CMC Arthritis Syllabus
2014-02-12
: Pdf Cmc Arthritis Syllabus CMC_Arthritis_Syllabus 2 2014 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 39
2/11/2014
1
Ruth Jackson Orthopaedic Society presents
The Little Joint with Big Problems
Anatomy, Treatment, and Challenges in CMC Arthritis
Amy L. Ladd MD
Professor & Chief, Chase Hand Center
Department of Orthopaedic Surgery
Assistant Dean, Stanford School of Medicine
Disclosures
Related
Funding
NIH RO1 2011-16
NIH SBIR 1,2 2005-08, 2009-11
OREF/RJOS/DePuy 2010
Royalties & Stock options- Extremity Medical,
Articulinx
Unrelated
Royalties - OrthoHelix
Stock, stock options - OsteoSpring, Illuminoss
RJOS President 2013-14
Assistant Dean of Medical Advising
Overview of Webinar
Current, clinically relevant information on CMC arthritis:
Why is it such a problem? – Ladd
Trapeziectomy and various approaches – Weiss
Less invasive procedures – Kakar
Role of instability - Wolf
2/11/2014
2
Introduction
Why is thumb CMC arthritis such a problem?
Anatomy review
Treatment – consensus and lack of consensus
Challenges in treatment and prevention
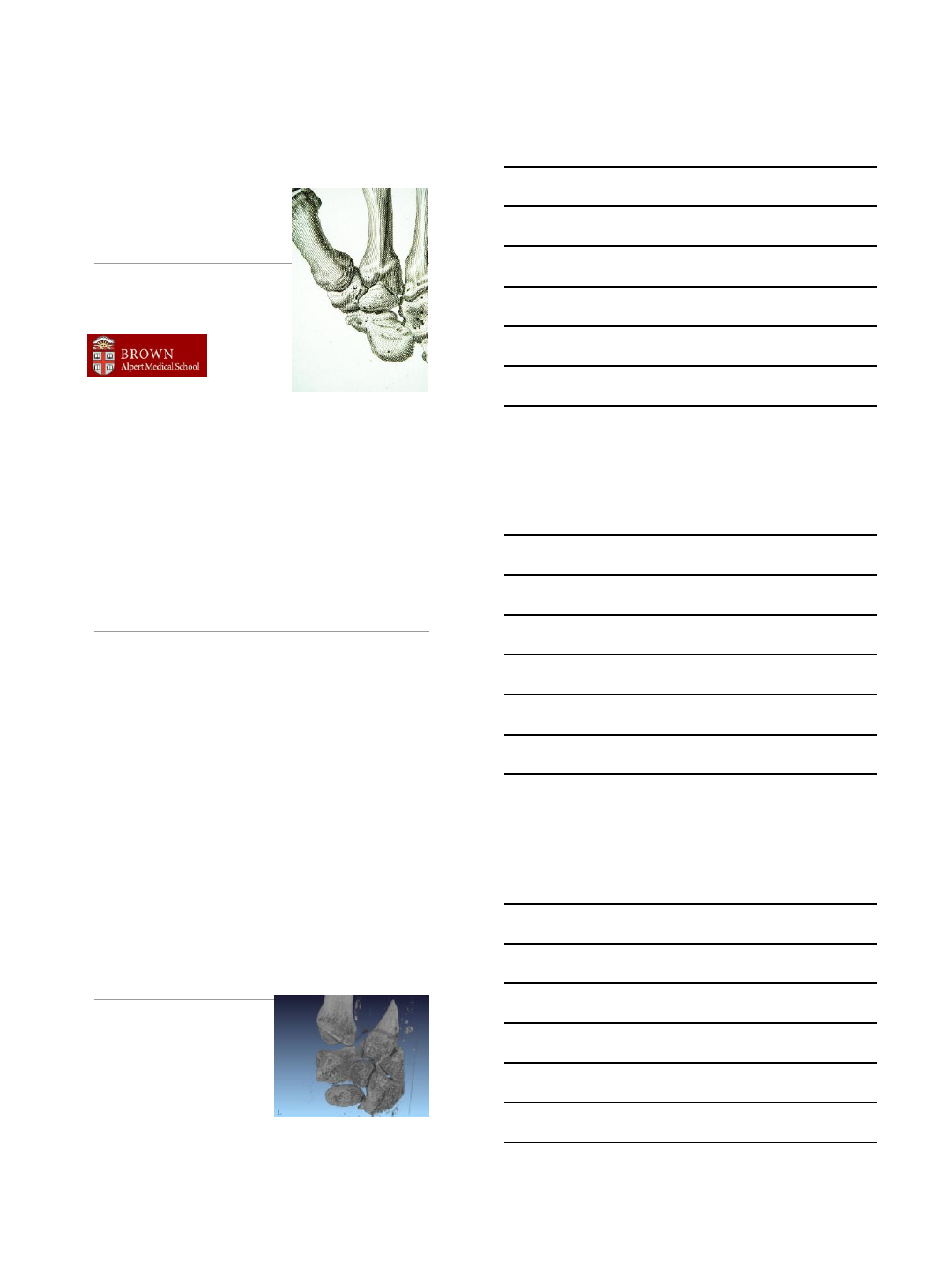
Normal Osteoarthritic
How does this joint wear out?
Anatomy – its not simple
Shape
Load
Movement
2/11/2014
3
Morphology
Trapezium
The joint surfaces are eccentric.
Eccentric shape
Out of plane from fingers
Both permit rotation and
opposition
Ligament stability
Stability is part structure and part proprioception.
Ligaments may only contribute part of stability.
2/11/2014
4
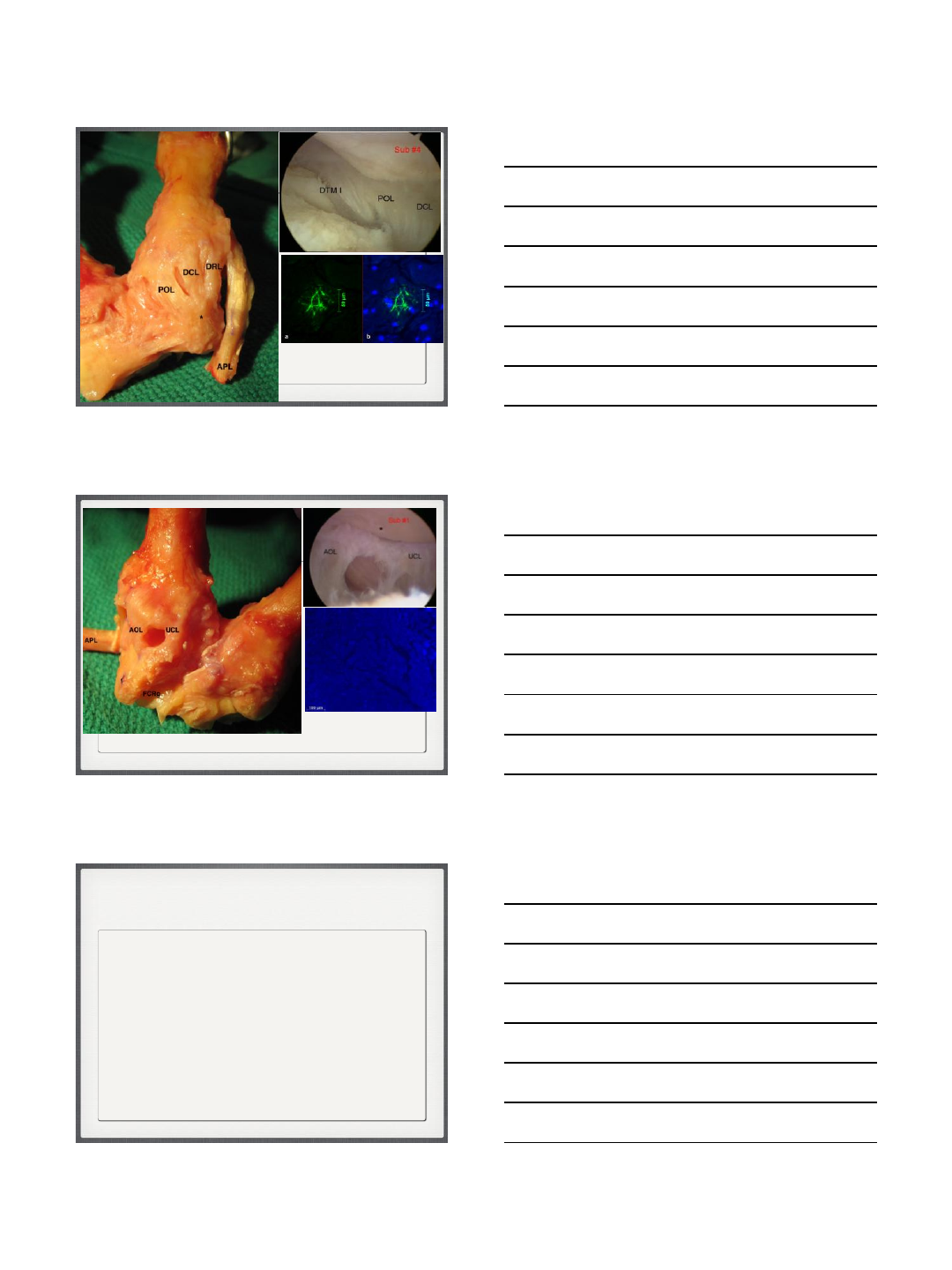
Dorsal ligament complex
Ladd, Lee, Hagert: JBJS 2012
Zhang, Hagert, van Nortwick, Ladd ASSH 2011, JWS 2013
Volar ligament complex
Ladd, Lee, Hagert: JBJS 2012
Zhang, Hagert, van Nortwick, Ladd ASSH 2011, JWS 2013
Load
Articular and trabecular wear patterns infer
biomechanical loading.
Abnormal loading may contribute to patterns of
arthritis.
