the designing surgeons
felt they could impact function with activities such as
climbing and descending stairs. Another effect of this
component stability may be enhanced post-operative
recovery. While patient reported outcomes up to two years
have favored the ATTUNE Knee versus other leading knee
systems, some early recovery data also lends support.
Specifically, a U.S. claims database study29 compared
1,178 ATTUNE Knee patients to 5,707 Stryker Triathlon®
knee patients implanted in 38 hospital systems that used
both products.
Sensitivity analyses in this study indicated that these effects
could not be explained by patient factors including age,
insurance or marital status.
A study from Germany on the early (six month) clinical
results with 55 prospective ATTUNE Knee patients
showed significant improvement in range of motion (112
degrees pre-op to 123 degrees post-op; p<.001) and
improved coronal stability throughout the range of motion
compared to pre-operative status.50 The stability tests
were carried out in a standardized fashion at zero, 30,
and 90 degrees of flexion. The study authors felt that the
improved kinematics observed in these patients were a
result of the femoral component design and the ability to
fine-tune the knee balance with one millimeter increments
in polyethylene thickness. An in-vivo fluoroscopic analysis
(video x-rays which allow researchers to study the relative
motion of the components during activities) of the ATTUNE
Knee gradually changing radius (ATTUNE GRADIUS™
Curve) compared to the SIGMA Knee multi-radius design
showed improved kinematic function and femoral roll-
back with the ATTUNE Knee.49 Both of these studies,
which focus on stability, are consistent with experimental
data performed by finite element analysis and previous
experimental laboratory research.24
The results showed a significant difference in the
length of hospital stay and use of extended care
facilities. The adjusted mean length of stay (LOS) for
ATTUNE Knee patients in this dataset was 0.19 days
shorter than for the Triathlon® patients (2.94 vs. 3.13;
p<0.001). The mean adjusted proportion of ATTUNE
Knee patients in this dataset who were discharged to
a skilled nursing facility (SNF) was 24.3%, compared
to 34.3% of the Triathlon® patients. The adjusted
odds of ATTUNE Knee patients in this dataset being
discharged to a SNF were 39% lower than for
the Triathlon® patients (Odds Ratio= 0.61; 95%
Confidence Interval: 0.50-0.75; p<.001).
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 14 of 20
Although a full cost and benefit profile for the ATTUNE
Knee does not currently exist, there is emerging evidence
that evaluates the economic implications of the ATTUNE
Knee System.
In a claims database evaluation of data from 2013-2014
of the ATTUNE Knee System versus the Triathlon® knee
system, within a sample of U.S. hospitals and surgeons,
the patients in the dataset who received the ATTUNE Knee
had a shorter length of stay; the length of stay for the
ATTUNE Knee patients was statistically significantly lower
than for Triathlon® patients, by an average 0.19 days
adjusted for case-mix.29 These results may be meaningful
in systems that are interested in reducing length of stay
and post-acute care. The ATTUNE Knee System could be
part of the care pathway that is aligned with the goals
of the healthcare system. Although small expressed in
per patient terms, this may be important where there is
a larger volume of patients, and, in the U.K. in particular,
lower length of stay has been found to reduce cost
sufficiently to improve the cost-effectiveness ratio.27 The
same study found that the adjusted odds of ATTUNE
Knee patients in the dataset being discharged to a skilled
nursing facility were 39% lower than for the Triathlon®
patients. Because such facilities are comparatively very
expensive, this may also improve cost-effectiveness.
Further research in this area would be beneficial.
Although revision rates and secondary procedures have
not been shown to impact on cost-effectiveness, the lower
reported patellofemoral complications32,43,53,62 that often
lead to reoperations, and the low revision rates for the
ATTUNE Knee reported in National Joint Registries5,9,11
suggests a source of reduction in overall costs.
Additionally, some studies indicate that there is evidence
of improved health related quality of life, as measured
by validated PROMs questionnaires, using the ATTUNE
Knee. For example, the study by Hamilton et al.31 showed
that ATTUNE Knee patients had consistently improved
one- year scores on a broad range of PROMs compared
with those patients who had other knee products,
although not all differences were statistically significant.
