ENDEAVOR – Overall Survival Analysis 49c19f2e 0bcd 42a1 B1b2 E15eb5dedcb6
2018-06-18
: Pdf 49C19F2E-0Bcd-42A1-B1B2-E15Eb5Dedcb6 49c19f2e-0bcd-42a1-b1b2-e15eb5dedcb6 6 2018 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 45

6/18/2018
1
Optimizing Therapy of Relapsed/Refractory
Multiple Myeloma
Noopur Raje, MD
Director, Center for Multiple Myeloma
MGH Cancer Center
Professor of Medicine
Harvard Medical School
Disclosures
•Consultant /Advisory Board: Celgene, Millenium
Takeda, Amgen-Onyx, Novartis, Janssen, BMS,
Merck, Bluebird
•Research Funding: Astra Zeneca
•Steering Committee: Amgen, Roche
Myeloma: Scope of the Problem
•Median time to first relapse with current therapies: 3-4 yrs
Kumar SK, et al. Leukemia. 2014;28:1122-1128.
> 100,000 pts living
with myeloma
OS (%)
Yrs
2006-2010
2001-2005
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
0 1 2 3 4 5 6

6/18/2018
2
Confronting Disease Relapse in Myeloma
Kumar SK, et al. Mayo Clin Proc. 2004;79:867-874.
Kumar SK, et al. Leukemia. 2012;26:149-157.
Pts (%)
100
80
60
40
0
20
012 24 36 48 60
Mos
OS
EFS
Events, n/N
170/286
217/286
Median, Mos
(Range)
9 (7-11)
5 (4-6)
12
10
8
6
0
2
First Second Third Fourth Fifth Sixth
Treatment Regimen
Median Response Duration (Mos)
4
Current estimates for patients refractory to both
IMiDs and PIs
From 1st relapse From PI and IMiD resistance
Kumar et al, Leukemia 2017
Altered Genes per PatientMutation Load by Disease Stage
Clonal Evolution with Progression
6/18/2018
3
Schaffer et al, Nature. 454. 226-31 Stewart. Science 2014;343:256-257; Lu et al Science 2014;343:305-309; Kronke et al. Science 2014;343:301-305
Targeting the drivers- Myc: IMiDs
Targeting the Proteasome
Gillmore, Cancer Cell, 12(2), p95–97, 14 August 2007; Anderson Clin Cancer Res 2016;22:5419-5427
Lonial S, M itsiades CS, Richardson PG. Clin Cancer Res 2011 ;17: 1264-77.
Rational combination strategies
in relapsed, refractory MM
+ MoAbs
3rd generation
IMiDs (POM)
2nd, 3rd generation
PI’s (CFLZ, IXA)
6/18/2018
4
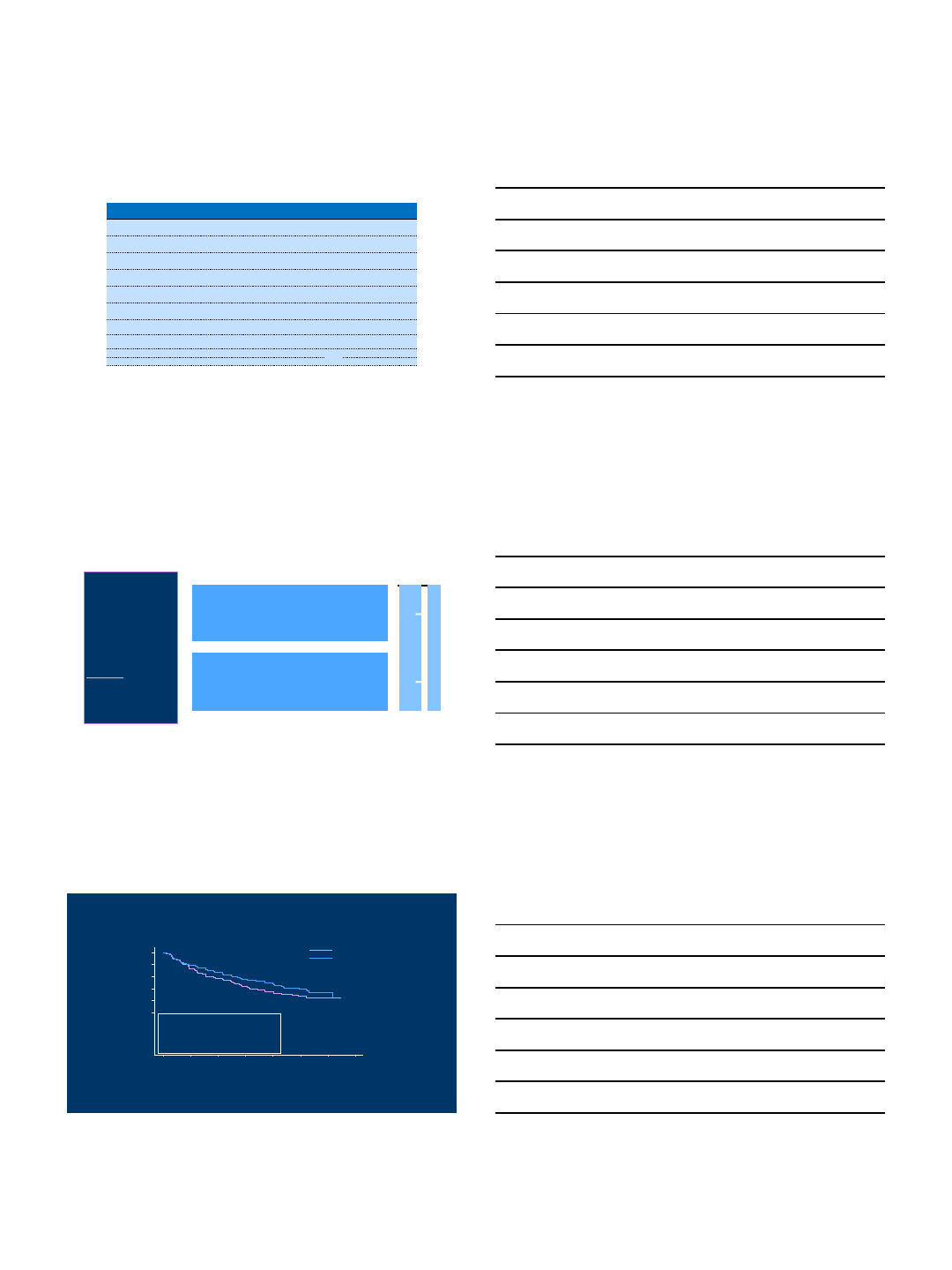
Selected phase III trials in relapsed
disease
Name of trial
No. prior lines
Arm
N
PFS (months)
ORR
≥VGPR
≥CR
ENDEAVOR
1
-3
Kd
464
18.7
77%
54%
13%
Vd
465
9.4
63%
29%
6%
TOURMALINE
-MM1
1
-3
IRd
360
20.6
78%
48%
12%
Rd
362
14.7
72%
39%
7%
ELOQUENT
-2
1
-3
Elo
-Rd
321
19.4
79%
33%
4%
Rd
325
14.9
66%
28%
7%
ASPIRE
1
-3
KRd
396
26.3
87%
70%
32%
Rd
396
17.6
67%
40%
9%
PANORAMA 1
1
-3
Pano
-Vd
387
11.99
61%
11%
Vd
381
8.08
55%
6%
NIMBUS (MM
-003)
≥2
§
Pd
302
4.0
31%
6%
1%
D
153
1.9
10%
1%
0%
CASTOR
≥1
Vd
-dara
251
NE
82.9%
59.2%
19.2%
Vd
247
7.2
63.2%
29.1%
9%
POLLUX
≥1
Rd
-dara
286
NE
93%
76%
43%
Rd
283
18.4
76%
44%
19%
A.R.R.O.W. Study Design
Arm B: Twice-weekly carfilzomib + dex
(10 min infusion of K)
Carfilzomib 20 mg/m2IV D1, 2 (Cycle 1)
Carfilzomib 27 mg/m2IV D8, 9, 15, 16 (Cycle 1), D1, 2, 8, 9, 15, 16
(Cycle 2+)
Dexamethasone 40 mg IV/PO D1, 8, 15 (All cycles)
Dexamethasone 40 mg IV/PO D22 (Cycles 1-9 only)
Arm A: Once-weekly carfilzomib + dex
(30 min infusion of K)
Carfilzomib 20 mg/m2IV D1 (Cycle 1)
Carfilzomib 70 mg/m2IV D8, 15 (Cycle 1), D1, 8, 15 (Cycle 2+)
Dexamethasone 40 mg IV/PO D1, 8, 15 (All cycles)
Dexamethasone 40 mg IV/PO D22 (Cycles 1-9 only)
1:1 Randomization
N = 478
•Relapsed and Refractory
MM
•2-3 prior lines
•Prior exposure to IMiD & PI
•PS 0-1
Stratification:
•ISS stage
•Refractory to bortezomib
•Age (<65 vs. ≥65)
28-day cycles
.
Follow-up for Disease Status until
Confirmed PD
Long-term Follow-up for Survival
Primary Endpoint: Progression-Free Survival Assessed by
Computational Algorithm Based on IMWG-URC
240 178 145 114 69 24 5 0
238 164 119 86 41 15 4 0
Kd 20/70
Kd 20/27
Number of Subjects at Risk:
++++++++
++ +
+
+
+++
+++
+
++
+++ +++++
++
+
+++++++
++++
+++++
+ +
+
+++++ ++
+++++++ ++
++ +
+++++ ++
+++ ++++ + +++ +
++++ ++
++ ++++
++
+
++++ +++
++ +
++++++++++++++
++++++
++
+++++
++
++++
+++
++
++++
++ ++
++++
+++ +++++++++++ ++
+++ +
++
++++ ++++ +++++ +
+++
0 3 6 9 12 15 18 21
Months from Randomization
0.0
0.2
0.4
0.6
0.8
1.0
Proportion Surviving Without Progression
Kd Once-weekly
Kd Twice-weekly
0.0014p-value (1-sided)
0.693 (0.544, 0.883)HR(Kd 20/70/Kd 20/27)(95% CI)
11.27.6Median PFS, months
126 (52.5%)148 (62.2%)Progression/Death,n (%)
----------------------
(N=240)(N=238)
Kd 20/70 mg/m 2
Kd 20/27 m g/m 2
Once-weeklyTwice-weekly

6/18/2018
5
What about Len refractory patients?
Len-refractory RRMM
Trial/Regimen Analysis set N PFS ORR MRD neg. rate at 10-5
CASTOR3
D-Vd vs Vd
Len-
refractory at last
prior line of therapy
D-Vd: n = 45
Vd: n = 60
Median: 9.3 mo vs 4.4 mo
HR: 0.36; 95% CI, 0.21-0.63; P= 0.0002
18-mo PFS rate: 34% vs 2%
81% vs 50%
P= 0.0021
9% vs 0%
P= 0.0082
MMY10014
D-Pd
All treated
(89% len-refractory) n = 103 Median: 9.9 mo
24-mo PFS rate: 31% 66% 7%
ENDEAVOR5,6
Kd vs Vd Len-refractory Kd: n = 113
Vd: n = 122
Median: 8.6 mo vs 6.6 mo5
HR: 0.80; 95% CI, 0.57-1.116N/R N/R
MM-0037
P-low d vs high d Len-refractory P-low d: n = 286
High d: n = 141
Median: 3.9 mo vs 1.9 mo
HR: 0.50; 95% CI, 0.40-0.62
30% vs 9%
P<0.0001 N/R
1
4
Ajai Chari, MD
Addition of DARA to SOC is effective in len-refractory RRMM
Len, lenalidomide; Vd, bortezomib/dexamethasone; PFS, progression-free survival; ORR,
overall response rate; MRD, minimal residual disease; HR, hazard ratio; Pd,
pomalidomide/dexamethasone; Kd, carfilzomib/dexamethasone; N/R, not reported; SOC,
standard of care.
1. Harousseau JL and Attal M. Bloo d 2017;130:963-973. 2. Sengsayadeth S, et al. Blood Cancer J 2017;7(3):e545. 3. Lentzsch S, et al. Oral presentation at JSH, Oct 20-22, 2017; Tokyo, Japan; Abstract OS3-12D-
2. 4. Facon T, et al. Poster presented at ASH, Dec 9-12, 2017; Atlanta, GA; Abstract 1824. 5. Moreau P, et al. Leuk emia 2017;31:115-122. 6. Dimopoulos MA, et al. Lancet Oncol 2016;17(1):27-38. 7. San-Miguel
J, et al. Lancet Oncol 2013;14(11):1055-1066.
Available Efficacy Data on Len-refractory RRMM Patients
Study Design: D-Kd Arm of MMY1001
1
5
Ajai Chari, MD
•Open-label, nonrandomized, multicenter, phase 1b study in RRMM patients
•Per protocol, DARA was administered as a single first dose (n = 10) or as a split first dose (n = 75)
ECOG, Eastern Cooperative Oncology Group; LVEF, left ventricular ejection fraction;
ANC, absolute neutrophil count; QW, every week; Q2W, every 2 weeks; Q4W, every 4
weeks; IV, intravenous; PO, oral; OS, overall survival; MRD, minimal residual disease;
NGS, next generation sequencing; PK, pharmacokinetic; IFE, immunofixation; IRR,
infusion-related reaction.
Eligibility/treatment
•Relapsed MM
–1-3 prior lines of therapy,
including bortezomib and an
IMiD
–Len-refractory pts allowed
•Carfilzomib-naïve
• ECOG status ≤2
• LVEF ≥40%
• ANC ≥1 × 109/L
• Platelet count ≥75 × 109/L
Dosing schedule (28-day cycles)
DARA:
•Split first dosea: 8 mg/kg Days 1-2 of Cycle 1
•Single first dose: 16 mg/kg on C1D1
•16 mg/kg IV QW on Cycles 1-2, Q2W on Cycles 3-6, and Q4W
thereafter until PD
Carfilzomibb:
•20 mg/m2IV Cycle 1 Day 1
•Escalated to 70 mg/m2Cycle 1 Day 8+; weekly (Days 1, 8, 15) until
PD
Dexamethasone: 40 mg/week (Days 1, 8, 15, 22) IV or PO until PD
Endpoints
Primary
•Safety, tolerability
Secondary
•ORR and duration of response
•OS
Exploratory
•PFS
•MRD (NGS)c
•PK
aIn 500-mL dilution volume.
bBoth 20 mg/m2and 70 mg/m2were administered as 30 -min IV infusions.
cAmong patients evaluated f or MRD, MRD was assessed using NGS at time of suspected CR and at 12 and 18 mo after initial dose. In cases where daratumumab is suspected of interfering with IFE and
preventing clinical CR response calls, subjects with VGPR may also be evaluated for MRD.

