Achilles Repair Syllabus
2013-05-20
: Pdf Achilles Repair Syllabus Achilles_Repair_Syllabus 5 2013 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 27
5/17/2013
1
Chronic tear of the Tendo Achillis
Minimally Invasive Achilles Repair
with Soft Tissue Augmentation
Nicola Maffulli MD, MS, PhD, FRCS(Orth)
VuMedi Webinar 20.05.2013
DISCLOSURE
•None relevant to this presentation
Chronic rupture of the Achilles tendon
•The Achilles tendon (AT) is the most commonly rupture
tendon in the human body.
•Complete ruptures of the AT: sedentary and athletes
patients
•Common in middle aged men who occasionally
participate in sport.
Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am 1999; 81(7):1019-36
Longo UG, Ronga M, Maffulli N. Acute ruptures of the achilles tendon. Sports Med
Arthrosc 2099;17(2):127-38
Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A
prospective study in 174 patients. Am J Sports Med 1998; 26(2):266-70
Epidemiology
5/17/2013
2
Chronic rupture of the Achilles tendon
•Variable
•Timeframe is to 4 to 6 weeks from the time of injury.
•When there has been a delay in treatment, ruptures
may be called chronic, neglected, or old.
Boyden EM, Kitaoka HB, Cahalan TD, An KN. Late versus early repair of Achilles tendon
rupture. Clinical and biomedical evaluation. Clin Orthop Relat Res 1995; (317):150-8.
Gabel S, Manoli A, 2nd. Neglected rupture of the Achilles tendon. Foot Ankle Int 1994;
15(9):512-7.
Mann RA, Holmes GB, Jr., Seale KS, Collins DN. Chronic rupture of the Achilles tendon:
a new technique of repair. J Bone Joint Surg Am 1991; 73(2):214-9.
Zadek I. Repair of old rupture of the tendo-Achilles by means of fascia. Report of a case.
J Bone Joint Surg 1940; 22(4):1070-1071.
Definition
Chronic rupture of the Achilles tendon
CASE 1
Chronic rupture of the Achilles tendon
•32 year old gentleman
