Cemented Vs Cementless TKA Syllabus
2013-07-09
: Pdf Cemented Vs Cementless Tka Syllabus Cemented_vs_Cementless_TKA_Syllabus 7 2013 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 80
7/7/2013
1
The Rationale and
Registry Data for
Cemented TKA
Michael J Dunbar MD, FRCSC, PhD
Professor of Surgery
Professor of Biomedical Engineering
Professor of Community Health and Epidemiology
Dalhousie University
Halifax, Nova Scotia
CANADA
Disclosures
Consultancy/Royalties
•Stryker
Boards
•Editorial Board, JBJS Br
•Editorial Board, The Journal of
Knee Surgery
•Medical Advisory Committee,
Arthritis Society of Canada
•Halifax Biomedical
Institutional/Research Support
•Canadian Institute of Health Research
•Atlantic Innovation Fund
•Natural Sciences and Engineering
Research Council of Canada
•Stryker
•Wright Medical
•Depuy
•Smith and Nephew
•Zimmer
Femoral Fixation (Hip) by Country 2010
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
USA Canada Denmark UK Norway Sweden
Cemented
Uncemented

7/7/2013
2
TKA Fixation by Country
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Hybrid
Cementless
Cemented
The Planar Surface of the Tibial
Cut is the Weak Link
Rationale for Cemented TKA
1. Improved initial fixation
2. Accommodate for small bone defects and
imprecise cuts
3. Lower Costs
7/7/2013
3
Rationale for Cemented TKA
1. Improved initial fixation
Leif Ryd
7/7/2013
4
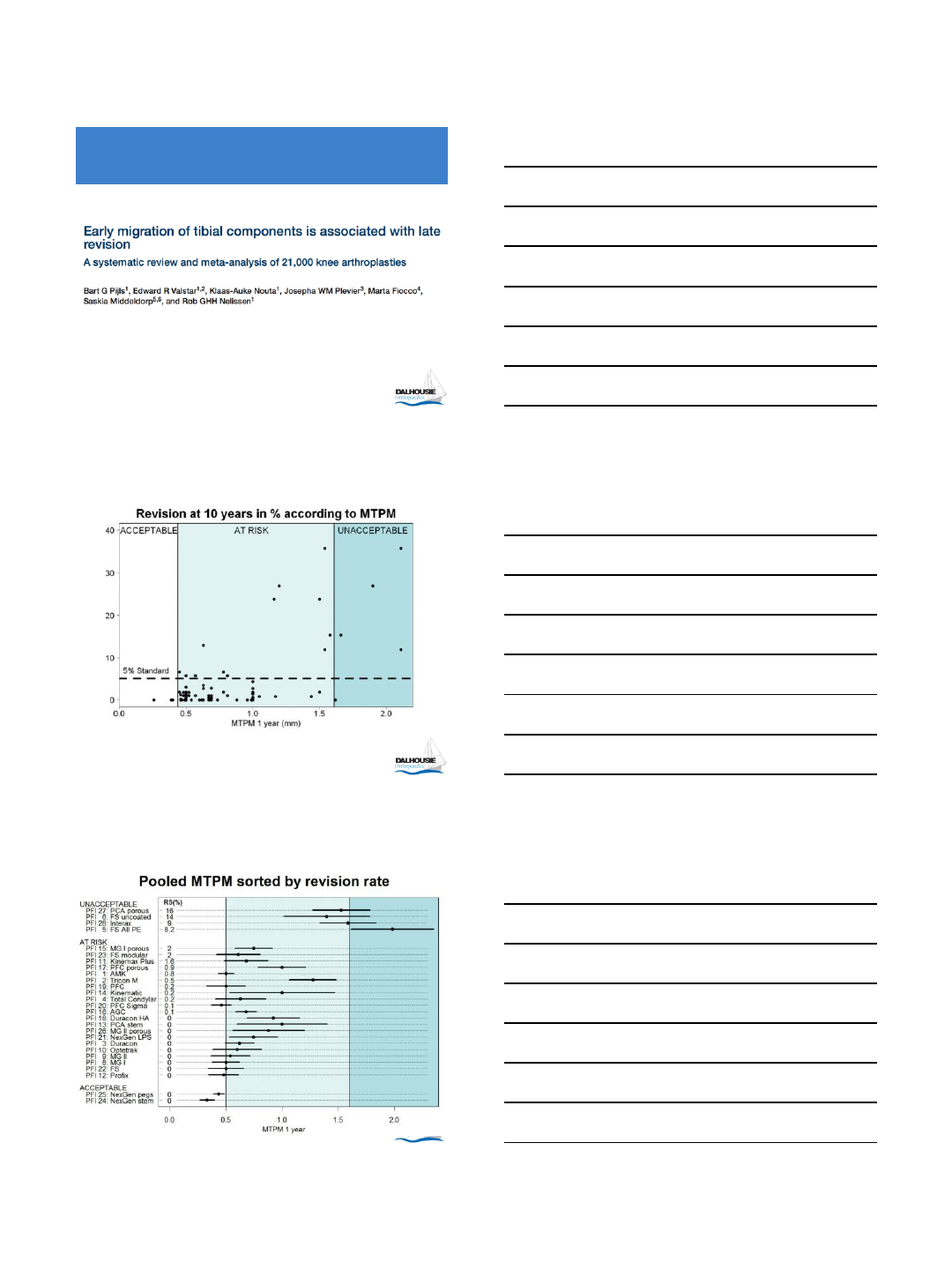
RSA Linked to Registry Data
7/7/2013
5
7/7/2013
6
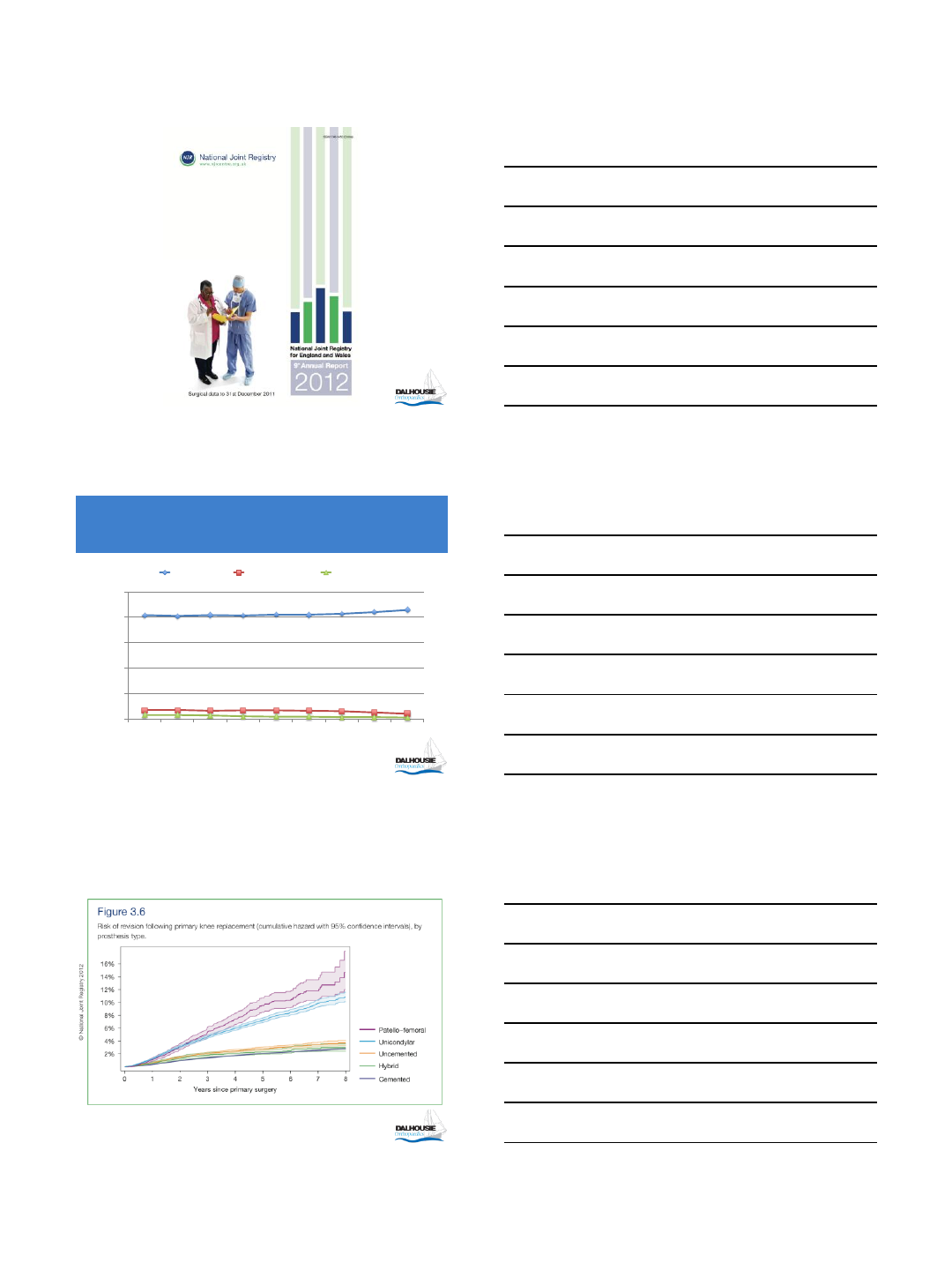
TKA Fixation Rates in UK by Year
0
20
40
60
80
100
1 2 3 4 5 6 7 8 9
Cemented Uncemented Hybrid
2003
2004
2005
2006
2007
2008
2009
2010
2011
7/7/2013
7
Patient Time Incidence Rates per
1,000 Years
Fixation Rate
Cemented 0.98
Uncemented 1.99
Hybrid 1.31
7/7/2013
8
Conclusions
•Cemented fixation in TKA offers advantages in
initial fixation
•Initial fixation is critical for TKA survivorship
•Cemented TKA is the gold standard in
registries around the world
7/7/2013
9
10 Year % Change in
Knee Cases
0
50
100
150
200
250
300
350
<45 45-54 55-64 65-74 75-84 85+ Total
Males Females
87%
>300%
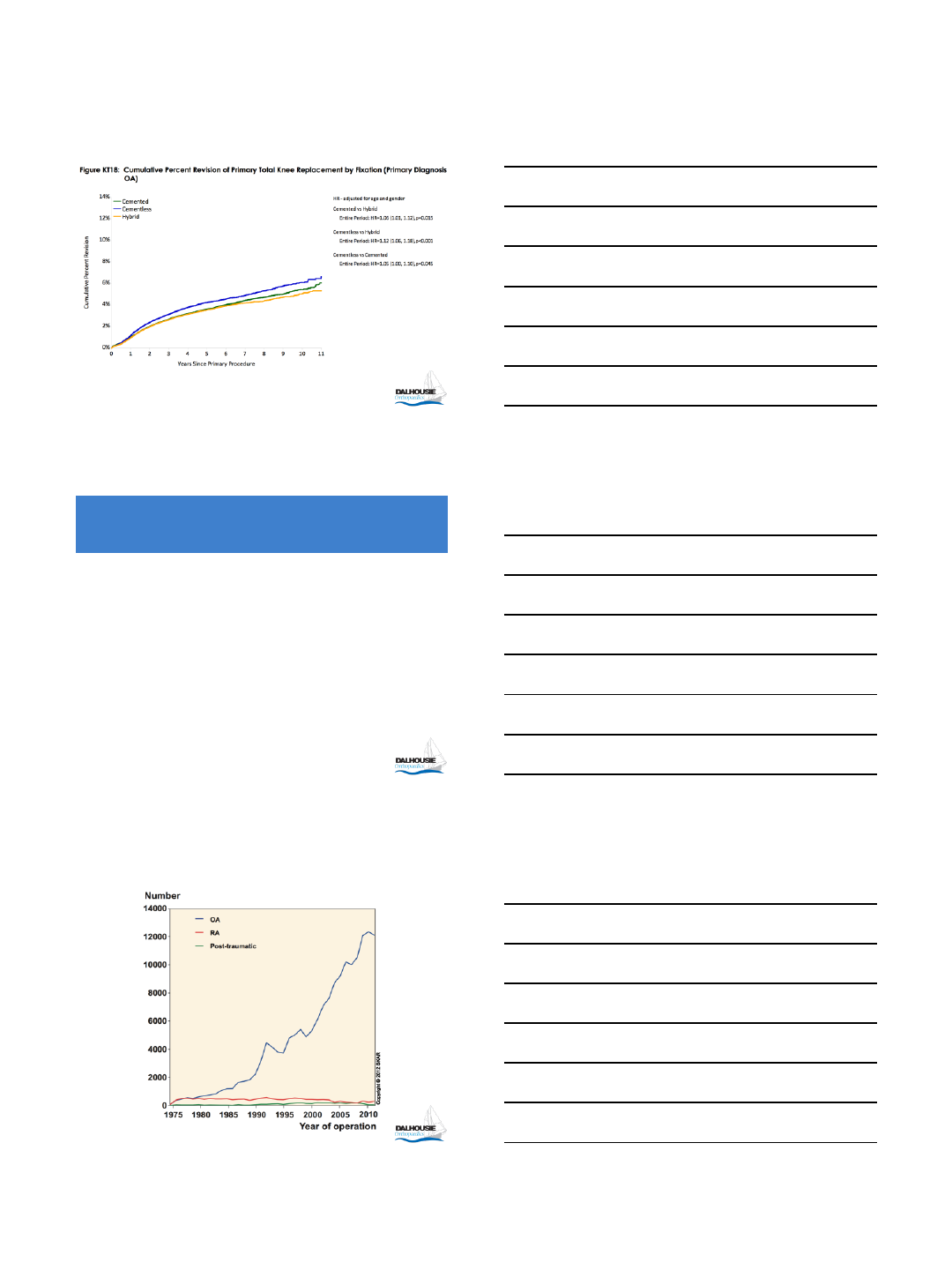
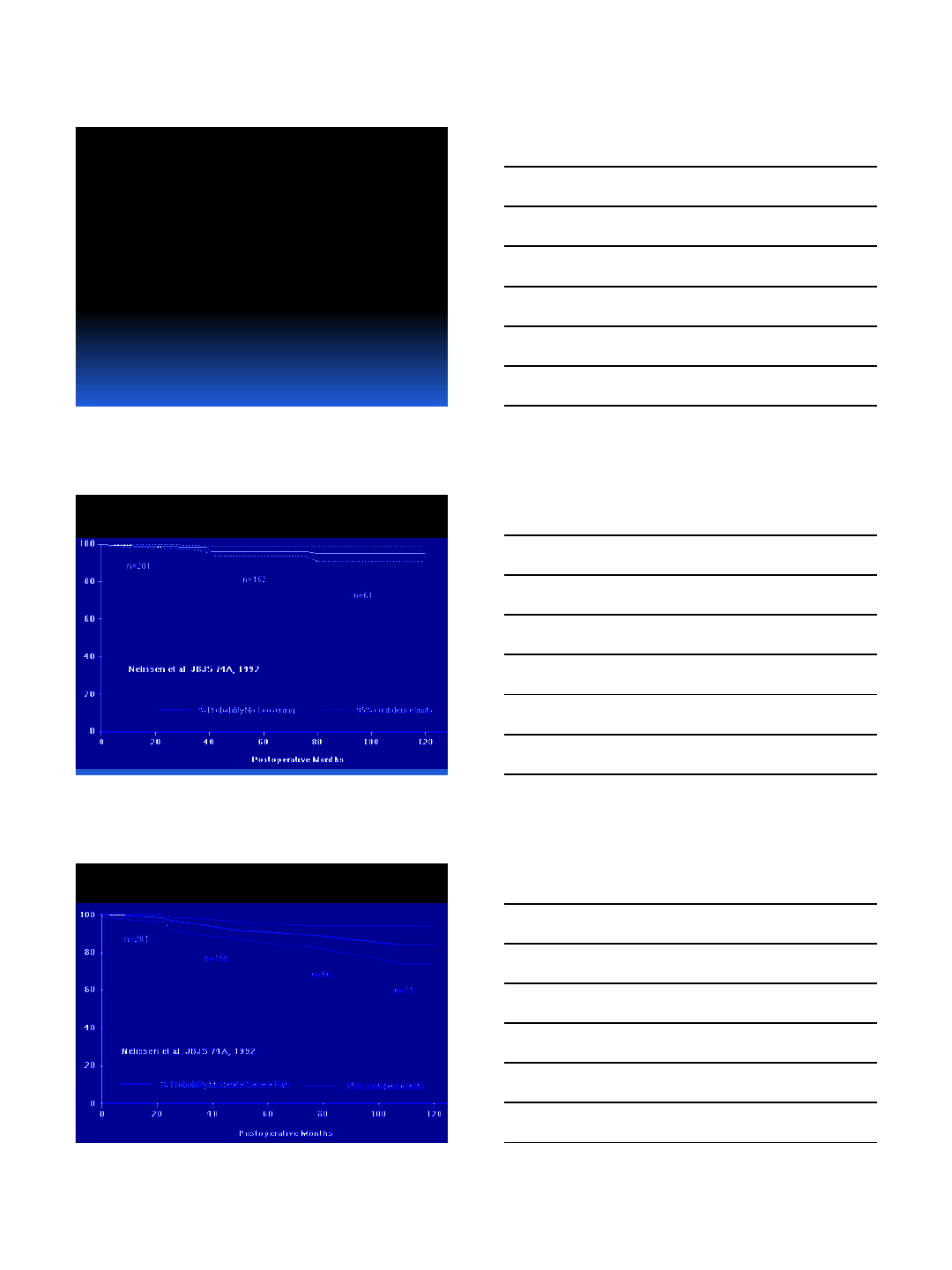
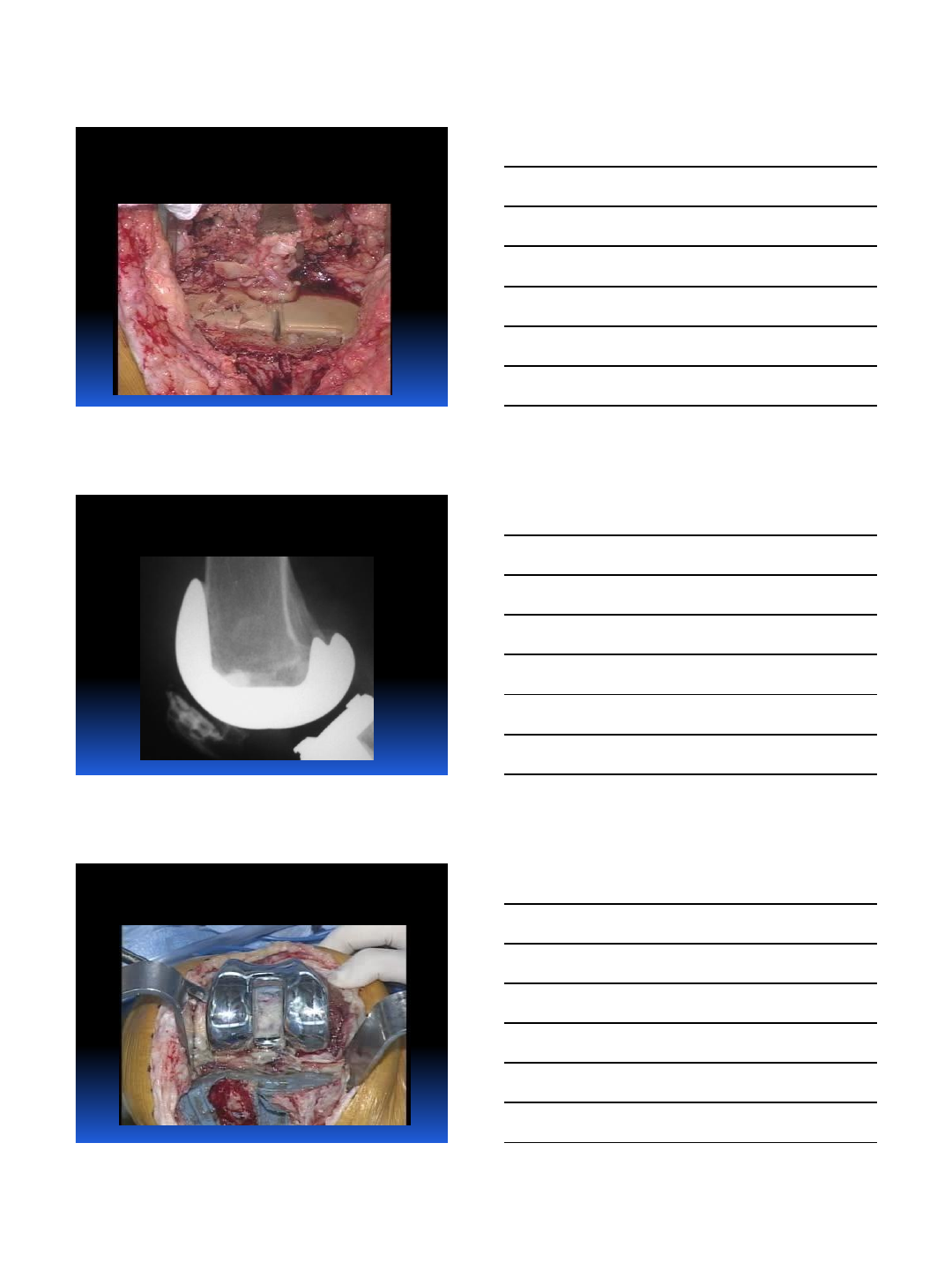
Cochrane Review 2012
•5 RCT’s on 297 patients
•RSA as Outcome
–MTPM and Object Based
RSA Outcomes of Tibial
Components at 2 Years
•Cemented Fixation = Smaller Displacement
•with and without hydroxyapatite
•MTPM (N = 167) mean difference = 0.52 mm
•95% confidence interval 0.31 to 0.74

7/7/2013
10
However - Future Risk?
