Philips Medical Systems North America OBRTBV1 Wireless Transducer User Manual ait fm manual
Philips Medical Systems North America Co. Wireless Transducer ait fm manual
Contents
- 1. User Manual
- 2. Users_Manual
User Manual

Instructions for Use
Avalon Fetal Monitor
FM20/30, FM40/50, Avalon CL
Release J.3. with Software Revision J.30.xx
Patient Monitoring
3
1Table of Contents
1Introduction 9
Who this Book is For 9
Confirm Fetal Life Before Using the Monitor 10
Introducing the Avalon Family of Fetal Monitors 11
2What's New 29
What's New in Release J.3 29
What's New in Release G.0 32
3Basic Operation 35
Supported Measurements 35
Avalon FM20 and FM30 36
Avalon FM40 and FM50 39
Avalon CL Transducer System 40
Getting to Know Your Avalon FM20/FM30 40
Getting to Know Your Avalon FM40/FM50 43
Transducers 45
Getting to Know Your Avalon CL 47
Cableless Transducers 51
CL Pods 55
Operating and Navigating 56
Operating Modes 63
Automatic Screen Layouts 64
Settings 64
Preparing to Monitor 67
Switching the Monitor to Standby 98
After Monitoring 98
Disconnecting from Power 99
Power On/Power Off Behavior 99
Monitoring After a Power Failure 99
Troubleshooting 100
4FM20/30 Battery Option 101
External Power Supply M8023A 102
Using Batteries 102
Optimizing Battery Performance 105
5Alarms 109
Alarm Mode 110
Nurse Call Systems 110
4
Visual Alarm Indicators 110
Audible Alarm Indicators 111
Acknowledging Alarms 114
Acknowledging Disconnect INOPs 114
Alarm Reminder 114
Pausing or Switching Off Alarms 115
Alarm Limits 117
Reviewing Alarms 118
Latching Alarms 118
Testing Alarms 120
Alarm Behavior at Power On 121
6Patient Alarms and INOPs 123
Alarm Messages 123
Technical Alarm Messages (INOPs) 126
7Admitting and Discharging 137
Admit/Discharge on the Monitor 137
New Patient Check 139
OB TraceVue/IntelliSpace Perinatal 139
8Non-Stress Test Timer 141
Setting NST Autostart/Autostop 141
Viewing the NST Timer 141
Timer Expiry Notification 142
Accessing the NST Setup Pop-up Keys 142
9Non-Stress Test Report 145
Setting Up an NST Report 145
NST Report Status Window 146
NST Criteria 148
Non-Reassuring Report 149
Non-Reactive NST Test 149
10 Cross-Channel Verification (CCV) 151
Misidentification of Heart Rates 151
Cross-Channel Verification Functionality 152
Overview of Cross-Channel Comparisons 152
Coincidence Examples 154
Recommended Actions for INOP Coincidence 156
11 Monitoring FHR and FMP Using Ultrasound 157
Technical Description 157
Limitations of the Technology 158
Misidentification of MHR as FHR 158
What You Need 158
5
Cableless Monitoring - Important Considerations 159
Preparing to Monitor 160
Selecting Fetal Heart Sound 161
Changing the Fetal Heart Sound Volume 161
Fetal Movement Profile 163
Troubleshooting 165
Additional Information 166
Testing Ultrasound Transducers 173
12 Monitoring Twin FHRs 175
Important Considerations 175
Monitoring Twins Externally 176
Monitoring Twins Internally 177
Separating FHR Traces 177
Troubleshooting 181
13 Monitoring Triple FHRs 183
Important Considerations 183
Monitoring Triplets 184
Separating FHR Traces 184
"Standard" Separation Order 184
"Classic" Separation Order 185
Switching Trace Separation On and Off 186
When Trace Separation is On 187
When Trace Separation is Off 188
Troubleshooting 188
14 Fetal Heart Rate Alarms 191
Changing Alarm Settings 191
Changing Signal Loss Delay 192
15 Monitoring Uterine Activity Externally 193
What You Need 193
External Toco Monitoring 194
Toco Sensitivity 195
Troubleshooting 195
Testing Toco Transducers 195
16 Monitoring Uterine Activity Internally 197
What You Need 197
Internal (IUP) Monitoring 199
Troubleshooting 199
17 Monitoring FHR Using DECG 201
Misidentification of MHR as FHR 201
What You Need 203
6
Making Connections 205
Monitoring DECG 206
Suppressing Artifacts 208
Troubleshooting 209
Testing DECG Mode 209
18 Monitoring Noninvasive Blood Pressure 211
Introducing the Oscillometric Noninvasive Blood Pressure Measurement 211
Preparing to Measure Noninvasive Blood Pressure 212
Starting and Stopping Measurements 214
Enabling Automatic Mode and Setting Repetition Time 215
Enabling Sequence Mode and Setting Up The Sequence 215
Choosing the Alarm Source 216
Assisting Venous Puncture 216
Calibrating NBP 216
Troubleshooting 217
19 Monitoring Maternal Temperature 219
Measuring Tympanic Temperature 219
20 Monitoring SpO2 227
Selecting an SpO2 Sensor 227
Applying the Sensor 227
Connecting SpO2 Cables 228
Measuring SpO2 228
SpO2 Signal Quality Indicator (Fast SpO2 only) 229
Assessing a Suspicious SpO2 Reading 230
Understanding SpO2 Alarms 230
Setting Up Tone Modulation 231
Setting the QRS Volume 231
21 Monitoring Maternal Heart / Pulse Rate 233
Priority for Maternal Heart / Pulse Rate 233
Misidentification of MHR for FHR 234
MHR from MECG Electrodes 235
Monitoring MECG Wave 238
Pulse Rate from Toco MP 240
Pulse Rate from SpO2 241
Adjusting the Heart Rate / Pulse Alarm Limits 241
Average Pulse Rate from Noninvasive Blood Pressure 242
Testing MECG Mode 242
7
22 Printing the ECG Waveform 243
23 Paper Save Mode for Maternal Measurements 249
24 Recovering Data 251
Recovering Traces on Paper 251
Recovering Traces on an OB TraceVue/IntelliSpace Perinatal System 252
Recording Stored Data 252
25 Care and Cleaning 255
General Points 255
Cleaning and Disinfecting 256
Cleaning and Disinfecting Monitoring Accessories 257
Cleaning and Disinfecting the Tympanic Temperature Accessories 258
Sterilizing 258
26 Maintenance 259
Inspecting the Equipment and Accessories 259
Inspecting the Cables and Cords 259
Maintenance Task and Test Schedule 260
Recorder Maintenance 260
Cleaning the Print Head 265
Disposing of the Monitor 266
27 Accessories and Supplies 267
Information on Latex 267
Avalon CL Base Station 268
Transducers 268
Fetal Accessories 268
MECG Accessories 270
Noninvasive Blood Pressure Accessories 270
SpO2 Accessories 273
Tympanic Temperature Accessories 277
Recorder Paper 277
Batteries 277
28 Specifications and Standards Compliance 279
Environmental Specifications 279
Physical Specifications 281
Performance Specifications 285
Recorder Specifications 294
Compatible External Displays: FM40/FM50 Only 296
Manufacturer's Information 296
Trademark Acknowledgment 296
Regulatory and Standards Compliance 297
Environment 306

1
9
1Introduction
Who this Book is For
This book is for trained healthcare professionals using the Avalon FM20, FM30, FM40 and FM50
Fetal/Maternal monitors, and the cableless monitoring system Avalon CL. It describes how to set up
and use the monitor and transducers. Familiarize yourself with all instructions including warnings and
cautions before starting to monitor patients. Read and keep the Instructions for Use that come with
any accessories, as these contain important information about application and care and cleaning that is
not repeated in this book.
You should be:
• Trained in the use of fetal heart rate (FHR) monitors.
• Trained in the interpretation of FHR traces.
• Familiar with using medical devices and with standard fetal monitoring procedures.
For information on how to configure and service the monitor, see the Configuration Guide and the
Service Guides, or contact your authorized service provider.
Your monitor may not have all of the features and options described in this guide. The exact
appearance of the monitor may differ slightly from that shown in the illustrations.
In this guide:
•A warning alerts you to a potential serious outcome, adverse event or safety hazard. Failure to
observe a warning may result in death or serious injury to the user or patient.
•A caution alerts you to where special care is necessary for the safe and effective use of the
product. Failure to observe a caution may result in:
– minor or moderate personal injury,
– damage to the product or other property,
– possibly in a remote risk of more serious injury.
•Monitor refers to the entire fetal/maternal monitor. Display refers to the physical display unit.
Screen refers to everything you see on the monitor's display, such as measurements, alarms,
patient data, and so forth.
FM30 • Whenever a monitor’s identifier appears to the left of a heading or paragraph, it means that the
information applies to that monitor only. Where the information applies to all models, no
distinction is made.

1Introduction
10
Avalon CTS
Avalon CL
Whenever one of these identifiers appear to the left of a heading or paragraph, it means that the
information applies to that cableless monitoring system. Where the information applies to both
systems, no distinction is made.
Confirm Fetal Life Before Using the Monitor
Fetal monitoring technology available today is not always able to differentiate a fetal heart rate (FHR)
signal source from a maternal heart rate (MHR) source in all situations. Therefore, you should confirm
fetal life by independent means before starting to use the fetal monitor, for example, by palpation of fetal
movement or auscultation of fetal heart sounds using a fetoscope, stethoscope, or Pinard stethoscope.
If you cannot hear the fetal heart sounds, and you cannot confirm fetal movement by palpation,
confirm fetal life using obstetric ultrasonography. Continue to confirm that the fetus is the signal
source for the FHR during monitoring.
Be aware that:
• an MHR trace can exhibit features that are very similar to those of an FHR trace, even including
accelerations and decelerations. Do not rely solely on trace pattern features to identify a fetal
source.
• Fetal Movement Profile (FMP) annotations on a fetal trace alone may not always indicate that the
fetus is alive. The body of a deceased fetus can move and cause the monitor to annotate fetal body
movements.
Here are some examples where the MHR can be misidentified as the FHR.
•When using an ultrasound transducer:
– It is possible to pick up maternal signal sources, such as the aorta or other large vessels.
– Misidentification may occur when the MHR is higher than normal (especially when it is over
100 bpm).
•When using a fetal scalp electrode:
– Electrical impulses from the maternal heart can sometimes be transmitted to the fetal monitor
through a recently deceased fetus via the spiral scalp electrode cable, appearing to be a fetal
signal source.
– The recorded MHR (and any artifact) can be misinterpreted as an FHR (especially when it is
over 100 bpm).
•When Fetal Movement Profile (FMP) is enabled:
FMP annotations in the absence of fetal life may be a result of:
– Movement of the deceased fetus during or following maternal movement.
– Movement of the deceased fetus during or following manual palpation of fetal movement
(especially if the pressure applied is too forceful).
– Movement of the ultrasound transducer.
– The ultrasound transducer detecting a maternal movement source, such as the mother
coughing.
See also “Monitoring FHR and FMP Using Ultrasound” on page 155 and “Monitoring FHR Using
DECG” on page 195.
To reduce the possibility of mistaking the MHR for an FHR, it is recommended that you monitor both
maternal and fetal heart rates. The monitor's cross-channel verification (CCV) facility can help by
automatically detecting when an MHR coincides with an FHR. For further details, see “Cross-Channel
Verification (CCV)” on page 149.
1 Introduction
11
Introducing the Avalon Family of Fetal Monitors
The Avalon family of fetal monitors consists of the Avalon FM20, FM30, FM40 and FM50. While the
FM20/FM30 and the FM40/FM50 have different form factors, the method of operation is very
similar for all monitors. The Avalon fetal monitors also share transducers, accessories, software, and
are compatible with the Avalon CL, and Avalon CTS Cableless Fetal Transducer Systems.
Intended Use
The Philips Avalon FM20 (M2702A), FM30 (M2703A), FM40 (M2704A) and FM50 (M2705A) Fetal/
Maternal Monitors are intended for:
• non-invasive monitoring of fetal heart rates and movements.
• non-invasive monitoring of maternal heart rates, maternal pulse rates, uterine activity, maternal
noninvasive blood pressure, maternal oxygen saturation, and maternal temperature.
• invasive monitoring of fetal Direct ECG and intrauterine pressure and for displaying and
recording of fetal and maternal ECG waves. (FM30 and FM50 only).
• displaying, storing, and recording patient data and parameter values, and for generating alarms
from fetal and maternal parameters.
• transmitting patient data and parameter values to a patient information and surveillance system
used by trained health care professionals.
• use in antepartum testing areas, in labor and delivery rooms, and during postpartum recovery in
the hospital environment. They are not intended for use in intensive care units or operating rooms.
• monitoring in a bath or shower. (Avalon CL cableless transducers Toco+ MP, Ultrasound, and
ECG/IUP only)
• transport situations in healthcare facilities, for healthcare facilities outside hospitals, such as
doctors’ offices, and for use in private households. (FM20 and FM30 only)
WARNING
The fetal/maternal monitors are not intended for:
• use during defibrillation, electro-surgery, or magnetic resonance imaging (MRI).
• ECG measurements on patients connected to electrical stimulator or with cardiac pacemakers.
• use of the invasive measurements IUP and fetal DECG, use of the patient module (M2738A) and
use of the Avalon CL system in domestic establishments and those connected directly to the
public low-voltage supply network that supplies buildings used for domestic purposes.
WARNING
No modification of the fetal monitors, transducers, and the Avalon CL base station is allowed.
CAUTION
US federal law restricts this device to sale by, or on the order of, a physician.
1Introduction
12
Connecting the Monitor to AC Mains
WARNING
• Always use the supplied power cord with the earthed mains plug to connect to an earthed AC
mains socket. Never adapt the mains plug from the fetal monitor to fit an unearthed AC mains
socket.
• Check that the line frequency is correctly configured in the Global Settings menu.
•FM20/FM30 only: The protective earth conductor is required for EMC purposes. It has no
protective function against electric shock. Double and/or reinforced insulation protects this
device against electric shock.
• Do not use AC mains extension cords or multiple portable socket-outlets.
Indications for Use
Avalon Fetal/Maternal Monitor FM20
Indicated for use by trained health care professionals whenever there is a need for monitoring of the
physiological parameters uterine activity, heart rate, oxygen saturation, noninvasive blood pressure,
pulse rate, and temperature of pregnant women and the fetal heart rates of single fetuses, twins, and
triplets in labor and delivery rooms, in antepartum testing areas, in private households and during
transports in healthcare facilities.
Avalon Fetal/Maternal Monitor FM30
Indicated for use by trained health care professionals whenever there is a need for monitoring of the
physiological parameters uterine activity, heart rate, ECG, oxygen saturation, noninvasive blood
pressure, and pulse rate and temperature of pregnant women and the fetal heart rates of single fetuses,
twins, and triplets in labor and delivery rooms, in antepartum testing areas, in private households and
during transports in healthcare facilities.
Avalon Fetal/Maternal Monitor FM40
Indicated for use by trained health care professionals whenever there is a need for monitoring of the
physiological parameters uterine activity, heart rate, oxygen saturation, noninvasive blood pressure,
and pulse rate and temperature of pregnant women and the fetal heart rates of single fetuses, twins,
and triplets in labor and delivery rooms and in antepartum testing areas.
Avalon Fetal/Maternal Monitor FM50
Indicated for use by trained health care professionals whenever there is a need for monitoring of the
physiological parameters uterine activity, heart rate, ECG, oxygen saturation, noninvasive blood
pressure, and pulse rate and temperature of pregnant women and the fetal heart rates of single fetuses,
twins, and triplets in labor and delivery rooms and in antepartum testing areas.
Safety Information
In this guide:
• A warning alerts you to a potential serious outcome, adverse event or safety hazard. Failure to
observe a warning may result in death or serious injury to the user or patient.
• A caution alerts you to where special care is necessary for the safe and effective use of the product.
Failure to observe a caution may result in minor or moderate personal injury or damage to the
product or other property, and possibly in a remote risk of more serious injury.
1 Introduction
13
WARNING
The fetal/maternal monitors are not intended for:
• use during defibrillation, electro-surgery, or magnetic resonance imaging (MRI).
• ECG measurements on patients connected to electrical stimulator or with cardiac pacemakers.
• use of the invasive measurements IUP and fetal DECG, use of the patient module (M2738A) and
use of the Avalon CL system in domestic establishments and those connected directly to the
public low-voltage supply network that supplies buildings used for domestic purposes.
WARNING
No modification of the fetal monitors, transducers, and the Avalon CL base station is allowed.
CAUTION
US federal law restricts this device to sale by, or on the order of, a physician.
WARNING
• Always use the supplied power cord with the earthed mains plug to connect to an earthed AC
mains socket. Never adapt the mains plug from the fetal monitor to fit an unearthed AC mains
socket.
• Check that the line frequency is correctly configured in the Global Settings menu.
•FM20/FM30 only: The protective earth conductor is required for EMC purposes. It has no
protective function against electric shock. Double and/or reinforced insulation protects this
device against electric shock.
• Do not use AC mains extension cords or multiple portable socket-outlets.
WARNING
• To avoid magnetic interference affecting the mode of the pacemaker, ensure that the Avalon CL
base station does not come into close contact with implanted pacemakers.
• This equipment generates, uses, and radiates radio-frequency energy, and if it is not installed and
used in accordance with its accompanying documentation, may cause interference to radio
communications. Operation of this equipment in a residential area may cause interference, in
which case the users must take whatever measures may be required to correct the interference.
1Introduction
14
WARNING
Do not change the date and time setting, if the fetal monitor is connected to a Philips OB TraceVue/
IntelliSpace Perinatal system via a LAN -setup. The monitor uses the OB TraceVue/IntelliSpace
Perinatal system date and time, including daylight saving time changes. As long as the fetal monitor is
connected to the OB TraceVue/IntelliSpace Perinatal system via the LAN-setup (locomotive icon
displayed on the monitor's screen), the option to change the date and time settings at the fetal monitor
are disabled, this is not valid for RS232 connections, or the connection to other systems.
WARNING
Short range radio connections are subject to interruption due to interference from other radio sources
in the vicinity, including microwaves, bluetooth devices, WLAN devices (802.11b,g,n) and cordless
phones. Depending on the strength and duration of the interference, the interruption may occur for an
extended period. A loss of connection, due to moving out-of-range, interference, or for other reasons,
is indicated with a No Host Monitoring INOP (here the host is the fetal monitor) on the NBP or
SpO2 Pods, or a cl NBP Disconnect or cl SpO₂ Disconnect INOP at the fetal monitor. Correct
channel configuration is important, refer to the Configuration Guide for details.
CAUTION
Check the fetal monitors housing for damage before you start to monitor as part of your safety
precautions.
WARNING
When connecting devices for acquiring measurements, always position cables and NBP tubing
carefully to avoid entanglement or potential strangulation.
CAUTION
Using recorder paper that is not approved by Philips can result in accelerated paper fading and can
damage the thermal line printhead. This type of damage is not covered by warranty.
WARNING
Never immerse the base station in liquid. You must protect it against water sprays or splashes. Place
the base station where there is no chance of contact with, or falling into water or other liquids.
1 Introduction
15
CAUTION
Avoid the use of pulsating water jets in the bath or shower while monitoring, as these can be
misinterpreted as an incorrect (or totally artificial) heart rate.
Toco Baseline drift: The accuracy specified for baseline drift cannot be guaranteed for underwater
usage. When using transducers under warm water the temperature increase causes a significant baseline
change due to internal pressure increase. The depth under water at which the Toco transducer is used
also has an effect on the Toco baseline, as the water pressure increases with depth. After immersion,
allow one to two minutes for the pressure to stabilize, then adjust the Toco baseline (between
contractions), and check it frequently.
When using the transducers underwater, the radio transmission range is reduced, and signal loss may
occur.
WARNING
• Always use the supplied power cord with the earthed mains plug to connect the external power
supply M8023A (option #E25) to an earthed AC mains socket. Never adapt the mains plug from
the power supply to fit an unearthed AC mains socket.
• Do not use AC mains extension cords or multiple portable socket-outlets. If a multiple portable
socket-outlet without an approved isolation transformer is used, the interruption of its protective
earthing may result in enclosure leakage currents equal to the sum of the individual earth leakage
currents, so exceeding allowable limits.
• Do not connect any devices that are not supported as part of a system.
• Any non-medical device placed and operated in the patient’s vicinity must be powered via an
approved isolation transformer that ensures mechanical fixing of the power cords and covering of
any unused power outlets.
WARNING
Do not touch the charging contacts for the cableless transducers at the Avalon base station while you
are touching the patient.)
CAUTION
Condition the battery with a monitor not currently in use. The monitor switches off automatically
when there is no battery power left.
1Introduction
16
WARNING
Use only Philips batteries part number M4605A. Use of a different battery may present a risk of fire
or explosion.
Do not open batteries, or dispose of them in fire, or cause them to short circuit. They may ignite,
explode, leak or heat up, causing personal injury.
If battery leakage should occur, avoid contact with skin. Refer to qualified and authorized service
personnel.
Dispose of used batteries promptly and in an environmentally-responsible manner. Do not dispose
of the battery in normal waste containers. Consult your hospital administrator to find out about local
arrangements. Do not expose batteries to liquids.
Do not crush, drop or puncture batteries - mechanical abuse can lead to internal damage and internal
short circuits which may not be visible externally.
If a battery has been dropped or banged against a hard surface, whether damage is visible externally or
not:
• discontinue use
• dispose of the battery in accordance with the disposal instructions above.
Keep batteries out of the reach of children.
CAUTION
Do not disassemble, heat above 100°C (212°F) or incinerate the batteries, to avoid the risk of fire and
burns. Keep batteries out of the reach of children and in their original package until you are ready to
use them.
If battery leakage should occur, use caution in removing the battery. Avoid contact with skin. Refer to
qualified and authorized service personnel.
Do not install or use pre-damaged batteries.
WARNING
Alarm systems of the monitor and those of the connected OB system are independent and not
synchronized.
WARNING
In INOP only mode, no fetal/maternal patient alarms are enabled or indicated.
1 Introduction
17
WARNING
Do not rely exclusively on the audible alarm system for fetal monitoring. Adjustment of alarm volume
to a low level or off during monitoring may result in a dangerous situation. Remember that the most
reliable method of fetal monitoring combines close personal surveillance with correct operation of
monitoring equipment.
WARNING
Be aware that the monitors in your care area may each have different alarm settings, to suit different
scenarios. Always check that the alarm settings are appropriate before you start monitoring.
CAUTION
In order to ensure that the settings are reset to user defaults for a new patient, always discharge the
previous patient from the fetal monitor.
WARNING
Performing ultrasound imaging or Doppler flow measurements together with ultrasound fetal
monitoring may cause false FHR readings, and the trace recording may deteriorate.
CAUTION
Never use ultrasound transducers connected to more than one fetal monitor on the same patient.
1Introduction
18
WARNING
• Ensure that the conductive parts of the fetal scalp electrode and the maternal leg plate electrode do
not contact other conductive parts, including earth.
• Indication of the heart-rate may be adversely affected by the operation of cardiac pacemaker pulses
or by cardiac arrhythmias.
• During ambulant FHR monitoring, the chance of losing the signal or detecting the maternal heart
rate is higher than during stationary monitoring. The frequency of the patient's walk may be
detected, and mistaken for a FHR signal.
• Check the mother’s pulse periodically during monitoring and compare this with the FHR signal.
Beware of mistaking a “doubled” maternal heart rate for FHR. In the case of a dead fetus, there is
a risk that the maternal heart rate is monitored and misinterpreted as the fetal heart rate.
Therefore, the simultaneous monitoring of maternal heart rate (preferably, the maternal ECG) is
encouraged.
• Do not interpret maternal movements as fetal movements.
• Artifacts: FMP artifacts are generated during fetal heart rate searching by changing the transducer
position, therefore Philips fetal monitors enable the FMP only after detecting a valid heart rate
signal for several seconds. FMP is not recommended when the mother is likely to move, and you
should disable Fetal Movement Profile (FMP) at the fetal monitor (FMP Off) if the mother is
walking.
• Gaps and maternal heart rate detection can occur:
– if the transducer is not correctly positioned.
– due to the pulsation of uterine blood vessels.
–if the fetus moves.
CAUTION
Using ultrasound gel not approved by Philips may reduce signal quality and may damage the
transducer. This type of damage is not covered by warranty.
WARNING
Periodically compare the mother's pulse with the signal coming from the monitor's loudspeaker to
ensure that you are monitoring fetal heart rate. Do not mistake a doubled or elevated MHR for FHR.
WARNING
Do not catheterize if placenta previa is diagnosed, or if uterine bleeding from an undetermined source
is present.
1 Introduction
19
WARNING
Never attempt to connect the fetal scalp electrode to anything other than the correct DECG adapter
cable.
WARNING
The fetal/maternal monitor is not a diagnostic ECG device. In particular, the display of fetal/maternal
ECG is intended only for evaluating signal quality for fetal/maternal heart rate as derived from the
ECG waveform.
When in doubt, it can be used to identify sources of compromised signal quality, such as noise or
muscle artifacts. It can subsequently be used to verify the result of measures taken to resolve them (e.g.
checking ECG cable connections or adapting the fetal ArtifactSuppress configuration).
The safety and effectiveness of the displayed fetal/maternal ECG waveform (i.e. P, QRS and T
segments) for evaluation of fetal/maternal cardiac status during labor have not been evaluated.
WARNING
Intravenous infusion: Do not use the NBP cuff on a limb with an intravenous infusion or arterial
catheter in place. This could cause tissue damage around the catheter when the infusion is slowed or
blocked during cuff inflation.
Skin Damage: Do not measure NBP in cases of sickle-cell disease or any condition where skin
damage has occurred or is expected.
Unattended measurement: Use clinical judgment to decide whether to perform frequent unattended
blood pressure measurements in cases of severe blood clotting disorders because of the risk of
hematoma in the limb fitted with the cuff.
WARNING
Do not use the thermometer in the presence of flammable anesthetics, such as a flammable anesthetic
mixture with air, oxygen or nitrous oxide.
1Introduction
20
WARNING
• Never apply the probe to the patient when the probe is not connected to the unit.
• Always use a single-use probe cover to limit patient cross-contamination.
• Measurement errors or inaccurate readings may result when:
– probe covers other than the specified probe covers are used (see “Tympanic Temperature
Accessories” on page 267)
• Insert the probe slowly and carefully to avoid damage to the ear canal and the tympanic
membrane.
• Inspect the probe for damage, holes, tears, or sharp edges to avoid injuring the skin.
• Always ensure that the used probe cover is removed before attaching a new probe cover.
CAUTION
• Do not immerse the probe in fluids, or drop fluids on the probe.
• Do not use a probe cover that has been dropped or is damaged.
• Do not autoclave. To prevent damage to the unit, probe and accessories, refer to the cleaning
procedures in the “Cleaning and Disinfecting” on page 246 chapter.
CAUTION
Do not use OxiCliq disposable sensors in a high humidity environment, or in the presence of fluids,
which may contaminate sensor and electrical connections causing unreliable or intermittent
measurements. Do not use disposable sensors when there is a known allergic reaction to the adhesive.
WARNING
Proper Sensor Fit: If a sensor is too loose, it might compromise the optical alignment or fall off. If it
is too tight, for example because the application site is too large or becomes too large due to edema,
excessive pressure may be applied. This can result in venous congestion distal from the application site,
leading to interstitial edema, hypoxemia and tissue malnutrition. Skin irritations or lacerations may
occur as a result of the sensor being attached to one location for too long. To avoid skin irritations and
lacerations, periodically inspect the sensor application site and change the application site regularly.
Venous Pulsation: Do not apply sensor too tightly as this results in venous pulsation which may
severely obstruct circulation and lead to inaccurate measurements.
Ambient Temperature: At elevated ambient temperatures be careful with measurement sites that are
not well perfused, because this can cause severe burns after prolonged application. All listed sensors
operate without risk of exceeding 41°C on the skin if the initial skin temperature does not exceed
35°C.
Extremities to Avoid: Avoid placing the sensor on extremities with an arterial catheter, an NBP cuff
or an intravascular venous infusion line.
1 Introduction
21
WARNING
• For fully conscious pediatric or adult patients, who have a normal function of perfusion and
sensory perception at the measurement site:
To ensure skin quality and correct optical alignment of the sensor, inspect the application site
when the measurement results are suspicious or when the patient complains about pressure at
the application site, but at least every 24 hours. Correct the sensor alignment if necessary.
Move the sensor to another site, if the skin quality changes.
• For all other patients:
Inspect the application site every two to three hours to ensure skin quality and correct optical
alignment. Correct the sensor alignment if necessary. If the skin quality changes, move the
sensor to another site. Change the application site at least every four hours.
• Injected dyes such as methylene blue, or intravascular dyshemoglobins such as methemoglobin
and carboxyhemoglobin may lead to inaccurate measurements.
• Inaccurate measurements may result when the application site for the sensor is deeply pigmented
or deeply colored, for example, with nail polish, artificial nails, dye or pigmented cream.
• Interference can be caused by:
– High levels of ambient light (including IR warmers) or strobe lights or flashing lights (such as
fire alarm lamps). (Hint: cover application site with opaque material.)
– Another SpO2 sensor in close proximity (e.g. when more than one SpO2 measurement is
performed on the same patient). Always cover both sensors with opaque material to reduce
cross-interference.
– Electromagnetic interference, especially at perfusion indicator values below 1.0 or signal
quality indicator below medium.
– Excessive patient movement and vibration.
WARNING
With pulse oximetry, sensor movement, ambient light (especially strobe lights or flashing lights) or
electromagnetic interference can give unexpected intermittent readings when the sensor is not
attached. Especially bandage-type sensor designs are sensitive to minimal sensor movement that might
occur when the sensor is dangling.
CAUTION
If you measure SpO2 on a limb that has an inflated noninvasive blood pressure cuff, a non-pulsatile
SpO2 INOP can occur. If the fetal monitor is configured to suppress this alarm there may be a delay of
up to 60 seconds in indicating a critical status, such as sudden pulse loss or hypoxia.
1Introduction
22
WARNING
The fetal/maternal monitor is not a diagnostic ECG device. In particular, the display of fetal/maternal
ECG is intended only for evaluating signal quality for fetal/maternal heart rate as derived from the
ECG waveform.
When in doubt, it can be used to identify sources of compromised signal quality, such as noise or
muscle artifacts. It can subsequently be used to verify the result of measures taken to resolve them
(e.g., checking ECG cable connections).
The safety and effectiveness of the displayed fetal/maternal ECG waveform (i.e., P, QRS and T
segments) for evaluation of fetal/maternal cardiac status during labor have not been evaluated.
WARNING
The fetal/maternal monitor is NOT intended for use during defibrillation, electro-surgery, or MRI.
Remove all transducers, sensors, and accessories before performing electro-surgery, defibrillation, or
MRI, otherwise harm to the patient or the user can result.
WARNING
• No alarm is possible when Toco MP or CL Toco+MP transducer is the source of the pulse rate.
• No QRS tone is audible when Toco MP or CL Toco+MP transducer is the source of the pulse
rate.
• The Toco MP or CL Toco+MP transducer signal is significantly less reliable if the patient is up
and moving about, or is pushing during the second stage of labor.
WARNING
No alarm is possible when noninvasive blood pressure is the source of the pulse rate.
CAUTION
Only use Philips paper. Using paper other than Philips paper may result in the failure to recover traces.
CAUTION
Ensure that you admit each patient by name, including other patient identification information, and
discharge the patient when you have finished monitoring, so that you can identify which trace period
(entry in the patient list) refers to which patient.
1 Introduction
23
WARNING
• Do not operate the monitor if it is wet. If you spill liquid on the monitor, contact your service
personnel or Philips service engineer.
• Do not perform underwater monitoring (for example, in a bath or shower) using wired
transducers.
• Place the monitor where there is no chance of contact with, or falling into water or other liquid.
• Do not dry equipment using heating devices such as heaters, ovens (including microwave ovens),
hair dryers and heating lamps.
• Do not put equipment or accessories in autoclave (for sterilization).
CAUTION
Solutions: Do not mix disinfecting solutions (such as bleach and ammonia) as hazardous gasses may
result.
Skin contact: To reduce the risk of skin irritations, do not allow a cleaning or disinfecting agent to
leave residues on any of the equipment surfaces - wipe it off with a cloth dampened with water, after
allowing the appropriate time for the agent to work, or before applying to a patient.
Hospital policy: Disinfect the product as determined by your hospital's policy, to avoid long term
damage to the product.
Local requirements: Observe local laws governing the use of disinfecting agents.
Touch display: To clean and disinfect the touch-enabled display, disable the touch operation by
switching off the monitor during the cleaning procedure, or by selecting and holding the Main Screen
key until the padlock symbol appears on it, indicating that touch operation is disabled. Select and hold
again to re-enable touch operation.
WARNING
Do not put device and accessories in autoclave (for sterilization).
WARNING
Schedule: Failure on the part of the responsible individual hospital or institution employing the use of
this equipment to implement a satisfactory maintenance schedule may cause undue equipment failure
and possible health hazards.
In case of problems: If you discover a problem with any of the equipment, contact your service
personnel, Philips, or your authorized supplier.
Electric shock hazard: Do not open the monitor housing. Refer all servicing to qualified service
personnel.
1Introduction
24
WARNING
To avoid contaminating or infecting personnel, the environment or other equipment, make sure you
disinfect and decontaminate the monitor appropriately before disposing of it in accordance with your
country's laws for equipment containing electrical and electronic parts. For disposal of parts and
accessories such as thermometers, where not otherwise specified, follow local regulations regarding
disposal of hospital waste.
WARNING
Reuse: Disposable accessories and supplies intended for single use, or single use only, and are
indicated as such on their packaging. Never reuse disposable accessories and supplies, such as
transducers, sensors, electrodes and so forth that are intended for single use, or single patient use only.
Approved accessories: Use only Philips-approved accessories.
Packaging: Do not use a sterilized accessory if its packaging is damaged.
Protection against electric shocks: The transducers and accessories listed in this chapter are
not defibrillator proof.
Electro-Surgery, Defibrillation and MRI: The fetal/maternal monitors are not intended for use
during defibrillation, electro-surgery, or MRI. Remove all transducers, sensors, and accessories before
performing electro-surgery, defibrillation, or MRI, otherwise harm can result.
WARNING
Explosion Hazard: Do not use in the presence of flammable anesthetics, such as a flammable
anesthetic mixture with air, oxygen, nitrous oxide, or in oxygen rich environment. Use of the devices in
such an environment may present an explosion hazard.
WARNING
• Do not use additional AC mains extension cords or multiple portable socket-outlets. If a multiple
portable socket-outlet is used, the resulting system must be compliant with IEC/EN 60601-1 A1:
2012.
• Do not connect any devices that are not supported as part of a system.
• Do not use a device in the patient vicinity if it does not comply with IEC/EN 60601-1 A1: 2012.
The whole installation, including devices outside of the patient vicinity, must comply with IEC/
EN 60601-1 A1: 2012. Any non-medical device, including a PC running an OB TraceVue system,
placed and operated in the patient's vicinity must be powered via a separating transformer
(compliant with IEC/EN 60601-1 A1: 2012) that ensures mechanical fixing of the power cords
and covering of any unused power outlets.
• Do not use USB devices with own power supplies unless an appropriate separation device is used
(either between USB interface and device or between device and power).
1 Introduction
25
CAUTION
•FM20/FM30 only: Although this is an electrical Class II device, it has a protective earth
conductor which is needed for EMC purposes.
• Always use the supplied power cord with the three-prong plug to connect the monitor to AC
mains. Never adapt the three-prong plug from the power supply to fit a two-slot outlet.
CAUTION
The use of accessories, transducers and cables other than those specified may result in increased
electromagnetic emissions or decreased electromagnetic immunity of the device.
WARNING
Do not use cordless/mobile phones or any other portable RF communication system within the
patient vicinity, or within a 1.0 m radius of any part of the fetal monitoring system.
WARNING
For paced patients: The radiated SRR power of the CL SpO2 and NBP Maternal Cableless
Measurement Devices, the CL Transmitter, and other sources of radio-frequency energy, when used in
very close proximity of a pacemaker, might be sufficient to interfere with pacemaker performance.
Due to shielding effects of the body, internal pacemakers are somewhat less vulnerable than external
pacemakers. However, caution should be exercised when monitoring paced patients.
In order to minimize the possibility of interference, avoid positioning and wearing the Cableless
Measurement Devices in very close proximity to a pacemaker. Consult the pacemaker manufacturer
for information on the RF susceptibility of their products
CAUTION
Fetal parameters, especially ultrasound and ECG, are sensitive measurements involving small signals,
and the monitoring equipment contains very sensitive high gain front-end amplifiers. Immunity levels
for radiated RF electromagnetic fields and conducted disturbances induced by RF fields are subject to
technological limitations. To ensure that external electromagnetic fields do not cause erroneous
measurements, it is recommended to avoid the use of electrically radiating equipment in close
proximity to these measurements.
CAUTION
The device should not be used adjacent to, or stacked with, other equipment unless otherwise
specified.
1Introduction
26
WARNING
•Leakage currents: If several items of equipment used to monitor a patient are interconnected,
the resulting leakage current may exceed allowable limits.
•ECG electrodes: NEVER allow ECG electrodes to contact other electrical conductive parts,
including earth.
WARNING
The fetal/maternal monitors are NOT intended for use during defibrillation, electro-surgery, or MRI.
Remove all transducers, sensors, and accessories before performing electro-surgery, defibrillation, or
MRI, otherwise harm to the patient or the user can result.
WARNING
The fetal/maternal monitors are not intended for use for ECG measurements on patients connected
to external electrical stimulator or with cardiac pacemakers.
1
27
Device Classification and Names within this Manual
New cableless measurements for fetal and maternal monitoring supplement the Avalon fetal monitor
family. The Avalon CL solution consists of the Avalon CL base station, the Avalon
CL transducers, and the IntelliVue CL Pods.
The IntelliVue CL Pods are only used for maternal measurements within the Avalon CL solution.
To differentiate between the CL transducers and the CL Pods, the CL Pod are also referred to as
maternal measurement Pods. The following table provides an overview of all the devices within the
solution.
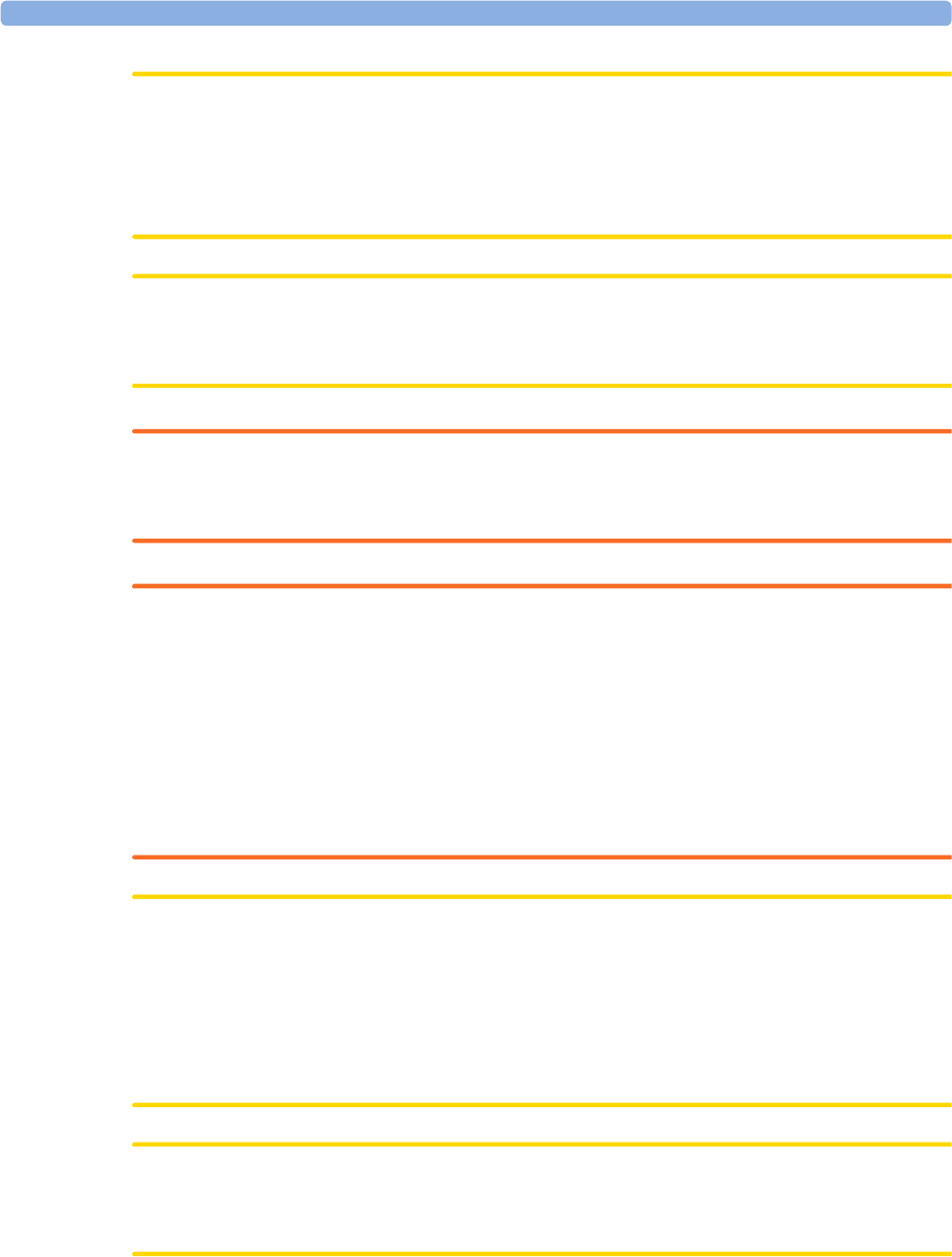
Avalon FM20/FM30 and FM40/
FM50
Wired Transducers
Avalon CL Base Station
Avalon CL Transducers
IntelliVue CL Pods
FM20/
FM30
M2702A and M2703A
FM40/
FM50
M2704A and M2705A
Avalon CL
Base Station
866074
US
transducer
wired
M2736A
Avalon CL
Toco+ MP
Transducer
cableless
866075
IntelliVue
CL NBP
Pod
cableless
865216
1Introduction
28
Toco/ Toco
MP
transducer
wired
M2734A and M2734B
Avalon CL
US
Transducer
cableless
866076
IntelliVue
CL SpO2
Pod
cableless
865215
Toco+
transducer
with ECG/
IUP
capability
wired
M2735A
Avalon CL
ECG/IUP
Transducer
cableless
866077
Patient
Module for
ECG/IUP
M2738A
Avalon FM20/FM30 and FM40/
FM50
Wired Transducers
Avalon CL Base Station
Avalon CL Transducers
IntelliVue CL Pods

2What's New
29
2What's New
This section lists the most important new features and improvements to the fetal monitors and their
user interface introduced with Release J.3.
You may not have all of these features, depending on the fetal monitor configuration purchased.
What's New in Release J.3
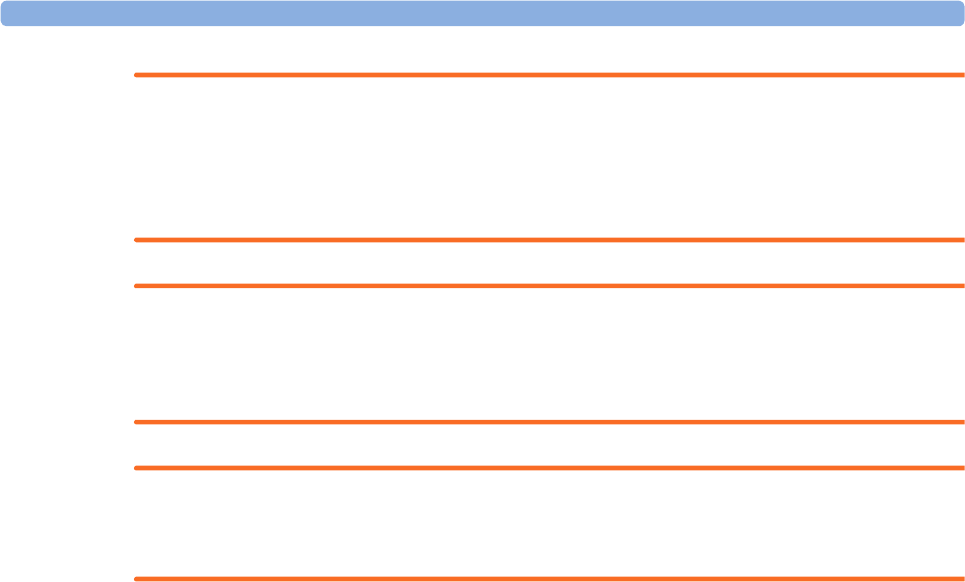
Avalon CL Transducer System
The Avalon CL system provides cableless monitoring with the Avalon FM20/FM30 and FM40/FM50
with the same functionality and performance as the wired measurement devices (e.g. twin and triplets
monitoring). The Avalon CL has a straight-forward handling and operating concept. The cableless
transducers are assigned by simply docking them at the base station, no further configurations are
necessary.
The Avalon CL system includes the following features:
• Cableless monitoring of twins and triplets
• Cableless maternal measurement Pods CL SpO2 and CL NBP
• Maternal pulse from a CL Toco+MP (Smart Pulse) transducer
• A cableless ECG/IUP transducer measuring IUP and fetal/maternal ECG
• Watertight cableless transducers that can be used to monitor in water
• Patient call that pages an ambulating mother with an audible signal emitted by the worn CL
transducers.
• Out of range audible signal emitted by the worn CL transducers to inform an ambulating mother
that she is approaching the limit of the active signal area of reach.
• A transducer finder LED on all cableless transducers to help identify the assigned transducer
Support For Use of Maternal Cableless Measurement Devices
The IntelliVue measurement pods are patient-worn, battery powered measurement devices for SpO2
and NBP. The devices provide measurement values on the built-in display and communicate them to
the fetal monitor using the wireless short range radio (SRR) interface of the Avalon CL base station.
Maternal Temperature Measurement
To measure maternal temperature, the new optional Tympanic Temperature device (866149) is
available for the Avalon fetal monitors. The measurement data is:
• fully documented at the local recorder and the OB system,
• can be displayed as a numeric on the screen,
• and is printed out on the recorder trace strip.

2What's New
30
Manually Entered Maternal Temperature Measurements
Manually measured temperatures can be entered manually into the fetal monitor and stored in the
database. They are also displayed as a numeric on screen, and are printed out on the recorder trace if
required.
New Design for the User Interface
The user interface for the fetal monitors has been redesigned to bring the presented information into
the foreground, letting the structural elements such as keys and frames retreat into the background.
Additionally special regard was given to making the "look and feel" similar to that of standard software
products.
New SmartKeys
•The Start ECG SmartKey is renamed to Record ECG .
•With the Call Patient SmartKey you can now page patients who are ambulating wearing cableless
transducers.
•With the Tele Info SmartKey you can call up the Tele Info window on the fetal monitor display. In
the Tele Info window you can control and view the status of the cableless transducers from the
connected Avalon CL system.
•With the Enter Temp SmartKey a pop-up window opens showing a numeric pad for entering
externally measured maternal temperature values.
Coincidence INOP Tone
When the cross-channel verification detects that the signal of the maternal heart rate coincides with the
fetal heart rate, the Coincidence INOP is issued with a tone at the fetal monitor. The Coincidence
INOP tone has a configurable delay.
Increased Internal Back-up Memory
The internal back-up memory is now able to store data at least 3 hours.
USB Interface
An optional USB interface allows the use of USB printers, bar code readers, and input devices such as
a keyboard or mouse.
Flexible Nurse Call Interface
An optional Flexible Nurse Call interface allows now the connection of a nurse call device to the fetal
monitors.
DHCP Support
The DHCP support offers an alternative to BOOTP. DHCP (dynamic host configuration protocol)
enables the fetal monitors to request an IP address (internet protocol address) from the connected
network (OB TraceVue/IntelliSpace Perinatal) automatically.

2What's New
31
Data Export Support
You can now export measurement values from the monitor to other devices via the LAN or RS232
interface.
NBP Configurable Measurement Sequence
Up to four measurement cycles can be set up which will run consecutively. For each cycle you can set
the number of measurements and the interval between them. By setting the last cycle to run
continuously you can have regular measurements continue after the sequence has run.
Alarms Enhancements
• In addition to the standard blue INOPs, some INOPs can now be configured as red or yellow
INOPs to provide a severity indication (ECG Leads Off, NBP Cuff Overpress, Cuff Not Deflated).
A small number of INOPs are always yellow or red to indicate a severity corresponding to red and
yellow alarms.
• For the invasive pressure measurement, the extreme pressure alarms Extreme High and Extreme
Low can be made available for your monitor in Configuration Mode and are additional to the
standard High and Low limit alarms.
•The
Review Alarms window now shows when the monitor was switched on (after being switched
off for longer than 1 minute) and any changes made to the Standby and paired status.
• In order to improve alarming on asystole under certain conditions, you can set Asystole Detect. in
Configuration Mode to Enhanced. In enhanced mode an asystole alarm will be suppressed for up
to five seconds if a valid beat-to-beat Pulse is detected from a Pressure.
Alarm Reminder
In Configuration Mode you can set now an Alarm Reminder. The Alarm Reminder emits an audible
reminder of alarm conditions that remain active after the alarm is acknowledged. This reminder may
take the form of a repetition of the alarm tone for a limited time, or an unlimited repetition of the
alarm tone (this is the same as a new alarm). The interval between silencing the alarm and sounding the
reminder tone can be set to one, two, or three minutes.
Auto Free
In Configuration Mode you can now set an Auto Free setting which discharges a patient automatically
when the fetal monitor is powered off, or is in standby mode for a set time. Only the demographic
patient data is deleted, the trace data is not affected.
What's New in Release G.0
Battery Option and Patient Transport Improvements for the Avalon
FM20 and FM30
• For the FM20/FM30, you can now switch between battery-powered and mains-powered operation
without interrupting monitoring. The monitor is connected to the AC mains power with the
external power supply.
• Traces of multiple patients can be recorded during transport and can automatically be uploaded to
OB TraceVue/IntelliSpace Perinatal (Rev. G or higher) when reconnected.

2What's New
32
• A bed hanger is available as a mounting option, especially for patient transport purposes within
healthcare facilities.
Maternal Pulse from Toco MP Transducer
• The new Toco MP transducer can measure the maternal pulse rate, in addition to the other
available sources; MECG, SpO2, and NBP. With sensors built-into the bottom cover of the Toco
MP transducer, and using a measurement technology similar to SpO2, it automatically gives you an
additional maternal pulse source for Cross-Channel Verification (CCV).
• The new Toco MP transducer is standard for the whole product family, Avalon FM20 to FM50.
Non Stress Test (NST) Analysis as Clinical Decision Support (CDS)
Application
• The optional NST Report Trace Interpretation feature allows you to automatically interpret FHR
traces and to generate a printed NST report, equivalent to the NST report functionality in OB
TraceVue Rev. F and based on the NICHD guidelines from 1997.
• The application can be adapted to domestic or hospital guidelines. A report of the NST analysis
can be printed automatically or on demand.
• This software option is available for the whole product family, Avalon FM20 to FM50.
FHR Sound Source
A newly-connected fetal measurement (FHR or DFHR) automatically becomes the FHR sound
source, without the need for manual intervention. If you prefer the previous behavior, this can be
changed in Configuration mode (Audio Select setting).
FHR Numeric Display
The FHR numeric display shows changes in fetal heart rate faster and is updated more frequently.
Improved FHR and DFHR Label Concept
A DFHR numeric (fetal heart rate from DECG measurement) now also has a unique number (DFHR1,
DFHR2, or DFHR3) to allow easier identification of the related trace in OB TraceVue/IntelliSpace
Perinatal.
New SmartKeys
You can control fetal heart sound volume directly with the configurable SmartKeys (FHR Vol. Up and
FHR Vol.Down) on the monitor’s screen.
Now the Toco Baseline SmartKey automatically turns into the Zero IUP SmartKey when switching to
IUP measurement.
Trace Separation On/Off Operation
Now you can switch the Trace Separation on or off in every FHR setup menu.
NBP
• To prevent the NBP measurement from being switched on or off accidentally, this operation is
now only available in Configuration Mode.

2
33
• You can enter the NBP setup menu by touching the NBP numeric (on the screen) before the first
measurement is taken.
• Algorithm enhancements (more tolerant of movement artifacts).
Alarms
• There is an individual Alarm Tone Volume setting for Yellow, Red and Cyan alarms.
• The new alarm settings available in Configuration Mode are:
–AutoIncrease Vol and IncreaseVolDelay
–AlarmsOffAtStart
–ConfirmAlarmsOff
For a detailed description of the settings see the Configuration Guide.
CCV INOP
There is a new INOP (technical alarm) Coincidence after 1 minute of persistent coincidence warning.
New Demographic Fields
•Date of Birth and Gestational Age can be entered for complete documentation in an NST Report
(supporting the optional NST Trace Interpretation software feature).
•A
Middle Name field is now available in the admission form - whether it appears is configurable.
• Two additional ID fields Lifetime ID and Encounter ID can also be configured to appear, and their
names can be customized to fit hospital requirements. The default label of the Lifetime ID is MRN.
Recorder
• It can now be configured whether the recorder speed can only be adjusted in Configuration mode,
or also in Monitoring mode.
• When recorder speed is changed, a new trace header is printed. Date and/or time changes are
annotated in real time recording.
Stored Data Recording
Printing progress is shown while printing a trace from the internal back-up memory.
FHR Sound Volume
Volume steps are optimized in the low range to allow finer FHR sound volume adjustments.
Avalon CTS
An antenna symbol is displayed next to MECG waves if an Avalon CTS is used.

2What's New
34

3 Basic Operation
35
3Basic Operation
This chapter gives you an overview of the monitor and its functions. It tells you how to perform tasks
that are common to all measurements (such as entering data, switching a measurement on, changing
some monitor settings, and setting up the recorder). The alarms section gives an overview of alarms.
The remaining sections tell you how to perform individual measurements, and how to care for and
maintain the equipment.
Supported Measurements
The following Fetal measurements are supported:
Fetal
Monitor or
Model
Fetal Heart Rate
(FHR) via US
(including Twins) Triple FHR via US Toco
FHR via Direct ECG
(DECG)
Intrauterine
Pressure (IUP)
FM20
Standard Optional Standard - -
Optional Optional Standard - -
FM30
Standard Optional Standard Standard Standard
Optional Optional) Standard Standard Standard
FM40
Standard Optional Standard - -
Optional Optional Standard - -
FM50
Standard Optional Standard Standard Standard
Optional Optional Standard Standard Standard
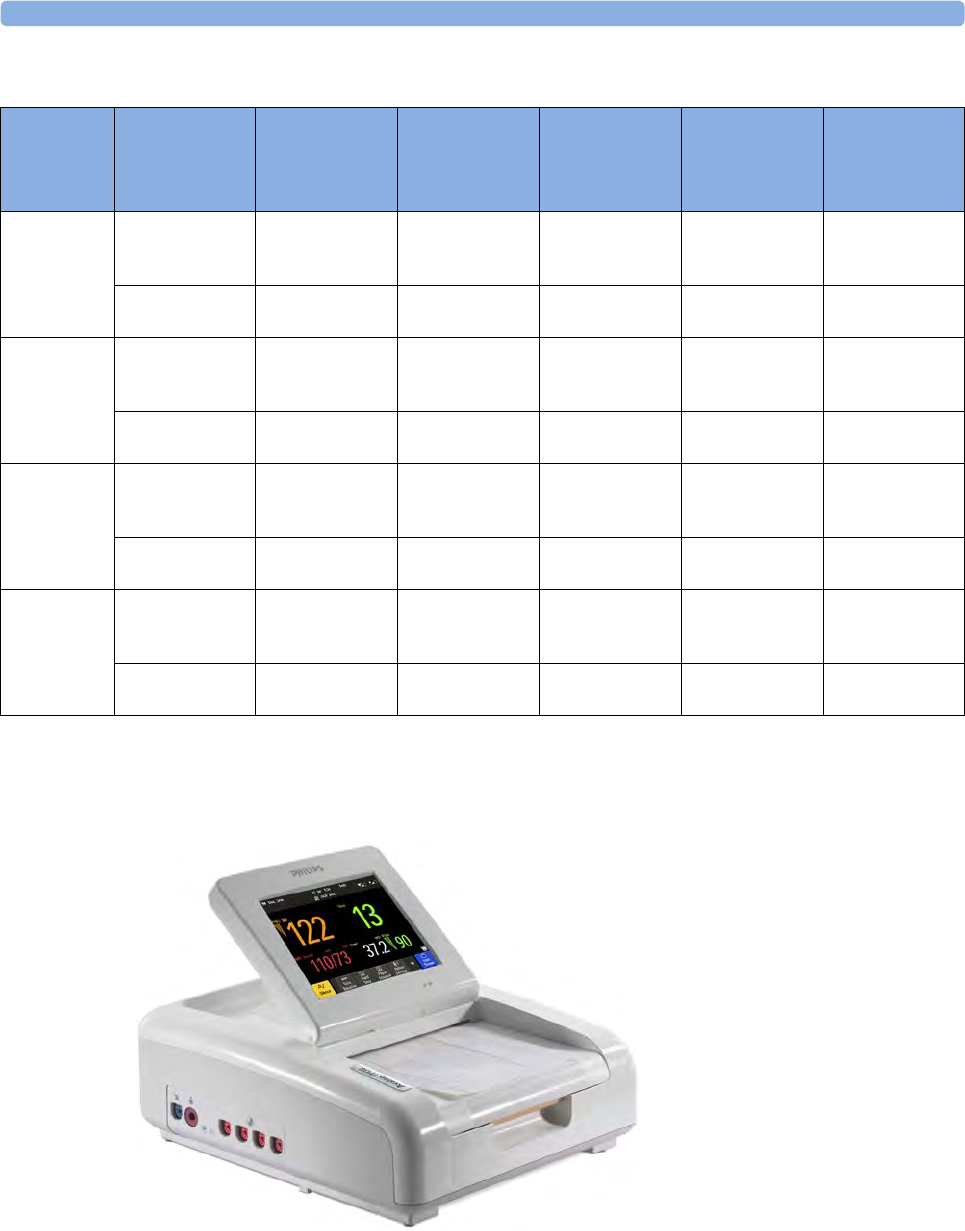
3 Basic Operation
36
The following Maternal measurements are supported:
Avalon FM20 and FM30
This section outlines the capabilities of your monitor.
Fetal
Monitor or
Model
Maternal Heart
Rate (MHR) via
Maternal ECG
Electrodes
Maternal ECG
(MECG) Wave
Maternal Pulse
from Toco
Non-invasive
Blood Pressure
with Pulse Rate
Pulse Oximetry
(Maternal SpO2)
with Pulse Rate
Maternal
Temperature
FM20
Standard -Standard Optional (built-in) -Optional
(Interface cable
and manual entry)
Standard -Standard Optional
(cableless)
Optional
(cableless)
-
FM30
Standard Standard Standard Optional (built-in) Optional (built-in) Optional
(Interface cable
and manual entry)
Standard Standard Standard Optional
(cableless)
Optional
(cableless)
-
FM40
Standard -Standard Standard (built-in) Standard (built-in) Optional
(Interface cable
and manual entry)
Standard
-
Standard Optional
(cableless)
Optional
(cableless)
-
FM50
Standard Standard Standard Standard (built-in) Standard (built-in) Optional
(Interface cable
and manual entry)
Standard Standard Standard Optional
(cableless)
Optional
(cableless) -
3 Basic Operation
37
Avalon FM20
The Avalon FM20 fetal/maternal monitor provides a solution for external fetal monitoring
applications, and optional noninvasive maternal vital signs.
You can monitor fetal heart rates (FHRs) externally using ultrasound, uterine activity and maternal
pulse using an external Toco transducer, and the maternal heart rate (MHR) with maternal ECG
electrodes, and optionally, noninvasive blood pressure and maternal oxygen saturation (SpO2).
Measurements are displayed on a 6.5-inch color display as numerics. The display is a touchscreen, and
you operate the monitor using this touchscreen interface. The integrated recorder documents fetal and
maternal measurements as well as the user-defined annotations.
You can connect the monitor to an OB TraceVue/IntelliSpace Perinatal system via the RS232
connection, or over a LAN connection (with OB TraceVue Revision E.00.00 and later, or IntelliSpace
Perinatal Revision H.0 and later).
Avalon FM30
The Avalon FM30 fetal/maternal monitor offers a solution for both external and internal fetal
monitoring applications, and optional noninvasive maternal vital signs.
The Avalon FM30 shares all the features and capabilities of the Avalon FM20. In addition, you can
monitor one FHR internally with a direct fetal electrocardiogram (DECG), uterine activity internally
using an intra-uterine pressure (IUP) catheter together with a Toco+ transducer or patient module.
The Avalon FM30 carries the IP label, indicating that it is capable of intrapartum monitoring.
FM20/30
with
Battery
Option
#E25 Only
The battery option for the FM20/30 provides support for the in-transport monitoring of all
measurements when disconnected from a power supply. Existing data storage is automatically
uploaded to OB TraceVue or IntelliSpace Perinatal after reconnecting it to the system. Trace printing
during transport is also possible.

3 Basic Operation
38
Avalon FM40 and FM50
This section outlines the capabilities of your monitor.
Avalon FM40
The Avalon FM40 fetal/maternal monitor provides a solution for external fetal monitoring
applications, and noninvasive maternal vital signs.
You can monitor fetal heart rates (FHRs) externally using ultrasound, uterine activity using an external
Toco transducer, and the maternal heart rate (MHR) via maternal ECG electrodes, and non-invasive
blood pressure and maternal oxygen saturation (SpO2).
Measurements are displayed on a 6.5-inch color display as numerics. The display is a touchscreen, and
you operate the monitor using this touchscreen interface. The integrated recorder documents fetal and
maternal measurements as well as the user-defined annotations.
You can connect the monitor to an OB TraceVue/IntelliSpace Perinatal system with the RS232
connection, or over a LAN connection (with OB TraceVue Revision E.00.00 and later, or IntelliSpace
Perinatal Revision H.0 and later).
Avalon FM50
The Avalon FM50 fetal/maternal monitor offers a solution for both external and internal fetal
monitoring applications, and noninvasive maternal vital signs.
The Avalon FM50 shares all the features and capabilities of the Avalon FM40. In addition, you can
monitor one FHR internally with a direct fetal electrocardiogram (DECG), and uterine activity
internally using an intra-uterine pressure (IUP) catheter together with a Toco+ transducer or patient
module.
The Avalon FM50 carries the IP label, indicating that it is capable of intrapartum monitoring.
3 Basic Operation
39
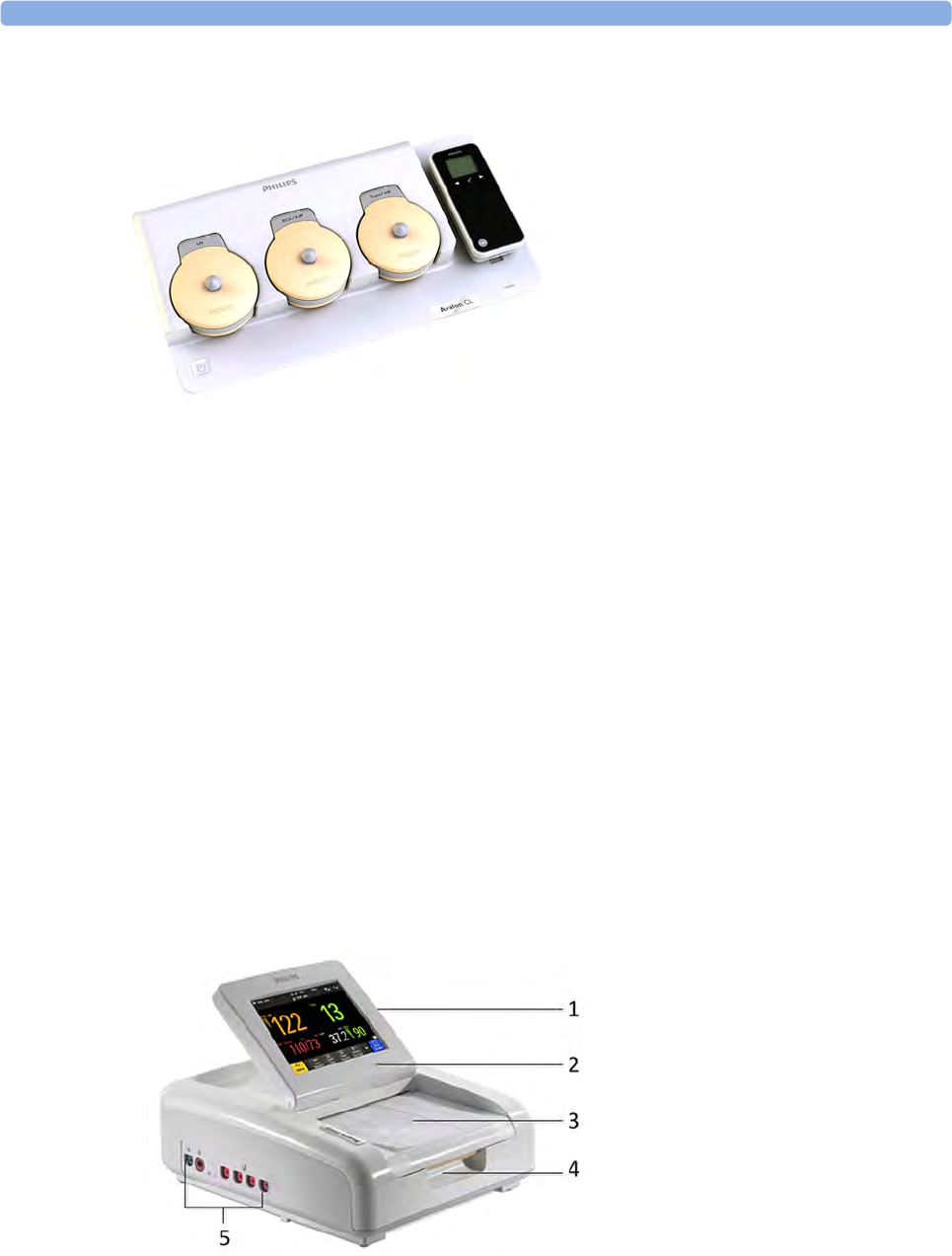
Avalon CL Transducer System
The Avalon CL Fetal Transducer System lets you monitor the patient continuously with cableless
transducers during the antepartum period, labor, and delivery. You can monitor the fetal heart rate
(FHR) using noninvasive CL Ultrasound transducers, or invasively using the CL ECG/IUP transducer
with the direct electrocardiogram (DECG). The uterine activity can be monitored using an external
CL Toco+ MP transducer. The fetal and maternal parameters are measured and transmitted via radio
frequency from the CL transducers to the CL base station, eliminating the need for patient cables.
With the Avalon CL Transducer System you can monitor a single fetus, twins and triplets.
The Avalon fetal monitor (FM20-FM50) connected to the CL base station displays and records the
parameters. All the CL transducers are watertight. You can continuously monitor patients in a bath or
shower using the CL Toco+MP and the CL Ultrasound transducers.
The system should only be used by, or under the direct supervision of, a licensed physician or other
health care practitioner, who is trained in the use of FHR monitors and in the interpretation of FHR
traces.
Getting to Know Your Avalon FM20/FM30
Overview
1Touchscreen Display (tilt and fold)
2Power LED
3Paper Drawer
4Paper Drawer release
5Connectors
3 Basic Operation
40
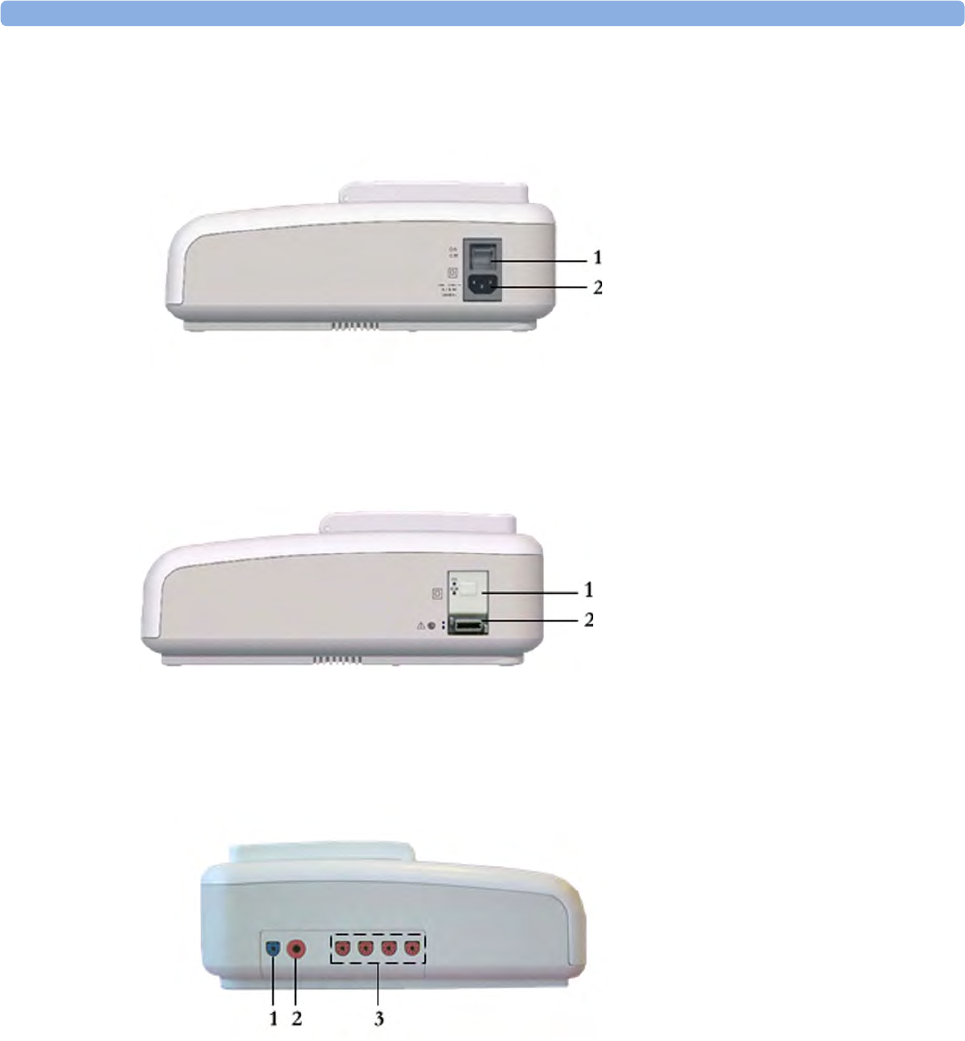
Right Side
with
Battery
Option
Left Side
Each of the fetal sensor sockets accepts any fetal transducer, one Avalon CL or one Avalon CTS
Cableless Fetal Transducer System base station, or an event marker.
1On/Off Switch
2Power Connector
1On/Standby Switch
2MSL Connector
1SpO2 Socket (optional)
2Noninvasive Blood Pressure Socket
(optional)
3Fetal Sensor Sockets
3 Basic Operation
41
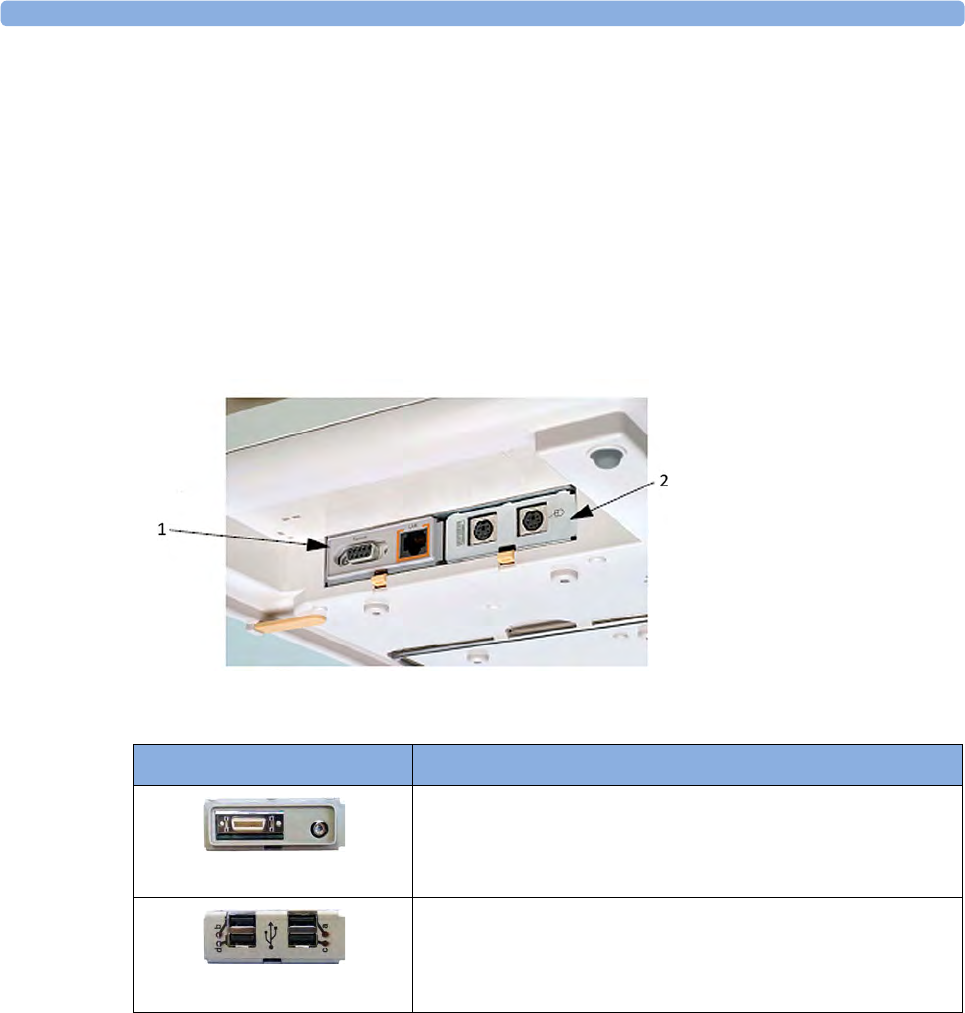
Bottom
There are five optional interfaces available for the Avalon FM20/30 monitor:
• LAN/RS232 system interface
• Dual PS/2 interface
• MIB/RS232 interface
• Flexible Nurse Call
• USB port
You can use two of the five optional interfaces at the same time.
1LAN/RS232 system
interface
2Dual PS/2 system
interface
Optional Interfaces Description
Flexible nurse call interface card
USB ports

3 Basic Operation
42
Rear
Getting to Know Your Avalon FM40/FM50
Front
Connect any fetal sensor or patient module at the fetal sensor sockets, including an Avalon CL or an
Avalon CTS via interface cable (with red connector).
1Display Release
2Carrying Handle
3Built-in Stand
1Touchscreen color display
2Transparent paper guide with
tear-off edge
3Paper eject button
4Power LED
5On/Standby switch
6Recorder paper table
7Fetal sensor sockets
8Noninvasive blood pressure socket
9SpO2 socket
3 Basic Operation
43
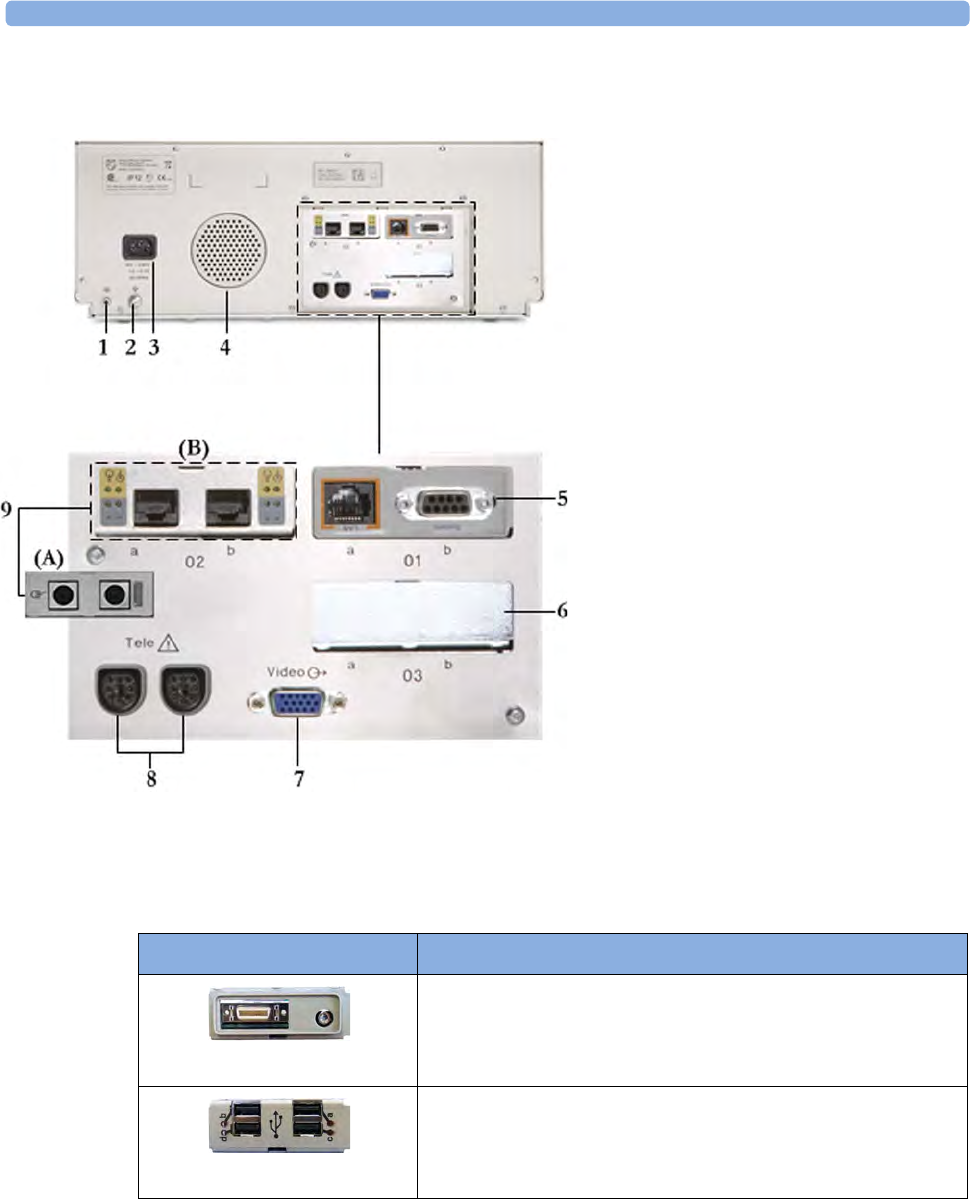
Rear
Two Avalon CL, or one Avalon CTS can be also connected to the Telemetry interface sockets using
the interface cable (with black connector).
Additional Optional Interfaces
1Reserved for future use: protective
earth intended for use in system
installations.
2Equipotential grounding point
3Power cord connector
4Loudspeaker
5Slot 01 for optional LAN/RS232
system interface (for connection to an
obstetrical information and
surveillance system)
6Slot 03 reserved for future use
7Video output (VGA)
8Telemetry interface
9Slot 02 for optional interfaces: Either
dual PS/2 system interface (A) for
mouse and keyboard connection) Or
MIB interface (B) for external touch
screen connection.
Optional Interfaces Description
Flexible nurse call interface card
USB ports

3 Basic Operation
44
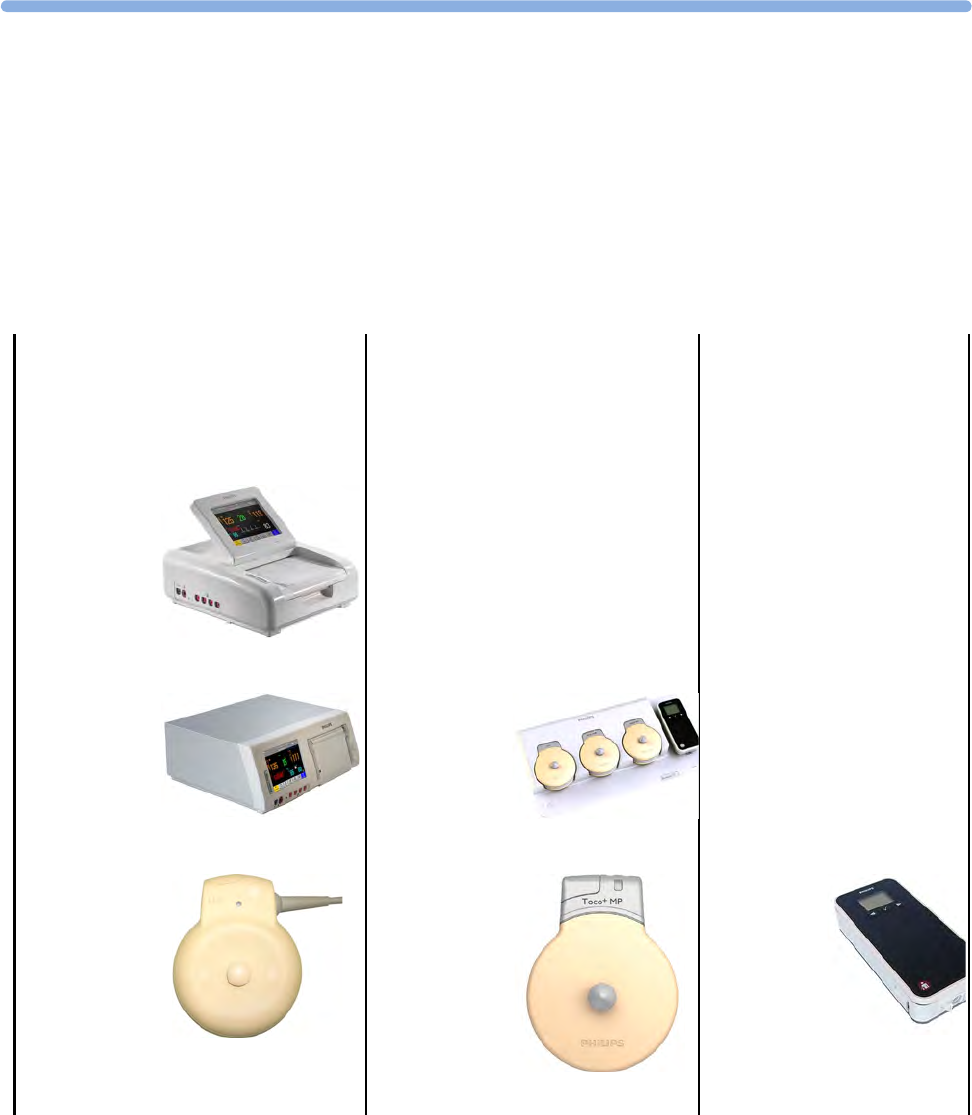
Transducers
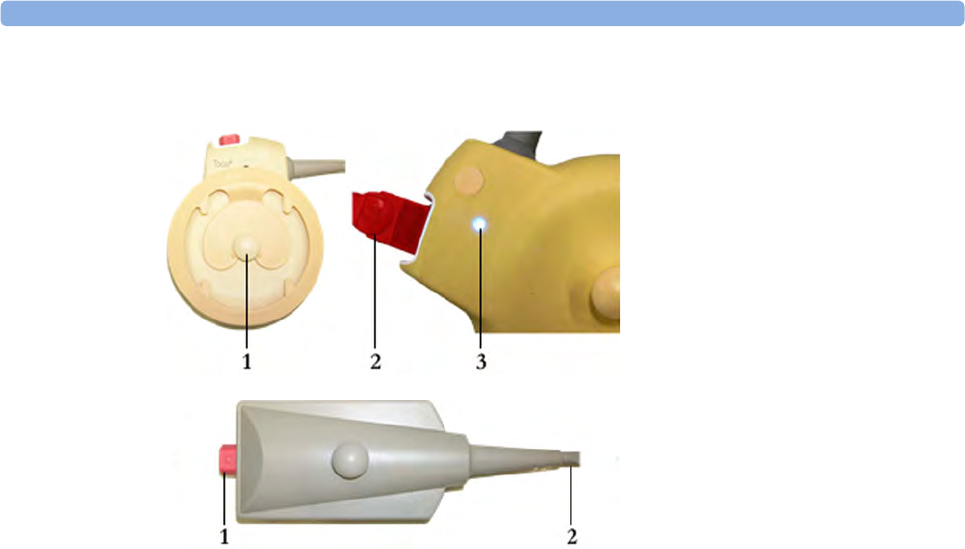
Toco (M2734A) and Toco MP Transducer (M2734B)
1Transducer finder LED - lights up
on the transducer providing the
measurement source
2"MP" for M2734B "Toco MP"
transducers (additionally capable
of providing the maternal pulse
measurement)
3Belt Button
Ultrasound Transducer (M2736A)
1Cable - connects to any of the
four fetal sensor sockets on the
monitor
The M2736AA US transducer is
identical to the M2736A US
transducer, including all specifications
Toco+ Transducer with ECG/IUP capability
(M2735A)
1Connector - for connecting
ECG/IUP adapter cables
(M2735A Toco+ transducer only)
3 Basic Operation
45
1Butterfly belt clip (shown fitted;
for use with belts without button
holes)
2Close-up of MECG adapter cable
connected to Toco+ transducer
3Close-up of active finder LED
Patient Module for ECG/IUP (M2738A)
1Connector - for connecting ECG/
IUP adapter cables (same as for
Toco+ transducer)
2Cable - connects to any of the four
fetal sensor sockets on the monitor