•Not known allergies
•Not relevant medical history
•No quinolones
•No corticosteroids
•No prodromal symptoms
•Sports (running and soccer) twice/week
•July 2012: “I felt a hit in the calf of the left leg while
running”
5/17/2013
3
Chronic rupture of the Achilles tendon
•Attends A&E
•Can walk, can plantar flex against gravity
•‘Sprained ankle’
•Given a walker, told to rest
•Discharged
Case
•6 weeks of immobilization
•6 weeks of physiotherapy
•After 4 months, patient walks flat footed, non-
propulsive gait, swollen ankle
•Can feel a three finger gap at the back of the ankle
•Reassured!!!
October 2012
What to do next?
•Physical examination:
-Calf squeeze test: no movement
-Knee flexion test: fall of affected foot
All the above documented in notes
Reassured
October 2012
5/17/2013
4
Goes to a pub, sees a friend (a rugby
playing lawyer), who makes the
diagnosis
Referred to CSEM
Diagnosis: chronic Achilles tendon rupture
Gap: 6 cm clinically
November 2012
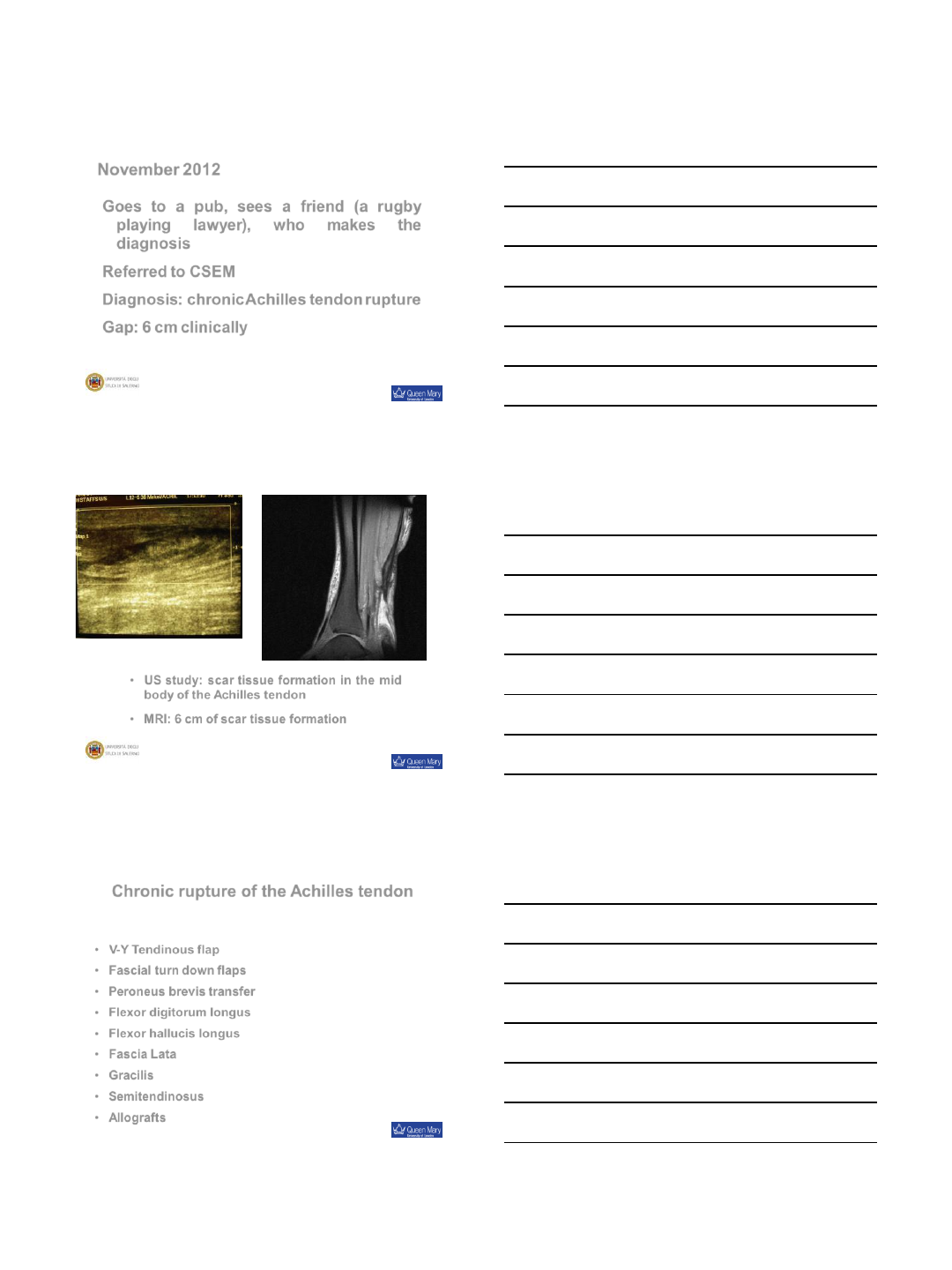
•US study: scar tissue formation in the mid
body of the Achilles tendon
•MRI: 6 cm of scar tissue formation
Chronic rupture of the Achilles tendon
•V-Y Tendinous flap
•Fascial turn down flaps
•Peroneus brevis transfer
•Flexor digitorum longus
•Flexor hallucis longus
•Fascia Lata
•Gracilis
•Semitendinosus
•Allografts
Operative management
5/17/2013
5
Chronic rupture of the Achilles tendon
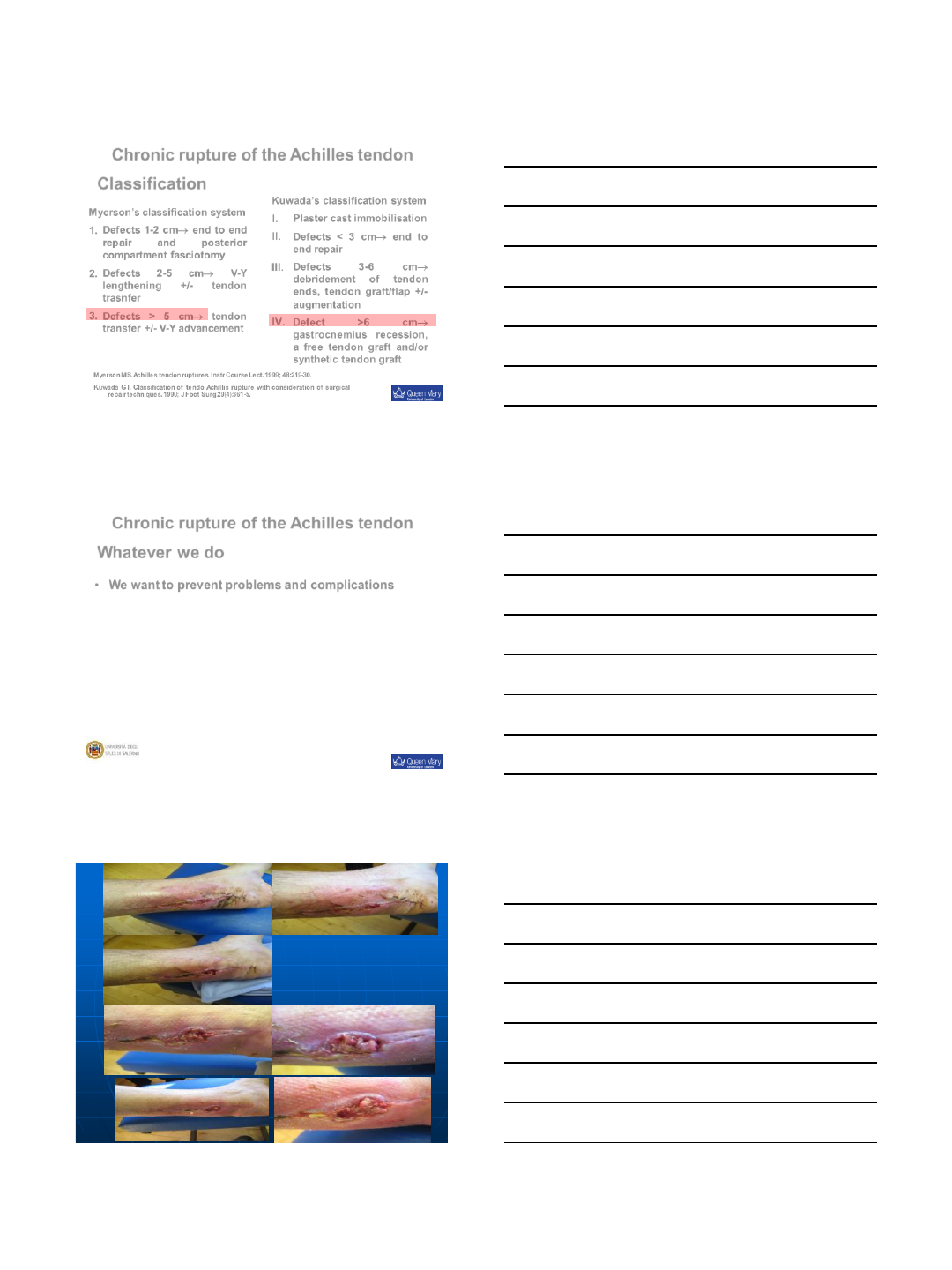
Myerson’s classification system
1. Defects 1-2 cm end to end
repair and posterior
compartment fasciotomy
2. Defects 2-5 cm V-Y
lengthening +/- tendon
trasnfer
3. Defects > 5 cm tendon
transfer +/- V-Y advancement
Myerson MS. Achilles tendon ruptures. Instr Course Lect. 1999; 48:219-30.
Kuwada GT. Classification of tendo Achillis rupture with consideration of surgical
repair techniques. 1990; J Foot Surg 29(4):361-5.
