HTO Syllabus
2014-07-01
: Pdf Hto Syllabus HTO_Syllabus 6 2014 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 51
6/30/2014
1
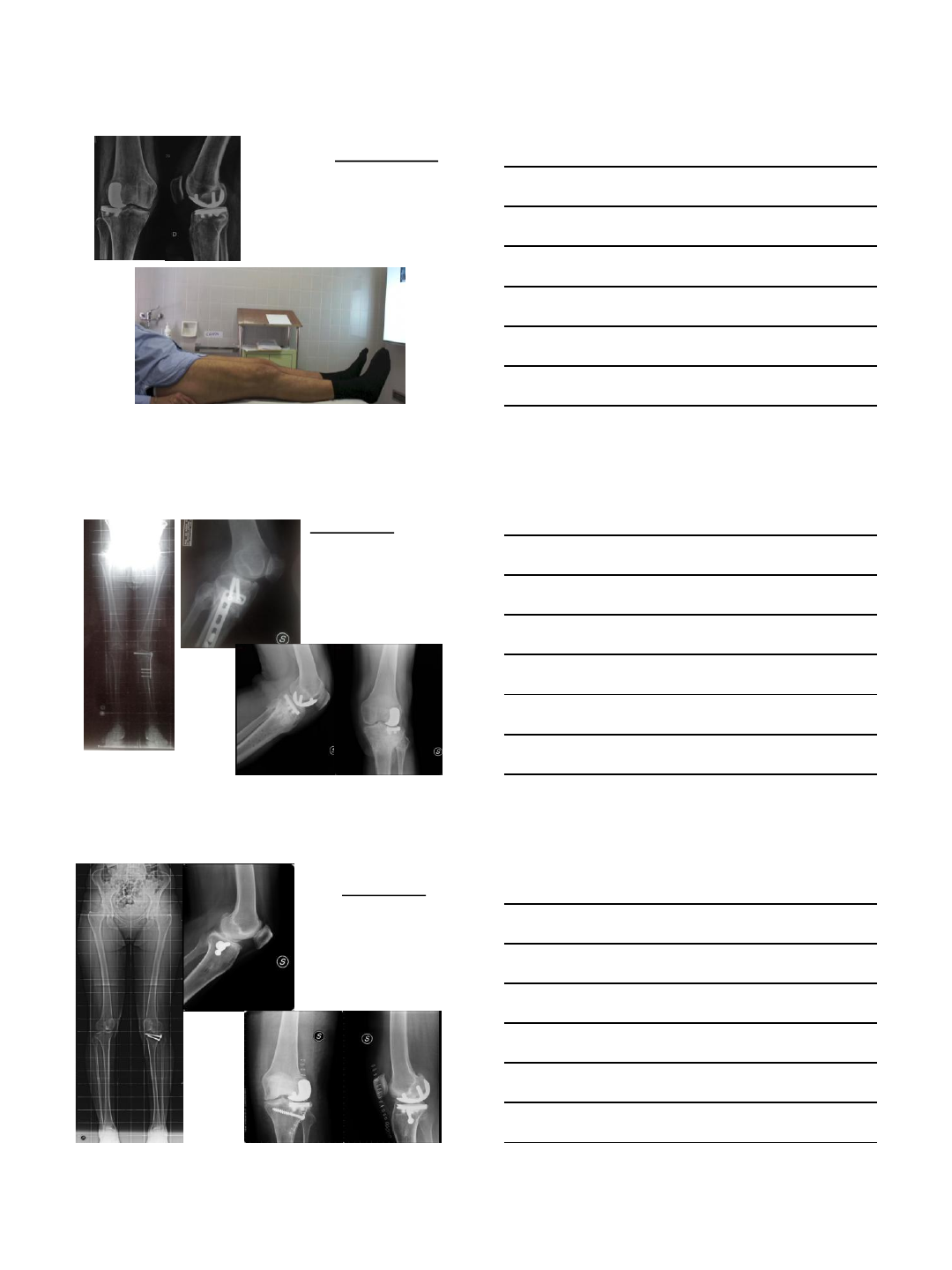
Fixed Unicompartmental Knee
Arthroplasty in Young Osteoarthritic Knee
F. Benazzo, SMP Rossi, M. Ghiara
Clinica Ortopedica e
Traumatologica
Università degli Studi di Pavia
Fondazione IRCCS Policlinico
San Matteo
Direttore: Prof. F. Benazzo
Disclosure
•LimaCorporate Consultant, Conceptor
•Zimmer Consultant, Conceptor
•Ceramtec Consultant
•Fidia Consultant
UNI and Young Patients
Focus on
•Dilemmas
•Indications and contraindications
•Implant selection with specific indications
•Up-to-date indications (combined implants,
ACL reconstruction, postrauma/osteotomy)
•Return to sport
6/30/2014
2
2012
- Surgeons, given identical information, do not concur
on treatment for patients with the same pathology.
- Decision making process heavily influenced by
radiographic findings but individual surgeons are
consistent with their own treatment choice.
-Consensus treatment for medial osteoarthritis of
the knee remains in question.
Dilemmas
Dilemmas
- If a more standardised approach to offering this surgical care is to be
achieved, then improved decision support for patients around this
specific treatment choice will be required.
- Comprehensive comparative data across the three treatment options
(UKA;TKA;HTO) is not available.
Uni vs TKR
•preservation of bone stock and soft tissues,
•more natural gait pattern and kinematics,
•improved range of motion
•reduced operative time
•reduced incision size.
Dilemmas

6/30/2014
3
Gait:
No differences were noted between the groups
(UKA or HTO) other than at 3 months after surgery
when there was a significant difference in the time-
distance variable of gait in favor of UKR. This
became insignificant at 1-year and 5-year follow-up
Borjesson M, Weidenhielm L, Mattsson E, Olsson E:
Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5-
year follow-up study.
Knee 2005, 12:121-127
Dilemmas
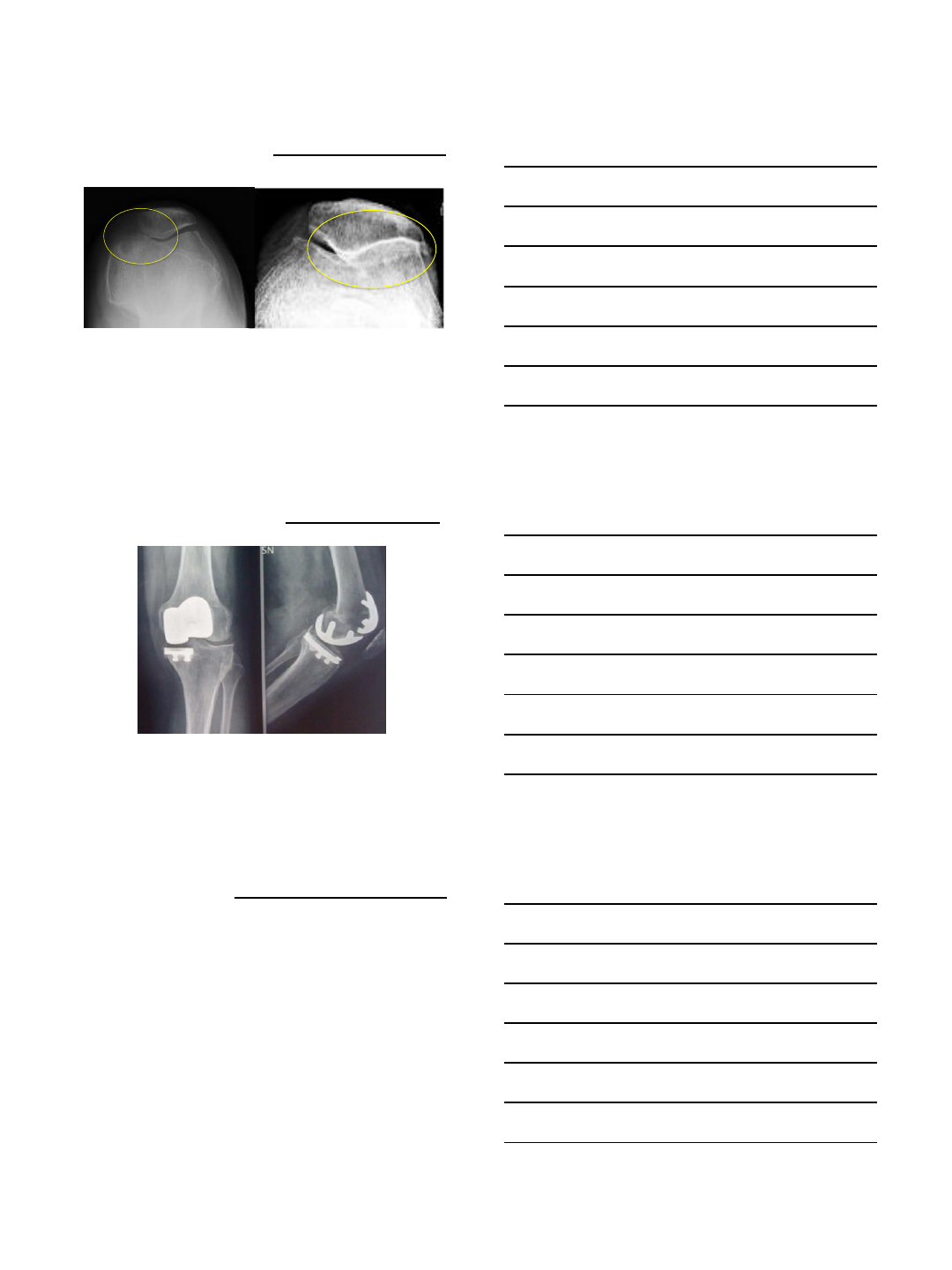
Indications
Classic:
•Unicompartmental degenerative disease (medial or
lateral) with mild degeneration of the opposite side
•Painful osteonecrosis/osteochondritic involvement of the
femoral condyle, with or without rim narrowing
6/30/2014
4
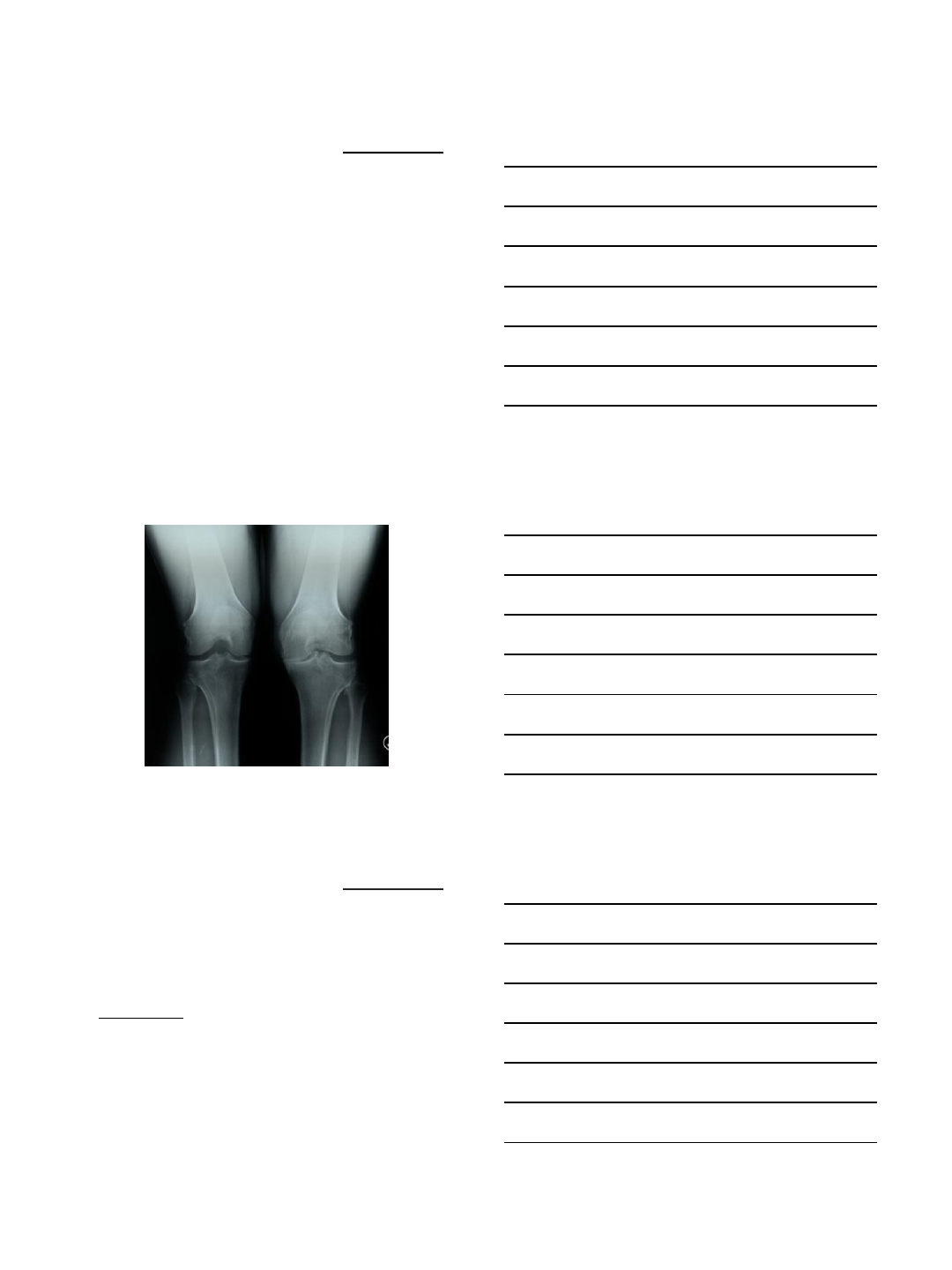
Indications
Classic:
•Deformity of the anatomical axis of the limb due to
narrowing of the joint line for the degenerative disease
and not to deformity of the tibia (schuss x-rays view)
•Deformity correctable manually (stress x-rays) and
therefore surgically, with the thickness of the implant
Indications
Classic:
•Healthy (functionally valid) ACL
•Full or almost full flexion (ROM almost normal)
•Finger sign positive
•Age > 60 years
•BMI < 30
•Varus /valgus deformity < 10°
•Flexion contracture < 10°
6/30/2014
5
Indications
Enlarged:
•Age < 60 years
•BMI >30 … < 32
•Presence of degenerative patello-femoral joint
without anterior knee pain (no full-thickness
chondral lesions or lateral facet involvement)
Indications
Enlarged:
•ACL deficient knee frequent in young patients
- low demanding patients tibial slope < 7°
- Possibility of ACL reconstruction together with the
UNI
Indications
ACL and Tibial slope:
->7° should be avoided
- particularly if the anterior cruciate ligament is absent at
the time of implantation.
- An intact anterior cruciate ligament, even when partly
degenerated, was associated with the maintenance of
normal anteroposterior stability of the knee for an average
of sixteen years following unicompartmental knee
arthroplasty.
Hernigou P, Deschamps G:
Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty.
J Bone Joint Surg Am 2004, 86:506-511
6/30/2014
6
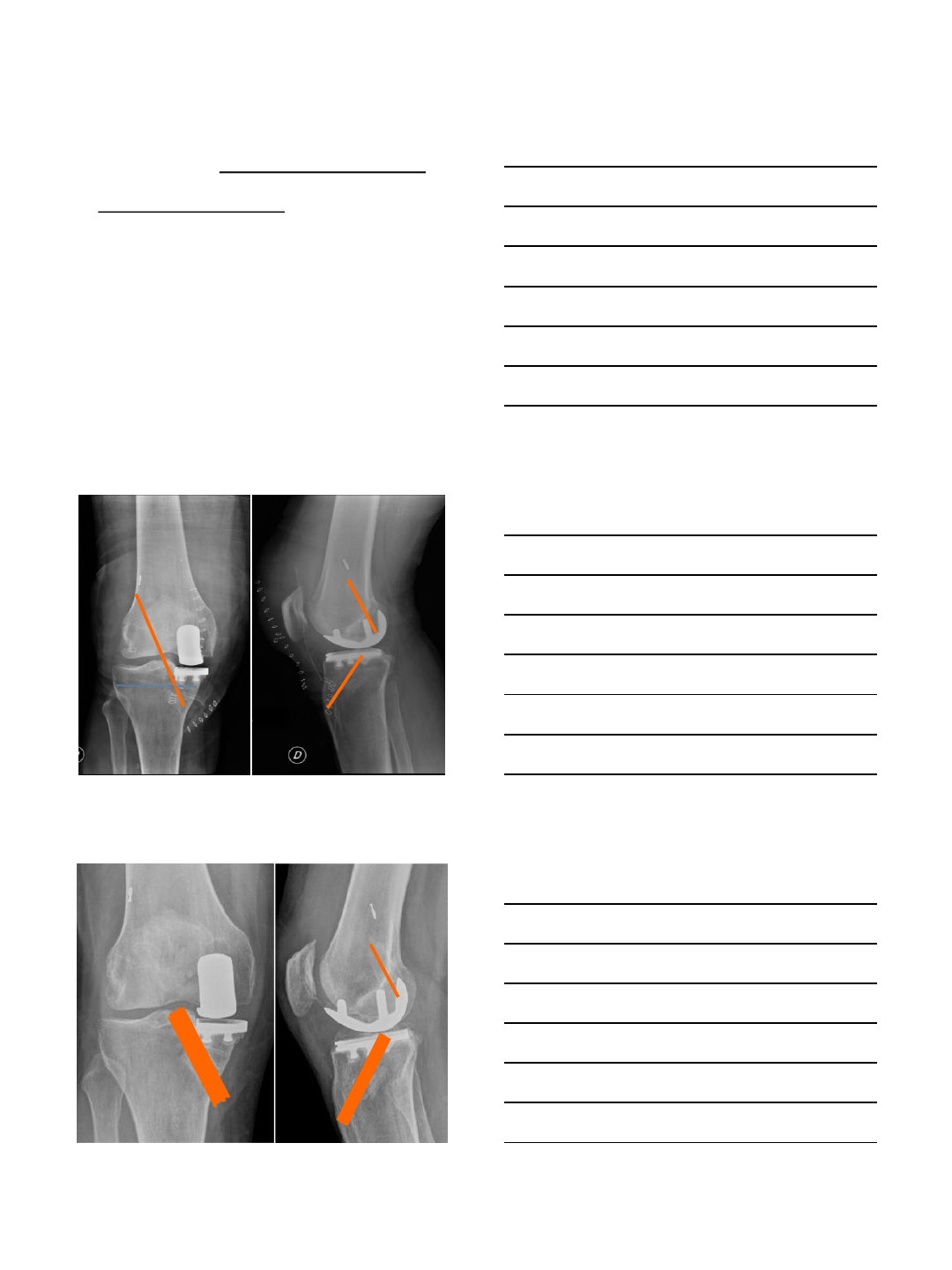
Implant selection
1) Resurfacing
2) Measured resection
Different philosophies
Slightly different indications
Choice is a matter of age
Implant selection
Resurfacing:
-“la uni c’est du resurfaçage” by Philippe Cartier
bone sparing and of respecting the joint
physiology
respect of the so called “Cartier angle”(angle
of tibial varus deviation)
Reaming of the cartilage surface on the
femoral side.
