A7b4dc18 1b23 41cf 9cde E5e992403cf5
2017-05-03
: Pdf A7B4Dc18-1B23-41Cf-9Cde-E5E992403Cf5 a7b4dc18-1b23-41cf-9cde-e5e992403cf5 5 2017 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 60
SIGMA® Primary
Knee System
Balanced Surgical Technique
INSTRUMENTS
INSTRUMENTS
RPF
DUOFIX

Introduction
Contemporary total knee arthoplasty demands high performance
instrumentation that provides enhanced efficiency, precision and
flexibility. Through a program of continuous development, DePuy Synthes
Joint Reconstruction now offers a single system of High Performance
instruments that supports your approach to knee replacement surgery.
This surgical technique provides instruction on the implantation of
the SIGMA® Knee System Family of Fixed Bearing and Rotating Platform
Knees utilizing the balanced resection instrumentation.
There are several approach options available to the surgeon, the most
common are: medial parapatellar, mini-midvastus and mini-subvastus.
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 1
Content
Surgical Summary 2
Incision and Exposure 4
Pattela Resection 7
Tibial Jig Assembly 9
Lower Leg Alignment 10
Tibial Resection 12
Femoral Alignment 13
Distal Femoral Resection 16
Extension Gap Assessment and Balancing 17
Femoral Sizing (Optional) 18
Femoral Rotation 19
Femoral Preparation - A/P and Chamfer Cuts 22
Femoral Resection Notch Cuts 24
Measuring the Flexion Gap 25
Trial Components (For Fixed Bearing, see Appendix A) 26
Tibial Preparation - MBT 29
Final Patella Preparation 31
Cementing Technique 32
Final Component Implantation 33
Closure 34
Appendix A: Fixed Bearing Modular Tibial Preparation 35
Appendix B: Tibial I.M. Jig Alignment 39
Appendix C: Spiked Uprod 42
Appendix D: Femoral Finishing 45
Appendix E: Femoral Finishing (Alternative) 46
Ordering Information 47
2 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
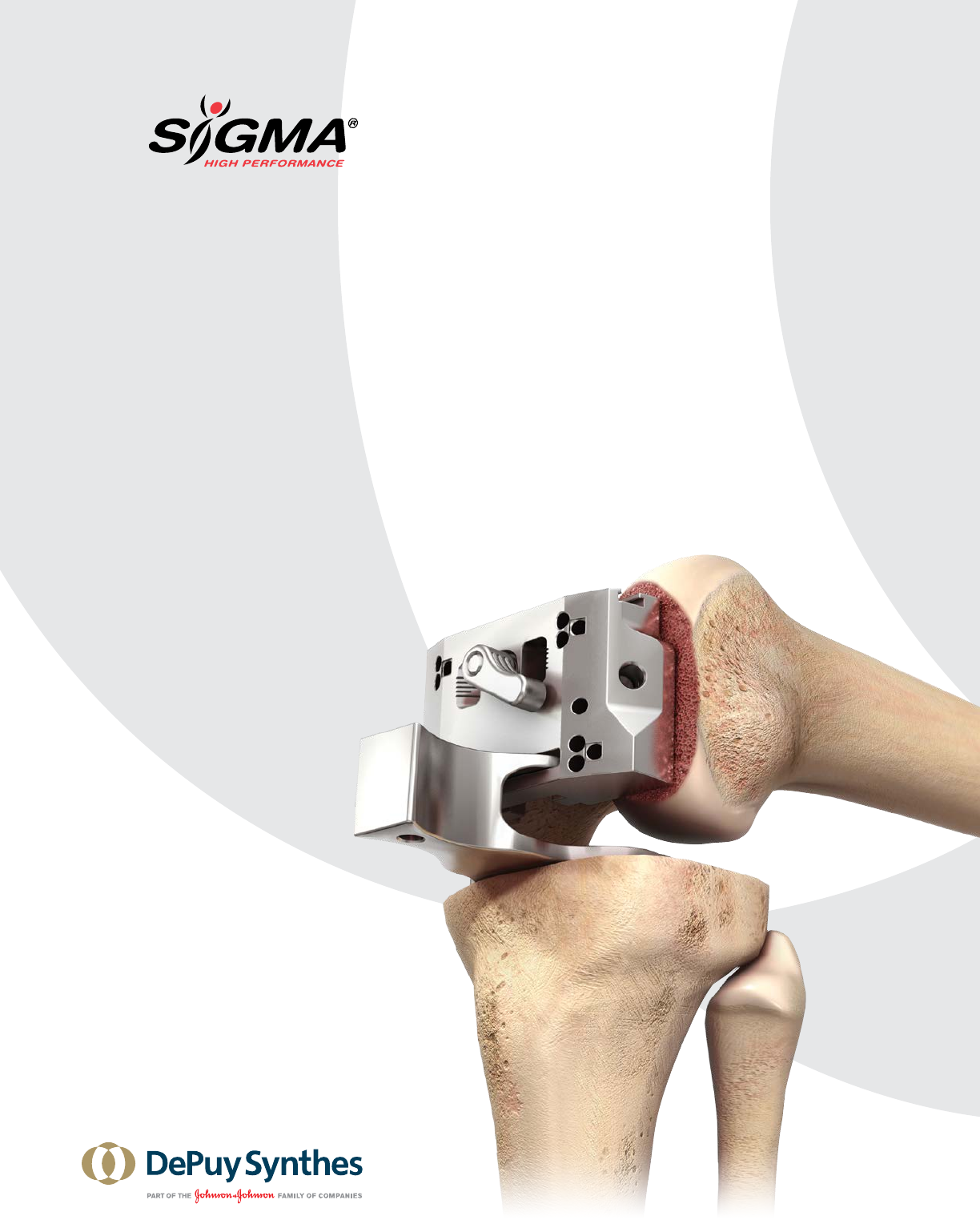
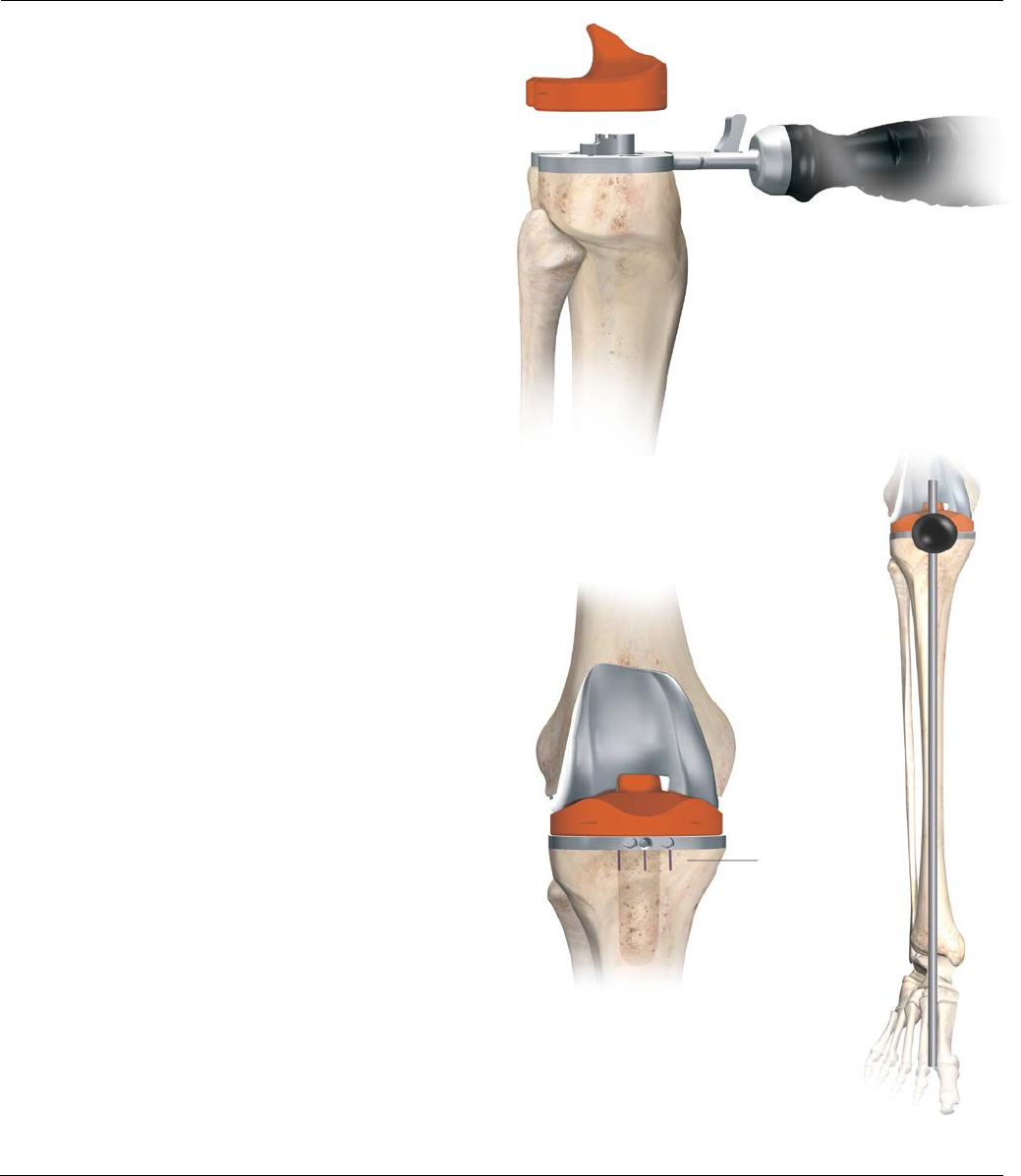
Surgical Summary
Step 1: Incision and
exposure
Step 7: Soft tissue
balancing
Step 8: Femoral rotation
Step 10: Determine
flexion gap
Step 11: Trial reduction
Step 2: Patellar resection Step 3: Lower leg
alignment
Step 4: Tibial resection
Step 5: Femoral alignment Step 6: Distal femoral
resection
Step 9: Femoral resection
notch cuts
(alternative)
Step 9: Femoral
preparation
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 3
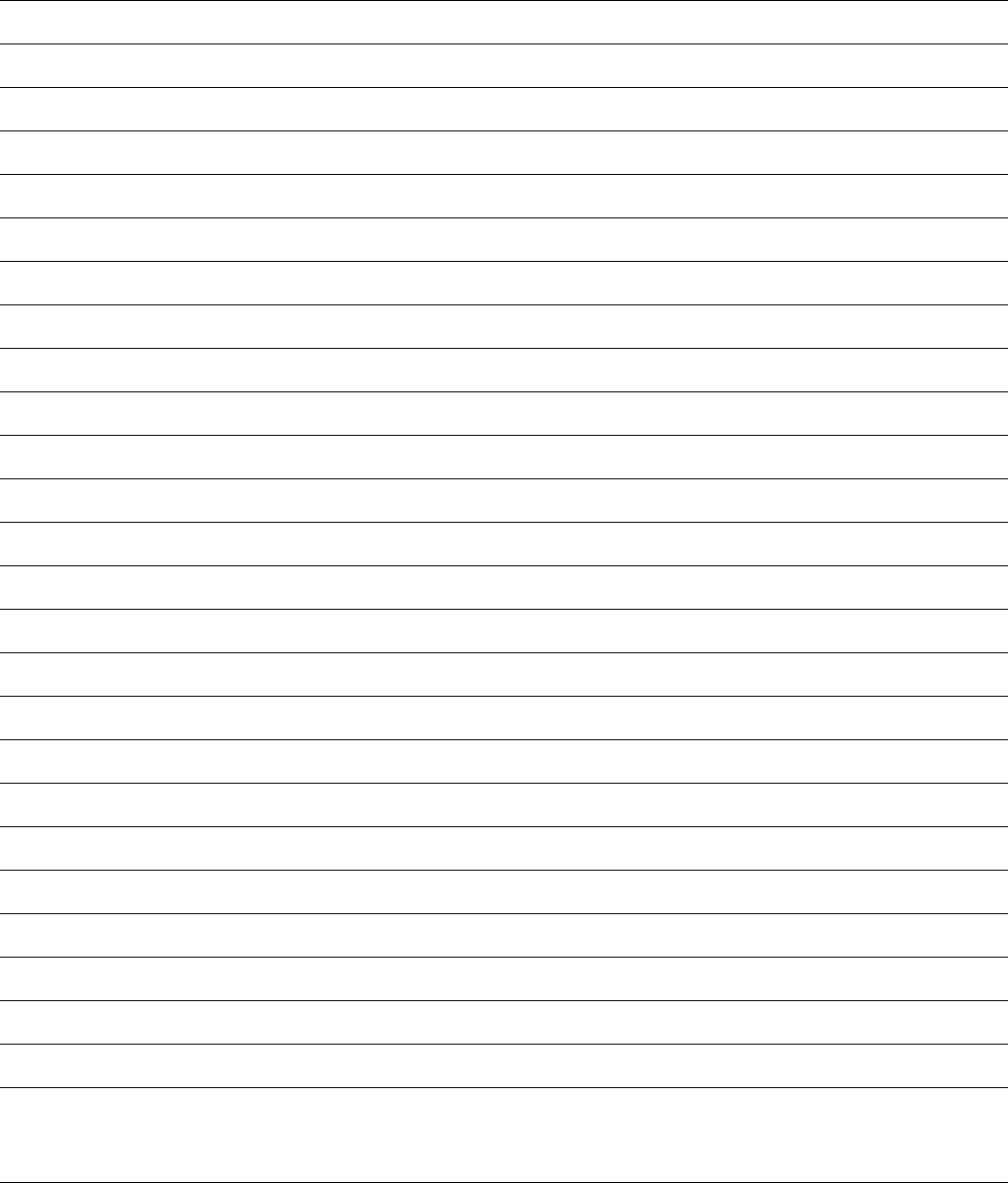
Surgical Summary
Step 12: Tibial preparation Step 13: Final patella
preparation
Step 14: Final component
implantation

4 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Incision and Exposure
The SIGMA High Performance Instrumentation is
designed for use with and without Ci Computer Assisted
Surgery, for both open and minimal invasive approaches
to the knee.
Make a straight midline skin incision starting from 2 to
4 cm above the patella, passing over the patella, and
ending at the tibial tubercle (Figure1).
There are three approach options available for the surgeon:
medial parapatellar, mini-midvastus and mini-subvastus.
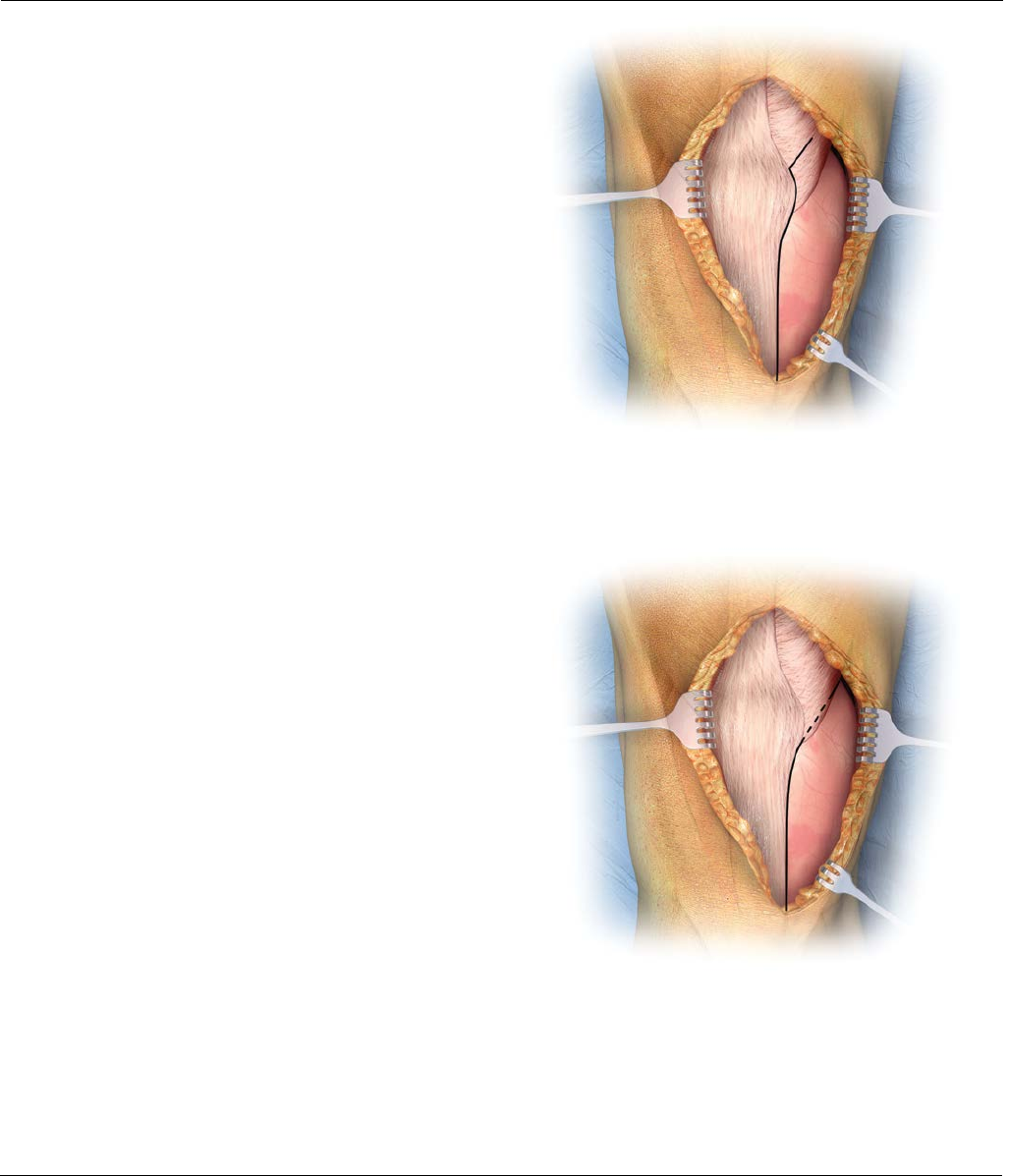
Figure2
Figure1
For surgeons choosing the medial parapatellar
approach (Figure 2):
Make a medial parapatellar incision through the
retinaculum, the capsule and the synovium, with neutral
alignment or with varus deformity. The medial
parapatellar incision starts proximal (4 cm) to the patella,
incising the rectus femoris tendon longitudinally, and
continues distally around the medial aspect of the patella
and ligamentum patella stopping just medial to the tibial
tubercle (Figure2). Following this incision, evert the
patella laterally to expose the entire tibio-femoral joint.
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 5
Incision and Exposure
For surgeons choosing the mini-midvastus
approach (Figure 3):
The midvastus approach starts 3-4 cm in the middle of
the Vastus Medialis Obliquus (VMO), running distal and
lateral to the muscle fibers towards the rectus femoris,
splitting the VMO.
Continue the incision distally around the medial aspect
of the patella and ligamentum patella stopping just
medial to the tibial tubercle (Figure3). Following this
incision, evert the patella laterally to expose the entire
tibio-femoral joint.
Figure4
Figure3
For surgeons choosing the subvastus approach:
The subvastus approach starts by lifting the VMO with a
90 degree stomp hook. A 3-4 cm incision is made in the
capsule underneath the VMO, running horizontal from
medial to lateral towards the mid portion of the patella.
The incision continues distally around the medial aspect
of the patella and ligamentum patella stopping just
medial to the tibial tubercle (Figure4). Following this
incision, evert the patella laterally to expose the entire
tibio-femoral joint.
Note: When having difficulties in correctly placing
the SIGMA High Performance Instruments in any of
these approaches, the incision should be further
extended to avoid over-retraction of the soft tissues.
6 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
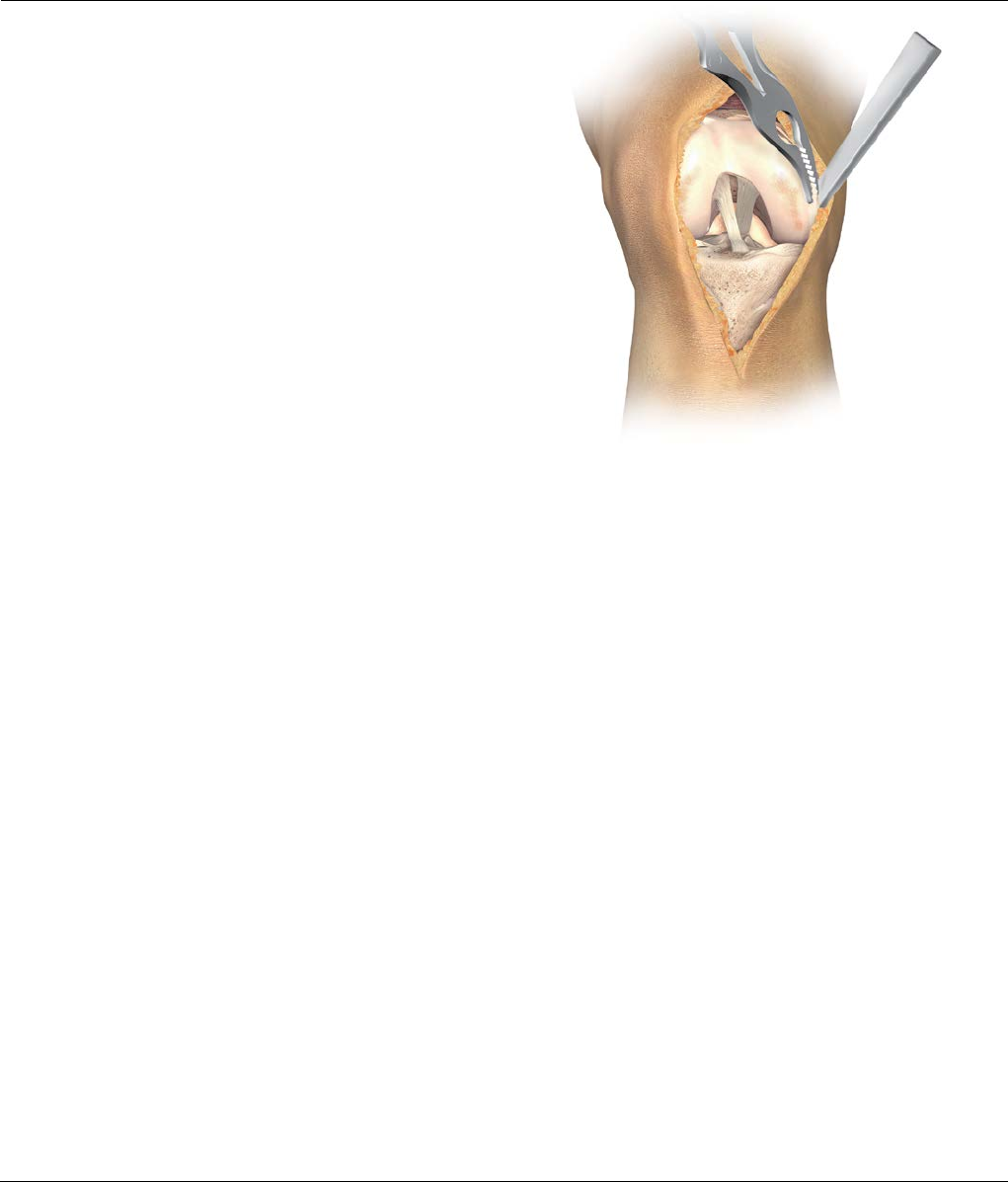
Figure5
Excise hypertrophic synovium if present and a portion of
the infrapatella fat pad to allow access to the medial,
lateral and intercondylar spaces.
Remove all osteophytes at this stage as they can affect
soft tissue balancing (Figure5).
Note: Particular attention should be given to
posterior osteophytes as they may affect flexion
contracture or femoral rotation.
Evaluate the condition of the posterior cruciate ligament
(PCL) to determine the appropriate SIGMA Component
to use. Resect the PCL if required.
Incision and Exposure
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 7
Patella Resection
Resection and preparation of the patella can be
performed sequentially or separately, as desired, and can
be performed at any time during surgery.
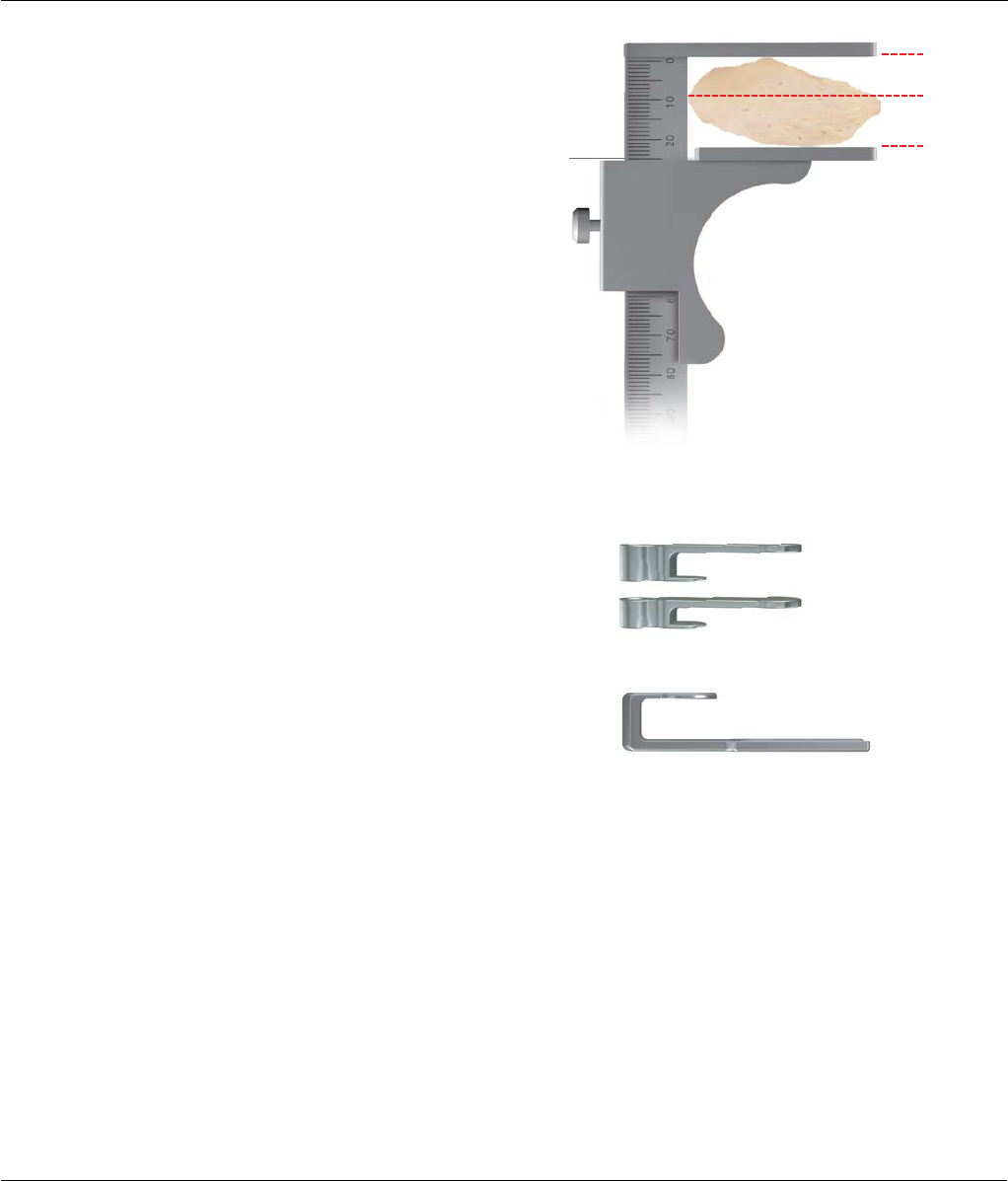
Determine the thickness of the patella and calculate the
level of bone resection (Figure6). The thickness of the
resurfaced patella should be the same as the natural
patella. There should be equal amounts of bone
remaining in the medial/lateral and superior/ inferior
portions of the patella.
Note: As a general rule, the resection usually
progresses from the medical chondro-osseous
function to the lateral chondro-osseous function.
Select a patella stylus that matches the thickness of the
implant to be used. The minimum depth of the patella
resection should be no less than 8.5 mm (Figure7).
However, when the patella is small, a minimal residual
thickness of 12 mm should be maintained to avoid fracture.
8.5 mm
16.5 mm
25 mm
Example (for a 38 mm size dome
or oval/dome patella): From a
patella 25 mm thick, resect 8.5 mm
of articular surface, leaving 16.5
mm of residual bone to
accommodate the 8.5 mm
thickness implant.
Size 41- resect 11 mm
Sizes 32, 35, 38 - resect 8.5 mm
Posterior
Anterior
Figure6
Figure7
12 mm remnant
Patella stylus
8 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
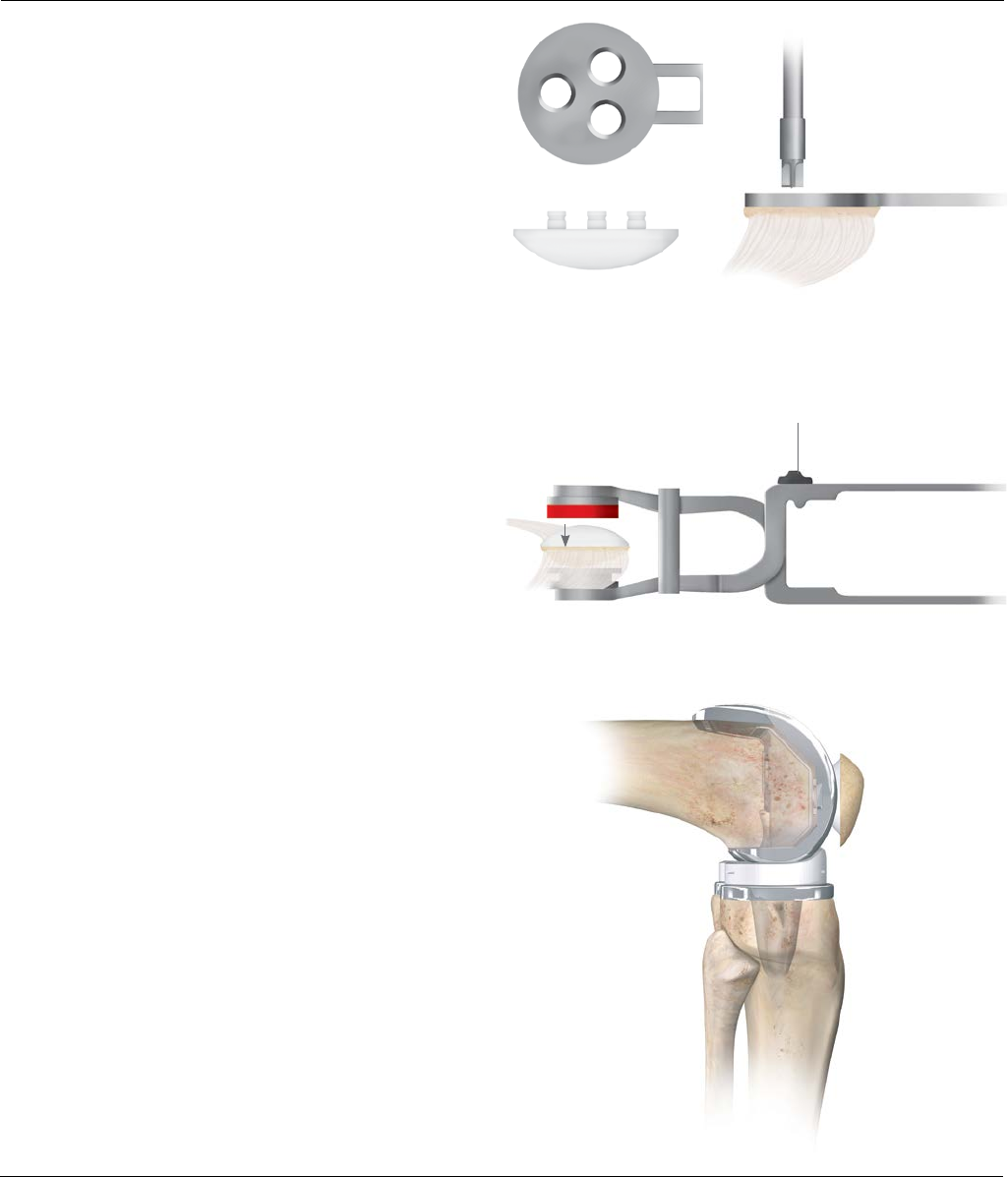
Patella wafer
Figure10
Patella Resection
A 12 mm remnant stylus can be attached to the
resection guide resting on the anterior surface of the
patella, to avoid over-resection (Figure8).
Place the leg in extension and evert the patella. Next
position the patella resection guide with the sizing stylus
against the posterior cortex of the patella with the
serrated jaws at the superior and inferior margins of the
articular surface. Close the jaws to firmly engage the
patella (Figure9).
Remove the stylus and perform the resection using an
oscillating saw through the saw capture and flush to the
cutting surface (Figure10).
A patella wafer can be hand placed on the resected
surface if required to protect the patella bone bed.
Figure9
Figure8