Classification
Kuwada’s classification system
I. Plaster cast immobilisation
II. Defects < 3 cm end to
end repair
III. Defects 3-6 cm
debridement of tendon
ends, tendon graft/flap +/-
augmentation
IV. Defect >6 cm
gastrocnemius recession,
a free tendon graft and/or
synthetic tendon graft
Chronic rupture of the Achilles tendon
•We want to prevent problems and complications
Whatever we do
5/17/2013
6
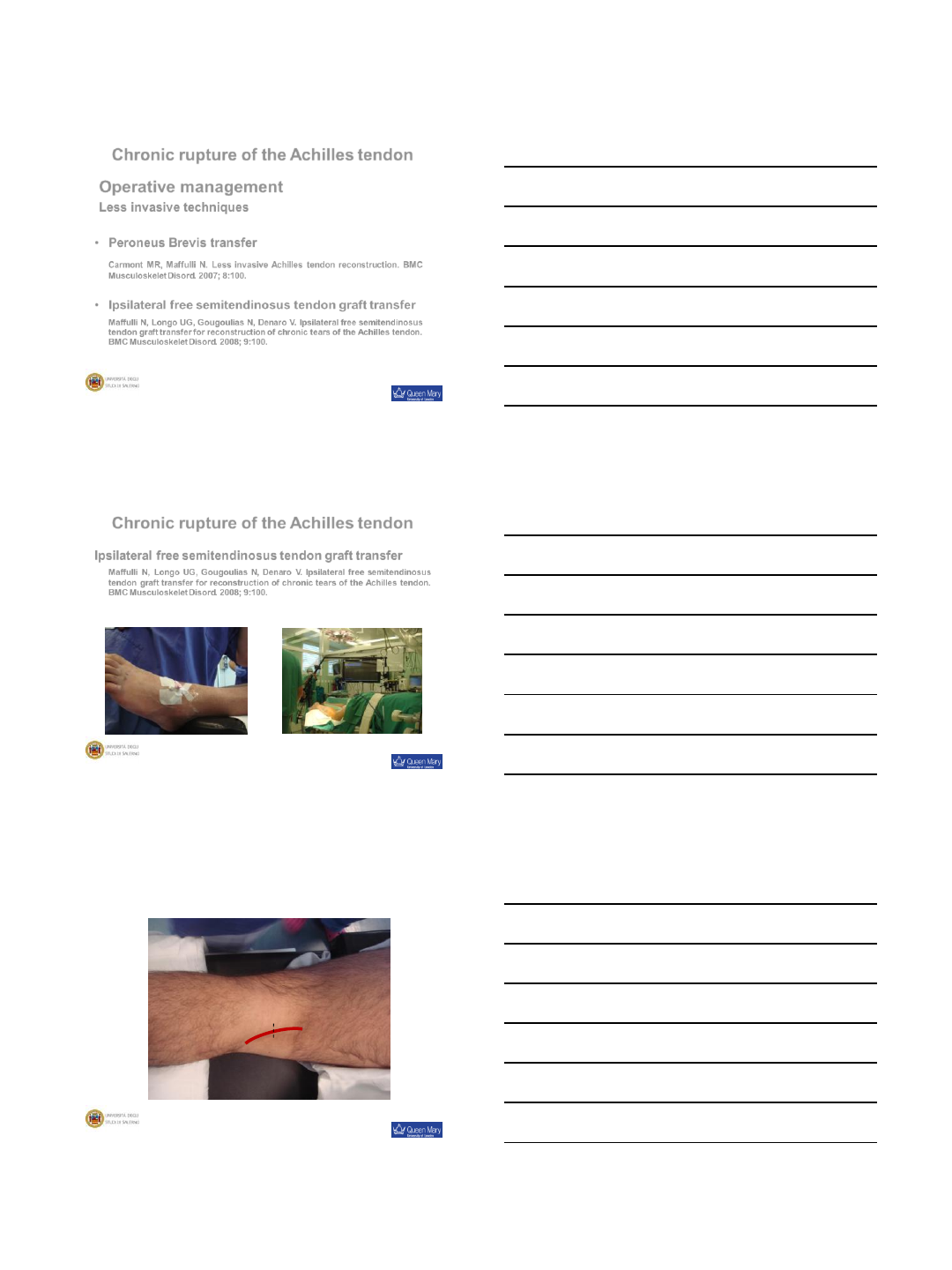
Chronic rupture of the Achilles tendon
•Peroneus Brevis transfer
Carmont MR, Maffulli N. Less invasive Achilles tendon reconstruction. BMC
Musculoskelet Disord. 2007; 8:100.
•Ipsilateral free semitendinosus tendon graft transfer
Maffulli N, Longo UG, Gougoulias N, Denaro V. Ipsilateral free semitendinosus
tendon graft transfer for reconstruction of chronic tears of the Achilles tendon.
BMC Musculoskelet Disord. 2008; 9:100.
Operative management
Less invasive techniques
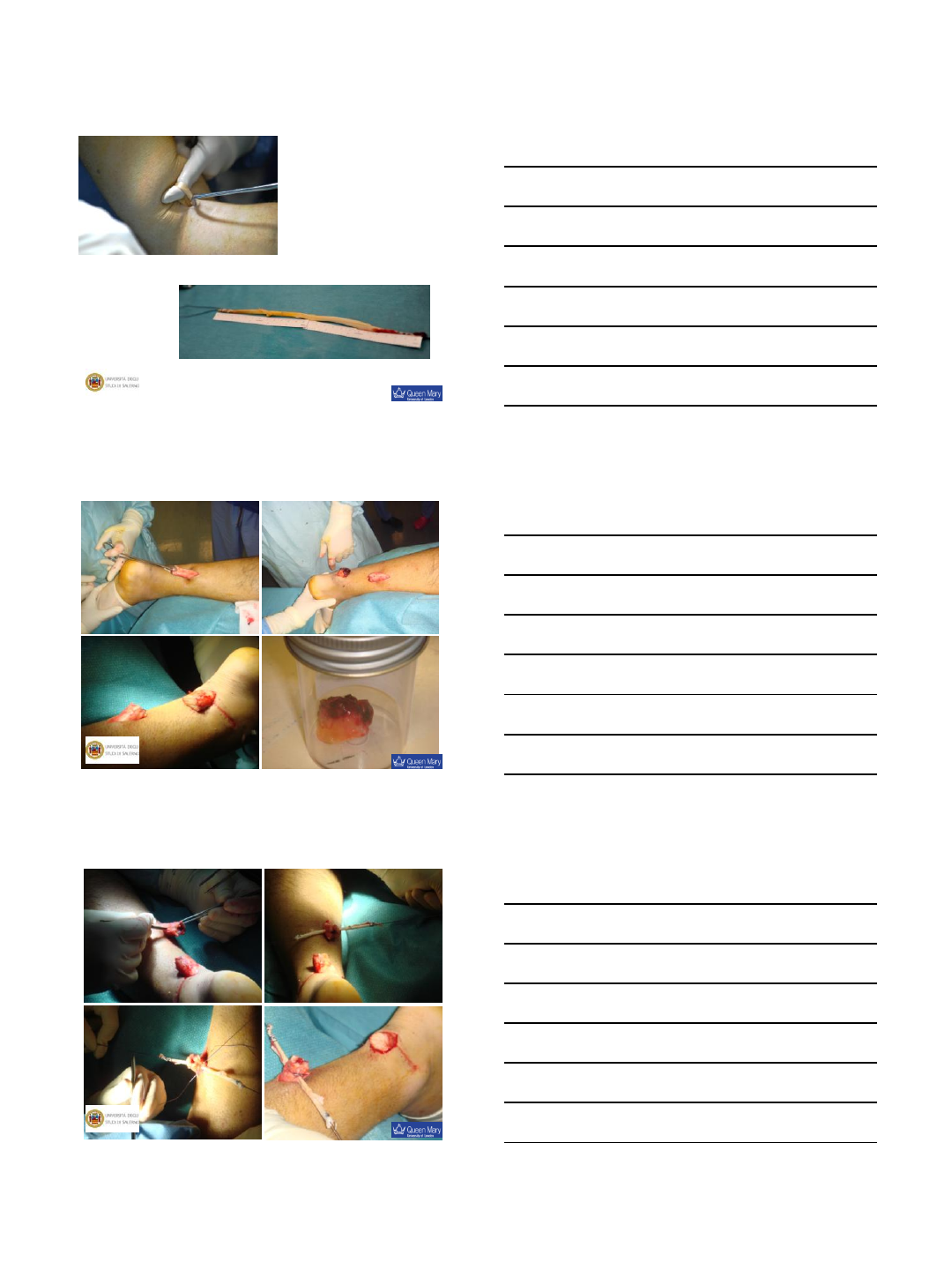
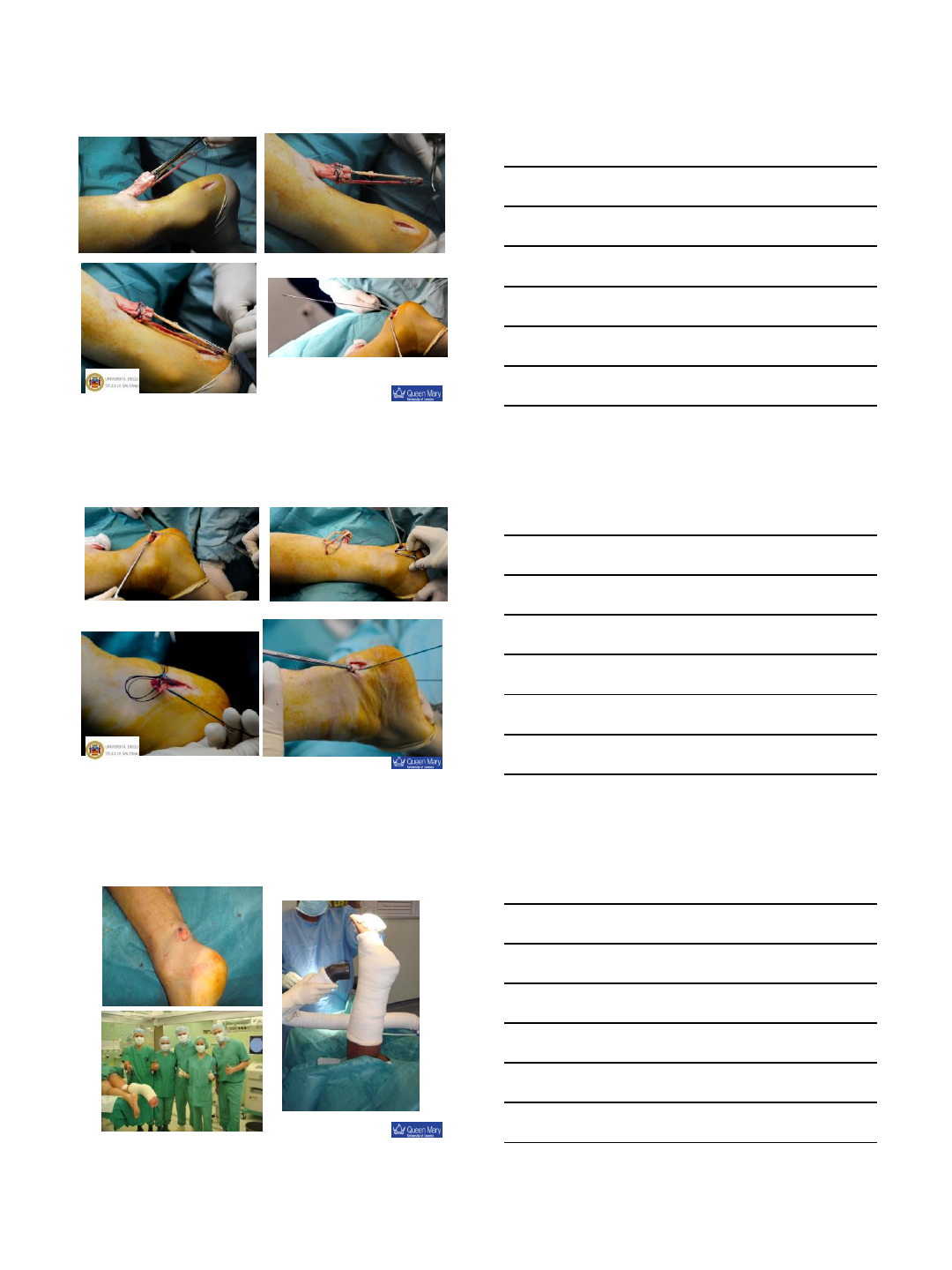
Chronic rupture of the Achilles tendon
Ipsilateral free semitendinosus tendon graft transfer
Maffulli N, Longo UG, Gougoulias N, Denaro V. Ipsilateral free semitendinosus
