Consensus In Chronic Ankle Instability OTSR CAI 20131
2014-01-26
: Pdf Otsr Consensus Cai 20131 OTSR_CONSENSUS_CAI_20131 1 2014 pdf
Open the PDF directly: View PDF ![]() .
.
Page Count: 9
- Consensus in chronic ankle instability: Aetiology, assessment, surgical indications and place for arthroscopy
Orthopaedics
&
Traumatology:
Surgery
&
Research
(2013)
99S,
S411—S419
Available
online
at
ScienceDirect
www.sciencedirect.com
REVIEW
ARTICLE
Consensus
in
chronic
ankle
instability:
Aetiology,
assessment,
surgical
indications
and
place
for
arthroscopy
S.
Guilloa,
T.
Bauerb,∗,
J.W.
Leec,
M.
Takao d,
S.W.
Konge,
J.W.
Stonef,
P.G.
Mangoneg,
A.
Molloyh,
A.
Pererai,
C.J.
Pearce j,
F.
Michelsk,
Y.
Tournél,
A.
Ghorbanim,
J.
Caldern
aClinique
du
Sport,
33300
Mérignac,
France
bDepartment
of
Orthopaedic
surgery,
Ambroise
Paré
Hospital,
92100
Boulogne
Billancourt,
France
cYonsei
University
College
of
Medicine,
Yonsei-ro
50,
Seodaemoon-gu,
120-752
Seoul,
South
Korea
dDepartment
of
Orthopaedic
Surgery
Teikyo
University
School
of
Medicine
2-11-1
Kaga,
Itabashi,
173-8605
Tokyo,
Japan
eFoot
and
Ankle
Surgery
Specialist
in
Orthopaedic
and
Traumatology,
Asia
Medical
Specialists,
Asia
fMedical
College
of
Wisconsin
Milwaukee,
WI
USA
gBlue
Ridge
Bone
and
Joint
ClinicAsheville,
NC
28801
Director,
Foot
and
Ankle,
Orthopaedic
Surgery
Service
Line,
Mission
Hospital,
Asheville,
NC
28801
hUniversity
Hospital
Aintree,
Lower
Lane
Liverpool
L9
7AL
UK
iUniversity
Hospital
of
Wales,
Cardiff
UK.
Spire
Cardiff
Hospital
and
London
Foot
and
Ankle
Centre
jJurong
Healthcare,
Alexandra
Hospital
Singapore
159964
kOrthopaedic
Department
AZ
Groeninge
Burg,
Vercruysselaan
5,
8500
Kortrijk,
Belgium
l15,
rue
de
la
République,
38000
Grenoble,
France
mClinique
Médipole
Garonne,
45,
rue
de
Gironis,
31036
Toulouse,
France
nChelsea
&
Westminster
Hospital,
369
Fulham
Road,
London
SW10
9NH,
UK
The
Fortius
Clinic,
17
Fitzhardinge
St,
London
W1H
6EQ,
UK
Accepted:
9
October
2013
KEYWORDS
Ankle
sprain;
Ankle
instability;
Lateral
ligament
injury;
Anterior
talo-fibula
ligament;
Ankle
arthroscopy
Summary
Ankle
sprains
are
the
most
common
injuries
sustained
during
sports
activities.
Most
ankle
sprains
recover
fully
with
non-operative
treatment
but
20—30%
develop
chronic
ankle
instability.
Predicting
which
patients
who
sustain
an
ankle
sprain
will
develop
instability
is
difficult.
This
paper
summarises
a
consensus
on
identifying
which
patients
may
require
surgery,
the
optimal
surgical
intervention
along
with
treatment
of
concomitant
pathology
given
the
evidence
available
today.
It
also
discusses
the
role
of
arthroscopic
treatment
and
the
anatomical
basis
for
individual
procedures.
Proof
of
evidence:
4.
©
2013
Published
by
Elsevier
Masson
SAS.
∗Corresponding
author.
E-mail
address:
th.bauer@orange.fr
(T.
Bauer).
1877-0568/$
–
see
front
matter
©
2013
Published
by
Elsevier
Masson
SAS.
http://dx.doi.org/10.1016/j.otsr.2013.10.009

S412
S.
Guillo
et
al.
Aetiology
of
chronic
ankle
instability
The
main
predisposing
factor
for
the
development
of
chronic
ankle
instability
(CAI)
is
the
history
of
at
least
one
previous
lateral
ankle
sprain
[1—3].
There
is
no
correlation
between
the
severity
of
the
initial
sprain
as
judged
at
the
time
of
injury
and
the
frequency
of
residual
instability
[2].
The
risk
of
developing
CAI
is
as
great
after
a
single
severe
ankle
sprain
as
after
one
or
multiple
minor
sprains.
Thus,
there
are
other
factors
contributing
to
the
development
of
CAI.
It
is
estimated
that
as
many
as
55%
of
patients
who
sus-
tain
an
ankle
sprain
do
not
seek
evaluation
or
treatment
from
a
healthcare
professional
[4].
The
absence
of
treat-
ment
after
an
ankle
sprain
predisposes
to
residual
symptoms
including
CAI
[5].
With
respect
to
giving-way
and
return
to
sport,
improved
stability
with
faster
recovery
was
noted
after
surgical
treatment
for
acute
ankle
sprain
compared
to
non-operative
treatment.
However,
the
advantages
of
this
operative
treatment
should
be
balanced
with
the
risk
of
complications
and
the
costs
[6—8].
Functional
treatment
after
acute
ankle
sprain
(with
early
proprioceptive
rehabili-
tation)
enables
better
results
and
faster
recovery
compared
to
immobilization
[9—12].
However,
there
are
still
contro-
versies
concerning
the
exact
role
of
rehabilitation
on
the
prevention
of
ankle
sprain
recurrence
[13].
Mechanical
instability
is
due
to
the
laxity
caused
by
ligaments
tears.
Functional
instability
is
due
to
propriocep-
tive
and
muscular
deficits
after
ankle
sprain
[14,15].
Both
mechanical
and
functional
instabilities
may
be
difficult
to
assess
or
distinguish
and
they
most
often
occur
as
a
combi-
nation
in
the
development
of
CAI.
The
level
of
activity
is
a
very
important
extrinsic
factor
influencing
the
impact
of
CAI
in
the
daily
life.
The
assess-
ment
of
activity
level
for
each
patient
is
useful
not
only
to
differentiate
patients
at
high
or
low
risk
of
developing
CAI
after
an
ankle
sprain,
but
also
to
find
the
optimal
treatment
and
also
allows
comparison
of
functional
results.
Different
factors
such
as
level
of
sport
activities
(professional,
ama-
teur
competitive,
leisure,
sedentary),
type
of
sport,
work
and
shoes
must
be
assessed
when
questioning
the
patient.
It
has
recently
been
suggested
that
there
may
be
a
role
for
those
early
operative
repair
of
the
ligaments
in
the
acute
stage
in
elite
athletes
with
a
severe
ankle
sprain
and
sig-
nificant
ankle
instability
as
this
is
known
to
reduce
the
risk
of
CAI
as
the
incidence
of
significant
symptoms
following
non-operative
management
is
approximately
20%
[16].
Lower
limb
varus
mal-alignment
has
been
described
as
an
important
factor
predisposing
to
ankle
sprain
and
CAI
[17].
Anatomical
variations
of
the
tibiotalar
joint
such
as
axis
of
rotation,
talar
dome
radius
or
retroposition
of
the
lateral
malleolus
can
predispose
to
ankle
sprain
and
CAI
[17—20].
Pathological
conditions
of
the
tibiotalar
joint
such
as
limitation
of
dorsiflexion
(anterior
impingement,
short
gastrocnemius),
chondral
problems
(ankle
osteochondral
defects,
loose
bodies)
or
bimalleolar
diastasis
can
provoke
or
increase
CAI
[21].
Subtalar
joint
anatomical
variations
(axis
of
rotation,
hindfoot
varus)
or
pathologies
(talocalcaneal
coalition,
subtalar
joint
laxity
due
to
injuries
of
the
cervical
lig-
ament,
the
talocalcaneal
ligament
or
the
interosseous
ligament)
act
as
risk
factors
of
CAI
[22—27].
Anatomical
and
histological
variations
of
the
collateral
lateral
ligament
(insertion
zones,
number
of
bands,
collagen
diseases)
are
also
important
intrinsic
risk
factors
for
CAI
[20,28—30].
Per-
oneal
tendons
pathologies
can
provoke
or
increase
a
CAI
[31]
and
pathologies
with
a
proprioceptive
deficit
or
imbalance
in
neuromuscular
control
are
a
frequent
cause
of
CAI
[17,32].