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 9
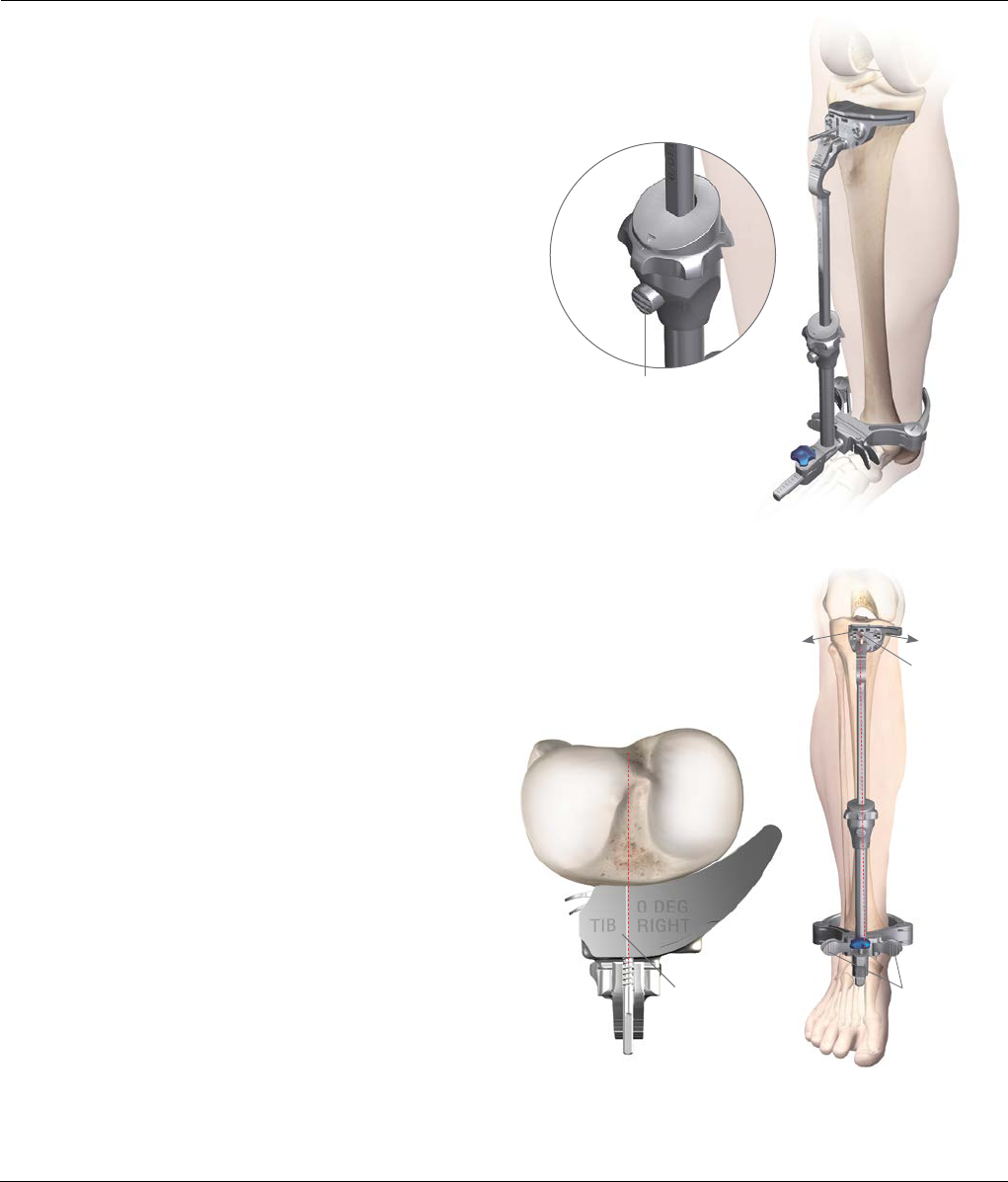
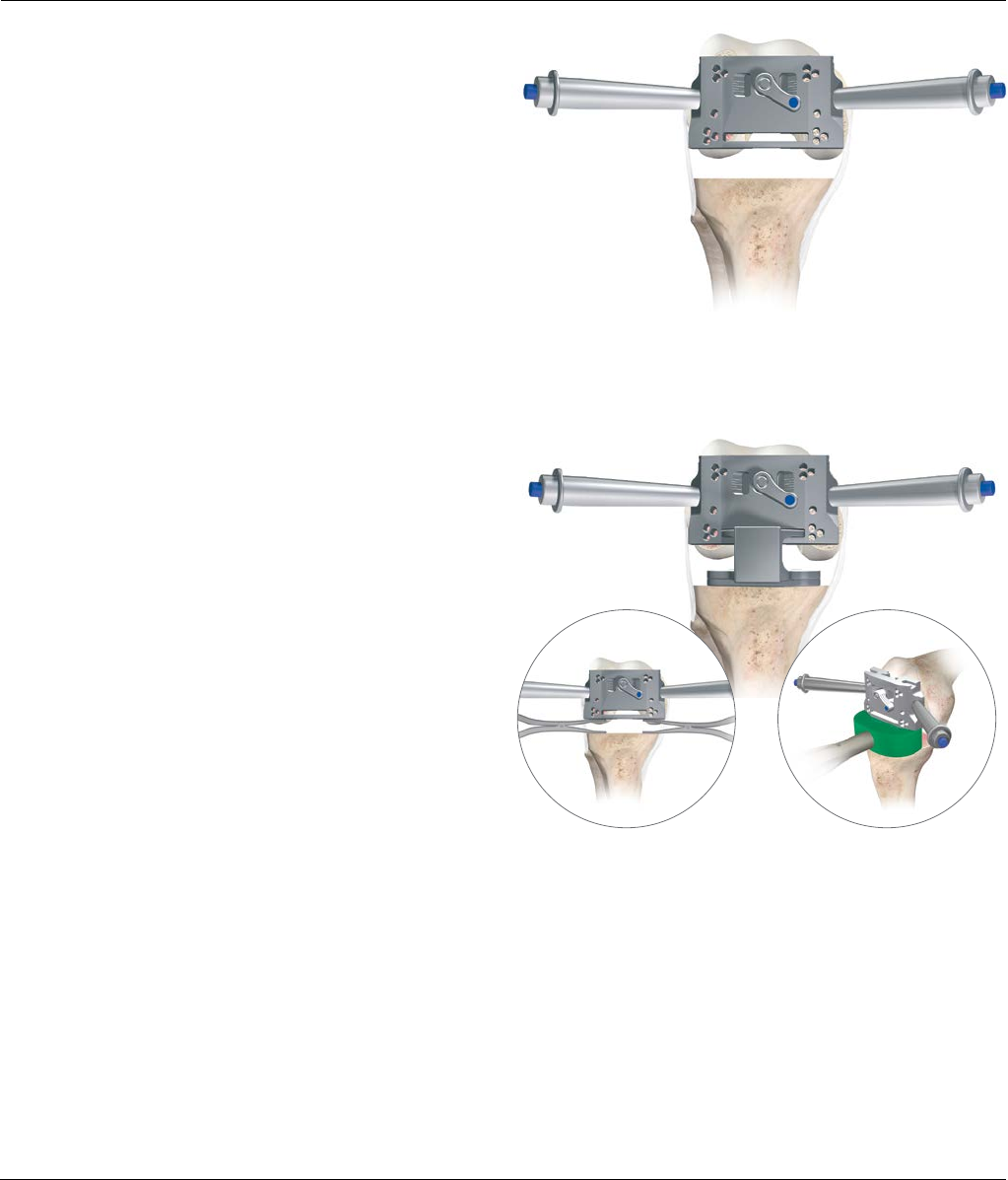
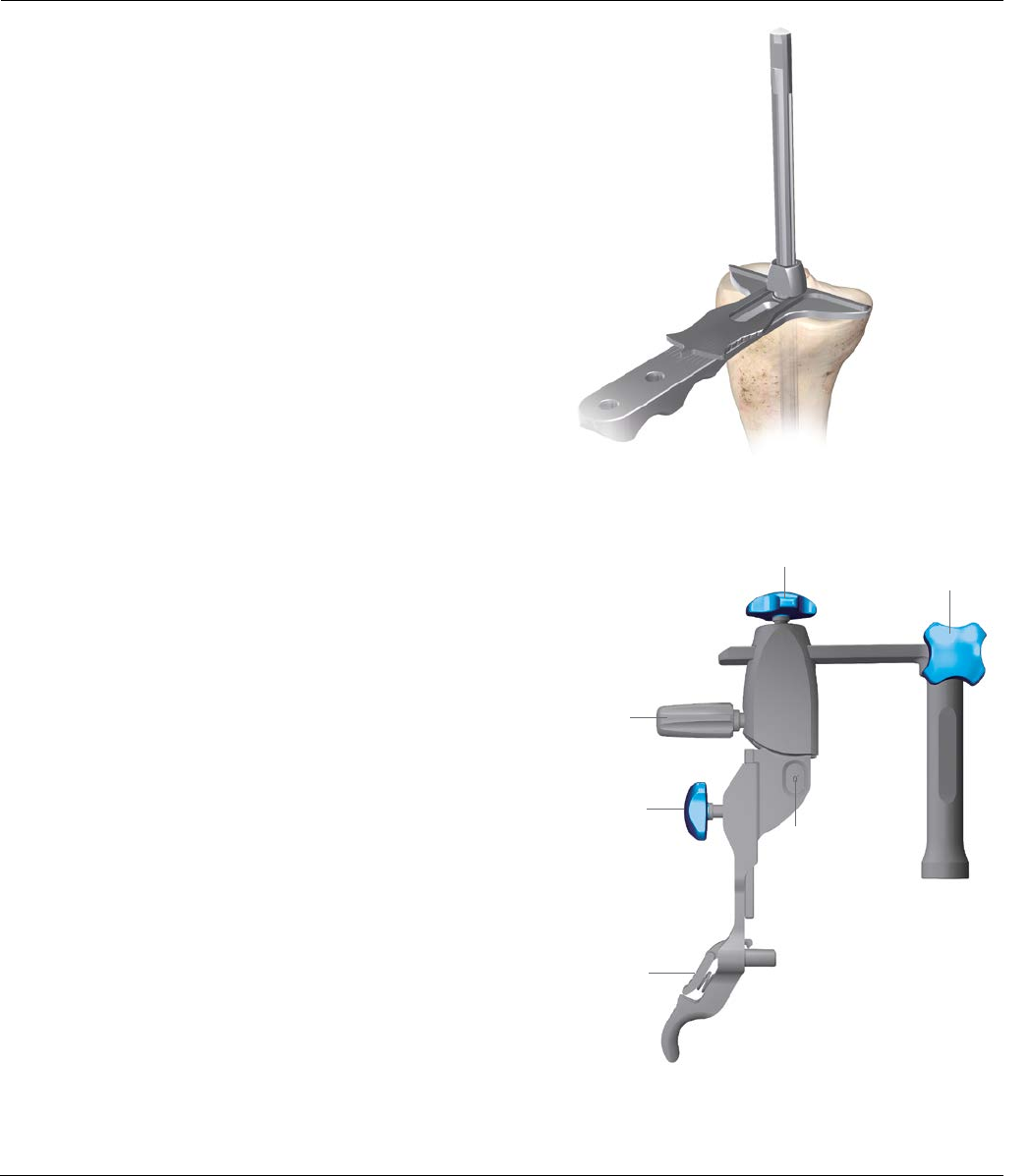
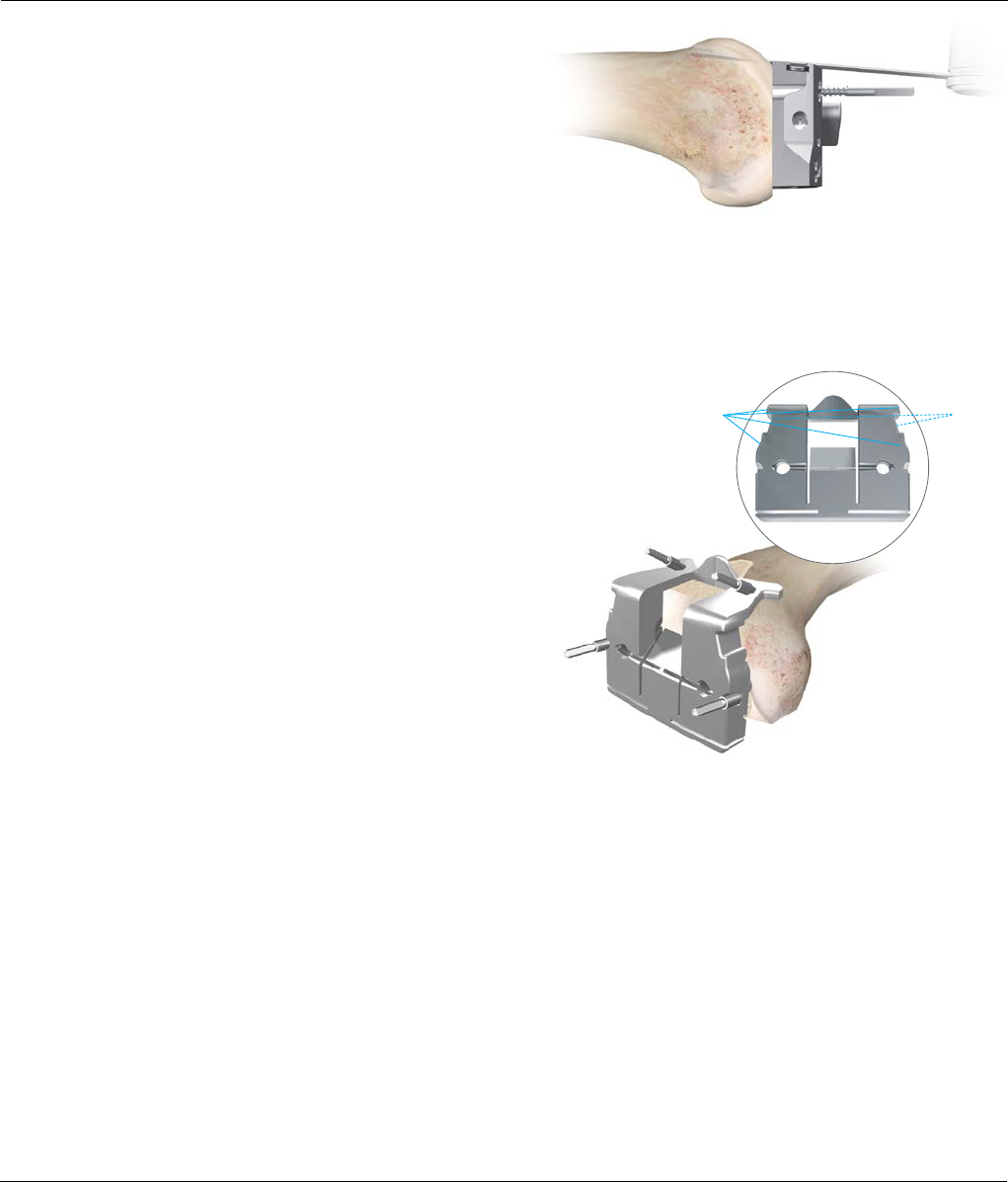
Tibial Jig Assembly
The tibia can now be resected to create more room in
the joint space.
Assemble the appropriate 0-3 degree, left/right or
symmetrical cutting block to the tibial jig uprod. Slide the
tibial jig uprod into the ankle clamp assembly (Figure11).
Tibial jig uprod
Figure11
Tibial Cutting Blocks
(Left/Right 0-3 degree)
Symmetrical Tibial Cutting
Block
Press down to
attach Cutting Block
When inserting the uprod
the button on the jig needs
to be pressed in.
10 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
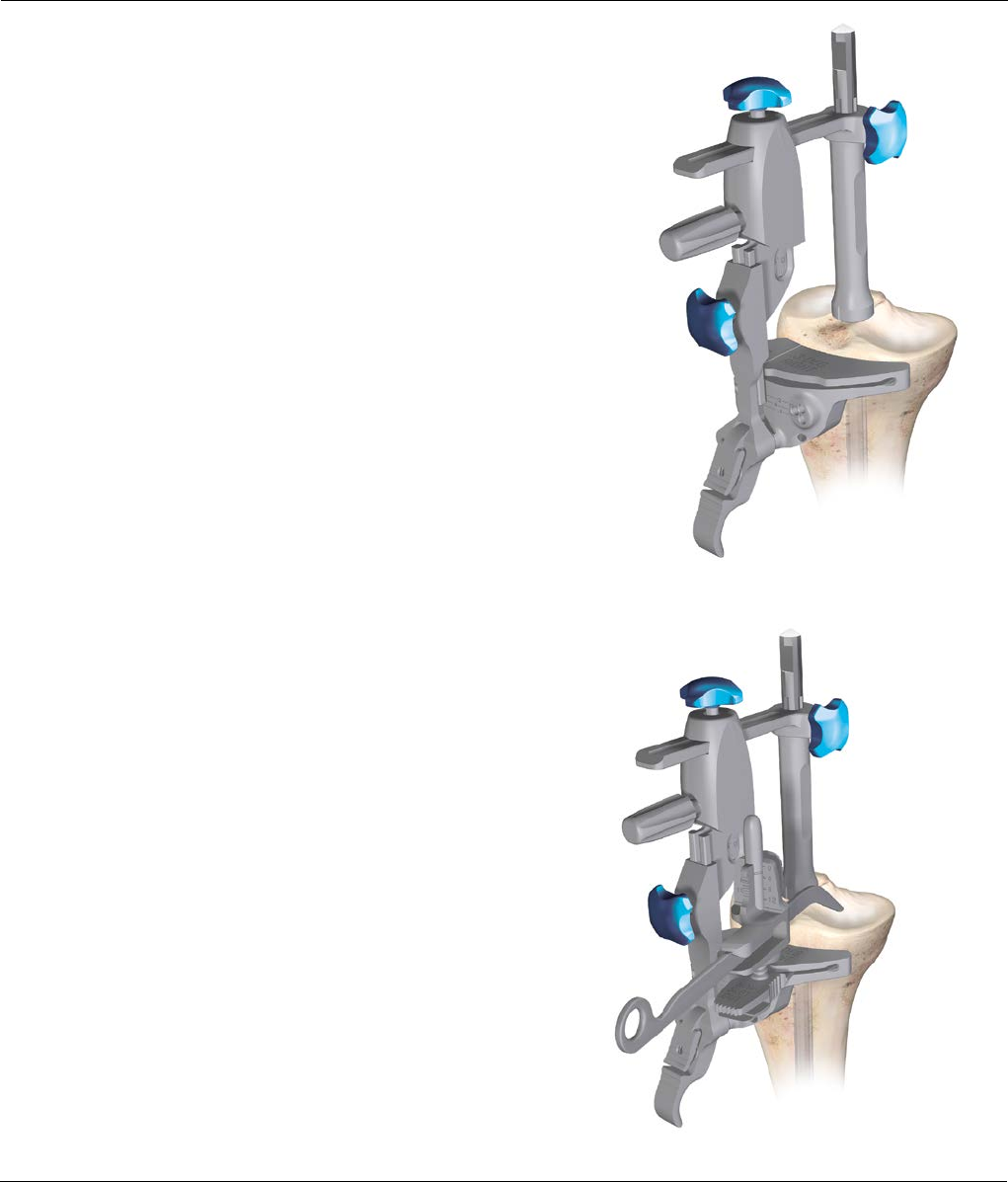
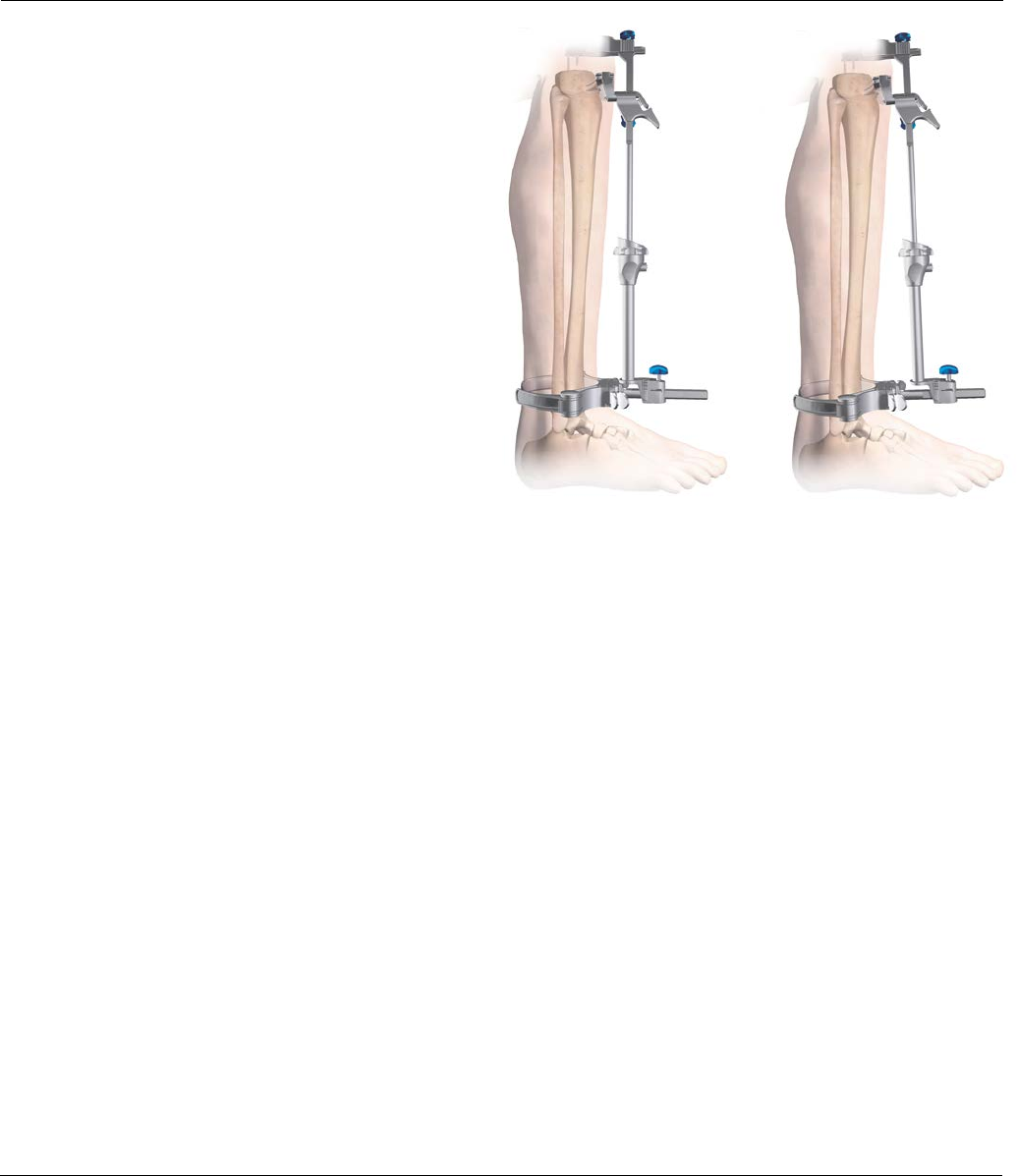
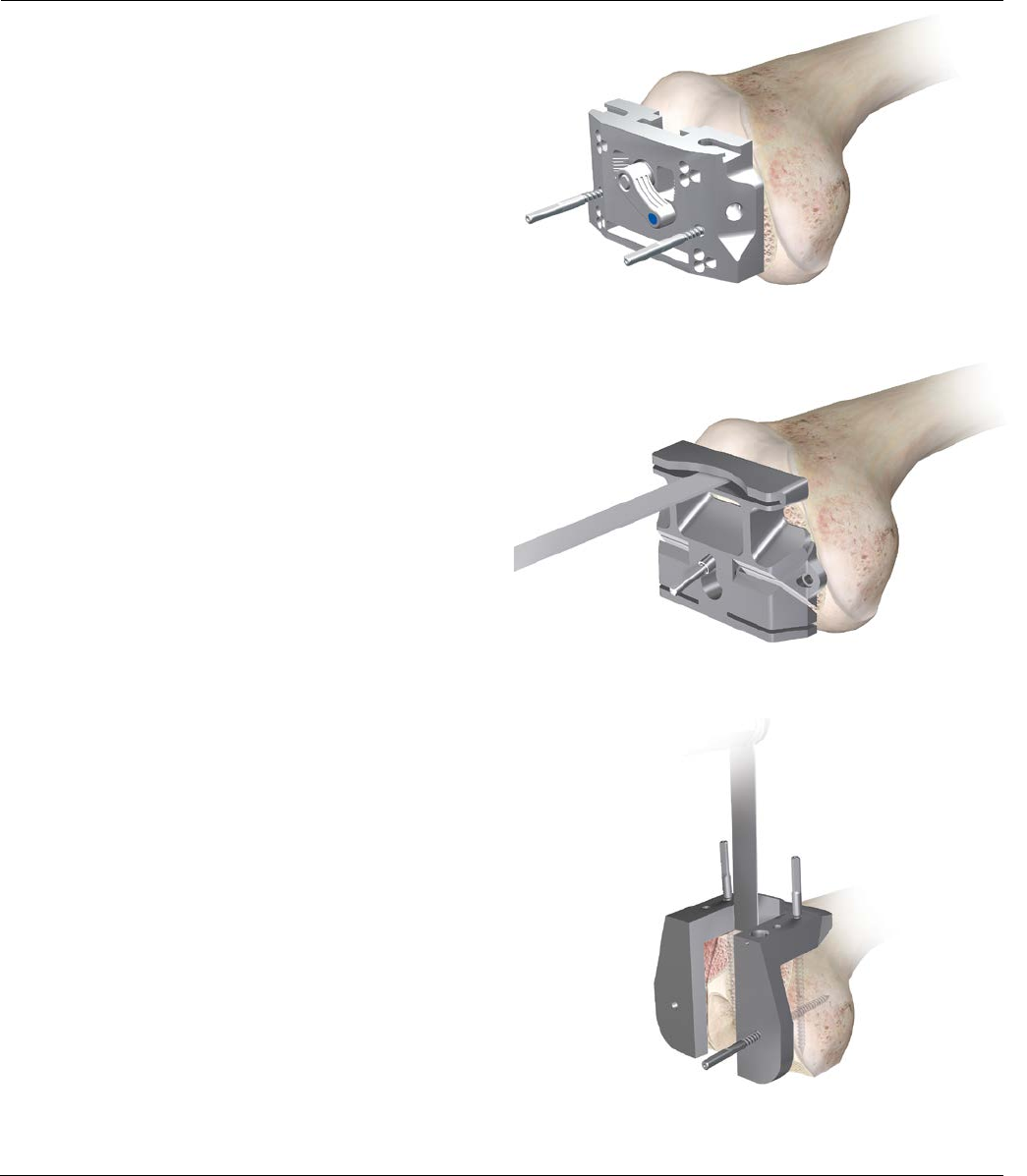
Lower Leg Alignment
Place the knee in 90 degrees of flexion with the tibia
translated anteriorly and stabilized. Place the ankle
clamp proximal to the malleoli (Figure12). Align the
proximal central marking on the tibia cutting block with
the medial one third of the tibial tubercle to set rotation.
To provide stability, insert a central pin through the
vertical slot in the cutting block to aid stability
(Figure12). Push the quick release button to set the
approximate resection level.
Varus / Valg us
Align the tibial jig ankle clamp parallel to the
transmalleolar axis to establish rotational alignment
(Figure13). The midline of the tibia is approximately 3-5
mm medial to the transaxial midline. Translate the lower
assembly medially (usually moving it one-two vertical
marks in from the mark furthest out). Each marking is
2.5 mm apart. There are also vertical scribe marks for
reference aligning to the middle of the talus (Figure14).
Slope
The tibial jig uprod and ankle clamp are designed
to prevent an adverse anterior slope. On an average size
tibia this guide gives approximately a 0 degree (Figure15)
tibial slope when the slope adjustment is translated
anteriorly until it hits the stop. In some cases, a slight
amount of slope will remain (1-2 degrees) (Figure16).
Vertical pin slot
Varus/Valgus wings
Quick release button
Figure14Figure13
Tibial Block
Reference Line:
for finding the
center of the tibia.
Figure12
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 11
Lower Leg Alignment
Increase the angle of the tibial slope to greater than 0
degrees if the patient has a greater natural slope
(Figure15). First, unlock the slope adjustment lock and
then translate the tibial slope adjuster anteriorly until the
desired angle is reached. For a Cruciate Substituting (CS)
design, a 0 degree posterior slope is recommended. For
a Cruciate Retaining (CR) design, a 3 degree posterior
slope is recommended.
As each patient’s anatomy varies, the EM tibial uprod can
be used for both smaller and larger patients. The length of
the tibia influences the amount of slope when translating
the adapter anteriorly. The 0 degree default position can be
overridden by moving the slope adjustment closer to the
ankle using the slope override button.
On the uprod 5, 6 and 7 zones are present, which
correspond to the length of the tibia. These markings
can be used to fine-tune the amount of slope. When the
uprod shows a larger zone (7) marking, this indicates
that when the lower assembly is translated 7 mm
anterior, it will give an additional 1 degree of posterior
slope (Figure16).
Height
When assessing from the less damaged side of the tibial
plateau set the stylus to 8 mm or 10 mm. If the stylus is
placed on the more damaged side of the tibial plateau,
set the stylus to 0 mm or 2 mm. Adjustment of resection
height on the stylus should be done outside the joint
space before locating the stylus in the cutting block.
If planning to resect through the slot, position the foot
of the tibial stylus marked “slotted” into the slot of the
tibial cutting block (Figure17). If planning to resect on
top of the cutting block, place the foot marked “non-
slotted” into the cutting slot.
The final resection level can be dialed in by rotating the
fine-tune mechanism clockwise (upward adjustment) or
counterclockwise (downward adjustment). Care should
be taken with severe valgus deformity, not to over resect
the tibia.
Figure17
Figure15 Figure16
Fine-tune adjustment
Slope override button
Non-slotted stylus foot
Slope adjustment lock