tendon graft transfer for reconstruction of chronic tears of the Achilles tendon.
BMC Musculoskelet Disord. 2008; 9:100.
5/17/2013
7
5/17/2013
8
5/17/2013
9
Chronic rupture of the Achilles tendon
•Immediate weight bear on metatarsal heads with crutches
•Mobilise toes against resistance
•2/52 : Walker with heel raises (remove one every other week); WB
as able
•Physiotherapy:
–Prevent dorsiflexion of the ankle
–Focus on propioception, plantar-flexion, inversion and
eversion
•8/52: discard walker; learn to walk properly
Postoperative management
Maffulli N, Tallon C, Wong J, Peng Lim K, Bleakney R. No adverse affect of early weight bearing following
open repair of acute tears of the Achilles tendon. J Sports Med Phys Fitness. 2003; 43(3):367-79.
Maffulli N, Tallon C, Wong J, Lim KP, Bleakney R. Early weightbearing and ankle mobilization after open
repair of acute midsubstance tears of the Achilles tendon. Am J Sports Med. 2003; 31(5):692-700.
Chronic rupture of the Achilles tendon
•Intensive mobilisation
•Prevent excessive dorsiflexion
•Gradual return to normal activities over 6 to 9/12
Postoperative management
Chronic rupture of the Achilles tendon
•Many different techniques can be used for
reconstruction.
