Improving Patient Safety Through Provider Communication Strategy Enhancements ://www.ahrq.gov/s/pub/advances2/vol3/advances Dingley_14 Advances Dingley 14
User Manual: Pdf ://www.ahrq.gov/s/pub/advances2/vol3/advances-dingley_14 Ultrasound
Open the PDF directly: View PDF ![]() .
.
Page Count: 18
Improving Patient Safety Through Provider
Communication Strategy Enhancements
Catherine Dingley RN, PhD, FNP; Kay Daugherty RN, PhD; Mary K. Derieg RN, DNP;
Rebecca Persing, RN, DNP
Abstract
The purpose of this study was to develop, implement, and evaluate a comprehensive provider/
team communication strategy, resulting in a toolkit generalizable to other settings of care. The
specific aims included implementation of a structured communication tool; a standardized
escalation process; daily multidisciplinary patient-centered rounds using a daily goals sheet; and
team huddles. The study setting was the 477-bed medical center of the Denver Health and
Hospital Authority, an integrated, urban safety-net system. Utilizing a pre-test/post-test design,
baseline and post-intervention data were collected on pilot units (medical intensive care unit,
acute care unit, and inpatient behavioral health units). Analysis of 495 communication events
after toolkit implementation revealed decreased time to treatment, increased nurse satisfaction
with communication, and higher rates of resolution of patient issues post-intervention. The
resultant toolkit provides health care organizations with the means to implement teamwork and
communication strategies in their own settings.
Introduction
Current research indicates that ineffective communication among health care professionals is one
of the leading causes of medical errors and patient harm.1, 2, 3 A review of reports from the Joint
Commission reveals that communication failures were implicated at the root of over 70 percent
of sentinel events.4 When asked to select contributing factors to patient care errors, nurses cited
communication issues with physicians as one of the two most highly contributing factors,
according to the National Council of State Boards of Nursing reports.5 In a study of 2000 health
care professionals, the Institute for Safe Medication Practices (ISMP) found intimidation as a
root cause of medication error; half the respondents reported feeling pressured into giving a
medication, for which they had questioned the safety but felt intimidated and unable to
effectively communicate their concerns.6
The growing body of literature on safety and error prevention reveals that ineffective or
insufficient communication among team members is a significant contributing factor to adverse
events. In the acute care setting, communication failures lead to increases in patient harm, length
of stay, and resource use, as well as more intense caregiver dissatisfaction and more rapid
turnover.7, 8, 9, 10, 11, 12 In multisite studies of intensive care units (ICUs), poor collaborative
communication among nurses and physicians, among other specific factors, contributed to as
much as a 1.8-fold increase in patient risk-adjusted mortality and length of stay.
13, 14, 15
1
Analysis of 421 communication events in the operating room found communication failures in
approximately 30 percent of team exchanges; one-third of these jeopardized patient safety by
increasing cognitive load, interrupting routine, and increasing tension in the OR setting.2 The
researchers found that communication problems were relatively straightforward and fell into four
categories: (1) communications that were too late to be effective, (2) failure to communicate with
all the relevant individuals on the team, (3) content that was not consistently complete and
accurate, and (4) communications whose purposes were not achieved—i.e., issues were left
unresolved until the point of urgency.2
Examining the outcomes of communication, other researchers have found associations between
better nurse-physician communication and collaboration and more positive patient outcomes, i.e.,
lower mortality, higher satisfaction, and lower readmission rates.16, 17, 18
Effective communication among health care professionals is challenging due to a number of
interrelated dynamics:
• Health care is complex and unpredictable, with professionals from a variety of disciplines
involved in providing care at various times throughout the day, often dispersed over several
locations, creating spatial gaps with limited opportunities for regular synchronous
interaction.7
• Care providers often have their own disciplinary view of what the patient needs, with each
provider prioritizing the activities in which he or she acts independently.7
• Health care facilities have historically had a hierarchical organizational structure, with
significant power distances between physicians and other health care professionals. This
frequently leads to a culture of inhibition and restraint in communication, rather than a sense
of open, safe communication (psychological safety).
• Differences in education and training among professions often result in different
communication styles and methods that further complicate the scenario and render
communications ineffective.
• Although teamwork and effective communication are crucial for safe patient care, the
educational curricula for most health care professions focus primarily on individual technical
skills, neglecting teamwork and communication skills.
A cultural barrier can be found in many organizations that can be traced to the belief that quality
of care and error-free performance result from professional training and effort, ignoring the
inherent limitations described in human factors science.3 In fact, human factors such as cognitive
overload; the effects of stress, fatigue, distractions and interruptions; poor interpersonal
communications; imperfect information processing; and flawed decisionmaking are all known to
contribute to errors in health care and other complex environments, such as aviation.3, 6 Failure to
recognize and understand these issues can lead to a culture of unrealistic expectations and blame,
diverting efforts away from effective team-based error management strategies.
Intervention-focused research that seeks to improve collaborative communication is lacking.19
As a means of improving patient safety and outcomes, interventions should focus on integrating
the critical attributes of collaboration, including open communication, shared responsibilities for
planning and problemsolving, shared decisionmaking, and coordination.19, 20 Additionally,
2
translating the theories and practices of teamwork and communication from aviation to health
care is gaining support from a number of researchers citing common elements in both industries.