12 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
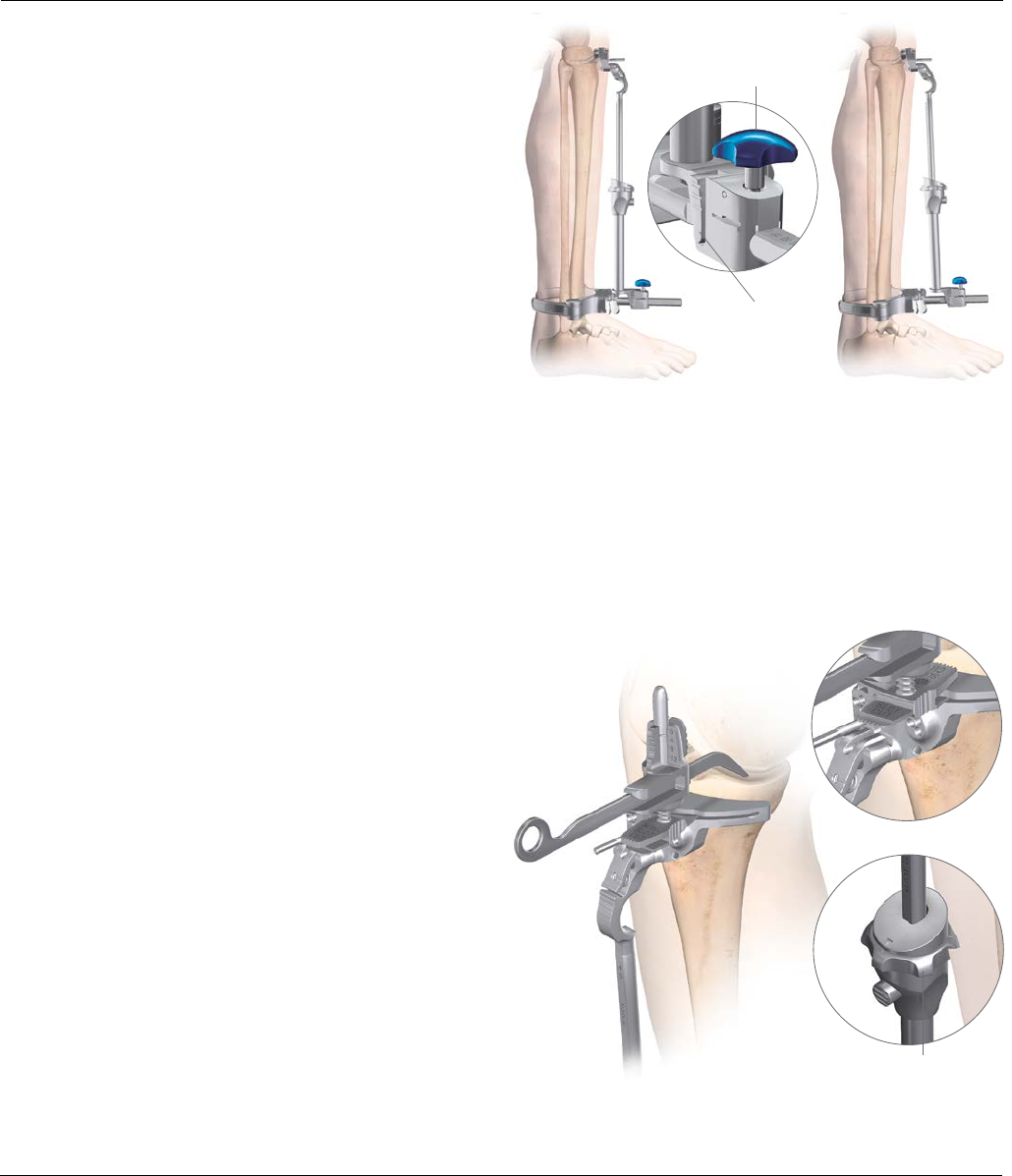
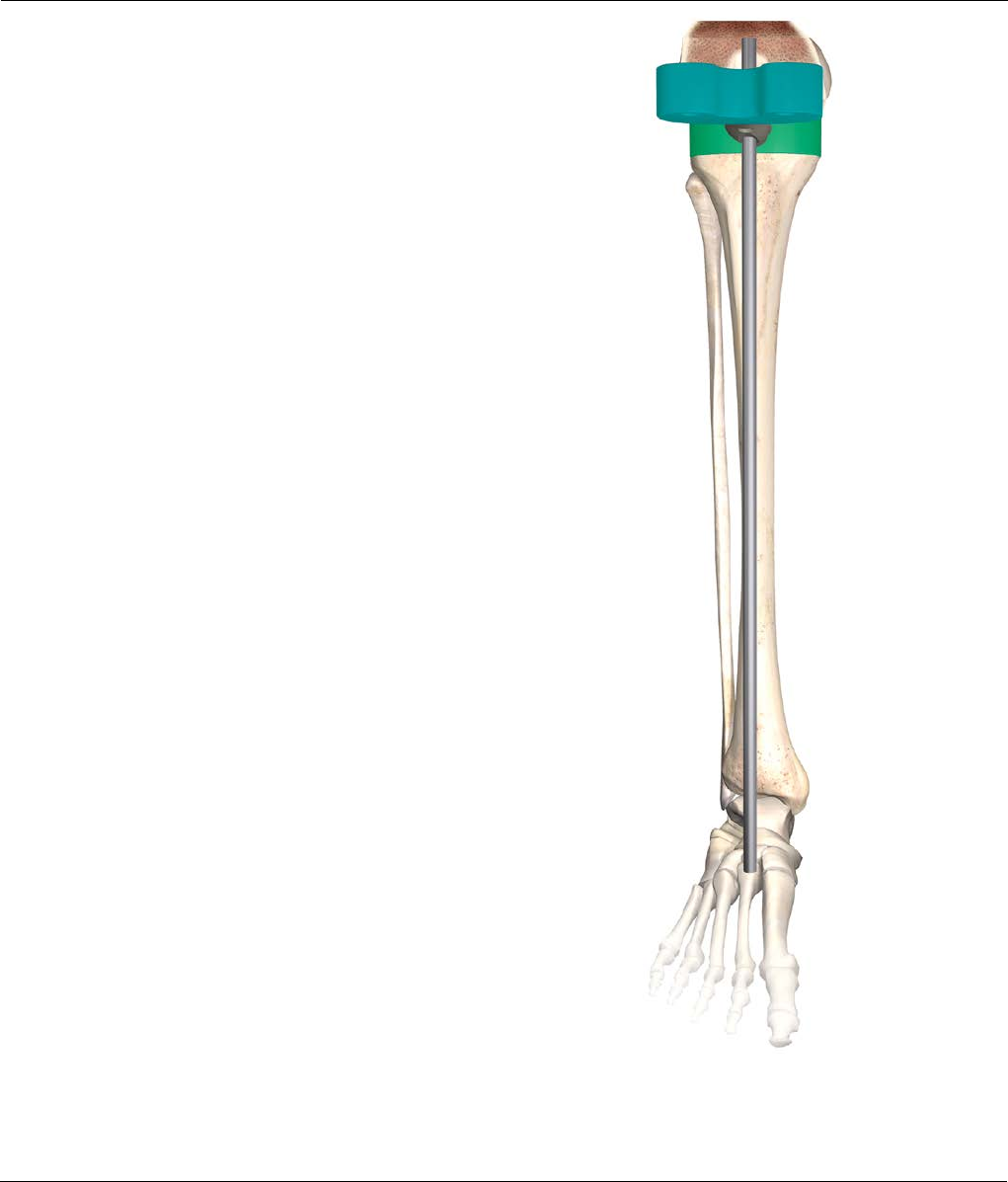
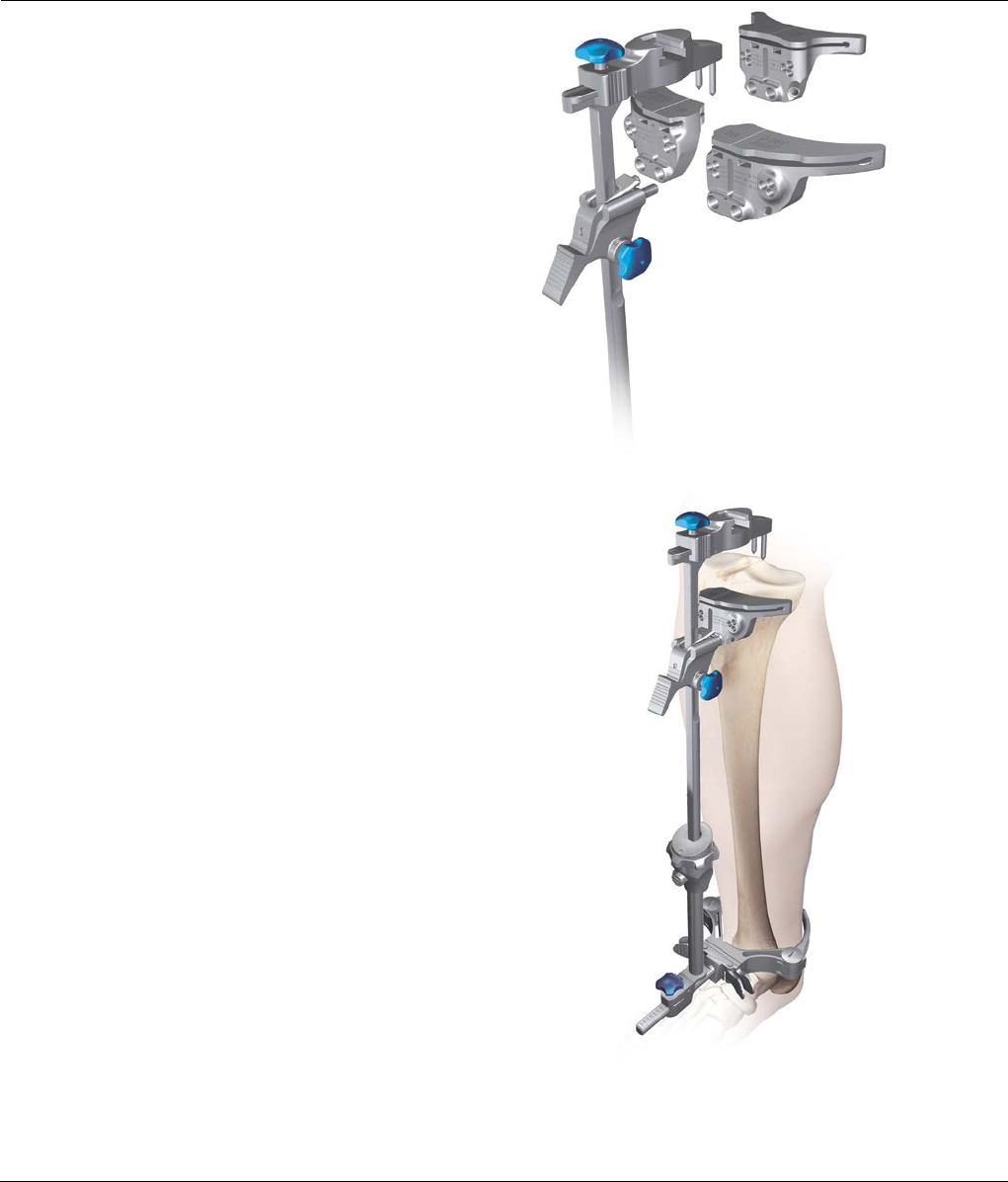
Tibial Resection
Optional: The alignment tower may be introduced
at this point into the two slots on the tibial cutting
block. With the alignment tower in place, drop an
alignment rod running from the tibial plateau to the
ankle. This may be helpful in assessing alignment
(Figure 18).
In addition a second alignment rod may be placed into
the tower in the M/L plane (Figure19). This will assist in
making sure the tibia is not cut in varus or valgus.
After the height has been set, pin the block through the
0 mm set of holes (the stylus may need to be removed
for access). +/-2 mm pinholes are available on the
resection blocks to further adjust the resection level
where needed.
The block can be securely fixed with a convergent non-
headed pin (Figure20).
Figure20
Figure18
Figure19