Conclusions
•The choice of management is partly guided by the size of
the tendon defect with the optimal management likely
being surgical.
•Chronic ruptures of tendo Achillis are uncommon but
debilitating.
•Less invasive techniques provide similar results to those
obtained with open surgery, with decreased perioperative
morbidity, decreased hospital stay, and reduced costs
5/17/2013
10
If you wish to know more …

5/17/2013
11
Thank you
n.maffulli@qmul.ac.uk
5/20/2013
1
Achilles rupture
- non-surgical augmentation
James Calder TD, MD, FRCS(Tr & Orth), FFSEM(UK)
Chelsea & Westminster Hospital NHS Trust, London
The Fortius Clinic, London
www.fortiusclinic.com
Mechanical
Stimulation NSAIDs
Growth
Factors
Neuronal
Factors
www.fortiusclinic.com
Mechanical Stimulation
Activates myofibroblasts
Lack of stimulation
detrimental
+ve effects in animals:
External fixators
Disarticulated limbs
www.fortiusclinic.com
5/20/2013
2
Mechanical Stimulation
Botulinum group:
Force to failure ↓30% @ 2/52
Stimulated group:
Callus larger and stronger
Virchenko, Asenberg; Acta Orthop 2006
Increased activity – shortening of tendon callus
(myofibroplastic)
Ackermann, Calder; Current Concepts 2008
www.fortiusclinic.com
Mechanical Improvements?
•Intermittent pneumatic
compression
–wound healing
–fracture healing
•Action:
–↑neuro-vascular in-growth
–2x expression sensory
neuropeptides
–↑ tissue perfusion
→ speeds fibroblast
→ proliferation/collagen organisation
Dahl et al, J Orthop Res 2007
?
www.fortiusclinic.com
Evaluation of recovery – ultra-high
resolution ultrasound
•600 axial images/0.2mm
•Reconstructed saggital &
•coronal planes
•Pixel brightness correlates
with intact, discontinuous,
fibrillous, cellular and fluid
Dr Hans van Schie (Netherlands)
www.fortiusclinic.com
5/20/2013
3
NSAIDs
www.fortiusclinic.com
Inflammatory
Mediators
NSAIDs
Blood-derived
Cells
Platelets
Leucocytes
Monocytes
Lymphocytes
Eicosanoids
Cytokines
Nitric Oxide
Growth Factors
Tissue-derived
Cells
Macrophages
Fibroblasts
Myofibroblasts
Endothelial Cells
Mast Cells
Chemotaxis
Vasodilation
Angiogenesis
Protein
synthesis
Collagen
synthesis
www.fortiusclinic.com
Inflammatory
Mediators
NSAIDs
Blood-derived
Cells
Cox inhibitors
- ↓ 1/3 fibrous strength Magra, N Clin J Sp Med 2006
- ↓bone-tendon strength in PT Ferry, Am J SP Med 2007
- effect lasts 2/52 Virchenko, Am J Sp Med 2004
HOWEVER
Start day 6 (inflammatory phase over)
- +ve effect on mech properties
- thinner / stronger Forrester, J Tr-injury inf crit care 1970
- celecoxib improves tendon healing Forslund, Act Orthop Scand 2003
www.fortiusclinic.com

5/20/2013
4
Growth Factors
Many Implicated
– delivery & short ½ life
Growth and
Differentiation Factors
(GDF)
Part of BMP family
Cartilage Derived
Morphogenic Protein
(CDMP)
www.fortiusclinic.com
Growth Factors
Many Implicated
– delivery & short ½ life
- GDF 5 & 6 on collagen
sponges
- ↑ tensile strength
- dose-dependent
Aspenberg, Acta Orthop Scand 1999
www.fortiusclinic.com
Growth Factors
Many Implicated
– delivery & short ½ life
- GDF-5 coated polyglactin
suture
- 80 rats, Achilles tendon
Rickert, Growth Factors 2001
- 44 rabbits, zone II flexor
Henn, J Hand Surg 2010
- tendons thicker and
stronger at 1,2 & 4 weeks
www.fortiusclinic.com
5/20/2013
5
Growth Factors
Many Implicated – delivery
CDMP1,2 or 3 injected
into haematoma @ 6hrs
-30% ↑ tensile strength in
rat
Forslund, J Orth Res 2003
-65% ↑ tensile strength in
rabbit at 14 days
- No difference at 28 days
Virchenko, J Med Sci Sports 2005
Useful for early
rehabilitation?
www.fortiusclinic.com
Platelet Rich Plasma
•PRP injection @6hrs
↑strength 30% up to 3/52
Aspenberg Acta Orthop Scand 2004
•rhPDGF-BB increases
strength in rat model
Shah, J Orth Res 2012
Virchenko Act Orthop 2006
•Relies upon mechanical
stimulation
–Early benefit
–Botox abolishes PRP
effect @ 2/52
Short-lived proliferative response allows mechanical
stimulation to begin earlier?
www.fortiusclinic.com
Platelet Rich Plasma
•Thrombin alone
–↑10% strength
•PRP gel with activated
thrombin have combined
effect
–↑42% strength
Virchenko Act Orthop 2006
•PRP gel with neutralised
thrombin
–↑22% strength
PRP Thrombin
Strength
↑42%
Strength
↑22%
www.fortiusclinic.com
5/20/2013
6
PRP - Human models
Schepull AJSM 2011
•No effect on strength of repair
However:
•17 x physiological
concentration of platelets
(?overstimulation)
•Very high inter-patient
variability (confounding
variables at play?)
Sanchez AJSM 2007
•Faster healing
•Less thickening of tendon
repair
•Higher levels of growth factors
in wound edges
•Supports earlier animal work
and also work on ACLs (faster
healing and greater maturity)
•Cross-over with animal models
and other anatomical areas
www.fortiusclinic.com
PRP overall evidence
Systematic review
•No effect in
tendinopathy
•Medium – large effect
in rupture
•Enhanced scar effect?
•Consistent improvement in
biomechanical properties
0.5 SD across all animal
models
Sadoghi, J Orth Res 2013
www.fortiusclinic.com
PRP overall evidence
Systematic review
•No effect in
tendinopathy
•Medium – large effect
in rupture
•Enhanced scar effect?
•Consistent improvement in
biomechanical properties
0.5 SD across all animal
models
Sadoghi, J Orth Res 2013
www.fortiusclinic.com
5/20/2013
7
PRP – questions?
