9ffd10fb 2767 4077 8da0 3d44a81102e9
2018-04-03
: Pdf 9Ffd10Fb-2767-4077-8Da0-3D44A81102E9 9ffd10fb-2767-4077-8da0-3d44a81102e9 4 2018 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 6
Cryopreserved Amniotic Membrane Improves Clinical
Outcomes Following Microdiscectomy
D. Greg Anderson, MD,*
w
Victor Popov, MD,
w
Andrew L. Raines, PhD,
z
and Julie O’Connell, PhD
z
Study Design: Prospective, randomized controlled trial.
Objective: To compare pain, physical/mental functional recov-
ery and recurrent herniation for patients following lumbar
microdiscectomy with and without the use of a cryopreserved
amniotic tissue graft.
Summary of Background Data: Although microdiscectomy
procedures are routinely successful for patients with lumbar
radiculopathy due to herniated disc disease, residual low back
pain, and recurrent herniation remain unsolved clinical prob-
lems.
Methods: Following Investigated Review Board approval, 80
subjects were randomized in a 1:1 ratio to either receive cry-
opreserved amniotic (cAM) tissue or no tissue following elective
lumbar microdiscectomy surgery. cAM grafts were applied to
the annular defect at the conclusion of the procedure. Patients
provided preoperative and postoperative clinical assessment
data out to 24 months using the Oswestry Disability Index
(ODI), Short Form-12 (SF-12) Health Survey, and Visual An-
alog Pain Scale for back and leg pain. Patients with symptom-
atic recurrent disc herniation were recorded.
Results: In total, 48 males and 32 females with an average age of
47.2 years were included. Mean ODI scores for subjects treated
with cAM graft demonstrated statistically greater improvement at
6 weeks (14.49 vs. 21.82; P= 0.05) and 24 months (6.62 vs. 14.40;
P= 0.02) compared with controls. Similarly, SF-12 Physical
Component Scores demonstrated statistically greater gains in the
cAM group at both the 6 weeks and 24 months. None of the
subjects in the cAM graft group sustained a recurrent herniation
at the same surgical level, whereas 3 patients in the control group
sustained a recurrent herniation at the same surgical level, with
2 requiring fusion to manage persistent pain.
Conclusions: The data demonstrate statistically superior clinical
outcomes following lumbar microdiscectomy as measured by
ODI and SF-12 (physical composite scale) and a lower rate of
recurrent herniation with the use of a cAM tissue graft
compared with traditional microdiscectomy.
Key Words: amniotic membrane, microdiscectomy, outcome
(Clin Spine Surg 2017;00:000–000)
Lumbar radiculopathy secondary to lumbar disc herniation
(LDH) is a common health problem that presents a large
economic burden to the medical system.1,2 Nonsurgical treat-
ment options for LDH include activity limitations, pharma-
cologic therapy, manipulation, physical therapy; and epidural
steroid injections.3Although nonsurgical treatments are often
successful, patients who are nonresponsive to conservative
therapies or those with progressive neurological symptoms
require surgical intervention.
Surgical treatment is generally successful in reliev-
ing or reducing radicular symptoms due to LDH.4,5
Unfortunately, with longer-term follow-up, residual/
recurrent axial back pain and/or recurrent disc herniation
with radiculopathy are significant unsolved problems,
with studies reporting reoperation rates following surgery
for LDH from 18.5%–25%.4,6 At present, there are
no proven treatments available to reduce the incidence
of postoperative axial back pain and recurrent disc
herniation.
The amniotic membrane (AM) is a placental-derived
tissue, sharing the same cellular origin as the developing fetus.
A primary function of the AM is to protect the fetus from the
maternal immune system and not surprisingly, the AM has
been demonstrated to possess potent anti-inflammatory
properties,7including the ability to reduce proinflammatory
and increase anti-inflammatory cytokine levels8and induce
apoptosis of proinflammatory cells.8,9 AM tissues have been
used clinically in a number of applications in ophthalmology,10
as well as a dressing for burns, nonhealing skin ulcers, and as
anaidtopromotewoundhealing.
11–13 In addition to its anti-
inflammatory properties, AM tissues have also been shown
to possess antiscarring properties.14,15 The anti-inflammatory,
regenerative and antiscarring activities of AM tissues have
recently been shown to be attributable to a unique glycoprotein
complex within the extracellular matrix called the HC-HA/
PTX3 complex.7
Received for publication April 27, 2016; accepted April 17, 2017.
From the *Department of Orthopaedic Surgery and Neurological Surgery,
Thomas Jefferson University; wRothman Institute, Philadelphia, PA; and
zAmniox Medical Inc., Atlanta, GA.
The study was partially funded by a grant for clinical research from
Amniox Medical Inc.
The authors declare no conflict of interest.
Reprints: D. Greg Anderson, MD, Departments of Orthopaedic Surgery and
Neurological Surgery Thomas Jefferson University and Rothman
Institute, 925 Chestnut St., 5th Floor, Philadelphia, PA 19107
(e-mail: davidgreganderson@comcast.net).
Copyright r2017 Wolters Kluwer Health, Inc. All rights reserved.
PRIMARY RESEARCH
Clin Spine Surg Volume 00, Number 00, ’’ 2017 www.clinicalspinesurgery.com |1
Copyright r2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.

One of the hallmarks of disc degeneration is an
increase in the expression and levels of various proin-
flammatory cytokines.16,17 The anti-inflammatory and
antiscarring actions of AM tissues make this tissue a
potentially attractive option to reduce postoperative
inflammation and promote healing of the annular defect
following microdiscectomy.