Training efforts—such as crew resource management (CRM) and a focus on the key concepts of
leadership, briefings, monitoring, cross-checking, decisionmaking, and review and modification
of plans—have enhanced communication and teamwork, thus providing a mechanism for
increased safety and a change in crew attitudes and behavior.21
Drawing on current research, the purpose of this study was to develop, implement, and evaluate a
comprehensive team communication strategy, resulting in a toolkit that can be generalized to
other settings of care. The specific aims included:
1. Implementation of a standardized communication tool, the SBAR (see description on next
page), as a guide for communicating changes in patient status.
2. Implementation of an escalation process tool to facilitate timely communication.
3. Daily multidisciplinary patient-centered rounds using a daily goals sheet.
4. Team huddles during each shift.
Methods
Utilizing a pre-test/post-test design, this study incorporated baseline data collection and
implementation of team communication interventions, followed by data collection and analysis
over a 24-month period. The goal of developing a user-friendly toolkit was accomplished as
feedback and findings from this study were revised and adapted.
Study Setting
Denver Health Medical Center, an urban public safety-net hospital, provided the site for this
study, with specific focus on three care settings utilized for pilot testing. These settings were
selected because they each provided a different type of unit organization and staff.
• Phase 1 focused on two settings: the Medical Intensive Care Unit (MICU) and the Acute
Care Unit (ACU). The ACU was selected because it had a very diverse patient population,
with multiple physician teams and services assigned to the unit at a given time. The MICU
was selected because it was a closed unit with fewer physician teams and one primary service
with more accessibility to physician consultation.
• Phase 2 focused on behavioral health units: an Adult Psychiatric Unit, an Adolescent
Psychiatric Unit, and an Acute Crisis Service (psych ED). The behavioral health units were
characterized by a unique patient population and unit milieu, with a more consistent
physician group.
Since post-intervention data collection has been completed on the Phase 1 units, this report is
focused on specific outcome measures based on Phase 1 results.
3

Interventions
The following communication strategies were included in the toolkit interventions and can be
accessed on the Denver Health Medical Center Web site (www.safecoms.org) for further detail:
Situational briefing guide: SBAR. A standardized communication format, the SBAR, was
utilized as a situational briefing guide for staff and provider communication regarding changes in
patient status or needs for nonemergent events, related issues, or for events on the unit, in the lab,
or within the health care team. SBAR is an acronym for:
• Situation: What is going on with the patient?
• Background: What is the clinical background or context?
• Assessment: What do I think the problem is?
• Recommendation: What do I think needs to be done for the patient?
Since SBAR provides a standardized means for communicating in patient care situations, it is
effective in bridging differences in communication styles and helps to get all team members in
the “same movie.”3 SBAR provides a common and predictable structure for communication, can
be used in any clinical domain, and has been applied in obstetrics, rapid response teams,
ambulatory care, ICUs, and other areas. SBAR also presents guidelines for organizing relevant
information when preparing to contact another team member, as well as the framework for
presenting the information, appropriate assessments, and recommendations.6 SBAR has been
utilized in Institute for Healthcare Improvement (IHI) collaboratives and has been endorsed by
the American College of Healthcare Executives and the American Organization of Nurse
Executives.
One important aspect of SBAR is its inherent recognition of nurses’ and other care providers’
expertise so that they are encouraged to assertively make recommendations to physicians, thus
facilitating a nonhierarchical structure. In a recent study of nursing home transfers from acute
care settings to skilled nursing facilities (SNF), SBAR implementation helped avert breakdowns
in communication that had previously resulted in patients arriving with incomplete information
and the need for important medications that were not available.3
In the current study, SBAR was used initially to organize and present information to
communicate changes in patient status. It was also found to be useful in preparing information
and for an anticipated difficult conversation with another staff member or provider. As
implementation of SBAR expanded across units, a number of various uses were established. It
was utilized to provide “kudos” for staff accomplishments, as a framework for reporting on
patients, as a means of structuring assessments, and to structure succinct e-mail communications.
A diagram of the SBAR process form and guidelines for use are presented in Table 1.
Team huddles. Provider and staff team huddles were implemented on the pilot units as a way to
communicate and share information concurrently with the team early in the shift. A team huddle
was defined as a quick meeting of a functional group to set the day/shift in motion via
commentary with key personnel. Huddles are microsystem meetings with a specific focus, based
on the function of a particular unit and team. Although both joint rounding and huddles aim to
4
Table 1. SBAR Practice Sheet
improve team
communication and
patient safety and care,
huddles differ in that they
have a primarily
operational focus. They
are interdisciplinary and
include operational and
care personnel.
S • B • A • R
Before you call, be prepared! Be clear, concise, focus on the
problem & only report what is relevant to the current situation!
Be sure you do the following:
• Assess the patient. • Determine the appropriate
person to call.
• Have the medical record
available when you call.
• Review appropriate parts of
the medical record (eg, flow
sheet, MAR, physician
notes/orders, labs).
• Use the following form to
organize your conversation.
Situation: 5-10 second “punch line” – What is happening now?
What are the chief complaints or acute changes?
This is __________. I’m calling about _______________________
______________________________________________________
______________________________________________________
Background: What factors led up to this event? Pertinent history
(eg, admitting diagnosis) & objective data (eg, vital signs, labs) that
support how patient got here.
The patient has__________________________________________
______________________________________________________
______________________________________________________
Assessment: What do you see? What do you think is going on? A
diagnosis is not necessary; include the severity of the problem.