•the risk of future aseptic loosening with
uncemented fixation was approximately half
that of cemented fixation according to the
arthroplasty instability classification
–RR 0.47, 95% CI 0.24-0.92
–16% absolute risk between groups
Future Risk for Revision (OA)
•Uncemented Fixation
–Thirteen people out of 100 had a future prediction
of arthroplasty instability.
•Cemented Fixation
–Twenty-nine people out of 100 had a future
prediction of arthroplasty instability with
cemented fixation.
Contemplation Before
Surgery
Joseph R. Wilder, MD
1
1
Cementing the Perfect TKA:
Assuring Longevity
Chitranjan S. Ranawat*, MD
Amar S. Ranawat**, MD
*Professor of Orthopaedic Surgery
**Associate Professor of Orthopedic Surgery
Weill Cornell Medical College
Hospital for Special Surgery
New York, NY
2
Disclosures
Chitranjan S. Ranawat, MD
Hospital for Special Surgery
Royalty and Research
Support Received From:
Stryker
DePuy
Family member consultant & Research:
Conformis
CeremTec
ConvaTec
Medtronic
Pipeline
Mako
3
•Evidence for superiority of
cemented fixation in TKR
over non-cemented fixation

2
4
Level of evidence to support cemented
fixation in TKR
Level I: Registry Data and Prospective Randomized
Study
Level II: Meta Analysis
Level III: Prospective Case Control
Level IV: Case Series
Level V: Opinion of Individual Surgeon
5
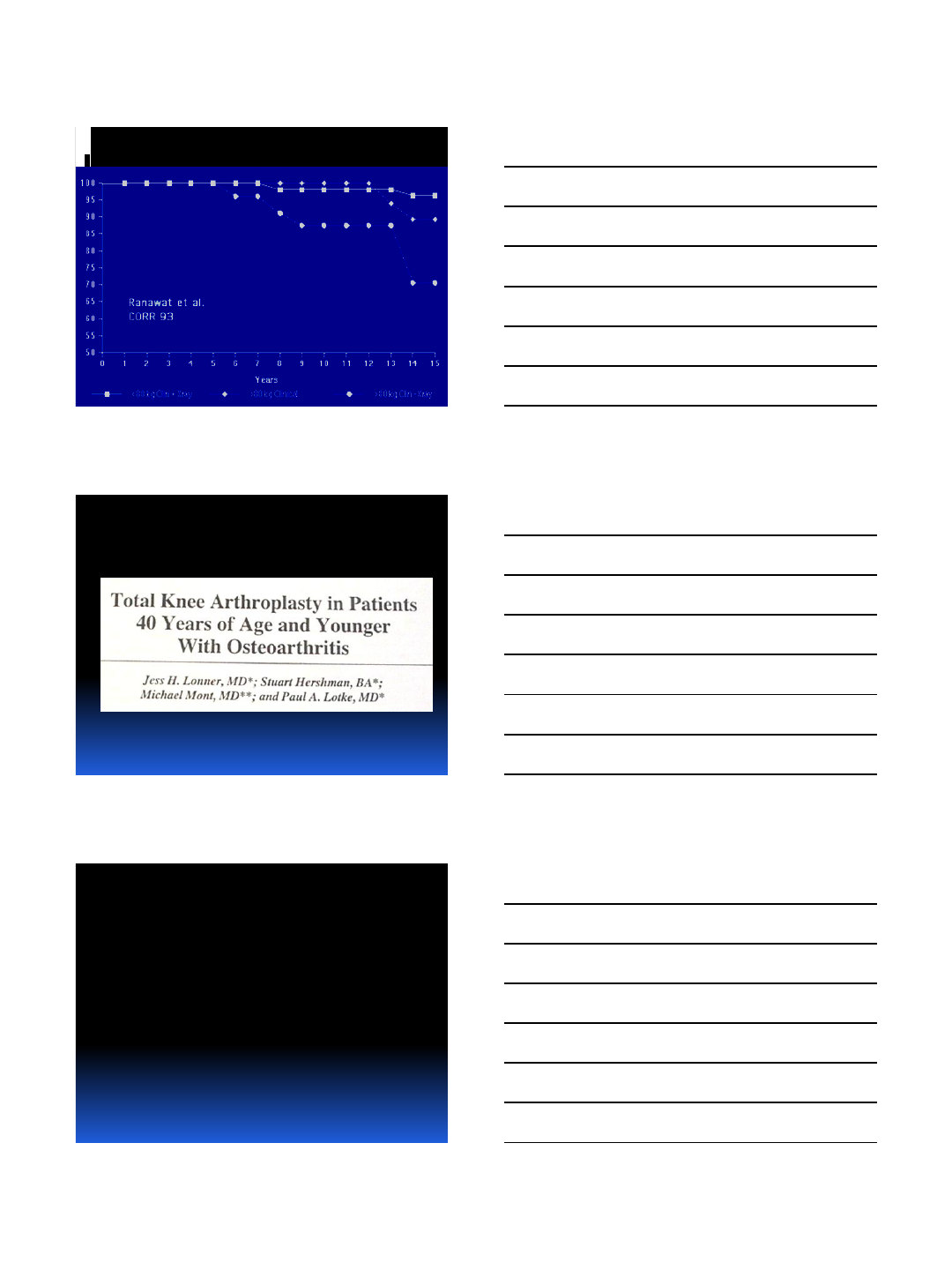
Survivorship for mechanical
fixation failure
6
Survival of Total Condylar Prosthesis
20-Year Follow-up
Mechanical Failure
0
10
20
30
40
50
60
70
80
90
100
110
0 2 4 6 8 10 12 14 16 18 20
TCP 220
% Survival
Ranawat et al, CORR, 2001
3
7
Survivorship for Mechanical Failure:
Literature Review
89 - 98% at 15 - 20 years
Lachiewicz et al, JBJS 2009
Abdeen et al, JOA 2009
Callaghan et al, JBJS 2005
Dixon et al, JBJS 2005
Buechel et al, J Knee Surg 2002
Ranawat et al, CORR 2001
Font-Rodriguez et al, CORR 1997
Ritter et al, CORR 1995
Ranawat et al, CORR 1993
8
Ranawat CS, JBJS, 2012
10 year Survivorship- RP-PS
9
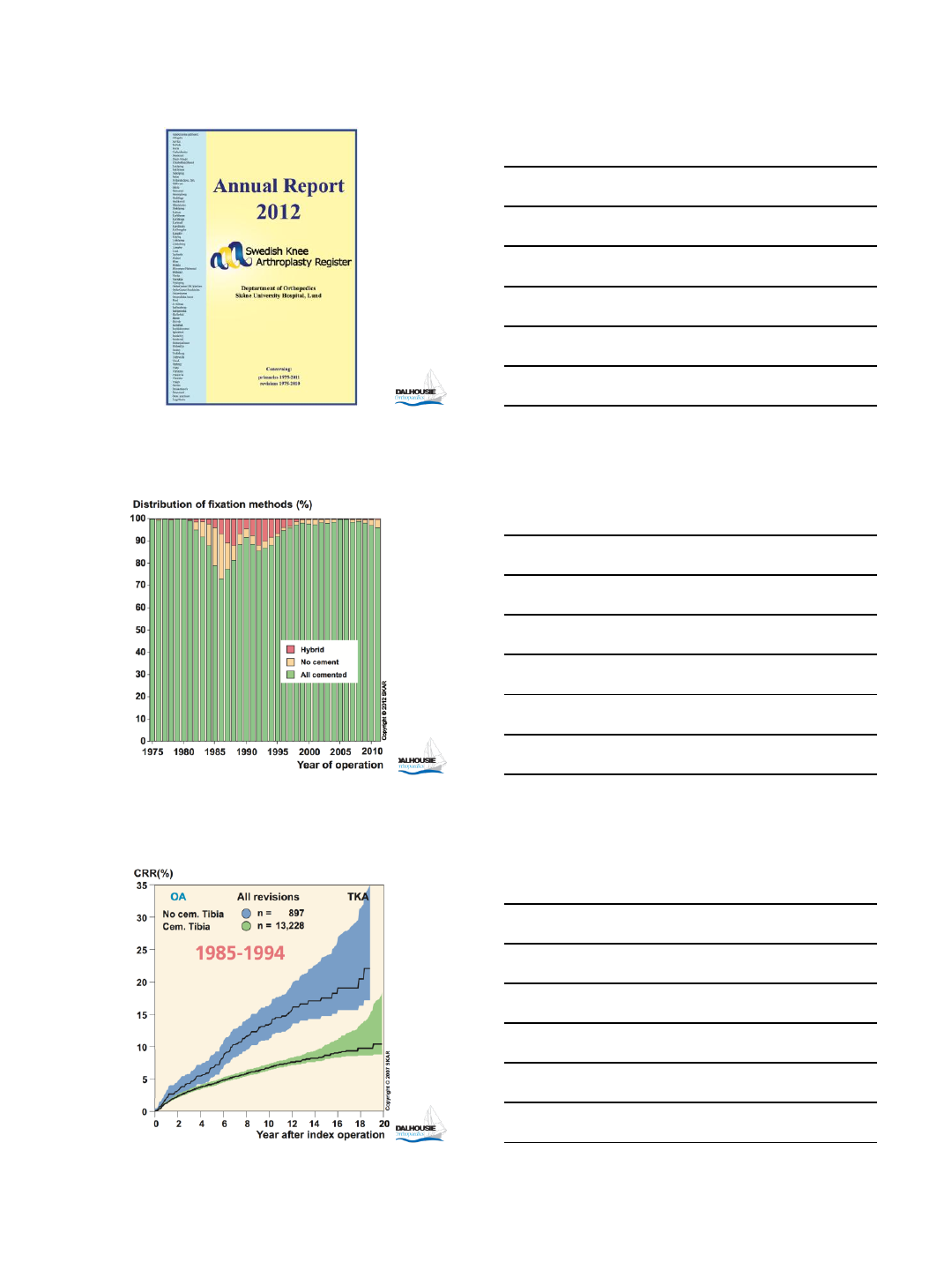
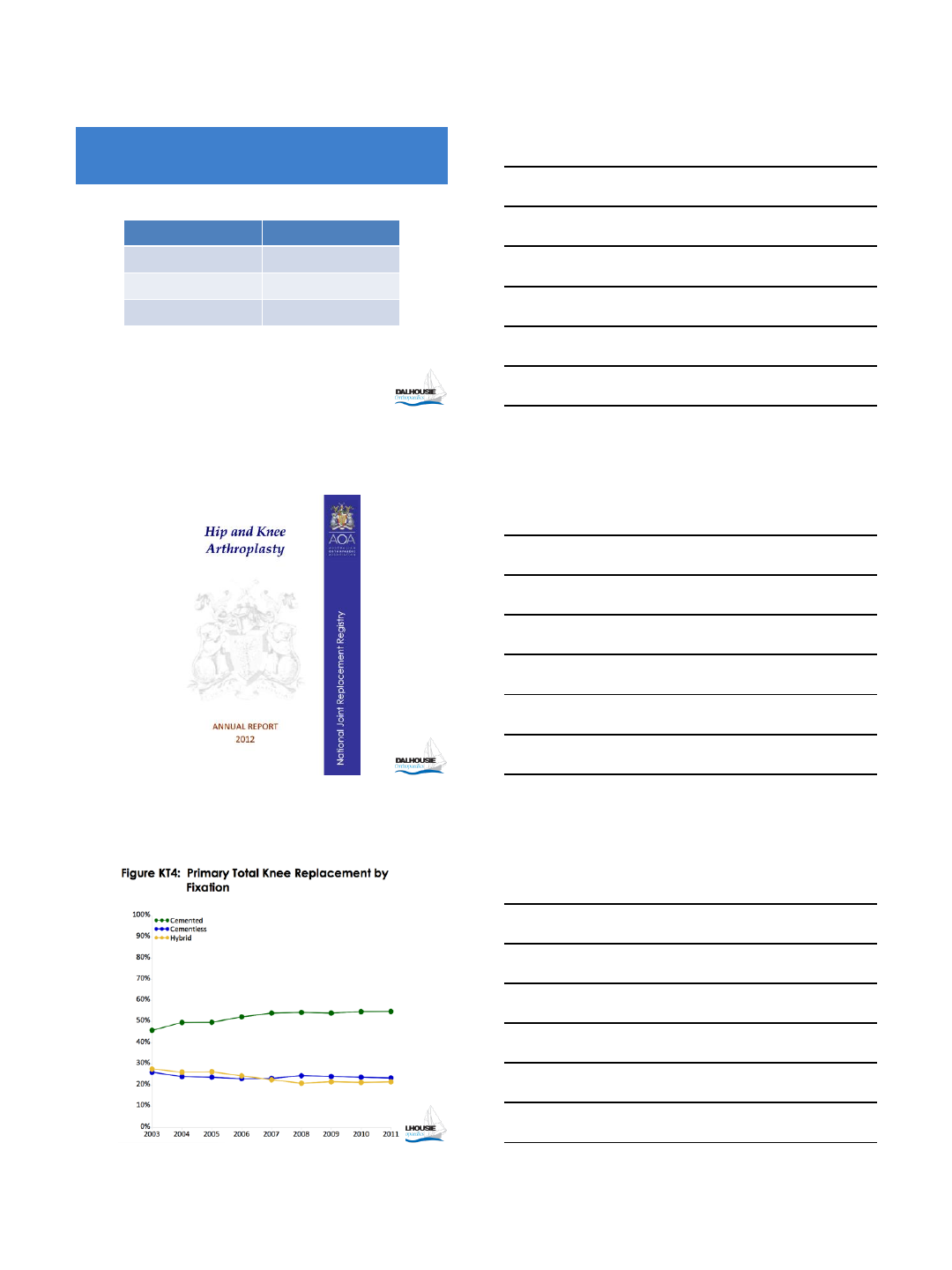
Registry Failure Rate (%)
NJR-England C: 3.81
NC: 4.75
Australian C: 5.6
NC: 6.2
Swedish (up to 1994) C: 9
NC: 23
New Zealand C: 4.28
NC: 6.93
Level I Evidence: Registry Failure Rate
4
10
Registry Usage (%)
NJR-England C 85
NC 5
Australian C 55
NC 29
Swedish (up to 1994) C 95
NC 3
New Zealand C 89
NC 4
Level I Evidence: Registry Data on Usage
11
Level I Evidence:
Prospective Randomized Study
Author/Journal/year Follow-UP
(Years) Conclusion
Park et al, JBJS-Br,
2011 14 For Cemented
Baker et al, JBJS
2007 15 For Cemented
12
Level II Evidence:
Meta Analysis
Gandhi et al. JBJS 2009
Improved survivorship of cemented
Knee
5
13
Discussion
•Although results for non-cemented
fixation in TKR are improving, level I,
II and III evidences are still in favor of
cemented fixation
14
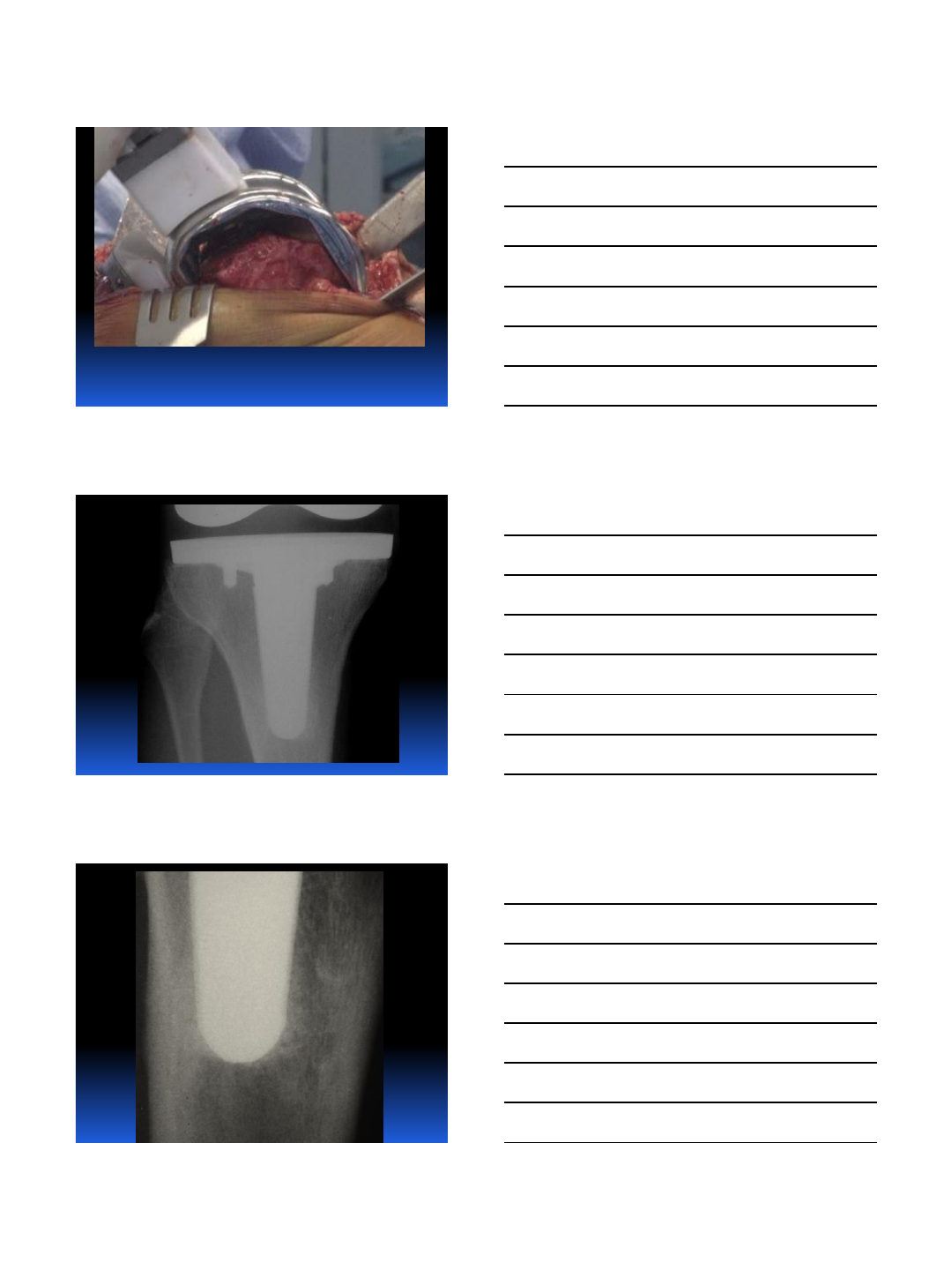
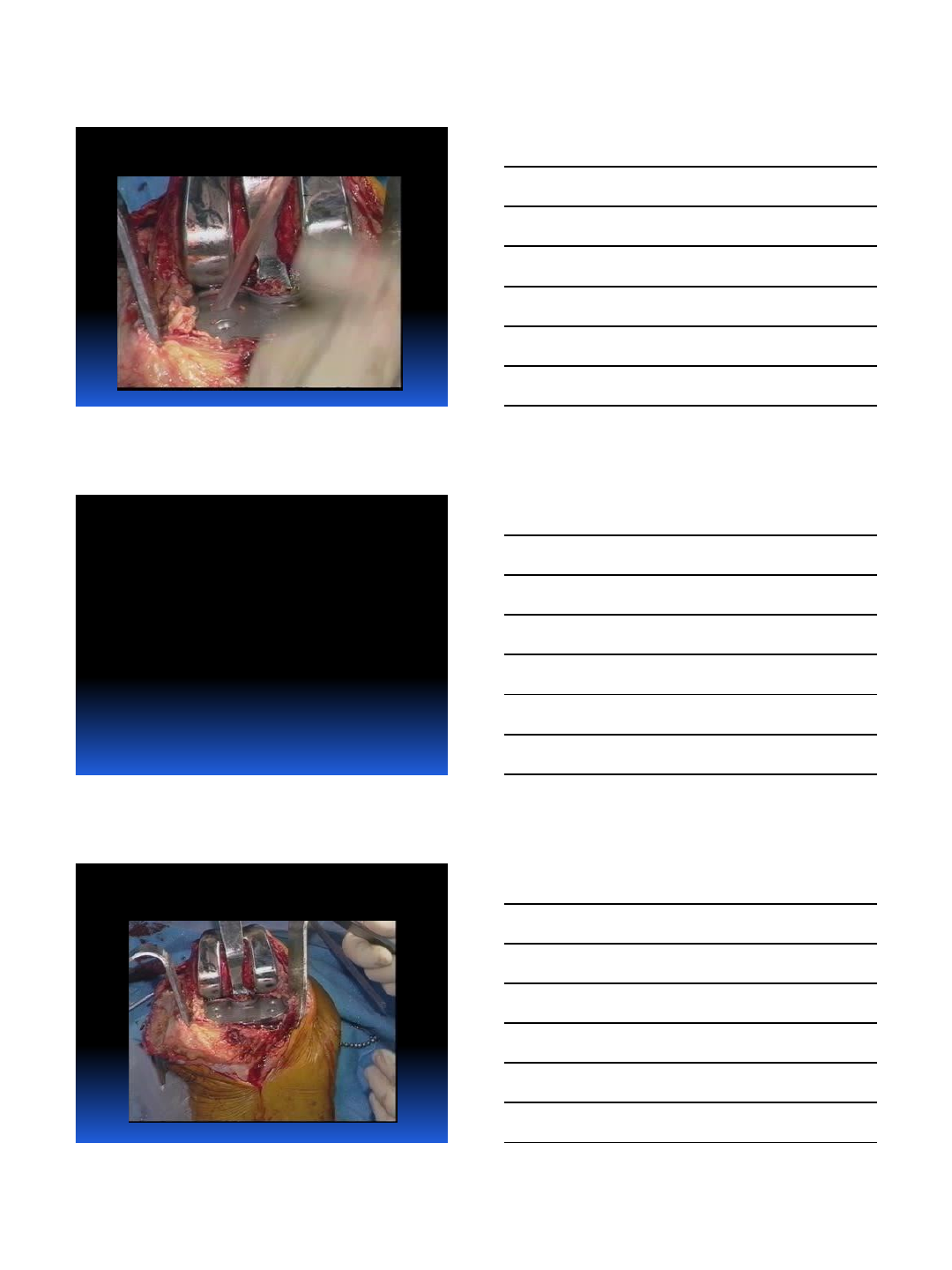
Technique
1. Proper exposure with adequate length of incision
2. Avoid cutting the quadriceps tendon in oblique direction
(medial-lateral plain)
3. Reduced Tissue Trauma Surgery (RTTS), no tourniquet
except for cementing
4. Deliver the tibia in front of the femur (Ran-Sal maneuver)
5. Preserve supra-patellar pouch, coagulate lateral genicular
artery
6. 8 to 10 mm tibial cut from the uninvolved side, identify the
cortex off the tibial cut
7. Adequate rotation, alignment, lateralization and restoration
of the posterior offset of the femoral component
15
Technique
8. Pulsatile lavage the cut surfaces to clean the cancellous bone
9. Drill holes in the sclerotic bone surface
10.Heated Simplex cement at doughy state
11.Apply cement on the bone surfaces including posterior femoral
condyles and pressurize, apply cement on the components as
well
12.Apply manual constant pressure
13.Remove excess cement from posterior femoral condyles, tibia
and patella (if resurfaced)
14.Further pressurization in extension with trial insert
15.Release the tourniquet and thorough irrigation
16.Closure in flexion without tourniquet and with good
approximation of dermal layer
6
16
17
Conclusion
Cemented fixation remains the
“Gold Standard” in TKR at
present
18
“All good things
ultimately prevail”
CSR
7
19
Thank you!