In the present study, we sought to determine the
safety and clinical efficacy of a cryopreserved amniotic
(cAM) tissue product as an adjunctive treatment applied
to the annular defect following lumbar microdiscectomy
surgery. Specifically, we set out to compare in a pro-
spective, randomized manner, the clinical outcomes and
symptomatic recurrence rates for patients treated with
and without cAM applied to the annular defect following
lumbar microdiscectomy surgery.
METHODS
Study Design
A single-center, single-blind, prospective, random-
ized controlled trial was conducted to determine the
safety and effectiveness of cryopreserved AM (cAM;
Amniox Medical Inc., Atlanta, GA) after lumbar micro-
discectomy. Because of the placement of cAM after mi-
crodiscectomy, only the patient could be blinded to
treatment assignment. The cAM tissue used in the study is
classified by the Food & Drug Administration as a human
cell, tissue, and human cellular and tissue product. Tissue
collection, processing, and use were followed according to
all applicable Food & Drug Administration regulations
and guidelines. Following Investigated Review Board
approval (Western Investigated Review Board Protocol
#20110656), enough patients were screened to be able to
enroll 80 patients randomized in a 1:1 ratio (treatment:-
control) to either receive cAM tissue (treatment) or no
tissue (control) following elective lumbar micro-
discectomy surgery. The primary exclusion criteria for the
study were a history of prior back surgery at the same
level as the herniation; inability to walk independently;
receipt of corticosteroids, radiation therapy, chemo-
therapy, or immunosuppressive agents within 1 month of
surgery; pregnancy, body mass index >50, severe renal
failure, hepatic insufficiency, cirrhosis; anemia, rheuma-
toid arthritis; or active local or systemic malignancy. Disc
herniations were diagnosed by combining clinical evalu-
ation and magnetic resonance imaging scanning of the
lumbar spine. All patients were treated by the same sur-
geon (D.G.A.). Patients randomized to the treatment arm
of the study received placement of cAM in the annular
defect after removal of the herniated disc fragments.
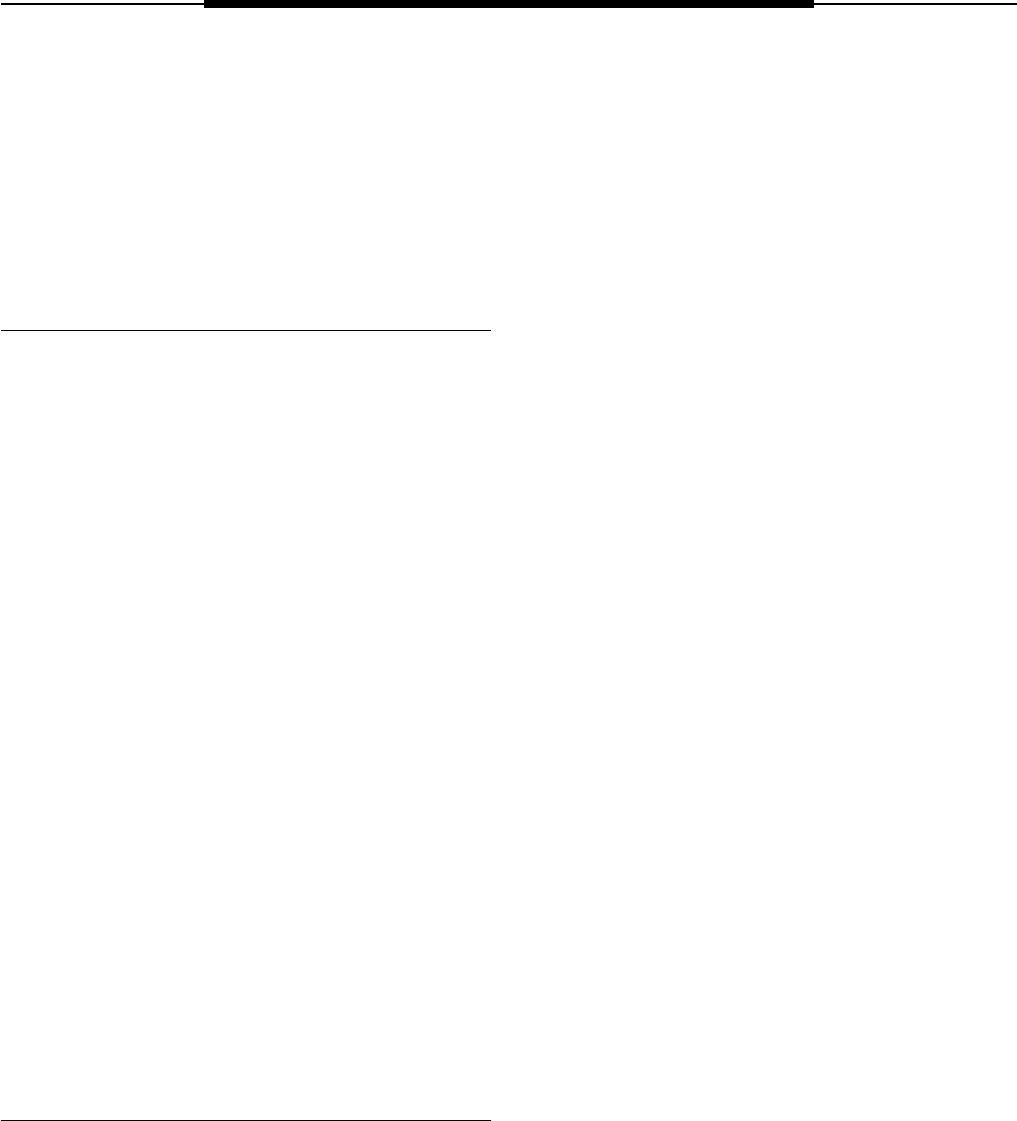
Operative Technique
All patients enrolled in the study underwent elective
lumbar microdiscectomy for symptoms of severe radicul-
opathy, unresponsive to nonoperative treatment. Briefly,
after the induction of anesthesia, patients were placed
prone on a radiolucent spine frame. The incision site was
localized fluoroscopically using an 18-G spinal needle. An
B20-mm incision was made on the symptomatic side and
then serial dilation was used to place a tubular retractor
(METRx, Medtronic Spine, Memphis, TN) at the affected
level. A laminotomy was performed by removing the
caudal edge of the proximal lamina and the cranial edge of
the distal lamina and intervening ligamentum flavum as
required to gain access the disc fragment. The traversing
nerve root was protected and retracted as necessary to
reach the herniated disc fragment. The membrane over the
extruded disc fragment was opened using a Penfield #4
dissector and the herniated disc material was removed using
a pituitary rongeur. The annular defect was identified and
explored to exclude or remove additional loose disc frag-
ments. After all loose disc fragments had been removed and
the nerve root adequately decompressed, cAM was placed
into the annular defect in the cohort of patients random-
izing to cAM treatment. In the cAM cohort, a 22cm
rectangular piece of cAM was placed into the annular de-
fect. Delivery of the cAM to the annular defect was
accomplished by placing the tissue on the back side of the