I think the problem is______________________________________
_______________________________________________________
_______________________________________________________
Recommendation: What action do you propose? State what the
patient needs (get a time frame).
I request that you_________________________________________
_______________________________________________________
_______________________________________________________
Current literature
indicates daily team
huddles result in fewer
interruptions during the
rest of the day and
immediate clarification of
issues.22 Team members
know there is a fixed time
when they will have
everyone else’s attention.
Daily briefings (similar to
those used in huddles)
have been shown to be
useful for a team to
quickly assess changes in
clinical workload,
identify relevant issues of
the day, and provide a
means to prioritize.3 In a
very short time, members
of a care team can all be
“on the same page” for
the day and be ensured
that relevant issues are
being addressed.3
Guidelines for huddles
include the following:
• Set a standard time each day.
• Use a consistent location.
• Stand up, don’t sit down.
• Make attendance mandatory.
• Limit duration to 15 minutes.
• Begin and end on time.
5
• Attempt to have the same structure every day.
• Keep the agenda to limited items.
Initial pilot testing of huddles occurred within two departments: radiology and laboratory
services. Huddle participants included all departmental and unit level staff members present at
the time. They typically occurred at the beginning of the day or shift, lasted approximately 9 to
20 minutes, and were led by a shift supervisor or department head.
Huddles were utilized to review pertinent issues of the day (e.g., inoperable equipment or
rooms), to go over the day’s schedule, and to plan for possible variations/problems. Information
sharing included relevant system-level messages of the day, information from recent
management meetings, and departmental issues or problems. Brief discussion of specific issues,
such as errors (e.g., mismarked films) was integrated with a review of the process, system issues,
and reminders on how to avoid the errors. On nursing units, huddles typically were led by the
nurse manager, charge nurse, or clinical nurse educator. Interviews revealed several benefits of
huddles, including:
• Preparing staff for the shift/day.
• Face-to-face communication.
• Immediate response to questions.
• Streamlined resolution of issues or concerns.
• Timely response to issues or concerns.
• Efficient dissemination of information.
• Improvement in teamwork and effective communication.
• Staff involvement in decisionmaking.
In some instances, if a huddle had been skipped for a particular shift/day, staff members took
notice and inquired about it. Huddles also served to enhance teamwork and the staff’s sense of
cohesion.
Multidisciplinary rounds using Daily Goals Sheet. Multidisciplinary rounds were
implemented in the MICU with the leadership and support of the unit medical director and nurse
manager. Rounds were patient-centered and could include any staff member or provider involved
in the patient’s care, such as a physician (e.g., attending, resident, intern, and fellow), respiratory
therapist (RT), physical therapist, occupational therapist, social worker (SW), pharmacist, charge
nurse, individual patient’s nurse, and pastoral care provider.
Rounds were focused on open and collaborative communication, decisionmaking, information
sharing, care planning, patient safety issues, cost and quality of care issues, setting daily goals of
care, and communicating with patients and/or family members as they were able. Information
shared during rounds was supplemented by communication at shift changes between the
incoming and the outgoing care providers.
The Daily Goals Sheet was an interdisciplinary communication tool that served as a simple way
of clarifying work goals among providers. It provided the means for the care team and patient
6
(when able) to explicitly define the goals for the day. The form was typically completed during
rounds on each patient, signed by the fellow or attending physician, and given to the patient’s
nurse. The care team—physicians, nurses, RTs, and pharmacists—provided input and reviewed
the goals for the day. The form was updated as the goals of care changed.
Current literature supports the value of multidisciplinary rounding. In a study of
multidisciplinary rounding focused on daily care goals in intensive care, the results showed
improved communication among providers, significant improvement in the proportion of
physicians and nurses who understood the goals of care for the day (from 10 to 95 percent), and
a 50 percent reduction in ICU length of stay.23
Prior to utilizing the patient-centered daily goals format, patient care rounds were provider-
centric and lacked clarity about tasks and care plans for the day. Staff often lacked understanding
of the tasks they needed to accomplish and the plan for communicating with patients, families,
and other caregivers. Physicians and nurses perceived that using this format improved
communication and patient care. The benefits of the goals sheet are founded on the theories of
CRM (crew resource management) and are currently used in a number of ICUs participating in
IHI and Veterans’ Health Administration improvement efforts.23
Escalation Process
The intent of the original study proposal was the development and implementation of an
escalation process algorithm for provider communication regarding changes in patient conditions
for noncode situations. The goal of the escalation process was timely, appropriate
communication between nursing staff and providers as changes in patient conditions occurred.
Previously, no standardized process existed at Denver Health for this purpose, resulting in
ambiguities in the decisionmaking process for each type of patient situation.
Peer-reviewed case studies revealed that the absence of a standardized and well-defined
communication process had led to confusion and delay in appropriate and adequate patient care,
when the need for escalating a concern existed. These issues are particularly relevant at academic
medical centers similar to Denver Health, since the organizational structure includes layers of
providers, such as attending physicians, fellows, senior and junior residents, and interns.
However, concurrent to the implementation phase of the project, the Department of Patient
Safety and Quality developed Rapid Response Escalation Criteria, which provided nurses with
patient parameters for escalation and an outline of providers to call along with a timeframe; the
criteria utilized SBAR for communicating changes in a patient’s condition.
