Contains Nonbinding Recommendations 2016 11 Technical Conformance Guide V3.2.1
User Manual: Pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 44

STUDY DATA
TECHNICAL CONFORMANCE GUIDE
Technical Specifications Document
This Document is incorporated by reference into the following
Guidance Document(s):
Guidance for Industry Providing Regulatory Submissions in Electronic
Format – Standardized Study Data
For questions regarding this technical specifications document, contact CDER at
cder-edata@fda.hhs.gov or CBER at cber.cdisc@fda.hhs.gov
U.S. Department of Health and Human Services
Food and Drug Administration
Center for Drug Evaluation and Research (CDER)
Center for Biologics Evaluation and Research (CBER)
November 2016

STUDY DATA
TECHNICAL CONFORMANCE GUIDE
November 2016
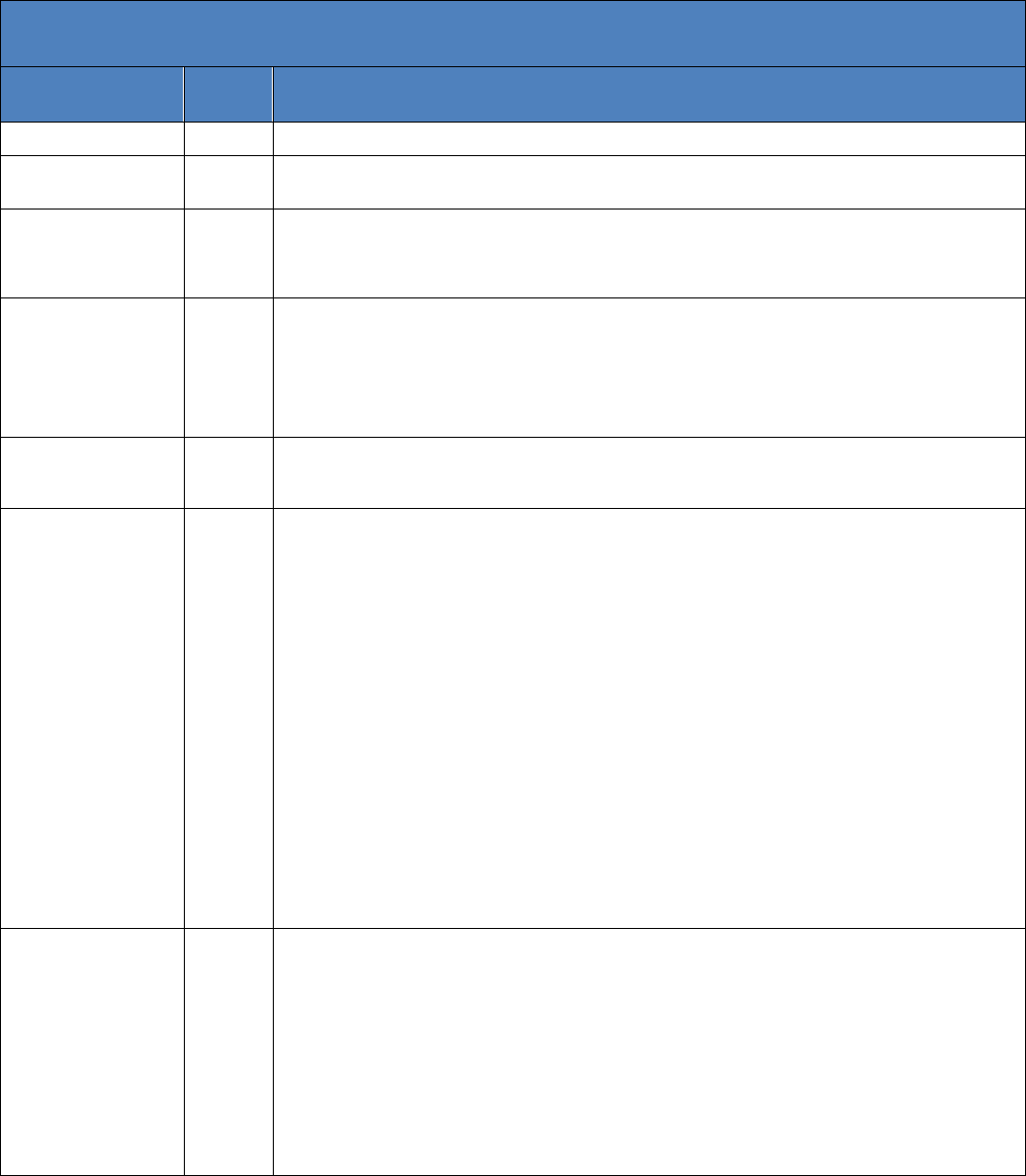
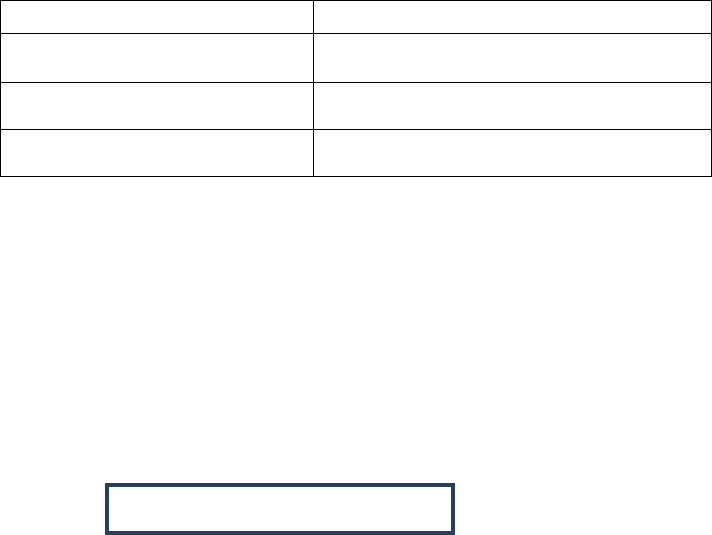
Revision History
Date
Versi
on
Summary of Revisions
January 2014
1.0
Initial Version
December 2014
2.0
Revisions based on the public comment period (February 2014 – May 2014); and CDER/CBER
internal review May 2014 – December 2014
March 2015
2.1
Revisions based on comments received to version 2.0. Updates to Sections 2.2 Study Data
Reviewer’s Guide (SDRG)
SDRG, 2.3 Analysis Data Reviewer’s (ADRG), 3.3.1 SAS Transport Format, 3.3.2. Dataset
Size and a revision of Section 4.1.4.5 Data Definition File
June 2015
2.2
Revisions based on comments received to version 2.1. Updates on Table of Contents; Sections
4.1, 4.1.1.2, 4.1.2.3. Updates to Trial Design. Added Exposure as Collected (EC Domain) and
Death Details (DD) subsections. Updates to 4.1.2.2, 4.1.2.3, 4.1.2.4, 4.1.2.5, 4.1.2.6, 4.1.2.8,
4.1.2.9.1, 4.1.2.9.2, 4.1.4 (header and all sub-headers updated to specify which standards
apply), 4.1.4.5, and 4.1.4.6. Added 5.1 subsection; 6.7, 6.7.1, 6.7.1.1. Updates on Section 7,
8.2.2 and Glossary.
October 2015
2.3
Updates to Section 1.3, Exposure as Collected (EC Domain) and Death Details (DD Domain).
Reorganization of Section 4.1.2 and corresponding updates to appropriate sub-sections. Updates
to Sections 4.1.4.5 and 5.1. Added Sections 7.1 and 7.2.
March 2016
3.0
Section 2.2 (Study Data Reviewer’s Guide) - Updated link for SDRG in Footnote 10
Section 3.3.2 (Dataset Size) - Increased Data Set Size
Section 4.1.1.2 (SDTM General Considerations) - Updated to reflect define.xml file and SDRG
reference.
Section 4.1.2.2 (Analysis Data Model - General Considerations) - Updated to reflect define.xml file
and SDRG reference.
Section 4.1.3.2 (Standard for Exchange of Nonclinical Data - General Considerations) - Updated to
reflect define.xml file and SDRG reference.
Section 4.1.4.5 (Data Definition Files for SDTM, SEND, and AdaM) - Updated to reflect define.xml
version 2.0 and data definition specification details
Section 5.1 (Therapeutic Area Standards – General) - Updated to reflect more detailed information
related to Therapeutic Area Standards
Section 5.2 (Supported Therapeutic Area Standards) - Added information related to acceptance testing
on the standard
Section 5.2.1 (Chronic Hepatitis C) - Added Section for this information.
Section 5.2.2 (Dyslipidemia) - Added Section for this information.
Section 6.1.2.1 (Use of the specific controlled term “OTHER”) - Added information related to
controlled terminology and the mapping to “Other”
Section 8.3.1 (Study Data Traceability Overview) - Update to Study Data Traceability flow diagram
reference.
July 2016
3.1
Section 2.1 (Study Data Standardization Plan) Updated to reflect acronym SDSP (Study Data
Standardization Plan) and added footnote 10.
Section 4.1.1.3 (SDTM Domain Specifications) – Updated Trial Design Model (TDM)
Section 4.1.3.3 (SEND Domain Specification) – Added Trial Design (TD)
Section 5.2.3 (Diabetes) - Added Section for this information.
Section 5.2.4 (QT Studies) - Added Section for this information.
Section 5.2.5 (Tuberculosis) - Added Section for this information.
Section 8.2.1.1 (Conformance validation) - Created Section Header and expanded information.
Section 8.2.1.2 (Quality checks) – Created Section Header and updated to reflect study data standard.
Section 8.2.2 (Support on Data Validation Rules) - Expanded information.
Section 3.2 (Portable Document Format) & Glossary – Updated International Council for
Harmonisation (ICH) name
Contains Nonbinding Recommendations
ii
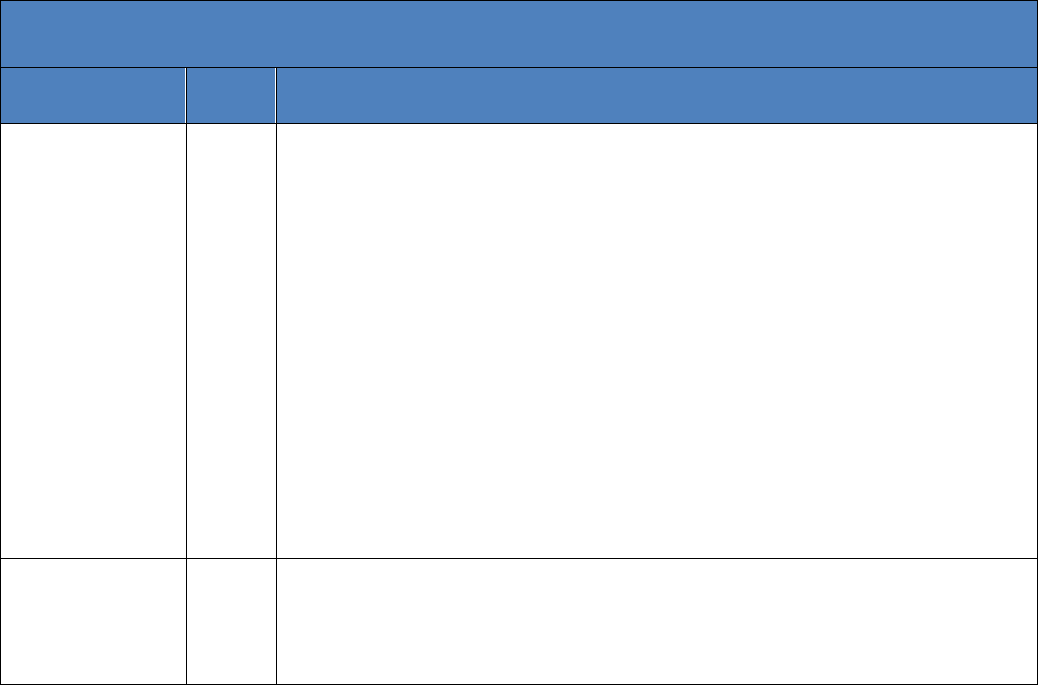
Revision History
Date
Versi
on
Summary of Revisions
October 2016
3.2
Section 2.2.1 (SDRG for Clinical Data) – Added naming convention
Section 2.2.2 (SDRG for Nonclinical Data) -Added naming convention
Section 2.3 (Analysis Data Reviewer’s Guide) – Provided additional information
Section 3.3.3 (Dataset Column Length) – Expanded Information
Section 4.1.1.2 (SDTM General Considerations) – Expanded Adjudication Data
Section 4.1.2.10 ( Software Programs) – Added more detail related to software programs
Section 4.1.3.2 (General Considerations) – Added VISITDY variable information
Section 4.1.3.3 (SEND Domain Specification) – Added Clinical Observations (CL) Domain.