nerve root retractor and the pushing the tissue into the
annular defect with a nerve hook (Fig. 1). The cAM tissue
is a thin membrane that is inserted into the void after
removal of the herniated disc material without any physical
attachment to retain the graft in position. An important
technical pearl is to reduce the intensity of suction during
delivery of the cAM tissue to prevent suctioning the tissue
up into the suction catheter. After placement of the cAM,
the nerve root retractor was removed and the tubular
retractor was withdrawn. In all patients, the fascia and skin
were closed using 2-0 absorbable suture followed by a
subcutaneous injection of 10 mL of 0.25% marcaine
(Baxter, Atlanta, GA). Patients randomized to the control
arm of the study underwent the same procedure without the
placementofcAM.
Postoperatively, patients were encouraged to begin
a walking program of at least 30 minutes per day and
all patients were referred for postoperative rehabilitation
by a physical therapist to improve core muscle strength-
ening and aerobic conditioning at 2-week postoperative
timepoint.
Outcomes Measures
Outcome instruments utilized in this study included
the Oswestry Disability Index (ODI), 10 cm Visual Ana-
log Pain Scale (VAS) (separately, for low back and leg
pain), and the Short Form-12 (SF-12) Health Survey
questionnaire. The data collection timepoints included
before surgery (baseline) and at the 2-week, 6-week,
6-month, 12-month, and 24-month postoperative timepoints.
At each in-office follow-up visit, outcome questionaires and
VAS were filled out by subjects and collected by a research
coordinator. At each out-of-office follow-up visit, subjects
were contacted by a research coordinator and provided
answers to questionaires over the phone.
Over the 24-month follow-up period, patients
were encouraged to report any symptoms of new, se-
vere back or leg pain. For patients with recurrent
Anderson et al Clin Spine Surg Volume 00, Number 00, ’’ 2017
2|www.clinicalspinesurgery.com Copyright r2017 Wolters Kluwer Health, Inc. All rights reserved.
Copyright r2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
symptoms following microdiscectomy surgery, gadoli-
dium enhance magnetic resonance imaging scanning
was utilized to diagnose recurrent LDH. Patients with
imaging evidence of disc herniation that correlated
clinically to the patient’s symptoms were identified.
Those with symptomatic disc herniation were divided
into disc herniation at the same level (characterized as
recurrent herniation) and herniation at another level
(new herniation).
Statistical Analysis
The mean ± SE for the ODI, VAS, and SF-12
scores were calculated and plotted for both the cAM and
control group at all timepoints (Microsoft Excel 2011).
Differences between groups were determined using an
unpaired ttest (SPSS Statistics, IBM, New York) with
Pr0.05 considered to be statistically significant.
RESULTS
A total of 80 patients were enrolled in the study and
randomized in a 1:1 ratio to either the cAM cohort or the
control cohort. A summary of the patient demographics
is presented in Table 1. Briefly, there were 48 males and 32
females included in the study population. The average age
was 47.2 years (range, 20–73 y). A breakdown of the
affected disc level for the entire study population is as
follows: 2 L1–L2; 4 L2–L3; 7 L3–L4; 26 L4–L5, 32 L5–
S1; 9 L4–L5, L5–S1. Overall, there were no statistically
FIGURE 1. AM tissue placement. A 22 cm piece of cryopreserved AM tissue (A). Following removal of the herniated disc,
cryopreserved AM tissue was inserted through the cannula (B) into the nucleus pulposus of the affected disc (C). AM indicates
amniotic membrane.