2/11/2014
5
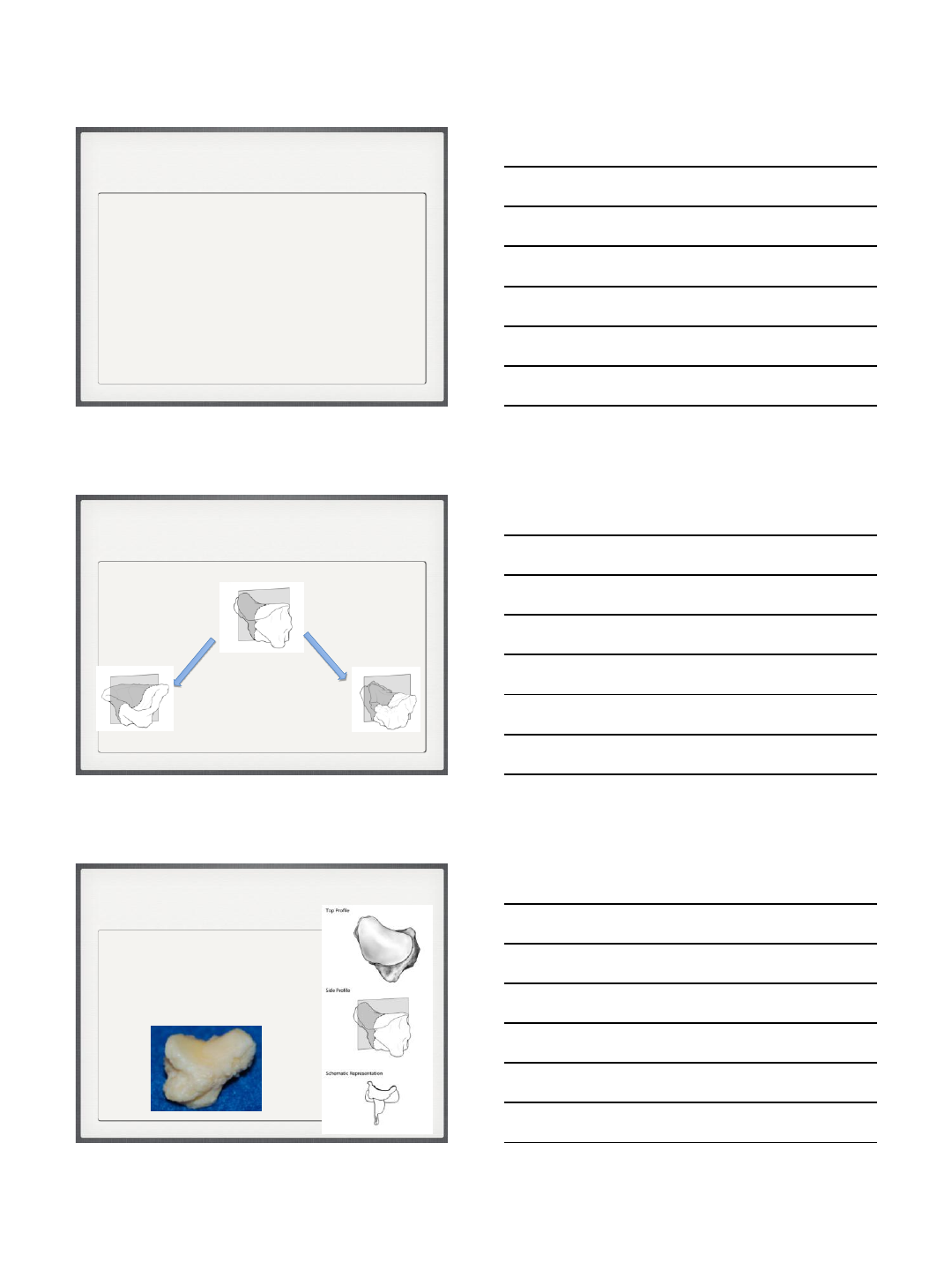
Clinical examples of wear patterns
Trapezial wear patterns
Dish 33% Cirque 19%
Saddle 47%
•Intra-rater reliability 0.97
•Inter-rater reliability 0.95
36 specimens
•27 Female (75%)
• 9 male (25%)
•age 64 (33-76)
Van Nortwick, Berger, Cheng, Lee, Ladd: J Wrist Surgery 2013
1- Retained saddle
•Retains concavo-convex surface
•Partial eburnation
•Few osteophytes
47%
Van Nortwick, Berger, Cheng, Lee, Ladd: J Wrist Surgery 2013
2/11/2014
6
2-Dish shape
A mortar and pestle
•Trapezium = mortar
•Metacarpal = pestle
•Full eburnation
•Rimming osteophytes
33%
Van Nortwick, Berger, Cheng, Lee, Ladd: J Wrist Surgery 2013
3-Cirque
•Volar eroded concave facet
•Retained convexity dorsally
• - half a saddle
19%
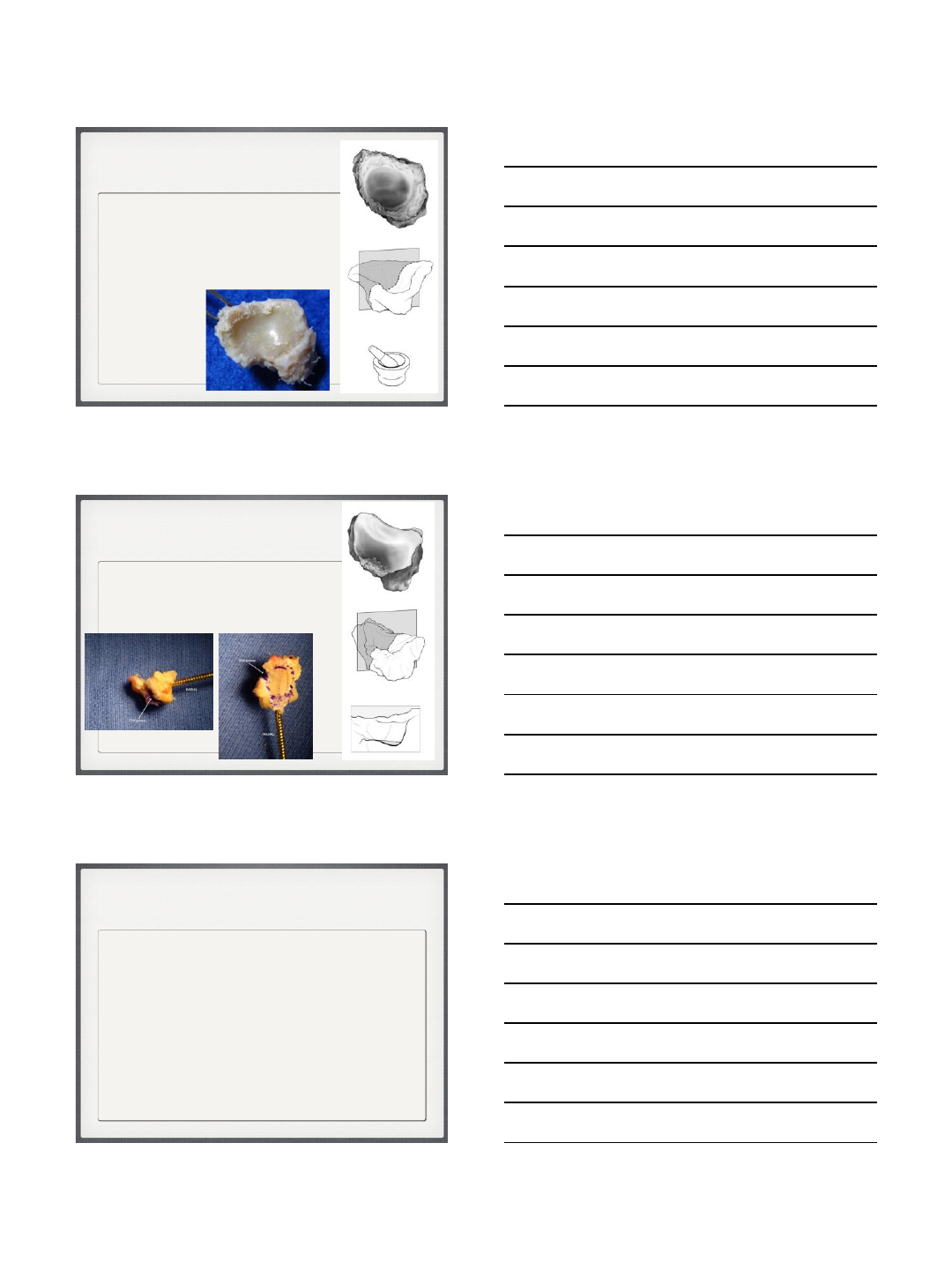
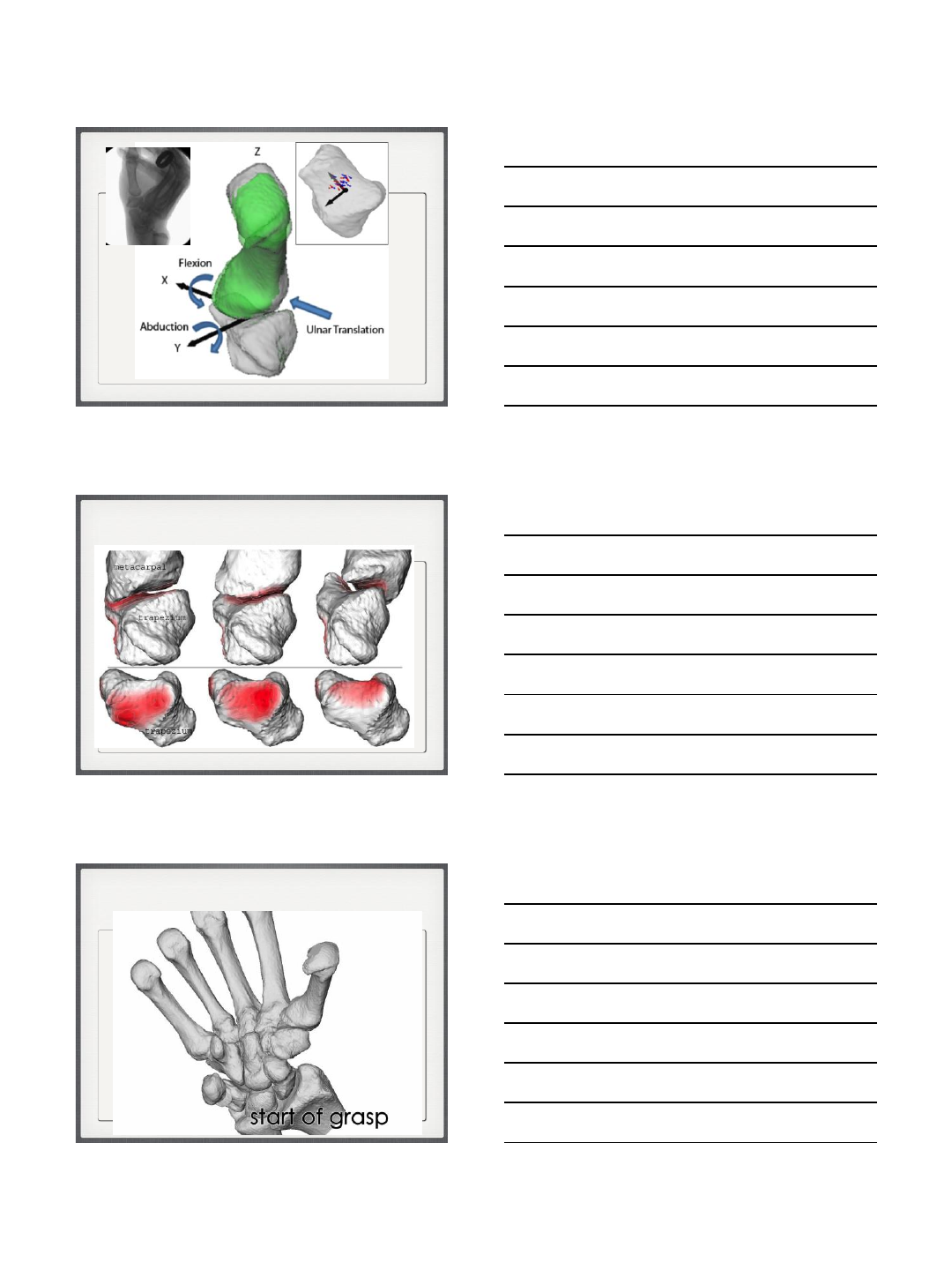
Movement
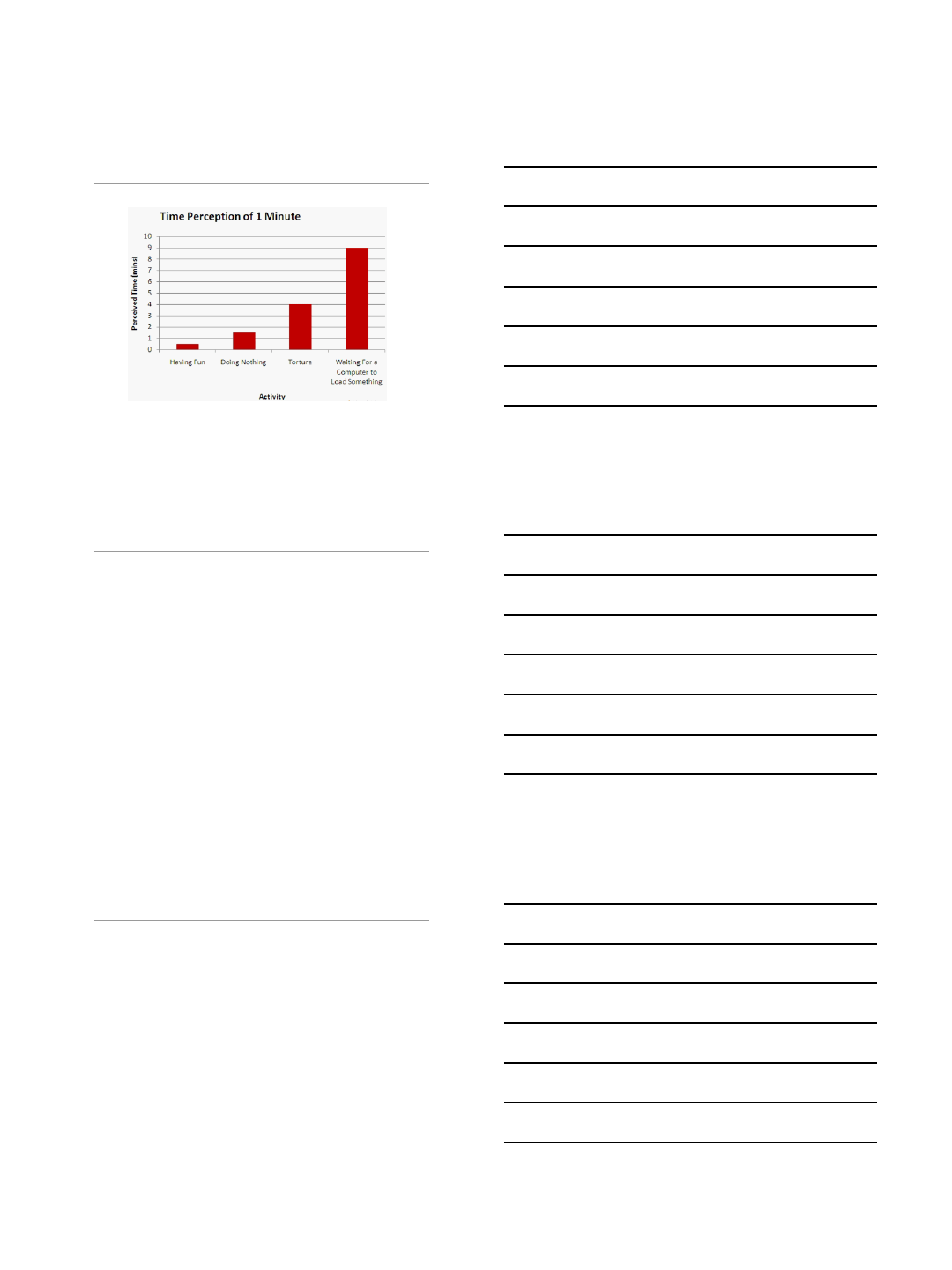
Understanding micro-motion in normal and
arthritic populations suggest better ways to
predict and treat arthritis.