•Which PRP?
–? Too many variables
–Internal variation (day
to day)
–Different concentrations
–Bone marrow derived
stem cells possibly
superior
Okamoto, JBJS(A) 2010
Chang, JBJS(A) 2007
?Bucket chemistry!
www.fortiusclinic.com
Thrombo-embolism
•Continuous LMWH
–↓33% strength
•Injection LMWH twice daily
–No effect
•Long-acting thrombin and
factor Xa inhibitors
–?cause for concern
–?intermittent use of LMWH OK
Dabigatran
Rivaroxaban
www.fortiusclinic.com
Neuropeptides
•Substance P (SP)
–Gives initial boost to tendon healing
–Accelerates reparative phase
•Injection of SP into paratenon after tendon repair in rats
–enhances fibroblast aggregation at 1st week (no difference
after this)
–collagen orientation faster from 2nd week
Burssens, FAI 2005
•Increase tensile strength of Achilles repair by 100%
Steyaert, Arch Phy Med Rehab 2006
www.fortiusclinic.com
5/20/2013
8
Neuropeptides
•Nerve Growth Factor
•In rats MCL
–↑Angiogenesis
–↑Nerve in-growth
–↑Mechanical strength 55%
Mammotto J Orth Res 2008
www.fortiusclinic.com
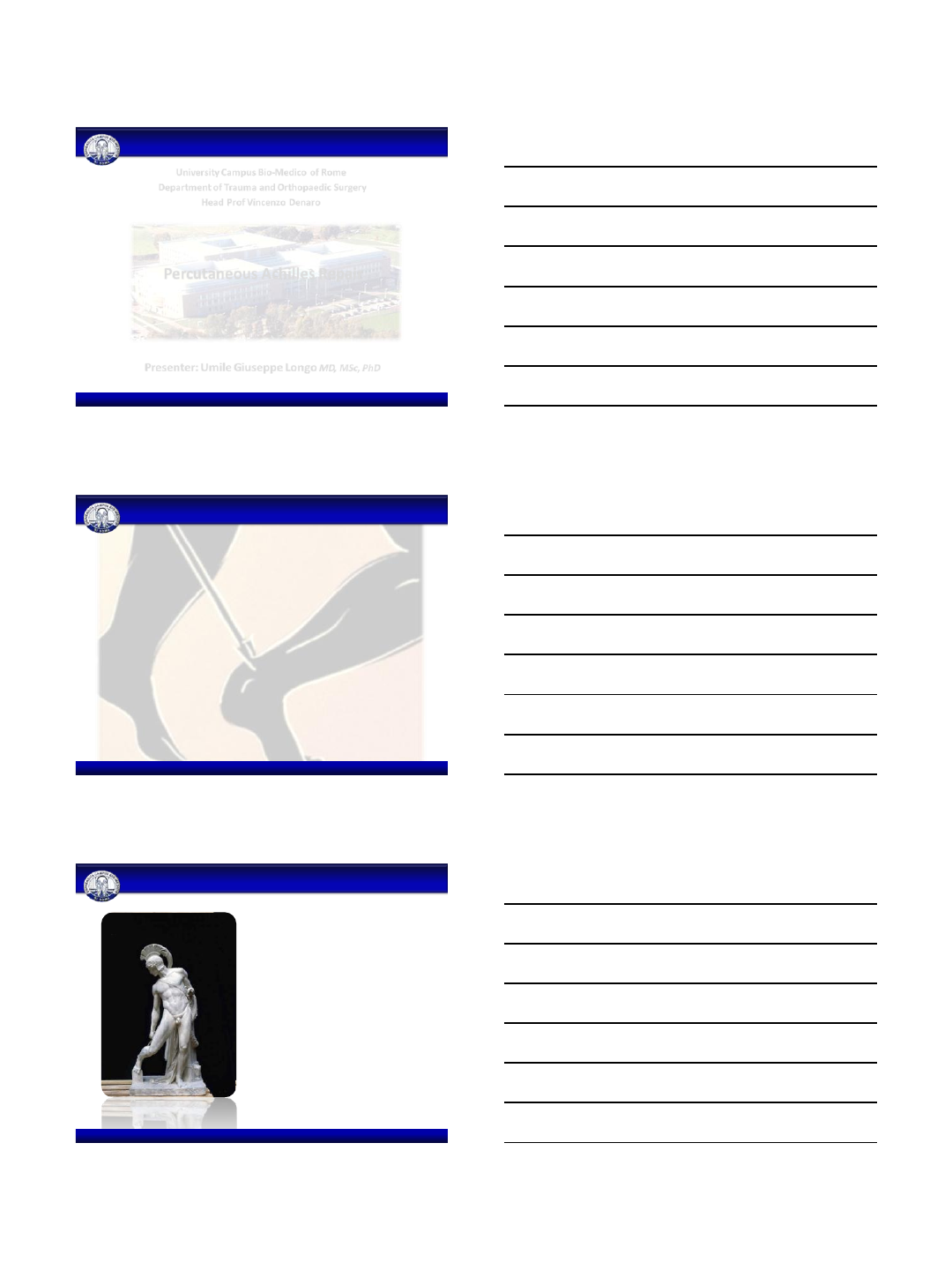
So what does this mean to the
practical orthopaedic surgeon today?
•Use mechanical
stimulation
–Early wt-bear
–Electrical calf stimulator?
www.fortiusclinic.com
So what does this mean to the
practical orthopaedic surgeon today?
•Use mechanical
stimulation
–Early wt-bear
–Electrical calf complex?
•NSAIDs not for 1/52 post
injury
(beneficial from 1/52)
www.fortiusclinic.com

5/20/2013
9
So what does this mean to the
practical orthopaedic surgeon today?
•Use mechanical stimulation
–Early wt-bear
–Electrical calf complex?
•NSAIDs not for 1/52 post
injury
(beneficial from 1/52)
•Significant risk of VTE but
consider problems with Xa
inhibitors for thrombo-
embolic prophylaxis
www.fortiusclinic.com
So what does this mean to the
practical orthopaedic surgeon today?
•Use mechanical stimulation
–Early wt-bear
–Electrical calf complex?