TABLE 1. Patient Demographics
Overall Control Amniotic Membrane
#Patients (N) 80 40 40
Age (mean) (y) 45.8 ± 11.3 47.2 ± 9.1 44.3 ± 13.1
Range 20–73 30–66 20–73
#Male 48 20 28
#Female 32 20 12
BMI 29.9 ± 6.1 28.2 ± 5.5 31.7 ± 6.3
Tobacco use 21/80 10/40 11/40
Affected level
L1–L2 2 2 0
L2–L3 4 3 1
L3–L4 7 4 3
L4–L5 26 15 11
L5–S1 32 13 19
L4–L5; L5–S1 9 3 6
BMI indicates body mass index.
Clin Spine Surg Volume 00, Number 00, ’’ 2017 Cryopreserved AM Improves Clinical Outcomes
Copyright r2017 Wolters Kluwer Health, Inc. All rights reserved. www.clinicalspinesurgery.com |3
Copyright r2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
significant differences between groups in terms of sex,
age, or affected level. Postoperatively, there were no
surgical complications encountered including surgical-site
infections, nerve root injuries, or dural laceration in either
study cohort.
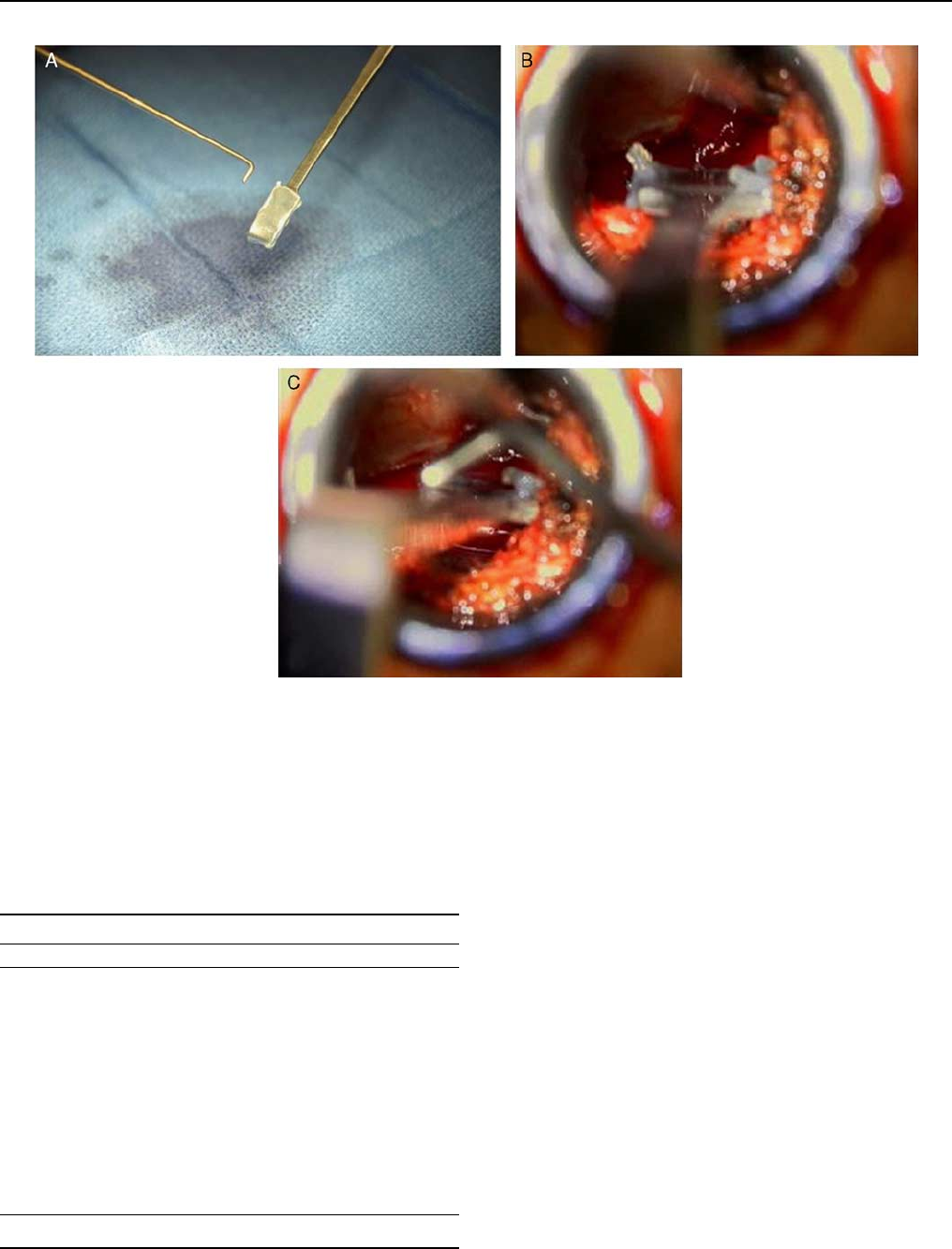
Scores for ODI were collected before surgery
(baseline) and at predetermined timepoints out to the
24-month postoperative timepoint. Before surgery, there
was no significant difference in ODI scores between the
cohorts (cAM: 48.63 ± 2.69; control: 51.95 ± 2.23). At
the 2-week postoperative timepoint, nonsignificant dif-
ferences between the cAM and control group were ob-
served (cAM: 25.44 ± 3.09; control: 31.64 ± 2.80). At the
6-week postoperative timepoint, the mean ODI score for
the cAM group was significantly lower than that of the
control group (cAM: 14.49 ± 2.63; control: 21.82 ± 2.75;
P= 0.05). Nonsignificant differences in ODI scores were
again observed between the cohorts at the 6-month
(cAM: 11.98 ± 2.50; control: 12.08 ± 2.31) and 12-month
(cAM: 9.29 ± 1.96; control: 12.83 ± 2.55) timepoints. At
the 24-month timepoint, the mean ODI scores were
significantly lower for cAM-treated patients compared
with control patients (cAM: 6.62 ± 1.30; control:
14.40 ± 3.29; P= 0.02). Reviewing the data trends, it can
be observed that the mean ODI score for cAM cohort
continued to decrease throughout the 24-month follow-
up period, whereas the control cohort experienced its
lowest mean ODI scores at the 6-month follow-up time-
point and subsequently experienced a trend of worsening
ODI scores at the 12- and 24-month timepoints. A plot of
the ODI scores versus time is shown in Figure 2.