3 Basic Operation
46
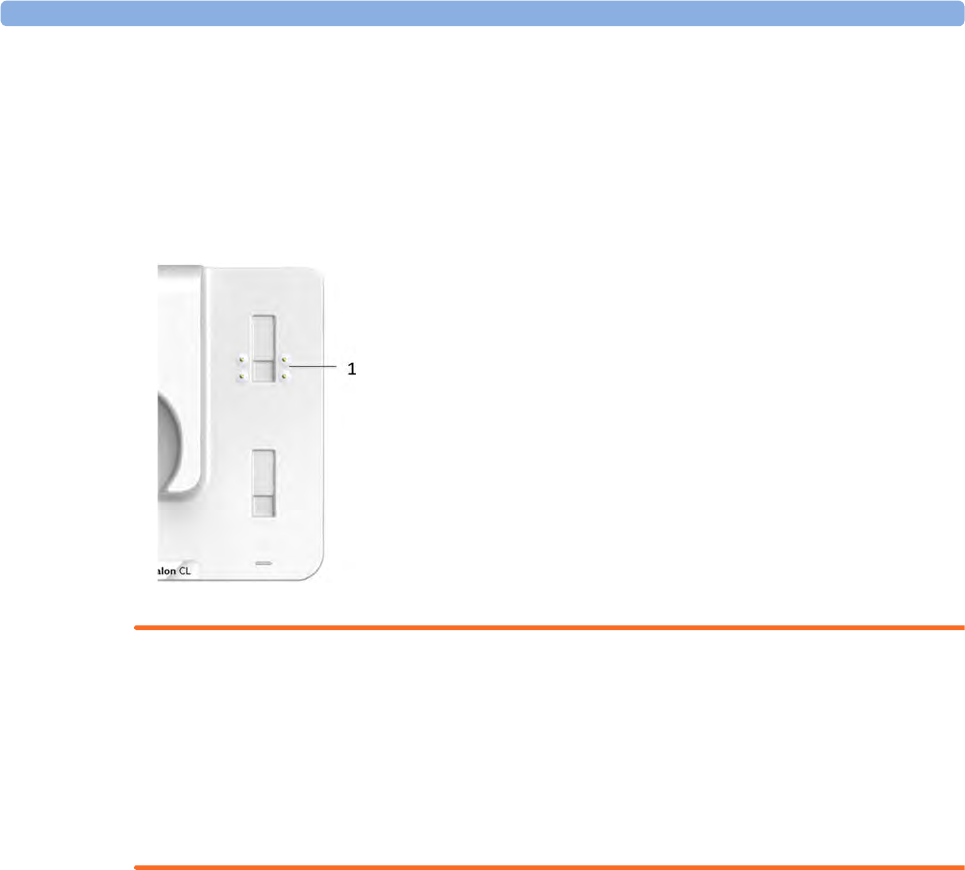
Getting to Know Your Avalon CL
Front
WARNING
• To avoid magnetic interference affecting the mode of the pacemaker, ensure that the Avalon CL
base station does not come into close contact with implanted pacemakers.
• This equipment generates, uses, and radiates radio-frequency energy, and if it is not installed and
used in accordance with its accompanying documentation, may cause interference to radio
communications. Operation of this equipment in a residential area may cause interference, in
which case the users must take whatever measures may be required to correct the interference.
1Transducer docking slots
2On/Standby button with power LED
3Device label
4LED for optional cableless pods
5Docking slots for cableless pods

3 Basic Operation
47
Docking Slot for Cableless Transducers
The Avalon CL base station has three docking slots to mechanically hold the CL transducers. The
flexible electronic contacts identify the transducer type after docking. The transducers are charged
while docked. The base station has a built-in radio interface with an integrated antenna to
communicate with the transducers for assignment, configuration, and for transducer firmware updates.
The transducers can be controlled with the base station and the fetal monitor.
On/Standby Button
Pressing the On/Standby button switches the Avalon CL base station between the two modes On and
Standby.
If you switch the base station to On, the LED button lights up green. The base station is ready for use.
The CL transducers are charging. When the transducers are picked up from their docking slot, the base
station sets up the radio communication to the CL transducer automatically. Wired transducers
connected to the fetal monitor are disabled, and the antenna symbol for the CL transducer is displayed
on the screen of the fetal monitor.
If you switch the base station to Standby, the LED button turns off. The base station is now in
Standby mode. The docked CL transducers continue charging. No radio communication occurs, any
existing radio communication is stopped.
If the LED of the On/Standby button turns red, it indicates a technical problem has occurred that
needs your attention. Check your monitor for a possible related INOP message.
1On/Standby button
3 Basic Operation
48
Docking Slots for Cableless Measurement Pods
The Avalon CL base station has one docking slot to mechanically hold an IntelliVue CL pod. The
electronic contacts identify the CL pod type after docking. The CL pod is charged while docked. The
LED under the docking slot indicates the battery status of the CL pod. The base station has a built-in
short range radio interface with an integrated antenna to communicate with the CL pod for assignment
and configuration. The CL pod can be controlled with the base station and the fetal monitor.
WARNING
Short range radio connections are subject to interruption due to interference from other radio sources
in the vicinity, including microwaves, bluetooth devices, WLAN devices (802.11b,g,n) and cordless
phones. Depending on the strength and duration of the interference, the interruption may occur for an
extended period. A loss of connection, due to moving out-of-range, interference, or for other reasons,
is indicated with a No Host Monitoring INOP (here the host is the fetal monitor) on the NBP or
SpO2 Pods, or a cl NBP Disconnect or cl SpO₂ Disconnect INOP at the fetal monitor. Correct
channel configuration is important, see the Configuration Guide for details.
1Docking slot for CL pods
3 Basic Operation
49
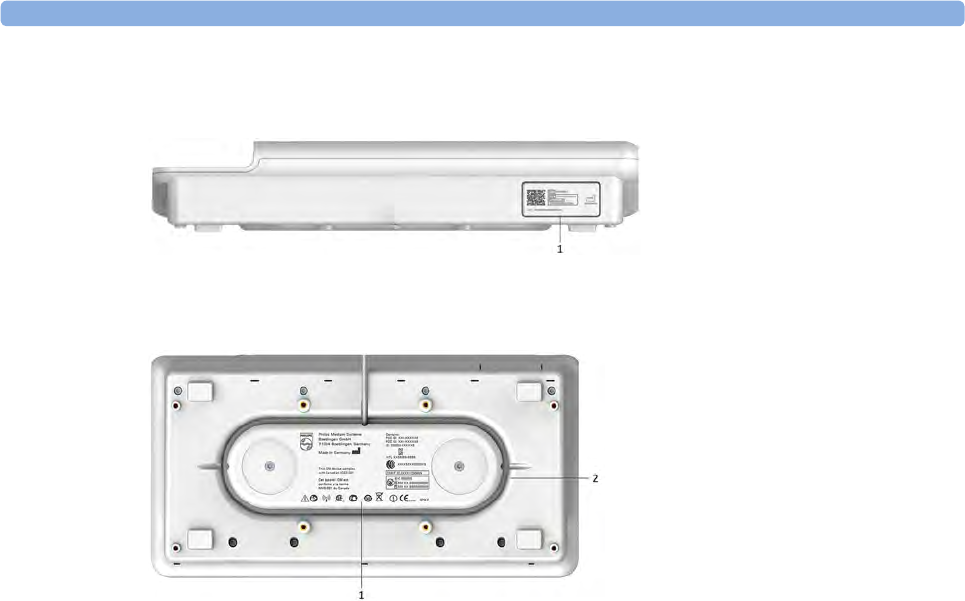
Rear and Bottom
1Name plate
1Manufacturer label
2Cable reel
3 Basic Operation
50
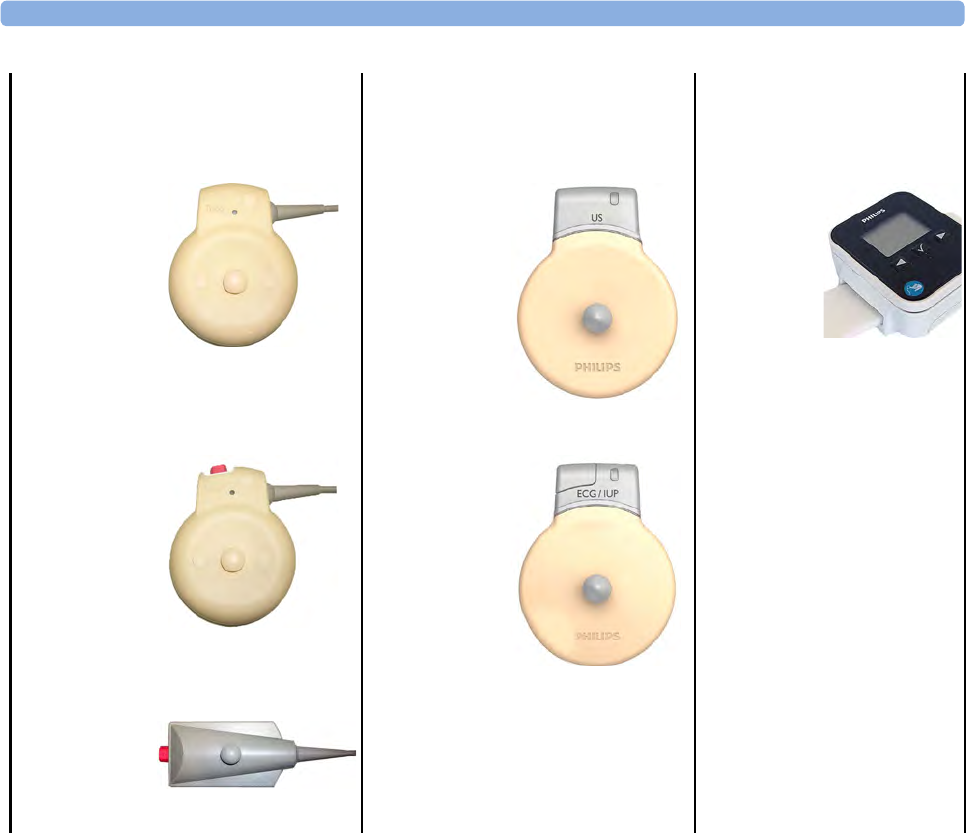
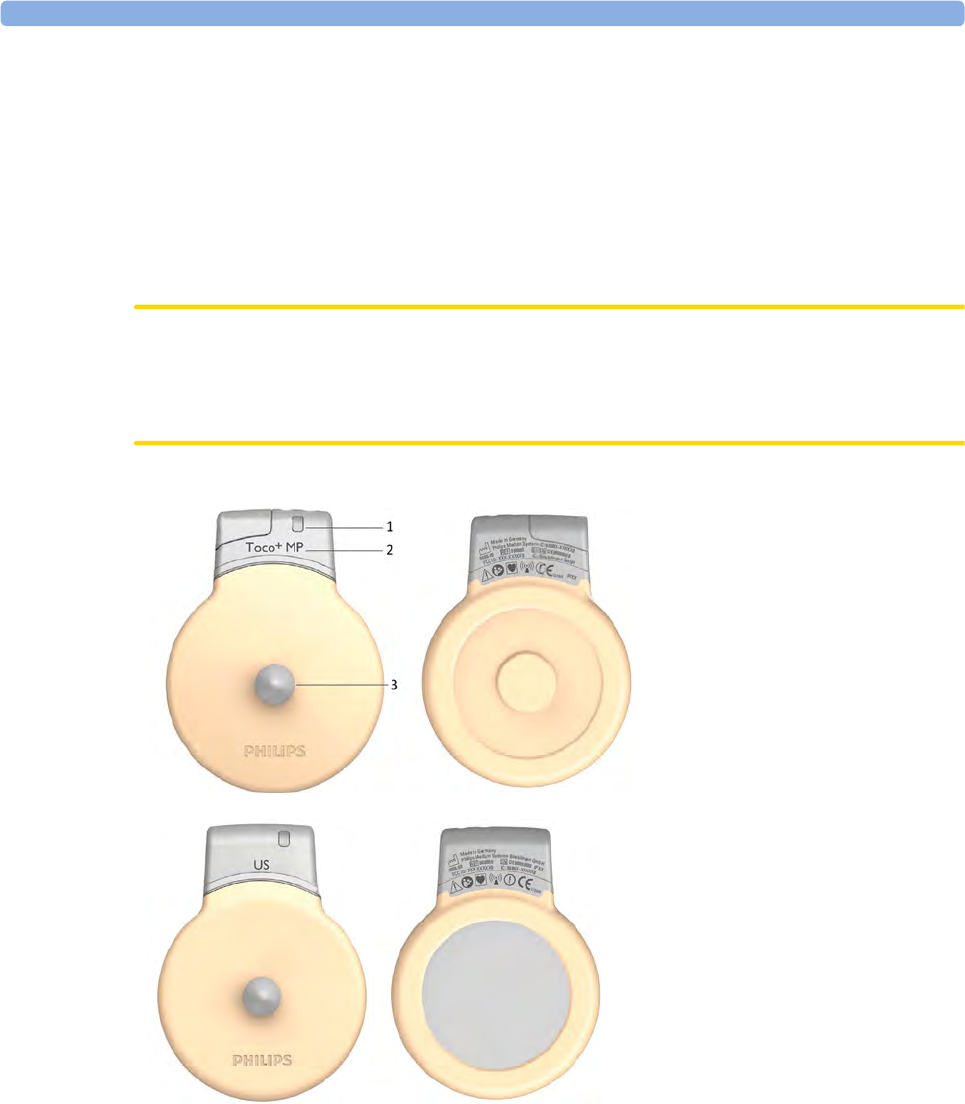
Cableless Transducers
The cableless Avalon CL transducers have a built-in radio interface with an on-board, integrated
antenna. The fetal monitor connected to the Avalon CL base station can control the transducer using
radio communication. The transducer transmits measured values, alarms, and status information to the
fetal monitor.
The cableless transducers are assigned by simply docking them at the Avalon CL base station. If they
are picked up from their docking slot at the base station, they are automatically activated.
CAUTION
To ensure the correct assignment of CL transducers to the fetal monitor in use, always dock them at
the base station connected to that fetal monitor before use. This is particularly important when you
add an additional CL transducer that was previously docked at another base station.
1Transducer finder LED - lights
up on the transducer providing
the measurement source.
2CL Toco+ MP transducers
(additionally capable of providing
the maternal pulse measurement)
3Belt button
CL Ultrasound transducer
3 Basic Operation
51
Radio Range of CL Transducers
The CL transducers have a operating range around the base station of at least 70 m in the line of sight.
Obstructions as walls, metal doors, elevators and other environment structures can lead to signal loss.
The Tele symbol indicator and the Tele Info window on the monitor's display (see “Screen
Elements” on page 56 and “Tele Info Window” on page 92)
provide information on the status of the signal strength.
When a patient is approaching the end of range, the US sound is replaced by an artificial QRS sound
(like DECG), and the DECG and MECG waves are no longer displayed on the monitor.
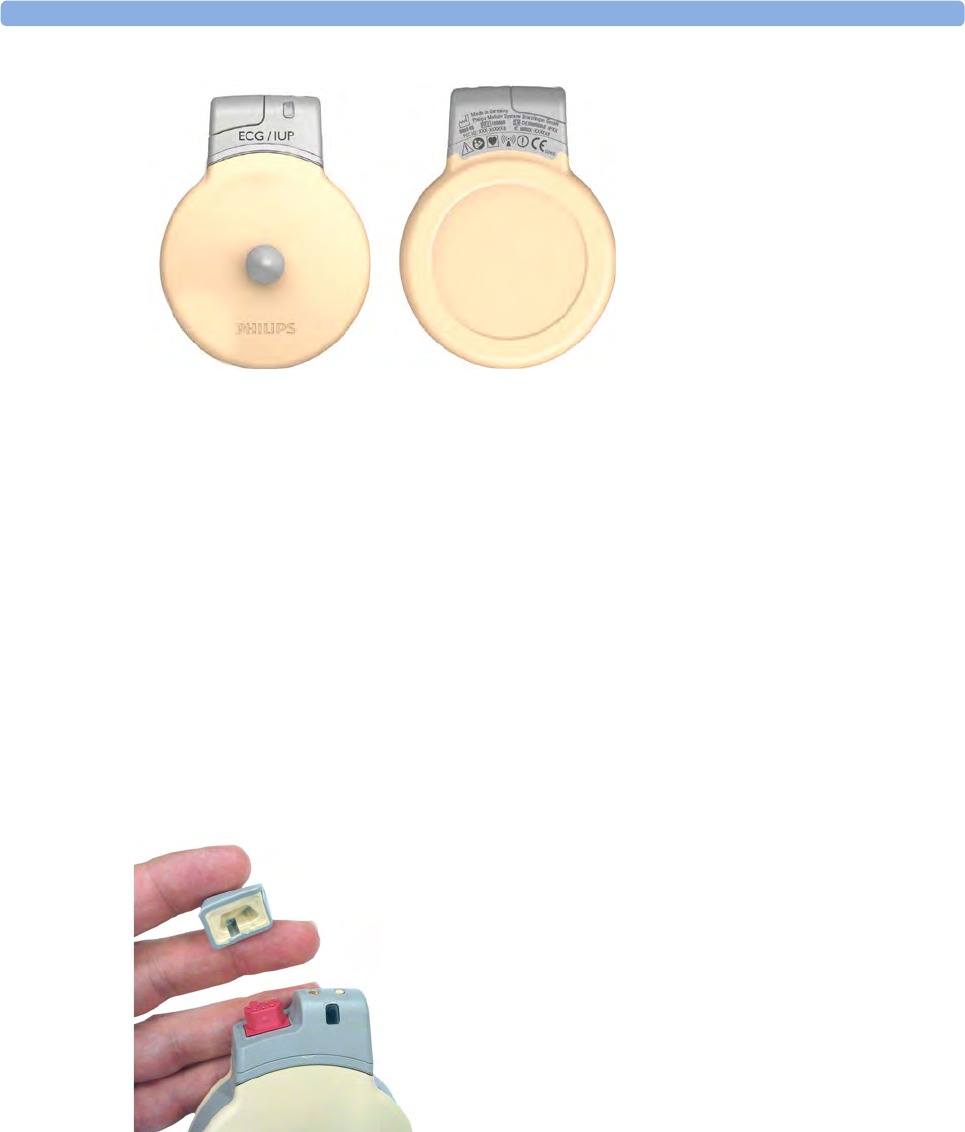
Connector Cap for the CL Toco+ MP Transducer
The CL Toco+MP transducer is delivered with a connector cap covering the MECG/DECG/IUP
connector. The connector cap is designed to cover the connector, not to protect it from water. (The
connector itself is water-proof and may be immersed in water). You can reorder lost connector caps in
a kit of 10 (989803184841).
CL ECG/IUP transducer
3 Basic Operation
52
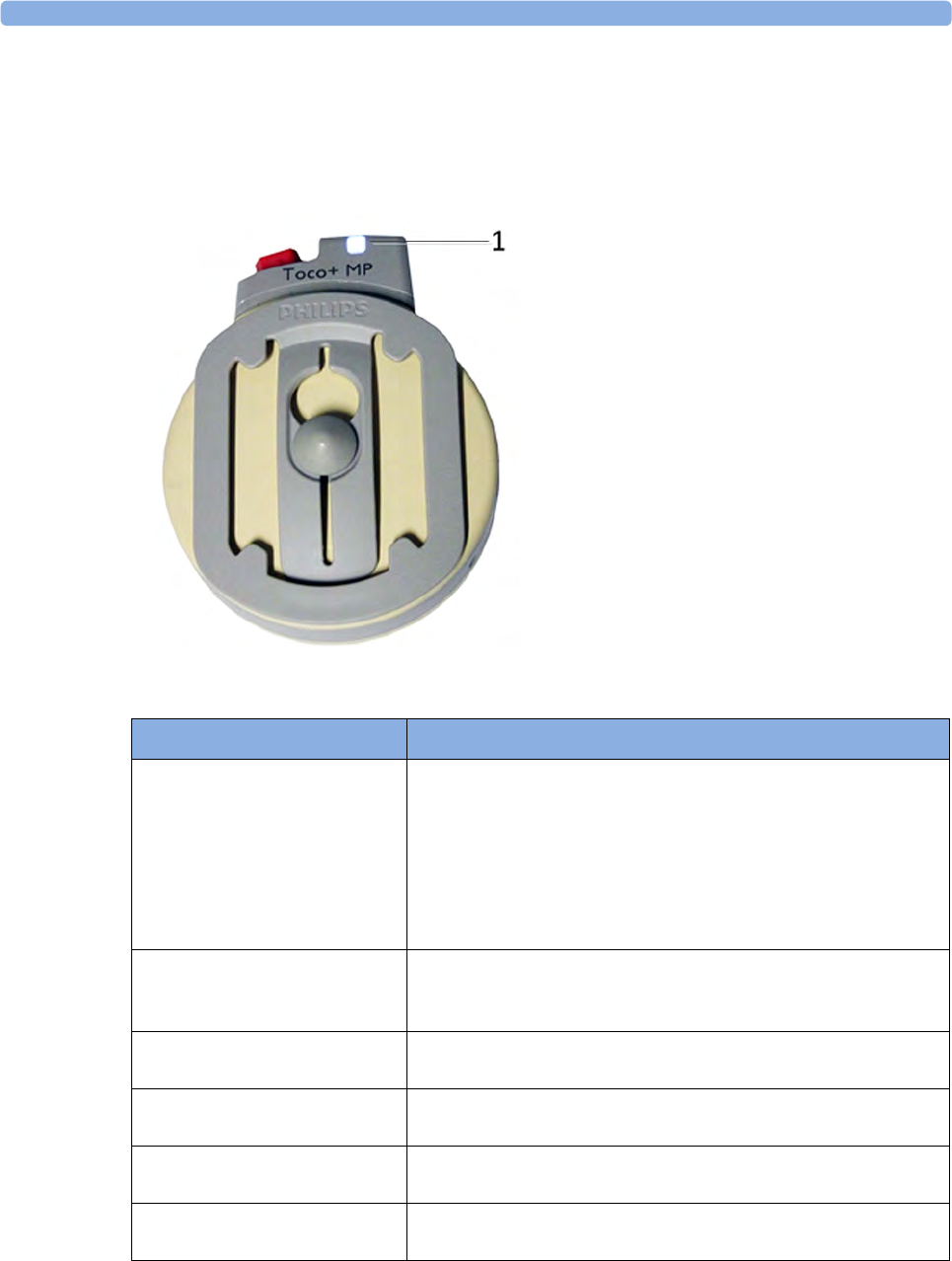
Cableless Transducer LED Indication
The cableless transducers have a multi-color LED that indicates the status of the transducer with
specific colors. This LED remains visible when the transducer is correctly attached to the transducer
belt (Philips standard belt).
1LED
LED Status Meaning
White The LED lights up to identify the US transducer among other US
transducers, and to easily verify the correct transducer assignment
(transducer finder). The transducer finder LED is controlled by
the fetal monitor. Click on the numerics to identify the
corresponding US transducer.
The LED also lights up when the mother is paged with the Call
Patient SmartKey.
White one short blink The LED shortly lights up to indicate that the transducer
successfully opened a radio communication with the base station
and that it is ready to use.
Green The LED lights up green when the transducer is fully charged and
docked at the base station.
Yellow The LED lights up yellow when the transducer is charging and
docked at the base station.
Red The LED lights up red when the transducer is out of battery and
has to be recharged.
Cyan The LED lights up cyan to indicate a technical problem that needs
your attention. Check your fetal monitor for a related INOP.
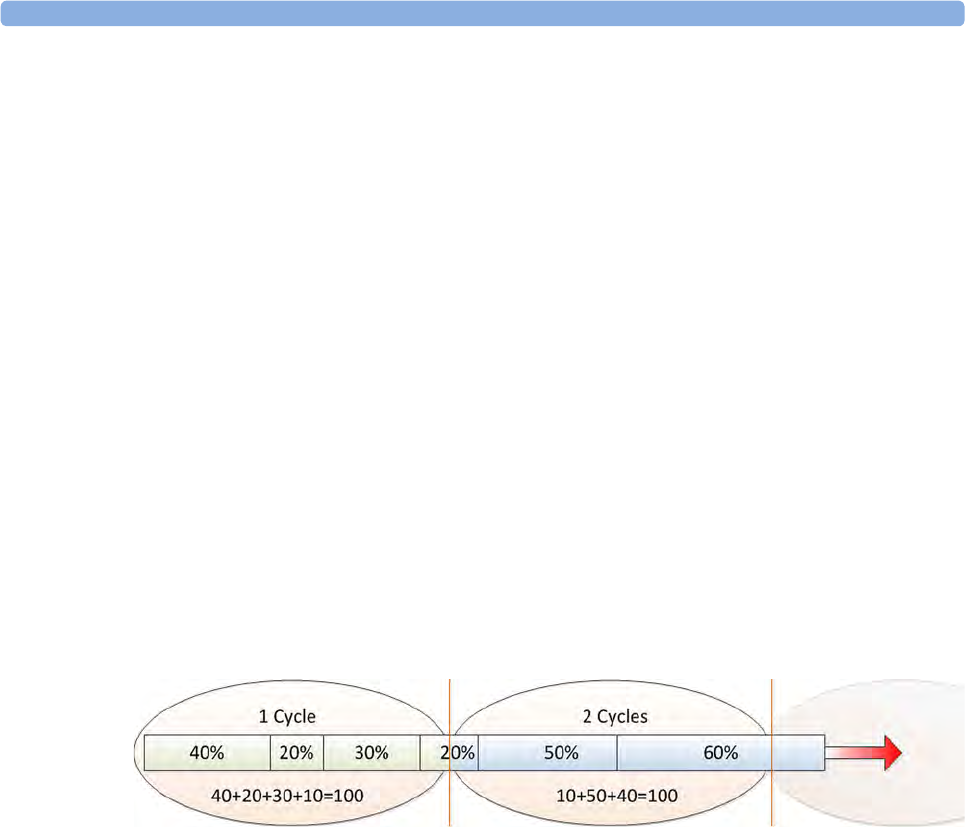
3 Basic Operation
53
CL Transducer Battery
Battery replacement is recommended after 500 charge/discharge cycles *2) or if the battery is older
than 4 years whatever is reached first. If the battery of a cableless transducer has aged and an exchange
of the battery is highly recommended, a prompt message is displayed at the fetal monitor for ca. 60
seconds. The prompt is repeated whenever the Tele Info window is opened until the battery is
replaced.
Depending on the transducer type the following messages are displayed:
cl US battery has aged. Replacement strongly recommended
cl Toco battery has aged. Replacement strongly recommended
cl ECG/IUP batt has aged. Replacement strongly recommended
If you are getting this message contact your service personnel so they can replace the CL transducer's
battery.
The date of manufacture and number of charge/discharge cycles can be inquired on the connected
fetal monitor.
For battery cycle and battery life specification of the CL pods (NBP and SpO2) please refer to the
Service Guide of the Cableless Measurements.
Charge Cycle
The CL transducer batteries are designed for frequent recharging. A complete charging cycle is only
reached and counted, when all recharging periods equal a 100% charge (900 mAh equal 8 hours
continued operation).
Audio Signal CL Transducers
The Avalon CL transducers have two audio signals:
• If a tone sequence is played, the transducer was triggered by the fetal monitor to page the patient
wearing it, or to locate a not docked transducer.
• An INOP tone indicates that the transducer has detected a technical problem (INOP). Check your
fetal monitor for a related INOP message.

3 Basic Operation
54
CL Pods
The two CL Pods provide measurement values for SpO2 and NBP on the built-in display, and
communicate them to other system components using a wireless short range radio (SRR) interface.
They are controlled with SRR from the Avalon CL base station and the connected fetal monitor.
The maternal measurement pods are easily assigned by docking them at the Avalon CL base station.
The SpO2 Pod and the NBP Pod have an LCD display and three keys for basic operation e.g. to assign
the device to a patient:
For further operational details read the IntelliVue Cableless Measurements Instruction for Use.
CL NBP Pod
CL SpO2 Pod
1Integrated LCD display
2Hard keys
3Measurement identifier
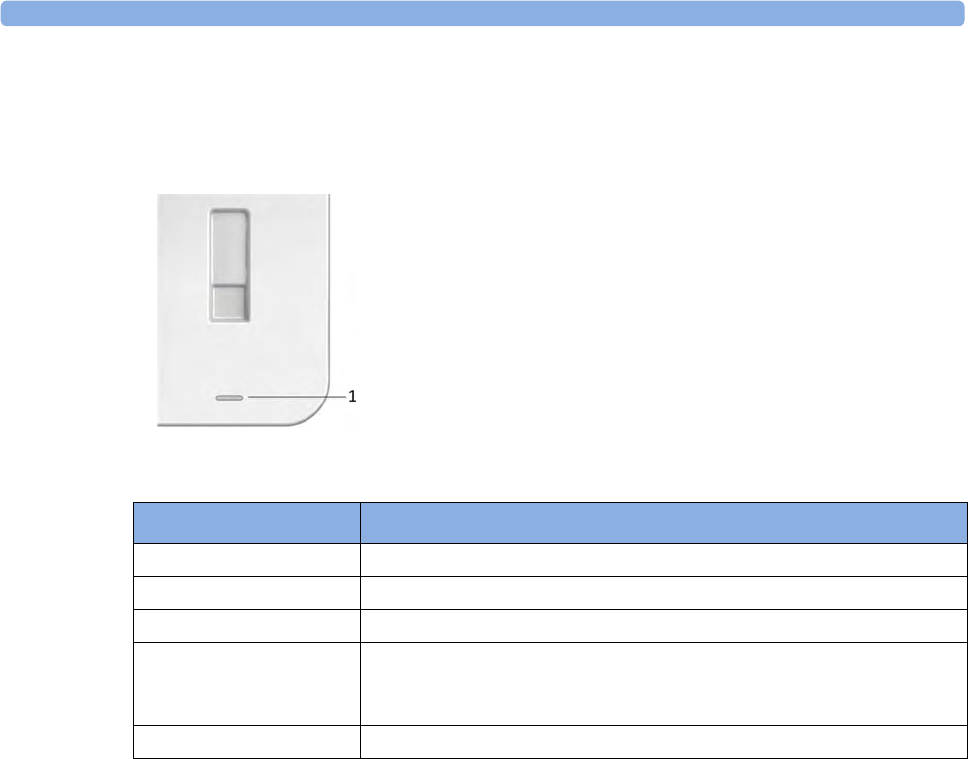
3 Basic Operation
55
Battery Status LED for CL Pods
The CL Pods do not have their own battery status LED. On the Avalon CL base station the battery
status LED for the CL Pods is located directly under the docking slot.
The battery status LED shows five different states:
Audio Signal
The Avalon CL base station has audio signals to let you know when a transducer's battery has to be
recharged, or if the base station cannot set up radio communication with a CL transducer or a CL Pod.
Only active CL transducers and CL Pods emit an audio signal.
• If the base station issues a descending tone sequence, the attempt to set up radio communication
to a CL transducer or a CL Pod has failed.
• If an interval tone is played, the battery of one or more the CL transducers or CL Pods need to be
recharged.
Operating and Navigating
Your monitor has a touchscreen. Everything you need to operate the monitor, except the on and off
switch, is contained on its screen. Most screen elements are interactive. Screen elements include
measurement numerics, screen keys, information fields, status indicators, alarms fields, and menus.
Operator
Position
The typical operator's position is in front of the monitor.
1Battery status LED for CL Pods
Status Meaning
Green The docked CL Pod is fully charged.
Yellow The docked CL Pod is charging.
Yellow blinking The communication is established with the docked CL Pod.
Cyan Indicates that the docked CL Pod or the charging slot has a technical
problem that needs your attention. Check your fetal monitor for a related
INOP message.
Off The battery status LED is off, when no CL Pod is docked.
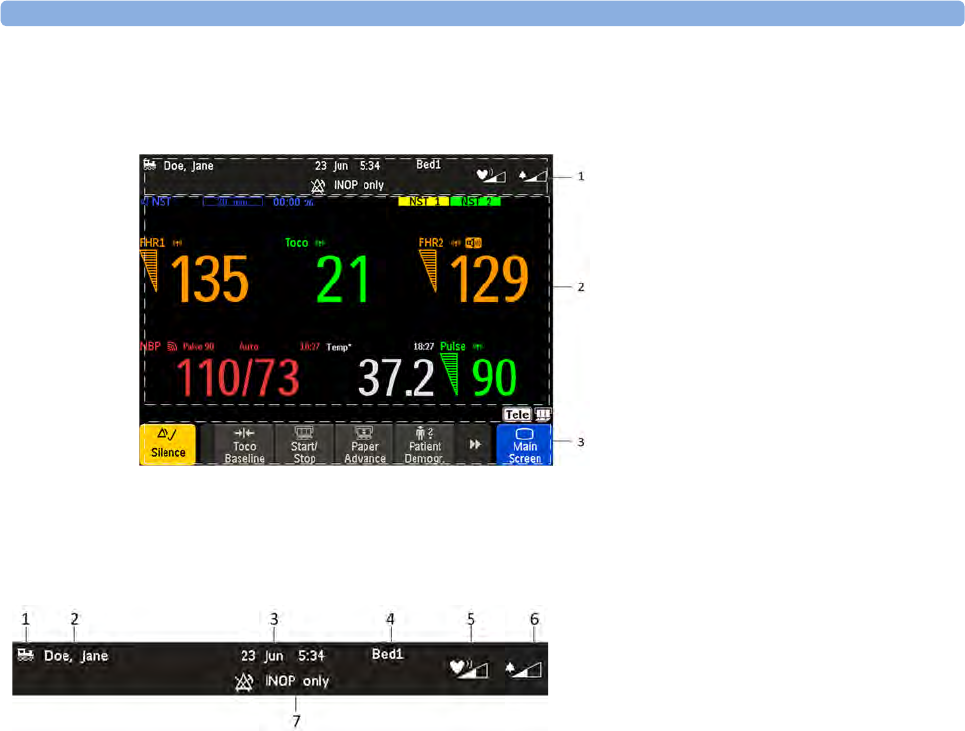
3 Basic Operation
56
FM40/50 If an optional external touch display is connected to the monitor, you can operate the monitor using
the external touch display.
Screen Elements
Monitor Information Line
1Monitor Information line
2Measurement area
3Key area
1LAN connection status indicator
only. RS232 system connection is not
indicated. The train icon indicates if
the fetal monitor is connected to OB
TraceVue/IntelliSpace Perinatal, via a
LAN cable or not.
2Patient identification
3Date and time
4Bed label (when connected to a
Philips OB TraceVue/IntelliSpace
Perinatal system)
5Fetal heart sound volume adjust/
indicator
6Alarm volume adjust/indicator
7INOP and alarm status area - shows
active alarm messages
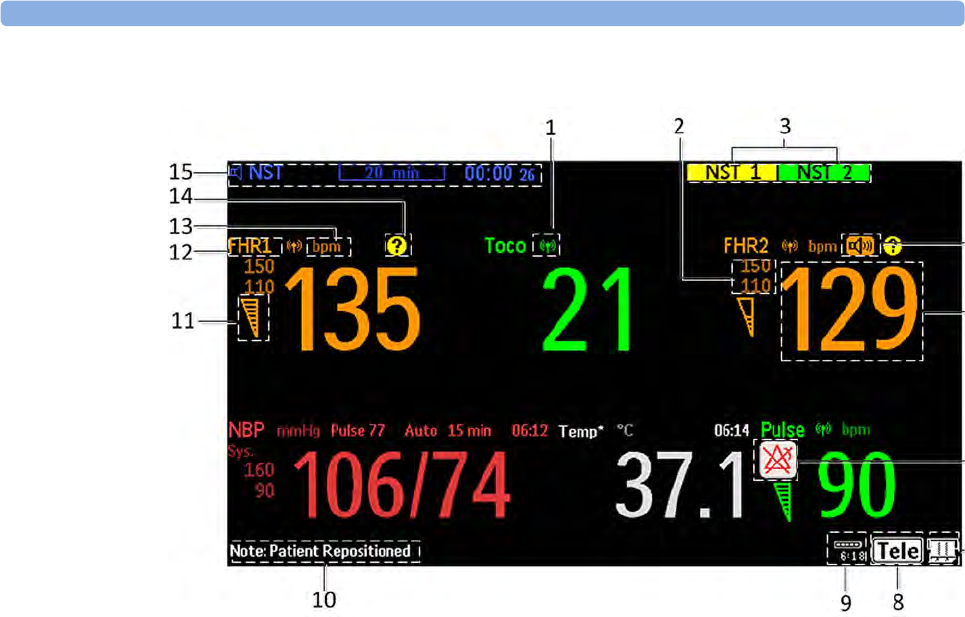
3 Basic Operation
57
Measurement Area
1Antenna symbol (indicates a cableless measurement from a connected Avalon CL or Avalon CTS
system).
2Configurable alarm limits
3NST test
4Audio source symbol
5Measurement numeric
6Alarms off symbol
7Fetal trace recorder - status indicator
8Avalon CL or Avalon CTS system - status indicator
9Battery status indicator
10 Status line - shows status and prompt messages
11 Signal quality indicator: good, acceptable, poor
12 Fetal heart rate measurement label
13 Measurement unit (configurable)
14 Cross-Channel Verification symbol (see “Cross-Channel Verification (CCV)” on page 149)
15 NST timer, if configured (default is Off)

3 Basic Operation
58
Screen Details
Icon Description
The antenna symbol indicates a cableless measurement
(Avalon CL or Avalon CTS).
Indicates a short range radio measurement (IntelliVue CL
Pods).
Signal quality indicator:
1Good
2Acceptable
3Poor
Fetal trace recorder - status indicator
Fetal recorder is on
Fetal recorder is off (when Paper Save Mode is off)
Fetal recorder is off (when Paper Save Mode is on)
There is a user-solvable recorder error (paper out, paper jam,
wrong paper scale set)
Fetal recorder is defective: call service
Avalon CL or Avalon CTS system - status indicator: An
interface cable is connected to the monitor, a base station is
connected, powered on, and at least one cableless transducer
has been taken from the base station and is active. Any
connected wired transducers are disabled.
An interface cable is connected to the monitor, the base station
is connected, powered on, and cableless transducers are ready
to use, but no cableless transducers are currently active (all are
still docked at the base station).
An interface cable is connected to the monitor, but the base
station is not connected to the interface cable, or it is
disconnected from AC mains, or is in Standby mode.
3 Basic Operation
59
Key Area
Keys
The monitor has three different types of keys.
Permanent Keys
A permanent key is a graphical key that remains permanently on the screen, giving you fast access to
functions.
The CL transducer is moved away from the base station
approaching the limit of the area of reach. The US sound is
replaced by an artificial QRS sound (like DECG). The DECG
and MECG waves are no longer displayed.
1SmartKeys - these
can vary
according to your
monitor's
configuration
2Main Screen -
which closes all
open menus and
windows and
returns to main
screen
3Scroll to display
more SmartKeys
4Silence - key
which
acknowledges all
active alarms by
switching off
audible alarm
indicators
Icon Description
Key Name Function
Silence Acknowledges all active alarms by switching off audible
alarm indicators.
Main Screen Closes all open menus and windows and returns to the
main screen.
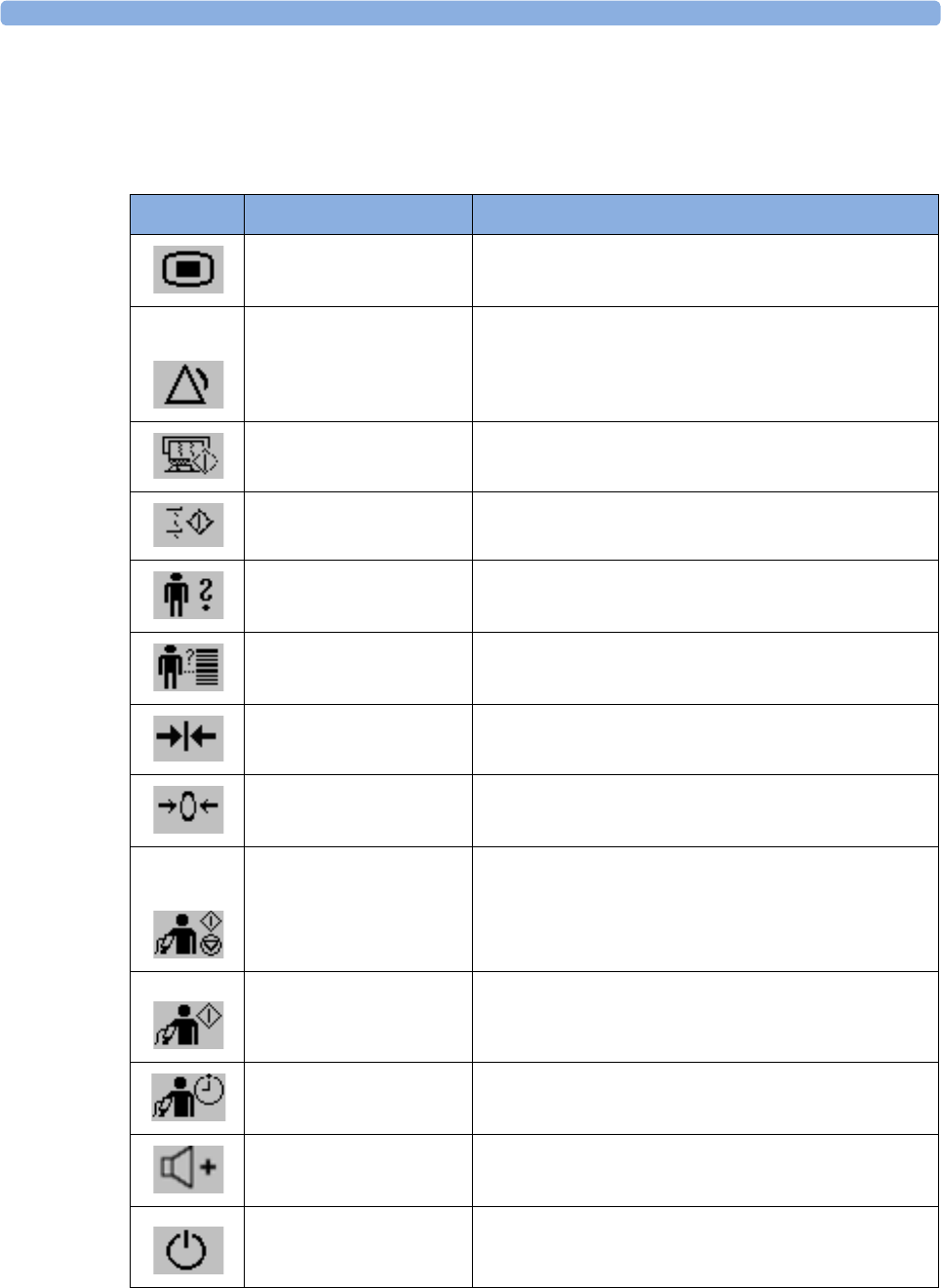
3 Basic Operation
60
SmartKeys
SmartKeys are configurable graphical keys, located at the bottom of the main screen. They give you
fast access to functions. The selection of SmartKeys available on your monitor depends on your
monitor configuration, and on the options purchased.
SmartKey Name Function
Main Setup Enters main setup menu
Pause Alarms Pauses alarm indicators. Pause duration depends on
monitor configuration. If the pause duration is infinite,
this key is labeled Alarms Off
Select again to immediately re-enable alarm indicators
Start Recordng Turns the trace recorder on
Record ECG Wave Starts printing the MECG, DECG or both waves, when
both are available
Patient Demogr. Enters the patient identification menu to admit/discharge
QuickAdmit Quick admits the patient for monitoring
Toco Baseline Resets Toco baseline
Zero IUP Zeros IUP measurement
Start/ Stop • Starts/stops manual noninvasive blood pressure
measurement
• Starts auto series
• Stops current automatic measurement within series
Start NBP • Starts manual noninvasive blood pressure
measurement
• Starts auto series
Repeat Time Sets the time interval between two noninvasive blood
pressure measurements
Sound Vol. Up Increases the fetal heart rate volume
Monitor Standby Enters the Standby mode, suspends monitoring. All
numerics and waves disappear from the display. All
settings and patient data information are retained
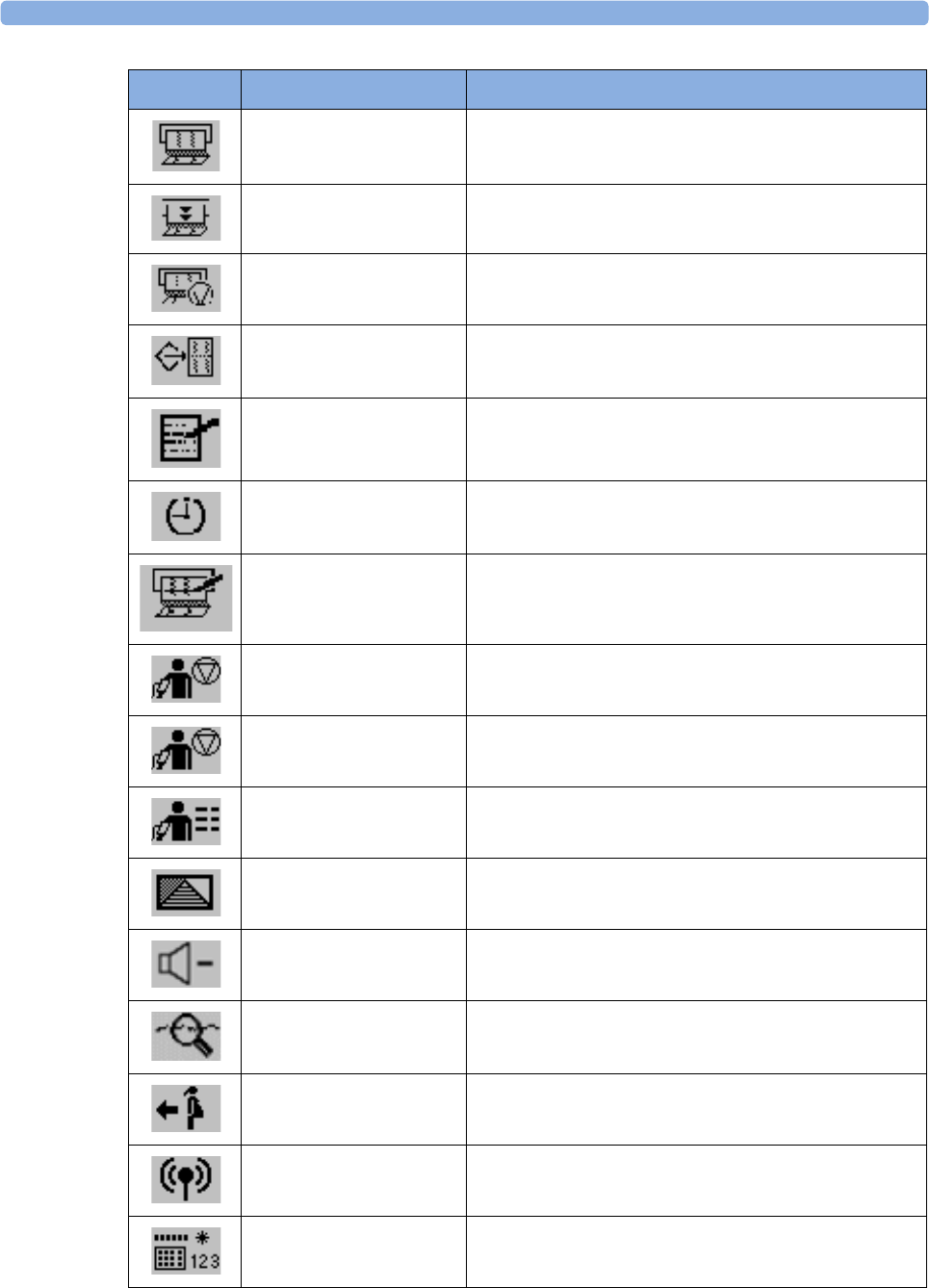
3 Basic Operation
61
Recorder Start/ Stop Turns the trace recorder on or off
Paper Advance Advances the paper automatically to the next fold
Stop Recordng Turns the trace recorder off
Stored Data Rec Prints trace data from the monitor's memory
Enter Notes Enters notes
Timer Enters NST timer window
Set Marker Marks an event
Stop All Stops all noninvasive blood pressure measurements
Stop NBP Stops manual noninvasive blood pressure measurement
Stops current automatic measurement within series
NBP Modes Access NBP mode selection and setup, with direct start/
stop function
Defaults Loads User Default
Sound Vol. Down Decreases the Fetal Heart Rate volume
NST Report Initiates an NST trace interpretation and obtains a Non-
stress test (NST) report
Call Patient Pages the patient. Only enabled if at least one
CL transducer is currently active
Tele Info Calls up the Tele Info window
Enter Temp Allows the manual input of the patient's temperature
SmartKey Name Function
3 Basic Operation
62
Pop-Up Keys
Pop-up keys are context-sensitive graphical keys that appear automatically on the monitor screen when
required. E.g. the Confirm pop-up key appears when you need to confirm a change.
Using the Touchscreen
Select screen elements by pressing them directly on the monitor's screen.
Disabling Touchscreen Operation
1To temporarily disable the touchscreen operation of the monitor, press and hold the Main Screen
permanent key for about three seconds. A red padlock will blink on the Main Screen permanent
key.
2Press and hold the Main Screen permanent key again for about three seconds to re-enable the
touchscreen operation.
Operating Modes
When you switch on the monitor, it starts up in Monitoring Mode. To change to a different mode:
1Select the Main Setup menu.
2Select Operating Modes and select a mode.
Your monitor has four operating modes. Some are passcode protected.
Mode Description Password
Protected
Monitoring Mode The Monitoring Mode is the normal operating mode to
monitor patients. You can change elements such as alarm
limits. When you discharge the patient, these elements
return to their default values.
You cannot select or change grayed out items. These items
are for your information only. To change these items, switch
to the Configuration Mode.
no
Demo Mode The Demo Mode is used for demonstration and training
purposes. Do not change into Demo Mode during
monitoring. When transducers are connected to the
monitor and the recorder is on, a demo trace is recorded.
But the demo trace is not transmitted to an information and
surveillance system such as OB TraceVue/IntelliSpace
Perinatal.
yes
3 Basic Operation
63
A field displayed at the fetal monitor screen indicates if the monitor is in Demonstration Mode,
Configuration Mode, or Service Mode. To change to a different mode, select this field.
Automatic Screen Layouts
Your monitor's preconfigured screen layouts define how measurement information is arranged on the
screen. The monitor automatically applies the correct screen layout for the measurements you are
monitoring. No user action is required.
Connecting or disconnecting transducers, or switching the noninvasive blood pressure measurement
on or off, results in an automatic adjustment of the screen layout. When a measurement is off, its
numerics are removed from the monitor's screen. The monitor stops acquiring data and generating
alarms for this measurement. If you disconnect a transducer while it is performing a measurement, the
monitor issues a disconnect INOP (and in the case of SpO2, replaces the measurement numeric with a
question mark).
Settings
This section describes the various settings available on the monitor.
Active Settings
What the monitor displays, and the way it operates, is controlled by its settings. They determine screen
content, layout, high and low alarm limits and so forth.
The "active settings" are the current settings the monitor uses, including any adjustments made by the
last user. Active settings are not permanent, but are retained after a loss of mains power.
There are also two preconfigured default settings:
•User Default
•Factory Default
Configuration Mode The Configuration Mode is for personnel trained in
configuration tasks. You can change and store the default
values and patient profiles permanently in the
Configuration Mode. These tasks are described in the
Configuration Guide. During installation, the fetal monitor
is configured for use in your environment. This
configuration defines the default settings you work with
when you switch on the fetal monitor.
yes
Service Mode The Service Mode is for trained and authorized service
personnel only.
yes
Mode Description Password
Protected
3 Basic Operation
64
User Default
The User Default is a complete configuration stored in the monitor's long-term memory. You can
store the active settings, modified to your preference, in the User Default (in Configuration Mode).
In monitoring mode, you can load the User Default settings to return to your preferred settings:
1Select the Defaults SmartKey
2Select Confirm in the dialog box to load the User Default.
Factory Default
The Factory Default is a complete configuration pre-defined at the factory. You cannot modify it. In
Configuration Mode, you can load the Factory Default as the active settings.
CAUTION
This resets all settings to factory defined values, but be aware that some values will differ from those
with which the fetal monitor was originally shipped from the factory (recorder speed and paper scale
type will need to be corrected, for instance). After loading the Factory Default, check the settings and,
if necessary, change them to the settings you normally use.
You can use the Factory Default as the basis for producing your User Default. See the Service Guide
for details.
Global Settings
General monitor configuration settings are stored in the Global Settings. These include settings for line
frequency, QRS type, and whether the monitor is automatically reset to the User Default after a power
interruption of more than one minute. You can change the Global Settings in Configuration Mode.
Changing Measurement Settings
Each measurement has a setup menu in which you can adjust all of its settings. You can enter a setup
menu:
1with the measurement numeric - select the measurement numeric on the screen to enter its setup
menu. For example, to enter the Setup FHR1 menu, select the FHR1 (fetal heart rate 1) numeric.
2with the Main Setup SmartKey - if you want to setup a measurement when the measurement is
switched off, use the Main Setup SmartKey and select Measurements. Then select the
measurement name from the pop-up list. With this SmartKey you can access any setup menu in
the monitor.
This guide always describes the entry method using the measurement's setup menu. You can use the
method you prefer.
3 Basic Operation
65
Switching the Noninvasive Blood Pressure Measurement On and
Off
The noninvasive blood pressure measurement is the only measurement that you can manually switch
on and off. To do this:
1Enter the noninvasive blood pressure measurement's setup menu.
2Select NBP to toggle between on and off. The screen display indicates the active setting.
Changing Monitor Settings
To change monitor settings such as brightness, or touch tone volume:
1Enter the Main Setup menu.
2Select the setting you want to change, or select User Interface to enter a sub menu where you can
change user interface settings.
Adjusting the Screen Brightness
1Enter the Main Setup menu.
2Select User Interface.
3Select Brightness.
4Select the appropriate setting for the screen brightness. 10 is the brightest, 1 is the least bright.
Optimum is suitable for most situations.
Adjusting Touch Tone Volume
The touch tone is the tone you hear when you select any field on the monitor screen. To adjust the
touch tone volume:
1Enter the Main Setup menu.
2Select User Interface.
3Select Touch ToneVolume, then select the appropriate setting for the touch tone volume: 10 is the
loudest and 1 is the quietest. Selecting zero switches the touch tone volume off.
Setting the Date and Time
The current date and time is displayed in its own element in the information section of the monitor
screen.
1Select the date and time screen element from the monitor's information line to enter the Date,
Time menu.
2Select, in turn, the Year, Month, Day, Hour (in 24 hour format) and Minute, as necessary.
3Select Store Date, Time to change the date and time.
3 Basic Operation
66
WARNING
Do not change the date and time setting, if the fetal monitor is connected to a Philips OB TraceVue/
IntelliSpace Perinatal system via a LAN -setup. The monitor uses the OB TraceVue/IntelliSpace
Perinatal system date and time, including daylight saving time changes. As long as the fetal monitor is
connected to the OB TraceVue/IntelliSpace Perinatal system via the LAN-setup (locomotive icon
displayed on the monitor's screen), the option to change the date and time settings at the fetal monitor
are disabled, this is not valid for RS232 connections, or the connection to other systems.
When disconnected from AC power, the monitor retains the date and time setting for at least two
months. If the monitor is off longer than two month, and the operating system detects that the date
and time settings are invalid, the monitor initiates a "cold" start and sets the date to 1 Jan 1997 and the
time to 00:00.
Checking Your Monitor Revision
1Select Main Setup, Revisions to open the Monitor Revision menu.
2From the Monitor Revision menu, select the monitor component for which you need revision
information.
Preparing to Monitor
Confirm fetal life before you begin fetal monitoring. Familiarize yourself with the basic operation
principles before you start to monitor.
CAUTION
Check the fetal monitors housing for damage before you start to monitor as part of your safety
precautions.
After you switch on the monitor:
1Check that you have the correct patient cables and transducers plugged in for the measurement
you want to monitor.
2If you use an Avalon CL or Avalon CTS system, check if the cableless transducers are ready and
charged (apparent by either a lit up green or yellow LED indicator).
3Admit your patient to the monitor (see “Admitting a Patient” on page 135).
4Check that the alarm limits, alarm and fetal heart rate volumes, patient category, and so forth are
appropriate for your patient. Change the settings if necessary.
5Refer to the appropriate measurement section for details of how to perform the measurements
you require.
6Start recording.

3 Basic Operation
67
Switching On: FM20/FM30
FM20/30 1Connect the monitor to AC mains and switch the monitor on.
– The green power-on LED lights up.
– The monitor performs a self-test as it starts up. Selftest: OK, the serial number, and revisions
for the software and firmware are printed on the fetal trace paper (if recorder Auto Start is
configured to On).
– The monitor display comes on.
– There is a start-up tone from the loudspeaker.
FM20/30
Battery
Option
• If this option has been chosen, the green power-on LED on both the external power supply and
the battery LED indicator will light up.
Switching On: FM40/FM50
FM40/50 1Connect the monitor to AC mains.
– The green LED lights up.
2Press the On/Standby switch.
– The monitor performs a self-test as it starts up. Selftest: OK, the serial number, and revisions
for the software and firmware are printed on the fetal trace paper (if recorder Auto Start is
configured to On).
– The monitor display comes on.
– There is a start-up tone from the loudspeaker.
Adjusting the Display Angle (FM20/FM30)
FM20/30 You can tilt the display on the FM20 and FM30 to one of five different positions, or you can fold it
completely down. The tilt/fold mechanism works on a one-way ratchet system. You hear a click as
each of the five positions is reached. The screen can be folded back down only after tilting the display
forwards as far as it will go.
To tilt the display from the folded position:
1Unlock the display by releasing the catch.
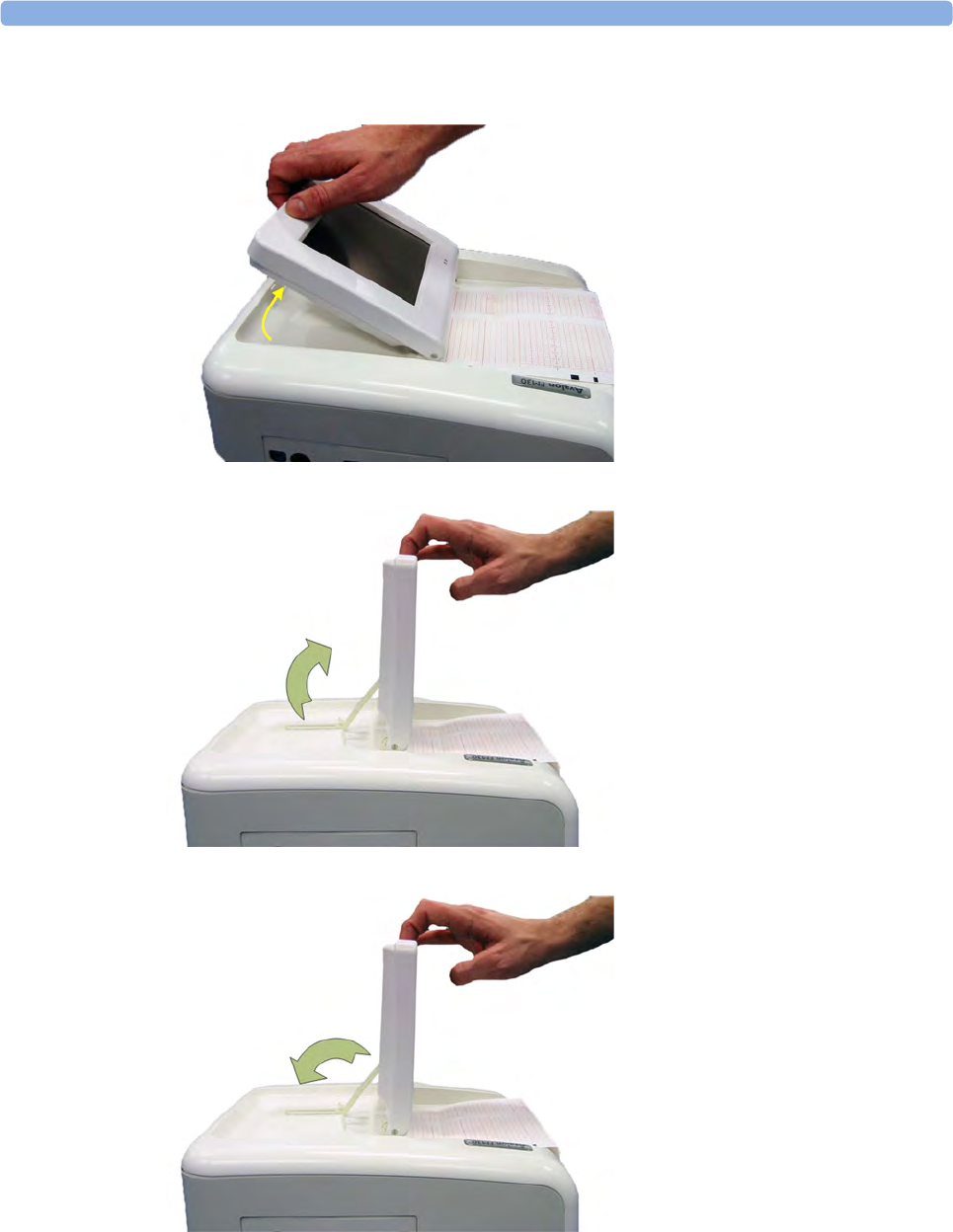
3 Basic Operation
68
2Lift the display forward. You will hear a click as the first position engages. If you want to tilt the
display further, lift the display further forward until you reach the desired angle.
3To fold the display, pull the display forwards as far as it will go
4Then push the display all the way back until it clicks shut.
If your monitor is wall-mounted, the display should be folded flat.

3 Basic Operation
69
Fastening Belts and Transducers
You can use more than one belt if, for example, you are monitoring uterine activity and FHR
simultaneously. There are two basic ways to fasten belts and transducers:
• Belts with button fixings.
• Velcro belts together with the butterfly belt clip.
What You Need
• Ultrasound transducer
• Toco MP or CL Toco+MP transducer
•Ultrasound gel
• Transducer belt (and optional butterfly belt clip, if applicable)
Using Belts with Button Fixings
1Place the transducer belt across the bed, so that the fixing button will face away from the mother
when it is fastened.
2Lie the patient on the bed and arrange the belt around her until it is tight but still comfortable.
3Fasten the belt by pushing the fixing button through the overlapping section of the belt. Ensure
that the fixing button and the loose ends of the belt are at the patient's side.

3 Basic Operation
70
4When you have positioned a transducer satisfactorily, you can attach it to the belt by pushing the
belt button on the transducer through one of the holes in the belt.
5Alternatively, attach the butterfly belt clip to the transducer belt button and use this to attach the
transducer to the belt. The clip allows you to slide the transducer for easy repositioning.
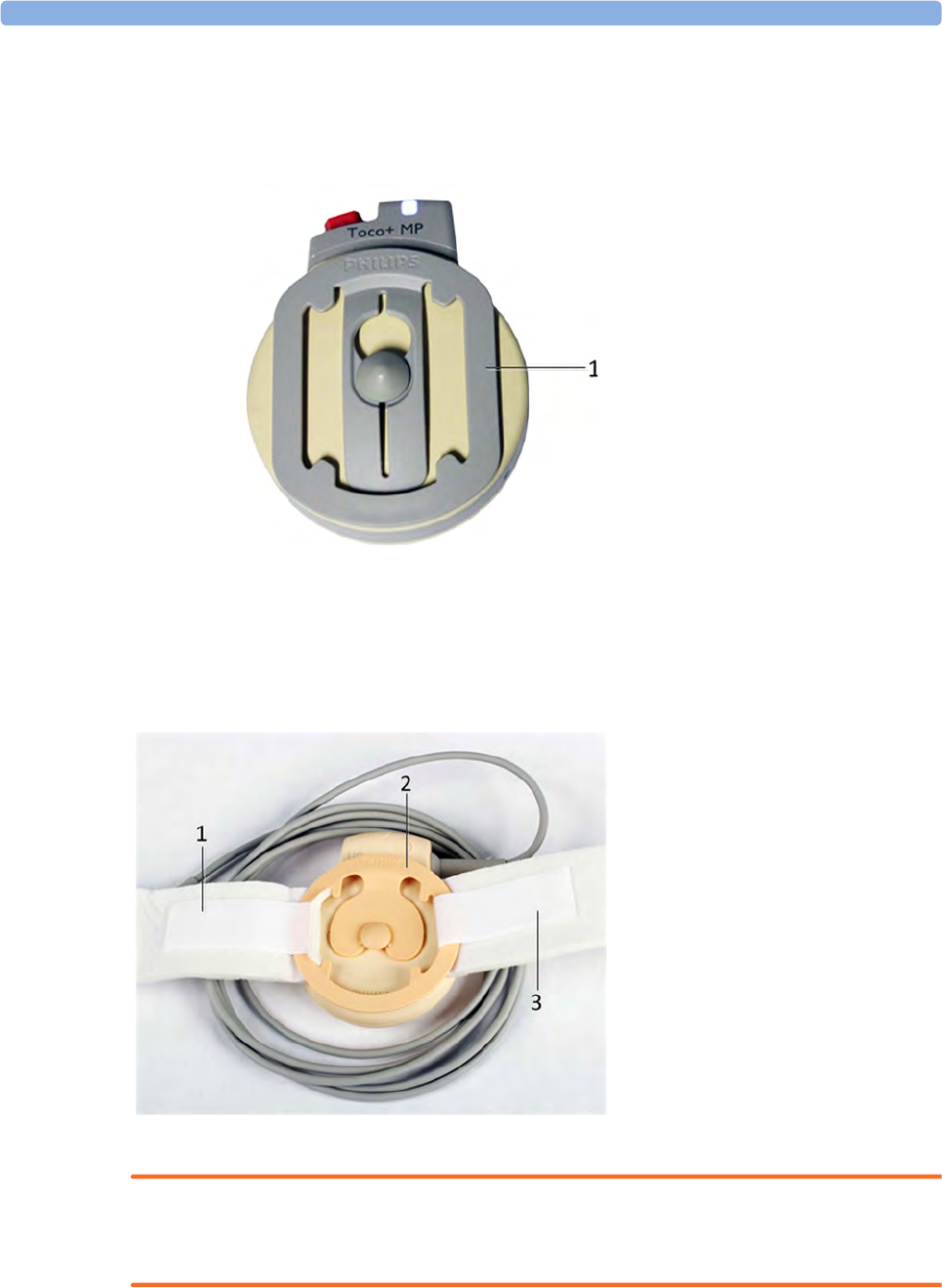
3 Basic Operation
71
Using CL Transducers with a Belt Clip
The Avalon CL transducers have their own belt clip. They can be optional ordered in a kit of 10
(989803184851).
Using Belt with Velcro Fixings
Insert one end of the belt between the belt guides on one side of the butterfly belt clip, and secure with
the velcro fixing. Insert the other end of the belt between the belt guides on the other side of the
butterfly belt clip, adjust for the correct tension, then secure with the velcro fixing.
WARNING
When connecting devices for acquiring measurements, always position cables and NBP tubing
carefully to avoid entanglement or potential strangulation.
1Avalon CL belt clip
1Velcro fixing
2Belt guides
3Velcro fixing