The Rapid Response form served both as a guide for identifying a patient’s condition that could
trigger a Rapid Response call and as a communication tool for physicians to convey their
assessment and plan of care. Instructions were also provided for physicians for followup with
senior/attending physicians within a 4-hour timeframe. This well-documented, standardized
escalation process provided role clarification and cleare patient parameters within a realistic
timeframe, defining whom to call and when, in a way that could be understood by all health care
team members.
7
Implementation
Staff and provider education and development were primary components of the communication
strategy implementation. An “Implementation Toolkit” was developed to serve as a guide for the
education and integration of communication and teamwork factors in clinical practice. Although
specific units served as pilot areas for pre- and post-data collection, it was necessary to involve
all departments and a maximum number of staff members due to the interdepartmental nature of
communication. The challenge to capture a broad audience of health care team members
mandated the creation of a standardized curriculum, teaching materials, and methods that could
be used by multiple disciplines in a variety of forums (e.g., new employees, department
orientation, student rotations, initial education, and ongoing refreshers for current employees).
Health care team members participating in this intervention included nurses, unlicensed assistive
personnel, physicians, respiratory therapists, occupational/physical therapists, dietitians, social
workers, pharmacists, chaplains, clerical/support staff, and radiology and laboratory staff.
The nature of the acute care hospital setting presented particular challenges that required
multiple teaching strategies to introduce the concepts, reinforce learning, facilitate translation of
the concepts into practice, and sustain the practice changes (Table 2).
The goals of the education program included:
• Provide consistent education for all members of the health care team on the concepts of
teamwork, psychological safety, and open, effective communication and its impact on patient
safety.
• Integrate safe communication strategies into the organizational culture.
• Sustain the culture of teamwork, psychological safety, and open, effective communication.
• Maintain consistency and high quality in all educational efforts.
• Develop educational tools that allow for flexibility in use and application in diverse practice
settings.
Table 2. Implementation methods for provider/staff education
Individual
education
Unit/department
education
Organization
education
Initial expert presentation ● ● ●
Video presentation ● ● ●
Fast talks ● ● ●
Communication education notebook ● ●
Practice scenarios (multidisciplinary) ● ●
SBAR practice worksheets ●
Concept poster campaign ● ●
Visual reminders (bookmarks, cards,
lanyards, T-shirts) ● ● ●
PowerPoint® presentation ● ●
Champion role ●
Web-based training ●
8
The education plan was composed of two parts: one, initial education and two, followup
education.
The initial (interdisciplinary) education component engaged team members and introduced the
foundational concepts of human factors, effective teamwork, and communication. More than 650
health care providers (representing all health care disciplines) attended presentations by a
nationally recognized patient safety expert, Michael Leonard, MD. Using “real-life” anecdotes
and an evidence-based approach to factors that influence health care workers’ practice,
Dr. Leonard fostered a commitment from providers to work toward improving the organizational
culture of patient safety.
In addition to the lecture portion of the presentation, attendees also participated in interactive
group activities. They applied the SBAR format to “real-life” patient situations and coached each
other in communicating patient needs. Involving an outside expert created a certain “buzz”
throughout the staff and organization that facilitated interest and involvement in the topic.
Feedback surveys of the initial education/presentation were overwhelmingly positive (Table 3).
Table 3. Feedback from initial expert presentation
Question prompt Agreea
(%)
Strongly
agreea
(%)
Positive
responsesa
(%)
This presentation increased my awareness of how
human factors can affect errors and patient safety. 29.8 67 96.8
This presentation helped me understand the need
for open, effective communication in the health
care team.
27 70 97.0
This presentation helped me realize there may be
times when others on my unit do not communicate
openly.
30.4 66.4 96.8
This presentation helped increase my awareness
of barriers to effective communication. 29.1 68.1 97.2
I think using SBAR would help facilitate better
communication with other care providers or staff. 31.5 66.5 98.0
SBAR is easy for me to understand. 33.2 64.9 98.1
SBAR will be understood by others on my unit. 44.5 50.9 95.4
SBAR could help decrease communication
problems. 35.7 61.8 97.5
SBAR could be rolled out on my unit with few
problems. 48.7 42.6 91.3
a N = 564 respondents
Source: Analysis of feedback from presentations to health care providers at Denver Health made by Michael
Leonard, MD, Physician Leader for Patient Safety at Kaiser Permanente.
9
The followup (unit/department) education component focused on a review of the initial concepts,
practice of effective communication skills, and strategies to create and sustain a culture of patient
safety. In contrast to the initial “kick-off” education sessions, the followup education was a
sustained effort over an extended period of time (months). Ongoing education and reinforcement
of learning were achieved through formal and informal sessions on the patient care unit. A
number of educational strategies were utilized including: “fast talks,” worksheets, posters, visual
cues and reminders, PowerPoint® presentations, unit-level champions, and a video of Dr.
Leonard’s initial presentation (see Table 2).
Fast talks. Feedback from direct caregivers, managers, and clinical educators indicated a need
for practical teaching strategies that could fit into staff’s daily work and routine. “Fast talks,” a
format that is concise (15 minutes), focused, and taken directly to staff members on the unit fit
these criteria. Key selected topics were presented and discussed with staff as they gathered
informally at convenient times during their shifts. Whenever possible, effort was made to include
a multidisciplinary group.