These improvements appear to be modest, which is to be
expected as TKAs in general have been shown to have a
positive effect on patients’ quality of life.60 However, as
the cost-effectiveness modelling evidence described earlier
shows, even a small improvement significantly raises cost-
effectiveness favorability when translated into gains in
Quality Adjusted Life Years.
These benefits have been observed in real world settings,
where many variables that effect LOS and other outcomes
that impact the value to payors and other stakeholders.
Advancements in the provision of TKA have reduced
the burden on patients with osteoarthritis of the knee
and technological advancements have led to improved
outcomes over time. The ATTUNE Knee has been
available for a number of years in a large number of
countries and was designed to improve patient outcomes
through advancements in implant design and surgical
workflow. The current data reviewed in this paper has
demonstrated improved outcomes compared to other
leading knee systems. Based on registry data collected
over time in multiple countries, the ATTUNE Knee
performs well in terms of implant survivorship to three
years; registry data will continue to be reviewed. For
the patient, this may mean enhanced recovery from
the surgical procedure (leading to earlier discharge,
and reduced follow-up requirements in some cases), an
earlier and higher return of knee function, and fewer
reoperations from procedure related complications
such as patellofemoral crepitation. The improvements
in function documented thus far include improved pain
level, activities of daily living, function in sports and
recreation, and quality of life after one year. For hospital
systems receiving bundled payments, decreased length
of stay and fewer transfers to extended care facilities
can reduce the cost of episodic care. These financial
savings could also benefit hospitals under the Healthcare
Resource Group (HRG)/Diagnosis Related Group (DRG)
reimbursement systems. Earlier discharge could assist
with capacity constraints, particularly where there are
extensive waiting lists for a wide variety of procedures.