3 Basic Operation
72
Repositioning Transducers
A patient possibly wears transducers for long periods without interruption. In rare cases, skin
irritations may occur if a transducer is attached to one location for a longer period. To ensure there are
no adverse effects on the patient's skin, inspect the transducer application site at least every three
hours. If the skin quality changes, move the transducer to another site.
The ultrasound transducer is often repositioned to follow the fetal heart as part of the normal
monitoring process, but this is not so for the Toco transducer. Therefore, remember to check its
application site (between contractions) at least every three hours.
To reduce the risk of skin irritations, do not allow a cleaning or disinfecting agent to remain on the
transducer. Follow all instructions that accompany the specific cleaning and disinfecting agents you are
using. Remove agent residues with a cloth dampened in water before applying a transducer to a patient.
See “Care and Cleaning” on page 245 for further information, and a list of approved agents.
Connecting a Transducer to the Monitor
1SpO2 socket
2Noninvasive blood pressure socket
3Fetal sensor sockets
You can plug a fetal transducer, an ECG/IUP patient module, an Avalon CL or
Avalon CTS Cableless Fetal Transducer System interface cable (red connector), or
an external event marker into any of the four fetal sensor sockets marked by the
fetal icon, or "Fetal Sensors" (depending on geography).
For measuring maternal SpO2, connect the sensor to the socket marked with the
SpO2 icon or "SpO2" (depending on geography).
For maternal non-invasive blood pressure, connect the cuff to the socket marked
with the NBP icon or "NBP" (depending on geography).
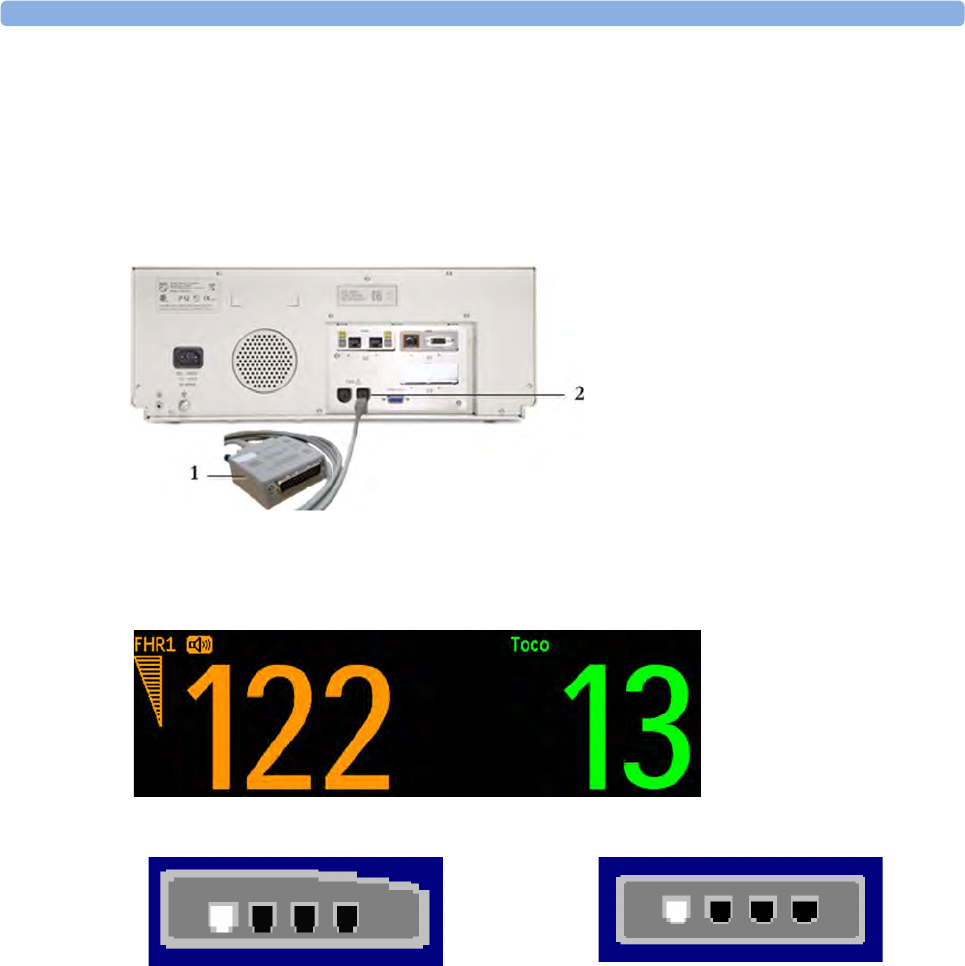
3 Basic Operation
73
For the FM20 and FM30, you can connect an Avalon CL Cableless Fetal Transducer system interface
cable (red connector) to one of the fetal sensor sockets at the left side of the monitor.
For the FM40 and FM50, you can connect an Avalon CL or Avalon CTS Cableless Fetal Transducer
System interface cable (black connector) to one of the two dedicated black sockets marked "Tele" at
the rear of the monitor, as an alternative to using one of the fetal sensor sockets (red connector) at the
front.
What You See on the Monitor
When you connect a transducer or sensor, the measurement numeric appears on the screen.
Fetal heart rate measurements are labeled in the order in which you plug in the transducers for those
measurements. It does not matter which fetal sensor socket you use, as the monitor allocates a channel
automatically. For instance, when monitoring triplets, the first transducer you connect is automatically
allocated a channel, and the measurement is labeled FHR1, the second FHR2, and the third FHR3. See
also chapters “Monitoring Twin FHRs” on page 171 and “Monitoring Triple FHRs” on page 179.
When you touch a measurement numeric on the screen, the setup menu for that measurement opens.
The fetal sensor socket to which the transducer for this measurement is connected is identified by the
transducer position indicator in the blue setup menu header.
1Interface cable to Avalon CL and
Avalon CTS Cableless Fetal
Transducer System.
2Connect the black connector to one
of the two black sockets (marked
"Tele") on the rear of the monitor.
for FM20/FM30 for FM40/FM50
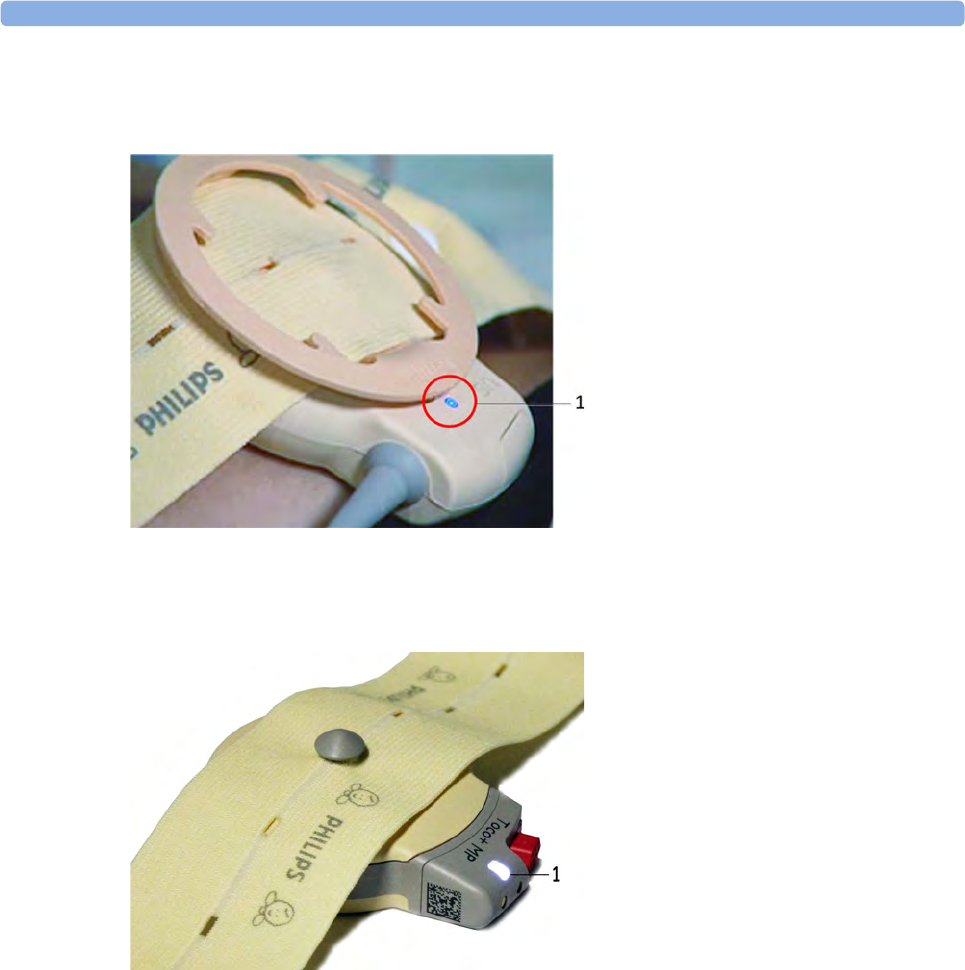
3 Basic Operation
74
The blue finder LED on a wired fetal transducer lights up when you touch the measurement on the
screen, allowing you to identify the corresponding transducer.
The white finder LED on a cableless fetal transducer lights up when you touch the measurement on
the screen, allowing you to identify the corresponding transducer.
The recorder prints an annotation showing the date, time, paper speed, and monitoring mode. It
repeats this every 10 minutes.
Start Recording
Checking/Setting Paper Scale
You can check the paper Scale Type (US for USA, or Internat'l for other geographies) in the Fetal
Recorder menu. In Monitoring Mode, you can see these settings (grayed out), but you cannot change
them. They can be changed in Configuration Mode, see the Configuration Guide.
1Finder LED
1Finder LED cableless transducer
3 Basic Operation
75
Paper Guide FM40/FM50
FM40/50 The recorder in the FM40 and FM50 features a transparent paper guide which:
• facilitates correct alignment of the paper, both during loading and while the recorder is running.
See “Loading Paper FM40/FM50” on page 84.
• incorporates a tear-off edge, which not only allows you to tear off the trace paper where you like
(not necessarily at a fold), but also helps to avoid paper misalignment while doing so (see “Tearing
Off the Paper” on page 80).
• is removable (see “Removing the Paper Guide: FM40/FM50” on page 250).
Switching the Recorder On and Off
In addition to the normal recording of real-time traces, you will sometimes see a trace recovery
printout from the monitor's internal backup memory at high speed when the recorder is started. For
details, see “Recovering Traces on Paper” on page 241.
For an explanation of the various symbols that can appear on the trace recording, see “Recorder
Specifications” on page 284.
To switch the recorder on, select in Main Setup the menu item Fetal Recorder, or press one of the
SmartKeys: Start/ Stop or Start Recordng.
The "recorder on" status indicator is displayed in the bottom right-hand corner of the screen when you
switch on the recorder.
The paper advances quickly for 2 cm and then returns to the set speed. Whenever the recorder is
switched on, a trace header is printed vertically on the trace paper, containing the following:
•Selftest: OK: confirmation that the monitor's self-test completed successfully, and that it is ready
to use.
• the software revision and firmware revision
•the serial number
•the time
•the date
• patient name and medical record number (if entered)
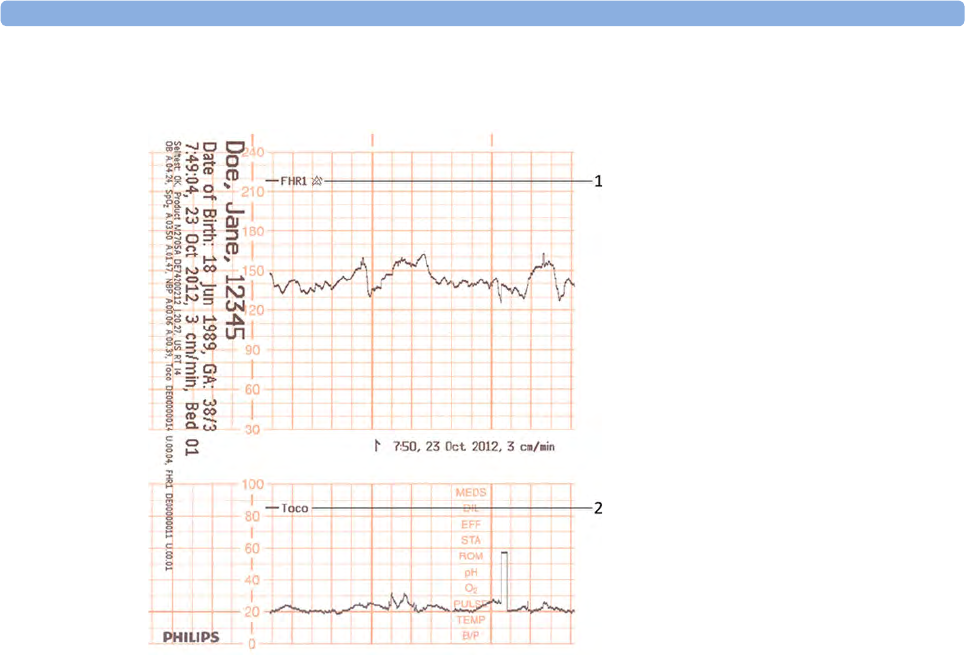
3 Basic Operation
76
•the Recorder Speed
The current monitoring modes (if any transducers are connected to the monitor) are printed.
Whenever a transducer's mode is changed, the following are printed:
•the time
•the date
• trace identification symbols
•the
Recorder Speed
The monitor prints the time, date, Recorder Speed, and monitoring modes in the trace header when
first switched on, in a periodic time stamp every ten minutes after, and if the monitoring modes
change. The time stamp begins with the symbol shown below. The data is reprinted in the header if the
1Fetal heart rate label
2Uterine activity label
3 Basic Operation
77
time and date are locally adjusted, or if an OB system is connected that readjusts the time and date
automatically.
The trace records maternal parameters also. When measuring noninvasive blood pressure, the
annotation is made at the end of the measurement. If the noninvasive blood pressure measurement
repetition time is short, the noninvasive blood pressure numeric may not always be printed.
The recording of notes (see “Entering Notes” on page 88) or time/date information may be
interrupted by connecting, or unplugging a transducer, or by a change in measurement-related setting
(for example, artifact suppression, Toco sensitivity, or alarm settings).
A new patient admission or a change to the paper scale setting stops all annotations, and prompts a
new vertical trace header to be printed.
To switch off the recorder:
1Either select Start/Stop from the Fetal Recorder menu.
2Or press one of the SmartKeys (depending on configuration): fetal recorder Start/ Stop or Stop
Recordng.
If your recorder is configured with Confirmed Stop on (a Configuration Mode setting), you will
need to confirm that you want to stop the recorder, before it will stop.
When the recorder is off, the "recorder off" status indicator is displayed in the bottom right-hand
corner of the screen: When the Paper Save Mode is set to Off the paper icon shows an x mark,
and when Paper Save Mode is On the icon shows a paper trace icon.
1Time stamp printed every ten
minutes
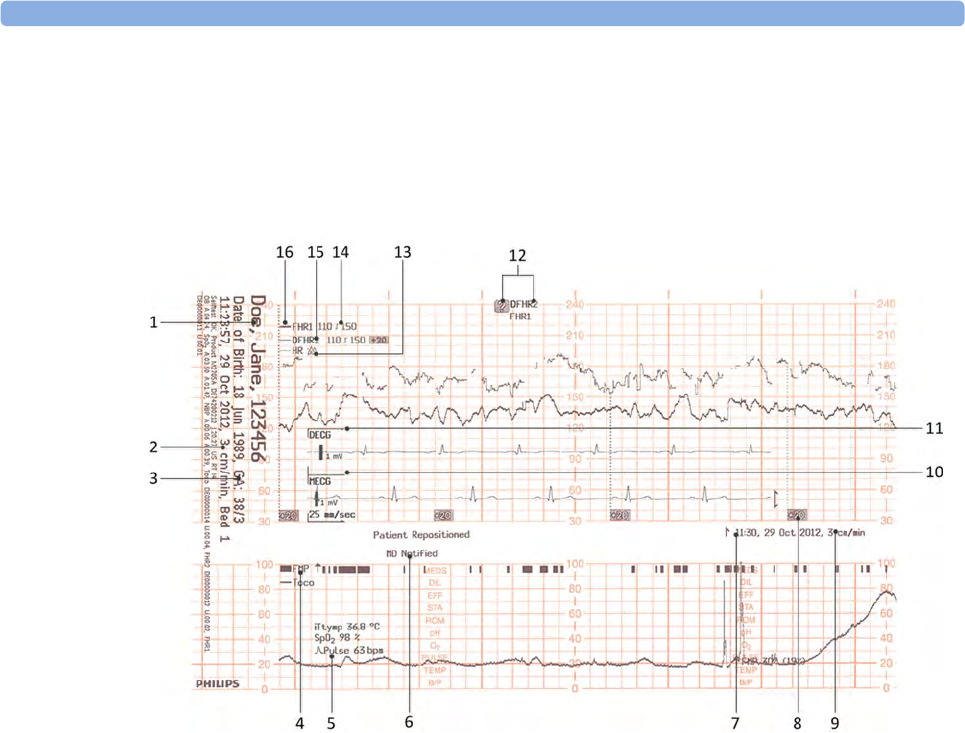
3 Basic Operation
78
Recording Elements
The trace paper of the recorder has much information printed on it. Here is an exemplary trace with
the most common print outs and their meaning. Each trace header contains the last name and first
name, the patient ID, patient date of birth, the current date and time, patient's bed label, and the
gestational age of the pregnancy.
1Name, patient ID, date of birth, current date and time
2Recorder Speed
3Gestational age and patient bed label
4FMP - Fetal Movement Profile
5Other measurement for the patient such as temperature, arterial oxygen saturation, and pulse.
6Entered notes such as patient repositioned, or MD notified, or others
7Time stamp
8Trace separation
9Recorder Speed
10 Maternal ECG
11 Direct ECG
12 Coincidence of heart rate detected
13 HR with Cross Bell
14 Alarm Limits
15 DFHR2 (second fetal heart rate from DECG)
16 FHR1 (first fetal heart rate)
3 Basic Operation
79
Choosing Paper Speed
You can choose a Recorder Speed of 1, 2, or 3 centimeters per minute (cm/min). The default setting
is 3 cm/min.
The ACOG technical bulletin on FHR monitoring states that "accurate pattern recognition is difficult if not
impossible at 1 cm/min and that 1 cm/min is only recommended for more economic screening. When FHR
abnormalities arise, the faster paper speeds will enhance FHR pattern recognition".
Additionally, because a change in Recorder Speed results in a change in the appearance of an FHR
trace, you are advised to ensure ALL monitors in your institution are set to the same speed.
To set the Recorder Speed (in Configuration Mode) see the Configuration Guide.
Advancing the Paper
You can advance the paper automatically to the next fold by pressing the Paper Advance SmartKey at
any time except during a stored data recording. This is also possible using the Fetal Recorder menu.
Marking an Event
You can record significant events on the trace paper (for example, when pain medication is
administered or when the mother changes position). The mother can use the remote event marker to
mark events herself. You connect the remote event marker to any free fetal sensor socket.
To mark an event on the trace paper you can:
1Either select the Set Marker SmartKey.
2Or press the button on the remote event marker. The remote event marker is connected to the
monitor via any fetal transducer socket.
A small arrow is printed on the heart rate scale on the trace paper.
3 Basic Operation
80
This reflects exactly when the marker button was first pressed; keeping the button pressed has no
influence on the annotation.
Tearing Off the Paper
CAUTION
Never pull on the paper to advance it, as this can cause misalignment of the paper. Always tear off the
paper along the perforation.
FM40/FM50 The recorder's paper guide incorporates a tear-off edge, allowing you to tear off the trace paper cleanly
where you like (not necessarily at a fold). When not using the paper guide, always tear off the paper
along the perforation.
To tear off the trace paper after monitoring using the paper guide:
1If the recorder is running (the "recorder on" status indicator is displayed), turn off the recorder by
selecting the fetal recorder Start/ Stop SmartKey or the Stop Recordng SmartKey.
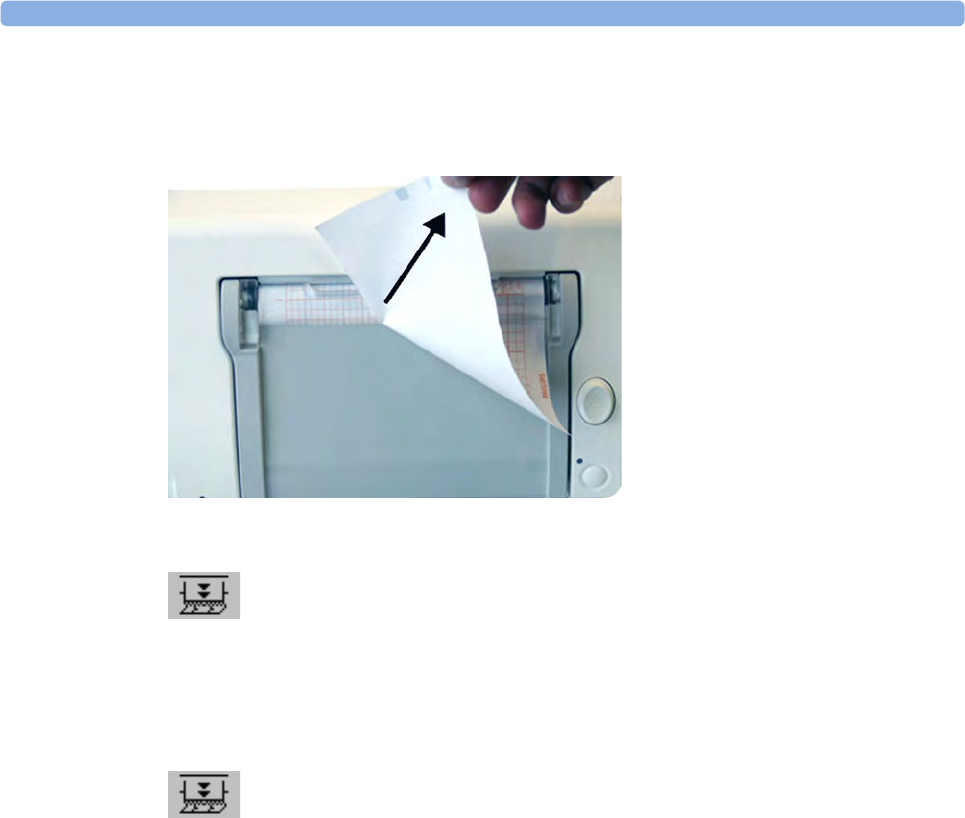
3 Basic Operation
81
2Tear off the paper as shown in the picture. To ensure a clean tear, always tear in an upwards
motion, as indicated by the arrows. You can start tearing from the left or right (right-handed user
shown). You may want to use both hands to guarantee that the paper is not misaligned during the
tear off.
3If you wish to tear off the paper at a fold, select the Paper Advance SmartKey, wait for the paper
to stop, then tear it off.
FM20/FM30 The FM20/FM30 does not have a paper guide. The procedure is the same as described for the FM40/
FM50 with the exception that you should advance the paper to a perforation.
If you wish to tear off the paper at a perforation, select the Paper Advance SmartKey, wait for the
paper to stop, then tear it off.
Paper-Out Indication
Each pack of paper has 150 pages. The monitor issues a paper-out warning in the status line at the
bottom of the screen, when there are five pages to go. If you switch on the recorder or press the paper
advance key when there are fewer than five pages remaining, it may take two pages before the alarm is
activated. Load a new pack in time.
If the recorder runs out of paper, an audible paper-out alarm is sounded, if so configured. See
“Loading Paper FM40/FM50” on page 84and “Loading Paper FM20/FM30” on page 82 to learn how
to reload paper.
Fetal traces continue to be recorded into the monitor's backup memory, and can be retrieved and
printed completely if new paper is loaded within one hour, when the Bridge Paperout setting is
enabled in Configuration Mode. See “Recovering Traces on Paper” on page 241 for further
information.
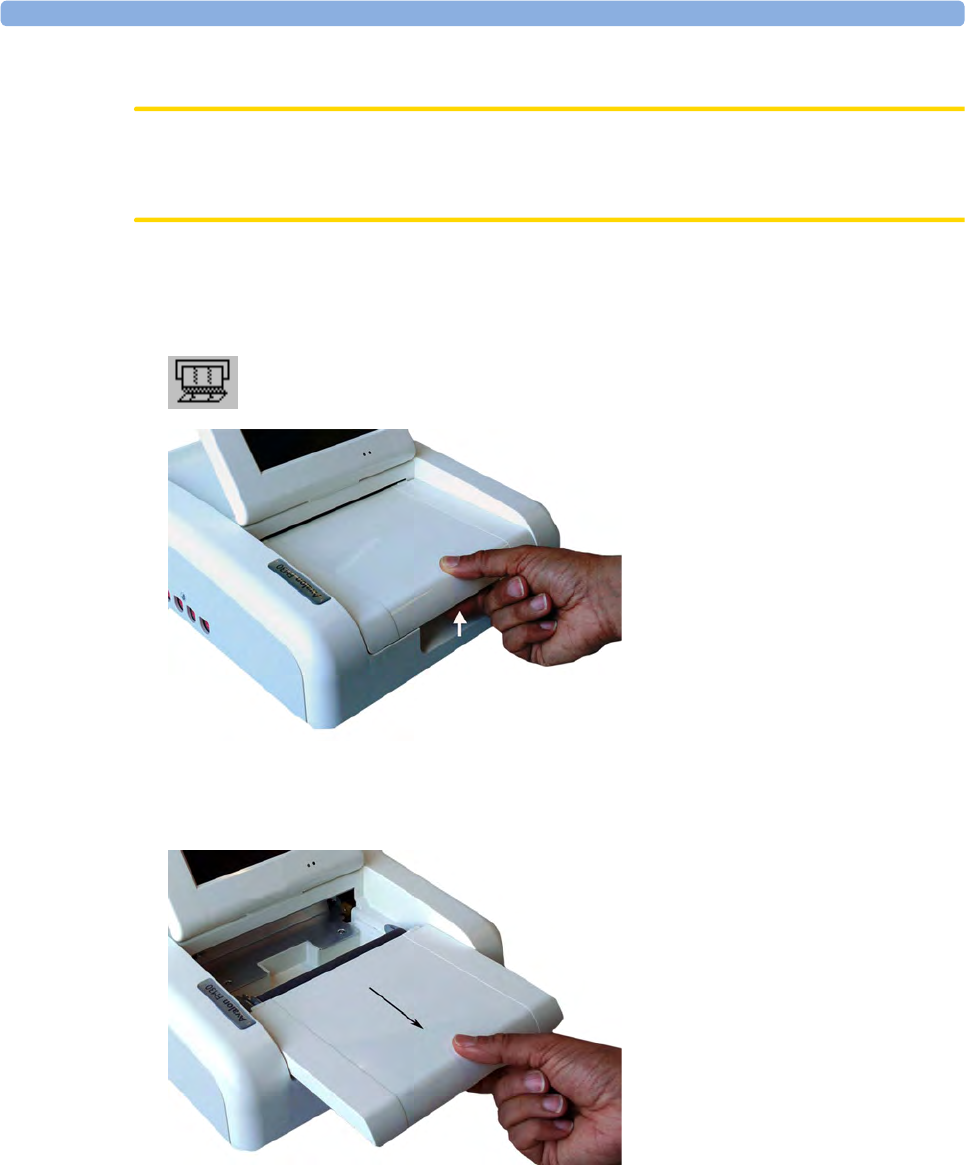
3 Basic Operation
82
Loading Paper FM20/FM30
CAUTION
Using recorder paper that is not approved by Philips can result in accelerated paper fading and can
damage the thermal line printhead. This type of damage is not covered by warranty.
FM20/FM30 To load a pack of paper:
1If the recorder is on, press the recorder Start/ Stop SmartKey or the Stop Recordng SmartKey to
turn it off before loading a new pack of paper.
1Press the paper table release to unlock the paper drawer and then pull the table forward to open it
fully.
2Lift out any remaining paper from the tray.
3Prepare to place the new pack of paper in the tray with the bottom side down. The bottom side is
indicated by the word STOP printed on the final page of the new pack.
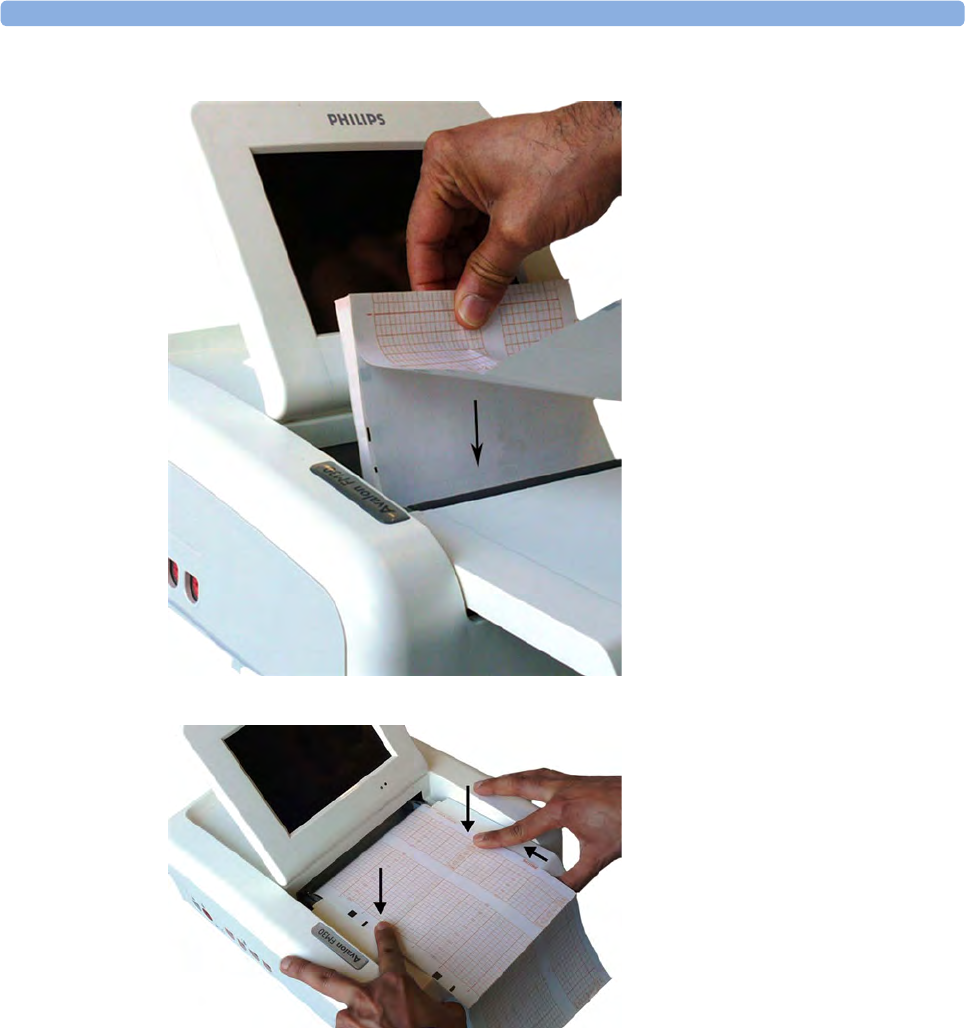
3 Basic Operation
83
4Unfold the top page of the pack and position the uterine activity scale on the right.
5Slide the pack into the tray.
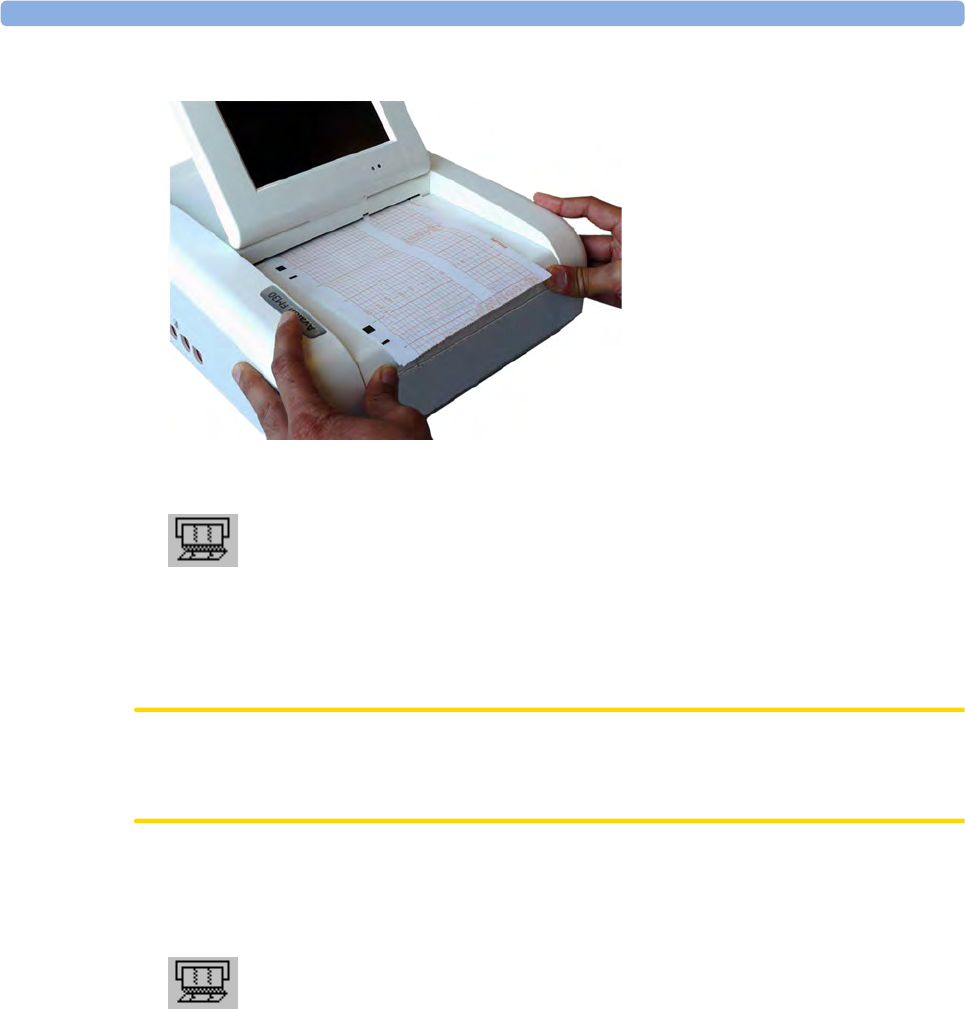
3 Basic Operation
84
6Push the paper drawer back until it "clicks" closed.
7Press the recorder Start/ Stop SmartKey or the Start Recordng SmartKey to switch on the
recorder.
Annotations of trace information are printed on the trace paper (see “Switching the Recorder On and
Off ” on page 75 for details).
Loading Paper FM40/FM50
CAUTION
Using recorder paper that is not approved by Philips can result in accelerated paper fading and can
damage the thermal line printhead. This type of damage is not covered by warranty.
FM40/FM50 To load a pack of paper:
1If the recorder is on, press the Start/ Stop Rec SmartKey or the Stop Recordng SmartKey to turn
it off before loading a new pack of paper.

3 Basic Operation
85
2Press the paper eject button to open the paper drawer.
3Lift out any remaining paper from the tray.
4Press and hold the paper eject button to partially eject the paper, thus making it easier to remove.
5Hinge the transparent paper guide forward. It is held in the closed position by a small protrusion
on each side of the holder.
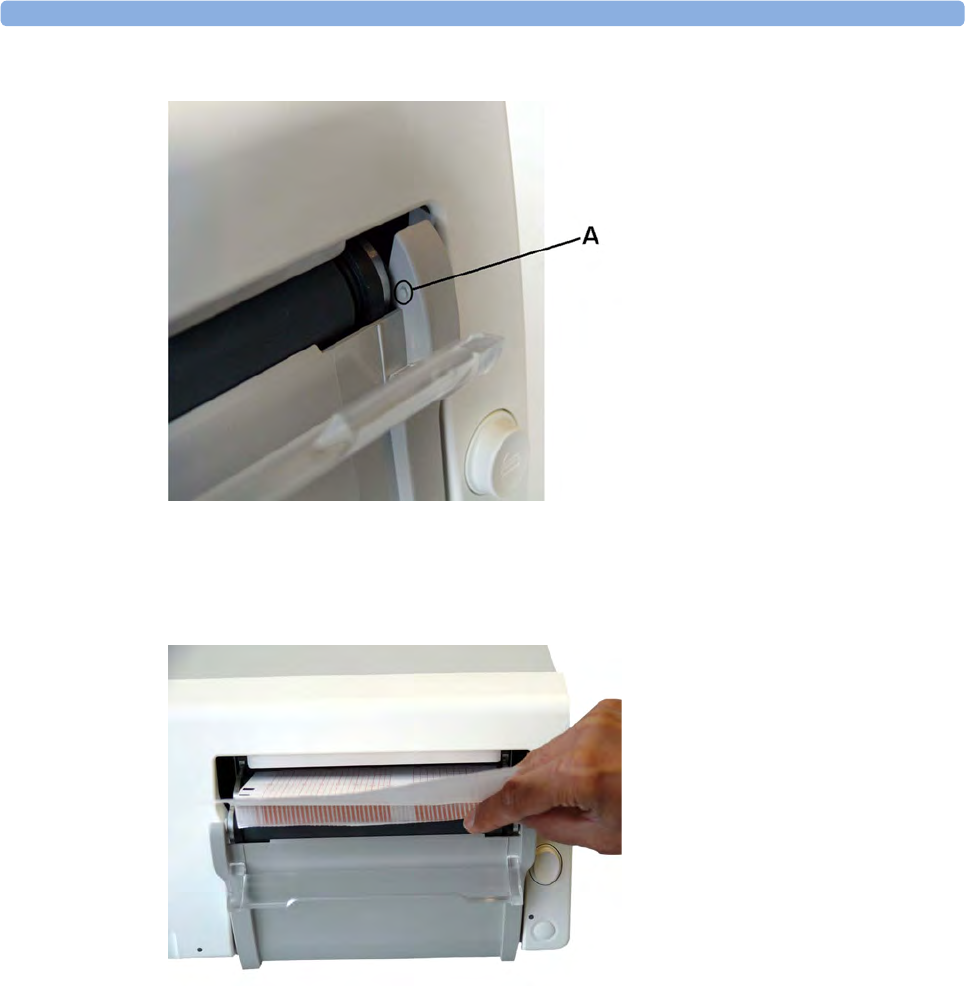
3 Basic Operation
86
6A - Protrusion holds paper guide in closed position.
7Prepare to place the new pack of paper in the tray with the bottom side down. The bottom side is
indicated by the word STOP printed on the final page of the new pack.
8Unfold the top page of the pack and position the uterine activity scale on the right.
9Slide the pack into the tray.
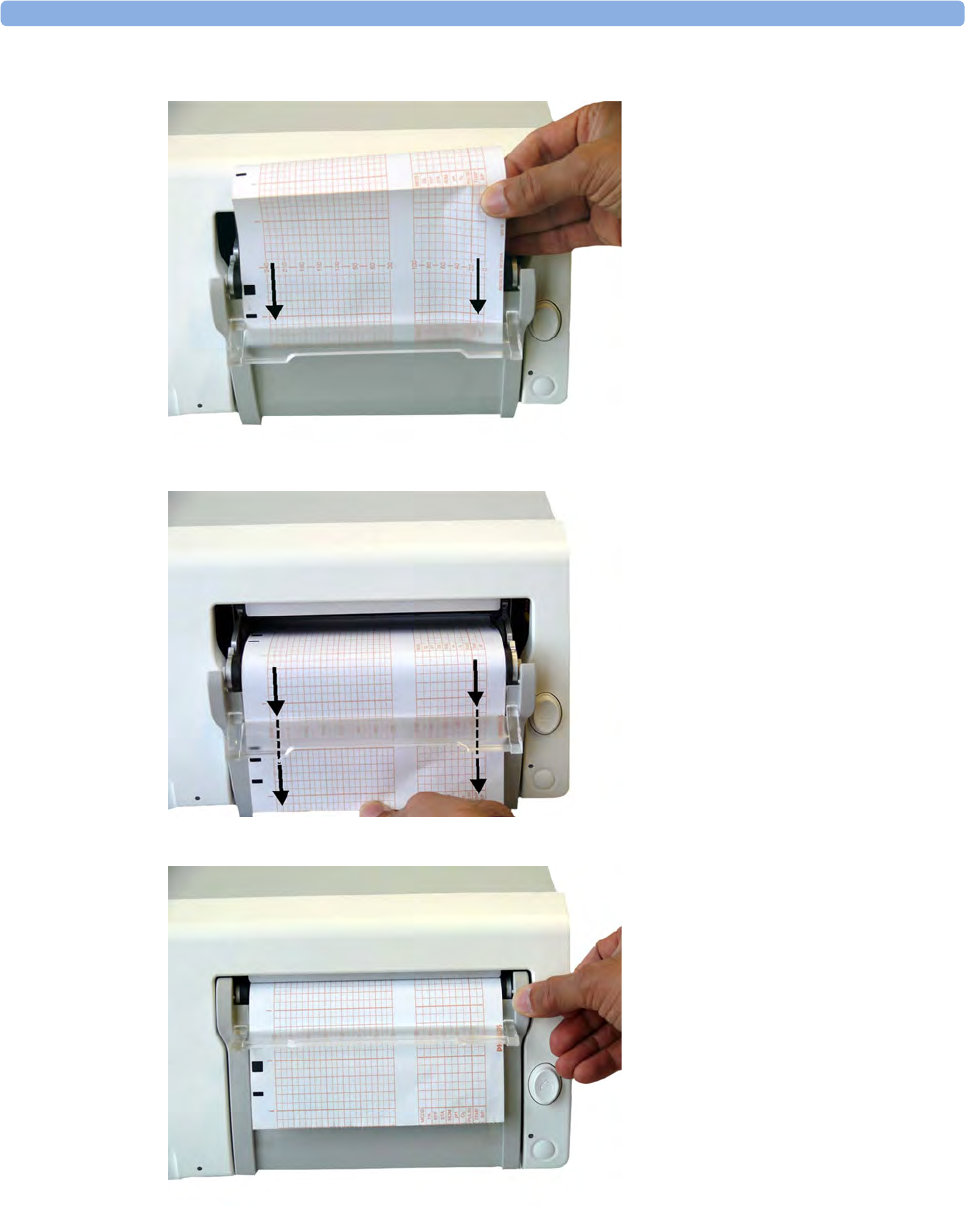
3 Basic Operation
87
10 Feed the paper evenly through the paper guide. Do not close the paper guide yet.
11 Close the paper drawer.
12 Now close the paper guide.
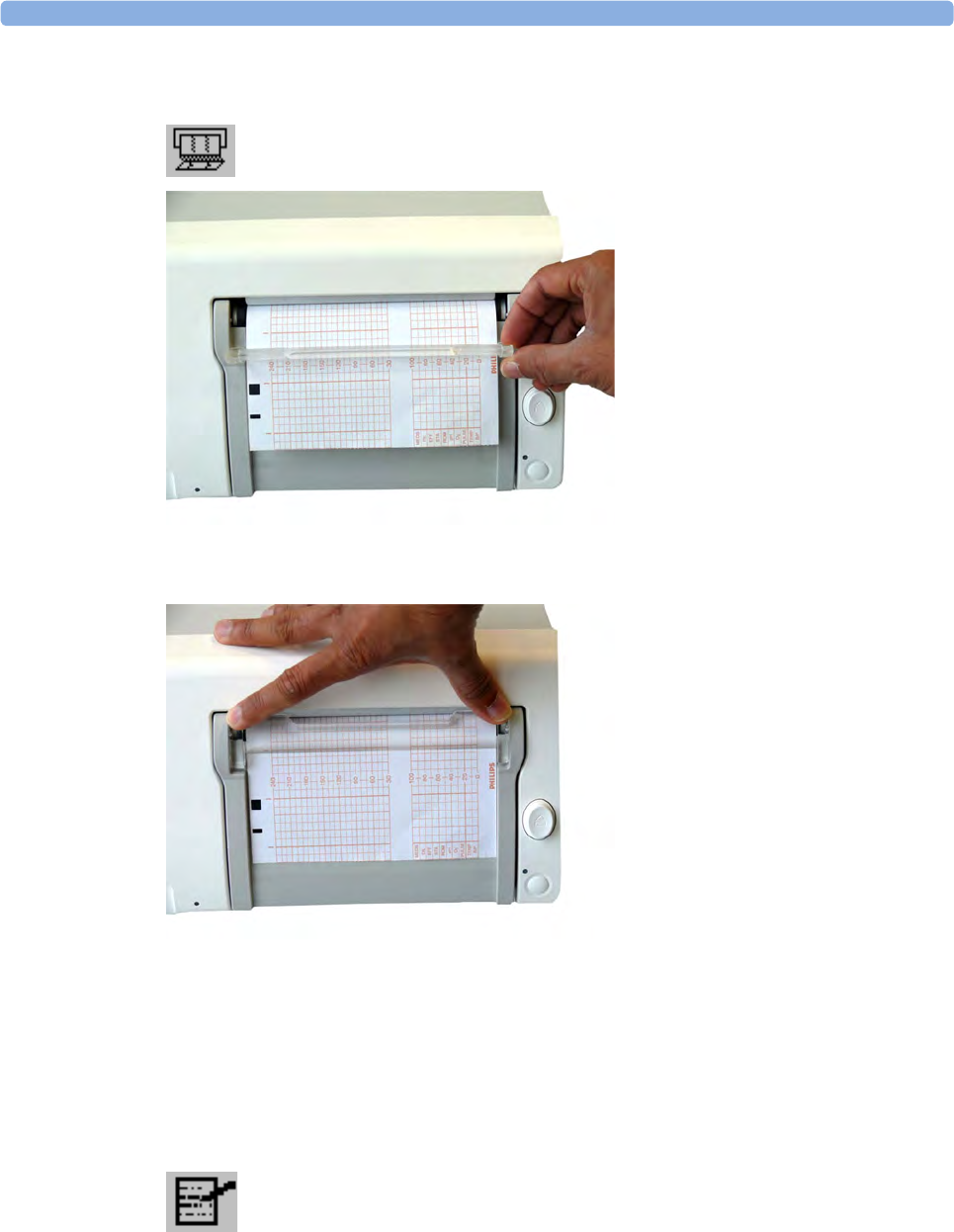
3 Basic Operation
88
13 Press the recorder Start/ Stop SmartKey or the Start Recordng SmartKey to switch on the
recorder.
Annotations of trace information are printed on the trace paper (see “Switching the Recorder On and
Off ” on page 75 for details).
Entering Notes
Your monitor has a set of 15 factory pre-configured notes (see below). The maximum length of one
single note is 30 characters. It is possible to edit the notes in Configuration mode (see the
Configuration Guide).
To enter a note:
1Press the Enter Notes SmartKey to open the Enter Note menu.
2Scroll if necessary, then select the note you wish to enter. A confirmation dialog box opens:
3Select Confirm to enter the note. The note is then shown in the status line of the display, and is
annotated on the fetal trace if the fetal recorder is on.

3 Basic Operation
89
4By default, notes are printed lengthwise in the direction of the trace, in the space between the FHR
grid and the uterine activity grid. If you prefer, you can configure the recorder to print across the
trace.
5You can change this in Configuration Mode by changing the Notes Recording setting in the Fetal
Recorder menu from Along (default) to Across (notes print width wise across the trace).
The following are the pre-configured notes from which to choose:
1Patient Repositioned
2Vaginal Examination
3MD Notified
4Sitting
5On Back
6Left Lateral
7Ambulating
8Tocolytic Given
9Membranes Ruptured
10 Amniotomy
11 Amniotic Fluid Clear
12 Amniotic Fluid Not Clear
13 Oxytocin
14 Urinary Catheter
15 Micro Blood Analysis
Up to two notes can be printed directly, and the monitor can temporarily store up to a further two
notes, and these are printed after the first two have been recorded. Any further notes are discarded.
For example, if you enter six notes in quick succession, the first two notes you entered are recorded
right away, the next two are stored in memory and then printed when the first two have been recorded,
and the last two are discarded.
If the printing of two notes happens to coincide with the regular recording of the time stamp that takes
place once every ten minutes, the time stamp is delayed until the notes have finished printing.
Signal Quality
During monitoring, if the fetal heart rate signal quality fluctuates, and becomes poor, it does not
necessarily mean that the transducer needs repositioning. The fluctuation may be caused by fetal
movement. Allow time for the signal to stabilize before deciding whether to reposition the transducer
(ultrasound), or apply a new electrode (ECG). For the best trace quality, the signal quality indicator
should be full, indicating good signal quality, even though it may be possible to make traces at a lower
signal quality level.

3 Basic Operation
90
Cableless Monitoring
Basics of Cableless Systems
The fetal monitors FM20/FM30 and FM40/FM50 are compatible with the Avalon CL and
Avalon CTS Cableless Fetal Transducer system. Regard the following points for cableless monitoring:
• You can connect one Avalon CL with a red connector to a FM20/FM30 or a FM40/FM50 (fetal
socket).
• You can connect up to two Avalon CLs with a black connector to a FM40/FM50 (Tele socket).
• You can connect one Avalon CTS system to a FM20/FM30 or FM40/FM50 at a time (either fetal
or Tele socket).
•You cannot connect Avalon CTS and an Avalon CL at the same time to the same fetal monitor.
• Monitoring multiple pregnancy using cableless transducers is supported by the Avalon CL system
only.
• Using a mixture of wired and cableless fetal transducers is not supported. You can use either wired
or cableless fetal transducers.
• If you cannot get sufficient signal quality using Avalon CTS transducers, switch to wired
transducers.
Assigning Cableless Transducers
The cableless transducers of the Avalon CL are assigned by simply docking them at the base station
connected to the patient’s fetal monitor. See the Avalon CTS Instruction for Use for the assignment of
the cableless transducers of this system.
Avalon CL Transducer System Avalon CTS Transducer System
3 Basic Operation
91
Activating Cableless Transducers
The CL transducers of the Avalon CL are activated by picking them up from the base station. If the
CL transducer is activated, an antenna symbol is displayed on the fetal monitor screen next to the
numeric of the measurement. See the Avalon CTS Instruction for Use for the activation of the
cableless transducers of this system.
Unassigning Cableless Transducers
The CL transducers of the Avalon CL are unassigned by manually removing them in the
corresponding setup menu from the group of assigned cableless devices, or by unassigning them
directly in the Tele Info window. See the Avalon CTS Instruction for Use for the unassignment of the
cableless transducers of this system.
Deactivating Cableless Transducers
The CL transducers of the Avalon CL are deactivated by redocking them at a base station. To
deactivate all cableless transducers at once press the Standby button of the Avalon CL base station. See
the Avalon CTS Instruction for Use for the deactivation of the cableless transducers of this system.
Configuration of Cableless Systems
For the Avalon CL and Avalon CTS Cableless Fetal Transducer system and the corresponding
channels have to be configured for the radio communication to work and not to interfere with any
other telemetry devices.
The configuration of a connected Avalon CL system is done in Configuration Mode or Service Mode
of the fetal monitor. Service Mode functions can be used to identify channel assignment conflicts in
the hospital environment. The configuration should be carried out by authorized and qualified service
personnel, either by the hospital's biomedical department, or by Philips Support.
For a detailed description of the configuration see the Avalon CL Service Guide and the Fetal Monitor
Configuration Guide. For details regarding the configuration of a connected Avalon CTS system see
the Avalon CTS Service Guide.
Setup OBR
Revisions A.00.00
Frequency Band
Channel
WMTS
4
Scan Duration
Start Scan
Stop Scan
15 min
Start RSSI Trace
Stop RSSI Trace
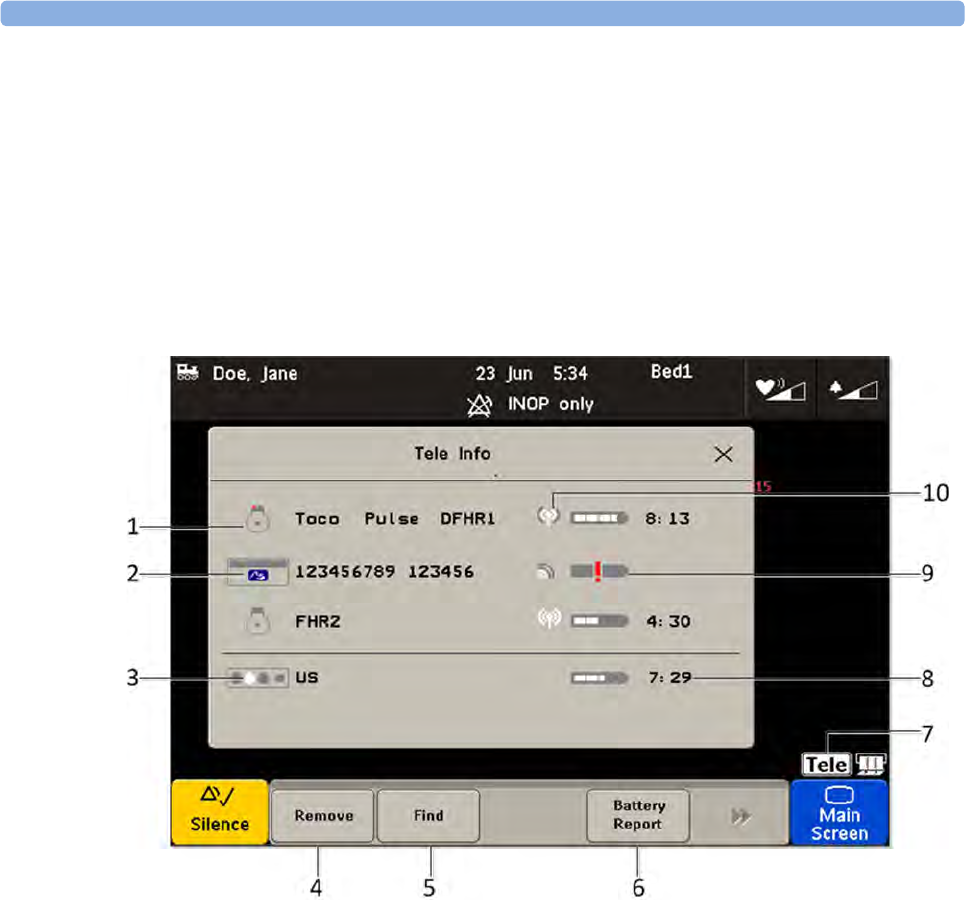
3 Basic Operation
92
Tele Info Window
The Tele Info window of the fetal monitors allows you to manage the Avalon CL system. Below is an
exemplary view of the Tele Info window. Your window may differ depending on the status of the
connected system.
To open the Tele Info window you can:
1Configure a Tele Info SmartKey to open the window,
2click on the TELE icon on the main screen, or
3select the Main Setup and then Tele Info.
1Transducer icon assigned with the parameter label
2Cableless module icon and equipment ID
3Base station icon with docking indication (the white slot indicates a
charging transducer)
4Key Remove
5Key Find
6Key Battery Report
7Tele icon
8Remaining battery time
9Out of battery icon
10 Indication of signal quality
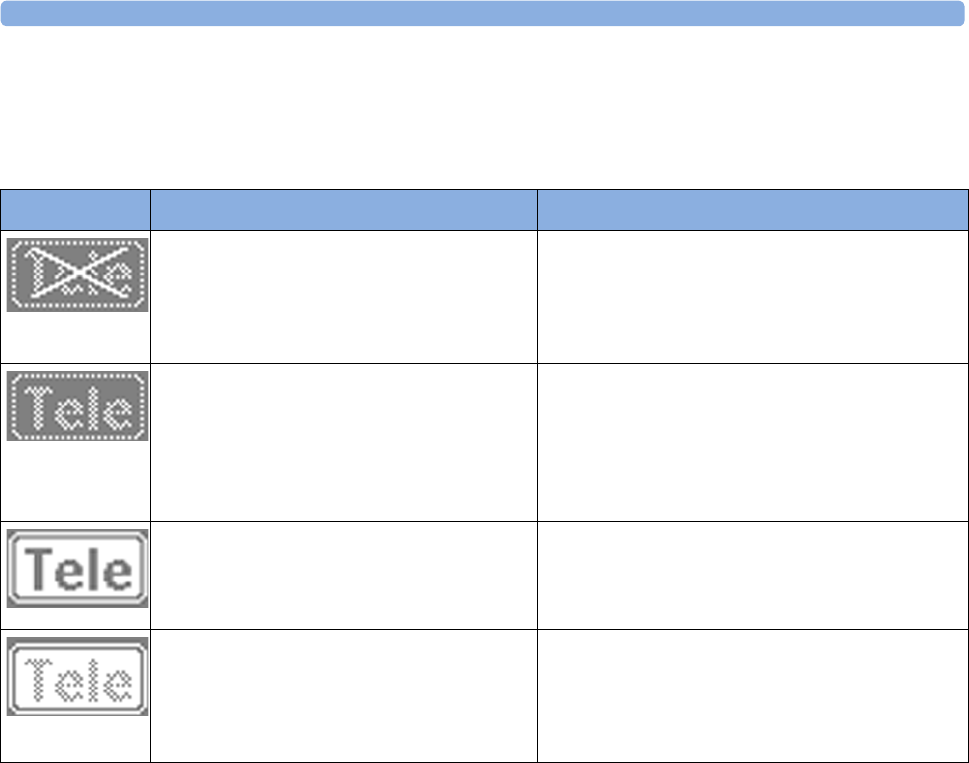
3 Basic Operation
93
Telemetry
When the monitor recognizes a connected Avalon CL or Avalon CTS interface cable (red or black
connector), it confirms the recognition with the following status indicators displayed in the lower
right-hand corner of the screen:
NOTE
A cableless transducer is considered still active, even if it has an INOP condition (e.g. cl US
Disconnect), until it is either deactivated by docking it at the base station, or until it is manually
removed from the Tele Info window.
CL transducers have priority over wired transducers. If an Avalon CL or Avalon CTS base station is
connected to the fetal monitor, and both wired and cableless transducers are connected to the monitor,
the wired transducers are disabled whenever one cableless transducer is active. If an CL Pod is
activated it does not automatically deactivate all wired transducers, just the one with the corresponding
measurement.
To switch back to using wired transducers, redock the cableless transducers at the base station, or
switch the base station to Standby mode, and continue monitoring with the wired transducers. If you
cannot get sufficient ultrasound signal quality using the Avalon CTS base station, try repositioning the
transducers, or switch to wired transducers. Using a Avalon CL base station you should get a better
signal by reducing the distance between CL transducer and base station.
• When using an Avalon CL or Avalon CTS you should be aware that FMP is not recommended
when the mother is likely to move, and you should disable Fetal Movement Profile (FMP) on the
fetal monitor (Fetal Movement Off) if the mother is walking. Maternal movements are likely to
create artifact in the FMP output. See also “Switching FMP On and Off ” on page 161, the
sections “Cableless Monitoring - Important Considerations” on page 156 and “Fetal Movement
Profile” on page 160.
Indicator Avalon CTS Avalon CL
Avalon CTS interface cable is connected to
the monitor, but the Avalon CTS base station
is not connected to the interface cable, or it is
disconnected from AC mains, or is in Standby
mode.
A base station is connected to the monitor, but the
base station is in Standby mode.
Avalon CTS interface cable is connected to
the monitor, Avalon CTS base station is
connected, powered on, and cableless
transducers are ready to use, but no cableless
transducers are currently active (all are still
docked at the base station).
A base station is connected to the monitor but no
cableless transducers and no cableless Pods are
currently active. All are still docked at the base
station, or the base station holds no transducers.
Avalon CTS interface cable is connected to
the monitor, Avalon CTS base station is
connected, powered on, and at least one
cableless transducer is active and assigned.
A base station is connected to the monitor, it is on,
and minimum one cableless transducer or cableless
Pod is active and assigned.
Not applicable for Avalon CTS. The CL transducer is moved away from the base
station approaching the end of range (at least 70 m).
The US sound is replaced by an artificial QRS
sound (like DECG). The DECG and MECG waves
are no longer displayed.
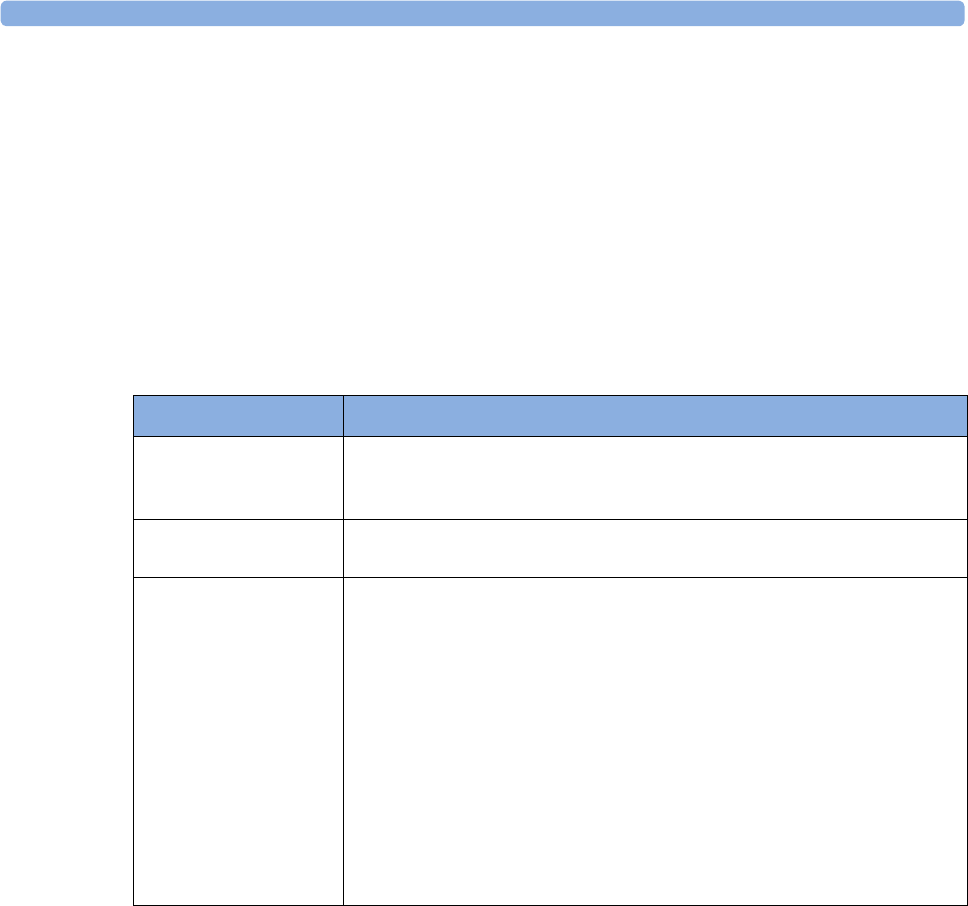
3 Basic Operation
94
• With the Avalon CL Transducer system you can now monitor twins and triplets with CL
transducers. The Avalon CTS System does not have this option.
About RF Signal Quality
Signal transmission can be disturbed if:
• the patient is out of range of the receiving area.
• there is interference from another, possibly stronger, RF signal (a broadcasting station, for
instance).
• the patient is near material that absorbs electromagnetic waves (for example, metal-reinforced
concrete, elevator doors) or the base station antenna is in an enclosed metal rack.
Pop-up Keys
Prompts
The fetal monitor issues prompt messages to certain user interactions. For example if the CL SpO2
Pod is picked up from the base station to activate it, the monitor displays the prompt message cl SpO₂
Added and the equipment lable of the Pod.
CL Transducer Assignment
The cableless transducers of the Avalon CL are assigned by simply docking them at the base station
connected to the patient’s fetal monitor.
Since twins and triplets can be monitored with the Avalon CL base station, it can be delivered with up
to seven CL transducers: one CL Toco+MP, three CL US, and three CL ECG/IUP transducers. Only
up to four CL transducer can be assigned at one time to the Avalon CL base station. Four assigned CL
transducers enable monitoring combinations such as 1 CL Toco+MP transducer + 3 CL US
transducers for monitoring triplets externally, or 1 CL Toco+MP transducer + 2 CL US transducer +
1 CL ECG/IUP transducer for monitoring twins.
Pop-Up Key Function
Remove Selecting the Remove key deactivates and unassigns the selected active
transducer or cableless Pod and removes it from the list. This key is disabled
if no active device is selected.
Find Selecting the Find key pages the selected active CL transducer or CL Pod.
This key is disabled if no active device is selected.
Battery Report Selecting the Battery Report key prints a combined battery report on the
built in recorder. The report contains at least the following information for
each CL transducer or CL Pod currently in the list:
• Cableless device identification (like in the Tele Info window list)
• Battery identification (e.g. part no.)
• Battery serial number
• Battery manufacturing date
• Battery capacity: remaining/when fully charged/battery temperature
• Number of cycles
This key is only available and enabled in Service mode.

3 Basic Operation
95
Three CL transducers can be docked and charged at the Avalon CL base station at the time. If a fourth
transducer should be assigned to the Avalon CL base station:
1Remove first the three already docked CL transducers from the base station and place them on the
patient.
2Then dock the remaining fourth transducer at the base station and wait until the LED of the
fourth transducer signals that it has communication with the base station.
3Place the fourth CL transducer on the patient and check on the fetal monitor in the Tele Info
window if the base station and the monitor have communication with all four transducers, and if
their numerics are displayed on the screen of the fetal monitor.
CL Transducer Unassignment
The cableless transducer are not unassigned by simply removing them from the base station. To
unassign a cableless transducer, there are two methods:
1Open the setup menu of the measurement e.g. FHR1 by pressing the numeric on the screen.
2Select Remove from the open setup menu.
3A confirmation window opens with the prompt Please Confirm and Device will be removed.
4Press the pop-up key Confirm. A prompt states then clDev has been removed.
or
1Open the Tele Info window.
2Select the symbol of the cableless transducer you want to unassign, and select Remove from the
pop-up menu.
3A confirmation window opens with the prompt Please Confirm and Device will be removed.
4Press the pop-up key Confirm. A prompt states then clDev has been removed.
NOTE
When a cableless transducer is unassigned, all the measurements from this transducer are no longer
monitored; e.g. if you unassign a CL Toco+MP, the Toco measurement, SpO2, and MECG are
possibly no longer monitored.
CL Pods Assignment
The cableless Pods of the Avalon CL are assigned by simply docking them at the base station
connected to the patient’s fetal monitor.
CL Pods Unassignment
To unassign a cableless Pods, there are four methods:
1Open the setup menu of the measurement e.g. SpO₂ by pressing the numeric on the screen.
2Select Remove from the open setup menu.
3A confirmation window opens with the prompt Please Confirm and Device will be removed.
4Press the pop-up key Confirm. A prompt states then clDev has been removed.
or
1Open the Tele Info window.
2Select the symbol of the cableless Pod you want to unassign, and select Remove from the pop-up
menu.

3 Basic Operation
96
3A confirmation window opens with the prompt Please Confirm and Device will be removed.
4Press the pop-up key Confirm. A prompt states then clDev has been removed.
or
Unassign the cableless Pods via it's user interface. See the Cableless Measurement Instruction for Use.
or
Dock the cableless Pod at another base station or charger and therefore assigning it to the new device.
Paging Patients
To page a patient currently not near the fetal monitor and base station select the SmartKey Call
Patient at the fetal monitor. The base station will then select the cableless transducer with the best
signal quality to emit the tone sequence to notify the patient.
Underwater Monitoring
Only the cableless transducers of the Avalon CL and Avalon CTS systems can be used to monitor
under water. You can use them to monitor patients in a bathtub or shower. This does not apply to the
maternal cableless SpO2 and NBP Pods, do not immerse the CL Pods into water.
Cableless transmission distances are shorter when monitoring under water. A metal bathtub is likely to
further reduce the operating range.
WARNING
Never immerse the base station in liquid. You must protect it against water sprays or splashes. Place
the base station where there is no chance of contact with, or falling into water or other liquids.
CAUTION
Avoid the use of pulsating water jets in the bath or shower while monitoring, as these can be
misinterpreted as an incorrect (or totally artificial) heart rate.
Toco Baseline drift: The accuracy specified for baseline drift cannot be guaranteed for underwater
usage. When using transducers under warm water the temperature increase causes a significant baseline
change due to internal pressure increase. The depth under water at which the Toco transducer is used
also has an effect on the Toco baseline, as the water pressure increases with depth. After immersion,
allow one to two minutes for the pressure to stabilize, then adjust the Toco baseline (between
contractions), and check it frequently.
When using the transducers underwater, the radio transmission range is reduced, and signal loss may
occur.
Water-proof belts like M1562B are recommended for the cableless transducers when monitoring in
water.
3
97
Switching the Monitor to Standby
To switch the monitor to Standby:
Either
1Select the Monitor Standby SmartKey.
Or
1Enter the Main Setup menu using the SmartKey.
2Select Monitor Standby.
3Pressing any key or selecting any field on the screen will resume monitoring.
Note
If a Avalon CL base station is connected to your FM 20/30 monitor, do not turn off the monitor if
you need to recharge the batteries of the CL transducers. They can only be recharged if the FM20/30
monitor is on. If an Avalon CL base station is connected to an FM40/50, the batteries of the CL
transducers can be recharged while the monitor is in Standby mode.
After Monitoring
1Discharge the patient.
2Remove the transducer from the patient and, using a soft tissue, remove any gel from it. Then
clean the transducer.
3Dock CL transducers to their base station so they can recharge.
4Tear off the paper at the fold. To avoid misalignment of the recorder mechanism, NEVER pull on
the paper to advance it, or try to tear it other than at a fold (unless using the paper guide with the
FM40/FM50).
5Switch off the monitor.

3 Basic Operation
98
Disconnecting from Power
FM20/30 To disconnect the monitor from AC power, switch the monitor off using the On/Off switch located
on the right side of the device, or unplug the power cord from the AC mains socket.
FM40/FM50
and FM20/
FM30 with
Battery
Option
The On/Standby button does not disconnect the monitor from the AC power source. To disconnect,
unplug the power cord from the AC mains socket. Note that if the power cord is unplugged from the
AC mains socket before the monitor is put into Standby, a beeper is activated. The beeper warns you if
the monitor is accidentally disconnected from AC mains.
Power On/Power Off Behavior
The general rules determining the behavior of the fetal monitors when connected to, or disconnected
from power are as follows:
• A fetal monitor that was switched on prior to a temporary power loss, switches on again when
power is restored.
• A fetal monitor that was switched off prior to a temporary power loss, remains off when power is
restored.
• When AC mains power is lost, a battery powered monitor (FM20/30) continues to run without
interruption on battery power.
Monitoring After a Power Failure
• A fetal monitor that was switched on prior to a temporary power loss switches on again when
power is restored.
• A fetal monitor that was switched off prior to a temporary power loss remains off when power is
restored.
• If the fetal monitor is without power for less than one minute, monitoring will resume with all
active settings unchanged.
• If the fetal monitor is without power for more than one minute, the behavior depends on your
configuration.
–If
Automat. Default is set to Yes, the default profile will be loaded when power is restored.
–If
Automat. Default is set to No, all active settings are retained, if power is restored within 48
hours. The Automat. Default setting is made in Configuration Mode.
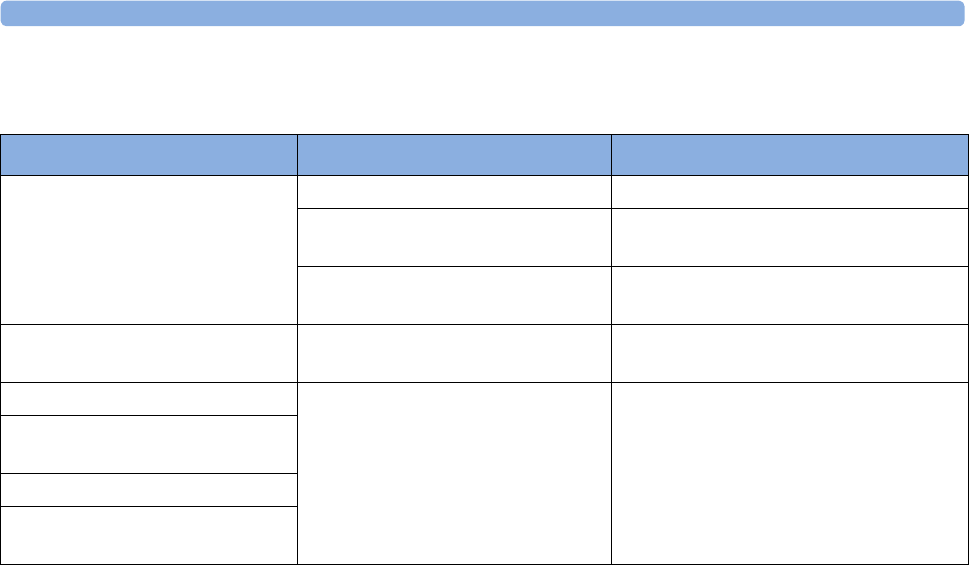
3 Basic Operation
99
Troubleshooting
Problem Possible Causes Solutions
Light or no trace. Wrong paper. Use recommended paper.
Dirty printhead. Clean printhead. See “Cleaning the Print
Head” on page 255.
FM20/30 only: Paper misaligned due
to drawer not being correctly shut.
Shut the drawer fully, pushing evenly with
both hands.
End of paper noted when pack not
finished.
Bad paper feed or wrong paper. Check paper feed and use recommended
paper.
Check Paper INOP is displayed. INOP messages always indicate
equipment problems.
See “Patient Alarms and INOPs” on
page 121.
FetRec Equip Malf INOP is
displayed.
Paper End INOP is displayed.
Wrong Paper Scale INOP is
displayed.

3 Basic Operation
100
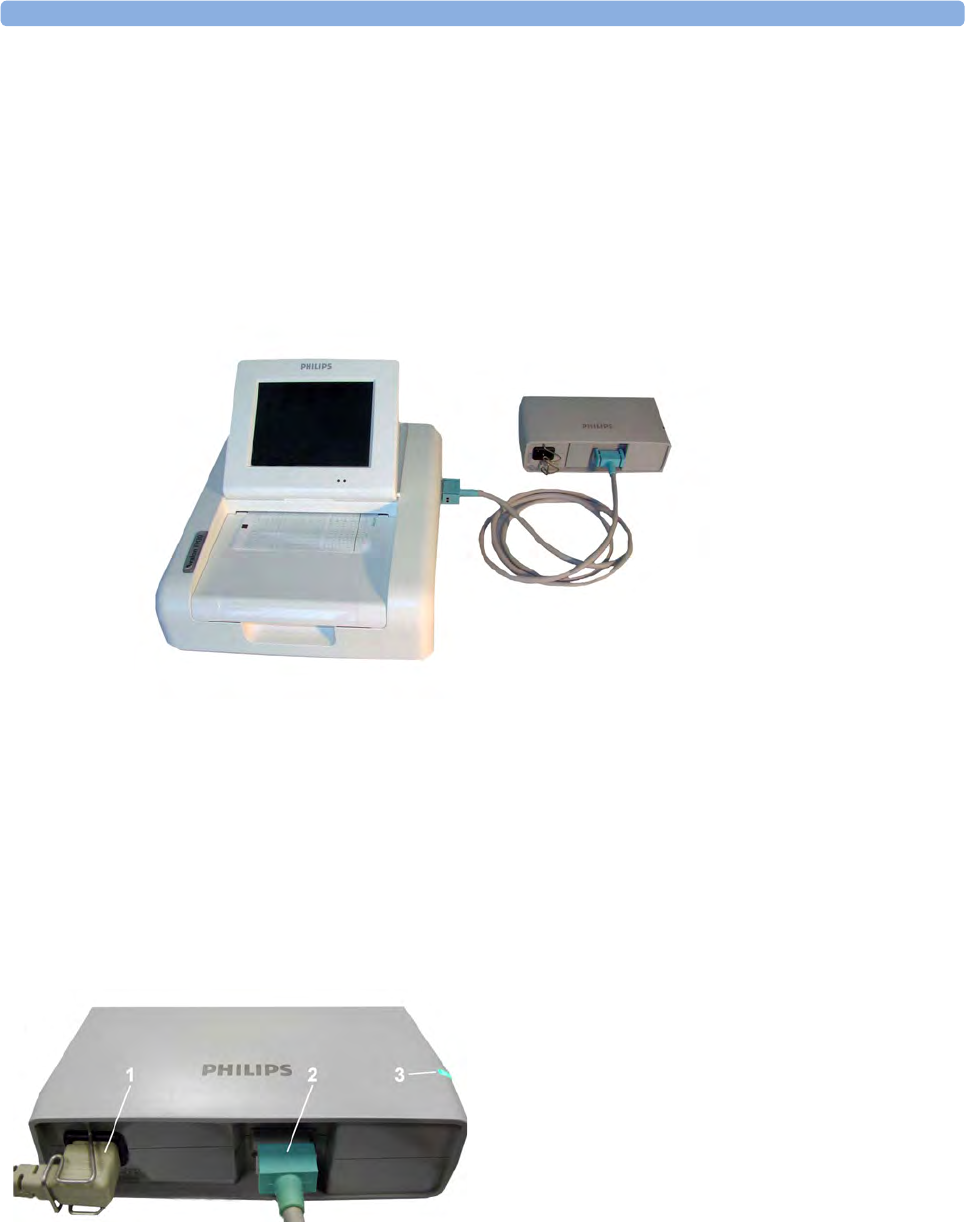
4 FM20/30 Battery Option
101
4FM20/30 Battery Option
You can switch between battery-powered and mains-powered (AC) operation without interrupting
monitoring.
The monitor is connected to the AC mains power via the external power supply.
NOTE
The battery option is not available for the FM40/FM50.
External Power Supply M8023A
The external power supply M8023A (option #E25) allows you to operate the fetal monitor from an
AC (alternating current) power source of 100 V to 240 V (± 10%) and 50/60 Hz (± 5%). If this option
is used, then the M8023A (option #E25) power supply is included for FM20/30.
1AC power cord. Connect to AC mains socket.
2Measurement Link (MSL) cable. Supplies power to
the monitor for operation and for battery charging.
3Power-on LED. The green light is on when the
external power supply is connected to AC mains.

4 FM20/30 Battery Option
102
WARNING
• Always use the supplied power cord with the earthed mains plug to connect the external power
supply M8023A (option #E25) to an earthed AC mains socket. Never adapt the mains plug from
the power supply to fit an unearthed AC mains socket.
• Do not use AC mains extension cords or multiple portable socket-outlets. If a multiple portable
socket-outlet without an approved isolation transformer is used, the interruption of its protective
earthing may result in enclosure leakage currents equal to the sum of the individual earth leakage
currents, so exceeding allowable limits.
• Do not connect any devices that are not supported as part of a system.
• Any non-medical device placed and operated in the patient’s vicinity must be powered via an
approved isolation transformer that ensures mechanical fixing of the power cords and covering of
any unused power outlets.
Using Batteries
The Lithium Ion batteries used in your monitor store a large amount of energy in a small package. This
allows reliable battery-operated monitoring but also requires care in use and handling of the batteries.
Follow the instructions in this chapter and see the Service Guide for further details.
Battery Power Indicators
The battery LED and battery status information on the Main Screen, in combination with INOP
messages and prompts, help you keep track of the battery power status. The indicators always show
the remaining capacity in relation to the battery's actual maximum capacity, which may lessen as the
battery ages. You can see the actual capacity in the Battery Status window.
Battery LED
The possible battery LED status on the right side of the monitor is described in the table below.
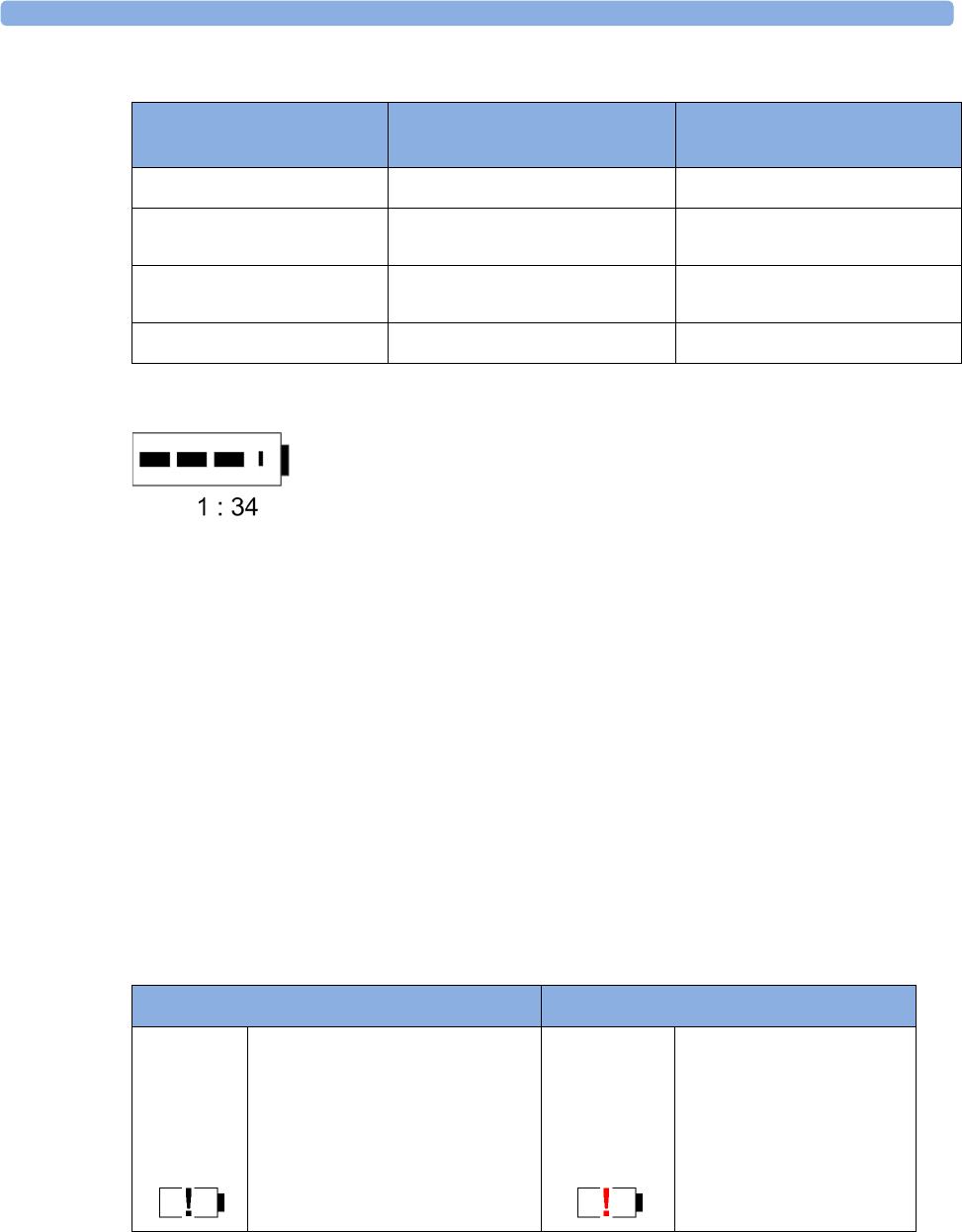
4 FM20/30 Battery Option
103
Battery Status on the Main Screen
Battery status information is permanently displayed on all screens. It shows the status of the battery,
with the battery power remaining, with an estimate of the monitoring time this represents.
Battery power gauge: This shows the remaining battery power. It is divided into sections, each
representing 20% of the total power. If three sections are filled, as in this example, this indicates that
60% battery power remains. If no data is available from the battery, a question mark is shown in the
gauge.
Monitoring Time Available: Below the battery power gauge a time is displayed. This is the estimated
monitoring time available with the current battery power. Note that this time fluctuates depending on
the system load (the display brightness, the recorder configuration, and how many measurements you
carry out).
Battery malfunction symbols: Normal battery function is indicated by the battery power gauge,
together with the remaining operating time, on the main screen. You are informed of problems or
changes in the status of the battery by the battery status/malfunction indicator. This consists of a blank
battery gauge containing a "!" symbol. If the symbol is red, this indicates a critical situation. You can
check the specific cause of the problem by looking at the symbol(s) displayed in the Battery Status
window.
Battery LED Colors If the monitor is connected to
mains power, this means
If the monitor is running on
battery power, this means
Green Battery power is > 90%
Yellow Battery charging (battery power
< 90%)
Red, flashing Less than 10 minutes power
remaining
Red, flashes intermittently Battery or charger malfunction Battery malfunction
Battery Status Indicator Battery Malfunction Indicator
Alternates with the battery gauge
on the main screen.
Check in the Battery Status
window to see which status symbol
is displayed to identify the cause.
The red exclamation mark
flashes. Critical battery
situation or malfunction.
Check in the Battery Status
window to see which
malfunction indicator is
displayed, or refer to the
INOP, to identify the cause.
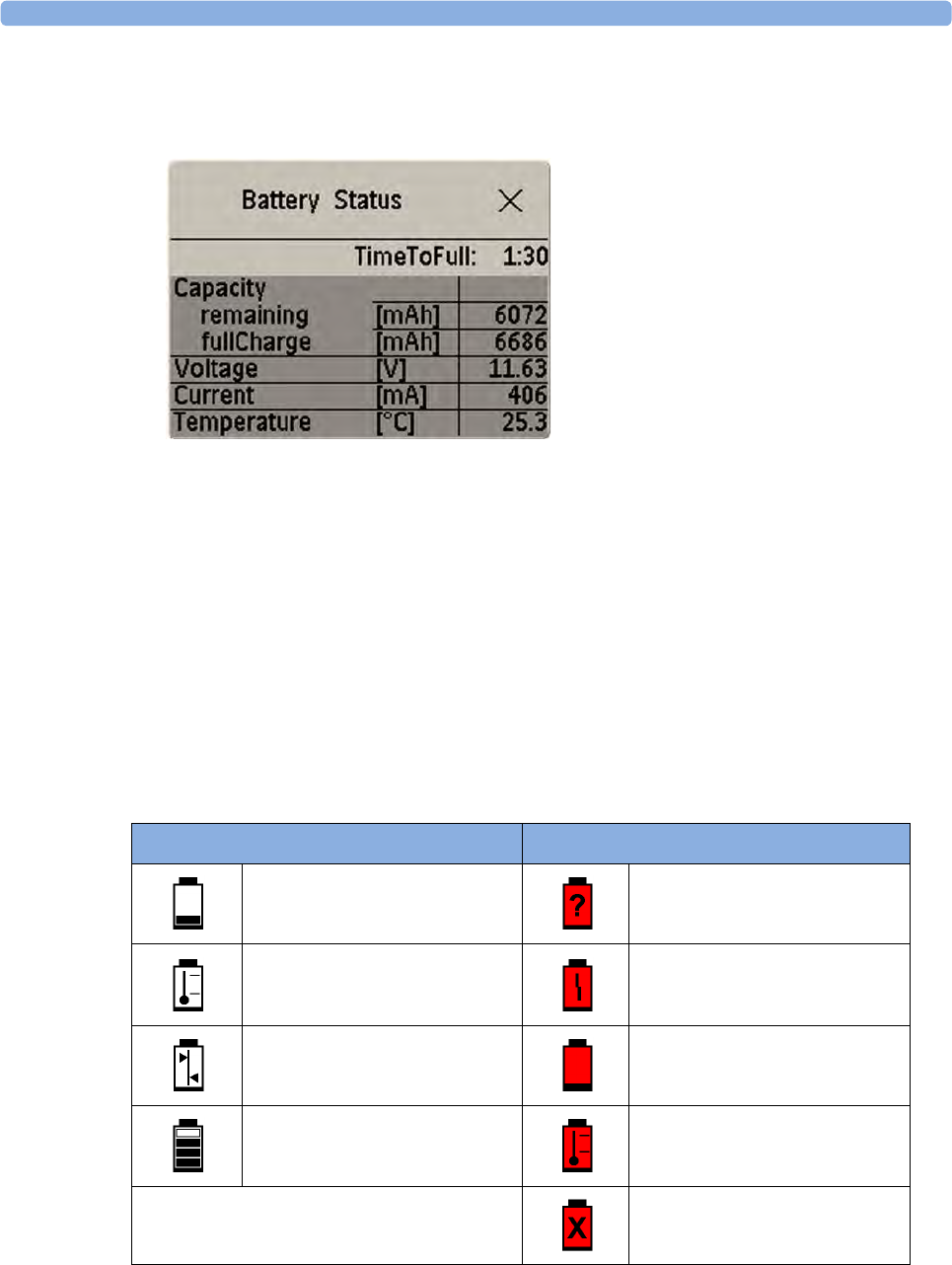
4 FM20/30 Battery Option
104
Battery Status Window
1To access the Battery Status window and its associated pop-up keys, select the battery status
information on the screen, or select Main Setup, Battery.
–Capacity, remaining tells you how much power is left in the battery.
–Capacity, fullCharge tells you how much power the battery can hold when fully charged.
–TimeToEmpty tells you approximately how long you can continue to use the monitor without
an AC connection. The time span fluctuates depending on the system load (the display
brightness and how many measurements you carry out), and the remaining capacity of the
battery.
–TimeToFull is shown in place of TimeToEmpty if the monitor is connected to a power supply,
and tells you how much time is left until the battery is charged to 90%. If >10 hrs is shown
here, the battery may not charge completely when the monitor is in use.
Battery status/malfunction symbols: If a problem is detected with the battery, an INOP may be
issued, and the following symbols are displayed in the Battery Status window, where they may be
accompanied by a status message providing more details.
Symbols indicating critical situations are colored red.
Battery Status Symbols Battery Malfunction Symbols
Battery is empty (Red) incompatible battery
Battery not charging as the
temperature is above or below the
specified range
(Red) battery malfunction
Battery requires maintenance (Red) battery has no power left
Charging stopped to protect the
battery
(Red) battery temperature too
high
(Red) battery is missing, insert
battery

4
105
Checking Battery Charge
To check the charge status of a battery, refer to the battery power gauge on the screen, or open the
Battery Status window.
When Battery Lifetime is Expired
When the battery is aged, either after 3 years from manufacturing date or after 500 charge/discharge
cycles, it is recommended to replace the battery. To remind you of this, a message will appear in the
Battery Status window. This message will only be displayed at the appropriate time when the date and
time on the monitor is correct.
Optimizing Battery Performance
The performance of rechargeable batteries may deteriorate over time. Battery maintenance as
recommended here can help to slow down this process.
Display Brightness Setting
1In the Main Setup menu, select User Interface, Brightness, then Optimum. This selects a level of
brightness suitable for most monitoring locations that uses less battery power than brighter
settings.
2Ensure that the current level of brightness is suitable for your monitoring location.
Charging the Battery
To charge the battery,
1Connect the monitor to the external power supply (M8023A).
2Charge the battery until it is full, the battery LED is green, and the battery power gauge is filled.
During high load of the monitor (usage of multiple measurements) the battery may not charge. To
remedy this:
• reduce the load by removing measurements,
• reduce the screen brightness or stop the recorder.
Internal temperature conditions can also cause the battery to not charge. This is necessary to protect
the battery from damage and does not indicate a malfunction. Keep the monitor at room temperature
and move it away from heat sources or out of direct sunlight. The battery will resume charging when
the temperature is within range again. The battery will charge more quickly if the monitor is switched
off.
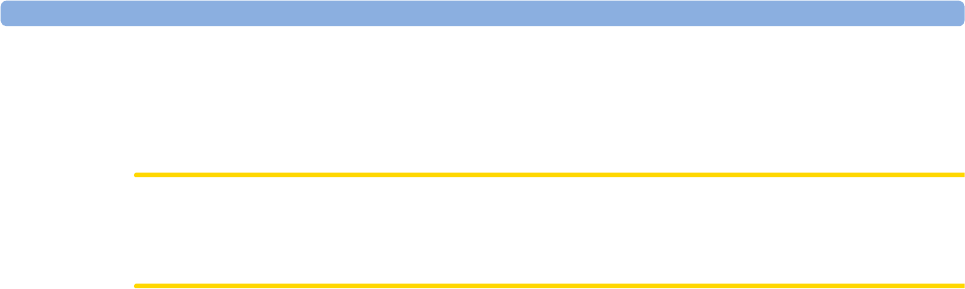
4 FM20/30 Battery Option
106
Conditioning the Battery
You must condition the battery when the "battery requires maintenance" symbol shows on the screen.
Do not interrupt the charge or discharge cycle during conditioning.
CAUTION
Condition the battery with a monitor not currently in use. The monitor switches off automatically
when there is no battery power left.
To condition the battery,
1Charge the battery until it is completely full. Open the Battery Status window and check that the
Batt fully charged message is displayed.
2Disconnect the monitor from mains power, and let the monitor run until there is no battery power
left and the monitor switches itself off.
3Reconnect the monitor to mains power and charge the battery until it is full for use or charge to
50% for storage.
Storing the Battery
The battery should not remain inside the monitor if it is not used for a longer period of time. Batteries
should be charged to a maximum of 50% for storage. For battery removal or exchange, contact your
service personnel.
NOTE
The battery will discharge over time in a monitor that is not connected to AC via the external power
supply (M8023A). The reported values for "remaining capacity" and "runtime" will become less
accurate when the battery is stored in this way for a longer period of time (that is, several weeks).
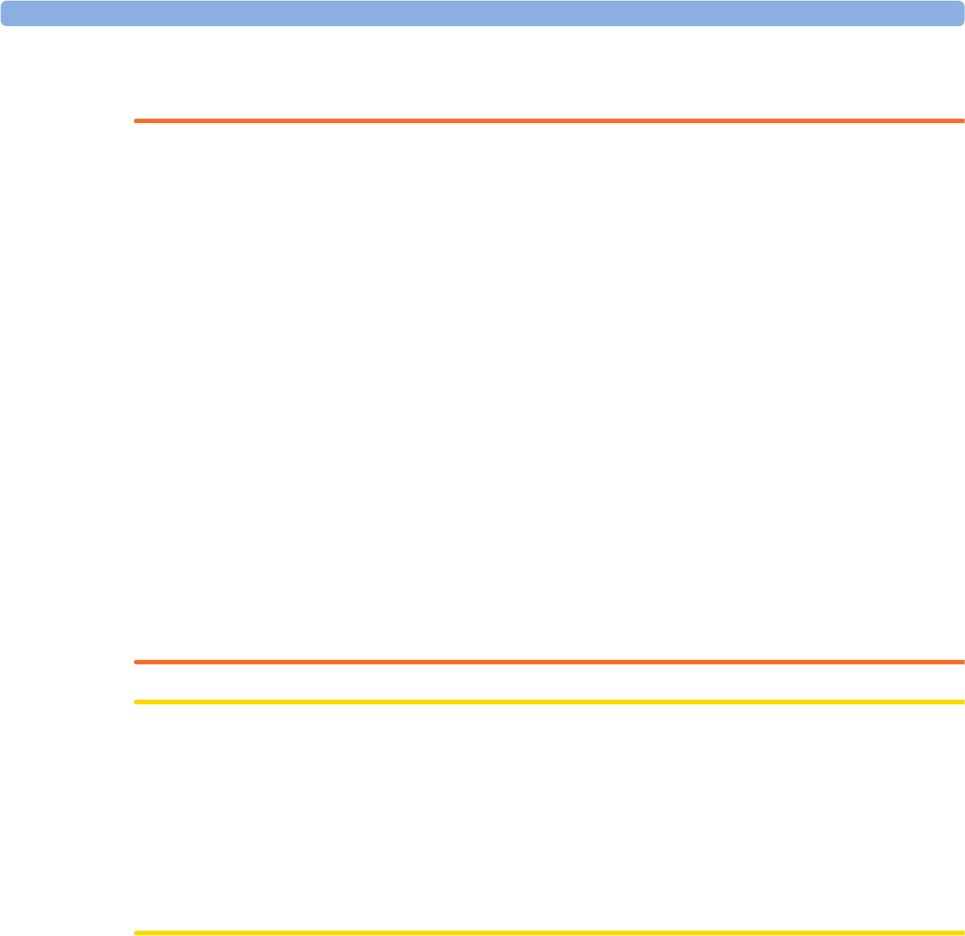
4 FM20/30 Battery Option
107
Battery Safety Information
WARNING
Use only Philips batteries part number M4605A. Use of a different battery may present a risk of fire
or explosion.
Do not open batteries, or dispose of them in fire, or cause them to short circuit. They may ignite,
explode, leak or heat up, causing personal injury.
If battery leakage should occur, avoid contact with skin. Refer to qualified and authorized service
personnel.
Dispose of used batteries promptly and in an environmentally-responsible manner. Do not dispose
of the battery in normal waste containers. Consult your hospital administrator to find out about local
arrangements. Do not expose batteries to liquids.
Do not crush, drop or puncture batteries - mechanical abuse can lead to internal damage and internal
short circuits which may not be visible externally.
If a battery has been dropped or banged against a hard surface, whether damage is visible externally or
not:
• discontinue use
• dispose of the battery in accordance with the disposal instructions above.
Keep batteries out of the reach of children.
CAUTION
Do not disassemble, heat above 100°C (212°F) or incinerate the batteries, to avoid the risk of fire and
burns. Keep batteries out of the reach of children and in their original package until you are ready to
use them.
If battery leakage should occur, use caution in removing the battery. Avoid contact with skin. Refer to
qualified and authorized service personnel.
Do not install or use pre-damaged batteries.