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 13
Note: Correct location of the medullary
canal is critical to avoid malposition of
the femoral component.
Figure21
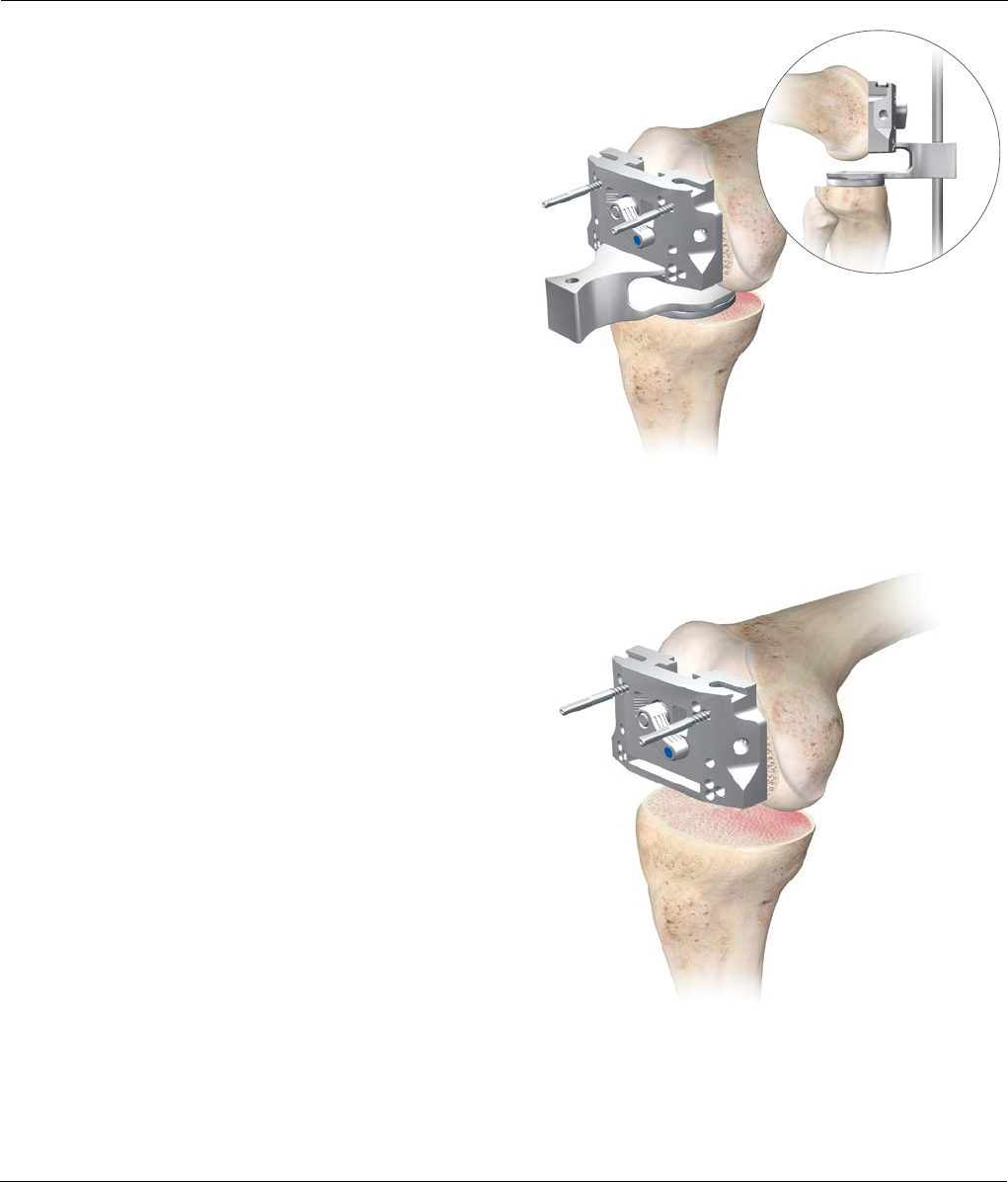
Femoral Alignment
Enter the medullary canal at the midline of the trochlea,
7 mm to 10 mm anterior to the origin of the PCL. Drill to
a depth of approximately 5 cm to 7 cm. Take care to
avoid the cortices (Figure21).
Stop drilling just before the step portion on the drill. Do
not use the step portion on the drill, as this will have an
adverse affect on the I.M. rod position when balancing.
Attach the T-handle to the I.M. rod and slowly introduce
the rod into the medullary canal, to the level of the
isthmus (Figure22).
Note: Avoid using excessive force to drive the rod
into the I.M. canal. If a large amount of force is
required to insert the rod, the femoral canal may be
overly bowed, or the distal entry hole may be too
tight to permit the rod to center in the canal. Should
this be encountered, using a shorter I.M. rod may be
more appropriate. Enlarging the distal entry hole
may help as well.
Isthmus level
Figure22

14 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Femoral Alignment
Use pre-operative radiographs to define the angle
between the femoral, anatomical and mechanical axis.
Set the valgus angle (left or right - 0 degrees to 9
degrees) on the femoral alignment guide by compressing
the two triggers and lock in place by rotating the blue
locking lever clockwise (Figure23).
Remove the T-handle and place the femoral alignment
guide on the I.M. rod and seat against the distal femur
(Figure24).
Rotate the knob counterclockwise until the arrow is
pointing to the padlock symbol. Slide the femoral
cutting block in the femoral block connector. Rotate the
knob clockwise to set the desired resection level. Every
click moves the femoral cutting block 1 mm proximal or
distal and represents a slotted resection. An open
resection will resect 4 mm less distal femur, so when an
open resection is desired, the dial should be set to take
an increased 4 mm of femur. Place the block connector
in the femoral resection guide so that the tang on the
connector slides in to the cutting slot on the cutting
block. The trigger should engage in the hole behind the
slot (Figure25 ).
Distal femoral
cutting block
Femoral block
connector
Femoral resection
guide
Figure23
Figure24
Figure25
Locking trigger in
the locked position
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 15
Femoral Alignment
Position the resection guide over the two legs of the
distal femoral alignment guide until the distal cutting
block touches the anterior femur (Figure26).
Optional: Adjust the internal/external rotation of
the alignment guide with reference to the trochlear
groove. When rotation is correct, secure the
alignment guide by inserting one threaded pin
through the medial hole.
Adjust the medial/lateral placement of the resection
block as desired and rotate until firmly seated on the
anterior condyles.
Secure the cutting block to the femur with two threaded
pins through the holes marked with a square. This will
allow a +2 or -2 mm adjustment to be made.
Resect at least 9 mm of distal femoral bone from the
most prominent condyle (Figure27).
Optional: The alignment tower may be introduced
at this point into the two slots on the distal
resection device. With the alignment tower in place,
connect two alignment rods, creating a line that
runs from the center of the hip to the ankle. This
may be helpful in assessing the mechanical axis
(Figure 28).
Distal femoral
cutting block
Figure26
Figure27
Figure28

16 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
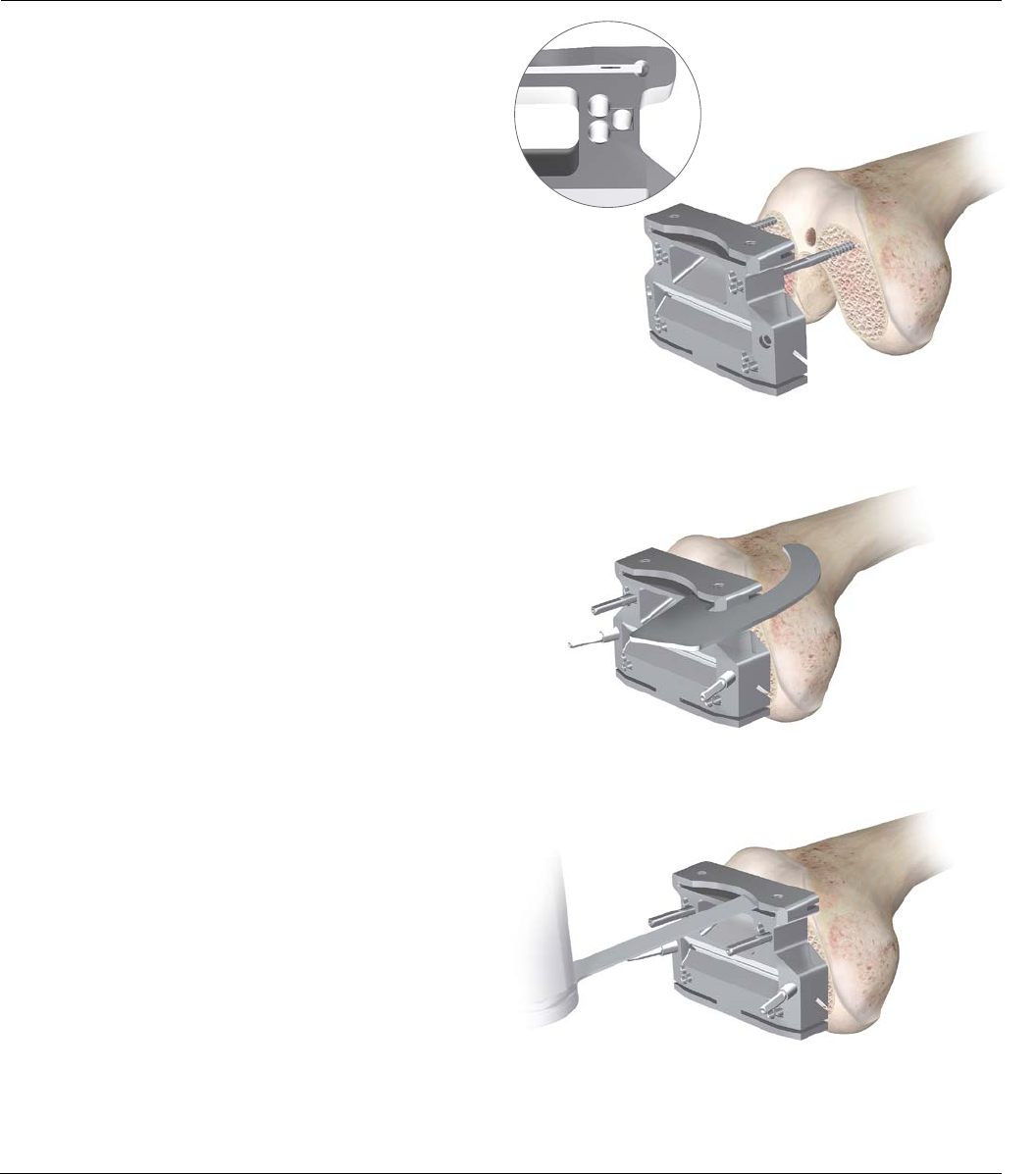
Distal Femoral Resection
After the correct amount of resection is set, add
a convergent pin through the medial hole in the block to
aid stability (Figure29).
Removal of the Femoral Alignment Guide
First attach the T-handle to the I.M. guide. Then unlock
the cutting block from the block connector, using your
thumb and index finger to release the attachment. Slide
the femoral resection guide upwards on the alignment
guide legs until the block connector disengages the
cutting block and in one motion remove the femoral
alignment guide by pulling the instruments distally in the
direction of the T-handle (Figure30).
Perform the distal femoral resection (Figure31). Resect
at least 9 mm from the most prominent condyle. After
performing the distal resection, use the power pin driver
to remove the threaded pins.
Optional: If drill pins or Steinmann pins were used
to fixate the cutting block, the pin puller can be used
to extract the pins.
Figure29
Figure30
Figure31
1. Slide femoral
resection guide
upwards
2. Remove femoral
alignment guide
towards the T-handle
Release attachment

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 17
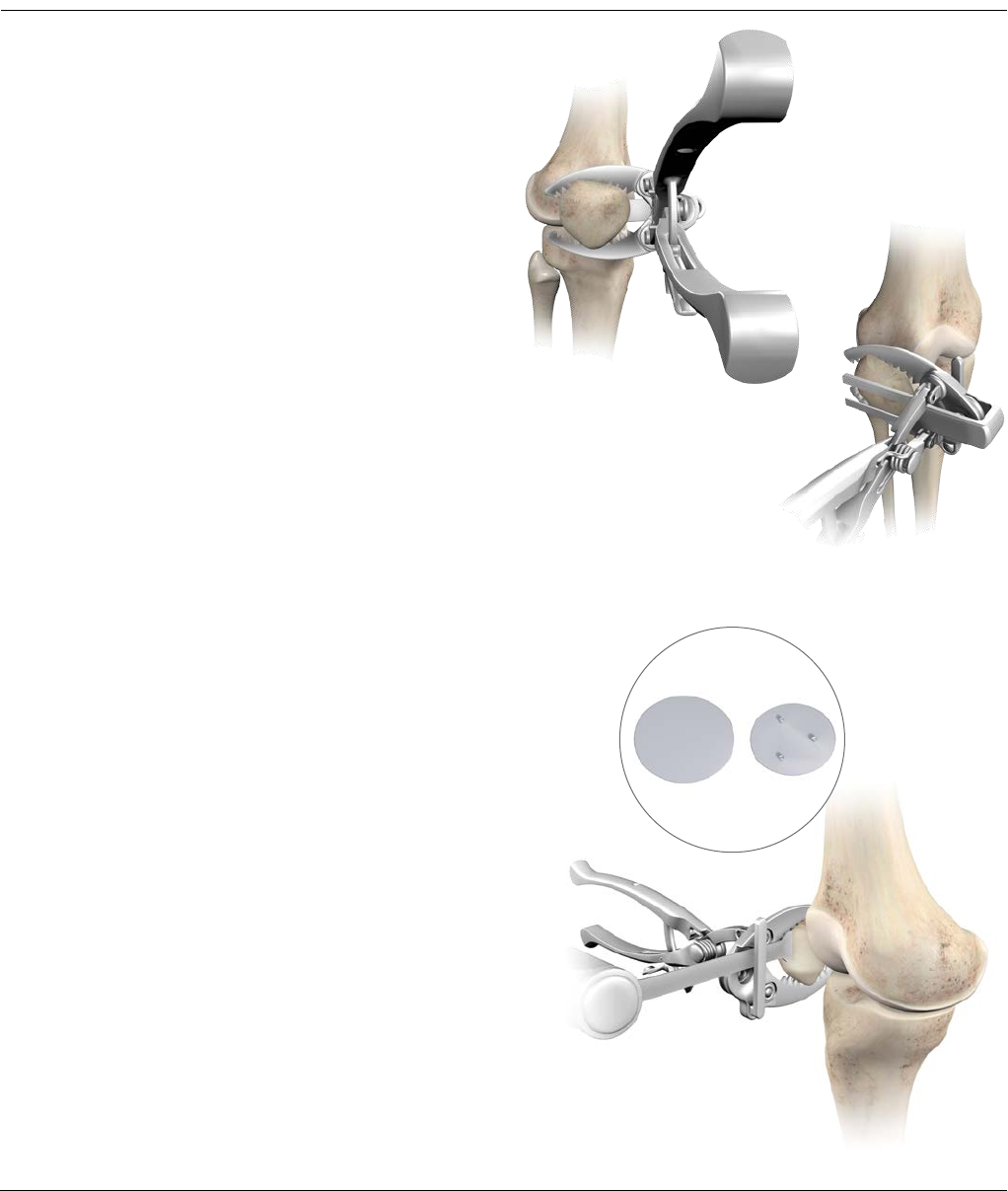
Extension Gap Assessment and balancing
Place the knee in full extension and apply lamina
spreaders medially and laterally. The extension gap must
be rectangular in configuration with the leg in full
extension. If the gap is not rectangular, the extension
gap is not balanced and appropriate soft tissue
balancing must be performed (Figure32).
A set of specific fixed bearing and mobile bearing spacer
blocks are available. Every spacer block has two ends,
one for determining the extension gap and one for the
flexion gap. At this step in the procedure, the extension
gap side of the spacer block can be used to determine
the appropriate thickness of the tibial insert and to
validate the soft tissue balance (Figure33).
Introduce the alignment rod through the spacer block.
This may be helpful in assessing alignment (Figure34).
Figure33 Figure34
Figure32
Spacer block

18 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Stylus scale
Femoral Sizing (Optional)
Place the Fixed Reference sizing guide (Figure35) or the
Classic sizing guide against the resected distal surface of
the femur, with the posterior condyles resting on the
posterior plate of the guide.
Optional: Secure the sizing guide against the distal
femur with threaded head pins (Figure 36).
Place the sizing guide stylus on the anterior femur with
the tip positioned at the intended exit point on the
anterior cortex to avoid any potential notching of the
femur. A scale on the surface of the stylus indicates the
exit point on the anterior cortex for each size of femur.
The scale is read from the distal side of the lock knob
(Figure36).
Tighten the blue locking lever downward and read the
size from the sizing window (Figure37).
Figure35
Figure36
Figure37
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 19
Femoral Rotation
Select the appropriate balanced block, based upon the
size of the femur. Then select the appropriate I.M. rod (3
or 5 degrees) with the correct left/right designation
positioned anteriorally, as determined during
pre-operative X-ray analysis. Slide the rod into the
SIGMA Knee or RP-F balanced resection block. Insert the
I.M. rod into the distal femoral I.M. canal taking care to
avoid over-pressurization (Figure38).
Note: The RP-F and standard SIGMA Blocks are
visually very similar. To help differentiate them,
the RP-F block has the letters “RP-F” engraved on
it, and a series of grooves rising from the posterior
cut face.
Assemble the femoral stylus to the medial anterior slot
of the SIGMA Knee or RP-F balanced block and tighten
it by turning the knurled screw clockwise (Figure39).
Note: Care should be taken to ensure the stylus is
completely tightened down on the balanced block.
Ensure the A/P resection block is unlocked and lower the
assembly on the I.M. plate. Translate the block
posteriorly until the anterior femoral stylus contacts the
anterior cortex of the femur. The stylus should rest on
the anterior femur at the approximate exit point of the
anterior cut. Fix the position of the balanced block by
turning the blue locking mechanism clockwise. Final
rotation has not been fixed at this stage. Remove the
anterior femoral stylus (Figure40).
Figure38
Figure39
Figure40
20 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Femoral Rotation
Two handles can be attached to the balanced cutting
block to help in visualizing the degree of rotation of the
balanced cutting block in respect to the transepicondylar
axis (Figure41).
Rotation is determined with the knee in 90 degrees of
flexion such that the posterior surface is parallel to the
resected tibial plateau. Introduce the femoral guide
positioner, (with the appropriate tibial shim added) into
the joint space engaging the posterior slot of the
balanced resection guide (Figure42). The femoral guide
positioner thickness should mirror the extension gap
previously determined with the spacer block.
The knee may be slightly flexed or extended until the
positioner lies flat on the resected proximal tibia.
Alternatively lamina spreaders or spacer blocks
(Figure42) can be used.
Figure41
Figure42
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 21
Femoral Rotation
If the flexion gap is too lax, thicker tibial shims should be
added to ensure that the positioner fits snugly (Figure43).
Note: If the flexion gap no longer matches the
extension gap, the distal cut will need to be
revisited.
Re-evaluate the tibial alignment by putting the external
alignment rod through the hole at the end of the femoral
guide positioner (Figure43).
The femoral rotation is set by the femoral guide positioner
and is based on the principle of equal compartment tension
and balanced collateral ligaments. Using the femoral guide
positioner this balance should automatically occur, because
the femur can freely rotate around the I.M. plate.
All adjustments should be made prior to pinning the
block. Pin the A/P resection block to the distal femur
using the two neutral central holes (marked with a square)
that are located in the anterior or posterior cluster of
three pin holes. The decision to pin through the neutral
posterior pin holes or neutral anterior pin holes should be
based upon the surgeon’s preferred workflow (Figure44).
Remove the Femoral Guide positioner.
Figure43
Figure44
22 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Femoral Preparation - A/P and Chamfer Cuts
Remove the balanced femoral cutting block, leaving the
pins in the distal femur. Select the SIGMA or SIGMA
RP-F Fixed Reference A/P Chamfer Block that matches
the femur size. Slide the block onto the pins through the
appropriate pin holes (Figure45).
The RP-F and standard SIGMA Cutting Blocks look very
similar. Care should be taken not to confuse the blocks
as this will result in under or over resection of the
posterior condyles. The RP-F block can be identified
through the letters “RP-F” on the distal face, and a
series of grooves along the posterior cut slot.
Place the block over the two threaded pins through the
0 mm pinholes.
Note: The block may be shifted 2 mm anteriorly or
posteriorly by selecting one of the offset holes
around the “0” hole.
After confirming cut placement with the reference
guide, or angel-wing, insert threaded headed pins into
the convergent pin holes on the medial and lateral
aspect of the A/P chamfer block (Figure46).
Resect the anterior and posterior femur
(Figures 47 and 48).
Figure45
Figure46
Figure47

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 23
Femoral Preparation - A/P and Chamfer Cuts
Place retractors to protect the MCL medially and the
popliteal tendon laterally.
Note: The posterior saw captures are open medially
and laterally to ensure completed saw cuts over a
wide range of femoral widths. To reduce the risk of
inadvertent sawblade kickout when making
posterior resections, insert the sawblade with a
slight medial angle prior to starting the saw.
Remove the initial locating pins and proceed with the
chamfer cuts (Figures 49 and 50).
Figure48
Figure50
Figure49

24 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Femoral Resection - Notch cuts
When using a stabilized SIGMA or SIGMA RP-F
Component, select and attach the appropriate femoral
Notch Guide. The SIGMA RP-F Component and standard
SIGMA Notch Guides look very similar. Care should be
taken not to confuse the blocks as this will result in
under-or-over resection of the box.
The SIGMA RP-F Guide can be identified through the
letters “RP-F” on the anterior face, and a series of
grooves along the notch distal anterior corner.
Position the notch guide on the resected anterior and
distal surfaces of the femur. Pin the block in place
through the fixation pin holes with at least three pins
before any bone cuts are made (Figures 51 and 52).
Figure51
Figure52
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 25
Measuring the Flexion Gap
The flexion side of the spacer block is used to evaluate
the flexion gap. Where RP-F spacer blocks are used,
flexion shims will need to be added.
An alignment rod assembled to the spacer block should
pass through the center of the talus and lie parallel to
the lateral tibial axis (Figure53).
Figure53

26 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Trial Components
Note: Either MBT or Fixed Bearing tibial
components can be trialed prior to performing
the tibial preparation step.
Femoral Trial
Attach the slap hammer or universal handle to the
femoral inserter/extractor. Position the appropriately
sized femoral trial on the inserter by depressing the two
triggers to separate the arms and push the trial against
the conforming poly surface. Release the triggers so that
the arms engage in the slots on the femur, and rotate
the handle clockwise to lock. Position the trial onto the
femur, impacting as necessary. To detach the inserter
from the femur, rotate the handle counterclockwise and
push the two triggers with thumb and index finger
(Figure54).
Tibial Trial
Place the appropriate sized MBT tray trial onto the
resected tibial surface. Position the evaluation bullet into
the cut-out of the MBT tray trial (Figure55). There are
two options available to assess the knee during trial
reduction. One or both may be used.
1. Trial reduction with the MBT tray trial free
to rotate
This option is performed using a non-spiked MBT
evaluation bullet. It is useful when the tibial tray
component is smaller than the femoral size.
Note: Mobile bearing tibial insert size MUST match
femoral component size.
With equivalent sizes the bearing rotation allowance is
8 degrees for SIGMA Knee and 20 degrees for SIGMA
RP-F Instruments. For a tibial tray one size smaller than
the femoral component, this bearing rotation allowance
reduces to 5 degrees. In this situation, finding the
neutral position with respect to the femur is therefore
more important in order to prevent bearing overhang
and soft tissue impingement. Position the evaluation
bullet into the cut-out of the MBT tray trial.
Figure55
Figure54