Evidence
from
peer-reviewed
literature
suggests
that
the
characteristics
of
patients
who
develop
chronic
ankle
insta-
bility
are
not
homogeneous.
The
aetiological
elements
of
CAI
are
a
continuum
of
pathologic
conditions
and
anatomic
variability.
A
good
knowledge
of
these
characteristics
will
improve
the
decisions
for
the
treatment.
Not
all
aetiological
aspects
are
yet
defined
and
more
studies
are
needed.
A
well-known
pathological
condition
is
the
patient
with
persisting
complaints
of
instability
asso-
ciated
with
pain,
but
without
any
objective
characteristics.
This
may
be
explained
by
formation
of
scar
tissue
and
arthro-
scopic
approach
may
be
useful
to
assess
the
ankle
joint
in
these
situations
[33].
Clinical
assessment
of
chronic
ankle
instability
History
of
an
ankle
sprain
must
precede
the
symptoms
of
CAI.
A
lateral
ankle
sprain
is
defined
as
an
episode
of
acute
inversion/supination
injury
of
the
ankle
associated
with
swelling,
lateral
ankle
pain
and
difficulty
weight-bearing.
Chronic
ankle
instability
is
defined
as
the
perception
by
the
patient
of
an
abnormal
ankle
with
a
combination
of
symptoms
including
recurrent
sprains,
pain
and
swelling
or
avoidance
of
activities.
The
following
standard
questions
should
be
asked
of
patients
with
ankle
instability:
•
how
long
ago
was
the
first
acute
event?
•
what
were
the
modalities
of
treatment?
•
does
the
ankle
continue
to
give
way?
(yes
or
no):
◦
if
yes,
with
what
frequency?
•
is
there
an
adaptation
or
avoidance
to
daily
or
sport
activ-
ities?
(yes
or
no);
•
is
there
an
ankle
pain
between
new
sprain
events?
(yes
or
no):
◦
if
yes,
the
location
of
the
pain
must
be
defined;
•
does
the
ankle
swell?
(yes
or
no):
◦
if
yes,
the
location
of
the
swelling
must
be
specified.
The
purpose
of
these
questions
is
to
establish
which
of
the
following
five
presentations
is
present
all
of
which
are
compatible
with
CAI:
•
recurrent
acute
ankle
sprain;
•
giving
way
of
the
ankle
without
new
sprain;
•
perception
of
an
insecure/unstable
ankle
by
the
patient;
•
avoidance
of/adaptation
to
daily
or
sporting
activities;
•
perception
of
an
abnormal
ankle
by
the
patient
(pain,
swelling).
The
physical
examination
must
include
comparative
assessment
of
both
ankles.
Lower
leg
and
hindfoot
align-
ment
must
be
assessed
whilst
standing
and
gait
should
be
evaluated.
Precise
location
of
tenderness
must
be
identified.
Active
and
passive
ankle
range
of
motion
(ROM)
Chronic
ankle
instability:
current-concepts
S413
is
measured
with
the
knee
extended
and
then
on
a
sit-
ting
position
with
the
legs
down
and
the
knees
flexed
to
90◦in
order
to
assess
gastrocnemius
tightness.
Hindfoot
inversion/eversion
is
compared
to
the
other
side.
In
view
of
the
difficulty
in
making
precise
measurements
of
hind-
foot
mobility,
grading
as
normal,
abnormal
(increased
or
decreased)
or
no
mobility
is
appropriate.
An
assessment
of
generalised
joint
laxity
is
important
(Beighton
scale).
Strength
and
pain
on
resisted
function
of
peroneal
and
tibialis
posterior
tendons
are
specifically
tested
and
neu-
rovascular
status
of
the
lower
legs
is
then
assessed.
Ankle
ligament
testing
is
comparative
and
performed
on
a
relaxed
patient
in
a
sitting
position
with
the
knee
flexed.
It
may
be
difficult
to
describe
the
degree
of
ankle
laxity
of
the
ante-
rior
drawer
test
between
examiners
and
therefore
a
simple
description
of
stable,
unstable,
unstable
with
sulcus
sign
may
be
preferred.
The
presence
of
varus
tilt
is
frequently
difficult
to
assess
and
laxity
or
absence
of
laxity
compared
to
the
other
side
is
likewise
preferred
[34,35].
Stability
and
proprioceptive
control
of
the
ankle
can
be
assessed
by
the
patient
standing
with
a
single
leg
stance
(eyes
open
and
then
eyes
closed).
This
test
may
be
helpful
to
differentiate
mechanical
from
functional
instability
[36,37].
Radiographic
assessment
The
standard
plain
radiographs
include:
standing
antero-
posterior,
lateral
and
mortise
views
and
a
comparative
Saltzmann
view
(or
Méary
view),
which
is
helpful
to
assess
hindfoot
alignment.
Comparative
stress
radiographic
views
with
anterior
drawer
test
and
varus
tilt
may
be
performed
although
it
should
be
recognised
that
these
have
a
high
rate
of
false
negative
results
[34,35].
Magnetic
resonance
imaging
may
be
helpful
in
the
pres-
ence
of
deep
pain
to
assess
for
osteochondral
lesions
and
tendon
injuries
and
it
will
also
confirm
the
presence
of
chronic
ligamentous
injury.
Ultrasonography
may
be
par-
ticularly
helpful
in
the
assessment
of
tendon
pathology.
Computer
tomography/MRI-arthrogram
scanning
is
not
rou-
tinely
advised
but
may
be
helpful
for
accurate
assessment
of
chondral
lesion.
Scoring
systems
for
chronic
ankle
instability
Quantifying
the
severity
of
ankle
instability
is
a
difficult
problem.
Many
patients
may
not
have
any
episodes
of
actual
giving
way
or
falling,
as
they
tend
to
avoid
aggravating
situa-
tions.
Instead,
the
main
complaint
is
often
just
a
feeling
of
vulnerability
and
this
is
hard
to
measure
objectively.
How-
ever,
an
attempt
has
to
be
made
to
gauge
the
severity
of
the
problem
in
order
to
facilitate
decisions
regarding
indi-
cations
for
surgery,
return
to
sport
and
of
course
assessing
the
quality
of
the
outcome
of
surgical
intervention.
The
history
of
outcome
scoring
for
instability
mirrors
the
experience
of
orthopaedics
as
a
whole,
moving
from
surgeon-designed
and
-administered
scores
to
more
objec-
tive
patient-centred
measures
(Table
1).
We
are
fortunate
that
in
this
area
we
have
some
objective
measures
(Table
2)
that
can
be
used
to
analyse
the
clinimetric
properties
of
the
various
outcome
scores
though
they
are
not
appropriate
for
everyday
clinical
use.
Table
1
Outcome
scores.
Generic
health
scores
Disease
specific
scores
SF12
[38]
Karlsson
1988
[44]
EuroQol
-EQ5D
[39]
Kaikkonen
1994
[45]
Ankle
joint
functional
assessment
tool
(AJFAT)
1999
[46]
Generic
foot
and
ankle
scores
Functional
Ankle
Disability
Index
(FADI)
Functional
Ankle
Disability
Sport
(FADI-Sport)
1999
[47]
American
orthopaedic
foot
and
ankle
score
(AOFAS)
[40]
Sports
ankle
rating
system
(SARS)
2003
[48]
Foot
and
ankle
outcome
score
(FAOS)
2001
[41]
Foot
and
ankle
assessment
measure
(FAAM)
2005
[49]
Ankle
instability
index
(AII)
2006
[50]
Activity
assessment
scales
Cumberland
Ankle
Instability
Tool
(CAIT)
2006
[51]
Tegner
1985
[42]
Foot
and
ankle
instability
questionnaire
(FAIQ)
2007
[52]
Halasi
2004
[43] Chronic
ankle
instability
scale
(CAIS)
2008
[53]
Identification
of
foot
and
ankle
instability
(IdFAI)
2011
[54]
To-date,
there
has
been
no
consensus
on
the
best
score
to
use.
A
variety
of
instruments
have
been
advocated,
many
of
which
are
not
validated
or
even
appropriate
for
instability
(Table
3).
A
number
of
studies
have
analysed
many
of
these
scores,
though
none
have
as
yet
proved
to
be
clearly
superior
[64—66].
The
IdFAI
score
is
the
most
recent
and
promising
score
but
it
is
yet
to
be
used
in
any
published
studies
[54].
The
authors
themselves
feel
that
it
is
a
starting
point
for
further
development
and
refinement
rather
than
a
definitive
measure.
Consensus
was
reached
that
this
area
needed
much
more
work
but
that
comparison
of
results
required
a
standard-
ised
approach.