Finally, for society more generally, the costs associated
with total knee arthroplasty may be lowered, which
could allow for more total knee patients to be treated or
scarce resources used to generate benefits in other areas.
Based on available data, the ATTUNE Knee appears to
be advancing outcomes for patients and creating value
for clinicians, providers and payors in a challenging and
dynamic healthcare environment. The DePuy Synthes
evidence program will continue to monitor the clinical
and economic performance of the ATTUNE Knee as more
data and longer term follow-up data becomes available.
2.3 Economic Evaluation of the ATTUNE Knee
CONCLUSIONS
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 15 of 20
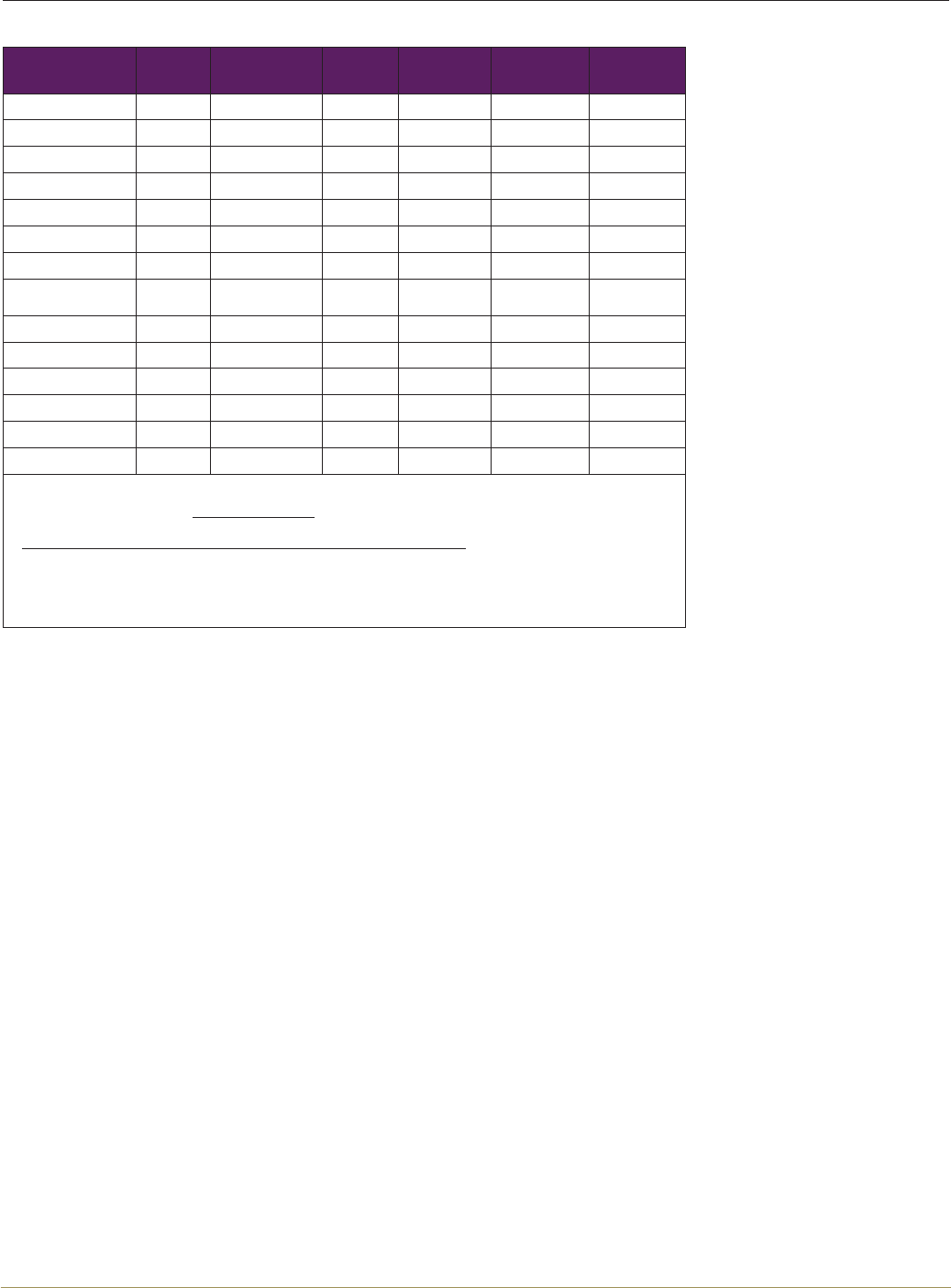
Study registration
number
Type of
Study
Functional
Outcomes Fixation Survivorship Safety Health
Economics
NCT01497730 C 1 X X
NCT01746524 C 1 X X
NCT01754363 C X X X X
NCT02339610 C X 1 X
NCT02251535 IIS 1
NCT02358434 IIS 1
NCT02323386 IIS 1
NCT02204748
NCT02613338 IIS 1
NCT02532933 IIS 1
UMIN000020380 IIS 1
NCT02177227 IIS 1 X
NCT02256098 IIS 1
NCT02103504 IIS 1
NCT02791477 Indep 1
Legend
• NCT#: Study is registered on www.clinicaltrials.gov
• UMIN: Study is registered on UMIN-Clinical Trials Registry,
www.upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000023536
• 1= primary objective
• C=Company Initiated Study
• IIS= Investigator Initiated Study funded by DePuy Synthes
• Indep= Independent study not funded by DePuy Synthes
Appendix Table 1: Summary of studies on the ATTUNE Knee with additional information available on Study Registration Sites
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System
Page 16 of 20
This white paper was commissioned by DePuy Synthes
Companies, and the lead authors received compensation
for their time associated with the development of the
document. Additional consultation on content and editing
was provided by: Kim Dwyer PhD, Vanessa Danielson MSc
and Bronwyn Do Rego MSc of DePuy Synthes Companies.
*David Fisher, M.D. is a paid consultant for DePuy Synthes
Companies and is member of the ATTUNE Knee surgeon
design team.