4 FM20/30 Battery Option
108

5 Alarms
109
5Alarms
The alarm information here applies to all measurements. Measurement-specific alarm information is
contained in the sections on individual measurements.
The fetal monitor has two different types of alarm: patient alarms and INOPs.
Patient Alarms
Red and yellow alarms are patient alarms. A red alarm indicates high priority, such as a potentially life
threatening situation (for example, SpO2 below the desaturation alarm limit). A yellow alarm indicates
a lower priority alarm (for example, a fetal heart rate alarm limit violation).
INOPs
INOPs are technical alarms. They indicate that the monitor cannot measure and therefore not detect
critical conditions reliably. If an INOP interrupts monitoring and alarm detection (for example, MECG
Leads Off), the monitor places a question mark in place of the measurement numeric and sounds an
audible tone. INOPs without this tone indicate that there may be a problem with the reliability of the
data, but that monitoring is not interrupted.
Most INOPs are light blue, however there are a small number of INOPs which are always yellow or
red to indicate a severity corresponding to red and yellow alarms. The following INOPs can also be
configured as red or yellow INOPs to provide a severity indication:
•MECG Leads Off
•<SpO₂ Label> No Pulse
•Tele Disconnected
•Battery Empty / Replace Battery
Alarm Delays
There is a delay between a physiological event at the measurement site and the corresponding alarm
indication at the monitor. This delay has two components:
•The general measurement delay time is the time between the occurrence of the
physiological event and when this event is represented by the displayed numerical values.
This delay depends on the algorithmic processing and, for certain measurements (SpO2, EEG and
BIS), on the configured averaging time. The longer the averaging time is configured, the longer it
takes until the numerical values reflect the physiological event.
•The time between the displayed numerical values exceeding an alarm limit and the alarm
indication on the monitor. This delay is the sum of the alarm delay configured for the specific
measurement plus the system alarm delay. The system alarm delay is the processing time the
system needs for any alarm on the monitor to be indicated after the measurement has triggered the
alarm. See the performance specifications in “Specifications and Standards Compliance” on
page 269 for the system alarm delay specification.
Multiple Alarms
If more than one alarm is active, the alarm messages are shown in the alarm status area in succession.
An arrow symbol next to the alarm message informs you that more than one message is active.
The monitor sounds an audible indicator for the highest priority alarm. If more than one alarm
condition is active in the same measurement, the monitor announces the most severe.
5 Alarms
110
WARNING
Alarm systems of the monitor and those of the connected OB system are independent and not
synchronized.
Alarm Mode
You can configure the alarm mode for your fetal monitor. There are two possible modes:
•All: alarms and INOPs are enabled, with all audible and visual indicators active.
•INOP only: only INOPs are enabled, with audible and visual indication active. This is the default
alarm mode.
WARNING
In INOP only mode, no fetal/maternal patient alarms are enabled or indicated.
The alarm status area for yellow and red alarms shows the INOP only indication in conjunction with
the "Alarms Off" symbol. No alarm limits or alarm off icons are displayed. No fetal/maternal patient
alarm settings are available in the setup menus.
Nurse Call Systems
If configured to do so, red, yellow and light blue alarms are indicated on a nurse call system which is
connected to the optional nurse call relay.
Visual Alarm Indicators
Alarm message: An alarm message appears in the alarm status area on the second line at the top of
the screen indicating the source of the alarm. If more than one measurement is in an alarm condition,
the message changes every two seconds, and has an arrow at the side. The background color of the
alarm message matches the alarm priority: red for red alarms, yellow for yellow alarms, and light blue
for INOPs. The asterisk symbols (*) beside the alarm message match the alarm priority: *** for red
alarms, ** for yellow alarms. INOPs are displayed without asterisks.
Depending on how your monitor is configured, it may display alarm limit violation messages:
• in text form, for example ** FHR1 Low or
• in numeric form, for example **FHR1 94<110, where the second number shows the currently set
alarm limit, and the first number shows the value at which that alarm limit was violated by the
widest margin.
Flashing numeric: The numeric of the measurement in alarm flashes.
Bright alarm limits: If the alarm was triggered by an alarm limit violation, the corresponding alarm
limit on the monitor screen is shown more brightly.
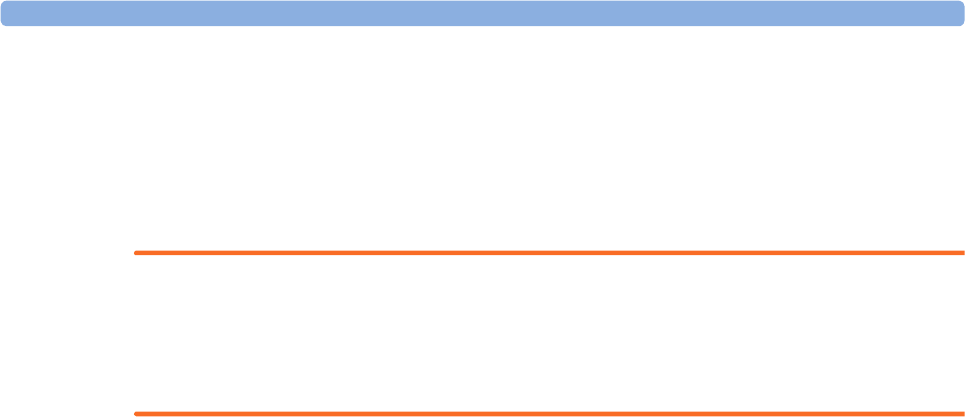
5 Alarms
111
Audible Alarm Indicators
The audible alarm indicators configured for your fetal monitor depend on which alarm standard
applies in your hospital. Audible alarm indicator patterns are repeated until you acknowledge the alarm
by switching it off or pausing it, or until the alarm condition ceases (if audible alarm indication is set to
non-latching).
WARNING
Do not rely exclusively on the audible alarm system for fetal monitoring. Adjustment of alarm volume
to a low level or off during monitoring may result in a dangerous situation. Remember that the most
reliable method of fetal monitoring combines close personal surveillance with correct operation of
monitoring equipment.
Alarm Tone Configuration
The audible alarm indicators of your monitor are configurable. In the monitor's Configuration Mode,
you can:
• increase the alarm volume of unacknowledged alarms at regular intervals
• change the interval between alarm sounds (ISO/IEC Standard alarms only)
• change the base volume of the red and yellow alarm tones and the INOP tones
• change the alarm sound to suit the different alarm standards valid in different countries.
Standard Philips Alarms
• Red alarms: a high pitched sound is repeated once a second.
• Two-star yellow alarms and yellow INOPs: a lower pitched sound is repeated every two seconds.
• One-star yellow alarms (short yellow alarms): the audible indicator is the same as for yellow
alarms, but of shorter duration.
• Standard INOPs: an INOP tone is repeated every two seconds.
ISO/IEC Standard 9703-2 Audible Alarms
• Red alarms and red INOPs: a high pitched tone is repeated five times, followed by a configurable
pause.
• Two-star yellow alarms and yellow INOPs: a lower pitched tone is repeated three times, followed
by a configurable pause.
• One-star yellow alarms (short yellow alarms): the audible indicator is the same as for yellow
alarms, but of shorter duration.
• Standard INOPs: a lower pitched tone is repeated twice, followed by a pause.
5 Alarms
112
Changing the Alarm Tone Volume
The alarm volume symbol at the top right of the monitor screen gives you an indication of the current
volume. To change the volume:
1Select the volume symbol.
2The volume scale pops up.
3Select the required volume from the volume scale.
When the alarm volume is set to zero (Off), the alarm volume symbol shows this symbol:
If you switch the alarm volume off, you will not get any audible indication of alarm conditions.
Minimum Volume for Severe Yellow or Red INOPs
Severe yellow or red INOPs require action to ensure the well-being of the patient. Therefore the
minimum volume for the INOP tone is set to at least alarm volume 8, irrespective of the current alarm
volume setting. The INOP tone will sound even if the monitor alarm volume is set to zero.
The severe INOPs for which this applies are:
Alarm Volume
INOP Factory Default INOP tone
Battery Empty cyan severe (fetal monitor with battery option)
hard (CL Pods)
soft (CL transducers)
ECG Leads Off cyan hard
NBP Cuff Overpress cyan severe
Cuff Not Deflated cyan severe
!! <SpO₂ Label> No Pulse cyan hard
5 Alarms
113
Power Loss Tone
FM20/30
with
Battery
Option,
FM40/50
When power is lost - no power is available from the AC power source or from the battery - a beeper
will sound. The tone can be silenced by pressing the On/Standby button.
Acknowledging Alarms
To acknowledge all active alarms and INOPs, select the Silence key This switches off the audible
alarm indicators.
A check mark beside the alarm message indicates that the alarm has been acknowledged.
If the condition that triggered the alarm is still present after the alarm has been acknowledged, the
alarm message stays on the screen with a check mark symbol beside it.
If the alarm condition is no longer present, all alarm indicators stop and the alarm is reset.
Switching off the alarms for the measurement in alarm, or switching off the measurement itself, also
stops alarm indication.
Acknowledging Disconnect INOPs
Acknowledging an INOP that results from a disconnected transducer switches off the associated
measurement.
Alarm Reminder
If Alarm Reminder is configured on for your monitor, you will get an audible reminder of alarm
conditions that remain active after you have acknowledged the alarm. This reminder may take the form
of a repetition of the alarm tone for a limited time, or an unlimited repetition of the alarm tone (this is
the same as a new alarm). Alarm Reminder is available only for yellow and red INOPs and not for
standard light blue INOPs.
In Configuration Mode, you can set the interval between silencing the alarm and sounding the
reminder tone to one, two, or three minutes.

5 Alarms
114
Pausing or Switching Off Alarms
If you want to temporarily prevent alarms from sounding, for example while you are moving a patient,
you can pause alarms. Depending on your fetal monitor configuration, alarms are paused for one, two,
or three minutes, or infinitely.
To view the alarm pause setting chosen for your unit:
1Select Main Setup, Alarms, Alarm Settings.
2Check the Alarms Off setting.
This setting can be changed in Configuration Mode.
There are some settings made in Configuration Mode that can affect the availability of the pause
alarms functionality.
•The
Pause Alarms / Alarms Off permanent key can be removed from the screen to avoid
unintentional switching off of alarms. In this case you can only pause alarms or switch alarms off
permanently in the Alarms menu, under Main Setup.
•The
Pause Alarms / Alarms Off permanent key and the corresponding hardkey can be
configured to pause or switch off red and yellow alarms, yellow alarms only, or not to function at
all. If they are configured not to function, you cannot pause alarms or switch alarms off
permanently at all.
When the alarms off priority is set to Yellow Only, the Pause Alarms / Alarms Off key becomes
the Pause Yellow / Yellow Al. Off.
To Pause All Alarms
If you have configured alarms to be paused for one, two, or three minutes, the SmartKey is labeled
Pause Alarms.
Select the Pause Alarms SmartKey to pause all alarms.
Or
1Select Main Setup.
2Select Alarms.
3Select Pause Alarms.
To Switch All Alarms Off
You can switch alarms off permanently if your monitor is configured to allow infinite alarms pause,
and the SmartKey is labeled Alarms Off.
Select the Alarms Off SmartKey.
Or
1Select Main Setup.
2Select Alarms.
5 Alarms
115
3Select Alarms Off.
To Switch Individual Measurement Alarms On or Off
This applies to alarm mode All.
1Select the measurement numeric to enter its setup menu.
2Select Alarms to toggle between On and Off.
The alarms off symbol is shown beside the measurement numeric.
While Alarms are Paused or Off
When red alarms are paused or off:
The red Alarms Paused lamp on the monitor front panel is lit.
In the alarm field, the monitor displays the message Al. Paused x:yy or Alarms Off, together with the
alarms paused symbol or the alarms off symbol.
When yellow alarms are paused or off:
The yellow Alarms Paused lamp on the monitor front panel is lit.
In the alarm field, the monitor displays the message YellowPaused x:yy or Yellow Alarms Off,
together with the alarms paused symbol or the alarms off symbol.
For red and yellow alarms:
• No alarms are sounded and no alarm messages are shown.
• INOP messages are shown but no INOP tones are sounded.
The following INOPs are the only exceptions:
NBP Cuff Overpress, Batt Empty and Batt Malfunction (these INOPs are issued even if alarms are
paused or off).
These INOPs switch the alarms on, and the INOP tones are sounded, even if alarms are paused or off.
You need to remove the INOP condition first before you can switch the alarm tones off again.
Restarting Paused Alarms
To manually switch on alarm indication again after a pause, select the SmartKey Pause Alarms (or
Alarms Off) again.
Alarm indication starts again automatically after the pause period expires. If the monitor is configured
to stay paused infinitely, you must select Alarms Off again to restart alarm indication.
Alarms Paused Alarms Off
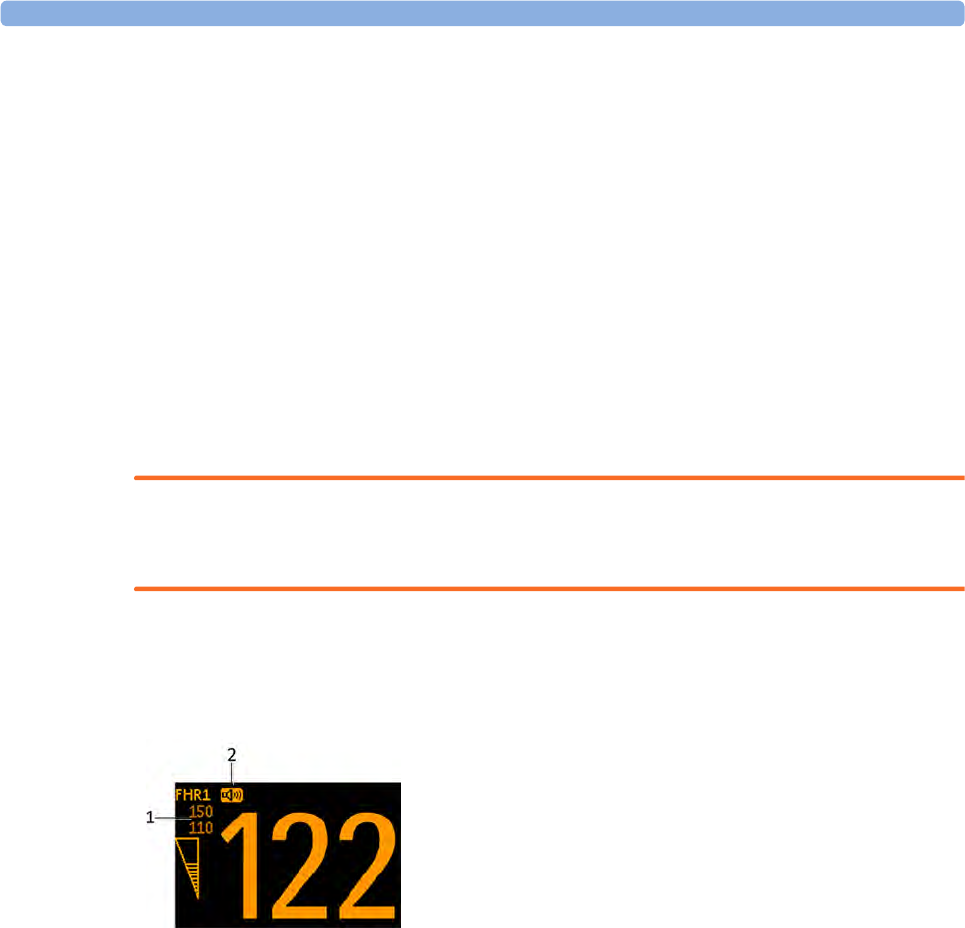
5 Alarms
116
Extending the Alarm Pause Time
If your monitor has the function extended alarm pause enabled, you can extend the alarm pause time.
Use this to prevent alarms being indicated, for example, while you are washing a patient or carrying out
a procedure. Only extend the alarm pause time when you are sure that clinical personnel are available
to monitor the patient's condition closely.
To extend the alarm pause time to five or 10 minutes,
1Select one of the alarm fields. This calls up the Alarm Messages window.
2Select either the pop-up key PauseAl. 5 min or the pop-up key PauseAl. 10 min. Each time you
select one of these pop-up keys, the Alarm Pause Time is reset to five (or 10) minutes.
Alarm Limits
The alarm limits you set determine the conditions that trigger yellow and red limit alarms.
WARNING
Be aware that the monitors in your care area may each have different alarm settings, to suit different
scenarios. Always check that the alarm settings are appropriate before you start monitoring.
Viewing Individual Alarm Limits (Alarm Mode "All" Only)
You can usually see the alarm limits set for each measurement next to the measurement numeric on
the main screen.
If your monitor is not configured to show the alarm limits next to the numeric, you can see them in the
appropriate measurement setup menu. Select the measurement numeric to enter the menu and check
the limits.
Changing Alarm Limits
To change individual measurement alarm limits using the measurement's setup menu:
1In the measurement's setup menu, select the alarm limit you want to change. This calls up a list of
available values for the alarm limit.
2Select a value from the list to adjust the alarm limit.
Alarm Limits
Audio source symbol
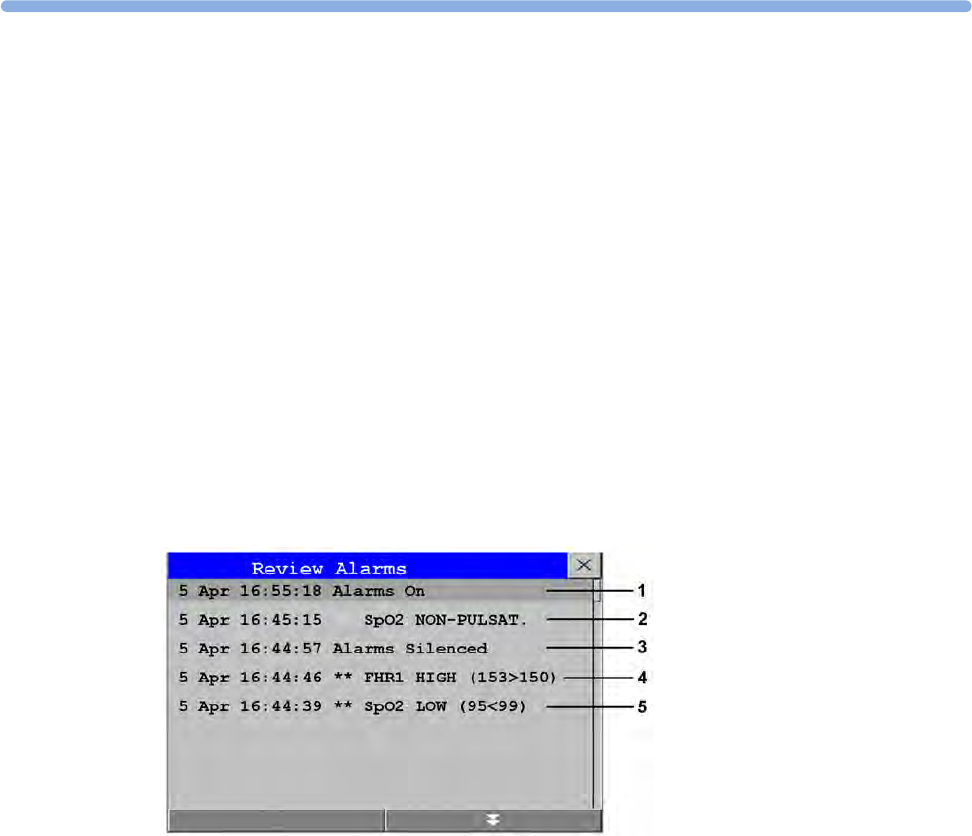
5
117
Reviewing Alarms
To review the currently active alarms and INOPs, select any of the alarm status areas on the fetal
monitor screen. The Alarm Messages window pops up. All alarms and INOPs are erased from the
monitor's alarm history when you discharge a patient, or if you enter Demonstration Mode.
Alarm Messages Window
The Alarm Messages window shows all the currently active alarms and INOPs in chronological order,
beginning at the top with the most recent. INOPs are shown on the left hand side, and alarms are
shown on the right hand side. Any active red alarms are shown first, followed by yellow alarms.
Acknowledged alarms or INOPs are shown with the check mark symbol.
The Alarm Messages window pop-up keys appear when the window is opened. Selecting the Review
Alarms pop-up key opens the Review Alarms window.
Review Alarms Window
The Review Alarms window contains a list of up to 300 of the most recent alarms and INOPs with
date and time information. If configured to do so, each alarm is shown with the alarm limit active
when the alarm was triggered and the maximum value measured beyond this limit. The Review Alarms
window also shows any changes made to the Alarms On/Off or Silence status. Only the main alarms
On/Off transitions are logged in the alarm history, and On/Off alarm transitions for individual
measurements are not logged.
The information in the Review Alarms window is deleted when a patient is discharged.
The Review Alarms window pop-up keys appear when the window is opened. Selecting the Active
Alarms pop-up key opens the Alarm Messages window.
1Alarms On
2SpO₂ No Pulse
3Alarms Silenced
4** FHR1 High
5** SpO₂ Low
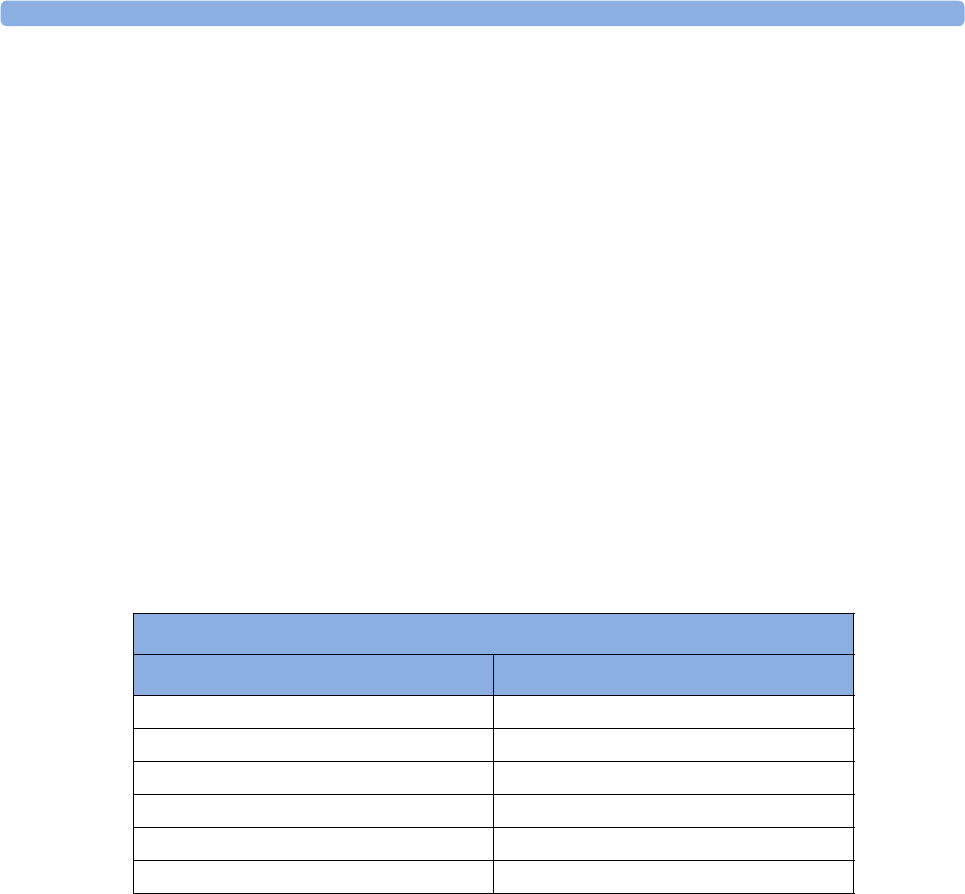
5 Alarms
118
Latching Alarms
The alarm latching setting for your monitor defines how the alarm indicators behave when you do not
acknowledge them. When alarms are set to non-latching, their indicators end when the alarm condition
ends. Switching alarm latching on means that visual and/or audible alarm indications are still displayed
or announced by the monitor after the alarm condition ends. The indication lasts until you
acknowledge the alarm.
Viewing the Alarm Latching Settings
To see the alarm latching setting for your monitor:
1In the monitor's Main Setup menu, select Alarms.
2Select Alarm Settings, and see the Visual Latching and Audible Latching settings.
This setting can be changed in Configuration Mode. You should be aware of the settings chosen for
your unit. There are three possible choices each for visual and audible latching: Red, Red & Yellow,
and Off. The audible latching configuration can never be configured to a higher level than that
configured for the visual latching. In other words, the audible latching setting is always the same level,
or lower, than the visual latching setting. For example, if visual latching is configured to Red Only,
then audible latching can only be set to Red or Off. The following table shows the possible
combinations for latching settings:
Possible Combinations for Alarm Latching Settings
Visual Latching Setting Audible Latching Setting
Red & Yellow Red & Yellow
Red & Yellow Red
Red & Yellow Off
Red Red
Red Off
Off Off
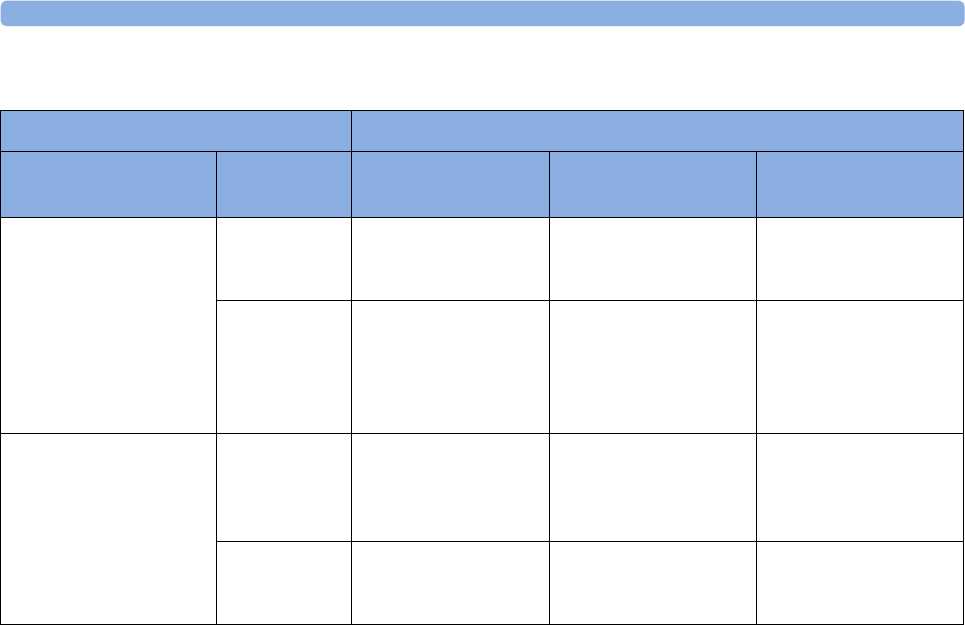
5 Alarms
119
Alarm Latching Behavior
All INOPs except the "unplugged" INOPs are non-latching.
Testing Alarms
In general, to test the functioning of visible and audible alarms, do the following:
1Enable the alarm.
2Set the alarm limits.
3Measure or simulate the parameter that is out of range, or signal loss.
4Verify that the visible and audible alarms are working.
As an example, to test the FHR alarms:
1Connect the US transducer to a fetal sensor socket.
2Enable the FHR alarming (see “Turning Alarms On or Off ” on page 185).
Set the high alarm limit and delay to 150 bpm and 60 seconds respectively, and the low alarm limit and
delay to 110 bpm and 60 seconds respectively (see “Changing Alarm Limits” on page 185).
1Generate a fetal heart rate of approximately 180 bpm (3 beats per second) for more than one
minute.
2Verify the functioning of the visible and audible alarm.
Alarm Condition Red and Yellow Measurement Alarms
Acknowledgment Presence Non-latching alarms Visual and audible
latching
Visual latching,
audible non-latching
Alarm has not been
acknowledged
Alarm
condition still
present
Alarm tone on Alarm
message
Alarm tone on Alarm
message Flashing
numerics
Alarm tone on Alarm
message Flashing
numerics
Alarm
condition no
longer present
All audible and visual
alarm indicators
automatically stop
Alarm tone on
Alarm message
Flashing numerics
Alarm message Flashing
numerics
Audible alarm
indicators automatically
stop
Alarm has been
acknowledged
Alarm
condition still
present
Alarm tone off. Alarm
message. Audible
alarm reminder (if
configured)
Alarm tone off Alarm
message Flashing
numerics Audible alarm
reminder (if configured)
Alarm tone off Alarm
message Flashing
numerics Audible alarm
reminder (if configured)
Alarm
condition no
longer present
Audible and visual
alarm indicators
automatically stop
Audible and visual
alarm indicators
automatically stop
Audible and visual
alarm indicators
automatically stop

5 Alarms
120
Alarm Behavior at Power On
If the monitor is switched off for longer than one minute and then switched on again, or after a loss of
power lasting longer than one minute, the monitor can be configured to restore either the alarm
settings from the monitor's User Defaults, or the most recently used alarm settings. When a patient is
discharged, the User Defaults of the monitor are always restored independent of the setting. After any
of these situations, you should check that the alarm settings are appropriate for your patient. If power
is lost for less than one minute, the alarm settings prior to the power loss are restored.
If AlarmsOffAtStart is enabled in Configuration Mode alarms will be initially paused or off the next
time the monitor is switched on (depending on the configuration setting for Alarms Off). Even if it is
enabled, this setting only takes effect if the power down time is more than one minute, and the Global
Setting Automat Default is set to Yes.
In order for alarms to be paused or switched off initially:
• the monitor must be switched off for more than one minute, and
• the main alarms were switched off or paused before the monitor was switched off.
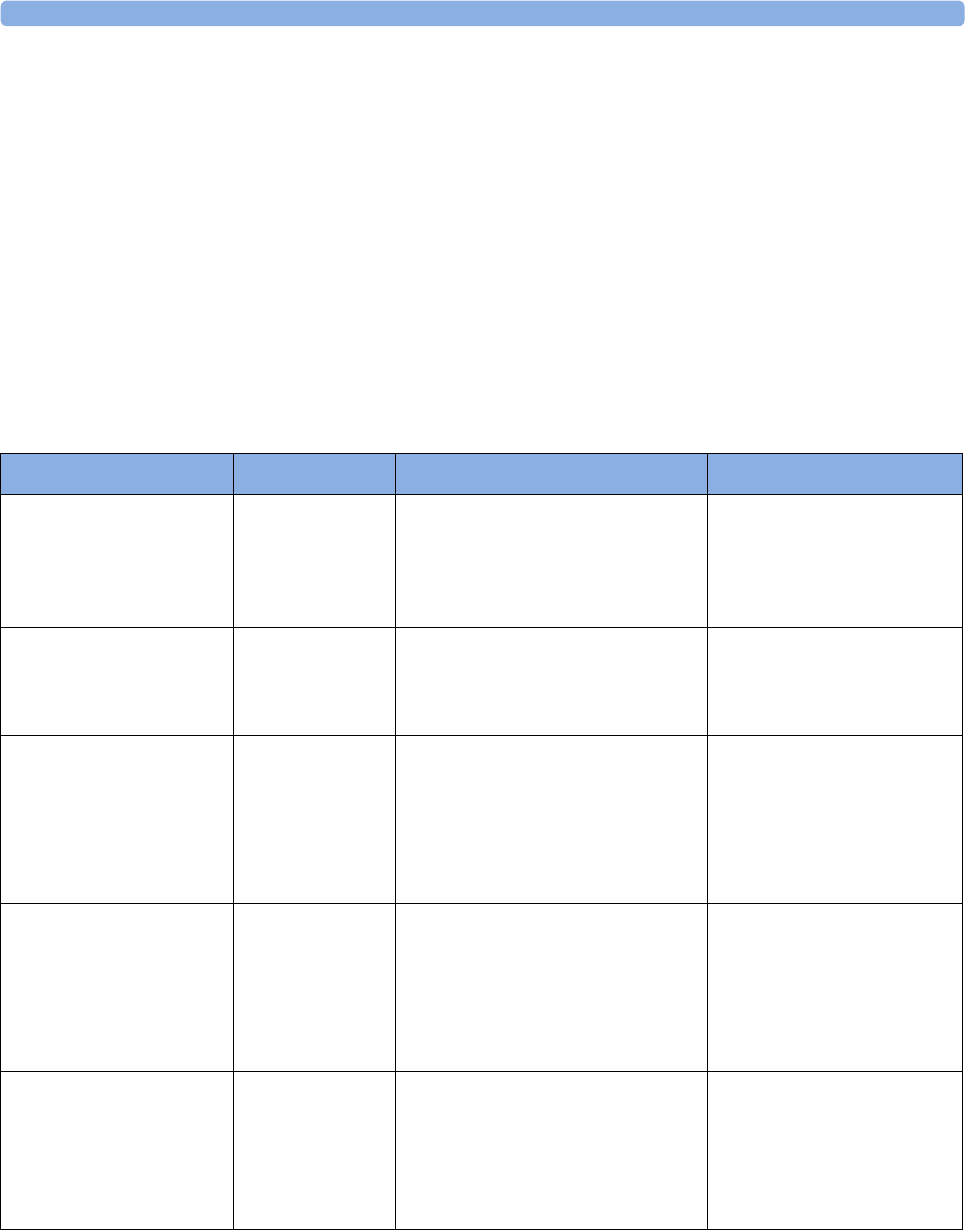
6 Patient Alarms and INOPs
121
6Patient Alarms and INOPs
This chapter lists alarms and technical alarms (INOPs) for the fetal monitors irrespective of their
priority.
Alarm Messages
Fetal alarms are identified by either "FHR" or "DFHR". All other alarms without these identifiers refer
to maternal parameters.
Alarm Message From Condition Indication
*** Brady (Pulse)
***Brady xxx < yyy
SpO2The heart rate from the Pulse signal
has fallen below the bradycardia
limit. xxx denotes the lowest
measured value; yyy is the
bradycardia limit.
Numeric flashes and alarm
limit is highlighted, red alarm
message, alarm tone.
*** Desat
*** Desat xx < yy
SpO2The SpO2 value has fallen below the
desaturation alarm limit. xx denotes
the lowest measured value, and yy is
the desaturation limit.
Numeric flashes, red alarm
message, alarm tone.
** DFHR1 High
** DFHR2 High
** DFHR3 High
**DFHR1 xxx>yyy
**DFHR2 xxx>yyy
**DFHR3 xxx>yyy
FHR (DECG) The fetal heart rate obtained from
DECG has risen above the high
alarm limit.
xxx denotes the highest measured
value, and yyy is the high alarm limit.
Numeric flashes and high
limit is highlighted, yellow
alarm message, alarm tone.
** DFHR1 Low
** DFHR2 Low
** DFHR3 Low
**DFHR1 xxx<yyy
**DFHR2 xxx<yyy
**DFHR3 xxx<yyy
FHR (DECG) The fetal heart rate obtained from
DECG has fallen below the low
alarm limit.
xxx denotes the lowest measured
value, and yyy is the low alarm limit.
Numeric flashes and low limit
is highlighted, yellow alarm
message, alarm tone.
*** Extreme Brady
***Brady xxx < yyy
MECG The maternal heart rate obtained
from the maternal ECG has fallen
below the extreme bradycardia limit.
xxx denotes the lowest measured
value, and yyy is the extreme
bradycardia limit.
Numeric flashes, red alarm
message, alarm tone.
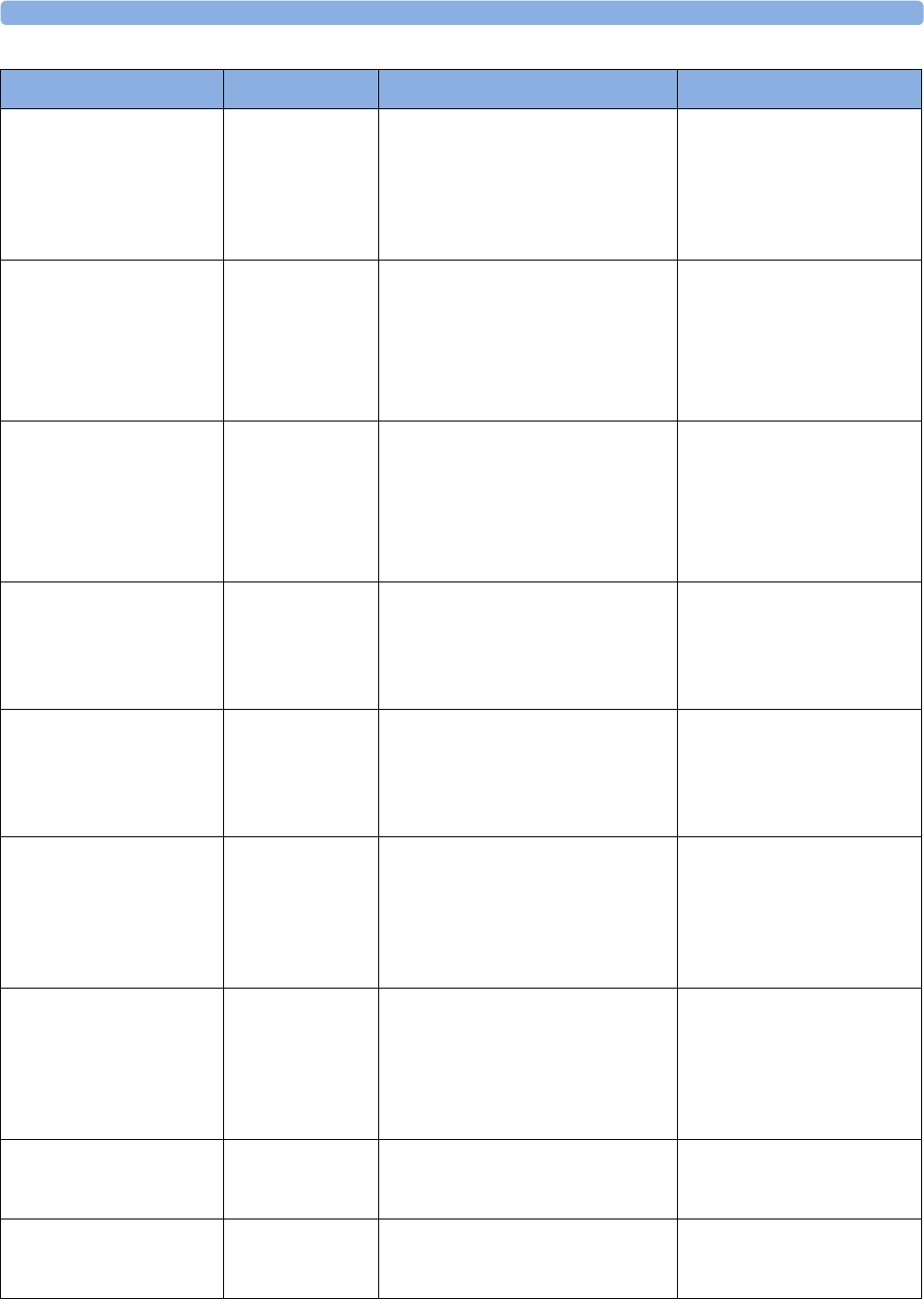
6 Patient Alarms and INOPs
122
*** Extreme Tachy
***Tachy xxx > yyy
MECG The maternal heart rate obtained
from the maternal ECG has risen
above the extreme tachycardia limit.
xxx denotes the highest measured
value, and yy is the extreme
tachycardia limit.
Numeric flashes, red alarm
message, alarm tone.
** FHR1 High
** FHR2 High
** FHR3 High
**FHR1 xxx>yyy
**FHR2 xxx>yyy
**FHR3 xxx>yyy
FHR (ultrasound) The fetal heart rate obtained from
ultrasound has risen above the high
alarm limit.
xxx denotes the highest measured
value, and yyy is the high alarm limit.
Numeric flashes and high
limit is highlighted, yellow
alarm message, alarm tone.
** FHR1 Low
** FHR2 Low
** FHR3 Low
**FHR1 xxx<yyy
**FHR2 xxx<yyy
**FHR3 xxx<yyy
FHR (ultrasound) The fetal heart rate obtained from
ultrasound has fallen below the low
alarm limit.
xxx denotes the lowest measured
value, and yyy is the low alarm limit.
Numeric flashes and low limit
is highlighted, yellow alarm
message, alarm tone.
** HR High
**HR xxx>yyy
MECG The maternal heart rate obtained
from the maternal ECG has risen
above the high alarm limit.
xxx denotes the highest measured
value, and yyy is the high alarm limit.
Numeric flashes and high
limit is highlighted, yellow
alarm message, alarm tone.
** HR Low
**HR xxx<yyy
MECG The maternal heart rate obtained
from the maternal ECG has fallen
below the low alarm limit.
xxx denotes the lowest measured
value, and yyy is the low alarm limit.
Numeric flashes and low limit
is highlighted, yellow alarm
message, alarm tone.
** NBPs High
** NBPd High
** NBPm High
Noninvasive
blood pressure
The measured noninvasive blood
pressure value is above the high
alarm limit.s, d, or m after the label s
indicates whether the systolic,
diastolic or mean pressure has
crossed the limit.
Numeric flashes and high
limit is highlighted, yellow
alarm message, alarm tone.
** NBPs Low
** NBPd Low
** NBPm Low
Noninvasive
blood pressure
The measured noninvasive blood
pressure value is below the low alarm
limit.s, d, or m after the label s
indicates whether the systolic,
diastolic or mean pressure has
crossed the limit.
Numeric flashes and low limit
is highlighted, yellow alarm
message, alarm tone.
** Pulse High SpO2The pulse rate has exceeded the high
alarm limit.
Numeric flashes and high
limit is highlighted, yellow
alarm message, alarm tone.
** Pulse Low SpO2The pulse rate has dropped below
the low alarm limit.
Numeric flashes and low limit
is highlighted, yellow alarm
message, alarm tone.
Alarm Message From Condition Indication
6 Patient Alarms and INOPs
123
** SpO₂ High SpO2The arterial oxygen saturation has
exceeded the high alarm limit.
Numeric flashes and high
limit is highlighted, yellow
alarm message, alarm tone.
** SpO₂ Low SpO2The arterial oxygen saturation has
fallen below the low alarm limit.
Numeric flashes and low limit
is highlighted, yellow alarm
message, alarm tone.
*** Tachy (Pulse)
***Tachy/P xxx>yyy
SpO2The heart rate from the Pulse signal
has exceeded the tachycardia limit.
xxx denotes the highest measured
value, and yyy is the tachycardia limit.
Numeric flashes, alarm limit is
highlighted, red alarm
message, alarm tone.
** <iTemp Label> High iTemp The temperature value has exceeded
the high alarm limit.
Numeric flashes and high
limit is high-lighted, yellow
alarm lamp, alarm tone
** <iTemp Label> Low iTemp The temperature value has dropped
below the alarm limit.
Numeric flashes and high
limit is high-lighted, yellow
alarm lamp, alarm tone
Alarm Message From Condition Indication
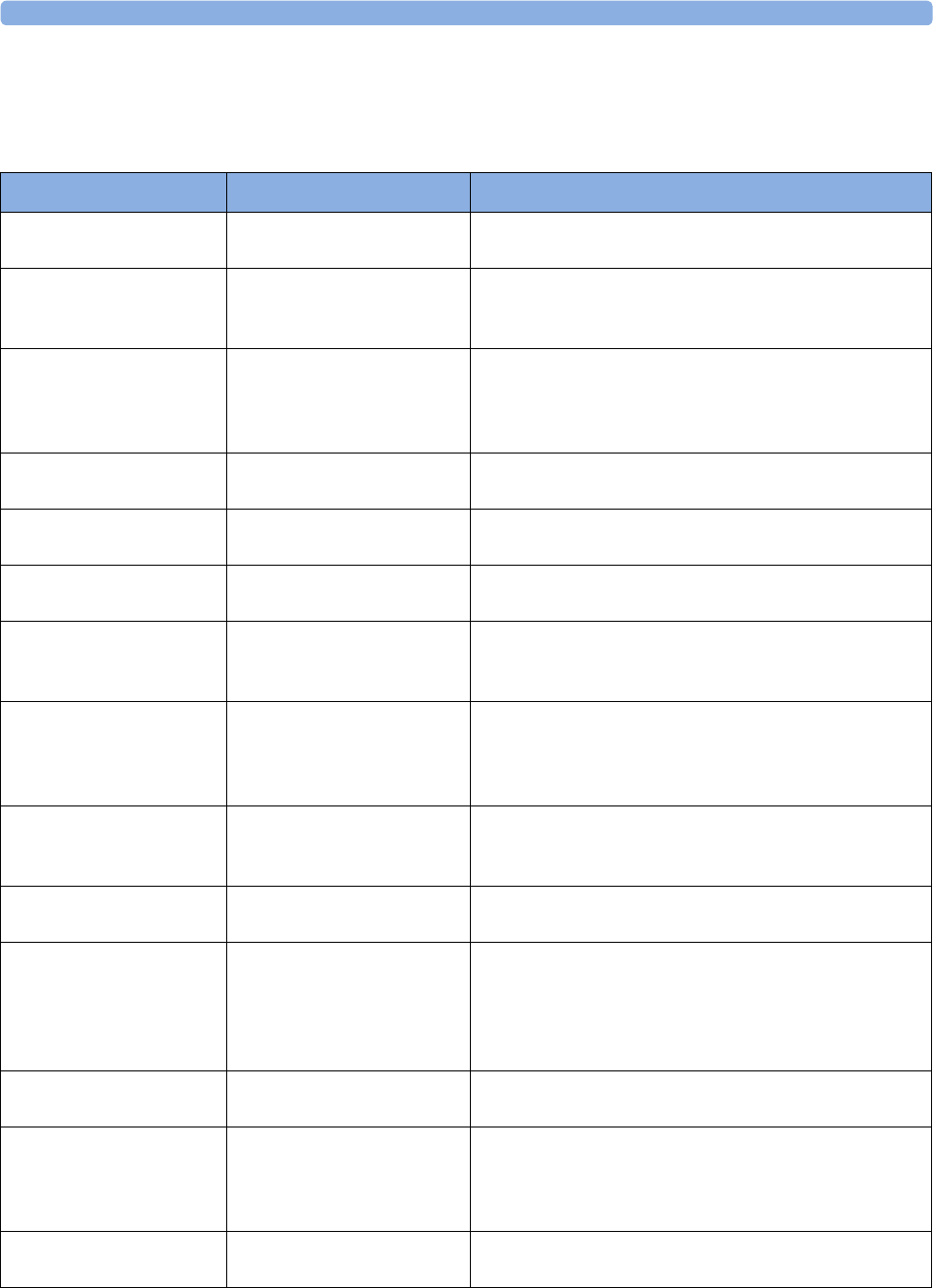
6 Patient Alarms and INOPs
124
Technical Alarm Messages (INOPs)
Monitor INOPs
INOP Message Indication What to do
Bus Master Malfunc Monitor: INOP tone There is a problem with the monitor's hardware. Contact
your service personnel.
Bus Master Incomp Monitor: INOP tone The Bus Master board or firmware is incompatible and
cannot be used with this monitor software revision.
Contact your service personnel.
Check Flex Texts Monitor: INOP tone If this INOP appears, check the monitor and patient
settings before you resume monitoring. If the settings are
unexpected, there may be a problem with the monitor
software. Contact your service personnel.
Check Monitor Func Monitor: INOP tone A potential internal problem with the monitor has been
detected. Contact your service personnel
Check Keyboard Monitor: INOP tone Perform a visual and functional check of the keyboard.
Contact your service personnel.
Check Mouse Monitor: INOP tone Perform a visual and functional check of the mouse input
device. Contact your service personnel.
Check OBR Config Monitor: INOP tone OBR (OB Radio) channel configuration is invalid or
settings are not present. Check channel configuration and
hardware option.
Check Settings Monitor: INOP tone If this INOP appears, check the monitor and patient
settings before you resume monitoring. If the settings are
unexpected, there may be a problem with the monitor
software. Contact your service personnel.
Check TI Config Monitor: INOP tone If this INOP appears, the monitor can be used normally,
except for the Trace Interpretation feature. Contact your
service personnel.
Check Touch Input Monitor: Display only Perform a visual and functional check of the touch input
device. Contact your service personnel.
Coincidence Monitor: INOP tone One or more fetal/maternal heart rates/pulse rates
persistently coincide with each other (see “Cross-Channel
Verification (CCV)” on page 149). The INOP tone has a
configurable delay. The default setting is an instant INOP
tone.
Internal.Comm.Malf Monitor: INOP tone There is a problem with I2C Bus communication in the
monitor. Contact your service personnel.
No Central Monit. Monitor: INOP tone There is a problem with the communication to the
network. Central monitoring is currently not possible (no
patient alarms or information). Check the connection.
Contact your service personnel.
Paper End Monitor: INOP tone The end of the paper pack is detected. Insert a new pack
of paper.
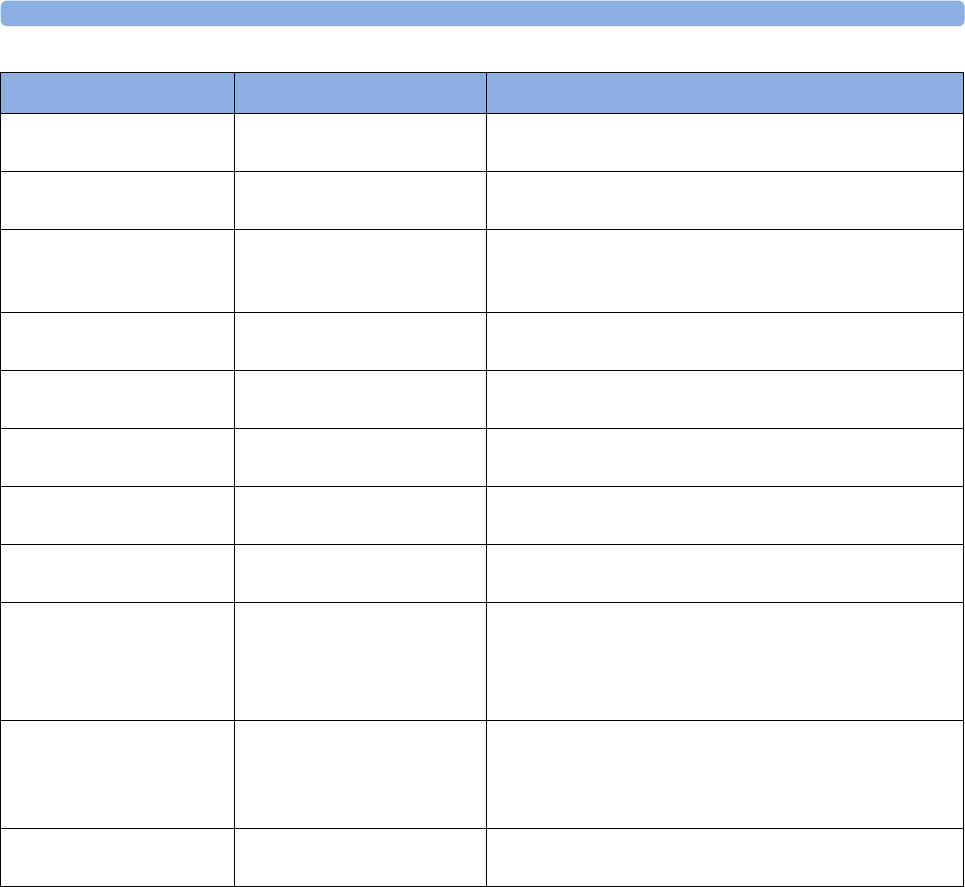
6 Patient Alarms and INOPs
125
Settings Malfunct Monitor: INOP tone The monitor cannot use the predefined settings for
monitoring. Contact your service personnel.
Speaker Malfunct Monitor: INOP tone Contact your service personnel to check the speaker and
the connection to the speaker.
SRR Incompatible Monitor: INOP tone The connected SRR (Short Range Radio) board or FW
cannot be used with this base station SW revision.
Contact your service personnel.
SRR Malfunction Monitor: INOP tone Malfunction in the SRR (Short Range Radio) module(s).
If the INOP persists, contact your service personnel.
SRR Invalid Chan Monitor: INOP tone The channel configuration of the Short Range Radio is
invalid. Check channel and channel mask configuration.
SRR Interference Monitor: INOP tone The short range radio connection has interference from
another device. Try using another channel.
Tele Malfunction Monitor: INOP tone Malfunction of the connected base station. If the INOP
persists contact your service personnel.
Tele Unsupported Monitor: INOP tone The base station is not supported by the monitor. Check
software revisions.
TimeExpired:NST Monitor: INOP tone
(Message and tone only if
Setup NST Timer,
Notification is set to Alarm.
The time has expired for the NST timer. Clearing the
timer clears the INOP.
Unsupported LAN Monitor: INOP tone There is a problem with the communication to the
network and central monitoring is currently not possible.
Check the connection. If the INOP persists, switch off
the monitor and contact your service personnel.
User I/F Malfunct Monitor: INOP tone Perform a visual and functional check of all the monitor
input devices. Contact your service personnel.
INOP Message Indication What to do
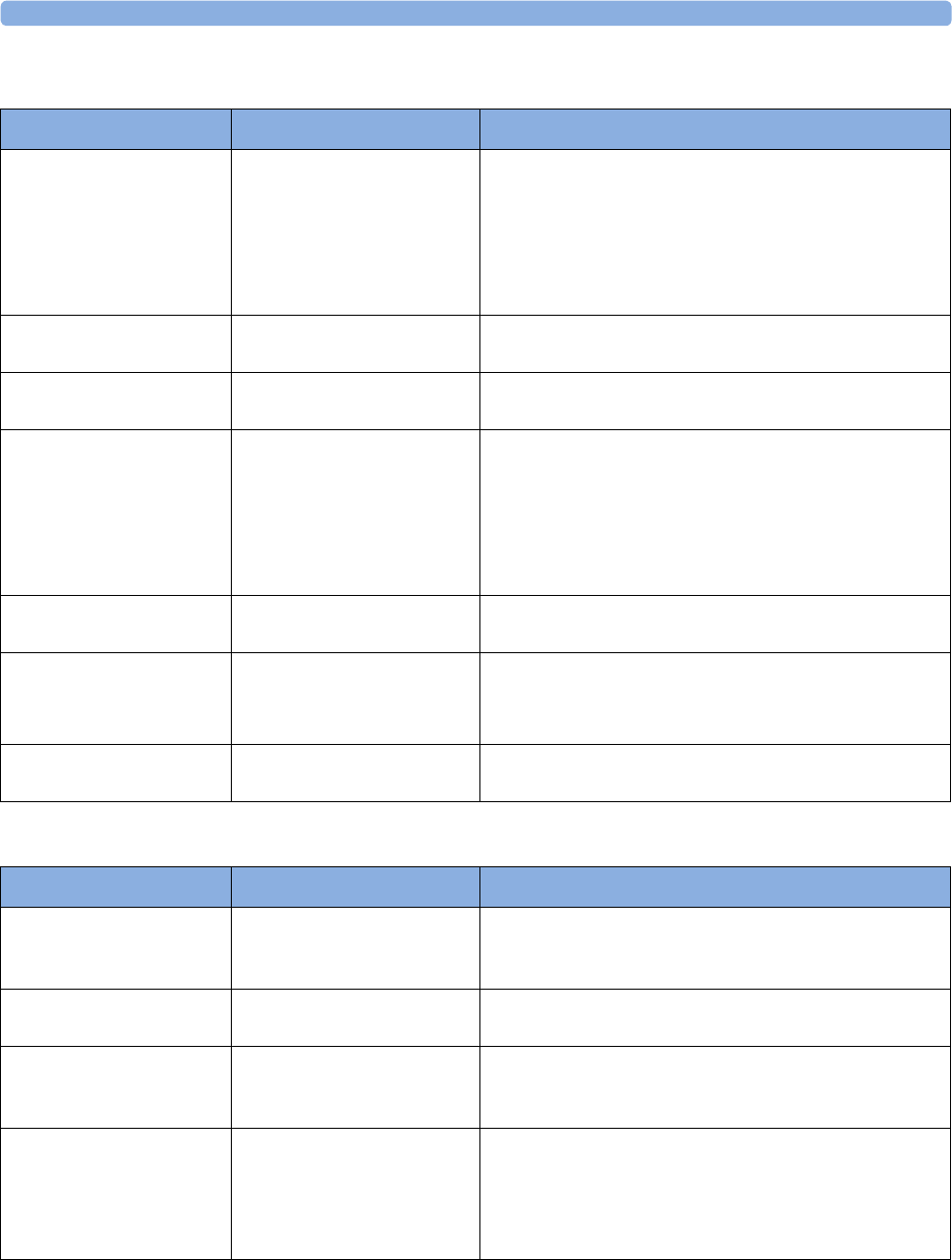
6 Patient Alarms and INOPs
126
FM20/FM30 Battery INOPs
Recorder INOPs
INOP Message Indication What to do
Batt Empty Monitor: INOP tone
Battery: battery LED flashes
during this INOP, alarms
cannot be paused or switched
off
The estimated remaining battery-powered operating time
is less than 10 minutes. Connect the monitor to AC
immediately.
If the condition persists and the monitor is not connected
to mains power, this INOP is re-issued two minutes after
you acknowledge it.
Batt Incompat Monitor: INOP tone The battery cannot be used with this monitor. Replace it
with the correct battery.
Batt Low Monitor: INOP tone The estimated battery-powered operating time remaining
is less than 20 minutes.
Batt Malfunction Monitor: INOP tone
Battery: battery LED flashes
during this INOP, alarms
cannot be paused or switched
off unless the monitor is
connected to mains power.
The monitor cannot determine the battery status. If the
INOP persists, replace the faulty battery. If the condition
persists and the monitor is not connected to mains
power, this INOP is reissued two minutes after you
acknowledge it.
Batt Missing Monitor: INOP tone No battery found in FM20/30. Contact your service
personnel.
Charger Malfunct Monitor: INOP tone
Battery: battery LED may
flash
There is a problem with the battery charger in the
monitor. Connect the monitor to mains power and
contact your service personnel.
Check Batt Temp Monitor: INOP tone The temperature of the battery is too high. Check that the
monitor is not exposed to heat.
INOP Message Indication What to do
Check Paper Monitor: display only
Recorder: Print-out
Check that there is no paper jam, that the print drawer is
properly shut, that the paper is loaded with the grid facing
upwards, and that the correct Philips paper is being used.
FetRec Equip Malf Monitor: INOP tone There is a problem with the fetal recorder hardware.
Contact your service personnel.
FetRec Chk Config Monitor: INOP tone Recorder Speed and/or Scale Type settings are set to
"Unknown" and need to be set to the correct values in
Configuration Mode before the recorder can be operated.
Printhead Overheat Monitor: INOP tone The printhead is too hot. The recorder stops, the
recorder Start/ Stop key is disabled, and remains so until
the printhead cools down sufficiently. Wait for the
printhead to cool down, then press the recorder Start/
Stop key or the Silence key to clear the INOP.
6 Patient Alarms and INOPs
127
Wired Transducer INOPs
FHR (Ultrasound)
IUP
Toco
Wrong Paper Scale Monitor: INOP tone
Recorder: Print-out
The grid scale of the paper in the monitor does not match
the grid scale configured in the monitor. Make sure that
you use the correct paper and scale for your institution:
pre-printed: 30-240 in US and Canada, 50-210 in other
geographies.
INOP Message Indication What to do
INOP Message Indication What to do
FHR1 Equip Malf
FHR2 Equip Malf
FHR3 Equip Malf
Monitor: INOP tone There is a problem with the FHR hardware. Contact your
service personnel.
FHR1 Signal Loss
FHR2 Signal Loss
FHR3 Signal Loss
Monitor: INOP tone
INOP tone if Alarm Mode is
set to ALL. No tone if Alarm
Mode is set to INOP only.
The input signal quality is not sufficient to process the
measurement. Adjust the position of the transducer to
obtain a better signal.
FHR1 Unplugged
FHR2 Unplugged
FHR3 Unplugged
Monitor: INOP tone Reconnect the FHR transducer to the monitor. Check all
connections are sound.
INOP Message Indication What to do
IUP Equip Malf Monitor: INOP tone There is a problem with the IUP hardware. Contact your
service personnel.
IUP Unplugged Monitor: INOP tone Reconnect the IUP transducer to the monitor. Check all
connections are sound.
INOP Message Indication What to do
Toco Equip Malf Monitor: INOP tone There is a problem with the Toco hardware. Contact your
service personnel.
Toco Unplugged Monitor: INOP tone Reconnect the Toco transducer to the monitor. Check all
connections are sound.
Pulse(Toco) Malf Monitor: INOP tone
Toco MP Maternal Pulse
Measurement
There is a problem with the Toco MP transducer
hardware. Contact your service personnel.
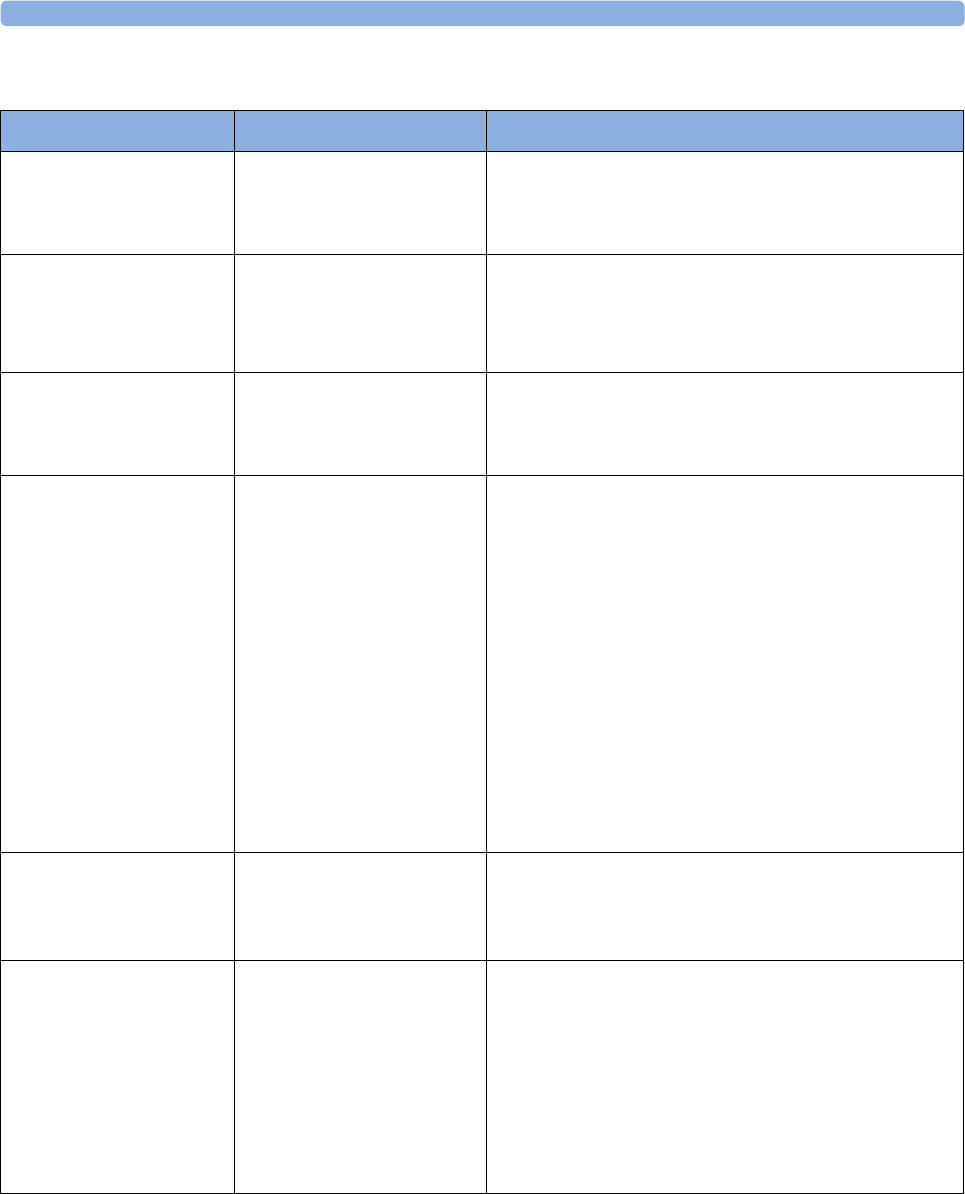
6 Patient Alarms and INOPs
128
Cableless Transducer INOPs
INOP Message Indication What to do
cl US Disconnect
cl Toco Disconnect
cl ECG/IUP Disconn
Monitor: INOP tone
CL transducer: tone and cyan
LED
The cableless transducer has lost the connection to the
monitor for more than 5 sec.
cl US Malfunction
cl Toco Malf
cl ECG/IUP Malf
Monitor: INOP tone
Numeric is replaced by a -?-
CL transducer: tone and cyan
LED
Malfunction of the transducer
cl US Batt Low
cl Toco Batt Low
cl ECG/IUP BattLow
Monitor: Display only
CL transducer: LED flashes
red
The remaining monitoring time with this transducer is
below 30 minutes. Charge battery.
cl US Batt Empty
!!cl US Batt Empty
!!!cl US BattEmpty
cl Toco Batt Empty
!!clToco BattEmpty
!!!clTocoBattEmpty
cl ECG/IUP Empty
!!cl ECG/IUP Empty
!!!clECG/IUP Empty
Monitor: Display only
CL transducer: LED flashes
red
The remaining monitoring time with this transducer is
below 15 minutes. Charge battery.
cl US Batt Malf
cl Toco Batt Malf
clECG/IUP BattMalf
Monitor: INOP tone
CL transducer: tone and cyan
LED
Malfunction of the battery system (charger circuit or
battery) detected (e.g. persistent communication error,
over-voltage, over-current, battery incompatible). Contact
your service personnel.
cl US Check Temp
cl Toco Chk Temp
clECG/IUP Chk Temp
Monitor: INOP tone
CL transducer: tone and cyan
LED
The temperature of the transducer or its battery is
critically high. If the transducer is docked on the base
station, charging is interrupted. Check that device is not
covered and do not expose device to heat sources. Do
not place the base station in a sunny window in a room
without active air conditioning. The environment
temperature to charge a transducer battery should not
exceed 40 °C. If the INOP persists, remove device from
patient and contact your service personnel.
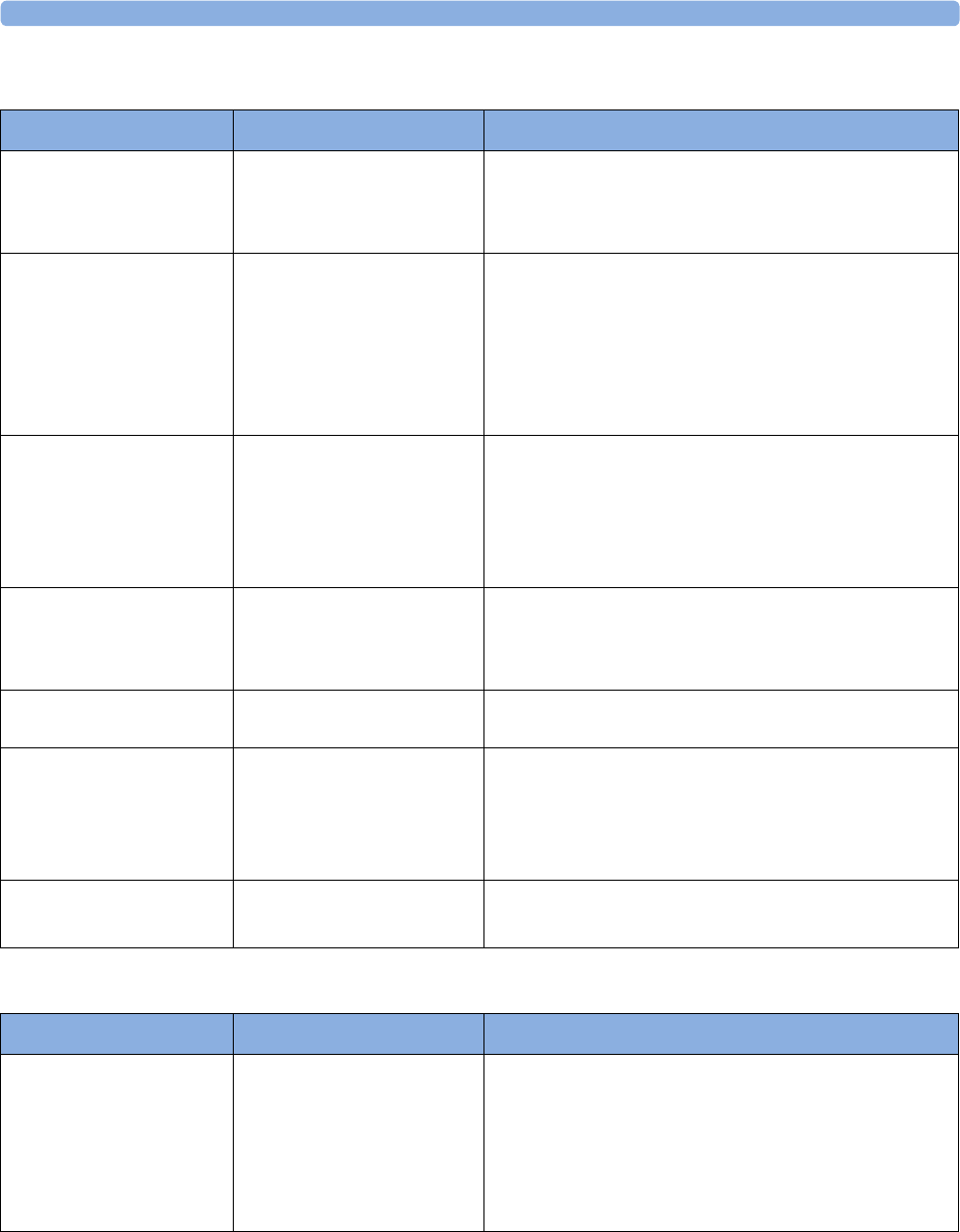
6 Patient Alarms and INOPs
129
DECG and MECG INOPs
NBP INOPs
INOP Message Indication What to do
DFHR1 Equip Malf
DFHR2 Equip Malf
DFHR3 Equip Malf
Monitor: INOP tone There is a problem with the DECG hardware. Contact
your service personnel.
DFHR1 Leads Off
DFHR2 Leads Off
DFHR3 Leads Off
Monitor: INOP tone
Numeric is replaced by a -?-
One or more DECG lead is not attached. Make sure that
all required leads are attached, and no electrodes have
been displaced. Check all connections are sound, and that
the legplate attachment electrode is properly attached. If
the INOP persists, try using another adapter cable, or
legplate attachment electrode. If the INOP persists,
contact your service personnel.
DFHR1 Signal Loss
DFHR2 Signal Loss
DFHR3 Signal Loss
Monitor: INOP tone
Numeric is replaced by a -?-
INOP tone if Alarm us set to
ALL. no tone if Alarm Mode
is set to INOP only.
The input signal quality is not sufficient to process the
measurement. Reapply the fetal scalp electrode.
DFHR1 Unplugged
DFHR2 Unplugged
DFHR3 Unplugged
Monitor: INOP tone
Numeric is replaced by a -?-
Reconnect the DECG transducer to the monitor. Check
all connections are sound.
MECG Equip Malf Monitor: INOP tone There is a problem with the MECG hardware. Contact
your service personnel.
MECG Leads Off Monitor: INOP tone
Numeric is replaced by a -?-
One or more MECG lead is not attached. Ensure that all
required leads are attached, and no electrodes have been
displaced. Check all connections are sound. If the INOP
persists, try using another adapter cable. If the INOP still
persists, contact your service personnel.
MECG Unplugged Monitor: INOP tone
Numeric is replaced by a -?-
Reconnect the MECG transducer to the monitor. Check
all connections are sound.
INOP Message Indication What to do
Cuff Not Deflated Monitor: INOP tone (severe
yellow/red INOP tone)
Numeric is replaced by a -?-
During this INOP, alarms
cannot be paused or switched
off.
Remove the cuff from the patient. Make sure that the
tubing is not kinked or twisted. Try restarting the
measurement. You can silence the INOP, but the INOP
message remains visible until the next measurement is
started or the Stop All SmartKey is selected.
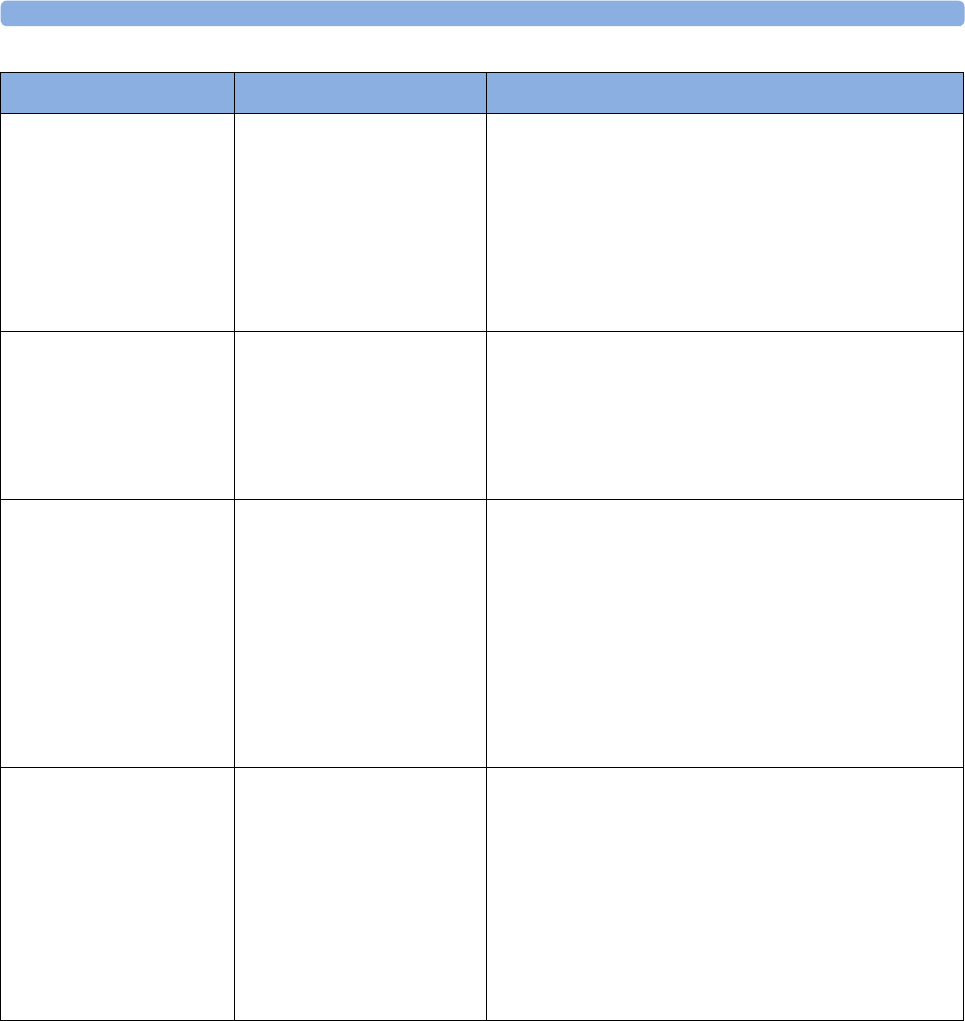
6 Patient Alarms and INOPs
130
NBP Cuff Overpress Monitor: INOP tone (severe
yellow/red INOP tone)
Numeric is replaced by a -?-
During this INOP, alarms
cannot be paused or switched
off.
The cuff pressure exceeds the overpressure safety limits.
Remove the cuff from the patient. Ensure that the tubing
is not kinked or twisted and that the correct patient
category is selected.
Try restarting the measurement. You can silence this
INOP, but the INOP message remains visible until the
next measurement is started or the Stop All SmartKey is
selected.
NBP Equip Malf Monitor: INOP tone
Numeric is replaced by a -?-
Remove the cuff from the patient. The noninvasive blood
pressure hardware is faulty. Contact your service
personnel.
You can silence this INOP, but the INOP message
remains visible until the next measurement is started or
the Stop All SmartKey is selected.
NBP Interrupted Monitor: INOP tone
Numeric is replaced by a -?-
Check the tubing and cuff for leakages or kinks. Check
that you are using the correct cuff size and placement,
and that the correct patient category is selected. Try
restarting the measurement. If the INOP occurs
repeatedly, contact your service personnel.
You can silence this INOP, but the INOP message
remains visible until the next measurement is started or
the Stop All SmartKey is selected. This INOP arises
when the measurement needed longer than the maximum
time for inflation, deflation or the total measurement.
NBP Measure Failed Monitor: INOP tone
Numeric is replaced by a -?-
Check that you are using the correct cuff size and
placement, and that the correct patient category is
selected. Try restarting the measurement.
You can silence this INOP, but the INOP message
remains visible until the next measurement is started or
the Stop All SmartKey is selected.
Check the condition and suitability of the patient for
noninvasive blood pressure monitoring. Use another cuff
to continue measuring.
INOP Message Indication What to do
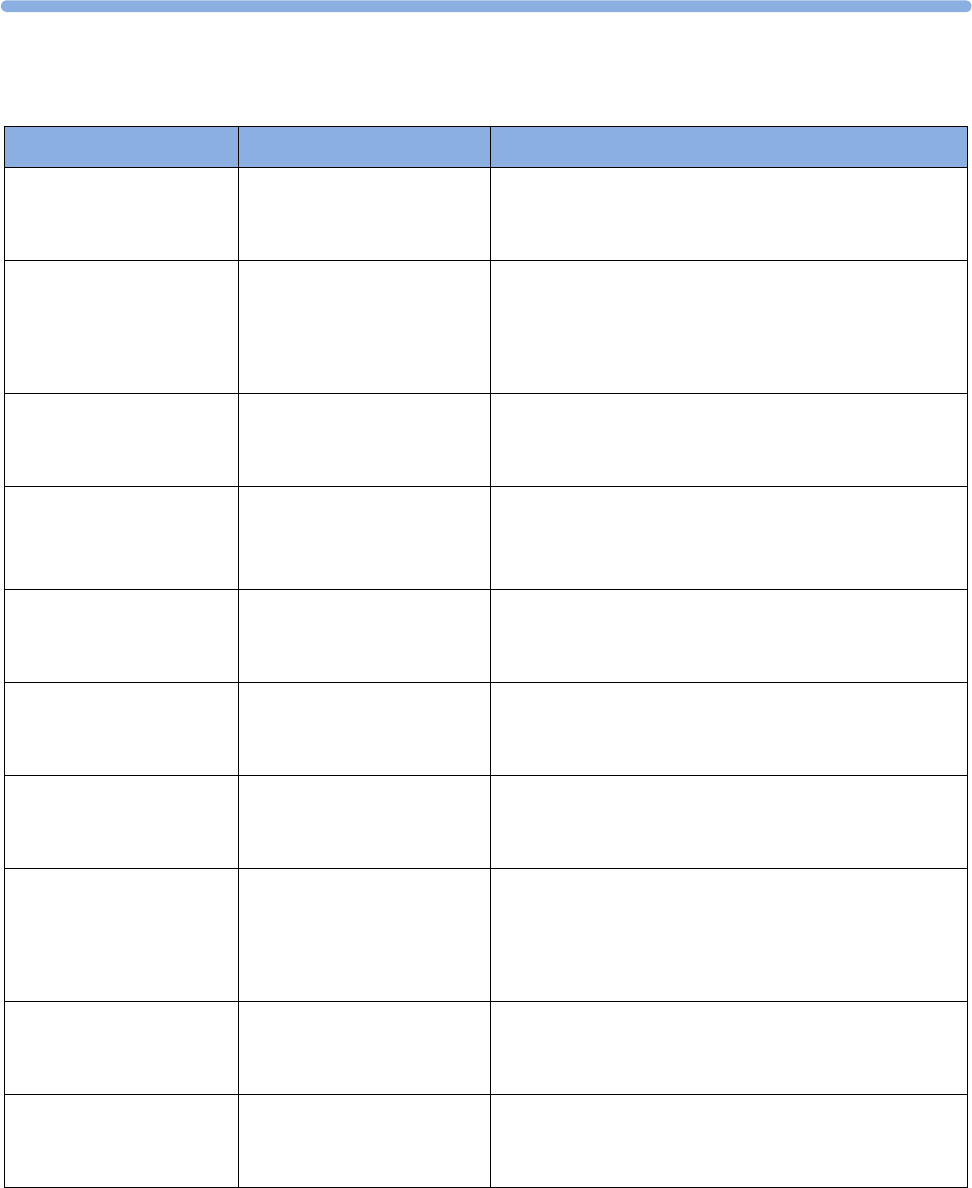
6
131
CL NBP Pod INOPs
INOP Message Indication What to do
cl NBP Disconnect Monitor: INOP tone
CL NBP Pod: INOP tone
and display message
The CL NBP Pod has lost the SRR connection to the
monitor.
cl NBP No Cradle Monitor: INOP tone
CL NBP Pod: display
message
The CL NBP Pod is not in the cradle. You can silence this
INOP, but the INOP message remains visible until the
CL NBP Pod is inserted into the cradle and the next
measurement is started or the Stop All SmartKey is
selected.
cl NBP Remove Monitor: INOP tone
CL NBP Pod: display
message
The temperature of the battery in the CL NBP Pod is too
high. Remove the Cableless Measurement Device from
the patient and contact service personnel.
cl NBP Batt Empty
!!cl NBP BattEmpty
!!!cl NBP BatEmpty
Monitor: INOP tone
CL NBP Pod: display
message
The remaining battery time of the CL NBP Pod is below
30 minutes. Charge the battery.
cl NBP Batt Incomp Monitor: INOP tone
CL NBP Pod: display
message
The battery in use with the CL NBP Pod is incompatible.
Replace it with one approved for use with the CL NBP
Pod.
cl NBP Batt Low Monitor: INOP tone
CL NBP POD: display
message
The remaining battery time of the CL NBP Pod is below
2 hours.
cl NBP Batt Malf Monitor: INOP tone
CL NBP Pod: display
message
There is a malfunction in the CL NBP Pod's battery
system. Contact your service personnel.
cl NBP Batt Temp Monitor: INOP tone
CL NBP Pod: display
message
The temperature of the battery in the CL NBP Pod is
critically high. Check that the Pod is not covered or
exposed to a heat source. If the INOP persists, remove
the Pod from the patient and contact your service
personnel.
cl NBP Check Batt Monitor: INOP tone
CL NBP Pod: display
message
The battery in the CL NBP Pod is nearing the end of its
useful life. Only 50 charge/discharge cycles remain.
Contact your service personnel to replace the battery.
cl NBP Serv Batt Monitor: INOP tone
CL NBP Pod: display
message
The battery in the CL NBP Pod has reached the end of its
useful life. It can no longer be charged. Contact your
service personnel to replace the battery.
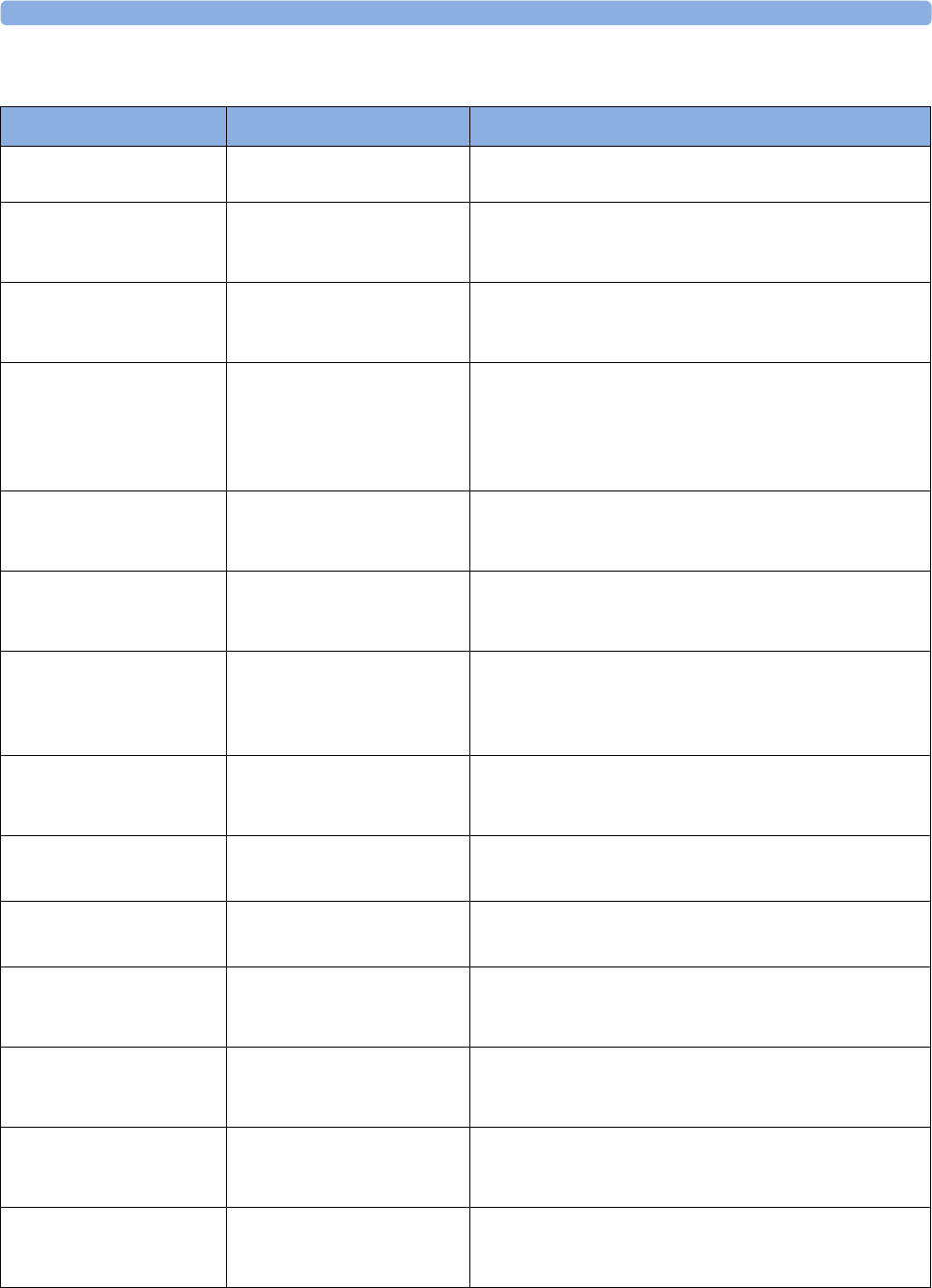
6 Patient Alarms and INOPs
132
SpO2 INOPs
INOP Message Indication What to do
SpO₂ Equip Malf Monitor: INOP tone There is a problem with the SpO2 hardware. Contact your
service personnel.
SpO₂ Erratic Monitor: INOP tone
Numeric is replaced by a -?-
Check the sensor placement. Try another adapter cable
and sensor. If the INOP persists, contact your service
personnel.
SpO₂ Extd.Update Monitor: display only
Numeric is replaced by a -?-
The update period of displayed values is extended due to
a noninvasive blood pressure measurement on the same
limb or an excessively noisy signal.
SpO₂Interference Monitor: INOP tone
Numeric is replaced by a -?-
There is too much interference, caused by a high level of
ambient light and/or electrical interference. Cover the
sensor to minimize ambient light. If the INOP persists,
ensure that the sensor cable is not damaged or positioned
too close to power cables.
SpO₂ Low Perf Monitor: display only
Numeric is replaced by a -?-
Accuracy may be compromised due to very low
perfusion. Stimulate circulation at sensor site. If INOP
persists, change the measurement site.
SpO₂ NoisySignal Monitor: INOP tone
Numeric is replaced by a -?-
Excessive patient movement or electrical interference is
causing irregular pulse patterns. Try to reduce patient
movement or to relieve the cable strain on the sensor.
SpO₂ No Pulse Monitor: INOP tone
Numeric is replaced by a -?-
Check the perfusion at measurement site. If necessary,
stimulate circulation or change measurement site. If the
INOP is due to noninvasive blood pressure measurement
on the same limb, wait until the measurement is finished.
SpO₂ No Sensor Monitor: INOP tone
Numeric is replaced by a -?-
Ensure the SpO2 sensor is connected. If the INOP
persists, try another adapter cable and sensor. If you
silence this INOP, the measurement will be switched off.
SpO₂ Poor Signal Monitor: display only
Numeric is replaced by a -?-
The signal condition of the SpO2 measurement is poor
and measurement accuracy may be compromised.
SpO₂ Pulse? Monitor: INOP tone
Numeric is replaced by a -?-
The detectable pulsations of the SpO2 signal are outside
the specified pulse rate range.
SpO₂ Searching Monitor: display only
Numeric unavailable
SpO2 is analyzing the patient signal to derive Pulse, and
SpO2 values. Please wait until the search analysis is
complete.
SpO₂ Sensor Malf Monitor: INOP tone
Numeric unavailable
The SpO2 sensor or adapter cable is faulty. Try another
adapter cable and sensor. If the INOP persists, contact
your service personnel.
SpO₂ Sensor Off Monitor: INOP tone
Numeric unavailable
The SpO2 sensor is not properly applied to the patient.
Apply the sensor following the instructions supplied by
the manufacturer.
SpO₂ Unkn.Sensor Monitor: display only
Numeric is replaced by a -?-
The connected sensor or adapter cable is not supported
by the SpO2 measurement. Use only specified sensors
and cables.
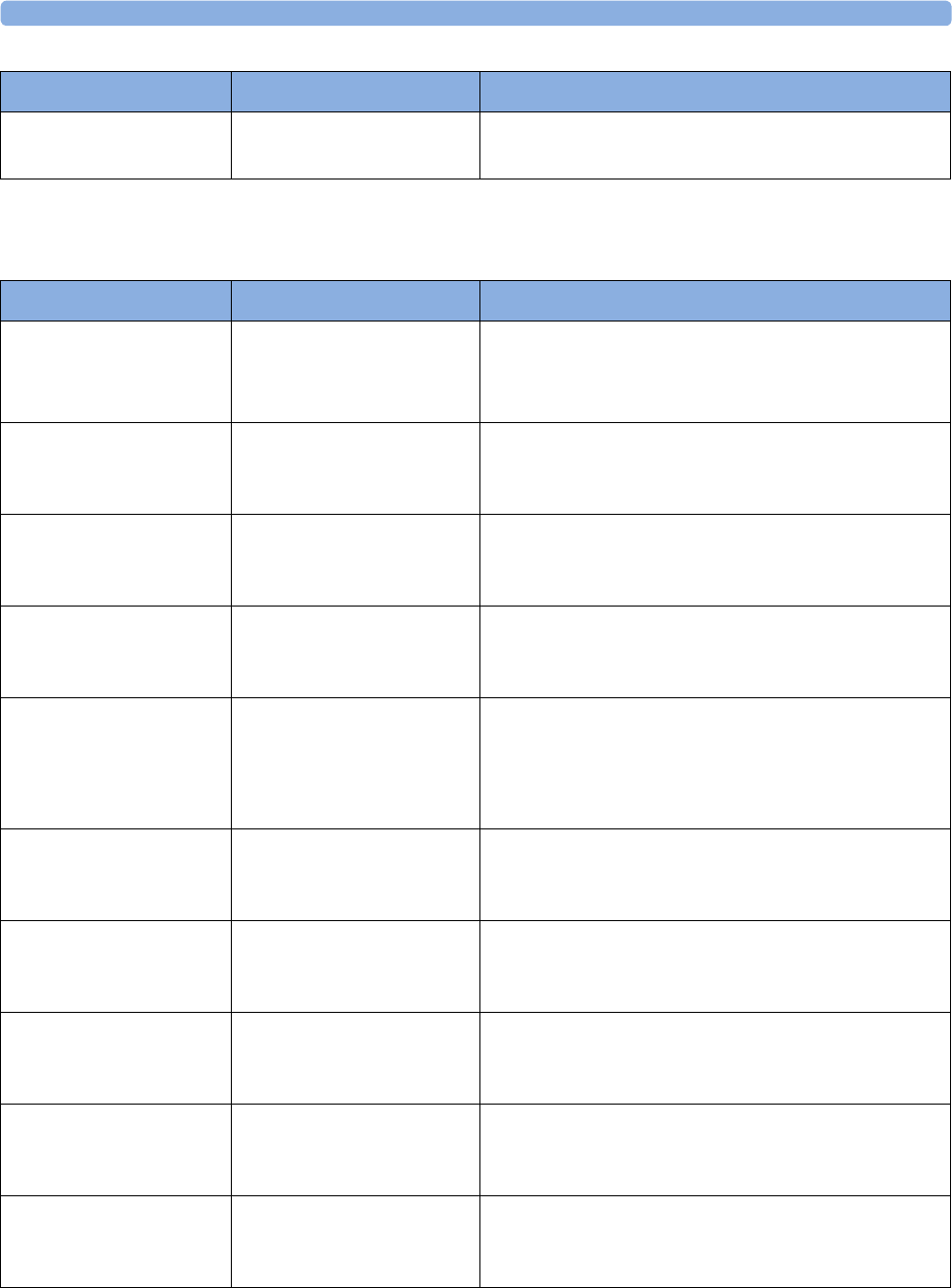
6 Patient Alarms and INOPs
133
CL SpO2 Pod INOPs
SpO₂ Upgrade Monitor: display only
Numeric unavailable
The SpO2 measurement is currently in UPGRADE
mode. Monitoring is not possible in this mode.
INOP Message Indication What to do
INOP Message Indication What to do
cl SpO₂ Batt Empty
!!cl SpO₂ BatEmpty
!!!cl SpO₂ BtEmpty
Monitor: INOP tone
CL SpO2 Pod: display
message
The remaining battery time of the CL SpO2 Pod is below
30 minutes. Charge the battery.
cl SpO₂ Batt Incmp Monitor: INOP tone
CL SpO2 Pod: display
message
The battery in use with the CL SpO2 Pod is incompatible.
Replace it with one approved for use with the CL SpO2
Pod.
cl SpO₂ Batt Low Monitor: INOP tone
CL SpO2 Pod: display
message
The remaining battery time of the CL SpO2 Pod is below
2 hours.
cl SpO₂ Batt Malf Monitor: INOP tone
CL SpO2 Pod: display
message
There is a malfunction in the CL SpO2 Pod's battery
system. Contact your service personnel.
cl SpO₂ Batt Temp Monitor: INOP tone
CL SpO2 Pod: display
message
The temperature of the battery in the CL SpO2 Pod is
critically high. Check that the Pod is not covered or
exposed to a heat source. If the INOP persists, remove
the Pod from the patient and contact your service
personnel.
cl SpO₂ Check Batt Monitor: INOP tone
CL SpO2 Pod: display
message
The battery in the CL SpO2 Pod is nearing the end of its
useful life. Only 50 charge/discharge cycles remain.
Contact your service personnel to replace the battery.
cl SpO₂ Serv Batt Monitor: INOP tone
CL SpO2 Pod: display
message
The battery in the CL SpO2 Pod has reached the end of
its useful life. It can no longer be charged. Contact your
service personnel to replace the battery.
cl SpO₂ Disconnect Monitor: INOP tone
CL SpO2 Pod: INOP tone
and display message
The CL SpO2 Pod has lost the SRR connection to the
monitor.
cl SpO₂ No Cradle Monitor: INOP tone
CL SpO2 Pod: display
message
The CL SpO2 Pod is not in its cradle.
cl SpO₂ Remove Monitor: INOP tone
CL SpO2 Pod: display
message
The temperature of the battery in the SpO2 Pod is too
high. Remove the SpO2 Pod from the patient and contact
service personnel.
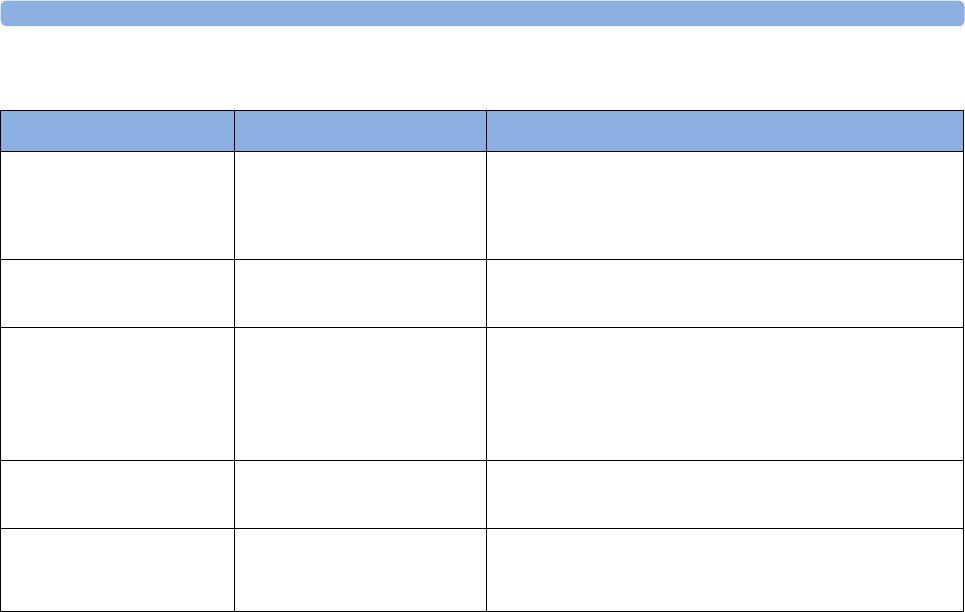
6 Patient Alarms and INOPs
134
Tympanic Temperature INOPs
INOP Message Indication What to do
<iTemp Label>
Malfunction
Monitor: INOP tone
Numeric is replaced by a -?-
The thermometer or the interface board are defective.
Check module on another monitor. Connect another
module to this monitor and replace the interface board. If
the problem persists, contact your service personnel.
<iTemp Label>
Incompat.
Monitor: INOP tone
Numeric is replaced by a -?-
The iTemp device firmware is not supported by the
monitor software.
<iTemp Label> Meas
Failed
Monitor: INOP tone
Numeric is replaced by a -?-
Ambient temperature is out of range. If ambient
temperature is within valid range, check the thermometer.
Try to end the stand-by mode by picking up a new probe
cover. If the problem persists, replace thermometer and
contact your service personnel.
<iTemp Lbl> NO DEVICE Monitor: INOP tone
Numeric unavailable
The thermometer is not connected to the monitor.
<iTemp Label>
Overrange
Monitor: INOP tone
Numeric is replaced by a -?-
Temperature measurement is out of range. If temperature
of measurement is within valid range, check with another
thermometer.