The
FAOS
score
was
selected
as
this
has
been
validated
for
use
in
ankle
ligament
reconstruction,
it
is
patient-centred
and
easy
to
complete
[41].
This
should
be
Table
2
Physical
tests.
Non-instrumented
Instrumented
Single
leg
balance
[36,37]
Force
platforms-
static
and
dynamic
testing
[58]
Hopping
tests
—
on-the-spot,
lateral,
figure-of-8
[55]
Surface
EMG-
peroneal
reaction
times
[59]
Y
balance
test
and
star
excursion
balance
test
[56]
Balance
error
scoring
system
[57]
S414
S.
Guillo
et
al.
Table
3
Review
of
instability
literature
from
foot
and
ankle
instability
2012
to
present.
Study
Outcome
score
used
Tourné
et
al.
2012
[60]
Karlsson
Good
Jones
Livingstone
Youn
et
al.
2012
[61] Karlsson
Miller
et
al.
2013
[62] FAAM
Vega
et
al.
2013
[63] AOFAS
used
in
conjunction
with
the
EQ5D,
a
5-item
generic
health
measure
that
is
similarly
quick
and
easy
to
complete.
There
is
a
wide
variation
in
the
type
of
patient
from
the
office
worker
to
the
‘week-end
warrior’
and
the
elite
ath-
lete.
Therefore
it
is
recommended
that
the
Halasi
activity
level
score,
a
modernised
version
of
the
Tegner
Score,
is
used
to
define
the
patient
population
of
individual
series’
in
order
to
inform
comparison
of
outcome
in
light
of
demand
and
expectation
[42,43].
Arthroscopic
assessment
in
chronic
ankle
instability
A
review
of
the
literature
shows
that
13
to
35%
of
patients
report
symptoms
such
as
pain
and
recurrent
instability
after
a
successful
ligament
reconstruction
[67—71].
Intra-
articular
pathology
has
been
suggested
as
the
cause
for
these
persistent
symptoms,
and
although
many
authors
have
reported
arthroscopic
findings
in
patients
with
chronic
lat-
eral
ankle
instability,
there
has
been
no
attempt
to
correlate
the
type
and
number
of
intra-articular
lesions
with
the
patient
outcome.
Previous
studies
stated
that
osteochondral
lesions
of
the
talus,
soft
tissue
impingement
lesions,
osseous
loose
bod-
ies,
peroneal
tendon
disorders
and
other
associated
injuries
could
be
sources
of
postoperative
pain
in
chronic
ankle
instability
patients
[20,71—75].
To
date,
there
have
been
few
reports
on
surgical
results
with
regard
to
intra-articular
lesions
in
patients
with
chronic
lateral
ankle
instability.
Choi
et
al.
have
shown
that
63
out
of
65
cases
of
ankle
instability
(96.9%)
had
intra-articular
lesions,
of
which
53
cases
(81.5%)
showed
soft
tissue
impingement
as
the
most
common
asso-
ciated
lesion
[21].
Other
associated
intra-articular
lesions
included
ossicles
at
the
lateral
malleolus
(38.5%),
syndesmo-
sis
widening
(29.2%),
and
osteochondral
lesion
of
the
talus
(23.1%).
One
of
the
notable
features
of
this
study
is
that
they
have
analyzed
the
clinical
outcome
relative
to
the
presence
of
intra-articular
lesions
and
have
shown
that
the
strongest
risk
indicators
for
patients’
dissatisfaction
were
syndesmo-
sis
widening,
osteochondral
lesions
of
the
talus
and
ossicles.
The
number
and
severity
of
lesions
was
greater
in
those
with
chronic
instability
and
this
was
also
associated
with
a
poor
clinical
outcome
following
surgery.
The
high
rate
of
soft
tissue
impingement
in
chronic
ankle
instability
may
be
a
response
to
a
coexisting
intra-articular
lesion
or
repetitive
inversion
stress
to
the
ankle.
The
term
‘‘soft
tissue
impingement’’
included
hypertrophic
synovial
and
fibrotic
scar
tissue
obliterating
the
joint
space
that
corresponded
to
localized
tenderness.
Soft
tissue
impinge-
ment
is
known
to
be
strongly
associated
with
osteochondral
lesions
due
to
the
self-regeneration
mechanism
of
synovial
osteoprogenitor
cells
that
migrate
to
the
lesion
site.
How-
ever,
there
is
disagreement
about
whether
this
would
affect
the
clinical
outcome
[76—78].
Lee
et
al.
described
the
diag-
nosis
and
arthroscopic
treatment
of
soft
tissue
impingement
in
38
patients
with
chronic
ankle
pain
after
trauma
[79].
Ossicles
at
the
tip
of
the
lateral
malleolus
are
frequently
found
in
patients
with
chronic
lateral
ankle
instability.
However,
the
relationship
between
the
presence
or
the
size
of
an
ossicle
and
the
outcome
of
ligament
recon-
struction
is
poorly
understood.
Kim
et
al.
reported
that
ankles
with
large
ossicles
improved
post-reconstruction
with
regards
to
varus
stability
but
not
anteroposterior
stability
[80].
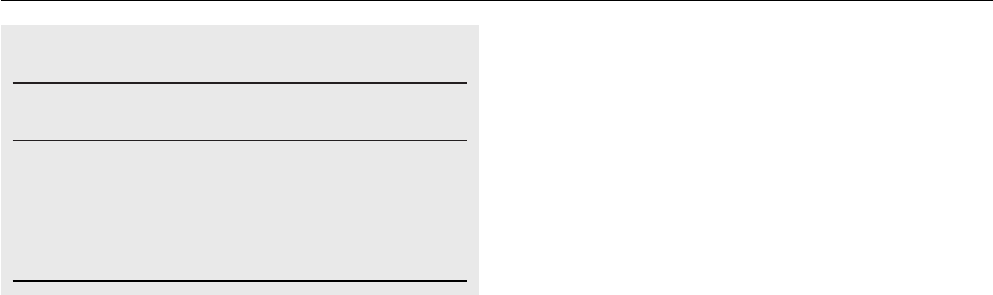
When
the
ossicle
is
large,
excision
and
the
modi-
fied
Broström
technique
may
not
be
suitable
to
achieve
mechanical
anteroposterior
stability.
Therefore,
fusing
the
ossicle
to
the
fibular
tip
or
using
other
methods
of
ligament
reconstruction
may
need
to
be
considered
in
chronic
ankle
instability
with
associated
large
ossicles
(Fig.
1).
Syndesmosis
widening
has
been
recognized
as
one
of
the
causes
of
prolonged
ankle
pain.
Injury
to
the
syn-
desmotic
ligaments
occurs
as
a
result
of
external
rotation
forces,
which
often
accompany
inversion
sprains.
Syn-
desmotic
instability
was
defined
as
the
ability
to
displace
the
fibula
laterally
more
than
2
mm
with
the
shoulder
of
the
probe
while
placed
in
the
syndesmotic
joint
[81—84].
This
criterion
was
based
on
the
study
by
Close
who
reported
that
the
maximum
widening
of
the
intra-articular
distal
tibiofibular
syndesmosis
was
approximately
1.5
mm
in
a
normal
ankle
[85].
Teramoto
and
Taylor
reported
that
a
pos-
sible
explanation
for
the
increased
incidence
of
recurrent
sprains
in
patients
with
syndesmosis
widening
is
altered
fibu-
lar
mobility
leading
to
altered
ankle
biomechanics
[86,87].
Disrupted
distal
fibular
migration
and
fibular
axial
motion
can
alter
normal
ankle
function.
The
resultant
alteration
in
ankle
function
may
predispose
the
ankle
to
inversion
sprains.
Therefore,
after
the
distal
tibiofibular
syndesmo-
sis
is
ruptured,
healing
is
protracted,
functional
disability
is
not
uncommon
and
prognosis
is
guarded.
Some
contro-
versy
exists
regarding
the
treatment
method
and
the
merits
of
screw
fixation
[82,88,89].
Han
et
al.
in
accordance
with
Ogilvie-Harris
and
Reed
suggested
that
soft
tissue
hyper-
trophy
and
its
subsequent
impingement
may
be
the
cause
of
pain
and
disability
in
chronic
tibiofibular
syndesmosis
injury
[81,82].
They
recommended
arthroscopic
marginal
resection
alone
if
it
has
been
determined
that
there
is
no
rupture
of
the
medial
deltoid
ligament
and,
thus,
no
effect
on
the
contact
surface
and
maximal
pressure
of
the
ankle
joint.
Poor
functional
outcome
from
residual
instability
of
the
distal
tibiofibular
joint
may
occur
after
lateral
ligament
reconstruction
and
anatomical
reconstruction
of
syndesmo-
sis
will
be
needed
to
restore
syndesmosis
stability.