1. Centers for Disease Control, www.cdc.gov/arthritis/basics/osteoarthritis.htm, last accessed.
2. ©2015 Global Data, 2016 MediPoint: Hip & Knee reconstruction- Global Analysis and MArket Forecast,
www.store.globaldata.com/market-reports/medical-devices/medipoint-hip-and-knee-reconstruction-
global-analysis-and-market-forecasts, last accessed 12-31-2015.
3. 13th Annual Report 2016 National Joint Registry for England, Wales, Nothern Ireland and the isle of
Man. Surgical data to 31 December 2015, www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/
Reports/13th%20Annual%20Report/07950%20NJR%20Annual%20Report%202016%20ONLINE%20
REPORT.pdf, last accessed 2-7-2017.
4. Arthritis Research UK, http://www.arthritisresearchuk.org/arthritis-information/data-and-statistics/data-by-
condition/osteoarthritis.aspx, last accessed 2-7-2017.
5. Australian Orthopaedic Association National Joint Replacement Registry Annual Report, Adelaide, AOA,
2016, last accessed 2-7-2017.
ACKNOWLEDGEMENTS AND DISCLOSURES
REFERENCES
Reason for Revision Number Percent
Loosening/Lysis 4990 28.1
Infection 3985 22.5
Patellofemoral Pain 2059 11.6
Pain 1535 8.7
Instability 1194 6.7
Patella Erosion 772 4.4
Arthrofibrosis 611 3.4
Fracture 486 2.7
Malalignment 403 2.3
Wear Tibial Insert 290 1.6
Metal Related Pathology 286 1.6
Incorrect Sizing 222 1.3
Other 897 5.1
Total 17730 100.0
Table KT7 : Primary Total Knee Replacement by Reason for Revision
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System

Page 17 of 20
6. Blue Cross Blue Shield, A study of cost variations for knee and hip replacement surgeries in the U.S..The
Extreme Cost Variation in Healthcare, www.bcbs.com/about-us/capabilities-initiatives/health-america/
health-of-america-report/study-cost-variations, last accessed 2-9-2017.
7. Department of Health and Human Services. Centers for Medicare & Medicaid Services. 42 CFR Part 510.
[CMS-5516-F], Medicare Program;Comprehensive Care for Joint Replacement Payment Model for Acute
Care Hospitals Furnishing Lower Extremity Joint Replacement, www.gpo.gov/fdsys/pkg/FR-2015-11-24/
pdf/2015-29438.pdf, last accessed 2-10-2017.
8. Finalised Patient Reported Outcome Measures (PROMs) in England - April 2014 to March 2015. Score
Comparison Tool [.xls], national figures, http://content.digital.nhs.uk/catalogue/PUB21189, last accessed
2-10-2017.
9. National Joint Registry, http://www.njrcentre.org.uk/, last accessed 2-7-2017.
10. NICE National Clinical Guidelines Center: Osteoarthritis Care and Management in Adults Clinical guideline
CG177, Feb 2014, www.nice.org.uk/guidance/cg177/evidence/full-guideline-191761309, last accessed
2-7-2017.
11. The New Zealand Joint Registry Seventeen Year Report, Jan 1999-December 2015, http://nzoa.org.nz/
system/files/NZJR%2017%20year%20Report.pdf, last accessed 2-7-2017.
12. US Department of Health and Human Services FDA Center for Drug Evaluation and Research, Guidance
for industry: patient-reported outcome measures: use in medical product development to support
labeling claims: draft guidance. http://www.fda.gov/downloads/drugs/guidances/ucm193282.pdf, last
accessed.
13. Appleby J, Devlin N, Parkin D Using patient reported outcomes to improve health care: John Wiley &
Sons, 2015.
14. Attarian DE, Wahl JE, Wellman SS, Bolognesi MP, Developing a high-efficiency operating room for total
joint arthroplasty in an academic setting. Clin Orthop Relat Res 2013;471:1832-6.
15. Azhar, Ali, Mannen, Erin, Smoger, Lowell, Haas, Brian, Laz, Peter, Rulkoetter, Paul, and Shelburne,
Kevin, Evaluation of in-Vivo Mechanics for Medialized Dome and Medialized Anatomic Patellofemoral
Geometries During Knee Extension and Lunge. International Society for Technology in Arthroplasty (ISTA):
e-Poster, Boston, MA, 10-5-2016.
16. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW, Validation study of WOMAC: a health
status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug
therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833-40.
17. Boraiah S, Joo L, Inneh IA, Rathod P, Meftah M, Band P, Bosco JA, Iorio R, Management of Modifiable
Risk Factors Prior to Primary Hip and Knee Arthroplasty: A Readmission Risk Assessment Tool. J Bone Joint
Surg Am 2015;97:1921-8.
18. Bourne RB, Chesworth B, Davis A, Mahomed N, Charron K, Comparing patient outcomes after THA and
TKA: is there a difference? Clin Orthop Relat Res 2010;468:542-6.
19. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD, Patient satisfaction after total knee
arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57-63.
20. Bozic KJ, Ward L, Vail TP, Maze M, Bundled payments in total joint arthroplasty: targeting opportunities
for quality improvement and cost reduction. Clin Orthop Relat Res 2014;472:188-93.
21. Brenkel, I, Chang, C, Clatworthy, M, Hamilton, W, Howard, J, Huey, V, Kantor, S, Lesko, J, Nunley, R,
Whittaker, JP, and Verdonk, P, Learning Curve with a New Primary TKA Implant: A Worldwide Perspective
with More than 2000 Patients. International Society for Technology in Arthroplasty (ISTA), Boston, MA.
22. Brooks R, EuroQol: the current state of play. Health Policy 1996;37:53-72.
23. Büker N, Akkaya S, Akkaya N, Gokalp O, Kavlak E, Ok N, Kiter AE, Kitis A, Comparison of effects of
supervised physiotherapy and a standardized home program on functional status in patients with total
knee arthroplasty: a prospective study. J Phys Ther Sci 2014;26:1531-6.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System

Page 18 of 20
24. Clary CW, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ, The influence of total knee arthroplasty geometry on
mid-flexion stability: an experimental and finite element study. J Biomech 2013;46:1351-7.
25. Coles TM, Dwyer KA, Mordin M, Williams V, Clatworthy M, Yates P, Hamilton W, Psychometric Evaluation
Of The Patient’s Knee Implant Performance (PKIP) Questionnaire For The Assessment Of Primary Total Knee
Arthroplasty. Value Health 2014;17:A568.
26. Conrad DN, Dennis DA, Patellofemoral crepitus after total knee arthroplasty: etiology and preventive
measures. Clin Orthop Surg 2014;6:9-19.
27. Dakin H, Gray A, Fitzpatrick R, Maclennan G, Murray D, Rationing of total knee replacement: a cost-
effectiveness analysis on a large trial data set. BMJ Open 2012;2:e000332.
28. Dalury DF, Pomeroy DL, Gorab RS, Adams MJ, Why are total knee arthroplasties being revised? J Arthroplasty
2013;28:120-1.
29. Etter K, Lerner J, De Moor C, Yoo A, Kalsekar I, Comparative Effectiveness of the ATTUNE® Knee System
vs. the Triathlon™ Knee System Real-world Hospital Length of Stay and Discharge Status. Value in Health
2016;19:A298. Premier Perspective™ Database analysis including 38 hospitals, representing 1,178 primary,
unilateral TKAs with the ATTUNE Knee and 5,707 primary, unilateral TKAs with Triathlon®. The analysis found
that the patients implanted with the ATTUNE Knee had statistically shorter length of stay and were more
frequently discharged home vs. a skilled nursing facility compared to the TKAs with Triathlon®.
30. Fang DM, Ritter MA, Davis KE, Coronal alignment in total knee arthroplasty: just how important is it? J
Arthroplasty 2009;24:39-43.
31. Hamilton, W, Brenkel, I., and Clatworthy, M., Early Patient Reported Outcomes With New Primary vs.
Contemporary Total Knee Arthroplasty: A Comparison of Two Worldwide, Multi-Center Prospective Studies.