Expanded Trial Arms and Trial Sets information.
Section 5.1 (General) – Expanded Information
Section 5.2 (Supported Therapeutic Areas) – Expanded Information
Section 7.1 (ECTD File Directory Structure) – Referenced the Guidance to Industry Providing
Regulatory Submissions in Electronic Format: Certain Human Pharmaceutical Product Applications
and Related Submissions Using the Electronic Common Technical Document Specifications and
added footnote
Section 7.2 (ECTD Sample Submission) – Change header to align with detailed information.
Section 8.2.1 (Types of Data Validation Rules) – Expanded Information
Section 8.2.1.1 (Conformance validation) – Expanded Information
Section 8.2.1.2 (FDA Business Rules) – Added new Section
Section 8.2.2 (Support on Data Validation Rules) – updated to reflect conformance rules
Section 8.3.1 (Overview (Study Data Traceability) – added relate counts information
November 2016
3.2.1
Section 8.2.2 (Support on Data Validation Rules) – Footnote 50 Added reference to the Standards
Webpage.
Section 4.1.3.3 (SEND Domain Specification) – Fixed Typo.
Global (Updated naming convention for clinical Study Data Reviewer’s Guide (“cSDRG.pdf”) and
the non-clinical Study Data Reviewer’s Guide (“nSDRG.pdf”) to reflect lower case instead of upper
case. eCTD requires lower case file names.
Contains Nonbinding Recommendations
i
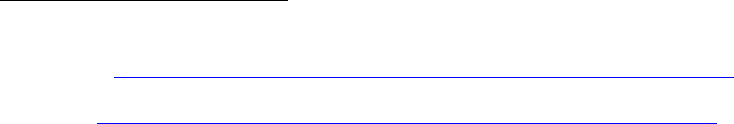
Table of Contents
1. INTRODUCTION .................................................................................................................................. 1
1.1 BACKGROUND .......................................................................................................................................... 1
1.2 PURPOSE ................................................................................................................................................. 1
1.3 DOCUMENT REVISION AND CONTROL ............................................................................................................ 2
1.4 ORGANIZATION AND SUMMARY OF THE GUIDE ............................................................................................... 2
1.5 RELATIONSHIP TO OTHER DOCUMENTS ......................................................................................................... 3
2. PLANNING AND PROVIDING STANDARDIZED STUDY DATA ................................................................. 4
2.1 STUDY DATA STANDARDIZATION PLAN .......................................................................................................... 4
2.2 STUDY DATA REVIEWER’S GUIDES ................................................................................................................ 4
2.2.1 SDRG for Clinical Data................................................................................................................. 5
2.2.2 SDRG for Nonclinical Data .......................................................................................................... 5
2.3 ANALYSIS DATA REVIEWER’S GUIDE .............................................................................................................. 5
3. EXCHANGE FORMAT – ELECTRONIC SUBMISSIONS ............................................................................. 6
3.1 EXTENSIBLE MARK-UP LANGUAGE ................................................................................................................ 6
3.2 PORTABLE DOCUMENT FORMAT .................................................................................................................. 6
3.3 FILE TRANSPORT FORMAT ........................................................................................................................... 6
3.3.1 SAS Transport Format ................................................................................................................. 6
3.3.2 Dataset Size ................................................................................................................................ 7
3.3.3 Dataset Column Length .............................................................................................................. 7
3.3.4 Variable and Dataset Descriptor Length ..................................................................................... 7
3.3.5 Special Characters: Variables and Datasets ............................................................................... 7
3.3.6 Variable and Dataset Names ...................................................................................................... 7
3.3.7 Variable and Dataset Labels ....................................................................................................... 8
4. STUDY DATA SUBMISSION FORMAT – CLINICAL AND NONCLINICAL ................................................... 8
4.1 CLINICAL DATA INTERCHANGE STANDARDS CONSORTIUM ................................................................................. 8
4.1.1 Study Data Tabulation Model ..................................................................................................... 9
4.1.1.1 Definition ......................................................................................................................................... 9
4.1.1.2 SDTM General Considerations ......................................................................................................... 9
4.1.1.3 SDTM Domain Specifications ......................................................................................................... 10
4.1.2 Analysis Data Model ................................................................................................................. 13
4.1.2.1 Definition ....................................................................................................................................... 13
4.1.2.2 General Considerations .................................................................................................................. 13
4.1.2.3 Dataset Labels ................................................................................................................................ 13
4.1.2.4 Subject Level Analysis Data ............................................................................................................ 13
4.1.2.5 Core Variables ................................................................................................................................ 14
4.1.2.6 Key Efficacy and Safety Variables ................................................................................................... 14
4.1.2.7 Timing Variables ............................................................................................................................. 14
4.1.2.8 Numeric Date Variables ................................................................................................................. 14
4.1.2.9 Imputed Data ................................................................................................................................. 15
4.1.2.10 Software Programs......................................................................................................................... 15
4.1.3 Standard for Exchange of Nonclinical Data .............................................................................. 15
4.1.3.1 Definition ....................................................................................................................................... 15
4.1.3.2 General Considerations .................................................................................................................. 15
4.1.3.3 SEND Domain Specification ............................................................................................................ 16
4.1.4 General Considerations: SDTM, SEND, and/or ADaM .............................................................. 17
4.1.4.1 Variables in SDTM and SEND: Required, Expected, and Permissible ............................................ 17
4.1.4.2 Dates in SDTM and SEND ............................................................................................................... 18
4.1.4.3 Naming Conventions in SDTM and SEND ....................................................................................... 18
4.1.4.4 SDTM and SEND Versions............................................................................................................... 18
Contains Nonbinding Recommendations
ii
4.1.4.5 Data Definition Files for SDTM, SEND, and ADaM.......................................................................... 18
4.1.4.6 Annotated Case Report Form (aCRF) for SDTM ............................................................................. 19
5. THERAPEUTIC AREA STANDARDS ...................................................................................................... 19
5.1 GENERAL ............................................................................................................................................... 19
5.2 SUPPORTED THERAPEUTIC AREAS ............................................................................................................... 20
5.2.1 Chronic Hepatitis C.................................................................................................................... 20
5.2.2 Dyslipidemia ............................................................................................................................. 20
5.2.3 Diabetes .................................................................................................................................... 20
5.2.4 QT Studies ................................................................................................................................. 20
5.2.5 Tuberculosis .............................................................................................................................. 20
6. TERMINOLOGY .................................................................................................................................. 20
6.1 GENERAL ............................................................................................................................................... 20
6.1.1 Controlled Terminologies .......................................................................................................... 21
6.1.2 Use of Controlled Terminologies ............................................................................................... 21
6.1.2.1 Use of the specific controlled term “OTHER” ................................................................................. 22
6.1.3 Maintenance of Controlled Terminologies................................................................................ 22
6.2 CDISC CONTROLLED TERMINOLOGY ........................................................................................................... 23
6.3 ADVERSE EVENTS .................................................................................................................................... 23
6.3.1 MedDRA .................................................................................................................................... 23
6.3.1.1 General Considerations .................................................................................................................. 23
6.4 MEDICATIONS ........................................................................................................................................ 23
6.4.1 FDA Unique Ingredient Identifier .............................................................................................. 23
6.4.1.1 General Considerations .................................................................................................................. 23
6.4.2 WHO Drug Dictionary ............................................................................................................... 24
6.4.2.1 General Considerations .................................................................................................................. 24
6.5 PHARMACOLOGIC CLASS ........................................................................................................................... 24
6.5.1 National Drug File -- Reference Terminology ............................................................................ 24
6.5.1.1 General Considerations .................................................................................................................. 24
6.6 INDICATION ............................................................................................................................................ 25
6.6.1 SNOMED CT .............................................................................................................................. 25
6.6.1.1 General Considerations .................................................................................................................. 25
6.7 LABORATORY TESTS ................................................................................................................................. 25
6.7.1 LOINC ........................................................................................................................................ 25
6.7.1.1 General Considerations .................................................................................................................. 25
7. ELECTRONIC SUBMISSION FORMAT .................................................................................................. 26
7.1 ECTD FILE DIRECTORY STRUCTURE ............................................................................................................. 26
7.2 ECTD SAMPLE SUBMISSION ...................................................................................................................... 29
8. STUDY DATA VALIDATION AND TRACEABILITY .................................................................................. 29
8.1 DEFINITION OF DATA VALIDATION .............................................................................................................. 29
8.2 STUDY DATA VALIDATION RULES ................................................................................................................ 29
8.2.1 Types of Study Data Validation Rules ....................................................................................... 29
8.2.1.1 Conformance Rules ........................................................................................................................ 29
8.2.1.2 FDA Business Rules ........................................................................................................................ 30
8.2.2 Support on Data Validation Rules ............................................................................................. 30
8.3 STUDY DATA TRACEABILITY ....................................................................................................................... 30
8.3.1 Overview ................................................................................................................................... 30
8.3.2 Legacy Study Data Conversion to Standardized Study Data ..................................................... 31
8.3.2.1 Traceability Issues with Legacy Data Conversion ........................................................................... 31
8.3.2.2 Legacy Data Conversion Plan and Report ...................................................................................... 33
Contains Nonbinding Recommendations
iii
APPENDIX: DATA STANDARDS AND INTEROPERABLE DATA EXCHANGE ............................................... 34
GLOSSARY .................................................................................................................................................. 37
Contains Nonbinding Recommendations
1
STUDY DATA
TECHNICAL CONFORMANCE GUIDE
This technical specifications document represents the Food and Drug Administration's
(FDA's) current thinking on this topic. It does not create or confer any rights for or on
any person and does not operate to bind FDA or the public. You can use an alternative
approach if the approach satisfies the requirements of the applicable statutes and
regulations. If you want to discuss an alternative approach, contact the FDA staff
responsible for implementing this guidance. If you cannot identify the appropriate FDA
staff, send an email to cder-edata@fda.hhs.gov or cber.cdisc@fda.hhs.gov.
1. Introduction
1.1 Background
This Study Data Technical Conformance Guide (Guide) provides specifications,
recommendations, and general considerations on how to submit standardized study data
using FDA-supported
1
data standards located in the FDA Data Standards Catalog
(Standards Catalog).
2
The Guide supplements the guidance for industry Providing
Regulatory Submissions in Electronic Format — Standardized Study Data (eStudy Data).
The eStudy Data guidance will implement the electronic submission requirements of
section 745A(a) of the Food Drug & Cosmetic (FD&C) Act with respect to standardized
study data contained in certain investigational new drug applications (INDs), new drug
applications (NDAs); abbreviated new drug applications (ANDAs); and certain biologics
license applications (BLAs) that are submitted to the Center for Drug Evaluation and
Research (CDER) or the Center for Biologics Evaluation and Research (CBER).
3
1.2 Purpose
This Guide provides technical recommendations to sponsors
4
for the submission of
animal and human study data and related information in a standardized electronic format
in INDs, NDAs, ANDAs, and BLAs. The Guide is intended to complement and promote
interactions between sponsors and FDA review divisions. However, it is not intended to
replace the need for sponsors to communicate directly with review divisions regarding
implementation approaches or issues relating to data standards. To better understand
why the FDA is now emphasizing the submission of standardized data for all studies,
please refer to the Appendix.
Because of the inherent variability across studies and applications, it is difficult to
identify all data needed by a review division prior to a scientific regulatory review. We
recommend that as early as the pre-IND meeting, sponsors should use the established
1
For the purposes of this document, “supported” means the receiving Center has established processes and
technology to support receiving, processing, reviewing, and archiving files in the specified file format.
2
Available at http://www.fda.gov/forindustry/datastandards/studydatastandards/default.htm.
3
See Providing Regulatory Submissions in Electronic Format — Standardized Study Data (section II.A)
available at http://www.fda.gov/forindustry/datastandards/studydatastandards/default.htm.
4
For the purposes of this document, the term “sponsor” refers to both “sponsors” and “applicants” who are
submitting study data to the Agency.
Contains Nonbinding Recommendations
2
regulatory process to discuss with the review division the key data necessary to support a
submission, the data elements that should be included in each dataset, and the
organization of the data within the datasets.
Some data standards may not require the use of all defined data elements to be collected
in any given study. For example, the Study Data Tabulation Model Implementation
Guide (SDTMIG)
5
classifies variables as required, expected, or permissible. What data
are collected and submitted is a decision that should be made based on scientific reasons,
regulation requirements, and discussions with the review division. However, all study-
specific data necessary to evaluate the safety and efficacy of the medical product should
be submitted in conformance with the standards currently supported by FDA and listed in
the Standards Catalog.