Several
studies
have
shown
that
chronic
lateral
ankle
instability
is
often
associated
with
chondral
lesions
in
the
ankle
[73—75,90].
It
is
clear
that
high
contact
pressure
and
shear
stress
adjacent
to
cartilage
defects
may
interfere
with
hyaline
cartilage
function
in
adjacent
areas
of
normal
car-
tilage
[91,92].
Such
a
deleterious
effect
may
explain
the
worse
clinical
outcome
with
osteochondral
lesions
in
spite
Chronic
ankle
instability:
current-concepts
S415
Figure
1
Treatment
algorithm
of
an
ossicle
of
the
lateral
malleoli
in
patients
with
chronic
ankle
instability.
of
a
successful
ligament
reconstruction.
Few
investigators
have
reported
on
the
differences
in
the
clinical
outcomes
of
arthroscopic
treatment
for
osteochondral
lesions
performed
on
lateral
ligament
reconstructed
ankles
versus
arthroscopy
done
in
isolated
osteochondral
lesions
in
lateral
ligament-
intact
ankles.
There
have
been
no
clear
criteria
to
help
surgeons
decide
whether
the
ligament
remnant
will
be
sufficient
for
Brostrom—type
procedures.
Judgment
of
this
has
his-
torically
been
unscientific,
merely
relying
on
the
surgeon’s
experience.
Normal
ligaments
consist
of
90%
type
1
col-
lagen,
which
is
primarily
responsible
for
the
stiffness
and
strength
of
the
ligament
[93—95].
Any
decrease
of
type
1
collagen
suggests
the
strength
of
the
ligament
is
weaker
than
the
normal.
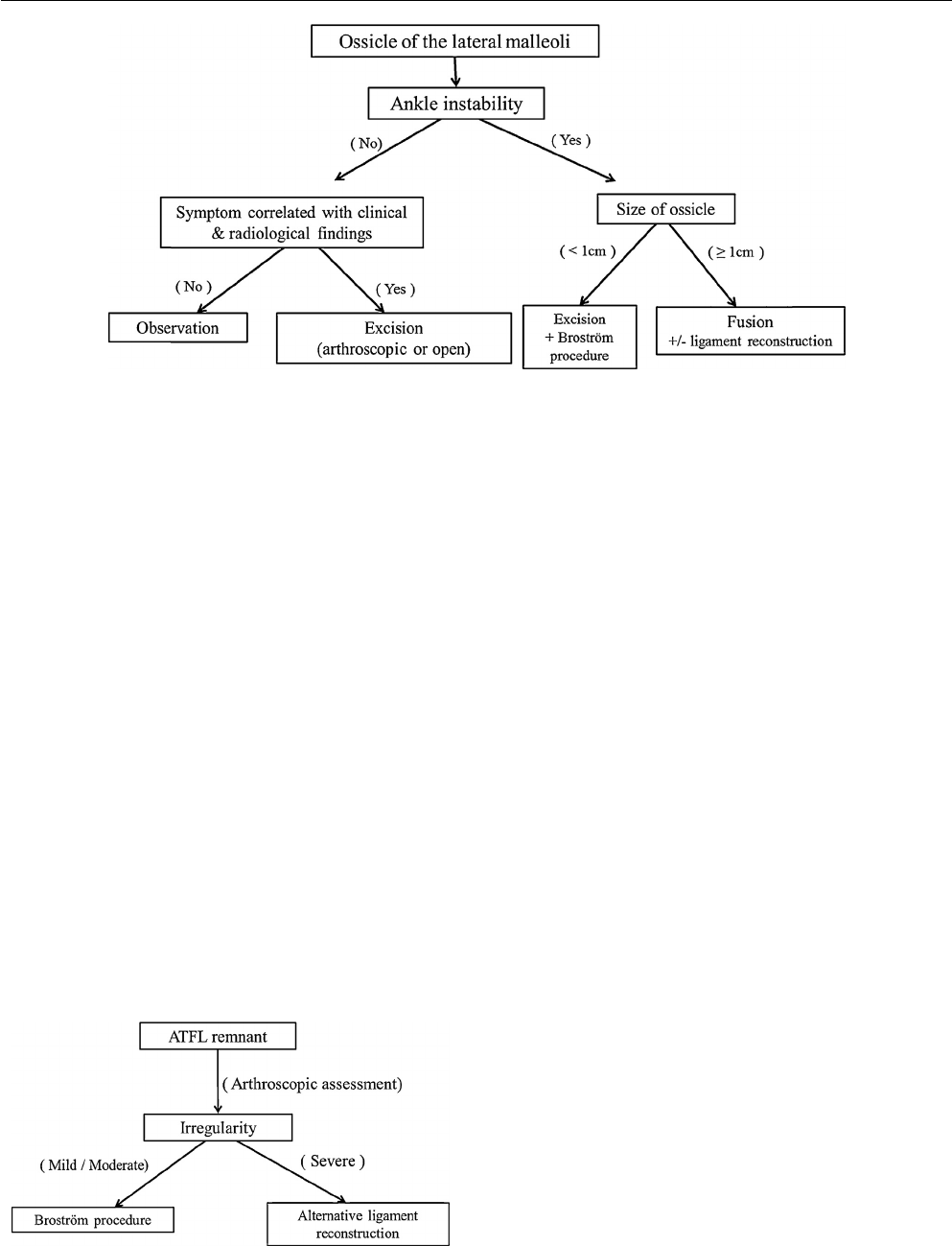
Yasui
and
Takao
compared
the
arthroscopic
and
histological
findings
of
the
ATFL
remnant,
and
clari-
fied
the
degree
of
irregularity
of
ATFL
fibre
in
arthroscopic
assessment.
If
the
ATFL
had
a
highly
irregular
appearance
in
arthroscopic
evaluation,
histology
showed
that
the
liga-
ment
fibres
consisted
of
scar
tissue
without
type
I
collagen
[96].
There
was
good
correlation
between
the
arthroscopic
assessment
of
irregularity
of
the
ATFL
remnant
and
the
his-
tological
appearance.
They
therefore
recommended
that
the
surgical
procedure
should
be
selected
according
to
the
arthroscopic
assessment
of
the
ATFL
remnant
(Fig.
2).
Figure
2
Selection
of
the
surgical
procedure
according
to
arthroscopic
evaluation
of
the
remnant
of
the
anterior
talofibu-
lar
ligament
(ATFL).
Therefore,
a
thorough
arthroscopic
assessment
is
indi-
cated
prior
to
lateral
ligament
reconstruction
in
addition
to
clinical
and
radiological
examination,
unless
a
patient
is
pain-free
with
negative
radiological
assessment.
This
assess-
ment
should
include
careful
inspection
for
any
soft
tissue
impingement,
syndesmosis
widening,
osteochondral
lesions
as
well
as
the
appearance
of
the
remnant
of
the
ATFL
in
order
to
determine
the
correct
surgical
strategy.
Surgical
indications
for
chronic
ankle
instability
Over
the
past
40
years,
the
orthopaedic
community
has
witnessed
an
evolution
in
knee
and
shoulder
surgery
for
unstable
joints
from
non-anatomic
reconstructions
utilizing
open
approaches
toward
anatomical
reconstructive
proce-
dures
performed
either
through
smaller
open
incisions
or
arthroscopically.
The
surgical
treatment
of
chronic
lateral
ankle
instability
is
currently
evolving
in
a
similar
manner.
Traditional
open
procedures
to
stabilize
the
ankle
using
ten-
don
grafts
placed
non-anatomically
can
result
in
a
stable
ankle.
However,
these
procedures,
such
as
the
Chrisman-
Snook,
Evans,
and
Watson-Jones,
may
over-constrain
both
the
ankle
and
subtalar
joints
resulting
in
limitation
of
joint
motion
and
long
term
development
of
degenerative
arthritis.
Contemporary
techniques
emphasize
anatomic
repair/reconstruction
to
restore
stability
while
attempting
to
minimize
these
complications.
For
the
purposes
of
this
article,
we
define
repair
as
the
primary
or
secondary
suturing
of
the
torn
lateral
ligaments.
A
reconstruction
refers
to
the
replacement
of
the
chroni-
cally
deficient
lateral
ligaments
with
local
tissues
or
with
autograft
or
allograft
tissue.
Local
ligament
soft
tissue
repair
techniques
The
classic
Broström
procedure
is
a
true
repair
of
the
lateral
ligaments
including
the
ATFL
and
the
CFL.
However,
it
is
rarely
performed
as
a
stand-alone
procedure.
Since
it
is
usu-
ally
augmented
with
a
transfer
of
the
extensor
retinaculum

S416
S.