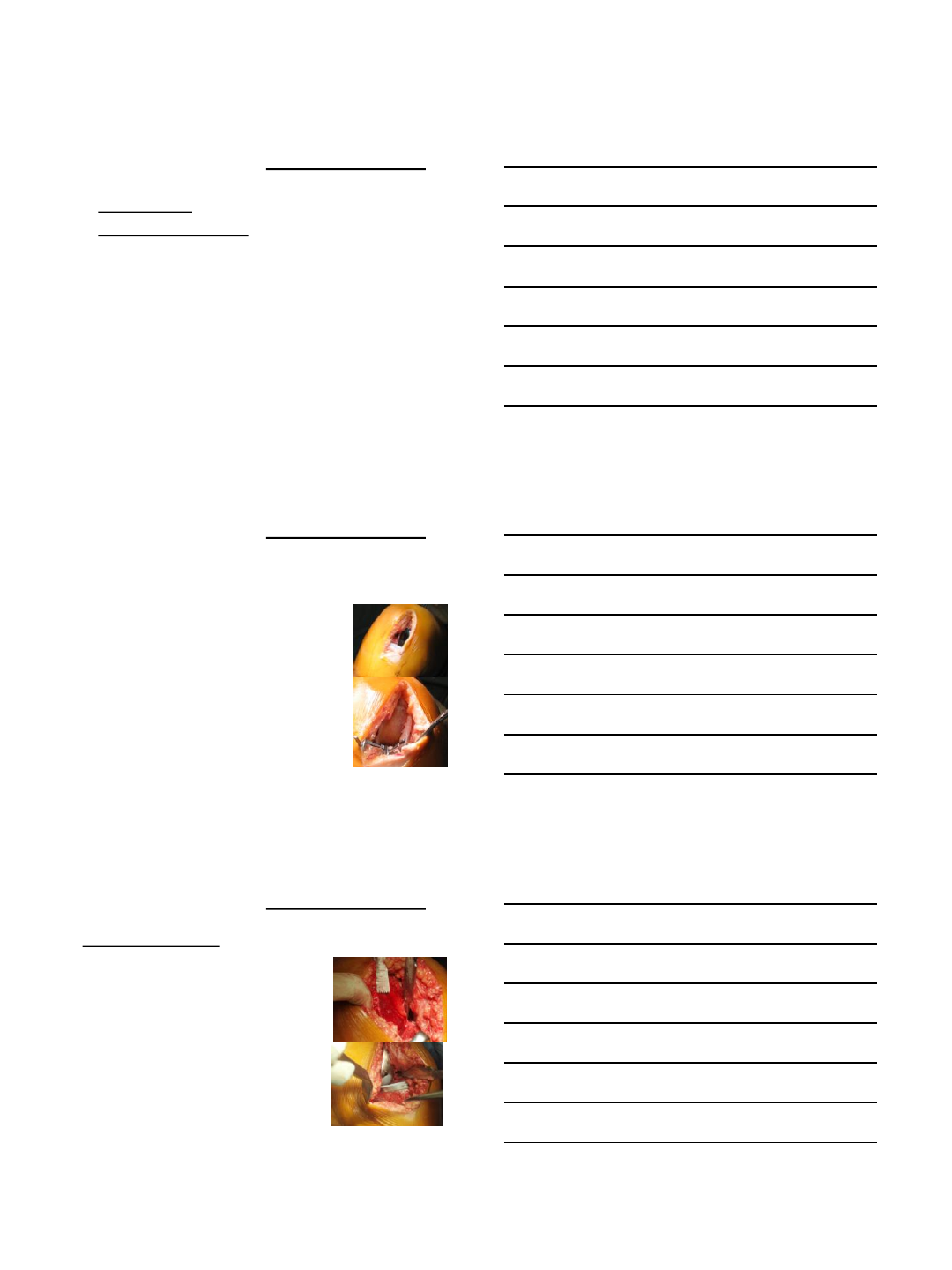
Implant selection
Measured resection:
- Implants and concepts that are
closer to a total knee design and
philosophy
- Tibial cut at 90° and a parallel cut
on the femoral side (based upon
the tibial cut)
6/30/2014
7
Implant selection
Indications
Our experience : resurfacing in case of more
degenerated OA with condylar recession
Less bone to be removed
Easier to avoid overcorrection
Resurfacing
Measured
resection Resurfacing
Measured
resection
Implant selection
Fixed vs mobile
- Good results with both implants
- Different philosophies
- Different techniques
6/30/2014
8
Implant selection
Indications:
•No specific indications according to each specific
design
Our opinion:
•ACL concomitant reconstruction, partially deficient
ACL: fixed bearing
•Lateral OA: fixed bearing
No matter the implant design
•Tibial sagittal plane: slope = native, mostly 3°-5°
•Tibial coronal plane: - 90°
- Pristine varus (Cartier angle)
•Osteophytes removal from tibia and femur: MCL
release
Surgical technique: medial Uni
No matter the implant design
•Femur: central /slightly lateral positioning of
the femoral component on the condyle,
avoiding notching with the tibial spine
•Balancing: slight looseness to avoid lateral
overloading (1-2 mm)
Surgical technique: medial Uni
6/30/2014
9
No matter the implant design
•Femur: no osteophyte removal from femoral
condyle. The osteophytic overgrowth can be
used to support the femoral component
particularly on hypoplastic condyles
•The component must be implanted as lateral
as possible
•Some remaining valgus (no full correction)
Surgical technique: lateral Uni
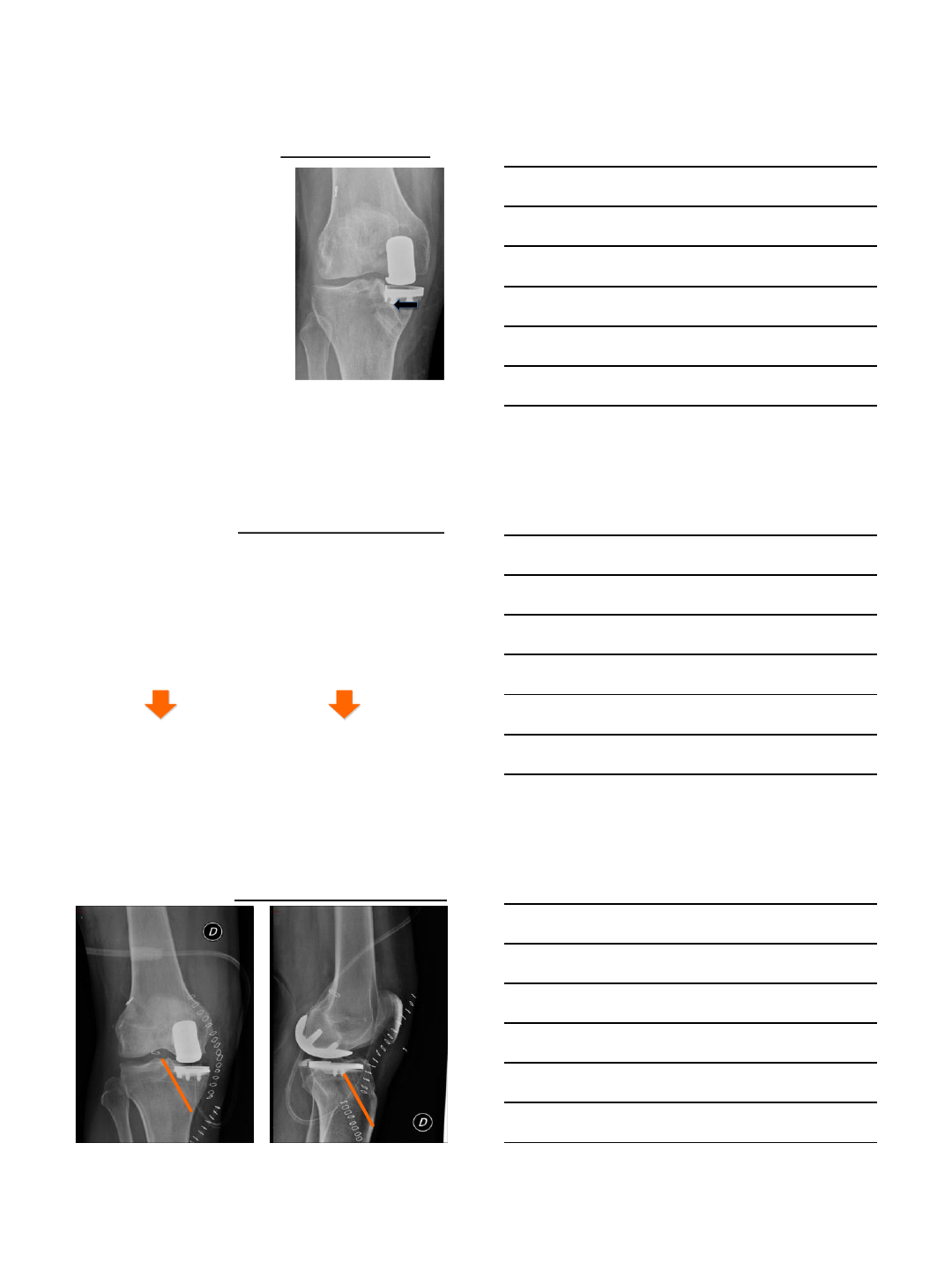
Up-to-date indications
Uni solo: “one finger sign” + slight AKP
with only medial facet involved
Beard et al
The influence of the presence and severity of pre-existing
patellofemoral degenerative changes on the outcome of the
Oxford medial unicompartmental knee replacement
Pre-operative clinical and radiological assessment of the
patellofemoral joint in unicompartmental knee replacement and its
influence on outcome JBJS Br, 2007 .
F. Benazzo, S. M. P. Rossi, L. Piovani, A. Combi, S. Perle
Bi-uni und bi-uni + femoropatellarer Gelenkersatz 2012
Up-to-date indications
6/30/2014
10
Up-to-date indications
Up-to-date indications
Considerations
•Uni insufficient to improve patellar
tracking and provide pain relief if lateral
facet involved
•TKA is an overkilling solution: ACL
sacrificed, lateral compartment sacrificed
Up-to-date indications
6/30/2014
11
Up-to-date indications
Uni and acl: technical issues
•tunnel positioning
•approach
•stability of the implant
6 months
6/30/2014
12
Uni + ACL Trans-tibial approach
Problems:
•Tunnel widening
•Possible secondary impingement
with metal back
•Possible tibial baseplate
subsidence
Up-to-date indications
Our solution: Acl trans-am reconstruction
•Tunnel widening: unavoidable
•Prosthesis site placement: unchangeable
•Transfer tibial tunnel from medial site closer to tt,
producing an anatomic foot print
Move away tunnel
from prosthesis
Reduce likelihood of
impingement between
new-ACL and baseplate
Up-to-date indications
Up-to-date indications
6/30/2014
13
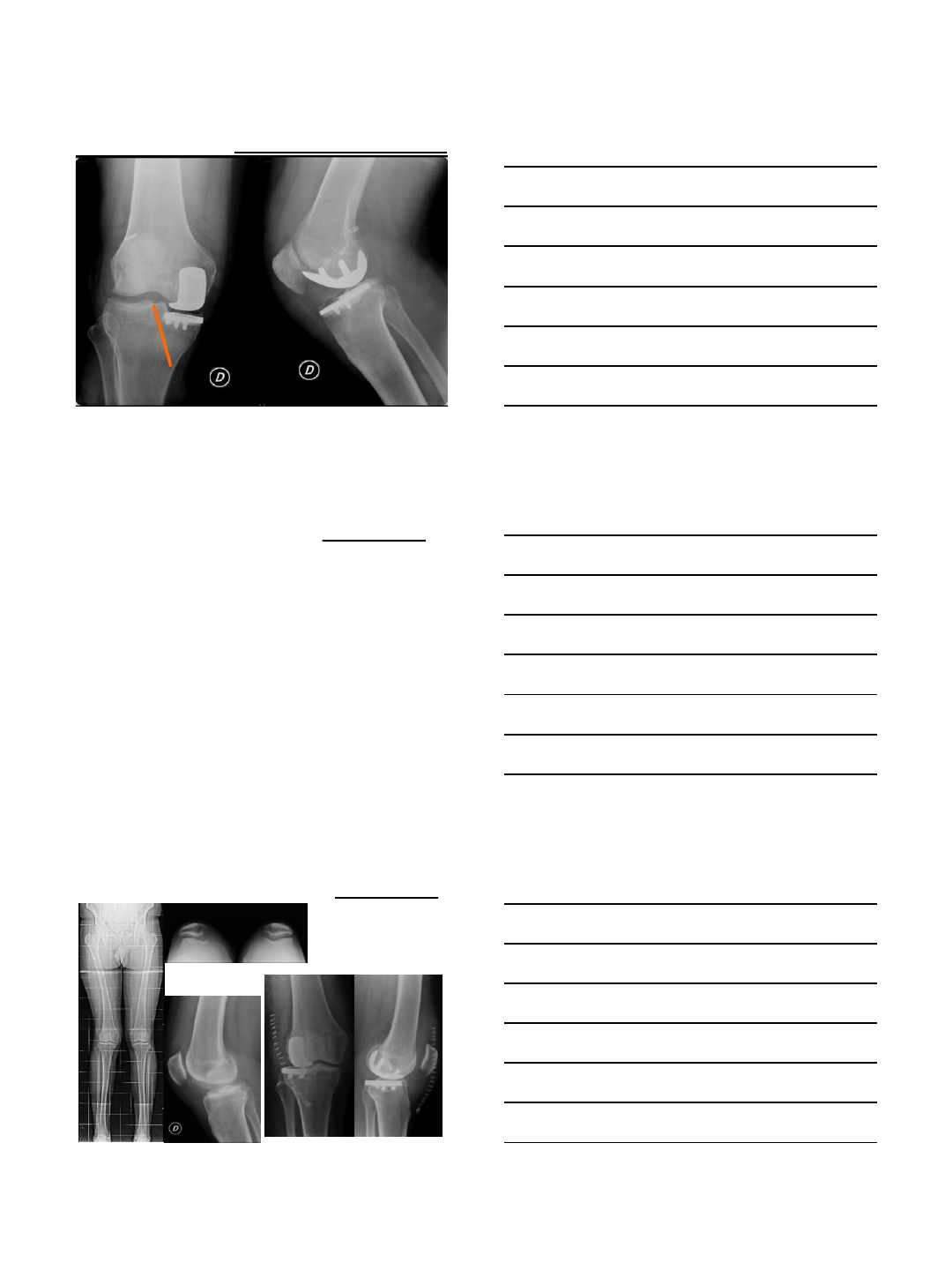
Up-to-date indications
1 year
Lateral UNI
Lateral arthritis: 10% of patients with knee OA
- Valgus knee
- Post-traumatic
- Post-osteotomy
Lateral UNI
6/30/2014
14
Lateral UNI
Follow-up 3
months
Lateral UNI
3.UNI
Lateral UNI
6/30/2014
15
Return to sport
- More patients returned to or increased sports
following UKA (P=.0003), but no sooner than TKA
patients.
- Patient-perceived Oxford and modified Grimby
scores were better and sporting activity was
greater following mini-incision UKA compared to
TKA.
Walton et al
Patient-perceived outcomes and return to sport and work: TKA versus mini-incision
unicompartmental knee arthroplasty.
J Knee Surg. 2006 Apr;19(2):112-6.
Return to sport
- The majority of patients returned to sports and recreational
activity UKA
- However, the numbers of different disciplines patients were
engaged in decreased as well as the extent of activities.
- Activities in which most patients participated were
primarily low- or midimpact.
- Patients scored higher on the SF-36 than age-related
norms, which might be due to the patient-selection process
for unicompartmental knee arthroplasty and geographical
differences.
Naal et al
Return to sports and recreational activity after unicompartmental knee arthroplasty.
AJSM, 2007
Conclusion
•UKA is a valid option to address the
unicompartmental degenerated knee
•Age is not anymore a limitation, assuming that
surgery is correctly performed
•Young patients can benefit from this
procedure, including those who seek for sport
activities

6/30/2014
1
VuMedi Webinar
HTO vs UKR
Mobile UKR
D Murray
Disclosure:
Personal & Institutional support - Biomet
High Activity patients
•Concern
–? Causes UKR wear & failure
•Fixed bearing UKR
–Wear inevitable esp second decade
–Small contact area, high contact stress
–Thin polyethylene
•Normal Knee
–Wear prevented by meniscus
–Reproduce function of meniscus
Minimise wear
•Reproduce meniscus
–Full congruent contact in
all positions
•Only achieved with
–Mobile bearing
–Spherical femur

6/30/2014
2
Oxford knee 1976
Articulation unchanged
•Femur spherical (1mm error)
•Tibia flat
•Mobile Bearing
–Fully congruent - low wear
–Unconstrained - low loosening
20 year wear
in vivo
•RSA (Kendrick et al 2010)
•7 knees, Phase 2
•Wear 0.4mm (max 0.6mm)
•Rate 0.02mm/yr (max 0.03)
•Order of magnitude less than fixed
•Ideal for young active patients
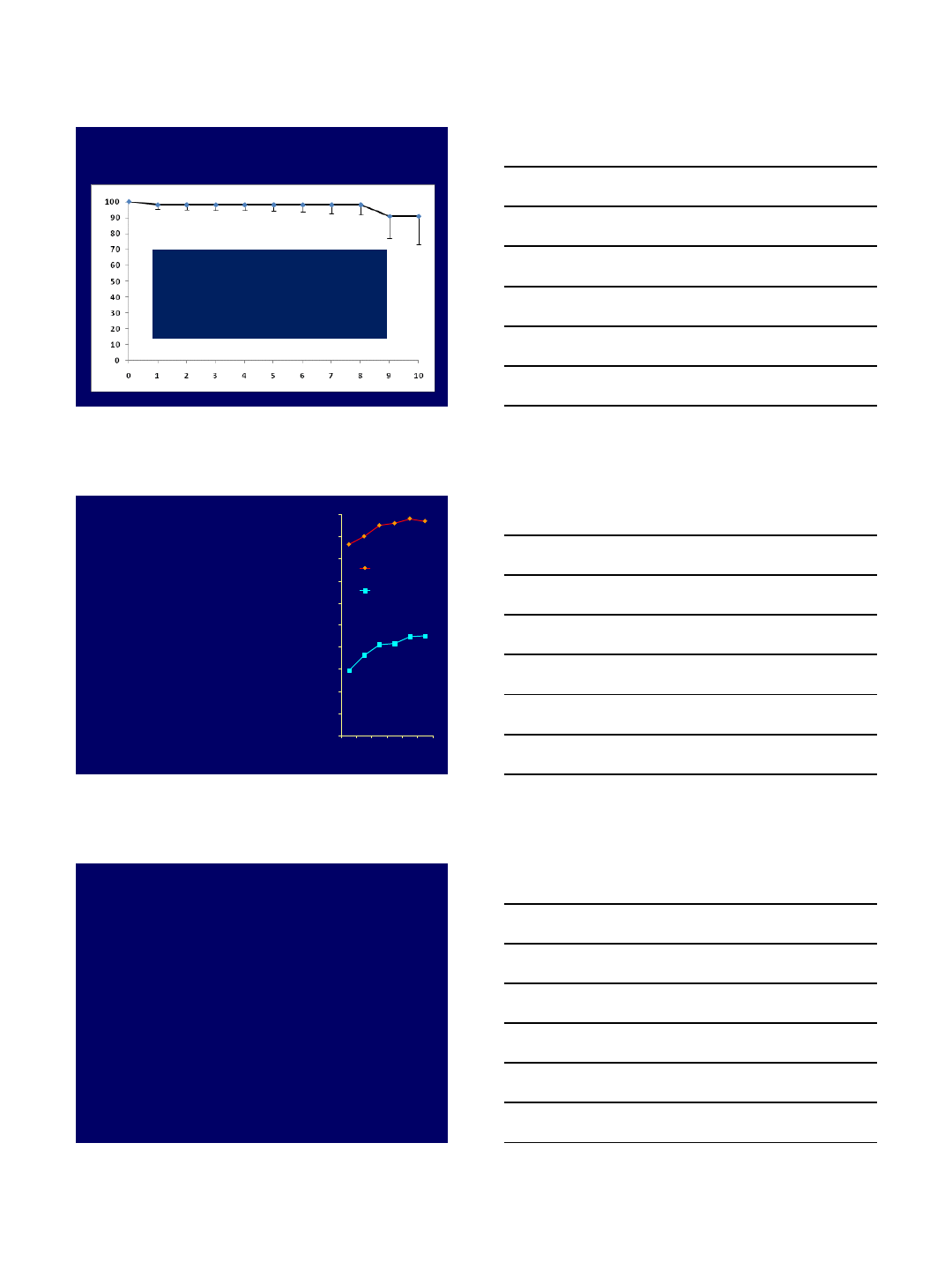
Survival %
Years
Independent Results (Svard 2006)
683 Oxford UKR
20 yr survival 92% CI 15
Better than other UKR
No failures due to wear
OA progression 2% at 20 yrs
6/30/2014
3
Phase 1 study (Svard 2013)
•1983 to 1988 – 25 to 30 years ago
•125 implants (104 patients)
•80% Dead, alive reviewed mean 25yr
•90% Definitive knee replacement with no
revision & Good/Excellent HSS score
•No TKR has better results
Medial OA – optimal treatment
•Young (? <60 25% of cases)
–UKR v Osteotomy
–Debate – no good comparative evidence
•Old (? >60 75% of cases)
–UKR v Osteotomy
–UKR better - no debate
UKR v HTO in elderly
•UKR definite solution
–Rapid recovery, Low morbidity, Good function
–90% patients die with without revision and
with good clinical outcome
•HTO
–Results not so good
–15yr Comparative study (Weale 1994)
–Meta-analysis (Virolainen)
6/30/2014
4
UKR v HTO in young
Controversial issues
•Bone-on-bone or Partial thickness
•Activity level
•Extent of varus deformity
•ACL deficiency
UKR v HTO in young -
Indications
•Bone – on – bone medial OA
–UKR reliably relieve symptoms, good long
term results
–HTO – not so reliable
•Partial thickness cartilage loss
–Diagnose – Xray or arthroscopy
–UKR not reliable – contra-indicated
–? HTO ideal if associated with Varus
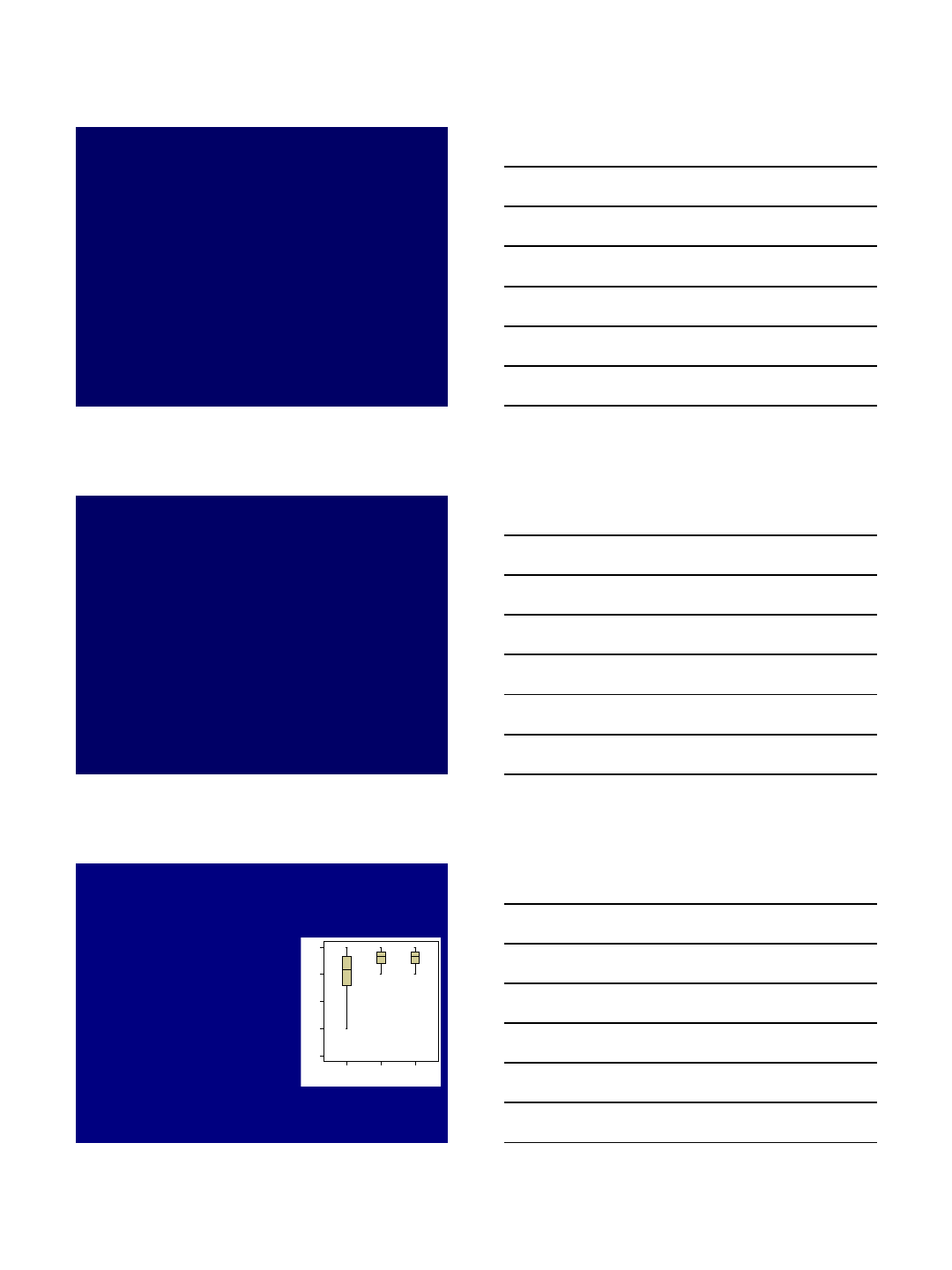
PTCL compared to Bone
Exposed (BE) & Bone loss (BL)
Groups
BLBEPTCL
OKS
48
36
24
12
0
p < 0.001
•PTCL worse score and
greater variability than BE or
BL (OKS 36 v 43)
•PTCL 21% worse or no
substantial improvement
(ΔOKS<6). BE & BL all
substantial improvement
•4 complications (pain
related) all PTCL (14%) Gulati et al (2010)

6/30/2014
5
Partial thickness loss
•UKR
–Not reliable – contraindicated
–Rare to have severe symptoms
•HTO
–PTCL + varus ? Best indication
–PTCL without varus ? Not indicated
Bone-on-bone HTO v UKR
•No RCT in young
•Age matched comparison (mean 55yr)
–Distraction osteoclasis 76, 6yr mean
–Oxford UKR 78, 6yr mean
–OKS (0-48) - HTO 27 UKR 38
–Perhaps not highly active
•HTO 10yr survival 66%
•Other series 60% - 80%
Oxford age < 60yrs
(mean 55, n=52, Price et al ESSKA 2000)
Years post operation
>60
<60
•15yr 92%
•No significant difference (p=0.8)
•Appears to be reliable in young
patients (50s)
6/30/2014
6
<50yr, 7 centre study
107 patients, Mean age 47
3 revisions: 2 for pain, 1 dislocation
7 yr survival = 98% (n=24)
10 yr survival = 91% (n=9)
High level activity
subgroup
•Does it compromise UKR
outcome?