7
135
7Admitting and Discharging
The fetal monitor can store basic patient demographic information used to identify patients.
Admit/Discharge on the Monitor
This section describes how you admit and discharge patients when using the monitor as a stand-alone
device (that is, when not used with an obstetrical information and surveillance system such as OB
TraceVue/IntelliSpace Perinatal).
Admitting a Patient
The fetal monitor displays physiological data as soon as a patient is connected. This lets you monitor a
patient who is not yet admitted. It is however important to admit patients properly so that you can
identify your patient on recordings.
Use the Patient Demographics window and its associated pop-up keys to admit and discharge
patients.
To admit a patient,
1Select the patient name field or select the Patient Demogr. SmartKey to open the Patient
Demographics window.
2Clear any previous patient data by selecting Dischrge Patient and then Confirm.
If you do not discharge the previous patient, you will not be able to distinguish data from the
previous and current patients, for example, on the recording.
3Select Admit Patient.
4Enter the patient information: select each field and use the on-screen keyboard.
If a conventional keyboard is connected to the monitor you can use this to enter patient
information:
–Last Name: Enter the patient's last name (family name), for example Doe.
–First Name: Enter the patient's first name, for example Jane.
–MRN: Enter the patient's medical record number (MRN), for example 12345678. Depending
on your configuration this field may be labeled differently e.g. "Record ID", "Lifetime Id",
"Account Number", "Serial Number", or "SSN".
–Gestational Age: Enter the gestational age of the pregnancy. Enter one numeric for the week
(0-50) and one numeric for the day (0-6).
–Date of Birth: Enter the patient's date of birth.
7 Admitting and Discharging
136
5Select Confirm. The patient status changes to admitted. If the recorder is running, the recorder
stops and immediately restarts to annotate the new patient data.
Quick Admitting a Patient
Use Quick Admit to quickly admit a patient using only a limited set of demographic data.
1Select the Quick Admit SmartKey.
2Enter the required data (ID fields or last name depending on configuration) with the keyboard or a
barcode scanner.
3Select Enter.
4In the confirmation window, select Confirm to stop monitoring for the previous patient or free up
the fetal monitor (if confirmation is configured).
5If the monitor is connected to an Information Center and only the ID field is entered, the patient
name may be set to - - - at the Information Center, depending on the configuration.
Complete the rest of the demographic details as soon as possible to fully identify the patient on the
network, on the monitor, and on printed reports. To complete the details, open the Patient
Demographics window and complete all required fields.
Editing Patient Information
To edit the patient information after a patient has been admitted, select the patient name field on the
main screen of the fetal monitor to open the Patient Demographics window, and enter the required
changes.
Discharging a Patient
You should always perform a discharge even if your previous patient was not admitted. A discharge:
– clears the information in the Patient Demographics window.
– resets all monitor settings to the settings defined in the User Default.
– advances the paper automatically if the recorder is running.
– stops the fetal recorder.
When a patient is discharged from the monitor, all patient demographic data is deleted (trace data is
not affected).
Depending on your configuration, monitoring for a patient may end automatically when the fetal
monitor has been powered off or in standby mode for a set time.
To discharge a patient,
1Select the patient name field to display the Patient Demographics window and associated pop-up
keys.
2Select the pop-up key for Dischrge Patient.
3Select Confirm to discharge the patient.
CAUTION
In order to ensure that the settings are reset to user defaults for a new patient, always discharge the
previous patient from the fetal monitor.

7 Admitting and Discharging
137
NOTE
In order to ensure a continuous record, it is recommended to discharge the patient at the monitor
before performing a new patient admission in OB TraceVue/IntelliSpace Perinatal.
New Patient Check
The fetal monitor can be configured to ask you in certain situations:
• after a specified power-off period
• after a specified standby period
whether a new patient is now being monitored. The pop-up window is entitled Is this a New Patient?
The monitor offers a Yes key to discharge the previous patient and begin monitoring a new patient,
and a No key to continue monitoring with the current patient data and settings.
The time periods for the two conditions can be configured independently.
OB TraceVue/IntelliSpace Perinatal
When the monitor is connected to an OB TraceVue/IntelliSpace Perinatal system over a LAN
connection, the OB TraceVue/IntelliSpace Perinatal system acts as the "master" over patient
demographic data. All patient and location-related data that is visible on the monitor is set, overwritten
or updated by the OB TraceVue/IntelliSpace Perinatal system. See the OB TraceVue/IntelliSpace
Perinatal Instructions for Use for details.
Transferring a Patient
When you are transferring a patient from one bed to another, both the monitor from which you are
transferring her and the monitor to which you are transferring her must be switched on and connected
to the OB TraceVue/IntelliSpace Perinatal network during the patient transfer.
OB TraceVue/IntelliSpace Perinatal via RS232
In contrast to a LAN connection, when the monitor is connected to an OB TraceVue/IntelliSpace
Perinatal system over an RS232 connection, the OB TraceVue/IntelliSpace Perinatal system has no
control over the monitor's patient admission and discharge functions.
Depending on how OB TraceVue/IntelliSpace Perinatal is configured, either the Last Name, First
Name and the bed label, or just the bed label alone, are taken from the OB TraceVue/IntelliSpace
Perinatal system. See the OB TraceVue/IntelliSpace Perinatal Instructions for Use for details.

7 Admitting and Discharging
138
8
139
8Non-Stress Test Timer
The non-stress test (NST) timer shows the elapsed time for the non-stress test. The timer counts up to
the time you set for the NST.
Setting NST Autostart/Autostop
You can set the recorder so that it starts automatically (NST Autostart) when the NST timer is started,
and stops automatically (NST Autostop) when the NST is complete (when the set run time has
elapsed). As default, NST Autostart is On, and NST Autostop is Off.
Viewing the NST Timer
You can configure the timer notification symbol, (the NST label), a progress bar and the elapsed time
to be displayed in the top left-hand corner of the screen. By default, the NST timer is not displayed on
the screen.
Alternatively, you can view the timer in the Timers window.
To open the Timers window:
Either
a. Press the Timer SmartKey.
Or
b. Access the NST pop-up keys (see “Accessing the NST Setup Pop-up Keys” on page 140), and
press the Timers key.
8 Non-Stress Test Timer
140
Timer Expiry Notification
When the timer expires, the color changes from blue to green, you hear a single tone, and a message
appears in the status line on the main screen.
The volume of the tone can be set in Configuration Mode.
Accessing the NST Setup Pop-up Keys
You control and set up the NST timer (for example, start, stop, or clear the timer, and set the run time)
using a selection of pop-up keys that you access via any one of three possible routes:
•Via the Timer SmartKey (Route 1).
•Via the Main Setup SmartKey (Route 2).
• Via the NST menu entry in the menu that pops-up when you touch the top left-hand corner of the
screen (Route 3).
Via the Timer SmartKey (Route 1)
♦Press the Timer SmartKey. The Timers window opens, and the pop-up keys for controlling/
setting up the NST timer appear (see “Pop-up Keys for NST Timer Setup” on page 141).
Via the Main Setup SmartKey (Route 2)
1Enter the Main Setup menu using the SmartKey.
2Select NST to enter the Setup NST menu. At the same time, the pop-up keys for setting up the
NST timer appear (see “Pop-up Keys for NST Timer Setup” on page 141).
Via the NST Field (Route 3)
♦Select the NST field displayed in the top left-hand corner of the screen (when so configured). The
pop-up keys for controlling/setting up the NST timer appear (see “Pop-up Keys for NST Timer
Setup” on page 141).
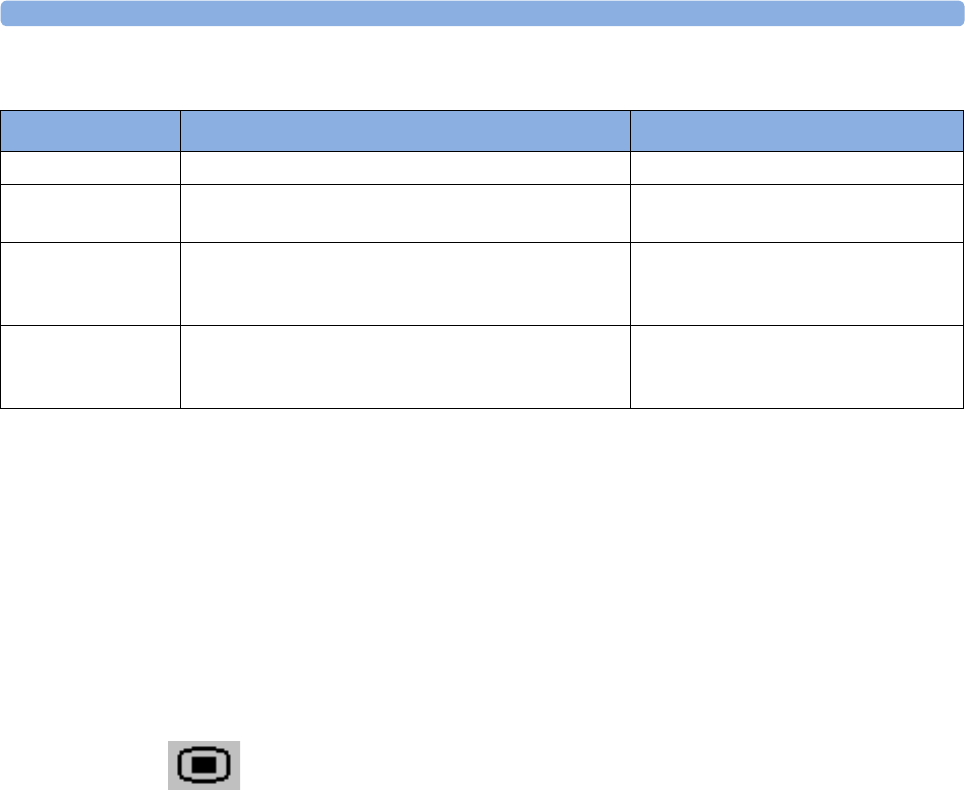
8 Non-Stress Test Timer
141
Pop-up Keys for NST Timer Setup
Run Time
The run time can be set from 10 to 60 minutes. To set the run time, you first need to enter the Setup
NST menu:
1To enter the Setup NST menu:
Either
Enter the Main Setup menu using the SmartKey. Then select NST.
Or
Access the NST pop-up keys (see “Accessing the NST Setup Pop-up Keys” on page 140), and
press the Setup NST key.
2Select Run Time.
Pop-Up Keys Selecting this pop-up key lets you.... Comments
Start Start the timer.
Stop Stop the timer, allowing either restarting after a pause
(Start) or clearing (Clear key).
Setup NST Enter the Setup NST menu. From here you can set the
run time.
This pop-up key is not available with
Route 2, as the Setup NST menu is
already open.
Timer Return to the Timers window. This pop-up key is not available with
Route 1, as the Timers window is
already open.

8 Non-Stress Test Timer
142

9 Non-Stress Test Report
143
9Non-Stress Test Report
It is generally accepted that a non stress test (NST) allows you to assess fetal well-being. The monitor's
NST report process uses fetal ultrasound (but not DECG) heart rate traces and the Maternal Toco
trace, generating a printed report when criteria are met and it is an indication of the fetal well-being.
The American term Non Stress Test (NST) is used for antepartum testing. The interpretation
algorithm and rule set are equivalent to those implemented in OB TraceVue Revision G.xx or
IntelliSpace Perinatal H.xx and higher, and are based on the 2008 NICHD guidelines.
An NST report is a diagnostic aid, but it does not replace the clinician’s judgment. The interpretation
and the appropriate clinical response remain with the clinician.
A fetus normally produces characteristic heart rate patterns. Average baseline variability and
acceleration of the FHR in response to fetal movement are considered reassuring signs. This test does
not take into account any form of external fetal stimulation.
For every active ultrasound fetal heart rate measurement, one NST report can reside in the monitor’s
memory. The reports are cleared when you discharge a patient and when you start a new NST report.
When the NST Report option is available and the "NST Report" feature is "on", the NST status for all
available ultrasound fetal heart rate measurements are displayed on the screen.
The minimum displayed information is:
• NST identification (by FHR number: 1, 2, 3)
• Current NST status (by color: inverse for "not started yet", white for "running", yellow for
"stopped", green for "finished")
Setting Up an NST Report
To setup NST Report functionality:
1Enter the Main Setup menu and select the NST Report or
2Select the NST Report SmartKey.
3Press the "Setup" pop-up key.
4Set your configuration options.
Select from:
•NST Analysis. Choose from On or Off.
This switches the report feature on or off. This is linked to the NST timer. Both must be set to On
for the NST report to function.
•Report Recording. Choose from:
–Manual - press the Record Report pop up key to trigger a manual request.
–After Recorder Stop - report is recorded as soon as recorder becomes idle.
–Immediately - If a realtime recording is running, the monitor pauses it. The recording is
continued after the report has been recorded.
Average short term variability (STV) value is documented in [bpm] and [ms] if STV is configured as
part of the NST Report. This parameter is not considered as reassuring criteria.

9 Non-Stress Test Report
144
NST Report Status Window
The NST Report window displays a detailed overview of the current NST status for any available
ultrasound fetal heart rate measurement. You can see:
• NST Status - whether it is ready, ongoing, or the time and date at which it was stopped, or at which
it finished.
• Elapsed time - the time that has elapsed since the NST began.
• Accelerations - the number of FHR accelerations detected so far.
• Baseline - the average baseline value.
• Variability - the average variability value.
• Short Term Variability - the current short term variability (STV) value.
• Decelerations - the number of FHR decelerations detected so far.
• FHR Availability - current statistical FHR availability value.
• Sinusoidal - the current status of sinusoidal rhythm detection.
For criteria not yet met, a white arrow symbol marks the overall status on the top line, and also appear
against every criterion not yet met. A yellow symbol indicates detection of severe or prolonged
decelerations.
The pop-up keys let you perform the following actions:
•FHR1, FHR2, FHR3 - switch to the window showing the current NST status for the fetal heart rate.
•Record Report - print the NST Report on paper.
•Record Trace - record the trace episode that belongs to the current report. Depending on device
usage, the trace recording might be incomplete.
•Setup - open the Setup NST Report window.
9
145
Example NST Report
Field Field Content
Report Title, with FHR
label and date
NST Report for FHR1 on 12 Oct. 2009
Product Information Product DE53102345 G.01.70, OB A.04.24,
Toco DE52401090, FHR1 DE00002345 A.05.26
Patient Information Rogers, Alice
Age: 27
Gestational Age: Week 34, Day 5
Start time, end time,
Elapsed time, configured
Run time
Time: 11:34 - 12:06
Elapsed time:32 minutes
Run time: 20 minutes
Overall one-line NST
result summary
NST Criteria*: not met
Title Trace Interpretation Summary
Result Accelerations Accelerations: 2
at: 11:59 12:02
Result: Contractions Contractions: 3
at: 11:57 12:00 12:04
Result: Baseline and
Variability
Baseline: 125 bpm (Range: 118 bpm - 129 bpm)
Variability: 23 bpm (Range: 20 bpm - 24 bpm)
Short Term Var.: 0.9 bpm (3.8 msec)
Statistics: FHR
availability
FHR available: 95%
Result: Decelerations Decelerations: 1
at: 11:58
severe
prolonged
9 Non-Stress Test Report
146
NST Criteria
The patient is monitored for a user-definable period of time (10 - 60 minutes in steps of 5 minutes).
The test is considered reassuring when the following criteria are met:
• The fetal heart rate is valid at least 90% (this is configurable) of the specified time span.
• The FHR features a user-defined minimum number of accelerations.
• The FHR features a user-defined maximum number of tolerated decelerations, and does not
include severe or prolonged decelerations, which are never tolerated.
• The average baseline fetal heart rate lies within the user-defined limits for low heart rate and high
heart rate over the whole time span.
• The FHR exhibits a moderate variability (user-defined) for the specified time span.
Result:
Sinusoidal Rhythm
detected
Sinusoidal: No
Result: Decelerations
before Reporting Period
Events before Reporting Period:
Decelerations: 1
at: 11:38
severe
prolonged
This field is enabled if there were decelerations between the
start of NST and the start of the reporting period.
Guideline / Criteria
Information
(*) Interpretation Criteria based on guideline "NICHD 2008,
v01"
User-defined criteria for CTG tracing:
• valid FHR for 90% of reporting period
• baseline heart rate between 120 and 160 bpm
• at least 2 accelerations in 10 min
• not more than 1 decelerations
• moderate baseline variability (5 - 25 bpm)
• short term var. greater than 5.0 msec
Additional Criteria:
• no severe or prolonged decelerations
• no sinusoidal pattern in reporting period
Field Field Content

9 Non-Stress Test Report
147
An NST Report is generated when the reassuring criteria are met the first time in the current
monitoring phase. When performing NST with twins or triplets, a separate NST Report is generated
for each fetus.
In the printed report, the average short term variability (STV) value is shown in bpm and ms. This is
not part of the reassurance criteria.
After the reassurance criteria have been met, the clinician can print the NST Report and then turn the
fetal monitor off, or may continue fetal monitoring and print the report at any time.
Non-Reassuring Report
If the reassurance criteria are not met when the test has run for 90 minutes, or if you stop anytime
during the 90 minute period, then the test is stopped, and a report is generated stating the reassurance
criteria have not been met.
Non-Reactive NST Test
If a non-reactive test occurs and you then use acoustic stimulation, you must exercise caution in
interpreting the resulting traces, as artificial stimulation is not taken into account when calculating test
results.

9 Non-Stress Test Report
148

10 Cross-Channel Verification (CCV)
149
10Cross-Channel Verification
(CCV)
Misidentification of Heart Rates
FHR detection by the monitor may not always indicate that the fetus is alive. Confirm fetal life before
monitoring, and continue to confirm that the fetus is the signal source for the recorded fetal heart rate
(see “Confirm Fetal Life Before Using the Monitor” on page 10).
To reduce the possibility of mistaking the maternal HR or pulse for FHR, or FHR1 for FHR2 or
FHR3, it is recommended that you monitor both maternal HR/pulse and the heart rates of all fetuses
(see “Monitoring FHR and FMP Using Ultrasound” on page 155, “Monitoring Twin FHRs” on
page 171, “Monitoring Triple FHRs” on page 179, and “Monitoring Maternal Heart / Pulse Rate” on
page 223).
Here are some examples where the MHR can be misidentified as the FHR, or one FHR for another
FHR (twins/triplets).
•When using an ultrasound transducer:
– It is possible to pick up maternal signal sources, such as the maternal heart, aorta, or other
large vessels. Especially if the recorded MHR, and any other artifact is over 100 bpm.
– It is possible to pick up the same fetal heart rate simultaneously with multiple transducers
NOTE
When an ultrasound transducer is connected to the monitor, but not applied to the patient, the
measurement may generate unexpected intermittent FHR readings.
•When Fetal Movement Profile (FMP) is enabled:
The FMP annotations on a fetal trace alone may not always indicate that the fetus is alive. For
example, FMP annotations in the absence of fetal life may be a result of:
– Movement of the deceased fetus during or following maternal movement.
– Movement of the deceased fetus during or following manual palpation of fetal position
(especially if the pressure applied is too forceful).
– Movement of the ultrasound transducer.
•When using a scalp electrode (DECG):
– Electrical impulses from the maternal heart can sometimes be transmitted to the fetal monitor
through a recently deceased fetus via the spiral scalp electrode, appearing to be a fetal signal
source.
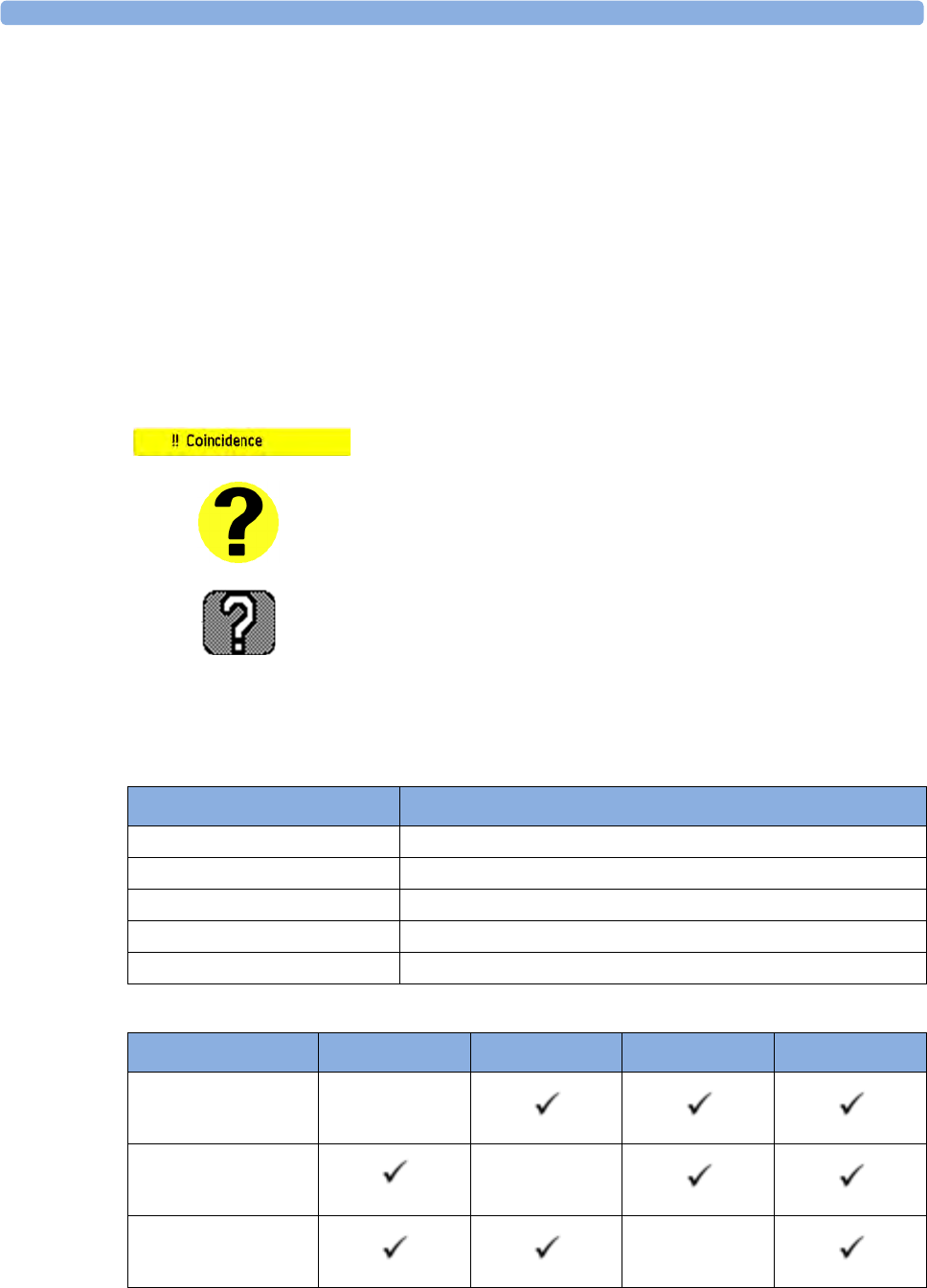
10 Cross-Channel Verification (CCV)
150
Cross-Channel Verification Functionality
The cross-channel verification functionality (CCV) of the fetal monitors compares all monitored heart
rates (maternal and fetal), and indicates automatically whether any two channels are picking up the
same signal, or monitoring similar values.
If the fetal monitor detects that any channels have the same or similar values the Coincidence INOP is
issued with an INOP tone that can have a configurable delay. In addition yellow questions marks
appear next to the numerics on the touch screen that have the same or similar values. On the recording
trace there is also a question mark printed out from the point where recorded traces continuously
overlap.
Visual Aids for CCV Detection
Overview of Cross-Channel Comparisons
Measurements from Transducers
Measurement Comparison Done by the Fetal Monitor for Cross-Channel Verification
Coincidence INOP appears on the touch screen of the fetal monitor.
Question mark next to the numerics that show the same or similar
values appears on the touch screen of the fetal monitor.
Question mark printed out on the recorder trace from the point where
two measured values coincide.
Measurement Transducer
FHR US From Ultrasound or CL Ultrasound transducer
DFHR (DECG) From a fetal scalp electrode
Maternal pulse From Toco MP, or CL Toco+MP transducer
Maternal pulse From SpO2 or CL SpO2 Pod
Maternal heart rate From MECG electrodes
FHR1 (US) FHR2 (US) FHR3 (US) DFHR (DECG)
FHR1 (US)
FHR2 (US)
FHR3 (US)

10
151
DFHR (DECG)
Maternal Pulse
(Toco MP)
Maternal Pulse
(SpO2)
Maternal HR
(MECG)
FHR1 (US) FHR2 (US) FHR3 (US) DFHR (DECG)

10
152
Coincidence Examples
Coincidence of Maternal Pulse and FHR
When the maternal pulse and FHR are being monitored, and the measured values are very similar or
the same, the coincidence question mark is displayed on the monitor’s screen above both of the
corresponding numerics (in this case maternal pulse and FHR). Often the signal loss or coincidence
happens because the fetal or maternal movement displaced the ultrasound transducer, and a
repositioning of the transducer is necessary.
1Coincidence INOP
2Coincidence question mark
by FHR1
3Coincidence question mark
by pulse from Toco MP
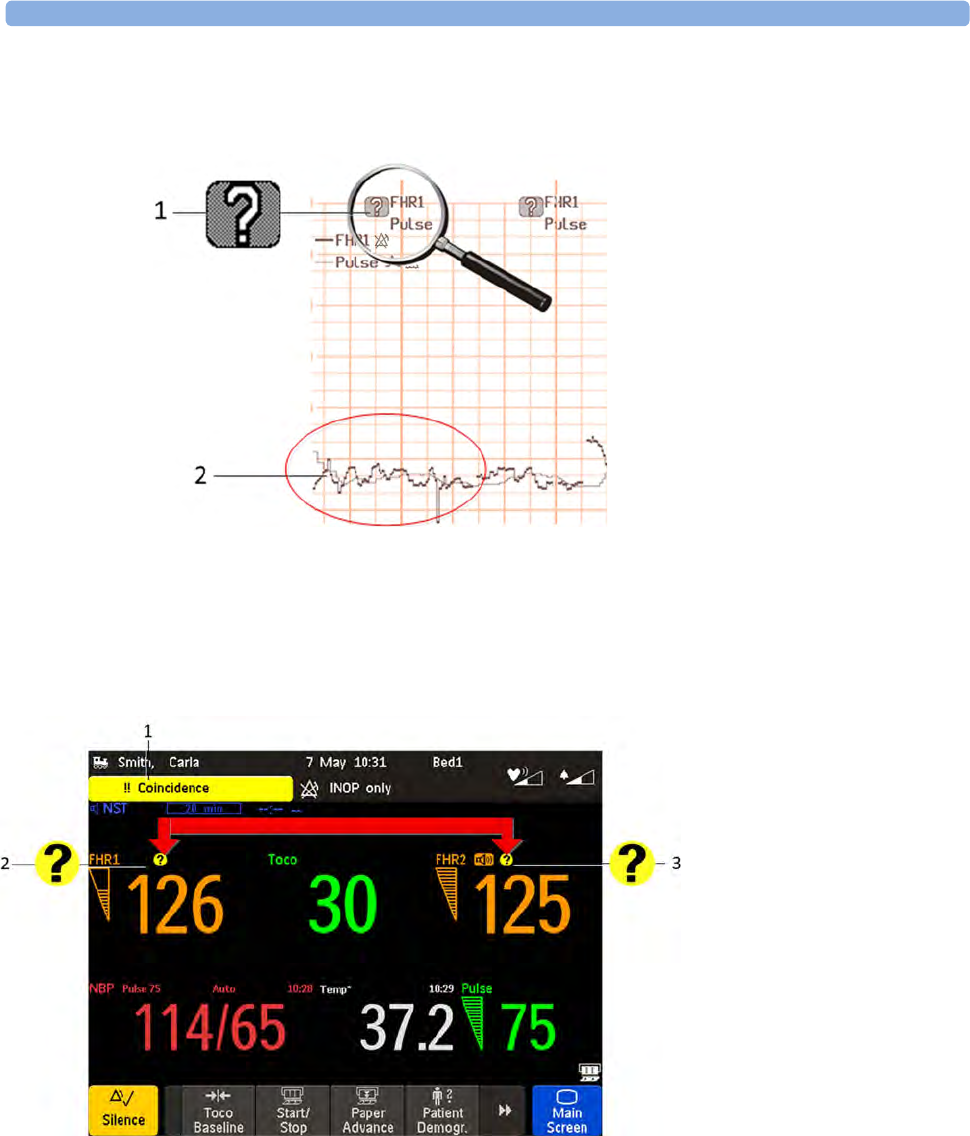
10 Cross-Channel Verification (CCV)
153
The coincidence question mark is also printed on the trace paper next to the corresponding FHR and
maternal pulse.
Coincidence of Twins/Triplets FHRs
When both FHR1 and FHR2 are being monitored, and the measured values are very similar or the
same, the coincidence question mark is displayed on the monitor’s screen above both of the
corresponding numerics (in this case FHR1 and FHR2).
1Printed coincidence question
mark on trace
2FHR1 and pulse traces
1Coincidence INOP
2Coincidence question
mark by FHR1
3Coincidence question
mark by FHR2
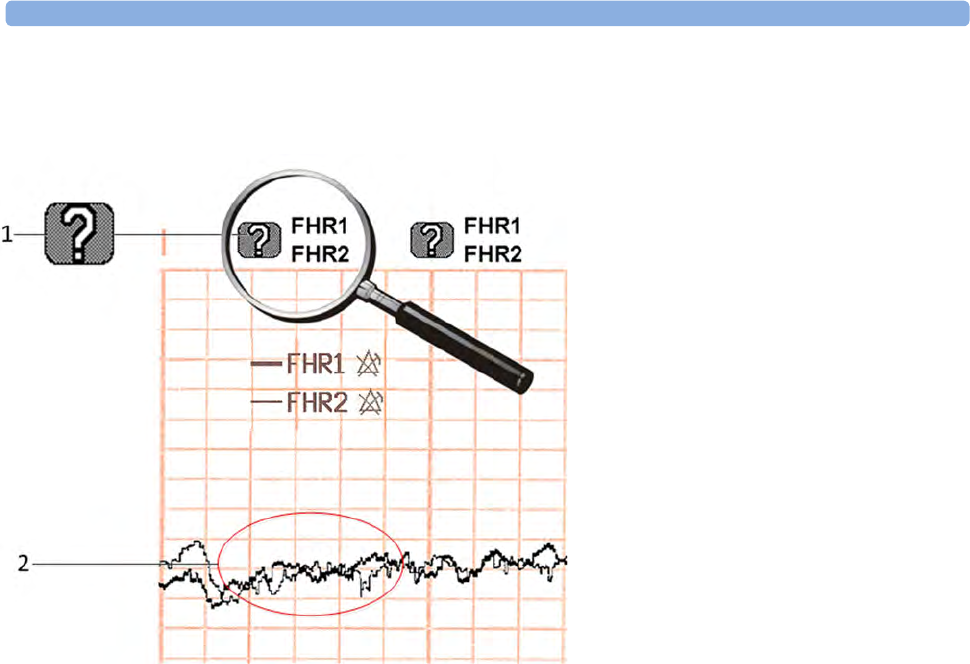
10 Cross-Channel Verification (CCV)
154
The coincidence question mark is also printed on the trace paper next to the corresponding FHR1 and
FHR2.
Recommended Actions for INOP Coincidence
1Confirm fetal life by palpation of fetal movement or auscultation of fetal heart sounds using a
fetoscope, stethoscope, or Pinard stethoscope.
2Manual determination of the maternal pulse and comparison with the fetal heart rate sound signals
from the loudspeaker.
3Reposition the transducer, or ensure that the fetal scalp electrode is placed correctly, until you
receive a clear signal and the monitor is no longer issuing the Coincidence INOP.
4In case of difficulties deriving a stable maternal pulse reading using the Toco MP or CL Toco+MP
transducer, use SpO2 or the CL SpO2 Pod instead. In case of similar problems with the pulse
measurement from SpO2, use MECG instead. Reasons to switch the method for deriving a
maternal pulse or heart rate include: motion artifacts, arrhythmia, and individual differences in
pulse signal quality on the abdominal skin (via Toco MP).
5If you cannot hear the fetal heart sounds, and you cannot confirm fetal movement by palpation,
confirm fetal life using obstetric ultrasonography.
1Printed coincidence question mark on
trace
2FHR1 and FHR2 traces
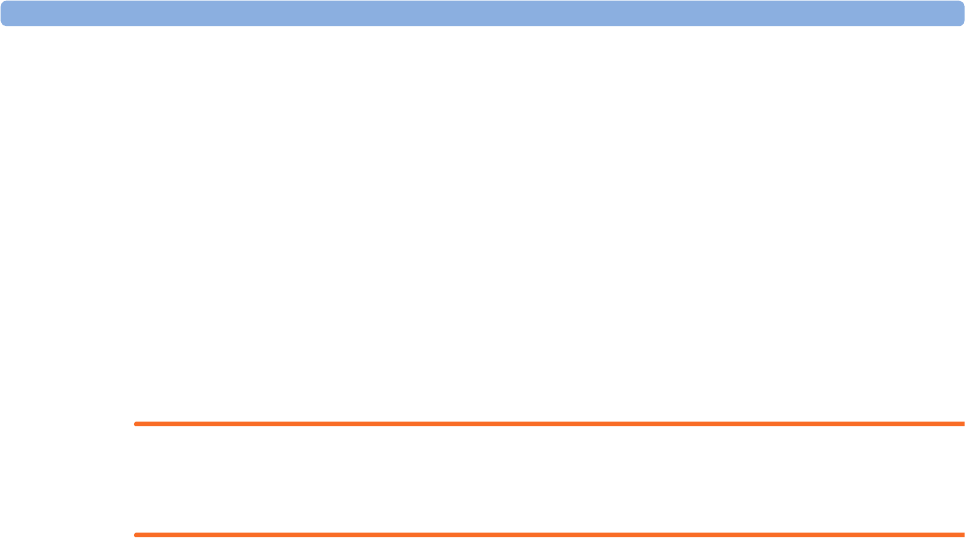
11 Monitoring FHR and FMP Using Ultrasound
155
11Monitoring FHR and FMP
Using Ultrasound
To monitor a single FHR externally, you use an ultrasound transducer attached to a belt around the
mother's abdomen. The ultrasound transducer directs a low-energy ultrasound beam towards the fetal
heart and detects the reflected signal. Your monitor can also detect fetal movements and print the fetal
movement profile (FMP) on the trace. Monitoring using ultrasound is recommended from the
25th week of gestation for non-stress testing or routine fetal monitoring.
WARNING
Performing ultrasound imaging or Doppler flow measurements together with ultrasound fetal
monitoring may cause false FHR readings, and the trace recording may deteriorate.
Technical Description
Fetal monitors use the ultrasound Doppler method for externally monitoring the fetal heart rate. Using
the Doppler method, the transducer (in transmitter mode) sends sound waves into the body which are
then reflected by different tissues. These reflections (Doppler echoes) are picked up by the transducer
(in listening mode). These Doppler echoes are amplified and sent to the monitor’s speaker through
which the fetal heart signal can be heard. In parallel the Doppler echoes are processed through an auto
correlation algorithm to determine the fetal heart rate (FHR). The FHR is displayed on the monitor’s
numeric display and on the recorded trace.
Properly representing the fetal heart rate using a device that derives heartbeats from motion is a
formidable task and the limitations of the technology will be discussed shortly. Basic fetal cardiac
physiology may contribute to difficulties in obtaining a reliable ultrasound signal.
A heart rate pattern of a fetus is capable of extraordinary variation, ranging from a stable pattern with
minimal variation while the fetus is “asleep” to robust accelerations of 40-60 bpm above baseline rate
over a few seconds, or exaggerated variability when the fetus is active. Decelerations of the rate
60-80 bpm below baseline may develop even more abruptly than the accelerations. The Beat-to-Beat
arrhythmias of the FHR may further exaggerate how much the the FHR variability at the bottom of
the variable decelerations, or in the presence of fetal breathing movements, which also tend to lower
the fetal heart rate. The recognition of these normal variations in fetal heart rate patterns will greatly
assist in the separation of genuine fetal information from the artifact.
Limitations of the Technology
All tissues moving towards or away from the transducer generate Doppler echoes. Therefore, the
resulting signal that is provided to the monitor’s speaker, and for further fetal heart signal processing,
can contain components of the beating fetal heart wall or valves, fetal movements, fetal breathing or
hiccup, maternal movements such as breathing or position changes, and pulsating maternal arteries.
The fetal heart signal processing uses an auto correlation algorithm to obtain periodic events such as
heart beats. If the signal is erratic such as from a fetal arrhythmia, the ultrasound device may have

11 Monitoring FHR and FMP Using Ultrasound
156
trouble tracking the abrupt changes, and may misrepresent the true FHR pattern. Signals such as those
from moving fetal limbs are usually very strong, thereby masking the fetal heart signal. During
prolonged movements where the fetal heart signal is masked, the FHR appears blank on the numeric
display and as a gap on the recorded trace. Fetal position changes, maternal position changes, or
uterine contractions can move the fetal heart partly or fully out of the ultrasound beam resulting in
signal loss, or even picking up Doppler echoes from pulsating maternal arteries. In these cases a
maternal heart rate or sometimes even a rate resulting from the mixture of fetal and maternal signals
may be displayed on the monitor’s numeric display and on the recorded trace.
In contrast to the timely well-defined R-peak of an ECG signal obtained with a fetal scalp electrode,
the ultrasound Doppler signal from a fetal heart consists of multiple components from atria (diastole),
ventricles (systole), valves, and pulsating arteries. These components vary depending on fetal and
transducer position and angle, and are further modulated by factors such as fetal or maternal breathing.
These effects may produce what is called “artifact”. Optimal transducer positioning therefore is key to
minimizing these effects and thereby minimizing artifact.
Misidentification of MHR as FHR
FHR detection by the monitor may not always indicate that the fetus is alive. Confirm fetal life before
monitoring, and continue to confirm that the fetus is the signal source for the recorded heart rate (see
“Confirm Fetal Life Before Using the Monitor” on page 10 and “Cross-Channel Verification (CCV)”
on page 149).
What You Need
• Ultrasound transducer
• Toco MP or CL Toco+MP transducer
•Ultrasound gel
• Transducer belt (and optional butterfly belt clip, if applicable)
Cableless Monitoring - Important Considerations
When using an Avalon CL or Avalon CTS Fetal Transducer system with your monitor, note the
following:
Refer to “Telemetry” on page 93 for general rules regarding the use of cableless transducers from an
Avalon CL or Avalon CTS Cableless Fetal Transducer system.
• When using a cableless ultrasound transducer from an Avalon CL or Avalon CTS system to
measure the fetal heart rate, note that you cannot use any other ultrasound transducer (whether
cableless or wired) at the same time.
CAUTION
Never use ultrasound transducers connected to more than one fetal monitor on the same patient.
• When using an Avalon CL or Avalon CTS you should be aware that FMP is not recommended
when the mother is likely to move, and you should disable Fetal Movement Profile (FMP) on the
fetal monitor (Fetal Movement Off) if the mother is walking. See also “Fetal Movement Profile”
on page 160.
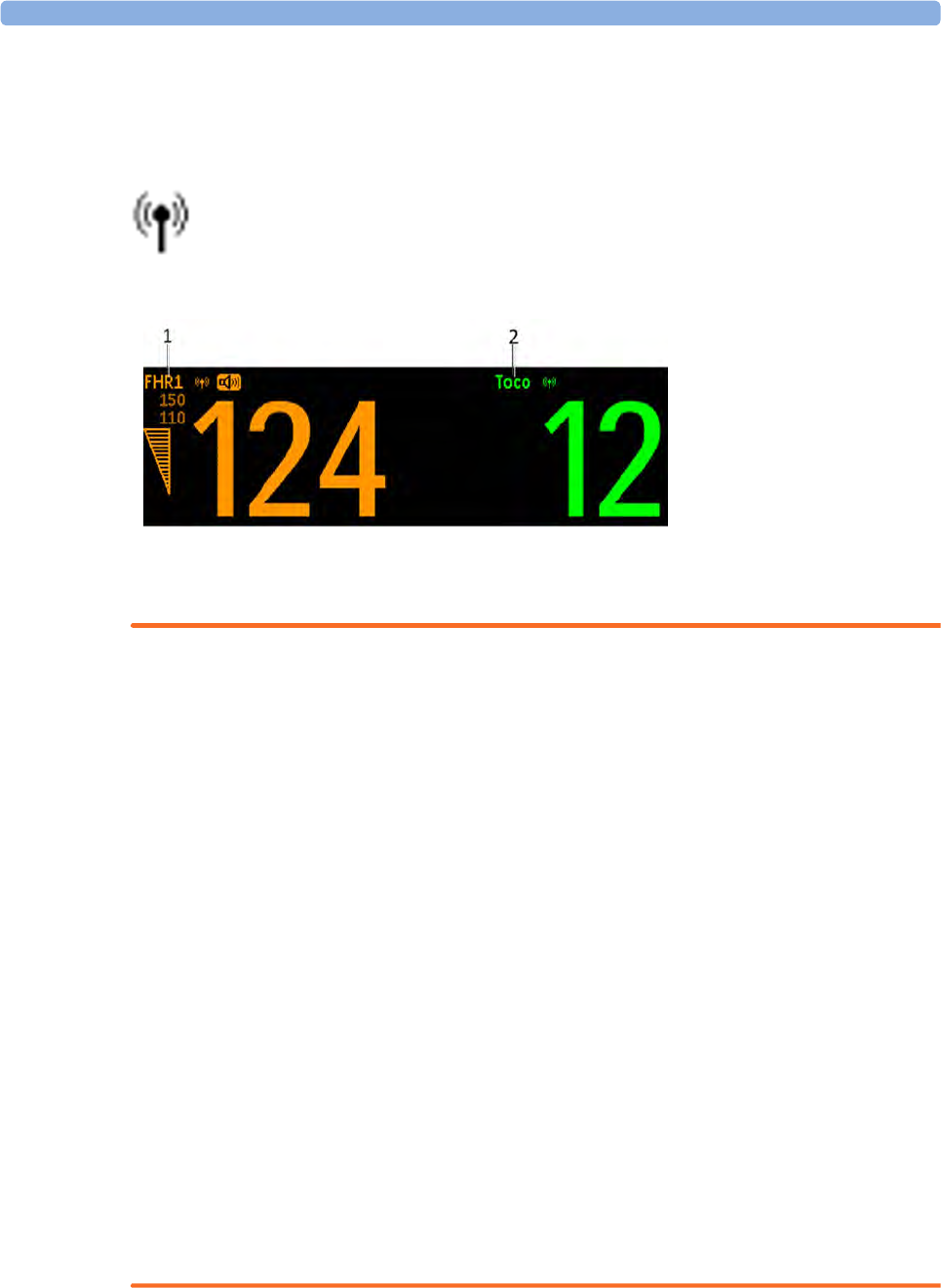
11 Monitoring FHR and FMP Using Ultrasound
157
• With the Avalon CL Transducer System you can now monitor twins and triplets with cableless
transducers. The Avalon CTS System does not have this option.
The wireless symbol appears next to the measurement label, indicating that the measurement is being
made by a cableless transducer.
WARNING
• Ensure that the conductive parts of the fetal scalp electrode and the maternal leg plate electrode do
not contact other conductive parts, including earth.
• Indication of the heart-rate may be adversely affected by the operation of cardiac pacemaker pulses
or by cardiac arrhythmias.
• During ambulant FHR monitoring, the chance of losing the signal or detecting the maternal heart
rate is higher than during stationary monitoring. The frequency of the patient's walk may be
detected, and mistaken for a FHR signal.
• Check the mother’s pulse periodically during monitoring and compare this with the FHR signal.
Beware of mistaking a “doubled” maternal heart rate for FHR. If a fetus is dead, there is a risk that
the maternal heart rate is monitored and misinterpreted as the fetal heart rate. Therefore, the
simultaneous monitoring of maternal heart rate (preferably, the maternal ECG) and the fetal heart
rate is encouraged.
• Do not interpret maternal movements as fetal movements.
• Artifacts: FMP artifacts are generated during fetal heart rate searching by changing the transducer
position, therefore Philips fetal monitors enable the FMP only after detecting a valid heart rate
signal for several seconds. FMP is not recommended when the mother is likely to move, and you
should disable Fetal Movement Profile (FMP) at the fetal monitor (Fetal Movement Off) if the
mother is walking.
• Gaps in maternal heart rate detection can occur:
– if the transducer is not correctly positioned.
– due to the pulsation of uterine blood vessels.
–if the fetus moves.
1FHR1
2Toco parameter
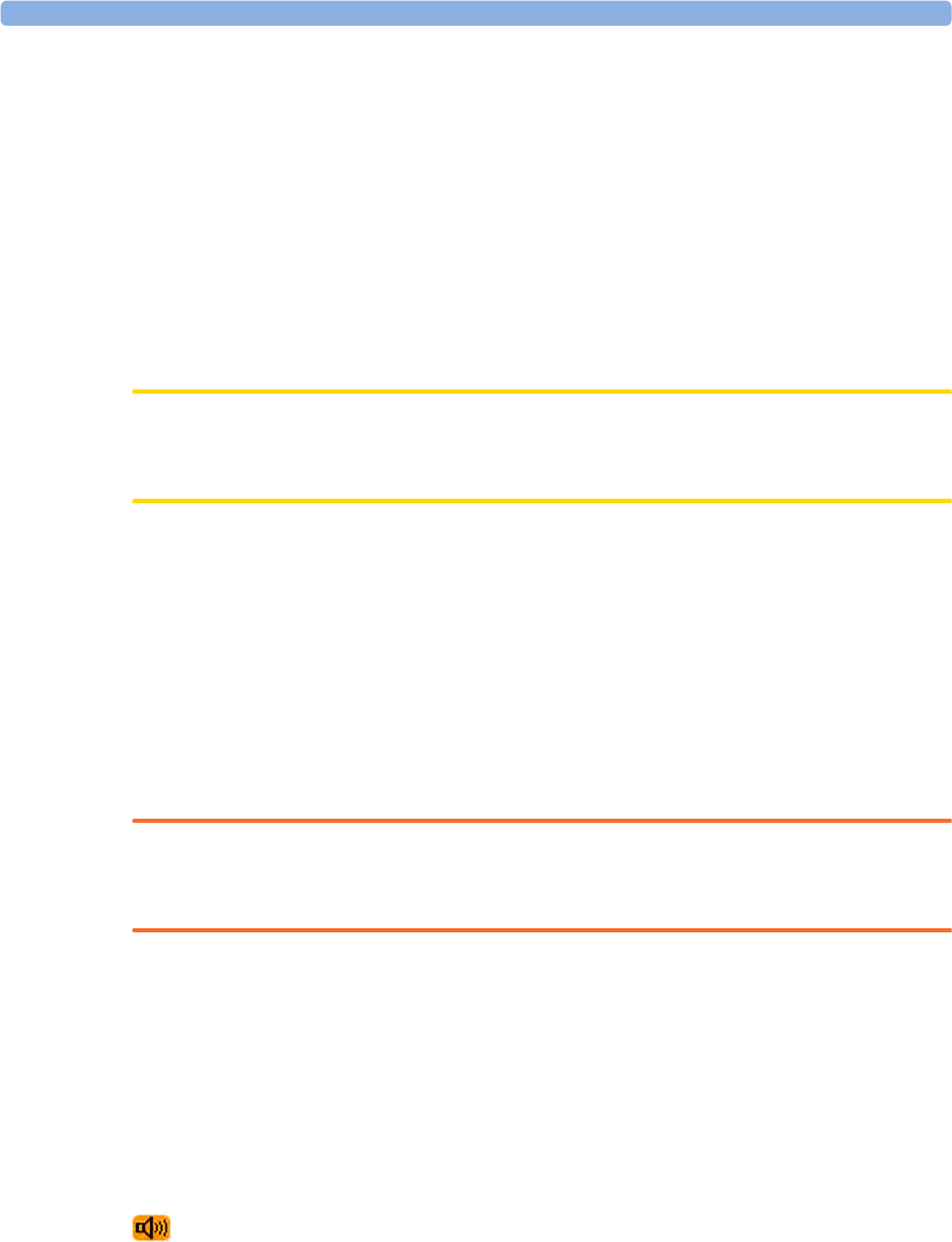
11 Monitoring FHR and FMP Using Ultrasound
158
Preparing to Monitor
Prepare for ultrasound monitoring using the list below. The standard procedures in use in your facility
determine the sequence of actions.
1Determine fetal position.
2Fasten the belt around the patient.
3Switch on the monitor and the recorder.
4Connect the transducer to a free socket. The signal quality indicator for the heart rate initially
displays an invalid signal.
5Apply a thin layer of ultrasound gel to the underside of the transducer.
CAUTION
Using ultrasound gel not approved by Philips may reduce signal quality and may damage the
transducer. This type of damage is not covered by warranty.
1Place the transducer on the abdomen, if possible over the fetal back or below the level of the
umbilicus in a full-term pregnancy of cephalic presentation, or above the level of the umbilicus in
a full-term pregnancy of breech presentation. Work the transducer in a circular motion to ensure
the gel layer makes good contact.
2When the sensor is connected correctly and you receive a good signal, the signal quality indicator
should be filled out. If an inadequate signal is produced, the signal quality indicator will indicate a
poor signal, and no numeric will appear on the screen.
3Adjust the audio volume of the monitor's loudspeaker to a clearly audible level, while moving the
transducer over the abdomen. When you have a good signal, secure the transducer in position
below the belt.
WARNING
Periodically compare the mother's pulse with the signal coming from the monitor's loudspeaker to
ensure that you are monitoring fetal heart rate. Do not mistake a doubled or elevated MHR for FHR.
The ultrasound transducer may warm slightly (less than 1°C/1.8°F above ambient temperature) when
applied to the patient,. When not applied, the transducer can reach a maximum temperature of 44°C/
112.2°F at an air temperature of 40°C/104°F.
Selecting Fetal Heart Sound
You can listen to the fetal heart sound from one ultrasound transducer at a time. When the fetal heart
sound is selected for an FHR channel, you see the audio source symbol next to the FHR numeric label
for that channel.
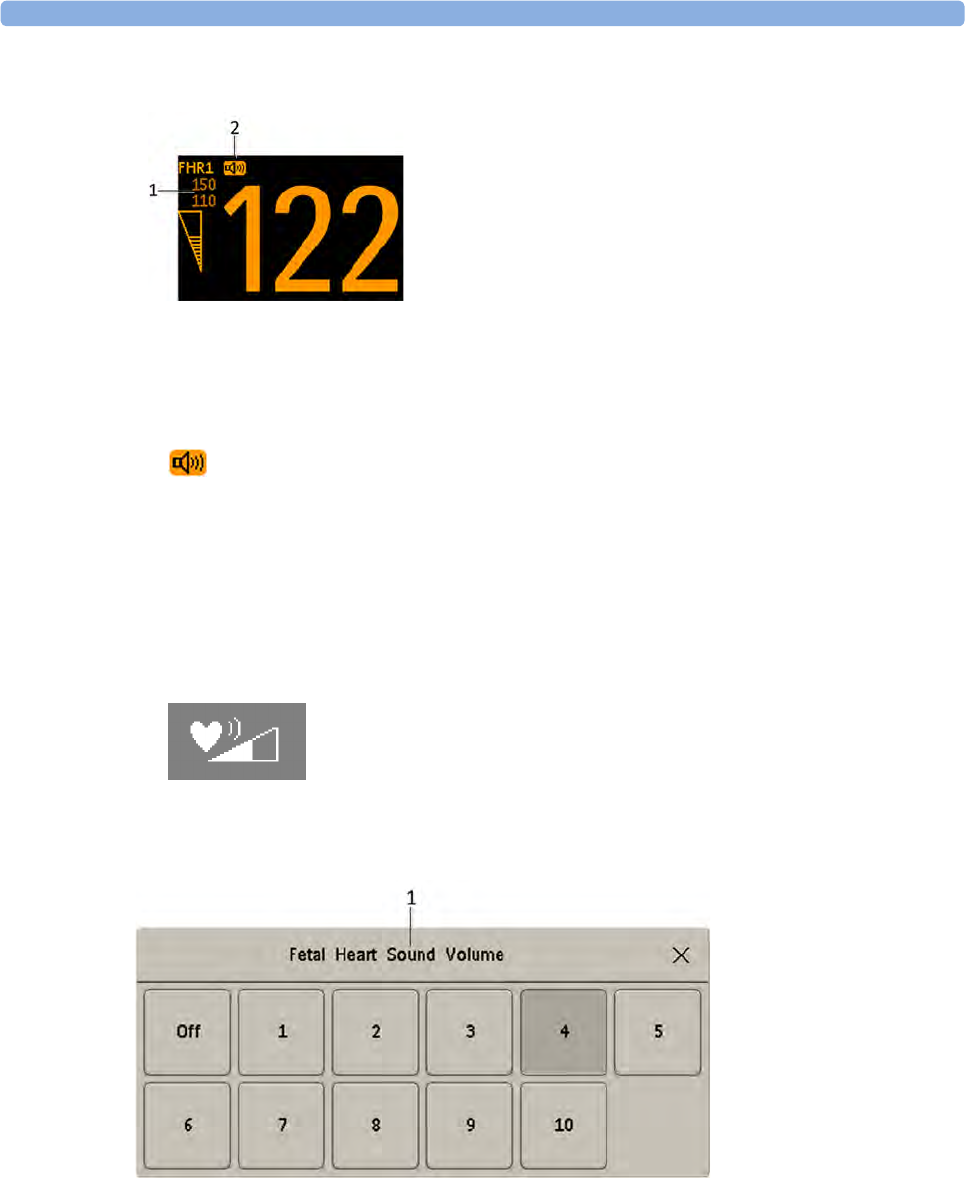
11 Monitoring FHR and FMP Using Ultrasound
159
To select the audio source for an FHR channel:
1Enter the Setup FHR1 menu for the channel you want to hear (FHR1 used as an example).
2Press Select Audio. It may take a few seconds for the audio source symbol to appear.
Changing the Fetal Heart Sound Volume
The FHR volume symbol at the top right of the Fetal Heart Sound Volume window gives you an
indication of the current volume. To change the volume:
1Select the volume symbol. The volume scale pops up.
2Select the required volume from the volume scale.
1FHR1
2Audio source symbol
1Fetal Heart Sound
Volume
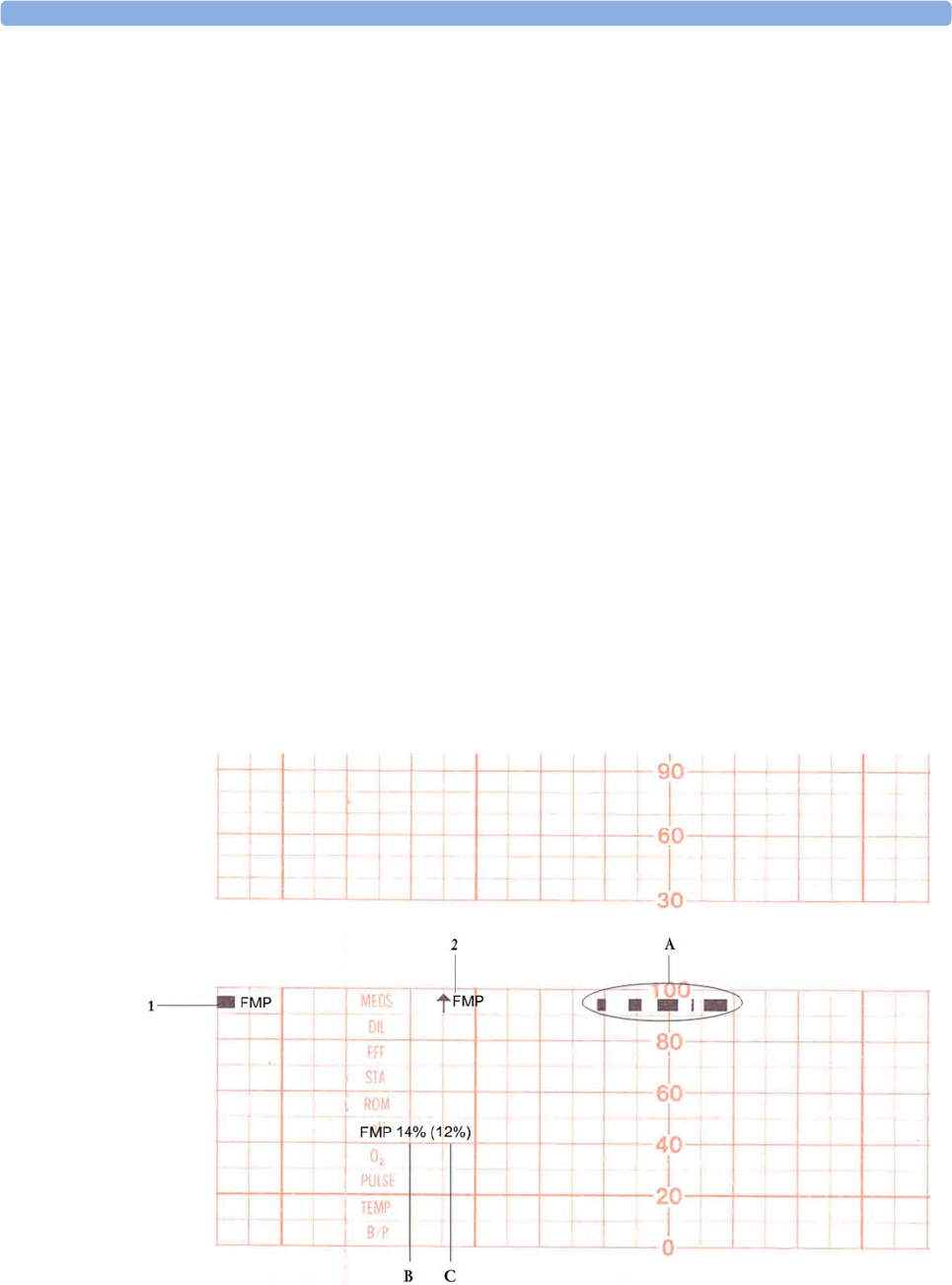
11 Monitoring FHR and FMP Using Ultrasound
160
Fetal Movement Profile
The Fetal Movement Profile (FMP) parameter detects fetal movements via an ultrasound transducer
connected to the monitor. Only the fetus monitored on the FHR1 channel is monitored for FMP.
Once you have enabled FMP (see “Switching FMP On and Off” on page 161), it is triggered
automatically whenever:
• You connect an ultrasound transducer.
• A patient is discharged.
When FMP is enabled, the ultrasound transducer detects most fetal body movements. Eye movements
are not detected and movement of the feet and hands may not be detected. Positioning or
repositioning of the transducer is recorded as fetal movement. Maternal movement, excessive fetal
breathing, or fetal hiccups may also be recorded as fetal movement (also in case of fetal demise or
during the second stage of labor). You can mark these artifacts on the trace paper using either the
remote event marker, or the event marker key as described in “Marking an Event” on page 79. FMP
should be interpreted with care, or disabled when the patient is ambulating or during 2nd stage of
labor. Ignore these movements when you interpret the FMP. When monitoring twins or triplets, only
the fetus monitored on the FHR1 channel is monitored for movement, but be aware that movements
recorded for FHR1 may also be caused by movement of the second or third fetus.
The fetal movement profile (FMP) appears as "activity blocks" (see A below) along the top of the
Toco Scale, the length of each block showing the duration of the activity.
FMP Statistics
FMP statistics are printed every ten minutes.
1FMP enabled
11 Monitoring FHR and FMP Using Ultrasound
161
The FMP detection activates after about half a minute of steady heart rate signals (signal indicator half-
full, or full) to minimize transducer positioning artifact. You will notice this deliberate delay:
• When a new patient is admitted. A patient discharge restarts the FMP statistics from zero.
• When you connect an ultrasound transducer.
Switching FMP On and Off
You can switch FMP on and off from any FHR channel. For example, to set it from the FHR1
channel:
1Enter the Setup FHR1 menu.
2Select Fetal Movement to toggle between On and Off.
3Return to the main screen.
2FMP started here
AIndication of current fetal movement.
BThe FMP statistics are presented as two percentage figures:
The first figure shows the percentage of detected fetal movements in the previous ten
minutes.
CThe second figure shows the percentage of detected fetal movements since the start of
recording.
To mark the start of the FMP statistic, FMP is printed on the paper with an arrow.
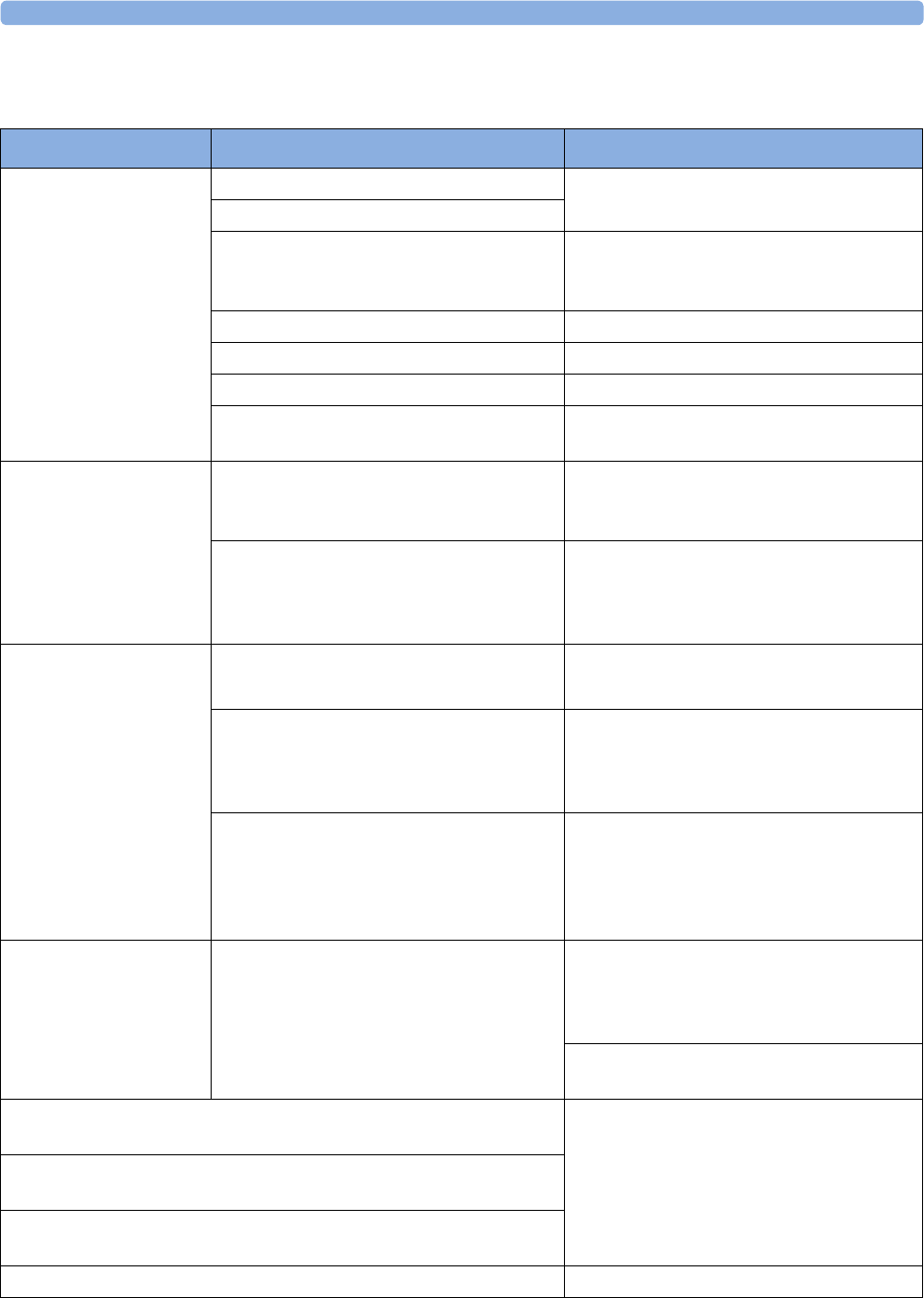
11 Monitoring FHR and FMP Using Ultrasound
162
Troubleshooting
Problem Possible Causes Solutions
Erratic trace
Erratic display
Fetal arrhythmia Consider monitoring FHR using DECG
after the rupture of membranes.
Obese patient
Transducer position not optimal Reposition transducer until signal quality
indicator shows a good signal (at least
half-full).
Belt loose Tighten belt
Too much gel Remove excess
Very active fetus -
Insufficient gel Use enough gel to ensure the transducer
makes good contact with the mother's skin.
Signal quality indicator is
continuously poor
Transducer position not optimal Reposition transducer until signal quality
indicator shows a good signal (at least
half-full).
FHR less than 50 bpm (and the FHR is
audible)
If membranes are ruptured, using a fetal
scalp electrode (FM30 and FM50 only)
allows measurement of FHR down to
30 bpm.
Questionable FHR Recording MHR by mistake Reposition transducer.
Confirm fetal life.
Recording periodic signals when the
transducer is not applied to the patient
Disconnect all NON-USED ultrasound
transducers, as continuous, regular
mechanical, or electromagnetic influences
can result in an artificial trace.
Recorded FHR appears to be suspiciously
higher, or suspiciously lower, than real FHR.
In very rare cases, half- or double-counting
of the FHR can occur.
If you have reason to question the validity of
the recorded FHR, always verify FHR by
independent means (by auscultation, for
example). Measure maternal pulse by
independent means.
FHR not recorded FHR is less than 50 bpm or over 240 bpm If membranes are ruptured, using a fetal
scalp electrode (FM30 and FM50 only)
allows measurement of FHR down to
30 bpm.
If FHR is outside of the specified range,
verify FHR by independent means.
FHR1 Equip Malf or FHR2 Equip Malf or FHR3 Equip Malf INOP
displayed.
See “Patient Alarms and INOPs” on
page 121.
FHR1 Signal Loss or FHR2 Signal Loss or FHR3 Signal Loss INOP
displayed.
FHR1 Unplugged or FHR2 Unplugged or FHR3 Unplugged INOP
displayed.
If you suspect the transducer is malfunctioning Test the transducer.

11 Monitoring FHR and FMP Using Ultrasound
163
Additional Information
Artifact in Fetal Heart Rate Measurement
How to detect it and reduce its occurrence using the Avalon Fetal Monitor
The ultrasound derived FHR measurement technique in Avalon fetal monitors, like all other
ultrasound fetal monitors’ FHR measurement techniques, has limitations that can lead to
misrepresentation of the fetal heart rate pattern and potential misinterpretation of the fetal condition.
An incorrect interpretation of the trace may lead to either unnecessary interventions, or to failure to
detect fetal distress and the need for intervention. Thus, the on-going evaluation of the recorded trace
requires regular confirmation that the trace represents the true FHR. Specific situations requiring such
confirmation include the following:
• After starting a measurement or changing a transducer
• After maternal position changes, for example during pushing with contractions
• When the tracing shows abrupt changes in baseline rate, variability, or pattern (decelerations to
accelerations) especially in the second stage of labor
• When the baseline maternal heart rate is within about 15 bpm of the FHR
• When the user is unable to determine a baseline rate and variability occurs between consecutive
contractions
There are several ways to verify the source and/or accuracy of the recorded fetal heart rate pattern.
These include:
Verification of the FHR with:
• An obstetric stethoscope,
• Ultrasound imaging, or
• A fetal scalp electrode
Verification of the maternal heart rate:
• Using pulse oximetry - for a maternal heart rate pattern displayed simultaneously with the FHR
(Cross-Channel Verification (CCV) feature),
• Using Maternal ECG - for a maternal heart rate pattern displayed simultaneously with the FHR
(CCV feature), or
• Manual determination of the maternal pulse
Whenever possible measure the maternal pulse rate to make use of the monitor’s Cross-Channel
Verification (CCV) feature, especially during the second stage of labor, or when the maternal pulse is
elevated over 100 bpm. The Philips Avalon fetal monitor provides a Toco MP or CL Toco+MP
transducer for maternal pulse detection and the creation of a maternal heart rate pattern plotted on the
same recorder as the FHR pattern. In case of difficulties deriving a stable maternal pulse reading using
the Toco MP or CL Toco+MP transducer, use SpO2 or MECG instead.
When either of these parameters is utilized, the monitor will automatically and continuously perform a
CCV of the maternal heart rate pattern against the FHR pattern displayed on the monitor. If the
patterns and rates are similar, the CCV provides an alarm that both rates are probably from the same
source (i.e., they both represent the maternal heart rate pattern and the fetus is not being monitored).
Repositioning the ultrasound transducer will usually correct this, but it may be necessary to apply a
fetal scalp electrode. Advising the mother to temporarily cease pushing during contractions may help
to more rapidly resolve any uncertainty in this situation.

11 Monitoring FHR and FMP Using Ultrasound
164
Doubling: The auto correlation algorithm can display a doubled fetal or maternal heart rate if the
duration of diastole and systole are similar to each other, and if the heart rate is below 120 bpm.
Doubling, usually brief, is accompanied by an abrupt switch of the trace to double the baseline value.
Halving: With fetal tachycardia (above 180 bpm) and some interference from breathing or maternal
arteries the auto correlation algorithm may only recognize every second beat resulting in a halved rate
for a limited time. If the actual FHR is above the maximum limit of the monitor (240 bpm), the
algorithm will also half-count. Halving is accompanied by an abrupt switch of the trace to exactly half
the prior baseline value. This switch may simulate a FHR deceleration and be referred to by clinicians
as a “false deceleration.”
Switching to maternal heart rate (also referred to as "Maternal Insertion"): The fetal heart can
move partly or fully out of the ultrasound beam and the auto correlation algorithm may then pick up
and display the maternal heart rate. Depending on the signal mix in the ultrasound signal, switching to
the maternal heart rate may mimic several conditions with the potential for erroneous interpretation
and response as follows:
•The switch to the maternal heart rate may simulate a FHR deceleration (i.e., a decrease of
the fetal heart rate, and be referred to by clinicians as a “false deceleration”).
•The maternal heart rate may simulate a normal fetal heart rate pattern (i.e., it may mask a
FHR deceleration or fetal demise).
Especially during pushing with contractions in the second stage of labor, the maternal heart rate
may increase to the point where it may equal or exceed the fetal rate. Here the maternal trace may
mimic a normal fetal trace while the fetus may be having decelerations or fetal demise has
occurred. This change from fetal to maternal heart rate pattern may not be at all obvious unless
CCV is used and represents the most dangerous pitfall of all the artifacts because fetal distress may
go unrecognized.
•The maternal heart rate may simulate a FHR acceleration, which is an increase of the fetal
heart rate.
During expulsive efforts, the maternal heart rate normally accelerates and may be at or above the
normal FHR range.
•The FHR may display gradual appearing decelerations. Generally, the “false decelerations”
described above are abrupt. Rarely, combinations of “noisy/erratic signal” associated with changes
in maternal and/or fetal rate or movement will produce more gradual appearing “false
decelerations” but these are usually short-lived with an abrupt return to an obviously stable FHR
baseline.
“Noisy/Erratic” signals: With mixed or weak signals the tracing may reveal very brief episodes of
erratic recorded traces. These represent the auto correlation algorithm finding brief sequences of
apparent and persistent heartbeats amidst a mixed or weak signal. These erratic recorded traces are
commonplace, especially in association with fetal or maternal movement. During prolonged periods
of such noisy/erratic signals, the fetus is not being adequately monitored.
Drop out: With mixed or weak signals there may be no heart rate tracing at all. These episodes reflect
that if the algorithm does not find an apparent and persistent heartbeat amidst a mixed or weak signal,
it will not print a heart rate on the tracing. Brief episodes of drop out are commonplace, especially in
association with fetal or maternal movement. During prolonged periods of drop out, the fetus is
not being adequately monitored.