International Society for Technology in Arthroplasty (ISTA): e-Poster. International Society for Technology in
Arthroplasty (ISTA): e-Poster (without short talk), Boston, MA, 10-5-2016.
32. Indelli PF, Pipino G, Johnson P, Graceffa A, Marcucci M, Posterior-stabilized total knee arthroplasty: a matched
pair analysis of a classic and its evolutional design. Arthroplasty Today 2016;2:193-8.
33. Insall J, Ranawat CS, Scott WN, Walker P, Total condylar knee replacement: preliminary report. 1976. Clin
Orthop Relat Res 2001:3-6.
34. Jacobs CA, Christensen CP, Factors influencing patient satisfaction two to five years after primary total knee
arthroplasty. J Arthroplasty 2014;29:1189-91.
35. Jacobs CA, Christensen CP, Karthikeyan T, Patient and intraoperative factors influencing satisfaction two to
five years after primary total knee arthroplasty. J Arthroplasty 2014;29:1576-9.
36. Keenan AC, Wood AM, Arthur CA, Jenkins PJ, Brenkel IJ, Walmsley PJ, Ten-year survival of cemented total
knee replacement in patients aged less than 55 years. J Bone Joint Surg Br 2012;94:928-31.
37. Keswani A, Tasi MC, Fields A, Lovy AJ, Moucha CS, Bozic KJ, Discharge Destination After Total Joint
Arthroplasty: An Analysis of Postdischarge Outcomes, Placement Risk Factors, and Recent Trends. J
Arthroplasty 2016;31:1155-62.
38. Kurtz S, Ong K, Lau E, Mowat F, Halpern M, Projections of primary and revision hip and knee arthroplasty in
the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5.
39. Lavernia CJ, Guzman JF, Gachupin-Garcia A, Cost effectiveness and quality of life in knee arthroplasty. Clin
Orthop Relat Res 1997:134-9.
40. Lewis S, Price M, Dwyer KA, O’Brien S, Heekin RD, Yates PJ, Beverland D, Mordin M, Development of a scale
to assess performance following primary total knee arthroplasty. Value Health 2014;17:350-9.
41. Losina E, Paltiel AD, Weinstein AM, Yelin E, Hunter DJ, Chen SP, Klara K, Suter LG, Solomon DH, Burbine SA,
Walensky RP, Katz JN, Lifetime medical costs of knee osteoarthritis management in the United States: impact
of extending indications for total knee arthroplasty. Arthritis Care Res (Hoboken ) 2015;67:203-15.
42. Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E,
Paltiel AD, Katz JN, Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital
volume. Arch Intern Med 2009;169:1113-21.
43. Martin JR, Jennings JM, Watters TS, Levy DL, McNabb DC, Dennis DA, Femoral Implant Design Modification
Decreases the Incidence of Patellar Crepitus in Total Knee Arthroplasty. The Journal of Arthroplasty.
44. Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J, The use of the Oxford hip and
knee scores. J Bone Joint Surg Br 2007;89:1010-4.
45. Navarro Espigares JL, Hernandez TE, Cost-outcome analysis of joint replacement: evidence from a Spanish
public hospital. Gac Sanit 2008;22:337-43.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System

Page 19 of 20
46. Neogi T, The Epidemiology and Impact of Pain in Osteoarthritis. Osteoarthritis Cartilage 20173;21:1145-53.
47. Parvizi J, Nunley RM, Berend KR, Lombardi AV, Jr., Ruh EL, Clohisy JC, Hamilton WG, Della Valle CJ, Barrack
RL, High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res
2014;472:133-7.
48. Pennington M, Grieve R, Black N, van der Meulen JH, Cost-Effectiveness of Five Commonly Used Prosthesis
Brands for Total Knee Replacement in the UK: A Study Using the NJR Dataset. PLoS One 2016;11:e0150074.
49. Pfitzner, T., Moewis, P, Boeth, Heide, and Trepczynski, Adam, In Vivo Analysis Of Femoro-Tibial Kinematics
In Cruciate Retaining Total Knee Arthroplasty At 2 Years After Index Surgery. 17th EFORT Congress 2016,
Geneva, CH.