•NSAIDs not for 1/52 post
injury
(beneficial from 1/52)
•Significant risk of VTE but
consider problems with Xa
inhibitors for thrombo-
embolic prophylaxis
•Current evidence appears to
support PRP or even
concentrated bone-marrow
aspirates
www.fortiusclinic.com
Achilles rupture
- non-surgical augmentation
James Calder TD, MD, FRCS(Tr & Orth), FFSEM(UK)
Chelsea & Westminster Hospital NHS Trust, London
The Fortius Clinic, London
www.fortiusclinic.com
5/20/2013
1
Percutaneous Achilles Repair
Presenter: Umile Giuseppe Longo MD, MSc, PhD
University Campus Bio-Medico of Rome
Department of Trauma and Orthopaedic Surgery
Head Prof Vincenzo Denaro
No conflicts to declare
Conflicts of interest
Achilles tendon ruptures
•INCIDENCE
–Annual average of 5 to 18 ruptures
per 100,000 people
–More common in males in the third
or fourth decade of life
•ETIOLOGY
–Most acute AT ruptures are
traumatic
–Possible occult degeneration
5/20/2013
2
•Open, limited open and percutaneous techniques are
options for treating patients with acute Achilles
tendon rupture.
•Strength of Recommendation: Weak
ATR Summary of Recommendations: number 8
•Operative management of acute AT ruptures significantly
reduces the risk of rerupture compared with nonoperative
treatment
•Open operative treatment is associated with a significantly
higher risk of other complications
•Operative risks may be reduced by performing surgery
percutaneously
Achilles tendon ruptures
Khan RJ et al Cochrane 2010
•Several percutenaous techniques available
•Pros
–Faster recovery time
–Shorter hospital stays
–Improved functional outcomes
•Cons
–Sural nerve damage
Percutaneous Achilles tendon repair
5/20/2013
3
Biomechanics of minimally invasive techniques for Achilles tendon
There were no differences in mean strength of suture, mean maximum load, mean
failure elongation, tension value, mean stiffness and mode of failure
Longo UG, Forriol F, Ca mpi, S, Ma ffulli N and Denaro V KSSTA (2012);20(7):1392-7
•1 incision over the
defect
•4 longitudinal stab
incisions 6 cm
proximal to the
palpable defect
Percutaneous Achilles tendon repair
Carmont and Maffulli KSSTA (2008) 16:199-203
Carmont and Maffulli KSSTA (2008) 16:199-203
Percutaneous Achilles tendon repair
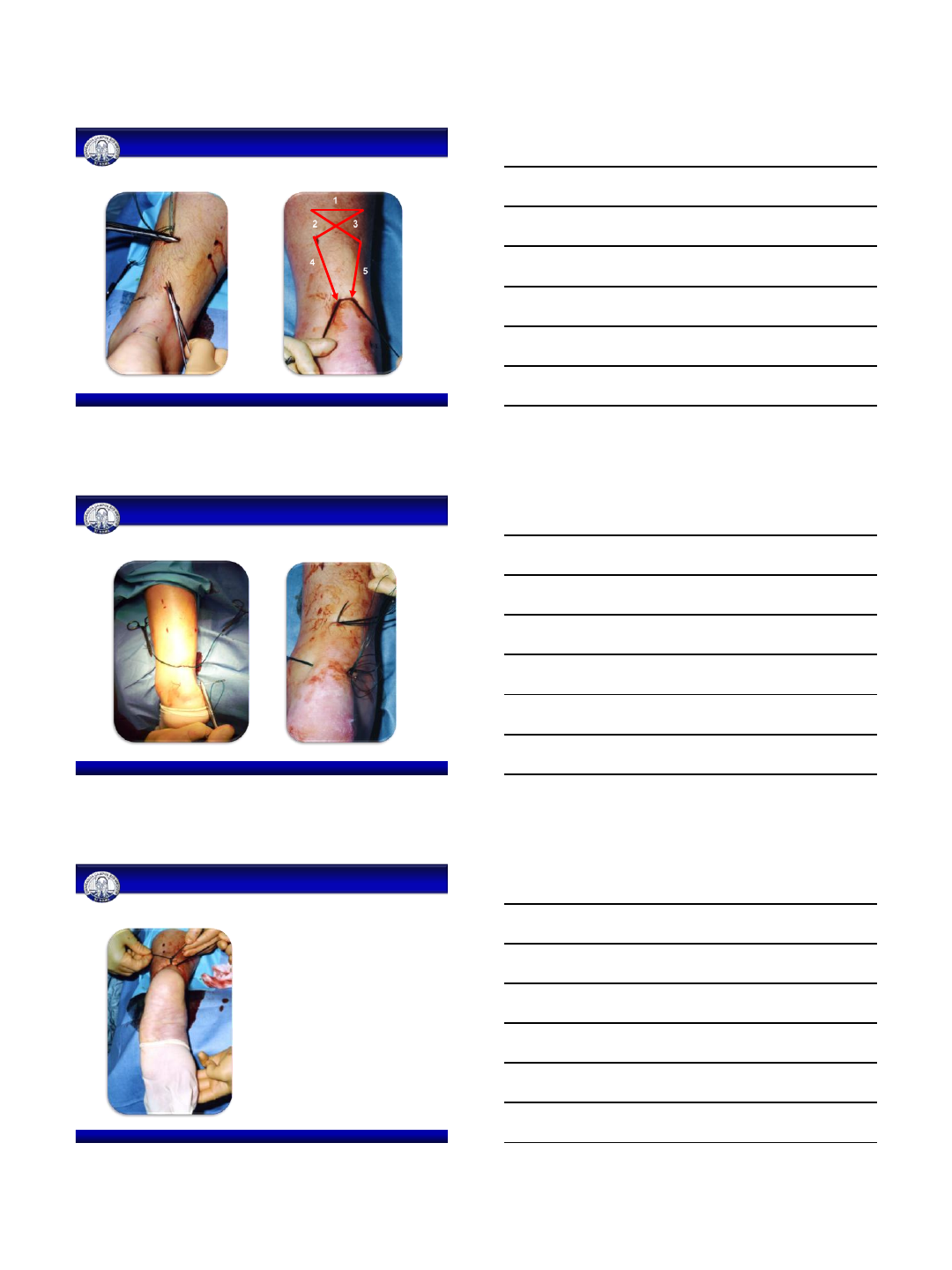
5/20/2013
4
Carmont and Maffulli KSSTA (2008) 16:199-203
Percutaneous Achilles tendon repair
1
2 3
4 5
Carmont and Maffulli KSSTA (2008) 16:199-203
Percutaneous Achilles tendon repair
•The ankle is held in full
plantar flexion, and in turn
opposing ends of the Maxon
thread are tied together
Carmont and Maffulli KSSTA (2008) 16:199-203
Percutaneous Achilles tendon repair