6/18/2018
6
Infusion Rates and IRRs: Split First Dose DARA (All Treated)
Ajai Chari, MD
Split first dose of DARA is feasible and improves patient convenience
IRR, n (%)
Median (range)
infusion time
Single
first infusion (n = 10)
Cycle 1 Day 1
Split first
infusion (n = 75)
Cycle 1 Day 1
Cycle 1 Day 2
5 (50.0%)
27 (36.0%)
3 (4.0%)
7.1 (6.5-8.9) h
4.3 (3.9-10.6) h
4.2 (3.9-8.6) h
Split first dose IRRs (>1 patient)
during all infusions
3
3
3
3
4
4
4
4
4
8
8
43
010 20 30 40 50
Hypertension
Chills
Nasal congestion
Cough
Flushing
Pyrexia
Nausea
Dyspnea
Throat irritation
Vomiting
Allergic rhinitis
Total
IRRs, %
IRR, infusion-related reaction.
•IRR % and infusion times were consistent between single
and split first dose for subsequent infusions
PFS
Ajai Chari, MD
PFS benefit observed in len-refractory patients
•Median follow up: 12.0 months
Median: 14.1 mo
(95% CI, 12.0-NE)
All-treated
Len-refractory
0
0 3 6 9 2412
60
40
20
80
100
% surviving without progression
Months
12-month PFS
1815
85
51
30
72
41
27
66
35
27
60
32
25
13
6
7
26
12
13
11
5
6
0
0
0
No. at risk
All-treated
Len-refractory
Len-exposed
21
8
3
5
71%
62%
90%
Len-exposed
What about Pomalidomide ?
6/18/2018
7
Efficacy Results of Pomalidomide + LoDEX in advanced
RR MM (Phase II/III Studies MM002 & MM003)
1.Richardson PG, et al. Blood 2014;123:1826-32. 2. San Miguel J, et al. Lancet Oncology
2013; 14:1055-1066. 3. San Miguel et al: ASH 2013; Oral Presentation and Abstract 686.
CR, complete response; DoR, duration of response; LoD EX, low-dose dexamethasone; MR, minimal
response; ORR, ove rall response rate; OS, ov erall survival; PFS, progression-fre e surviv al; POM,
pomalidomide; PR, partial response; sCR, stringent complete response; VGPR, very good partial response.
31
7
30 24
12 8
0
10
20
30
40
50
MM-002 MM-003
MR
PR
VGPR
CR/sCR
ORR = 33% ORR = 32%
Percentage response
MM-0021MM-0032,3
Median follow
-up, months 14.2 15.4
Median
DoR, months 8.3 7.5
Median PFS, months
4.2 4.0
Median OS,
months 16.5 13.1
Efficacy Results of POM-based Triple Therapy
Combinations in Advanced RRMM
5 5 1
31
07
18 15 15
25
27
37
27 41
32
38
43
26
20 7
20
13
0
10
20
30
40
50
60
70
80
90
100
POM+PRED+Cy POM+DEX+Cla POM+DEX±Cy POM+DEX+BORT POM+DEX+CFZ POM+DEX+BORT
(MM-005)
MR PR VGPR CR
Percentage response
ORR
51%
ORR
61% ORR
48%
ORR
70%
ORR
70%
Study Larocca1Mark2Baz3Mikhael4Shah5Richardson6
Phase 1/2 2 1/2 2 1/2 1/2
N55a114 70 16 79 27
Population
1–3 prior
therapies;
LEN-relapsed
or refractory
≥ 3 prior
therapies
including LEN
(not all
refractory)
≥ 2 prior
therapies;
LEN-refractory
1–4 prior
therapies,
resistant or
refractory to LEN
Relapsed and/or
refractory;
LEN-refractory
1-4 prior
therapies;
LEN-refractory,
prior BORT
1. Larocca A, et al. Blood. 2013;122:2799−2806.
2. Mark et al: ASH 2013; Poster Presentation and Abstract 1955..
3. Baz et al: ASH 2013; Poster Presentation and Abstract 3200.
4. Mikhael J et al. ASH 2013; Poster Presentation and Abstract 1940.
5. Shah et al: ASH 2013; Oral Presentation and Abstract 690.
6. Richardson et al: ASH 2013; Oral Presentation and Abstract 8589.
BORT, bortezomib; CFZ, carfilzomib; Cla, clarithromycin; CR, complete response; Cy,
cyclophosphamide; DEX, dexamethasone; LEN, lenalidomide; LoDEX, low-dose de xamethasone; MR,
minimal response; ORR, overall response rate ; POM, pomalidomide; PR, partial r esponse; PR ED,
prednisone; VGPR, very good partial response.
a Data reported here for MTD and Phase II pts only
ORR
94%
OPTIMISMM Study Design and methods
21
a Patients with PD during therapy or within 60 days of the last dose of a BORT-containing therapy under the approved dosing schedule of 1.3 mg/m2twice weekly were excluded.
BORT, bortezomib; DOR, duration of response; IMWG, International Myeloma Working Group; LT, long-term; PFS2, progression-free survival after next line of therapy; TTR, time to response.
•Stratification
– age (≤ 75 y vs > 75 y)
–number of prior antimyeloma regimens (1 vs > 1)
– β2-microglobulin levels at screening
(< 3.5 mg/L vs ≥ 3.5 to ≤ 5.5 mg/L vs > 5.5 mg/L)
•Study endpoints
–Primary: PFS
–Secondary: OS, ORR by IMWG criteria, DOR, safety
–Key exploratory: TTR, PFS2, efficacy analysis in subgroups
•Data cutoff: October 26, 2017
PD, subsequent antimyeloma Tx,
and survival
PD or Unacceptable Toxicity
PVd (n = 281)
POM 4 mg days 1-14/21
BORT 1.3 mg/m2
cycles 1-8: days 1, 4, 8, 11/21
cycles 9+: days 1 and 8/21
LoDEX 20 mg (≤ 75 y) or 10 mg (> 75 y)
day of and day after BORT
Vd (n = 278)
BORT 1.3 mg/m2
cycles 1-8: days 1, 4, 8, 11/21
cycle 9+: days 1 and 8/21
LoDEX 20 mg (≤ 75 y) or 10 mg (> 75 y)
day of and day after BORT
RRMM
•1-3 prior regimens including ≥ 2 cycles of LEN
Tx
• ECOG PS ≤ 2
•Prior BORT Tx allowed (except if PD with
twice weekly dose)a
(N = 559)
LT follow-up

6/18/2018
8
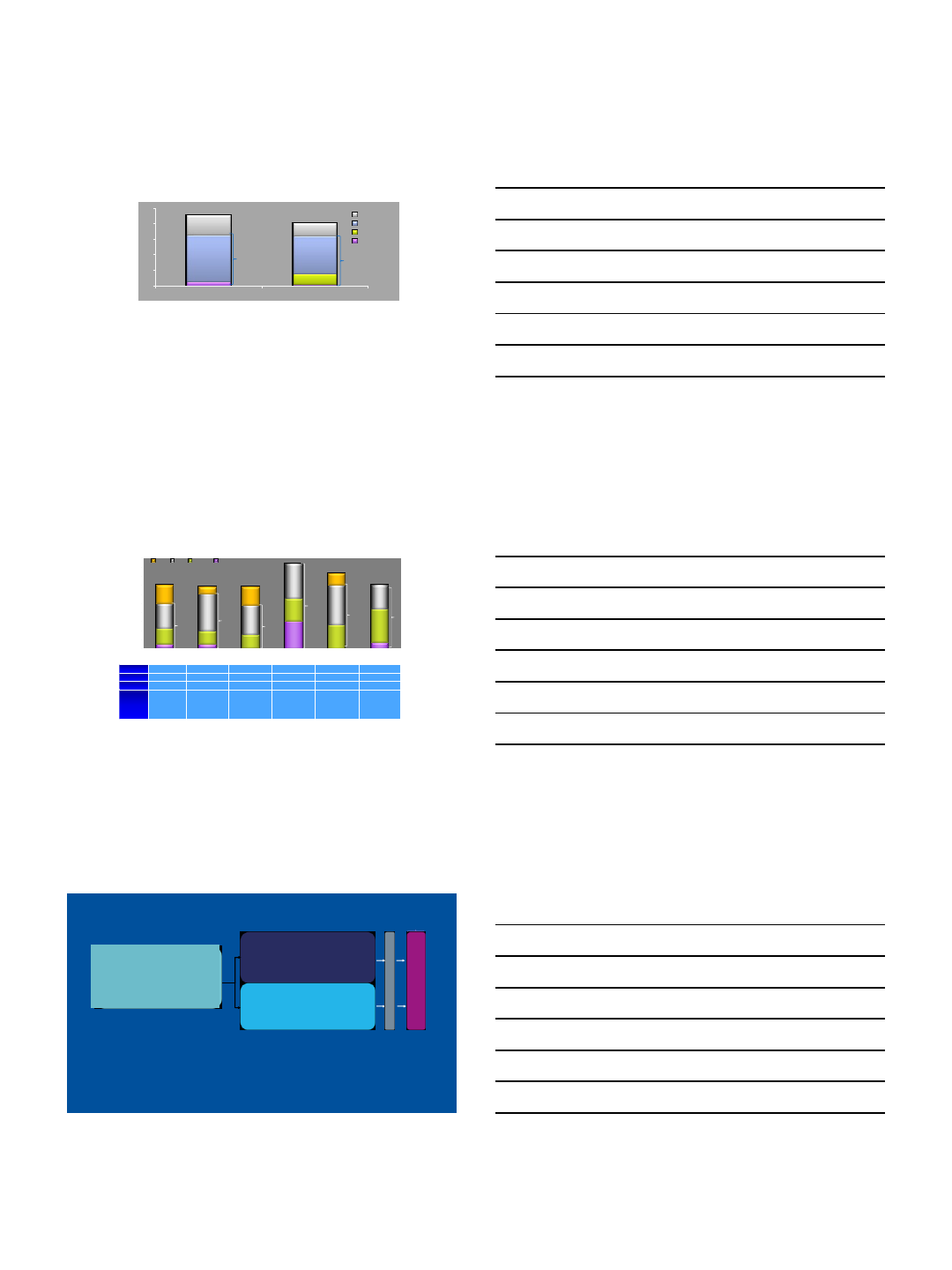
Progression-Free Survival (ITT Population)
1.0
0.9
0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0.0
0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45
Months
Probability of
Progression-Free Survival
Events/N Median PFS,
mo
HR (95% CI)
P Value
PVd 154/281 11.20 0.61 (0.49-0.77)
< .0001
Vd 162/278 7.10
•OPTIMISMM met its primary endpoint, demonstrating a clinically meaningful and
statistically significant improvement in PFS with PVd vs Vd
Abstract 8001 : OPTIMISMM—Paul Richardson, MD
278 176 112 66 42 30 20 14 4 4 3 2 2 0
281 233 182 128 94 67 47 28 13 7 4 2 1 0
0
1
0
1
No. at Risk
PVd
Vd
•Ixazomib
•Oprozomib
•Marizomib
Oral
proteasome
inhibitors
•Elotuzumab
•Daratumuma
b
•Isatuximab
Monoclonal
antibodies
•Vermurafeni
b
•Afuresertib
•Dinaciclib
•PIM
(LGH447)
•Trametinib
Kinase
inhibitors
•Panobinost
at
•Ricolinostat
•ACY 241
HDACi
•Venetoclax
•Selinexor
Novel
mechanism
s
•PDL-1/PD-1
•CAR-T
•BITE
Immuno-
therapies
HDACi, histone deacetylas e inhibitor
•CC-122
•CC-220
New
IMiDs
What is New in MM
Vij R et al. Blood. 201 4;124. Abstract 34.
Authors’ Conclusions
The most common grade ≥3 nonhematologic AEs were diarrhea, nausea, and
vomiting; rates of treatment-emergent PN and rash were low.
Recommended phase 2 dose and schedule: 240/300 mg/day in the 2/7 step-up
schedule and 150/180 mg/day in the 5/14 step-up schedule.
Preliminary data suggest that step-up dosing is associated with improved
tolerability.
Enrollment of patients with MM continues both schedules in the phase 2 study
with a target of 94 patients; all patients are now receiving a new (extended-
release) formulation of oprozomib.
Single-agent oprozomib has promising antitumor activity, with responses
observed in patients who had carfilzomib-refractory MM.
Oprozomib in Myeloma: still in development