If there is a question regarding a specific submission or a particular data standard
implementation, the sponsor should contact the review division for specific submission
questions or the appropriate contact for data standards issues (cder-edata@fda.hhs.gov or
cber.cdisc@fda.hhs.gov).
This Guide supersedes all previous Study Data Specifications documents (Versions 1.0 -
2.0) and CDER Study Data Common Issues Documents (Versions 1.0 -1.1).
1.3 Document Revision and Control
FDA intends to post updated versions of the Guide to the Study Data Standards
Resources Web page (Standards Web page)
6
. The plan is to publish updated versions in
March and October of each calendar year. However, this guide will be posted sooner if
important issues arise. The revision history page of the Guide will contain sufficient
information on the changes made by section.
1.4 Organization and Summary of the Guide
This document is organized as follows:
Section 1: Introduction – provides information on regulatory policy and guidance
background, purpose, and document control.
Section 2: Planning and Providing Standardized Study Data – recommends and
provides details on preparing an overall study data standardization plan, a
study data reviewer’s guide and an analysis data reviewer’s guide.
Section 3: Exchange Format - Electronic Submissions – presents the specifications,
considerations, and recommendations for the file formats currently supported
by FDA.
5
See http://www.cdisc.org.
6
The Standards Web page can be accessed at
http://www.fda.gov/forindustry/datastandards/studydatastandards/default.htm.
Contains Nonbinding Recommendations
3
Section 4: Study Data Submission Format: Clinical and Nonclinical – presents
general considerations and specifications for sponsors using, for example, the
following standards for the submission of study data: Study Data Tabulation
Model (SDTM), Analysis Data Model (ADaM), and Standard for Exchange of
Nonclinical Data (SEND).
Section 5: Therapeutic Area Standards – presents supplemental considerations and
specific recommendations when sponsors submit study data using FDA-
supported therapeutic area standards (TA).
Section 6: Terminology – presents general considerations and specific recommendations
when using controlled terminologies/vocabularies for clinical trial data.
Section 7: Electronic Submission Format – provides specifications and
recommendations on submitting study data using the electronic Common
Technical Document (eCTD) format.
Section 8: Study Data Validation and Traceability – provides general
recommendations on conformance to standards, data validation rules, data
traceability expectations, and legacy data conversion.
1.5 Relationship to Other Documents
This Guide integrates and updates information discussed previously in the Study Data
Specifications and the CDER Common Data Standards Issues documents. As noted
above, this Guide supersedes all previous Study Data Specifications documents (Versions
1.0 - 2.0) and CDER Study Data Common Issues Documents (Versions 1.0 -1.1). The
examples of issues and concerns discussed in the Guide are intended as examples only of
common issues, and not an inclusive list of all possible issues.
This Guide is incorporated by reference into the Guidance to Industry Providing
Regulatory Submissions in Electronic Format: Standardized Study Data. In addition,
sponsors should reference the following:
Study Data Standards Resources Web page (See section 1.3)
FDA Data Standards Catalog (See section 1.1)
FDA Portable Document Format Specifications (See section 3.2)
Guidance to Industry Providing Regulatory Submissions in Electronic Format:
Submissions Under Section 745A(a) of the Federal Food, Drug, and Cosmetic
Act
7
Guidance to Industry Providing Regulatory Submissions in Electronic Format:
Certain Human Pharmaceutical Product Applications and Related Submissions
Using the Electronic Common Technical Document Specifications
8
7
http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm384686.pdf
8
www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm333969.pdf
Contains Nonbinding Recommendations
4
2. Planning and Providing Standardized Study Data
2.1 Study Data Standardization Plan
For clinical and nonclinical studies, sponsors should include a plan (e.g., in the IND)
describing the submission of standardized study data to FDA. The Study Data
Standardization Plan (SDSP) assists FDA in identifying potential data standardization
issues early in the development program. Sponsors may also initiate discussions at the
pre-IND stage. For INDs, the SDSP should be located in the general investigational
plan. The SDSP should include, but is not limited to the following:
1. List of the planned studies
2. Type of studies (e.g., phase I, II or III)
3. Study designs (e.g., parallel, cross-over, open-label extension)
4. Planned data standards, formats, and terminologies and their versions or a
justification of studies that may not conform to the currently supported standards
The FDA’s Study Data Standards Resources Web page provides recommendations for
preparing a SDSP.
9
,
10
The SDSP should be updated in subsequent communications with FDA as the
development program expands and additional studies are planned. Updates to the SDSP
should not be communicated each time a study is started. The cover letter accompanying
a study data submission should describe the extent to which the latest version of the
SDSP was executed.
2.2 Study Data Reviewer’s Guides
The preparation of a Study Data Reviewer’s Guide (SDRG)
11
is recommended as an
integral part of a standards-compliant study data submission. The SDRG should describe
any special considerations or directions that may facilitate an FDA reviewer's use of the
submitted data and may help the reviewer understand the relationships between the study
report and the data.
12
9
http://www.fda.gov/downloads/ForIndustry/DataStandards/StudyDataStandards/UCM447119.pdf
10
A specific template for a Study Data Standardization Plan is not specified. However, an example of a
Study Data Standardization Plan (template, completion guidelines and examples) can be found at
http://www.phusewiki.org/wiki/index.php?title=Study_Data_Standardization_Plan_%28SDSP%29
11
A specific template for a Study Data Reviewer’s Guide is not specified. However, an example of a Study
Data Reviewer’s Guide (template, completion guidelines and examples) can be found at
http://www.phusewiki.org/wiki/index.php?title=Study_Data_Reviewer%27s_Guide
12
For submissions to CBER, sponsors and applicants should continue to provide the Data Interpretation
and Validation Report (DIVR). The DIVR can be incorporated into the Study Data Reviewer’s Guide. The
DIVR can be found at
http://www.fda.gov/BiologicsBloodVaccines/DevelopmentApprovalProcess/ucm209137.htm
Contains Nonbinding Recommendations
5
There are two study guides: clinical and nonclinical. The SDRG for nonclinical studies
(nSDRG) and SDRG clinical studies (cSDRG) should be placed with the study data in
Module 4 and 5, respectively, in the Electronic Common Technical Document (eCTD).
13
2.2.1 SDRG for Clinical Data
An SDRG for clinical data should be named csdrg (the prefix ‘c’ designates ‘clinical’)
and the document should be named ‘csdrg’ and provided as a PDF file upon submission
(csdrg.pdf)
The FDA announced in the Federal Register (Docket No. FDA-2015-N-2523) its intent
to review the cSDRG and recommends its use.
2.2.2 SDRG for Nonclinical Data
An SDRG for nonclinical data should be named nsdrg (the prefix ‘n’ designates
‘nonclinical’) and the document should be named ‘nsdrg’ and provided as a PDF file
upon submission (nsdrg.pdf).
2.3 Analysis Data Reviewer’s Guide
The preparation of an Analysis Data Reviewer’s Guide (ADRG)
14
is recommended as an
important part of a standards-compliant analysis data submission. The ADRG provides
FDA reviewers with context for analysis datasets and terminology, received as part of a
regulatory product submission, additional to what is presented within the data definition
file (i.e., define.xml). The ADRG also provides a summary of ADaM conformance
findings. The ADRG purposefully duplicates limited information found in other
submission documentation (e.g., the protocol, statistical analysis plan [SAP], clinical
study report, define.xml) in order to provide FDA reviewers with a single point of
orientation to the analysis datasets. It should be noted that the submission of an ADRG
does not eliminate the requirement to submit a complete and informative define.xml file
corresponding to the analysis datasets.
The ADRG for a clinical study should be placed with the analysis data in Module
5 of the Electronic Common Technical Document (eCTD).
An ADRG for clinical data should be called an ADRG and the document should
be a PDF file ‘ADRG.pdf’ upon submission.
13
The Study Data Reviewer’s Guides are separate documents from an overall reviewer’s guide which is
placed in Module 1 of the eCTD.
14
A specific template for an Analysis Data Reviewer’s Guide is not specified. However, an example of an
Analysis Data Reviewer’s Guide (template, completion guidelines and examples) can be found at
http://www.phusewiki.org/wiki/index.php?title=Analysis_Data_Reviewer's_Guide.
Contains Nonbinding Recommendations
6
3. Exchange Format – Electronic Submissions
3.1 Extensible Mark-up Language
Extensible Mark-up Language (XML), as defined by the World Wide Web Consortium
(W3C), specifies a set of rules for encoding documents in a format that is both human-
readable and machine-readable.
15
,
16
XML facilitates the sharing of structured data across
different information systems. An XML use case is CDISC’s define.xml file. All XML
files should use .xml as the file extension. Although XML files can be compressed, the
define.xml should not be compressed.
3.2 Portable Document Format
Portable Document Format (PDF) is an open file format used to represent documents in a
manner independent of application software, hardware, and operating systems.
17
A PDF
use case includes, e.g., the annotated CRF (aCRF / blankcrf), and other documents that
align with the International Conference on Harmonization (ICH) M2.
18
FDA PDF
specifications are located on FDA’s Electronic Common Technical Document (eCTD)
Web site.
19
The Standards Catalog lists the PDF version(s) that are supported by FDA.
All PDF files should use .pdf as the file extension.
3.3 File Transport Format
3.3.1 SAS Transport Format
The SAS Transport Format (XPORT) Version 5 is the file format for the submission of
all electronic datasets.
20
The XPORT is an open file format published by SAS Institute
for the exchange of study data. Data can be translated to and from XPORT to other
commonly used formats without the use of programs from SAS Institute or any specific
vendor. There should be one dataset per transport file, and the dataset in the transport file
should be named the same as the transport file (e.g., “ae” and ae.xpt, “suppae” and
suppae.xpt).
XPORT files can be created by the COPY Procedure in SAS Version 5, Version 6 and
higher of the SAS Software. SAS Transport files processed by the SAS CPORT cannot
be reviewed, processed, or archived by FDA. Sponsors can find the record layout for
SAS XPORT transport files through SAS technical document TS-140.
21
All SAS XPORT
transport files should use .xpt as the file extension. There should be one dataset per
XPORT file and the files should not be compressed.
15
See http://en.wikipedia.org/wiki/XML.
16
See http://www.w3.org/XML/.
17
Adobe Systems Incorporated, PDF Reference, sixth edition, version 1, Nov. 2006, p. 33.
18
See http://www.ich.org/products/electronic-standards.html.
19
Available at
http://www.fda.gov/Drugs/DevelopmentApprovalProcess/FormsSubmissionRequirements/ElectronicSubmi
ssions/ucm153574.htm
20
See http://www.sas.com
21
Available at http://support.sas.com/techsup/technote/ts140_2.pdf
Contains Nonbinding Recommendations
7
3.3.2 Dataset Size
Each dataset should be provided in a single transport file. The maximum size of an
individual dataset that FDA can process depends on many factors. Datasets greater than
5 gigabytes (GB) in size should be split into smaller datasets no larger than 5 GB.
Sponsors should submit these smaller datasets, in addition to the larger non-split datasets,
to better support regulatory reviewers. The split datasets should be placed in a separate
sub-directory labeled “split” (See section 7.1). A clear explanation regarding how these
datasets were split needs to be presented within the relevant data reviewer’s guide.
3.3.3 Dataset Column Length
The allotted length for each column containing character (text) data should be set to the
maximum length of the variable used across all datasets in the study except for suppqual
datasets. For suppqual datasets, the allotted length for each column containing character
(text) data should be set to the maximum length of the variable used in the individual
dataset. This will significantly reduce file sizes. For example, if USUBJID has a
maximum length of 18, the USUBJID’s column size should be set to 18, not 200.
3.3.4 Variable and Dataset Descriptor Length
The length of variable names, descriptive labels, and dataset labels should not exceed the
maximum permissible number of characters described below.
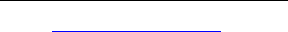
Table 1: Maximum Length of Variables and Dataset Elements
Element
Maximum Length in Characters
Variable Name
8
Variable Descriptive Label
40
Dataset Label
40
3.3.5 Special Characters: Variables and Datasets
Variable names, as well as variable and dataset labels should include American Standard
Code for Information Interchange (ASCII) text codes only.
3.3.6 Variable and Dataset Names
Variable and dataset names should not contain punctuation, dashes, spaces, or other non-
alphanumeric symbols. In addition, the variable and dataset names should not contain
special characters, including:
\ / * ,? < > | “ ‘ : % # + ( ) { } [ ]
Contains Nonbinding Recommendations
8
3.3.7 Variable and Dataset Labels
Variable and dataset labels can include punctuation characters. However, special
characters should not be provided, such as,
1. Unbalanced apostrophe, e.g., Parkinson's.
2. Unbalanced single and double quotation marks.
3. Unbalanced parentheses, braces or brackets, e.g., ‘(‘, ‘{‘and ‘[‘.
4. ‘<’ less-than sign and ‘>’ greater-than sign.