Guillo
et
al.
either
as
a
proximal
advancement
(Gould
procedure)
or
as
a
pedicle
flap
of
retinaculum,
we
classify
this
procedure
as
a
repair/augmentation.
There
is
question
as
to
whether
the
extensor
retinaculum
truly
provides
mechanical
ankle
and
subtalar
stability
through
its
attachment
to
the
calcaneus
or
if
it
simply
provides
for
an
enhanced
proprioceptive
environment.
No
matter
the
method
of
effectiveness,
the
retinacular
augmentation
is
regarded
as
a
critical
element
of
this
procedure’s
success.
The
procedure
may
be
performed
the
traditional
manner
with
drill
holes
or
bone
anchors
with
attached
nonabsorbable
suture
may
be
uti-
lized.
It
is
the
consensus
of
the
ankle
instability
group
that
this
procedure
is
the
appropriate
first-line
consideration
for
patients
with
chronic
lateral
ankle
ligament
laxity
requiring
surgical
treatment.
Ligament
reconstruction
using
tendon
graft
or
transfer
Anatomic
reconstruction
with
tendon
graft
or
transfer
Traditionally
these
types
of
procedures
have
been
reserved
for
patients
who
have
failed
a
prior
Broström-Gould
repair.
However,
patients
who
may
stress
their
ankle
to
a
greater
degree
than
normal,
including
those
with
high
body
mass
index,
heavy
labor
occupation
or
sports
requirements,
or
patients
with
congenital
ligament
laxity
may
benefit
from
performing
ligament
reconstruction
as
the
primary
proce-
dure.
Although
isometry
of
the
lateral
ankle
ligaments
has
not
been
proven,
placement
of
the
tendon
grafts
at
the
ligaments’
anatomical
origin
and
insertion
should
be
per-
formed.
The
goal
is
to
achieve
good
ankle
stability
without
overconstraining
the
ankle
or
subtalar
joints.
Non-anatomic
positioning
of
the
graft
may
alter
the
biomechanics
of
the
joints
resulting
in
joint
loading
alterations
which
may
lead
to
joint
degeneration
over
time.
These
procedures
have
in
common
the
routing
of
the
transferred
tendon
graft
in
such
a
way
as
to
replicate
the
anatomic
positions
of
the
ATFL
and
CFL
origin
and
inser-
tion
sites.
They
vary
in
the
means
by
which
they
attain
that
positioning,
including
the
number
and
angle
of
tunnels
in
the
fibula
and
the
fixation
techniques
selected
in
each
bone
tunnel
location.
There
are
many
different
ways
the
liga-
ment
graft
can
be
secured
in
the
bone
including
anchors,
bone
tunnels
with
interference
screws,
and
endobutton
type
devices.
The
selected
fixation
device
should
be
secure
enough
to
maintain
appropriate
tension
on
the
recon-
struction
intra-operatively
as
well
as
support
healing
and
potentially
allow
for
early
joint
motion.
The
surgeon
may
elect
to
use
hamstring
autograft
or
allograft
depending
on
patient
requirements
and
the
resources
and
training
avail-
able
to
the
surgeon.
Non-anatomical
reconstruction
with
tendon
transfer
or
graft
Non-anatomic
reconstructions
of
the
lateral
ankle
ligaments
have
a
long
track
record
in
the
orthopaedic
literature
where
they
have
been
shown
historically
to
work
well
to
establish
a
stable
hindfoot
for
functional
activities.
Similar
to
the
non-anatomical
instability
procedures
performed
in
the
knee
and
shoulder,
the
long-term
results
in
the
ankle
reveal
an
increased
incidence
of
degenerative
changes
in
the
hindfoot.
Several
of
these
procedures
utilize
a
segment
or
the
entire
peroneal
tendon
as
either
a
graft
or
transfer.
The
peroneal
tendons
are
important
dynamic
stabilizers
of
the
hindfoot
and
harvesting
these
tendons
for
grafts
or
trans-
fers
may
result
in
long-term
weakness
and
loss
of
dynamic
stabilization
of
the
ankle
and
subtalar
joints.
Our
consensus
is
that
with
modern
fixation
techniques
and
the
known
long-
term
degenerative
sequelae
associated
with
non-anatomical
reconstruction,
these
procedures
should
be
avoided.
Arthroscopic
lateral
ligament
procedures
Numerous
articles
describe
a
high
incidence
of
intra-
articular
pathology
when
ankle
arthroscopy
is
performed
at
the
time
of
ligament
reconstruction
[21,72—74,82—84].
This
finding
has
prompted
many
surgeons
to
recommend
per-
forming
arthroscopy
in
association
with
a
lateral
ligament
reconstruction
[33,83].
In
the
last
five
years
there
have
been
several
arthro-
scopically
assisted
techniques
to
perform
lateral
ankle
ligament
reconstruction
described
in
the
orthopaedic
liter-
ature
[63,97—104].
These
techniques
show
early
promising
results
in
level
IV
studies
with
short-term
follow-up.
These
procedures
have
in
common
the
use
of
arthroscopic
tech-
niques
to
thoroughly
clean
out
the
lateral
gutter
to
expose
the
anatomic
origin
of
the
lateral
ligaments
on
the
distal
fibula
followed
by
placement
of
one
or
more
suture
anchors
into
the
fibula.
There
are
various
approaches
to
passing
the
sutures
through
the
ATFL,
CFL,
and
retinaculum
to
affect
a
repair/augmentation
procedure,
which
effectively
repli-
cates
the
Broström-Gould
procedure.
The
procedure
may
be
further
refined
as
specific
instrumentation
is
devised
to
facilitate
the
repair/augmentation.
Techniques
are
also
being
developed
to
perform
anatomic
reconstructions
using
tendon
graft
using
an
all
arthroscopic
approach.
These
procedures
are
very
technically
demanding
and
they
are
early
in
their
development.
We
believe
that
further
investigation
and
reporting
of
results
are
required
before
these
techniques
can
be
adopted
as
routine.
We
recommend
that
before
performing
arthroscopic
repair
or
reconstruction
in
the
ankle,
the
surgeon
should
be
highly
skilled
in
arthroscopy
of
the
ankle
and
should
have
gained
experience
on
the
procedures
in
cadaver
workshops
or
with
an
experienced
mentor.
The
presence
of
a
fibular
ossicle
can
complicate
per-
formance
of
a
lateral
ligament
reconstruction
[21].
Recent
studies
indicate
that
an
ossicle
of
less
than
1
cm
in
great-
est
dimension
can
be
safely
excised
and
a
local
soft
tissue
reconstruction
be
performed.
However,
if
the
ossicle
is
more
than
1
cm
in
any
dimension,
it
is
recommended
that
the
sur-
geon
either
fuse
the
ossicle
and
proceed
with
a
local
soft
tissue
procedure;
or
excise
the
ossicle
and
proceed
with
an
anatomic
tendon
graft/transfer
type
procedure.
Conclusion
Standardised
assessment
of
the
ankle
pre-operatively
and
at
follow-up
is
imperative
in
order
to
allow
compari-
son
of
outcome
from
treatment
with
various
techniques.
The
recording
of
clinical
information
along
with
standard-
ised
radiological
evaluation
as
has
been
described
above

Chronic
ankle
instability:
current-concepts
S417
following
this
consensus
group
meeting
will
help
and
the
recommendations
made
here
have
been
evaluated
and
are
evidence-based.
There
is
a
move
towards
patient-orientated
outcome
scores
which
is
why
the
ankle-specific
validated
systems
have
been
advocated
as
they
are
relatively
simple
to
use
with
less
chance
of
information
loss
and
increased
chance
patient
compliance.
The
anatomical
repairs
are
still
the
best
methods
of
treatment
in
symptomatic
chronic
insta-
bility
and
with
the
high
incidence
of
intra-articular
pathol-
ogy
it
is
recommended
that
an
arthroscopy
is
performed
at
the
time
of
surgery
unless
intra-articular
pathology
has
been
excluded
by
MRI
scan
and
there
is
no
history
of
pain.
There
is
a
move
towards
the
development
of
arthroscopic
anatomical
lateral
ligament
repair
which
may
well
take
over
from
the
open
approaches
that
are
currently
performed
in
a
similar
way
to
how
knee
and
shoulder
ligament
surgery
has
developed
over
the
past
10—15
years.
Anatomical
recon-
struction
with
tendon
grafts/augmentation
is
preferable
in
the
revision
cases
or
those
with
gross
laxity
or
insuffi-
cient
innate
tissue.
Non-anatomical
procedures
should
be
avoided
in
these
situations.
Early
reconstruction
of
acute
ligament
injuries
may
also
be
considered
in
the
athlete
as
this
improves
stability,
reducing
the
incidence
subsequent
complications
from
recurrent
sprains
without
compromising
or
delaying
return
to
sports.