11 Monitoring FHR and FMP Using Ultrasound
165
Multiple Fetuses
With multiple fetuses, the potential to experience these artifacts is increased. Positioning of the
transducer is even more critical. Ultrasound scanning should be used to help with positioning of
individual transducers. See also “Monitoring Twin FHRs” on page 171 and “Monitoring Triple FHRs”
on page 179.
Obtaining a Good Heart Signal
To successfully position the ultrasound transducer, first determine the fetal position using palpation.
Position the transducer over the strongest audible fetal heart sound from the monitor’s speaker and
wait at least six seconds after each transducer adjustment to verify a good signal quality displayed
on the Signal Quality Indicator and a consistent FHR numeric display. Having determined the position
that provides a strong fetal signal, fix the transducer on the abdomen with the belt.
If the quality of the signal or the appearance of the heart rate trace from the ultrasound transducer is
questionable, the transducer should be repositioned as described above. Alternatively, the use of an
ultrasound scanner will greatly facilitate the determination of the optimal site for the ultrasound heart
rate transducer. Factors during the second stage of labor that may influence the quality of the FHR
tracing obtained with ultrasound include:
• Uterine contractions
• Changing contour of the maternal abdomen
• Maternal body movement - positioning
• Maternal expulsive efforts - pushing
• Maternal tachycardia/accelerations with contractions
• Fetal decelerations, Fetal tachycardia
• Delayed return of the fetal heart rate from a deceleration
• Descent of the fetus in the birth canal
• Rotation of the fetus in the birth canal
In some cases during the second stage of labor, a good and reliable ultrasound FHR signal may not be
obtainable, and the use of a fetal scalp electrode must be considered (fetal ECG).
Heart Rate Sound
The heart rate sound emitted by the device is a representation of movement that, in most cases,
permits accurate auscultation of the FHR corresponding to the FHR displayed on the monitor and rate
pattern depicted on the trace recording. On occasion, the user may hear a FHR that differs from the
FHR display and the recorded trace. This may occur in situations where the fetal heart moves partly
out of the transducer ultrasound beam. In these cases, the user may hear the FHR emitted from the
monitor’s speaker, even though another periodic signal (usually the maternal heart rate) has become
stronger. The auto correlation algorithm will display the stronger maternal heart rate, despite the
persistence of a weaker fetal signal. These occurrences are usually very brief and, if persistent, can be
addressed by repositioning the transducer.
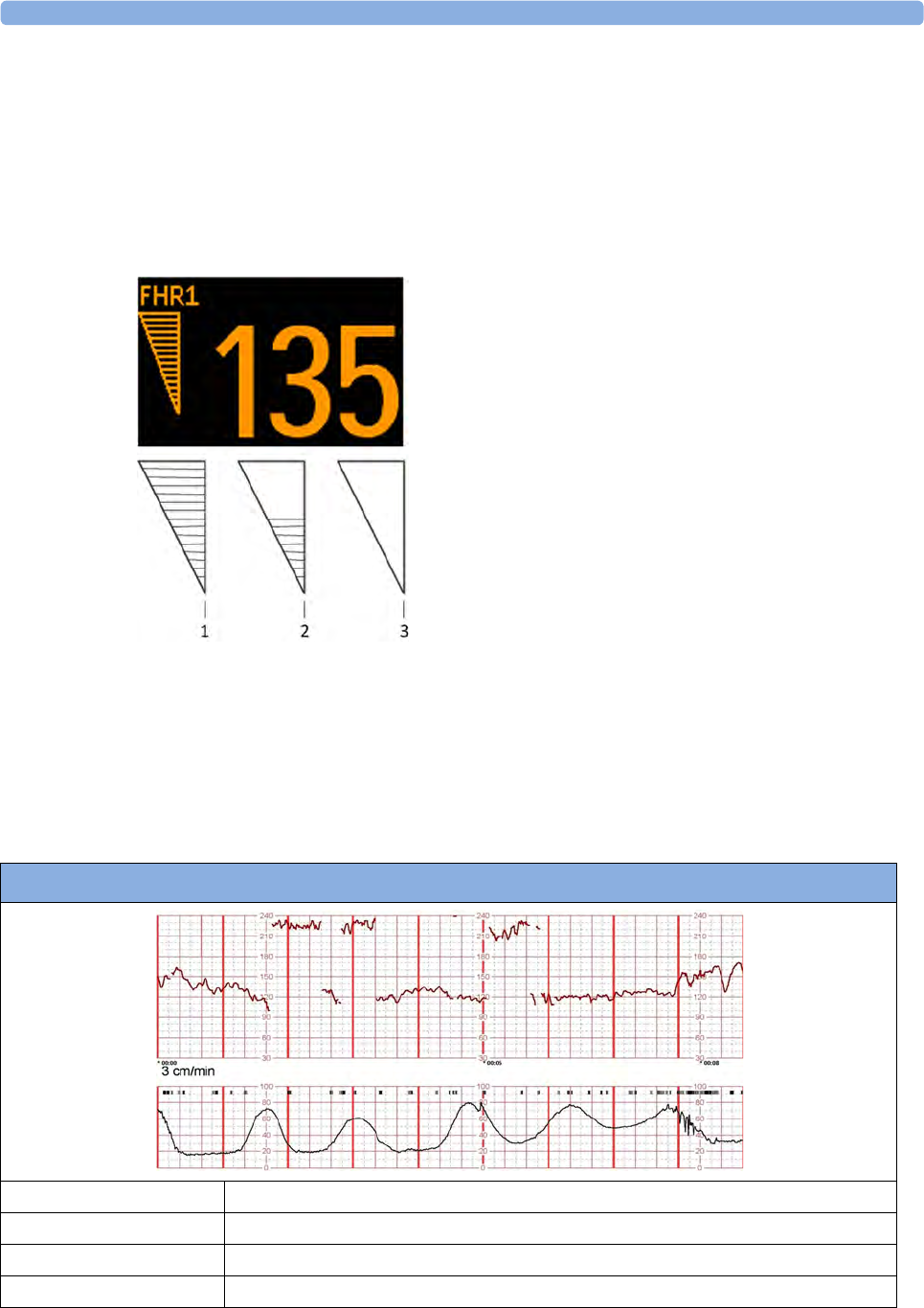
11 Monitoring FHR and FMP Using Ultrasound
166
Signal Quality Indicator
Avalon compared with its predecessor, the Series 50
Signal quality indicator on Avalon fetal monitors:
Instead of a traffic light-like design (red – yellow – green) used on the Series 50, the signal quality on
the Avalon fetal monitor is indicated by a triangle on the touch screen that is displayed in one of three
ways:
Examples of Artifacts
When monitoring the maternal ECG, a beat-to-beat maternal heart rate trace is printed alongside the
FHR recorded trace. When monitoring the maternal SpO2 derived pulse rate, a filtered and averaged
heart rate trace is printed.
Following are recorded trace examples of complaints received regarding inaccurate output from the
Avalon monitors. Scaling is 3 cm/min and 30 bpm/cm.
Avalon fetal monitor signal quality indicator display:
1Completely filled triangle, indicating good signal quality
(good/full).
2Half-filled triangle, indicating limited signal quality. This
condition may indicate a weak or ambiguous signal. If this
status persists, reposition the transducer (acceptable/
medium).
3Empty triangle, indicating insufficient signal quality. No
FHR is displayed on the monitor’s numeric display or the
recorded trace. If this status persists, reposition the
transducer (poor/no signal).
Double-Counting
Baseline Rate 120
Baseline Variability Moderate
Accelerations Present
Decelerations Not apparent
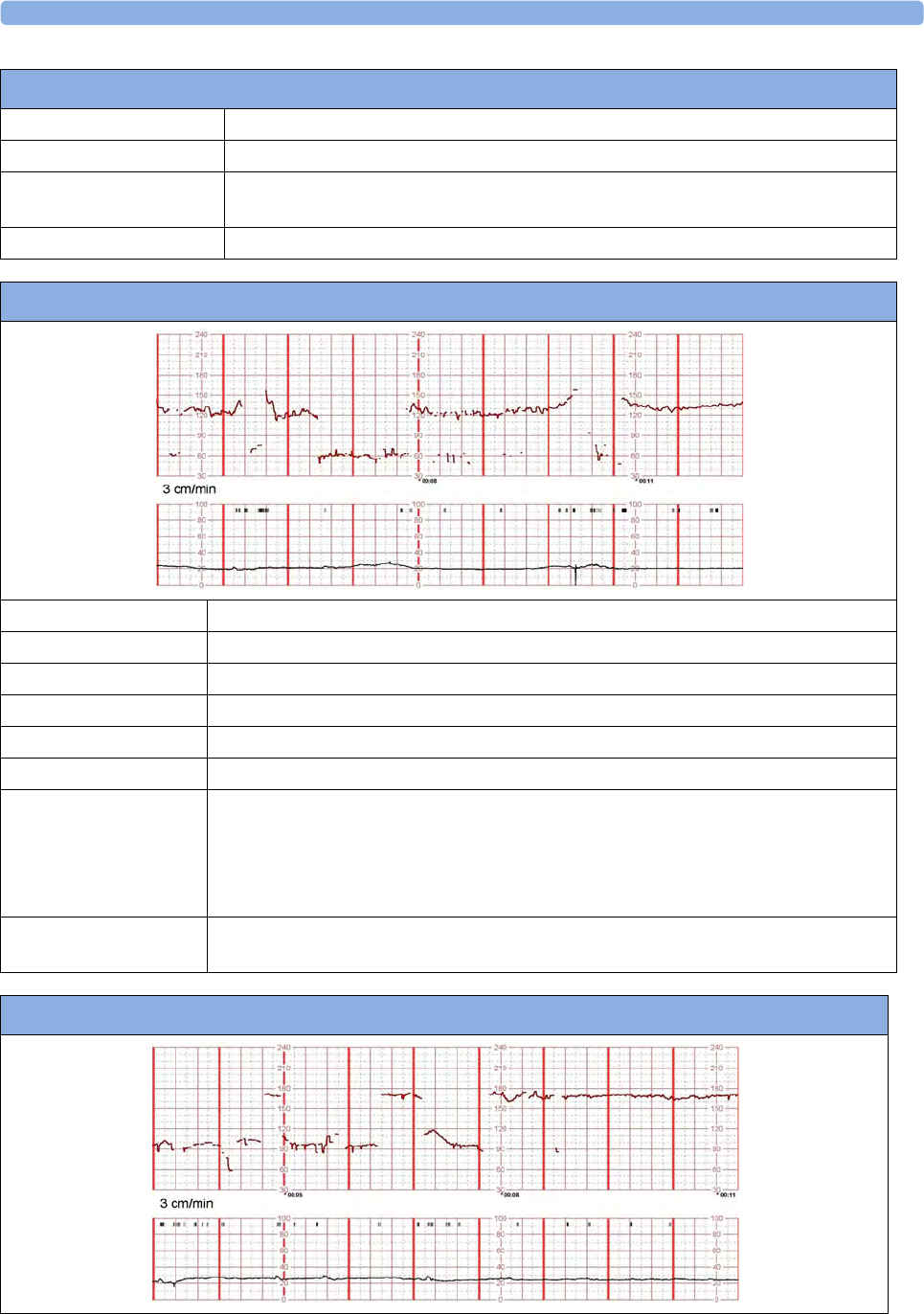
11 Monitoring FHR and FMP Using Ultrasound
167
Contractions Excessive, coupling, hypertonus
Artifact Double-Counting
Comment Reassuring tracing. The excessive uterine activity should prompt discontinuation of
any oxytocic agent.
Remediation The true fetal rate can be confirmed by auscultation or by fetal scalp electrode.
Double-Counting
Half-Counting
Baseline Rate 120
Baseline Variability Moderate
Accelerations Present
Decelerations Not apparent
Contractions Minimal
Artifact Half-counting, noise, drop out
Comment Reassuring tracing. The half-count at 4-5 minutes into the tracing may simulate a fetal
deceleration, but the abruptness and the lack of any compensatory changes when the
normal rate returns suggests that this is half-counting. Insertion of the maternal heart
rate (see below) may produce a similar pattern. Note also very brief episodes of half-
counting, maternal insertion, and signal drop out.
Remediation Auscultation or the application of a direct scalp electrode, if feasible, will reveal the true
fetal heart rate.
Maternal-Switching (Maternal Insertion)
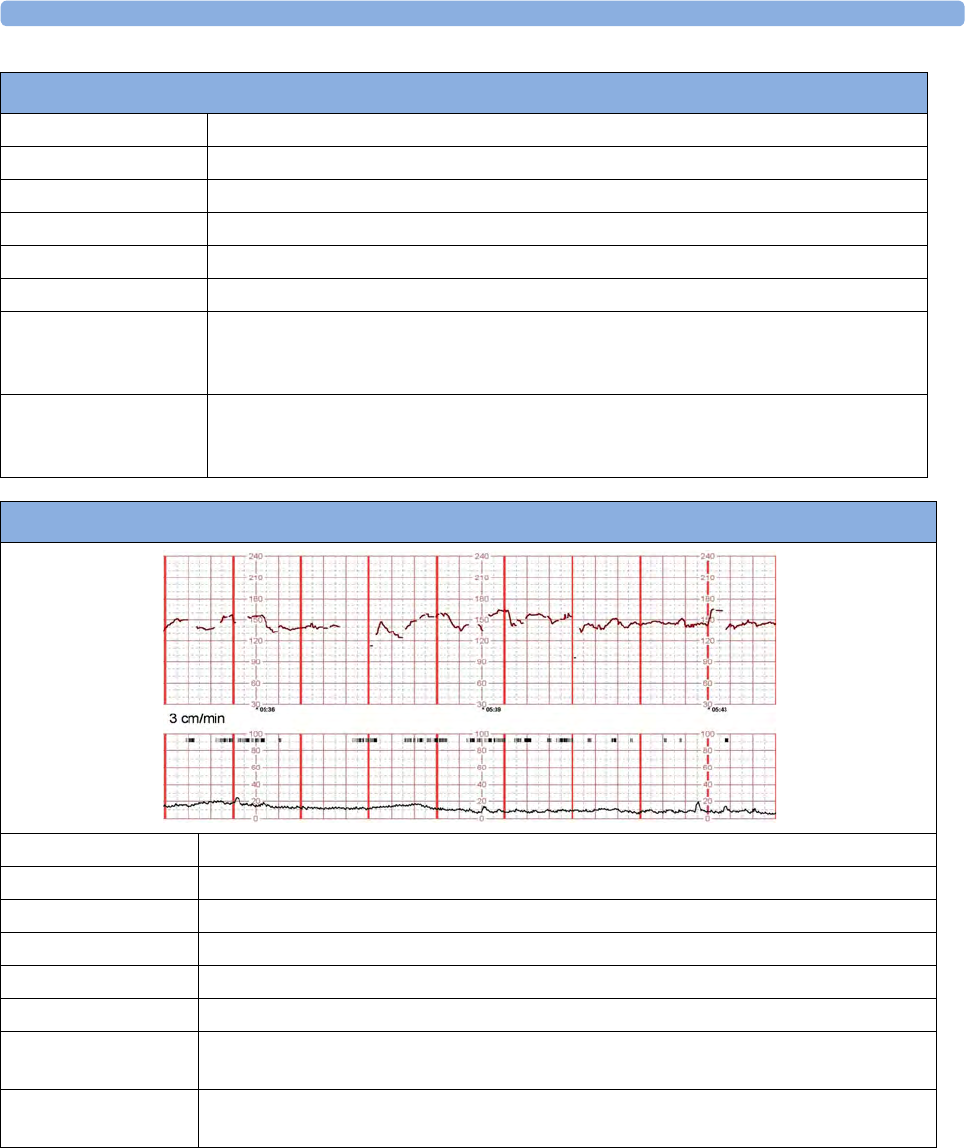
11 Monitoring FHR and FMP Using Ultrasound
168
Selection of Literature References on Artifacts
___________________________________________________________
Fetal Monitoring, A Multidisciplinary Approach, Seventh edition
Susan M. Tucker, Lisa A. Miller, David A. Miller
Mosby Inc. 2009, ISBN 978-0-323-08352-2
___________________________________________________________
Baseline Rate 170 - Tachycardia
Baseline Variability Moderate
Accelerations Unable to determine
Decelerations Absent
Contractions Absent
Artifact Maternal insertion, noise
Comment The fetus has an elevated baseline rate of about 170 bpm with minimal to moderate
variability. The ability to assess fetal status is limited because about half of the tracing
displays the maternal heart rate.
Remediation The application of a maternal transducer (ECG or pulse oximeter) will likely resolve any
possible confusion with the tracing. Repositioning the transducer may produce a more
reliable tracing. Consideration must also be given to applying a fetal scalp electrode.
Maternal-Switching (Maternal Insertion)
Noisy/Erratic Signal and Dropout
Baseline Rate 140
Baseline Variability Moderate
Accelerations Present
Decelerations Absent
Contractions Minimal
Artifact Noisy signal, drop-out
Comment Reassuring tracing. Note that there is episodic drop out of the signal with discontinuity of
the fetal tracing.
Remediation Either improving the position of the transducer or the application of a fetal scalp
electrode will reduce the amount of artifact in the tracing.

11
169
Signal ambiguity resulting in unexpected outcome with external fetal heart rate monitoring
By Duncan R. Neilson Jr, MD; Roger K. Freeman, MD; Shelora Mangan, RNC, MSN, CNS
American Journal of Obstetrics & Gynecology, June 2008:
___________________________________________________________
Antepartal and Intrapartal Fetal Monitoring, 3rd Edition (2007)
By Michelle L. Murray, PhD, RNC
Springer Publishing Company, ISBN 0-8261-3262-6
Page 2, Table 2: Limitations of Continuous EFM
Item 15: “The US may detect maternal aortic wall movement and the MHR will be printed. A failure
to recognize the lack of a FHR may delay appropriate management.”
Page 38, “Solving Equipment Problems”, Table 3: The Ultrasound Transducer
___________________________________________________________
JOGC (Journal of Obstetrics and Gynaecology Canada)
Volume 29, Number 9, September 2007
Chapter 2: Intrapartum Surveillance
Page S35: “Methods of Electronic Fetal Monitoring”
“… Among its disadvantages are the need for readjustment with maternal or fetal movements and the
following: the transducer may record the maternal pulse, it may be difficult to obtain a clear tracing in
obese women or those with polyhydramnios, artifact may be recorded, and there may be doubling or
halving of the fetal heart rate when it is outside of the normal range.”
___________________________________________________________
Maternal of Fetal Heart Rate? Avoiding Intrapartum Misidentification
by Michelle L. Murray
JOGNN Clinical Issues, April 2003, 33, 93-104; 2004. DOI: 10.1177/0884217503261161
Figure 9 "The recording is of the MHR with occasional doubling."
___________________________________________________________
Maternal Heart Rate Pattern – A Confounding Factor In Intrapartum Fetal Surveillance
Schifrin BS, Harwell R, Hamilton-Rubinstein T, Visser G:
Prenat Neonat Med 2001; 6:75-82.
___________________________________________________________
Fetal Monitoring in Practice, 2nd Edition 1998
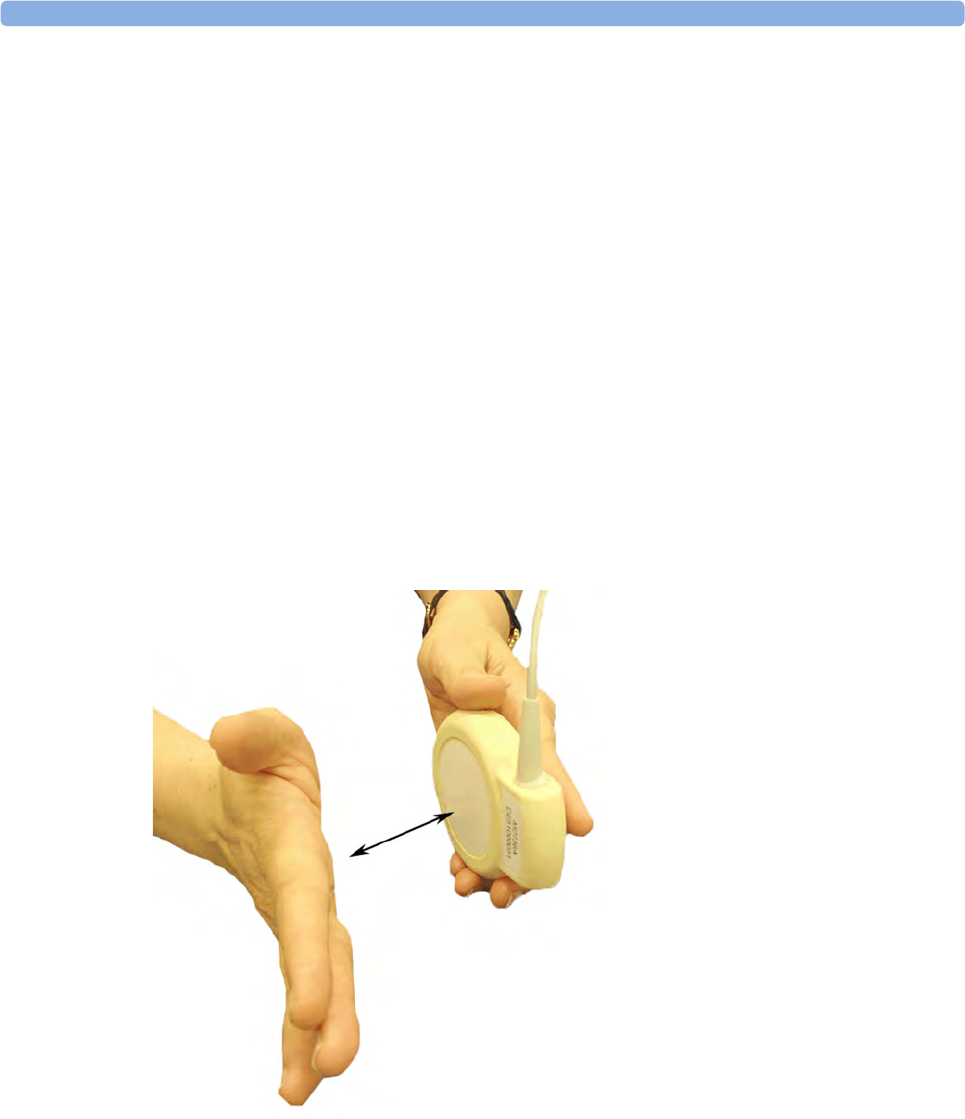
11 Monitoring FHR and FMP Using Ultrasound
170
By Donald Gibb, S. Arulkumaran
Butterworth-Heinemann, ISBN 0-7506-3432-2
Page 65, “False or erroneous baseline because of double counting of low baseline FHR”
Page 66, “Bradycardia: fetal or maternal”
___________________________________________________________
Role of Maternal Artifact in Fetal Heart Rate Pattern Interpretation
Klapholz, Henry M, MD; Schifrin, Barry S. MD; Myrick, Richard RS
Obstetrics & Gynecology, September 1974, Volume 44, Issue 3
___________________________________________________________
Testing Ultrasound Transducers
If any of the following tests fail, repeat the test using another transducer. If the second transducer
passes the tests, confirming that the first transducer is defective, contact your service personnel.
If the second transducer also fails the tests, contact your service personnel.
You can test all ultrasound transducers, including the cableless ones as described above.
To test an ultrasound transducer:
1Switch on the monitor and the
recorder.
2Connect the transducer to the fetal
monitor.
3Select the fetal heart sound for this
channel.
4Increase the loudspeaker volume
to an audible level.
5Holding the transducer in one
hand, move your other hand
repeatedly towards and then away
from the surface.
6Check that a noise is heard from
the loudspeaker.

12 Monitoring Twin FHRs
171
12Monitoring Twin FHRs
The FHRs of twins are externally monitored using two ultrasound transducers. The Avalon CL
Transducer system provides the option to monitor twins with cableless transducers. The Avalon CTS
system does not have this option.
FM30/50 Twin FHRs are monitored throughout labor and delivery. After rupture of the membranes, you can
monitor one twin externally using ultrasound, and the other internally using DECG.
Refer to the appropriate preceding chapters for contraindications, and more information about the
available measurement methods.
FHR detection by the monitor does not always indicate that the fetuses are alive. Confirm fetal life
before monitoring, and continue to confirm that the fetuses are the signal source for the recorded fetal
heart rates. See “Confirm Fetal Life Before Using the Monitor” on page 10 and “Cross-Channel
Verification (CCV)” on page 149.
Important Considerations
When monitoring:
• Ensure that you are recording two different fetal heart rates. The cross-channel verification feature
alerts you if the two heart rates coincide (if both transducers are recording the same FHR). If this
happens, check the trace and if necessary, reposition an ultrasound transducer to detect the second
FHR correctly.
• Fetal heart rate measurements are labeled in the order in which you plug in the transducers for
those measurements. It does not matter which fetal sensor socket you use, as the monitor allocates
a channel automatically. For instance, the first transducer you connect is automatically allocated a
channel, and the measurement is labeled FHR1, the second is labeled FHR2, and so on.
If you need to disconnect the transducers measuring the FHR temporarily, with the intention to
continue monitoring after the temporary break (for example, if the mother needs to go to the
bathroom), it is important that you reconnect the transducers in the same order as you originally
connected them to make sure the measurement labels remain consistent.
Upon discharge of the patient all connected transducers are reset from left to right. Example: Only
one transducer is still connected to the monitor, it was labeled FHR2 while monitoring the previous
discharged patient; it is now reset to FHR1.
• The transducer Finder LED lets you identify at a glance which transducer is monitoring which
heart rate channel.
• The fetal sensor socket to which a transducer is connected is identified by the transducer position
indicator in the blue setup menu header:
FM20/FM30 FM40/FM50
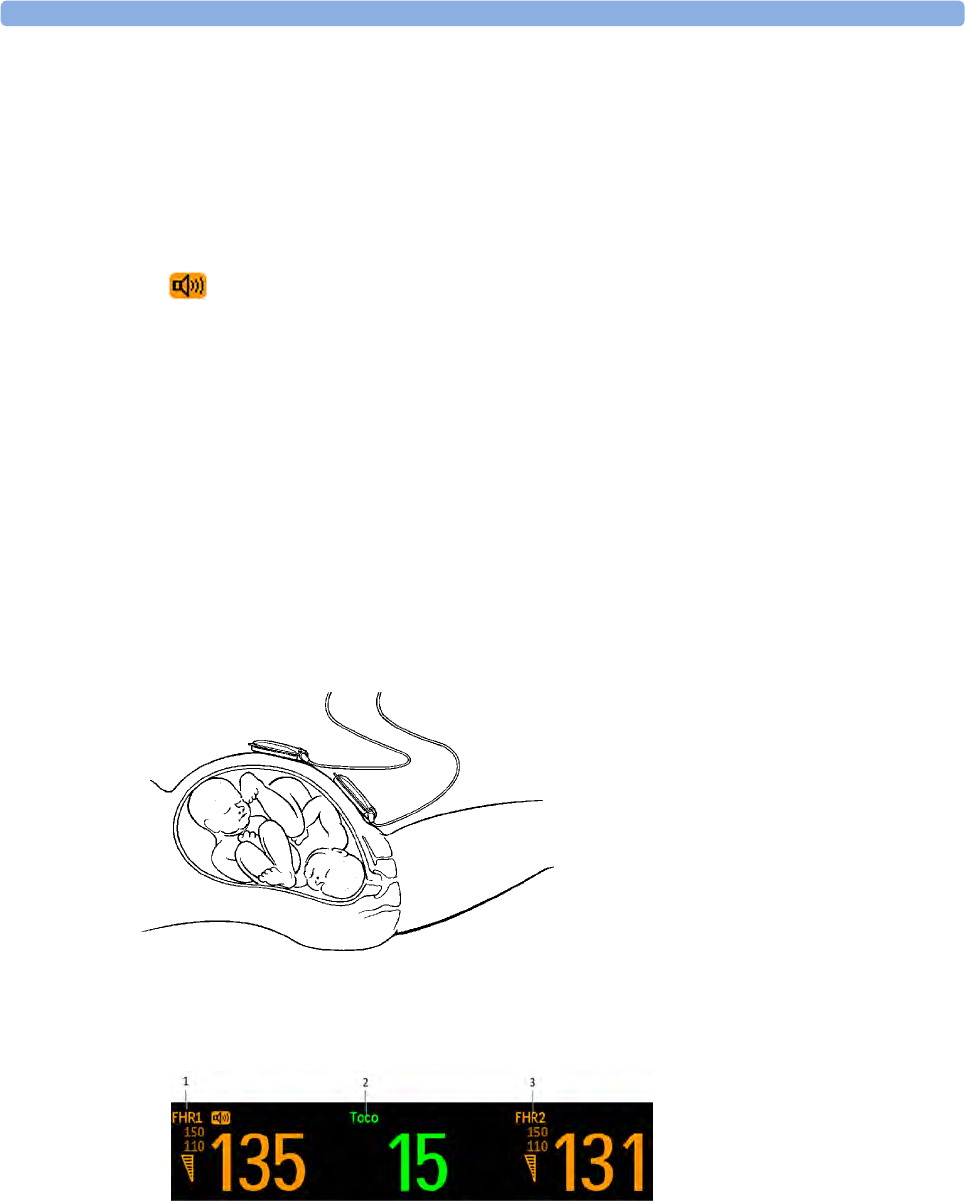
12 Monitoring Twin FHRs
172
• The trace recorded for FHR1 is thicker (darker) than that recorded for FHR2. This ensures that
the two heart rates are easily distinguishable. The thickness of the recorded trace can be changed in
Configuration Mode.
• Remember that only one fetal heartbeat can be heard from the loudspeaker at any time.
• The audio source symbol shows you which fetus you are listening to. To hear the other fetal
heartbeat, select the fetal heart rate sound for this channel (see “Selecting Fetal Heart Sound” on
page 158).
• Monitor maternal pulse, especially during later stages of labor, to avoid mistaking maternal heart
rate for FHR.
• Make sure you are recording the best possible signals by referring to the signal quality indicators
and repositioning the transducers if necessary.
• For the Avalon CL transducer system see “Cableless Monitoring - Important Considerations” on
page 156.
Monitoring Twins Externally
To monitor twin FHRs externally you need two ultrasound transducers. Follow the procedures
described in “Monitoring FHR and FMP Using Ultrasound” on page 155. The transducer Finder LED
lets you identify at a glance which transducer is monitoring which FHR channel, and lights when you
select the FHR numeric field on the screen.
Example of the screen showing ultrasound monitoring of twin FHRs:
1FHR 1
2Toco parameter
3FHR 2
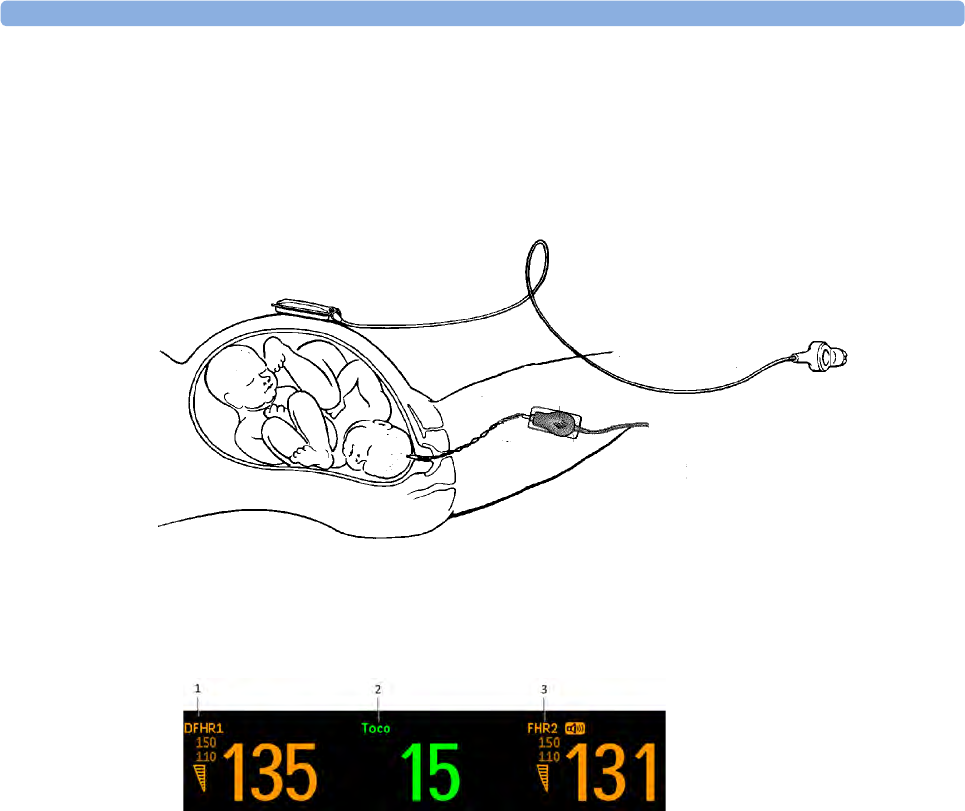
12 Monitoring Twin FHRs
173
Monitoring Twins Internally
FM30/50 Monitor one twin using the procedures described in “Monitoring FHR and FMP Using Ultrasound”
on page 155. Monitor the second twin using the procedures described in “Monitoring FHR Using
DECG” on page 195.
Example of a screen showing twin monitoring using a combination of US and DECG (the fetal heart
rate monitored via DECG is labeled "DFHR1"/"DFHR2"/"DFHR3" on the screen):
Separating FHR Traces
To help you to interpret traces with similar baselines, you can separate the baselines by an offset of
20 bpm by switching trace separation on. For details of the offset, see “Separation Order Type” on
page 174.
Switching Trace Separation On and Off
Connect transducers to the monitor to measure FHR. Depending on the measurement method, you
need either two ultrasound transducers or:
FM30/50 One ultrasound and one Toco+ transducer, or one CL ECG/IUP transducer (to monitor DECG).
1Enter the Main Setup menu by pressing the Main Setup.
2Select Fetal Recorder.
3Select Trace Separation to toggle between On and Off.
4Exit the Main Setup menu.
1DFHR 1
2Toco parameter
3FHR 2
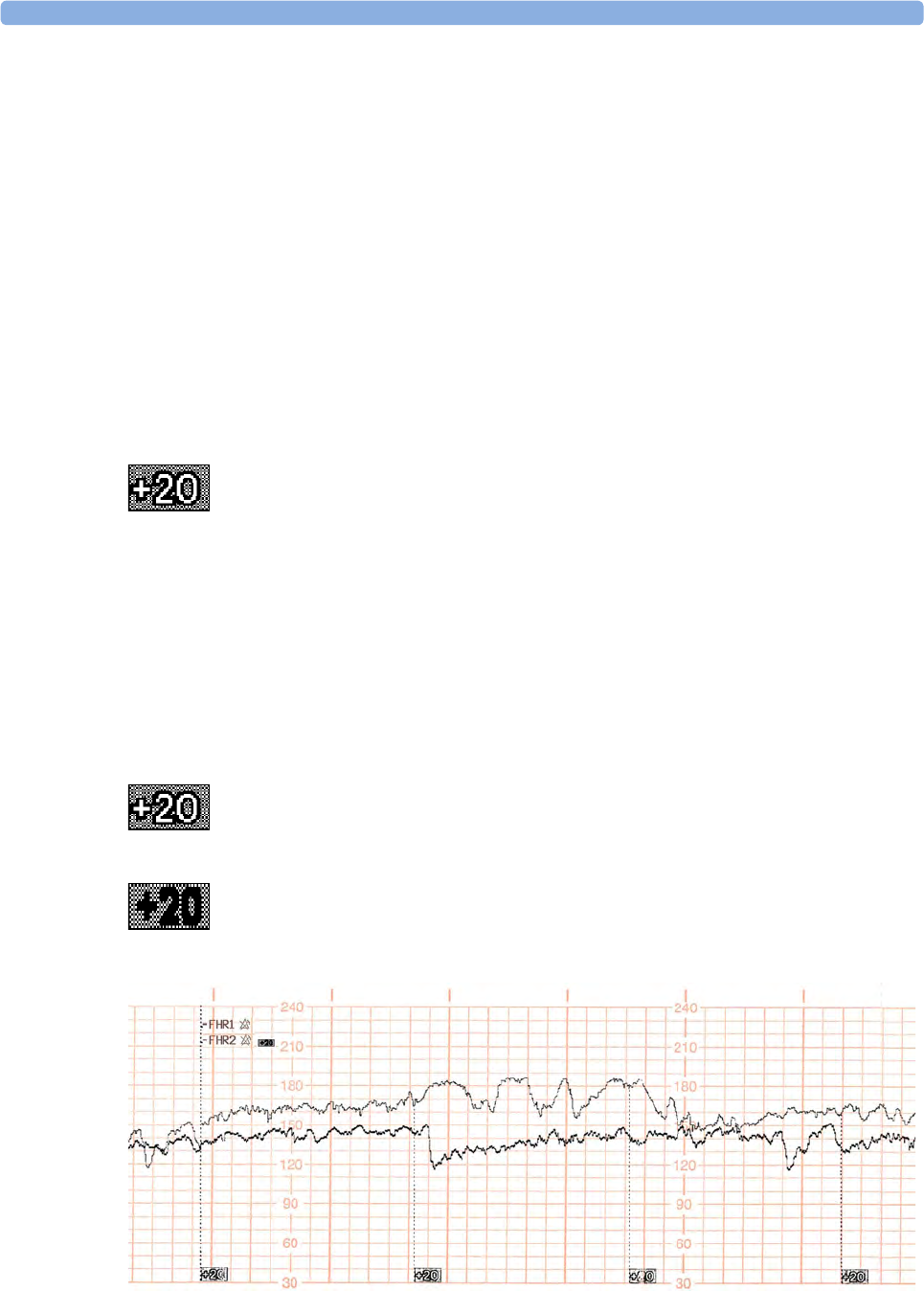
12 Monitoring Twin FHRs
174
Separation Order Type
In Configuration Mode, you can choose between two different ways, Standard and Classic, for
dealing with the trace offsets on the recording (the order in which they are separated) when Trace
Separation is On.
•Standard: the FHR2 trace is shifted up by 20 bpm (it is recorded 20 bpm higher than it really is).
No offset is ever applied to the FHR1 trace - it stays where it is. (In case of a third FHR, this is
shifted down by 20 bpm.)
•Classic: the FHR1 trace is shifted up by 20 bpm when there is more than one FHR measurement.
No offset is ever applied to the FHR2 trace - it stays where it is. (In case of a third FHR, this is
shifted down by 20 bpm.)
When Trace Separation is On
When trace separation is turned on, the recorder prints a dotted line labeled with the two FHRs at the
top, and +20 at the bottom.
Examples of the two methods (Standard, Classic) for determining the trace separation order are
provided here.
"Standard" Separation Order
To make differentiating the traces easier, the trace from the ultrasound transducer connected to the
FHR2 channel is separated from that of FHR1 by 20 bpm. In other words, the trace for FHR2 is
recorded 20 bpm higher than it really is. The trace for FHR1 is never shifted.
The recorder prints a dotted line labeled +20 across the FHR scale, to identify the trace for FHR2. The
FHR trace is labeled +20 every 5 cm:
The label for FHR2 is annotated with a black filled +20:
The following trace shows trace separation switched on.
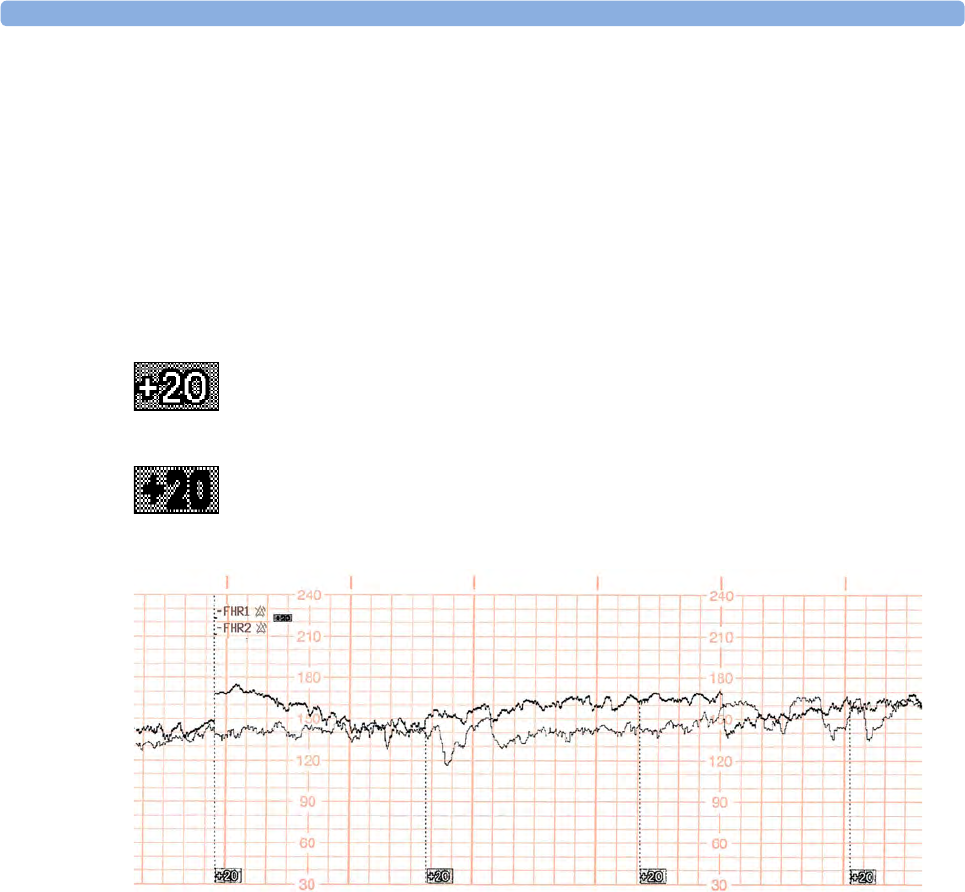
12 Monitoring Twin FHRs
175
Only the FHR2 trace is offset. The numerical FHR value displayed on the monitor remains
unchanged. Subtract 20 from the recorded trace for FHR2 to obtain the true FHR2 value. For
example, if the recorded trace shows 160, then the true FHR is 140.
"Classic" Separation Order
To make differentiating the traces easier, the trace from the ultrasound transducer connected to the
FHR1 channel is separated from that of FHR2 by 20 bpm. In other words, the trace for FHR1 is
recorded 20 bpm higher than it really is. The trace for FHR2 is never shifted.
The recorder prints a dotted line labeled+20 across the FHR scale, to identify the trace for FHR1. The
FHR trace is labeled +20 every 5 cm:
The label for FHR1 is annotated with a black filled +20:
The following trace shows trace separation switched on.
Only the FHR1 trace is offset. The numerical FHR value displayed on the monitor remains
unchanged. Subtract 20 from the recorded trace for FHR1 to obtain the true FHR1 value. For
example, if the recorded trace shows 160, then the true FHR is 140.
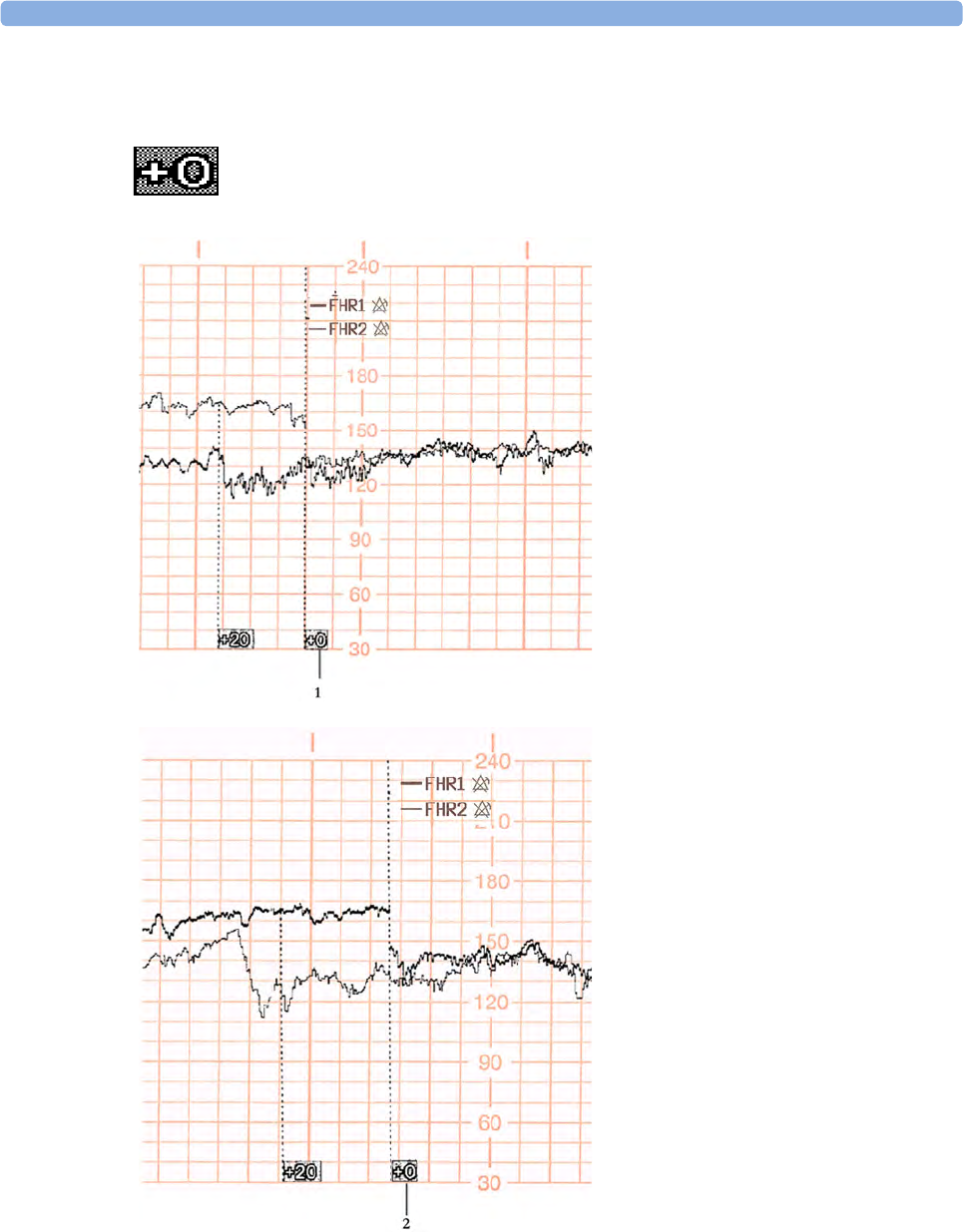
12 Monitoring Twin FHRs
176
When Trace Separation is Off
To indicate that trace separation is switched off, a dotted line labeled +0 prints across the FHR scale.
1Standard trace separation switched
off here
2Classic trace separation switched off
here
12
177
Troubleshooting
Common problems that may occur when monitoring FHR using ultrasound are listed in “Monitoring
FHR and FMP Using Ultrasound” on page 155. See also “Monitoring FHR Using DECG” on
page 195 for common problems you might encounter when monitoring FHR directly.
The following problem may occur when monitoring twins.
For more information, see “Additional Information” on page 163.
Problem Possible Cause Solution
The question mark is
printed repeatedly, and
appears on the screen and
the INOP Coincidence is
issued.
Both transducers are recording the
same FHR, or one fetal transducer is
recording the MHR.
Reposition an ultrasound
transducer. See “Recommended
Actions for INOP Coincidence” on
page 154.

12 Monitoring Twin FHRs
178
13 Monitoring Triple FHRs
179
13Monitoring Triple FHRs
If your monitor is equipped with the triplets option, it carries the label.
You can monitor triple FHRs externally using three ultrasound transducers. With the Avalon CL
Transducer system you can now monitor triplets with cableless transducers. The Avalon CTS system
does not have this option.
Refer to the appropriate preceding chapters for contraindications, and more information about the
available measurement methods.
FHR detection by the monitor may not always indicate that the fetuses are alive. Confirm fetal life
before monitoring, and continue to confirm that the fetuses are the signal source for the recorded fetal
heart rates. See “Confirm Fetal Life Before Using the Monitor” on page 10 and “Cross-Channel
Verification (CCV)” on page 149.
Important Considerations
• The procedures and any contraindications that apply for twins monitoring also apply for
monitoring triplets. In addition, when monitoring triplets: Be aware that monitoring three FHRs is
inherently more difficult than monitoring single or twin FHRs. The nature of the application
increases the likelihood that a fetal heart rate is monitored by more than one transducer.
• Ensure that you are recording three different fetal heart rates. Pay particular attention to any
coincidence of heart rates detected by the monitor's cross-channel verification feature.
• Fetal heart rate measurements are labeled in the order in which you plug in the transducers for
those measurements. It does not matter which fetal sensor socket you use, as the monitor allocates
a channel automatically. For instance, the first transducer you connect is automatically allocated a
channel, and the measurement is labeled FHR1, the second is labeled FHR2, and the third FHR3.
If you need to disconnect the transducers measuring the FHR temporarily, with the intention to
continue monitoring after the temporary break (for example, if the mother needs to go to the
bathroom), it is important that you reconnect the transducers in the same order as you originally
connected them to make sure the measurement labels remain consistent.
Upon discharge of the patient all connected transducers are reset from left to right. Example: Only
one transducer is still connected to the monitor, it was labeled FHR2 while monitoring the previous
discharged patient; it is now reset to FHR1.
• The transducer Finder LED lets you identify at a glance which transducer is monitoring which
heart rate channel.
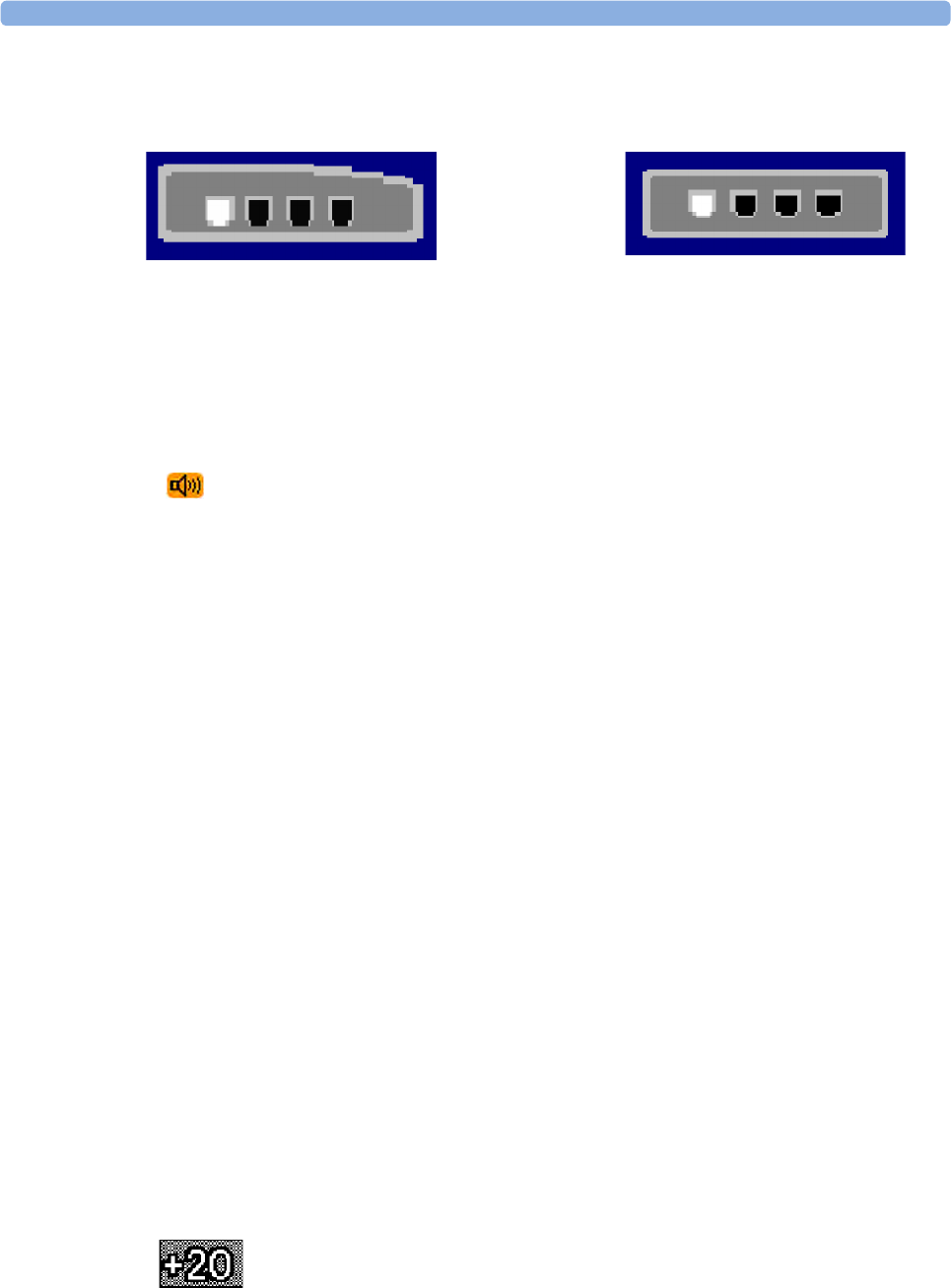
13 Monitoring Triple FHRs
180
• The fetal sensor socket to which a transducer is connected, is identified by the transducer position
indicator in the blue setup menu header:
• The trace recorded for the FHR3 is thicker (darker) than that recorded for FHR1, which is thicker
than that for FHR2. This ensures that the three heart rates are easily distinguishable. The thickness
of the recorded trace can be changed in Configuration Mode.
• Remember that only one fetal heartbeat can be heard from the loudspeaker at any time. The audio
source symbol shows you which fetus you are listening to. To hear the other fetal heartbeat, select
the fetal heart rate sound for this channel (see “Selecting Fetal Heart Sound” on page 158).
• Monitor maternal pulse to avoid mistaking maternal heart rate for FHR.
• Ensure you are recording the best possible signals by referring to the signal quality indicators and
repositioning the transducers if necessary.
For the Avalon CL transducer system see “Cableless Monitoring - Important Considerations” on
page 156.
Monitoring Triplets
To monitor triple FHRs you need three ultrasound transducers. Follow the procedures described in
“Monitoring FHR and FMP Using Ultrasound” on page 155 and in “Monitoring Twin FHRs” on
page 171. The transducer Finder LED lets you identify at a glance which transducer is monitoring
which heart rate channel.
Separating FHR Traces
To help you to interpret traces with similar baselines, you can separate the baselines by an offset of
20 bpm by switching trace separation on. For details of the offset, see “Separation Order Type” on
page 174.
"Standard" Separation Order
To make differentiating the traces easier, the trace for FHR2 is offset by +20 bpm, and the trace for
FHR3 is offset by -20 bpm. In other words, the trace for FHR2 is recorded 20 bpm higher than it
really is, while the trace for FHR3 is recorded 20 bpm lower than it really is. The trace for FHR1 is
never shifted.
FM20/FM30 FM40/FM50
The recorder prints a dotted line labeled +20 across the FHR scale, to identify the
trace for FHR2.
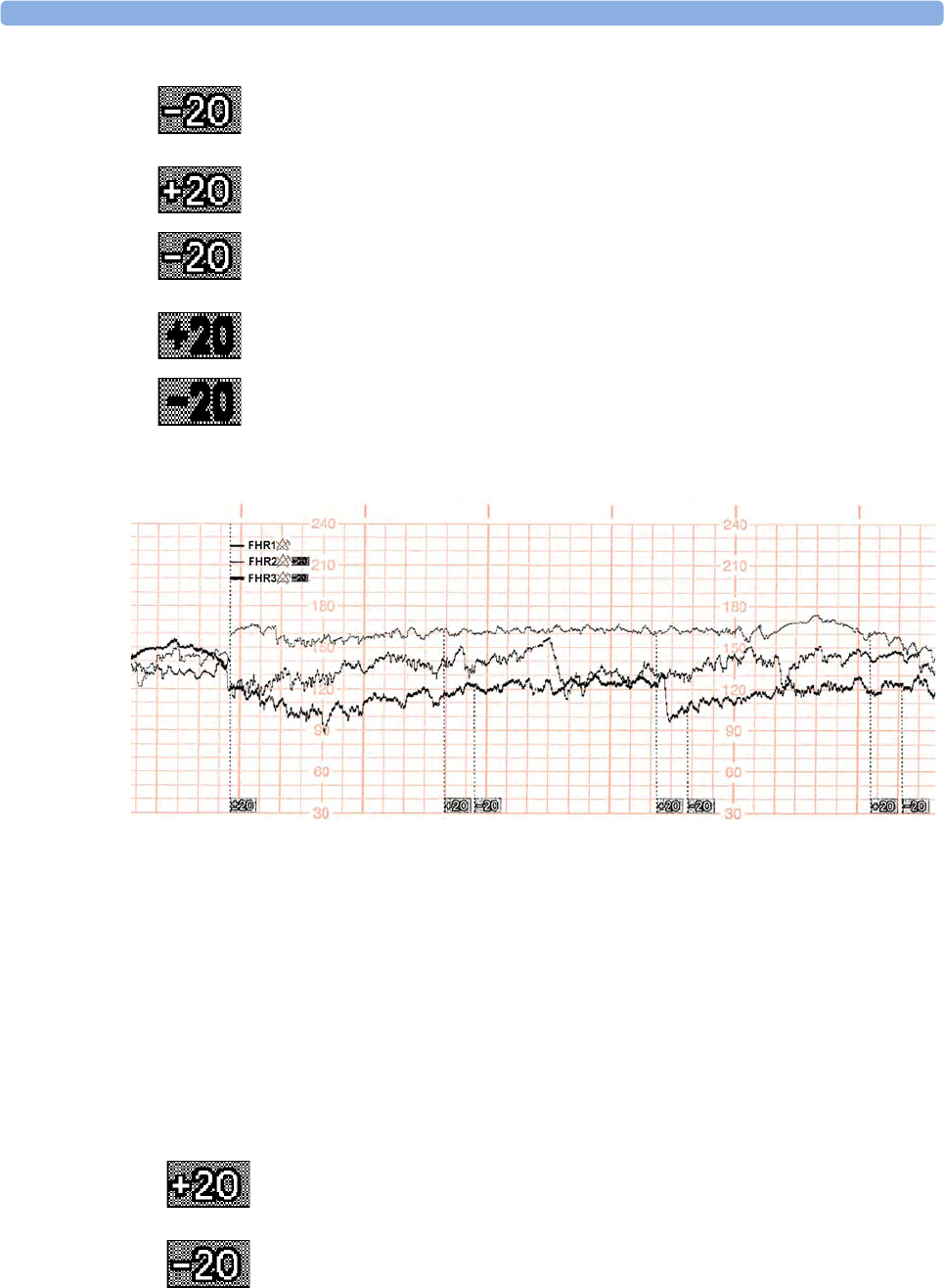
13 Monitoring Triple FHRs
181
The following trace shows triplets with Trace Separation on, and using Standard separation order.
The traces for FHR2 and FHR3 are offset. The numerical FHR values displayed on the monitor
remain unchanged. Subtract 20 from the recorded trace for FHR2 to obtain the true FHR2. For
example, if the recorded trace shows 160, then the true FHR is 140. Similarly, add 20 to the recorded
trace for FHR3 to obtain the true FHR3.
"Classic" Separation Order
To make differentiating the traces easier, the trace for FHR1 is offset by +20 bpm, and the trace for
FHR3 is offset by -20 bpm. In other words, the trace for FHR1 is recorded 20 bpm higher than it
really is, while the trace for FHR3 is recorded 20 bpm lower than it really is. The trace for FHR2 is
never shifted.
The recorder prints a dotted line labeled -20 across the FHR scale, to identify the
trace for FHR3.
The FHR trace is labeled every 5 cm.
The label for FHR2 is annotated with +20 and the FHR3 label is annotated with -
20.
The recorder prints a dotted line labeled +20 across the FHR scale, to identify the
trace for FHR1.
The recorder prints a dotted line labeled -20 across the FHR scale, to identify the
trace for FHR3.

13 Monitoring Triple FHRs
182
The following trace shows triplets with Trace Separation on, and using Classic separation order.
The traces for FHR1 and FHR3 are offset. The numerical FHR values displayed on the monitor
remain unchanged. Subtract 20 from the recorded trace for FHR1 to obtain the true FHR1. For
example, if the recorded trace shows 160, then the true FHR is 140. Similarly, add 20 to the recorded
trace for FHR3 to obtain the true FHR3.
Switching Trace Separation On and Off
1Connect three ultrasound transducers to the monitor to measure FHR.
2See “Switching Trace Separation On and Off ” on page 173 for details of how to switch trace
separation on or off.
When Trace Separation is On
When trace separation is turned on, the recorder prints a dotted line labeled with the three FHRs at the
top, and ±20 at the bottom. Examples of the two methods (Standard, Classic) for determining the
trace separation order are provided here.
The FHR trace is labeled every 5 cm.
The label for FHR1 is annotated with +20 and the FHR3 label is annotated with -
20.
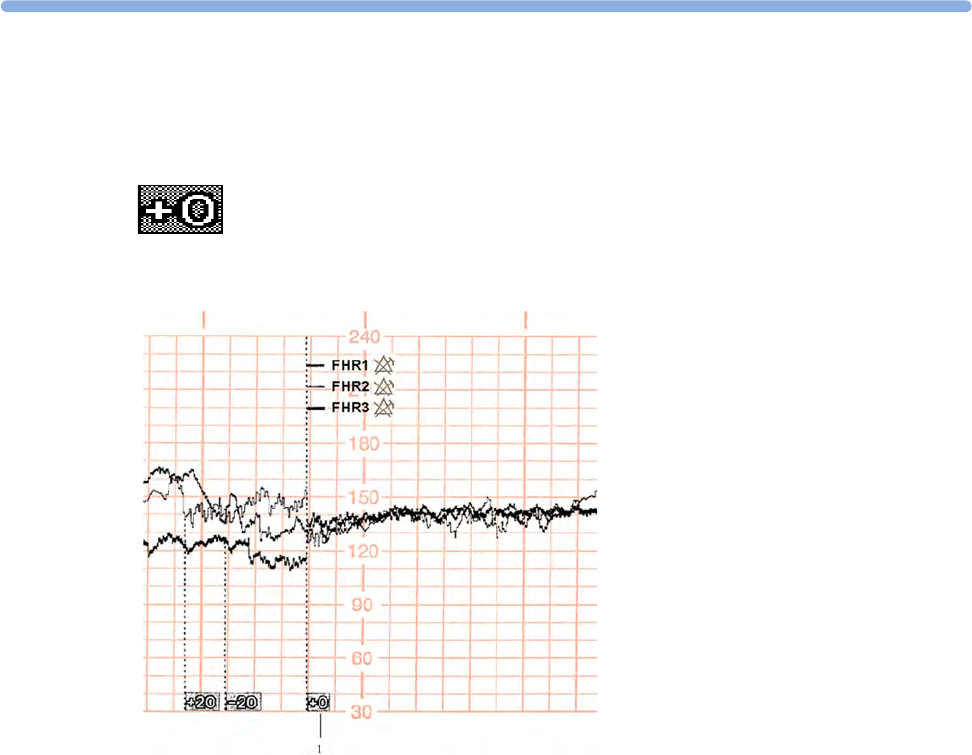
13
183
When Trace Separation is Off
To indicate that trace separation is switched off, a dotted line labeled +0 prints across the FHR scale.
1Standard trace separation
switched off here
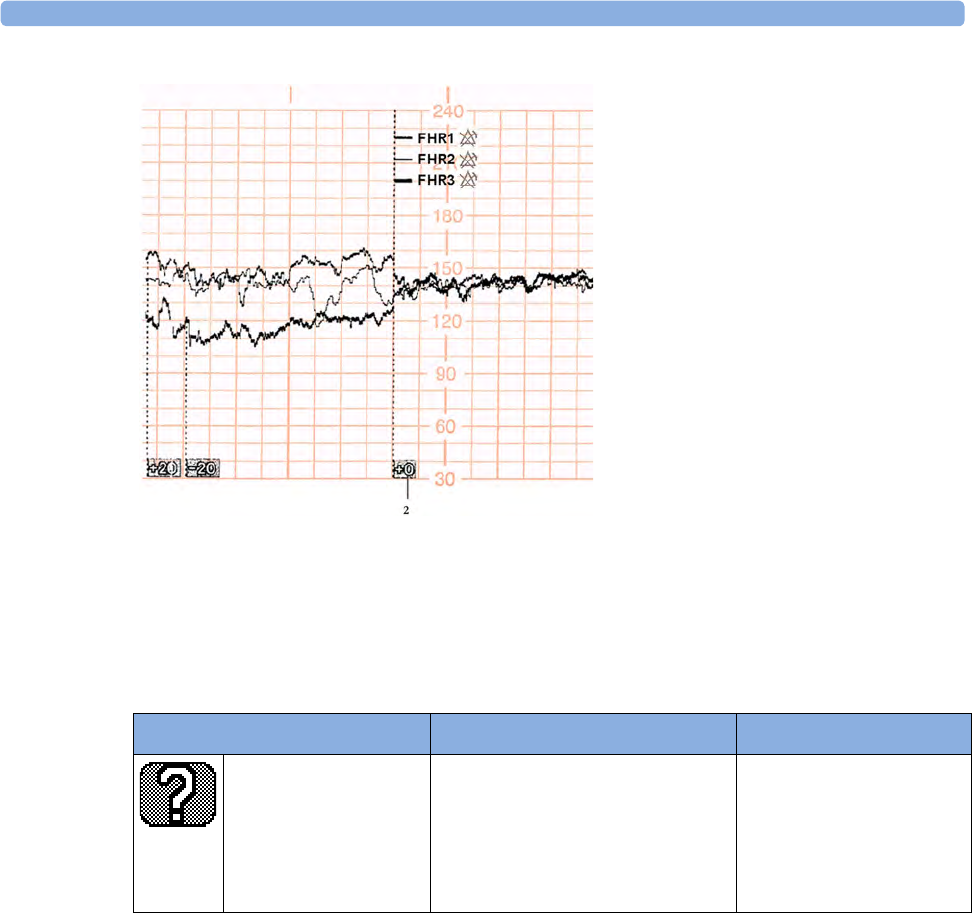
13 Monitoring Triple FHRs
184
Troubleshooting
Common problems that may occur when monitoring FHR using ultrasound are listed in “Monitoring
FHR and FMP Using Ultrasound” on page 155.
The following problem may occur when monitoring triplets.
For more information, see “Additional Information” on page 163.
2Classic trace separation switched
off here
Problem Possible Cause Solution
The question mark is
printed repeatedly, and
appears on the screen
and the INOP
Coincidence is issued.
More than one transducer is
recording the same FHR, or a fetal
transducer records the same heart
rate as the MHR.
Reposition one or more
ultrasound transducer, as
appropriate. See
“Recommended Actions
for INOP Coincidence” on
page 154

14
185
14Fetal Heart Rate Alarms
Fetal heart rate (FHR) alarms can give both audible and visual warning of a non-reassuring fetal
condition. Your monitor must be configured to alarm mode All to enable the FHR alarms (see
“Alarms” on page 109).
Changing Alarm Settings
When you do any of the following actions for any FHR measurement channel, this applies for all active
FHR measurements, both ultrasound and DECG:
• Turning FHR alarms on or off.
• Changing alarm limits.
• Changing alarm delays.
• Changing signal loss delay.
The monitor retains these settings, even when switched off. The alarm limits are printed on the trace
every few pages if alarms are on.
Turning Alarms On or Off
1Connect either an ultrasound or a DECG transducer to a free socket on the monitor.
2Enter the Setup menu for a connected FHR measurement.
3Select Alarms to toggle between On and Off.
Changing Alarm Limits
1Connect either an ultrasound or a DECG transducer to a free socket on the monitor.
2Enter the Setup menu for a connected FHR measurement.
3To change the high alarm limit, select High Limit and select the alarm limit from the pop-up list.
4To change the low alarm limit, select Low Limit and select the alarm limit from the pop-up list.
Changing Alarm Delays
You can change the alarm delays if the Alarm Mode is set to All.
1Connect either an ultrasound or a DECG transducer to a free socket on the monitor.
2Enter the Setup menu for a connected FHR measurement.

14 Fetal Heart Rate Alarms
186
3To change the high alarm limit delay time, select High Delay and select the delay time (in seconds)
from the pop-up list.
4To change the low alarm limit delay time in seconds, select Low Delay and select the delay time (in
seconds) from the pop-up list.
Changing Signal Loss Delay
The signal loss delay is the configurable delay before a Signal Loss INOP is issued. You can change
the delay:
1Connect either an ultrasound or a DECG transducer to a free socket on the monitor.
2Enter the Setup menu for a connected FHR measurement.
3Select SignalLoss Delay and select the signal loss INOP delay time (in seconds) from the pop-up
list.
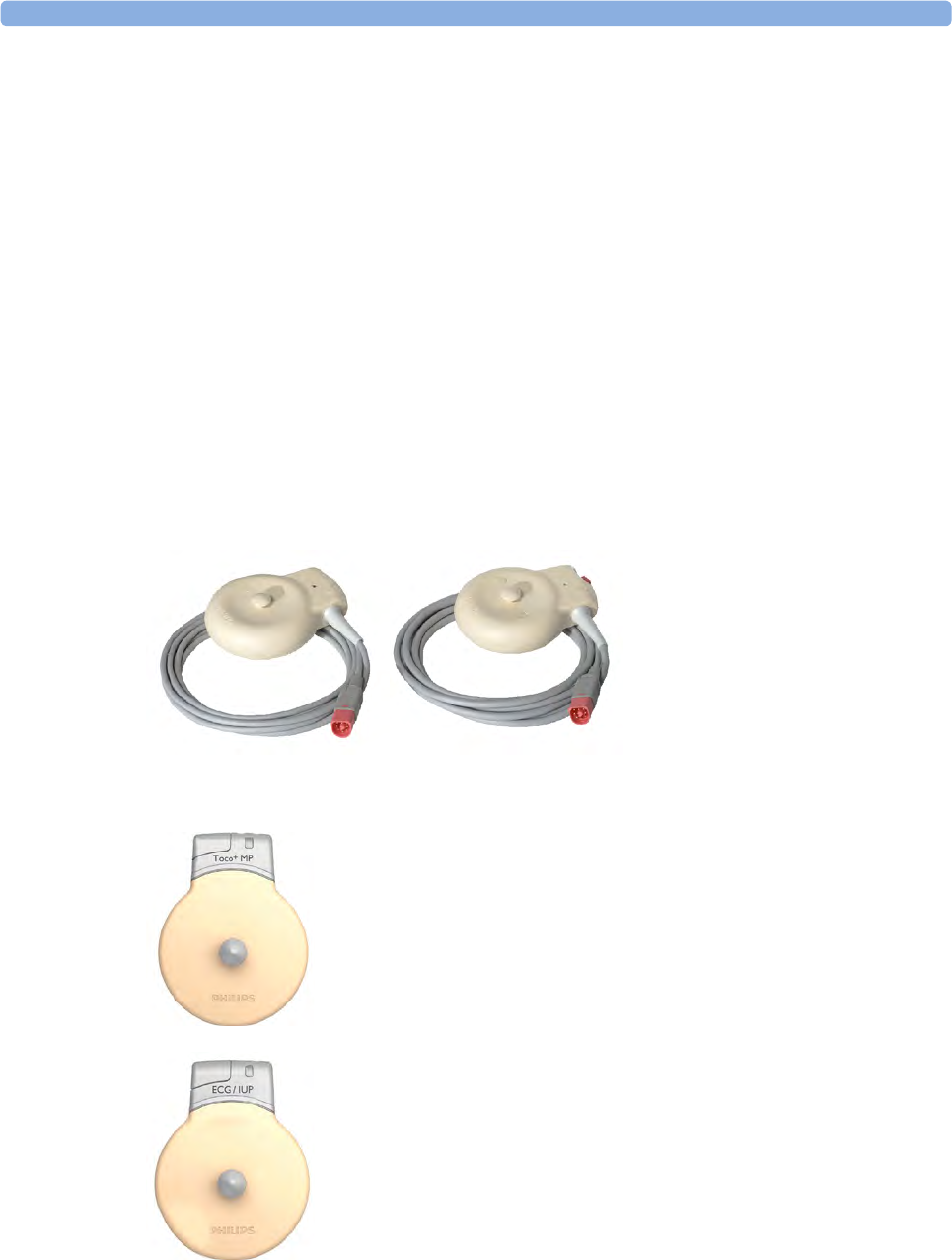
15 Monitoring Uterine Activity Externally
187
15Monitoring Uterine Activity
Externally
You can measure uterine activity externally using a Toco transducer. You can also use a Toco+,
Toco MP, or a CL Toco+MP transducer for the same purpose, although they also have more (ECG/
IUP and Pulse) capabilities.
The external Toco transducer measures the frequency, duration and relative strength of contractions,
but not their absolute intensity. Amplitude and sensitivity depend on various factors such as the
position of the transducer, the belt tension and the size of the patient.
What You Need
Toco, Toco MP, or Toco+ transducer
CL Toco+MP transducers (additionally capable of providing the
maternal pulse measurement)
CL ECG/IUP transducer
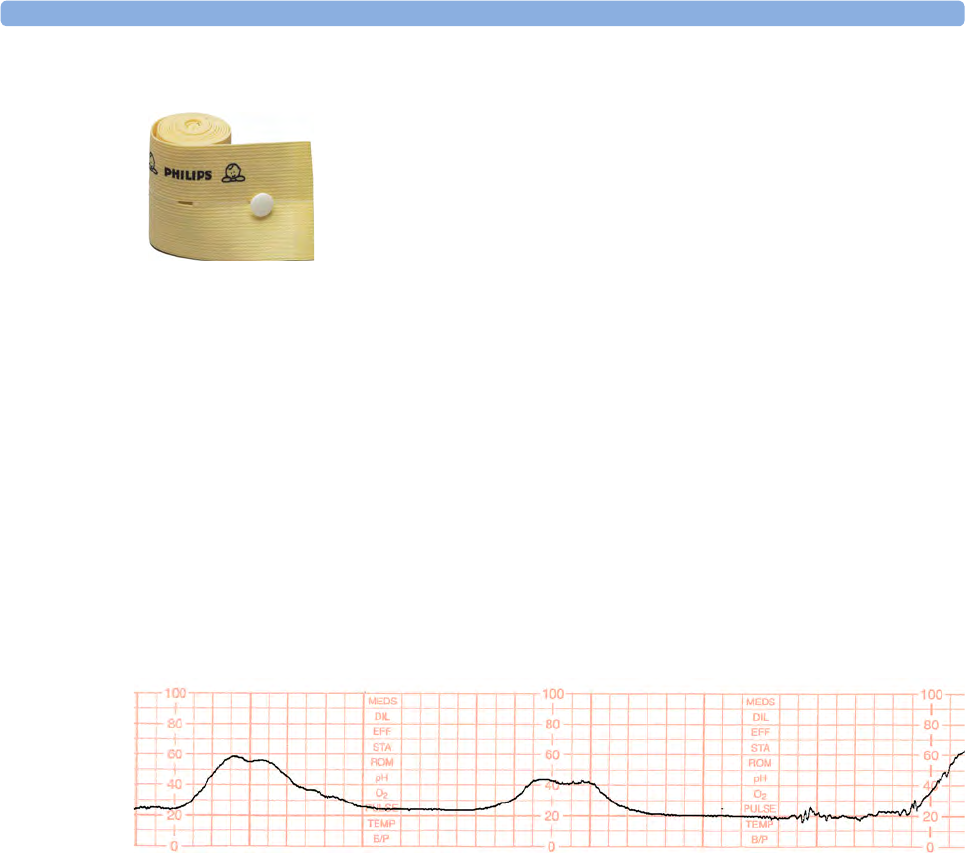
15 Monitoring Uterine Activity Externally
188
External Toco Monitoring
Prepare for Toco monitoring using the list below. The standard procedures in use in your facility
determine the sequence of actions.
1Fasten the abdominal transducer belt around the patient.
2Connect the Toco transducer to a free socket on the monitor. The Toco baseline is automatically
reset. The Toco display shows 20. "Toco", indicating external uterine measurement, is printed on
the trace at intervals.
3Place the transducer on the patient's fundus to ensure the optimum recording of uterine activity.
4Reset the Toco baseline as necessary (see “Resetting the Toco Baseline” on page 188), but not
during a contraction.
The following example trace shows two contractions.
Resetting the Toco Baseline
1Press the Toco Baseline SmartKey. This resets the Toco baseline to 20 on the display and trace.
2If the Toco value is negative for more that five seconds, the Toco baseline is automatically reset to
0 units.
Toco Sensitivity
If the Toco sensitivity is too high, and the Toco trace exceeds the paper scale, you can reduce the Toco
sensitivity to 50%. The default setting is 100%.
To change the Toco sensitivity:
1Enter the Setup Toco menu.
2Select Gain to toggle between 100% and 50%.
Abdominal Belt (disposable shown)
15
189
Troubleshooting
Testing Toco Transducers
If any of the following tests fail, repeat the test using another transducer. If the second transducer
passes the tests, confirming that the first transducer is defective, contact your service personnel.
External Toco Monitoring
Problem Possible Causes Solutions
Quality of the trace deteriorates
or the Toco baseline varies
The belt is incorrectly fastened and is
too slack or too tight, or the belt has lost
its elasticity.
The belt must be tight enough to ensure
good contact between the patient's skin
and the entire surface of the transducer
without causing discomfort. Ensure you
are using the correct belt. Adjust it as
necessary.
Fetal movement Check if the belt is correctly fastened
and adjust it as necessary. Reposition the
transducer and reset the Toco baseline if
necessary.
Maternal respiration superimposed on
trace
Check if belt is not too loose.
Maternal movement/change of position Following maternal movement, reset
Toco baseline
Toco sensitivity is too high
(above 100 units)
Toco trace is exceeding the paper
scale
Physical transmission of pressure from
the uterus to the sensor is much higher
than the average value.
Check if the belt is too tightly fastened.
Select 50% Toco sensitivity.
Toco Equip Malf is displayed. See “Patient Alarms and INOPs” on
page 121.
Toco Unplugged is displayed. See “Patient Alarms and INOPs” on
page 121.
If you suspect the signal from the transducer. Test the Transducer (see “Testing Toco
Transducers” on page 189 below).

15 Monitoring Uterine Activity Externally
190
If the second transducer also fails the tests, contact your service personnel.
You can test all Toco transducers, including the cableless ones, as described above.
To test a Toco transducer:
1Switch on the monitor and the
recorder.
2Connect the transducer to the fetal
monitor.
3Gently apply pressure to the pick-
up button.
4Check if after a few seconds the
values on the display and paper
show this change in pressure.
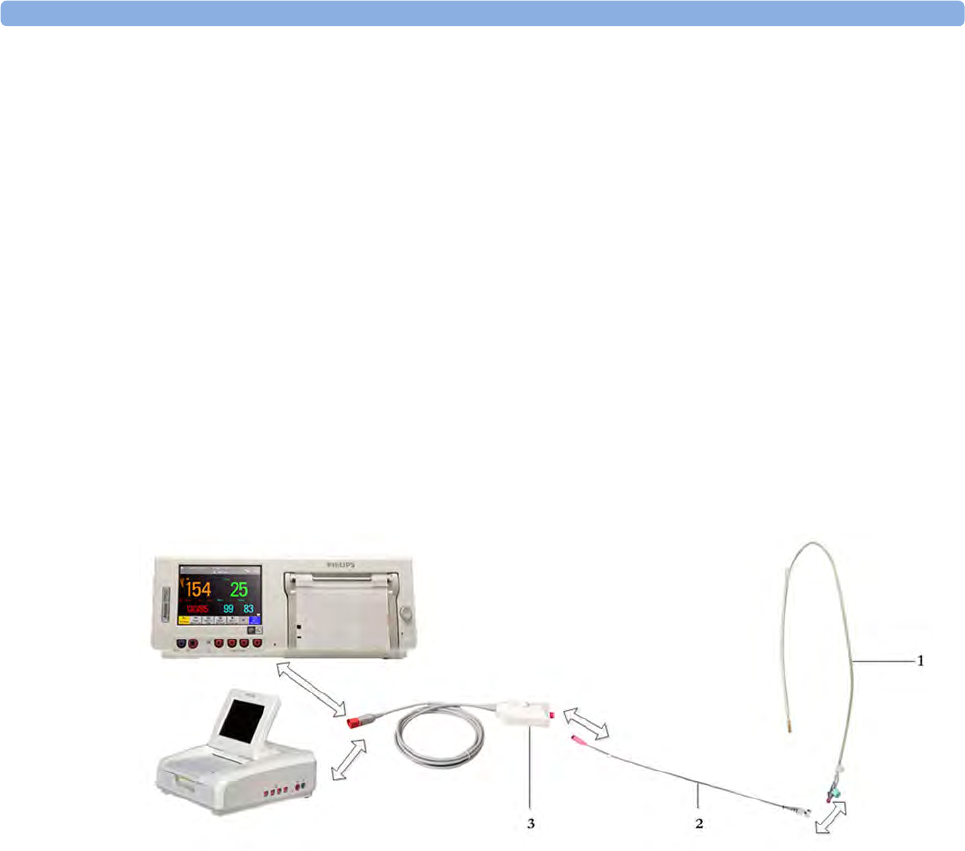
16 Monitoring Uterine Activity Internally
191
16Monitoring Uterine Activity
Internally
FM30/50 You can monitor intrauterine pressure (IUP) using an intrauterine catheter together with a patient
module, Toco+, or the CL ECG/IUP transducer, after rupture of the membranes and the cervix is
sufficiently dilated.
What You Need
Illustration 1 shows the complete connection chain from the IUP catheter to the fetal monitor using
the patient module:
1Disposable Koala IUP Catheter (M1333A)
2Reusable Koala IUP Adapter Cable (9898 031 43931)
3Patient Module (M2738A)
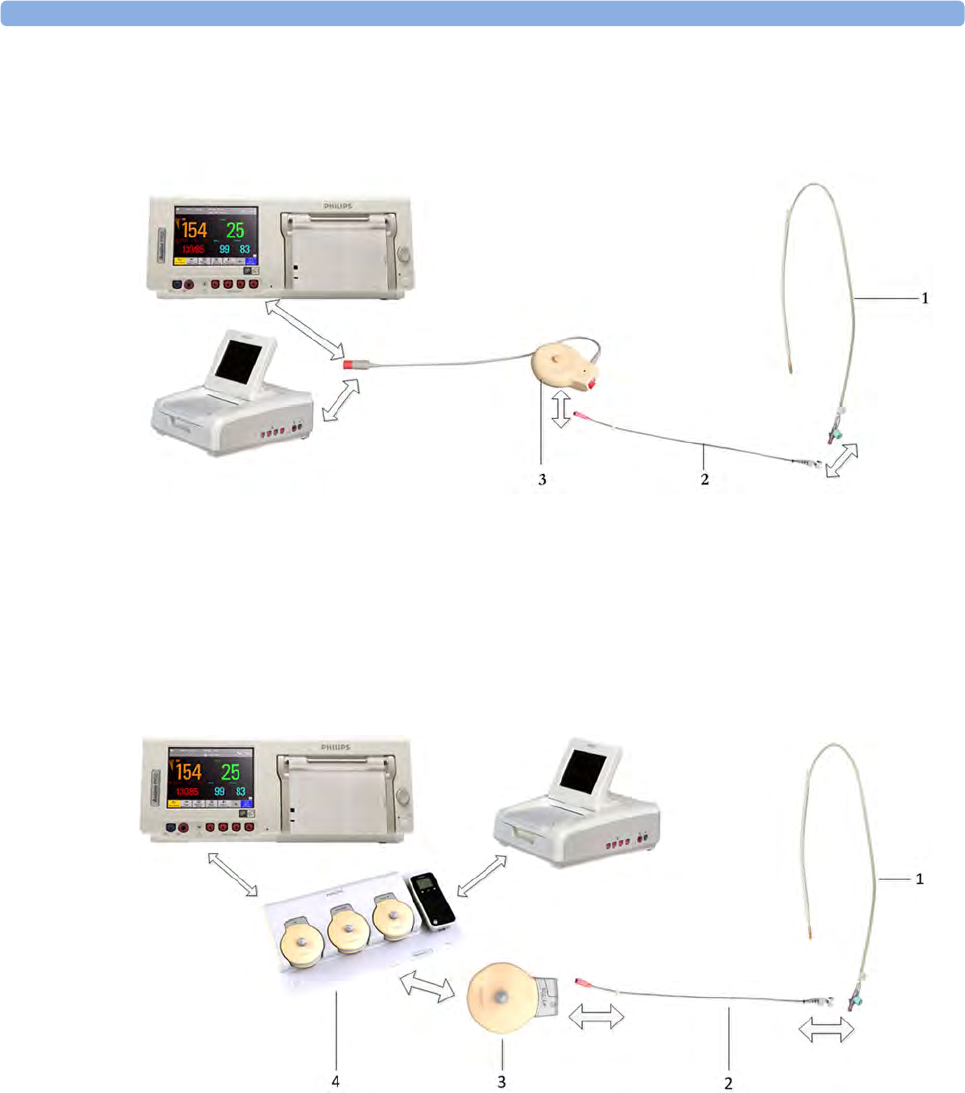
16 Monitoring Uterine Activity Internally
192
Illustration 2 shows the complete connection chain from the IUP catheter to the fetal monitor using
the Toco+ transducer:
Illustration 3 shows the complete connection chain from the IUP catheter to the fetal monitor using
the CL ECG/IUP transducer:
1Disposable Koala IUP Catheter (M1333A)
2Reusable Koala IUP Adapter Cable (9898 031 43931)
3Toco+ transducer (M2735A)
1Disposable Koala IUP Catheter (M1333A)
2Reusable Koala IUP Adapter Cable (9898 031 43931)
3CL ECG/IUP transducer (866077)
4Avalon CL base station (866074)
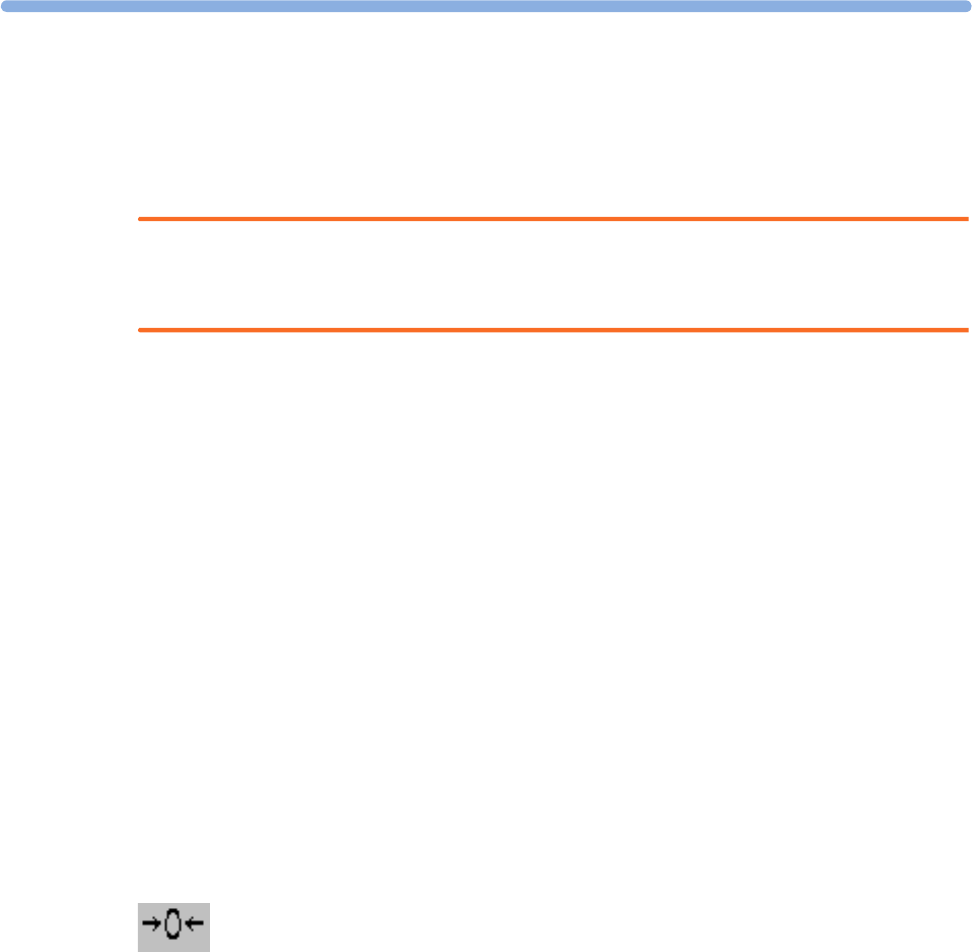
16
193
Internal (IUP) Monitoring
Read the instructions that accompany the intrauterine catheter and the adapter cable before you start
monitoring. Zero the monitor when instructed.
WARNING
Do not catheterize if placenta previa is diagnosed, or if uterine bleeding from an undetermined source
is present.
Prepare for IUP monitoring using the list below. The standard procedures in use in your facility
determine the sequence of actions.
1Perform a complete clinical evaluation.
2Catheterize after membrane rupture. Insert the catheter according to its accompanying
instructions.
3Connect the catheter to the socket on the patient module.
4Connect the patient module to a free socket on the monitor. The monitor is automatically zeroed.
The IUP display shows 0. "IUP", indicating internal measurement, is printed at intervals on the
trace.
5Zero the monitor (see “Zeroing the Monitor” on page 193).
6If you suspect the catheter is not responding appropriately, flush as directed in the catheter's
Instructions for Use. A pressure spike appears on the trace if you flush after connecting the
transducer to the monitor.
Zeroing the Monitor
Zero the monitor by selecting the Zero IUP SmartKey, or selecting Zero IUP in the Setup IUP menu.
This resets the display and trace to 0. If you do not zero the monitor properly, the pressure trace may
exceed the paper scaling.
Selecting the IUP Unit
You can select between mmHg (default) and kPa for the IUP unit.
1Enter the Setup IUP menu.
2Press Unit to toggle between mmHg and kPa.
16 Monitoring Uterine Activity Internally
194
Troubleshooting
Internal (IUP) Monitoring
Problem Possible Causes Solutions
No change in pressure during
contraction.
Dry environment or possible extra-
ovular placement of sensor tip.
Refer to catheter Instructions for Use.
Only pressure peaks can be
seen (baseline not visible).
Zero adjustment is incorrect. Zero the system.
Trace is a straight line. Transducer is defective. Remove and touch the catheter. If the trace
does not show up and down movements, use a
new transducer.
Catheter blocked. Refer to catheter Instructions for Use.
Trace is superimposed with
noise.
End of catheter is in the uterine wall. Refer to catheter Instructions for Use.
IUP Equip Malf INOP is displayed. See “Patient Alarms and INOPs” on
page 121.
IUP Unplugged INOP is displayed.