6/18/2018
9
25
CC-122: New IMiD
Ribrag V, et al. Blood. 2014;124 [poster
3500].
Venetoclax Background
▪BCL-2 and MCL-1 promote multiple myeloma (MM) cell survival
▪Venetoclax is a selective, orally available small molecule BCL-2 inhibitor1 and
bortezomib can indirectly inhibit MCL-1
▪Venetoclax enhanced bortezomib activity in vitro and in vivo2
1. Roberts AW et al. NEJM 2015
2. Punnoose E et al. Mol Cancer Ther 2016
Phase 1 Venetoclax for RRMM:
response and TTP in all patients and by
t(11;14) status
0
1 0
2 0
3 0
4 0
5 0
P er ce n ta g e of P a tie n ts
sC R C R V G P R P R
A ll P a ti e nt s
N = 6 6
t( 1 1 ; 1 4 )
n = 3 0
O R R 2 1 %
O R R 4 0 %
n o n -t ( 1 1 ; 1 4 )
n = 3 6
O R R 6 %
6%
8%
13%
4%
10%
13%
3%
3%
3%
4%
Data cutoff of 19Aug2016
Kumar ASH 2016 Abstract 488
0 2 4 6 8 1 0 1 2 1 4 1 6 1 8 2 0 2 2 2 4
0
2 5
5 0
7 5
100
M o nt hs s in c e fi rs t d o se
% N o t P ro g re s se d
t( 1 1 ; 1 4 )
n o n - t( 1 1 ;1 4 )
No . at risk 66 33 27 2 0 1 6 9 3 1 1 1 1 1
No . at risk 30 20 19 1 7 1 3 7 2 1 1 1 1 1
No . at risk 36 13 8 3 3 2 1
T im e t o P ro g re s sio n
A ll P a tie nts
0 2 4 6 8 1 0 1 2 1 4 1 6 1 8 2 0 2 2 2 4
0
2 5
5 0
7 5
100
M o nt hs s in c e fi rs t r e sp o ns e
t( 1 1 ; 1 4 )
n o n - t( 1 1 ;1 4 )
14 14 13 13 9 3 2 1 1 1 1
12 12 11 11 8 3 2 1 1 1 1
2 2 2 2 1
D u r at io n o f O v e r a ll R e s p o ns e
A ll P a tie nts
6/18/2018
10
Criteria
Response
%
(36 pts)
CR
9% (3)
VGPR
11% (4)
PR
25% (10)
Ven (50-500mg po daily); Btz (1.3mg/msq days 1,4,8,11);
Dex (20mg days 1-2, 4-5, 8-9, 11-12) x8 cycles N=32
Chanan-Khan Lugano 2015
A Phase 3, multicenter, randomized, double blind, placebo-controlled study of
venetoclax plus bortezomib and dexamethasone in subjects with relapsed or
refractory myeloma in 1-3 prior lines of therapy and are sensitive or naïve to
proteasome inhibitors
Ph 1: Venetoclax in combination with Btz+Dex
Cytogenetics
ORR %
(36 pts)
t(11;14)
(n=4)
75%
t(4;14) (n=3)
33%
del17p (n=8)
25%
Hyperdiploid
(n=14)
64%
DOR median 6mos.
29
▪Exportin 1 (XPO1) is the only nuclear
exporter for the majority of tumor
suppressor proteins (TSPs), the
glucocorticoid receptor (GR), and eIF4E-
bound oncoprotein mRNAs
▪Selinexor is a first-in-class XPO1 inhibitor
that induces nuclear retention and
activation of TSPs and the GR in the
presence of steroids and suppresses
oncoprotein expression
Selinexor Mechanism of Action
BRAF c.1799T>A, p.V600E
Genomic control Myeloma-GT
Tracking Genetic Hetrogeneity
Lohr et al, Science Trans Med 2016
BM and Blood Biopsies
6/18/2018
11
BASKET STUDY: VEMURAFENIB
for BRAF mutant MM (n=9)
Raje et al, ASH 2015
An open-label, pilot study of dabrafenib
and/or trametinib in patients with
relapsed and/or refractory multiple
myeloma
Jens Lohr, MD PhD
Noopur Raje, MD

6/18/2018
12
GSK 2857916:Background
▪BCMA: expressed on differentiated B cells;
requisite for long-lived plasma cells’ survival
▪BCMA is broadly expressed on malignant
plasma cells
▪GSK2857916: humanized, afucosylated IgG1
anti-BCMA antibody; neutralization
of soluble BCMA
▪Preclinical studies demonstrate its selective
and potent activity1
GSK2857916
–Enhanced ADCC
Afucosylation
–Stable in
circulation
Linker
–MMAF (non-cell
permeable, highly
potent auristatin
Cytotoxic
agent
ADC, antibody-drug conjugate; ADCC, antibody-dependent cell-mediated cytotoxicity; BCMA, B-cell maturation antigen; IgG, immunoglobulin G;
MMAF, monomethyl auristatin-F
1Tai YT, et al. Blood 2014;123(20):3128-38.
Four mechanisms of action:
1. ADC mechanism
2. ADCC mechanism
3. Immunogenic cell death
4. BCMA receptor signaling inhibition
1
4
3
1
BCMA
Effector
cell
x
BCMA
BCMA
BCMA
Lysosome
Fc
receptor
ADCC
ADC
Cell death
Malignant
plasma
cell
2
3
4
DREAMM-1 Part 2: Maximum % Reduction in
M-Protein or Free Light Chain from Baseline
CI, confidence interval; CR, complete response; FLC, free light chain; M-protein, myeloma protein; ORR, overall response rate;
PD, progressive disease; PR, partial response; sCR, stringent complete response; SD, stable disease; VGPR, very good partial response
ORR = 21/35 (60%; 95% CI: 42.1%, 76.1%)
•1 sCR, 2 CR, 15 VGPR, 3 PR
*
*One patient with a VGPR had a <90% reduction in serum M-protein due to missing laboratory data, which was confirmed by investigators
as too small to quantify after the data cut-off
DREAMM-1 Part 2: Efficacy –
Progression-free Survival and duration of response
Number of subjects 35
Progressed or died 15 (43%)
Censored, f/u ended 3 (9%)
Censored, f/u ongoing 17 (49%)
Progression-free survival (months)
Q1 (95% CI) 2.3 (0.7, 6.8)
Median (95% CI) 7.9 (3.1, -)
Q3 (95% CI) N/A
CI, confidence interval; f/u, follow-up; N/A, not available; Q, quartile
Number of subjects 21
Progressed or died 4 (19%)
Censored, f/u ended 0
Censored, f/u ongoing 17 (81%)
Duration of response (months)
Q1 (95% CI) 6.7 (1.6, -)
Median (95% CI) N/A (6.7, -)
Q3 (95% CI) N/A
3
6
6/18/2018
13
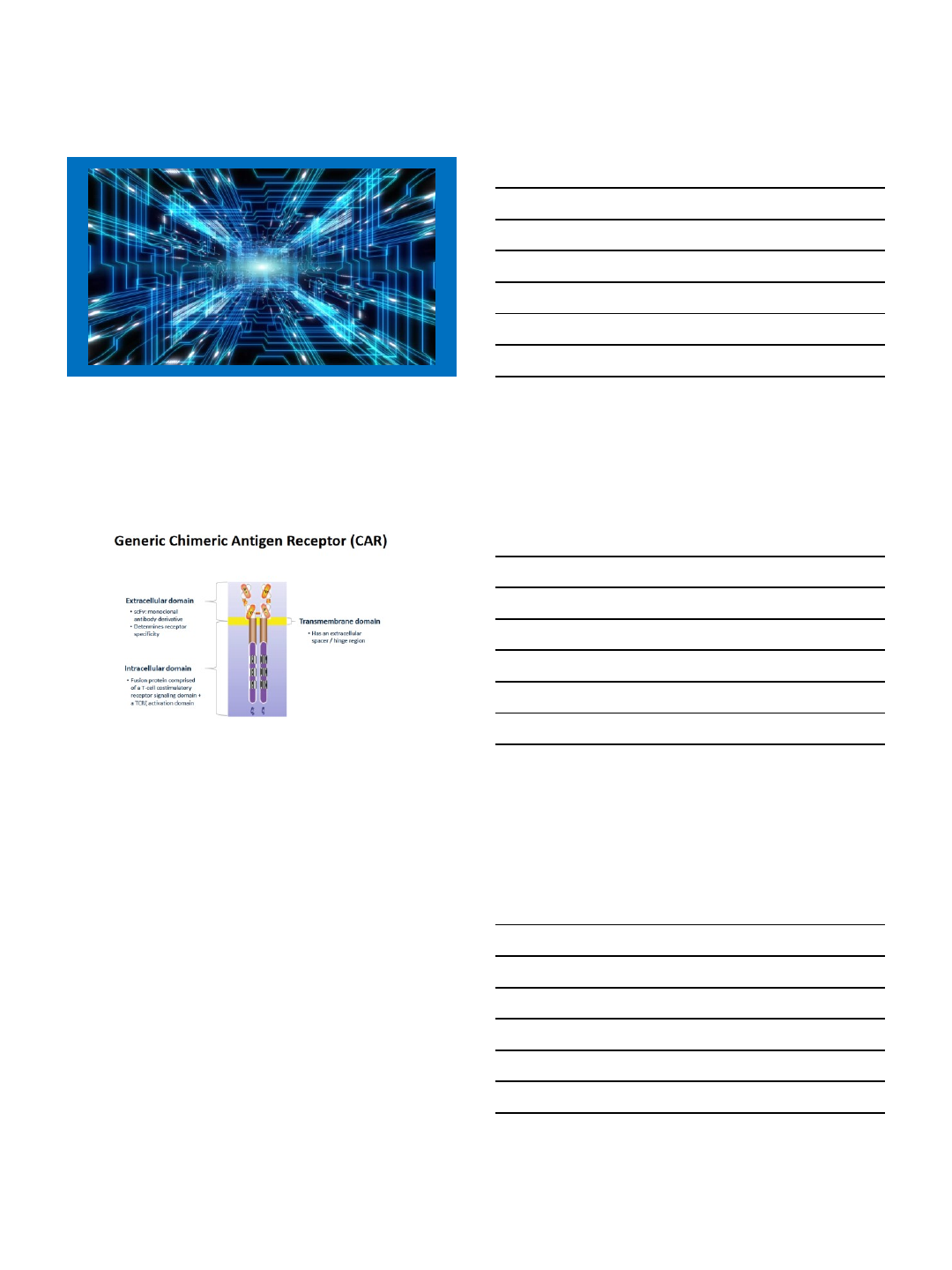
Chimeric Antigen Receptor (CAR) T cells
•Autologous T cells transduced with a lentiviral vector encoding a CAR specific for human BCMA
•State of the art lentiviral vector system
•Optimal 4-1BB costimulatory signaling domain: associated with less acute toxicity and more
durable CAR T cell persistence than CD28 costimulatory domain1
bb2121: AN OPTIMAL BCMA CAR T CELL DESIGN
1. Ali SI, et al. Bloo d. 2016;128(13):1688-700.
bb2121 CAR Design
SP Anti-BCMA scFv CD3z4-1BBMND CD8
Tumor binding domain Signaling Domains
Linker
Promoter
PROGRESSION-FREE SURVIVAL
PFS at Inactive (50 ×106) and Active (150–800 ×106) Dose LevelsaPFS in MRD-Negative Patientsa
Data cutoff: March 29, 2018. Median and 95% CI from Kaplan-Meier estimate. NE, not estimable. aPFS in dose escalation cohort.
•mPFS of 11.8 months at active doses (≥150 ×106CAR+ T cells) in 18 subjects in dose escalation phase
•mPFS of 17.7 months in 16 responding subjects who are MRD-negative
mPFS = 11.8 mo
mPFS = 2.7 mo
mPFS = 17.7 mo

6/18/2018
14
Current Understanding
•Combinations will allow us to improve responses
and cure a higher fraction of patients.
•Drugs with different MOA will overcome genetic
heterogeneity
•High risk disease can be identified and
specifically targeted

6/18/2018
1
Future Directions in Myeloma Post ASCO:
Clinical Trials
Krina Patel MD MSc
Assistant Professor
Department of Lymphoma/Myeloma
University of Texas MD Anderson Cancer Center
Optimizing Dosing Schedule
Once-weekly Versus Twice-weekly Carfilzomib Dosing in Patients with Relapsed and Refractory Multiple Myeloma: Results of the Randomized Phase 3 Study A.R.R.O.W.
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting

6/18/2018
2
A.R.R.O.W. Study Rationale
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting
A.R.R.O.W. Study Design
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting
Primary Endpoint: PFS<br />
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting
6/18/2018
3
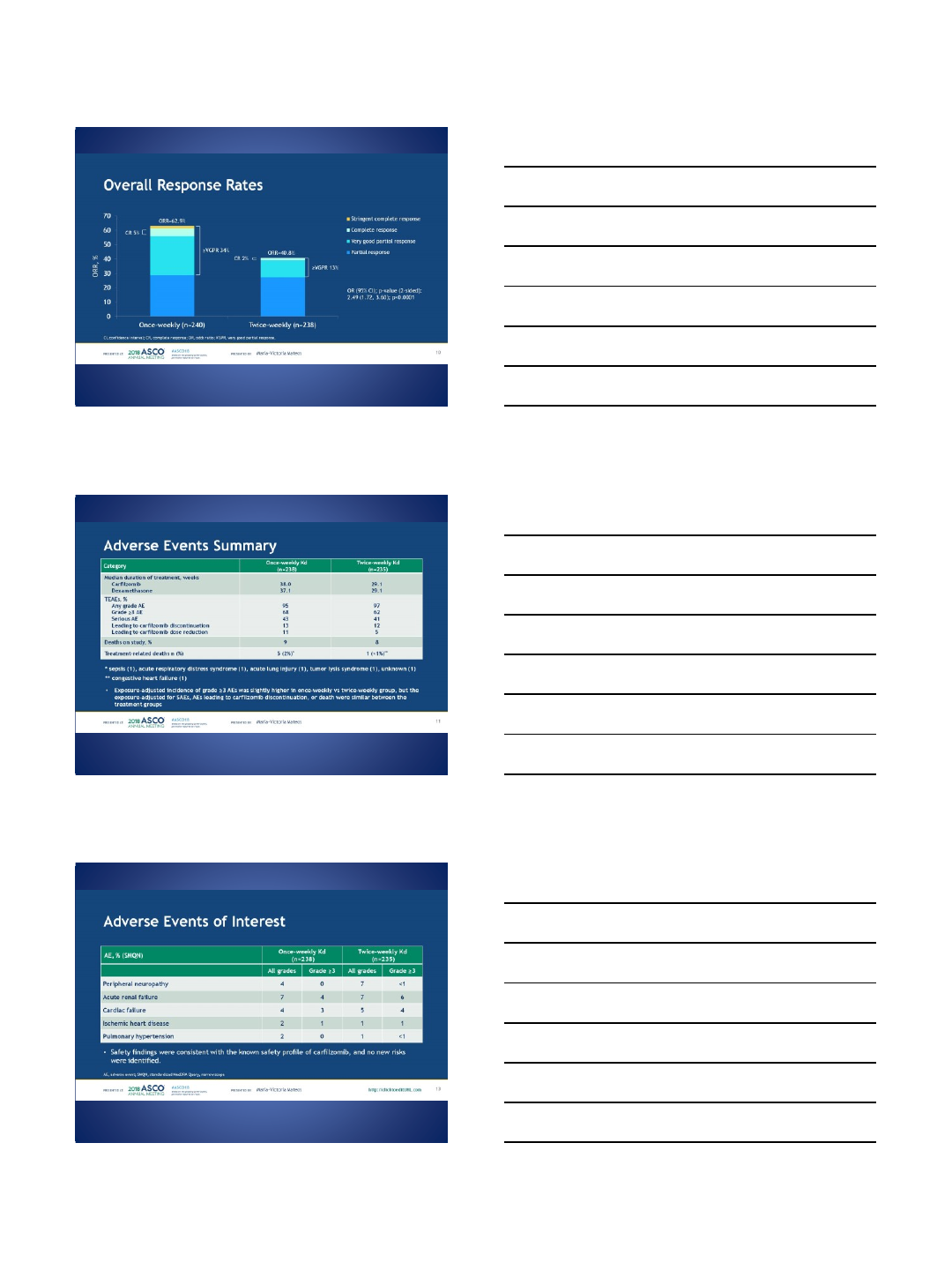
Overall Response Rates
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting
Adverse Events Summary<br />
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting
Adverse Events of Interest
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting

6/18/2018
4
Overall Survival (OS)
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting
Conclusions
Presented By Maria-Victoria Mateos at 2018 ASCO Annual Meeting
Maintenance Revlimid
Does dose matter?

6/18/2018
5
Maintenance Therapy with 25 versus 5 mg Lenalidomide after Prolonged Lenalidomide Consolidation Therapy <br / >in Newly-Diagnosed, Transplant-Eligible Patients with Multiple
Myeloma
Presented By Elizabeth O''Donnell at 2018 ASCO Annual Meeting
Study Design
Presented By Elizabeth O''Donnell at 2018 ASCO Annual Meeting
Dosage
Presented By Elizabeth O''Donnell at 2018 ASCO Annual Meeting

6/18/2018
6
Response
Presented By Elizabeth O''Donnell at 2018 ASCO Annual Meeting
EFS and OS
Presented By Elizabeth O''Donnell at 2018 ASCO Annual Meeting
Safety
Presented By Elizabeth O''Donnell at 2018 ASCO Annual Meeting

6/18/2018
7
Conclusions
Presented By Elizabeth O''Donnell at 2018 ASCO Annual Meeting
Targeted therapy
Phase 2 Study of Venetoclax Plus Carfilzomib and Dexamethasone in Patients With Relapsed/Refractory Multiple Myeloma
Presented By Luciano Costa at 2018 ASCO Annual Meeting

6/18/2018
8
Study Overview
Presented By Luciano Costa at 2018 ASCO Annual Meeting
Dosing
Presented By Luciano Costa at 2018 ASCO Annual Meeting
Enrollment and Patient Disposition
Presented By Luciano Costa at 2018 ASCO Annual Meeting

6/18/2018
9
Summary of Safety (N=42)
Presented By Luciano Costa at 2018 ASCO Annual Meeting
Objective Responses in All Patients and Those Refractory t o PIs and IMiDs
Presented By Luciano Costa at 2018 ASCO Annual Meeting
Conclusions
Presented By Luciano Costa at 2018 ASCO Annual Meeting

6/18/2018
10
New combinations with “old”drugs
abstract 8001
Presented By Paul Richardson at 2018 ASCO Annual Meeting
Phase 3 OPTIMISMM Study Design
Presented By Paul Richardson at 2018 ASCO Annual Meeting

6/18/2018
11
Patient Disposition (ITT)
Presented By Paul Richardson at 2018 ASCO Annual Meeting
Progression-Free Survival (ITT)
Presented By Paul Richardson at 2018 ASCO Annual Meeting
Response
Presented By Paul Richardson at 2018 ASCO Annual Meeting
6/18/2018
12
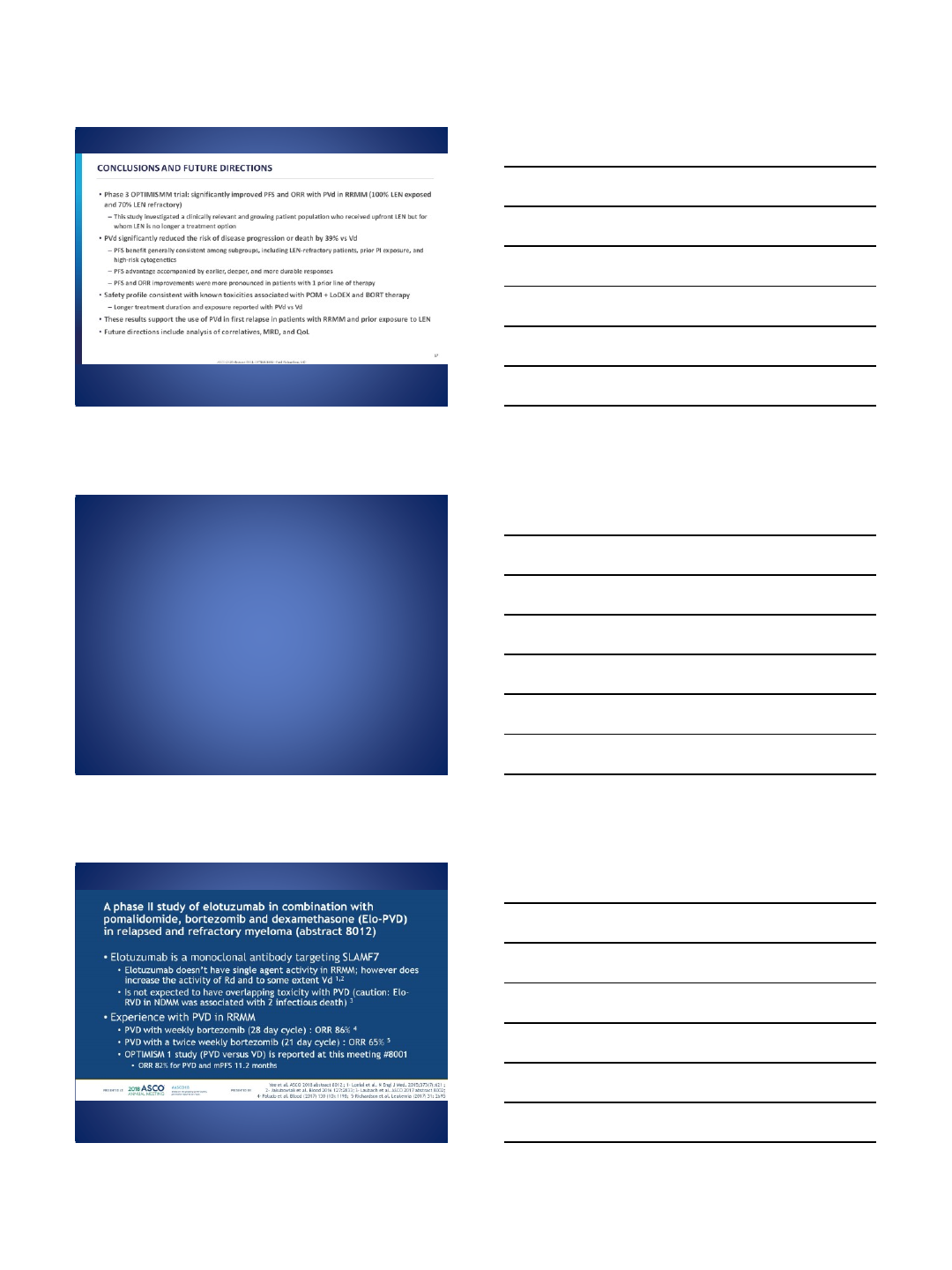
Conclusions and future directions
Presented By Paul Richardson at 2018 ASCO Annual Meeting
Improving Monoclonal Antibodies
A phase II study of elotuzumab in combination with pomalidomide, bortezomib and dexamethasone (Elo–PVD) in relapsed and refractory myeloma (abstract 8012)<br />
Presented By Rachid Baz at 2018 ASCO Annual Meeting

6/18/2018
13
Elo-PVD Results
Presented By Rachid Baz at 2018 ASCO Annual Meeting
Subcutaneous daratumumab in patients with relapsed or refractory multiple myeloma (RRMM): Part 2 update of the open label, multicenter, dose escalation Phase Ib study (PAVO)
(abstract 8013)
Presented By Rachid Baz at 2018 ASCO Annual Meeting
Dara IV or SC?
Presented By Rachid Baz at 2018 ASCO Annual Meeting

6/18/2018
14
Phase 1b Study of Isatuximab and Carfilzomib for the Treatment of Relapsed and/or Refractory Multiple Myeloma (abstract 8014)
Presented By Rachid Baz at 2018 ASCO Annual Meeting
KD with Isa or Dara?
Presented By Rachid Baz at 2018 ASCO Annual Meeting
Conclusions
•Available myeloma treatments are increasing at a
rate higher than ever before.
•Trials are aimed at continuing to improve efficacy
as well as quality of life.
•Optimal combinations of the varying categories
of treatments and sequence of these
combinations needs continued evaluation.