2/11/2014
7
Ladd, Weiss, Crisco, Hagert, Wolf, Yao, Glickel: AAOS ICL 2012
24 subjects
12 male (ave age 38)
12 female (ave age 43)
CMC contact
pinch grasp jar opening
1 mm interbone distance contours
Putting it together
2/11/2014
9
The role of the MP joint
Challenges
Where else can we find clues?
As in other joints, what is
the role of:
Instability - imbalance
Impingement
Proprioception
2/11/2014
10
Summary - Ultimate goal
•Apply what we know about
anatomy and disease
•Decipher the paradox of
mobility and stability
•Use this to predict, prevent,
and treat thumb arthritis
Thank you
2/11/2014
1
Thumb CMC Arthroplasty
Suture Suspension
Technique
Arnold-Peter C. Weiss, M.D.
R. Scot Sellers Scholar of Hand Surgery
Professor of Orthopaedics
Disclosure
None
Why should I care?
Most studies show equal outcomes
Gerwin, Kriegs-Au, Davis
Third most common joint requiring surgery
Most common reconstructive hand surgery
BUT…
Surgical times can differ
Eliminating K-wire
Cost factors
2/11/2014
2
Surgical Factors to Consider
•Time of procedure: Less is better
Surgical Factors to Consider
•Eliminating K-wire: Less discomfort post-op
•Possibility of collapse: Longer term issue
•Cost: Lower is better
•Tendon: Do we really need it?
Study Question
•Standard complete trapeziectomy
•Suspend by a “weave” of #2 Fiberwire between the
APL and FCR at their distal most insertions
•No tendon graft
•Casted for 4 weeks
•Standard post-op hand therapy protocol
2/11/2014
3
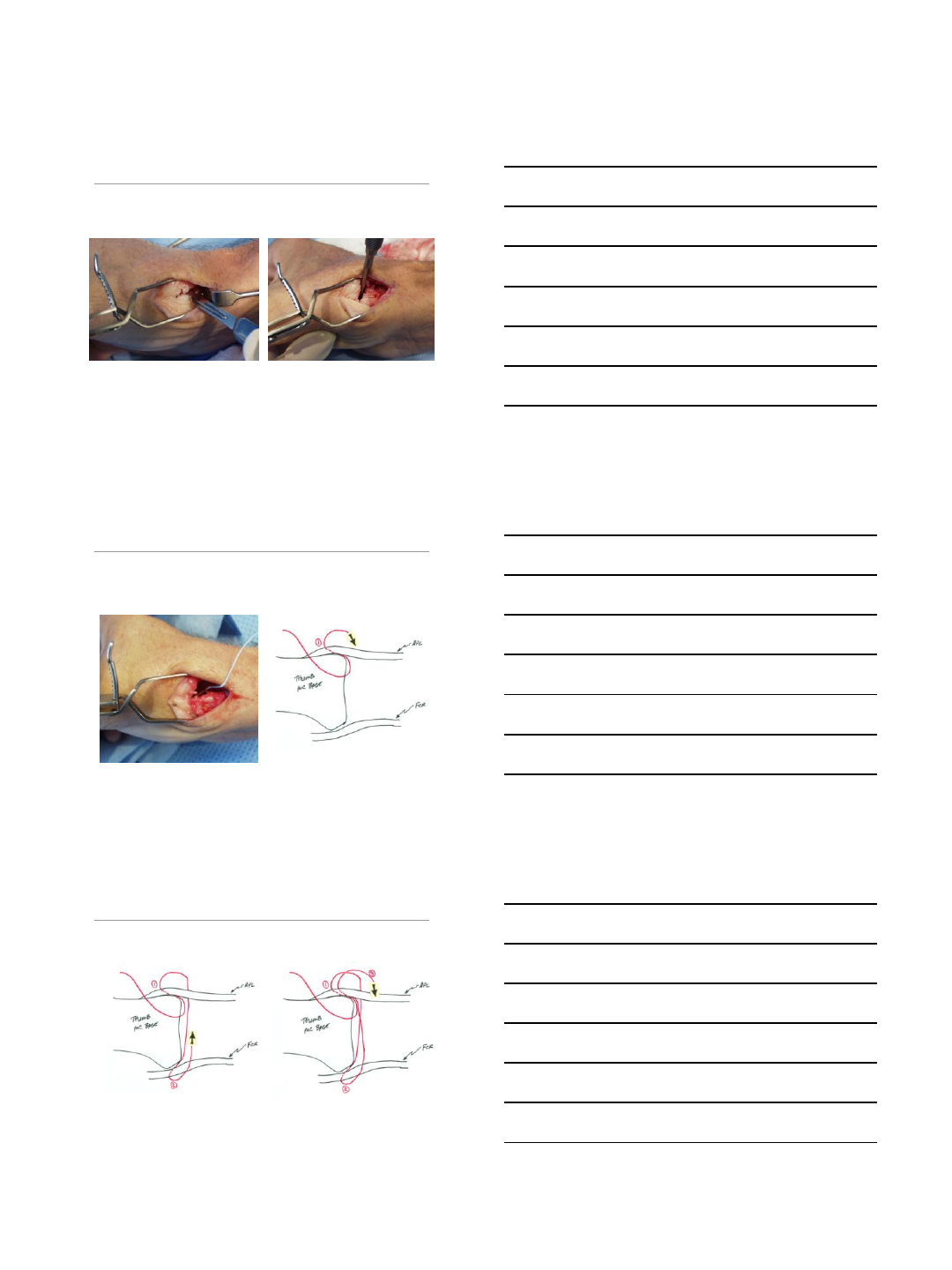
Suture Suspension Technique
(n=65)
•Complete trapeziectomy
Suture Suspension Technique
(n=65)
•#2 Fiberwire through distal APL insertion then
through distal FCR then back through APL and
once more through FCR
Suture Suspension Technique
(n=65)
2/11/2014
4
Suture Suspension Technique
(n=65)
Suture Suspension Technique
(n=65)
•Tie the suture ends and test longitudinal stability
NO – don’t tether the two tendons
2/11/2014
5
Results
•Minimum of 2 year follow-up examination
•Age: 51.3 yrs
•Average OR time = 23 minutes
•No radiographic collapse in any patient
•Pinch & grip strength plateau at 4 months
•Pain: VAS score of 0.2 (0 – 10) at final F/U exam
Discussion
•Clinical results and outcomes equal to other
reported techniques
•Shortened operative time; Inexpensive
•Intrinsic & immediate stability
•A viable alternative to time intensive techniques
•Data is preliminary but promising
Thank You
1
“Minimally” Invasive Options & Role
of Tightrope in the Management of
Basilar Thumb Arthritis
Sanj Kakar MD, MRCS
Associate Professor of Orthopaedic Surgery
Mayo Clinic, Rochester
SOMOS SL Symposium Summary.pptx
Disclosures
•Basic Science Research Grants
•ASSH
•Mayo Foundation
•Consulting
•Arthrex
•Skeletal Dynamics
No financial relationship with Tightrope
Anatomy of 1st CMC Jt
•Biconcave saddle shaped joint
•Little osseous stability
•Semi-constrained, relatively incongruent
•Motion:
•Flex-extension
•Abduction-adduction
•Rotation
2
Forces to Consider
Cooney WP. JBJS 1977
•Forces across TM joint
–Simple pinch
–12 kg force
–Strong grasp
–120 kg force
–Important consideration
especially in a young
patient
Ideal surgical procedure for
1st CMC arthritis
•Pain relief
•CMC motion / position
•MP joint (hyperextension)
•Pinch and grip strength
•Minimal complications
•Reproducible
•Long lasting
Treatment: Operative
•Trapezial resection alone
•Trapeziectomy & suspension
•Arthrodesis
•Implant arthroplasty
•Altering normal anatomy & mechanical
function
•↓ span of hand & dexterity with fine manipulation
(fusion)
•Prolonged recovery
•What’s the salvage when they fail ?
e.g. young pt, manual labourer
3
Are there minimally
invasive treatment
options?
Can we maintain the trapezium?