The implementation toolkit included a fast talk notebook of teaching materials for discussion
topics on concept review, practice scenarios, and practice implementation. Key concepts were
presented on 1 to 2 pages that included a headline sentence to convey the essential implications
for practice. Brief bulleted statements served as a guide for more detailed review. Discipline- and
patient population-specific practice scenarios were also included in the notebook. A narrative
described a scenario followed by appropriate SBAR format prompts. Participants worked either
as a group or individually to structure the required communications. A facilitator guide included
examples of potential communications.
SBAR blank communication forms/worksheets. Pads of tear-off sheets that included the
SBAR, instructions for use, and a guide for preparing to contact another team member or
provider were created (Table 1). Feedback from staff indicated the importance of meeting the
needs of both novice and expert team members. “Novice” forms included expanded cues for
section content. “Expert” forms were more streamlined. These sheets were used for
practice/learning and to prepare/organize upcoming communications about actual patient
situations. Tablets of the communication forms were placed on units in strategic locations (e.g.,
near the phone) and utilized in presentations as handouts.
Concept posters. One-line headlines capturing key concepts were developed into laminated
posters and placed on units in strategic locations (e.g., nurse’s stations, staff bulletin boards, and
resident work stations). Clinical nurse educators, managers, and unit champions used the posters
to review key concepts and reinforce previous teaching during staff meetings, huddles, and/or on
an individual basis.
Visual reminders. Visual reminders—such as phone cards, bookmarks, name badge holders,
T-shirts, pocket cards, and pocket notebooks—were developed to provide ongoing reminders and
maintain awareness until practice changes were incorporated into unit/organization culture.
These items were also used as incentives for participating in education events and to reward
observed practice changes. Visual reminder “giveaways” were particularly effective because
10
staff members and providers were eager to obtain them, and because they reinforced previously
presented concepts, providing reminders throughout the day.
PowerPoint® presentation. Developed for use in unit meetings, orientation classes, and other
occasions, these presentations provided a standardized introduction and brief overview of key
concepts. PowerPoint presentations were typically utilized during staff meetings and new
employee orientations.
Champion role. Unit-based champions were identified by unit leadership and served as
implementation “experts,” reinforcing effective learning strategies and culture changes.
Champions embraced the key concepts of teamwork and communication, sharing their strategies
with other units. Examples included advertising educational events using SBAR format and
developing an “SBAR Kudos” form to recognize coworker contributions to the unit.
Data Collection
This implementation project was evaluated using several different approaches:
• Process analysis of communication events, based on observations of communication between
health care providers.
• Evaluation of patient occurrence reports: hospital data from the University Healthsystems
Consortium Web-based occurrence reporting system (Patient Safety Net).
• Hospital Survey on Patient Safety Culture: staff survey responses to the Agency for
Healthcare Research and Quality (AHRQ)-developed patient safety culture survey.24
• Evaluation of staff understanding of patient daily goals: a brief self-report survey on
individual providers’ understanding of the patient plan of care.
• Focus group interviews with hospital staff.
This report will focus on the process analysis of communication events, both pre- and post-
implementation on Phase 1 units. Further results from other evaluation methods will be reviewed
in future publications.
We defined process analysis as focused observations that utilized trained data collectors to
record their observations on the communication process within the health care team. Our process
analysis data collection methods were founded on the concepts of industrial engineering and
observational research methodology. The data collection team—which was made up of nursing
staff from various clinical, research, and administrative backgrounds—worked closely with an
industrial engineer, who was trained in analyzing and improving processes. Guided by the
study’s co-principal investigator and industrial engineer, the team developed standard data
collection guidelines, data collection tools, and coding guides.
Initial training involved observation of communication on units in teams of two or more, pilot
testing the data collection forms and tools, and debriefing the data collection process. Particular
attention was given to team consensus on the various components of the communication events.
Observations were also reviewed to ensure inter-rater reliability.
11
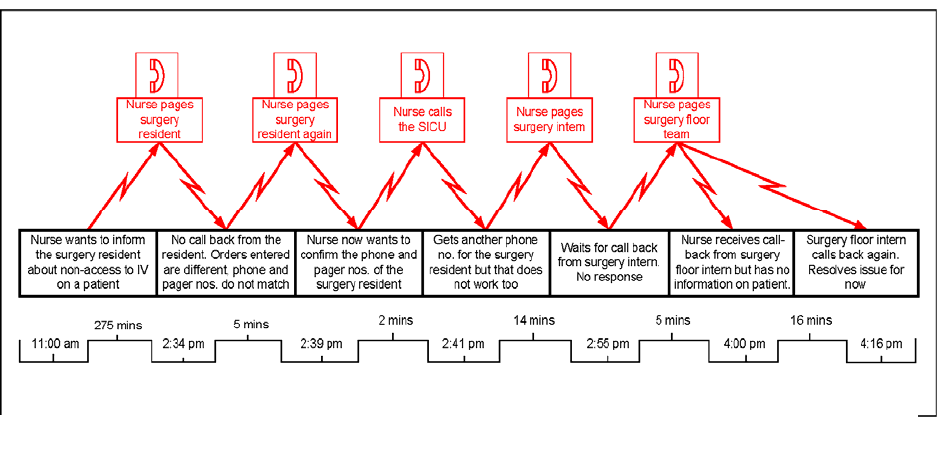
The team defined a “communication event” as nurse-initiated communication with another
health care team member (e.g., physician, respiratory therapist, pharmacist) regarding an existing
or potential problem/issue related to a patient’s health status or plan of care. The communication
event was considered complete once an answer or resolution of the particular patient issue was
received. An “event” may not necessarily end in an immediate treatment. However, it can give
the nurse further direction for the plan of care (Figure 1).