6/18/2018
15
Thank you!
Slides from ASCO meeting library
kpatel1@mdanderson.org
6/18/2018
1
Future Role of CAR T Therapies
in Multiple Myeloma
Nina Shah
University of California San Francisco
B cell maturation antigen (BCMA)
•Consistently expressed on plasma cells/MM cells1
•Possibly protects MM cells in BM niche2
•BMCA expression increases with disease progression3
•Limited expression on normal, non-hematopoietic cells1
1. Carpenter et al, Clinical Cancer Research, 2013
2. Novak et al, Blood 2004
3. Sanchez, 2012
6/18/2018
2
Summary of ongoing BCMA CAR-T Trials for
MM
Name Anti-BCMA CAR Bb2121 LCAR-B38M CART-BCMA
Group NCI
Bluebird/Celgene
Nanjng/Legend
Biotech Novartis/Penn
Binder/co-
stimulatory
signal
Murine/CD3
ζ
, CD28
Murine/CD3ζ, 4-
1BB
Murine/CD3
ζ, 4
-
1BB
Fully
human/CD3ζ, 4-
1BB
Transfection
γ-retroviral Lentiviral Lentiviral Lentiviral
BCMA
expression
required? Yes Yes Yes No
ABSTRACT 8007
bb2121 Anti-BCMA CAR T Cell Therapy in Patients
With Relapsed/Refractory Multiple Myeloma:
Updated Results From a Multicenter Phase I Study
Noopur Raje, MD,1Jesus Berdeja, MD,2Yi Lin, MD, PhD,3Nikhil Munshi, MD,4David Siegel, MD, PhD,5Michaela Liedtke, MD,6Sundar Jagannath, MD,7
Deepu Madduri, MD,7Jacalyn Rosenblatt, MD,8Marcela Maus, MD, PhD,1Ashley Turka,9Lyh Ping Lam, PharmD,9Richard A. Morgan, PhD,9
M. Travis Quigley,9Monica Massaro, MPH,9Kristen Hege, MD,10 Fabio Petrocca, MD,9and James N. Kochenderfer, MD11
1Massachusetts General Hospital Canc er Center, Boston, MA; 2Sarah Cannon Researc h Institute and Tenness ee Oncology, Nashville, TN; 3Mayo Clinic , Rochester, MN;
4Dana-Farber Cancer Institute, Boston, MA; 5Hackensack Univers ity Medical Center, Hackensack, NJ; 6Stanford University Medical Center, Palo Alto, CA; 7Mount Sinai
Medical Center, New York, NY; 8Beth Israel Deaconess Medical Center, Boston, MA; 9bluebird bio, Inc, Cambridge, MA; 10Celgene Corporation, San Francisco, CA;
11Experimental Transplantation and Immunology Branch, National Cancer Institute/National Institutes of Health, Bethesda, MD
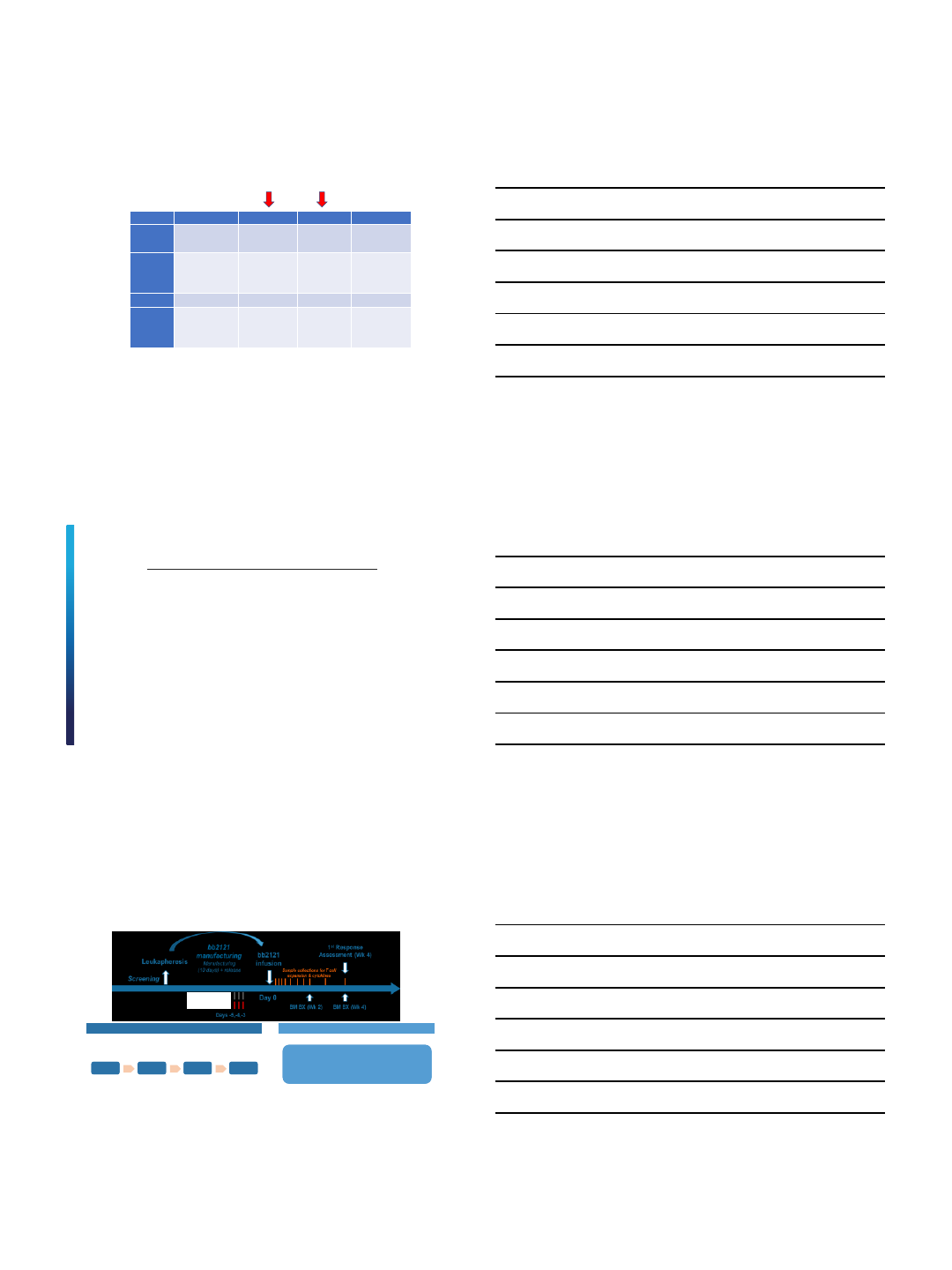
CRB-401 PHASE 1 STUDY DESIGN
≥50% BCMA expression
<50% BCMA expression (n=10)
≥50% BCMA expression (n=12)
Dose range: 150–450 ×106CAR+ cells
<50% BCMA expression (n=10)
≥50% BCMA expression (n=12)
Dose range: 150–450 ×106CAR+ cells
Dose Escalation (N=21) Dose Expansion (N=22)
Flu 30 m/m2
Cy 300 mg/m2
Manufacturing success rate of 100%
150 ×106
150 ×106450 ×106
450 ×106800 ×106
800 ×106
50 ×106
50 ×106

6/18/2018
3
Escalation (N=21) Expansion (N=22)
Exposed Refractory Exposed Refractory
Prior
therapies, n (%)
Bortezomib 21 (100) 14 (67) 22 (100) 16 (73)
Carfilzomib 19 (91) 12 (57) 21 (96) 14 (64)
Lenalidomide 21 (100) 19 (91) 22 (100) 18 (82)
Pomalidomide 19 (91) 15 (71) 22 (100) 21 (96)
Daratumumab 15 (71) 10 (48) 22 (100) 19 (86)
Exposed/Refractory, n (%)
Bort/Len 21 (100) 14 (67) 22 (100) 14 (64)
Bort/Len/Car/Pom/Dara 15 (71) 6 (29) 21 (96) 7 (32)
Escalation
(N=21)
Expansion
(N=22)
Median (
min, max) prior regimens 7 (3, 14) 8 (3, 23)
Prior autologous SCT, n (%)
21 (100) 19 (86)
00 3 (14)
1 15 (71) 14 (64)
>1 6 (29) 5 (23)
TREATMENT HISTORY
Data cutoff: March 29, 2018. SCT, stem cell transplant.
ADVERSE EVENTS OF SPECIAL INTEREST
TEAE, n (%)
Overall Grade ≥3
Cytokine
release syndromea27 (63) 2 (5)
Neurotoxicity
b14 (33) 1 (2)
Neutropenia
35 (81) 34 (79)
Thrombocytopenia
26 (61) 22 (51)
Anemia
24 (56) 19 (44)
Infection
c
Overall
First Month
26 (61)
10 (23)
9 (21)
2 (5)
CAR T Treatment-Emergent Adverse Events
All Infused Patients (N=43)
Data cutoff: March 29 , 2018. NE, not estimable. aCRS uniformly graded per Lee DW, et al. Blood. 2014;124(2):188-195. bEvents occurring in first 28 d and including dizziness, bradyphrenia, somnolence, confusional state, nystagnmus,
insomnia, memory impairment, depressed level of consciousness, neurotoxicity, lethargy, tremor and hallucination. cI ncludes the SOC Infections and Infestations. Events observed in >10% include upper respiratory tract infection and
pneumonia. dIncludes patients treated with active doses (150–800 ×106CAR+ T cells; N=40). Median and 95% CI fr om Kaplan-Meier estimate. eTime from first bb2121 infusion to the fir st grade ≤2 event after day 32.
Neutropenia
(n=9)
Thr ombocytopenia
(n=18)
Events
710
Median (95% CI), mo
2 (1.2–2.6) 3 (1.9–NE)
Time to Recovery of Grade 3/4 Cytopenias in Patients
Without Recovery by Month 1d
Probability of Recovery, %
Time After bb2121 Infusion, monthse
•No grade 4 CRS events
•No fatal CRS or neurotoxicity events
•31/40 (78%) recovered ANC to ≥1000/µL by Day 32
•22/40 (55%) recovered PLT to ≥50,000/µL by Day 32
CYTOKINE RELEASE SYNDROME: MOSTLY LOW GRADE
AND MANAGEABLE
Parameter
Dosed Patients
(N=43)
Patients with a CRS event, n (%)
27 (63)
Maximum CRS
gradea
None
1
2
3
4
16 (37)
16 (37)
9 (21)
2 (5)
0
Median (min, max) time to onset, d
2 (1, 25)
Median (min, max) duration
, d 6 (1, 32)
Tocilizumab use, n (%)
9 (21)
Corticosteroid
use, n (%) 4 (9)
Cytokine Release Syndrome Parameters
Data cutoff: Ma rch 29, 2018. aC RSuniformly graded according to Lee DW, et al. Blood. 2014;124(2):188-195.b3 patients were treated at the 50 x 106 dose level for a total of 43 patien ts.
Cytokine Release Syndrome By Dose Level
Dose Levelb
16.7
50.0
22.2
22.7
9.1
0
10
20
30
40
50
60
70
80
90
100
150 x 106 >150 x 106
Patients, %
3 2 1
39%
82%
>150 × 106
(n=22)
150 ×106
(n=18)
Maximum Toxicity Gradea