Disclosure
of
interest
The
authors
declare
that
they
have
no
conflicts
of
interest
concerning
this
article.
References
[1]
Garrick
JG.
The
frequency
of
injury,
mechanism
of
injury
and
epidemiology
of
ankle
sprains.
Am
J
Sports
Med
1977;5:241—2.
[2]
Konradsen
L,
Bech
L,
Ehrenbjerg
M,
Nickelsen
T.
Seven
years
follow-up
after
ankle
inversion
trauma.
Scand
J
Med
Sci
Sports
2002;12:129—35.
[3]
Hertel
J.
Functional
anatomy,
pathomechanics,
and
patho-
physiology
of
lateral
instability.
J
Athl
Train
2002;37:364—75.
[4]
McKay
GD,
Goldie
PA,
Payne
WR,
Oakes
BW.
Ankle
injuries
in
basketball:
injury
rate
and
risk
factors.
Br
J
Sports
Med
2001;35:103—8.
[5]
Pijnenburg
ACM,
can
Dijk
CN,
Bossuyt
PMM,
Marti
RK.
Treatment
of
ruptures
of
the
lateral
ankle
ligaments:
a
meta-
analysis.
J
Bone
Joint
Surg
Am
2000;82A:761—8.
[6]
Kannus
P,
Renstrom
P.
Current
concepts
review:
treatment
for
acute
tears
of
the
lateral
ligaments
of
the
ankle-operation,
cast,
or
controlled
mobilization.
J
Bone
Joint
surg
Am
1991;73:305—12.
[7]
Pijnenburg
ACM,
Boogaard
K,
Krips
R,
Marti
RK,
Bossuyt
PMM,
van
Dijk
CN.
Operative
and
functional
treatment
of
rupture
of
the
lateral
ligament
of
the
ankle.
J
Bone
Joint
Surg
Br
2003;85B:525—30.
[8]
Kerkhoffs
GMMJ,
Handoll
HH,
de
Bie
R,
Rowe
BH,
Struijs
PAA.
Surgical
versus
conservative
treatment
for
acute
injuries
of
the
lateral
ligament
complex
of
the
ankle
in
adults.
Cochrane
Database
Syst
Rev
2007;18(2):CD000380
[Cochrane
Review].
[9]
Karlsson
J,
Sancone
M.
Management
of
acute
ligament
injuries
of
the
ankle.
Foot
Ankle
Clin
N
Am
2006;11:521—30.
[10]
Karlsson
J,
Eriksson
BI,
Swärd
L.
Early
functional
treatment
for
acute
ligament
injuries
of
the
ankle
joint.
Scand
J
Med
Sci
Sports
1996;6:341—5.
[11]
Ardevol
J,
Bolibar
I,
Belda
V,
Argilaga
S.
Treatment
of
complete
rupture
of
the
lateral
ligaments
of
the
ankle:
a
randomized
clinical
trial
comparing
cast
immobilization
with
functional
treatment.
Knee
Surg
Sports
Traumatol
Arthrosc
2002;10(6):371—7.
[12]
Kerkhoffs
GMMJ,
Struijs
PAA,
Marti
RK,
Blankevoort
L,
Assendelft
WJJ,
van
Dijk
CN.
Functional
treatments
for
acute
rupture
of
the
lateral
ankle
ligament.
Acta
Orthop
Scand
2003;74:69—77.
[13]
Guillodo
Y,
Simon
T,
Le
Goff
A,
Sarau
A.
Interest
of
rehabili-
tation
in
healing
and
preventing
recurrence
of
ankle
sprains.
Ann
Phys
Rehabil
Med
2013;56(7-8):503—14.
[14]
Bosien
WR,
Staples
OS,
Russel
SW.
Residual
disability
following
acute
ankle
sprains.
J
Bone
Joint
Surg
Am
1955;37:1237—43.
[15]
Hiller
CE,
Kilbreath
SL,
Refshauge
KM.
Chronic
ankle
instabil-
ity:
evolution
of
the
model.
J
Athl
Train
2011;46:133—41.
[16]
van
den
Bekerom
MP,
Kerkhoffs
GM,
McCollum
GA,
Calder
JD,
van
Dijk
CN.
Management
of
acute
lateral
ankle
ligament
injury
in
the
athlete.
Knee
Surg
Sports
Traumatol
Arthrosc
2013;21(6):1390—5.
[17]
Bonnel
F,
Toullec
E,
Mabit
C,
Tourné
Y.
Chronic
ankle
instability:
biomechanics
and
pathomechanics
of
ligaments
injury
and
associated
lesions.
Orthop
Traumatol
Surg
Res
2010;96:424—32.
[18]
Coughlin
MJ,
Mann
RA,
Saltzman
CL.
Surgery
of
the
foot
and
ankle.
Philadelphia,
PA:
Mosby
Elsevier;
2007.
p.
1467—8.
[19]
Sammarco
GJ,
Burstein
AH,
Frankel
VH.
Biomechanics
of
the
ankle:
a
kinematic
study.
Orthop
Clin
North
Am
1973;4:75—96.
[20]
Scranton
PE,
McDermott
JE,
Rogers
JV.
The
relation-
ship
between
chronic
ankle
instability
and
variations
in
mortise
anatomy
and
impingement
spurs.
Foot
Ankle
Int
2000;21:657—64.
[21]
Choi
WJ,
Lee
JW,
Han
SH,
Kim
BS,
Lee
SK.
Chronic
lat-
eral
ankle
instability.
The
effect
of
intra-articular
lesions
on
clinical
outcome.
Am
J
Sports
Med
2008;36:2167—72,
http://dx.doi.org/10.1177/0363546508319050.
[22]
Inman
VT.
The
joints
of
the
ankle.
Baltimore,
MD:
Williams
&
Wilkins;
1976.
[23]
Van
Bergeyk
AB,
et
al.
CT
analysis
of
hindfoot
align-
ment
in
chronic
lateral
ankle
instability.
Foot
Ankle
Int
2002;23:37—42.
[24]
Brennan
SA,
Kiernan
C,
Maleki
F,
Bergin
D,
Kearns
SR.
Talonav-
icular
synostosis
with
lateral
ankle
instability
—
a
case
report
and
review
of
the
literature.
Foot
Ankle
Surg
2012;18:e34—6.
[25]
Kjaersgaard-Andersen
P,
Wethelund
J,
Helmig
P,
et
al.
The
sta-
bilizing
effect
of
the
ligamentous
structures
in
the
sinus
and
canalis
tarsi
on
movements
in
the
hindfoot:
an
experimental
study.
Am
J
Sports
Med
1988;16:512—6.
[26]
Seebauer
CJ,
Bail
HJ,
Rump
JC,
Hamm
B,
Walter
T,
Teich-
gräber
UK.
Ankle
laxity:
stress
investigation
under
MRI
control.
AJR
2013;201:496—504.
[27]
Tochigi
Y,
Amendola
A,
Rudert
MJ,
et
al.
The
role
of
the
interosseous
talocalcaneal
ligament
in
subtalar
joint
stability.
Foot
Ankle
Int
2004;25:588—96.
[28]
Golano
P,
Vega
J,
de
Leeuw
PAJ,
Malagelada
F,
Manzanares
MC,
Götzens
V,
et
al.
Anatomy
of
the
ankle
ligaments:
a
pictorial
essay.
Knee
Surg
Sports
Traumatol
Arthrosc
2010;18:557—69.
[29]
Wiersma
PH,
Griffioen
FMM.
Variations
of
three
lateral
liga-
ments
of
the
ankle.
A
descriptive
anatomical
study.
The
Foot
1992;2:218—24.
[30]
Hubbard-Turner.
Relationship
between
mechanical
ankle
joint
laxity
and
subjective
function.
Foot
Ankle
Int
2012;33:852—6.
[31]
Hatch
GF,
Labib
SA,
Hutton
W.
Role
of
the
peroneal
tendons
and
superior
peroneal
retinaculum
as
static
stabilizers
of
the
ankle.
J
Surg
Orthop
Adv
2007;16:187—91.

S418
S.
Guillo
et
al.
[32]
Hiller
CE,
Nightingale
EJ,
Lin
CW,
Coughlan
GF,
Caulfield
B,
Delahunt
E.
Characteristics
of
people
with
recurrent
ankle
sprains:
a
systematic
review
with
meta-analysis.
Br
J
Sports
Med
2011;45:660—72.
[33]
Kerr
H-L,
Bayley
E,
Jackson
R,
Kothari
P.