7/8/2013
1
7/8/2013 1
Best Available Evidence for Cementless TKA
R. Michael Meneghini, MD
Director, IU Joint Replacement Fellowship
Indiana University School of Medicine
•Consulting Payments and Royalties:
• Stryker
•Research Support:
• Stryker
•Fellowship Funding:
• OREF
•Editorial Boards:
• J Arthroplasty
• JBJS Knee Newsletter
Disclosures
Fixation in Total Knee Replacement
•Cement Fixation: “The Gold
Standard”
–Reliable long-term results
•Uncemented Fixation Increasing
•Cementless Fixation is more
biologic
Eventually “The Gold Standard”
7/8/2013
2
Cemented TKR: “The Gold Standard”
•85% Survivorship at 21 years1
–Cemented Total Condylar
–Mean Age = 65 years
–95% survivorship at 15 years !
•98% Survivorship at 20 years2
–Cemented AGC
–Mean Age = 70.4 years
1. Ranawat CS, et al.
CORR
, 1993;286: 94-
102.
2. Ritter MA, et al.
CORR
, 2001;388: 51-7.
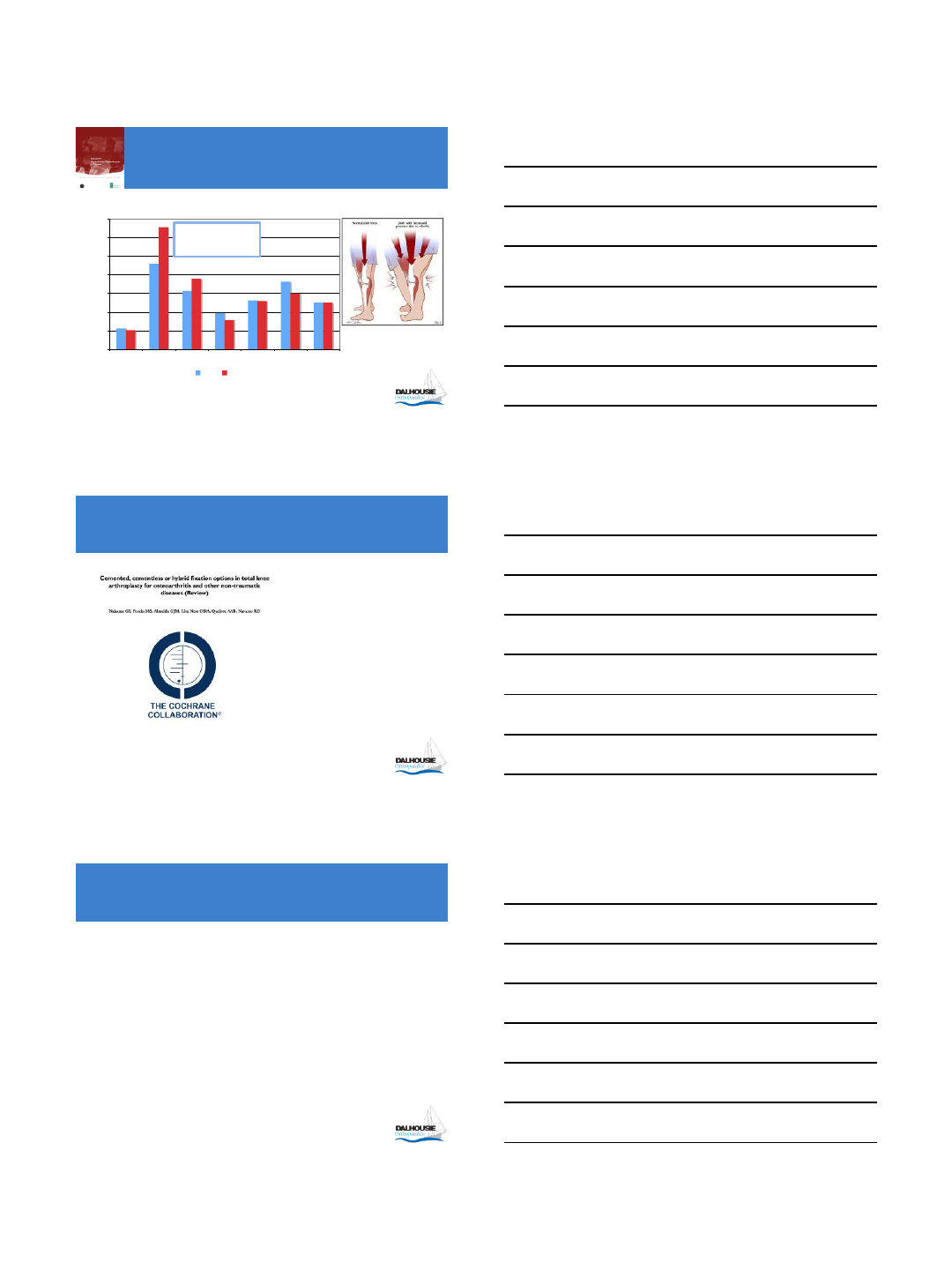
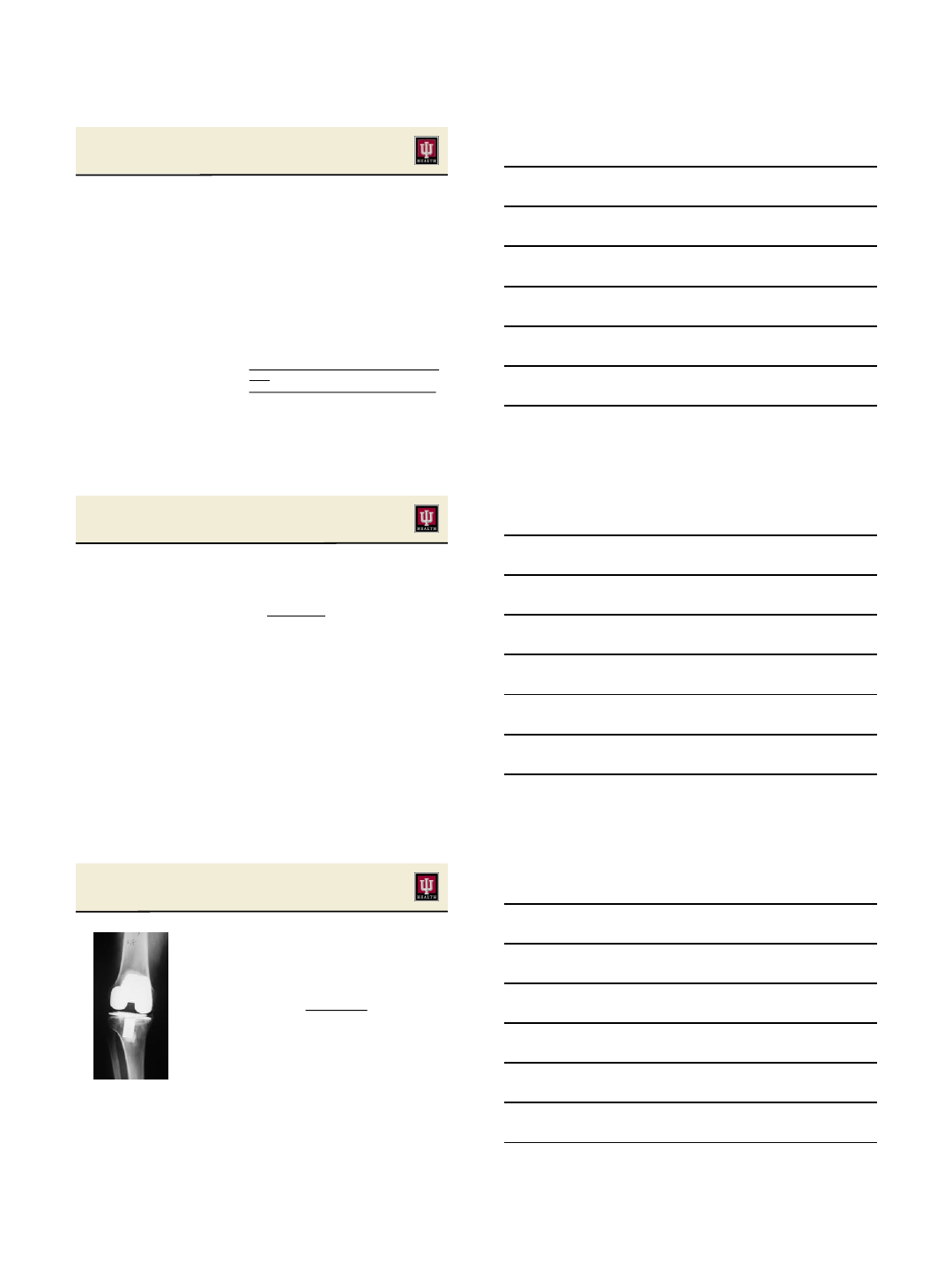
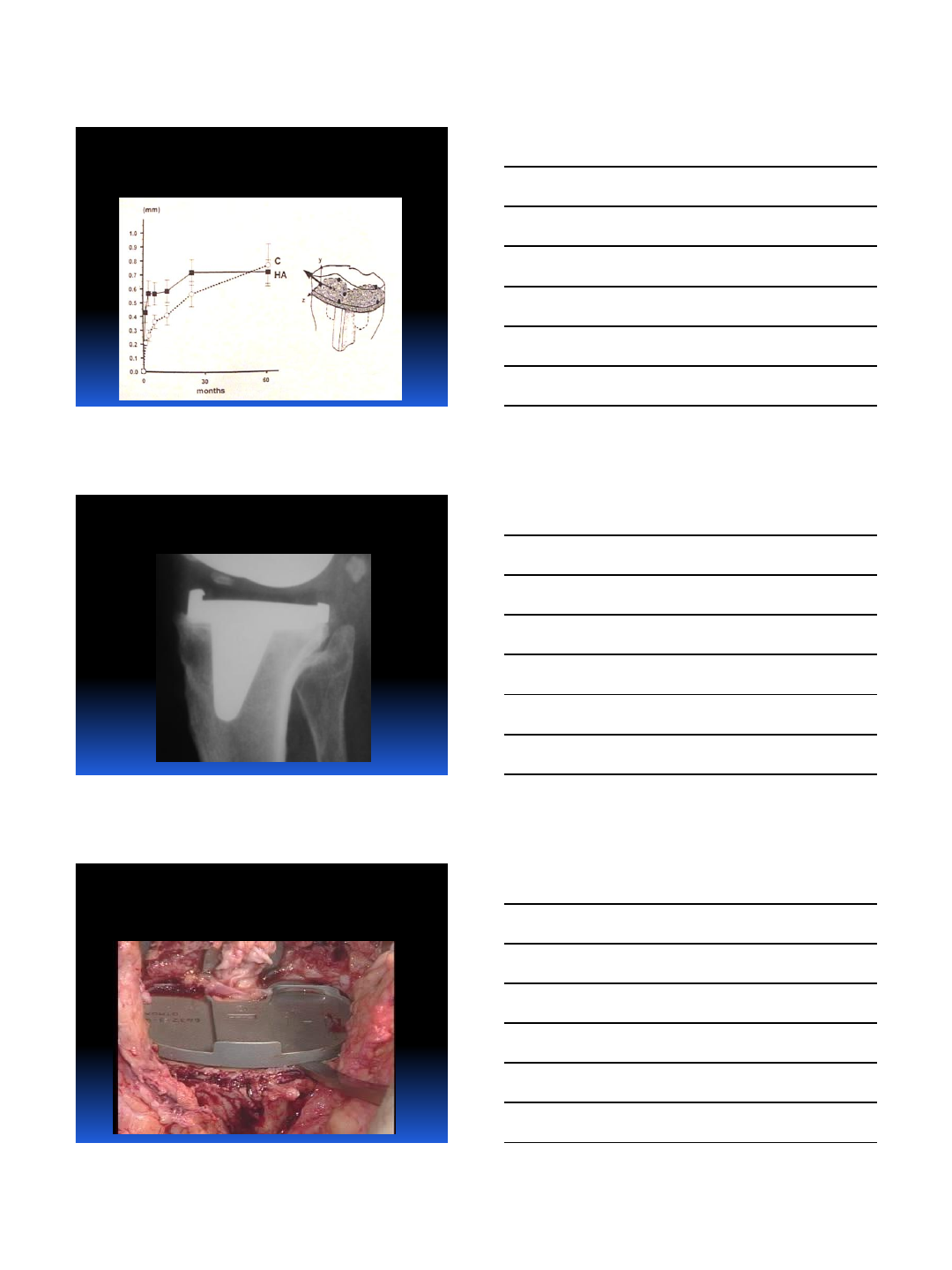
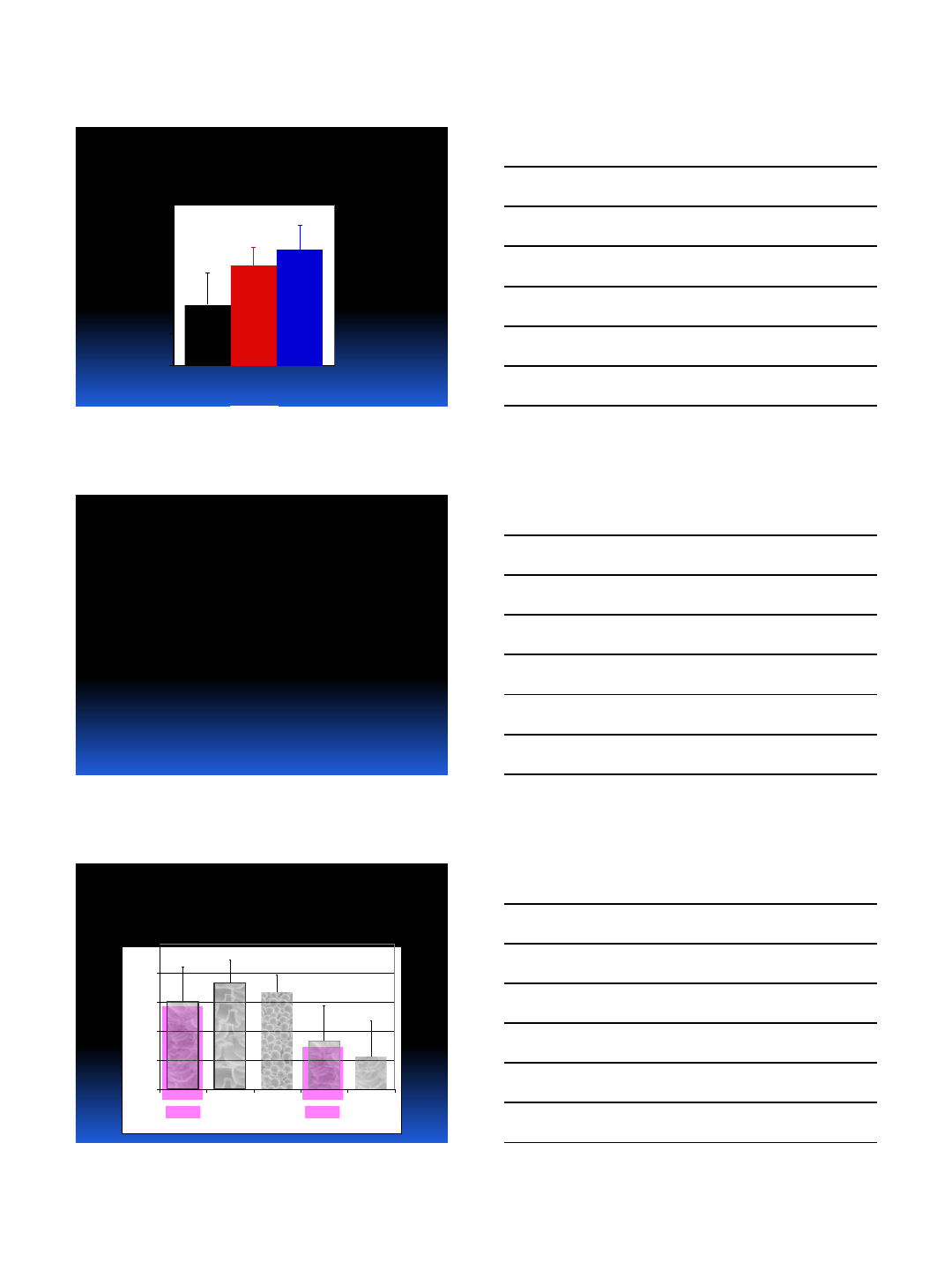
Cemented TKR: Young Patients
•Younger age at TKR = lower survival rate
–Gioe et al
CORR
2004
•Cemented TKR patients under 55
–Survival rates from 85-95% at 10-18 years
–Better for RA versus OA
–Concern regarding survivorship past 15 years
•TKR in younger patients increasing !!