5/20/2013
5
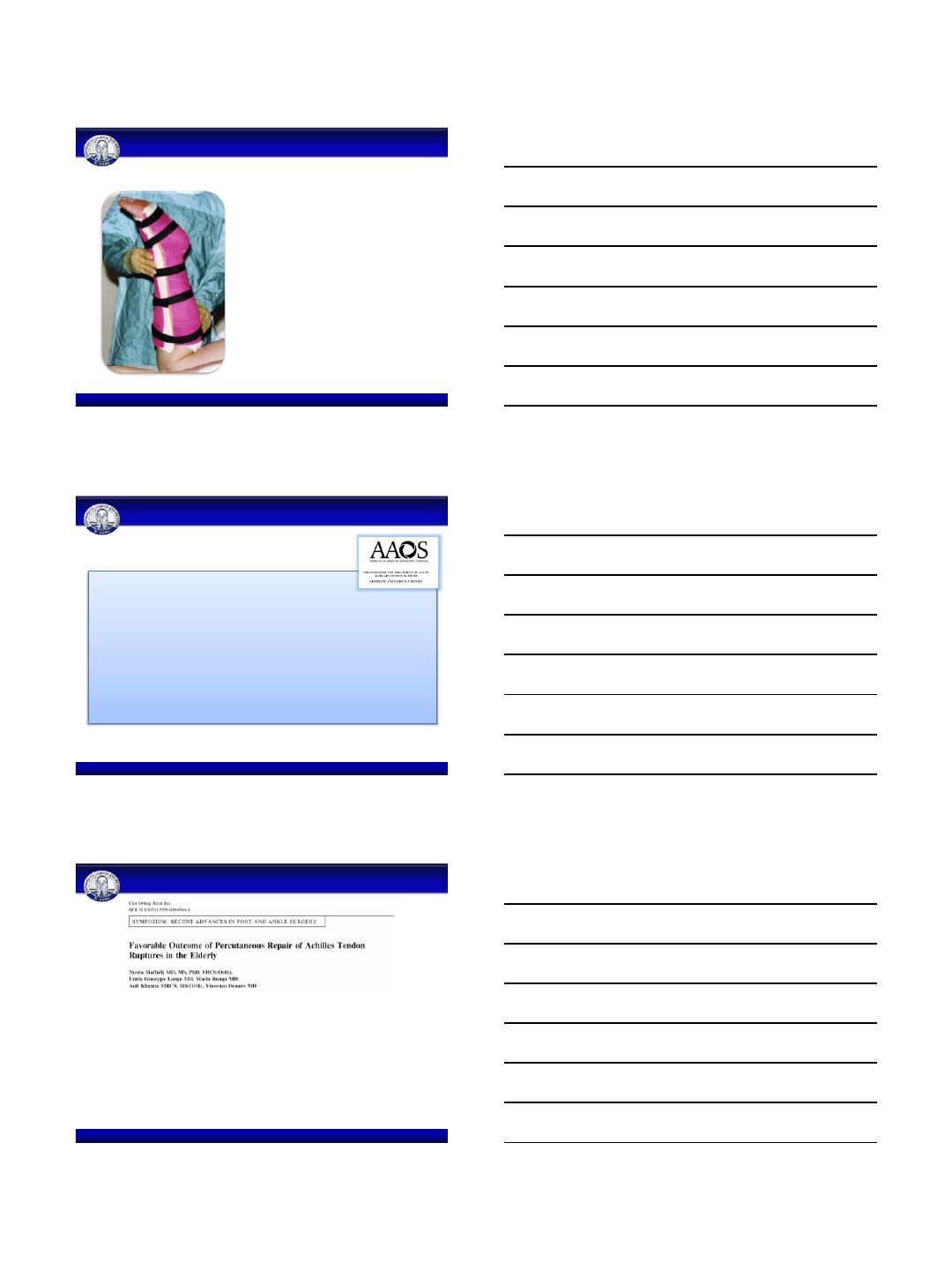
•At 2 weeks, the back shell of
the cast is removed
•The front shell remains in
place for 6 weeks to prevent
forced dorsiflexion of the
ankle.
Carmont and Maffulli KSSTA (2008) 16:199-203
Percutaneous Achilles tendon repair
ATR Summary of Recommendations: number 6
•In the absence of reliable evidence, it is the opinion of the work group that
although operative treatment is an option, it should be approached more
cautiously in patients with diabetes, neuropathy, immunocompromised
states, age above 65, tobacco use, sedentary lifestyle, obesity (BMI >30),
peripheral vascular disease or local/systemic dermatologic disorders.
•Strength of Recommendation: Consensus
Percutaneous Achilles tendon repair
Maffulli N, Longo UG, Ronga M, Kha nna A, De naro V CORR 2011
•26 men and 9 women with a mean age of 73.4
•Follow up 49 months
•The ATRS had a postoperative average rating of 69.4 ± 14 (range, 56–93)
•Two patients experienced a re-rupture (protected the operated limb in the cast
for only 2 and 4 weeks after surgery, respectively)
5/20/2013
6
•3 patients had superficial infection
•3 patients had hypesthesia over the area of
distribution of the sural nerve
•The hypesthesia resolved over 6 months in two
of the three patients.
•In the third patient, the hypesthesia persisted
but did not interfere with the patient’s
activities of daily living or with the wearing of
shoes
Percutaneous Achilles tendon repair
Maffulli N, Longo UG, Ronga M, Kha nna A, De naro V CORR 2011
•39 subjects
•ATRS score: post-operative average rating of 70.4 ± 13 (range 55–
92).
•All patients were able to fully weight bear on the operated limb by
the end of the eighth post-operative week.
•Eight patients suffered from a superficial infection of the surgical
wound.
Percutaneous Achilles tendon repair
Maffulli N, Longo UG, Maffulli GD, Khanna A, De naro V AOTS 2011;131(1):33-8
•Seventeen elite athletes
•Average time to return to full sport participation was 4.8 ± 0.9
months
•Two of the 15 elite athletes on whom we have full data suffered
from a superficial infection of the surgical wound
Percutaneous Achilles tendon repair
Maffulli N, Longo UG, Maffulli GD, Khanna A, De naro V FAI 2011;32(1):9-15
5/20/2013
7
Conclusions
•Similar results to those obtained with open surgery
•Decreased perioperative morbidity
•Decreased duration of hospital stay
•Reduced costs
•Randomized controlled trials are required
Percutaneous Achilles tendon repair
Umile Giuseppe Longo - Email: ug.longo@gmail.com
University Campus Bio-Medico of Rome
Department of Trauma and Orthopaedic Surgery