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 27
Trial Components
2. Trial reduction with MBT tray trial fixed in place
This trial reduction can be done instead or in addition to
the one described before.
Place the appropriately sized MBT tray trial onto the
resected tibial surface (Figure56).
Assess the position of the tray to achieve maximal tibial
coverage (align the tibial tray handle with the
electrocautery marks if procedure described in tibial trial
1 has been followed). The rotation of the MBT tray trial
is usually centered on the junction between the medial
and central one-third of the tibial tubercle. Secure the
keel punch impactor to the spiked evaluation bullet and
position into the cut-out of the MBT tray trial. Tap down
lightly to secure the tray to the proximal tibia (Figure57).
Figure56
Figure57
28 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Trial Components
Select the tibial insert trial that matches the chosen
femoral size and style, curved or stabilized, and insert it
onto the MBT tray trial (Figure58). Carefully remove the
tibial tray handle and, with the trial prosthesis in place,
extend the knee carefully, noting the anterior/posterior
stability, medial/lateral stability and overall alignment in
the A/P and M/L plane. If there is any indication of
instability, substitute a tibial insert trial with the
next greater thickness and repeat the reduction.
Select the tibial insert trial that gives the greatest
stability in flexion and extension while still allowing full
extension (Figure59).
Adjust rotational alignment of the MBT tray trial with the
knee in full extension, using the tibial tray handle to rotate
the tray and trial insert into congruency with the femoral
trial. The rotation of the MBT tray trial is usually centered
on the junction between the medial and central one-third
of the tibial tubercle. Overall alignment can be confirmed
using the two-part alignment rod, attaching it to the tibial
alignment handle (Figure60). The appropriate position is
marked with electrocautery on the anterior tibial cortex.
Fully flex the knee, and remove the trial components.
Figure59
Figure58
Cautery
marks
Figure60

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 29
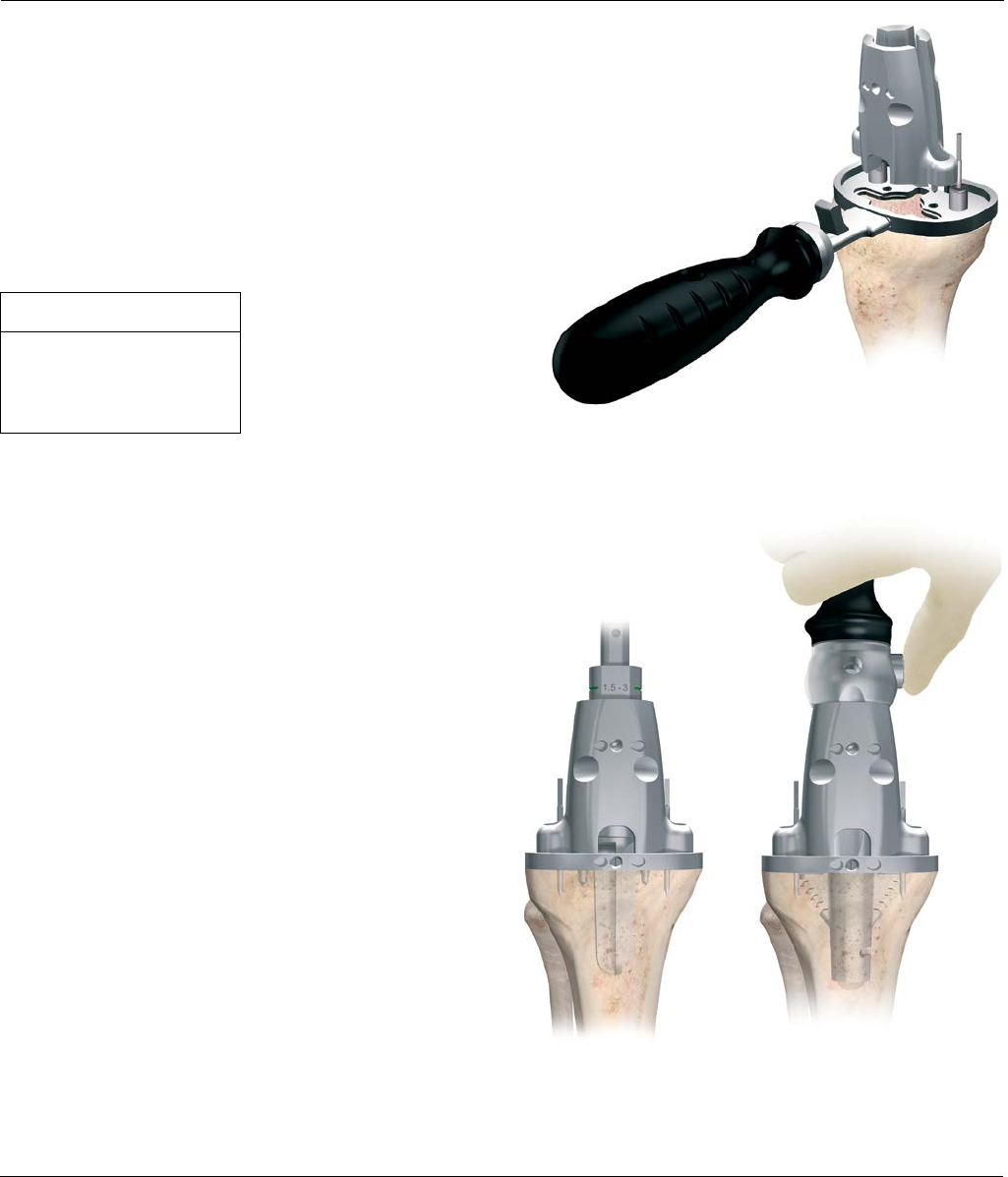
Tibial Preparation - MBT
Tibial Preparation
Align the tibial trial to fit with the tibia for maximum
coverage or, if electrocautery marks are present, use
these for alignment. Pin the trial with two pins. The tray
trial allows for standard and MBT keeled (Figure61).
Attach the MBT drill tower to the tray trial. Control the
tibial reaming depth by inserting the reamer to the
appropriate colored line (Figures 62 and 63). An optional
Modular Drill Stop is available to provide a hard stop
when reaming. See table for appropriate size.
Note: For cemented preparation, select the
“Cemented” instruments, and for non-cemented or
line-to-line preparation, select the “Non-Cemented”
tibial instruments. The Cemented instruments will
prepare for a 1 mm cement mantle around the
periphery of the implant.
Tray Size Line Color
1-1.5 Green
2-3 Yellow
4-7 Purple
Figure61
Figure62 Figure63
Tray fixation pins

30 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
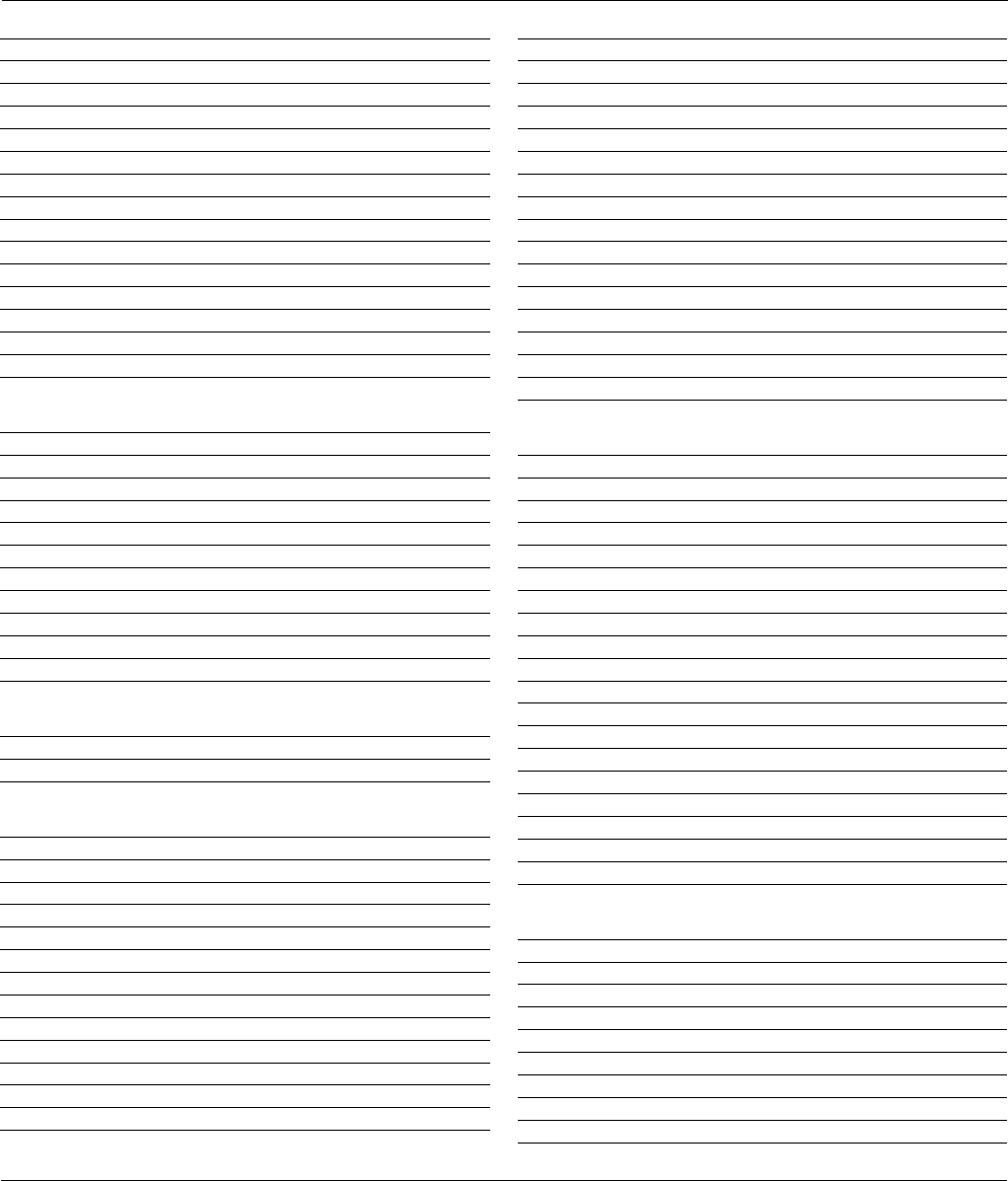
Tibial Preparation - MBT
Keeled Tray Option
If a keeled MBT tray is to be employed and the bone of
the medial or lateral plateau is sclerotic, it is helpful to
initially prepare the keel slot with an oscillating saw or
high speed burr. Assemble the MBT keel punch impactor
to the appropriately-sized MBT keel punch by pressing
the side button and aligning the vertical marks on both
impactor and keel punch (Figure64). Insert assembly
into the MBT Drill Tower, taking care to avoid
malrotation. Impact the assembly into the cancellous
bone until the shoulder of the keel punch impactor is in
even contact with the MBT Drill Tower (Figure65).
Non-Keeled Tray Option
For a non-keeled tray option, attach the MBT non-keeled
punch and follow the same routine (Figure66).
Final Trialing Option
A secondary and final trialing step can be performed
after tibial preparation. Remove the keel punch impactor
from the keel punch by pressing the side button and
remove the drill tower as well. Place the trial femoral
component on the femur. Then place the appropriate
tibial insert trial onto the tray trial and repeat previous
trial evaluation.
Figure64
Figure65
Figure66
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 31
Final Patella preparation
Figure67 Figure68
Locking
switch
Figure69
Figure70
Select a template that most adequately covers
the resected surface without overhang (Figure67).
If used, remove the patella wafer from the patella.
Position the template handle on the medial side of the
everted patella. Firmly engage the template to the
resected surface and drill the holes with the appropriate
drill bit (Figure68).
Cement the patellar implant. Thoroughly cleanse
the cut surface with pulsatile lavage. Apply cement to
the surface and insert the component. The patellar
clamp is designed to fully seat and stabilize the implant
as the cement polymerizes. Center the silicon O-ring
over the articular surface of the implant and the metal
backing plate against the anterior cortex, avoiding skin
entrapment. When snug, close the handles and hold by
the ratchet until polymerization is complete. Remove all
extruded cement with a curette. Release the clamp by
unlocking the locking switch and squeezing the handle
together (Figure69).
Reduce the patella and evaluate the patella implant.
Unrestricted range of motion, free bearing movement
and proper patellar tracking should be evident
(Figure70).

32 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Cementing Technique
Prepare the sclerotic bone to ensure a continuous
cement mantle with good cement interdigitation. This
can be done by drilling holes and cleansing the bone by
pulsatile lavage (Figure71). Any residual small cavity
bone defects should be packed with cancellous
autograft, allograft or synthetic bone substitutes such as
CONDUIT® TCP Granules.
Note: Blood lamination can reduce the mechanical
stability of the cement, therefore it is vital to choose
a cement which reaches its working phase early.
Whether mixed by the SMARTMIX® Vacuum Mixing Bowl
or the SMARTMIX CEMVAC® Cement System, SMARTSET®
HV Bone Cement or MV Bone Cement offers convenient
handling characteristics for the knee cementation process.
A thick layer of cement can be placed either on the bone
(Figure72) or on the implant itself.
Figure71
Figure72

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 33
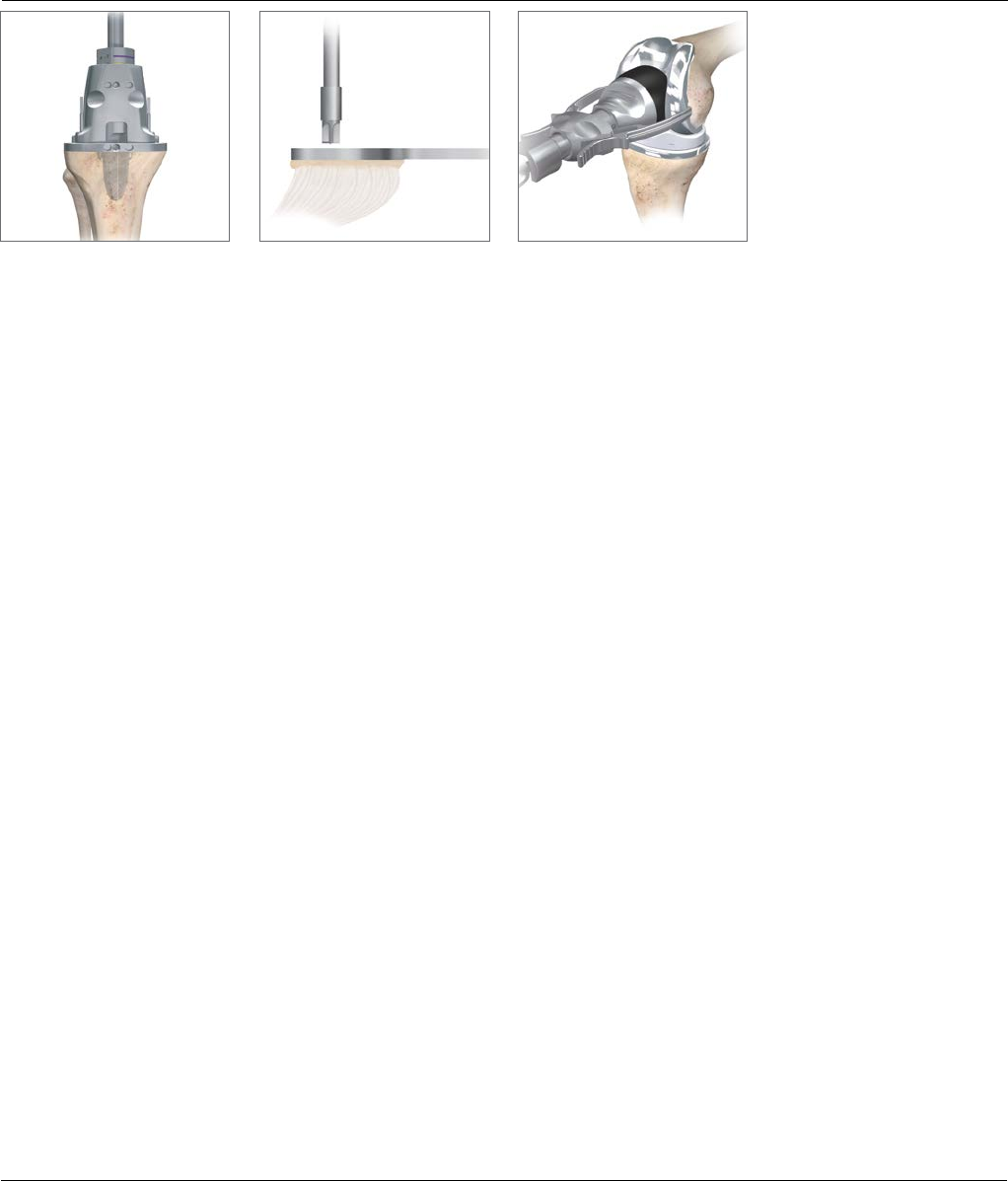
Final Component Implantation
Tibial Implantation
Attach the MBT tibial impactor by inserting the plastic
cone into the implant and tighten by rotating the lock
knob clockwise. Carefully insert the tibial tray avoiding
malrotation (Figure73). When fully inserted, several
mallet blows may be delivered to the top of the tray
inserter. Remove all extruded cement using a curette.
Optional: To perform a trial reduction with an
insert trial, place the MBT Trial Plateau Post into
the tibial tray component and place the insert trial
over this post and proceed with the trial reduction
(Figure 74).
Polyethylene Implantation
Remove loose fragments or particulates from the
permanent tibial tray. The appropriate permanent tibial
insert can be inserted.
Femoral Implantation
Hyperflex the femur and sublux the tibia forward. Attach
the slap hammer or universal handle to the femoral
inserter/extractor. Position the appropriately sized
femoral component on the inserter/extractor by
depressing the two triggers to separate the arms and
push the femoral component against the conforming
poly. Release the triggers so that the arms engage in the
slots on the femoral component and rotate the handle
clockwise to lock (Figure75).
Extend the knee to approximately 90 degrees for final
impaction. Release the inserter/extractor by rotating the
handle counterclockwise and push the two triggers with
thumb and index finger. For final femur impaction, use
the femoral notch impactor to seat the femoral
component. In SIGMA CS and SIGMA RP-F Instruments
(not SIGMA Knee CR) cases the impactor can be used in
the notch to prevent adverse flexion positioning
(Figure76). Clear any extruded cement using a curette.
Figure75
Figure76
Locking knob
Figure74
Figure73
34 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
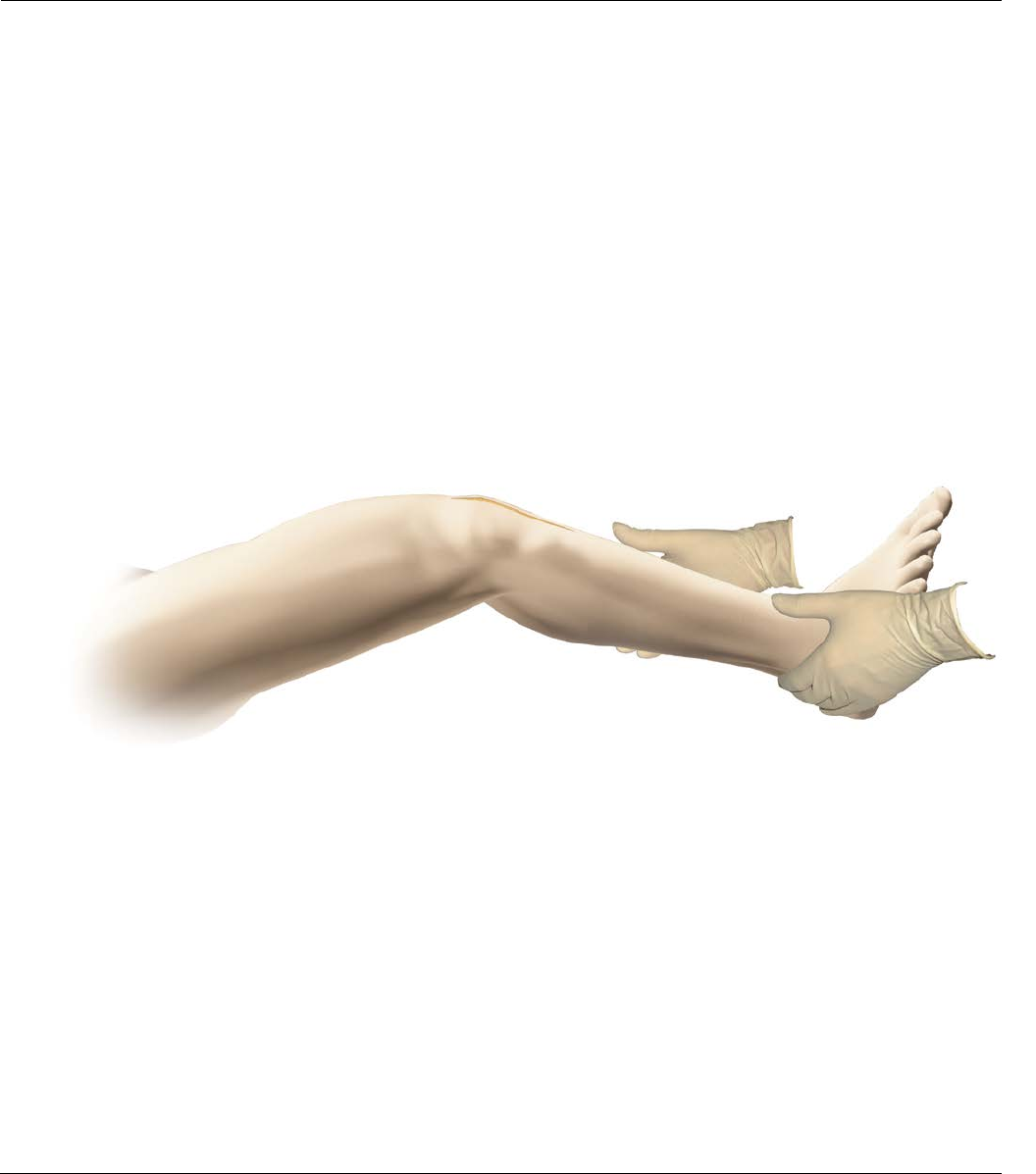
Figure77
Closure
Release the tourniquet and control bleeding
by electrocautery.
Place a closed-wound suction drain in the suprapatellar
pouch and bring out through the lateral retinaculum.
Reapproximate the fat pad, quadriceps mechanism, patella
tendon, and medial retinaculum with interrupted sutures.
Fully rotate the knee from full extension to full flexion to
confirm patellar tracking and the integrity of the capsular
closing (Figure77).
Note: the final flexion against gravity for post-
operative rehabilitation. Reapproximate
subcutaneous tissue and close the skin with sutures
or staple.