–Greatest increase in <65 and <45 year-old groups
–Kurtz et al.
JBJS-Am
July 2005
Cement in TKR
•Additional interface to fail
•3rd body wear-failure mode
•Most durable long-term fixation
is osseointegration
•Increasingly, surgeons are
eager to embrace
7/8/2013
3
Why Cementless TKR ?
•Patients younger & more active
•Demand for OR efficiency
•Established long-term success via biologic fixation
•Past problems identified and correctable
•Improved biomaterials for fixation and wear
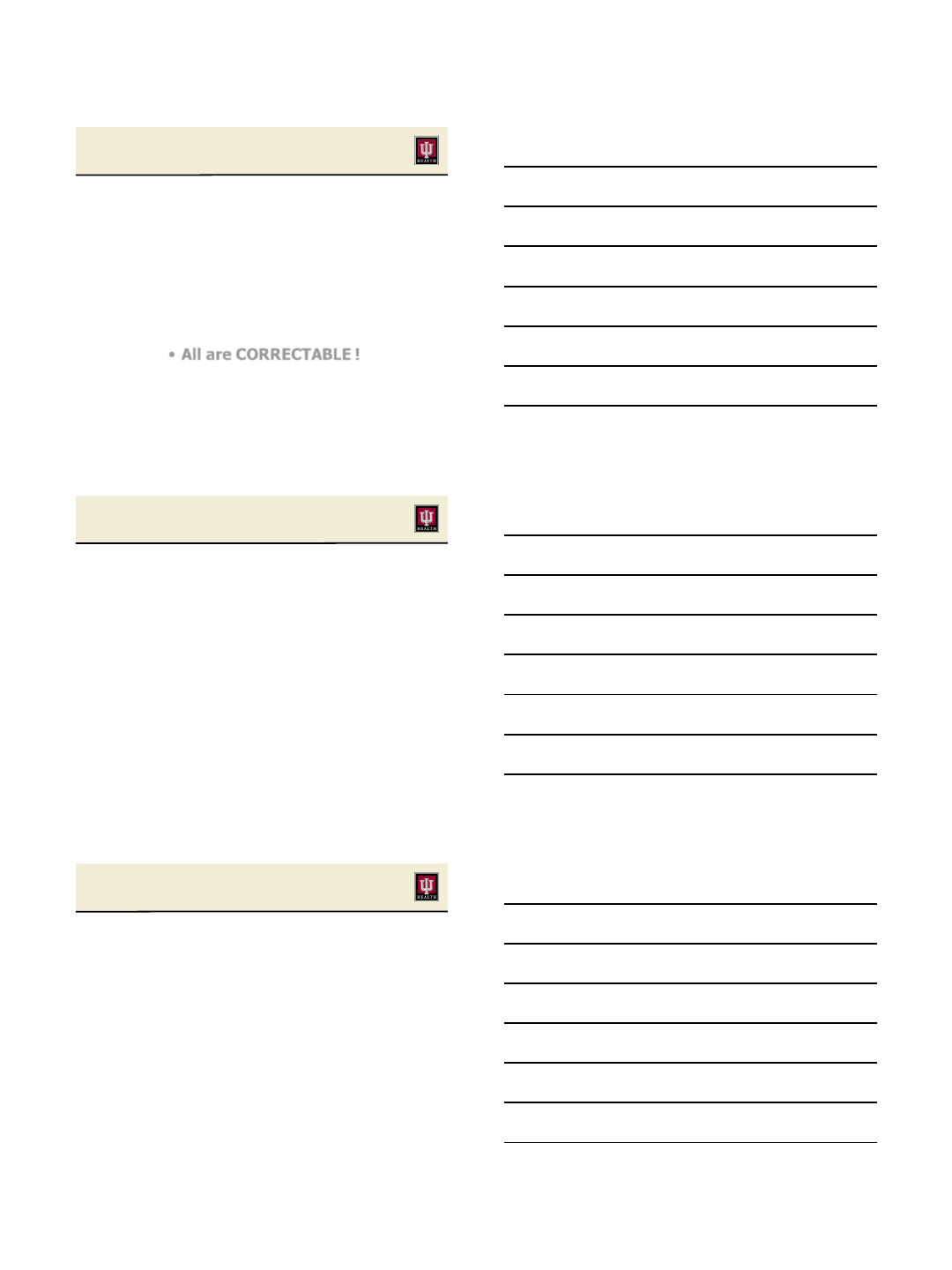
Cementless Fixation: Hip Replacement
•
Cementless surpassed
Cement Fixation in 2000
0
50
100
150
200
250
Units
2003 2004 2005 2006 2007 2008 2009
Cement
Porous
Minimizing Surgical Time
•Need for increased OR efficiency
•Idle time in OR for curing cement
Inefficient and wasteful
Less surgical time decreases infection
•Decrease in TKR reimbursement
7/8/2013
4
Past Failures of Cementless TKR
•Patch porous coating
•Screw osteolysis
•Poor polyethylene / locking mechanism
•Fatigue failure of femoral components
•Failure of metal-backed patellar components
•All are CORRECTABLE !
Long-Term Cementless TKR
•Hardeman (2007) 10 yr – 97.1% ProFix
•Epinette (2007) 10 yr – 98.1% HA Omnifit
•Khaw (2002) 10 yr – 95.6% PFC
•Hofmann (2002) 10 yr - 99.0% Natural
•Schroder (2001) 10 yr - 97.1% AGC-2000
•Watanabe (2004) 13 yr - 96.7% Osteonics
Long-Term Cementless TKR
•Tai (2006) 12 yr – 97.5% HA
•Watanabe (2004) 13 yr - 96.7% Osteonics
•Goldberg (2004) 14 yr - 99.0 % MG-I
•Tarkin (2005) 17 yr - 97.9 % LCS-RP
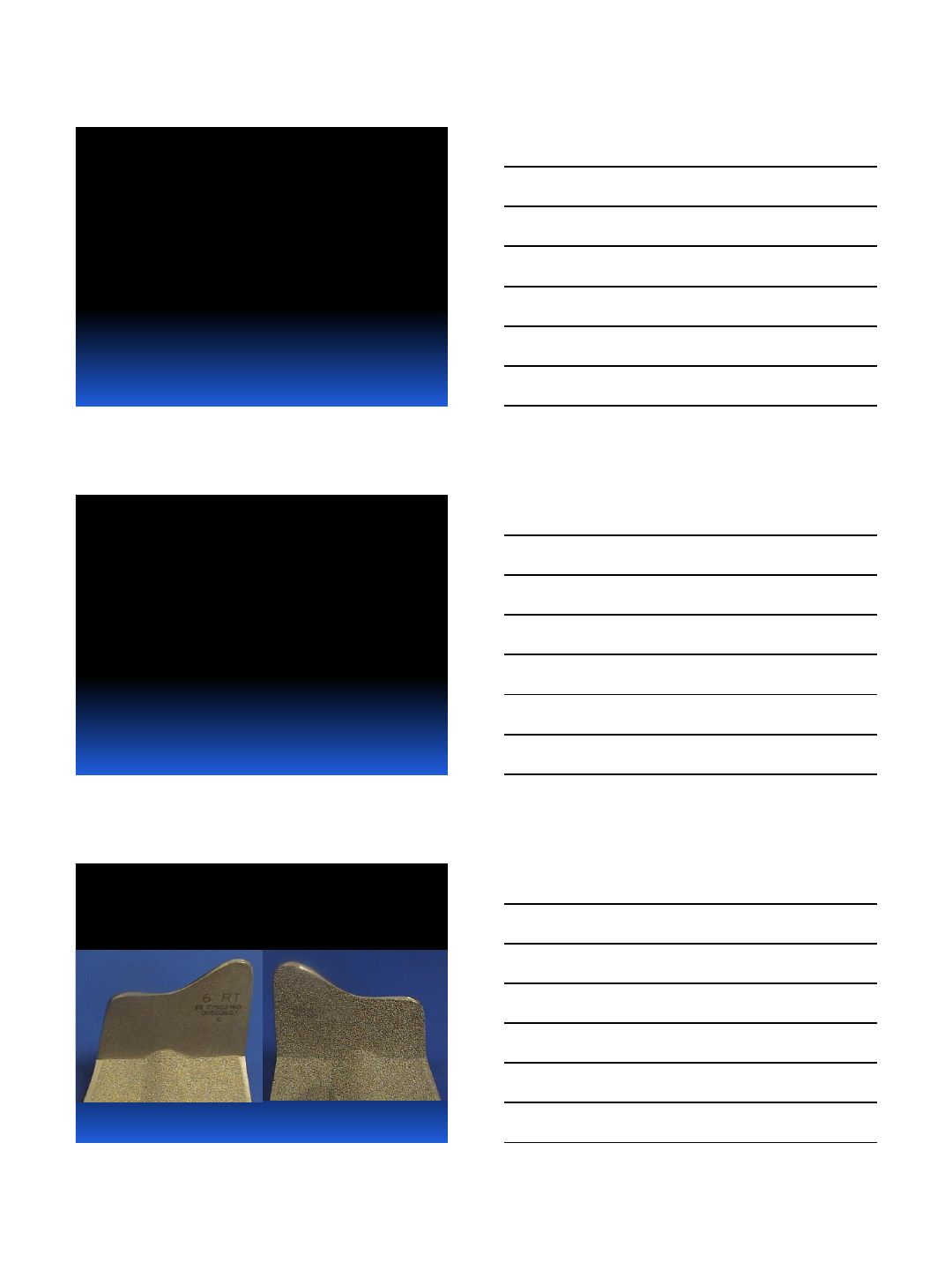
•Whiteside (2002) 18 yr - 98.6% Ortholoc-I
•Buechel (2002) 20 yr - 97.7% LCS-RP
7/8/2013
5
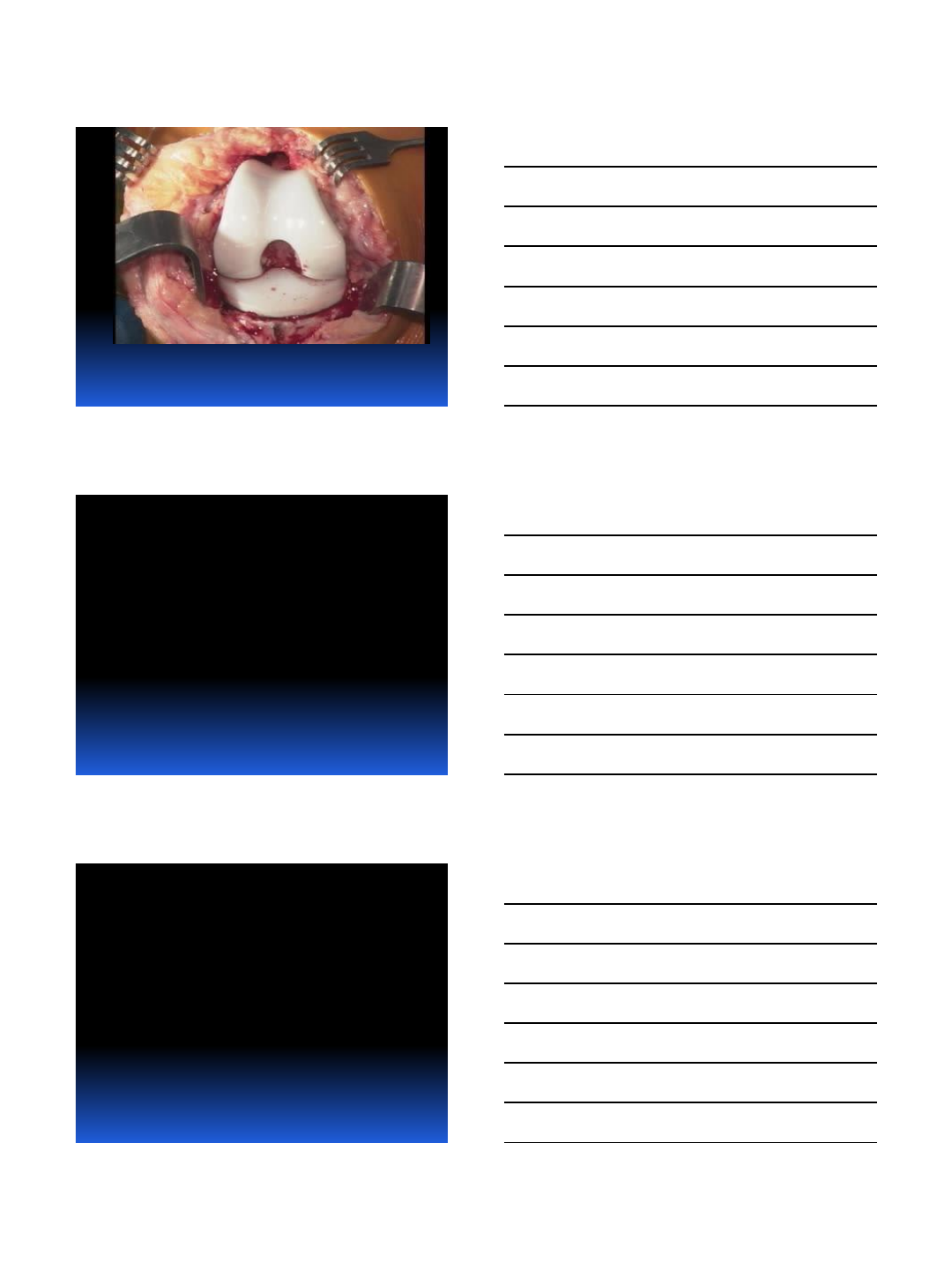
Long-Term FU Cementless TKR
•10 Year Follow-up: PFC Design
•Cementless (224) Cemented (277)
•95.6% 95.3%
Khaw FM, et al. JBJS 84-B:658, 2002
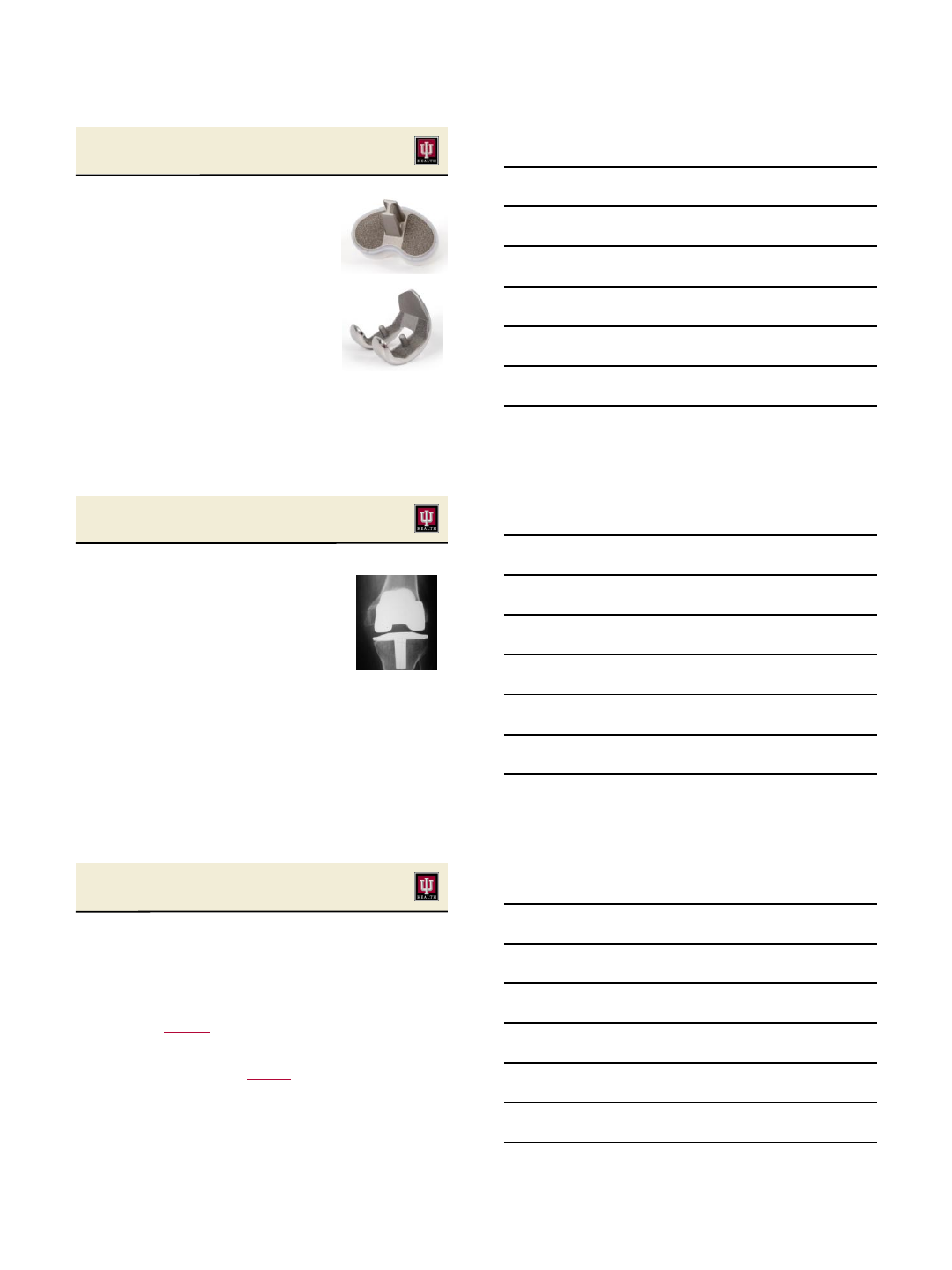
Cemented and Cementless AGC TKR
Kavolous, Ritter, et al CORR 1991
Cementless AGC TKR
Remove 12 Metal-Backed Patella Failures
Time (Years)
Survival Probability
0 5 10 15 20
0.2
0.4
0.6
0.8
1.0
Uncemented AGC
Survival Probability
5 Yr .9861
10 Yr .9675
15 Yr .9675
20 Yr .9675
Cementless AGC Knees n=73
Cementless AGC knees, n= 2 failures in 73 knees (2.7%)
7/8/2013
6
Cementless AGC at 20-Years
Ritter & Meneghini, J Arthroplasty 2010
• 1983 - 1986
• 73 Cementless AGC TKR
• No adjuvant screw-fixation
• Females: 58%
• Mean Age: 59 years (range, 18-
79)
• All minimum 10-Year Follow-up
• None Lost to Follow-up
• Minimum 20 Year Follow-up: 24
Cementless AGC at 20-Years
Ritter & Meneghini, J Arthroplasty 2010
• Two tibial aseptic failures
–
1.1 and 2.2 years
• 12 failed metal-backed patellae
• 97% Survivorship at 20 years
•Equal Survivorship as Cemented AGC
Younger patients by mean 11 years !