6/18/2018
4
12.5 9.1
50.0
27.3
37.5
54.5
0
10
20
30
40
50
60
70
80
90
100
450 x 106 low 450 x 106 high
Objective Response Rate, %
sCR/CR
VGPR
PR
33.3
7.1 9.1
7.1
36.4
42.9
50.0
0
10
20
30
40
50
60
70
80
90
100
50 x 106 150 x 106 >150 x 106
Objective Response Rate, %
sCR/CR
VGPR
PR
TUMOR RESPONSE: DOSE-RELATED; INDEPENDENT OF TUMOR
BCMA EXPRESSION
Data cutoff: March 29, 201 8. CR, complete respons e; mDOR, median duration of response; ORR, objective r esponse rate; PD, progressive disease; PR, partial response; sCR, stringent CR; VGPR, very good partial
response. aPatients with ≥2 months of response data or PD/death within <2 months. ORR is defined as attaining sCR, CR, VGPR, or PR, including confirmed and unconfirmed respons es. Low BCMA is <50% bone
marrow plasma cells expression of BCMA; high BCMA is defined as ≥50%.
Tumor Response By DoseaTumor Response By BCMA Expressiona
ORR=33.3%
mDOR=1.9 mo
ORR=57.1%
mDOR=NE
150 ×106
(n=14) >150 × 106
(n=22)
50 ×106
(n=3)
ORR=95.5%
mDOR=10.8 mo
450 ×106
High BCMA
(n=11)
Median follow-up
(min, max), d 87
(36, 638)
84
(59, 94) 194
(46, 556) Median follow-up
(min, max), d
450 ×106
Low BCMA
(n=8)
311
(46, 556)
ORR=100%
ORR=91%
168
(121, 184)
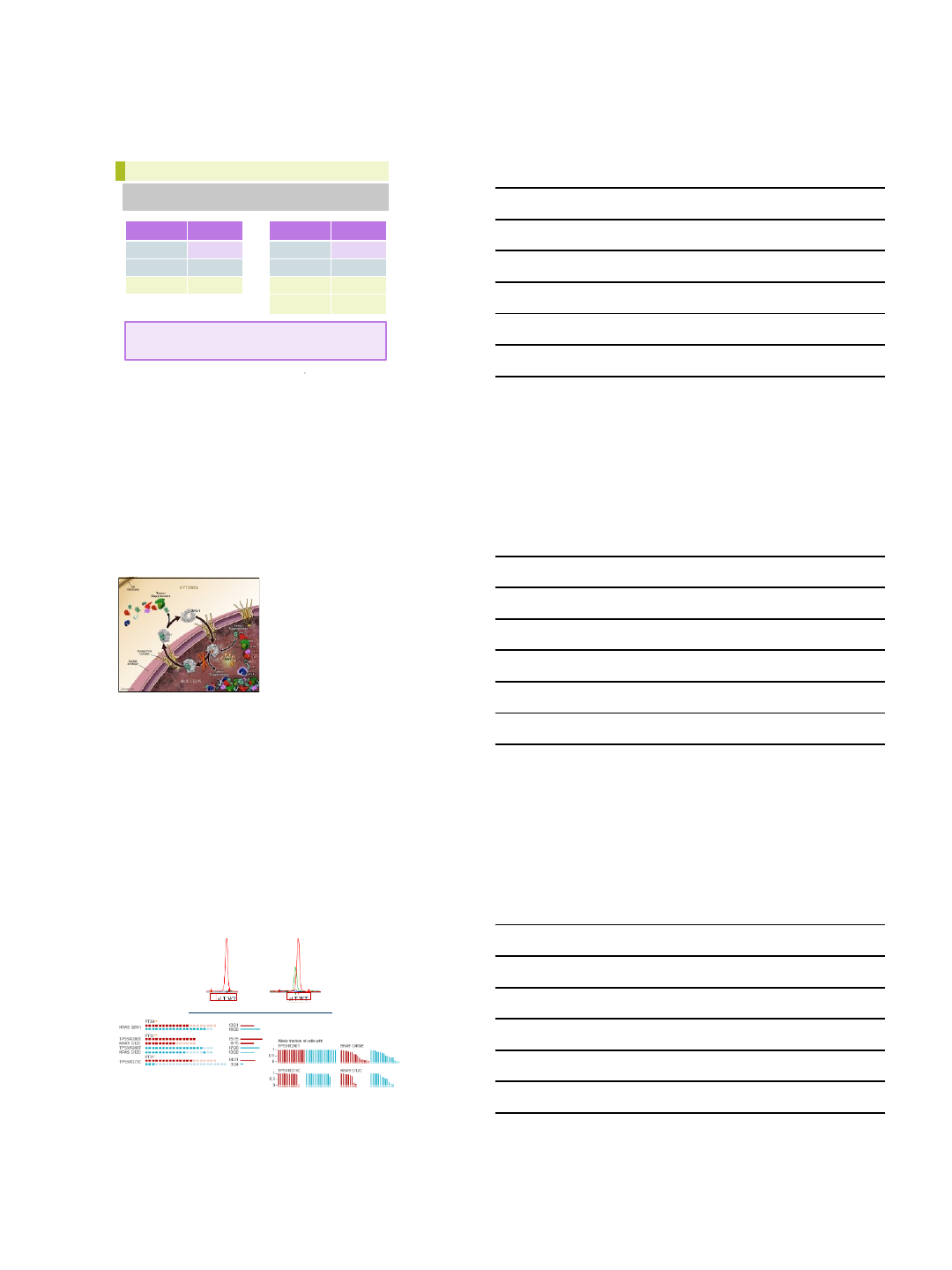
PROGRESSION-FREE SURVIVAL
PFS at Inactive (50 ×106) and Active (150–800 ×106) Dose LevelsaPFS in MRD-Negative Patients
Data cutoff: March 29 , 2018. Median and 95% CI from Kaplan-Meier estimate. NE, not estimable. aPFS in dose escalation cohort.
50 ×106
(n=3)
150
–800 ×106
(n=18)
Events
310
mPFS
(95% CI),
mo
2.7
(1.0–2.9)
11.8
(8.8–NE)
150–800 ×106
(n=16)
mPFS
(95% CI),
mo
17.7
(5.8–NE)
•mPFS of 11.8 months at active doses (≥150 ×106CAR+ T cells) in 18 subjects in dose escalation phase
•mPFS of 17.7 months in 16 responding subjects who are MRD-negative
mPFS = 11.8 mo
mPFS = 2.7 mo
mPFS = 17.7 mo
Summary of ongoing BCMA CAR-T Trials for
MM Name Anti-BCMA CAR Bb2121 LCAR-B38M CART-BCMA
Group NCI Bluebird/Celgene Nanjng/Legend
Biotech Novartis/Penn
Binder/co-
stimulatory
signal
Murine/CD3ζ, CD28
Murine/CD3
ζ, 4-
1BB
Murine/CD3ζ, 4-
1BB
Fully human/CD3ζ,
4-1BB
Transfection γ-retroviral Lentiviral Lentiviral Lentiviral
BCMA
expression
required?
Yes Yes Yes No
Median prior
lines of tx 7, 11 7 3 9
Efficacy
1 sCR (relapsed), 1
VGPR, 2 PR, 8 SD
Responses in highest
cell dose;
9/11 in top
dose
10 CRs, 6 VGPR, 1
PRs (4 eventual PD),
n=18
at >5 e7 : 94% RR
9 MRD neg
33 CR or VGPR,
n=35, 1 relapse; 5
MRD neg > 1 yr
6/9, 2/5, 5/6
responses in 3
cohorts
Safety
Toxicity substantial
(Gr3-4CRS) but
reversible esp in
highest doses (9
e6/kg); protocol
modified to pts with
lower tumor burden
CRS in 71%;
transient Gr3 10%; 5
deaths (cardio
-
pulm
arrest, unrelated, 1
MDS, 3 PD at lowest
dose)
Early report of 1 Gr
4 neurotoxicity
Transient CRS
29/35, no
neurotox
CRS in 17/21 pts (6
with Gr2), with
neurotox in 3 pts
1 death –
candidemia/PD
6/18/2018
5
16
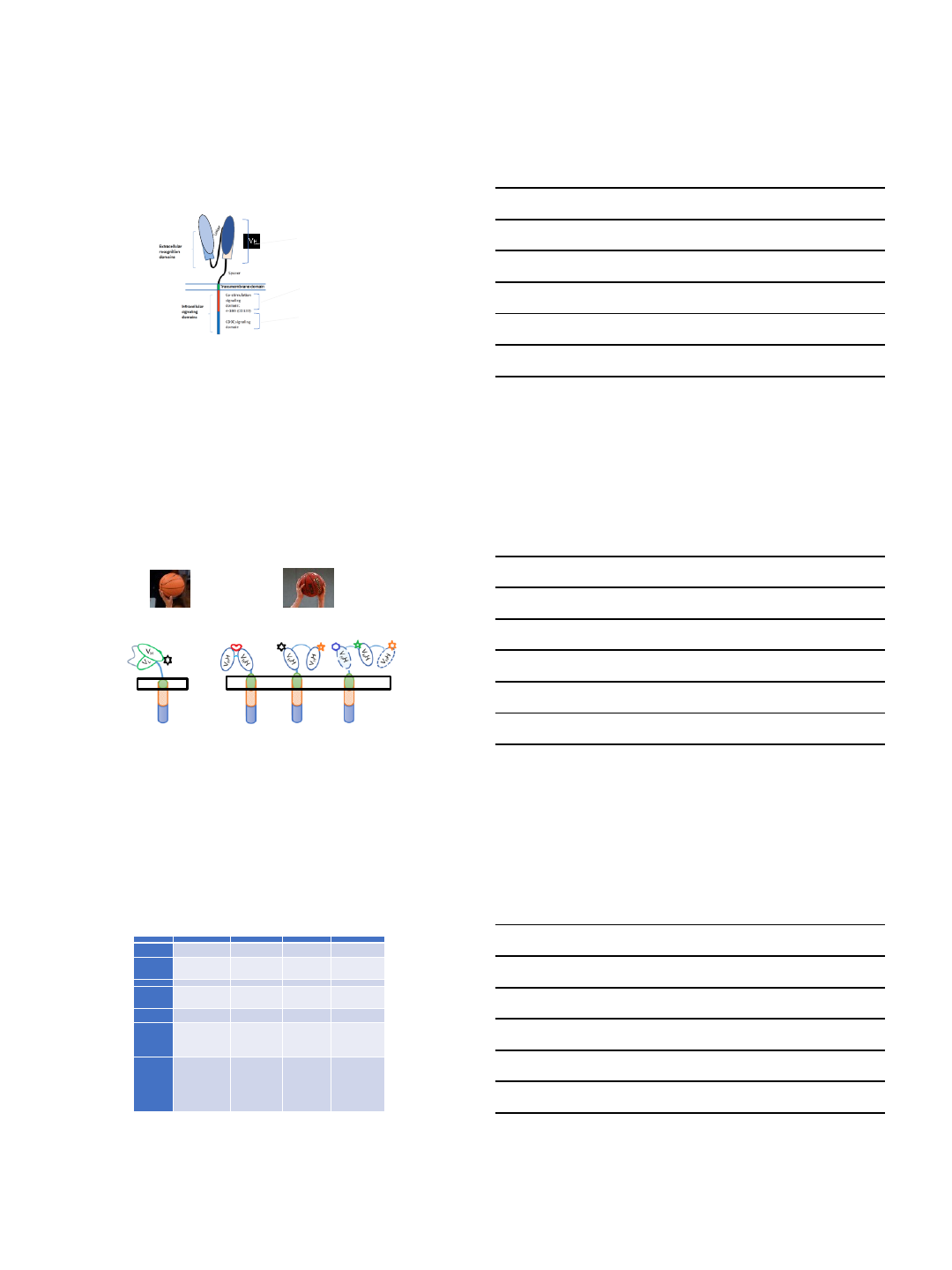
JNJ-68284528 (LCAR-B38M CAR-T cells)
Genetically modified autologous T-cell immunotherapy directed at B-cell maturation antigen (BCMA) which is being developed for the treatment of
Multiple Myeloma
VHH VHH
Linker = (Glycine)4Serine
2 different anti-BCMA VHH
domains for enhanced
avidity –T cell function is
avidity driven
4-1BB: built-in “2nd
Signal” costimulatory
signaling
CD3z: TCR-like
activation
JNJ-528 is a unique bispecific CAR that binds with high affinity to 2 different epitopes on BCMA, enabling tight
binding of the CAR to the BCMA-expressing cells Courtesy of Janssen
JNJ-68284528 (LCAR-B38M) CAR T cell: designed for high affinity interaction
with BCMA-expressing tumor cells
Conventional CAR-T LCAR-B38M VHH multi-specific CAR
scFv-Conventional CAR VHH-Bi-epitope CAR VHH-multi-specific CAR
BCMA Target A Target B
Courtesy of Janssen
Summary of ongoing BCMA CAR-T Trials for
MM Name Anti-BCMA CAR Bb2121 LCAR-B38M CART-BCMA
Group NCI Bluebird/Celgene Nanjng/Legend
Biotech Novartis/Penn
Binder/co-
stimulatory
signal
Murine/CD3ζ, CD28
Murine/CD3
ζ, 4-
1BB
Murine/CD3ζ, 4-
1BB
Fully human/CD3ζ,
4-1BB
Transfection γ-retroviral Lentiviral Lentiviral Lentiviral
BCMA
expression
required?
Yes Yes Yes No
Median prior
lines of tx 7, 11 7 3 9
Efficacy
1 sCR (relapsed), 1
VGPR, 2 PR, 8 SD
Responses in highest
cell dose;
9/11 in top
dose
ORR= 57% , 96% in
pts @>150 e6
;
mPFS
11.8
mo, 17.7 mo
in
MRD neg pts
33 CR or VGPR,
n=35, 1 relapse; 5
MRD neg > 1 yr
6/9, 2/5, 5/6
responses in 3
cohorts
Safety
Toxicity substantial
(Gr3-4CRS) but
reversible esp in
highest doses (9
e6/kg); protocol
modified to pts with
lower tumor burden
CRS in 71%;
transient Gr3 10%; 5
deaths (cardio
-
pulm
arrest, unrelated, 1
MDS, 3 PD at lowest
dose)
Early report of 1 Gr
4 neurotoxicity
Transient CRS
29/35, no
neurotox
CRS in 17/21 pts (6
with Gr2), with
neurotox in 3 pts
1 death –
candidemia/PD
6/18/2018
6
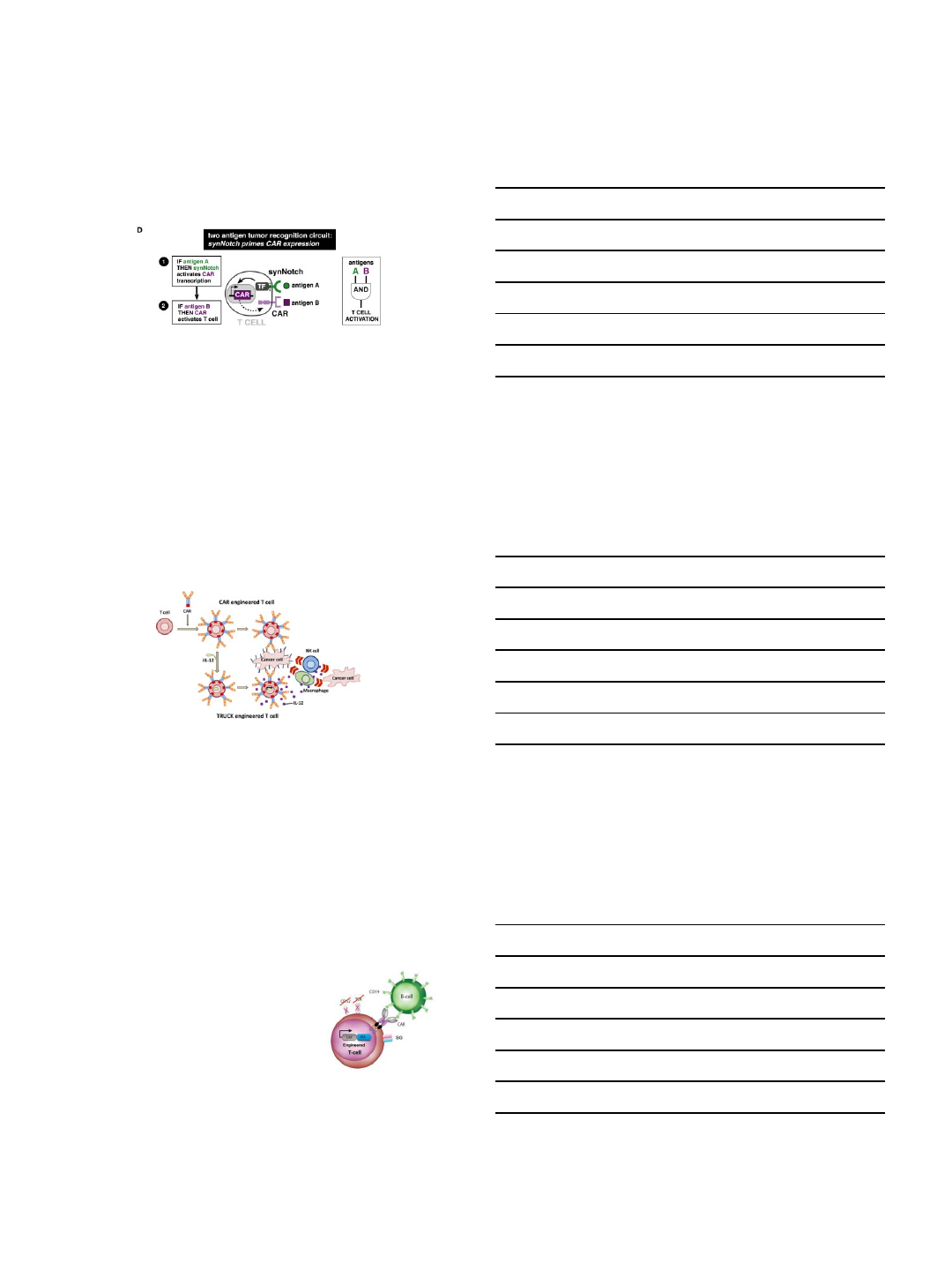
Challenges in CAR T therapy for MM
•CRS (hopefully not as much of an issue as with ALL)
•Persistence
•Lymphodepletion
•Cytokine-based T-reg elimination
•Virus-specific T cells as primary CAR-T population
Virus-specific T cells as primary CAR-T
population
1. Maus et al, CCR 2016
Challenges in CAR T therapy for MM
•CRS (hopefully not as much of an issue as with ALL)
•Persistence
•Lymphodepletion
•Cytokine-based T-reg elimination
•Virus-specific T cells as primary CAR-T population
•Optimizing co-stimulatory signaling
•41BB>CD28
•Nature of MM is waxing and waning, should the cells be that way as
well?
•“ON-switch” CARs
•Targeting multiple antigens
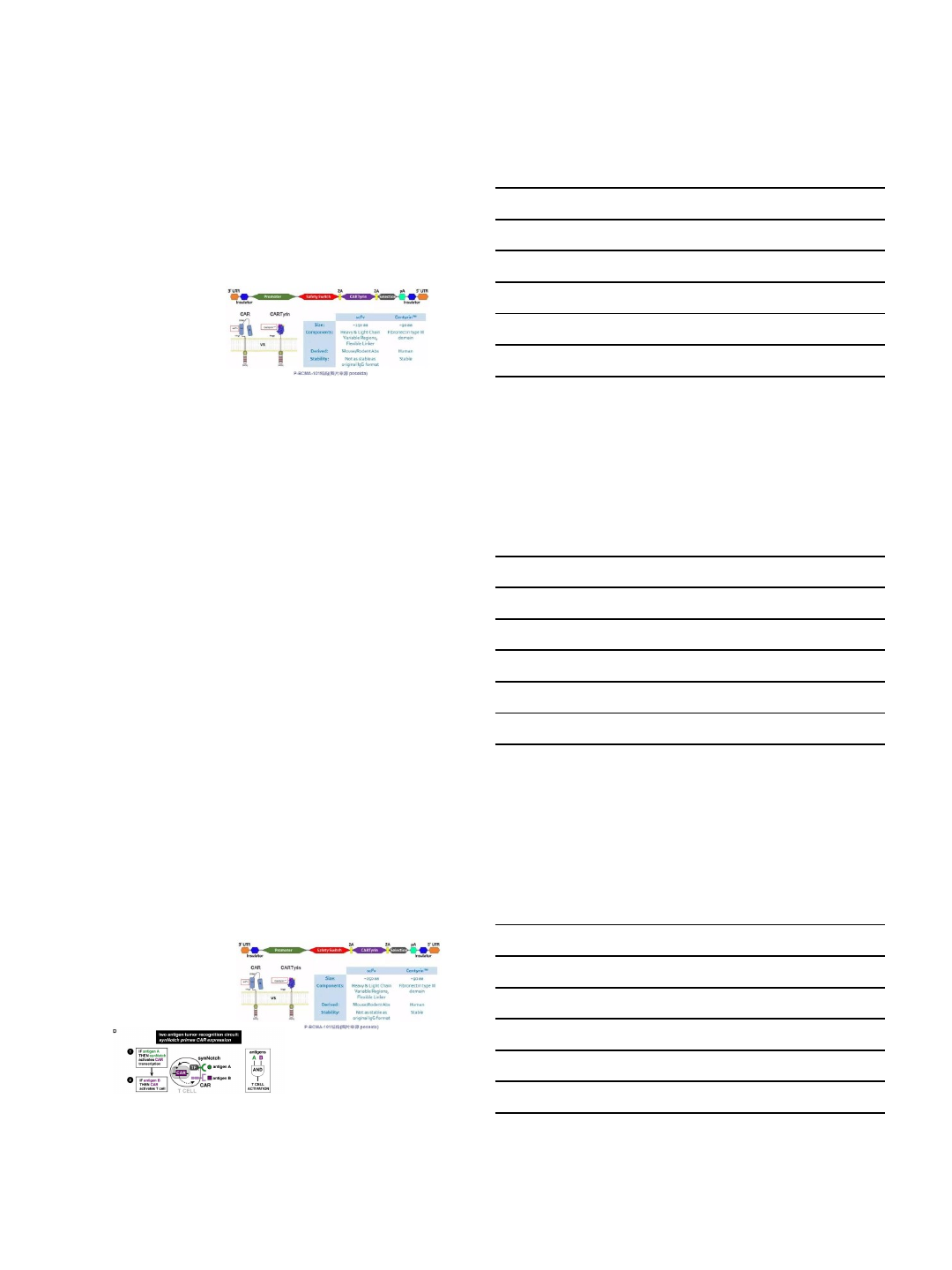
•T cells redirected for universal cytokine-mediated killing (TRUCKs)
6/18/2018
7
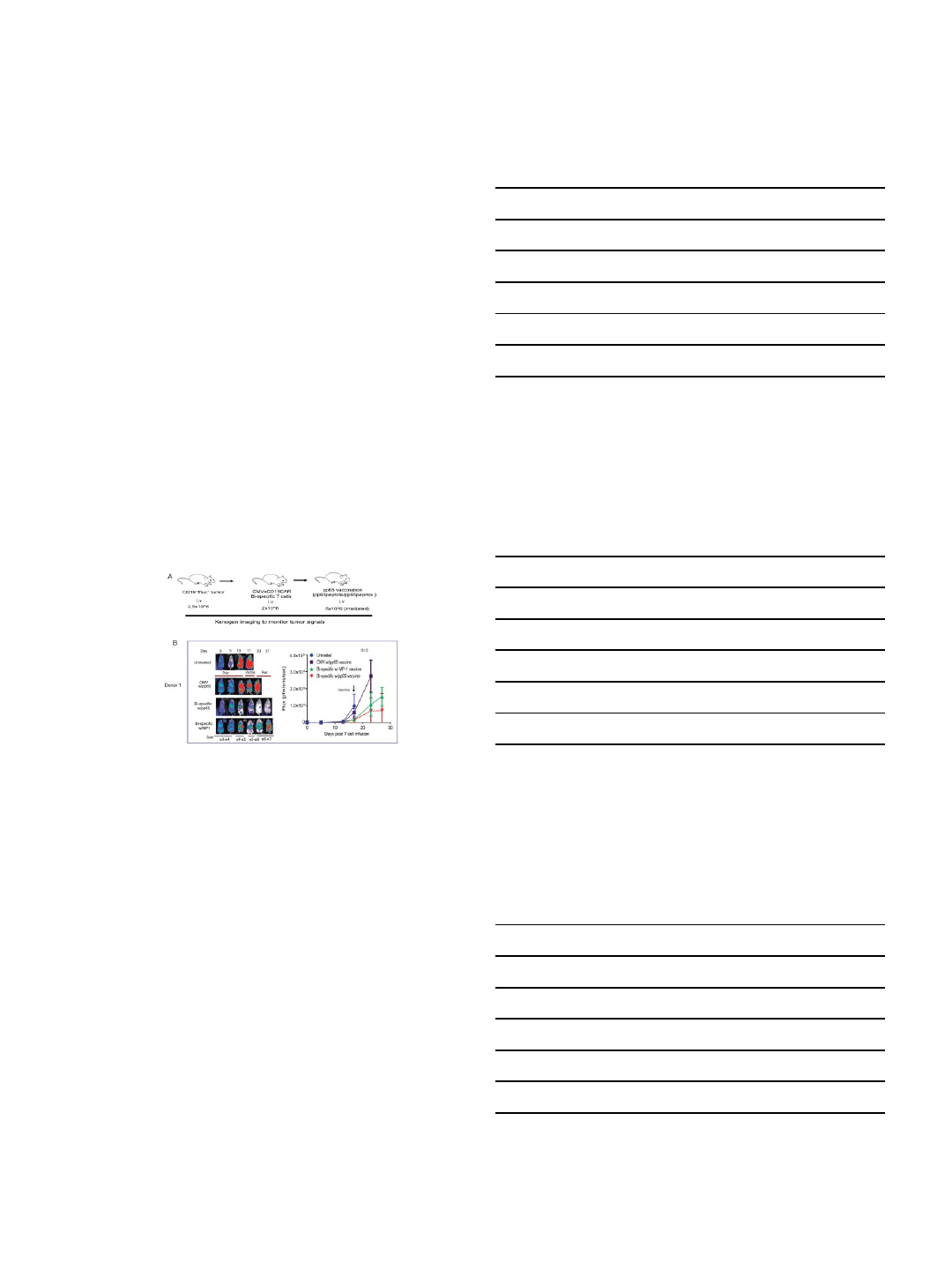
“On” switch CAR T cells
1. Roybal et al, Cell 2016
T cells redirected for universal cytokine-
mediated killing (TRUCKs)
1. Chiemelewski et al, Immunological Reviews, 2013
Cellectis Universal SLAMF7-Specific CAR T
(abs 502)
•“Off-the-shelf”
•Normal healthy PB donors
•Inactivation of the TCRα constant (TRAC)
gene using TALEN®gene-editing technology
to prevent GVHD and expression of T cell
SLAMF7.
6/18/2018
8
Poseida: CARTyrin (abs 3068)
•DNA transposon system
•iCasp9-based safety switch
•Anti-BCMA CARTyrin
•Selection gene (~ 100% pure CAR+product)
•Enrich stem cell memory T cell subset
But where are we really going…?
•Timing of CART
•Disease burden
•Position relative to autologous transplant
•Cost
•Time and financial cost of proving superiority
•Clinical trial design
•MRD as endpoint
“It’s my CAR-T and I’ll cry if I want to…”
•Persistence
•Inducibility