The
role
of
arthroscopy
in
the
treatment
of
functional
insta-
bility
of
the
ankle
Foot
Ankle
Surg
2013;
2013,
http:/dx.doi.org/10.1016/j.fas.2013.06.008.
[34]
Bauer
T,
Hardy
P.
Entorse
de
la
cheville.
EMC
(Elsevier
Masson
SAS,
Paris),
Appareil
locomoteur,
14-089-A-10,
2011.
[35]
Tourné
Y,
Besse
JL,
Mabit
C,
Sofcot.
Chronic
ankle
insta-
bility.
Which
tests
to
assess
the
lesions?
Which
therapeutic
options?
Orthop
Traumatol
Surg
Res
2010;96(4):433—46,
http://dx.doi.org/10.1016/j.otsr.2010.04.005.
[36]
Friden
TZR,
Lindstrand
A,
et
al.
A
stabilometric
technique
for
evaluation
of
lower
limb
instabilities.
Am
J
Sports
Med
1989;17:118—22.
[37]
Lentell
GKL,
Walters
MR.
The
relationship
between
muscle
function
and
ankle
instability.
J
Orthop
Sports
Phys
Ther
1990;11:605—11.
[38]
Patel
AADD,
Albert
T.
The
36-item
short
form.
J
Am
Acad
Orthop
Surg
2007;15:126—34.
[39]
Group
E.
EuroQol-
a
new
facility
for
the
measurement
of
heath-related
quality
of
life.
The
EuroQol
Group.
Health
Pol-
icy
1990;16(3):199—208.
[40]
SooHoo
NFSM,
Fleming
LL.
Evaluation
of
the
AOFAS
clinical
rating
system.
Foot
Ankle
Int
2003;24:50—5.
[41]
Roos
EBS,
Karlsson.
Validation
of
the
foot
and
ankle
out-
come
score
for
ankle
ligament
reconstruction.
Foot
Ankle
Int
2001;22(10):788—94.
[42]
Tegner
YLJ.
Rating
systems
in
the
evaluation
of
knee
ligament
injuries.
Clin
Orth
Rel
Res
1985;196:43—9.
[43]
Halasi
TKA,
Tallay
A,
Berkes
I.
Development
of
a
new
activity
score
for
the
evaluation
of
ankle
instability.
Am
J
Sports
Med
2004;32(4):899—908.
[44]
Karlsson
JPL.
Evaluation
of
ankle
joint
function:
the
use
of
a
scoring
scale.
The
Foot
1991;1:15—9.
[45]
Kaikkonen
ALH,
Kannus
P,
Jarvinen
M.
Long-term
functional
outcome
after
surgery
of
chronic
ankle
instability:
a
5
year
follow-up
of
the
modified
Evans
procedure.
Scand
J
Med
Sci
Sports
1999;9:239—44.
[46]
Rozzi
SLLS,
Sterner
R,
Kuligowski
L.
Balance
training
for
per-
sons
with
functionally
unstable
ankles.
J
Orthop
Sports
Phys
Ther
1999;29:478—86.
[47]
Hale
SAHJ.
Reliability
and
sensitivity
of
the
foot
and
ankle
disability
index
in
subjects
with
chronic
ankle
instability.
J
Ath
Train
2005;40(1):35—40.
[48]
Williams
GMJ,
DeBerardino
T,
Arciero
R,
Taylor
D.
Evalu-
ation
of
the
sports
ankle
rating
system
in
young
athletic
indivduals
with
acute
lateral
ankle
sprains.
Foot
Ankle
Int
2003;24(3):274—82.
[49]
Martin
RLIJ,
Burdett
RG,
Conti
SF,
Van
Swearingen
JM.
Evi-
dence
of
validity
for
the
foot
and
ankle
ability
measure.
Foot
Ankle
Int
2005;26:968—83.
[50]
Docherty
CAB,
Hurwitz
S.
Development
and
reliability
of
the
ankle
instability
index.
J
Ath
Train
2006;41:154—8.
[51]
Hiller
CERK,
Bundy
AC,
Herbert
RD,
Kilbreath
SL.
The
Cumber-
land
ankle
instability
tool:
a
report
of
validity
and
reliability
testing.
Arch
Phys
Med
Rehab
2006;87:1235—41.
[52]
Hubbard
TKL,
Denegar
C,
Hertel
J.
Correlations
among
multip
measures
of
functional
and
mechanical
instability
in
subjects
with
chronic
ankle
instability.
J
Ath
Train
2007;42(3):361—6.
[53]
Eechaute
CVP,
Duquet
W.
The
chronic
ankle
instability
scale:
clinimetric
properties
of
a
mulit-dimensional,
patient-
assessed
instrument.
Phys
Ther
Sport
2008;9:57—66.
[54]
Simon
JDM,
Docherty
C.
Development
of
the
identi-
fication
of
functional
ankle
instability.
Foot
Ankle
Int
2012;33(9):755—63.
[55]
Buchanan
ASDC,
Schrader
J.
Functional
performance
test-
ing
in
participants
with
functional
ankle
instability
and
in
a
healthy
control
group.
J
Ath
Train
2008;43:342—6.
[56]
Gribble
PAHJ,
Plisky
P.
Using
the
star
excursion
balance
test
to
assess
dynamic
postural-control
deficits
and
outcomes
in
lower
extremity
injury:
a
literature
and
systematic
review.
J
Ath
Train
2012;24(3):339—57.
[57]
Docherty
CLVMT,
Shultz
S.
Postural
control
deficits
in
par-
ticipants
with
functional
ankle
instability
as
measured
by
the
balance
error
scoring
system.
Clin
J
Sports
Med
2006;16:203—8.
[58]
Isakov
EMJ.
Is
balance
impaired
by
recurrent
sprained
ankle?
Br
J
Sports
Med
1997;31:65—7.
[59]
Hoch
MCMP.
Peroneal
reaction
time
following
ankle
sprain:
a
systematic
review
and
meta-analysis.
Med
Sci
Sport
Exerc
2013
[epub
ahead
of
print].
[60]
Tourné
YMC,
Moroney
P,
Chaussard
C,
Saragaglia
D.
Long-term
follow-up
of
lateral
reconstruction
and
extensor
retinac-
ulum
flap
for
chronic
ankle
instability.
Foot
Ankle
Int
2012;33(12):1079—86.
[61]
Youn
HKY,
Lee
J,
Choi
WJ,
Lee
JW.
Percutaneous
lateral
lig-
ament
reconstruction
with
allograft
for
chronic
lateral
ankle
instability.
Foot
Ankle
Int
2012;33(2):99—104.
[62]
Miller
ARS,
Ahmad
J.
Near-anatomic
allograft
tenode-
sis
of
chronic
lateral
ankle
instability.
Foot
Ankle
Int
2013;34(11):1501—7.
[63]
Vega
J,
Golano
P,
Pellegrino
A,
Rabat
E,
Pena
F.
All
insaide
arthroscopic
lateral
collateral
ligament
repair
for
ankle
insta-
bility
with
a
knotless
suture
anchor
technique.
Foot
Ankle
Int
2013,
http://dx.doi.org/10.1177/1071100713502322.
[64]
Donahue
MSJ,
Docherty
C.
Critical
review
of
self-
reported
functional
ankle
instability.
Foot
Ankle
Int
2011;32(12):1140—6.
[65]
Eechaute
CVP,
Van
Aerschott
L,
Asman
S,
Duquet
W.
The
clinimetric
properties
of
patient-assessed
instruments
for
measuring
chronic
ankle
instability:
a
systematic
review.
BMC
Musculoskeletal
Disorders
2007;8(6):1—11.
[66]
Burn
ABY,
Chopra
S,
Winkler
M,
Crevoisier
X.
Critical
evalua-
tion
of
outcome
scales
assessment
of
lateral
ankle
ligament
reconstruction.
Foot
Ankle
Int
2013;34(7):995—1005.
[67]
Eyring
EJ,
Guthrie
WD.
A
surgical
approach
to
the
problem
of
severe
lateral
instability
at
the
ankle.
Clin
Orthop
Relat
Res
1986;206:185—91.
[68]
Karlsson
J,
Bergsten
T,
Lansinger
O,
Peterson
L.
Reconstruc-
tion
of
the
lateral
ligaments
of
the
ankle
for
chronic
lateral
instability.
J
Bone
Joint
Surg
Am
1988;70:581—7.
[69]
Rechtine
GR,
McCarroll
JR,
Webster
DA.
Reconstruction
for
chronic
lateral
instability
of
the
ankle:
a
review
of
twenty-
eight
surgical
patients.
Orthopedics
1982;5:44—50.
[70]
Sammarco
GJ,
DiRaimondo
CV.
Surgical
treatment
of
lateral
ankle
instability
syndrome.