Cementless vs Cementless TKA
Nakama GY et al. Cochrane Database Review 2012
•5 RCTs, 297 patients
•Meta-Analyses of RSA data
•Greater displacement of uncemented TKA
compared to cemented
–Up to 2 years
–Mean 0.5mm max total point motion
•Cementless risk of future loosening one-
half that of cemented TKA
–Based on RSA inferred classification
7/8/2013
7
Improved Biomaterials
•Hydroxyapitite / Periapitite
•Porous Tantalum
•Highly porous Titanium
•Highly Cross-Linked Polyethylene
Cementless vs Cementless TKA
Bercovy M et al. JBJS-Br 2012
•157 cementless versus 146 cemented TKA
–Rotating Platform Bearing, HA-coated
•Mean follow-up 7.6 years (range, 5-11)
•After 3-months, no radiolucent lines in
cementless group
–p < 0.01
•Identical survivorship of 99% both groups
•Less operative time cementless TKA
–p < 0.006
Posterior-Stabilized Cementless TKA
Harwin et al, J Arthroplasty 2013
•Peri-apetite Coated
•Adjuvant Tibial Screw Fixation
•PS-Design
•114 TKRs, Mean age 62 years
•Mean 36-month follow-up
•No failures or aseptic loosening
7/8/2013
8
•70 pts randomized
–Uncemented tantalum tibia
–Cemented Tibia
•RSA data at 6, 12 and 24 months
•9 of 28 TM patients migrated extensively at 1
year, but stabilized and 0% at risk for failure
•4/21 cemented tibias “at risk”
•5-yr follow up: no further TM migration
–Acta Orthop 2012
Cementless Fixation in Tantalum TKA
Dunbar et al, JBJS-Am 2009
Posterior-Stabilized Cementless TKA
Kamath et al, J Arthroplasty 2011
•100 cementless TKRs under age 55
•PS monoblock porous tantalum tibia
•Cementless CoCr femoral component
•Compared to 312 cemented controls
•No failures due to loss of fixation at minimum
5 years in cementless group
Mid-Term Registry Results
Cementless Porous Tantalum Tibia*
•Finnish Arthroplasty Registry
•2003-2010
•1143 Tantalum TKAs
•100% tibial survivorship for
loosening at 7 years
* Niemelainen, et al. J Arthroplasty,
2013

7/8/2013
9
Summary: Cementless TKA
•There is sufficient evidence to
support cementless fixation
•Cementless TKR is increasing
•Cementless fixation is more biologic
•Caution!!
–Further study / development
–Patient selection likely critical
•Will eventually be “Gold-Standard”
Thank You
7/8/2013 26
7/9/2013
1
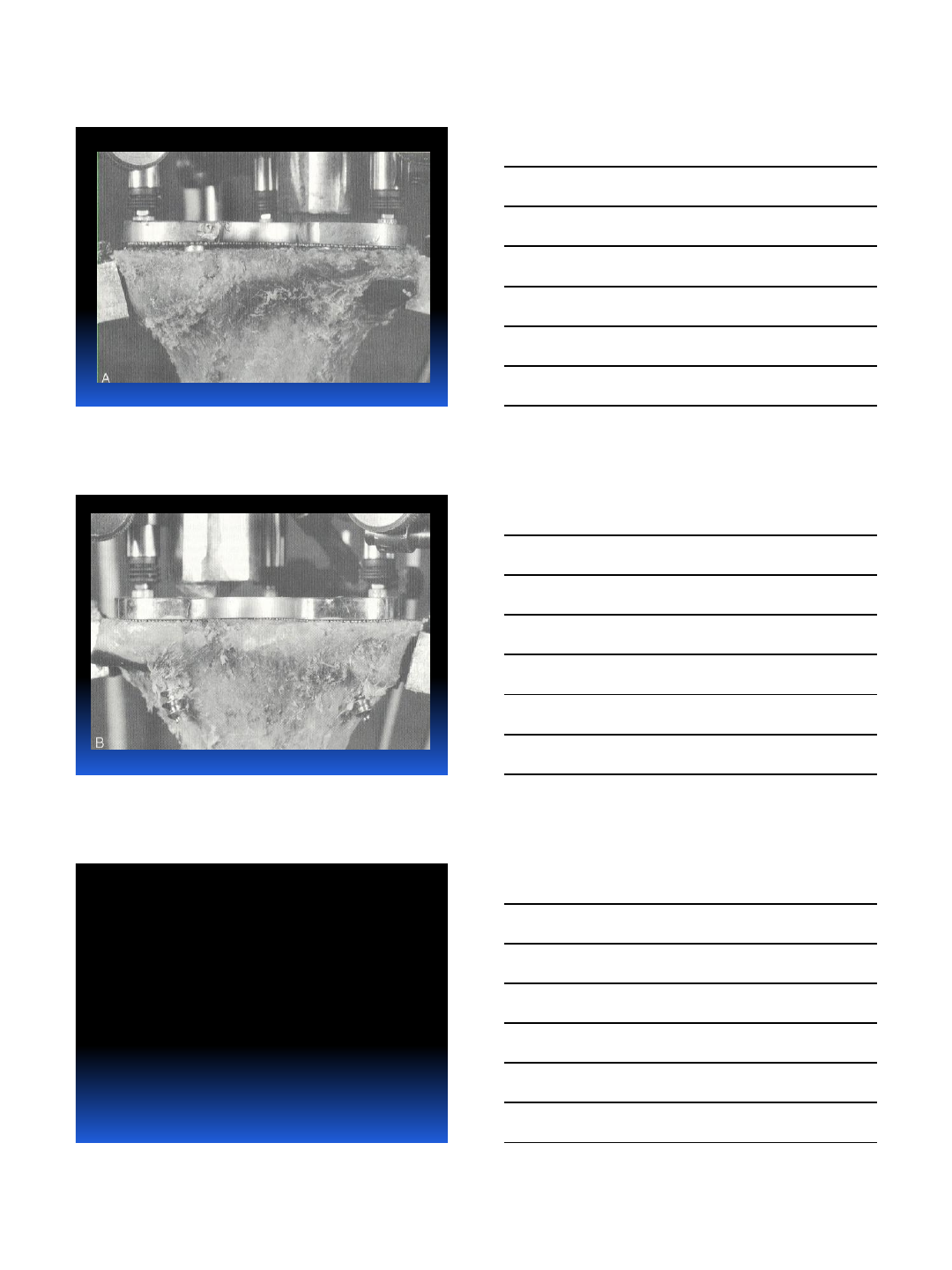
Osteointegration
in TKA
Design
Porous Technology
Instruments
Technique
Early reports were
NOT favorable due to
inadequate design and
engineering
Inadequate
Fixation

7/9/2013
2
Metal-Backed Patellar Component
Gamma-Irradiated Poly
Polyethylene Locking Mechanism
7/9/2013
3
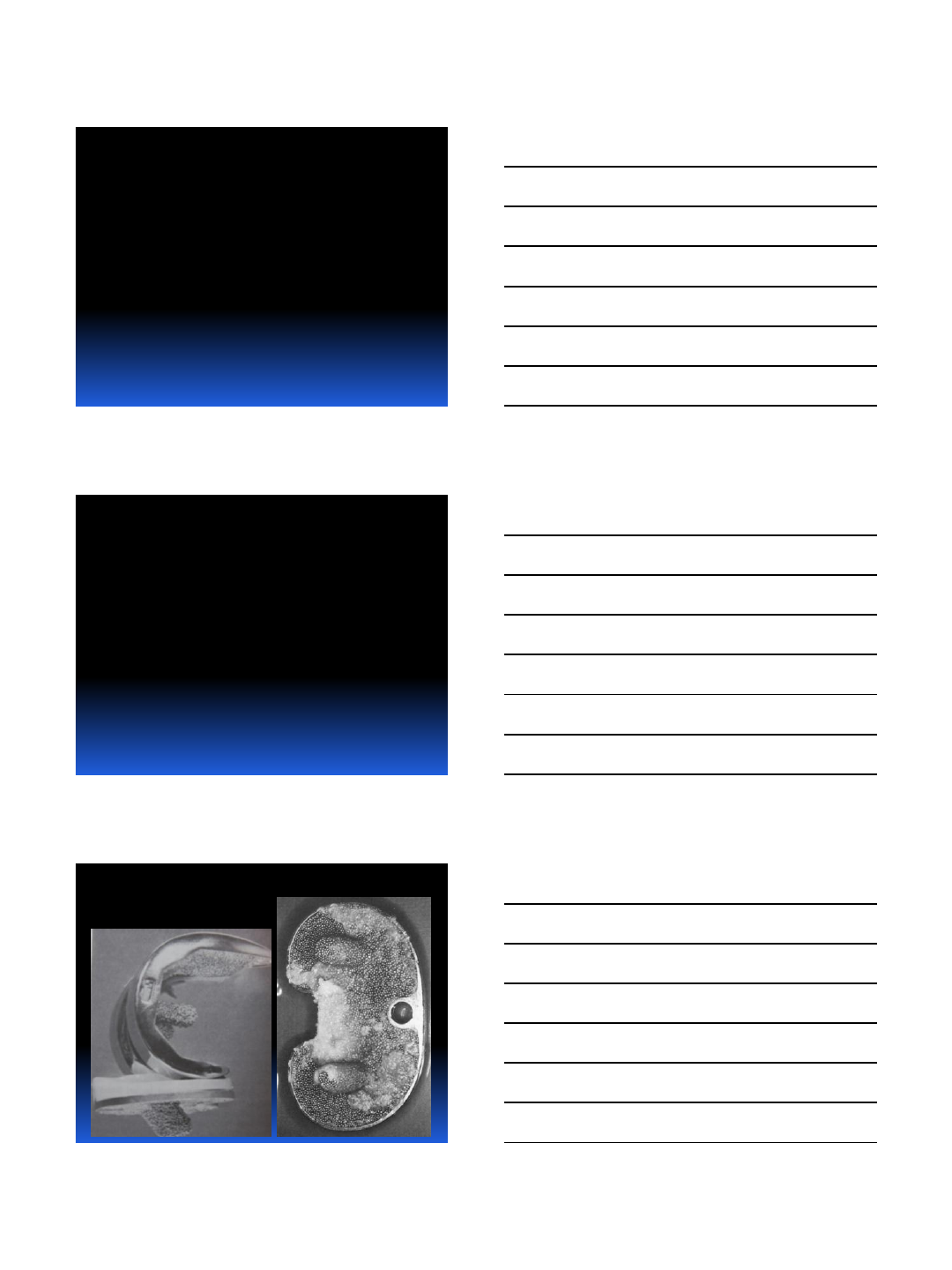
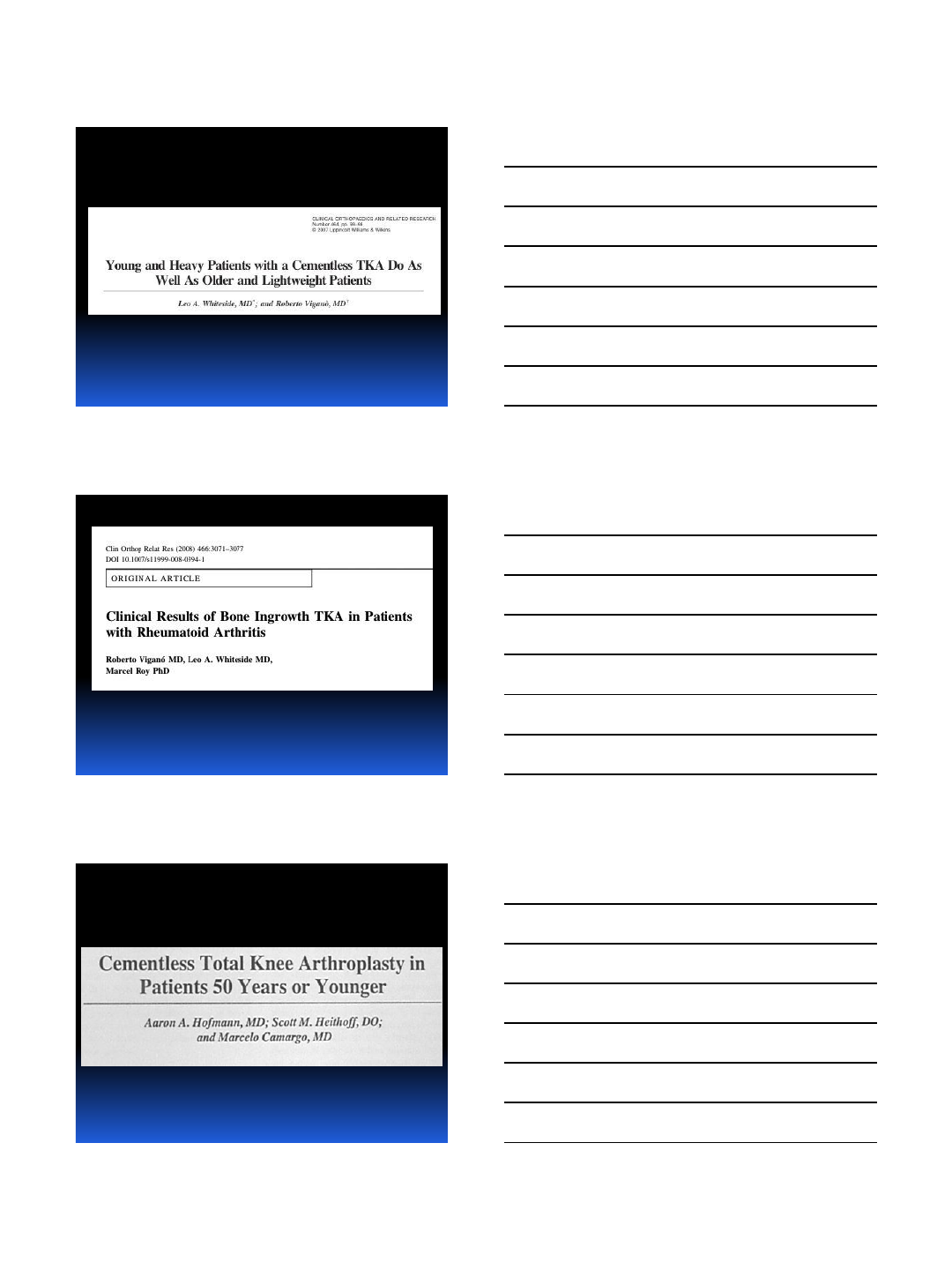
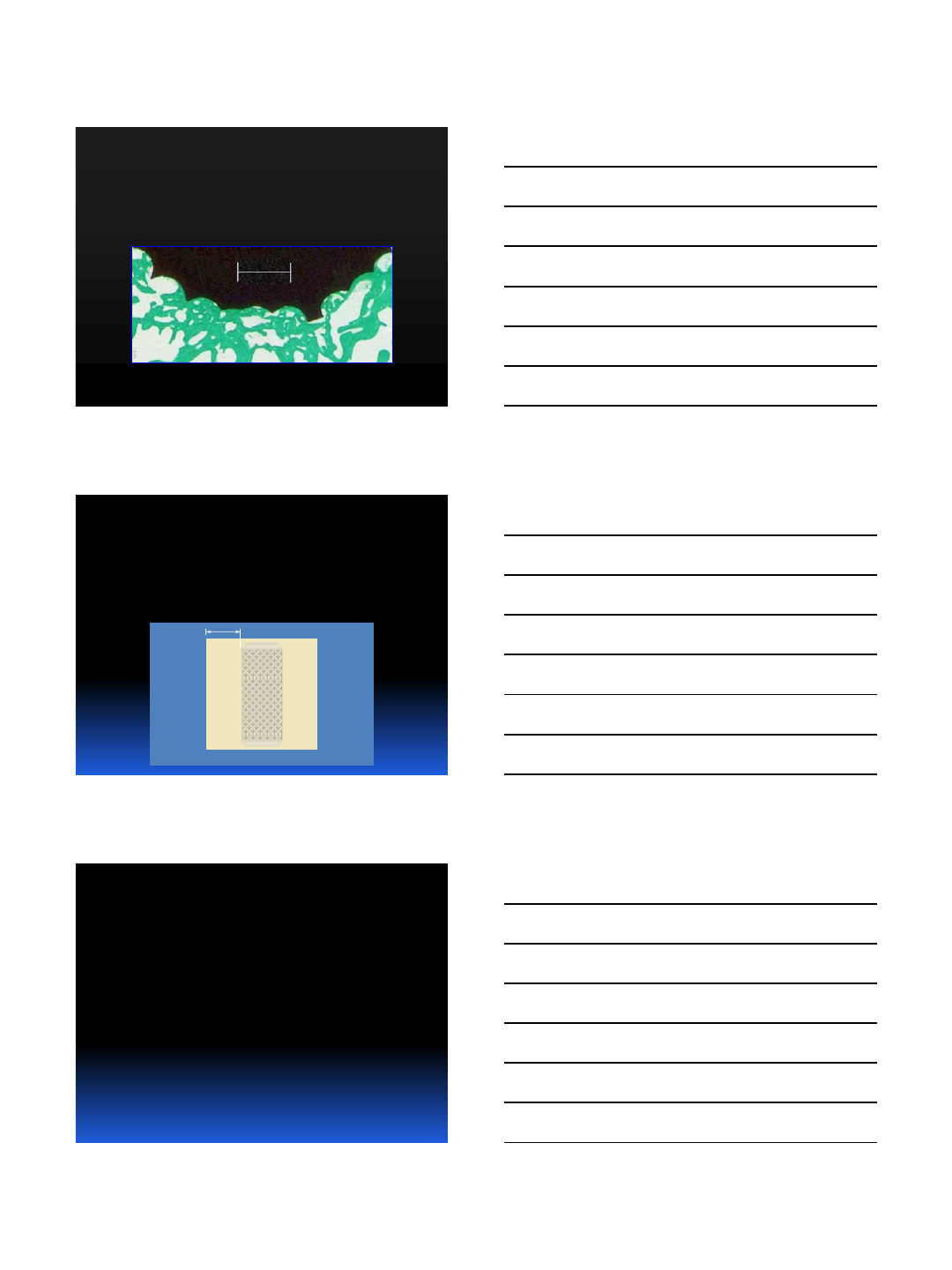
Porous Coating Configuration
Porous Coating Configuration
Effect of Porous Coating on Strength

7/9/2013
4
But reliable
technology has been
available since since
1980.