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 35
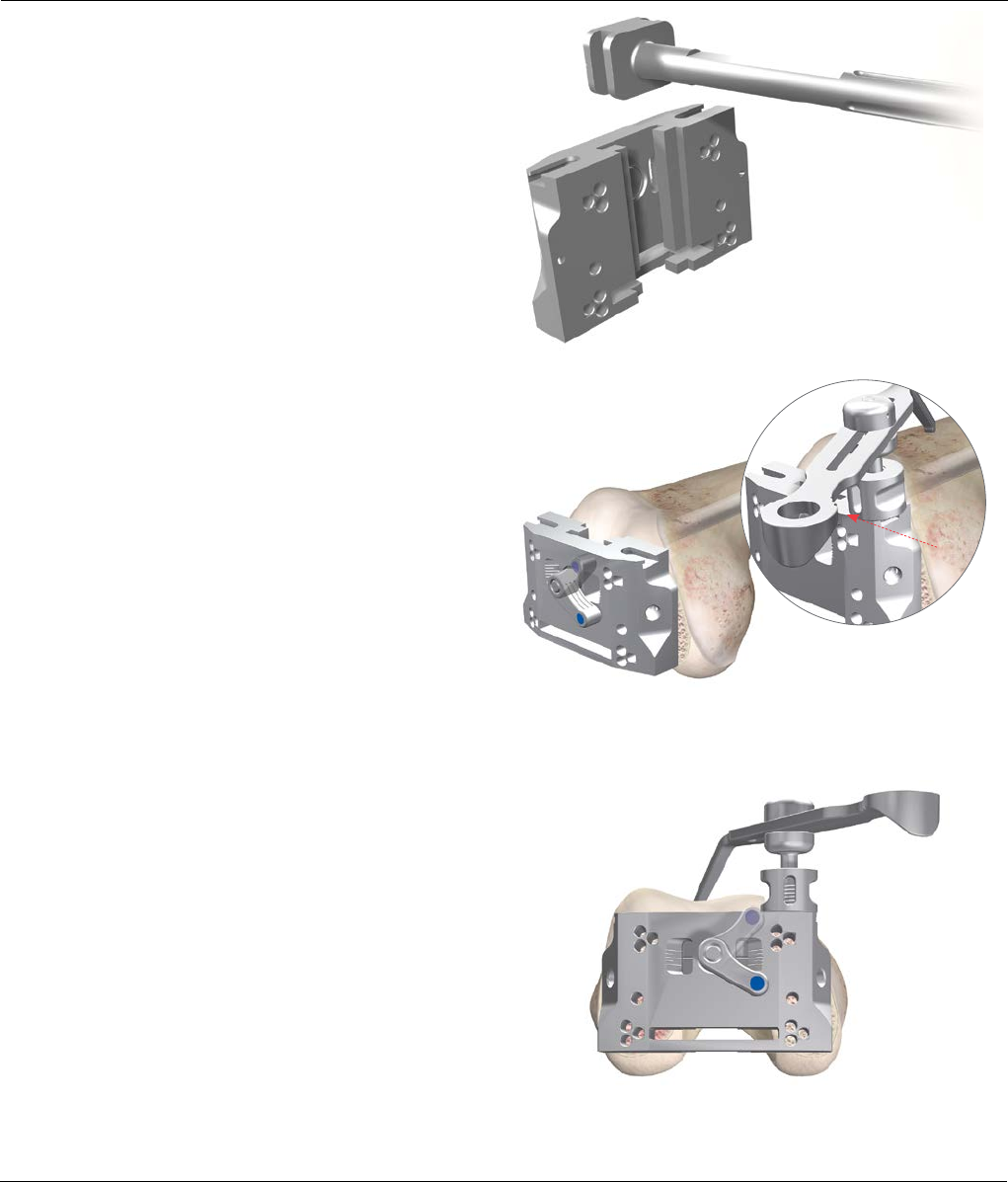
Appendix A: Fixed Bearing Modular Tibial Preparation
Femoral Trial
Attach the slap hammer or universal handle to the
femoral inserter/extractor. Position the appropriately
sized femoral trial on the inserter by depressing the two
triggers to separate the arms and push the trial against
the conforming poly surface. Release the triggers so that
the arms engage in the slots on the femur, and rotate
the handle clockwise to lock. Position the trial onto the
femur, impacting as necessary. To detach the inserter
from the femur, rotate the handle counterclockwise and
push the two triggers with thumb and index finger.
Position the femoral trial onto the femur (Figure78).
There are two options available to assess the knee
during trial reduction. One or both may be used.
1. Trial reduction with the fixed bearing tray
trial free to rotate.
• This option is useful when allowing normal internal/
external extension of the tibial components during
flexion/extension to dictate optimal placement of the
tibial tray.
• Select the trial bearing size determined during implant
planning and insert onto the tray trial. Place the knee
in approximately 90 to 100 degrees of flexion. With
the knee in full flexion and the tibia subluxed
anteriorly, attach the alignment handle to the tray trial
by retracting the lever. Position the tray trial on the
resected tibial surface, taking care to maximize the
coverage of the tray trial on the proximal tibia
(Figure79).
Figure78
Figure79

36 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Appendix A: Fixed Bearing Modular Tibial Preparation
• With the trial prostheses in place, the knee is carefully
and fully extended, noting medial and lateral stability
and overall alignment in the A/P and M/L plane.
Where there is any indication of instability, substitute
the next greater size tibial insert and repeat
reduction. Select the insert that gives the greatest
stability in flexion and extension and allows full
extension. Where there is a tendency for lateral
subluxation or patellar tilt in the absence of medial
patellar influence (thumb pressure), lateral retinacular
release is indicated.
• Adjust rotational alignment of the tibial tray with the
knee in full extension, using the alignment handle to
rotate the tray and trial insert into congruency with
the femoral trial. The appropriate position is marked
with electrocautery on the anterior tibial cortex.
(Figures 80 and 81).
2. Trial reduction with the fixed bearing tray trial
fixed in place.
• Assess the position of the tray to achieve maximal
tibial coverage (align the tibial tray handle with the
electrocautery marks, if procedure described in 1 has
been followed.) The rotation of the tray trial is usually
centered on the junction between the medial and
central one-third of the tibial tubercle. Secure the
fixed bearing keel punch impactor to the evaluation
bullet and position into the cut-out of the tray trial.
Tap down lightly to secure the tray to the proximal
tibia (Figure82).
• Carefully remove the tibial tray handle and repeat the
trial reduction step from Step 1.
Cautery
marks
Figure80
Figure82
Figure81
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 37
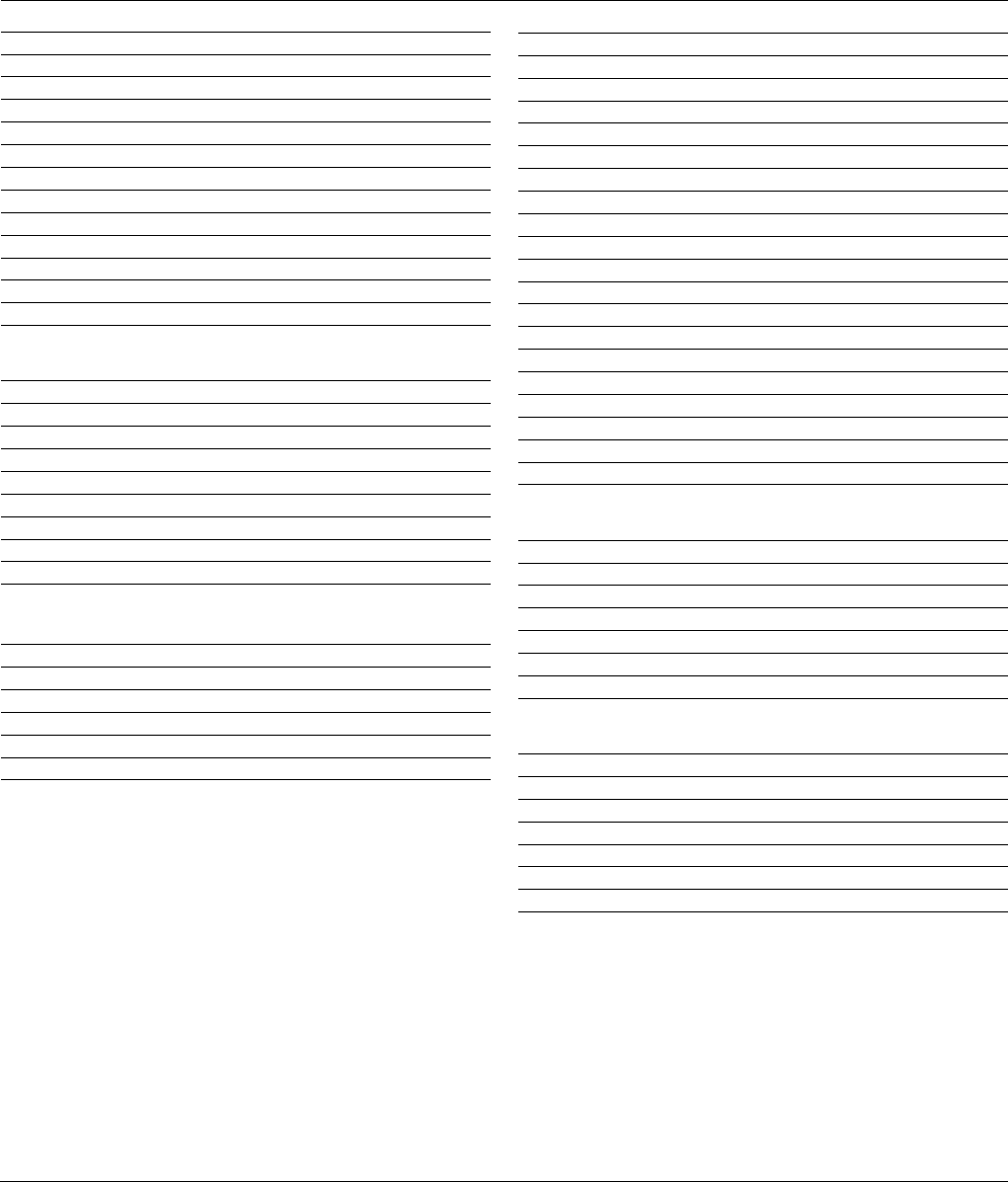
Appendix A: Fixed Bearing Modular Tibial Preparation
SIGMA Modular Total Knee System
& UHMWPE Tray:
Select the appropriate fixed bearing drill tower, drill
bushing, drill and modular keel punch system. Pin the
trial with two pins. Remove the alignment handle from
the tray trial and assemble the fixed bearing drill tower
onto the tray trial (Figure83).
Fully advance the matching drill through the drill tower
into the cancellous bone (Figure84) to the appropriate
line shown in Table below.
Note: For cemented preparation, select the
“Cemented” instruments, and for non-cemented or
line-to-line preparation, select the “Non-Cemented”
tibial instruments. The Cemented instruments will
prepare for a 1 mm cement mantle around the
periphery of the implant.
Insert the fixed bearing keel punch impactor and keel
punch through the drill tower and impact until the
shoulder of the punch is in contact with the guide
(Figure85). Remove the keel punch impactor by pressing
the side button taking care that the punch configuration
is preserved.
Figure84 Figure85
Figure83
Tray Size Line Color
1.5-3 Green
4-5 Yellow
6 Purple

38 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Appendix A: Fixed Bearing Modular Tibial Preparation
SIGMA Cruciform Keel Tray: Pin the trial with two pins.
Remove the alignment handle from the tray trial and
assemble the appropriately sized cruciform keel punch
guide to the tray trial (Figure86).
For cemented preparation, sequentially prepare the tibia
starting with the standard punch, followed by the
cemented punch. For non-cemented preparation, use
the standard punch only (Figure87).
Assemble an appropriately sized standard or cemented
keel punch onto the fixed bearing impactor handle.
Insert the punch through the guide and impact until the
shoulder of the punch is in contact with the guide. Free
the stem punch, taking care that the punch
configuration is preserved.
Figure86
Figure87

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 39
Appendix B: Tibial I.M. Jig Alignment
The entry point for the intramedullary alignment rod is a
critical starting point for accurate alignment of the
intramedullary alignment system.
In most cases, this point will be centered on the tibial
spine in both medial/lateral and anterior/ posterior
aspect. In some cases, it may be slightly eccentric.
Flex the knee maximally, insert the tibial retractor over
the posterior cruciate ligament and then sublux the tibia
anteriorly. All soft tissue is cleared from the intercondylar
area. Resect the tibial spine to the highest level of the
least affected tibial condyle.
Position the correct size fixed bearing or MBT tray trial
on the proximal tibia to aid in establishing a drill point.
Drill a hole through the tray trial to open the tibia
intramedullary canal with the I.M. step drill (Figure88).
Take care not to use the step portion of the drill. Using
the step portion of the drill will create a large diameter
hole in the tibia, which in turn creates toggle when
using the I.M. Tibial Jig.
The intramedullary rod is passed down through the
medullary canal until the isthmus is firmly engaged
(Figure89).
Figure88
Figure89
40 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Appendix B: Tibial I.M. Jig Alignment
Optional
Remove the handle and place the I.M. rotation guide
over the I.M. rod to define the correct rotational tibia
axis, referring to the condylar axis, medial 1/3 of the
tibia tubercle and the center of the ankle (Figure90).
The angle can also be checked relative to the posterior
condylar axis by moving the slider forward and rotating
it until it is aligned with the posterior condyles. The
marks on the rotation guide are in 2 degree increments
and give an indication of the angle between the
posterior condylar axis and the chosen rotation.
The rotation can then be marked through the slot on the
rotation guide. The rotation guide can then be removed.
Assemble the appropriate 3 degree SIGMA HP Handed
(left/right) or Symmetrical Tibia Cutting Block to the HP
I.M. tibial jig in line with the marked rotation (Figure91).
After the correct rotation has been marked, slide the
I.M. tibial jig over the I.M. rod and rotate the I.M. jig
until the rotation is correct (if the rotation guide was
used, use the rotation line on the jig and line it up with
the previous markings made.)
A 3 degree cutting block is recommended to
compensate for the anterior angled I.M. rod position in
the I.M. canal. This will prevent an adverse anterior slope
position. This results in an overall 0 degree position,
which is recommended for the SIGMA
Cruciate Substituting Components.
Additional posterior slope can be added through
the slope adjustment knob, when using SIGMA Cruciate
Retaining Components.
Note: The number in the window indicates the
amount of ADDITIONAL SLOPE that has been added.
Figure90
Figure91
Tibial cutting block
release button
I.M. rod lock
A/P slide
adjustment lock
Distal proximal lock
Slope adjustment
Slope scale
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 41
Appendix B: Tibial I.M. Jig Alignment
Slide the appropriate fixed or adjustable stylus in the
HP tibial cutting block slot. When assessing from the less
damaged side of the tibia plateau set the stylus to 8 mm
or 10 mm. If the stylus is placed on the more damaged
side of the tibia plateau, set the stylus to 0 mm or 2 mm
(Figure92).
Slide the total construct as close as possible towards the
proximal tibia and lock this position.
Adjust the correct degree of slope by rotating
the slope adjustment screw. For SIGMA Cruciate
Retaining Components, a 3 degree slope is
recommended. For SIGMA Cruciate Substituting
Components a 0 degree slope is recommended
as previously described. Ensure that the slope scale
reads zero.
Obtain the correct block height by unlocking the distal
proximal lock and lowering the bottom half of the block
until the stylus is resting on the desired part of the tibia.
Lock the device, by turning the distal proximal locking
screw, when the correct position has been reached.
After the height has been set, insert two pins through
the 0 mm set of holes in the block (the stylus may need
to be removed for access). The block can be securely
fixed with one extra convergent pin.
+ and –2 mm pinholes are available on the cutting
blocks to further adjust the resection level where
needed.
Check the position of the resection block with an
external alignment guide before making any cut.
Unlock the intramedullary alignment device from the
cutting block and remove the I.M. rod (Figure93).
Figure92
Figure93
42 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Appendix C: Spiked Uprod
Assemble the appropriate 0-3 degree, left/right or
symmetrical cutting block to the spiked uprod. Slide the
spiked uprod into the ankle clamp assembly.
Place the knee in 90 degrees of flexion with the tibia
translated anteriorly and stabilized. Place the ankle
clamp proximal to the malleoli and insert the larger of
the two proximal spikes in the center of the tibial
eminence to stabilize the EM alignment device. Loosen
the A/P locking knob and position the cutting block
roughly against the proximal tibia and lock the knob.
Position the cutting block at a rough level of resection
and tighten the proximal/distal-sliding knob (Figure94).
Varus / Valg us
Establish rotational alignment by aligning the tibial jig
ankle clamp parallel to the transmalleolar axis. The
midline of the tibia is approximately 3-5 mm medial to
the transaxial midline.
Translate the lower assembly medially (usually to the
second and third vertical mark) by pushing the varus/
valgus adjustment wings.
There are vertical scribe marks for reference aligning to
the middle of the talus (Figure95).
Figure95
Figure94
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 43
Appendix C: Spiked Uprod
Slope
The spiked uprod and ankle clamp are designed to
prevent an adverse anterior slope. On an average size
tibia, this guide will give approximately a 0 degree tibial
slope when the slope adjustment is translated anteriorly
until it hits the stop. In some cases, a slight amount of
slope will remain (1-2 degrees).
The angle of the tibial slope can be increased to greater
than 0 degrees should the patient have a greater natural
slope (Figure96). First, unlock the slide locking position
and then translate the tibial slope adjuster anteriorly
until the desired angle is reached. For a Cruciate
Substituting (CS) design, a 0 degree posterior slope is
recommended.
As each patient’s anatomy varies, the spiked uprod can
be used for both smaller and larger patients. The length
of the tibia influences the amount of slope when
translating the adapter anteriorly. The 0 degree default
position can be overridden by moving the slope
adjustment closer to the ankle.
On the spiked uprod 5, 6 and 7 zones are present, which
correspond to the length of the tibia. These markings
can by used to fine-tune the amount of slope.
When the spiked uprod shows a larger zone (7) marking,
this indicates that when the lower assembly is translated
7 mm anterior, it will give an additional 1 degree of
posterior slope (Figure97).
Figure96 Figure97