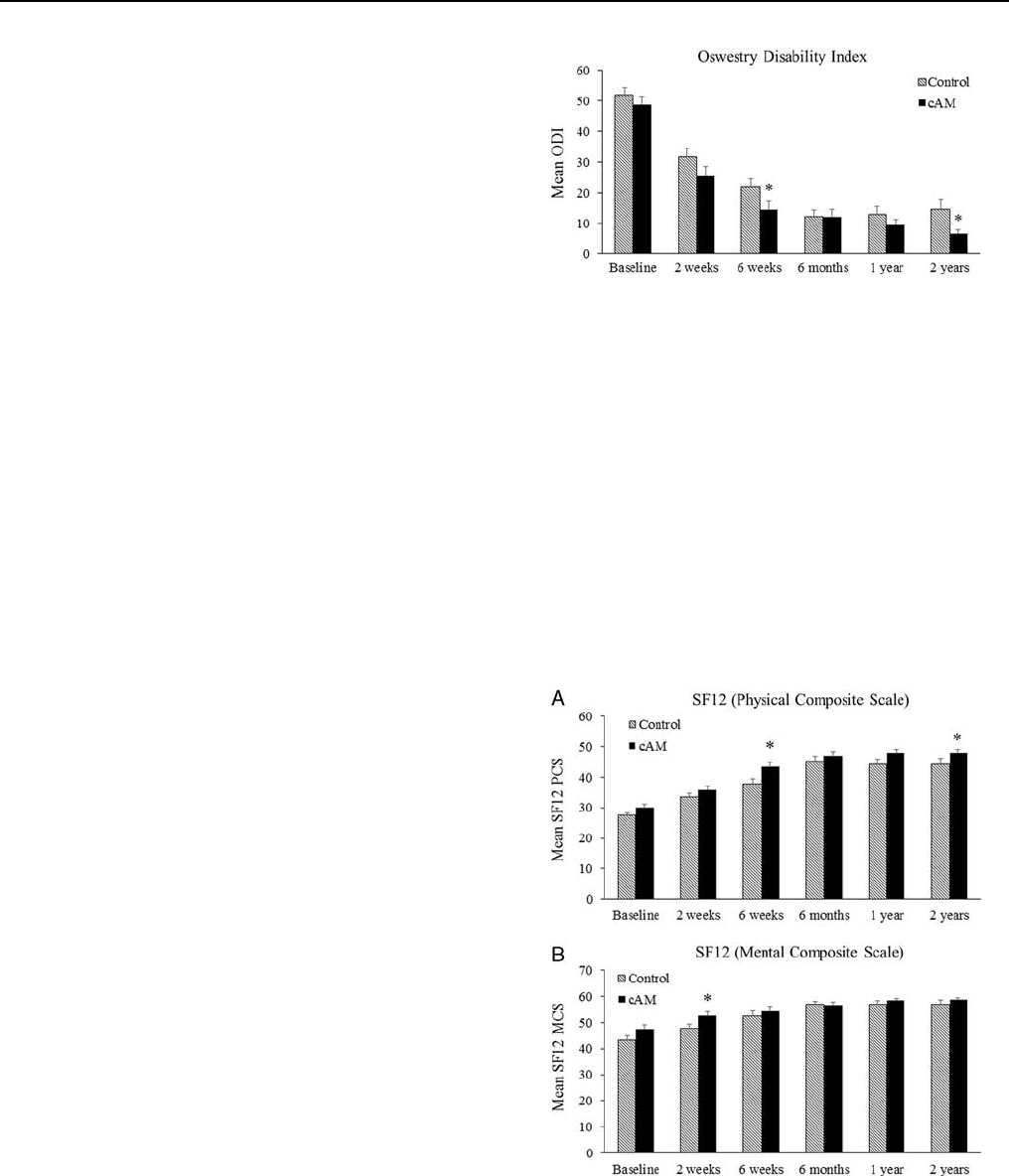
Mental and physical health was assessed using the
SF-12 Health Survey questionnaire. A plot of the physical
composite scores and mental composite scores is shown
in Figures 3A, B. Similar to the ODI scores, patients
receiving cAM tissue demonstrated a significantly im-
proved mean SF-12 physical composite score at the
6 weeks (P= 0.018) and 24 months (P= 0.05) post-
operative timepoints in comparison with the control
cohort. Nonsignificant differences were observed at the
other timepoints. No significant differences were observed
in the SF-12 mental composite scores between the
2 groups except for the 2-week timepoint where the cAM-
treated cohort demonstrated a significant improvement
compared with the control group (P= 0.04) (Fig. 3B).