Figure 1. Graphic presentation of a process analysis communication event
Observations were made by one or two data collectors, who remained on the study unit for 1 to 4
hours at a time at different periods throughout the day and night shifts. Stationing observers on
the nursing unit allowed data collectors to record communication events from multiple nurses at
one geographic location. Data collectors took field notes on their observations using a standard
form, asked questions of health care team members to clarify what they were observing, and
asked nurses their perceptions of the communication event.
Data collected about the communication event included: who was communicating; the patient’s
issue or problem; method of communication (e.g., phone, page, face-to-face contact); any
activities taking place during the event (e.g., searching for a phone number, traveling to a
different part of the unit, finding a part of the medical record); the amount of time needed to
communicate and resolve the issue; and followup questions on the nurse’s perceptions about the
resolution of the issue, including his/her satisfaction with the communication. Following
observation of a communication event, data collectors asked nurses two questions:
• To what extent do you think this patient issue has been resolved?
• How satisfied were you with the interaction/communication?
Nurses answered on a 3- or 4-point Likert scale, depending on the question: 1 - not resolved;
2 - somewhat resolved; 3 - resolved; and 1 - not satisfied; 2 - somewhat satisfied; 3 - satisfied;
12
4 - very satisfied. Resolution and satisfaction scores were then recoded into positive and
nonpositive responses (i.e., resolved, satisfied, or very satisfied).
The data collection team observed and analyzed 495 discrete communication events: 224 (112
pre-intervention and 112 post-intervention) on the MICU and 271 events (135 pre-intervention
and 136 post-intervention) on the ACU.
Results
Data Analysis
Communication events were reviewed and coded by the data collection team post hoc and then
entered and analyzed using SPSS® 15.0 software. Initial descriptive statistics and frequencies
were analyzed for each coded category.
During any given communication event, multiple forms of communication and activities could
be evident, such as an initial phone call with a followup face-to-face conversation. Thus,
communication types were not mutually exclusive categories and were coded as either present or
not present for each event. Most communication events on the MICU (74.6 percent) involved
verbal or face-to-face communications, whereas most such events on the ACU (61.6 percent)
involved numeric pages with followup/return phone calls. The most common nurse activities
observed in both the MICU and ACU pre- and post-intervention were waiting for a return phone
call after a page was sent or traveling to a different part of the nursing unit, either to speak with a
provider or to find information (e.g., the on-call physician’s phone number or a patient’s bedside
medical record). Of the 495 communication events observed in both the MICU and ACU, 123
(24.8 percent) involved a nurse communicating with another team member to clarify a patient’s
orders or plan of care.
One of the key elements observed in the process analysis was the time it took health care
providers to communicate and resolve a patient issue. [Due to a violation of assumptions for
parametric statistics (t-test), we used nonparametric statistics (Mann-Whitney U) to compare pre-
and post-intervention times.] In the MICU, we observed a significant post-intervention decrease
(P <0.01) in the mean communication/issue resolution time (Table 4). In the ACU, we observed
a decrease in mean time that, while not statistically significant (P = 0.27), may have been
clinically significant due to a reduction in time to treatment and nursing time spent away from
other patient care activities. Given the volume of patients and daily communications that occur
on the ACU, a 21 percent decrease in mean time for post-intervention communications could
have positive effects.
Each communication event was further analyzed for “problematic” time that contributed to the
total event time. Problematic time was defined as time that nurses spent attempting, but failing,
to communicate with the correct provider (e.g., paging/calling the incorrect team) or searching
for information to determine the appropriate provider or phone number (system issues). When
problematic time was deducted from communication events, we reasoned, the resulting
“adjusted” time was a more accurate representation of provider-to-provider communication time.
13
Table 4. Results of communications process analysis
Time for resolution of
communication/issue Pre-
intervention Post-
intervention P-value
(1-sided)a
MICU
Time for communication (min) (N = 112) (N = 112)
Mean 7.19 3.69 0.007
Range 1 - 312 1 - 51
Adjusted mean 4.52 3.37 0.01
Adjusted range 1 - 55 1 - 51
ACU
Time for communication (min) (N = 135) (N = 136)
Mean 8.29 6.51 0.27
Range 1 - 136 1 - 61
Adjusted mean 6.63 5.27 0.31
Adjusted range 1 - 135 1 - 60
Resolution and satisfaction
MICU Pre-
intervention Post-
intervention P-value
(2-sided)b
Positive nurse responses (%) (N = 99)
67.7
(N = 111)
80.2 0.04
Satisfied/very satisfied nurse responses (%) (N = 103)
85.5
(N = 111)
92.8 0.08
ACU (N = 135) (N = 136)
Positive nurse responses (%) 66.7 75 0.13
Satisfied/very satisfied nurse responses (%) 77.1 80.1 0.53
a t-test
b chi-square
As shown in Table 4, the results were similar for adjusted communication time: a significant
decrease (P = 0.01) in mean adjusted communication time for the MICU and a nonsignificant
decrease (P = 0.31) in mean adjusted communication time for the ACU. The ranges for post-
intervention times—both total and adjusted—were narrower, had smaller standard deviations,
and were therefore more closely clustered around the post-intervention means, indicating a
decrease in the lengthy outlier communications found in the pre-intervention data.