Am
J
Sports
Med
1988;16:501—11.
[71]
Taga
I,
Shino
K,
Inoue
M.
Articular
cartilage
lesions
in
ankles
with
lateral
ligament
injury:
an
arthroscopic
study.
Am
J
Sports
Med
1993;21:120—7.
[72]
DiGiovanni
BF,
Fraga
CJ,
Cohen
BE.
Associated
injuries
found
in
chronic
lateral
ankle
instability.
Foot
Ankle
Int
2000;21:809—15.
[73]
Hintermann
B,
Boss
A,
Schafer
D.
Arthroscopic
findings
in
patients
with
chronic
ankle
instability.
Am
J
Sports
Med
2002;30:402—29.
[74]
Komenda
AG,
Ferkel
RD.
Arthroscopic
findings
associated
with
the
unstable
ankle.
Foot
Ankle
Int
1999;20:708—13.
[75]
Okuda
R,
Kinoshita
M,
Morikawa
J,
Yasuda
T,
Abe
M.
Arthro-
scopic
findings
in
chronic
lateral
ankle
instability:
do
focal
chondral
lesions
influence
the
results
of
ligament
reconstruc-
tion?
Am
J
Sports
Med
2005;33:35—42.
[76]
Urguden
M,
Soyuncu
Y,
Ozdemir
H,
et
al.
Arthroscopic
treatment
of
anterolateral
soft
tissue
impingement
of
the
Chronic
ankle
instability:
current-concepts
S419
ankle:
evaluation
of
factors
affecting
outcome.
Arthroscopy
2005;21:317—22.
[77]
Deberardino
TM,
Arciero
RA,
Taylor
DC.
Arthroscopic
treat-
ment
of
soft
tissue
impingement
of
the
ankle
in
athletes.
Arthroscopy
1997;13:492—8.
[78]
Ferkel
RD,
Karzel,
Del
Pizzo
W.
Arthroscopic
treatment
of
anterolateral
impingement
of
the
ankle.
Am
J
Sports
Med
1991;19:440—6.
[79]
Lee
JW,
Suh
JS,
Huh
YM,
Moon
ES,
Kim
SJ.
Soft
tissue
impinge-
ment
syndrome
of
the
ankle:
diagnostic
efficacy
of
MRI
and
clinical
results
after
arthroscopic
treatment.
Foot
Ankle
Int
2004;25:896—902.
[80]
Kim
BS,
Choi
WJ,
Kim
YS,
Lee
JW.
The
effect
of
an
ossicle
of
the
lateral
malleolus
on
ligament
reconstruction
of
chronic
lateral
ankle
instability.
Foot
Ankle
Int
2010;31:191—6.
[81]
Han
SH,
Lee
JW,
Kim
SJ,
Suh
JS,
Choi
YR.
Chronic
tibiofibu-
lar
syndesmosis
injury:
the
diagnostic
efficiency
of
magnetic
resonance
imaging
and
comparative
analysis
of
operative
treatment.
Foot
Ankle
Int
2007;28:336—42.
[82]
Ogilvie-Harris
D,
Reed
S.
Disruption
of
the
ankle
syndesmosis:
diagnosis
and
treatment
by
arthroscopic
surgery.
Arthroscopy
1994;10:561—8.
[83]
Takao
M,
Ochi
M,
Oae
K,
Naito
K,
Uchio
Y.
Diagnosis
of
a
tear
of
the
tibiofibular
syndesmosis.
The
role
of
arthroscopy
of
the
ankle.
J
Bone
Joint
Surg
Br
2003;85(3):324—9.
[84]
Van
den
Bekerom
MP,
Haverkamp
D,
Kerkhoffs
GM,
van
Dijk
CN.
Syndesmotic
stabilization
in
pronation
external
rotation
ankle
fractures.
Clin
Orthop
Relat
Res
2010;468(4):991—5.
[85]
Close
JR.
Some
applications
of
the
functional
anatomy
of
the
ankle
joint.
J
Bone
Joint
Surg
Am
1956;38:761—81.
[86]
Teramoto
A,
Kura
H,
Uchiyama
E,
Suzuki
D,
Yamashita
T.
Three-dimensional
analysis
of
ankle
instability
after
tibiofibu-
lar
syndesmosis
injuries.
Am
J
Sports
Med
2008;36:348—52.
[87]
Taylor
DC,
Englehardt
DL,
Bassett
FH.
III.
Syndesmosis
sprains
of
the
ankle:
the
influence
of
heterotopic
ossification.
Am
J
Sports
Med
1992;20:146—50.
[88]
Burn
W,
Prakash
K,
Adeaar
R.
Tibiotalar
joint
dynamics:
indi-
cations
for
the
syndesmotic
screw
—
a
cadaver
study.
Foot
Ankle
1993;14:153—8.
[89]
Clanton
TO,
Paul
P.
Syndesmosis
injuries
in
athletes.
Foot
Ankle
Clin
2002;7:529—49.
[90]
Van
Dijk
CN,
Bossuyt
PMM,
Marti
RK.
Medial
ankle
pain
after
lateral
ligament
rupture.
J
Bone
Joint
Surg
Br
1996;78:562—7.
[91]
Smith
RL,
Trindade
MCD,
Ikenoue
T,
et
al.
Effects
of
shear
stress
on
articular
chondrocyte
metabolism.
Biorheology
2000;37:95—107.
[92]
Wilson
W,
van
Rietbergen
B,
van
Donkelaar
CC,
Huiskes
R.
Pathways
of
load-induced
cartilage
damage
causing
carti-
lage
degeneration
in
the
knee
after
meniscectomy.
J
Biomech
2003;36:845—51.
[93]
Frank
C,
Shrive
N,
Hiraoka
H,
et
al.
Optimisation
of
the
biology
of
soft
tissue
repair.
J
Sci
Med
Sport
1999;2:190—210.
[94]
Frank
C,
Amiel
D,
Woo
SL,
Akeson
W.
Normal
ligament
properties
and
ligament
healing.
Clin
Orthop
Relat
Res
1985;196:15—25.
[95]
Girard
P,
Anderson
RB,
Davis
WH,
Isear
JA,
Kiebzak
GM.
Clin-
ical
evaluation
of
the
modified
Brostrom-Evans
procedure
to
restore
ankle
stability.
Foot
Ankle
Int
1999;20:246—52.
[96]
Yasui
Y,
Takao
M.
Comparison
of
Arthroscopic
and
Histologi-
cal
Evaluation
on
the
Injured
Anterior
Talofibular
Ligament.
Chicago,
USA:
The
American
Academy
of
Orthopaedic
Sur-
geons
(AAOS)
2013
annual
meeting;
2013.
[97]
Maiotti
M,
Massoni
C,
Tarantino
U.
The
use
of
arthroscopic
thermal
shrinkage
to
treat
chronic
lateral
ankle
instability
in
young
athletes.
Arthroscopy
2005;21(6):751—7.
[98]
Lui
TH.
Arthroscopic-assisted
lateral
ligamentous
reconstruc-
tion
in
combined
ankle
and
subtalar
instability.
Arthroscopy
2007;23(5):554e1—5.
[99]
Corte-Real
NM,
Moreira
RM.
Arthroscopic
repair
of
lateral
ankle
instability.
Foot
Ankle
Int
2009;30:213—7.
[100]
Kim
ES,
Lee
KT,
Park
JS,
et
al.
Arthroscopic
anterior
talofibu-
lar
ligament
repair
for
chronic
ankle
instability
with
a
suture
anchor
technique.
Orthopedics
2011;34(4):1—5.
[101]
Nery
C,
Raduan
F,
Del
Buono
A,
et
al.
Arthroscopic-assisted
Broström-Gould
for
chronic
ankle
instability:
a
long-term
follow-up.
Am
J
Sports
Med
2011;39(11):2381—8.
[102]
Acevedo
JI,
Mangone
PG.
Arthroscopic
lateral
ankle
ligament
reconstruction.
Tech
Foot&Ankle
2011;10:111—6.
[103]
Giza
E,
Shin
EC,
Wong
SE,
Acevedo
JI,
Mangone
PG,
Olson
K,
Anderson
MJ.
Arthroscopic
suture
anchor
repair
of
the
lateral
ligament
ankle
complex:
a
cadaveric
study.
Am
J
Sports
Med
2013,
http://dx.doi.org/10.1177/0363546513500639.
[104]
Cottom
JM,
Rigby
RB.
The
‘‘all-inside’’
arthroscopic
Broström
procedure:
a
prospective
study
of
40
consecutive
patients.
J
Foot
Ankle
Surg
2013;52(5):568—74,
http://dx.doi.org/10.1053/j.jfas.2013.02.022.