4. Study Data Submission Format – Clinical and Nonclinical
4.1 Clinical Data Interchange Standards Consortium
Clinical Data Interchange Standards Consortium (CDISC) is an open, multidisciplinary,
neutral, nonprofit standards development organization (SDO) that has been working
through consensus-based collaborative teams to develop global data standards for clinical
and nonclinical research.
22
Data format specifications for the tabulation datasets of clinical and nonclinical
toxicology studies are provided by SDTM and SEND, respectively, while data format
specifications for the analysis datasets of clinical studies are provided by ADaM. It
should be noted that data format specifications for the analysis datasets of nonclinical
toxicology studies have not been developed yet. As noted in section 1.1, the Standards
Catalog provides a listing of the currently supported data standards with links to
reference materials.
Although the SDTM and SEND formats facilitate review of the data, they do not always
provide the data structured in a way that supports all analyses needed for review.
Analysis files are critical for FDA to understand, on a per subject basis, how the specific
analyses contained in the study report have been created. Therefore, sponsors should
supplement the SDTM with ADaM analysis datasets as described below.
There may be instances in which current implementation guides (e.g., SDTMIG,
SENDIG) do not provide specific instruction as to how certain study data should be
represented. In these instances, sponsors should discuss their proposed solution with the
review division and submit supporting documentation that describes these decisions or
solutions in the appropriate SDRG at the time of submission.
22
See http://www.cdisc.org.

Contains Nonbinding Recommendations
9
4.1.1 Study Data Tabulation Model
4.1.1.1 Definition
The Study Data Tabulation Model (SDTM) defines a standard structure for human
clinical trials tabulation datasets.
4.1.1.2 SDTM General Considerations
It is recommended that sponsors implement the SDTM standard for representation of
clinical trial tabulation data prior to the conduct of the study. The use of case report
forms that incorporate SDTM standard data elements (e.g., Clinical Data Acquisition
Standards Harmonization (CDASH)) allows for a simplified process for the creation of
SDTM domains.
The SDTMIG should be followed unless otherwise indicated in this Guide or in the
Standards Catalog. The conformance criteria listed in the SDTMIG should not be
interpreted as the sole determinant of the adequacy of submitted data. If there is
uncertainty regarding implementation, the sponsor should discuss application-specific
questions with the review division and general standards implementation questions with
the specific center resources identified elsewhere in this Guide (See section 1.2). Each
submitted SDTM dataset should have its contents described with complete metadata in
the define.xml file (See section 4.1.4.5) and within the cSDRG as appropriate (See
section 2.2). No data should be imputed in SDTM datasets. Data should only be imputed
in ADaM datasets (See section 4.1.2.9).
Except for variables that are defined in the SDTMIG as being coded, no numerically
coded variables should typically be submitted as part of the SDTM datasets. Numeric
values generated from validated scoring instruments or questionnaires do not represent
codes, and therefore have no relevance for this issue. There may be special instances
when codes are preferred, hence sponsors should refer to the review division for
direction, if there are any questions.
Subject Identifier (SUBJID)
The SUBJID is an ID of the entity (i.e., person) that participates in a trial. If the same
subject is screened more than once in a trial, then the subject’s SUBJID should be
different.

Contains Nonbinding Recommendations
10
Unique Subject Identifier (USUBJID)
Each individual subject should be assigned a single unique identifier across the entire
application. This is in addition to the subject ID (SUBJID) used to identify subjects in
each study and its corresponding study report. An individual subject should have the
exact same unique identifier across all datasets, including between SDTM and ADaM
datasets. Subjects that participate in more than one study should maintain the same
USUBJID across all studies. It is important to follow this convention to enable pooling
of a single subject’s data across studies (e.g., a randomized control trial and an extension
study).
Sponsors should not add leading or trailing spaces to the USUBJID variable in any
dataset. For example, applications have been previously submitted in which the
USUBJID variable for each individual subject appeared to be the same across datasets;
however, in certain datasets, the actual entry had leading zeros added, or zeros added
elsewhere in the entry. This does not allow for machine-readable matching of individual
subject data across all datasets. Improper implementation of the USUBJID variable is a
common error with applications and often requires sponsors to re-submit their data.
Adjudication Data
There are no existing standards or best practices for the representation of adjudication
data as part of a standard data submission. Until standards for adjudication data are
developed, it is advised that sponsors discuss their proposed approach with the review
division and also include details about the presence, implementation approach, and
location of adjudication data in the SDRG.
Whenever adjudication data is provided it should be clearly identified so that the
reviewer can distinguish the results of adjudication from data as originally collected.
4.1.1.3 SDTM Domain Specifications
SUPPQUAL (Supplemental Qualifier)
A SUPPQUAL dataset is a special SDTM dataset that contains non-standard variables
which cannot be represented in the existing SDTM domains. SUPPQUAL should be
used only when key data cannot be represented in SDTM domains. In general, variables
used to support key analyses should not be represented in SUPPQUAL. Discussion with
the review division should occur if the sponsor intends to include important variables
(e.g., that support key analyses) in SUPPQUAL datasets, and reflected in the SDRG.
Contains Nonbinding Recommendations
11
DM Domain (Demographics)
In the DM domain, each subject should have only one single record per study.
Screen failures, when provided, should be included as a record in DM with the ARM
field left blank. For subjects who are randomized in treatment group but not treated, the
planned arm variables (ARM and ARMCD) should be populated, but actual treatment
arm variables (ACTARM and ACTARMCD) should be left blank.
23
DS Domain (Disposition)
When there is more than one disposition event, the EPOCH variable should be used to aid
in distinguishing between them. This will allow identification of the EPOCH in which
each event occurred. If a death of any type occurs, it should be the last record and should
include its associated EPOCH. It is expected that EPOCH variable values will be
determined based on the trial design and thus should be defined clearly and documented
in the define.xml.
SE Domain (Subject Elements)
The Subject Elements domain should be included to aid in the association of subject data
(e.g., findings, events, and interventions) with the study element in which they occurred.
AE Domain (Adverse Events (AE))
Currently, there is no variable in the AE domain that indicates if an AE was “treatment-
emergent.” The AE domain should include all adverse events that were recorded in the
subjects’ case report forms, regardless of whether the sponsor determined that particular
events were or were not treatment-emergent.
The entry of a “Y” for the serious adverse event variable, AESER, should have the
assessment indicated, (e.g., as a death, hospitalization, or disability/permanent damage).
Frequently, sponsors omit the assessment information, even when it has been collected on
the CRF. The criteria that led to the determination should be provided. This information
is critical during FDA review to support the characterization of serious AEs.
Custom Domains
The SDTMIG permits the creation of custom domains if the data do not fit into an
existing domain. Prior to creating a custom domain, sponsors should confirm that the
data do not fit into an existing domain. If it is necessary to create custom domains,
sponsors should follow the recommendations in the SDTMIG. In addition, sponsors
should present their implementation approach in the cSDRG.
23
Although this convention is inconsistent with the SDTMIG, FDA recommends its use so that “Screen
Failure” is not specified as a treatment arm.

Contains Nonbinding Recommendations
12
LB Domain (Laboratory)
The size of the LB domain dataset submitted by sponsors is often too large to process
(See section 3.3.2). This issue can be addressed by splitting a large LB dataset into
smaller datasets according to LBCAT and LBSCAT, using LBCAT for initial splitting.
If the size is still too large, then use LBSCAT for further splitting. For example, use the
dataset name lb1.xpt for chemistry, lb2.xpt for hematology, and lb3.xpt for urinalysis.
Splitting the dataset in other ways (e.g., by subject or file size) makes the data less
useable. Sponsors should submit these smaller files in addition to the larger non-split
standard LB domain file. Sponsors should submit the split files in a separate sub-
directory/split that is clearly documented in addition to the non-split standard LB domain
file in the SDTM datasets directory (See section 7).
Trial Design Model (TDM)
The SDTMIG TDM should be followed to define the treatment groups and planned visits
and assessments that will be experienced by trial subjects. The TDM defines a standard
structure for representing the planned sequence of events and the treatment plan for the
trial. The TDM includes Trial Arms, Trial Elements, Trial Visit, Trial
Inclusion/Exclusion Criteria, Trial Summary, and Trial Disease Assessment.
All TD datasets should be included, as appropriate for the specific clinical trial, in SDTM
submissions as a way to describe the planned conduct of a clinical trial. Specifically, the
Trial Summary (TS) dataset will be used to determine the time of study start. The
requirement to submit using a particular study data standard is dependent on its support
by FDA as listed in the FDA Data Standards Catalog at the time of study start.
TSPARMCD = SSTDTC will allow the determination of the study start date and should
be included in all SDTM submissions.
As noted in section 1.1, the submission of standardized study data will be required
according to the timetable specified in the eStudy Data guidance. Sponsors submitting
legacy data should provide a TS dataset (ts.xpt) which includes the study start date in the
form of SSTDTC (TSPARMCD = SSTDTC) and TSVAL= “yyyy-mm-dd”.
EC Domain (Exposure as Collected)
The Exposure as Collected domain provides for protocol-specified study treatment
administrations, as-collected. The EC domain may address some challenges in providing
a subject’s exposure to study medication.
DD (Death Details)
The Death Details domain provides for supplemental data that are typically collected
when a death occurs, such as the official cause of death.

Contains Nonbinding Recommendations
13
4.1.2 Analysis Data Model
4.1.2.1 Definition
Specifications for analysis datasets for human drug product clinical studies are provided
by the Analysis Data Model (ADaM) and its implementation by the ADaMIG. ADaM
datasets should be used to create and to support the results in clinical study reports,
Integrated Summaries of Safety (ISS), and Integrated Summaries of Efficacy (ISE), as
well as other analyses required for a thorough regulatory review. ADaM datasets can
contain imputed data or data derived from SDTM datasets.
4.1.2.2 General Considerations
Generally, ADaM facilitates FDA review. One of the expected benefits of analysis
datasets that conform to ADaM is that they simplify the programming steps necessary for
performing an analysis. As noted above, ADaM datasets should be derived from the data
contained in the SDTM datasets. There are features built into the ADaM standard that
promote traceability from analysis results to ADaM datasets and from ADaM datasets to
SDTM datasets. To ensure traceability, all SDTM variables utilized for variable
derivations in ADaM should be included in the ADaM datasets when practical. Each
submitted ADaM dataset should have its contents described with complete metadata in
the define.xml file (See section 4.1.4.5) and within the ADRG as appropriate (See section
2.3).
4.1.2.3 Dataset Labels
Each dataset should be described by an internal label that is shown in the define.xml file.
The label names of ADaM datasets should be different from those of the SDTM datasets.
For example, the SDTM adverse event dataset (i.e., AE) and the ADaM adverse event
dataset (i.e., ADAE) should not share the exact same dataset label, such as “Adverse
Events.”
4.1.2.4 Subject Level Analysis Data
Subject Level Analysis Data (ADSL) is the subject-level analysis dataset for ADaM. All
submissions containing standard analysis data should contain an ADSL file for each
study. In addition to the variables specified for ADSL in the ADaMIG such as those
listed below in the core variables section (See section 4.1.2.5); the sponsor should include
multiple additional variables representing various important baseline subject
characteristics / covariates presented in the study protocol. Some examples of baseline
characteristics / covariates include, but are not limited to, disease severity scores such as
Acute Physiology and Chronic Health Evaluation (APACHE) scores
24
, baseline organ
function measurements such as calculated creatinine clearance or Forced Expiratory
Volume in 1 second (FEV1), range categories for continuous variables, and numeric date
variables in non-International Standards Organization (ISO) formats.
24
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985). “APACHE II: a severity of disease
classification system.” Critical Care Medicine, 13 (10): 818–829.29.
Contains Nonbinding Recommendations
14
4.1.2.5 Core Variables
Core variables, which include covariates presented in the study protocol that are
necessary to analyze data, should be included in each ADaM dataset, and are typically
already included in the ADSL dataset (See section 4.1.2.4). The core variables included
in an ADaM dataset should be necessary for the analysis need in that dataset. Examples
of core variables include study/protocol number, center/site number, geographic region,
country, treatment assignment information, sex, age, race, analysis population flags (e.g.,
Intent-to-Treat (ITTFL), Full Analysis Set (FASFL), Safety (SAFFL), and Per-Protocol
(PPROTFL)), and other important baseline demographic variables. Note that all
variables that contain coded data should be accompanied by a variable that provides the
decoded information.