In addition to decreased time for communication/issue resolution, there was also an increase in
the overall nurses’ positive perception of communication events. Chi-square analyses of pre- and
post-intervention positive resolution and satisfaction scores revealed a significant increase in
positive resolution scores (P = 0.04) and a difference in satisfaction scores approaching
significance (P = 0.08) in the MICU and nonsignificant increases in resolution and satisfaction
scores (P = 0.13, P = 0.53, respectively) in the ACU. Positive responses to both the resolution
and satisfaction questions in the post-intervention period increased.
14

Discussion
Our study demonstrates the value of utilizing teamwork and communication strategies among
health care team members in the patient care setting. After implementation of
team/communication strategies, communication time surrounding a patient concern or issue was
decreased, thus bringing resolution and treatment in a timelier manner. Post-intervention, nurses
(the communication initiators) perceived increased satisfaction with communication and higher
rates of resolution of patient issues. Further collection and analysis of additional data measuring
staff perception of the organizational safety culture, the effect of team and communication
factors in patient occurrence reports, and staff and provider focus group interviews are ongoing
and will provide further insight into the effectiveness of the study interventions.
The toolkit developed as a result of this study offers other health care organizations a means to
implement teamwork and communication strategies in their own settings and is available on the
Internet at www.safecoms.org. The intervention tools are adaptable and easily modified for use
in a variety of settings. In addition, the toolkit includes an education plan and facilitator guide;
fast talk book with case scenarios for nursing, medicine, lab, physical therapy, social work,
dietary, and spiritual care; and templates for SBAR communication forms/worksheets, concept
posters, bookmarks, pocket cards, and PowerPoint® presentations. The toolkit also includes
guidelines for the data collection methods used in this project, should an organization wish to
evaluate its own implementation.
Throughout the study, a number of “lessons learned” provided insight that could be useful for
other organizations considering similar implementation of teamwork and communication
strategies. First, it is paramount to secure administrative and clinical support on all management
levels, from the executive to the unit level support. It was important for management and leaders
to demonstrate that teamwork and communication were valued as important factors contributing
to patient safety and staff satisfaction. Furthermore it was important that they provided the means
for staff to attend presentations, encouraged further unit level education, and facilitated
integration of the concepts into practice.
The degree of leadership support varied from unit to unit and clearly made a difference in the
integration of the communication strategies into practice. Those areas with less leadership
support for the project required more mentoring and coaching from the study team over a longer
period of time. In contrast, when leaders embraced the concepts of teamwork and
communication, units integrated the practices into their daily functions in a variety of ways.
Engaged leaders “role-modeled” the use of the communication strategies, and their staff
responded in like fashion. The degree of leadership support may be one of the important factors
contributing to variations in the findings among the Phase 1 units.
We also found that staff members were acutely aware of the culture within an organization and
on their unit as it related to psychological safety, reporting patient occurrences, and team
communication. Once again, those leaders who were committed to teamwork and open
communication set the tone for psychological safety and created an environment for staff to
communicate freely and professionally without fear or inhibition. Other units required additional
efforts on the part of the study team to help create and point out experiences that demonstrated a
safe culture and additional mentoring for the unit leadership.
15

The issue of “problematic time” (i.e., the time nurses spent attempting, but failing, to
communicate with the correct provider or searching for information to determine an appropriate
provider or phone number) was an important system-related finding that warrants further
investigation. As data collection progressed, it became apparent that “communication events”
were complex and included time spent “hunting and gathering” for the correct information
related to whom to call, how to best contact them, and what to do when the primary person was
not available. On average, “problematic time” consisted of 10 to 40 percent of total
communication time, indicating a clear need for clarification in communication procedures that
are unit-specific and easily implemented. It is likely that other academic medical centers face
similar challenges and that this project could provide further insights and guidance toward
potential solutions. Updates on this topic will be included on the www.safecoms.org Web site as
they are developed.
There are also a number of other challenges to achieving interdisciplinary education and training
in an academic setting such as ours. Physician engagement is particularly challenging due simply
to the nature of the academic setting, with resident rotations, various levels of providers, and the
number of physician teams. Our study team developed specific educational strategies that could
be presented during existing meeting times, such as noon conferences, resident orientation, and
outcomes conferences. The support and engagement of the chief medical resident and chief
hospitalist were instrumental in these efforts. In addition, we integrated the perspectives of other
disciplines/departments by eliciting their participation in the development of discipline-specific
case scenario examples for the curriculum.
Finally, as with other new practices and skills, an important consideration in the overall
implementation plan is keeping the strategies and practices going. The ability to educate new
staff and continue integrating communication practices presents a challenge that should be
considered early in the planning stage. Since few formal education programs across disciplines
include teamwork and communication strategies in their curricula, it is particularly incumbent
upon health care organizations to incorporate them into staff education and training. We have
integrated teamwork and communication concepts and skills into department- and unit-level
orientation for new staff and nursing skills fairs for current staff, and we are working on
integrating them into competency skills testing.
Conclusion
Our study suggests that strategies to enhance teamwork and communication can be successfully
implemented in the acute care setting, and that they result in more efficient and effective
communication. Because ineffective communication among health care team members
contributes to patient harm and adverse events, interventions and implementation methods
become instrumental in preventing negative patient outcomes. This project provided the
opportunity to develop, implement, and evaluate an educational program and interventions using
multiple measures across diverse patient care units. The resultant toolkit is available on the
Internet and can be adapted for use in a variety of settings. Further efforts to evaluate the
strategies using additional measures are ongoing. Recommendations for future research include
implementation of the strategies in different health care settings (e.g., outpatient clinics, rural
16
hospitals, and nonacademic settings); integration of the strategies into simulation projects;
longitudinal studies to determine the effectiveness and sustainability of the strategies over time;
and utilizing specific patient-centered outcome measures and staff-related measures, such as
satisfaction, recruitment and retention.