44 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Appendix C: Spiked Uprod
Height
Loosen the proximal/distal sliding knob, insert the
adjustable tibial stylus into the cutting block and adjust
to the correct level of resection.
When assessing from the less damaged side of the tibial
plateau, set the stylus to 8 mm or 10 mm. If the stylus is
placed on the more damaged side of the tibial plateau,
set the stylus to 0 mm or 2 mm. Adjustment of resection
height on the stylus should be done outside the joint
space before locating the stylus in the cutting block.
If planning to resect through the slot, position the foot
of the tibial stylus marked “slotted” into the slot of the
tibial cutting block (Figure98). If planning to resect on
top of the cutting block, place the foot marked “non-
slotted” into the cutting slot. Drop the block and stylus
assembly so that the stylus touches the desired point on
the tibia. Care should be taken with severe valgus
deformity, not to over resect the tibia.
Tibial Resection
After the height has been set, lock the proximal/ distal
sliding knob and pin the block through the 0 mm set of
holes (the stylus may need to be removed for access).
+/-2 mm pinholes are available on the resection blocks
to further adjust the resection level where needed.
The block can be securely fixed with one extra
convergent pin.
Spiked Uprod Removal
Loosen the A/P locking knob. Press the cutting block
release button and translate the spiked uprod anterior to
disengage from the cutting block.
Connect the slap hammer to the top of the spiked uprod
and disengage the spikes from the proximal tibia.
Remove the tibial jig and perform the appropriate
resection (Figure99).
Figure98
Figure99
Non-slotted stylus foot
Press release trigger to
disengage the tibial
cutting block
After disengaging from
the tibial block, use the
slap hammer to
disengage the spikes
from the proximal tibia
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 45
Appendix D: Femoral Finishing
Resect the anterior cortex using the balanced femoral
cutting block. Remove the pins and the resected bone
(Figure100).
Select the appropriate sized SIGMA or SIGMA RP-F
Femoral Finishing Block and position the block on the
resected anterior and distal surfaces of the femur.
Note: The posterior aspect of the block corresponds
exactly to the M/L dimension of the final implant
and can be used to visualize the correct M/L
position. In addition, the anterior flange on the
cutting block represents the medial flange of the
implant, with the proximal anterior protrusions
representing the lateral implant flange (Figure 101).
Pin the block in place through the fixation pinholes with
at least three threaded pins before any bone cuts are
made. Perform the final resections: posterior resection,
notch cut, anterior and posterior chamfer resections
(Figure101).
Figure100
Figure101
Lateral Implant position
Medial Implant
position
46 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Appendix E: Femoral Finishing (Optional)
Alternatively use the appropriate SIGMA or SIGMA RP-F
A/P Cutting Block to perform the 4-in-1 cuts. To position
this block, pin the balanced block through the pin holes
located in the middle of the balanced block, (Figure102)
then remove the pins.
Position the appropriate SIGMA or SIGMA RP-F Chamfer
Block in the pre-drilled medial and lateral holes. Secure
and stabilize the SIGMA or SIGMA RP-F Classic A/P
Chamfer Block by drilling a headed drill pin through the
central pinhole. Alternatively, medial and lateral pins can
be inserted into the convergent pin holes. Place
retractors to protect the MCL medially and the popliteal
tendon laterally. After securely fixing the femoral
chamfer block, resect the anterior cortex, the posterior
condyles and the anterior/posterior chamfers
(Figure103).
Note: On both the classic A/P chamfer block
and the femoral finishing block, the RP-F and
standard SIGMA Blocks look very similar. To easily
identify them, the RP-F block has the letters “RP-F”
on the distal face, and the area above the posterior
cut has several grooves.
When using a stabilized SIGMA or SIGMA RP-F Instrument,
select and attach the appropriate femoral notch guide. The
SIGMA RP-F Instruments and standard SIGMA Notch
Guides look very similar. Care should be taken not to
confuse the blocks as this will result in under-or-over
resection of the box.
Note: The RP-F guide can be identified through the
letters “RP-F” on the anterior face, and a series of
grooves along the notch distal anterior corner.
Position the notch guide on the resected anterior and
distal surfaces of the femur. Pin the block in place
through the fixation pin holes with at least three pins
before any bone cuts are made. Make notch cuts with a
small saw blade (Figure104).
Figure103
Figure102
Figure104
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 47
Ordering Information
Tibia Resection
9505-01-228 HP EM Tibial Jig Uprod
9505-01-229 HP EM Tibial Jig Ankle Clamp
9505-01-202 HP I.M. Tibia Rotation Guide
9505-01-203 HP I.M. Tibia Jig
9505-01-204 SIGMA HP 0 degrees Symmetrical Cut Block
9505-01-222 SIGMA HP 0 degrees Left Cut Block
9505-01-223 SIGMA HP 0 degrees Right Cut Block
9505-01-205 SIGMA HP 3 degrees Symmetrical Cut Block
9505-01-224 SIGMA HP 3 degrees Left Cut Block
9505-01-225 SIGMA HP 3 degrees RIght Cut Block
9505-01-209 SIGMA HP Adj Tibial Stylus
9505-01-230 HP EM Tibial Jig Spiked Uprod
9505-01-164 SIGMA HP Slot Stylus 0/2 mm
9505-01-167 SIGMA HP Nonslotted Stylus 0/2 mm
9505-01-211 SIGMA HP Slotted Stylus 8/10 mm
9505-01-213 SIGMA HP Nonslotted Stylus 8/10 mm
Femoral Resection
96-6120 SP2 I.M. Rod 400 mm
9505-01-239 SIGMA HP Revision Distal Femoral Cutting Block
99-2011 I.M. Rod Handle
96-6121 I.M. Rod 300 mm
9505-02-079 HP Step I.M. Reamer
9505-01-234 SIGMA HP Distal Femoral Align Guide
9505-01-235 SIGMA HP Distal Femoral Resect Guide
9505-01-238 SIGMA HP Distal Femoral Connector
9505-01-236 SIGMA HP Distal Femoral Block
9505-01-307 HP Alignment Tower
9505-01-207 HP Alignment Rod
96-6530 Reference Guide
Femoral Sizing
9505-01-263 HP Fixed Reference Femoral Sizer
9505-01-277 HP Classic Posterior Up Femoral Sizer
9505-01-272 HP Classic Anterior Down Femoral Sizer
Primary Balanced Femoral Resection
9505-02-126 SIGMA HP Balanced A/P Block Size 1.5
9505-02-127 SIGMA HP Balanced A/P Block Size 2
9505-02-128 SIGMA HP Balanced A/P Block Size 2.5
9505-02-129 SIGMA HP Balanced A/P Block Size 3
9505-02-130 SIGMA HP Balanced A/P Block Size 4
9505-02-131 SIGMA HP Balanced A/P Block Size 5
9505-02-132 SIGMA HP Balanced A/P Block Size 6
9505-02-141 SIGMA HP Balanced A/P Block Stylus
9505-02-142 SIGMA HP Balanced I.M. Rod 5 Degrees
9505-02-143 SIGMA HP Balanced I.M. Rod 3 Degrees
9505-02-144 SIGMA HP Balanced RP Femoral Positioner
9505-02-145 SIGMA HP Balanced FB Femoral Positioner
9505-02-146 SIGMA HP Balanced Femoral Positioner Shim 10 mm
9505-02-147 SIGMA HP Balanced Femoral Positioner Shim 12.5 mm
9505-02-148 SIGMA HP Balanced Femoral Positioner Shim 15 mm
9505-02-149 SIGMA HP Balanced Femoral Positioner Shim 17.5 mm
96-6147 Removable Handles (Pack of 2)
9505-02-152 SIGMA HP Fixed Ref AP Block Size 1.5
9505-02-153 SIGMA HP Fixed Ref AP Block Size 2
9505-02-154 SIGMA HP Fixed Ref AP Block Size 2.5
9505-02-155 SIGMA HP Fixed Ref AP Block Size 3
9505-02-156 SIGMA HP Fixed Ref AP Block Size 4
9505-02-157 SIGMA HP Fixed Ref AP Block Size 5
9505-02-158 SIGMA HP Fixed Ref AP Block Size 6
9505-01-000 SP2 MI Fem Notch Guide Size 1.5
9505-01-001 SP2 MI Fem Notch Guide Size 2
9505-01-002 SP2 MI Fem Notch Guide Size 2.5
9505-01-003 SP2 MI Fem Notch Guide Size 3
9505-01-004 SP2 MI Fem Notch Guide Size 4
9505-01-005 SP2 MI Fem Notch Guide Size 5
9505-01-006 SP2 MI Fem Notch Guide Size 6
Balanced Femoral Resection-Additional Options
9505-01-279 SIGMA HP Femoral Finish Block Size 1.5
9505-01-280 SIGMA HP Femoral Finish Block Size 2
9505-01-281 SIGMA HP Femoral Finish Block Size 2.5
9505-01-282 SIGMA HP Femoral Finish Block Size 3
9505-01-283 SIGMA HP Femoral Finish Block Size 4
9505-01-284 SIGMA HP Femoral Finish Block Size 5
9505-01-285 SIGMA HP Femoral Finish Block Size 6
9505-02-133 RP-F HP Balanced A/P Block Size 1
9505-02-134 RP-F HP Balanced A/P Block Size 1.5
9505-02-135 RP-F HP Balanced A/P Block Size 2
9505-02-136 RP-F HP Balanced A/P Block Size 2.5
9505-02-137 RP-F HP Balanced A/P Block Size 3
9505-02-138 RP-F HP Balanced A/P Block Size 4
9505-02-139 RP-F HP Balanced A/P Block Size 5
9505-02-140 RP-F HP Balanced A/P Block Size 6
9505-01-286 SIGMA RP-F HP Femoral Finish Block Size 1
9505-01-287 SIGMA RP-F HP Femoral Finish Block Size 1.5
9505-01-288 SIGMA RP-F HP Femoral Finish Block Size 2
9505-01-289 SIGMA RP-F HP Femoral Finish Block Size 2.5
9505-01-290 SIGMA RP-F HP Femoral Finish Block Size 3
Balanced Femoral Resection-Additional Options
9505-01-291 SIGMA RP-F HP Femoral Finish Block Size 4
9505-01-292 SIGMA RP-F HP Femoral Finish Block Size 5
9505-01-293 SIGMA RP-F HP Femoral Finish Block Size 6
96-6278 PFC Chamfer Guides Size 1.5
96-6272 PFC Chamfer Guides Size 2
96-6279 PFC Chamfer Guides Size 2.5
96-6273 PFC Chamfer Guides Size 3
96-6274 PFC Chamfer Guides Size 4
96-6275 PFC Chamfer Guides Size 5
96-6277 PFC Chamfer Guides Size 6
48 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Ordering Information
Fixed Bearing Preparation
9505-02-040 SIGMA HP FBT Tray Trial Size 1.5
9505-02-041 SIGMA HP FBT Tray Trial Size 2
9505-02-042 SIGMA HP FBT Tray Trial Size 2.5
9505-02-043 SIGMA HP FBT Tray Trial Size 3
9505-02-044 SIGMA HP FBT Tray Trial Size 4
9505-02-045 SIGMA HP FBT Tray Trial Size 5
9505-02-046 SIGMA HP FBT Tray Trial Size 6
9505-02-053 SIGMA HP FBT Evaluation Bullet Size 1.5-3
9505-02-054 SIGMA HP FBT Evaluation Bullet Size 4-6
9505-02-055 SIGMA HP FBT Keel Punch Impact
9505-02-060 SIGMA HP FBT Drill Tower
2178-30-123 MBT Tray Fixation Pins
9505-02-028 HP Tibial Tray Handle
9505-02-068 FBT Modular Drill Stop
Fixed Bearing Modular Tray Preparation
9505-02-047 HP FBT Cemented Keel Punch Size 1.5-3
9505-02-048 HP FBT Cemented Keel Punch Size 4-5
9505-02-049 HP FBT Cemented Keel Punch Size 6
9505-02-056 SIGMA HP FBT Cemented Drill Size 1.5-3
9505-02-057 SIGMA HP FBT Cemented Drill Size 4-6
9505-02-050 HP FBT Non Cemented Keeled Punch Size 1.5-3
9505-02-051 HP FBT Non Cemented Keeled Punch Size 4-5
9505-02-058 HP FBT Non Cemented Drill Size 1.5-3
9505-02-059 HP FBT Non Cemented Drill Size 4-6
9505-02-052 HP FBT Non Cemented Keeled Punch Size 6
Fixed Bearing Standard Tray Preparation
9505-02-061 HP FBT Standard Tibial Punch Guide Size 1.5-4
9505-02-062 HP FBT Standard Tibial Punch Guide Size 5-6
9505-02-063 HP FBT Standard Tibial Punch Size 1.5-2
9505-02-064 HP FBT Standard Tibial Punch Size 2.5-4
9505-02-065 HP FBT Standard Tibial Punch Size 5-6
9505-02-066 HP FBT Standard Cemented Tibial Punch Size 1.5-2
9505-02-067 HP FBT Standard Cemented Tibial Punch Size 2.5-6
MBT Preparation
9505-02-000 HP MBT Tray Trial Size 1
9505-02-001 HP MBT Tray Trial Size 1.5
9505-02-002 HP MBT Tray Trial Size 2
9505-02-003 HP MBT Tray Trial Size 2.5
9505-02-004 HP MBT Tray Trial Size 3
9505-02-006 HP MBT Tray Trial Size 4
9505-02-007 HP MBT Tray Trial Size 5
9505-02-008 HP MBT Tray Trial Size 6
9505-02-009 HP MBT Tray Trial Size 7
9505-02-022 HP MBT Spiked Evaluation Bullet Size 1-3
9505-02-023 HP MBT Spiked Evaluation Bullet Size 4-7
9505-02-099 HP MBT Evaluation Bullet Size 1-3
9505-02-098 HP MBT Evaluation Bullet Size 4-7
9505-02-027 HP MBT Drill Tower
9505-02-024 HP MBT Keel Punch Impact
2178-30-123 MBT Tray Fixation Pins
9505-02-028 HP Tibial Tray Handle
9505-02-029 MBT Modular Drill Stop
9505-02-038 MBT Central Stem Punch
2178-30-137 MBT RP Trial Button
2178-30-121 MBT RP Plateau Trial Post
MBT Keeled Preparation
9505-02-025 HP MBT Cemented Central Drill
9505-02-010 HP MBT Cemented Keel Punch Size 1-1.5
9505-02-011 HP MBT Cemented Keel Punch Size 2-3
9505-02-012 HP MBT Cemented Keel Punch Size 4-7
9505-02-026 HP MBT Non Cemented Central Drill
9505-02-013 HP MBT Non Cemented Keeled Punch Size 1-1.5
9505-02-014 HP MBT Non Cemented Keeled Punch Size 2-3
9505-02-015 HP MBT Non Cemented Keeled Punch Size 4-7
MBT Non Keeled Preparation
9505-02-025 HP MBT Cemented Central Drill
9505-02-016 HP MBT Cemented Punch Size 1-1.5
9505-02-017 HP MBT Cemented Punch Size 2-3
9505-02-018 HP MBT Cemented Punch Size 4-7
9505-02-026 HP MBT Non Cemented Central Drill
9505-02-019 HP MBT Non Cemented Punch Size 1-1.5
9505-02-020 HP MBT Non Cemented Punch Size 2-3
9505-02-021 HP MBT Non Cemented Punch Size 4-7
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 49
Ordering Information
Femoral Trials
96-1007 SIGMA Femur Cruciate Retaining Femur Trial Size 1.5 Left
96-1002 SIGMA Femur Cruciate Retaining Femur Trial Size 2 Left
96-1008 SIGMA Femur Cruciate Retaining Femur Trial Size 2.5 Left
96-1003 SIGMA Femur Cruciate Retaining Femur Trial Size 3 Left
96-1004 SIGMA Femur Cruciate Retaining Femur Trial Size 4 Left
96-1005 SIGMA Femur Cruciate Retaining Femur Trial Size 5 Left
96-1006 SIGMA Femur Cruciate Retaining Femur Trial Size 6 Left
96-1017 SIGMA Femur Cruciate Retaining Femur Trial Size 1.5 Right
96-1012 SIGMA Femur Cruciate Retaining Femur Trial Size 2 Right
96-1018 SIGMA Femur Cruciate Retaining Femur Trial Size 2.5 Right
96-1013 SIGMA Femur Cruciate Retaining Femur Trial Size 3 Right
96-1014 SIGMA Femur Cruciate Retaining Femur Trial Size 4 Right
96-1015 SIGMA Femur Cruciate Retaining Femur Trial Size 5 Right
96-1016 SIGMA Femur Cruciate Retaining Femur Trial Size 6 Right
96-6202 Distal Femoral Lug Drill W/Hudson End
96-1047 SIGMA Femur Cruciate Substituting Box Trial Size 1.5
96-1042 SIGMA Femur Cruciate Substituting Box Trial Size 2
96-1048 SIGMA Femur Cruciate Substituting Box Trial Size 2.5
96-1043 SIGMA Femur Cruciate Substituting Box Trial Size 3
96-1044 SIGMA Femur Cruciate Substituting Box Trial Size 4
96-1045 SIGMA Femur Cruciate Substituting Box Trial Size 5
96-1046 SIGMA Femur Cruciate Substituting Box Trial Size 6
96-6295 SP2 Femur Box Trial Screwdriver
2960-00-400 SIGMA CR Femur Trial Size 4N Left
2960-01-400 SIGMA CR Femur Trial Size 4N Right
RP-F Femoral Trials
95-4210 RP-F Trial Femur Size 1 Left
95-4211 RP-F Trial Femur Size 1.5 Left
95-4212 RP-F Trial Femur Size 2 Left
95-4213 RP-F Trial Femur Size 2.5 Left
95-4214 RP-F Trial Femur Size 3 Left
95-4215 RP-F Trial Femur Size 4 Left
95-4216 RP-F Trial Femur Size 5 Left
95-4217 RP-F Trial Femur Size 6 Left
95-4220 RP-F Trial Femur Size 1 Right
95-4221 RP-F Trial Femur Size 1.5 Right
95-4222 RP-F Trial Femur Size 2 Right
95-4223 RP-F Trial Femur Size 2.5 Right
95-4224 RP-F Trial Femur Size 3 Right
95-4225 RP-F Trial Femur Size 4 Right
95-4226 RP-F Trial Femur Size 5 Right
95-4227 RP-F Trial Femur Size 6 Right
Fixed Bearing Insert Trials
Posterior Lipped
96-1210 SIGMA PLI Tibial Insert Trial Size 1.5 8 mm
96-1211 SIGMA PLI Tibial Insert Trial Size 1.5 10 mm
96-1212 SIGMA PLI Tibial Insert Trial Size 1.5 12.5 mm
96-1213 SIGMA PLI Tibial Insert Trial Size 1.5 15 mm
96-1214 SIGMA PLI Tibial Insert Trial Size 1.5 17.5 mm
96-1215 SIGMA PLI Tibial Insert Trial Size 1.5 20 mm
96-1220 SIGMA PLI Tibial Insert Trial Size 2 8 mm
96-1221 SIGMA PLI Tibial Insert Trial Size 2 10 mm
96-1222 SIGMA PLI Tibial Insert Trial Size 2 12.5 mm
96-1223 SIGMA PLI Tibial Insert Trial Size 2 15 mm
96-1224 SIGMA PLI Tibial Insert Trial Size 2 17.5 mm
96-1225 SIGMA PLI Tibial Insert Trial Size 2 20 mm
96-1230 SIGMA PLI Tibial Insert Trial Size 2.5 8 mm
96-1231 SIGMA PLI Tibial Insert Trial Size 2.5 10 mm
96-1232 SIGMA PLI Tibial Insert Trial Size 2.5 12.5 mm
96-1233 SIGMA PLI Tibial Insert Trial Size 2.5 15 mm
96-1234 SIGMA PLI Tibial Insert Trial Size 2.5 17.5 mm
96-1235 SIGMA PLI Tibial Insert Trial Size 2.5 20 mm
96-1240 SIGMA PLI Tibial Insert Trial Size 3 8 mm
96-1241 SIGMA PLI Tibial Insert Trial Size 3 10 mm
96-1242 SIGMA PLI Tibial Insert Trial Size 3 12.5 mm
96-1243 SIGMA PLI Tibial Insert Trial Size 3 15 mm
96-1244 SIGMA PLI Tibial Insert Trial Size 3 17.5 mm
96-1245 SIGMA PLI Tibial Insert Trial Size 3 20 mm
96-1250 SIGMA PLI Tibial Insert Trial Size 4 8 mm
96-1251 SIGMA PLI Tibial Insert Trial Size 4 10 mm
96-1252 SIGMA PLI Tibial Insert Trial Size 4 12.5 mm
96-1253 SIGMA PLI Tibial Insert Trial Size 4 15 mm
96-1254 SIGMA PLI Tibial Insert Trial Size 4 17.5 mm
96-1255 SIGMA PLI Tibial Insert Trial Size 4 20 mm
96-1260 SIGMA PLI Tibial Insert Trial Size 5 8 mm
96-1261 SIGMA PLI Tibial Insert Trial Size 5 10 mm
96-1262 SIGMA PLI Tibial Insert Trial Size 5 12.5 mm
96-1263 SIGMA PLI Tibial Insert Trial Size 5 15 mm
96-1264 SIGMA PLI Tibial Insert Trial Size 5 17.5 mm
96-1265 SIGMA PLI Tibial Insert Trial Size 5 20 mm
96-1270 SIGMA PLI Tibial Insert Trial Size 6 8 mm
96-1271 SIGMA PLI Tibial Insert Trial Size 6 10 mm
96-1272 SIGMA PLI Tibial Insert Trial Size 6 12.5 mm
96-1273 SIGMA PLI Tibial Insert Trial Size 6 15 mm
96-1274 SIGMA PLI Tibial Insert Trial Size 6 17.5 mm
96-1275 SIGMA PLI Tibial Insert Trial Size 6 20 mm
50 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Curved
96-1320 SIGMA Curved Tibial Insert Trial Size 1.5 8 mm
96-1321 SIGMA Curved Tibial Insert Trial Size 1.5 10 mm
96-1322 SIGMA Curved Tibial Insert Trial Size 1.5 12.5 mm
96-1323 SIGMA Curved Tibial Insert Trial Size 1.5 15 mm
96-1324 SIGMA Curved Tibial Insert Trial Size 1.5 17.5 mm
96-1325 SIGMA Curved Tibial Insert Trial Size 1.5 20 mm
96-1330 SIGMA Curved Tibial Insert Trial Size 2 8 mm
96-1331 SIGMA Curved Tibial Insert Trial Size 2 10 mm
96-1332 SIGMA Curved Tibial Insert Trial Size 2 12.5 mm
96-1333 SIGMA Curved Tibial Insert Trial Size 2 15 mm
96-1334 SIGMA Curved Tibial Insert Trial Size 2 17.5 mm
96-1335 SIGMA Curved Tibial Insert Trial Size 2 20 mm
96-1340 SIGMA Curved Tibial Insert Trial Size 2.5 8 mm
96-1341 SIGMA Curved Tibial Insert Trial Size 2.5 10 mm
96-1342 SIGMA Curved Tibial Insert Trial Size 2.5 12.5 mm
96-1343 SIGMA Curved Tibial Insert Trial Size 2.5 15 mm
96-1344 SIGMA Curved Tibial Insert Trial Size 2.5 17.5 mm
96-1345 SIGMA Curved Tibial Insert Trial Size 2.5 20 mm
96-1350 SIGMA Curved Tibial Insert Trial Size 3 8 mm
96-1351 SIGMA Curved Tibial Insert Trial Size 3 10 mm
96-1352 SIGMA Curved Tibial Insert Trial Size 3 12.5 mm
96-1353 SIGMA Curved Tibial Insert Trial Size 3 15 mm
96-1354 SIGMA Curved Tibial Insert Trial Size 3 17.5 mm
96-1355 SIGMA Curved Tibial Insert Trial Size 3 20 mm
96-1360 SIGMA Curved Tibial Insert Trial Size 4 8 mm
96-1361 SIGMA Curved Tibial Insert Trial Size 4 10 mm
96-1362 SIGMA Curved Tibial Insert Trial Size 4 12.5 mm
96-1363 SIGMA Curved Tibial Insert Trial Size 4 15 mm
96-1364 SIGMA Curved Tibial Insert Trial Size 4 17.5 mm
96-1365 SIGMA Curved Tibial Insert Trial Size 4 20 mm
96-1370 SIGMA Curved Tibial Insert Trial Size 5 8 mm
96-1371 SIGMA Curved Tibial Insert Trial Size 5 10 mm
96-1372 SIGMA Curved Tibial Insert Trial Size 5 12.5 mm
96-1373 SIGMA Curved Tibial Insert Trial Size 5 15 mm
96-1374 SIGMA Curved Tibial Insert Trial Size 5 17.5 mm
96-1375 SIGMA Curved Tibial Insert Trial Size 5 20 mm
96-1380 SIGMA Curved Tibial Insert Trial Size 6 8 mm
96-1381 SIGMA Curved Tibial Insert Trial Size 6 10 mm
96-1382 SIGMA Curved Tibial Insert Trial Size 6 12.5 mm
96-1383 SIGMA Curved Tibial Insert Trial Size 6 15 mm
96-1384 SIGMA Curved Tibial Insert Trial Size 6 17.5 mm
96-1385 SIGMA Curved Tibial Insert Trial Size 6 20 mm
Ordering Information
Curved Plus
97-2320 SIGMA Curved+ Insert Trial 1.5 8 mm
97-2321 SIGMA Curved+ Insert Trial 1.5 10 mm
97-2322 SIGMA Curved+ Insert Trial 1.5 12.5 mm
97-2323 SIGMA Curved+ Insert Trial 1.5 15 mm
97-2324 SIGMA Curved+ Insert Trial 1.5 17.5 mm
97-2330 SIGMA Curved+ Insert Trial 2 8 mm
97-2331 SIGMA Curved+ Insert Trial 2 10 mm
97-2332 SIGMA Curved+ Insert Trial 2 12.5 mm
97-2333 SIGMA Curved+ Insert Trial 2 15 mm
97-2334 SIGMA Curved+ Insert Trial 2 17.5 mm
97-2335 SIGMA Curved+ Insert Trial 2 20 mm
97-2340 SIGMA Curved+ Insert Trial 2.5 8 mm
97-2341 SIGMA Curved+ Insert Trial 2.5 10 mm
97-2342 SIGMA Curved+ Insert Trial 2.5 12.5 mm
97-2343 SIGMA Curved+ Insert Trial 2.5 15 mm
97-2344 SIGMA Curved+ Insert Trial 2.5 17.5 mm
97-2345 SIGMA Curved+ Insert Trial 2.5 20 mm
97-2350 SIGMA Curved+ Insert Trial 3 8 mm
97-2351 SIGMA Curved+ Insert Trial 3 10 mm
97-2352 SIGMA Curved+ Insert Trial 3 12.5 mm
97-2353 SIGMA Curved+ Insert Trial 3 15 mm
97-2354 SIGMA Curved+ Insert Trial 3 17.5 mm
97-2355 SIGMA Curved+ Insert Trial 3 20 mm
97-2360 SIGMA Curved+ Insert Trial 4 8 mm
97-2361 SIGMA Curved+ Insert Trial 4 10 mm
97-2362 SIGMA Curved+ Insert Trial 4 12.5 mm
97-2363 SIGMA Curved+ Insert Trial 4 15 mm
97-2364 SIGMA Curved+ Insert Trial 4 17.5 mm
97-2365 SIGMA Curved+ Insert Trial 4 20 mm
97-2370 SIGMA Curved+ Insert Trial 5 8 mm
97-2371 SIGMA Curved+ Insert Trial 5 10 mm
97-2372 SIGMA Curved+ Insert Trial 5 12.5 mm
97-2373 SIGMA Curved+ Insert Trial 5 15 mm
97-2374 SIGMA Curved+ Insert Trial 5 17.5 mm
97-2375 SIGMA Curved+ Insert Trial 5 20 mm
97-2380 SIGMA Curved+ Insert Trial 6 8 mm
97-2381 SIGMA Curved+ Insert Trial 6 10 mm
97-2382 SIGMA Curved+ Insert Trial 6 12.5 mm
97-2383 SIGMA Curved+ Insert Trial 6 15 mm
97-2384 SIGMA Curved+ Insert Trial 6 17.5 mm
97-2385 SIGMA Curved+ Insert Trial 6 20 mm
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 51
Ordering Information
Stabilized
96-1410 SIGMA Stabilized Tibial Insert Trial Size 1.5 8 mm
96-1411 SIGMA Stabilized Tibial Insert Trial Size 1.5 10 mm
96-1412 SIGMA Stabilized Tibial Insert Trial Size 1.5 12.5 mm
96-1413 SIGMA Stabilized Tibial Insert Trial Size 1.5 15 mm
96-1414 SIGMA Stabilized Tibial Insert Trial Size 1.5 17.5 mm
96-1420 SIGMA Stabilized Tibial Insert Trial Size 2 8 mm
96-1421 SIGMA Stabilized Tibial Insert Trial Size 2 10 mm
96-1422 SIGMA Stabilized Tibial Insert Trial Size 2 12.5 mm
96-1423 SIGMA Stabilized Tibial Insert Trial Size 2 15 mm
96-1424 SIGMA Stabilized Tibial Insert Trial Size 2 17.5 mm
96-1425 SIGMA Stabilized Tibial Insert Trial Size 2 20 mm
96-1426 SIGMA Stabilized Tibial Insert Trial Size 2 22.5 mm
96-1427 SIGMA Stabilized Tibial Insert Trial Size 2 25 mm
96-1430 SIGMA Stabilized Tibial Insert Trial Size 2.5 8 mm
96-1431 SIGMA Stabilized Tibial Insert Trial Size 2.5 10 mm
96-1432 SIGMA Stabilized Tibial Insert Trial Size 2.5 12.5 mm
96-1433 SIGMA Stabilized Tibial Insert Trial Size 2.5 15 mm
96-1434 SIGMA Stabilized Tibial Insert Trial Size 2.5 17.5 mm
96-1435 SIGMA Stabilized Tibial Insert Trial Size 2.5 20 mm
96-1436 SIGMA Stabilized Tibial Insert Trial Size 2.5 22.5 mm
96-1437 SIGMA Stabilized Tibial Insert Trial Size 2.5 25 mm
96-1440 SIGMA Stabilized Tibial Insert Trial Size 3 8 mm
96-1441 SIGMA Stabilized Tibial Insert Trial Size 3 10 mm
96-1442 SIGMA Stabilized Tibial Insert Trial Size 3 12.5 mm
96-1443 SIGMA Stabilized Tibial Insert Trial Size 3 15 mm
96-1444 SIGMA Stabilized Tibial Insert Trial Size 3 17.5 mm
96-1445 SIGMA Stabilized Tibial Insert Trial Size 3 20 mm
96-1446 SIGMA Stabilized Tibial Insert Trial Size 3 22.5 mm
96-1447 SIGMA Stabilized Tibial Insert Trial Size 3 25 mm
96-1450 SIGMA Stabilized Tibial Insert Trial Size 4 8 mm
96-1451 SIGMA Stabilized Tibial Insert Trial Size 4 10 mm
96-1452 SIGMA Stabilized Tibial Insert Trial Size 4 12.5 mm
96-1453 SIGMA Stabilized Tibial Insert Trial Size 4 15 mm
96-1454 SIGMA Stabilized Tibial Insert Trial Size 4 17.5 mm
96-1455 SIGMA Stabilized Tibial Insert Trial Size 4 20 mm
96-1456 SIGMA Stabilized Tibial Insert Trial Size 4 22.5 mm
96-1457 SIGMA Stabilized Tibial Insert Trial Size 4 25 mm
96-1460 SIGMA Stabilized Tibial Insert Trial Size 5 8 mm
96-1461 SIGMA Stabilized Tibial Insert Trial Size 5 10 mm
96-1462 SIGMA Stabilized Tibial Insert Trial Size 5 12.5 mm
961463 SIGMA Stabilized Tibial Insert Trial Size 5 15 mm
96-1464 SIGMA Stabilized Tibial Insert Trial Size 5 17.5 mm
96-1465 SIGMA Stabilized Tibial Insert Trial Size 5 20 mm
96-1466 SIGMA Stabilized Tibial Insert Trial Size 5 22.5 mm
96-1467 SIGMA Stabilized Tibial Insert Trial Size 5 25 mm
96-1470 SIGMA Stabilized Tibial Insert Trial Size 6 8 mm
96-1471 SIGMA Stabilized Tibial Insert Trial Size 6 10 mm
96-1472 SIGMA Stabilized Tibial Insert Trial Size 6 12.5 mm
96-1473 SIGMA Stabilized Tibial Insert Trial Size 6 15 mm
96-1474 SIGMA Stabilized Tibial Insert Trial Size 6 17.5 mm
96-1475 SIGMA Stabilized Tibial Insert Trial Size 6 20 mm
96-1476 SIGMA Stabilized Tibial Insert Trial Size 6 22.5 mm
96-1477 SIGMA Stabilized Tibial Insert Trial Size 6 25 mm
Mobile Bearing Insert Trials
RP Curved
97-3001 SIGMA RP Curved Tibial Insert Trial Size 1.5 10 mm
97-3002 SIGMA RP Curved Tibial Insert Trial Size 1.5 12.5 mm
97-3003 SIGMA RP Curved Tibial Insert Trial Size 1.5 15.0 mm
97-3004 SIGMA RP Curved Tibial Insert Trial Size 1.5 17.5 mm
96-3011 SIGMA RP Curved Tibial Insert Trial Size 2 10 mm
96-3012 SIGMA RP Curved Tibial Insert Trial Size 2 12.5 mm
96-3013 SIGMA RP Curved Tibial Insert Trial Size 2 15.0 mm
96-3014 SIGMA RP Curved Tibial Insert Trial Size 2 17.5 mm
96-3021 SIGMA RP Curved Tibial Insert Trial Size 2.5 10 mm
96-3022 SIGMA RP Curved Tibial Insert Trial Size 2.5 12.5 mm
96-3023 SIGMA RP Curved Tibial Insert Trial Size 2.5 15.0 mm
96-3024 SIGMA RP Curved Tibial Insert Trial Size 2.5 17.5 mm
96-3031 SIGMA RP Curved Tibial Insert Trial Size 3 10 mm
96-3032 SIGMA RP Curved Tibial Insert Trial Size 3 12.5 mm
96-3033 SIGMA RP Curved Tibial Insert Trial Size 3 15.0 mm
96-3034 SIGMA RP Curved Tibial Insert Trial Size 3 17.5 mm
96-3041 SIGMA RP Curved Tibial Insert Trial Size 4 10 mm
96-3042 SIGMA RP Curved Tibial Insert Trial Size 4 12.5 mm
96-3043 SIGMA RP Curved Tibial Insert Trial Size 4 15.0 mm
96-3044 SIGMA RP Curved Tibial Insert Trial Size 4 17.5 mm
96-3051 SIGMA RP Curved Tibial Insert Trial Size 5 10 mm
96-3052 SIGMA RP Curved Tibial Insert Trial Size 5 12.5 mm
96-3053 SIGMA RP Curved Tibial Insert Trial Size 5 15.0 mm
96-3054 SIGMA RP Curved Tibial Insert Trial Size 5 17.5 mm
96-3061 SIGMA RP Curved Tibial Insert Trial Size 6 10 mm
96-3062 SIGMA RP Curved Tibial Insert Trial Size 6 12.5 mm
96-3063 SIGMA RP Curved Tibial Insert Trial Size 6 15.0 mm
96-3064 SIGMA RP Curved Tibial Insert Trial Size 6 17.5 mm
52 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Ordering Information
RP Stabilized
97-3101 SIGMA RP Stabilized Tibial Insert Trial Size 1.5 10.0 mm
97-3102 SIGMA RP Stabilized Tibial Insert Trial Size 1.5 12.5 mm
97-3103 SIGMA RP Stabilized Tibial Insert Trial Size 1.5 15.0 mm
97-3104 SIGMA RP Stabilized Tibial Insert Trial Size 1.5 17.5 mm
96-3105 SIGMA RP Stabilized Tibial Insert Trial Size 1.5 20.0 mm
96-3111 SIGMA RP Stabilized Tibial Insert Trial Size 2 10.0 mm
96-3112 SIGMA RP Stabilized Tibial Insert Trial Size 2 12.5 mm
96-3113 SIGMA RP Stabilized Tibial Insert Trial Size 2 15.0 mm
96-3114 SIGMA RP Stabilized Tibial Insert Trial Size 2 17.5 mm
96-3115 SIGMA RP Stabilized Tibial Insert Trial Size 2 20.0 mm
96-3116 SIGMA RP Stabilized Tibial Insert Trial Size 2 22.5. mm
96-3117 SIGMA RP Stabilized Tibial Insert Trial Size 2 25 mm
96-3121 SIGMA RP Stabilized Tibial Insert Trial Size 2.5 10.0 mm
96-3122 SIGMA RP Stabilized Tibial Insert Trial Size 2.5 12.5 mm
96-3123 SIGMA RP Stabilized Tibial Insert Trial Size 2.5 15.0 mm
96-3124 SIGMA RP Stabilized Tibial Insert Trial Size 2.5 17.5 mm
96-3125 SIGMA RP Stabilized Tibial Insert Trial Size 2.5 20.0 mm
96-3126 SIGMA RP Stabilized Tibial Insert Trial Size 2.5 22.5 mm
96-3127 SIGMA RP Stabilized Tibial Insert Trial Size 2.5 25 mm
96-3131 SIGMA RP Stabilized Tibial Insert Trial Size 3 10.0 mm
96-3132 SIGMA RP Stabilized Tibial Insert Trial Size 3 12.5 mm
96-3133 SIGMA RP Stabilized Tibial Insert Trial Size 3 15.0 mm
96-3134 SIGMA RP Stabilized Tibial Insert Trial Size 3 17.5 mm
96-3135 SIGMA RP Stabilized Tibial Insert Trial Size 3 20.0 mm
96-3136 SIGMA RP Stabilized Tibial Insert Trial Size 3 22.5. mm
96-3137 SIGMA RP Stabilized Tibial Insert Trial Size 3 25 mm
96-3141 SIGMA RP Stabilized Tibial Insert Trial Size 4 10.0 mm
96-3142 SIGMA RP Stabilized Tibial Insert Trial Size 4 12.5 mm
96-3143 SIGMA RP Stabilized Tibial Insert Trial Size 4 15.0 mm
96-3144 SIGMA RP Stabilized Tibial Insert Trial Size 4 17.5 mm
96-3145 SIGMA RP Stabilized Tibial Insert Trial Size 4 20.0 mm
96-3146 SIGMA RP Stabilized Tibial Insert Trial Size 4 22.5. mm
96-3147 SIGMA RP Stabilized Tibial Insert Trial Size 4 25 mm
96-3151 SIGMA RP Stabilized Tibial Insert Trial Size 5 10.0 mm
96-3152 SIGMA RP Stabilized Tibial Insert Trial Size 5 12.5 mm
96-3153 SIGMA RP Stabilized Tibial Insert Trial Size 5 15.0 mm
96-3154 SIGMA RP Stabilized Tibial Insert Trial Size 5 17.5 mm
96-3155 SIGMA RP Stabilized Tibial Insert Trial Size 5 20.0 mm
96-3156 SIGMA RP Stabilized Tibial Insert Trial Size 5 22.5. mm
96-3157 SIGMA RP Stabilized Tibial Insert Trial Size 5 25 mm
96-3161 SIGMA RP Stabilized Tibial Insert Trial Size 6 10.0 mm
96-3162 SIGMA RP Stabilized Tibial Insert Trial Size 6 12.5 mm
96-3163 SIGMA RP Stabilized Tibial Insert Trial Size 6 15.0 mm
96-3164 SIGMA RP Stabilized Tibial Insert Trial Size 6 17.5 mm
96-3165 SIGMA RP Stabilized Tibial Insert Trial Size 6 20.0 mm
96-3166 SIGMA RP Stabilized Tibial Insert Trial Size 6 22.5. mm
96-3167 SIGMA RP Stabilized Tibial Insert Trial Size 6 25 mm
RP-F
95-4110 RP-F Tibial Insert Trial 10 mm Size 1
95-4111 RP-F Tibial Insert Trial 12.5 mm Size 1
95-4112 RP-F Tibial Insert Trial 15 mm Size 1
95-4113 RP-F Tibial Insert Trial 17.5 mm Size 1
95-4114 RP-F Tibial Insert Trial 10 mm Size 1.5
95-4115 RP-F Tibial Insert Trial 12.5 mm Size 1.5
95-4116 RP-F Tibial Insert Trial 15 mm Size 1.5
95-4117 RP-F Tibial Insert Trial 17.5 mm Size 1.5
95-4120 RP-F Tibial Insert Trial 10 mm Size 2
95-4121 RP-F Tibial Insert Trial 12.5 mm Size 2
95-4122 RP-F Tibial Insert Trial 15 mm Size 2
95-4123 RP-F Tibial Insert Trial 17.5 mm Size 2
95-4125 RP-F Tibial Insert Trial 10 mm Size 2.5
95-4126 RP-F Tibial Insert Trial 12.5 mm Size 2.5
95-4127 RP-F Tibial Insert Trial 15 mm Size 2.5
95-4128 RP-F Tibial Insert Trial 17.5 mm Size 2.5
95-4130 RP-F Tibial Insert Trial 10 mm Size 3
95-4131 RP-F Tibial Insert Trial 12.5 mm Size 3
95-4132 RP-F Tibial Insert Trial 15 mm Size 3
95-4133 RP-F Tibial Insert Trial 17.5 mm Size 3
95-4140 RP-F Tibial Insert Trial 10 mm Size 4
95-4141 RP-F Tibial Insert Trial 12.5 mm Size 4
95-4142 RP-F Tibial Insert Trial 15 mm Size 4
95-4143 RP-F Tibial Insert Trial 17.5 mm Size 4
95-4150 RP-F Tibial Insert Trial 10 mm Size 5
95-4151 RP-F Tibial Insert Trial 12.5 mm Size 5
95-4152 RP-F Tibial Insert Trial 15 mm Size 5
95-4153 RP-F Tibial Insert Trial 17.5 mm Size 5
95-4160 RP-F Tibial Insert Trial 10 mm Size 6
96-4161 RP-F Tibial Insert Trial 12.5 mm Size 6
95-4162 RP-F Tibial Insert Trial 15 mm Size 6
95-4163 RP-F Tibial Insert Trial 17 mm Size 6
Patella Resection
9505-01-121 SIGMA HP Patella Resection Guide
9505-01-242 SIGMA HP Patella Resection Stylus 32-38 mm
9505-01-243 SIGMA HP Patella Resection Stylus 41 mm
9505-01-247 SIGMA HP Patella Resection Stylus 12mm Remnant
9505-01-923 HP Patella Wafer Small
9505-01-623 HP Patella Wafer Large
86-9188 Patella Calliper
86-5035 Patella Clamp
86-8801 Oval Patella Drill w/Hudson End
96-1100 PFC*SIGMA Oval/Dome Patella Trial 3 Peg 32 mm
96-1101 PFC*SIGMA Oval/Dome Patella Trial 3 Peg 35 mm
96-1102 PFC*SIGMA Oval/Dome Patella Trial 3 Peg 38 mm
96-1103 PFC*SIGMA Oval/Dome Patella Trial 3 Peg 41 mm
96-6601 Patellar Drill Guide 38 mm & 41 mm
96-6602 Patellar Drill Guide 32 mm & 35 mm
Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 53
Ordering Information
Spacer Blocks
Fixed Bearing
9505-02-105 SIGMA HP FBT Spacer Block 8 mm
9505-02-106 SIGMA HP FBT Spacer Block 10 mm
9505-02-107 SIGMA HP FBT Spacer Block 12.5 mm
9505-02-108 SIGMA HP FBT Spacer Block 15 mm
9505-02-109 SIGMA HP FBT Spacer Block 17.5 mm
9505-02-110 SIGMA HP FBT Spacer Block 20 mm
9505-02-111 SIGMA HP FBT Spacer Block 22.5 mm
9505-02-112 SIGMA HP FBT Spacer Block 25 mm
9505-02-113 SIGMA HP FBT Spacer Block 30 mm
9505-02-193 Flexion/Extension Cap Size 6
Mobile Bearing
9505-02-114 HP MBT Spacer Block 10 mm
9505-02-115 HP MBT Spacer Block12.5 mm
9505-02-116 HP MBT Spacer Block 15 mm
9505-02-117 HP MBT Spacer Block 17.5 mm
9505-02-118 HP MBT Spacer Block 20 mm
9505-02-119 HP MBT Spacer Block 22.5 mm
9505-02-120 HP MBT Spacer Block 25 mm
9505-02-121 HP MBT Spacer Block 30 mm
9505-02-193 Flexion/Extension Cap Size 6
RP-F
9505-02-104 SIGMA RP-F HP Flex SHIM Size 1
9505-02-100 SIGMA RP-F HP Flex SHIM Size 1.5
9505-02-101 SIGMA RP-F HP Flex SHIM Size 2
9505-02-102 SIGMA RP-F HP Flex SHIM Size 2.5-5
9505-02-103 SIGMA RP-F HP Flex SHIM Size 6
9505-02-193 Flexion/Extension Cap Size 6
Pinning
9505-02-070 HP Pin Impactor/Extractor
9505-02-071 HP Power Pin Driver
9505-02-072 HP Quick Pin Drills
9505-02-073 HP Quick Pin Drills Headed
9505-02-088 HP Threaded Pins
9505-02-089 HP Threaded Pins Headed
2267-12-000 Smooth 3 Inch Pins (5 Pack)
9505-02-300 SIGMA HP Quick Drill Pins-Sterile
9505-02-302 SIGMA HP Threaded Pins-Sterile
9505-02-303 SIGMA HP Threaded Pins Headed-Sterile
Insertion Femur
9505-01-218 SIGMA HP Femoral Notch Impactor
9505-01-171 HP Femoral Imp/Ext
9505-01-308 HP Slap Hammer
9505-01-305 HP Universal Handle
Mobile Bearing Tibia
9505-01-558 MBT Tibial Impactor
96-5383 MBT Tray Impactor
9505-01-559 MBT Tibial Impactor Replacement Parts
Fixed Bearing Tibia
9505-01-306 SIGMA FB Tibial Impactor
2581-11-000 F.B.T. Tray Inserter
96-6385 F.B.T. Poly PS
9505-01-170 SIGMA FBT Tibia Impactor Replacement Parts
96-6384 F.B.T. Tray Inserter
Anterior First
9505-02-090 SIGMA HP Anterior 1st Resection Guide
9505-02-092 SIGMA HP Anterior 1st Ledge Size 1.5-2
9505-02-093 SIGMA HP Anterior 1st Ledge Size 2.5-3
9505-02-094 SIGMA HP Anterior 1st Ledge Size 4-6
9505-02-095 SIGMA HP Anterior 1st Femoral Alignment Guide
9505-02-096 SIGMA HP Anterior 1st Femoral Resection Guide
Re-cut Kit
9505-01-294 SIGMA HP Re-cut Blk +2 mm
9505-01-295 SIGMA HP Re-cut Blk +3 Deg
9505-01-296 SIGMA HP Re-cut Blk 2 Deg V/V Left
9505-01-297 SIGMA HP Re-cut Blk 2 Deg V/V Right
9505-01-394 SIGMA HP Re-cut Kit Reference Arm
9505-01-395 SIGMA HP Re-cut Kit Slotted Adapter
Instrument Trays
General
9505-02-800 HP Base Femur & Tibia
9505-02-802 SIGMA HP Spacer Blocks
9505-02-808 SIGMA HP Patella & Insertion Instruments
9505-02-840 SIGMA HP Insertion Instruments
Femoral Sizing & Resection
9505-02-801 SIGMA HP Fixed Reference Femur Preparation
9505-02-803 SIGMA HP RP-F Fixed Reference Femur Preparation
9505-02-810 SIGMA HP Classic Reference Femur Preparation
9505-02-809 SIGMA HP RP-F Classic Reference Femur Preparation
9505-02-811 SIGMA HP Balanced Femur Preparation
9505-02-816 SIGMA HP RP-F Balanced Femur Preparation
9505-02-820 SIGMA HP Femoral Finishing Blocks
9505-02-826 SIGMA HP Macro Case
9505-02-843 SIGMA HP Micro Case
54 DePuy Synthes SIGMA® Primary Knee System Balanced Surgical Technique
Fixed Bearing Preparation & Trials
9505-02-812 SIGMA HP FB Tibial Preparation
9505-02-837 SIGMA HP Standard Tibial Guides & Punches
9505-02-835 SIGMA HP FB PLI Insert Trials
9505-02-813 SIGMA HP Curved Insert Trials
9505-02-814 SIGMA HP Stabilized Insert Trials
9505-02-827 SIGMA HP Curved Plus Case
9505-02-833 SIGMA HP FB Micro 1.5 Trial Case
9505-02-834 SIGMA HP FB Macro Trial Case
Mobile Bearing Preparation & Trials
9505-02-806 SIGMA HP MBT Tibia Preparation
9505-02-807 SIGMA HP RP Insert Trial
9505-02-832 SIGMA HP Macro RP Insert Case
9505-02-842 SIGMA HP RP Micro Insert Case
Femoral Trials
9505-02-804 SIGMA HP Femoral Trials
9505-02-815 SIGMA HP RP-F Trials
Miscellaneous
9505-02-841 SIGMA HP Quick Kit FB Case
9505-02-823 SIGMA HP Quick Kit Base Case
9505-02-824 SIGMA HP Quick Kit MBT Case
9505-02-821 SIGMA HP Upgrade #1 Case
9505-02-825 SIGMA HP Anterior First Case
9505-02-830 SIGMA HP Recut Kit Case
Ordering Information