6/18/2018
9
Case
•65 YO M without significant PMH presents with new back pain and
incidentally found abnormal protein level
•Further work-up shows IgG kappa M-spike 3.8 g/dL
•Additional labs: normal Cr, Ca; Hb=11.8 g/dL
•MRI shows new L4 compression fracture
•BM biopsy: 60% kappa-restricted plasma cells, normal cytogenetics, FISH
positive for t(11;14)
Treatment course
•VRD induction→achieves VGPR after 6 cycles
•Mel 200 ASCT→sCR at day 100 with MRD negativity
•Len maintenance x 2.5 y--> biochemical progression
•KRD with PR; Goes 18 months but then presents with new bone
lesions
•Starts DRD→Stable x 12 months but then presents wit new anemia.
BM with 70% plasma cells and clonal evolution (-16)
Now what??
Thank you!
nina.shah@ucsf.edu
6/18/2018
1
Smoldering Myeloma
Irene Ghobrial, MD
Associate Professor of Medicine
Harvard Medical School
Dana Farber Cancer Institute
Boston, MA
Ductal Carcinoma in Situ
MGUS
Multiple Myeloma
Metastatic breast cancer
Treat as early
as possible
CURE
Watch and
wait until end
organ damage
NO CURE
Is it time to treat patients with Smoldering MM
Kyle R. N Engl J Med 2007; 356:2582-90; Greipp RR, et al. J Clin Oncol 2005;23:3412–3420
Which patient population to consider for SMM?
100
80
60
40
20
0
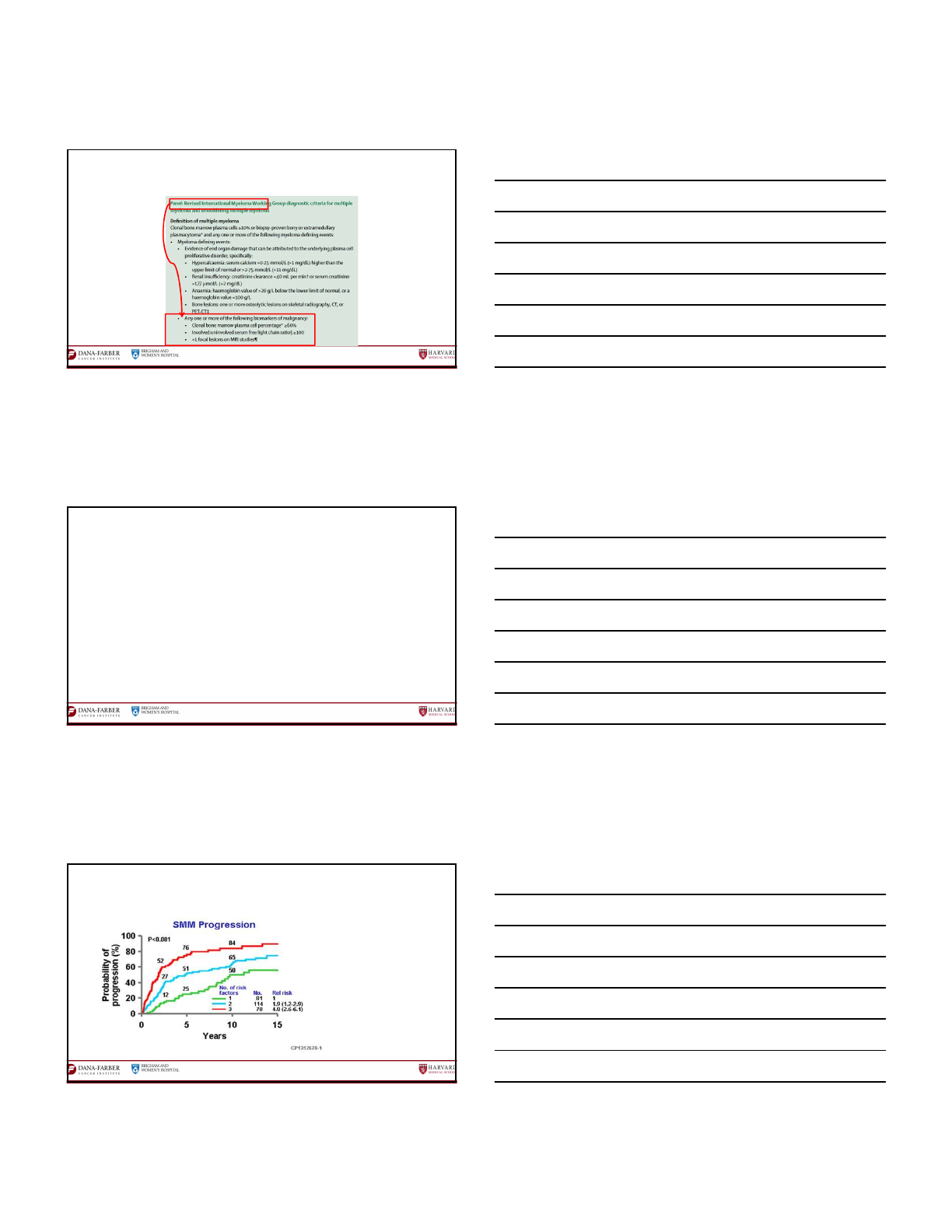
27% will convert in 15 years
Roughly 2% per year
51% will convert in first 5 yrs
~ 10% per yr
0510 15 20 25
Probability of Progression (%)
51
66
73 78
410 16 21
MGUS
Smoldering MM
Yrs Since Diagnosis
27% more will convert in remaining 15 yrs
~ 2% per yr
6/18/2018
2
Rajkumar et al. Lancet Oncology 2014; 15: e538-48
What is the definition of MM or SMM?
Identification of high-risk SMM50% of progression risk at 2y
•Mayo Clinic: ≥10% clonal plasma cell bone marrow infiltration, and ≥30g/L of serum M-protein, and
serum-free light ratio >0.125 or <8
•Spanish: ≥95% of aberrant plasma cells measured by flow plus >25% decrease in one or both uninvolved
immunoglobulins
•Heidelberg: Tumor mass defined by Mayo risk model plus t(4;14)/del17p/gains of 1q/
•Japanese: Beta 2-microglobulin ≥ 2.5 mg/L plus M-protein increment rate > 1 mg/dL/day
•SWOG: serum M-protein ≥2 g/dL plus involved free light chain >25 and GEP >-0.26 (71% of risk progression at 2 yrs)
•PENN: ≥ 40% clonal PCBM infiltration plus sFLC ratio ≥ 50 plus Albumin 3.5 mg/dL (81% of risk at 2 yrs
•Czech & Heidelberg: immunoparesis plus serum M-protein ≥ 2.3 g/dL plus involved/uninvolved sFLC > 30
(81% of risk at 2 yrs)
•Barcelona: evolving pattern plus serum M-protein ≥ 3 g/dL plus immunoparesis (80% of risk at 2 yrs)
What is high risk SMM?
Dispenzieri A. Blood 2008; 111:785-9
Mayo Clinic model: serum immunoglobulin
free-light chain (FLC) ratio (n:273)
PCsBM Infiltration ≥ 10%
Serum M protein ≥ 3 g/dL
Serum FLC ratio <1/8 or >8