Acknowledgments
Funding was provided by the Agency for Healthcare Research and Quality, Partnerships in
Implementing Patient Safety Grants, 1 U18 HS015846. We thank Denise Johnson, Karin Rees,
and Amy Irwin for their valuable contributions. Special recognition and thanks to Michael
Leonard, MD, for his insightful consultation and willingness to work closely with us on this
project.
Author Affiliations
Denver Health Medical Center, Denver, CO.
Address correspondence to: Catherine Dingley, RN, PhD, Department of Nursing Quality,
Outcomes, Research, and Evidence Based Practice, Denver Health Medical Center, 777 Bannock
Street MC 0260, Denver, CO 80204-4507; e-mail: Catherine.Dingley@dhha.org or
CDingley@aol.com; project Web site: www.safecoms.org.
References
1. Woolf SH, Kuzel AJ, Dovey SM, et al. A string of
mistakes: The importance of cascade analysis in
describing, counting, and preventing medical errors.
Ann Fam Med 2004; 2: 317-326.
2. Lingard LS, Espin S, Whyte G, et al. Communication
failures in the operating room: An observational
classification of recurrent types and effects. Qual Saf
Health Care 2004; 13: 330-334.
3. Leonard M, Graham S, Bonacum D. The human
factor: The critical importance of effective teamwork
and communication in providing safe care. Qual Saf
Health Care 2004; 13: 85-90.
4. Joint Commission on Accreditation of Healthcare
Organizations. 2005 National Patient Safety Goals.
Available at:
www.jointcommission.org/PatientSafety/NationalPatie
ntSafetyGoals/. Accessed February 6, 2008.
5. National Council of State Boards of Nursing.
Available at: www.ncsbn.org. Accessed February 6,
2008.
6. Institute for Safe Medication Practices: Medication
safety alert. Intimidation: Practitioners speak up about
this unresolved problem (Part I). Available at:
www.ismp.org/MSAarticles/IntimidationPrint.htm.
Accessed February 6, 2008.
7. Zwarenstein M, Reeves S. Working together but apart:
Barriers and routes to nurse-physician collaboration. Jt
Comm J Qual Improv 2002; 28: 242-247.
8. Fagin C. Collaboration between nurses and physician:
No longer a choice. Acad Med 1997; 5: 295-303.
9. Fisher B, Peterson C. She won’t be dancing anyway:
A study of surgeons, surgical nurses, and elder
patients. Qual Health Res 1993; 3: 165-183.
10. Kendrick K. Nurses and doctors: A problem of
partnership. In: Soothill K, Mackay L, Web C, editors.
Interprofessional relationships in healthcare. London:
Eward Arnold; 1995. p. 239-252.
11. Larson E. The impact of physician-nurse interaction
on patient care. Holist Nurs Prac 1999; 13: 38-47.
12. Sexton J. Error, stress, and teamwork in medicine and
aviation: Cross sectional surveys. Br Med J 2002; 320:
745-749.
17
13. Knaus WA, Draper EA, Wagner DP, et al. An
evaluation of outcome from intensive care in major
medical centers. Ann Intern Med 1986; 104: 410-418.
14. Shortell SM, Zimmerman JE, Rousseau DM, et al. The
performance of intensive care units: Does good
management make a difference? Med Care 1994; 32:
508-525.
15. Zimmerman JE, Shortell SM, Rousseau DM, et al.
Improving intensive care: Observations based on
organizational case studies in nine intensive care units:
A prospective, multicenter study. Crit Care Med 1993;
21: 1443-1451.
16. Baggs JG, Schmitt MH, Mushlin AI, et al. Association
between nurse-physician collaboration and patient
outcomes in three intensive care units. Crit Care Med
1999; 27: 1991-1998.
17. Baggs JG, Ryan SA, Phelps CE, et al. The association
between interdisciplinary collaboration and patient
outcomes in a medical intensive care unit. Heart Lung
1992; 21: 18-24.
18. Mitchell PH, Armstrong S, Simpson TF, et al.
American Association of Critical-Care Nurses
Demonstration Project: Profile of excellence in critical
care nursing. Heart Lung 1989; 18: 219-237.
19. Boyle DK, Kochinda C. Enhancing collaborative
communication of nurse and physician leadership in
two intensive care units. J Nurs Adm 2004; 34: 60-70.
20. Baggs JG. Development of an instrument to measure
collaboration and satisfaction about care decisions. J
Adv Nurs 1994; 20: 176-182.
21. Helmreich PL. On error management: Lessons from
aviation. Br Med J 2000; 320: 781-785.
22. Harnish V. The daily “adrenaline” meeting. Catalyst
Mag 2004; 1-3.
23. Pronovost P, Berenholtz S, Dorman T, et al.
Improving communication in the ICU using daily
goals. J Crit Care 2003; 18: 71-75.
24. Agency for Healthcare Research and Quality. Patient
safety culture surveys. Available at:
www.ahrq.gov/qual/hospculture/. Accessed February
6, 2008.
18