•Analysis of 1000 Oxford UKR
with 5 to 15yr follow-up
•Overall with increased activity
–Increased 12yr survival (p=0.025)
–Increased OKS (p<0.01)
•High activity does not cause failure
•Pandit 2014
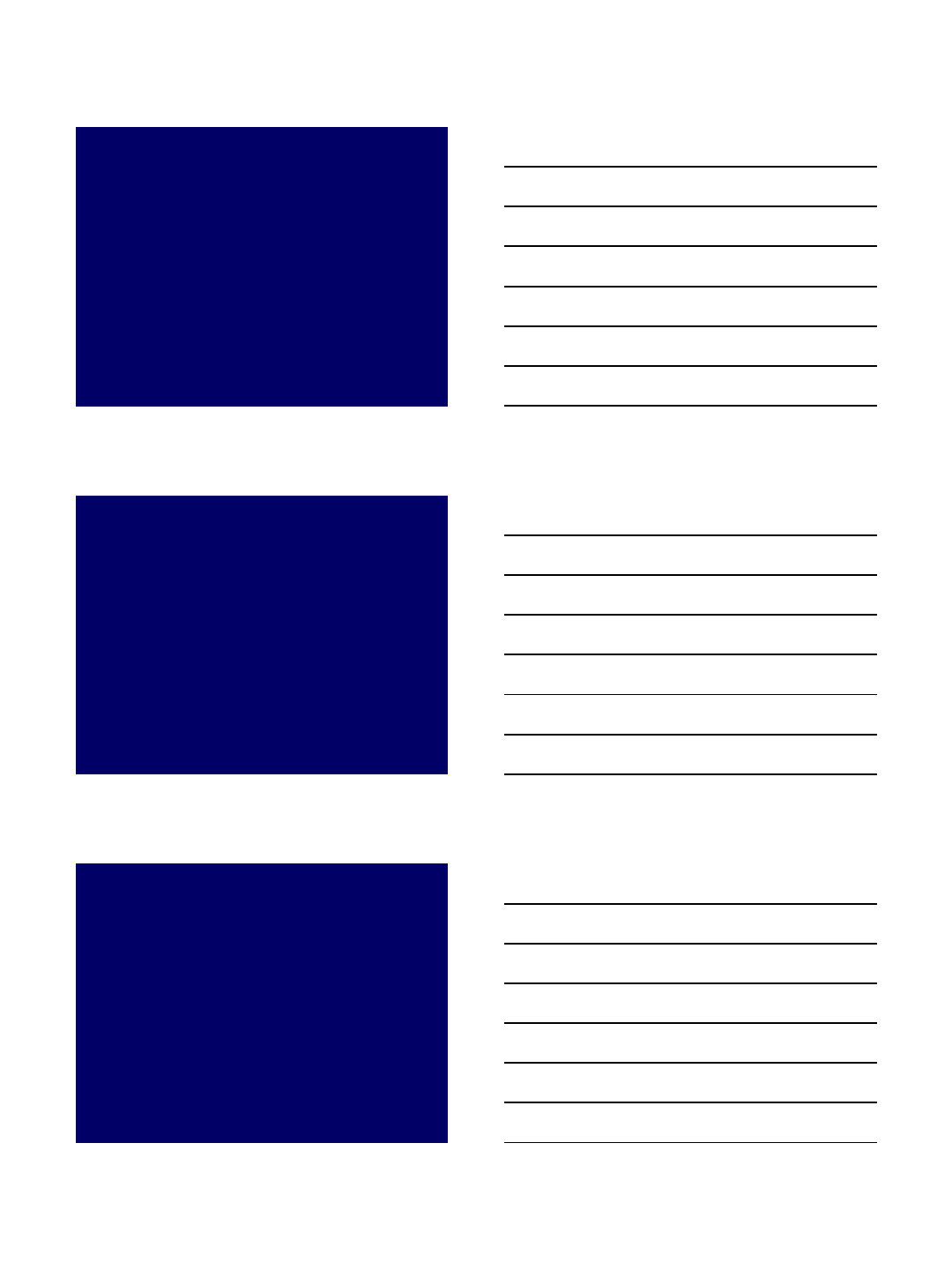
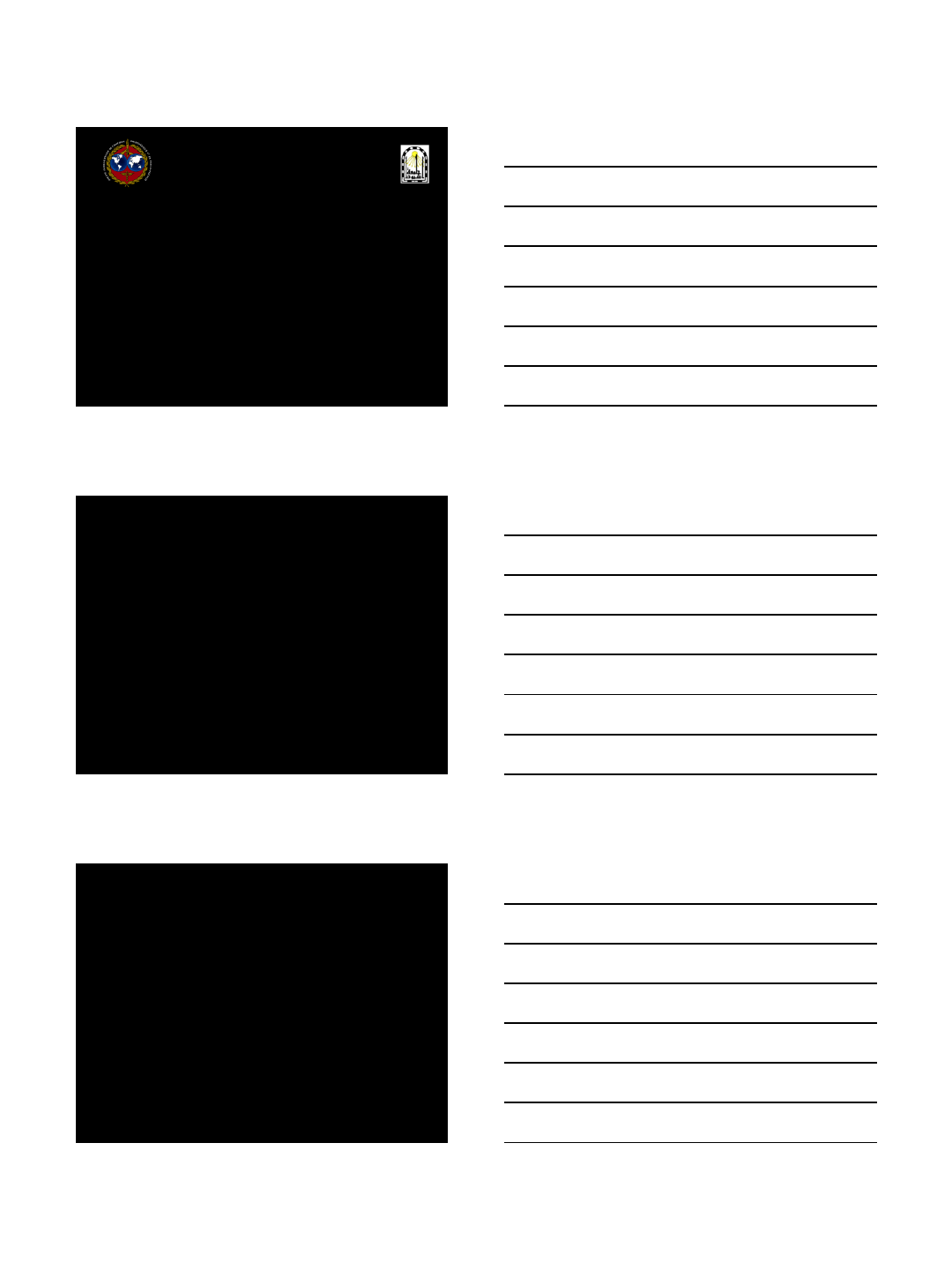
0
10
20
30
40
50
60
70
80
90
100
0-1 2 3 4 5 ≥6
Tegner
12yr survival
OKS
High level activity in UKR
•High activity group patients (Tegner ≥ 5)
–(Tegner 5 = Heavy labour, competitive cycle, jog
uneven ground)
–n=115
–12 year survival 97.3% (95%CI: 92-99).
–OKS 45 (SD 5)
–KSS-O 82 (SD 16) KSS-F 95 (10)
•Activity does not compromise outcome
•Not contraindication, can be recommended
6/30/2014
7
High activity in HTO
•Tegner score ≥ 5
•Bone on bone arthritis
•12 year survival ??? – not nearly 97%
•Mean 6 year clinical follow-up
–OKS ??? – not as good as 45
Activity - summary
•UKR function well so high activity
achieved
•High activity does not cause failure
•Is high activity so reliably achieved after
HTO and if so is long term survival so
good?
Tibia vara & medial OA
•Determine site and severity of deformity
•Intra-articular (usually 5º to 10º)
–Corrected by operation
•Extra-articular (usually 0º to 10º)
–Tibia vara
–Not corrected by operation,
•Alignment restored to pre-disease state
•? Does tibia vara compromise outcome?
6/30/2014
8
Tibia Vara & Oxford UKR
•Incidence of tibia vara
–5º tibia vara 20%
–10º tibia vara 5%
•Tibia vara
–Does not cause long term failure
–Does not compromise function
•Tibia vara not contra-indication
ACLD & medial OA
•Primary ACLD with
secondary medial OA
•Postero-medial tibial defect
•Combined UKR & ACLR if
–Young and active
–Bone on bone
–Normal MCL & lateral side
(stress Xray)
Technique
•Depends on presenting
symptoms
•Pain
–Simultaneous procedure
–Open, BTB
•Instability
–ACL first
–Arthroscopic, Hamstring
–UKR if symptoms persist
6/30/2014
9
Results
(Weston-Simons 2013)
•52 cases
•Mean age 51yr (36-57)
•Mean follow up 5yr (1 – 10)
•10yr survival 91%
–2 failures – infected, lat OA
•Mean OKS 41
•98% pleased
•Kinematically normal
Other factors to consider
•Predictability – UKR better
•Speed of recovery - UKR better
•Cosmesis - UKR better
•Ease of revision
–UKR usually simple (fracture & infection)
–HTO variable (? Opening wedge easier)
Summary