17 Monitoring FHR Using DECG
195
17Monitoring FHR Using DECG
FM30/50 This chapter describes how to monitor a single fetal heart rate via direct ECG (DECG), using a spiral
fetal scalp electrode in the intrapartum period.
Read and adhere to the instructions that accompany the fetal scalp electrode, the DECG
adapter cable, and the attachment electrode. Pay attention to all the contraindications,
warnings, and for the DECG adapter cable, the cleaning and disinfection procedures.
Before starting to monitor, first define the fetal position, and ensure that it is suitable for DECG
monitoring.
Misidentification of MHR as FHR
Confirm fetal life before monitoring, and continue to confirm that the fetus is the signal source for the
FHR during monitoring. Here are two examples where the MHR can be misidentified as the FHR
when using a fetal scalp electrode:
• Electrical impulses from the maternal heart can sometimes be transmitted to the fetal monitor
through a recently deceased fetus via the spiral scalp electrode, appearing to be a fetal signal
source.
• The recorded MHR, and any artifact, can be misinterpreted as a FHR especially when it is over
100 bpm.
To reduce the possibility of mistaking the MHR for FHR, monitor both maternal and fetal heart rates
(see “Monitoring Maternal Heart / Pulse Rate” on page 223). The monitor's cross-channel verification
(CCV) facility can help by automatically detecting when the same heart rate is being recorded by
different transducers. See “Confirm Fetal Life Before Using the Monitor” on page 10 and “Cross-
Channel Verification (CCV)” on page 149.
If the Coincidence INOP is issued at the fetal monitor if you are measuring FHR with DECG:
1Confirm that the scalp electrode is placed correctly.
2Confirm fetal life by palpation of fetal movement or auscultation of fetal heart sounds using a
fetoscope, stethoscope, or Pinard stethoscope.
3If you cannot hear the fetal heart sounds, and you cannot confirm fetal movement by palpation,
confirm fetal life using obstetric ultrasonography.
4In case of difficulties deriving a stable maternal pulse reading using the Toco MP or CL Toco+MP
transducer, use SpO2 instead. In case of similar problems with the pulse measurement from SpO2,
use MECG instead. Reasons to switch the method for deriving a maternal pulse or heart rate
include: motion artifacts, arrhythmia, and individual differences in pulse signal quality on the
abdominal skin (via Toco+MP).
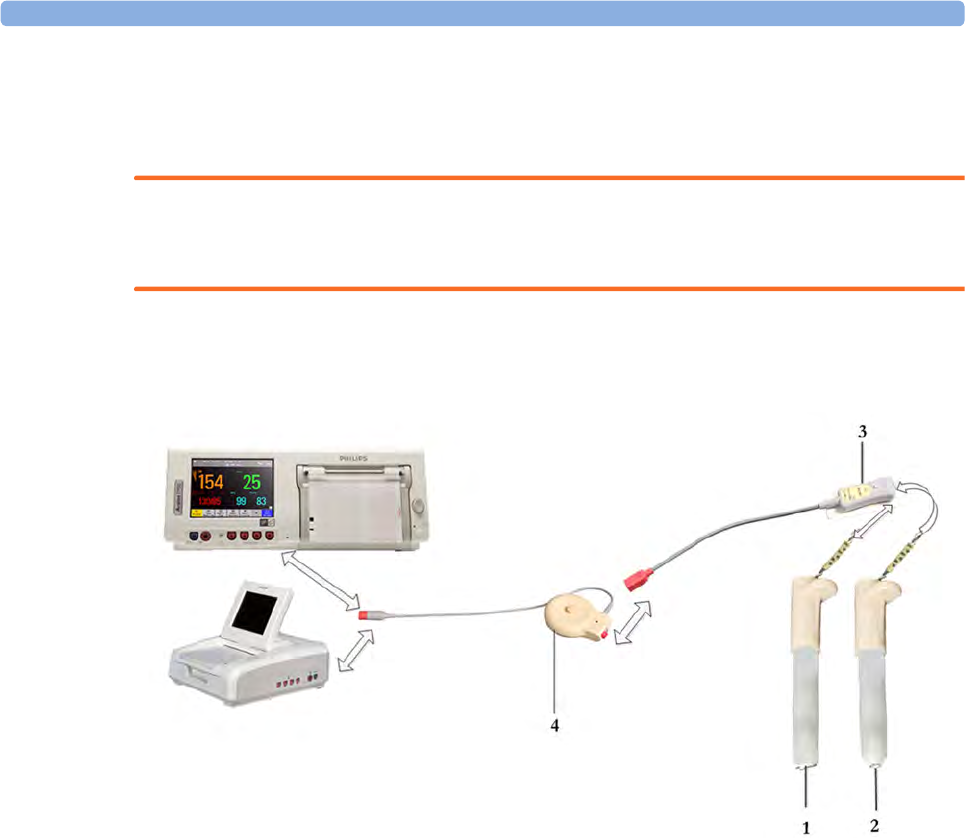
17 Monitoring FHR Using DECG
196
What You Need
You can measure fetal DECG using the equipment combinations shown in the following illustrations.
WARNING
Never attempt to connect the fetal scalp electrode to anything other than the correct DECG adapter
cable.
Illustration 1 shows the complete connection chain from the fetal scalp electrode to the fetal monitor
using the Toco+ transducer.
1Fetal Scalp Electrode, single spiral (9898 031 37631)
2Fetal Scalp Electrode, double spiral, Europe only, not for USA (9898 031 37641)
3DECG Adapter Cable (9898 031 37651) with Pre-gelled Attachment Electrode (9898 031
39771)
4Toco+ transducer (M2735A)
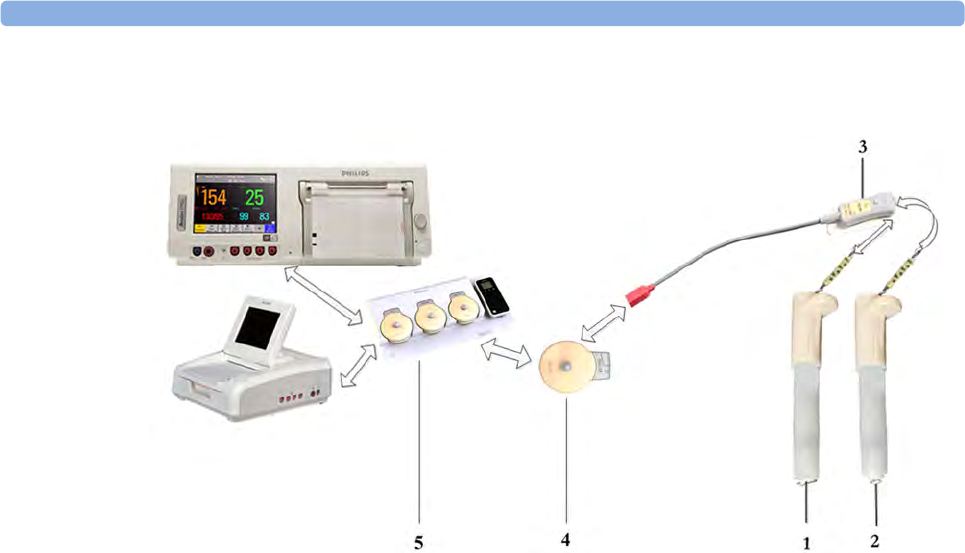
17 Monitoring FHR Using DECG
197
Illustration 2 shows the equivalent chain using the CL Toco+MP or CL ECG/IUP transducer.
1Fetal Scalp Electrode, single spiral (9898 031 37631)
2Fetal Scalp Electrode, double spiral, Europe only, not for USA (9898 031 37641)
3DECG Adapter Cable (9898 031 37651) with Pre-gelled Attachment Electrode (9898 031
39771)
4CL Toco+MP or CL ECG/IUP transducer (866077)
5Avalon CL base station (866074)
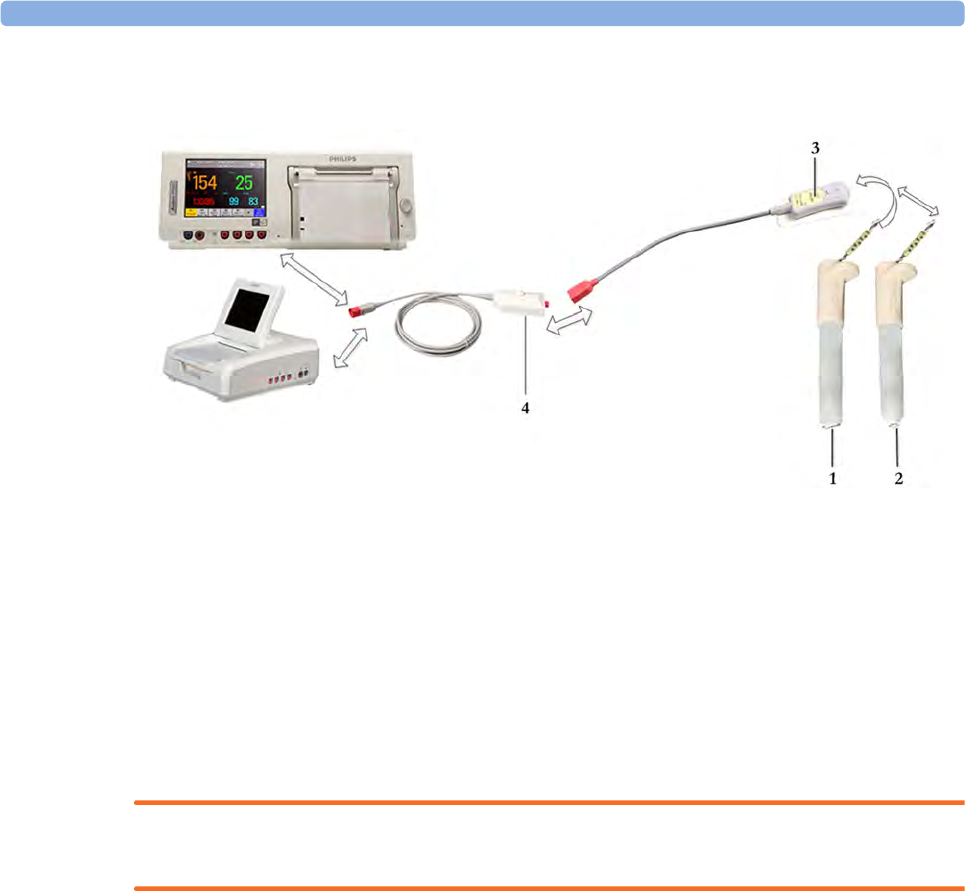
17 Monitoring FHR Using DECG
198
Illustration 3 shows the equivalent chain using the patient module.
Making Connections
WARNING
Follow the instructions supplied with each of the monitoring accessories you are using.
Prepare for DECG monitoring using the list below. The standard procedures in use in your facility
determine the sequence of actions.
1If changing monitoring mode from US to DECG, first disconnect the US transducer.
2Depending on the equipment you are using, ensure that the Toco+ transducer, CL Toco+MP, the
CL ECG/IUP transducer, or the patient module is connected to the fetal monitor.
3Attach the fetal scalp electrode to the fetus, following the instructions supplied with the fetal scalp
electrode.
4Attach a pre-gelled attachment electrode to the DECG adapter cable, following the instructions
supplied with the DECG adapter cable.
5Fix the attachment electrode to the mother's thigh, following the instructions supplied with the
attachment electrode.
Depending on the equipment you are using, connect the red connector plug on the DECG
adapter cable to the red connector on the Toco+ transducer, CL Toco+MP, the CL ECG/IUP
transducer, or the patient module.
6Connect the fetal scalp electrode to the DECG adapter cable.
1Fetal Scalp Electrode, single spiral, (9898 031 37631)
2Fetal Scalp Electrode, double spiral, Europe only, not for USA (9898 031 37641)
3DECG Adapter Cable (9898 031 37651) with Pre-gelled Attachment Electrode (9898 031
39771)
4Patient Module (M2738A)
17 Monitoring FHR Using DECG
199
You are now ready to begin monitoring DECG.
WARNING
The fetal/maternal monitor is not a diagnostic ECG device. In particular, the display of fetal/maternal
ECG is intended only for evaluating signal quality for fetal/maternal heart rate as derived from the
ECG waveform.
When in doubt, it can be used to identify sources of compromised signal quality, such as noise or
muscle artifacts. It can subsequently be used to verify the result of measures taken to resolve them (e.g.
checking ECG cable connections or adapting the fetal ArtifactSuppress configuration).
The safety and effectiveness of the displayed fetal/maternal ECG waveform (i.e. P, QRS and T
segments) for evaluation of fetal/maternal cardiac status during labor have not been evaluated.
Monitoring DECG
To simultaneously measure DECG and MECG, you need the CL ECG/IUP transducer or the patient
module for DECG, and a Toco+, CL Toco+MP, or CL ECG/IUP transducer for MECG (see
“Monitoring Maternal Heart / Pulse Rate” on page 223). Alternatively, you can monitor the maternal
pulse rate via pulse oximetry (see “Pulse Rate from SpO2” on page 230). You can also monitor
maternal pulse with the Toco MP or CL Toco+MP transducer. In any case where you would use a
Toco+ or Toco MP transducer, you can also monitor with a CL Toco+MP transducer.
1Switch on the recorder.
2The heart rate monitored via DECG is labeled DFHR1 / DFHR2 / DFHR3 on the screen. If
configured, the DECG wave is displayed automatically on the screen, labeled DECG and fetal. If
MECG is being monitored, both waves are displayed, with the DECG wave above the MECG
wave. The MECG wave is labeled MECG and maternal.
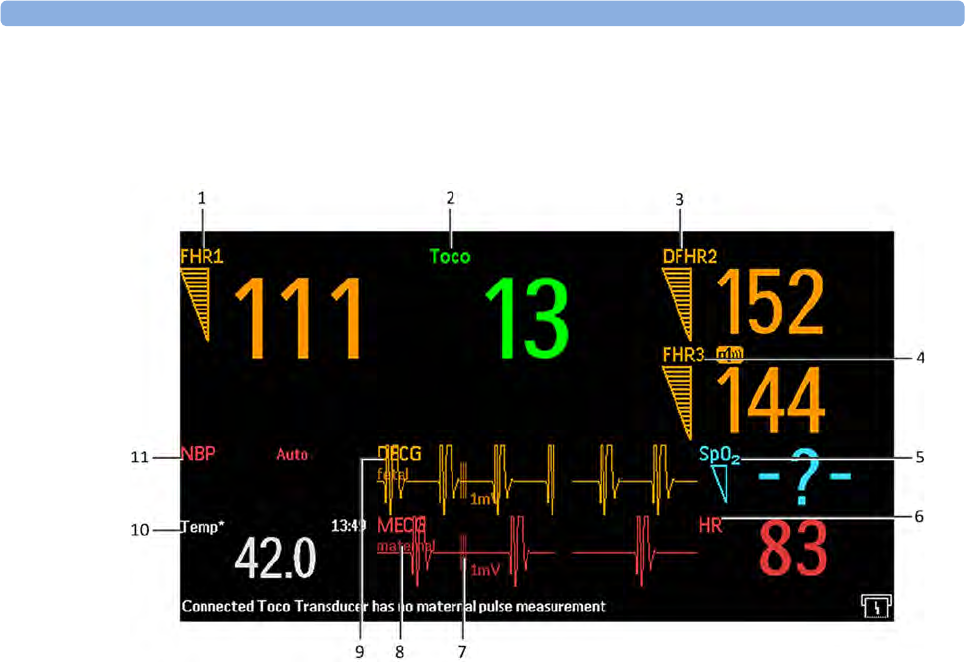
17 Monitoring FHR Using DECG
200
3Check the artifact suppression setting and change it if necessary (see “Suppressing Artifacts” on
page 201).
NOTE
The 1mV scale bar for the DECG and MECG wave is not displayed on the screen if you monitor
DECG or MECG with an Avalon CTS system. The Avalon CTS system does not provide a scaled
ECG.
1Measurement label (FHR1)
2Measurement label (Toco)
3Measurement label (DFHR2)
4Measurement label (FHR3)
5Measurement label (SpO2)
6Measurement label (HR)
71mV scale bar
8MECG wave with maternal label
9DECG wave with fetal label
10 Measurement label (Temp) maternal temperature
11 Measurement label NBP
17
201
WARNING
Periodically compare the mother's pulse with the signal coming from the monitor's loudspeaker to
ensure that you are monitoring fetal heart rate. If the MHR coincides with the FHR, do not
misinterpret the MHR as the FHR (see also “Confirm Fetal Life Before Using the Monitor” on
page 10 and “Cross-Channel Verification (CCV)” on page 149.
Suppressing Artifacts
When the monitor's artifact suppression is on, instantaneous heart rate changes of 28 bpm or more,
however caused, are not recorded. Fetal arrhythmia will also be suppressed. If you suspect fetal
arrhythmia, switch artifact suppression off. When artifact suppression is off, all recorded fetal
heartbeats within the specified range are shown. The default setting is On (artifacts are suppressed).
To change the setting:
1Enter the Setup DFHR1 menu.
2Select ArtifactSuppress to toggle between artifact suppression On (artifacts are suppressed) and
Off (no artifact suppression, use this setting if you suspect fetal arrhythmia).
When artifact suppression is off, Artifact Suppression Off is annotated on the trace recording.
Printing the Waveform
You can print the DECG wave onto the trace paper. Refer to “Printing the ECG Waveform” on
page 233.
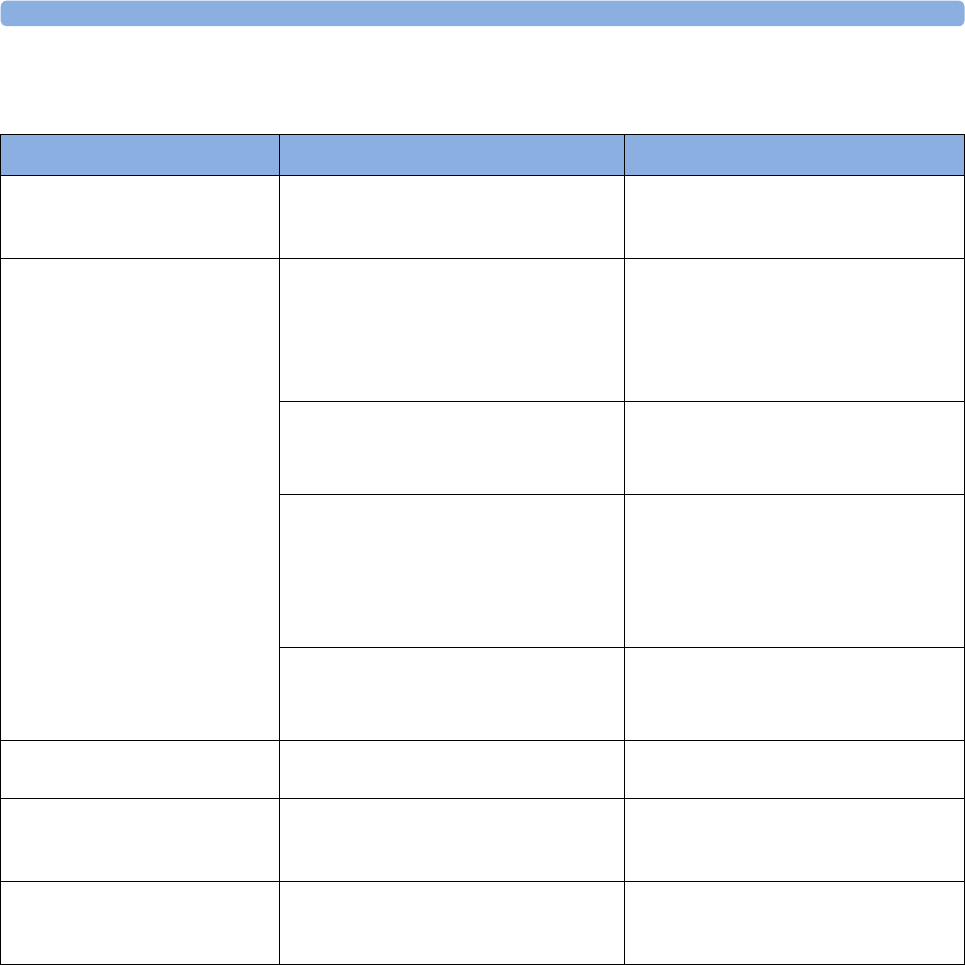
17 Monitoring FHR Using DECG
202
Troubleshooting
Testing DECG Mode
See the monitor's Service Guide.
Problem Possible Cause Solutions
DFHR1 Equip Malf
DFHR2 Equip Malf
DFHR3 Equip Malf
Malfunctioning equipment See “Patient Alarms and INOPs” on
page 121.
DFHR1 Leads Off
DFHR2 Leads Off
DFHR3 Leads Off
Numeric is displayed with a -?-;
INOP tone
See also “Patient Alarms and
INOPs” on page 121.
Erratic trace
Erratic display
Fetal scalp electrode detached at
connector
Reconnect the fetal scalp electrode
If the wave is configured to be displayed
on the monitor, you can observe if the
ECG signal is clear, or if it shows
interruptions and noise
Poor or no contact between leg
attachment electrode and mother
Check all connections
Disconnect and reconnect the connector
several times
No contact between the DECG adapter
cable and the leg attachment electrode
No contact between the fetal scalp
electrode connector and the DECG
adapter cable
Check all connections
Disconnect and reconnect the connector
several times
If problem persists, use a new fetal scalp
electrode
No ECG signal
Poor contact between the reference
electrode and the mother
Check for fetal demise
Use a new fetal scalp electrode if
necessary
Signal quality indicator
continuously shows a poor signal
Fetal arrhythmia Use a new fetal scalp electrode if
necessary
DFHR1 Signal Loss
DFHR2 Signal Loss
DFHR3 Signal Loss
No signal See “Patient Alarms and INOPs” on
page 121.
DFHR1 Unplugged
DFHR2 Unplugged
DFHR3 Unplugged
No connection See “Patient Alarms and INOPs” on
page 121.

18 Monitoring Noninvasive Blood Pressure
203
18Monitoring Noninvasive Blood
Pressure
This fetal monitor uses the oscillometric method for the noninvasive blood pressure measurement. In
adult mode the blood pressure measurements determined with this device comply with the American
National Standard for Electronic or Automated Sphygmomanometers (ANSI/AAMI SP10-1992) in
relation to mean error and standard deviation, when compared to intra-arterial or auscultatory
measurements (depending on the configuration) in a representative sample population. For the
auscultatory reference, the fifth Korotkoff sound was used to determine the diastolic pressure.
A physician must determine the clinical significance of the measurement information.
Introducing the Oscillometric Noninvasive Blood
Pressure Measurement
Oscillometric devices measure the amplitude of pressure changes in the occluding cuff as the cuff
deflates from above systolic pressure. The amplitude suddenly increases as the pulse breaks through
the occlusion in the artery. As the cuff pressure decreases further, the pulsations increase in amplitude,
reach a maximum (which approximates to the mean pressure), and then diminish.
Studies show that, especially in critical cases (arrhythmia, vasoconstriction, hypertension, shock),
oscillometric devices are more accurate and consistent than devices using other noninvasive measuring
techniques.
WARNING
Intravenous infusion: Do not use the NBP cuff on a limb with an intravenous infusion or arterial
catheter in place. This could cause tissue damage around the catheter when the infusion is slowed or
blocked during cuff inflation.
Skin Damage: Do not measure NBP in cases of sickle-cell disease or any condition where skin
damage has occurred or is expected.
Unattended measurement: Use clinical judgment to decide whether to perform frequent unattended
blood pressure measurements in cases of severe blood clotting disorders, because of the risk of
hematoma in the limb fitted with the cuff.
Measurement Limitations
Measurements are impossible with heart rate extremes of less than 40 bpm or greater than 300 bpm, or
if the patient is on a heart-lung machine.
The measurement may be inaccurate or impossible:
• with excessive and continuous patient movement such as during contractions
• if a regular arterial pressure pulse is hard to detect
• with cardiac arrhythmias

18 Monitoring Noninvasive Blood Pressure
204
• with rapid blood pressure changes
• with severe shock or hypothermia that reduces blood flow to the peripheries
• with obesity, where a thick layer of fat surrounding a limb dampens the oscillations coming from
the artery
• on an edematous extremity.
Measurement Methods
There are three measurement methods:
•Manual - measurement on demand. Results are displayed for up to one hour.
•Auto - continually repeated measurements (between one and 120 minute adjustable interval). You
can make a manual measurement between two measurements in Auto Mode.
•Sequence- up to four measurement cycles which will run consecutively, with number of
measurements and interval between them configurable for each cycle.
Reference Method
The measurement reference method can be Auscultatory (manual cuff) or Invasive (intra-arterial). For
further information, see the Application Note supplied on the monitor documentation DVD.
To check the current setting, select Main Setup, Measurements, NBP, and check whether the
Reference setting is set to Auscultatory or Invasive. This setting can be changed in Configuration
Mode.
Preparing to Measure Noninvasive Blood Pressure
If possible, avoid taking measurements during contractions because the measurement may be
unreliable and may cause additional stress for the patient.
1Connect the cuff to the air tubing.
2Plug the air tubing into the red NBP connector. Avoid compression or restriction of pressure
tubes. Air must pass unrestricted through the tubing.
3Make sure that you are using a Philips-approved correct sized cuff and that the bladder inside the
cover is not folded or twisted.
A wrong cuff size, and a folded or twisted bladder, can cause inaccurate measurements. The width
of the cuff should be in the range from 37% to 47% of the limb circumference. The inflatable part
of the cuff should be long enough to encircle at least 80% of the limb.
4Apply the cuff to a limb at the same level as the heart. If it is not, you must use the measurement
correction formula to correct the measurement.
The marking on the cuff must match the artery location. Do not wrap the cuff too tightly around
the limb. It may cause discoloration, and ischemia of the extremities. Inspect the application site
regularly to ensure skin quality and inspect the extremity of the cuffed limb for normal color,
warmth and sensitivity. If the skin quality changes, or if the extremity circulation is being affected,
move the cuff to another site or stop the blood pressure measurements immediately. Check more
frequently when making automatic or stat measurements.
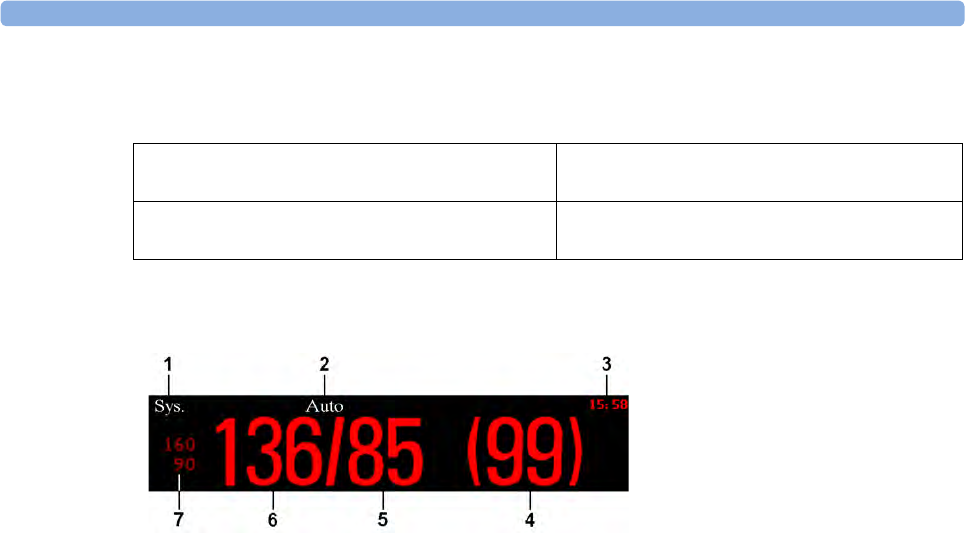
18 Monitoring Noninvasive Blood Pressure
205
Correcting the Measurement if Limb is not at Heart Level
To correct the measurement if the limb is not at heart level, to the displayed value
Understanding the Numerics
Depending on the numeric size, not all elements may be visible. Your monitor may be configured to
display only the systolic and diastolic values. If configured to do so, the pulse from NBP will display
with the NBP numeric.
Aging Numerics
The measured NBP value, together with the corresponding pulse rate if this is switched on, will be
displayed for one hour. After that the values are regarded as invalid and are no longer displayed.
During this time, measurement values may be grayed out or disappear from the screen after a set time,
if configured to do so. This avoids older numerics being misinterpreted as current data. The time can
be set in Configuration Mode. In Auto Mode the measurement values may disappear more quickly (to
be replaced by new measurement values), if the repeat time is set to less than one hour.
NBP and SpO2 numerics from intermittent measurements can be configured to be grayed out or to
disappear from the screen after a set time. This avoids older numerics being misinterpreted as current
data. The time can be set individually for SpO2 and NBP in Configuration Mode.
Alarm Sources
If you have parallel alarm sources, the sources are displayed instead of the alarm limits.
Add 0.75 mmHg (0.10 kPa) for each centimeter
higher or
Deduct 0.75 mmHg (0.10 kPa) for each
centimeter lower or
Add 1.9 mmHg (0.25 kPa) for each inch higher. Deduct 1.9 mmHg (0.25 kPa) for each inch
lower.
1Alarm source
2Measurement Mode
3Timestamp/Timer
4Mean pressure
5Diastolic
6Systolic
7Alarm limits
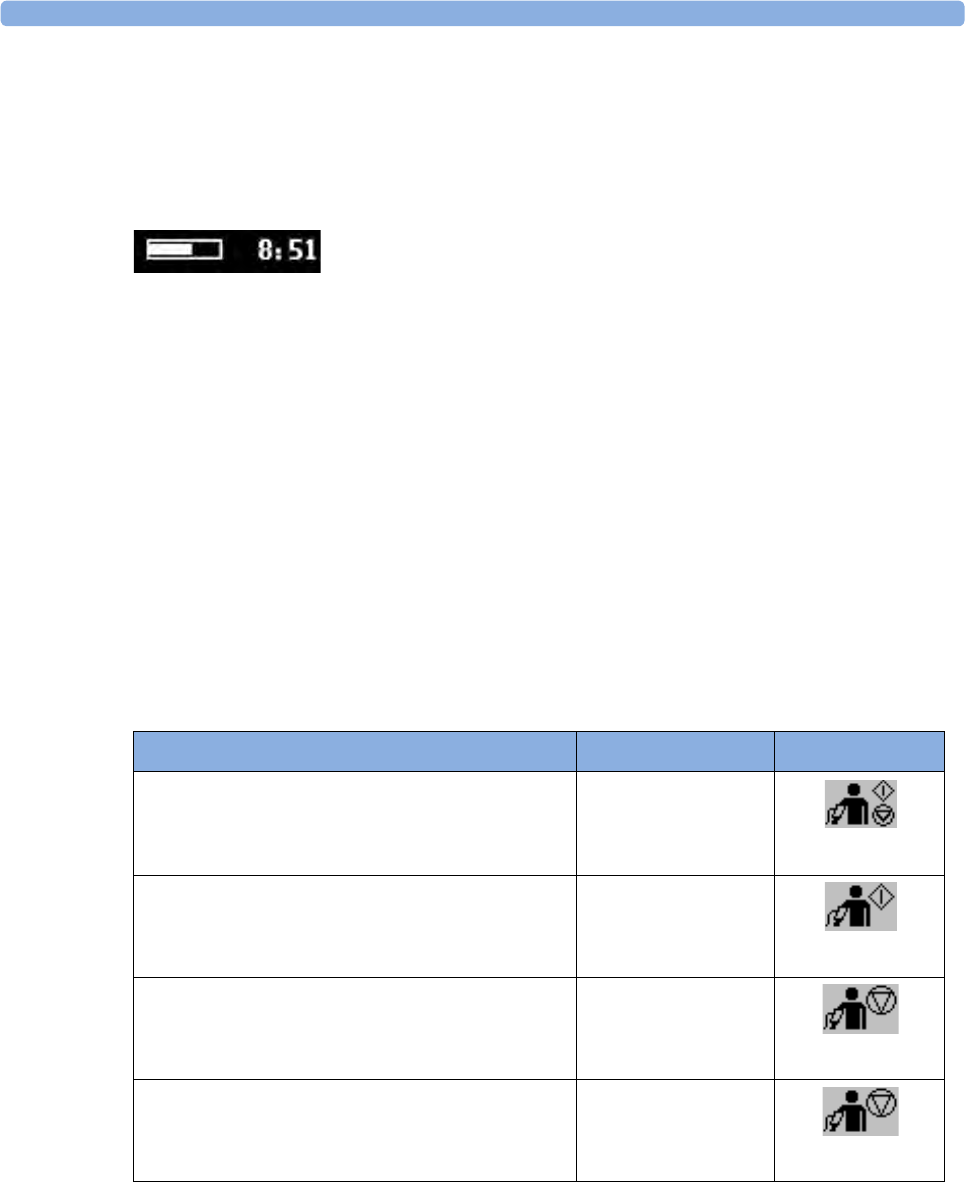
18 Monitoring Noninvasive Blood Pressure
206
NBP Measurement Timestamp
Depending on your configuration, the time shown beside the NBP numeric can be:
– the time of the most recent NBP measurement, also known as the "timestamp", or
– the time until the next measurement in an automatic series, displayed with a graphic
representation of the remaining time, as shown here.
• The NBP timestamp will normally show the completion time of the NBP measurement.
NBP Measurement Start Time
In Auto or Sequence mode the monitor is configured to synchronize the measurements in a
measurement series to an "easy-to-document" time. For example, if you start the first measurement at
08:23, and the Repeat Time is set to 10 min, the monitor automatically performs the next
measurement at 8:30, then 8:40 and so on, unless it has been configured to NotSynchron..
During Measurements
The cuff pressure is displayed instead of the units and the repeat time. An early systolic value gives you
a preliminary indication of the systolic blood pressure during measurement.
Starting and Stopping Measurements
Use the Setup menu or the SmartKeys to start and stop measurements.
Action to be performed Setup menu SmartKeys
Start/Stop manual measurement
Start Auto series
Stop current automatic measurement
Start/Stop
Start/ Stop
Start manual measurement
Start Auto series
-
Start
Stop manual measurement
Stop current automatic measurement
-
Stop
Stop automatic, or manual measurement AND series Stop All NBP
Stop All
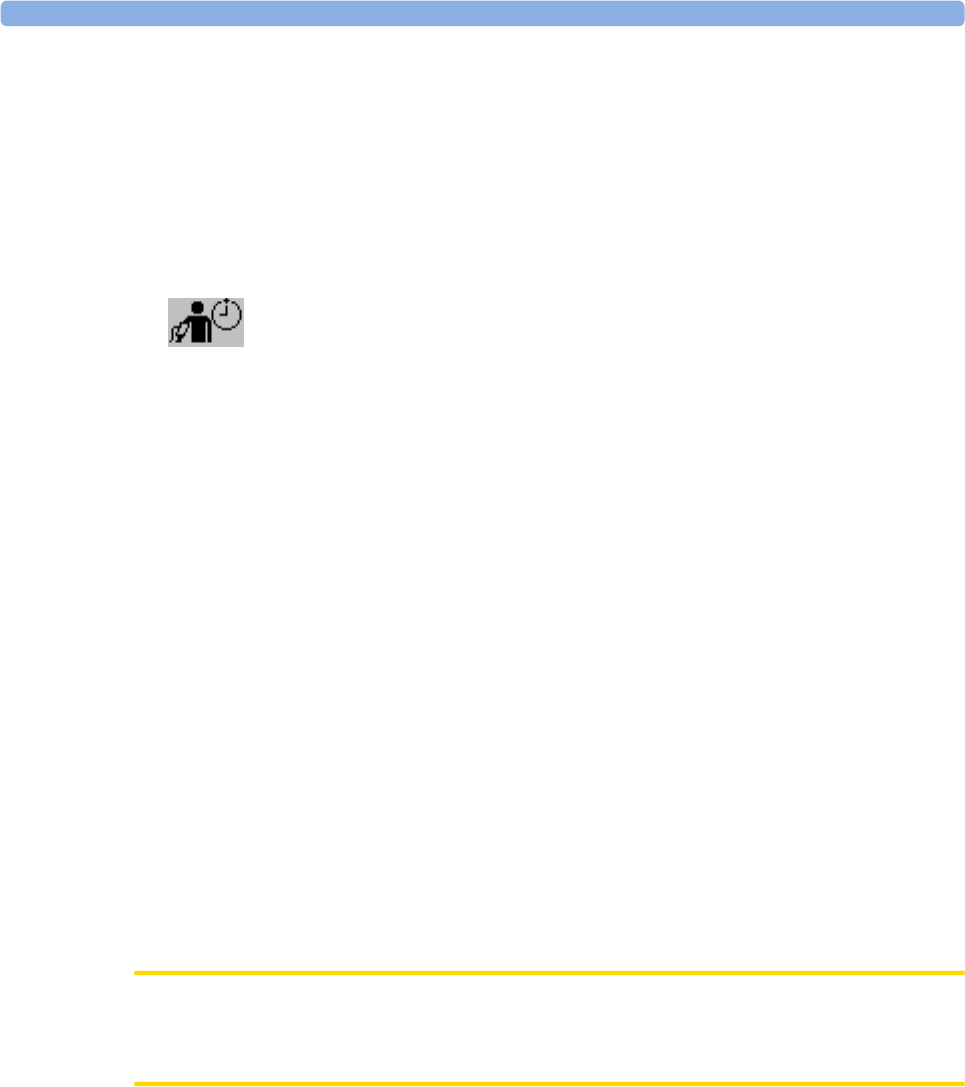
18 Monitoring Noninvasive Blood Pressure
207
Enabling Automatic Mode and Setting Repetition
Time
1In the Setup NBP menu, select Mode.
2Toggle between Auto and Manual, if necessary, to pick the measurement method.
3If making an automatic measurement, select Repeat Time or press the Repeat Time SmartKey
and set the time interval between two measurements.
NOTE
Be aware that a combination of a recorder speed of less than 3 cm/min and a repetition time of less
than five minutes can result in not all noninvasive blood pressure measurements being recorded on the
fetal trace. For example, if the recorder speed is set to 1 cm/min and the repetition time is set to
two minutes, due to the low speed setting, the recorder will only be able to record every other
noninvasive blood pressure measurement. This affects only the local fetal trace recording, and all
measurements are displayed as normal on the monitor's screen.
Enabling Sequence Mode and Setting Up The
Sequence
1In the Setup NBP menu, select Mode and select Sequence from the pop-up menu.
2Select Setup Sequence to open the Setup Sequence window.
Up to four measurement cycles can be setup which will run consecutively. For each cycle you can
set the number of measurements and the interval between them. If you want to run less than four
cycles in a sequence, you can set the number of measurements for one or more cycles to Off.
3Select each sequence in turn, and select the number of measurements and the time interval
between the measurements.
4To have measurements continue after the sequence, set the number of measurements for your last
cycle to Continuous and this cycle will run indefinitely.
CAUTION
Be aware that, if none of the cycles are set to Continuous, NBP monitoring will end after the last
measurement of the cycle.
When the NBP measurement mode is set to Sequence, the repetition time for Auto Mode cannot be
changed.
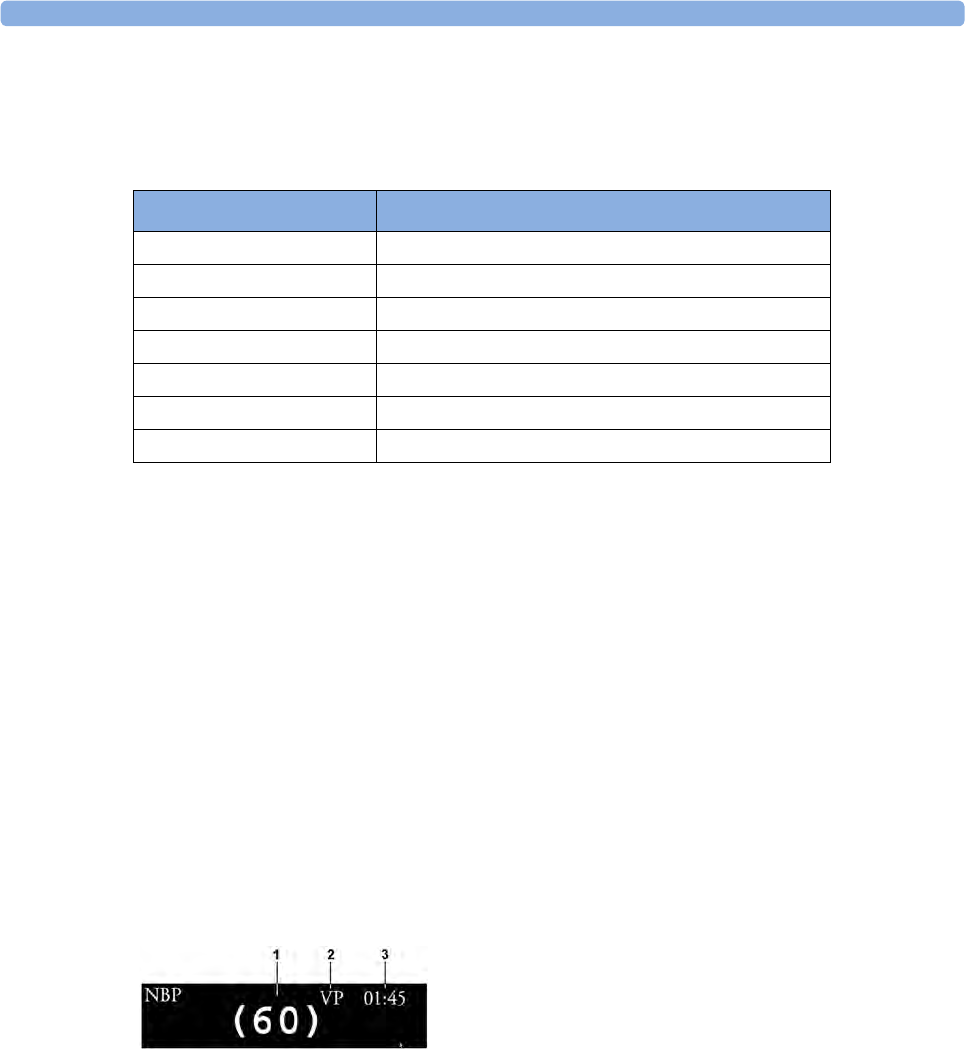
18 Monitoring Noninvasive Blood Pressure
208
Choosing the Alarm Source
You can monitor for alarm conditions in systolic, diastolic, and mean pressure, either singly or in
parallel. Only one alarm is given, with the priority of mean, systolic, diastolic.
If mean is not selected as alarm source (Sys., Dia., or Sys & Dia selected), but the fetal monitor can
only derive a mean value, mean alarms will nevertheless be announced using the most recent mean
alarm limits. Check that the mean alarm limits are appropriate for the patient, even when not using
mean as the alarm source. When no value can be derived an NBP Measure Failed INOP will be
displayed.
Assisting Venous Puncture
You can use the cuff to cause sub-diastolic pressure. The cuff deflates automatically after a set time if
you do not deflate it.
1In the Setup NBP menu select VeniPuncture.
2Puncture vein and draw blood sample.
3Reselect VeniPuncture to deflate the cuff.
During measurement, the display shows the inflation pressure of the cuff and the remaining time in
venous puncture mode.
Calibrating NBP
NBP is not user-calibrated. NBP pressure transducers must be verified at least once every two years by
a qualified service professional, and calibrated, if necessary. See the Service Guide for details.
Menu option Pressure value monitored
Sys. systolic
Dia. diastolic
Mean mean
Sys & Dia systolic and diastolic in parallel
Dia & Mean diastolic and mean in parallel
Sys & Mean systolic and mean in parallel
Sys&Dia&Mean all three pressures in parallel
1Cuff pressure
2Venous puncture measurement mode
3Time left in venous puncture mode
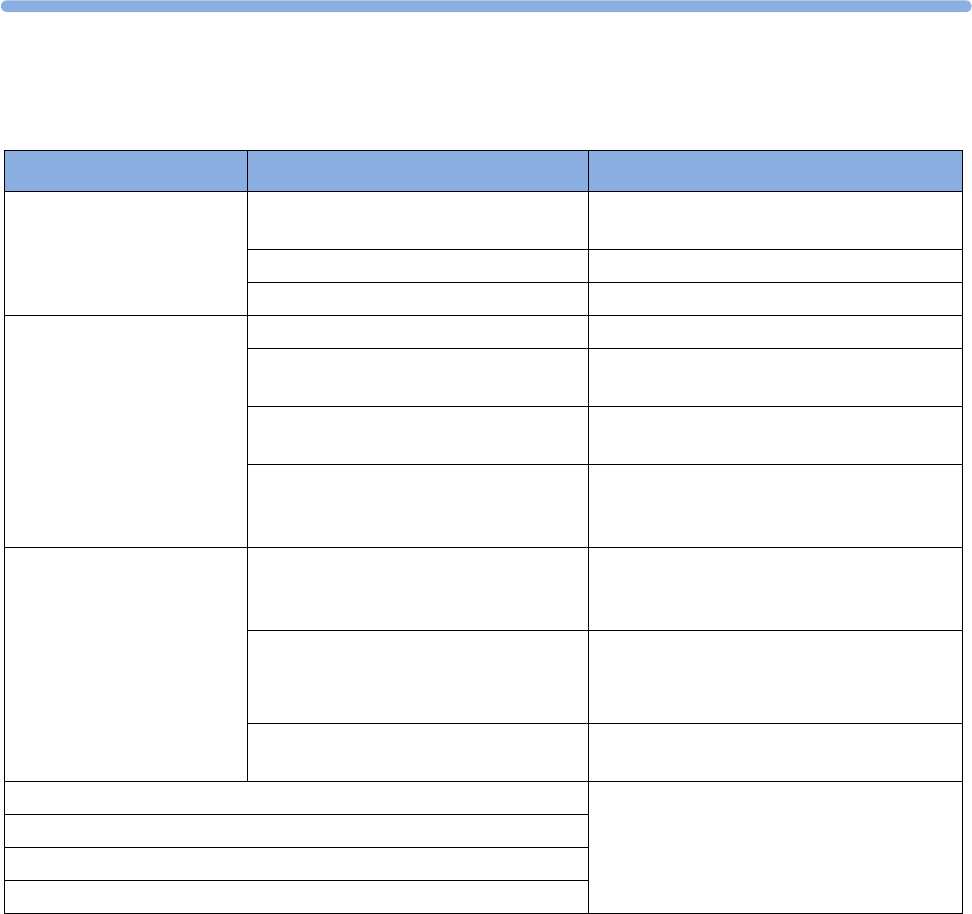
18
209
Troubleshooting
Problem Possible Causes Solutions
Cuff will not inflate Monitor is in Service or Configuration
Mode
Technical defect Call service
Cuff tubing not connected Connect cuff tubing
High or low values
measured (against clinical
expectations)
Contraction occurring Wait until contraction has finished
Patient talking before or during
measurement
Allow patient to rest quietly, then try again
after three to five minutes
Incorrect cuff size or cuff not at heart
level
Check cuff size, level, and position
Noninvasive blood pressure reference
method set incorrectly
Check the reference method configured
(auscultation or intra-arterial) and correct if
necessary in Configuration Mode
Displays zeros for systolic
and diastolic values.
Measurement automatically
repeats
Severe vasoconstriction at cuff site Move cuff to another limb, check for shock,
or verify blood pressure using another
method
Erratic blood pressure fluctuations due
to arrhythmias or rapid-acting drugs or
contractions
Try again, if unsuccessful, verify blood
pressure using another method
Wait until contraction has finished.
Excessive patient movement or
convulsions
Restrain movement or verify blood pressure
using another method
NBP Cuff Overpress INOP is displayed See “Patient Alarms and INOPs” on
page 121.
NBP Equip Malf INOP is displayed
NBP Interrupted INOP is displayed
NBP Measure Failed

18 Monitoring Noninvasive Blood Pressure
210
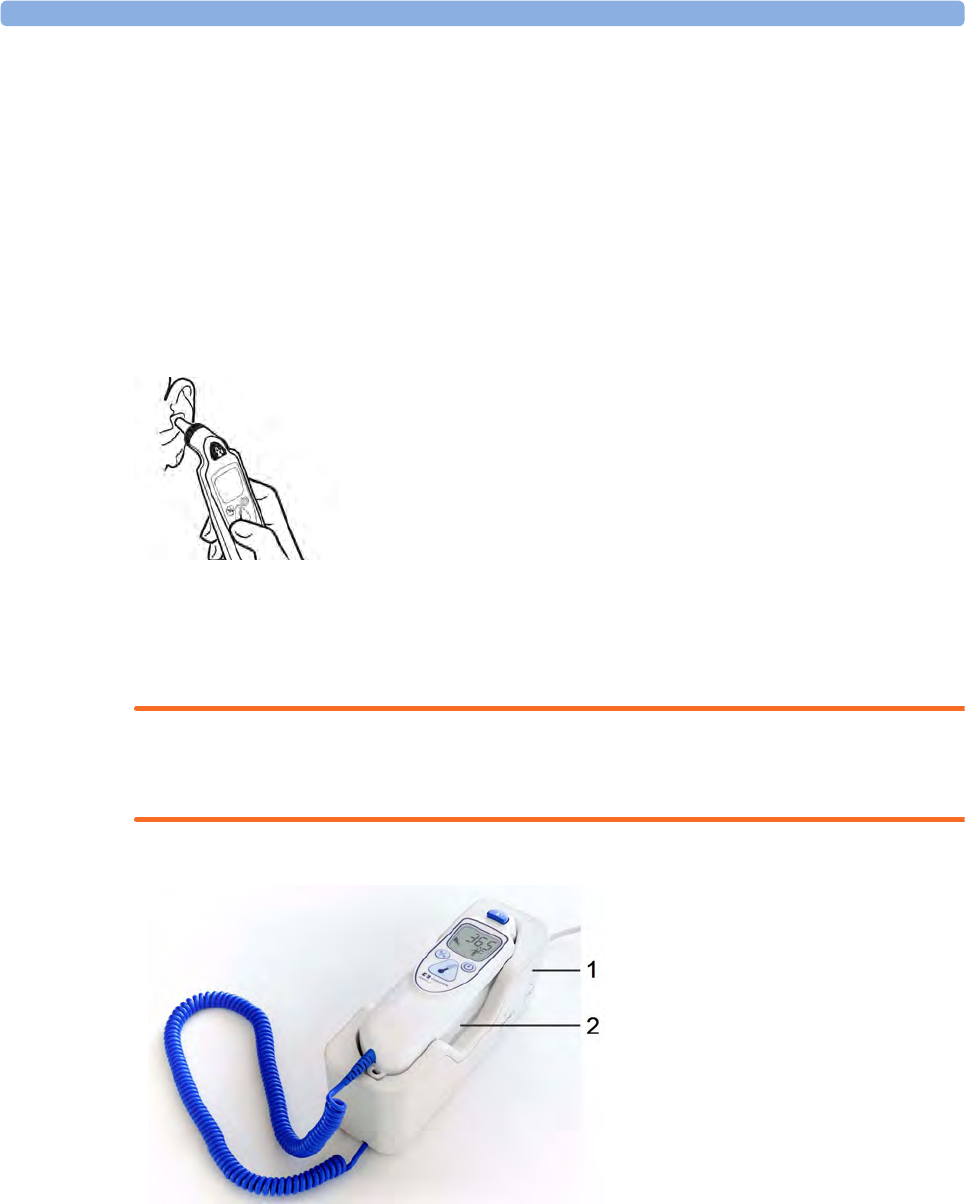
19 Monitoring Maternal Temperature
211
19Monitoring Maternal
Temperature
Measuring Tympanic Temperature
The tympanic thermometer measures the patient's temperature in the ear using infrared technology.
The result of this measurement can be automatically adjusted to correspond to a different body
reference site. The result is displayed on the screen of the thermometer and transmitted to the
monitor.
The thermometer is used with single-use probe covers for infection control during measurement.
WARNING
Do not use in the presence of flammable anesthetics, such as a flammable anesthetic mixture with air,
oxygen or nitrous oxide.
Place the thermometer into its base station, when it is not in use. The base station allows flexible
mounting of the thermometer at the point of care. The base station is connected to the monitor's
MIB/RS232 interface (optional) via a cable. It has storage space for up to 32 probe covers.
1Base station
2Thermometer
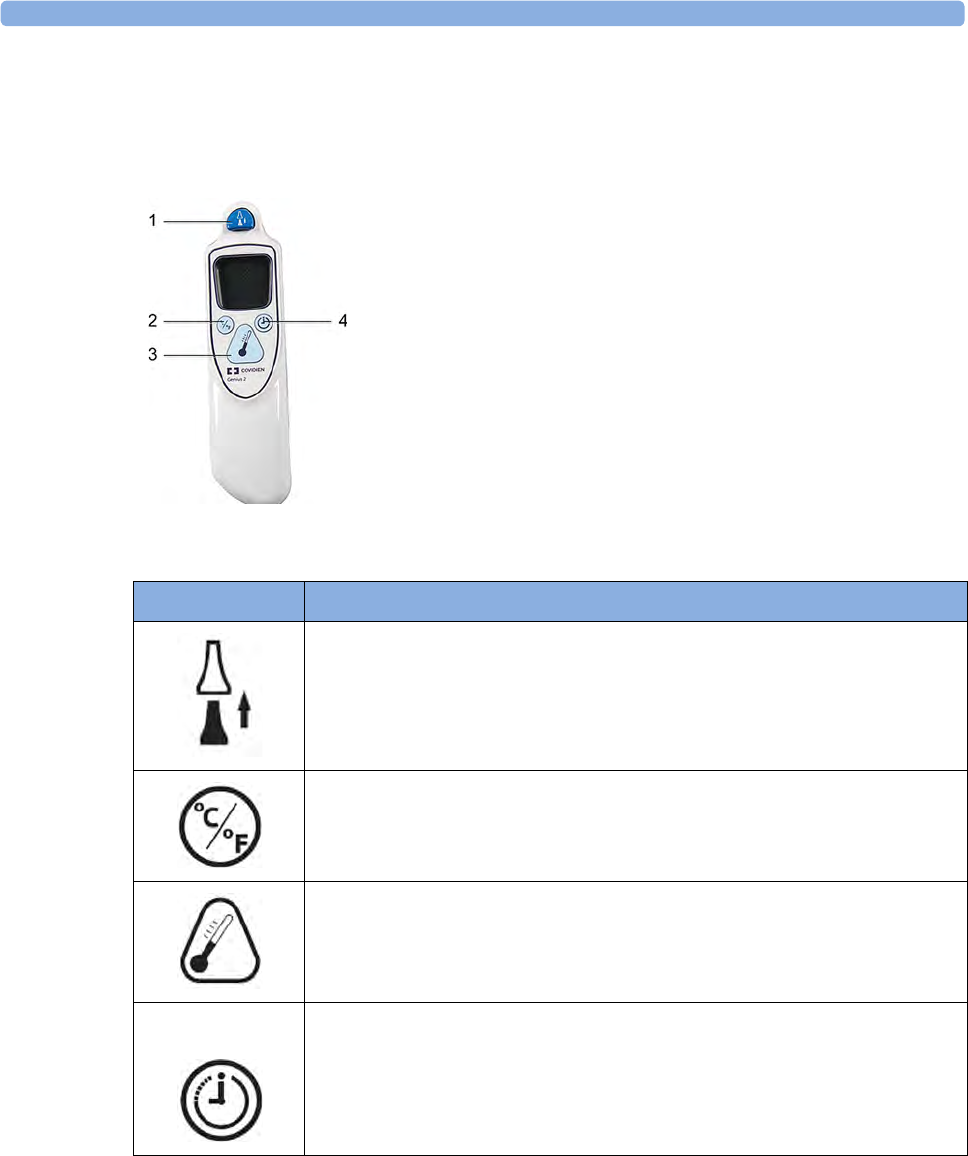
19 Monitoring Maternal Temperature
212
Thermometer Display and Controls
The tympanic thermometer has a liquid crystal display. The display shows the patient's temperature in
numerics and guides you with symbols through the measurement process.
1Eject key
2Change unit key: °Celsius / °Fahrenheit
3Start measurement key
4Pulse timer key
Functional Keys Description of Use
Press the eject key to eject the probe cover. The eject key symbol is shown on
the display when a measurement has been taken and transmitted.
Press the change unit key after a measurement to switch between °C and °F.
Press the start measurement key when you are ready to take a patient's
temperature.
The pulse timer key can be used to time vital signs you take manually.
Press and hold the pulse timer key to enter timer mode. Press the pulse timer key
again to start the timer.
The thermometer will issue a one beep at 15 seconds, two beeps at 30 seconds,
three beeps at 45 seconds, and four beeps at 60 seconds.
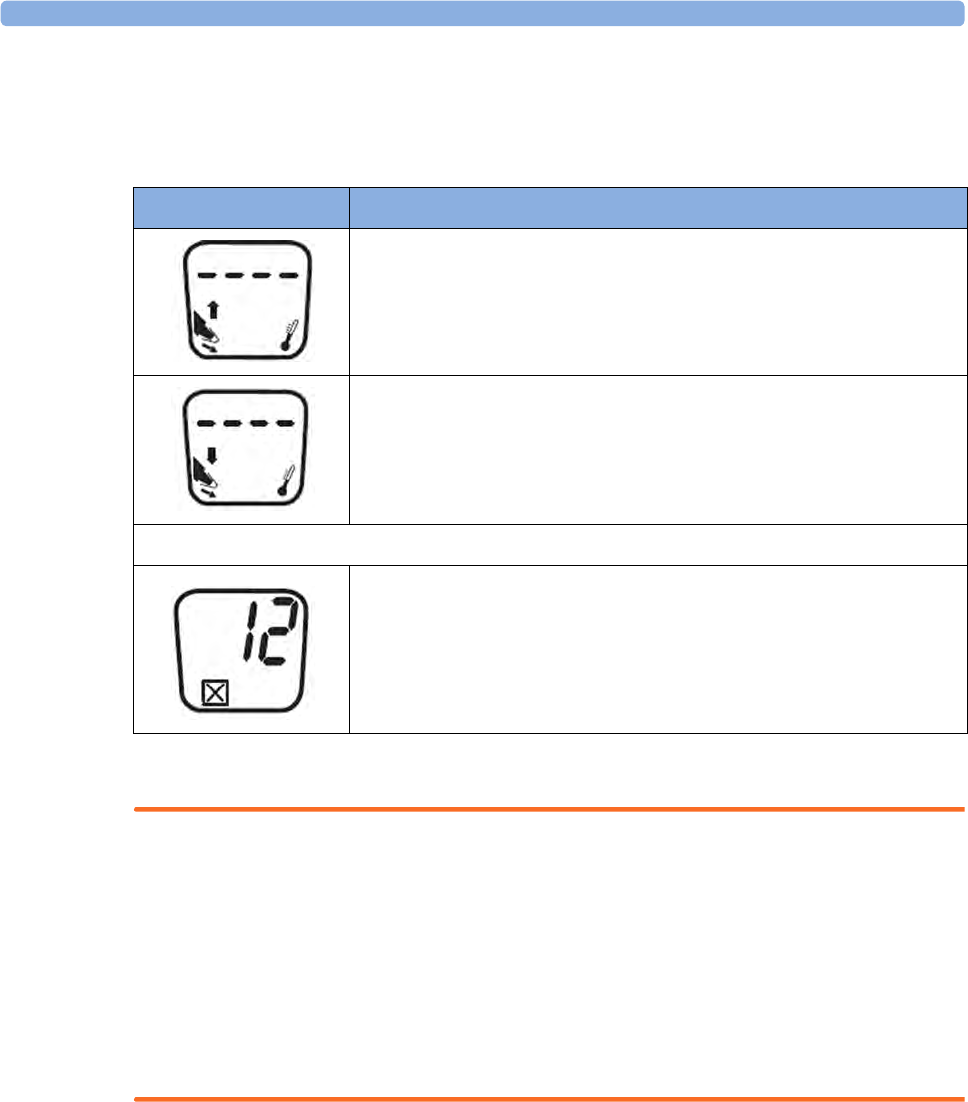
19 Monitoring Maternal Temperature
213
Status Screens
The thermometer performs an internal test at every start-up to verify that the system components are
functioning properly. It measures the ambient temperature. During start-up and measurement, the
thermometer screens communicate the current status.
Making a Temperature Measurement
WARNING
Inaccurate measurement results can be caused by:
• incorrect application of the thermometer.
• anatomical variations in the ear.
• build up of earwax in the ear.
• excessive patient movement during the measurement.
• absent, defective or soiled probe covers.
• probe covers other than the specified probe covers.
1Ensure that the base station is connected via the appropriate cable to the connector on the
monitor.
2Remove the thermometer from the base station.
The thermometer is latched to the base station to avoid an accidental fall when the base station is
moved. To pick up the thermometer from the base station move it slightly up and then lift it from
the base station to release the latch.
3Press the eject key on the thermometer to discard any probe that may have been left on the
thermometer from a previous use.
Images Description
Ambient Temperature above specified range
Ambient Temperature below specified range
System errors
System error 12 - there is a problem with the settings. Contact your
service personnel to have them check the settings and reset them, if
necessary.
If the display shows any other system error, then reset the thermometer by
picking up a probe cover. If the system error does not clear, contact your
service personnel.
19 Monitoring Maternal Temperature
214
4Pick up a new probe from the probe container on the base station.
5Inspect the probe cover to make sure it is fully seated (no space between cover and tip base) and
there are no holes, tears, or wrinkles in the plastic film.
6Place the thermometer with the probe in the ear canal, sealing the opening with the probe tip. For
consistent results, ensure that the probe shaft is aligned with the ear canal.
7Press and release the start-up key gently.
8Wait until you hear the three beeps.
9Remove the probe from the ear.
The temperature values are displayed both on the thermometer itself and on the connected
monitor.
10 Check that the correct temperature label for the measurement site is displayed: iTrect, iToral,
iTcore, or iTtymp
11 Press the eject key to eject the probe cover into a suitable waste receptacle.
12 Return the thermometer to the base station.
The thermometer switches to stand-by mode after 30 seconds when not used.
Possible INOPs
Images Description
Patient temperature above measurement range.
Patient temperature below measurement range.
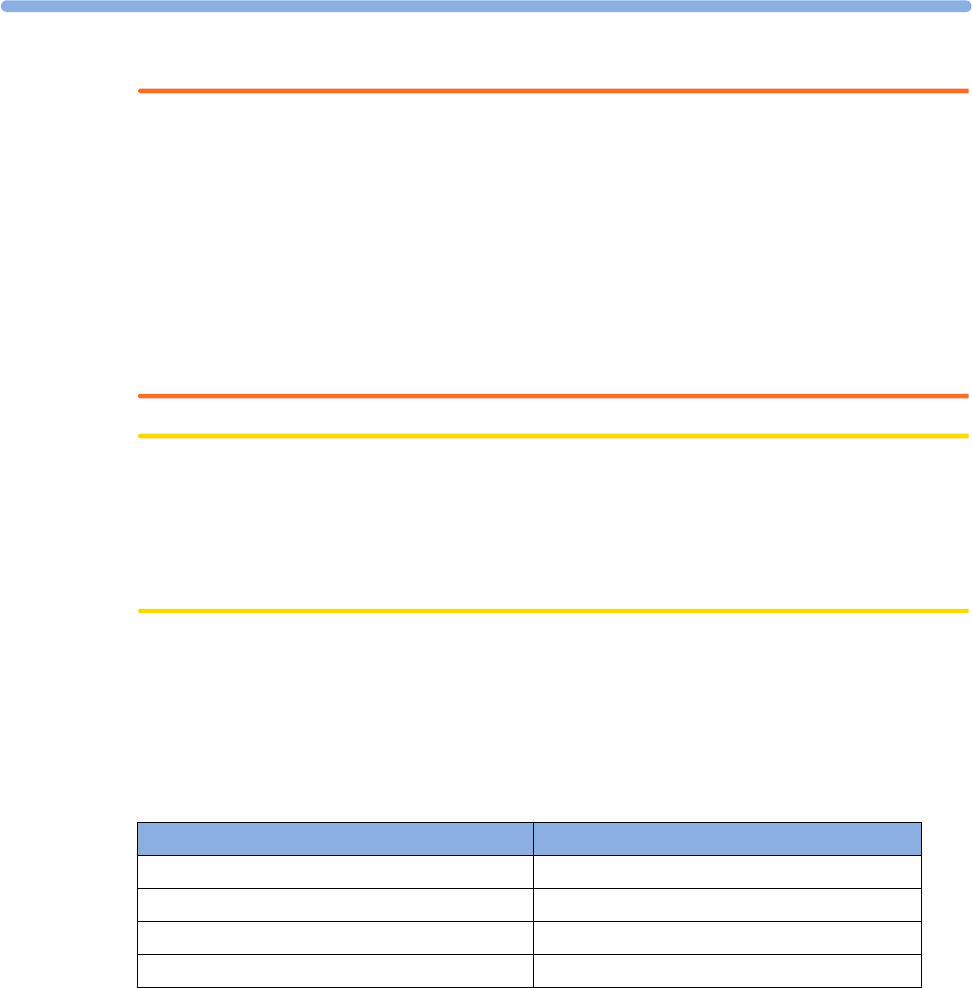
19
215
WARNING
• Never apply the probe to the patient when the probe is not connected to the unit.
• Always use a single-use probe cover to limit patient cross-contamination.
• Measurement errors or inaccurate readings may result when probe covers other than the specified
probe covers are used (see “Tympanic Temperature Accessories” on page 267)
• Insert the probe slowly and carefully to avoid damage to the ear canal and the tympanic
membrane.
• Inspect the probe for damage, holes, tears, or sharp edges to avoid injuring the skin.
• Always ensure that the used probe cover is removed before attaching a new probe cover.
CAUTION
• Do not immerse the probe in fluids, or drop fluids on the probe.
• Do not use a probe cover that has been dropped or is damaged.
• Do not autoclave. To prevent damage to the unit, probe and accessories, refer to the cleaning
procedures in the “Cleaning and Disinfecting” on page 246 chapter.
Body Reference Sites and Monitor Labels
The tympanic thermometer measures the patient's temperature in the ear. The thermometer can be
configured to adjust the result of the measurement to correspond to a different body reference site.
The measurement label displayed on the monitor corresponds to the body reference site that is
configured. The following body reference sites are available:
The body reference site can be selected in the Biomed mode of the tympanic thermometer. See the
Service Guide for more information.
The measured maternal temperature is only transmitted to a connected OB TraceVue/IntelliSpace
Perinatal, when the tympanic thermometer is configured to the iTtymp body reference site, and the
iTtymp label is displayed on the fetal monitor screen and printed out on the trace paper.
Body Reference Site Label on Monitor
Ear temperature (no adjustment) iTtymp
Oral temperature iToral
Core temperature iTcore
Rectal temperature iTrect
19 Monitoring Maternal Temperature
216
Entering Temperature Manually
A temperature measurement can be entered manually.
1Press the SmartKey Enter Temp.
2A numeric pad opens.
3Enter the temperature values.
4Press the Enter key.
The aging time (time the entered value is valid) can be configured in the Configuration Mode.
20 Monitoring SpO2
217
20Monitoring SpO2
FM30/40/50 The pulse oximetry measurement (SpO2) is intended for use with maternal patients.
Philips pulse oximetry uses a motion-tolerant signal processing algorithm, based on Fourier Artifact
Suppression Technology (FAST). It provides two measurements:
• Oxygen saturation of arterial blood (SpO2) - percentage of oxygenated hemoglobin in relation to
the sum of oxyhemoglobin and deoxyhemoglobin (functional arterial oxygen saturation).
• Pulse rate - detected arterial pulsations per minute. This is derived from the SpO2 value, and is one
of four sources of the maternal heart/pulse rate used for cross-channel verification (see
“Monitoring Maternal Heart / Pulse Rate” on page 223 and “Cross-Channel Verification (CCV)”
on page 149).
Selecting an SpO2 Sensor
See “Accessories and Supplies” on page 257 for a list of sensors, and the patient population and
application sites for which they are appropriate.
Familiarize yourself with the Instructions for Use supplied with your sensor before using it.
CAUTION
Do not use OxiCliq disposable sensors in a high humidity environment, or in the presence of fluids,
which may contaminate sensor and electrical connections causing unreliable or intermittent
measurements. Do not use disposable sensors when there is a known allergic reaction to the adhesive.
Applying the Sensor
1Follow the SpO2 sensor's Instructions for Use, adhering to all warnings and cautions.
2Remove colored nail polish from the application site.
3Apply the sensor to the patient. The application site should match the sensor size so that the
sensor can neither fall off, nor apply excessive pressure.
4Check that the light emitter and the photodetector are directly opposite each other. All light from
the emitter must pass through the patient's tissue.
20 Monitoring SpO2
218
WARNING
Proper Sensor Fit: If a sensor is too loose, it might compromise the optical alignment or fall off. If it
is too tight, for example because the application site is too large or becomes too large due to edema,
excessive pressure may be applied. This can result in venous congestion distal from the application site,
leading to interstitial edema, hypoxemia and tissue malnutrition. Skin irritations or lacerations may
occur as a result of the sensor being attached to one location for too long. To avoid skin irritations and
lacerations, periodically inspect the sensor application site and change the application site regularly.
Venous Pulsation: Do not apply sensor too tightly as this results in venous pulsation which may
severely obstruct circulation and lead to inaccurate measurements.
Ambient Temperature: At elevated ambient temperatures be careful with measurement sites that are
not well perfused, because this can cause severe burns after prolonged application. All listed sensors
operate without risk of exceeding 41°C on the skin if the initial skin temperature does not exceed
35°C.
Extremities to Avoid: Avoid placing the sensor on extremities with an arterial catheter, an NBP cuff
or an intravascular venous infusion line.
Connecting SpO2 Cables
Connect the sensor cable to the color-coded socket on the monitor. If you are using a disposable
sensor, plug the sensor into the adapter cable and connect this to the monitor. Connect reusable
sensors directly to the monitor.
CAUTION
Extension cables: Do not use more than one extension cable (M1941A). Do not use an extension
cable with Philips reusable sensors or adapter cables with part numbers ending in -L (indicates "long"
cable version).
Electrical Interference: Position the sensor cable and connector away from power cables, to avoid
electrical interference.
Measuring SpO2
During measurement, ensure that the application site:
– has a pulsatile flow, ideally with a signal quality indicator of at least medium.
– has not changed in its thickness (for example, due to edema), causing an improper fit of the
sensor.

20 Monitoring SpO2
219
WARNING
• For fully conscious maternal patients, who have a normal function of perfusion and sensory
perception at the measurement site:
To ensure skin quality and correct optical alignment of the sensor, inspect the application site
when the measurement results are suspicious or when the patient complains about pressure at
the application site, but at least every 24 hours. Correct the sensor alignment if necessary.
Move the sensor to another site, if the skin quality changes.
• For all other patients:
Inspect the application site every two to three hours to ensure skin quality and correct optical
alignment. Correct the sensor alignment if necessary. If the skin quality changes, move the
sensor to another site. Change the application site at least every four hours.
• Injected dyes such as methylene blue, or intravascular dyshemoglobins such as methemoglobin
and carboxyhemoglobin may lead to inaccurate measurements.
• Inaccurate measurements may result when the application site for the sensor is deeply pigmented
or deeply colored, for example, with nail polish, artificial nails, dye or pigmented cream.
• Interference can be caused by:
– High levels of ambient light (including IR warmers) or strobe lights or flashing lights (such as
fire alarm lamps). (Hint: cover application site with opaque material).
– Another SpO2 sensor in close proximity (e.g. when more than one SpO2 measurement is
performed on the same patient). Always cover both sensors with opaque material to reduce
cross-interference.
– Electromagnetic interference, especially at perfusion indicator values below 1.0 or signal
quality indicator below medium.
– Excessive patient movement and vibration.
SpO2 Signal Quality Indicator (Fast SpO2 only)
The SpO2 numeric is displayed together with a signal quality indicator (if configured and enough space
is available) which gives an indication of the reliability of the displayed values.
The level to which the triangle is filled shows the quality of the signal; the indicator below shows a
medium signal quality, the signal quality is at a maximum when the triangle is completely filled.
20 Monitoring SpO2
220
Assessing a Suspicious SpO2 Reading
Traditionally, pulse rate from SpO2 was compared with heart rate from ECG to confirm the validity of
the SpO2 reading. With newer algorithms, such as FAST-SpO2, this is no longer a valid criteria because
the correct calculation of SpO2 is not directly linked to the correct detection of each pulse.
When pulse rate is very low, or strong arrhythmia is present, the SpO2 pulse rate may differ from the
heart rate calculated from ECG but this does not indicate an inaccurate SpO2 value.
WARNING
With pulse oximetry, sensor movement, ambient light (especially strobe lights or flashing lights) or
electromagnetic interference can give unexpected intermittent readings when the sensor is not
attached. Especially bandage-type sensor designs are sensitive to minimal sensor movement that might
occur when the sensor is dangling.
Understanding SpO2 Alarms
This refers to SpO2 specific alarms. See the “Alarms” on page 109 chapter for general alarm
information. SpO2 offers high and low limit alarms, and a high priority desat alarm. You cannot set the
low alarm limit below the desat alarm limit.
CAUTION
If you measure SpO2 on a limb that has an inflated noninvasive blood pressure cuff, a non-pulsatile
SpO2 INOP can occur. If the fetal monitor is configured to suppress this alarm there may be a delay of
up to 60 seconds in indicating a critical status, such as sudden pulse loss or hypoxia.
Alarm Delays
There is a delay between a physiological event at the measurement site and the corresponding alarm at
the monitor. This delay has two components:
• The general system delay time is the time between the occurrence of the physiological event and
when this event is represented by the displayed numerical values. This delay depends on the
algorithmic processing and the averaging time.
• The time between the displayed numerical values crossing an alarm limit and the alarm indication
on the monitor. This delay is the combination of the configured alarm delay time plus the general
system alarm signal delay time.
Adjusting the SpO2 Alarm Limits
In the Setup SpO₂ menu:
•Select
High Limit then choose the upper alarm limit.
•Select
Low Limit then choose the lower alarm limit.

20
221
Adjusting the Desat Limit Alarm
The Desat alarm is a high priority (red) alarm notifying you of potentially life threatening drops in
oxygen saturation.
1In the Setup SpO₂ menu, select Desat Limit.
2Adjust the limit.
Adjusting the Pulse Alarm Limits
See “Adjusting the Heart Rate / Pulse Alarm Limits” on page 230.
Setting Up Tone Modulation
If tone modulation is on, the QRS tone pitch lowers when the SpO2 level drops. Remember, the QRS
tone is derived from either heart rate (from MECG) or pulse (from built-in SpO2) depending on which
is currently displayed (see “Priority for Maternal Heart / Pulse Rate” on page 223).
NOTE
Pulse from CL SpO2 and Toco MP does not provide a QRS tone.
Setting the QRS Volume
In the Setup SpO₂ menu, select QRS Volume and set the appropriate QRS tone volume.