Denervation of CMC
Joint
Proposed Advantages
•Pain relief
•Without compromise of ROM & strength
•Minimal rehabilitation
•Doesn’t burn bridges for future tx
4
Innervation of Thumb CMC Jt
•SBRN
1. dorso-radial collateral of thumb
2. Lejar’s branch
3. dorso-ulnar collateral of thumb
4. dorso-radial collateral of index
5. Anastomoses between 3 & 4
•LABCN
•Cruveilhier’s branch
•Median nerve
•Thenar branch
•Palmar cutaneous nerve
•Branch of deep motor ulnar nerve
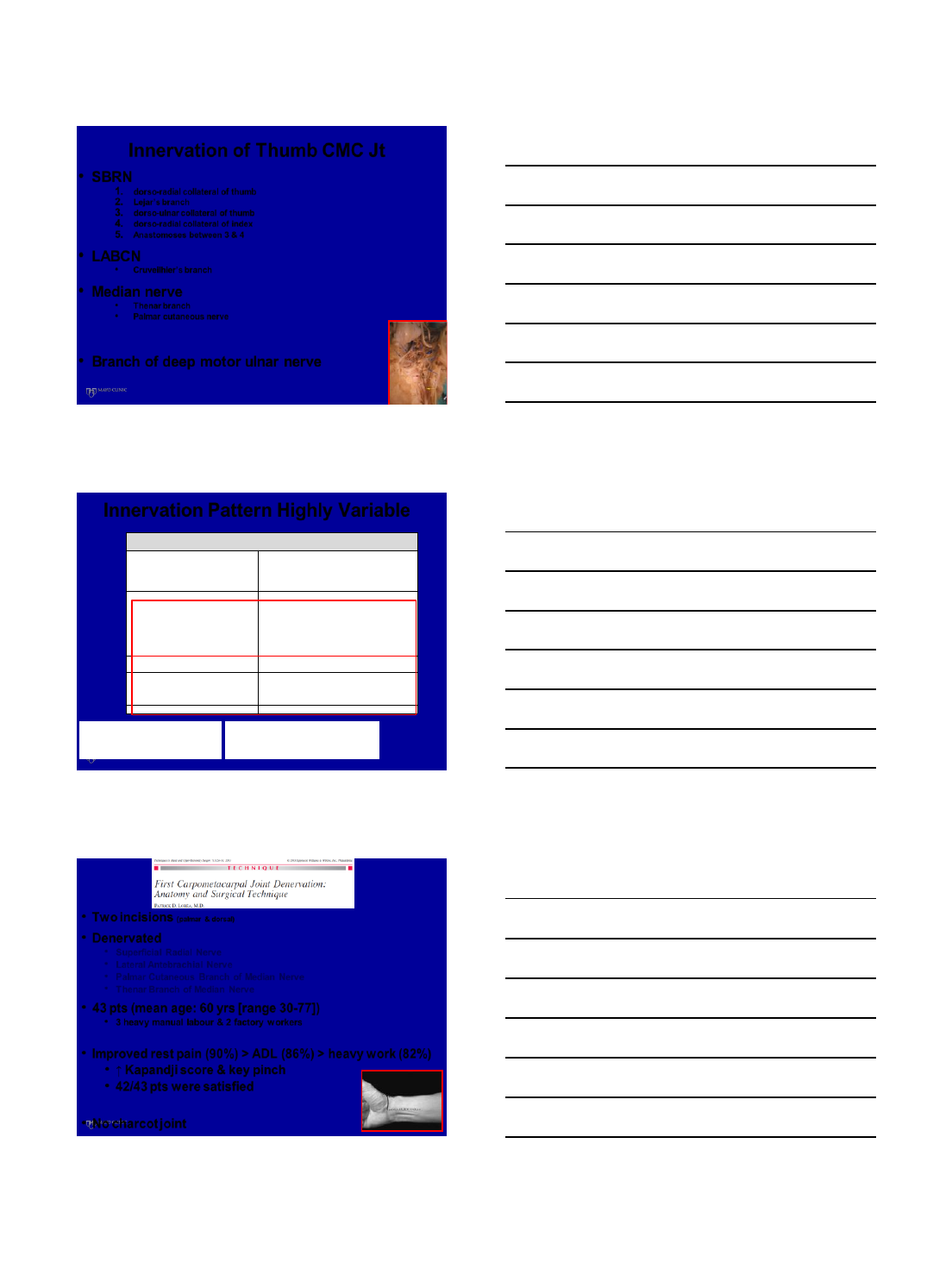
Table 1 - Innervation Patterns of the Trapezio-Metacarpal Joint
Author
Cozzi
Loréa et al
Poupon et al
Miki et al
Year
1991
2002
2004
2011
Limbs
500
10
15
19
Right side
-
-
8
10
Male
-
-
-
7
Posterior Interosseous Nerve
-
0
-
-
Sup. Rad. N. not otherwise specified
100%
10 (100%)
15 (100%)
11 (58%)
Dorso-radial collateral of the thumb
70%
+
15 (100%)
-
Dorso-ulnar collateral of the thumb
+
+
3 (20%)
-
Dorso-radial collateral of the first finger
+
+
1 (7%)
-
Lejars branch
30%
-
14 (93%)
-
Dorsal articular nerve of Winckler's first
interosseous space
-
**9 (90%)
***3 (20%)
-
Lateral Antebrachial Nerve
-
+
-
-
Cruveilhier's branch
-
10 (100%)
-
-
Anterior Interosseous Nerve
-
0
-
-
Palmar Cutaneous branch
* - (5%)
9 (90%)
11 (73%)
0
Thenar Branch Median branch
* - (5%)
9 (90%)
13 (87%)
9 (47%)
Intra-canal branch of thenar branch
-
2 (20%)
5 (30%)
-
Motor Branch of Ulnar Nerve
-
0
-
9 (47%)
-: did not look at this nerve or branch
+: looked at this nerve or branch, but did not note a
number of articulation branches
0: looked at this nerve or branch, but did not find any
articulating branches
* estimation by author
** originated from dorso–ulnar digital nerve of the thumb in
2, dorso-radial digital nerve of the index finger in 3 and for
the bifurcation between these branches in 4
*** derived from dorso-radial collateral of the first finger
DeMooj, Berger & Kakar 2014 (in works)
Innervation Pattern Highly Variable
•Two incisions (palmar & dorsal)
•Denervated
•Superficial Radial Nerve
•Lateral Antebrachial Nerve
•Palmar Cutaneous Branch of Median Nerve
•Thenar Branch of Median Nerve
•43 pts (mean age: 60 yrs [range 30-77])
•3 heavy manual labour & 2 factory workers
•Improved rest pain (90%) > ADL (86%) > heavy work (82%)
•↑ Kapandji score & key pinch
•42/43 pts were satisfied
•No charcot joint
5
•Wagner approach
•Denervated
•Superficial Radial Nerve
•Lateral Antebrachial Nerve
•Palmar Cutaneous Branch of Median Nerve
•Thenar Branch of Median Nerve
•16 pts (18 thumbs)
•14/16 pts → satisfied or very satisfied
•NO formal pain assessment/?degree of arthritis
•Complications: 2 pts → painful HT scar
1 pt → hypoaesthesia over dorsum thumb
Tech Hand & Upper Extrem Surg 2012
Thumb Metacarpal
Osteotomy
Pelligrini VD Jr. et al J Hand Surg,
1991;16A:967-974
Ligament Laxity Theory of Thumb
Arthritis
•Volar beak ligament degenerates & detaches
•Abnormal shear stresses across anterior
compartment of joint causes CMC arthritis
- Degeneration of palmar metacarpal cartilage
- Exacerbated by pinching (flexion & adduction of 1st metacarpal)
•Extension osteotomy of 1st metacarpal
- Palmar contact unloaded & contact pressure moved dorsally
- Indications: Eaton stage 1 disease
Pelligrini VD Jr. et al J Hand Surg, 1996;21A:16-
23
Pelligrini VD Jr. et al
6
•Prospective study (12 pts, Eaton stage 1)
•Average f/up 2.1 yrs
•300 metacarpal extension osteotomy
•Results
•Union at 7 wks
•11/12 pts satisfied
•↑ grip & pinch strength
•All pts returned to work
•8 pts (3 Eaton stage 1, 3 Eaton stage 2 & 2 Eaton stage 3)
•Average f/up 9 yrs
•Results
•↑ grip strength (108% of contralateral side)
•↑ appositional pinch strength (129%)
•↑ oppositional pinch strength (103%)
•6/8 pts → excellent functional outcomes
•Eaton stage preserved 5/8 pts
Arthroscopic Treatment
7
Arthroscopy for CMC OA
•Technique - Berger, JHS, 1997
•Portals (locate with 18 g needle +/- fluoro)
•1R (radial to APL at CMC jt)
•1U (ulnar to EPB at CMC jt)
•Dangers
•SBRN, radial artery
•Equipment
•Thumb in txn (5-10lbs)
•Insufflate jt (2mls 1U portal)
•1.9mm short barrel scope
•2mm shaver through 1R to debride synovitis
(use 2.9mm burr once space ↑ within a 3.5mm sheath to prevent
clogging during trapeziectomy)
•Replace 1R with thenar portal
•Arthroscope in 1U portal
•Thenar portal 900 to 1U portal
•Results (thenar portal)
•Good working portal
•↓ sword fighting
•Didn’t violate the dAOL
•Further away from sensory nerves than 1R
•23mm away from recurrent motor branch median nerve
Advantages of CMC Arthroscopy Menon 1996
•↓ invasion compared to open approach
•↓ postop pain & stiffness
•Quicker rehabilitation
•Doesn’t burn any bridges
8
•Stage 1
•Synovitis & ligamentous laxity
•Synovectomy +/- thermal shrinkage
•Stage 2
•Cartilage loss on ½ trapezium
•Metacarpal extension osteotomy
•Arthroscopic tx
•Stage 3
•Diffuse cartilage loss
•Arthroscopic hemitrapeziectomy
What Does The Literature Show
As To Efficacy of Tx !!!