•Medial OA, bone-on-bone, intact ACL
–UKR better (function, survival, etc)
•Partial thickness loss
–UKR contraindicated
–? HTO if associated varus
•Very young (<40), Very high activity
(contact sport), ACLD deficient
–Still debatable (we do UKR)
6/30/2014
1
The Role of Osteotomy
around the knee
Hannover – München - Innsbruck – Bozen
Ph. Lobenhoffer
AO Trauma Europe
Disclosures:
I have no financial relationship to techniques or products mentioned
in this presentation
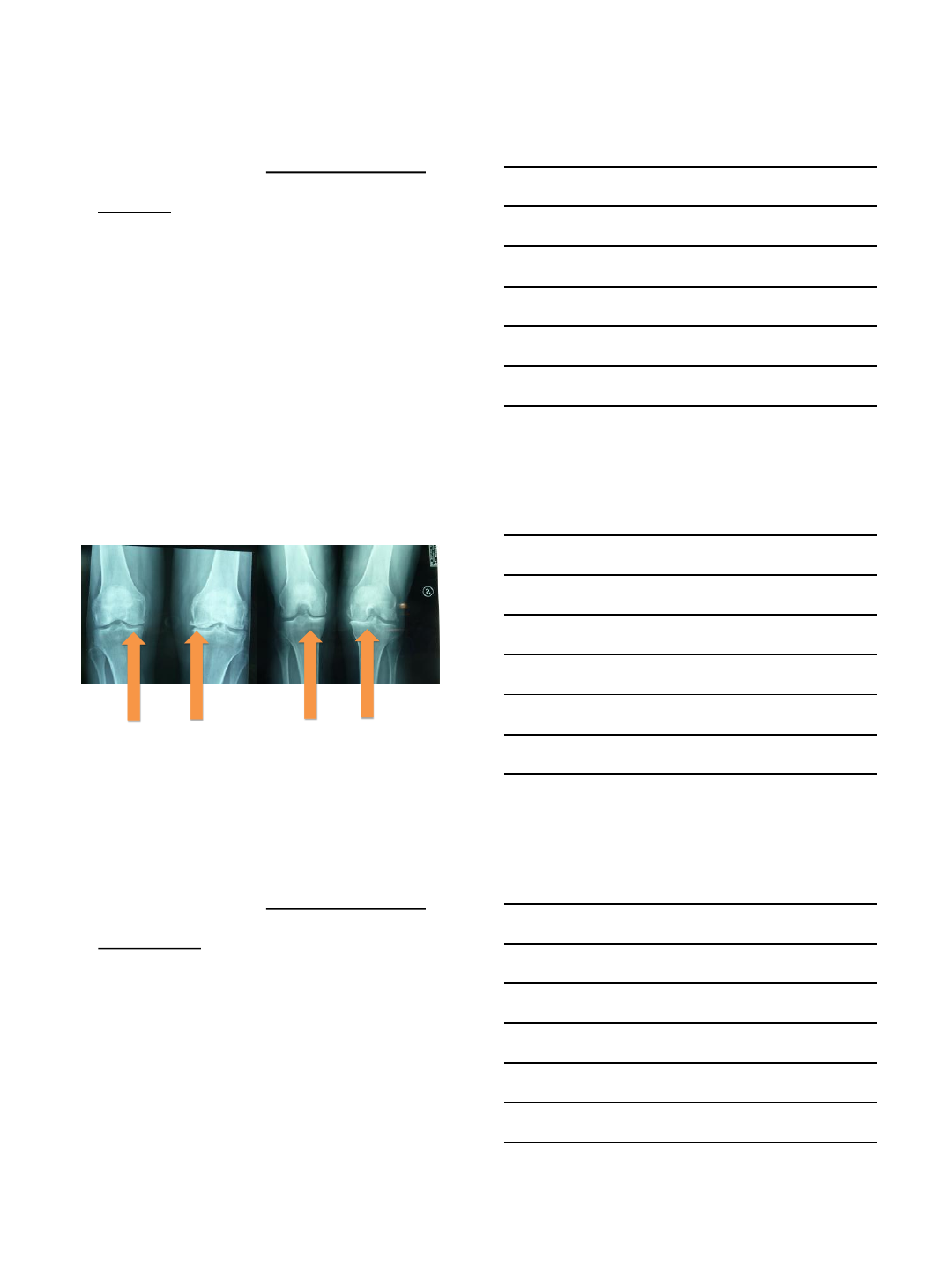
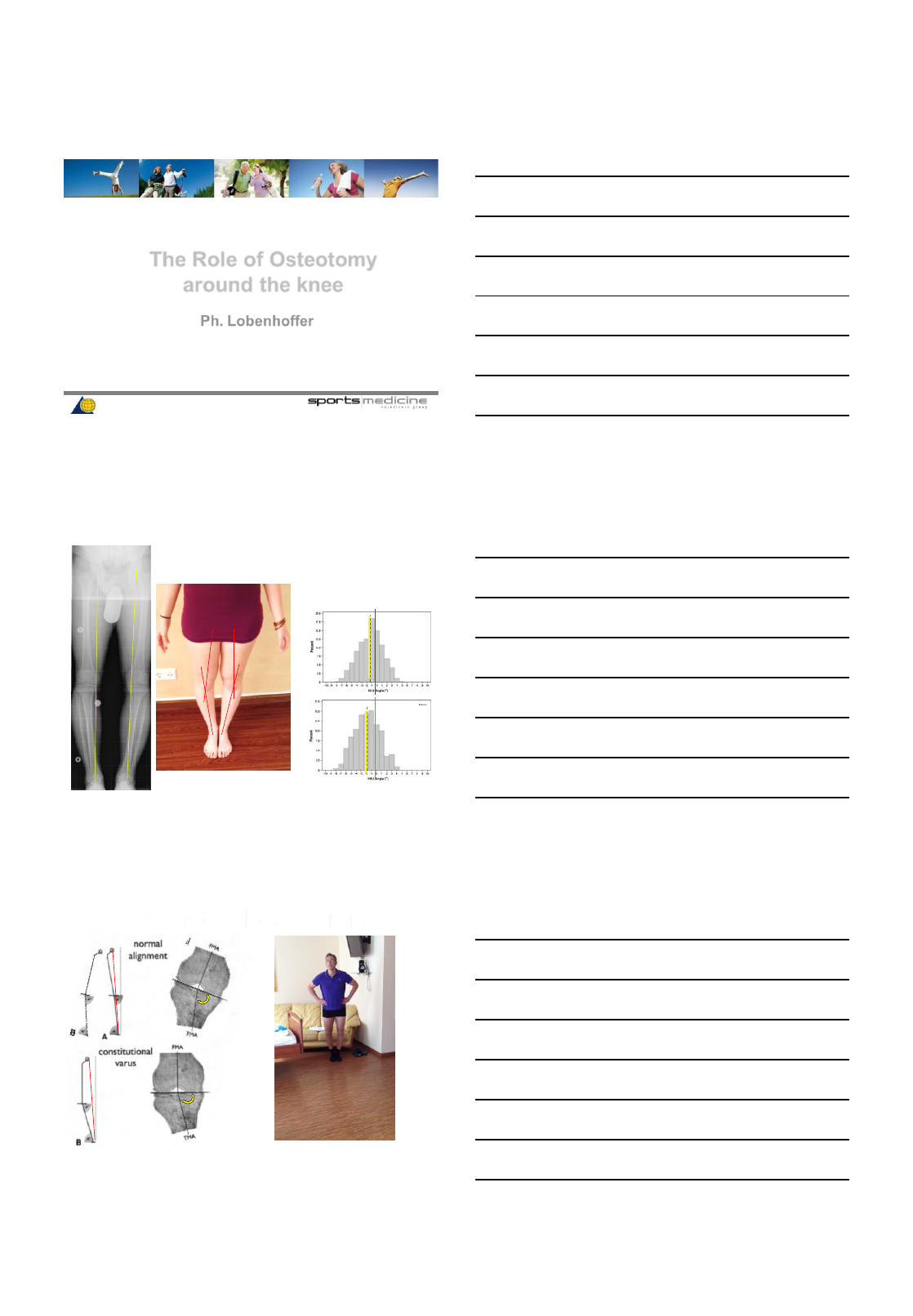
Frontal plane alignment Constitutional Varus
deformity:
•32% males
•17% females
Bellemans CORR 2012
HKA
0°
ALL
MALE
HKA: mechanical axis femur / tibia
Constitutional Varus
J. Victor CORR 2013
knee outwards
foot inwards
WBL shifts medial
6/30/2014
2
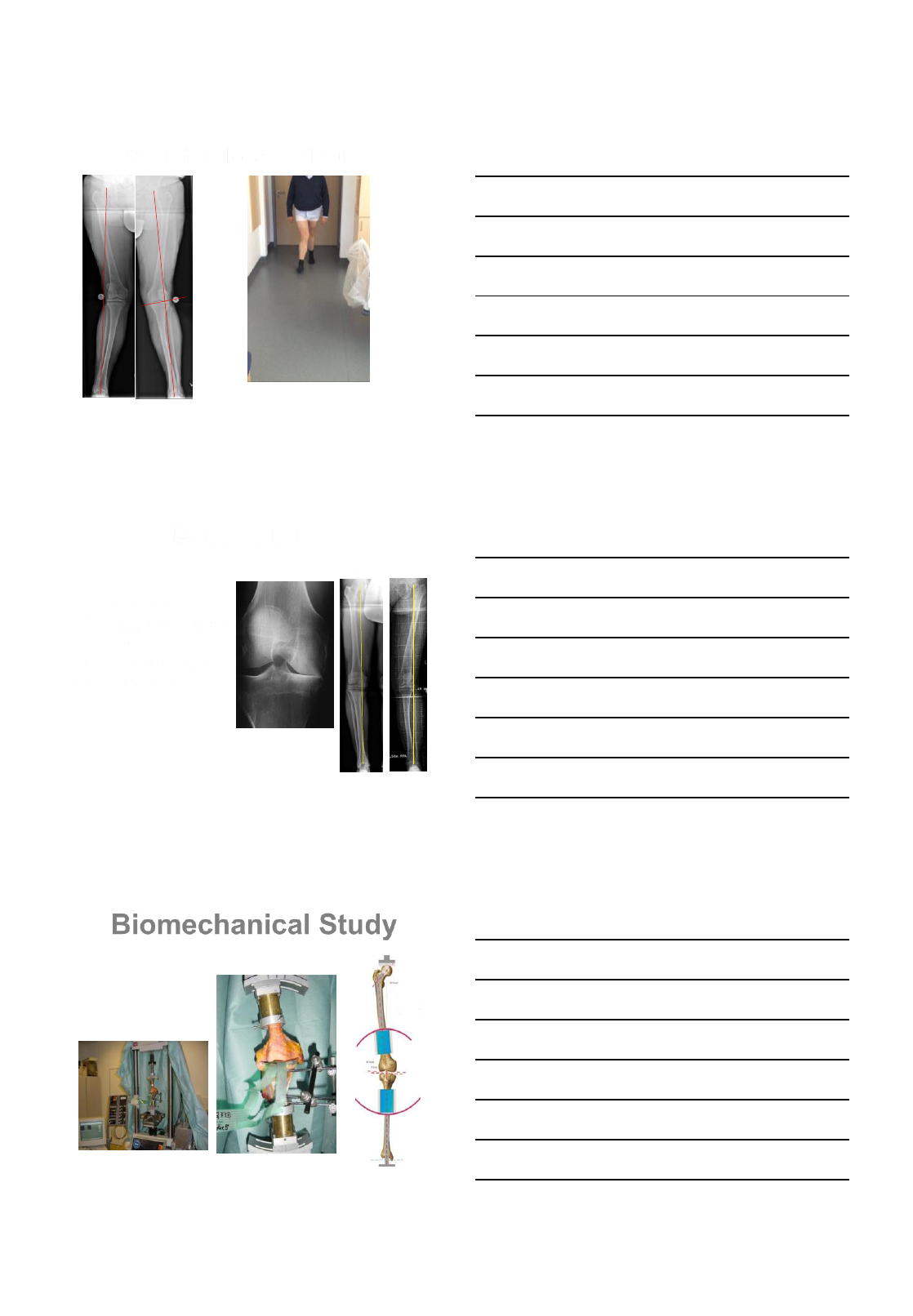
Constitutional Valgus
Knee inwards
foot outwards
WBL shifts lateral
Epidemiology
Osteoarthritis is a disease of mechanics
D.T. Felson JAMA 2013
4 degrees of deformity: 3 x risk for OA
Progression 10 to 20 x faster with deformity
Felson 2013, Brouwer 2007, Sharma 2001, 2009, 2010, 2012, Cerejo 2002 Framingham, MOST, other studies
A frontal plane
deformity more than
3° leads to
osteoarthritis and
should be corrected
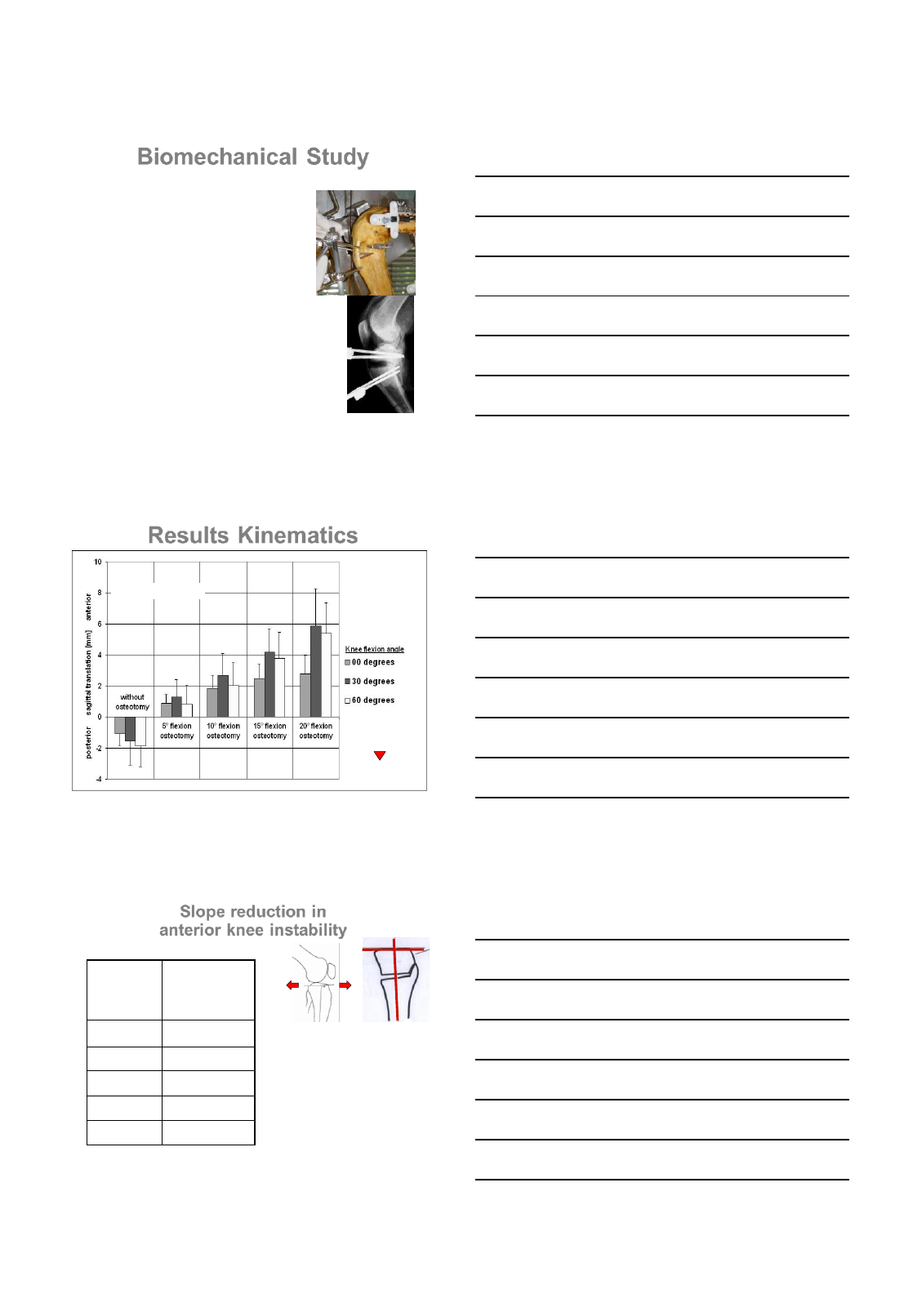
Biomechanical Study
6 human knees
Axial load in mechanical
testing system (mts) in
extension
Bi-cardanic fixation
Ligaments and menisci
intact
Agneskirchner, Hurschler*, Lobenhoffer , Arthroscopy 23, 2007
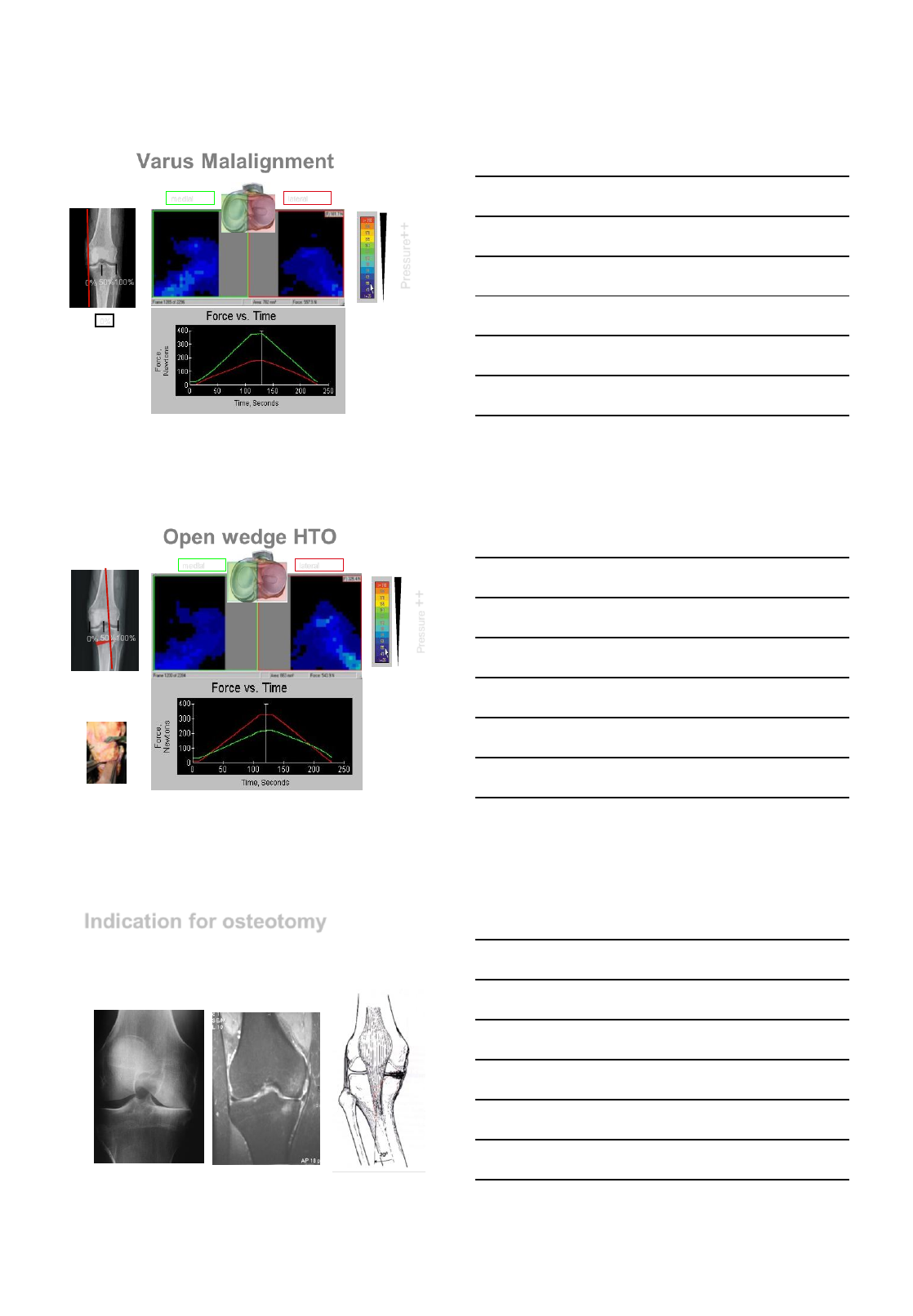
6/30/2014
3
Varus Malalignment
0% 50%
100%
0%
medial lateral
Pressure++
Agneskirchner,
Hurschler, Lobenhoffer
Arthroscopy 23, 2007
Open wedge HTO
0% 50%
100%
WBL to 62%
HTO 9mm,
MCL 100% released
medial lateral
Pressure ++
Agneskirchner,
Hurschler, Lobenhoffer
Arthroscopy 23, 2007
Indication for osteotomy
•Congenital deformity
•Posttraumatic deformity
•Unilateral Osteoarthritis
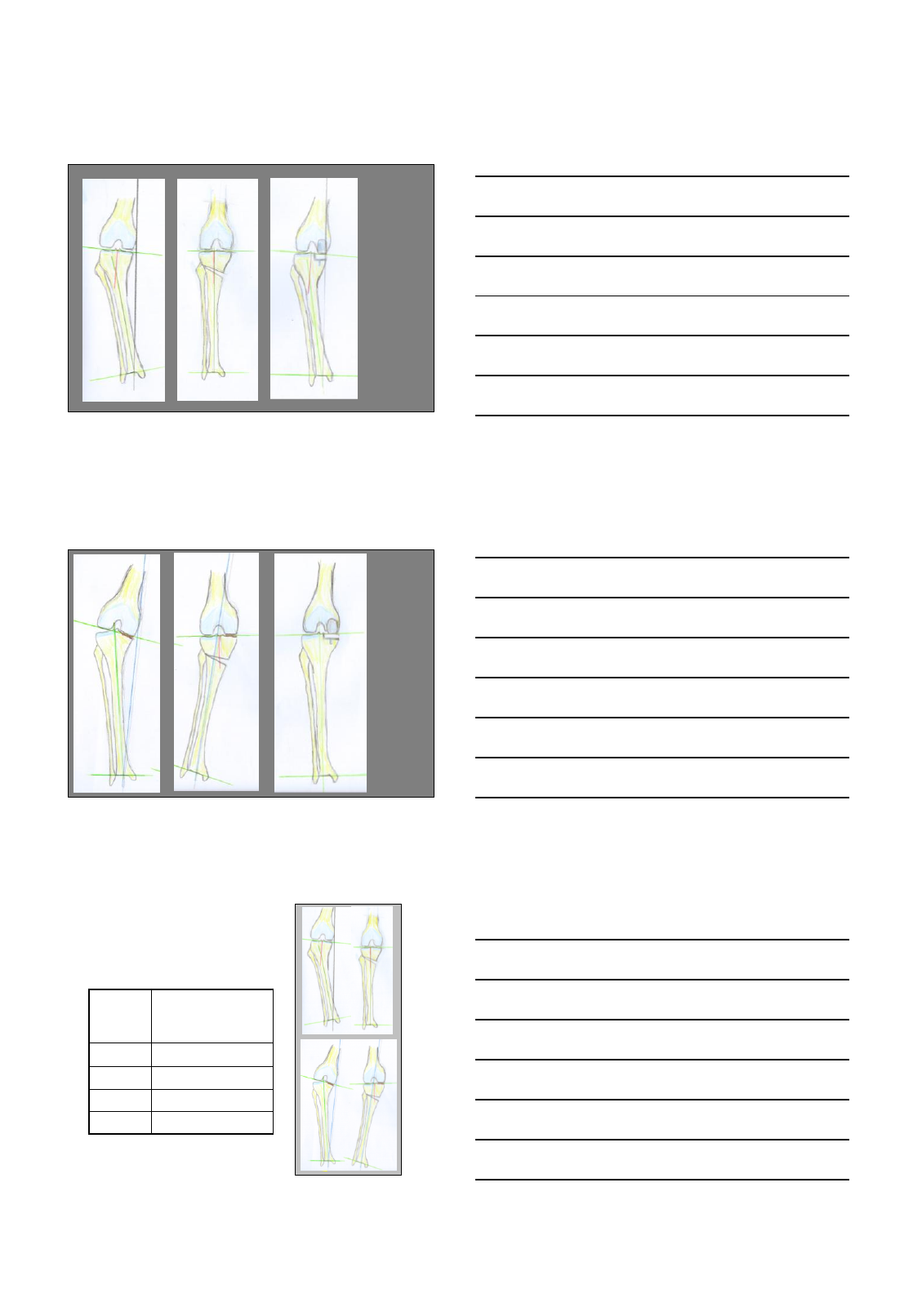
6/30/2014
4
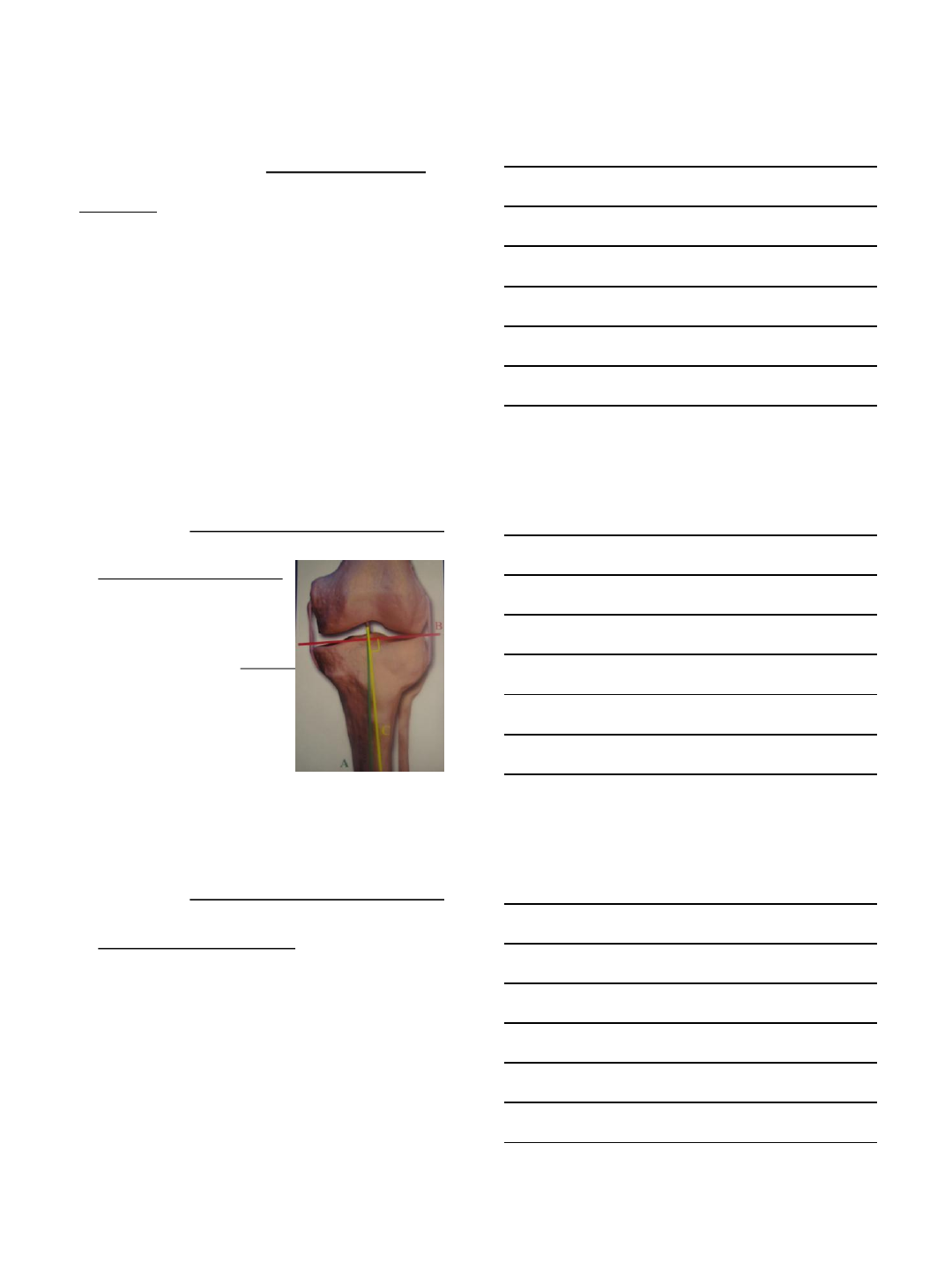
Frontal plane alignment and correction
Constitutional
deformity
Frontal plane alignment and correction
Intraarticular
defect
Patient criteria
Metaphyseal deformity (TBVA)
Tibial Bone Varus Angle
Bonnin,Orthopäde 2004
Niemeyer Arthroscopy 2009
Tibial
Bone
Varus
Angle
Good / excell.