In addition, it is important to note that SDTM datasets do not have core variables (such as
demographic and population variables) repeated across the different domains. The
duplication of core variables across various domains can be fulfilled through their
inclusion in the corresponding analysis datasets. For example, the SDTM AE dataset
does not allow for the inclusion of variables such as treatment arm, sex, age, or race.
These and other variables should be included in the adverse event ADaM dataset (i.e.,
ADAE).
4.1.2.6 Key Efficacy and Safety Variables
Sponsors should submit ADaM datasets to support key efficacy and safety analyses. At
least one dataset should be referenced in the data definition file as containing the primary
efficacy variables. Further, variables pertaining to the primary and secondary endpoints
of a trial, along with their derivations (as applicable), should be provided as well as
documented appropriately (i.e., variable-level metadata or parameter value-level
metadata) in the data definition file.
4.1.2.7 Timing Variables
A variable for relative day of measurement or event, along with timing variables for visit
should be included when an ADaM dataset contains multiple records per subject (i.e.,
repeated measures data).
4.1.2.8 Numeric Date Variables
Numeric date variables are needed for analysis and review purposes. Apply formats to
all numeric date variables using a format that is understandable by SAS XPORT Version
5 files as per Section 3.3.1 above. The software specific (as opposed to trial specific)
date of reference used to calculate numeric dates should be specified within the ADRG.
In the event of partial dates, imputation should be performed only for dates required for
analysis according to the SAP, and appropriate corresponding ADaM imputation flags
should be utilized. When numeric time or date time variables are needed, all
considerations apply as previously discussed for numeric dates.
For traceability purposes, SDTM character dates formatted as ISO 8601 should be
included in the ADaM datasets as well.
Contains Nonbinding Recommendations
15
4.1.2.9 Imputed Data
When data imputation is utilized in ADaM, sponsors should submit the relevant
supporting documentation (i.e., define.xml and ADRG) explaining the imputation
methods.
4.1.2.10 Software Programs
Sponsors should provide the software programs used to create all ADaM datasets along
with the tables and figures associated with primary and secondary efficacy analyses in
order to help reviewers to better understand how the datasets, tables and figures were
created. The specific software utilized should be specified in the ADRG. The main
purpose of requesting the submission of these programs is to understand the process by
which the variables for the respective analyses were created and to confirm the analysis
algorithms. Sponsors should not submit software programs with executable file
extensions. Sponsors should submit in ASCII text format.
4.1.3 Standard for Exchange of Nonclinical Data
4.1.3.1 Definition
The Standard for Exchange of Nonclinical Data (SEND) provides the organization,
structure, and format of standard nonclinical (animal toxicology studies) tabulation
datasets for regulatory submission. Currently, the SEND Implementation Guide
(SENDIG) supports single-dose general toxicology, repeat-dose general toxicology, and
carcinogenicity studies.
4.1.3.2 General Considerations
The SENDIG provides specific domain models, assumptions, conformance and business
rules, and examples for preparing standard tabulation datasets that are based on the
SDTM. If there is uncertainty regarding SEND implementation, the sponsor should
discuss the issue with the review division.
The ideal time to implement SEND is prior to the conduct of the study as it is very
important that the results presented in the accompanying study report be traceable back to
the original data collected. Each submitted SEND dataset should have its contents
described with complete metadata in the define.xml file (See section 4.1.4.5) and within
the nSDRG as appropriate (See section 2.2).
Sponsors should use the VISITDY variable if findings which were intended to be
analyzed together were collected across multiple study days. This includes postmortem
findings in OM, MA, MI, terminal body weight in BW, and in-life observations in other
Findings domains that are grouped in the Study Report. For example, an ECG might be
collected on Day 20, determined to be uninterpretable, and repeated on Day 21. If those
ECG findings are grouped for analysis in the Study Report, VISITDY should be provided
and set to Day 20 for both ECG collections to provide traceability in the SEND dataset.

Contains Nonbinding Recommendations
16
4.1.3.3 SEND Domain Specification
SUPPQUAL (Supplemental Qualifier)
A SUPPQUAL dataset is a special SEND dataset that contains non-standard variables
which cannot be represented in the existing SEND domains. Discussion with the review
division should occur if the sponsor intends to include important variables (i.e., that
support key analyses) in SUPPQUAL datasets and this should be reflected in the nSDRG.
Currently, SUPPQUAL should be used to capture some collected information (e.g.,
pathology modifiers) until the SEND is further refined to adequately represent such
information.
Microscopic Findings (MI) Domain
Sponsors should ensure that the transformation of findings from MIORRES to
MISTRESC closely adheres to the instructions in the SENDIG. Modifiers for which there
are variables available (e.g. MISEV, MILAT, etc.) should be placed appropriately.
Severities (e.g., minimal, mild, etc.) should be placed in MISEV, and not duplicated in
MISTRESC or SUPPMI. Non-neoplastic findings in MISTRESC, where controlled
terminology has not yet been established, should be standardized in a way to ensure
traceability between counts in tables, listings, and figures and the terms in MISTRESC.
Clinical Observations (CL) Domain
Only Findings should be provided in CL; ensure that Events and Interventions are not
included. Sponsors should ensure that the standardization of findings in CLSTRESC
closely adheres to the SENDIG. The information in CLTEST and CLSTRESC, along
with CLLOC and CLSEV when appropriate, should contain sufficient information to
ensure traceability between counts in tables, listings, and figures to the unique terms in
CLSTRESC. For example, if “vomitus, food” and “vomitus, clear” are tabulated
separately in the study report, CLSTRESC should be standardized to “vomitus, food” and
“vomitus, clear” rather than “vomitus”. Differences between the representation in CL and
the presentation of Clinical Observations in the Study Report should be mentioned in the
nSDRG.
Custom Domains
The SENDIG allows for the creation of custom domains if the data do not fit into an
existing domain.
Trial Design Model (TDM)
The TDM defines a collection of domains which describe the planned study design.
All TD datasets should be included in SEND submissions as a way to describe the
planned conduct of a nonclinical trial. Specifically, the Trial Summary (TS) dataset will
be used to determine the time of study start. The requirement to submit using a particular
study data standard is dependent on its support by FDA as listed in the FDA Data
Standards Catalog at the time of study start. TSPARMCD = STSTDTC will allow the
determination of the study start date and should be included in all SEND submissions.

Contains Nonbinding Recommendations
17
Ensure that Trial Arms and Trial Sets represented in TA and TX closely adhere to the
SENDIG in study designs with recovery and/or toxicokinetic animals. Recovery and/or
toxicokinetic animals should typically be presented in separate Trial Sets from the main
arm.
As noted in section 1.1, the submission of standardized study data will be required
according to the timetable specified in the eStudy Data guidance. Sponsors submitting
legacy data should provide a TS dataset (ts.xpt) which includes the study start date in the
form of TSPARMCD = STSTDTC and TSVAL= “yyyy-mm-dd.
Tumor Dataset
Carcinogenicity studies should include an electronic dataset of tumor findings to allow
for a complete review. At this time sponsors should include a tumor.xpt file while
following the specification in the SENDIG for its creation regardless of whether or not
the study is in SEND format (See www.cdisc.org/send).
4.1.4 General Considerations: SDTM, SEND, and/or ADaM
4.1.4.1 Variables in SDTM and SEND: Required, Expected, and Permissible
CDISC data standards categorize SDTM and SEND variables as being Required,
Expected, and Permissible. In some instances, sponsors have interpreted Permissible
variables as being optional and, in other cases, sponsors have excluded Expected
variables. For the purposes of SDTM and SEND submissions, all Required, Expected,
and Permissible variables that were collected, plus any variables that are used to compute
derivations, should be submitted.
25
SDTM datasets should not contain imputed data. FDA recognizes that SDTM contains
certain operationally derived variables that have standard derivations across all studies
(e.g., --STDY, EPOCH). If the data needed to derive these variables are missing, then
these variables cannot be derived and the values should be null. The following are
examples of some of the Permissible and Expected variables in SDTM and SEND that
should be included, if available:
1. Baseline flags (e.g., last non-missing value prior to first dose) for Laboratory
results, Vital Signs, ECG, Pharmacokinetic Concentrations, and Microbiology
results. Currently, for SDTM, baseline flags should be submitted if the data were
collected or can be derived.
2. EPOCH designators. Please follow CDISC guidance for terminology.
26
The
variable EPOCH should be included for clinical subject-level observation (e.g.,
adverse events, laboratory, concomitant medications, exposure, and vital signs).
This will allow the reviewer to easily determine during which phase of the trial
25
See CDISC SDTM Implementation Guide at www.cdisc.org for additional information on variables
referenced throughout this Guide
26
See http://www.cancer.gov/cancertopics/terminologyresources/page6.
Contains Nonbinding Recommendations
18
the observation occurred (e.g., screening, on-therapy, follow-up), as well as the
actual intervention the subject experienced during that phase.
3. Whenever --DTC, --STDTC or --ENDTC, which have the role of timing
variables, are included, the matching Study Day variables (--DY, --STDY, or --
ENDY, respectively) should be included. For example, in most Findings
domains, --DTC is Expected, which means that --DY should also be included. In
the Subject Visits domain, SVSTDTC is Required and SVENDTC is Expected;
therefore, both SVSTDY and SVENDY should be included.
4.1.4.2 Dates in SDTM and SEND
Dates in SDTM and SEND domains should conform to the ISO 8601 format. Examples
of how to implement dates are included in the SDTMIG and SENDIG.
27
4.1.4.3 Naming Conventions in SDTM and SEND
Naming conventions (variable name and label) and variable formats should be followed
as specified in the SDTMIG and SENDIG.
4.1.4.4 SDTM and SEND Versions
When submitting clinical or nonclinical data, sponsors should not mix versions within a
study. As noted above, the Standards Catalog lists the versions that are supported by
FDA.
4.1.4.5 Data Definition Files for SDTM, SEND, and ADaM
The data definition file describes the metadata of the submitted electronic datasets, and is
considered arguably the most important part of the electronic dataset submission for
regulatory review. This data definition specification for submitted datasets defines the
metadata structures that should be used to describe the datasets, variables, possible values
of variables when appropriate, and controlled terminologies and codes. An insufficiently
documented data definition file is a common deficiency that reviewers have noted.
Consequently, the sponsor needs to provide complete detail in this file, especially for the
specifications pertaining to derived variables. In addition, sponsors should also make
certain that the code list and origin for each variable are clearly and easily accessible
from the data definition file. The version of any external dictionary should be clearly
stated both in the data definition file and, where possible, in the updated Trial Summary
(TS) domain (i.e., SDTMIG 3.1.2 or greater; SENDIG 3.0 or greater). The internal
dataset label should also clearly describe the contents of the dataset. For example, the
dataset label for an efficacy dataset might be “Time to Relapse (Efficacy).”
Separate data definition files should be included for each type of electronic dataset
submission, i.e., a separate data definition file for the SDTM datasets of a given clinical
study, a separate data definition file for the SEND datasets of a given nonclinical study,
and a separate data definition file for the ADaM datasets of a given clinical study. The
data definition file should be submitted in XML format, i.e., a properly functioning
define.xml
28
. In addition to the define.xml, a printable define.pdf should be provided if
27
See http://www.cdisc.org
28
See http://www.cdisc.org/define-xml

Contains Nonbinding Recommendations
19
the define.xml cannot be printed
29
. To confirm that a define.xml is printable within the
CDER IT environment, it is recommended that the sponsor submit a test version to cder-
edata@fda.hhs.gov prior to application submission. The Standards Catalog lists the
currently supported version(s) of define.xml. It should be noted that define.xml version
2.0 is the preferred version. Sponsors should include a reference to the style sheet as
defined in the specification and place the corresponding style sheet in the same
submission folder as the define.xml file.
4.1.4.6 Annotated Case Report Form (aCRF) for SDTM
An Annotated Case Report Form (aCRF) is a PDF document that maps the clinical data
collection fields used to capture subject data (electronic or paper) to the corresponding
variables or discrete variable values contained within the SDTM datasets. Regardless of
whether the clinical database is legacy or SDTM compliant, an aCRF should be
submitted. The aCRF should be provided as a PDF with the file name “acrf.pdf.”
30
The
SDTM Metadata Submission Guidelines should be used for additional information on
annotated CRFs.
31
The aCRF should include treatment assignment forms, when applicable, and should map
each variable on the CRF to the corresponding variables in the datasets (or database). The
aCRF should include the variable names and coding for each CRF item.
When data are recorded on the CRF but are not submitted, the CRF should be annotated
with the text "NOT SUBMITTED.” There should be an explanation in the SDRG stating
why data have not been submitted.