Whiteside and Summers Orthopaedic
Transactions 1982
CORR 1989
Bartel and Burstein
7/9/2013
5
Medium-Term Followup
Ortholoc Knee CORR 1994
256 Knees
Mean Age
77 (18-93)
95% OA
5% Inflam
Medium-Term Followup Ortholoc
TKA……CORR 1994
Complications
1 Loosening
1 Acute Infection
4 Late-Onset Infection
3 Unexplained Pain
2 Fatpad Impingement
5 Osteolysis and Wear
1 Patellar Tendon Avulsion
MEDIUM-TERM
ORTHOLOC TKA
7/9/2013
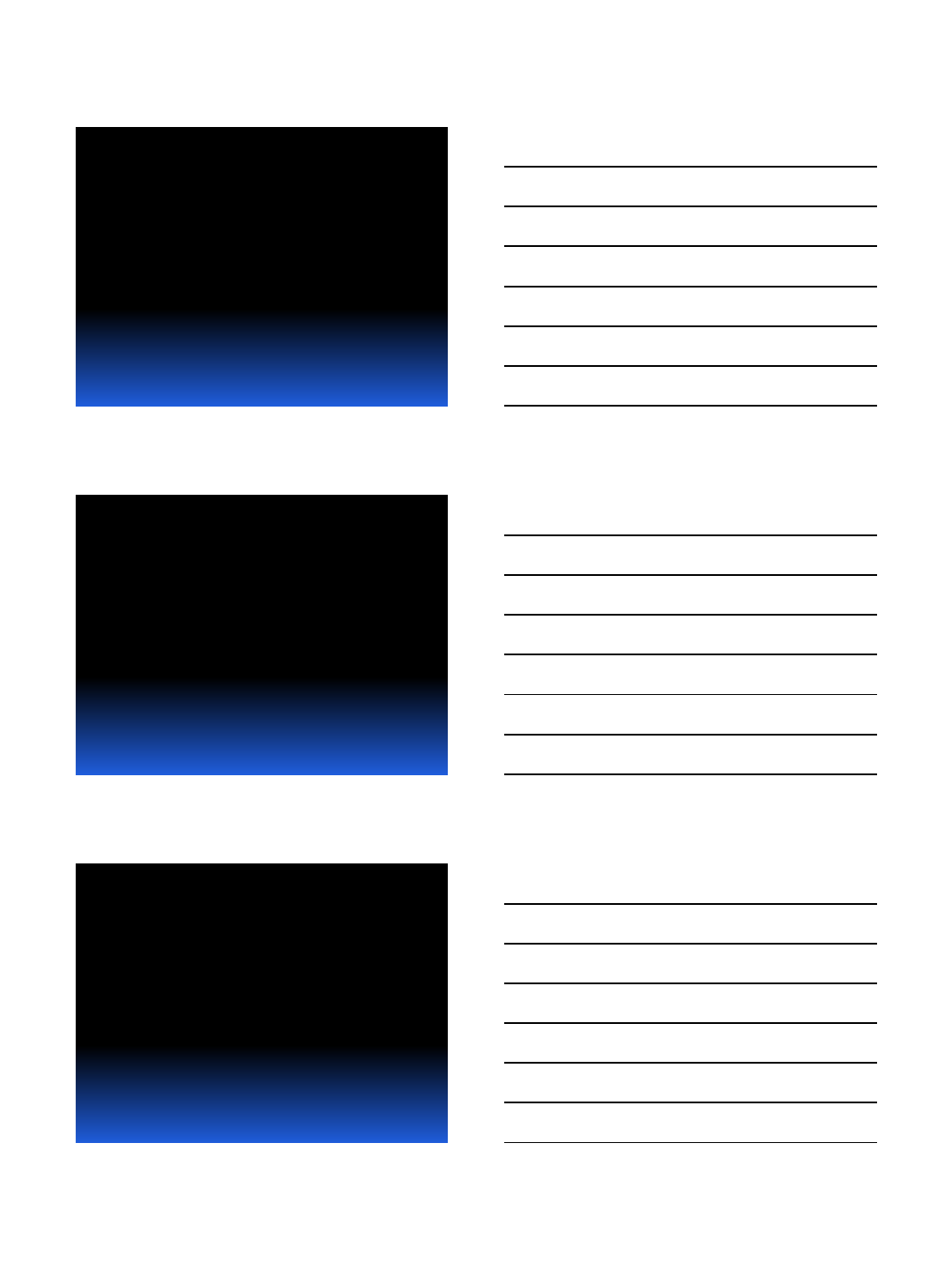
6
Long-Term Followup Ortholoc TKA
CORR 2001
Clinical and Radiographic
Loosening Survivorship >99%
Pain Results
Pre-op 10.8
2 yr 48.3
5 yr 45.4
10 yr 46.3
20 yr 47.3
Bone Ingrowth Ortholoc TKA
7/9/2013
7
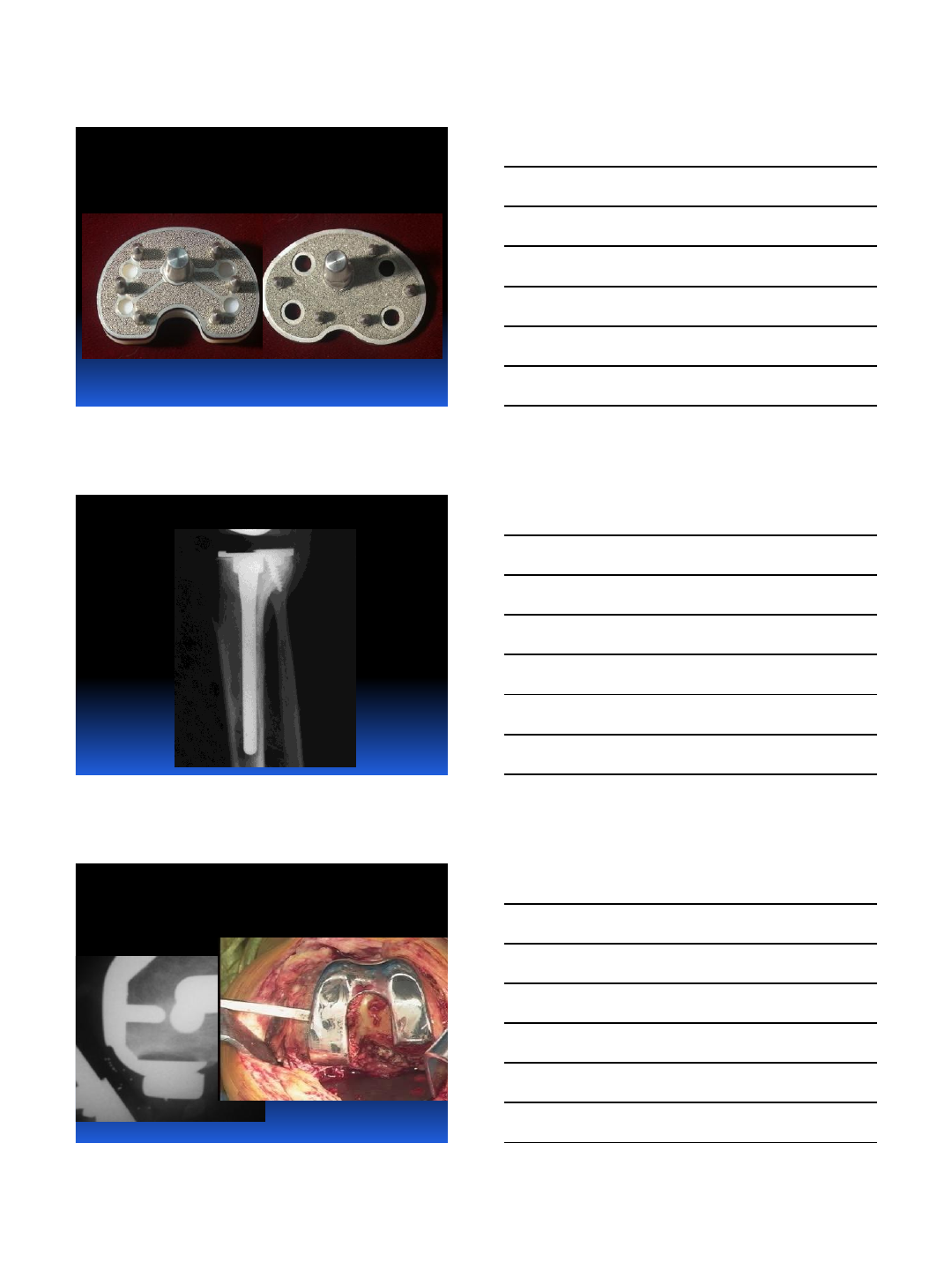
Osteointegration: How to
do it right
Instruments
and
Implant Design
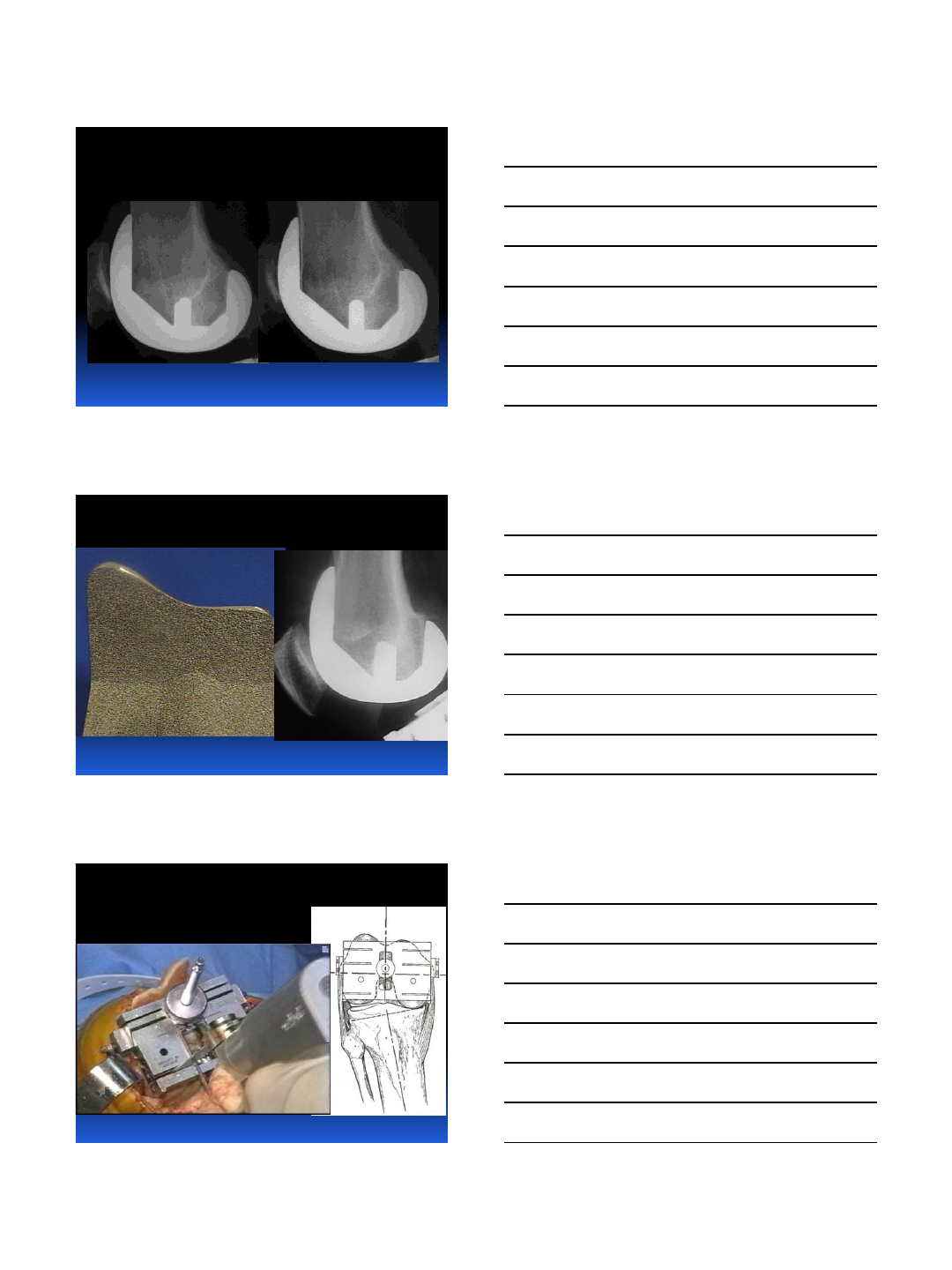
Porous Coating
Femoral Component
Missouri Bone & Joint
7/9/2013
8
Porous Coating
Femoral Component
23% Anterior RLL
Second Generation
4% Anterior Radiolucent Line
Surface Preparation
Accuracy
Viability
7/9/2013
9
Re-cut if needed
Careful Irrigation
Rigid Fixation,
Full Porous Coat
Hiromasa Miura
7/9/2013
10
Missouri Bone & Joint
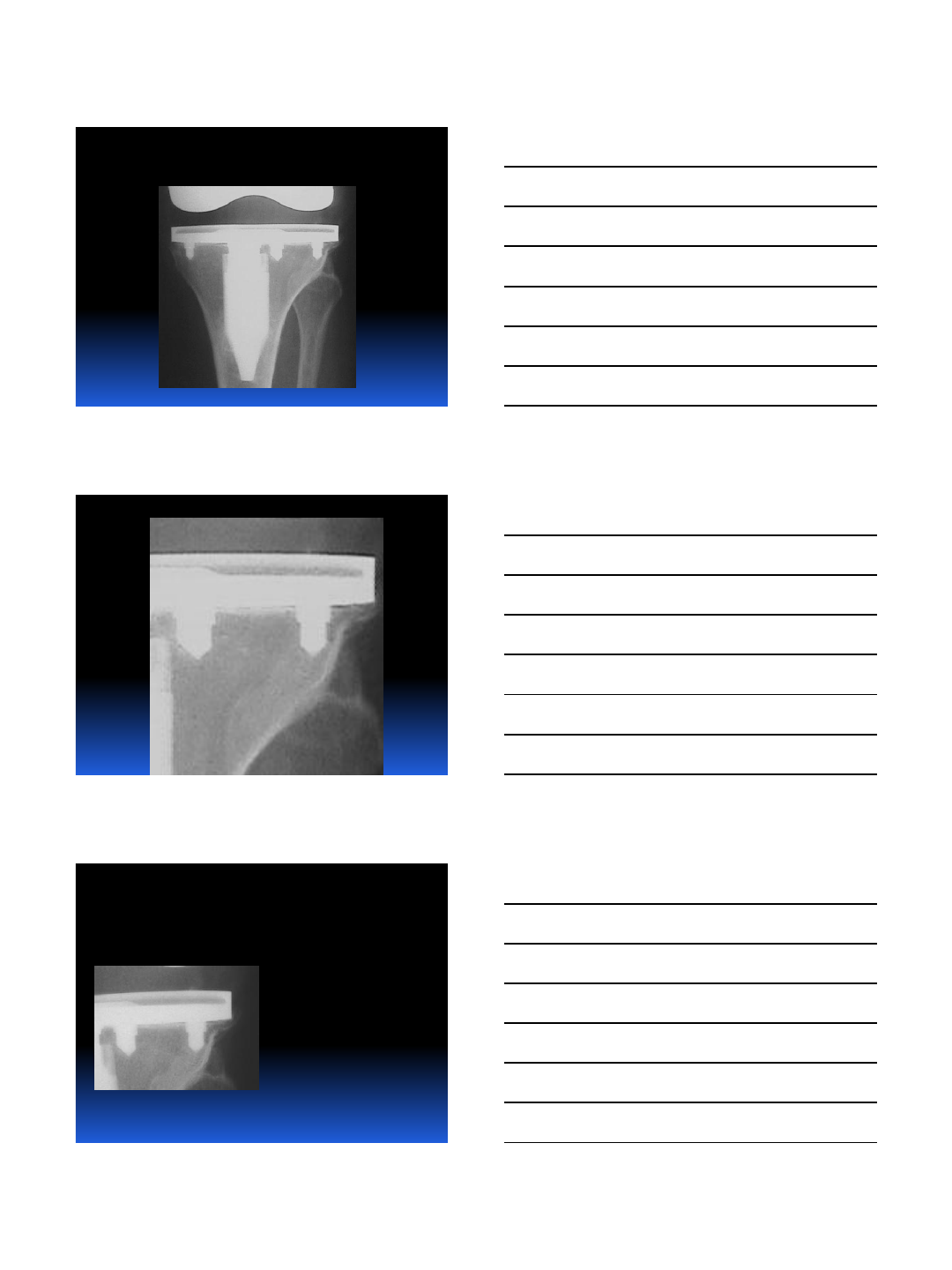
Missouri Bone & Joint
2 yr: (1567) 100%
5 yr: (954) 99.7%
10 yr: (443) 99.3%
12 yr: (257) 98.8%
None Revised for Loosening
Bone Ingrowth Profix TKA
Survivorship 1,567 Knees
7/9/2013
11
10 years: No Loosening
10 years: No Loosening
Challenging Cases:
CORR 2002
0 Loosening at 10 yrs
7/9/2013
12
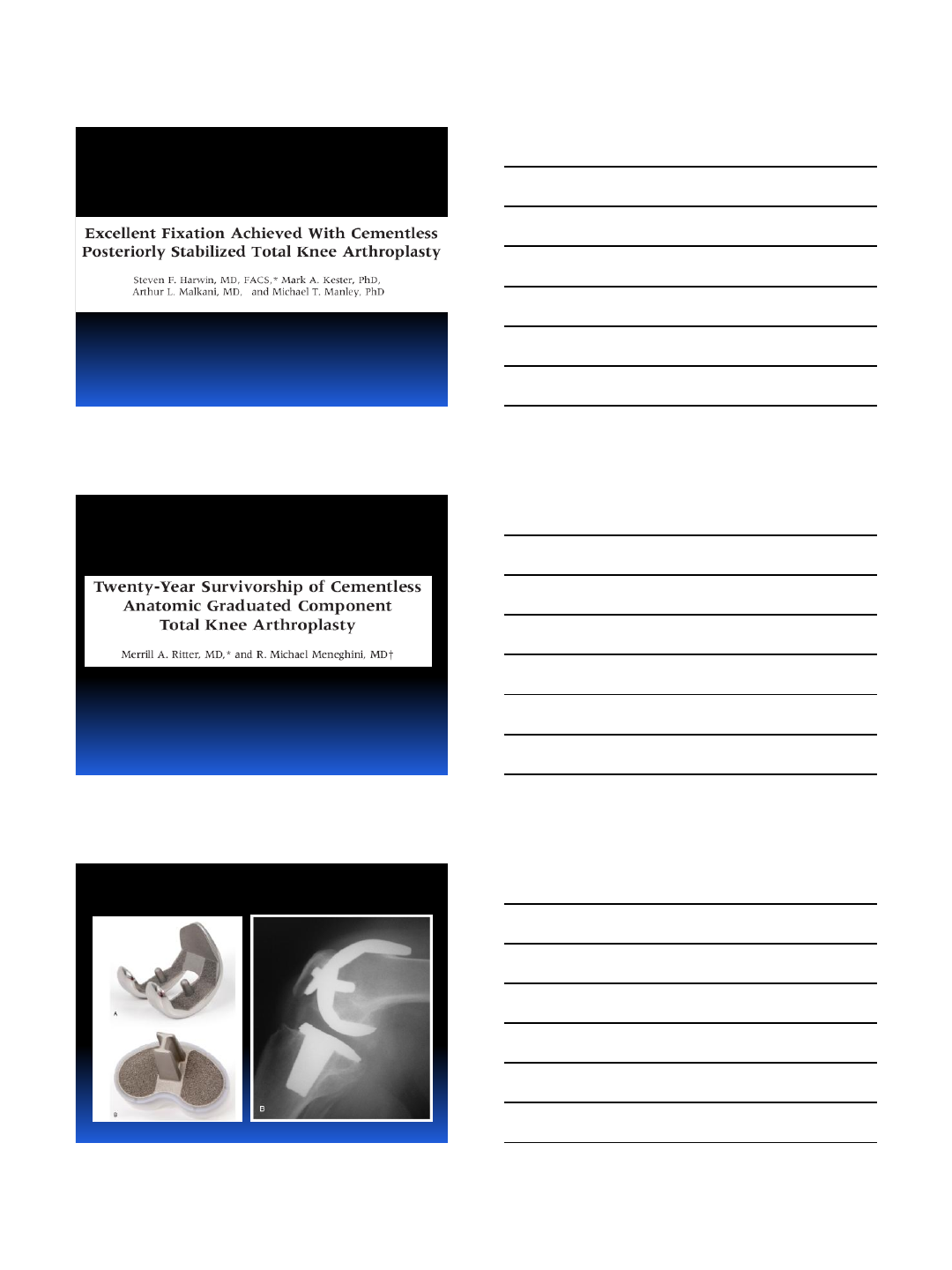
Current Literature
Current Literature
Current Literature
7/9/2013
13
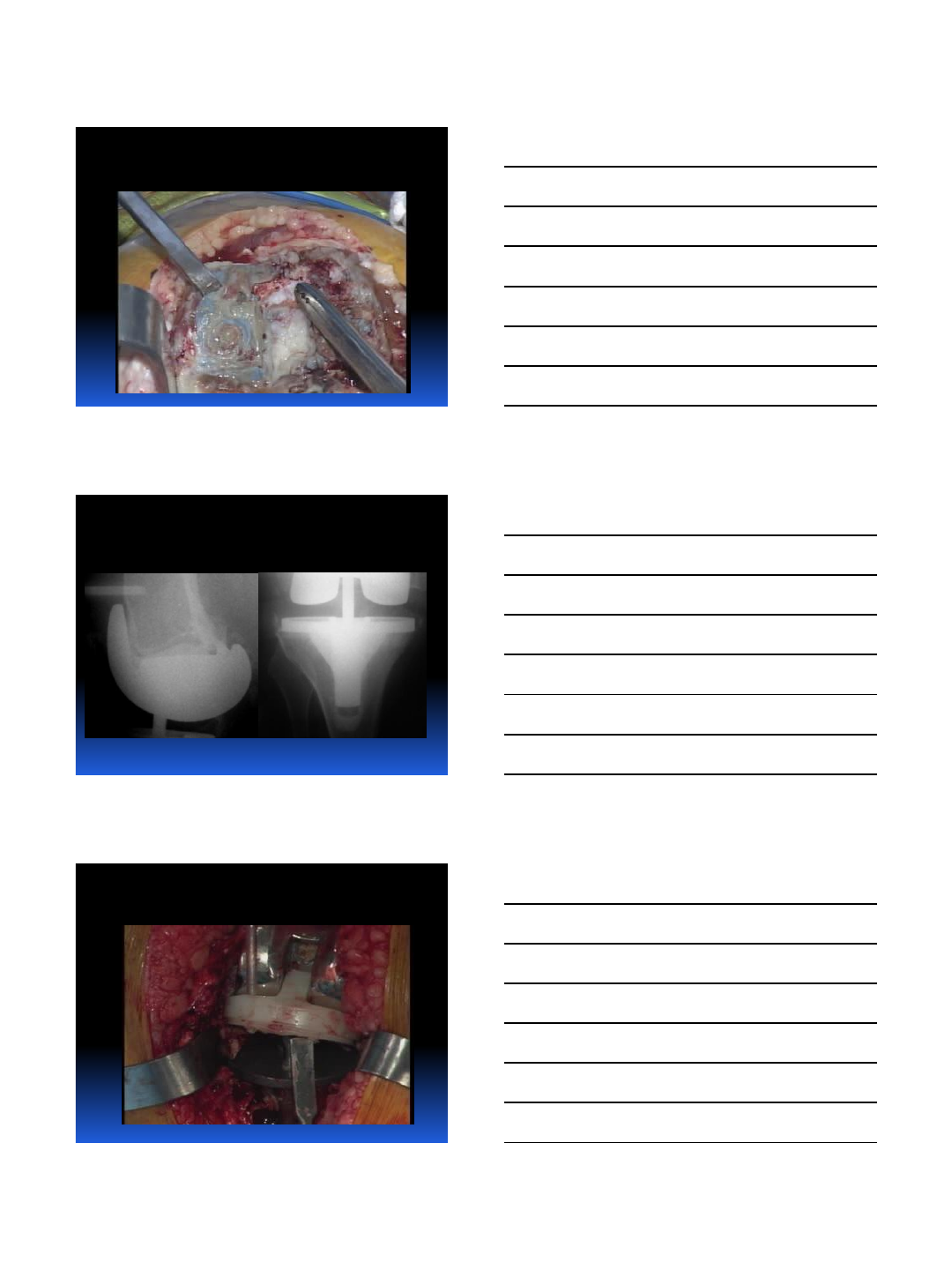
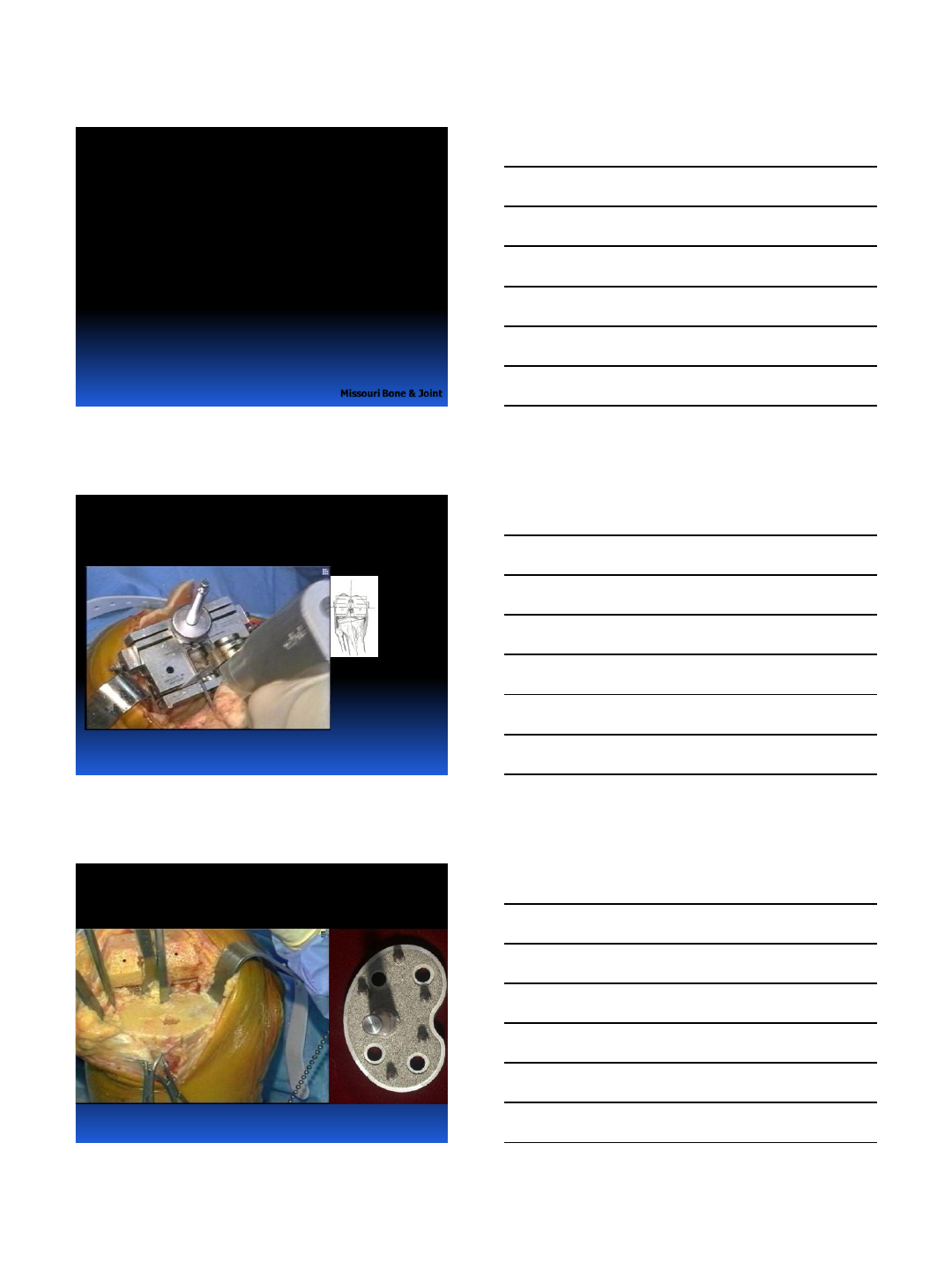
Current Practice
and Techniques
Thin Saw Blade
Viable Bone Surfaces
Accurate Bone Cuts
Viable Bone Surfaces
7/9/2013
14
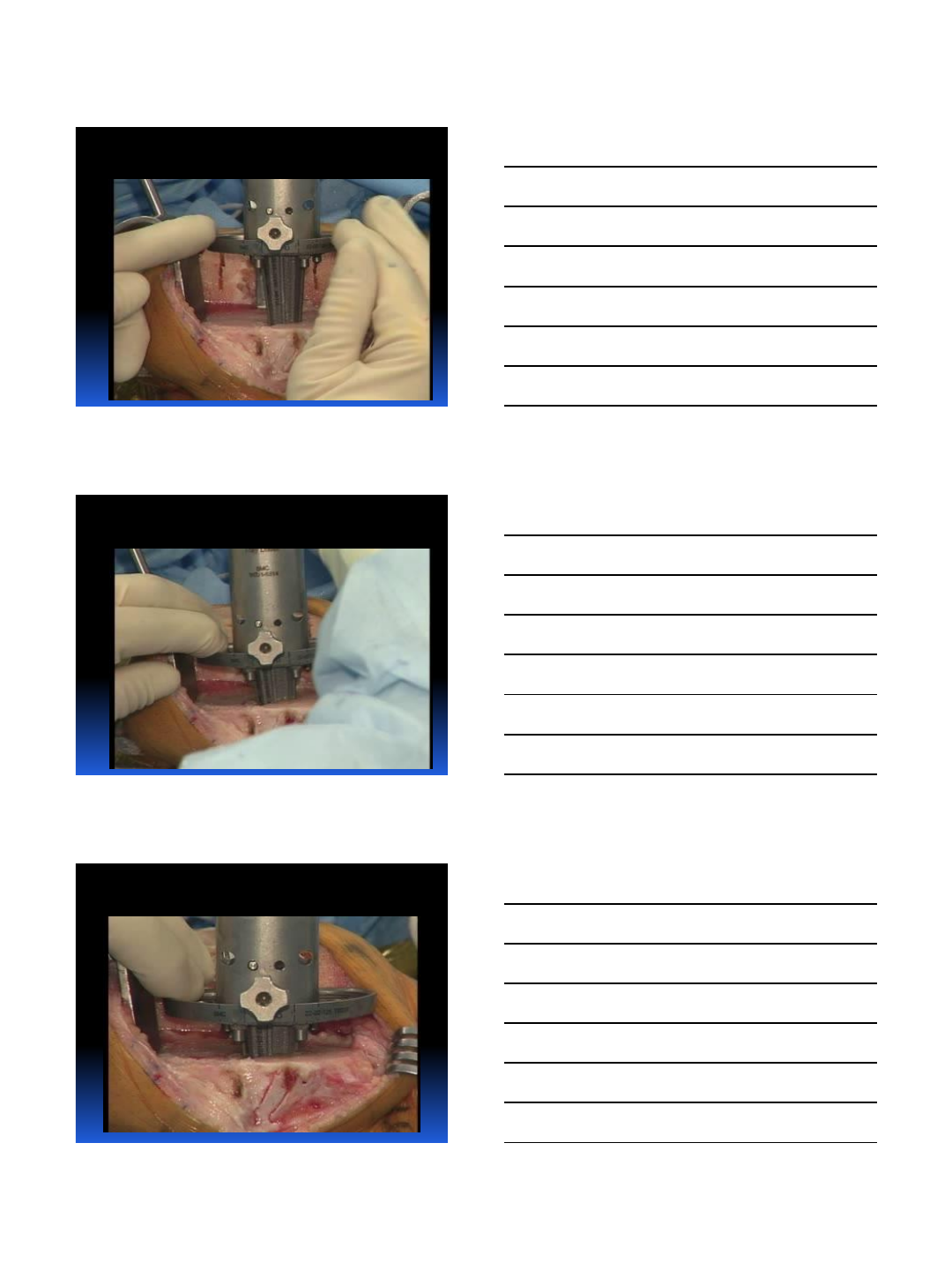
Check Surface:Recut if needed
Re-cut tibia if necessary
Rigid Fixation
7/9/2013
15
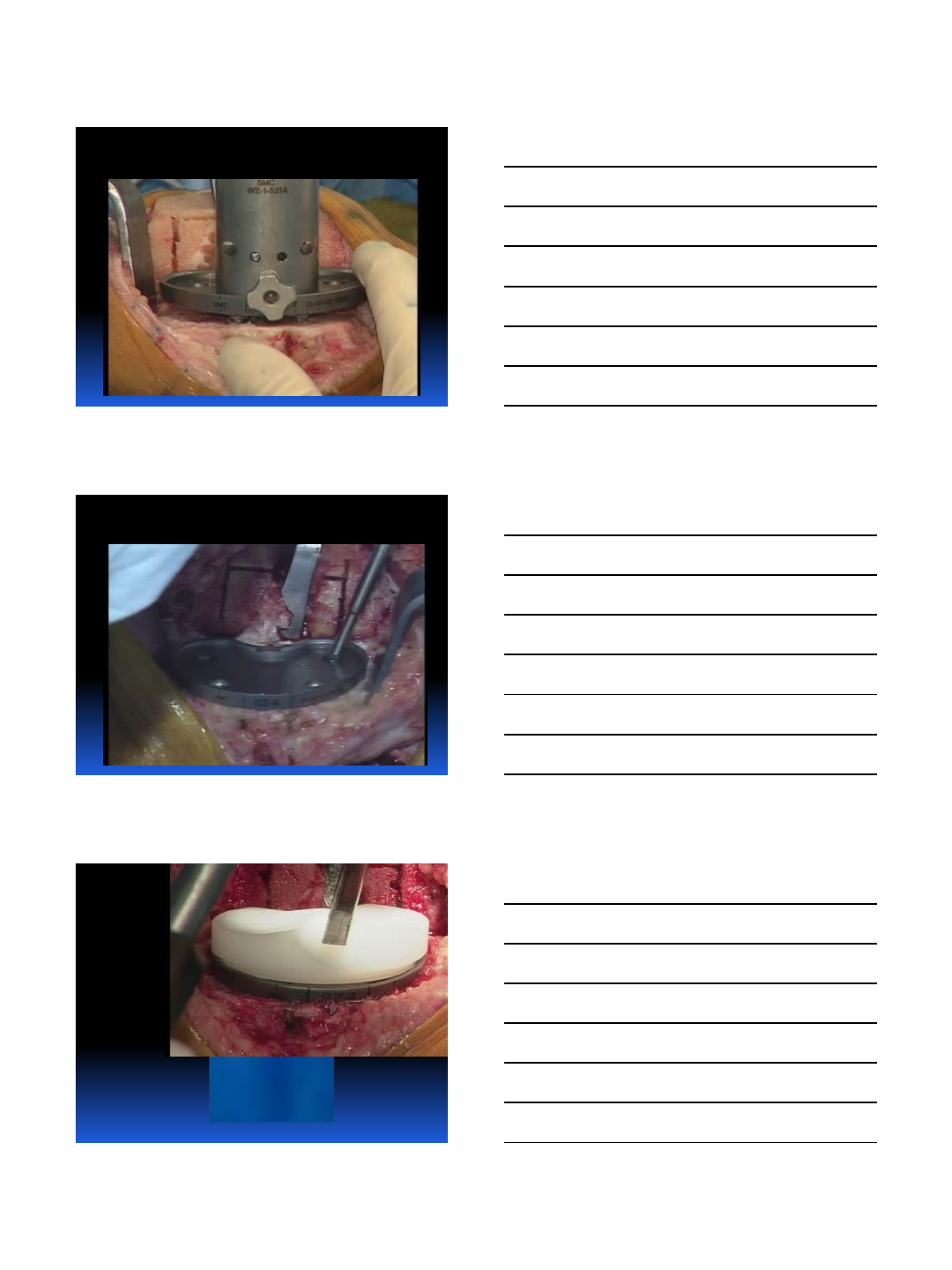
Rigid Fixation
Rigid Fixation
Rigid Fixation
7/9/2013
16
Rigid Fixation
Rigid Fixation
Secure
Locking and
Sealing
7/9/2013
17
Rigid Fixation:
Strong Implant

7/9/2013
18
Advanced Porous Surface
Strong Implant
Fail-safe Surface Fixation
Fixation and Strength
New Technology:
BEWARE

7/9/2013
19
Current Practice
New Technology
Porous-Coated Ceramics
New Technology
Porous-Coated Ceramics
7/9/2013
20
New Technology
Porous-Coated Ceramics
Osteointegration
in TKA
Design
Porous Technology
Instruments
Technique
New Developments
are all in
Osteointegration
7/9/2013
21
Current Literature:
Pertinent Studies
122 Studies
10 Negative
101 Neutral
11 Positive
Current Literature:
Comparative Studies
46 studies
5 negative
31 neutral
10 positive
Controlled Studies
5 studies
2 negative
3 positive
7/9/2013
22
Hybrid
13 Studies
2 Negative
11 Positive
Cemented TKA: Loosening
Cemented TKA: Pain
7/9/2013
23
Cemented TKA: Body Wt
Cemented TKA:
CORR 2000
Missouri Bone & Joint
12.5% Loosening at 8 yrs
Cemented TKA
McKaskie et al JBJS ’99
Randomized Study PFC
Cemented vs Non-Cemented
Significantly Higher RLL’s
with Cement
7/9/2013
24
Bone Ingrowth
vs Cemented TKA
Nielsen J .Arthroplasty ‘96
Failure of Cement Bond