•23 pts (Eaton stage 1 & 2)
•Arthroscopic synovectomy & debridement & splint 1wk
•Control grp: 21 pts non op tx
•Evaluated 1 yr later
•Results
•83% surgical pts → good to exc results
•Surgical pts:
•↓ pain, ↑ DASH & pinch strength
•Complications
•Wound infection (1)
•DSRN irritation (1R)
9
•23 pts (Eaton stage 3)
•Hemitrapeziectomy (3-4mm)
•CMC jt pinned (3-4 wks)
•>4 year follow up
•Results
•19/23 pts pleased with results
•↑ DASH & pinch & grip strength
•Proximal migration ~ 3mm
•Complications
•1 Wound infection
•1 DSRN irritation (1R)
•1 pt → LRTI
•14 pts (Eaton 2 & 3)
•Hemitrapeziectomy & interposition (PL, FCR)
•F/up: 11 months (3.3-17.3)
•Results
•VAS ↓8.6→ 1.8 (p<0.005)
•90% restoration grip & pinch strength
•10/11 pts → “much better”
•Complications
•1 CRPS
•? 1Graft extrusion
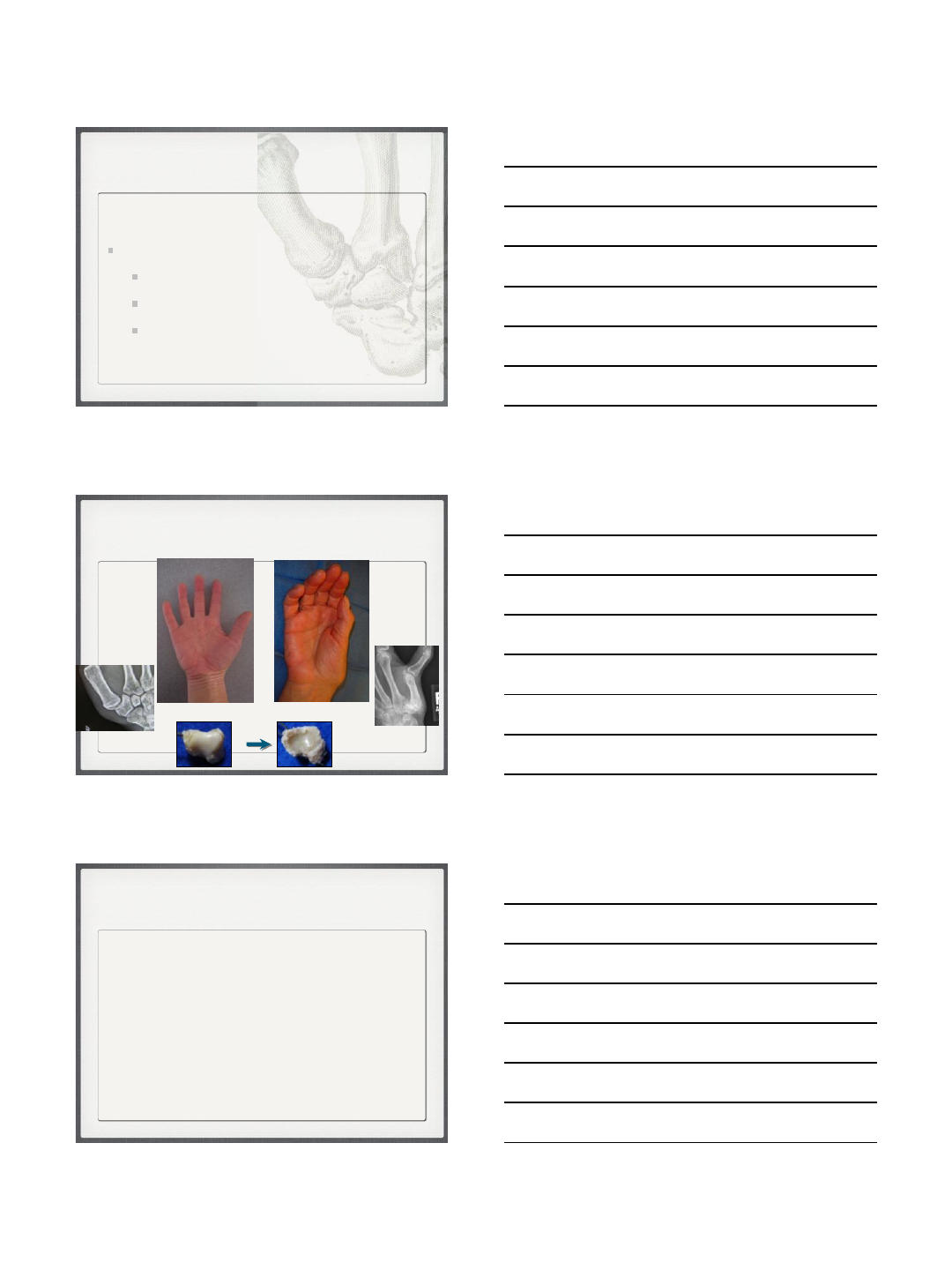
Tightrope
Suspension Arthroplasty
10
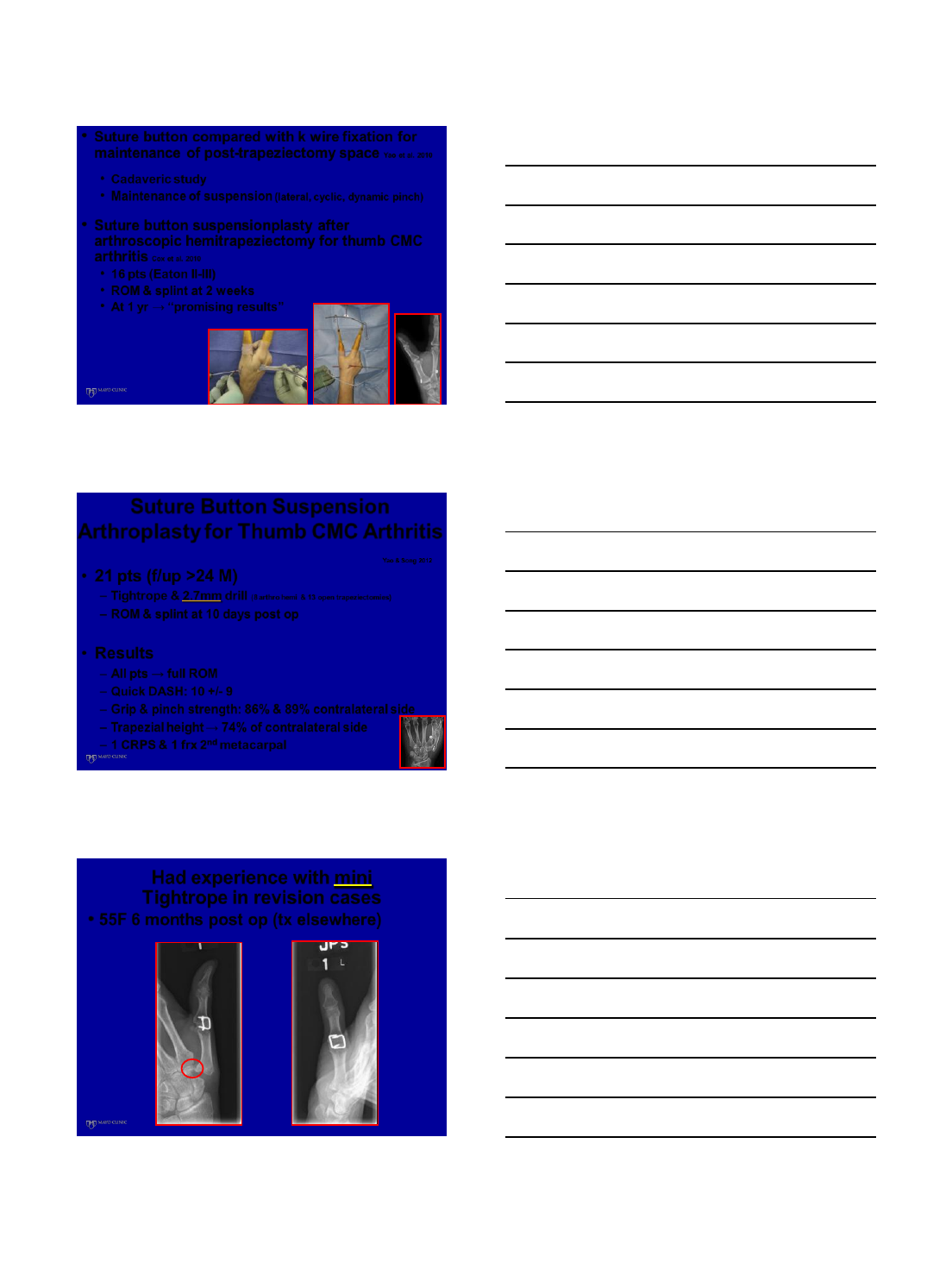
•Suture button compared with k wire fixation for
maintenance of post-trapeziectomy space Yao et al. 2010
•Cadaveric study
•Maintenance of suspension (lateral, cyclic, dynamic pinch)
•Suture button suspensionplasty after
arthroscopic hemitrapeziectomy for thumb CMC