10-y. results
>5° 83%
2-5° 71%
0-2° 56%
<0° 36%
TBVA
> 5°
TBVA
= 0°
6/30/2014
5
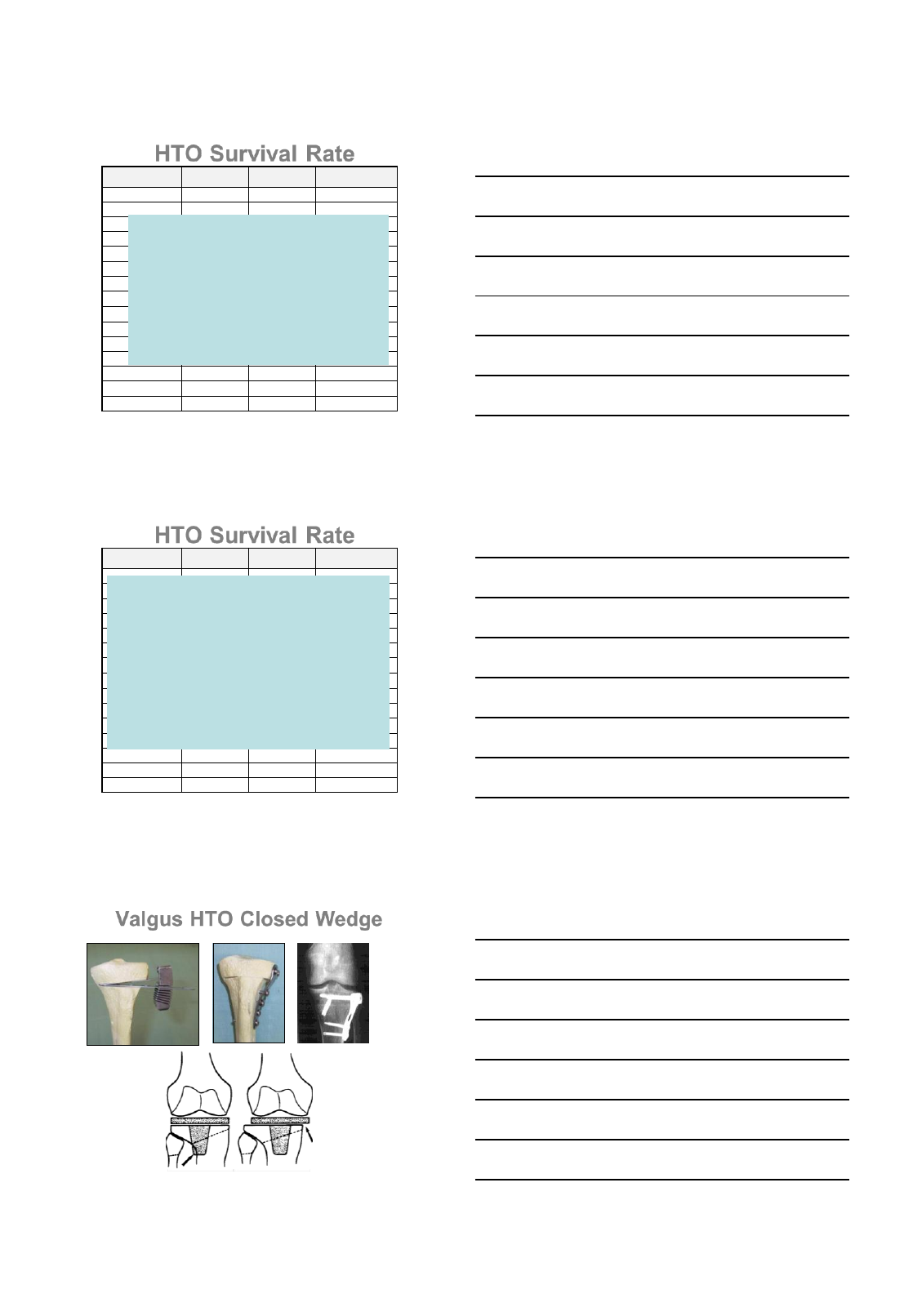
HTO Survival Rate
5 Jahre 10 Jahre > 10 Jahre
Insall 85% 66%
Yashuda 63% 18%
Berman 77% 62% 59%
Rudan 78% 70%
Matthews 50% 28%
Rininapoli 73% 46%
Ivarsson 57% 43%
Hernigou 90% 45%
Aglietti 96% 78% 57%
Levigne 69% 54%
Gstöttner 94% 80% 54%
Van Raaij 75%
Akizuki 98% 90%
Flecher 85%
Billings 85% 53%
Cochrane Database :
Brouwer et al 2007
Silver Evidence:
70% of patients benefit
from an osteotomy for 10
years
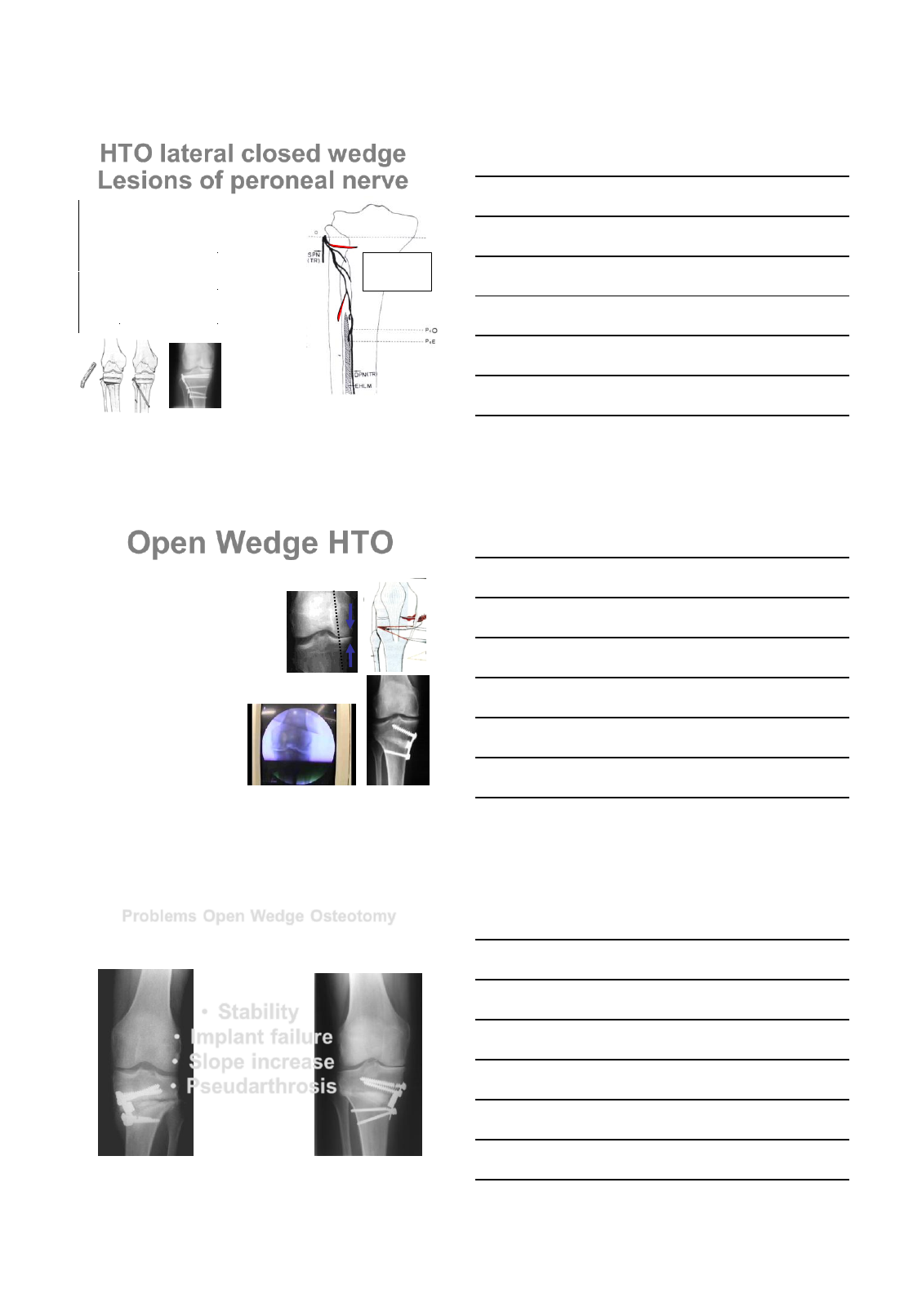
HTO Survival Rate
5 Jahre 10 Jahre > 10 Jahre
Insall 85% 66%
Yashuda 63% 18%
Berman 77% 62% 59%
Rudan 78% 70%
Matthews 50% 28%
Rininapoli 73% 46%
Ivarsson 57% 43%
Hernigou 90% 45%
Aglietti 96% 78% 57%
Levigne 69% 54%
Gstöttner 94% 80% 54%
Van Raaij 75%
Akizuki 98% 90%
Flecher 85%
Billings 85% 53%
Spahn G, KSSTA 2013
46 studies HTO
5-8 years after HTO:
91% no further surgery
9 – 12 years after HTO:
84% no further surgery
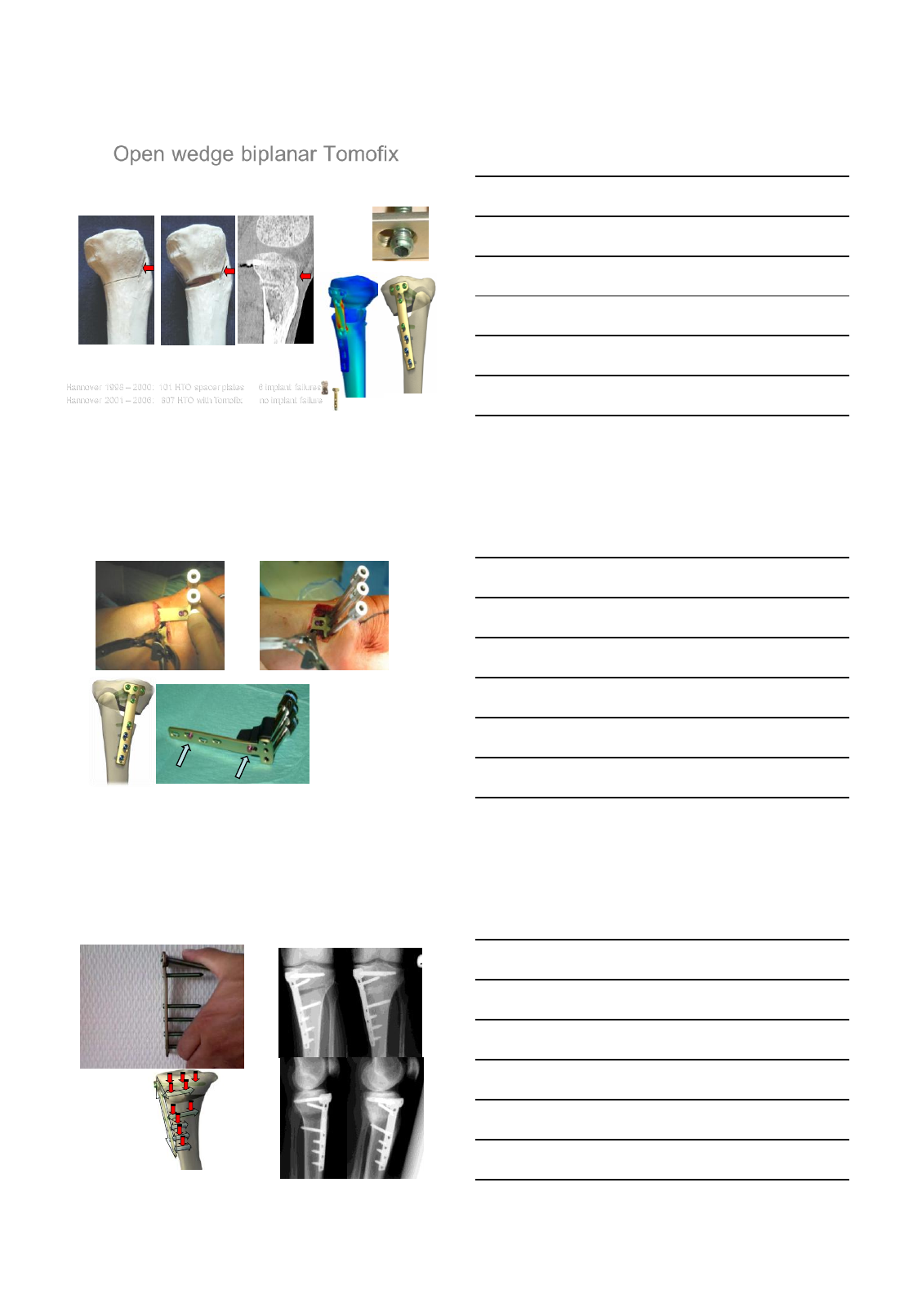
Valgus HTO Closed Wedge
Lateral translation of
shaft
Impaction medial
hinge
Loss of correction
Pape et al. Orthopäde 2/2004
42 Pat RSA-Analysis HTO
Convent. implant > 8° correction
week 0 – 3:
3 mm. fragment
movement
6/30/2014
6
HTO lateral closed wedge
Lesions of peroneal nerve
Coventry 1988 3.3%
30 Osteotomies
Jackson 1974 11,9 %
229 Osteotomies
Vainionpää 1981 2%
103 Osteotomies
Aydogdu 2000 27% (EMG)
11 Osteotomies
Kirgis, A., JBJS 1992
Motor branches of
peroneal nerve
endangered by
fibula osteotomy
No fibula osteotomy
No risk for peroneal nerve
No muscle detachment
Only 1 osteotomy cut
Intraoperative fine-tuning
No leg shortening
W. Blauth 1986
P.Hernigou 1987
GC Puddu 1999
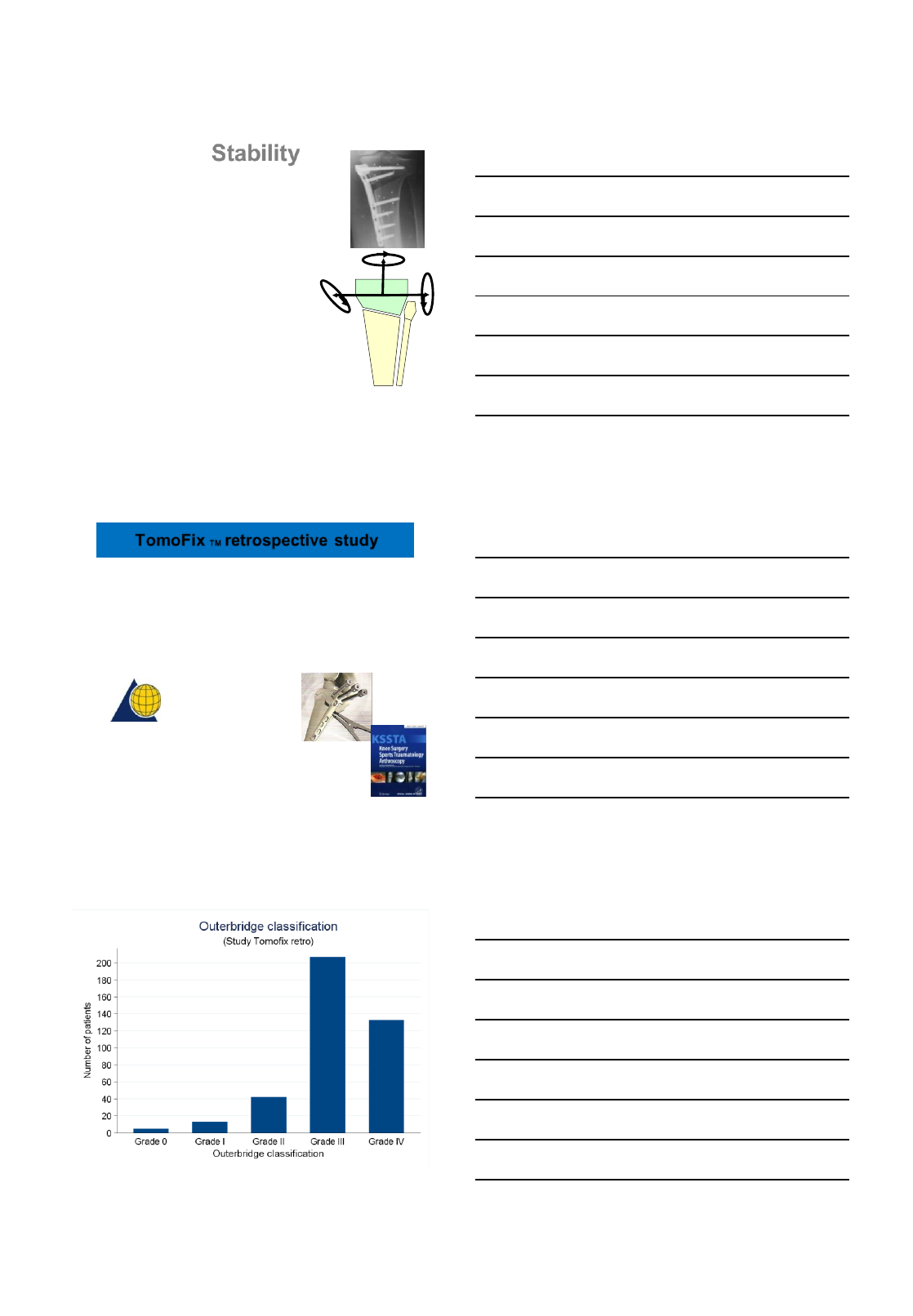
Open Wedge HTO
•Stability
•Implant failure
•Slope increase
•Pseudarthrosis
Lobenhoffer KSSTA 2003, Paccola KSSTA 2004, Jakob A´scopy 2004
Problems Open Wedge Osteotomy
6/30/2014
7
Increased stability
Rapid healing full weight-bearing
Open wedge biplanar Tomofix
3 weeks postop
Locking
screws
Hannover 1998 – 2000: 101 HTO spacer plates 6 implant failures
Hannover 2001 – 2006: 807 HTO with Tomofix no implant failure Lobenhoffer KSSTA 2003
Percutaneous Plate fixator Tomofix
Distance holders
•Subcutaneous
placement
•No compression of
MCL, Pes anserinus
Spontaneous bone healing
No substitute or graft necessary
2 Y. postop
Elastic
motion
induces
callus
formation
6/30/2014
8
Stability
RSA studies
Heerwaarden 2006:
42 cases open wedge Tomofix
no relevant migration,
no difference to closed wedge Tomofix
Heerwaarden Acta Orthop Scan2010:
14 vs 23 patients
full weight-bearing /partial weight bearing
no differences after one year
Immediate full weight bearing allowed
Brinkman, Lobenhoffer, Agneskirchner, Staubli, Wymenga, Heerwaarden JBJS (Br) 12, 2008
Functional outcome assessment in patients treated with open wedge
high tibial osteotomy (HTO) for knee osteoarthritis using TomofixTM.
533 patients, 3 centers, op. 4/2004 to 4/2006
75% follow-up rate, BMI 27, 9,8 mm opening
•D. Freiling
•S. Meyer
•S. Friedmann
•P. Lobenhoffer
•A.Staubli
•S. Schröter
•D. Hoentzsch
TomoFix TM retrospective study
AO Foundation
Clinical Investigation
Flörkemeier et al, KSSTA 1/2013
6/30/2014
9
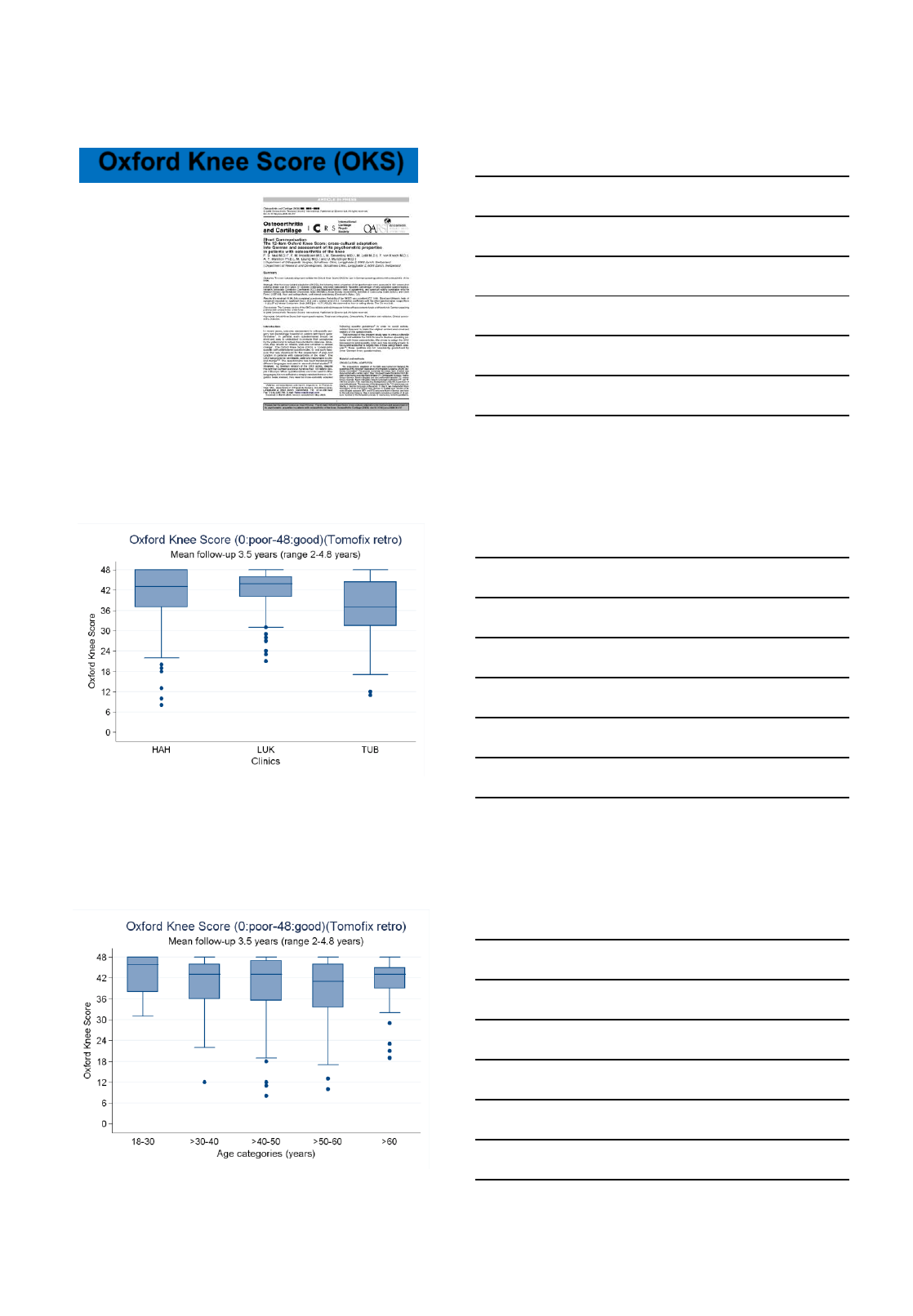
Oxford Knee Score (OKS)
Subjective score
Internationally accepted
Available in Englisch
Translated/Validated by AOCID
12 questions, 5 answers
(excellent 4 P., bad 0 P.)