Balanced Surgical Technique SIGMA® Primary Knee System DePuy Synthes 55
Total and Unicompartmental Knee Prostheses
Important:
This Essential Product Information sheet does not
include all of the information necessary for selection
and use of a device. Please see full labeling for all
necessary information.
Intended Use:
Total or unicompartmental knee arthroplasty is
intended to provide increased patient mobility and
reduced pain by replacing the damaged knee joint
articulation in patients where there is evidence of
sufficient sound bone to seat and support the
components. Total or unicompartmental knee
replacement may be considered for younger patients
if, in the opinion of the surgeon, an unequivocal
indication for total or unicompartmental knee
replacement outweighs the risks associated with the
age of the patient, and if limited demands regarding
activity and knee joint loading can be assured. This
includes severely crippled patients with multiple joint
involvement for whom a gain in knee mobility may
lead to an expectation of significant improvement in
the quality of their lives.
Indications:
Candidates for total or unicompartmental knee
replacement include patients with a severely painful and/
or severely disabled joint resulting from osteoarthritis,
post-traumatic arthritis, rheumatoid arthritis, or a failed
previous implant. In candidates for unicompartmental
knee arthroplasty, only one side of the joint (the medial
or lateral compartment) is affected.
THE SIGMA C/R POROCOAT FEMORAL
COMPONENTS ARE INTENDED FOR CEMENTED
OR CEMENTLESS USE AS THE FEMORAL
COMPONENT OF A TOTAL KNEE REPLACEMENT
SYSTEM.
IN THE US THIS POROUS COATED COMPONENT
HAS BEEN CLEARED FOR CEMENTED USE ONLY.
ANY NON-POROUS COATED COMPONENT IS
INTENDED FOR CEMENTED USE ONLY.
Contraindications:
The following conditions are contraindications for
total or unicompartmental knee replacement:
1. Active local or systemic infection.
2. Loss of bone or musculature, osteoporosis,
neuromuscular compromise or vascular deficiency
in the affected limb in sufficient degree to render
the procedure unjustifiable (e.g., absence of
musculoligamentous supporting structures, joint
neuropathy).
3. Severe instability secondary to advanced loss of
osteochondral structure or the absence of
collateral ligament integrity.
4. Unicompartmental knee replacement is
contraindicated in patients with a severe (over 30°)
fixed valgus or varus deformity.
NOTE: Diabetes, at present, has not been established
as a contraindication. However, because of the
increased risk for complications such as infection,
slow wound healing, etc., the physician should
carefully consider the advisability of knee replacement
in the severely diabetic patient.
Warnings and Precautions:
CAUTION:
• Implants and trial components from different
manufacturers or implant systems should
never be used together.
• Knee prosthesis components should never be
reimplanted. Even though the implant
appears undamaged, the implant may have
developed microscopic imperfections which
could lead to failure.
• Always use a trial prosthesis for trial
purposes. Trials should not be assembled with
any components intended for permanent
implantation. Trials must have the same
configuration size, as the corresponding
components to be permanently implanted.
• Do not alter or modify implants in any way.
• Avoid drilling multiple pin holes in the
proximal tibia which may affect the
compressive strength of the tibia.
These total and unicompartmental knee
prostheses have not been evaluated for safety
and compatibility in the MR environment. These
total and unicompartmental knee prostheses
have not been tested for heating or migration in
the MR environment. The risks of exposure to
MR include heating and/or displacement of a
metallic implant. Image artifacts including dead
zones and distortion may occur, especially in the
immediate area around the implant, requiring
optimization of imaging parameters. Please
refer to current local MR safety guidelines for
additional investigation, patient monitoring and
patient follow-up advice. DePuy recommends
that a professional familiar with the specific MRI
apparatus to be used, assess the patient prior to
any MRI examination of or therapy.
CAUTION: The following conditions, singularly or
concurrently, tend to impose severe loading on the
affected extremity thereby placing the patient at
higher risk of failure of the knee replacement:
1. Obesity or excessive patient weight.
2. Manual Labor.
3. Active sports participation.
4. High levels of patient activity.
5. Likelihood of falls.
6. Alcohol or drug addiction.
7. Other disabilities, as appropriate.
In addition to the above, the following physical
conditions, singularly or concurrently, tend to
adversely affect the fixation of knee replacement
implants:
1. Marked osteoporosis or poor bone stock.
2. Metabolic disorders or systemic pharmacological
treatments leading to progressive deterioration of
solid bone support for the implant (e.g., diabetes
mellitus, teroid therapies, immunosuppressive
therapies, etc.).
3. History of general or local infections.
4. Severe deformities leading to impaired fixation or
improper positioning of the implant.
5. Tumors of the supporting bone structures.
6. Allergic reactions to implant materials (e.g. bone
cement, metal, polyethylene).
7. Tissue reactions to implant corrosion or implant
wear debris.
8. Disabilities of other joints (i.e., hips or ankles).
A higher incidence of implant failure has been
reported in paraplegics and in patients with cerebral
palsy or Parkinson Disease.
WHEN THE SURGEON DETERMINES THAT KNEE
REPLACEMENT IS THE BEST MEDICAL OPTION
AVAILABLE AND DECIDES TO USE THIS PROSTHESIS
IN A PATIENT WHO HAS ANY OF THE ABOVE
CONDITIONS OR WHO IS SIMPLY YOUNG AND
ACTIVE, IT IS IMPERATIVE THAT THE PATIENT BE
INSTRUCTED ABOUT THE STRENGTH LIMITATIONS OF
THE MATERIALS USED IN THE DEVICE AND FOR
FIXATION AND THE RESULTANT NEED TO
SUBSTANTIALLY REDUCE OR ELIMINATE ANY OF THE
ABOVE CONDITIONS.
The surgical and postoperative management of the
patient must be carried out with due consideration
for all existing conditions. Mental attitudes or
disorders resulting in a patient's failure to adhere to
the surgeon's orders may delay postoperative recovery
and/or increase the risk of adverse effects including
implant or implant fixation failure.
Excessive physical activity or trauma to the replaced
joint may contribute to premature failure of the knee
replacement by causing a change in position, fracture,
and/or wear of the implants. The functional life
expectancy of prosthetic knee implants is, at
present, not clearly established. The patient
should be informed that factors such as weight and
activity levels may significantly affect wear.
DePuy’s Single Use devices have not been designed to
undergo or withstand any form of alteration, such as
disassembly, cleaning or re-sterilization, after a single
patient use. Reuse can potentially compromise device
performance and patient safety.
Adverse Events:
The following are the most frequent adverse events
after knee arthroplasty: change in position of the
components, loosening, tibial subsidence, bending,
cracking, fracture, deformation or wear of one or
more of the components, infection, tissue reaction to
implant materials or wear debris; pain, dislocation,
subluxation, flexion contracture, decreased range of
motion, lengthening or shortening of leg caused by
improper positioning, looseness or wear of
components; fractures of the femur or tibia.

Limited Warranty and Disclaimer: DePuy Synthes products are sold with a limited warranty to the original purchaser against defects in workmanship
and materials. Any other express or implied warranties, including warranties of merchantability or fitness, are hereby disclaimed.
Please also refer to the package insert(s) or other labeling associated with the devices identified in this surgical technique for additional information.
CAUTION: Federal Law restricts these devices to sale by or on the order of a physician.
Some devices listed in this surgical technique may not have been licensed in accordance with Canadian law and may not be for sale in Canada.
Please contact your sales consultant for items approved for sale in Canada.
Not all products may currently be available in all markets.
DePuy Orthopaedics, Inc.
700 Orthopaedic Drive
Warsaw, IN 46582
USA
Tel: +1 (800) 366-8143
Fax: +1 (800) 669-2530
www.depuysynthes.com
© DePuy Synthes 2014, 2017. All rights reserved.
DSUS/JRC/0716/1692 04/17
DePuy International, Ltd.
St Anthony’s Road
Leeds LS11 8DT
England
Tel: +44 (0) 113 270 0461
DePuy (Ireland)
Loughbeg, Ringaskiddy
Co. Cork
Ireland
Tel: + 353 21 4914 000
Fax: + 353 21 4914 199
0086
Enztec Limited
26 Dakota Crescent
Stockburn, Christchurch
8042, New Zealand