arthritis Cox et al. 2010
•16 pts (Eaton II-III)
•ROM & splint at 2 weeks
•At 1 yr → “promising results”
•21 pts (f/up >24 M)
–Tightrope & 2.7mm drill (8 arthro hemi & 13 open trapeziectomies)
–ROM & splint at 10 days post op
•Results
–All pts → full ROM
–Quick DASH: 10 +/- 9
–Grip & pinch strength: 86% & 89% contralateral side
–Trapezial height → 74% of contralateral side
–1 CRPS & 1 frx 2nd metacarpal
Suture Button Suspension
Arthroplasty for Thumb CMC Arthritis
Yao & Song 2012
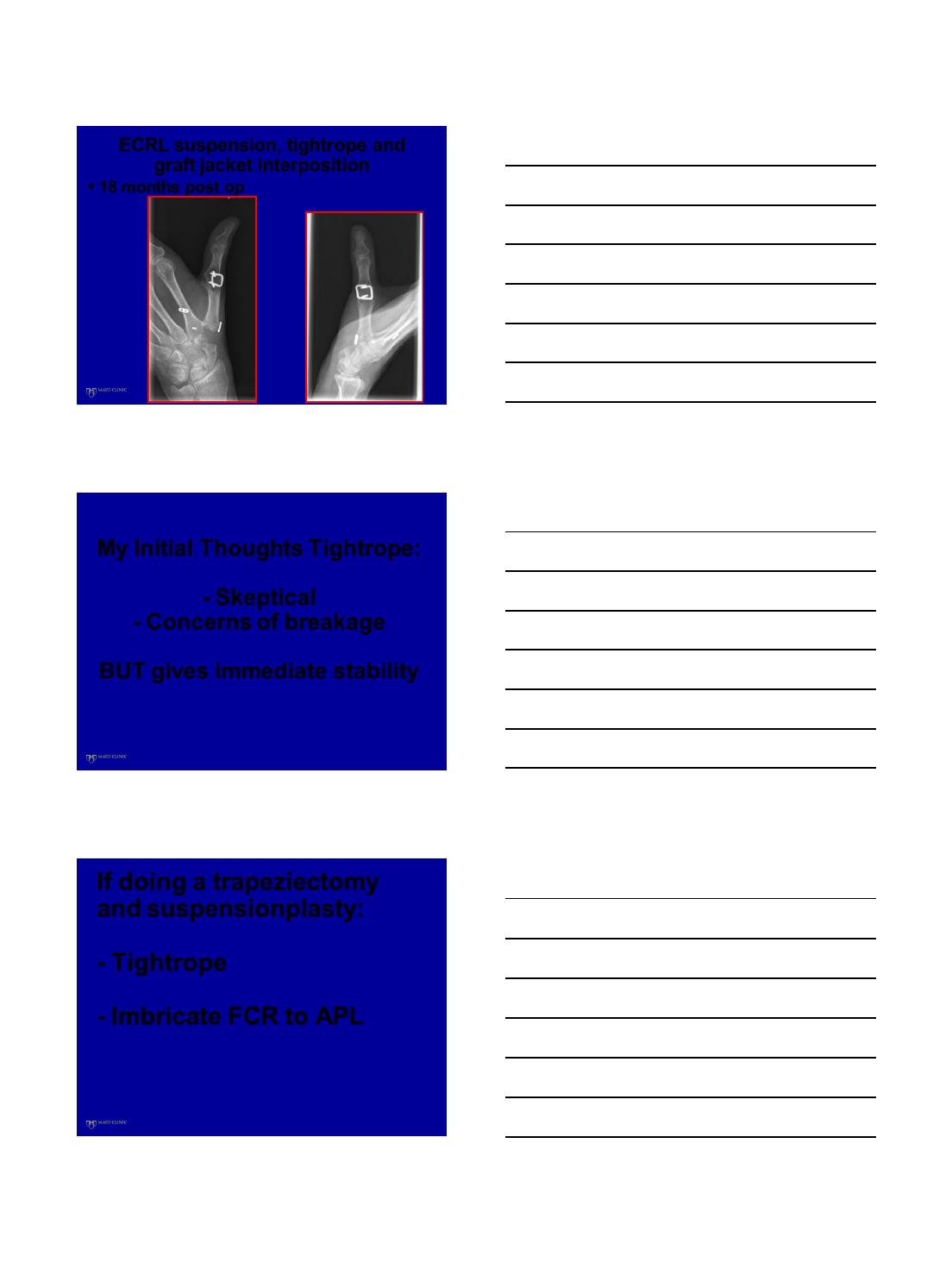
Had experience with mini
Tightrope in revision cases
•55F 6 months post op (tx elsewhere)
11
ECRL suspension, tightrope and
graft jacket interposition
•18 months post op
My Initial Thoughts Tightrope:
- Skeptical
- Concerns of breakage
BUT gives immediate stability
If doing a trapeziectomy
and suspensionplasty:
- Tightrope
- Imbricate FCR to APL
12
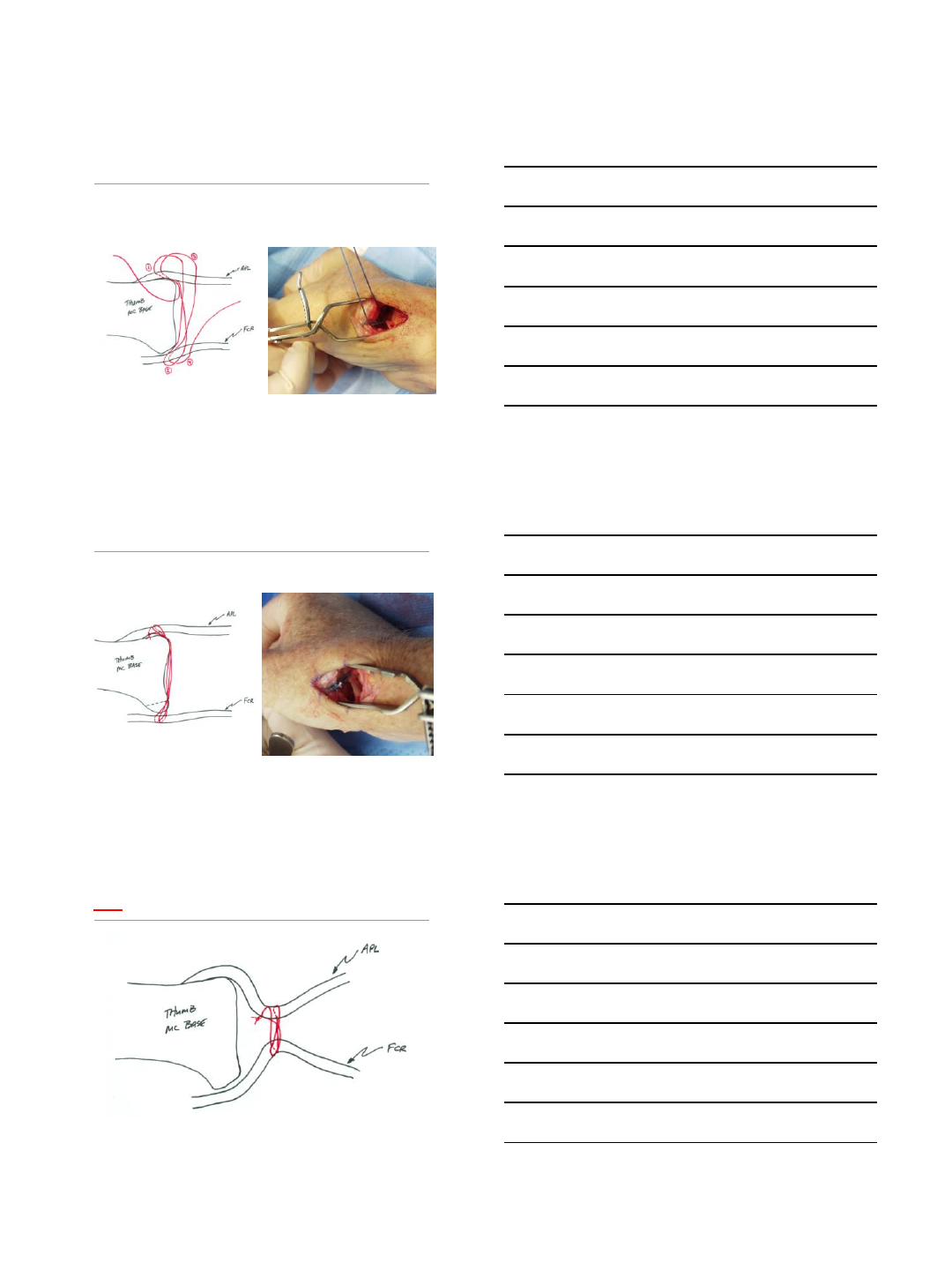
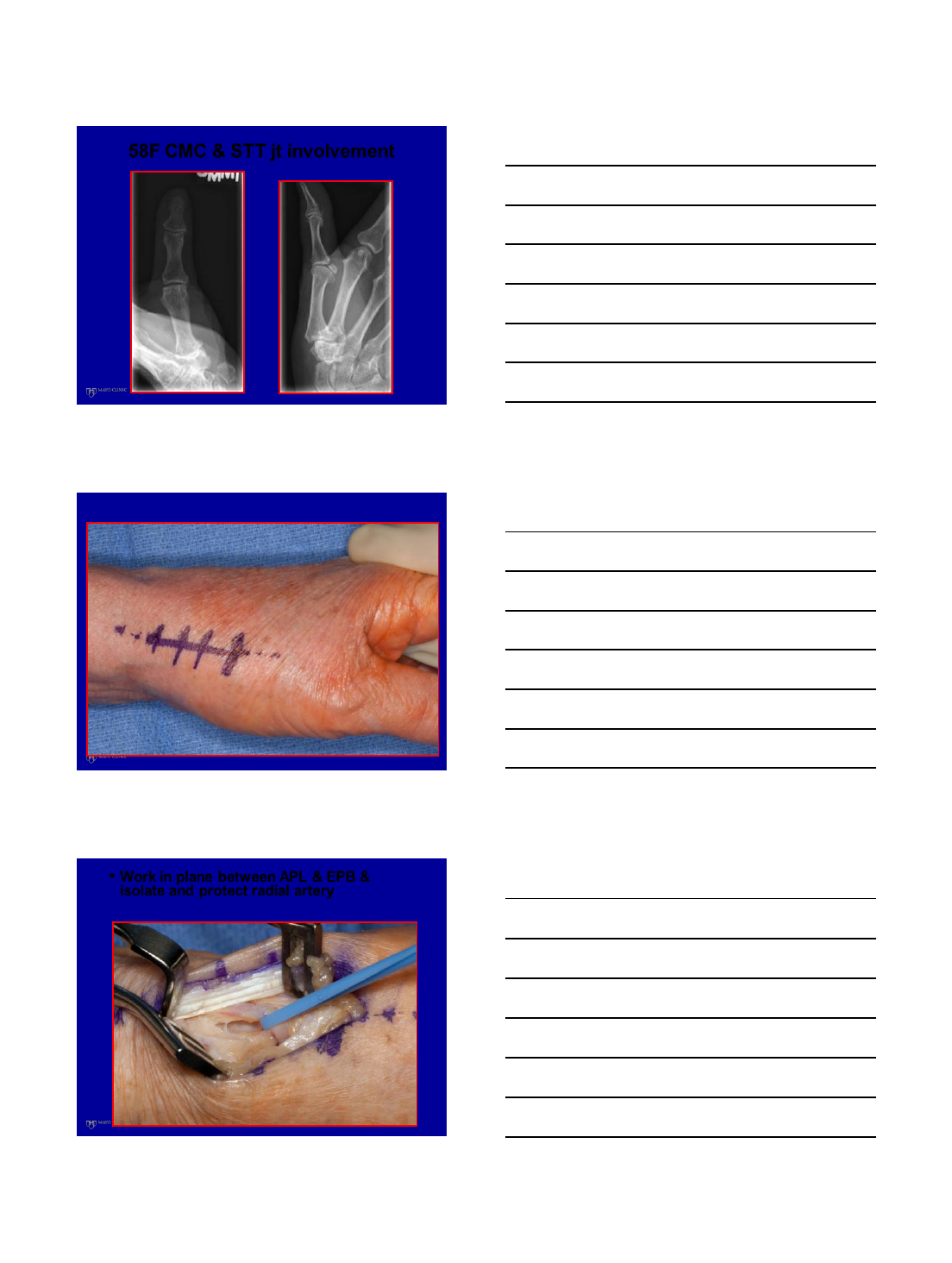
58F CMC & STT jt involvement
•Work in plane between APL & EPB &
isolate and protect radial artery
13
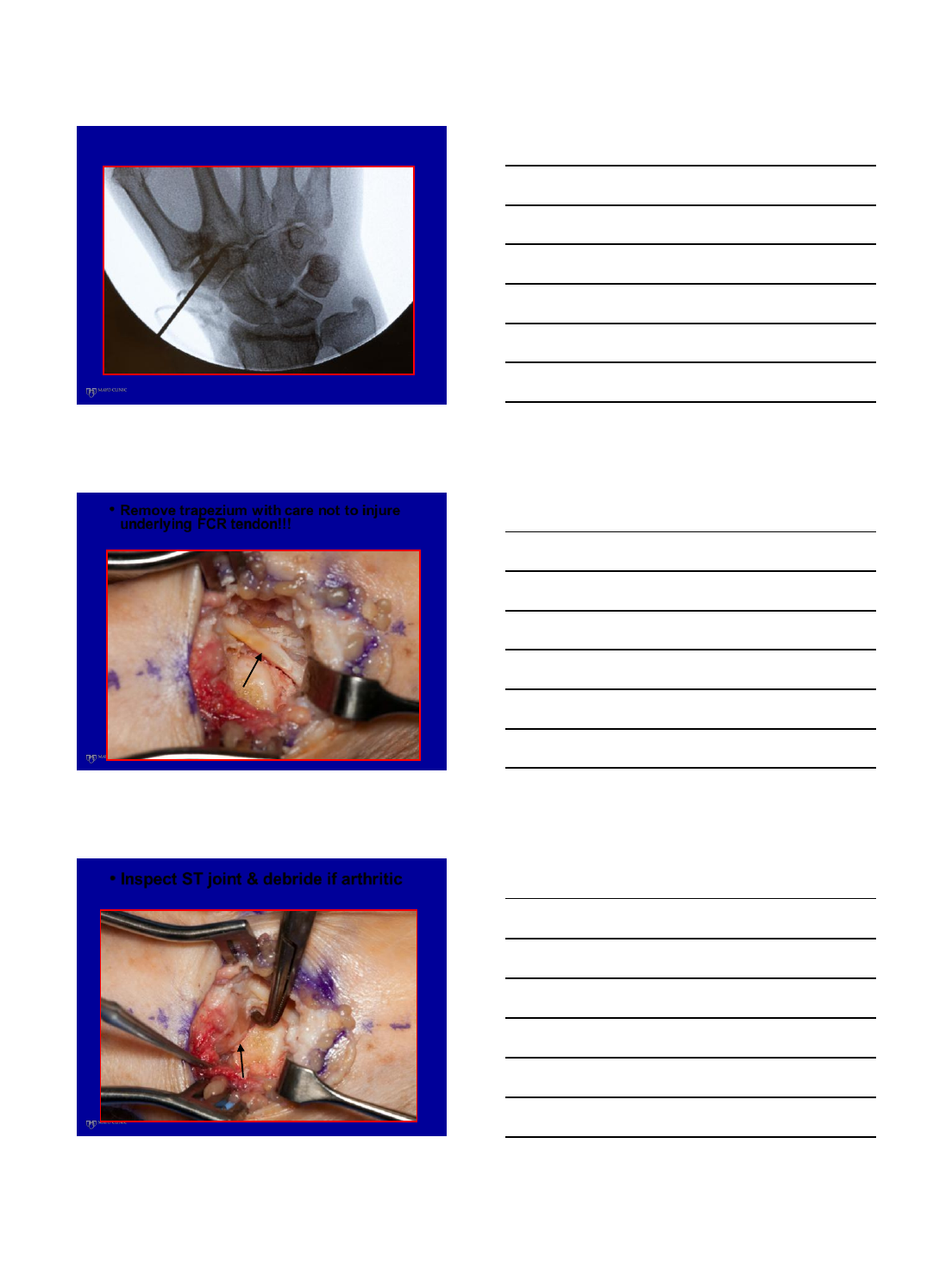
•Remove trapezium with care not to injure
underlying FCR tendon!!!