48 points: excellent result
0 points: bad result
Comparison with Unicondylar
and Total Knee
Present version of OKS:
48 points best result
0 points worst results
Ø 43 (0-48)
Results better than UKA, TKA
Ø 51,6 (20-60)
No correlation to age
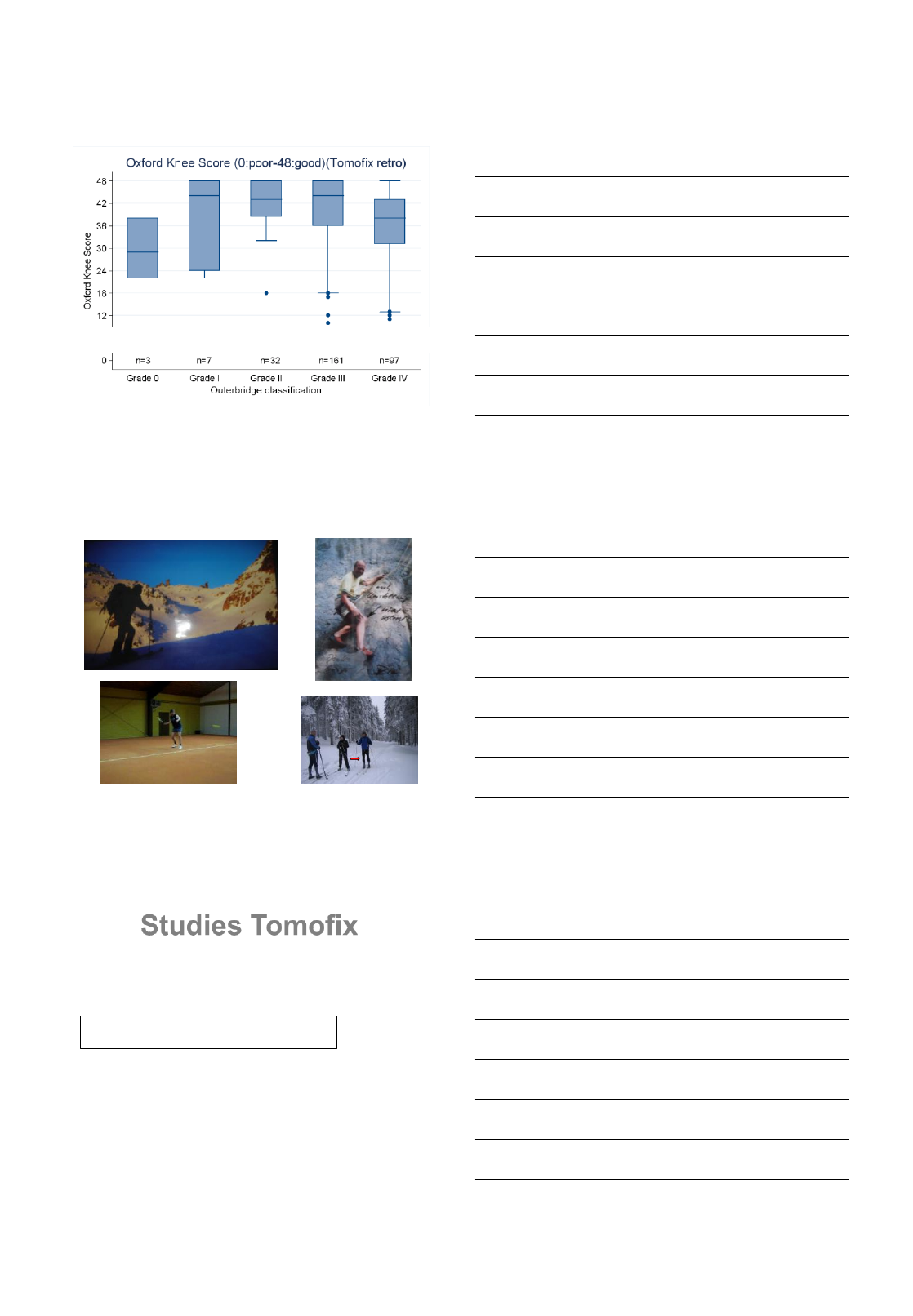
6/30/2014
10
Ø 51,6 (20-60)
No correlation to stage of osteoarthritis
Activity
3 Mo.after Tomofix right side
6 Mo. after Tomofix both sides
3 Mo. after Tomofix right side
.
6 Mo. after Tomofix right side
Salzmann GM, Imhoff, AB et al AJSM 2009
65 patients Tomofix 36 months postop
91% engaged in sports activity
2 sessions /4 hours per week
Lysholm 70, Tegner 4,3
Downhill skiing, mountain biking
Studies Tomofix
6/30/2014
11
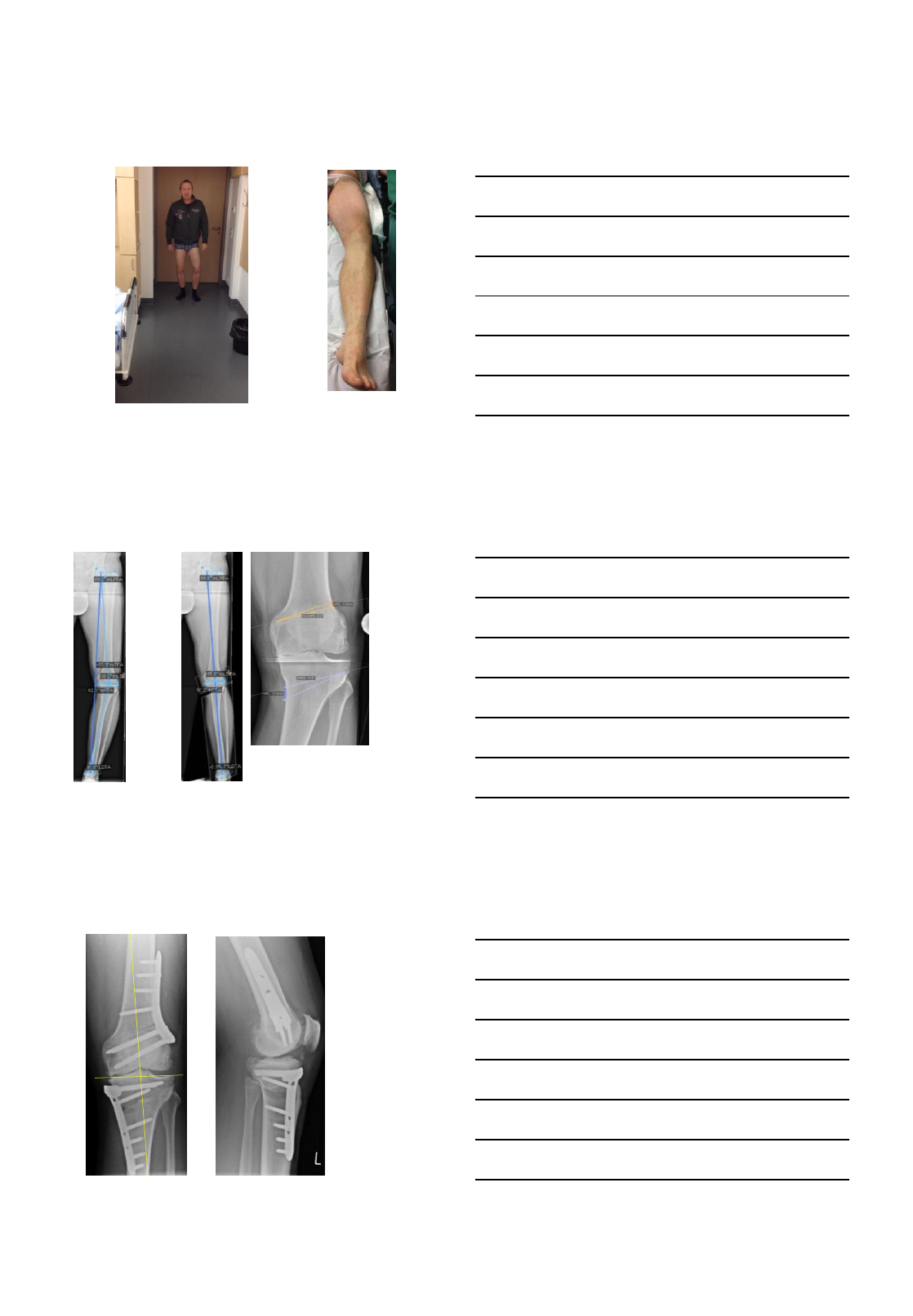
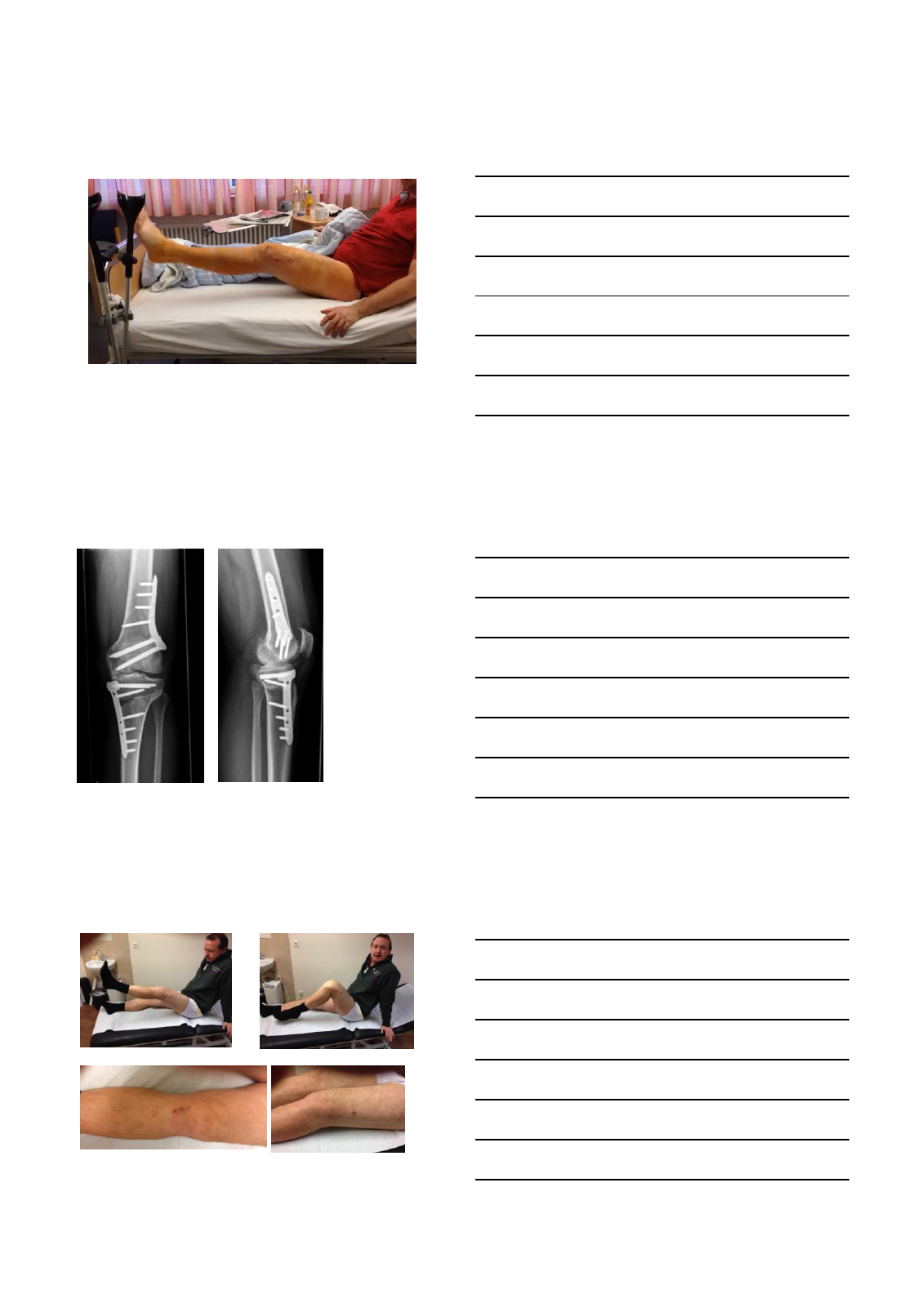
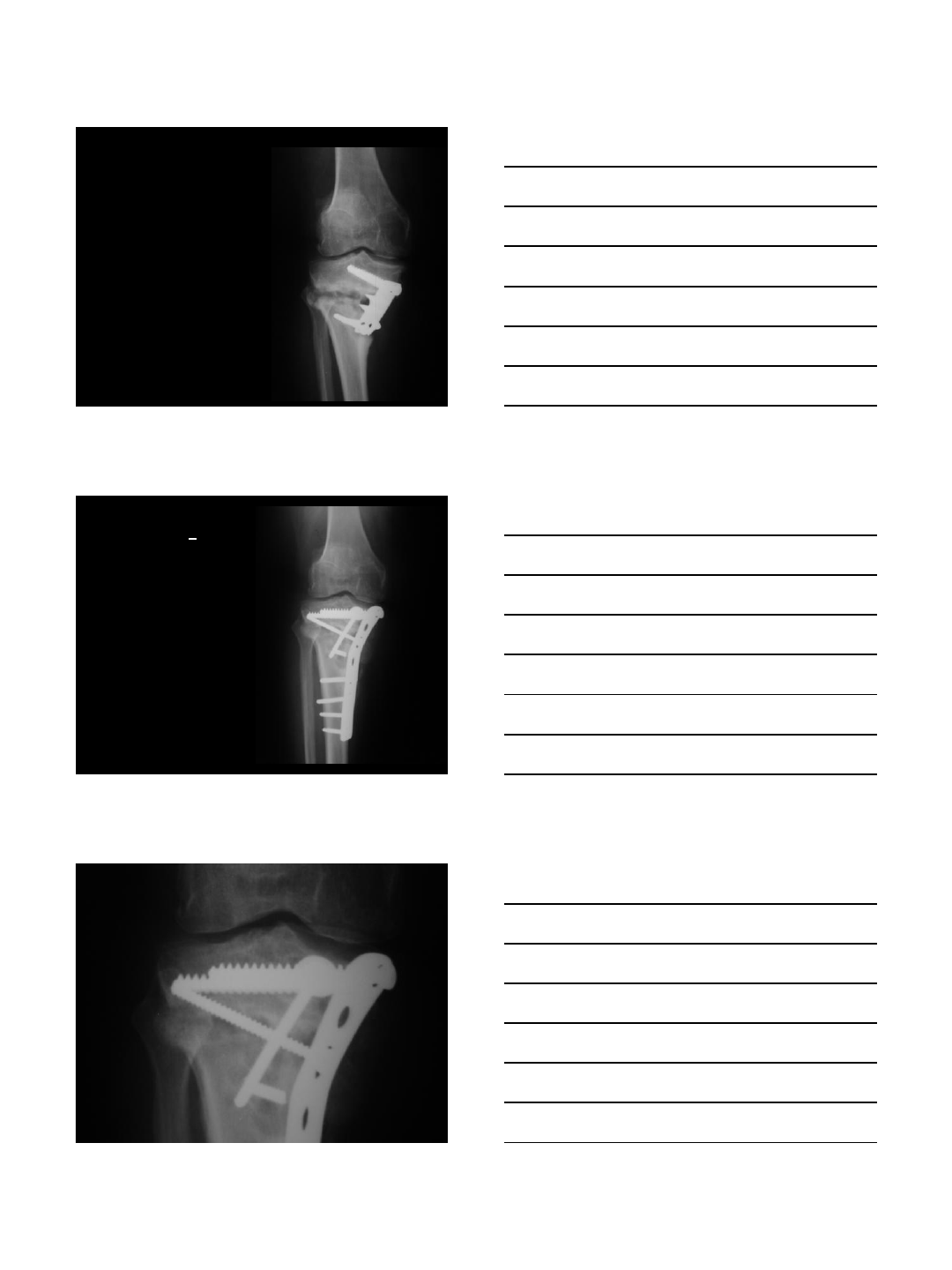
W., U., 51 y., male
former German champion 400 m running
orthopaedic surgeon
2 x arthroscopic debridement, medial
meniscectomy
Medial pain
ADL
MPTA 85°
W., U., 51 y.
PreOP Plan Software: 7° correction, 10 mm opening
W., U., 51 y.
6 days
postop
5 weeks
postop 6 days
postop
5 weeks
postop
FWB and working 5 weeks postop
6/30/2014
12
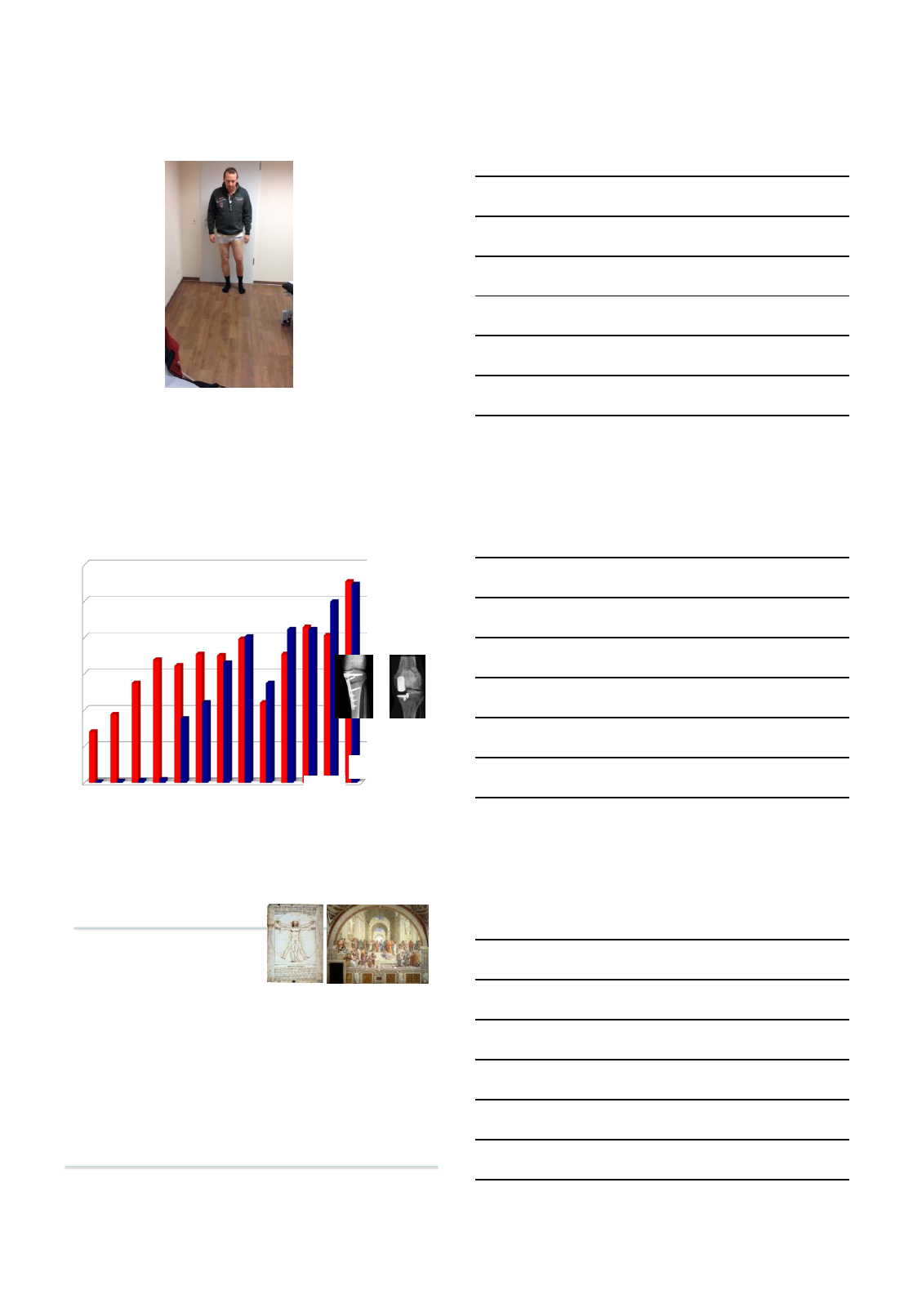
W., U., 51 y., male, 9 months postop
9 months postop: 10 days trekking up to 6000 m.
no pain!