Failure of Cement Bond
7/9/2013
25
Failure of Cement Bond
Failure of Cement Bond
Failure of Cement Bond
7/9/2013
26
Failure of Cement Bond
Failure of Cement Bond
Failure of Cement Bond
7/9/2013
27
256 Knees
Mean Age
77 (18-93)
95% OA
5% Inflam
16-18 Yr
Followup
Long-Term Followup Ortholoc TKA……
CORR July 2001
256 Knees
Mean Age
77 (18-93)
95% OA
5% Inflam
16-18 Yr
Followup
Ortholoc Knee: 1980
Missouri Bone & Joint
Clinical and Radiographic
Loosening Survivorship >99%
Missouri Bone & Joint
7/9/2013
28
Pain Results
Pre-op 10.8
2 yr 48.3
5 yr 45.4
10 yr 46.3
20 yr 47.3
Bone Ingrowth Ortholoc TKA
Missouri Bone & Joint
Accurate Surface Preparation
Missouri Bone & Joint
Final Components
Missouri Bone & Joint

7/9/2013
29
2 yr: (1556) 99.8%
5 yr: (954) 99.7%
10 yr: (443) 99.3%
12 yr: (257) 98.8%
Bone Ingrowth Profix TKA
Survivorship 1,556 Knees
Missouri Bone & Joint
Bone Ingrowth TKA:
CORR 2002
Missouri Bone & Joint
0 Loosening at 10 yrs
Stable Interface
7/9/2013
30
Stable Interface
Missouri Bone & Joint
Stable Interface
Missouri Bone & Joint
Stable Interface
7/9/2013
31
Stable Interface
Missouri Bone & Joint
Durable Osteointegrated Bond
Durable Osteointegrated Bond
7/9/2013
32
Durable Osteointegrated Bond
Durable Osteointegrated Bond
Durable Osteointegrated Bond
7/9/2013
33
New Developments:
All are in Osteointegration
Hydroxy-Apatite on
Porous
Porous Surface on
Ceramic Components
Porous Metals
Missouri Bone & Joint
New Developments:
All are in Osteointegration
Missouri Bone & Joint
New Developments:
All are in Osteointegration
Missouri Bone & Joint

7/9/2013
34
New Developments:
All are in Osteointegration
Missouri Bone & Joint
New Developments:
All are in Osteointegration
Beware of New Technology
Missouri Bone & Joint
Beware of New Technology
Missouri Bone & Joint

7/9/2013
35
Metal-Backed Patellar Component
Missouri Bone & Joint
Macro-Textured Surface
Missouri Bone & Joint
Macro-Textured Surface
0
5
10
15
20
25
Micromotion (µm) at medial distal LVDT
Row Numbers
Micromotion with 50kg Medial Posterior Load
Oxidized
Zr
Fully
coated
CoCr
Partially
Coated
CoCr
7/9/2013
36
Macro-Textured Surface
Missouri Bone & Joint
Macro-Textured Surface
17 out of 18 Loosened
Current Implants and
Surgical Technique
Missouri Bone & Joint
7/9/2013
37
Peripheral Capture
Missouri Bone & Joint
Press-Fit Femoral
Missouri Bone & Joint
Results Bone Ingrowth TKA
>90 Kg: <55 y/o
167 Knees (125 pts)
90% OA, 68% Male
7-10 yr Followup
No Revisions for Loosening
Missouri Bone & Joint
7/9/2013
38
12 Years Post-Op
Missouri Bone & Joint
New Technology in
Osteointegration
7/9/2013
39
New Technology in
Osteointegration
0
5
10
15
20
25
Micromotion (µm) at medial distal LVDT
Row Nu mbers
Micromotion with 50kg Medial Posterior Load
Oxidized
Zr
Fully
coated
CoCr
Partially
Coated
CoCr
The Study
Model:
Skeletally mature sheep
6-week implantation in distal femur
5 implant sample groups
12 implants per sample group
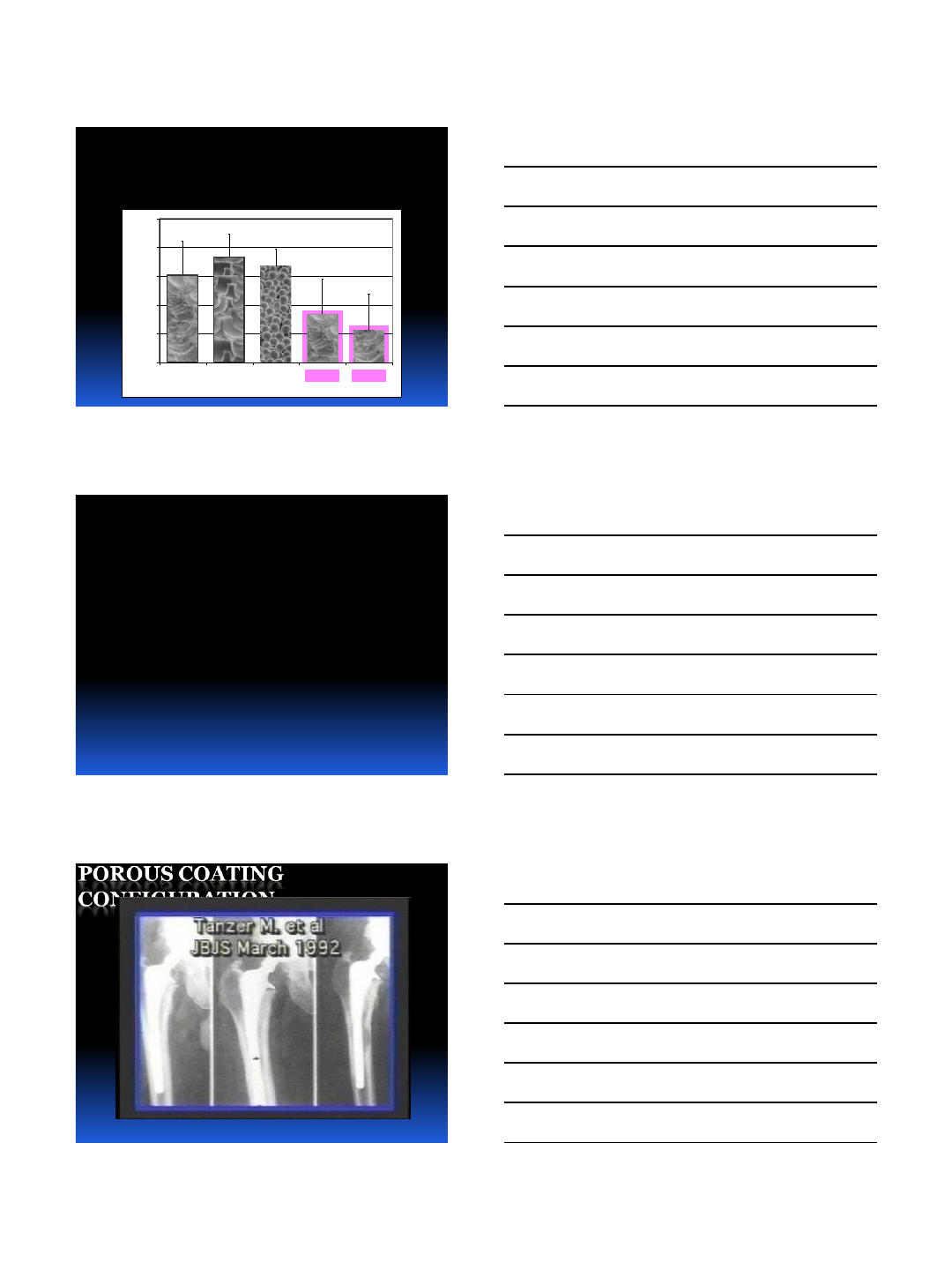
Mechanical Testing Results
Oxidized vs. Non-oxidized Textured Zr-2.5Nb (p =
0.04)
1.0
1.5
2.0
2.5
3.0
3.5
CT-OZ TT-OZ SB-CC CT-Zr CT-Ti
Fixation Surface
Push-out Load [kN]
7/9/2013
40
Reason?