•Inspect ST joint & debride if arthritic
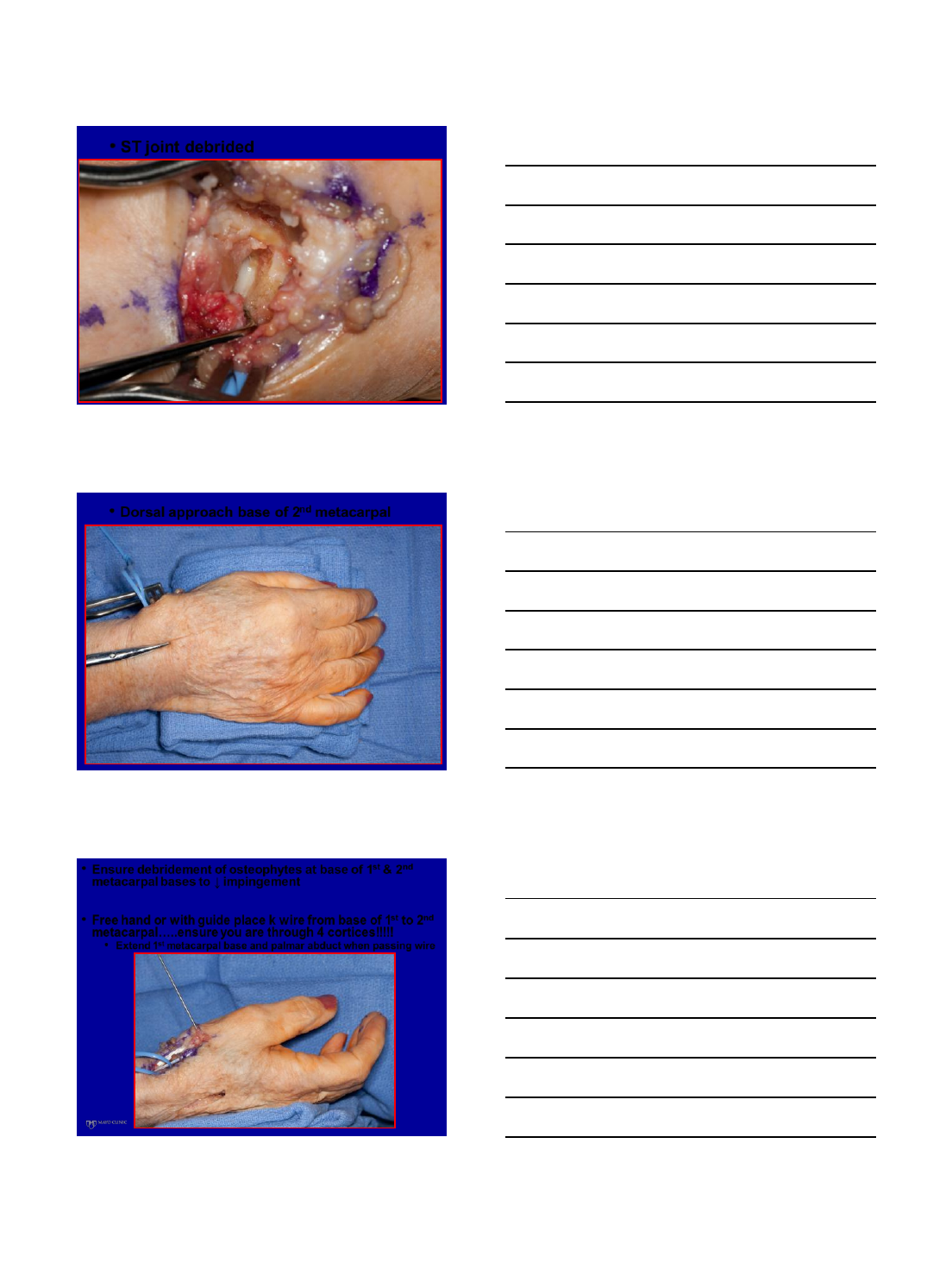
14
•ST joint debrided
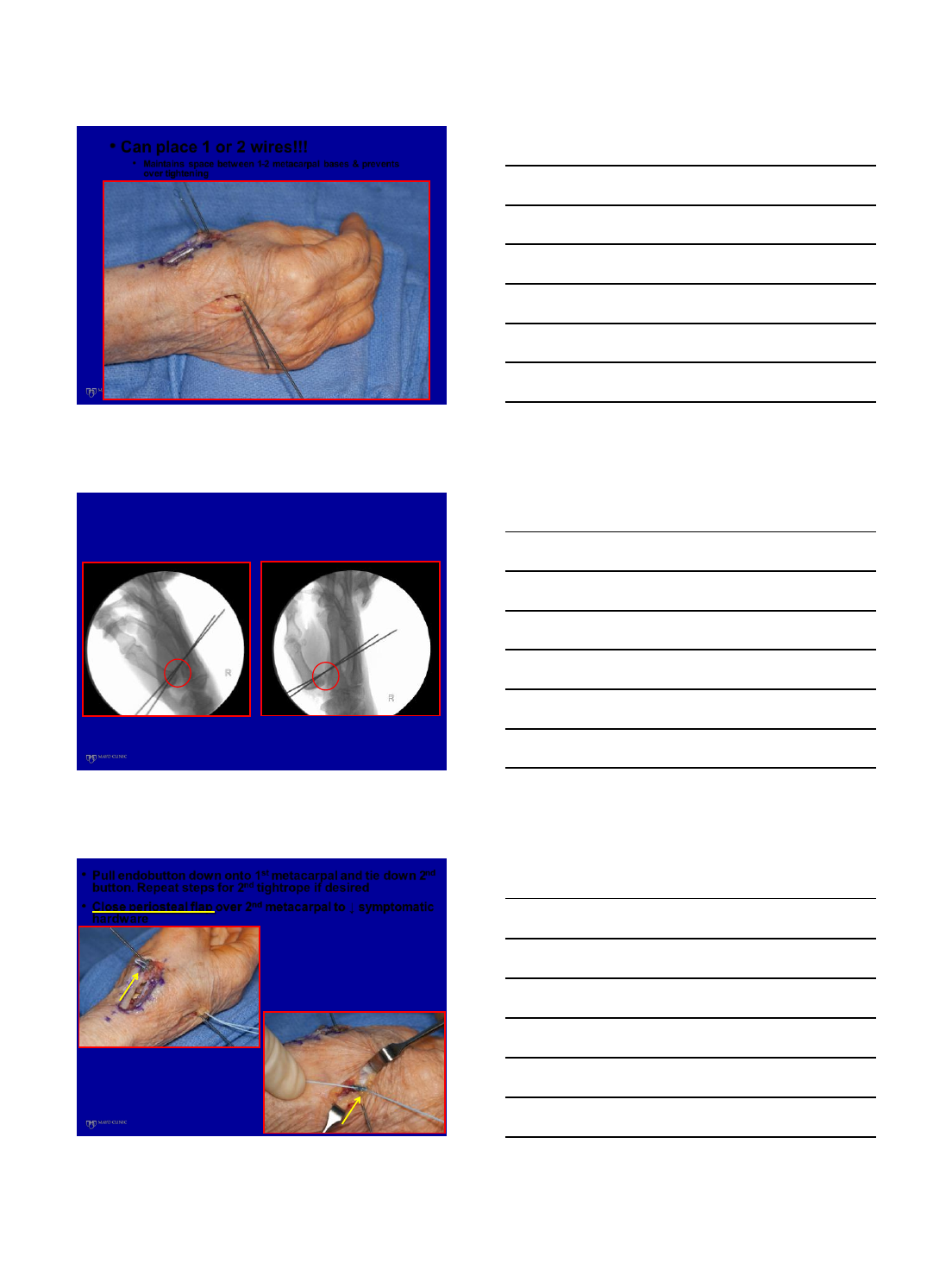
•Dorsal approach base of 2nd metacarpal
•Ensure debridement of osteophytes at base of 1st & 2nd
metacarpal bases to ↓ impingement
•Free hand or with guide place k wire from base of 1st to 2nd
metacarpal…..ensure you are through 4 cortices!!!!!
•Extend 1st metacarpal base and palmar abduct when passing wire
15
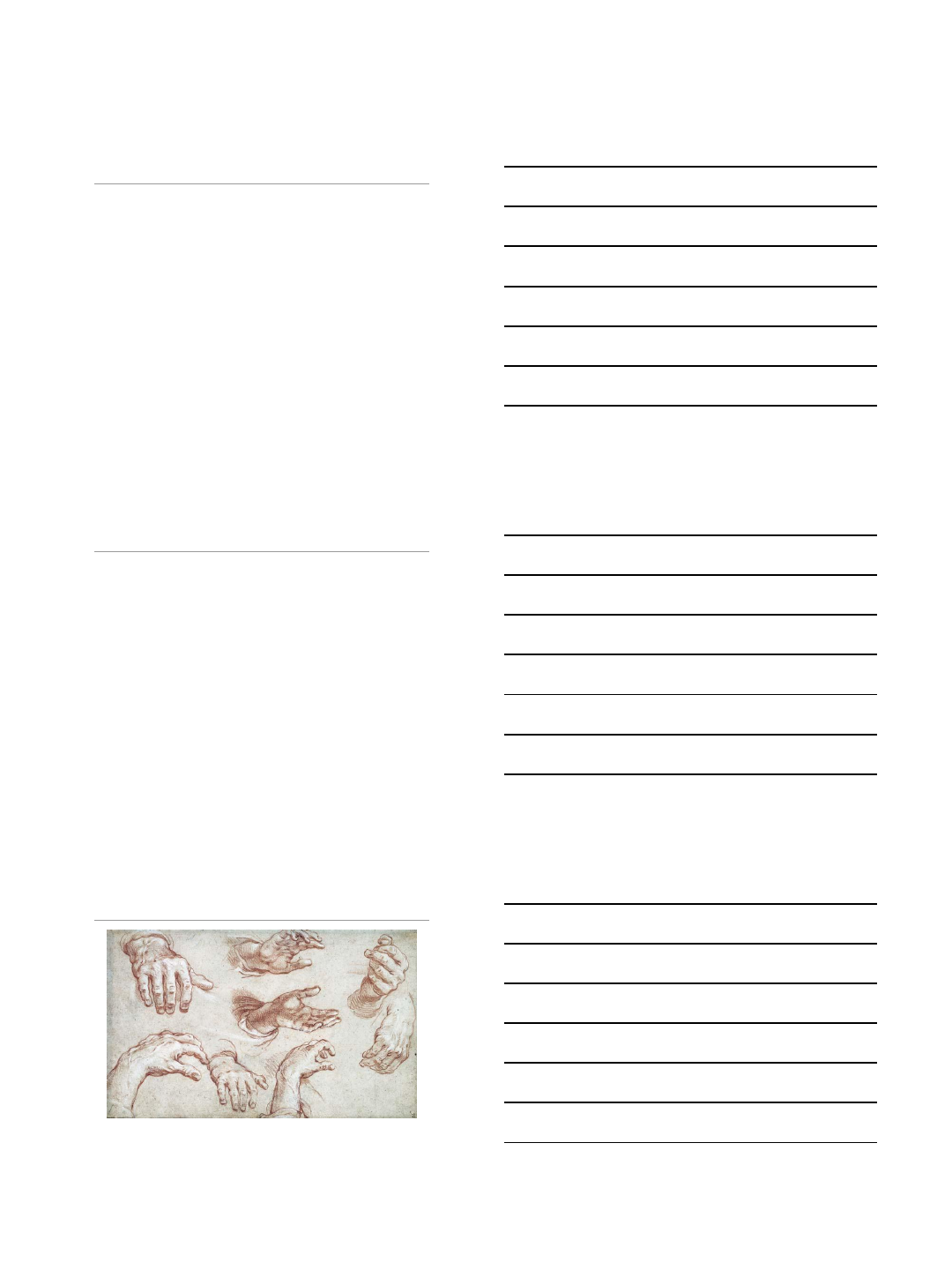
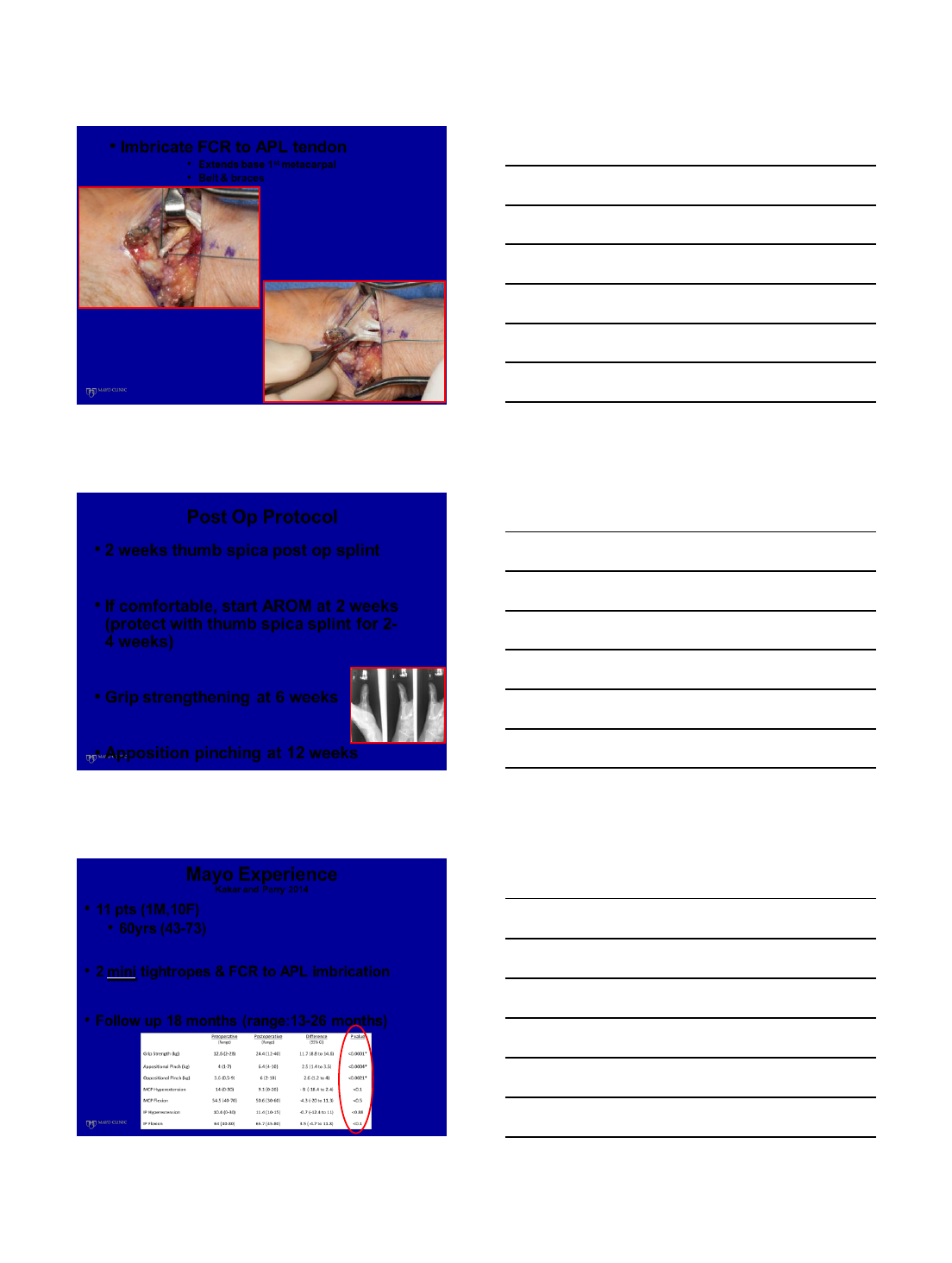
•Can place 1 or 2 wires!!!