5. Therapeutic Area Standards
5.1 General
CDISC Therapeutic Area (TA) Standards are comprised of existing data elements, but
may introduce new data elements (e.g. domains, variables, terminologies). These data
elements are components of current CDISC implementation guides or will be integrated
into future implementation guides. CDISC publishes a user guide for each therapeutic
area use case which describes the most common data elements for clinical studies
(http://www.cdisc.org/therapeutic). The CDISC Therapeutic Area User Guide (TAUG)
shall not be interpreted as FDA guidance, and may be used as a reference/use case for the
therapeutic area standard.
29
Detailed FDA PDF specifications are located on FDA’s Electronic Common Technical Document
(eCTD) Web site,
http://www.fda.gov/drugs/developmentapprovalprocess/formssubmissionrequirements/electronicsubmissio
ns/ucm153574.htm
30
Previously acrf.pdf was called blankcrf.pdf.
31
See Study Data Tabulation Model Metadata Submission Guidelines (SDTM-MSG)
(http://www.cdisc.org/sdtm).
Contains Nonbinding Recommendations
20
5.2 Supported Therapeutic Areas
Generally, when a data standard is released for public use by the SDO, it is not supported
by FDA until FDA performs acceptance testing to determine its ability to support new
TA data elements. The sponsor may use the new data elements listed in a Therapeutic
Area User Guide (TAUG) but they are not required until the data elements are included
in a SDTMIG version supported by FDA (the supported SDTMIG is listed in the Data
Standards Catalog). When using new data elements that are not in a SDTMIG currently
supported by FDA, sponsors should describe the rationale for their use in the cSDRG.
The CDISC data elements associated with the following therapeutic areas are currently
supported by FDA (the list will not be published in the Data Standards Catalog):
5.2.1 Chronic Hepatitis C
5.2.2 Dyslipidemia
5.2.3 Diabetes
5.2.4 QT Studies
5.2.5 Tuberculosis
6. Terminology
6.1 General
Common dictionaries should be used across all clinical studies and throughout the
submission for each of the following: adverse events, concomitant medications,
procedures, indications, study drug names, and medical history. FDA recommends that
sponsors use, where appropriate, the terminologies supported and listed in the Standards
Catalog. It is important that coding standards, if they exist, be followed (e.g., ICH
Medical Dictionary for Regulatory Activities (MedDRA) Term Selection: Points-to-
Consider document). Frequently, sponsors submit data that do not conform to
terminology standards, for example, misspelling of MedDRA or WHO Drug terms, lack
of conformance to upper / lower case, or the use of hyphens. All controlled terms
submitted in datasets should conform to the exact case and spelling used by the
terminology maintenance organization (e.g., MedDRA, CDISC controlled terminology).
These conformance issues make it difficult to use or develop automated review and
analysis tools. The use of a dictionary that is sponsor-defined or an extension of a
standard dictionary should be avoided if possible, but, if essential, its use should be
documented in the define.xml file and the SDRG.
Contains Nonbinding Recommendations
21
6.1.1 Controlled Terminologies
Controlled terminology standards are an important component of study data
standardization and are a critical component of achieving semantically interoperable data
exchange (See Appendix). Generally, controlled terminology standards specify the key
concepts that are represented as definitions, preferred terms, synonyms, codes, and code
system.
The analysis of study data is greatly facilitated by the use of controlled terms for clinical
or scientific concepts that have standard, predefined meanings and representations.
Standard terminology for adverse events perhaps represents the earliest example of using
standards for study data. For example, myocardial infarction and heart attack are
synonyms, and as such should be mapped to the same term in a standard dictionary. This
level of standardization facilitates an efficient analysis of events that are coded to the
standard term. In electronic study data submissions, sponsors should provide the actual
verbatim terms that were collected (e.g., on the case report form), as well as the coded
term.
Controlled terminology is also useful when consistently applied across studies to
facilitate integrated analyses (that are stratified by study) and cross-study comparative
analyses (e.g., when greater statistical power is needed to detect important safety signals).
Cross-study comparisons and pooled integrated analyses occasionally provide critical
information for regulatory decisions, such as statistical results that support
effectiveness,
32
as well as important information on exposure-response relationships
33
and population pharmacokinetics
34
.
6.1.2 Use of Controlled Terminologies
FDA recognizes that studies are conducted over many years, during which time versions
of a terminology may change. Generally, FDA expects sponsors to use the most current
version of an FDA-supported terminology available at the time of coding. It is
acceptable to have different studies use different versions of the same dictionary within
the same application. There are some situations where it may be acceptable to use a
single older version of a dictionary across multiple studies, even though that version may
32
See the guidance for industry Providing Clinical Evidence of Effectiveness for Human Drugs and
Biological Products, available at
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm072008.
pdf. We update guidance periodically. To make sure you have the most recent version of guidance, check
the FDA Drugs guidance Web page at
http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm.
33
See the guidance for industry Exposure-Response Relationships — Study Design, Data Analysis, and
Regulatory Applications,
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm072109.
pdf.
34
See the guidance for industry Population Pharmacokinetics, available at
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm072137.
pdf.

Contains Nonbinding Recommendations
22
not be the most current for the later studies. The study data submission should describe
the impact, if any, of the older version on the study results in the SDRG. For example, if
the sponsor anticipates pooling coded data across multiple studies, then it may be
desirable to use a single version across those studies to facilitate pooling. If a sponsor
selects this approach, then the approach and the justification should be documented in the
Standardization Plan, or in an update to the plan.
Regardless of the specific versions used for individual studies, pooled analyses of coded
terms across multiple studies (e.g., for an integrated summary of safety) should be
conducted using a single version of a terminology. This will ensure a consistent and
coherent comparison of clinical and scientific concepts across multiple studies. Sponsors
should specify the terminologies and versions used in the study in the SDRG.
6.1.2.1 Use of the specific controlled term “OTHER”
It is understood that the expansion of controlled terminology may lag behind scientific
advancement, and that sometimes there may not be a relevant term within a controlled
terminology’s value set to describe a clinical trial event, finding, or observation.
However, it is not recommended to map a collected value to “OTHER” when there is a
controlled term available to match the collected value – even when the terminology
allows for Sponsor expansion. Each unique value in a --TERM field mapped to a --
DECODE value of “OTHER” should have a clear rationale outlined in the Study Data
Reviewer’s Guide (clinical or non-clinical).
6.1.3 Maintenance of Controlled Terminologies
The use of supported controlled terminologies is recommended wherever available. If a
sponsor identifies a concept for which no standard term exists, FDA recommends that the
sponsor submit the concept to the appropriate terminology maintenance organization as
early as possible to have a new term added to the standard dictionary. FDA considers
this good terminology management practice. The creation of custom terms (i.e., so-
called extensible code lists) for a submission is discouraged, because this does not
support semantically interoperable study data exchange. Furthermore, the use of custom
or “extensible” code lists should not be interpreted to mean that sponsors may substitute
their own nonstandard terms in place of existing equivalent standardized terms.
Terminology maintenance organizations generally have well-defined change control
processes. Sponsors should allow sufficient time for a proposed term to be reviewed and
included in the terminology, as it is desirable to have the term incorporated into the
standard terminology before the data are submitted. If custom terms cannot be avoided,
the submitter should clearly identify and define them within the submission, reference
them in the SDRG, and use them consistently throughout the application.
If a sponsor identifies an entire information domain
35
for which FDA has not accepted a
specific standard terminology, they may select a standard terminology to use, if one
35
By information domain, we mean a logical grouping of clinical or scientific concepts that are amenable
to standardization (e.g., adverse event data, laboratory data, and histopathology data, imaging data).
Contains Nonbinding Recommendations
23
exists. FDA recommends that sponsors include this selection in the Standardization Plan
(See section 2.1) or in an update to the existing plan, and reference it in the SDRG. If no
controlled terminology exists, the sponsor may define custom terms. The non-FDA
supported terms (whether from a non-supported standard terminology or sponsor-defined
custom terms) should then be used consistently throughout all relevant studies within the
application.
6.2 CDISC Controlled Terminology
Sponsors should use the terminologies and code lists in the CDISC Controlled
Terminology, which can be found at the NCI (National Cancer Institute) Enterprise
Vocabulary Services.
36
For variables for which no standard terms exists, or if the
available terminology is insufficient, the sponsor should propose its own terms. The
sponsor should provide this information in the define.xml file and in the SDRG.
6.3 Adverse Events
6.3.1 MedDRA
6.3.1.1 General Considerations
MedDRA should be used for coding adverse events. The spelling and capitalization of
MedDRA terms should match the way the terms are presented in the MedDRA dictionary
(e.g., spelling and case). Common errors that have been observed include the incorrect
spelling of a System Organ Class (SOC) and other MedDRA terms.
Generally, the studies included in an application are conducted over many years and may
have used different MedDRA versions. To avoid potential confusion or incorrect results,
the preparation of the adverse event dataset for the ISS should include MedDRA
Preferred Terms from a single version of MedDRA. The reason for an ISS based on a
single version of MedDRA is that reviewers often analyze adverse events across studies,
including the use of Standardized MedDRA Queries.
37
In addition, sponsors should use
the MedDRA-specified hierarchy of terms. The SDTM variables for the different
hierarchy levels should represent MedDRA-specified primary SOC-coded terms.
6.4 Medications
6.4.1 FDA Unique Ingredient Identifier
6.4.1.1 General Considerations
The FDA Unique Ingredient Identifier (UNII)
38
should be used to identify active
ingredients (specifically, active moieties) that are administered to investigational subjects
in a study (either clinical or nonclinical). This information should be provided in the
SDTM Trial Summary (TS) domain. UNIIs should be included for all active moieties of
investigational products (TSPARM=TRT or TRTUNII), active comparators
36
See http://www.cancer.gov/cancertopics/terminologyresources/page6.
37
See http://www.meddra.org/standardised-meddra-queries.
38
See http://www.fda.gov/ForIndustry/DataStandards/SubstanceRegistrationSystem-
UniqueIngredientIdentifierUNII/

Contains Nonbinding Recommendations
24
(TSPARM=COMPTRT), and any protocol-specified background treatments
(TSPARM=CURTRT).
If a medicinal product has more than one active moiety, then multiple records in TS
should be provided, one for each active moiety. For example, if the investigational
product is Bactrim (a combination of sulfamethoxazole and trimethoprim), then TS will
contain two records for TSPARM=TRT: one for sulfamethoxazole and one for
trimethoprim.
The preferred substance names and UNII codes can be found by searching FDA’s
Substance Registration System, hosted by the National Library of Medicine.
39
We
recognize that unapproved substances may not yet have registered UNII codes. We
recommend that sponsors obtain UNII codes for unapproved substances as early in drug
development as possible, so that relevant information, such as study data, can be
unambiguously linked to those substances.
6.4.2 WHO Drug Dictionary
6.4.2.1 General Considerations
World Health Organization (WHO) Drug Dictionary
40
is a dictionary maintained and
updated by Uppsala Monitoring Centre. WHO Drug Dictionary contains unique product
codes for identifying drug names and evaluating medicinal product information,
including active ingredients and therapeutic uses.
Typically, WHO Drug is used to code concomitant medications. --DECOD should be
populated with the generic name from the WHO dictionary, and --CLAS populated with
the drug class, if the utilized dictionary codes drugs to a single class. When using
WHODRUG, generally, --CLAS would not be filled because a drug may have multiple
classes. However, one Anatomic Therapeutic Code (ATC) level 4 code could be mapped
to --CLAS and the remainder of the ATC codes could be placed in SUPPCM.
6.5 Pharmacologic Class
6.5.1 National Drug File -- Reference Terminology
6.5.1.1 General Considerations
The Veterans Administration’s National Drug File – Reference Terminology (NDF-RT)
41
should be used to identify the pharmacologic class(es) of all active investigational
substances that are used in a study (either clinical or nonclinical). This information
should be provided in the SDTM Trial Summary (TS) domain. The information should
be provided as one or more records in TS, where TSPARM=PCLAS.
39
The Substance Registration System can be accessed at http://fdasis.nlm.nih.gov/srs
40
See http://www.who-umc.org/
41
See http://mor.nlm.nih.gov/download/rxnav/NdfrtAPIs.html#
Contains Nonbinding Recommendations
25
Pharmacologic class is a complex concept that is made up of one or more component
concepts: mechanism of action (MOA), physiologic effect (PE), and chemical structure
(CS).
42
The established pharmacologic class is generally the MOA, PE, or CS term that
is considered the most scientifically valid and clinically meaningful. Sponsors should
include in TS the established pharmacologic class of all active moieties of investigational
products used in a study. FDA maintains a list of established pharmacologic classes of
approved moieties.