6/18/2018
3
Evolution pattern of the M-spike:
evolving vs nonevolving (n:207)
Fernández Larrea C et al. ASH 2014
Evolving SMM (52 (25%)):
at least 10% increase within the first 6 months from diagnosis when
M-Protein was ≥30 g/L or progressive increase in M-Protein in each of the annual consecutive measurements during a period of 3 years
in patients with an initial MP < 30 g/L
Non-evolving (75%):
Stable serum M-protein until progression occurs
Evolving SMM
• Risk progression at 2 years: 45%
• Risk progression at 5 years: 78%
• IgA isotype:
(41,2% frente a 23,8%, p=0,02)
Median TTP 3 years
Mediana TTP 19,4 years
p< 0,001
Each model appears to identify patients at high risk, with some but not complete overlap
Bone
marrow
clonal
plasma
cells
≥10%
and
any
one
or
more
of
the
following:
•Serum
M
protein
≥3.0gm/dL
•IgA
SMM
•Immunoparesis
with
reduction
of
two
uninvolved
immunoglobulin
isotypes
•Serum
involved/uninvolved
free
light
chain
ratio
≥8
(but
less
than
100)
•Progressive
increase
in
M
protein
level
(Evolving
type
of
SMM)
†
•Bone
marrow
clonal
plasma
cells
50-60%
•Abnormal
plasma
cell
immunophenotype
(≥95%
of
bone
marrow
plasma
cells
are
clonal)
and
reduction
of
one
or
more
uninvolved
immunoglobulin
isotypes
•t
(4;14)
or
del
17p
or
1q
gain
•Increased
circulating
plasma
cells
•MRI
with
diffuse
abnormalities
or
1
focal
lesion
(≥5mm)
•PET-CT
with
one
focal
lesion
(≥5mm)
with
increased
uptake
without
underlying
osteolytic
bone
destruction
•Monoclonal
light
chain
excretion
of
500mg/24
hours
or
higher
Which patient population to consider for high risk SMM?
Rajkumar et al, Blood 2015
Should we consider therapeutic interventions in SMM
Manier, Salem, et al. Nat Rev Clin Oncol, 2016

6/18/2018
4
Whole-exome and targeted sequencing of SMM BM samples
Non-pr ogressors -
26
Progressors - 37
A.
B.
C.
D.
Bustoros et al, Unpublished data
Should we use single agents or combination
therapy to treat high-risk SMM
Genomic profile of high risk SMM indicates that it is similar to overt MM
Treatment goals for high-risk
smouldering myeloma
Landgren et al, Clin Cancer Research 2011
Early Therapeutic Intervention
Mateos MV, et al. NEJM 2013
Mateos MV, et al. Lancet Oncology 2016

6/18/2018
5
As of 08/14/2015 11 patients were enrolled on Arm B (Elotuzumab
and Revlimid). As of 1/15/16, the protocol was amended to
continue enrollment to Arm A (Elotuzumab, Revlimid, and
Dexamethasone) and halt enrollment to Arm B . To date, 40 patients
have been enrolled on Arm A.
2
Months
Elotuzumab Days 1, 8,
15, 22
Revlimid Days 1-21
6
Months
Elotuzumab Days 1, 15
Revlimid Days 1-21
16
Months
Elotuzumab Day 1
Revlimid Days 1-21
End of
Treatment
Event
Monitoring
(Up to 3 years)
2
Months
Elotuzumab Days 1, 8,
15, 22
Revlimid Days 1-21
Decadron Days 1, 8,
15, 22
6
Months
Elotuzumab Days 1, 15
Revlimid Days 1-21
Decadron Days 1, 8, 15
16
Months
Elotuzumab Day 1
Revlimid Days 1-21
End of
Treatment
Event
Monitoring
(Up to 3 years)
Arm
B
Stem Cell Mobilization and Collection
Arm
A
Stem Cell Mobilization and Collection
Phase II trial of Elotuzumab/Len/Dex in high risk SMM
Ghobrial I, et al. ASH 2016. Abstract 976
GEM-CESAR: Study Design
• Multicenter, open-label, phase II trial
Induction
6 x 28-day
cycles
*High-risk was defined according to the Mayo and/or Spanish models
- Patients with any one or more of the biomarkers predicting imminent risk of progression to MM were
allowed to be included but…
- New imaging assessments were mandatory at screening and if bone disease was detected by CT or
PET-CT, patients were excluded
High-risk*
Smouldering
MM patients
N=90
Carfilzomib i.v.
20/36 mg/m
2
Days 1, 2, 8, 9, 15,
16
Lenalidomide
25 mg
Days 1–21
Dexamethasone
40 mg
Days 1, 8, 15 & 22
Carfilzomib i.v.
20/36 mg/m
2
Days 1, 2, 8, 9, 15,
16
Lenalidomide
25 mg
Days 1–21
Dexamethasone
40 mg
Days 1, 8, 15 & 22
High-dose
Melphalan
[200 mg/m
2
]
Followed by
ASCT
High-dose
Melphalan
[200 mg/m
2
]
Followed by
ASCT
Carfilzomib i.v.
20/36 mg/m
2
Days 1, 2, 8, 9, 15,
16
Lenalidomide
25 mg
Days 1–21
Dexamethasone
40 mg
Days 1, 8, 15 & 22
Carfilzomib i.v.
20/36 mg/m
2
Days 1, 2, 8, 9, 15,
16
Lenalidomide
25 mg
Days 1–21
Dexamethasone
40 mg
Days 1, 8, 15 & 22
Consolidation
2 x 28-day
cycles
Lenalidomide
10 mg
Days 1–21
Dexamethaso
ne
20 mg
Days 1, 8, 15
& 22
Lenalidomide
10 mg
Days 1–21
Dexamethaso
ne
20 mg
Days 1, 8, 15
& 22
Maintenance
24 x 28-day
cycles
Mateos MV, et al. ASH 2017, abstract 402
Current Studies in High-Risk Smoldering MM
• Lenalidomide or observation (phase III)
1
•Ixazomib + lenalidomide + dexamethasone (phase II)
2
• Isatuximab (phase II)
3
• Daratumumab single agent at different doses (Centaurus trial)
4
•Dara ph II for high-risk MGUS and low-risk smoldering
5
•Randomized Ph III AQUILA (sc)
6
1. ClinicalTrials.gov. NCT01169337.
2. ClinicalTrials.gov. NCT02916771.
3. ClinicalTrials.gov. NCT02960555.
4. Hofmeister CC, et al. Blood 2017 130:510
5. ClinicalTrials.gov. NCT03236428.
6. ClinicalTrials.gov. NCT03301220.
Recruitment status: Recruiting
Start date: November 2017
Estimated completion date: December 2025

6/18/2018
6
Center for Prevention of Progression of Blood Cancers
PCROWD
Biology
Screening
Therapeutic
Retrospective
Studies
www.dana-farber.org/cpop
pcrowd.dana-farber.org/
Predicting progression of developing Myeloma in a
High-Risk screened population
(PROMISE)

6/18/2018
7
Gad Getz, V iktor Adelsteinsson, Ken Anderson, Rob Soiffer, Nikhil Mun shi, P aul Richardson, Ben Ebert.
Other collaborators: David Scadden, Shaji Kumar, Ola Landgren, Antonio Palumbo, Herve Ave L’oiseau, Xavier Leleu,, Leif Bergsagel, Marta
Chesi, Bruno Paiva, Jesus San Miguel, Richard Hynes, George Daley, Jon Licht, Gad Getz, David Root. Viktor Adalsteinsson
Aldo Roccaro, Salomon Manier, Jihye P ark, Antonio Sacco, Yujia Shi, Yuji Mishima, Oksana Zavidij, Marzia Capelletti, Daisy Huynh, Karma
Salem, Yawara Kawano, Sioban Glavey , Jiantao Shi, Michele Moschetta, A driana Perilla-Glen, Patrick Henrick, Kim Noonan, K aitlen
Reyes,, Joe Cappuccio, Aaron Caola.
http://ghobriall ab.dana farberde v.org/