•Maintains space between 1-2 metacarpal bases & prevents
over tightening
•Pull endobutton down onto 1st metacarpal and tie down 2nd
button. Repeat steps for 2nd tightrope if desired
•Close periosteal flap over 2nd metacarpal to ↓ symptomatic
hardware
16
•Imbricate FCR to APL tendon
•Extends base 1st metacarpal
•Belt & braces
Post Op Protocol
•2 weeks thumb spica post op splint
•If comfortable, start AROM at 2 weeks
(protect with thumb spica splint for 2-
4 weeks)
•Grip strengthening at 6 weeks
•Apposition pinching at 12 weeks
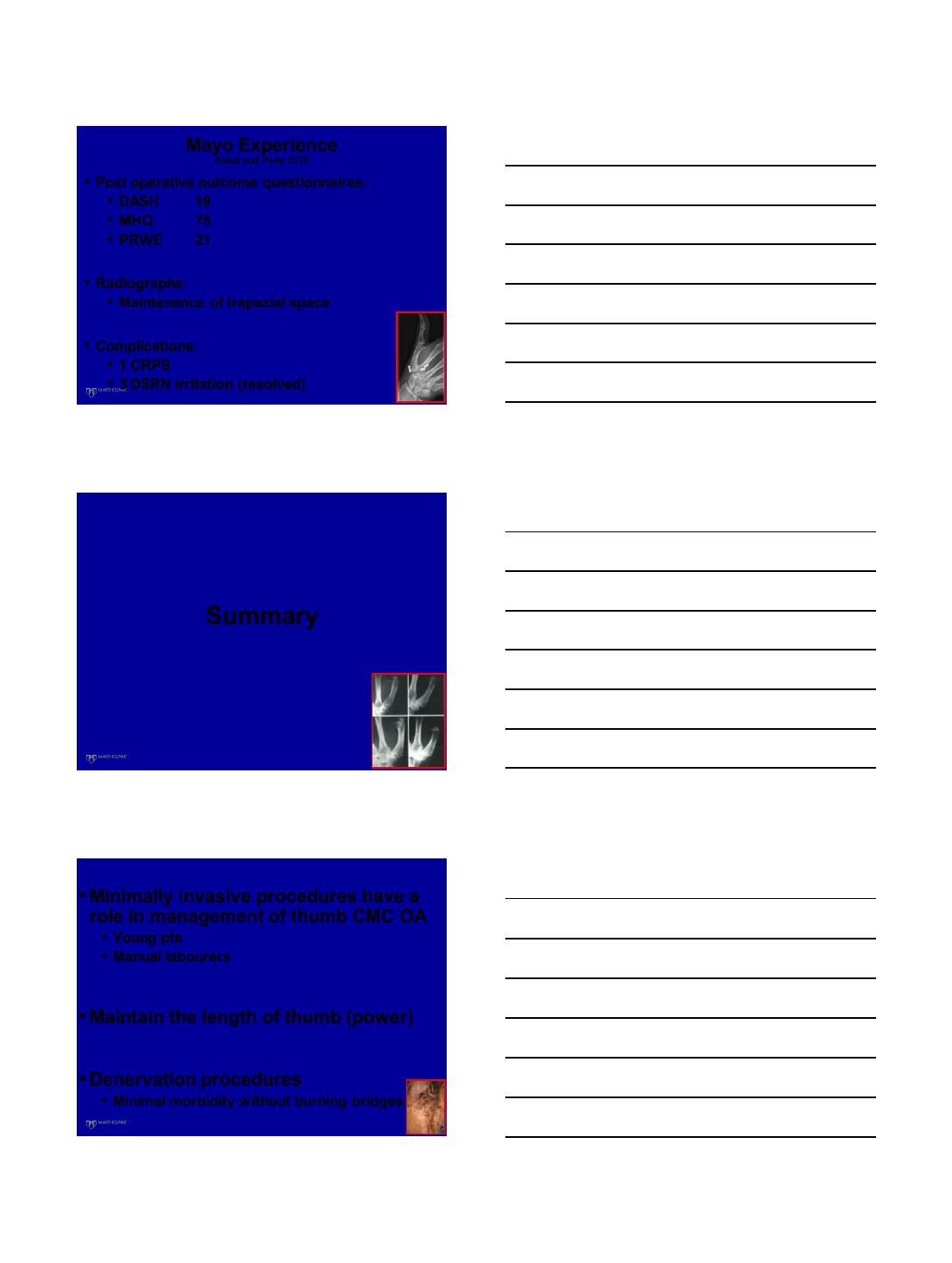
Mayo Experience
Kakar and Parry 2014
•11 pts (1M,10F)
•60yrs (43-73)
•2 mini tightropes & FCR to APL imbrication
•Follow up 18 months (range:13-26 months)
17
Mayo Experience
Kakar and Parry 2013
•Post operative outcome questionnaires:
•DASH 19
•MHQ 75
•PRWE 21
•Radiographs:
•Maintenance of trapezial space
•Complications:
•1 CRPS
•3 DSRN irritation (resolved)
Summary
•Minimally invasive procedures have a
role in management of thumb CMC OA
•Young pts
•Manual labourers
•Maintain the length of thumb (power)
•Denervation procedures
•Minimal morbidity without burning bridges
18
•Arthroscopy
•Similar results to open tx
•No PRCT compared to open tx
•Eaton 1:
•Debridement & synovectomy
•Metacarpal extension osteotomy
•Eaton 2-3:
•Hemitrapeziectomy +/- interposition +/-
tightrope
•Eaton 4:
•Trapeziectomy +/- tightrope
Thank You For Your Attention
Email:
Kakar.sanjeev@mayo.edu
2/11/2014
1
VuMEDI:
Why Do Men Get Thumb
CMC Arthritis?
Jennifer Moriatis Wolf, MD
Associate Professor
Department of Orthopedic Surgery
University of Connecticut
Disclosures
Grant Funding – AFSH, OREF, University of
Connecticut
Salary – Deputy Editor of Journal of Hand
Surgery, Elsevier Updates Editor
Overview
Epidemiology
Sex Differences
2/11/2014
2
Epidemiology
Incidence of thumb CMC OA
increases with increasing age
in both sexes
Women >> Men
Radiographic
Clinical
Radiographic Differences
Haara et al – large Finnish population study
Incidence of Kellgren-Lawrence grade 3/4 OA of the TM
joint JBJS-A, 2004
14.5% in women
10% in men
Sodha et al – large study of ED radiographs for fracture
JBJS-A, 2005
Noted increasing rate of TM OA with age
In worst TM OA – 66% prevalence in women compared to
23% of men
Symptomatic Differences
Framingham study – prevalence in TM joint
5% in women
2.5% in men Zhang et al, Am J Epidemiol, 2002
Physician-diagnosed TM OA in Sweden
Primarily captured public health system
Overall prevalence of 2.2% in women and
0.69% in men
Men diagnosed over a decade later than
women
Wolf et al, Arthr Care Res, 2013
2/11/2014
3
Why the Sex Difference?
Not known
Anatomy
Biomechanics
Hormones
Occupation
Genetics
Anatomy
Saddle-shaped joint
Stabilized by ligaments to
provide mobility and stability
Ligaments have been studied
for strength
Best recent data indicates
dorsoradial ligament (DRL)
major stabilizer Ladd, Hagert JBJS-A, 2012
As opposed to thinner AOL
JAAOS, 2010
Sex Difference in Bony/
Ligamentous Anatomy
Study in 18 female and 13 male cadavers
Average age 71.4 years
Used micro-calipers to measure
Metacarpal width
Trapezial width
Ligament thickness
Men had greater width of metacarpal and trapezium (mean
18.83 mm vs. 16.65 mm)
Men had thicker DRL, sAOL
Gerhardt, Baldini, Wolf, unpublished data
2/11/2014
4
Biomechanical Differences
Bettinger et al – studied material properties of TM
stabilizing ligaments in 10 male and 10 female cadavers
Ultimate load and stress of AOL significantly higher
in men
Ultimate strain of DT-II MC ligament greater in
women
Bettinger et al, J Hand Surg Am, 1994
Role of laxity
Women have greater overall laxity than males
Larsen et al, Arthr Rheum, 1987
Possible abnormal loading playing a greater role in
women
Men and TM Subluxation
Hunter et al – Framingham study
Osteoarth Cartilage, 2005
203 men and 431 women
Hand radiographs in 1967 and 1993
Evaluated for TM subluxation
Noted that baseline TM
subluxation correlated with
development of later TM OA in
men only
Occupation
No studies evaluating occupation directly between sexes
Framingham study – evaluated grip strength and associated
development of hand OA Chaisson et al, Arthr Rheum, 1999
453 eligible subjects over 30 years
Highest maximal grip strength in men associated with increased
risk of PIP, MCP, and thumb CMC OA
Women’s grip showed correlation with MCP OA only
2/11/2014
5
Hormones
Sex hormones attractive target
Estrogen
Progesterone
Testosterone
Relaxin
Primary evidence in animal studies of OA
Relaxin levels higher in post-menopausal women than
age matched men Wolf et al, J Hand Surg Am, 2013
Further studies ongoing
Genetics
Multiple studies have shown genetic
component in hand OA in general
Ishimori et al showed osteophyte distribution to
be genetically linked Arthr Res Ther, 2010
Mutations in matrilin-3 (ECM protein gene)
linked to more severe form of TM OA
Eliasson et al, Scand J Rheumatol, 2006
Conclusions
Men with TM OA
Present later than women
Possibly different mechanism
?more direct joint load vs. ligament attenuation
Anatomic differences in men and women
Interaction between anatomy, genetics, and
environment may be different in men

2/11/2014
6
THANK YOU