50. Pfitzner T, von RP, Preininger B, Perka C, Does the ideal total knee arthroplasty for younger patients exist? Z
Orthop Unfall 2014;152:393-8.
51. Pollock DC, Ammeen DJ, Engh GA, Synovial entrapment: a complication of posterior stabilized total knee
arthroplasty. J Bone Joint Surg Am 2002;84-A:2174-8.
52. Porter ME, What is value in health care? N Engl J Med 2010;363:2477-81.
53. Ranawat CS, White PB, West S, Ranawat AS, Clinical and Radiographic Results of Attune and PFC Sigma
Knee Designs at 2-Year Follow-Up: A Prospective Matched-Pair Analysis. J Arthroplasty 2017;32:431-6.
54. Rasanen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynanen OP, Roine RP, Effectiveness of hip or
knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop 2007;78:108-15.
55. Rissanen P, Aro S, Sintonen H, Asikainen K, Slatis P, Paavolainen P, Costs and cost-effectiveness in hip and
knee replacements. A prospective study. Int J Technol Assess Health Care 1997;13:575-88.
56. Roos EM, Lohmander LS, The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to
osteoarthritis. Health Qual Life Outcomes 2003;1:64.
57. Rothwell AG, Hooper GJ, Hobbs A, Frampton CM, An analysis of the Oxford hip and knee scores and their
relationship to early joint revision in the New Zealand Joint Registry. J Bone Joint Surg Br 2010;92:413-8.
58. Ruiz D, Jr., Koenig L, Dall TM, Gallo P, Narzikul A, Parvizi J, Tongue J, The direct and indirect costs to society
of treatment for end-stage knee osteoarthritis. J Bone Joint Surg Am 2013;95:1473-80.
59. Scott CE, Howie CR, MacDonald D, Biant LC, Predicting dissatisfaction following total knee replacement: a
prospective study of 1217 patients. J Bone Joint Surg Br 2010;92:1253-8.
60. Shan L, Shan B, Suzuki A, Nouh F, Saxena A, Intermediate and long-term quality of life after total knee
replacement: a systematic review and meta-analysis. J Bone Joint Surg Am 2015;97:156-68.
61. Sharkey PF, Miller AJ, Noise, numbness, and kneeling difficulties after total knee arthroplasty: is the outcome
affected? J Arthroplasty 2011;26:1427-31.
62. Toomey S., Himden S., Daccach J, Shah J, Lesko J, and Hamilton W, Comparing the Incidence of
Patellofemoral Complications in a New Total Knee Arthroplasty (TKA) System vs. Currently Available Products
in Two, WorldWide, Multi-Center, Prospective Clinical Studies. 26th AAHKS Annual Meeting: Podium
presentation, 11-10-2016.
63. Ware JE, Jr., Sherbourne CD, The MOS 36-item short-form health survey (SF-36). I. Conceptual framework
and item selection. Med Care 1992;30:473-83.
64. Yu S, Garvin KL, Healy WL, Pellegrini VD, Jr., Iorio R, Preventing Hospital Readmissions and Limiting the
Complications Associated With Total Joint Arthroplasty. Instr Course Lect 2016;65:199-210.
DePuy Synthes Companies Improving the Value of Primary Total Knee Arthroplasty: the ATTUNE® Knee System

www.depuysynthes.com
www.ATTUNEevidence.com
The third party trademarks used herein are the trademarks of their respective owners.
© DePuy Synthes 2017. All rights reserved. DSUS/JRC/0217/1996 Issued 3/17
DePuy Orthopaedics, Inc.
700 Orthopaedic Drive
Warsaw, IN 46582
USA
Tel: +1 (800) 366-8143
Fax: +1 (800) 669-2530
DePuy (Ireland)
Loughbeg, Ringaskiddy
Co. Cork, Ireland
Tel: +353 21 4914 000
Fax: +353 21 4914 199
DePuy International, Ltd.
St Anthony’s Road
Leeds LS11 8DT
England
Tel: +44 (0) 113 270 0461