Pain was accessed using the 10 cm VAS. Significant
improvements in both back and leg pain were observed in
both the cAM-treated and control cohorts compared with
baseline at all timepoints postoperatively. No significant
differences in VAS scores were found between the treat-
ment cohorts (Tables 2, 3).
In the cAM cohort, there were no instances of
recurrent herniation at the same level during the
24-month follow-up period. However, in the control
cohort, 3 patients presented with a recurrent herniated
disc at the same level. All 3 patients failed to respond to a
minimum 6-week course of nonsurgical care consisting of
activity limitations, analgesic medications, nonsteroidal
anti-inflammatory drugs, and epidural steroid injections.
These 3 patients were ultimately treated with additional
surgery. One of the 3 (2.5% of the control cohort) had
predominantly radicular pain and was treated with
revision microdiscectomy. The other 2 patients (5% or
the control cohort) had a substantial component (> 50%
of the overall pain complex) of mechanical low back pain
and were treated with lumbar fusion.
No adverse events attributable to the cAM were
reported during the study period.
FIGURE 2. ODI. Before surgery and at specified timepoints
postoperatively, ODI scores were collected for all patients.
Values presented are mean ± SEM. cAM indicates
cryopreserved amniotic; ODI, Oswestry Disability Index.
*P< 0.05 versus control.
FIGURE 3. SF-12 Health Survey Scores. Before surgery and at
specified timepoints postoperatively, patients filled out the
SF-12 health survey. Scores for the PCS (A) and MCS (B) were
collected for all patients. Values presented are mean ± SEM.
cAM indicates cryopreserved amniotic; MCS, mental
composite scale; PCS, physical composite scale; SF-12, Short
Form-12. *P< 0.05 versus control.
Anderson et al Clin Spine Surg Volume 00, Number 00, ’’ 2017
4|www.clinicalspinesurgery.com Copyright r2017 Wolters Kluwer Health, Inc. All rights reserved.
Copyright r2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.
DISCUSSION
The present investigation was performed to study the
clinical efficacy and safety of a cAM tissue product placed in
the annular defect for patients undergoing routine lumbar
microdiscectomy. This prospective, randomized controlled
trial, demonstrated that cAM was able to produce better
clinical outcomes at the 6-week and 24-month timepoints as
measured by the ODI and SF-12 physical composite scores
compared with the current standard of care. In addition, in
patients treated with cAM, there were no recurrent hernia-
tions at the same level.
Recurrent disc herniation following micro-
discectomy remains an unsolved problem. In a systematic
review of the microdiscectomy literature between 2009
and 2015, the rate of recurrent herniation varied from as
little as 0.2% to 20%,18 although most of the 57 articles
reviewed reported recurrence rates between 2%–10%. In
the present study, the rate of recurrent disc herniation in
the control group (7.5%) was consistent with prior
studies, whereas patients receiving cAM did not experi-
ence any recurrent herniation at the same level (0%). This
finding is potentially quite significant and deserves more
investigation using larger patient cohorts to confirm these
early observations.
The AM has been used clinically for over a cen-
tury19 in a number of applications in ophthalmology8and
wound healing.20–22 The clinical success of cAM as a
potent anti-inflammatory and antiscarring agent has
recently expanded interest into the potential applications
of this unique tissue form in reconstructive procedures
where inflammation and adhesion formation might be
harmful. Clinical protocols have been studied for
tendon23 and nerve repair24–26 and investigations are
ongoing for various spinal applications.27
A well-characterized hallmark of disc degeneration
is the increased expression of proinflammatory cytokines,
including Interleukin-1b, resulted on activation normal
T-cell expressed, tumor necrosis factor-a, and substance
P.24,25 These proinflammatory cytokines likely play a role
in the clinical pain syndromes that require medical inter-
vention. cAM has been shown to downregulate proin-
flammatory and upregulate anti-inflammatory cytokine
signaling.26 In addition, cAM has been shown to decrease
adhesion and proliferation of proinflammatory cells and
induce selective apoptosis of proinflammatory cells.26,27
cAM also downregulates TGF-b1 signaling, an important
component in the pathway of scar formation following
injury.13,28 This tissue acts to limit the differentiation of
fibroblasts into myofibroblasts to prevent collagen con-
traction, the mechanism responsible for inducing scar and
adhesion formation.29,30 AM has been investigated as a
material to reduce epidural adhesions after laminectomy
in both rat31 and canine32 models. These studies docu-
mented a reduced volume and density of scar tissue, less
inflammatory cell infiltration, and reduced fibroblast
proliferation in animals treated with AM.
The immunomodulatory and antiscarring actions of
cAM tissue are modulated by a unique component of the
extracellular matrix called the HC-HA/PTX3 complex.
This complex is formed by tight association between
pentraxin 3 (PTX3) and HC-HA, which consists of high
molecular weight hyaluronic acid (HA) covalently linked
to heavy chain 1 of inter-a-trypsin inhibitor (IaI) through
the catalytic action of tumor necrosis factor-stimulated
gene-6 (TSG-6).33,34
The potential mechanisms of the benefits seen in the
current study for patients treated with cAM could theo-
retically be due to the down-regulation of proin-
flammatory cytokines, proinflammatory cells, and/or
inhibition of the scar formation pathway resulting in an
enviroment more conducive to healing of the interverte-
bral tissue.26–28 It is compelling to note the ongoing
clinical improvement was seen at each timepoint in the
mean ODI scores of the cAM treatment cohort compared
with the control group. Additional research to better
characterize the mechanism of action of cAM within the
annulus fibrosus is certainly warranted.