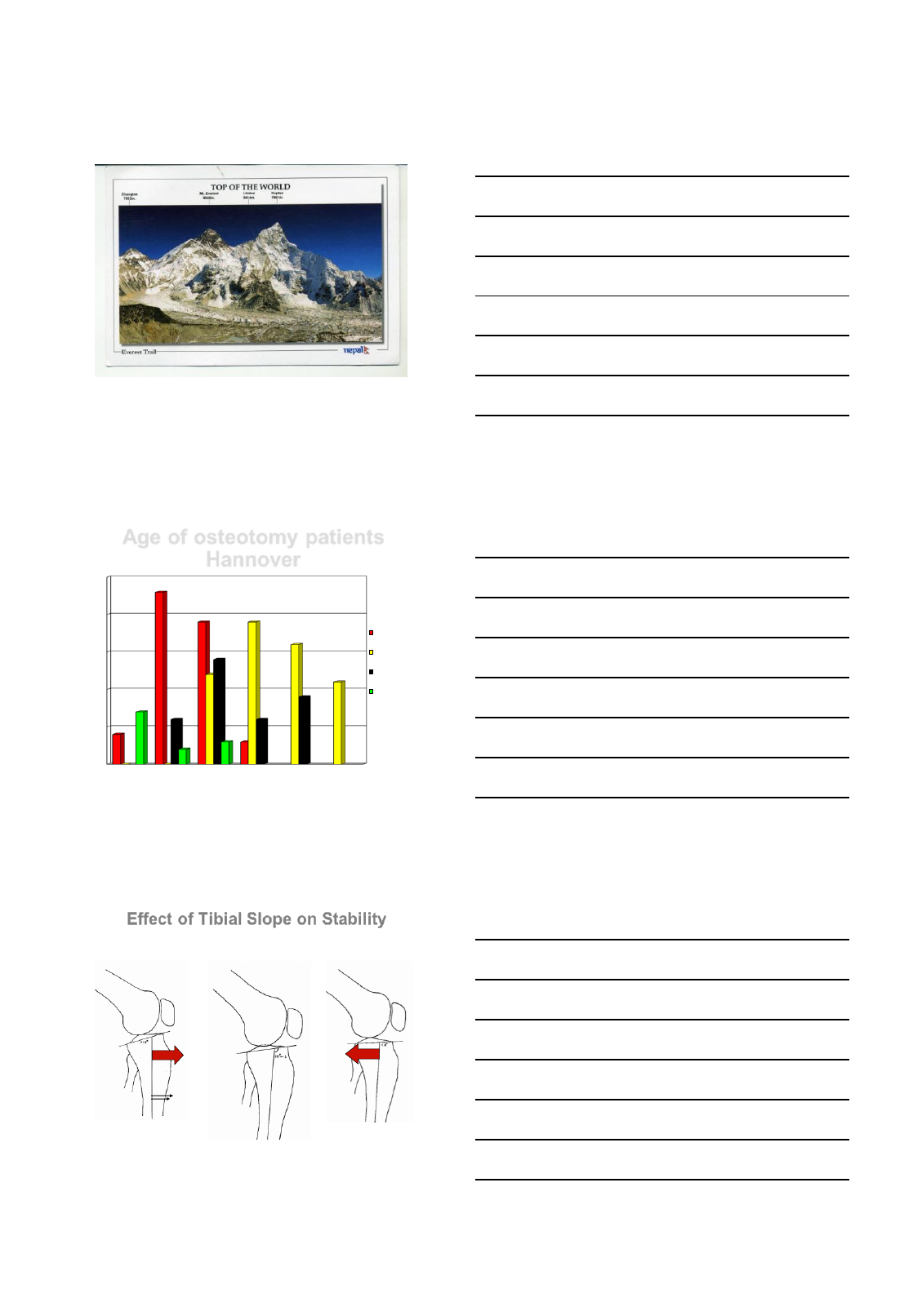
Age of osteotomy patients
Hannover
Instability
Osteoarthritis
Instab + OA
Deformity
years
1100 patients
Mean age: 40,5 years
Effect of Tibial Slope on Stability
Flexion Osteotomy:
Slope increase
10°
Extension Osteotomy:
Slope reduction
PCL
Instability ACL
Instability
6/30/2014
13
•Human cadaver joints
•Flexion osteotomy
•Gradual increase of slope
(0° 5 ° 10° 15°
20°)
•Computer-regulated isokinetic
extension movement of knee
(Knee Kinemator)
Biomechanical Study
J. Agneskirchner, C. Hurschler, A. Imhoff, P. Lobenhoffer
Winner of AGA DonJoy Award 2004
Archives Orthop Trauma Surg 4/2004
Results Kinematics
Durchtrennung hinteres Kreuzband
PCL transsected
posterior
subluxation
of tibia
reduction by
slope increase
Slope reduction in
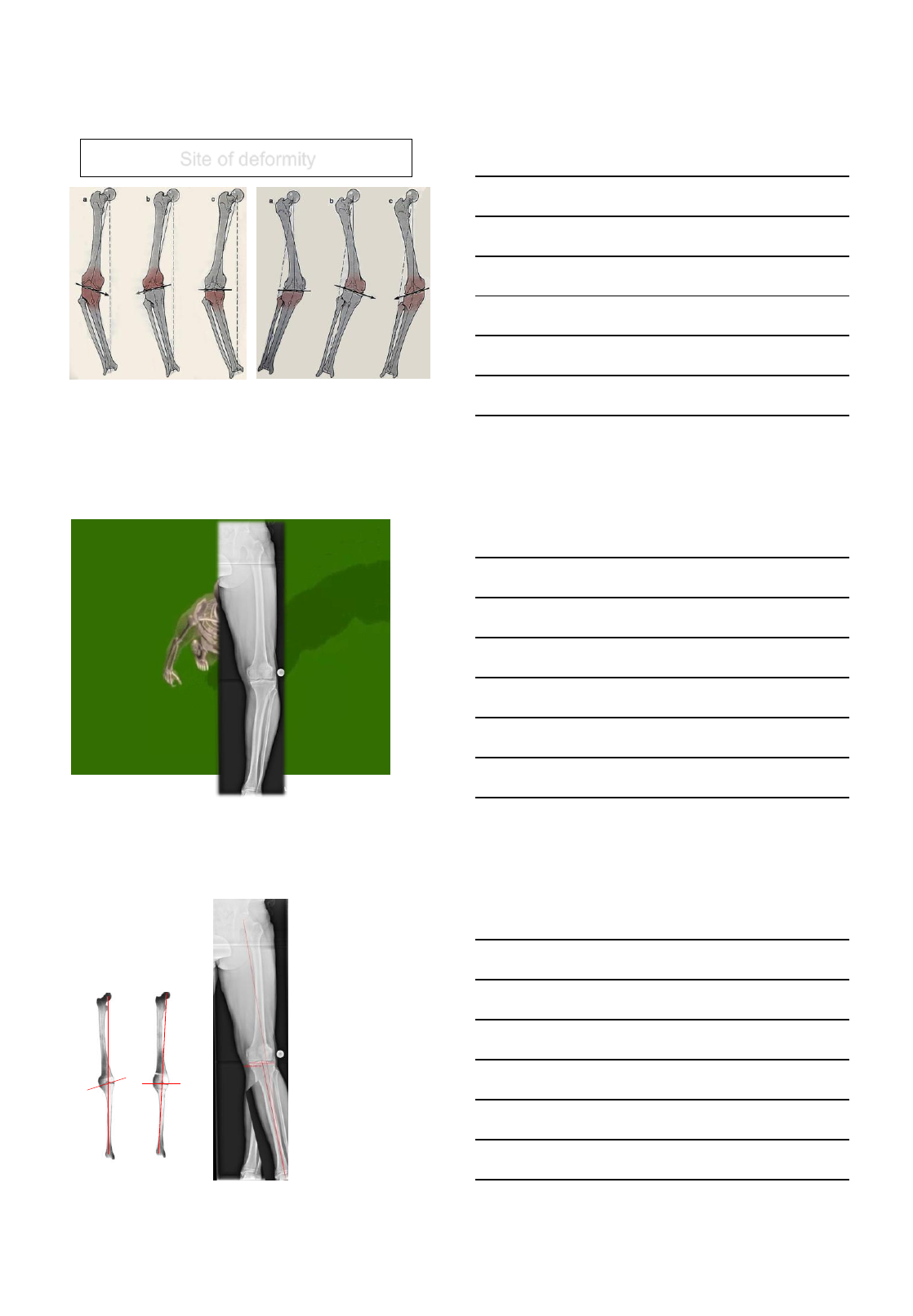
anterior knee instability
Tibial
Slope Anterior
Translation
force
0° 130 N
5° 235 N
10° 340 N
15° 443 N
20° 541 N
70 Kg, 20° Flexion, monopedal stance
10° slope
difference produce
6,8 mm. anterior
translation of tibia
in monopedal
stance
M. Bonnin, Lyon 1990
6/30/2014
14
Site of deformity
Femoral SCO correction
Single level osteotomy producing joint line obliquity
Not all
deformities
can be
adressed at
the tibia
The
importance
of the joint
line
What have
we learnt?
6/30/2014
15
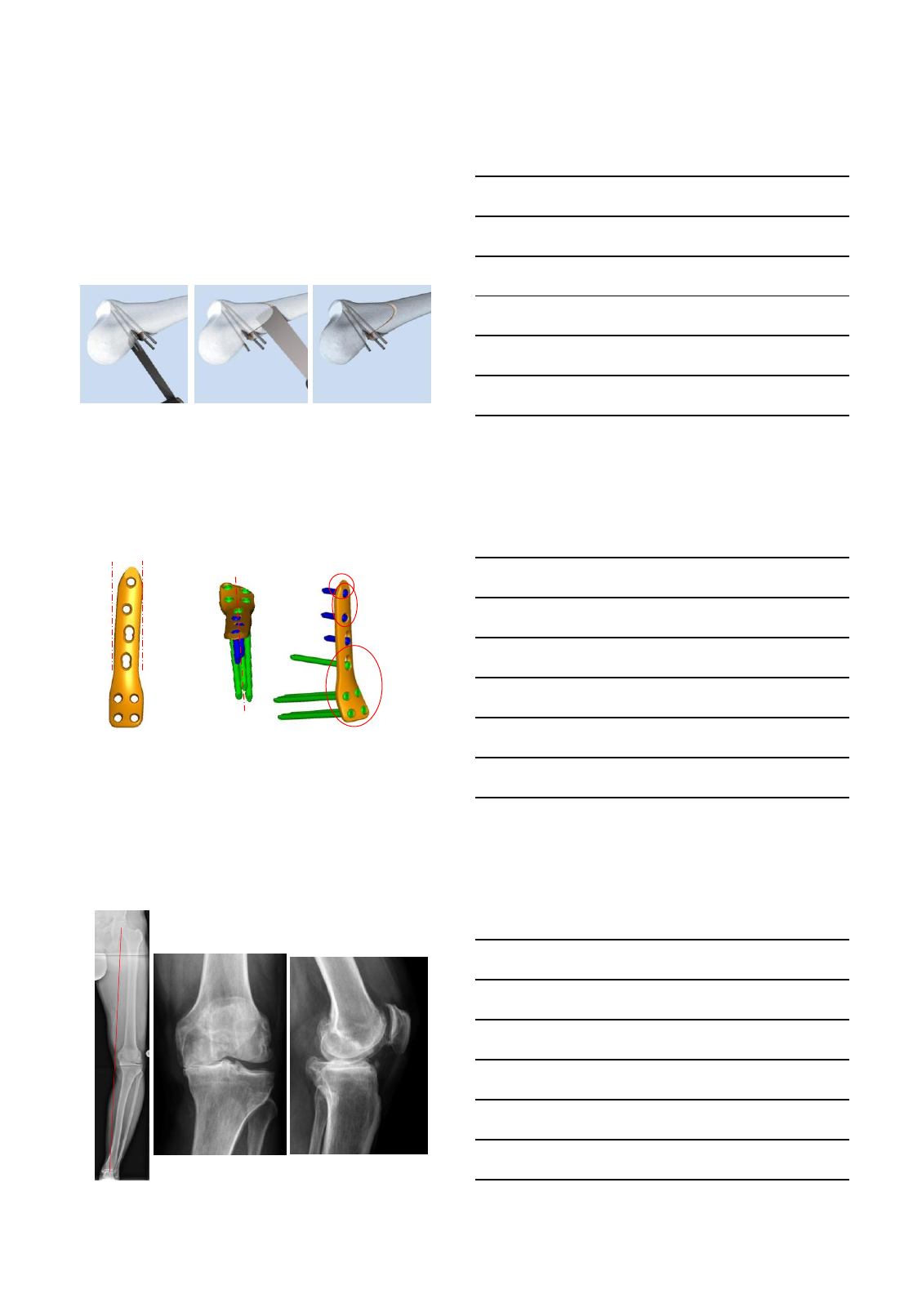
Femur biplanar closed wedge
osteotomy technique
post 2/3 femur: transverse bone cuts of closing
wedge along K-wires
ant 1/3 femur: ascending bone cut parallel to
posterior femur cortex
ww w.sportsclinicgermany.com
Design new Tomofix MDF plate
Less invasive
Optimized for
osteotomies
Optimal anatomic fit Even load distribution
for increased stability
Antecurvation
Twisted shaft
MIPO tapered tip
2 most proximal
holes allow
locking only
Twisted shaft ->
screws all point
in one direction
46
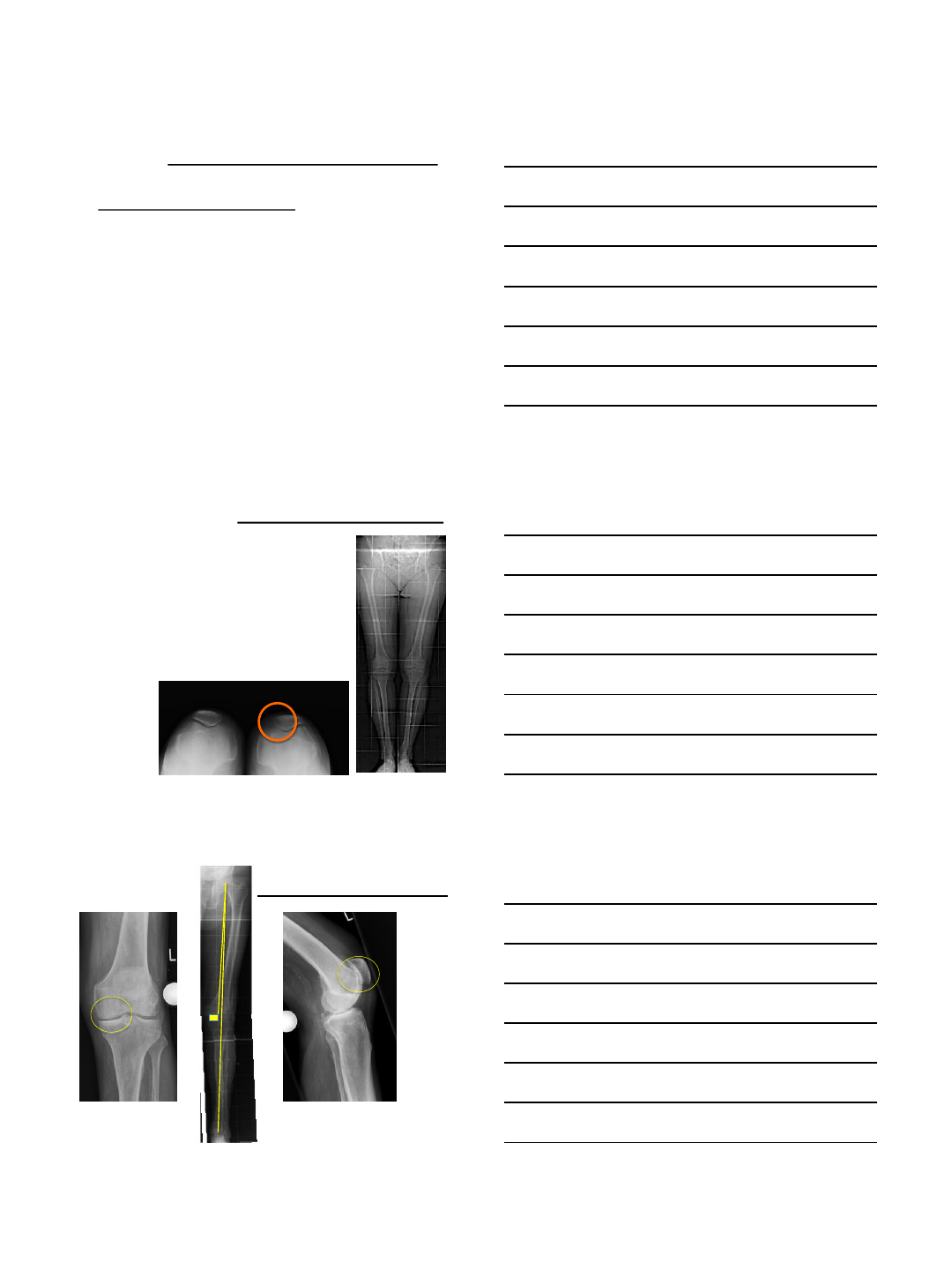
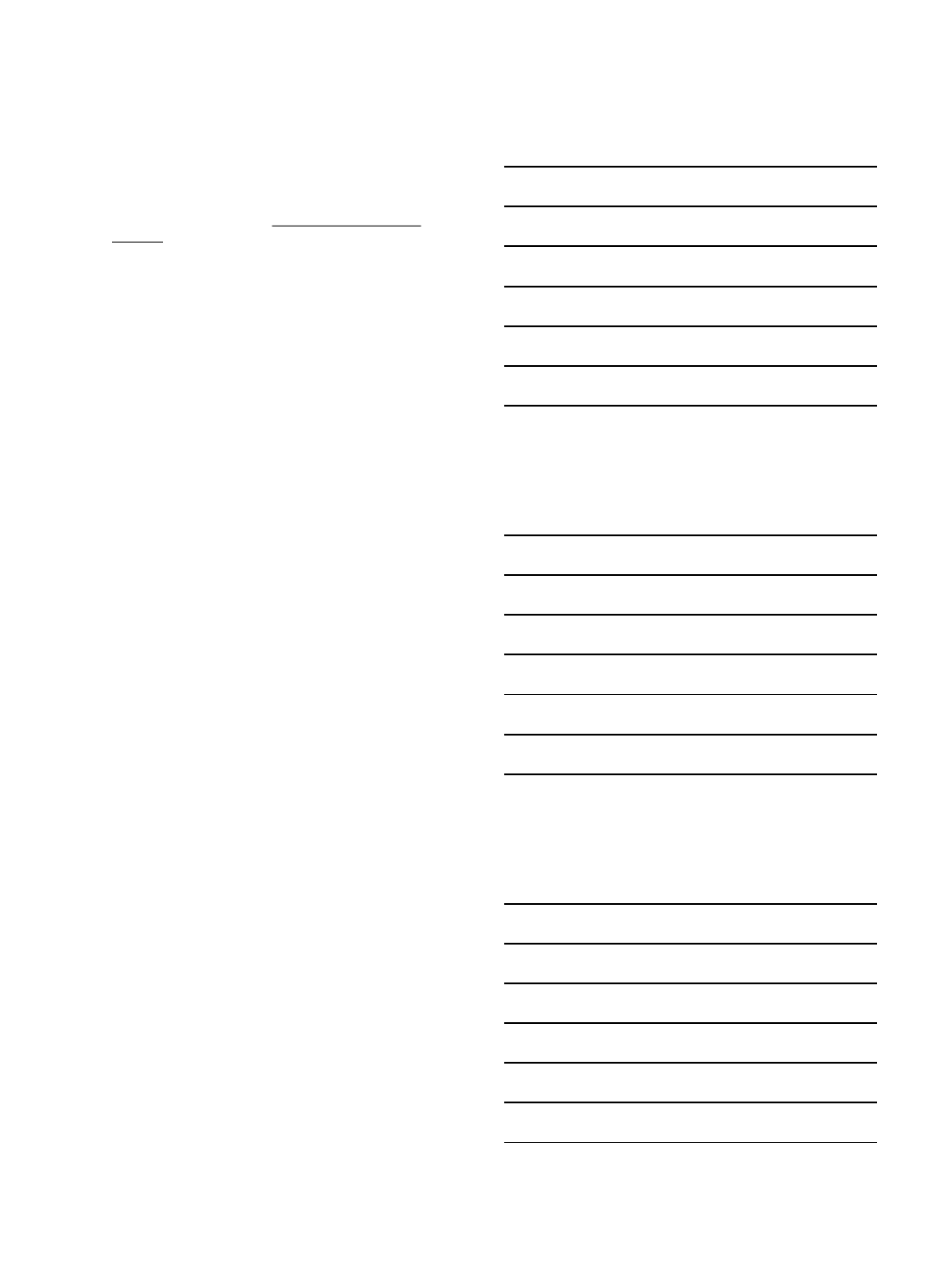
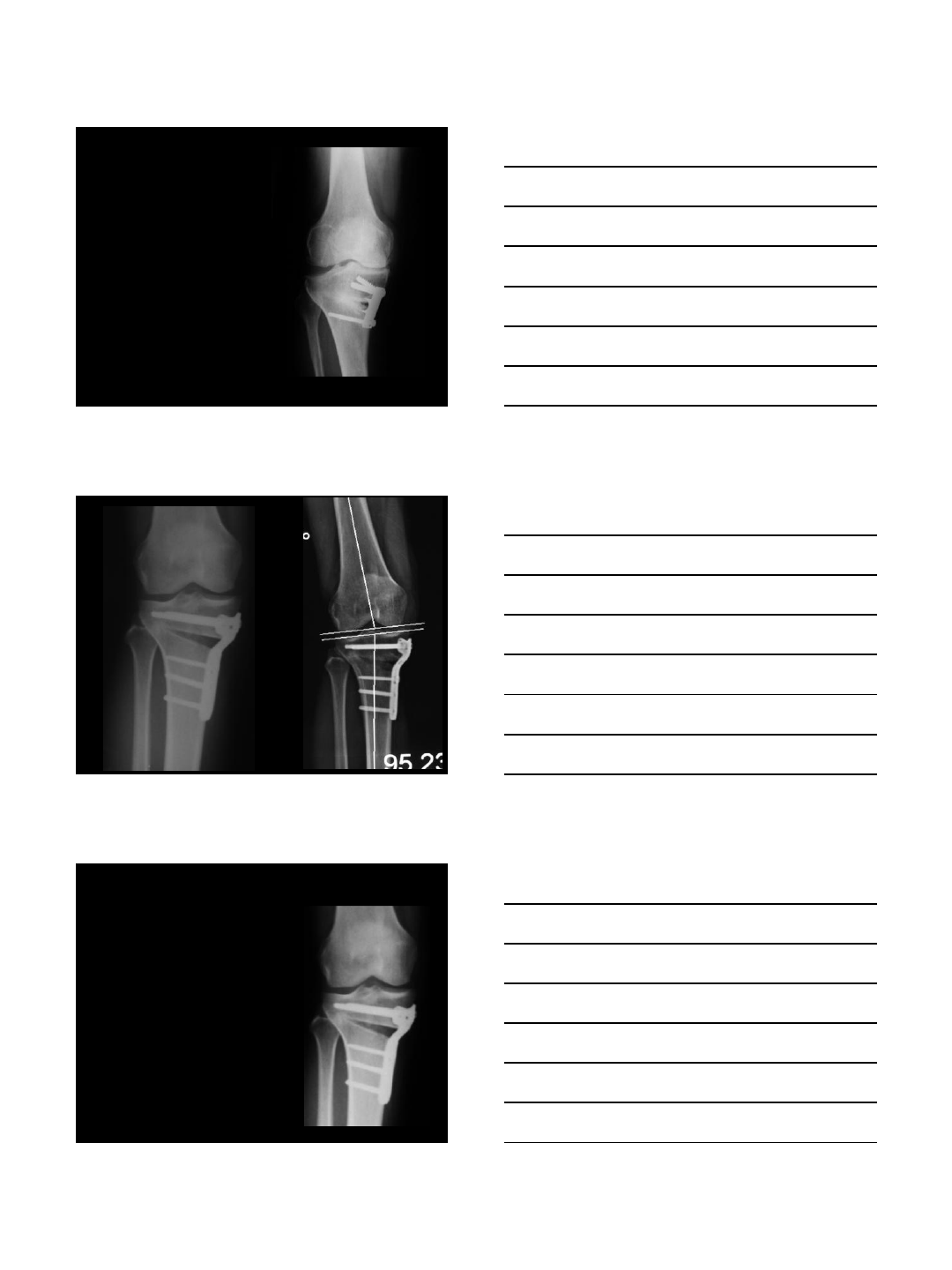
M.S., male, 46 y., tennis trainer
6/30/2014
16
M.S.,male, 46 y.