Oxide structurally reinforce the texture
asperities
more resistant to shear
Hardened textured surface abrades bone
rather than becoming abraded with press-
fit insertion
self-grafting effect
Mechanical Testing Results
Oxidized vs. Non-oxidized Textured Zr-2.5Nb (p =
0.04)
1.0
1.5
2.0
2.5
3.0
3.5
CT-OZ TT-OZ SB-CC CT-Zr CT-Ti
Fixation Surface
Push-out Load [kN]
Porous Sintered
Beads
–SB-CC
TecoTex
–TT-OZ
TecoTex
–TT-OZ
ChemTex
–CT-Ti, CT-Zr, CT-OZ
ChemTex
–CT-Ti, CT-Zr, CT-OZ
7/9/2013
41
Mechanical Testing Results
Textured Ti-6Al-4V vs. Textured Zr-2.5Nb (p = 0.39)
1.0
1.5
2.0
2.5
3.0
3.5
CT-OZ TT-OZ SB-CC CT-Zr CT-Ti
Fixation Surface
Push-out Load [kN]
Conclusions
Chemically textured surfaces do not
inhibit bone growth
Chemically textured and oxidized Zr-
2.5Nb is equivalent to or better than other
clinically available biological fixation
surfaces
POROUS COATING
CONFIGURATION
7/9/2013
42
POLY REVISION
IN TKA
Missouri Bone & Joint
Polyethylene Insert Micromotion and
Backside Wear
Harman, Banks, Campbell, Hodge
AAOS 2003
Minimal or no Backside Wear
Minimal Upside Wear
Tighter as Time Passed
No Complications Related to
Modular Poly
Revision for
Wear
Missouri Bone & Joint
7/9/2013
43
Revision for Wear
Missouri Bone & Joint
Worn Poly, Minimal Osteolysis,
Good Locking Mechanism
Missouri Bone & Joint
Minimal Backside Wear
Missouri Bone & Joint
7/9/2013
44
Minimal Osteolysis
Missouri Bone & Joint
Best Solution:
Revision Poly
Tension Ligaments
Missouri Bone & Joint
7/9/2013
45
Final Poly
Missouri Bone & Joint
Correctly Designed and Carefully
Manufactured
No Known Problems with Modularity
Missouri Bone & Joint
Correctly Designed and Carefully
Manufactured
Missouri Bone & Joint
7/9/2013
46
New Osteointegration Technology
CEMENTLESS TKA
Mechanical Testing Results
Co-Cr Beads vs. Textured & Oxidized Zr-2.5Nb (p >
0.24)
1.0
1.5
2.0
2.5
3.0
3.5
CT-OZ TT-OZ SB-CC CT-Zr CT-Ti
Fixation Surface
Push-out Load [kN]
7/9/2013
47
1.0
1.5
2.0
2.5
3.0
3.5
CT-OZ TT-OZ SB-CC CT-Zr CT-Ti
Fixation Surface
Push-out Load [kN]
Mechanical Testing Results
Pin Push-out Testing
Bone sectioned away from each end of pin
Steel plunger and restricter plate used to
axially push the pin out of the bone
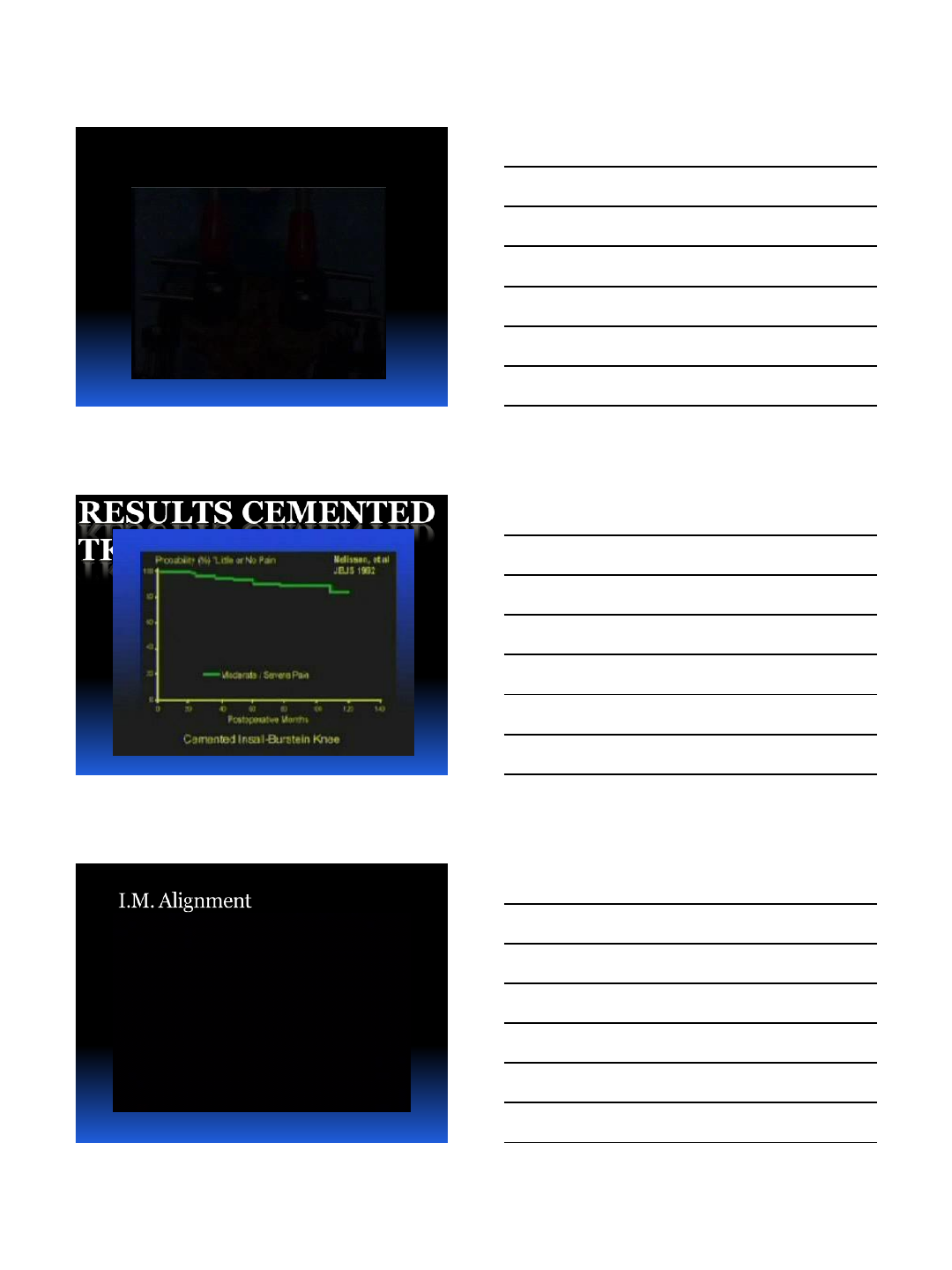
Histological Assessment
Bone formed in direct
apposition to the deepest
recesses of each test
surface
mechanical interdigitation
1 mm
CT-Ti
1 mm
CT-Zr
1 mm
CT-OZ
1 mm
TT-OZ
1 mm
SB-CC
Bone labels indicated that
bone formation had:
–started within 2 weeks
–continued out to 5 weeks
7/9/2013
48
1 mm
Histological Analysis
Sections were ground and stained with
light green
Histological Analysis
Bone sectioned at least 5 mm from test
surfaces
Specimens fixed, dehydrated, and cleared
5 mm
Bone Labels
Bone labeling solutions given to 4
sheep in each group
calcein injection @ 2 weeks
oxytetracycline injection @ 5 weeks
Sheep euthanized and femora
harvested @ 6 weeks
7/9/2013
49
New Technology in
Osteointegration
RESULTS CEMENTED
TKA
I.M. Alignment

7/9/2013
50
Trial Implants
Missouri Bone & Joint
I-M Alignment
Video IM Alignment
Missouri Bone & Joint
A-P Axis
Missouri Bone & Joint
7/9/2013
51
Measured Resection
Missouri Bone & Joint
Tibial IM Alignment
Missouri Bone & Joint
Femoral Resection
•Diverging
•Irrigation
7/9/2013
52
Tibial Resection
•Rough Cut
•Irrigation
Tibial Resection
•Finish Cut
•Irrigation
Trial Components
7/9/2013
53
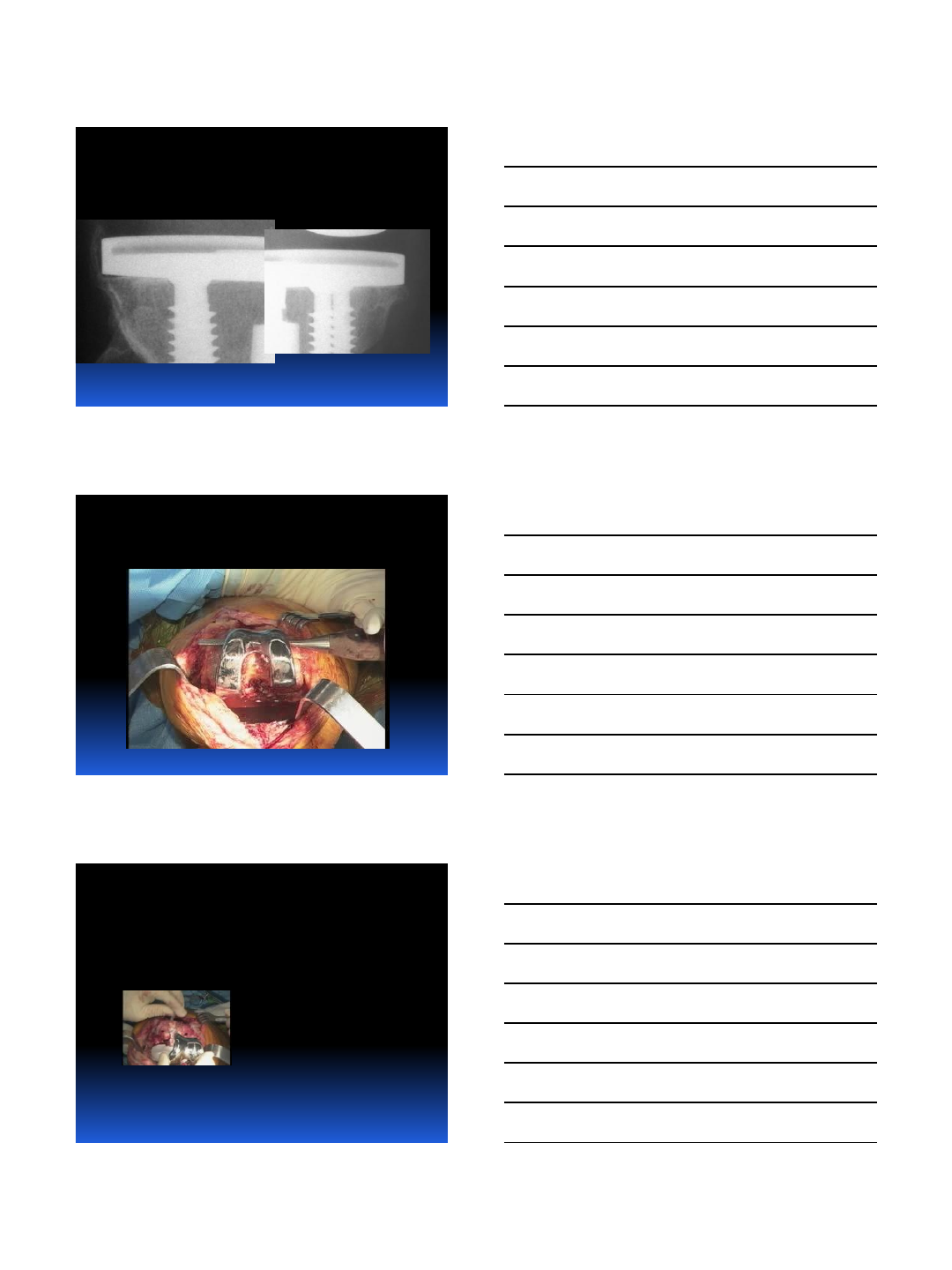
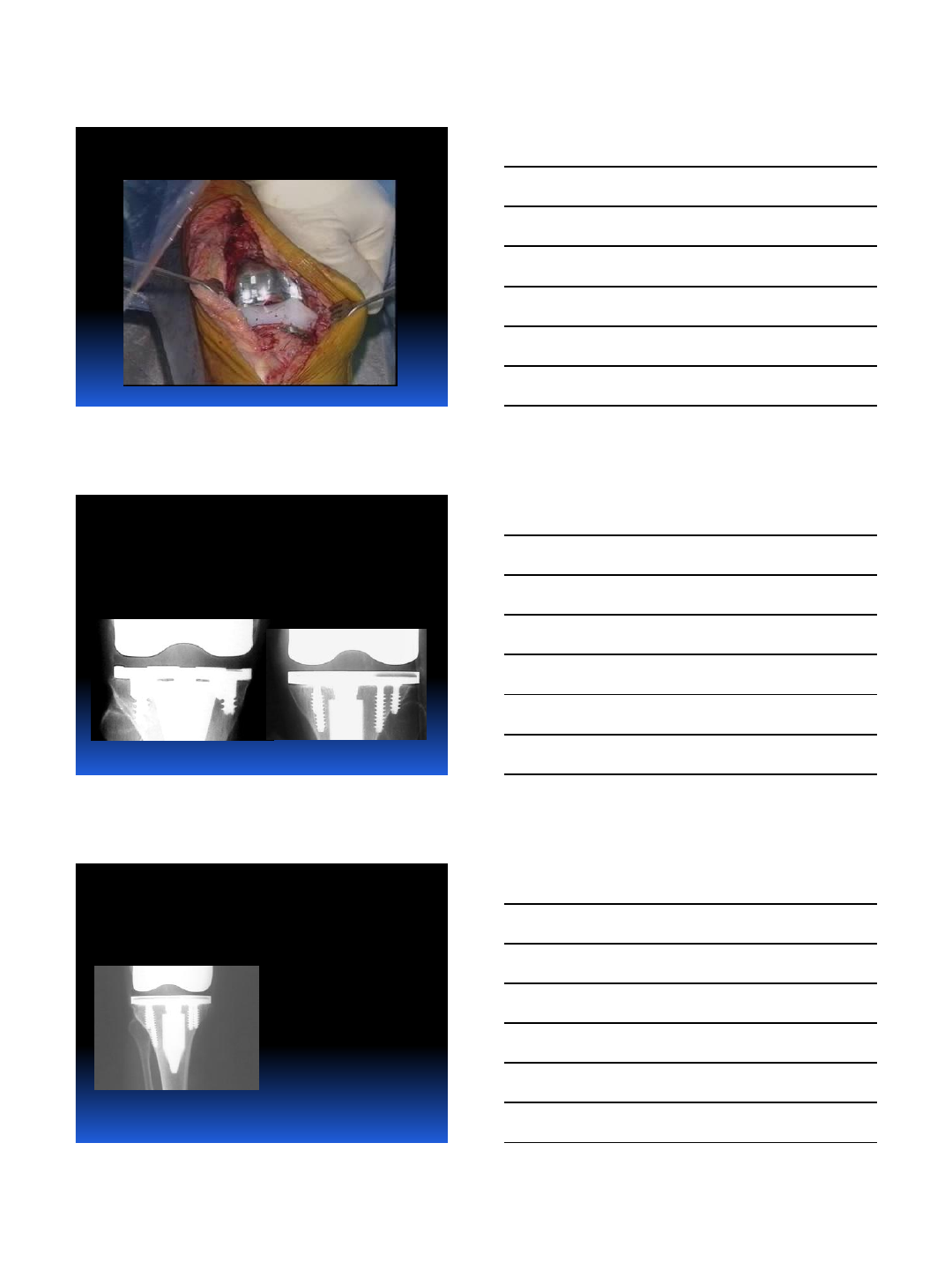
Tibial Component
•Porous Undersurface
•Grit Blasted Stem
•Screws
Femoral Component
•Porous Undersurface
•Femoral Pegs
Accurate Reference Landmanks

7/9/2013
54
New Technology in
Osteointegration in TKA
Hydroxyapatite on Porous
New Porous Metals
Porous Coating on
Ceramic Implants
Bone Growth Factors
Missouri Bone & Joint