As with any new therapy, the cost of the proposed
new treatment versus its benefits should be evaluated.
This study was a single-center, early evauation of cAM as
an adjunct in lumbar microdiscectomy, and was not de-
signed to have an economic endpoint. However, the lack
of recurrent herniation in the cAM group compared with
the control group may lead to a cost-savings by reducing
office visits, medications, and repeat or additional surgical
procedures. The potential ability of cAM to reduce
TABLE 2. VAS Back Pain Data Summary
Amniotic Membrane
Mean ODI ± SE
% Decrease
From Baseline P
Baseline 5.72 ± 0.33 — —
2 wk 3.31 ± 0.48 42.1 < 0.001
6 wk 2.17 ± 0.41 62.1 < 0.001
6 mo 1.56 ± 0.37 72.7 < 0.001
Control
Baseline 5.77 ± 0.33 — < 0.001
2 wk 3.71 ± 0.46 35.7 < 0.001
6 wk 2.97 ± 0.45 48.5 < 0.001
6 mo 1.73 ± 0.47 70.0 < 0.001
ODI indicates Oswestry Disability Index; VAS, Visual Analog Pain Scale.
TABLE 3. VAS Leg Pain Data Summary
Amniotic Membrane
Mean ODI ± SE
% Decrease
From Baseline P
Baseline 8.19 ± 0.24 — —
2 wk 3.54 ± 0.46 56.8 < 0.001
6 wk 2.68 ± 0.47 67.3 < 0.001
6 mo 1.66 ± 0.40 79.7 < 0.001
Control
Baseline 8.14 ± 0.18 < 0.001
2 wk 3.82 ± 0.50 53.1 < 0.001
6 wk 3.09 ± 0.56 62.0 < 0.001
6 mo 1.81 ± 0.54 77.8 < 0.001
ODI indicates Oswestry Disability Index; VAS, Visual Analog Pain Scale.
Clin Spine Surg Volume 00, Number 00, ’’ 2017 Cryopreserved AM Improves Clinical Outcomes
Copyright r2017 Wolters Kluwer Health, Inc. All rights reserved. www.clinicalspinesurgery.com |5
Copyright r2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.

overall costs associated with lumbar microdiscectomy and
recurrent low back pain in particular, should be evaluated
in a larger, multicenter clinical study.
Certain limitations of the current study should be
acknowledged. First, a relatively small number of patients
were enrolled although this deficiency is partially offset by
the prospective randomization strategy of the current
study design. Second, all operations were performed by a
single investigator although the surgical technique was
standardized and commonplace for this type of pathol-
ogy. Third, the 2-year follow-up period represents a
medium-term outcome report. For this reason, we have
submitted an amended protocol to continue the current
research follow-up out to the 5 year timepoint to assess
longer-term differences between the cohorts.
CONCLUSIONS
Cryopreserved AM placed in the annular defect
following microdiscectomy led to improved clinical
outcome as measured by the ODI and SF-12 Physical
Component Scale at the 6-week and 24-month timepoints
compared with standard microdiscectomy. In this study,
there were no reported recurrent disc herniations at the
same level in the cohort treated with cAM compared with
standard microdiscectomy (control) which saw a 7.5%
rate of recurrent disc herniation. Overall, these results are
intriguing and further, larger studies are warranted.
REFERENCES
1. Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin.
2007;25:387–405.
2. Dagenais S, Caro J, Haldeman S. A systematic review of low back
pain cost of illness studies in the United States and internationally.
Spine J. 2008;8:8–20.
3. Sonntag VKH. Treatment of the herniated lumbar disc: persistent
problem. World Neurosurg. 2010;74:574–575.
4. Aichmair A, Du JY, Shue J, et al. Microdiscectomy for the
treatment of lumbar disc herniation: an evaluation of reoperations
and long-term outcomes. Evid Based Spine Care J. 2014;5:77–86.
5. Shriver MF, Xie JJ, Tye EY, et al. Lumbar microdiscectomy
complication rates: a systematic review and meta-analysis. Neuro-
surg Focus. 2015;39:E6.
6. Soliman J, Harvey A, Howes G, et al. Limited microdiscectomy for
lumbar disk herniation: a retrospective long-term outcome analysis.
J Spinal Disord Tech. 2014;27:E8–E13.
7. Tseng SCG. HC-HA/PTX3 purified from amniotic membrane as
novel regenerative matrix: insight into relationship between inflam-
mation and regeneration. Invest Ophthalmol Vis Sci. 2015;56:1–8.
8. He H, Zhang S, Tighe S, et al. Immobilized heavy chain-hyaluronic
acid polarizes lipopolysaccharide-activated macrophages toward M2
phenotype. J Biol Chem. 2013;288:25792–25803.
9. He H, Li W, Tseng DY, et al. Biochemical characterization and
function of complexes formed by hyaluronan and the heavy chains
of inter-alpha-inhibitor (HC-HA) purified from extracts of human
amniotic membrane. J Biol Chem. 2009;284:20136–20146.
10. Liu J, Sheha H, Fu Y, et al. Update on amniotic membrane
transplantation. Expert Rev Ophthalmol. 2010;5:645–661.
11. Bose B. Burn wound dressing with human amniotic membrane. Ann
R Coll Surg Engl. 1979;61:444–447.