43
If the established pharmacologic class is not available for an active
moiety, then the sponsor should discuss the appropriate MOA, PE, and CS terms with the
review division. For unapproved investigational active moieties where the
pharmacologic class is unknown, the PCLAS record may not be available.
6.6 Indication
6.6.1 SNOMED CT
6.6.1.1 General Considerations
The International Health Terminology Standards Organization’s (IHTSDO) Systematized
Nomenclature of Medicine – Clinical Terms (SNOMED CT)
44
should be used to identify
the medical condition or problem that the investigational product in a study is intended to
affect (treat, diagnose or prevent, i.e., the indication). This information should be
provided in the SDTM Trial Summary (TS) domain as a record where TSPARM=INDIC
and TSPARM=TDIGRP. SNOMED CT was chosen to harmonize with Indication
information in Structured Product Labeling (SPL)
45
. A reviewer should be able to take
the indication term from product labeling and readily search for clinical or nonclinical
studies of that indication without having to translate.
6.7 Laboratory Tests
6.7.1 LOINC
6.7.1.1 General Considerations
The Logical Observation Identifiers Names and Codes (LOINC) is a clinical terminology
housed by the Regenstrief Institute.
46
LOINC codes are universal identifiers for
laboratory and other clinical observations that enable semantically interoperable clinical
data exchange. The laboratory portion of the LOINC database contains the categories of
chemistry, hematology, serology, microbiology (including parasitology and virology),
toxicology, and more.
42
See the guidance for industry and review staff Labeling for Human Prescription Drug and Biologic
Products —Determining Established Pharmacologic Class for Use in the Highlights of Prescribing
Information, available at
http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm186607.
pdf.
43
Available at
http://www.fda.gov/downloads/ForIndustry/DataStandards/StructuredProductLabeling/UCM346147.zip
44
http://www.ihtsdo.org/snomed-ct/.
45
See http://www.fda.gov/ForIndustry/DataStandards/StructuredProductLabeling/ucm163377.htm.
46
See http://www.regenstrief.org/
Contains Nonbinding Recommendations
26
The SDTM already supports the exchange of LOINC codes using the LBLOINC
variable.
7. Electronic Submission Format
7.1 eCTD File Directory Structure
Study datasets and their supportive files should be organized into a specific file directory
structure when submitted in the eCTD
47
format (See Figure 1 and Table 2 below). Note
that this structure is distinct from the eCTD headings and hierarchy folder structure, and
does not affect it. Submission of files within the appropriate folders allows automated
systems to detect and prepare datasets for review, and minimizes the need for manual
processing.
The define.xml and supportive style sheet should reside in the same folder as the datasets
they pertain to (e.g., for SDTM, place in “tabulations\sdtm\”). Do not submit empty file
folders. Do not submit additional subfolders. If you feel that additional folders are
needed, please consult with the appropriate center in advance for guidance.
If you need to split a file that exceeds file size limits (See section 3.3.2), you should
submit the smaller split files in the “split” sub-folder in addition to the larger non-split
file in the original data folder. There is no need for a second define.xml file to be
submitted within the split subfolder.
47
See http://www.ich.org/products/ctd.html.
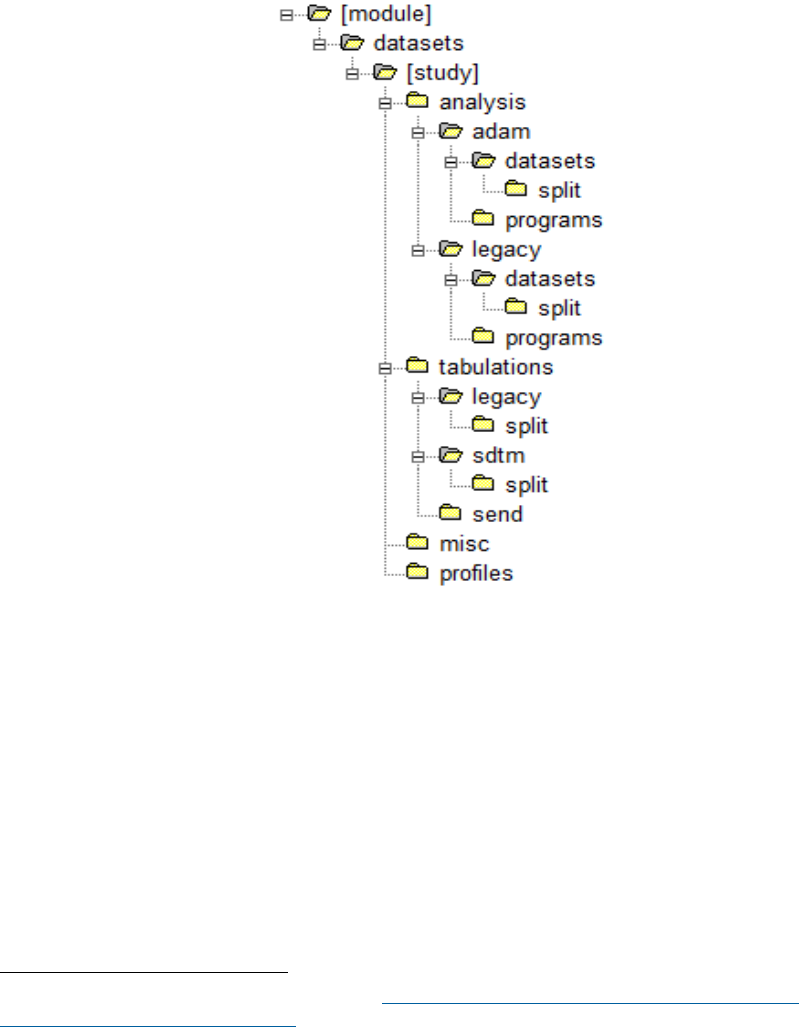
Contains Nonbinding Recommendations
27
For information on how to incorporate datasets into the eCTD, please reference the
“Guidance to Industry Providing Regulatory Submissions in Electronic Format: Certain
Human Pharmaceutical Product Applications and Related Submissions Using the
Electronic Common Technical Document Specifications.” .
48
The file folder structure
for study datasets is summarized in Figure 1. Table 2 provides the study dataset and file
folder structure and associated description.
Figure 1: Folder Structure for Study Datasets
48
See “eCTD Technical Conformance Guide” (Electronic Common Technical Document Technical
Conformance Guide (PDF – 160KB)) for further details.
Contains Nonbinding Recommendations
28
Table 2: Study Dataset and File Folder Structure and Description
Folder Name Folder Level Description/Contents
[module]
1
Refers to the eCTD module in which study data is being
submitted. Name this folder m4 for nonclinical data and
m5 for clinical data. Do not place files at this level.
datasets
2
Resides within the module folder as the top-level folder
for study data (nonclinical or clinical) being submitted for
the specified module (m4 or m5). Do not place files at
this level.
[study]
3
Name this folder with the study identifier or analysis
type performed (e.g., study123, iss, ise). Do not place
files at this level.
analysis
4
Contains folders for analysis datasets and software
programs; arrange in designated level 6 subfolders. Do
not place files at this level.
adam
5
Contains subfolders for ADaM datasets and
corresponding software programs. Do not place files at
this level.
datasets
6
Place ADaM datasets in this subfolder.
split
7
Place any split ADaM datasets in this subfolder.
programs
6
Place software programs for ADaM datasets, tables and
figures in this subfolder.
legacy
5
Contains legacy formatted analysis datasets and
corresponding software programs. Do not place files at
this level.
datasets
6
Place legacy analysis datasets in this subfolder.
split
7
Place split legacy analysis datasets in this subfolder.
programs
6
Place software programs for legacy analysis datasets,
tables and figures in this subfolder.
misc
4
Place miscellaneous datasets that don’t qualify as
analysis, profile, or tabulation datasets in this subfolder.
This subfolder was formerly named “listings”.
profiles
4
Place patient profiles in this subfolder.
tabulations
4
Contains subfolders for tabulation datasets. Do not
place files at this level.
legacy
5
Place legacy (non-standardized) tabulation datasets in
this folder.
split
6
Place any split legacy tabulations datasets in this
subfolder.
sdtm
5
Place SDTM tabulation datasets in this subfolder. Should
only be used in m5 for clinical data.
split
6
Place any split SDTM files in this subfolder.
send
5
Place SEND tabulation datasets in this subfolder. Should
only be used in m4 for animal data.
Contains Nonbinding Recommendations
29
7.2 eCTD Sample Submission
CDER would like to work closely with people who plan to provide a submission using
the eCTD specifications and offer to help smooth the process. The agency also offers a
process for submitting sample standardized datasets for validation. Sample submissions
are tests only and not considered official submissions. They are not reviewed by FDA
reviewers at any time. The Electronic Submissions page provides more information
regarding test submission process.
49
8. Study Data Validation and Traceability
8.1 Definition of Data Validation
For purposes of this Guide, data validation is a process that attempts to ensure that
submitted data are both compliant and useful. Compliant means the data conform to the
applicable and required data standards. Useful means that the data support the intended
use (i.e., regulatory review and analysis).
8.2 Study Data Validation Rules
Study data validation relies on a set of rules that are used to verify that study data
conform to a minimum set of quality standards. The data validation process can identify
data issues early in the review that may adversely affect the use of the data. FDA
recognizes that it is impossible or impractical to define a priori all the relevant validation
rules for any given submission. Sometimes serious issues in the submitted data are only
evident through manual inspection of the data and may only become evident once the
review is well under way. Often these issues are due to problems in data content (i.e.,
what was or was not submitted, or issues with the collection of original source data),
and not necessarily how the data were standardized.
8.2.1 Types of Study Data Validation Rules
Study data validation is performed using rules that assess whether the data:
1. Conform to a standard listed in the FDA Data Standards Catalog
2. Support regulatory review and analysis.
8.2.1.1 Conformance Rules
Conformance validation rules help ensure that the data conform to the study data
standards listed in the FDA Data Standards Catalog. Standards Development
Organizations (e.g., CDISC) should develop and provide access to rules that assess
conformance to its published standards.
49
See:
http://www.fda.gov/Drugs/DevelopmentApprovalProcess/FormsSubmissionRequirements/ElectronicSubmi
ssions/ucm174459.htm

Contains Nonbinding Recommendations
30
8.2.1.2 FDA Business Rules
FDA business rules help to ensure that study data will support meaningful review and
analysis. FDA’s list of business rules will grow and change with agency understanding
and experience. The FDA may publish additional business rules preferring a particular
option when multiple options are offered within a standard.
8.2.2 Support on Data Validation Rules
The Standards Web page
50
provides links to the currently available business rules.
Sponsors should validate their study data before submission using the conformance rules
published by an SDO and the FDA business rules. Sponsors should either correct any
validation errors or explain in the Reviewer’s Guide (i.e., nSDRG, cSDRG or ADRG)
why certain validation errors could not be corrected. The recommended pre-submission
validation step is intended to minimize the presence of validation errors at the time of
submission.
8.3 Study Data Traceability
8.3.1 Overview
An important component of a regulatory review is an understanding of the provenance of
the data (i.e., traceability of the sponsor’s results back to the CRF data). Traceability
permits an understanding of the relationships between the analysis results (tables, listings
and figures in the study report), analysis datasets, tabulation datasets, and source data.
Traceability enables the reviewer to accomplish the following:
Understand the construction of analysis datasets
Determine the observations and algorithm(s) used to derive variables
Understand how the confidence interval or the p-value was calculated in a
particular analysis
Relate counts from tables, listings, and figures in a study report to the underlying
data
Based upon reviewer experience, establishing traceability is one of the most problematic
issues associated with legacy study data converted to standardized data. If the reviewer is
unable to trace study data from the data collection of subjects participating in a study to
the analysis of the overall study data, then the regulatory review of a submission may be
compromised. Traceability can be enhanced when studies are prospectively designed to
collect data using a standardized CRF, e.g., CDASH. Traceability can be further
enhanced when a flow diagram is submitted showing how data move from collection
through preparation and submission to the Agency.
50
See: http://www.fda.gov/downloads/ForIndustry/DataStandards/StudyDataStandards/UCM384744.pdf
Contains Nonbinding Recommendations
31
8.3.2 Legacy Study Data Conversion to Standardized Study Data
Sponsors should use processes for legacy data conversion that account for traceability.
Generally, a conversion to a standard format will map every data element as originally
collected to a corresponding data element described in a standard. Some study data
conversions will be straightforward and will result in all data converted to a standardized
format. In some instances, it may not be possible to represent a collected data element as
a standardized data element. In these cases, there should be an explanation in the SDRG
as to why certain data elements could not be fully standardized or were otherwise not
included in the standardized data submission. The legacy data (i.e., aCRF, legacy
tabulation data, and legacy analysis data) may be needed in addition to the submission of
converted data.