Double osteotomy
Femur closed wedge 7 mm
Tibia closed wedge 11 mm
LDFA 90°
MPTA 82°
Double osteotomy
1 week postop
Femur closed wedge
7 mm
Tibia closed wedge
11 mm
6/30/2014
17
Double osteotomy
4 days postop
Double osteotomy
6 weeks postop
Femur closed wedge
7 mm
Tibia closed wedge
11 mm
Double osteotomy
6 weeks postop
6/30/2014
18
Double osteotomy
6 weeks postop left side
Left side:
Femur closed wedge
7 mm
Tibia closed wedge
11 mm
Osteotomy versus Uni
Osteotomy
Uni
2013
2001 – 2013
2049 osteotomies
1752 Uni
2013:
20% DFO, DO
Key Points
Osteotomy around the knee works
Best indication metaphyseal deformity
HTO can treat ACL/PCL deficiency
Plate fixator/biplanar technique is safe
Osteotomy stimulates regeneration in
involved compartment
Renaissance of
osteotomy

6/30/2014
19
6/30/2014
1
Technical Pearls in OW HTO
Avoiding Complications
Hatem Said
Prof. Orthopaedic & Trauma
Assiut University, Egypt
SICOT Editorial Secretary
No Financial Disclosures
Complications
1. Overstuffing the joint
2. Lateral cortex break (6-20%)
3. Intra-articular Fracture (3%)
4. Changing the slope (1%)
5. Delayed (12%) / Nonunion (3%)
6. Loss of correction (1%)
7. Joint Line Tilt.
Martin et al, JAAOS 2014
6/30/2014
2
Technique
Non- Locked - Short
Lateral Hinge
BG
Locked T
No BG
1- Overstuffing
•Proper MCL release Lobenhoffer et al, 2007
MCL Release
6/30/2014
3
2- Lateral cortex break
• 1 cm from lat. Cortex
–Too short – Intra-artic fr.
•Lateral Hinge
– Non-Locked plates
•Locked plates:
–change principle - procedure
–Positional Fixation – plate
•Osteotomy too long
•Large opening
•Opening of lateral
cortex.
Lateral cortex break
Lat. break - Ttt
•Expose Lateral hinge
•Axial & Valgus Pr.
– Lat. cortex
•Staples
6/30/2014
4
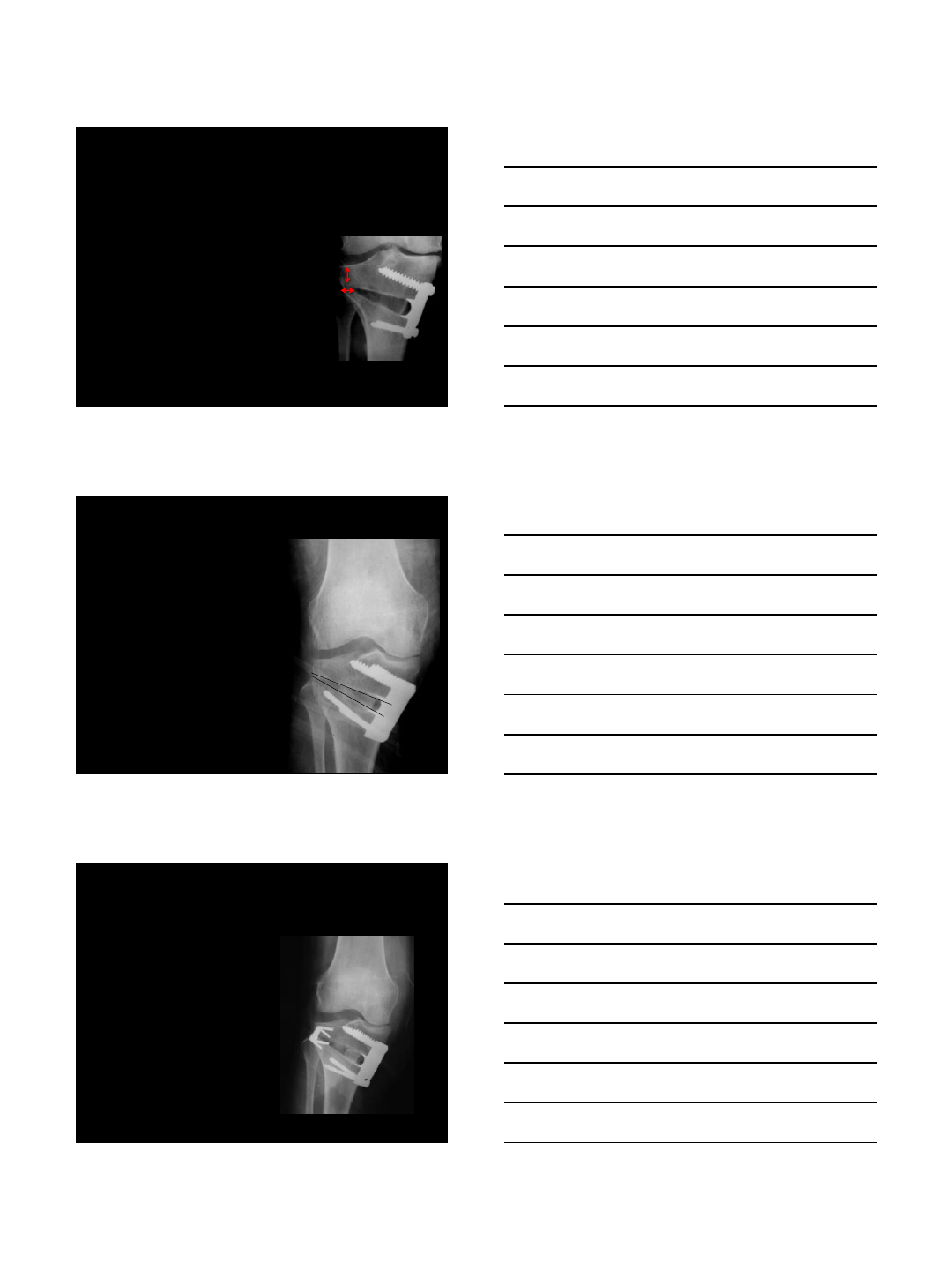
Intraop 1 m
•Osteotomy:
–Too high
–Too short
•Use Image intensifier
•Saw Under Wire
3- Intra-articular fractures
Intra-articular Fr.
7 wks
6/30/2014
5
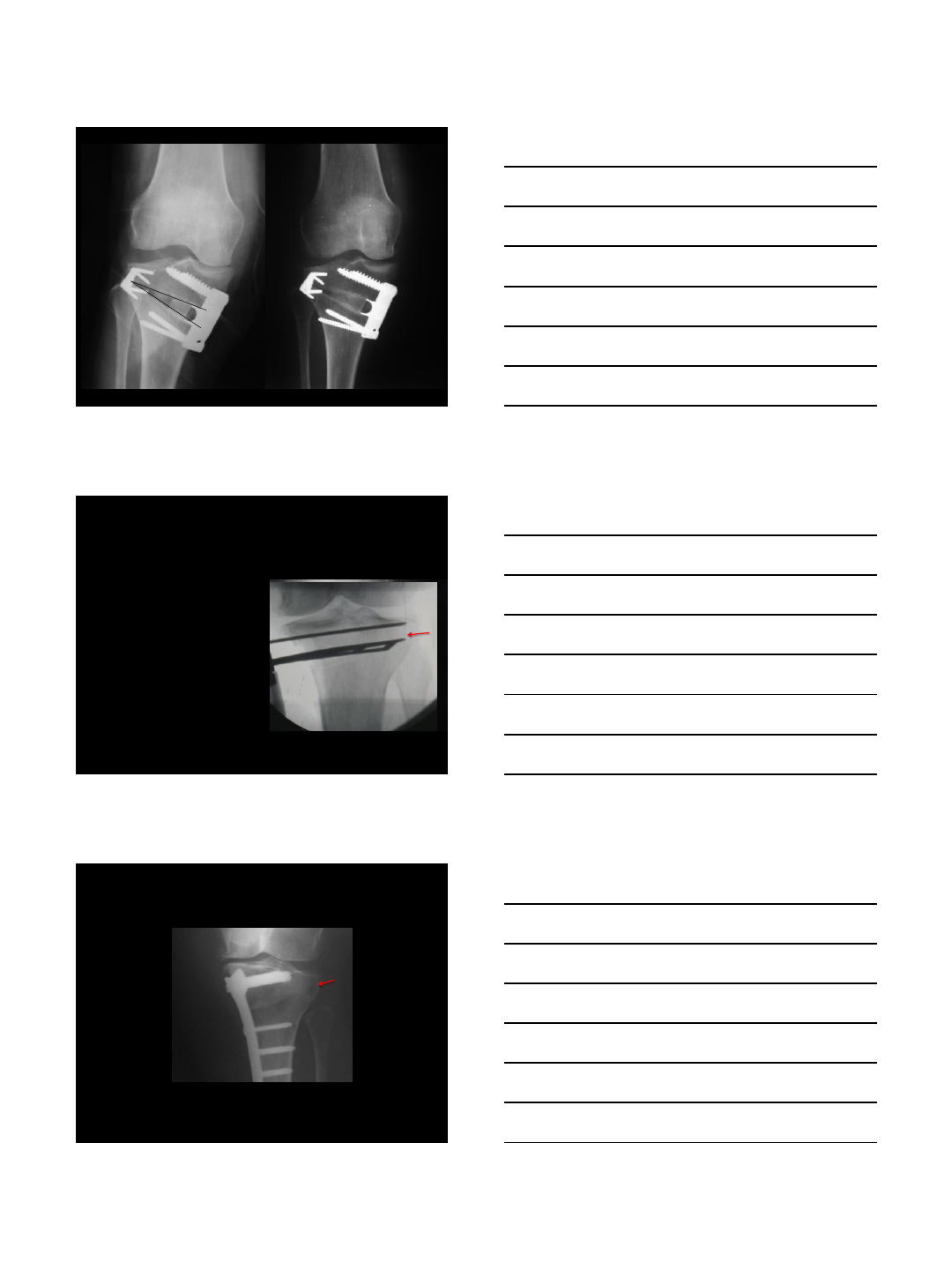
Displaced:
Loosen screws, valgus force, Lag screw.
Intra-op 5 weeks
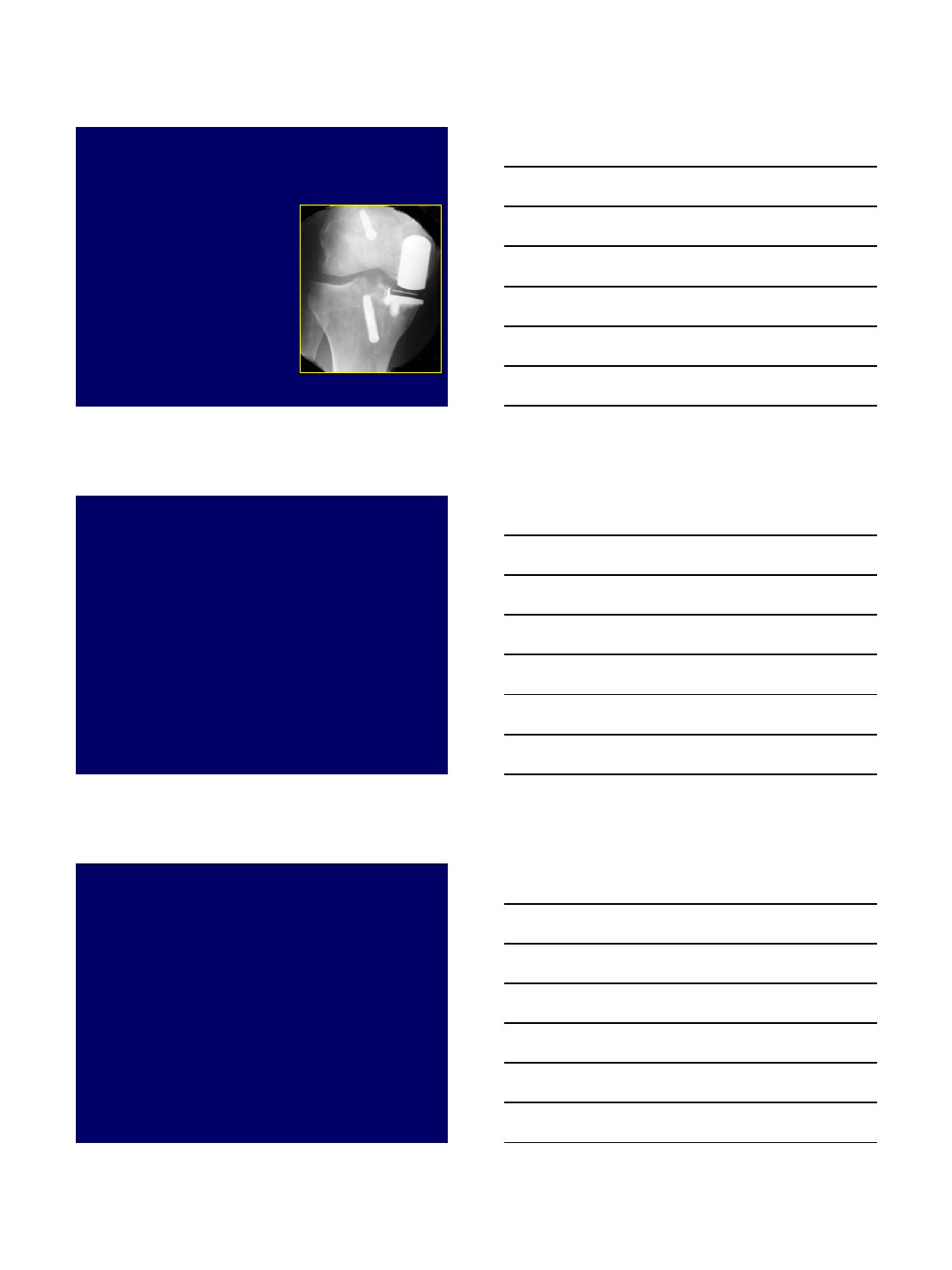
4- Changing the slope
Medial
Ant
Post
Lateral
9 Deg.
6/30/2014
6
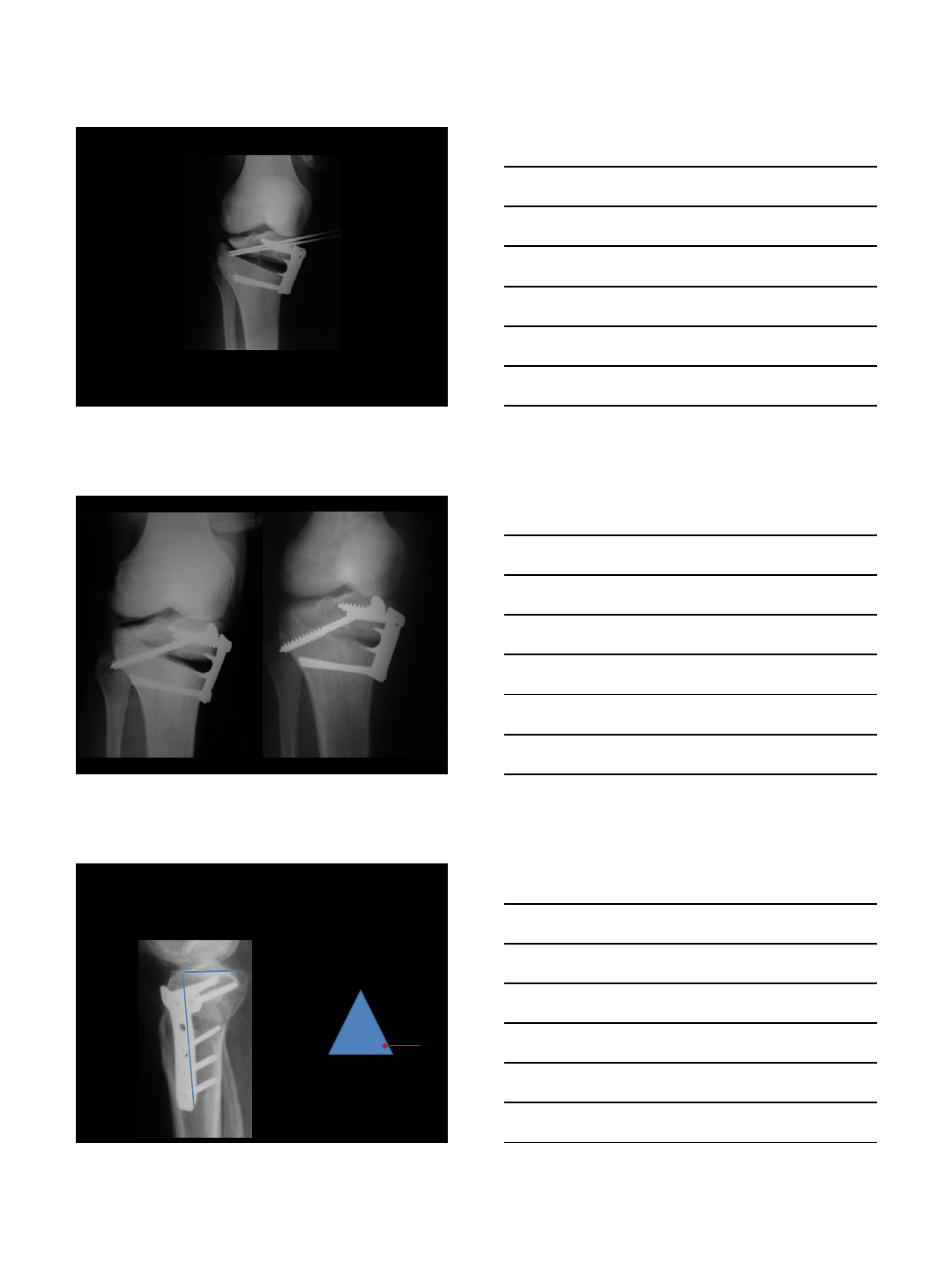
•Inc Slope:
–PCL deficient
•Dec Slope
–ACL Def
PCL/Varus:
15 Deg.
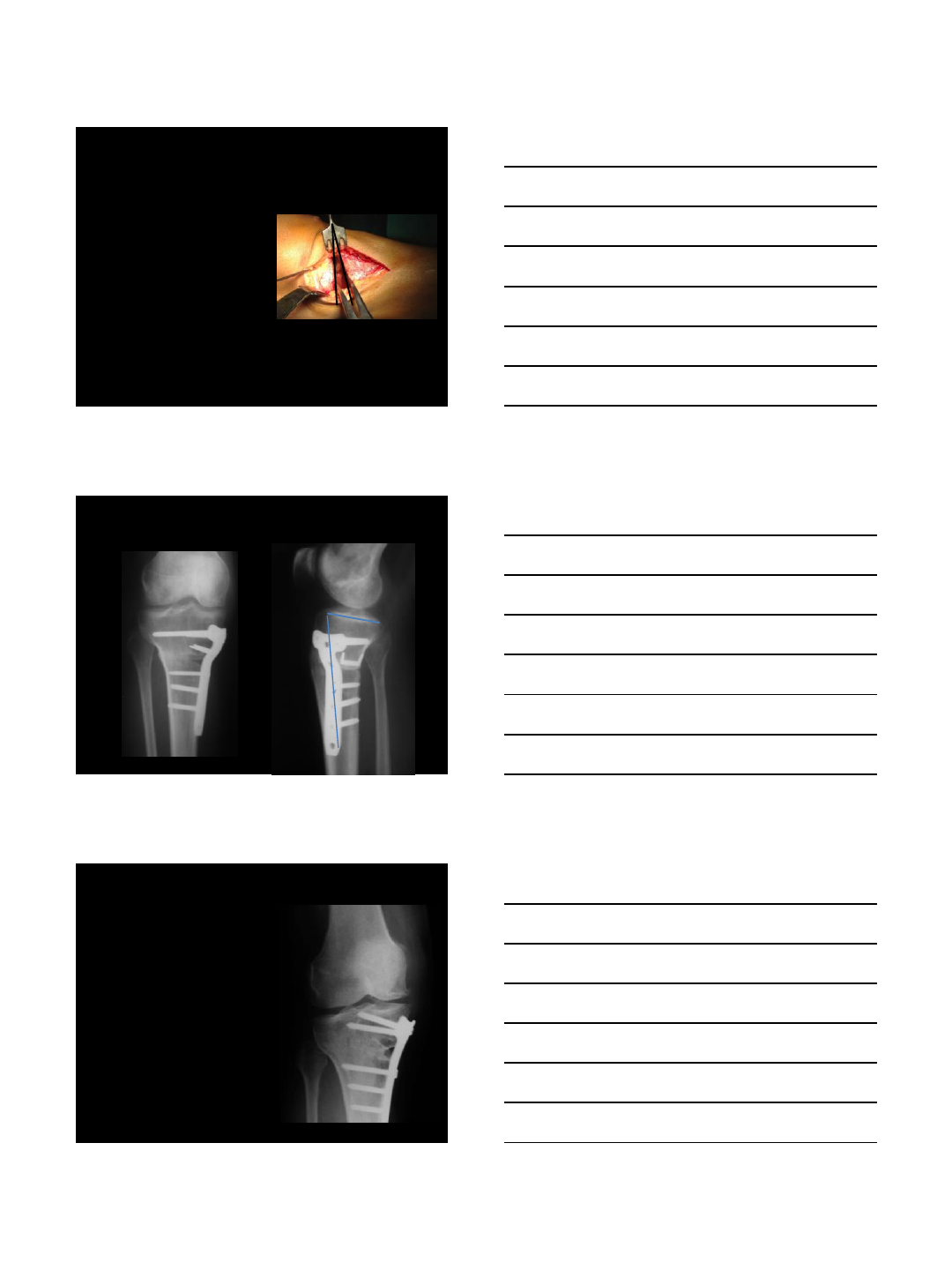
5- Delayed healing:
•65% Locked plates
–10% length
Roderer et al, 2014
6/30/2014
7
•Mechanical
–Inadequate fixation
–Lateral cortex break
•Not Biological
–No BG
•El-Assal et al. KSSTA 2010
5- Non Union
13 m
2.5 m
Long fixation + grafting
6/30/2014
8
6- Loss of Correction:
•Undercorrection
•Weak fixation
–Osteoporotic bone
•Locked plates
7- Joint Line Tilt:
Valgus 10
Summary
•MCL release
•Locked Plates:
–Lateral Cortex Break
–Intra-artic Fr.
•Slope
•Delayed / Nonunion
•Loss of correction
•Joint Line Tilt