12. Gruss JS, Jirsch DW. Human amniotic membrane: a versatile
wound dressing. Can Med Assoc J. 1978;118:1237–1246.
13. Stern W. The grafting of preserved amniotic membranes to burned
and ulcerated surfaces, substituting skin grafts. JAMA. 1913;60:973.
14. Li W, He H, Chen Y-T, et al. Reversal of myofibroblasts by amniotic
membrane stromal extract. JCellPhysiol. 2008;215:657–664.
15. Tseng SC, Li DQ, Ma X. Suppression of transforming growth
factor-beta isoforms, TGF-beta receptor type II, and myofibroblast
differentiation in cultured human corneal and limbal fibroblasts by
amniotic membrane matrix. J Cell Physiol. 1999;179:325–335.
16. Kepler CK, Markova DZ, Koerner JD, et al. Substance P receptor
antagonist suppresses inflammatory cytokine expression in human
disc cells. Spine (Phila Pa 1976). 2015;40:1261–1269.
17. Kepler CK, Markova DZ, Hilibrand AS, et al. Substance P
stimulates production of inflammatory cytokines in human disc
cells. Spine (Phila Pa 1976). 2013;38:E1291–E1299.
18. Anichini G, Landi A, Caporlingua F, et al. Lumbar endoscopic
microdiscectomy: where are we now? an updated literature review
focused on clinical outcome, complications, and rate of recurrence.
Biomed Res Int. 2015;2015:417801.
19. Davis JS. Skin grafting at the Johns Hopkins Hospital. Johns
Hopkins Hosp Rep. 1910;15:542–549.
20. Ellington JK, Ferguson CM. The use of amniotic membrane/
umbilical cord in first metatarsophalangeal joint cheilectomy: a
comparative bilateral case study. Surg Technol Int. 2014;25:63–67.
21. DeMill SL, Granata JD, McAlister JE, et al. Safety analysis of
cryopreserved amniotic membrane/umbilical cord tissue in foot and
ankle surgery: a consecutive case series of 124 patients. Surg Technol
Int. 2014;25:257–261.
22. Warner M, Lasyone L. An open-label, single-center, retrospective
study of cryopreserved amniotic membrane and umbilical cord
tissue as an adjunct for foot and ankle surgery. Surg Technol Int.
2014;25:251–255.
23. Demirkan F, Colakoglu N, Herek O, et al. The use of amniotic
membrane in flexor tendon repair: an experimental model. Arch
Orthop Trauma Surg. 2002;122:396–399.
24. Mohammad J, Shenaq J, Rabinovsky E, et al. Modulation of
peripheral nerve regeneration: a tissue-engineering approach. The
role of amnion tube nerve conduit across a 1-centimeter nerve gap.
Plast Reconstr Surg. 2000;105:660–666.
25. Kim SS, Sohn SK, Lee KY, et al. Use of human amniotic membrane
wrap in reducing perineural adhesions in a rabbit model of ulnar
nerve neurorrhaphy. J Hand Surg Eur Vol. 2010;35:214–219.
26. Meng H, Li M, You F, et al. Assessment of processed human
amniotic membrane as a protective barrier in rat model of sciatic
nerve injury. Neurosci Lett. 2011;496:48–53.
27. Subach BR, Copay AG. The use of a dehydrated amnion/chorion
membrane allograft in patients who subsequently undergo reexplo-
ration after posterior lumbar instrumentation. Adv Orthop.
2015;2015:501202.
28. Lee SB, Li DQ, Tan DT, et al. Suppression of TGF-beta signaling in
both normal conjunctival fibroblasts and pterygial body fibroblasts
by amniotic membrane. Curr Eye Res. 2000;20:325–334.
29. Abdel MP, Morrey ME, Barlow JD, et al. Myofibroblast cells are
preferentially expressed early in a rabbit model of joint contracture.
J Orthop Res. 2012;30:713–719.
30. Powell DW, Mifflin RC, Valentich JD, et al. Myofibroblasts. I.
Paracrine cells important in health and disease. Am J Physiol. 1999;
277(pt 1):C1–C9.
31. Choi HJ, Kim KB, Kwon Y-M. Effect of amniotic membrane to
reduce postlaminectomy epidural adhesion on a rat model. J Korean
Neurosurg Soc. 2011;49:323–328.
32. Tao H, Fan H. Implantation of amniotic membrane to reduce
postlaminectomy epidural adhesions. Eur Spine J. 2009;18:
1202–1212.
33. Zhang S, He H, Day AJ, et al. Constitutive expression of inter-a-
inhibitor (IaI) family proteins and tumor necrosis factor-stimulated
gene-6 (TSG-6) by human amniotic membrane epithelial and
stromal cells supporting formation of the heavy chain-hyaluronan
(HC-HA) complex. J Biol Chem. 2012;287:12433–12444.
34. Zhang S, Zhu Y-T, Chen S-Y, et al. Constitutive expression of
pentraxin 3 (PTX3) protein by human amniotic membrane cells
leads to formation of the heavy chain (HC)-hyaluronan (HA)-PTX3
complex. J Biol Chem. 2014;289:13531–13542.
Anderson et al Clin Spine Surg Volume 00, Number 00, ’’ 2017
6|www.clinicalspinesurgery.com Copyright r2017 Wolters Kluwer Health, Inc. All rights reserved.
Copyright r2017 Wolters Kluwer Health, Inc. Unauthorized reproduction of this article is prohibited.