In cases where the data were collected on a Case Report Form (CRF) or electronic CRF
but were not included in the converted datasets, the omitted data should be apparent on
the annotated CRF and described in the SDRG. The tabular list of studies in the
Standardization Plan should indicate which studies contained previously collected non-
standard data that were subsequently converted to a standard format.
8.3.2.1 Traceability Issues with Legacy Data Conversion
FDA does not recommend a particular approach to legacy study data conversion, but
rather explains the issues that should be addressed so that the converted data are traceable
and adequate to support review.
Table 3 presents some of the issues that can be observed during a review when legacy
study data are converted to SDTM and submitted with legacy analysis datasets.
Table 3: Traceability Issues: Legacy Data Conversion to SDTM Only
1. Limited ability to determine location of collected CRF variables in the converted
SDTM data unless the legacy aCRF is re-annotated.
2. Limited traceable path from SDTM to the legacy analysis data.
3. Limited ability to replicate/confirm legacy analysis datasets (i.e., analysis
variable imputation or derived variables) using SDTM datasets.
4. Limited ability to confirm derivation of intermediate analysis datasets or custom
domains.
5. Difficulty in understanding the source or derivation methods for imputed or
derived variables in integrated/pooled data, supplemental qualifiers, and related
records.
Contains Nonbinding Recommendations
32
Table 4 presents the issues when legacy study data and legacy analysis data are
independently converted to SDTM and ADaM formats, respectively, rather than ADaM
datasets being created directly from the SDTM datasets (converted from legacy study
data).
Table 4: Traceability Issues: Independent Legacy Data Conversion to SDTM
and ADaM
Issues
1. Limited ability to determine location of collected CRF variables in the converted
SDTM data unless the legacy aCRF is re-annotated.
2. Limited traceable path from SDTM to the legacy analysis data.
3. Limited ability to replicate/confirm legacy analysis datasets (i.e., analysis
variable imputation or derived variables) using SDTM datasets.
4. Limited ability to confirm derivation of intermediate analysis datasets or custom
domains.
5. Limited traceable path from SDTM to the ADaM datasets.
6. Limited ability to replicate ADaM datasets (i.e., analysis variable imputation or
derived variables) using SDTM datasets.
7. Limited traceable path from ADaM to the Tables, Figures and the Clinical Study
Report (CSR).
8. Difficulty in understanding the source or derivation methods for imputed or
derived variables in integrated/pooled data, supplemental qualifiers, and related
records.
Table 5 presents the issues when legacy data are converted to SDTM and ADaM formats
in sequence (i.e., converting legacy study data to SDTM and then creating ADaM from
the SDTM). The key concern is the traceability from ADaM to the Tables, Figures and
CSR.
Table 5: Traceability Issues: Legacy Data Conversion to SDTM and ADaM in
Sequence
1. Limited ability to determine location of collected CRF variables in the converted
SDTM data unless the legacy aCRF is re-annotated.
2. Limited traceable path from SDTM to the legacy analysis data.
3. Limited ability to replicate/confirm legacy analysis datasets (i.e., analysis
variable imputation or derived variables) using SDTM datasets.
4. Limited ability to confirm derivation of intermediate analysis datasets or custom
domains.
5. Limited traceable path from ADaM to the Tables, Figures and the CSR.
6. Difficulty in understanding the source or derivation methods for imputed or
derived variables in integrated/pooled data, supplemental qualifiers, and related
records.
Contains Nonbinding Recommendations
33
8.3.2.2 Legacy Data Conversion Plan and Report
Sponsors should evaluate the decision involved in converting previously collected non-
standardized data (i.e., legacy study data) to standardized data (i.e., SDTM, SEND, and
ADaM). Sponsors should provide the explanation and rationale for the study data
conversion in the SDRG. To mitigate traceability issues when converting legacy data,
FDA recommends the following procedures:
1. Prepare and Submit a Legacy Data Conversion Plan and Report.
The plan should describe the legacy data and the process intended for the
conversion.
The report should present the results of the conversions, issues encountered
and resolved, and outstanding issues.
The plan and report should be provided in the SDRG.
2. Provide an aCRF, for clinical data, that maps the legacy data elements.
Sponsors should provide two separate CRF annotations, one based on the
original legacy data, and the other based on the converted data (i.e., SDTM)
when legacy datasets are submitted. The legacy CRF tabulation data should
include all versions and all forms used in the study.
3. Record significant data issues, clarifications, explanations of traceability, and
adjudications in the SDRG. For example, data were not collected or were
collected using different/incompatible terminologies, or were collected but will
not fit into, for example, SDTM format.
4. Legacy data (i.e., legacy aCRF, legacy tabulation data, and legacy analysis data)
may be needed in addition to the converted data.

Contains Nonbinding Recommendations
34
Appendix: Data Standards and Interoperable Data Exchange
This appendix provides some of the guiding principles for the Agency’s long-term study
data standards management strategies. An important goal of standardizing study data
submissions is to achieve an acceptable degree of semantic interoperability (discussed
below). This appendix describes different types of interoperability and how data
standards can support interoperable data exchange now and in the future.
At the most fundamental level, study data can be considered a collection of data elements
and their relationships. A data element is the smallest (or atomic) piece of information
that is useful for analysis (e.g., a systolic blood pressure measurement, a lab test result, a
response to a question on a questionnaire).
A data value is by itself meaningless without additional information about the data (so
called metadata). Metadata is often described as data about data. Metadata is structured
information that describes, explains, or otherwise makes it easier to retrieve, use, or
manage data.
51
For example, the number 44 itself is meaningless without an association
with Hematocrit and the unit of measurement (e.g. "%"). Hematocrit in this example is
metadata that further describes the data.
Just as it is important to standardize the representation of data (e.g., M and F for male and
female, respectively), it is equally important to standardize the metadata. The
expressions Hematocrit = 44; Hct = 44, or Hct Lab Test = 44 all convey the same
information to a human, but an information system or analysis program will fail to
recognize that they are equivalent because the metadata is not standardized. It is also
important to standardize the definition of the metadata, so that the meaning of a
Hematocrit value is constant across studies and submissions.
In addition to standardizing the data and metadata, it is important to capture and represent
relationships (also called associations) between data elements in a standard way.
Relationships between data elements are critical to understand or interpret the data.
Consider the following information collected on the same day for one subject in a study:
Systolic Blood Pressure = 90 mmHg
Position = standing
Systolic Blood Pressure = 110 mmHg
Time = 10:23 a.m.
Time = 10:20 a.m.
51
Metadata is said to “give meaning to data” or to put data “in context.” Although the term is now
frequently used to refer to XML (extensible markup language) tags, there is nothing new about the concept
of metadata. Data about a library book such as author, type of book, and the Library of Congress number,
are metadata and were once maintained on index cards. SAS labels and formats are a rudimentary form of
metadata, although they have not historically been referred to as metadata.
Contains Nonbinding Recommendations
35
Position = lying
When presented as a series of unrelated data elements, they cannot reliably be
interpreted. Once the relationships are captured, as shown below using arrows, the
interpretation of a drop in systolic blood pressure of 20 mmHg while standing, and
therefore the presence of clinical orthostatic hypotension, is possible. Standardizing
study data therefore involves standardizing the data, metadata, and the representation of
relationships.
Time = 10:20 a.m. Position = lying Systolic Blood Pressure = 110 mmHg
Time = 10:23 a.m. Position = standing Systolic Blood Pressure = 90 mmHg
With these fundamental concepts of data standardization in mind, data standards can be
considered in the context of interoperable data exchange.
Interoperability
Much has been written about interoperability, with many available definitions and
interpretations within the health care informatics community. In August 2006, the
President signed an Executive Order mandating that the Federal Government use
interoperable data standards for health information exchange.
52
Although this order was
directed at Federal agencies that administer health care programs (and therefore not the
FDA), it is relevant to this guidance because it defined interoperability for use by Federal
agencies:
“Interoperability” means the ability to communicate and exchange data accurately,
effectively, securely, and consistently with different information technology systems,
software applications, and networks in various settings, and exchange data such that
clinical or operational purpose and meaning of the data are preserved and unaltered.
Achieving interoperable study data exchange between sponsors and applicants and FDA
is not an all-or-nothing proposition. Interoperability represents a continuum, with higher
degrees of data standardization resulting in greater interoperability, which in turn makes
the data more useful and increasingly capable of supporting efficient processes and
analyses by the data recipient. It is therefore useful to understand the degree of
interoperability that is desirable for standardized study data submissions.
In 2007, the Electronic Health Record Interoperability Work Group within Health Level
Seven issued a white paper that characterized the different types of interoperability based
on an analysis of how the term was being defined and used in actual practice.
53
Three
types of interoperability were identified: technical, semantic, and process
interoperability. A review of these three types provides insight into the desired level of
interoperability for standardized study data submissions.
52
See http://www.cga.ct.gov/2006/rpt/2006-R-0603.htm.
53
See Coming to Terms: Scoping Interoperability for Health Care http://www.hln.com/assets/pdf/Coming-
to-Terms-February-2007.pdf.
Contains Nonbinding Recommendations
36
Technical interoperability describes the lowest level of interoperability whereby two
different systems or organizations exchange data so that the data are useful. The focus of
technical interoperability is on the conveyance of data, not on its meaning. Technical
interoperability supports the exchange of information that can be used by a person but not
necessarily processed further. When applied to study data, a simple exchange of non-
standardized data using an agreed-upon file format for data exchange (e.g., SAS transport
file) is an example of technical interoperability.
Semantic interoperability describes the ability of information shared by systems to be
understood, so that nonnumeric data can be processed by the receiving system. Semantic
interoperability is a multi-level concept with the degree of semantic interoperability
dependent on the level of agreement on data content terminology and other factors. With
greater degrees of semantic interoperability, less human manual processing is required,
thereby decreasing errors and inefficiencies in data analysis. The use of controlled
terminologies and consistently defined metadata support semantic interoperability.
Process interoperability is an emerging concept that has been identified as a
requirement for successful system implementation into actual work settings. Simply put,
it involves the ability of systems to exchange data with sufficient meaning that the
receiving system can automatically provide the right data at the right point in a business
process.
An example of process interoperability in a regulatory setting is the ability to quickly and
automatically identify and provide all the necessary information to produce an expedited
adverse event report in a clinical trial upon the occurrence of a serious and unexpected
adverse event. The timely submission of this information is required by regulation to
support FDA’s mandate to safeguard patient safety during a clinical trial. Process
interoperability becomes important when particular data are necessary to support time-
dependent processes.
Because the vast majority of study data are submitted after the study is complete,
achieving process interoperability for study data submissions in a regulatory setting is
relatively unimportant, at least for the foreseeable future. It is reasonable to conclude that
it is most desirable to achieve semantic interoperability in standardized study data
submissions.
In summary, the goal of standardizing study data is to make the data more useful and to
support semantically interoperable data exchange between sponsors, applicants, and the
FDA such that it is commonly understood by all parties.
Contains Nonbinding Recommendations
37
Glossary
The following list of acronyms and terms used in this Guide:
aCRF: Annotated Case Report Form
ANDA: Abbreviated New Drug Application
ADaM: Analysis Data Model
ADRG Analysis Data Reviewer’s Guide
ADSL: Subject Level Analysis Data
ASCII: American Standard Code for Information Interchange
CBER: Center for Biologics Evaluation and Research
CDASH: Clinical Data Acquisition Standards Harmonization
CDER: Center for Drug Evaluation and Research
CDISC: Clinical Data Interchange Standards Consortium
CS: Chemical Structure
Domain: A collection of observations with a topic-specific commonality
eCTD: Electronic Common Technical Document
ICH: International Conference on Harmonisation
IND: Investigational New Drug
ISE: Integrated Summary of Efficacy
ISO: International Organization for Standardization
ISO 8601: ISO character representation of dates, date/times, intervals, and durations
of time
ISS: Integrated Summary of Safety
ITT: Intent-To-Treat
MedDRA: Medical Dictionary for Regulatory Activities
MOA: Mechanism of Action
NDA: New Drug Application
NDF-RT: National Drug File – Reference Terminology
PDF: Portable Document Format
PE: Physiologic Effect
SDRG Study Data Reviewer’s Guide
SDTM: Study Data Tabulation Model
SNOMED: Systematized Nomenclature of Medicine
UNII: FDA Unique Ingredient Identifier
WHO: World Health Organization
XML: eXtensible Markup Language
XPORT: SAS Transport Version 5