20 Monitoring SpO2
222
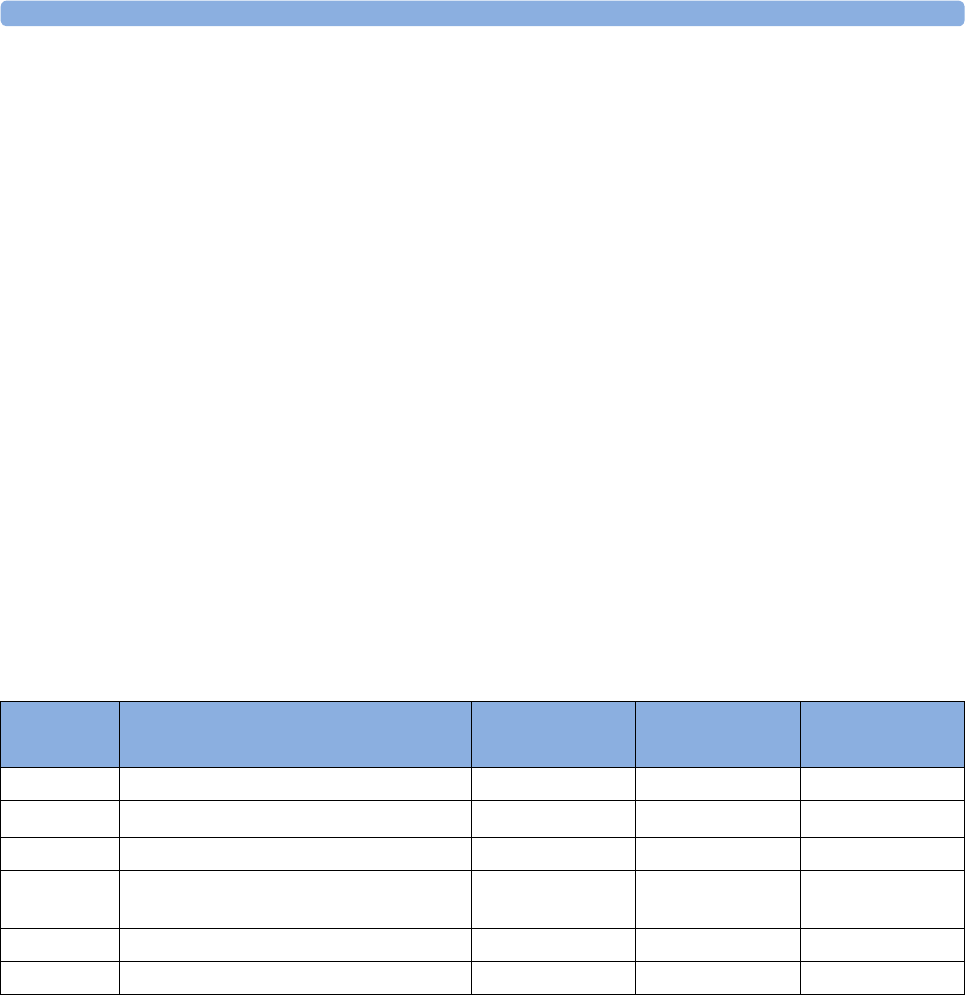
21 Monitoring Maternal Heart / Pulse Rate
223
21Monitoring Maternal Heart /
Pulse Rate
You can monitor the maternal heart/pulse rate using one of four sources:
• Maternal pulse from Toco MP or CL Toco+MP transducer (pulse rate)
•SpO
2 (pulse rate)
• Maternal heart rate (MHR) via MECG electrodes
• NBP (pulse rate)
Maternal heart / pulse rates derived from Toco MP or CL Toco+MP, SpO2 and MECG are
continuous measurements, and are compared against the FHR for cross-channel verification. Average
pulse rate derived from noninvasive blood pressure is an intermittent measurement, and is therefore
not used for cross-channel verification.
Priority for Maternal Heart / Pulse Rate
Only one Maternal Heart Rate / Pulse Rate numeric will be displayed and recorded at a time (see
priority table). If higher-priority measurements are connected but temporarily not providing valid
numerics, lower-priority numerics may be displayed and recorded instead.
Misidentification of MHR for FHR
To reduce the possibility of mistaking the MHR for FHR, it is recommended that you monitor both
maternal and fetal heart rates (see “Confirm Fetal Life Before Using the Monitor” on page 10 and
“Cross-Channel Verification (CCV)” on page 149).
Priority Maternal Heart / Pulse Rate Source Alarming Used for CCV Provides QRS
Tone
1 HR from MECG measurement Yes Yes Yes
2 Pulse from SpO2 measurement Yes Yes Yes
3 Pulse from CL SpO2 Pod measurement Yes Yes No
4 Pulse from Toco MP measurement
cableless or cabled
No Yes No
5 Pulse from CL NBP Pod measurement No No No
6 Pulse from NBP measurement No No No
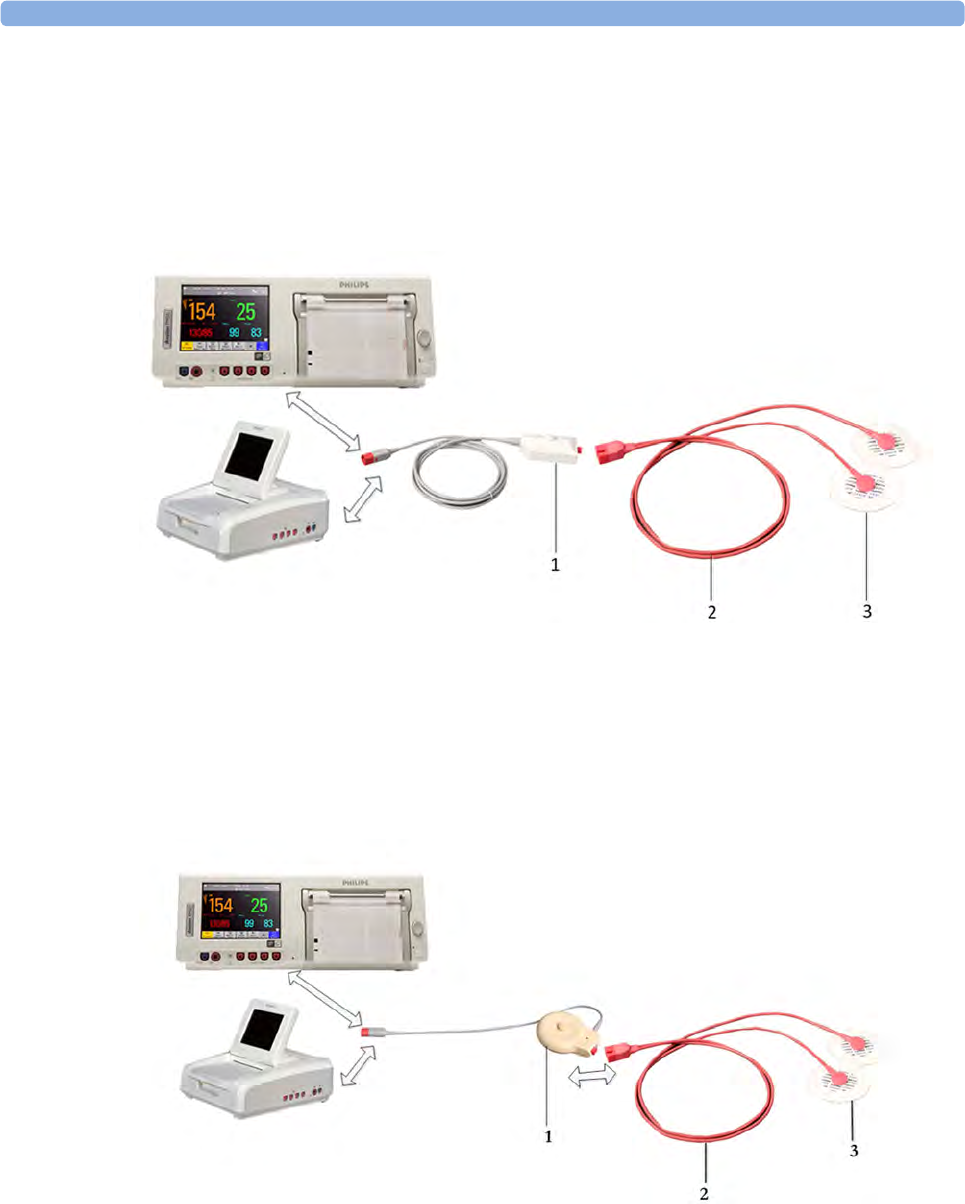
21 Monitoring Maternal Heart / Pulse Rate
224
MHR from MECG Electrodes
You can measure MHR using the equipment combinations shown in the following illustrations.
Illustration 1 shows the complete connection chain from the foam electrodes applied to the patient to
the fetal monitor using the patient module.
Illustration 2 shows the equivalent chain using the Toco+ transducer.
1Patient Module (M2738A)
2MECG Adapter Cable (M1363A)
3Pre-gelled Foam Electrodes (40493A/B/C/D/E)
1Toco+ Transducer (M2735A)
2MECG Adapter Cable (M1363A)
3Pre-gelled Foam Electrodes (40493A/B/C/D/E)
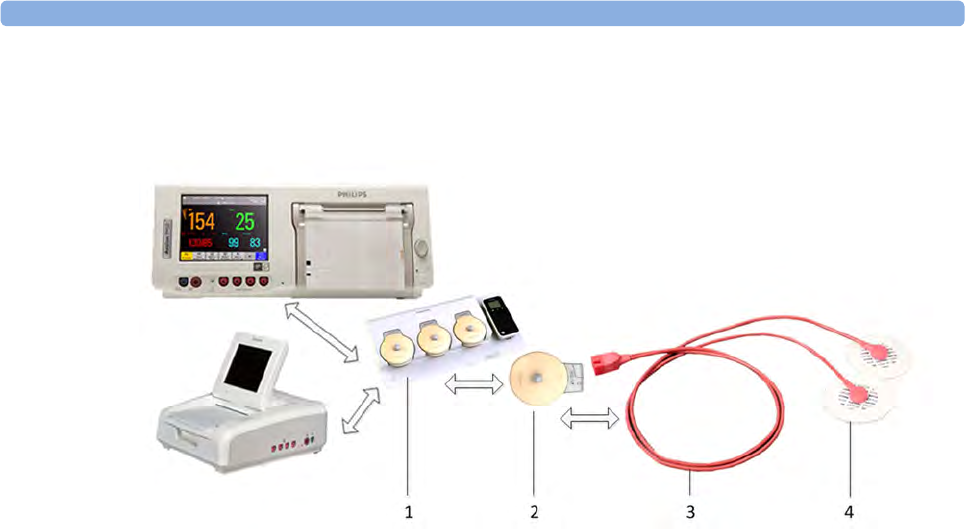
21 Monitoring Maternal Heart / Pulse Rate
225
Illustration 3 shows the equivalent chain using a CL Toco+MP transducer or a CL ECG/IUP
transducer.
To simultaneously measure DECG and MECG, you can use a Toco+, a CL Toco+MP, or a CL
ECG/IUP transducer for MECG. For measuring DECG you need a CL ECG/IUP transducer or a
patient module (see also “Monitoring FHR Using DECG” on page 195).
1Avalon CL base station (866074)
2CL Toco+MP or CL ECG/IUP transducer (866075 or 866077)
3MECG Adapter Cable (M1363A)
4Pre-gelled Foam Electrodes (40493A/B/C/D/E)
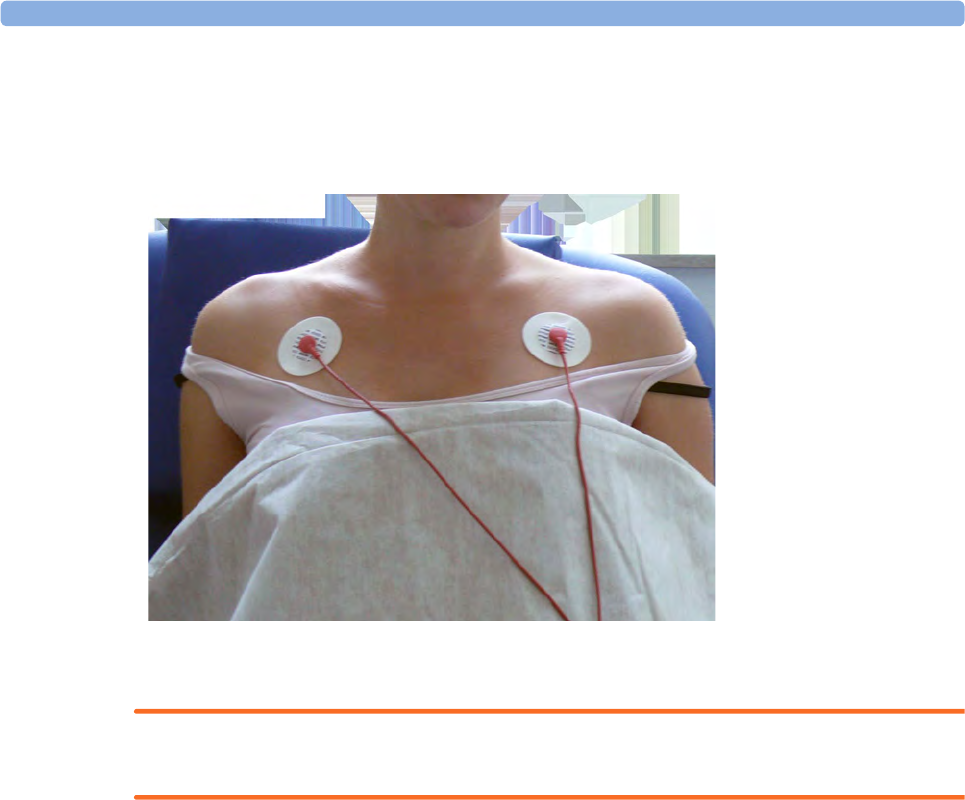
21 Monitoring Maternal Heart / Pulse Rate
226
Applying Electrodes
To derive the MHR (when you do not want to view the MECG waveform), you can place the
electrodes just below the outer end of the clavicle near each shoulder.
Making Connections
WARNING
Follow the instructions supplied with each of the monitoring accessories you are using.
Prepare for monitoring MHR using the list below. The standard procedures in use in your facility
determine the sequence of actions.
1Depending on the equipment you are using, ensure that either the Patient Module or the Toco+
transducer is connected to the fetal monitor. If you are using cableless monitoring use the
CL ECG/IUP or the CL Toco+MP transducer.
2Connect a pre-gelled foam electrode to each of the two leads on the MECG adapter cable.
3Apply the foam electrodes to the patient, following the instructions supplied with the foam
electrodes.
4Depending on the equipment you are using, connect the pink connector plug on the MECG
adapter cable to the pink connector on either the Patient Module or the Toco+ transducer. If you are
using cableless monitoring connect the MECG Adapter cable to the connectors of the CL ECG/
IUP or the CL Toco+MP transducer.
You are now ready to monitor MHR.
Monitoring MHR
1Switch on the recorder.
2The maternal heart rate is labeled HR on the screen.
1MECG Electrodes
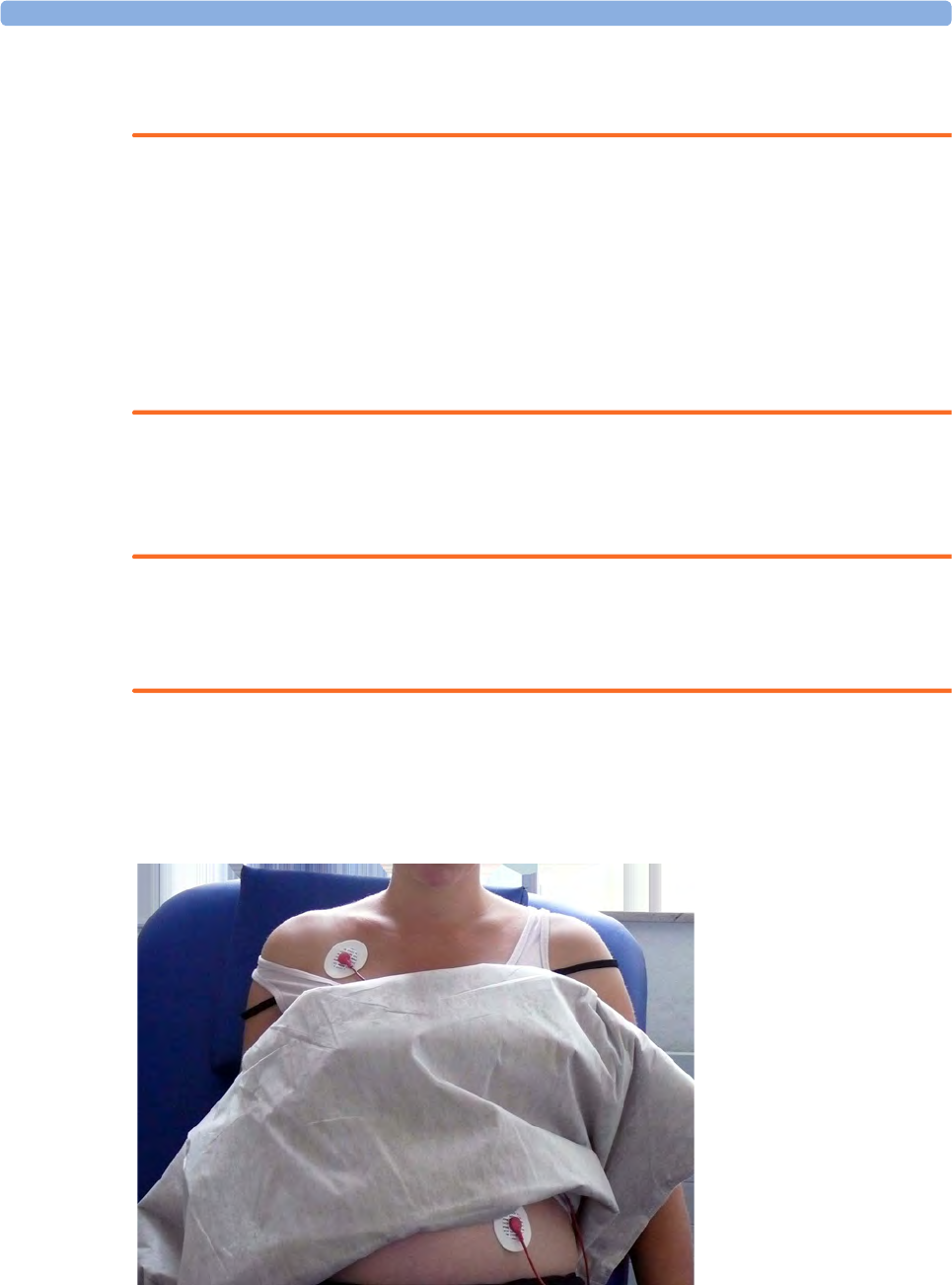
21 Monitoring Maternal Heart / Pulse Rate
227
Monitoring MECG Wave
WARNING
The fetal/maternal monitor is not a diagnostic ECG device. In particular, the display of fetal/maternal
ECG is intended only for evaluating signal quality for fetal/maternal heart rate as derived from the
ECG waveform.
When in doubt, it can be used to identify sources of compromised signal quality, such as noise or
muscle artifacts. It can subsequently be used to verify the result of measures taken to resolve them
(e.g., checking ECG cable connections or adapting the fetal ArtifactSuppress configuration).
The safety and effectiveness of the displayed fetal/maternal ECG waveform (i.e., P, QRS and T
segments) for evaluation of fetal/maternal cardiac status during labor have not been evaluated.
FM30/50 When measuring MECG with the Avalon FM30 or FM50, the MECG waveform, along with the heart
rate numeric, is displayed on the screen when using a Toco+, CL Toco+MP transducer, a patient
module, or a CL ECG/IUP transducer.
WARNING
The fetal/maternal monitor is NOT intended for use during defibrillation, electro-surgery, or MRI.
Remove all transducers, sensors, and accessories before performing electro-surgery, defibrillation, or
MRI, otherwise harm to the patient or the user can result.
Applying Electrodes
To obtain a satisfactory maternal ECG waveform you must use the RA to LL (lead II) position of the
standard 5-lead ECG.
1Place the RA electrode
(A) directly below the
clavicle and near the
right shoulder.
2Place the LL electrode
(B) on the left lower
abdomen.
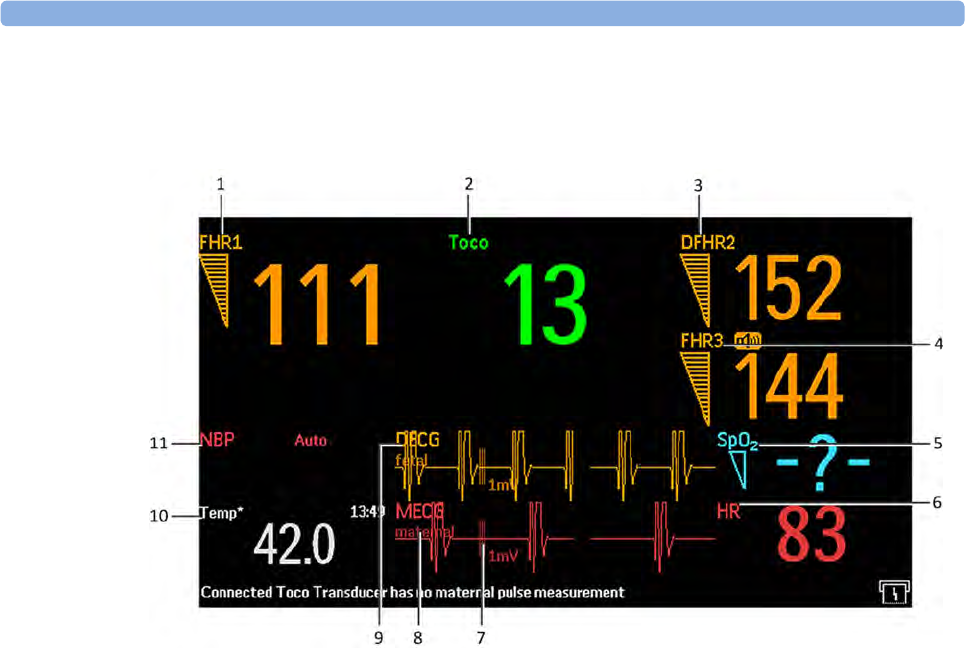
21 Monitoring Maternal Heart / Pulse Rate
228
Viewing the Waveform on the Screen
NOTE
The 1mV scale bar for the DECG and MECG wave is not displayed on the screen if you monitor
DECG or MECG with an Avalon CTS system. The Avalon CTS system does not provide a scaled
ECG.
For the FM30/50, the MECG wave is displayed automatically on the screen, labeled MECG. If DECG is
also being monitored (FM30/50), and the DECG Wave is configured to On, both waves are displayed,
with the DECG Wave above the MECG wave. The DECG Wave is labeled DECG.
1Measurement label (FHR1)
2Measurement label (Toco)
3Measurement label (DFHR3)
4Measurement label (FHR1)
5Measurement label (SpO2)
6Measurement label (HR)
71mV scale bar
8MECG wave with maternal label
9DECG wave with fetal label
10 Measurement label (Temp) maternal temperature
11 Measurement label NBP
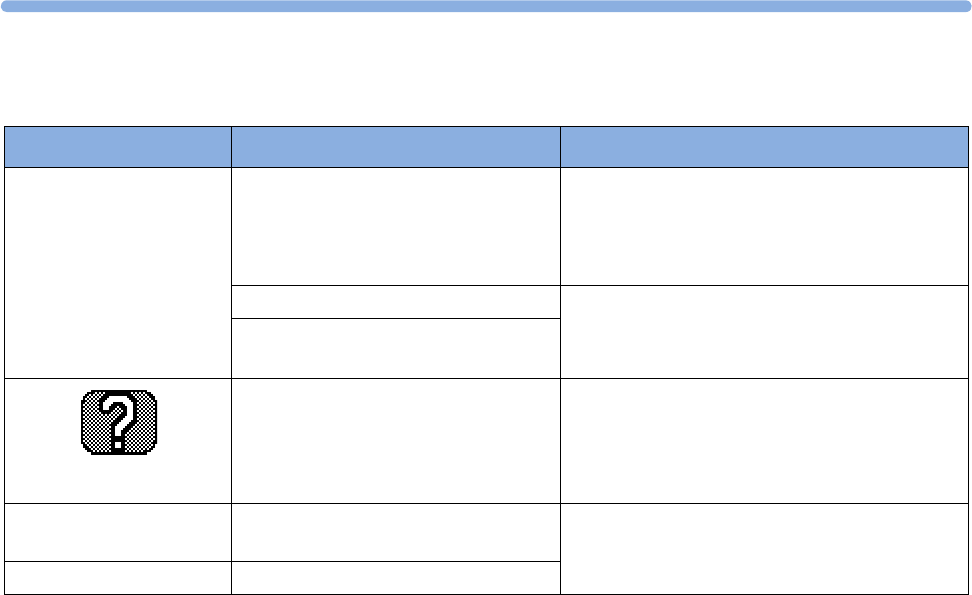
21
229
Troubleshooting
Printing the Waveform
You can print the MECG wave onto the trace paper. Refer to “Printing the ECG Waveform” on
page 233.
Pulse Rate from Toco MP
The maternal pulse is taken from the Toco MP or CL Toco+MP transducer when SpO2 or MECG
measurements are not used or have signal loss. When the pulse rate is very low, or strong arrhythmia is
present, the pulse rate measured by the Toco MP or CL Toco+MP transducer may differ from the
heart rate calculated from MECG. If the mother is moving about, or began pressing during the second
stage of labor, this can cause longer gaps in the recording of the maternal pulse signal. In this case use
the SpO2 or MECG measurement to derive the maternal heart rate.
Problem Possible Causes Solutions
MECG Leads Off
displayed.
Numeric is displayed with
a -?- for 10 seconds;
INOP tone
See also “Patient Alarms
and INOPs” on page 121
One or more MECG leads is not
attached.
Make sure that all required leads are attached
If the wave is configured to be displayed on the
monitor, you can observe if the ECG signal is
clear, or if it shows interruptions and noise
Bad electrical contact Check positioning of the electrode, ensuring that
none are displaced
Check electrodes and replace if necessary
Electrodes defective
prints repeatedly
The ultrasound transducer is
measuring maternal pulse.
Reposition the ultrasound transducer. See
“Recommended Actions for INOP
Coincidence” on page 154
MECG Equip Malf
displayed
Equipment malfunctions See “Patient Alarms and INOPs” on page 121.
MECG Unplugged Equipment not connected
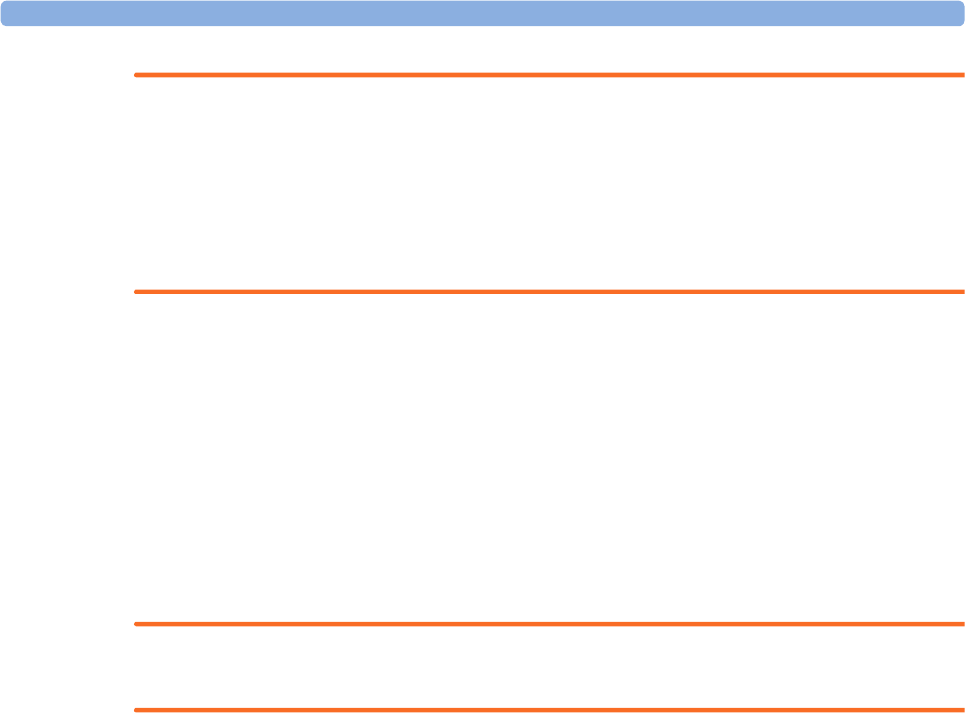
21 Monitoring Maternal Heart / Pulse Rate
230
WARNING
• No alarm is possible when Toco MP or CL Toco+MP transducer is the source of the pulse rate.
• No QRS tone is audible when Toco MP or CL Toco+MP transducer is the source of the pulse
rate.
• The Toco MP or CL Toco+MP transducer signal is significantly less reliable if the patient is up
and moving about, or is pushing during the second stage of labor.
NOTE
In rare cases it is possible to pick up a fetal signal source. When a Toco MP or CL Toco+MP
transducer is connected to the monitor but not applied to the patient, the measurement may generate
unexpected intermittent pulse readings.
Pulse Rate from SpO2
If you are not monitoring MHR via MECG electrodes, but you are monitoring SpO2, the maternal
pulse rate is derived from the SpO2 measurement. The pulse numeric is labeled Pulse on the screen.
WARNING
No QRS tone is audible when the CL SpO2 Pod is the source of the pulse rate.
Adjusting the Heart Rate / Pulse Alarm Limits
To adjust the pulse alarm limits for SpO2:
1In the Setup SpO₂ menu, select Pulse (SpO₂). This opens the Setup Pulse (SpO₂) menu.
2Ensure Pulse (SpO₂) is On. Select Pulse (SpO₂) to toggle between On and Off.
3Set the pulse alarm limit:
– Select High Limit then choose the upper alarm limit for tachycardia from the pop-up list.
– Select Low Limit then choose the lower alarm limit for bradycardia from the pop-up list.
To adjust the pulse alarm limits for MECG:
1In the Setup MECG menu, select MECG/Pulse Alarms. This opens the Setup Pulse (MECG) menu.
2Ensure Pulse MECG is On. Select Pulse MECG to toggle between On and Off.
3Set the pulse alarm limit.
– Select High Limit then choose the upper alarm limit for tachycardia from the pop-up list.
– Select Low Limit then choose the lower alarm limit for bradycardia from the pop-up list.
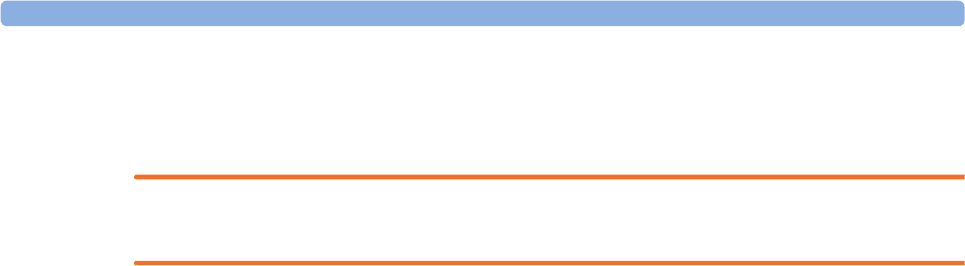
21 Monitoring Maternal Heart / Pulse Rate
231
Average Pulse Rate from Noninvasive Blood
Pressure
WARNING
No alarm is possible when noninvasive blood pressure is the source of the pulse rate.
When you are measuring noninvasive blood pressure, the monitor can also calculate the average pulse
rate. This occurs in either manual or automatic mode, when neither MECG, SpO2 nor pulse from
Toco MP or CL Toco+MP transducer are measured. The value is displayed on the screen, and printed
on the trace. It is not the actual pulse value, but an average pulse rate, taken during the most recent
noninvasive blood pressure measurement. The value is updated after each successive measurement. If
you need a continuous measurement, you should monitor using MECG, SpO2 or pulse from Toco MP
or CL Toco+MP transducer.
Testing MECG Mode
See the monitor's Service Guide.

21 Monitoring Maternal Heart / Pulse Rate
232
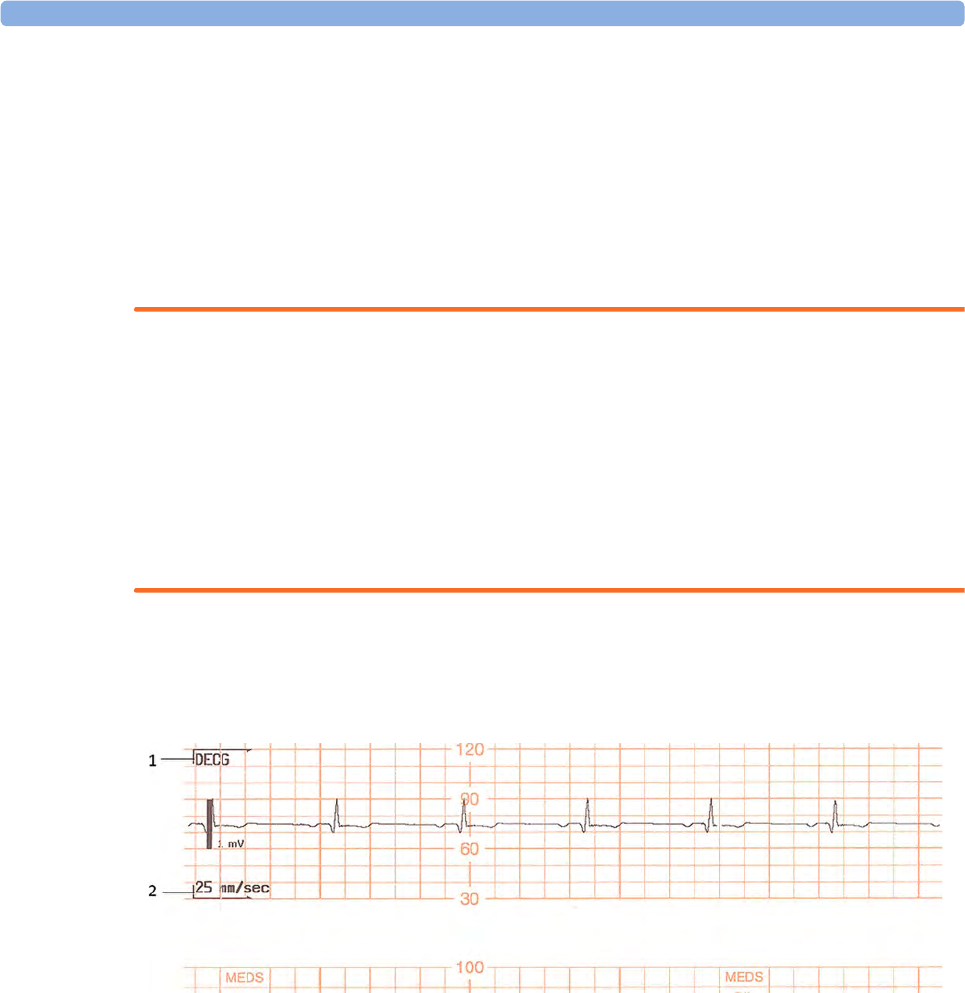
22 Printing the ECG Waveform
233
22Printing the ECG Waveform
FM30/50 You can print the ECG wave onto the trace paper. If you are monitoring both DECG and MECG,
both waves will be printed. The start of the wave recording is annotated above the wave with MECG
for Maternal ECG, with DECG for Direct fetal ECG, and with 25 mm/sec below the wave.
WARNING
The fetal/maternal monitor is not a diagnostic ECG device. In particular, the display of fetal/maternal
ECG is intended only for evaluating signal quality for fetal/maternal heart rate as derived from the
ECG waveform.
When in doubt, it can be used to identify sources of compromised signal quality, such as noise or
muscle artifacts. It can subsequently be used to verify the result of measures taken to resolve them
(e.g., checking ECG cable connections or adapting the fetal ArtifactSuppress configuration).
The safety and effectiveness of the displayed fetal/maternal ECG waveform (i.e., P, QRS and T
segments) for evaluation of fetal/maternal cardiac status during labor have not been evaluated.
The ECG waveform is printed along the bottom of the heart rate grid, and the three different
possibilities look like this:
DECG waveform on its own
1DECG
2Paper speed
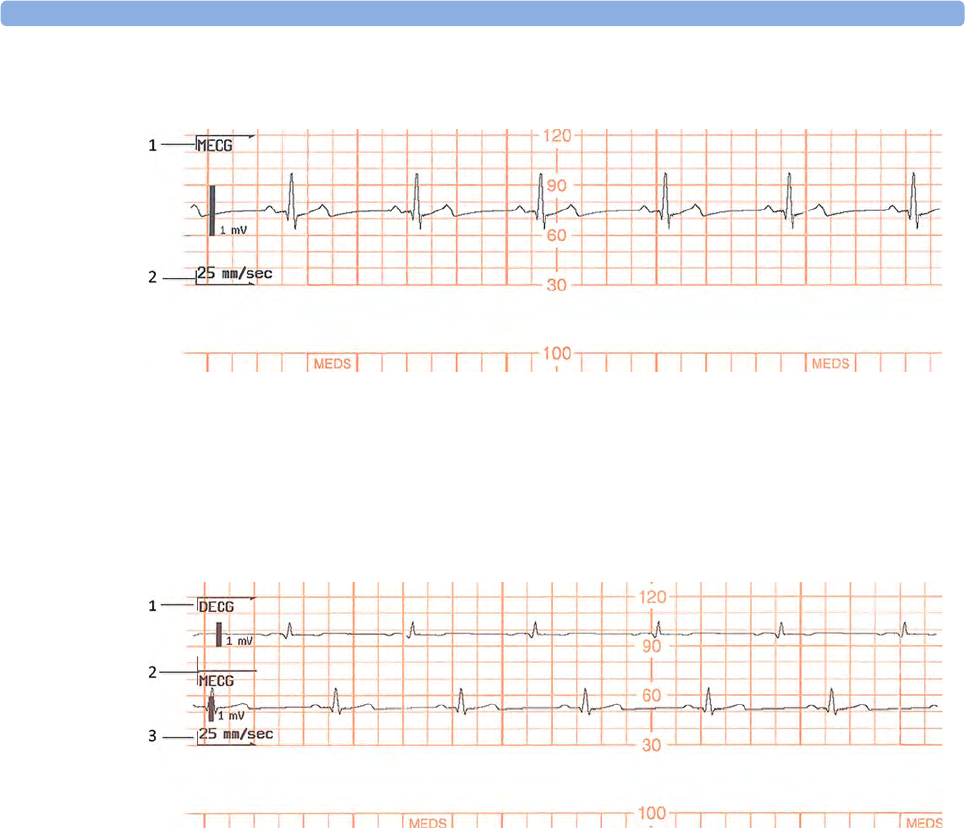
22 Printing the ECG Waveform
234
MECG waveform on its own
DECG and MECG waveforms
When the recorder is on, there are two choices for printing the ECG wave:
•Separate: This recording mode gives you a six-second ECG strip on the fetal trace paper in fast
printout mode. The real-time fetal trace recording is temporarily interrupted while the ECG strip
1MECG
2Paper speed
1DECG
2Paper speed
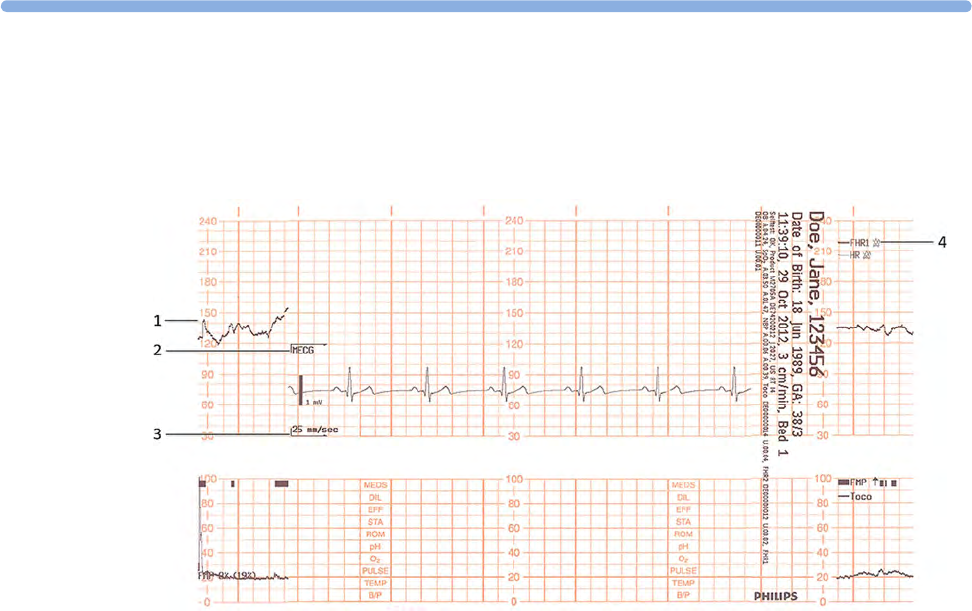
22
235
prints. A new trace header is printed out to mark where the MECG print-out starts and another
FHR header mark signals when the fetal trace resumes.
The following trace shows the MECG waveform:
•Overlap: This recording mode gives you a delayed six-second snapshot of the maternal and/or
direct fetal ECG for documentation on the fetal strip, but without interrupting the fetal trace. It
takes 5 minutes to print this six-second snapshot at a recorder speed of 3 cm/min. It is
documented as if it was recorded at 25 mm/s.
1FHR1 trace interrupted
2MECG header
3Paper speed
4FHR1 trace resume
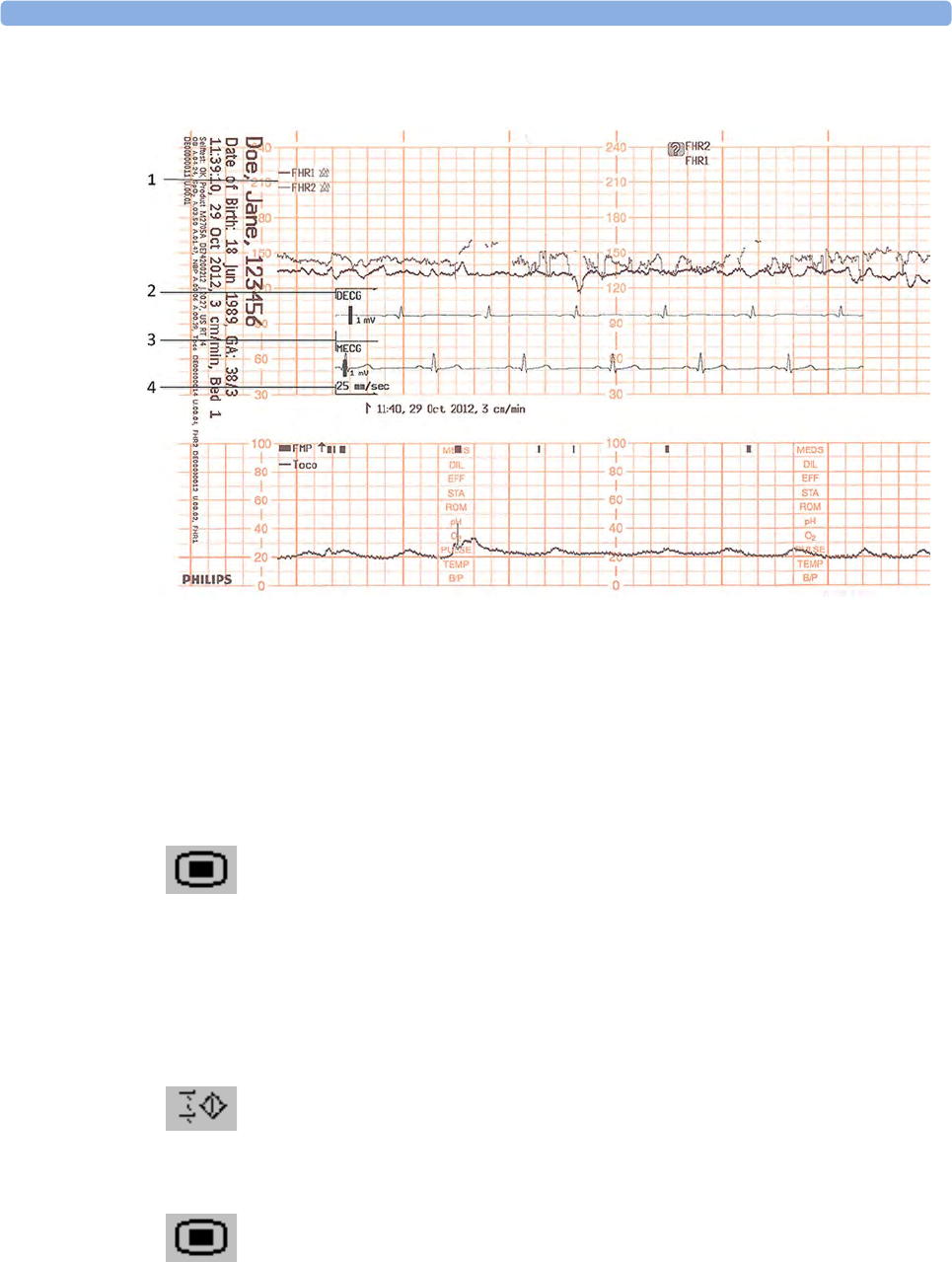
22 Printing the ECG Waveform
236
The following trace shows both the DECG and MECG waveforms:
To make your choice:
1Enter the Main Setup menu.
2Select Fetal Recorder to enter the Fetal Recorder menu.
3Select ECG Wave to toggle between Separate and Overlap.
To print the ECG wave(s):
Either
Select the Record ECG Wave SmartKey.
Or
1Enter the Main Setup menu by selecting the SmartKey.
2Select Fetal Recorder to enter the Fetal Recorder menu.
3Select Record ECG Wave.
1FHR1 and FHR2
2DECG header
3MECG header
4Paper speed

22
237
Or
1Select the ECG Wave.
2Select Record ECG Wave in the ECG wave menu.

22 Printing the ECG Waveform
238
23 Paper Save Mode for Maternal Measurements
239
23Paper Save Mode for Maternal
Measurements
Your monitor's recorder features a Paper Save Mode, where maternal vital signs are recorded using less
paper than during a normal trace recording.
When Paper Save Mode is enabled, and if the recorder is stopped, it will start automatically to print
data from maternal measurements as they occur, and then stop again to save paper. You enable Paper
Save Mode in Configuration Mode (default is off).
• A header is printed first before the measurements are recorded. A new header is also printed when
there is a date change at midnight.
• Each NBP measurement is recorded. The time when the measurement ended is recorded.
• Each Temperature measurement is recorded. The time when the measurement ended is recorded.
• Other maternal parameters (SpO2, maternal heart rate or Pulse) are recorded every five minutes.
The rules described in the section “Priority for Maternal Heart / Pulse Rate” on page 223 apply.
• Paper Save Mode recording stops if there are no valid maternal measurements for more than one
hour, and a message will notify you that there are no active parameters. Paper Save Mode recording
will restart automatically when another valid measurement is made.
Event Paper Save Mode
Reactivation
One of the maternal measurements (see above) is valid again. yes
The recorder is turned on and off again or a report has been recorded
(e.g. NST Report).
yes
The Paper Advance function is used. yes
The Paper Save Mode setting is set off and on again. yes
ADT information has changed (e.g. because patient information has
been completed or updated).
no
The monitor is restarted (e.g. by switching it off and on again). yes
The date has changed (e.g. at midnight). no

23 Paper Save Mode for Maternal Measurements
240
24
241
24Recovering Data
The monitor stores trace data, including annotations, in its internal backup memory. This allows the
monitor to recover trace data that would otherwise be lost under certain circumstances. This trace
recovery data can be automatically retrieved and printed in the event of the paper running out, or
automatically transmitted to an OB TraceVue/IntelliSpace Perinatal system (LAN connection only),
allowing continuity of data.
The fetal trace printed from the trace recovery data contains all data from the real-time trace, with the
exception of the maternal heart rate, the pulse numeric and the MECG wave.
Note that the data in the memory is cleared when a software upgrade is performed.
CAUTION
Only use Philips paper. Using paper other than Philips paper may result in the failure to recover traces.
Recovering Traces on Paper
The monitor is able to recover traces by printing them out at a high speed from the monitor's backup
memory. If the monitor runs out of paper, or if the paper drawer is open, the exact time when this
happens is annotated in the backup memory. If the Bridge Paperout setting is set to On (default),
when new paper is loaded and the recorder is started, a trace recovery printout of the data recovered
from the backup memory is automatically printed out at high speed (up to 20 mm/s), starting from the
time noted in the backup memory. This ensures that no data is lost. A minimum of one hour of trace
recovery data can be printed out from the backup memory. When the trace recovery printout has
finished, the recorder automatically switches back to continue recording the current trace at the normal
speed.
Note the following:
• If you press the fetal recorder Start/ Stop SmartKey during a trace recovery printout, the
recording stops and the next recording following a recorder restart will be a normal, real-time
trace.
After switching the monitor off and then back on again, or following a power failure, the time of
the last Check Paper INOP or paper-out detection is lost, and therefore any trace recovery data in
the backup memory is no longer available to print. The next recording made following a restart of
the recorder is a normal, real-time trace.
24 Recovering Data
242
• The change back to a real-time recording from a trace recovery printout prompts the recording to
restart. A new vertical trace header annotation consisting of the time, date and paper speed is
printed, letting you see where the trace recovery printout ends, and where the real-time trace
continues.
• There can be a gap of up to 30 seconds between the trace recovery printout and the beginning of
the real-time trace.
Recovering Traces on an OB TraceVue/IntelliSpace
Perinatal System
The trace recovery data stored in the monitor's backup memory can also be uploaded at high speed to
an OB TraceVue/IntelliSpace Perinatal system connected over the LAN interface (OB TraceVue
Revision E.00.00 or later, and IntelliSpace Perinatal H.0 or later).
When the OB TraceVue/IntelliSpace Perinatal system reconnects to the fetal monitor and detects that
there is trace recovery data in the monitor's backup memory that has not yet been transmitted to the
system, this data is transferred at high speed to the system. No user action is required.
The exact length of the recovered trace will vary depending on the amount of trace information, but
will cover at least one hour of trace data, regardless of how many parameters are being measured.
To recover traces on an OB TraceVue/IntelliSpace Perinatal system, the following applies:
• The trace data in the monitor's internal memory must relate to a specific patient in the OB
TraceVue/IntelliSpace Perinatal system. In other words, there were no discharge events made on
the monitor that would change the patient context.
• The patient must have an open episode. No data will be uploaded if the patient is not admitted to
OB TraceVue/IntelliSpace Perinatal. For this reason, it is not possible to use the monitor to collect
patient data offline for later transmission to OB TraceVue/IntelliSpace Perinatal.
• Current online trace data is held back until the fast upload is complete.
Recording Stored Data
If the recorder is not running, you can choose to print trace data from the monitor's memory at any
time. You can see a list of all stored traces, showing patient identification and trace period, in the
Stored Data Recording window, from which you can choose one entry at a time.
CAUTION
Ensure that you admit each patient by name, including other patient identification information, and
discharge the patient when you have finished monitoring, so that you can identify which trace period
(entry in the patient list) refers to which patient.
Trace storage can be triggered by:
• Discharging a patient
• Powering on the monitor
•Entering Standby
• Entering Service Mode
24 Recovering Data
243
Traces are not available for periods the monitor was switched off, in Service mode, in Standby, or if
the trace period was shorter than one minute. To delete all stored trace periods press the Erase All key.
The speed of the printout depends on the configured recorder speed and on the amount of trace data
available. The fetal trace printed from the trace data contains all data from the real-time trace, with the
exception of the maternal heart rate, the pulse numeric and the ECG wave.
Information for scale type, trace separation and recorder speed are not stored in the trace memory, but
is applied when the stored recording starts. While the stored recording is printing, all functions are
disabled, except that for stopping the recorder.
To start a stored data recording:
Either
1Select the Stored Data Rec SmartKey.
Or
1Enter the Main Setup menu using the SmartKey.
2Select Fetal Recorder to open the Fetal Recorder menu.
3Select Stored Data Rec to open the Stored Data Recording window.
4Select an entry for a patient.
5Select All to print all stored trace data for the selected entry, or select one of the choices on the
other pop-up keys to print only a specified portion of the entry (for example, Last 15 min for the
last 15 minutes of trace data).
To delete all stored trace periods:
Either
1Select the Stored Data Rec SmartKey.
Or
1Enter the Main Setup menu using the SmartKey.
2Select Fetal Recorder to open the Fetal Recorder menu.
3Select Stored Data Rec to open the Stored Data Recording window.
4Select the Erase All key to delete all stored trace periods listed.
5Select the Confirm key.
The current patient’s entry is at the top of the list. The oldest entry at the bottom of the list has no start
time specified, as part of the data originally stored may have been over-written by the current patient’s
data. The first part of the data, including the information for the start time, is no longer accessible.

24 Recovering Data
244
It may be that you only see one entry (the current patient’s data) in the Stored Data Recording
window if that patient was monitored for a period long enough to erase any earlier entries.
If you make a stored data recording for an old entry (that is, not for the current patient), the recorder
performs a fast trace printout of the stored data, advances the paper to the next paper fold, then stops.
If you make a stored data recording for the current patient, the recorder performs a fast trace printout
of the stored data, and then reverts automatically to recording the real-time trace.

25
245
25Care and Cleaning
Use only the Philips-approved substances and methods listed in this chapter to clean or disinfect your
equipment. Warranty does not cover damage caused by using unapproved substances or methods.
Philips makes no claims regarding the efficacy of the listed chemicals or methods as a means for
controlling infection. Consult your hospital’s Infection Control Officer or Epidemiologist. For
comprehensive details on cleaning agents and their efficacy refer to “Guideline for Disinfection and
Sterilization in Healthcare Facilities” issued by the U.S. Department of Health and Human Services,
Public Health Service, Centers for Disease Control, Atlanta, Georgia, 2008. See also any local policies
that apply within your hospital, and country.
General Points
The transducers and patient modules are sensitive instruments. Handle them with care.
Keep your monitor, transducers, patient modules, cables and accessories free of dust and dirt. After
cleaning and disinfection, check the equipment carefully. Do not use if you see signs of deterioration
or damage. If you need to return any equipment to Philips, always decontaminate it first before
sending it back in appropriate packaging.
Observe the following general precautions:
• Always follow carefully and retain the instructions that accompany the specific cleaning and
disinfecting substances you are using.
• Always dilute according to the manufacturer's instructions or use lowest possible concentration.
• Do not allow liquid to enter the case.
• Do not immerse the monitor in liquid. Protect it against water sprays or splashes.
• Do not pour liquid onto the system.
• Never use abrasive material (such as steel wool or silver polish).
• Never use bleach.

25 Care and Cleaning
246
WARNING
• Do not operate the monitor if it is wet. If you spill liquid on the monitor, contact your service
personnel or Philips service engineer.
• Do not perform underwater monitoring (for example, in a bath or shower) using wired
transducers.
• Place the monitor where there is no chance of contact with, or falling into water or other liquid.
• Do not dry equipment using heating devices such as heaters, ovens (including microwave ovens),
hair dryers and heating lamps.
• Do not put equipment or accessories in autoclave (for sterilization).
Cleaning and Disinfecting
Clean and disinfect the Avalon FM20, FM30, FM40 and FM50 fetal monitors and the transducers
M2734A, M2734B, M2735A, M2736A, and M2738A (including ECG adapter cables) and the
Avalon CL base station and the cableless transducers after each use. Clean equipment before
disinfecting. For other accessories, see “Cleaning and Disinfecting Monitoring Accessories” on
page 247.
Clean with a lint-free cloth, moistened with warm water (40°C/104°F maximum) and soap, a diluted
non-caustic detergent, tenside, or phosphate based cleaning agent (see “Recommended Disinfectants”
on page 247). Do not use strong solvents such as acetone or trichloroethylene. After cleaning, disinfect
using only the approved disinfecting agents listed.
CAUTION
Solutions: Do not mix disinfecting solutions (such as bleach and ammonia) as hazardous gasses may
result.
Skin contact: To reduce the risk of skin irritations, do not allow a cleaning or disinfecting agent to
leave residues on any of the equipment surfaces - wipe it off with a cloth dampened with water, after
allowing the appropriate time for the agent to work, or before applying to a patient.
Hospital policy: Disinfect the product as determined by your hospital's policy, to avoid long term
damage to the product.
Local requirements: Observe local laws governing the use of disinfecting agents.
Touch display: To clean and disinfect the touch-enabled display, disable the touch operation by
switching off the monitor during the cleaning procedure, or by selecting and holding the Main Screen
key until the padlock symbol appears on it, indicating that touch operation is disabled. Select and hold
again to re-enable touch operation.
Take extra care when cleaning the screen of the monitor because it is more sensitive to rough cleaning
methods than the housing. Do not permit any liquid to enter the monitor case and avoid pouring it on
the monitor while cleaning. Do not allow water or cleaning solution to enter the measurement
connectors. Wipe around and not over connector sockets, or those of the Toco+, CL Toco transducer,
ECG and IUP Patient Modules, CL ECG/IUP transducer and adapter cables.
Wash soiled reusable belts with soap and water. Water temperature must not exceed 60°C/140°F.
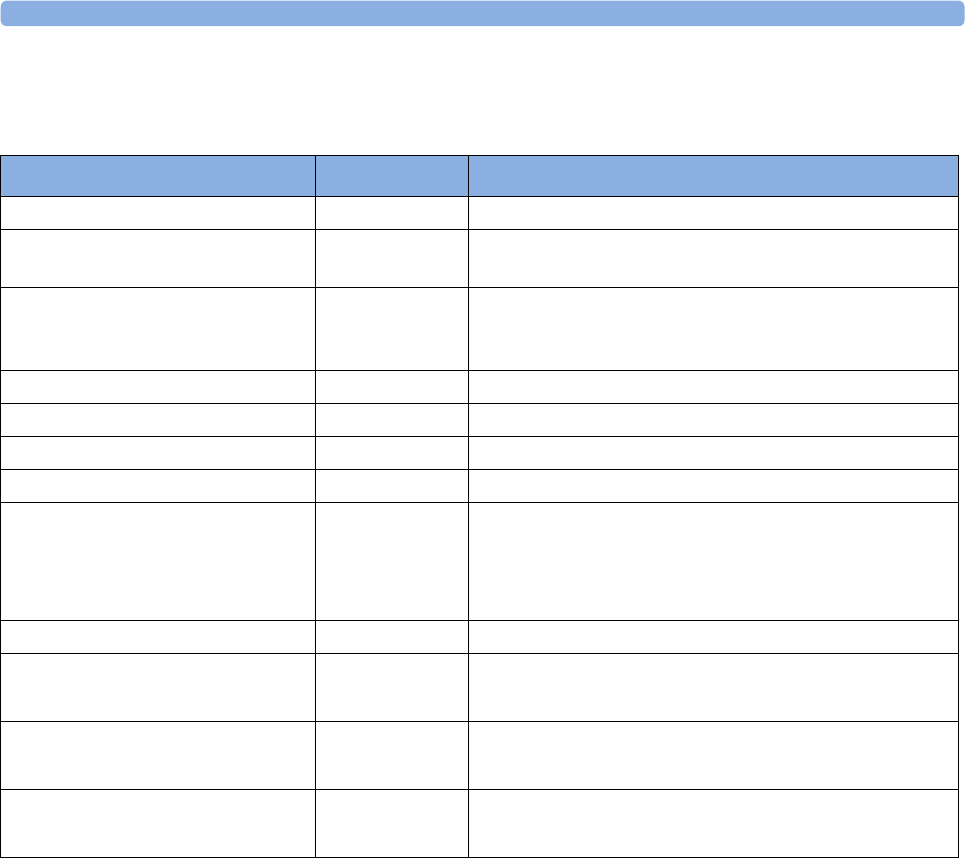
25 Care and Cleaning
247
Recommended Disinfectants
We recommend that you use one of the following disinfectants:
Cleaning and Disinfecting Monitoring Accessories
To clean, disinfect and sterilize reusable transducers, sensors, cables, leads, and so forth, refer to the
instructions delivered with the accessory.
Do not allow a cleaning or disinfecting agent to leave residues on any of the equipment surfaces. Wipe
residues off, after allowing the appropriate time to for the agent to work, with a cloth.
Product Name Product Type Ingredients
Isopropanol liquid Isopropanol 80%
Bacillol® AF liquid, spray 100 g concentrate contains:
Propan-1-ol 45.0 g; Propan-2-ol 25.0 g; Ethanol 4.7 g.
Bacillol®25 liquid Ethanol 100 mg/g
Propan-2-ol (= 2-Propanol) 90 mg/g; Propan-1-ol (= 1-
Propanol) 60 mg/g
Meliseptol® spray 50% 1-Propanol
Accel TB RTU liquid 0.5% accelerated hydrogen peroxide
Oxivir® Tb Cleaner Disinfectant spray 0.5% accelerated hydrogen peroxide
Oxivir® Tb Wipes wipes 0.5% accelerated hydrogen peroxide
Carpe DiemTM/MC Tb
Ready-to-Use General Virucide,
Bactericide, Tuberculocide,
Fungicide, Sanitizer
spray 0.5% accelerated hydrogen peroxide
Carpe DiemTM/MC Tb Wipes wipes 0.5% accelerated hydrogen peroxide
Super Sani-Cloth
Germicidal Disposable Wipes
wipes isopropanol 55%
quaternary ammonium chlorides 0.5%
SANI-CLOTH® PLUS
Germicidal Disposable Wipes
wipes isopropanol 15%
quaternary ammonium chlorides 0.25%
SANI-CLOTH® HB Germicidal
Germicidal Disposable Wipes
wipes isopropanol < 0.15%
quaternary ammonium chlorides 0.14%
25 Care and Cleaning
248
Cleaning and Disinfecting the Tympanic
Temperature Accessories
Probe and Thermometer Body
1Wipe the thermometer body clean with a damp cloth. The water temperature should not exceed
55°C (130°F). Do not soak, rinse, or submerge the thermometer under water.
You may add a mild detergent to the water.
2Clean the probe tip with a lint free swab. If the probe tip is soiled, clean it with a dampened swab.
3After you have removed all foreign matter, clean the thermometer lens at the end of the probe tip
with a lint free swab or lens wipe. The thermometer lens must be free from fingerprints and/or
smudges for proper operation.
4Thoroughly dry all surfaces before using the equipment.
CAUTION
Do not use cleaners and disinfectants such as Spray-Nine™*, Phisohex™*, Hibiclens™*, or Vesta-
Syde™* as they may result in damage to the thermometer case.
Occasional use of a 10:1 water and hypochlorite mixture or a damp isopropyl alcohol wipe or
Cidex™* or ManuKlenz™* or VIROX™* or CaviWipes™* cleansing agents is acceptable, however,
prolonged or repeated use of these chemicals may result in damage to the thermometer case and
display area.
Use of a cloth or sponge is recommended for cleaning. Never use an abrasive pad or an abrasive
cleaner on the thermometer.
The thermometer is non-sterile. Do not use ethylene oxide gas, heat, autoclave, or any other harsh
method to sterilize this thermometer.
Sterilizing
Sterilization is not recommended for this monitor, related products, accessories or supplies unless
otherwise indicated in the Instructions for Use that accompany the accessories and supplies.
WARNING
Do not put device and accessories in autoclave (for sterilization).
26 Maintenance
249
26Maintenance
WARNING
Schedule: Failure on the part of the responsible individual hospital or institution employing the use of
this equipment to implement a satisfactory maintenance schedule may cause undue equipment failure
and possible health hazards.
In case of problems: If you discover a problem with any of the equipment, contact your service
personnel, Philips, or your authorized supplier.
Electric shock hazard: Do not open the monitor housing. Refer all servicing to qualified service
personnel.
Inspecting the Equipment and Accessories
You should perform a visual inspection before each use, and in accordance with your hospital's
policy. With the monitor switched off:
1Examine unit exteriors for cleanliness and general physical condition. Make sure that the housings
are not cracked or broken, that everything is present, that there are no spilled liquids that may have
entered the housing, and that there are no signs of abuse.
2Inspect all accessories (transducers, sensors and cables, and so forth). Do not use a damaged
accessory.
3Avoid frequent drops of the transducers.
4Switch the monitor on and make sure the display is bright enough. If the brightness is not
adequate, contact your service personnel or your supplier.
Batteries Preventive Maintenance
For the FM20/30 with a battery option refer to “Using Batteries” on page 102.
Inspecting the Cables and Cords
1Examine all system cables, the power plug and cord for damage. Make sure that the prongs of the
plug do not move in the casing. If damaged, replace it with an appropriate power cord.
2Inspect the cables, leads and their strain reliefs for general condition. Make sure there are no
breaks in the insulation. Make sure that the connectors are properly engaged at each end to
prevent rotation or other strain.
3Carry out performance assurance checks as described in the monitor's Service Guide.
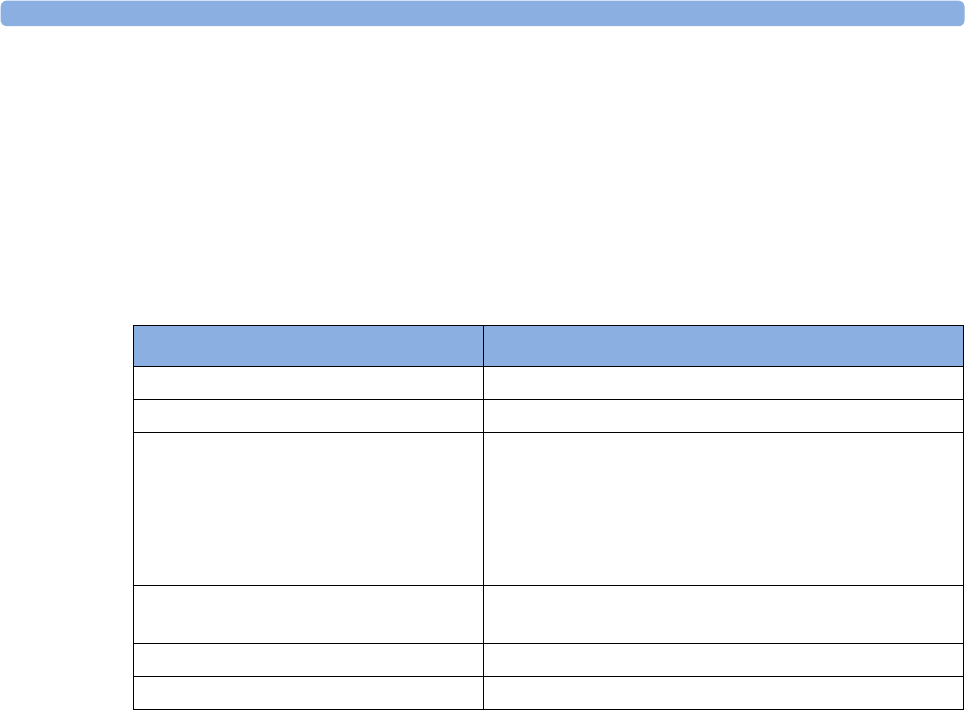
26 Maintenance
250
Maintenance Task and Test Schedule
The following tasks are for Philips-qualified service professionals. All maintenance tasks and
performance tests are documented in detail in the service documentation supplied on the monitor's
documentation DVD.
Ensure that these tasks are carried out as indicated by the monitor's maintenance schedule, or as
specified by local laws, whichever comes sooner. Contact a Philips-qualified service professionals if
your monitor needs a safety or performance test. Clean and disinfect equipment to decontaminate it
before testing or maintaining it.
Recorder Maintenance
Removing the Paper Guide: FM40/FM50
FM40/50 The paper guide is removable, and you can use the recorder without it. When not using the paper
guide, ALWAYS tear off the paper along the perforation to avoid possible paper misalignment (see
“Tearing Off the Paper” on page 80).
Maintenance and Test Schedule Frequency
Visual Inspection Before each use.
Clean and disinfect the equipment After each use.
Safety checks according to IEC 60601-1,
and where applicable, to national
standards
At least once every two years, or as specified by local laws.
After any repairs where the power supply has been
replaced (by an authorized service professional).
If the monitor has been dropped, it must be repaired/
checked by an authorized service agent.
Performance assurance for all
measurements
At least once every two years, or if you suspect the
measurement values are incorrect.
Noninvasive blood pressure calibration At least once every two years, or as specified by local laws.
Clean the thermal printhead At each paper pack change, or every 500 m of paper run.

26 Maintenance
251
To remove the paper guide:
1Press the paper eject button to
open the paper drawer.
2Hinge the transparent paper
guide forward.
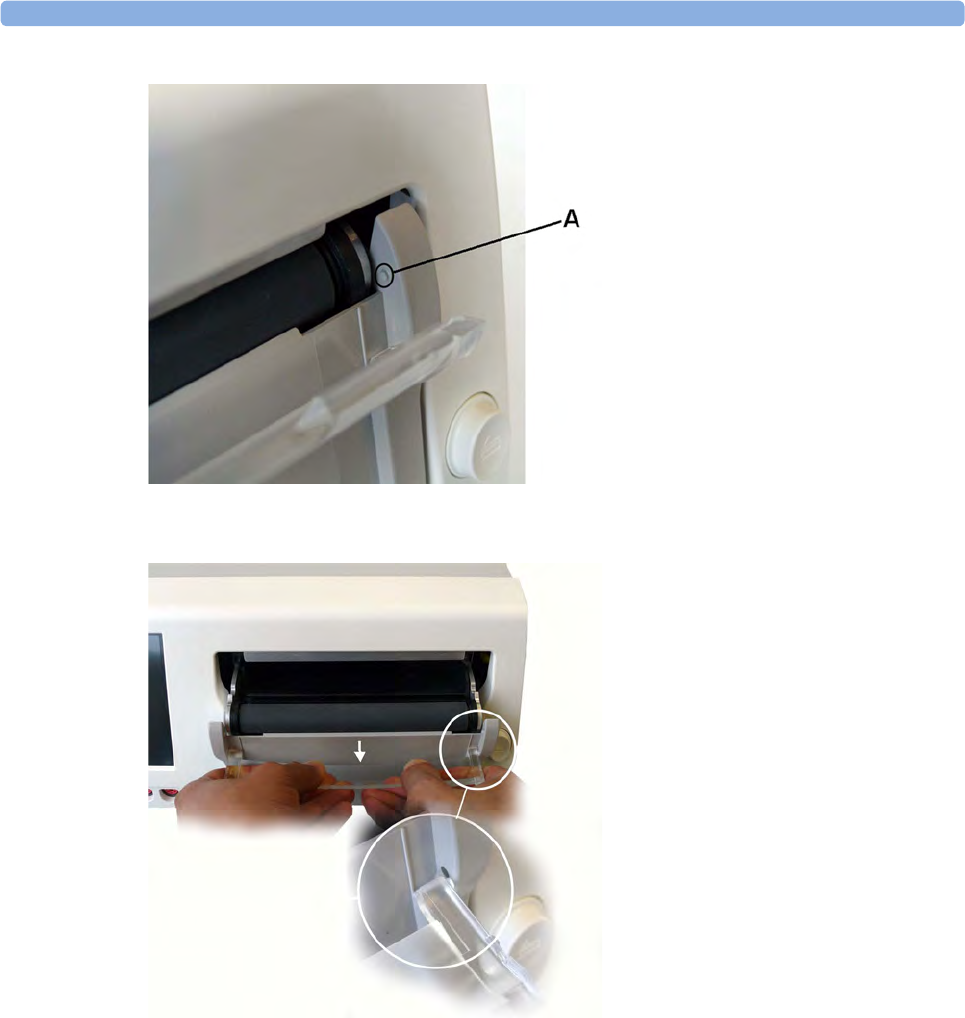
26 Maintenance
252
AProtrusion holds paper guide in
closed position.
3Release the paper guide from one
side of the holder.

26
253
4Then remove the paper guide.
Refitting is a reversal of the
removal procedure.

26 Maintenance
254
Storing Recorder Paper
Recorder paper is not intended for long-term archival storage. Another medium should be considered
if this is required.
Dyes contained in thermal papers tend to react with solvents and other chemical compounds that are
being used in adhesives. If these compounds come into contact with the thermal print, the print may
be destroyed over time. You can take the following precautionary measures to help avoid this effect:
• Store the paper in a cool, dry and dark place.
• Do not store the paper at temperatures over 40°C (104°F).
• Do not store the paper where the relative humidity exceeds 60%.
• Avoid intensive light (UV light), as this may cause the paper to turn gray or the thermal print to
fade.
• Avoid storing the thermal paper in combination with the following conditions:
– Papers that contain organic solvents. This includes papers with tributyl and/or dibutyl
phosphates, for example recycled paper.
– Carbon paper and carbonless copy paper.
– Products containing polyvinyl chlorides or other vinyl chlorides for example (but not
exclusively) document holders, envelopes, letter files, divider sheets.
– Detergents and solvents, such as alcohol, ketone, ester and others, including cleaning and
disinfecting agents.
– Products containing solvent-based adhesives such as (but not exclusively) laminating film,
transparent film or labels sensitive to pressure.
To ensure long lasting legibility and durability of thermal printouts, store your documents separately in
an air-conditioned place and use:
• only plasticizer-free envelopes or divider sheets for protection.
• laminating films and systems with water-based adhesives.
Using such protective envelopes cannot prevent the fading effect caused by other, external agents.
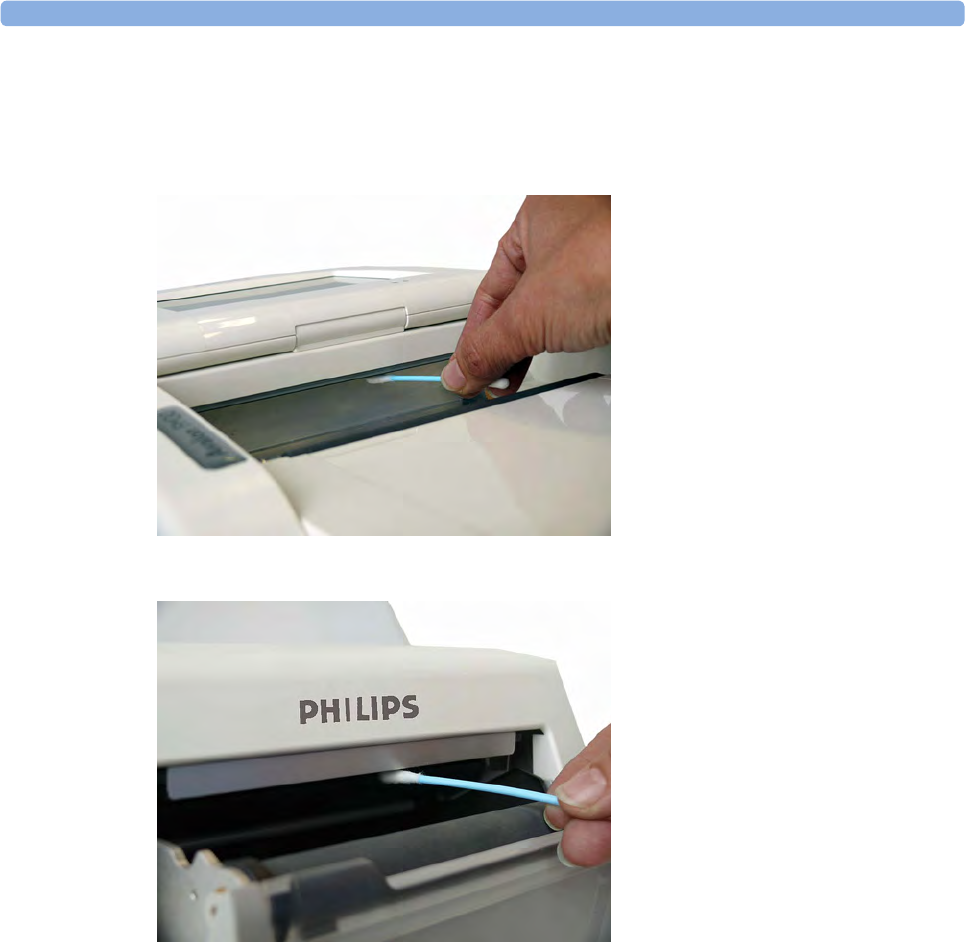
26 Maintenance
255
Cleaning the Print Head
To clean the recorder's thermal print-head:
FM20/30
1Switch off the monitor.
2Open the paper drawer, and
remove the paper if necessary, to
gain access to the thermal print
head.
3Gently clean the thermal print
head with a cotton swab or soft
cloth soaked in isopropyl
alcohol.
FM40/50
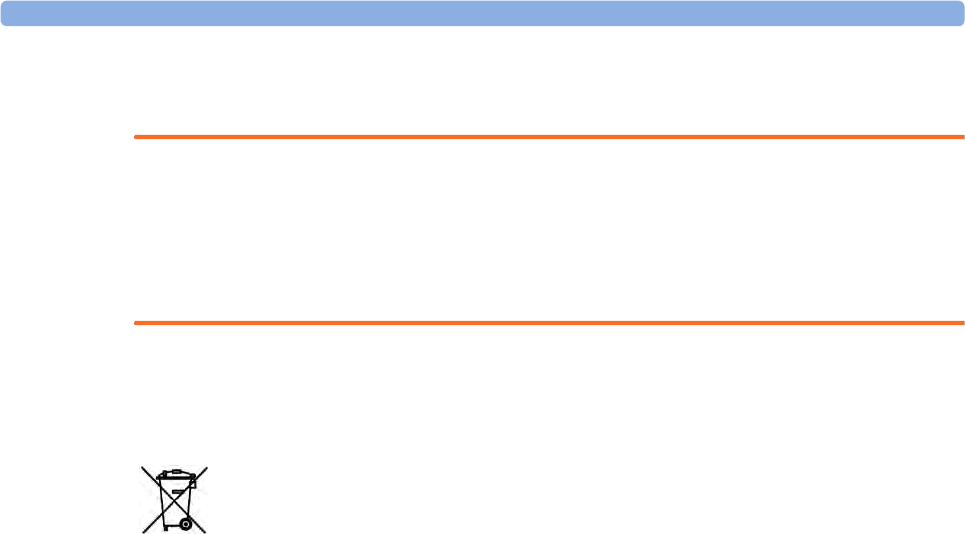
26 Maintenance
256
Disposing of the Monitor
WARNING
To avoid contaminating or infecting personnel, the environment or other equipment, make sure you
disinfect and decontaminate the monitor appropriately before disposing of it in accordance with your
country's laws for equipment containing electrical and electronic parts. For disposal of parts and
accessories such as thermometers, where not otherwise specified, follow local regulations regarding
disposal of hospital waste.
You can disassemble the monitor and the transducers as described in the Installation and Service
Manual. You will find detailed disposal information on the following web page: http://
www.healthcare.philips.com/main/about/Sustainability/Recycling/pm.wpd
The Recycling Passports located there contain information on the material content of the equipment,
including potentially dangerous materials which must be removed before recycling (for example,
batteries and parts containing mercury or magnesium).
Do not dispose of waste electrical and electronic equipment as unsorted
municipal waste. Collect it separately, so that it can be safely and properly reused,
treated, recycled, or recovered.
27 Accessories and Supplies
257
27Accessories and Supplies
All accessories listed for the fetal monitor may not be available in all geographies. You can order parts,
accessories and supplies from Philips supplies at www.healthcare.philips.com or consult your local
Philips representative for details. All accessories and supplies listed here are reusable, unless indicated
otherwise.
WARNING
Reuse: Disposable accessories and supplies intended for single use, or single patient use only, and are
indicated as such on their packaging. Never reuse disposable accessories and supplies, such as
transducers, sensors, electrodes and so forth that are intended for single use, or single patient use only.
Approved accessories: Use only Philips-approved accessories.
Packaging: Do not use a sterilized accessory if its packaging is damaged.
Protection against electric shocks: The transducers and accessories listed in this chapter are
not defibrillator proof.
Electro-Surgery, Defibrillation and MRI: The fetal/maternal monitors are not intended for use
during defibrillation, electro-surgery, or MRI. Remove all transducers, sensors, and accessories before
performing electro-surgery, defibrillation, or MRI, otherwise harm can result.
Information on Latex
All Philips transducers and accessories are latex-free, unless indicated otherwise in the following tables.
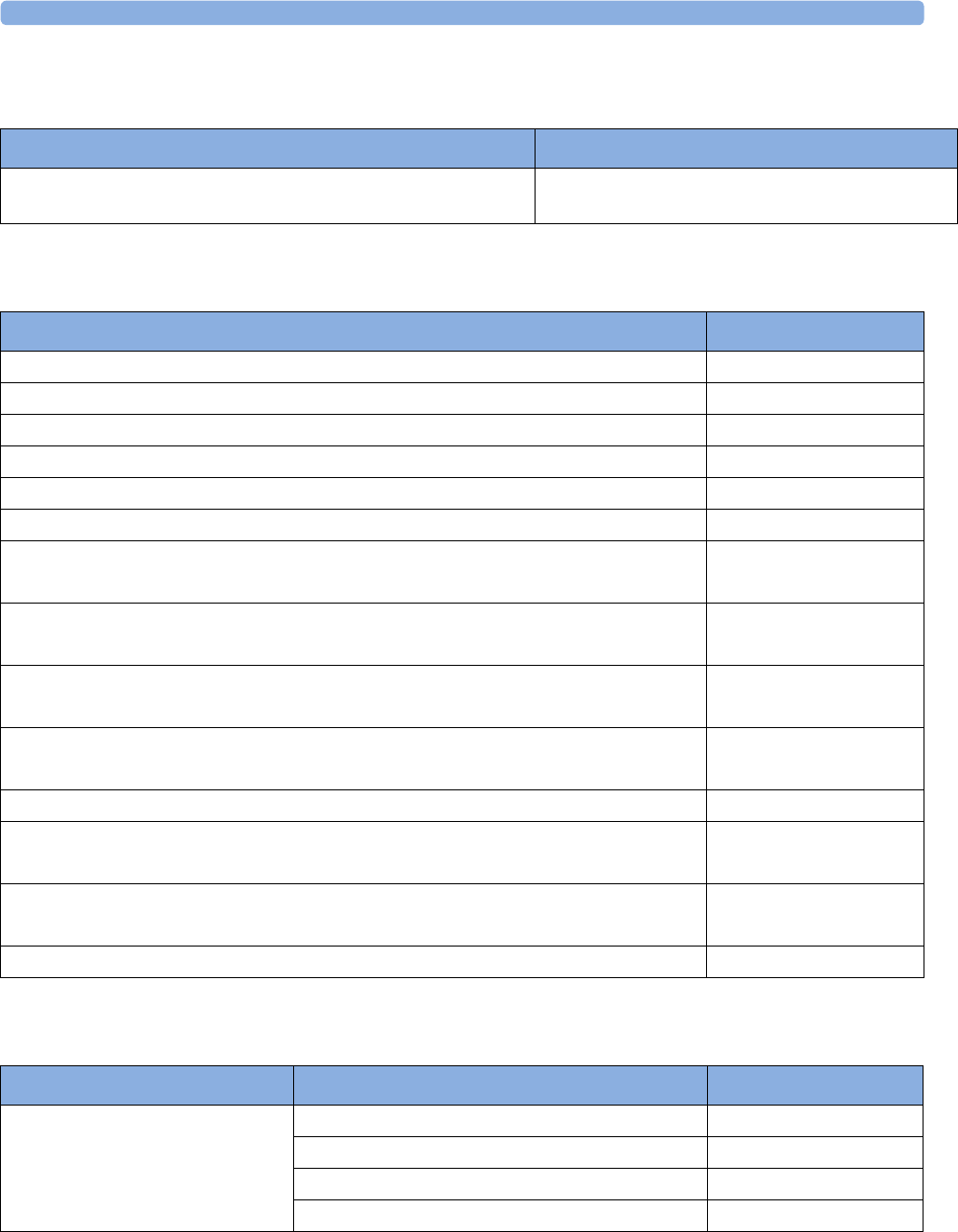
27 Accessories and Supplies
258
Avalon CL Base Station
Transducers
Fetal Accessories
CL Base Station Part Number
Avalon CL Base Station can either be ordered with the option K30
(red connector) or K40 (black connector)
866074
Transducer Part Number
Avalon Toco Transducer M2734A
Avalon Toco+ Transducer for Toco, DECG, MECG or IUP monitoring M2735A
Avalon Toco MP Transducer for Toco and Maternal Pulse M2734B
Avalon Ultrasound Transducer M2736A
Avalon Ultrasound Transducer USA M2736AA
ECG/IUP Patient Module (for DECG, MECG or IUP) M2738A
Avalon CL Toco+ MP Transducer
for use with the Avalon CL base station
866075
Avalon CL Ultrasound Transducer
for use with the Avalon CL base station
866076
Avalon CL ECG/IUP Transducer
for use with the Avalon CL base station
866077
Connector Caps for Avalon CL Cableless Smart Transducers (kit of 10)
for use with the Avalon CL Toco+ MP transducer
989803184841
Belt Clip for Avalon CL Cableless Smart Transducers (kit of 10) 989803184851
CL SpO2 Pod
for use with the Avalon CL base station
865215
CL NBP Pod
for use with the Avalon CL base station
865216
Remote Event Marker 989803143411
Accessory Description Part Number
Belt
(reusable, gray, water resistant)
32 mm wide, 15 m roll M4601A1
60 mm wide, 5 belts M4602A
60 mm wide, 15 m roll M4603A
50 mm wide, 5 belts M1562B
27 Accessories and Supplies
259
Belt
(reusable, brown, contains latex)
32 mm wide, 15 m roll 1500-06281
50 mm wide, 5 belts M1562A
60 mm wide, 5 belts 1500-0642
60 mm wide, 15 m roll 1500-0643
Belt
(disposable, yellow, water resistant)
60 mm wide, pack of 100 M2208A
Ultrasound gel 12 Bottles 40483A
5 liter refill (with dispenser) for 40483A
Shelf life: 24 months max.
40483B
Belt buttons (kit of 10) M1569A
Butterfly belt clip (kit of 6) 989803143401
Avalon CL Connector Caps Connector Caps for Avalon CL Cableless Smart
Transducers (kit of 10)
989803184841
Avalon CL Belt Clip Belt Clip for Avalon CL Cableless Smart
Transducers (kit of 10)
989803184851
Avalon CL Battery Replacement Kit 989803184861
Cable Management Kit 989803148841
Belt Clips for Avalon Smart Transducers (kit of 6) 989803143401
DECG Accessories:
New Philips DECG Solution
(NOT compatible with QwikConnect
Plus Solution accessories)
DECG reusable legplate adapter cable (with
flushing port)
989803137651
DECG leg attachment electrode for DECG legplate
adapter cable 989803139771
DECG fetal scalp electrode: single spiral, worldwide
availability
989803137631
DECG fetal scalp electrode: double spiral, Europe
only. Not for USA
989803137641
Disposable Koala IUP catheter M1333A
Reusable Koala IUP adapter cable 989803143931
Accessory Description Part Number
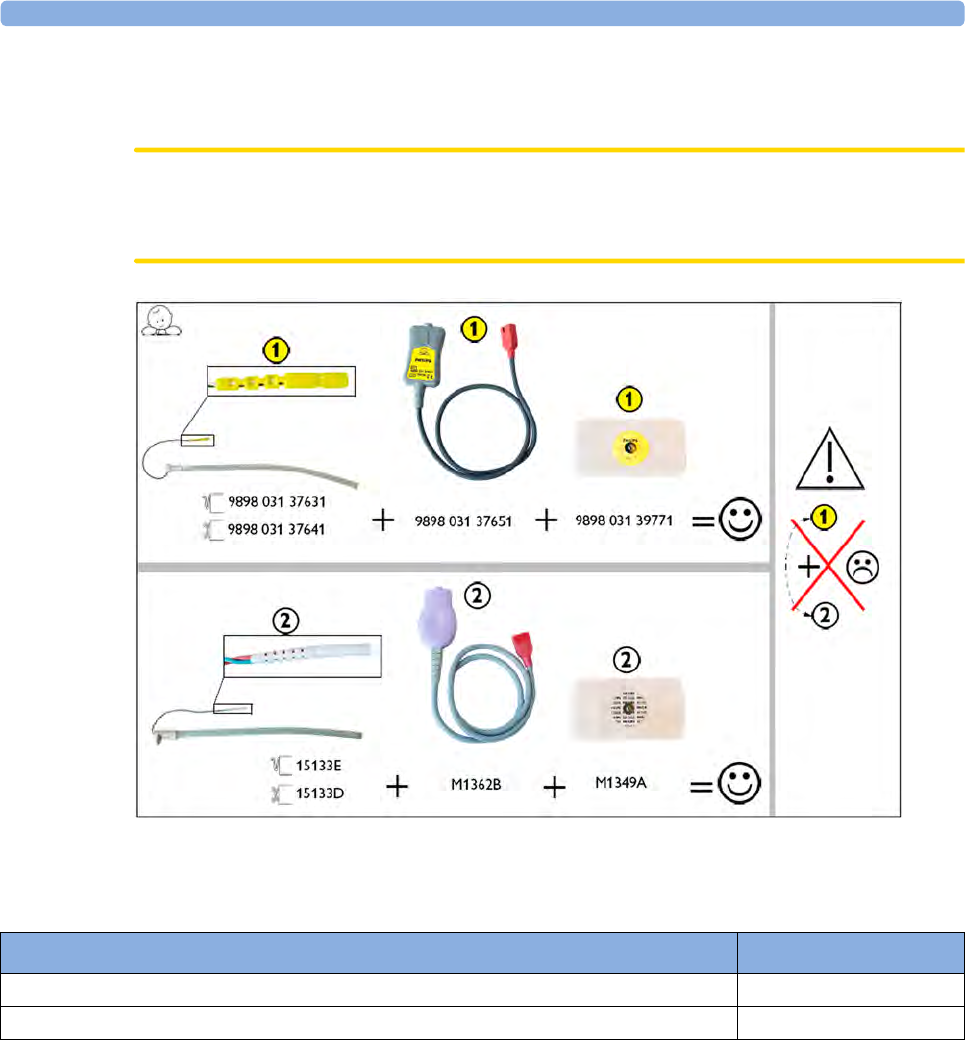
27 Accessories and Supplies
260
DECG Accessories: Component Compatibility
Use the following pictorial guide to check component compatibility for DECG accessories.
CAUTION
Do not mix accessories from the New Philips DECG Solution (marked 1) with those from the
QwikConnect Plus Solution (marked 2).
MECG Accessories
Noninvasive Blood Pressure Accessories
The following accessories are approved for use with the fetal monitor:
Accessory Part Number
MECG reusable adapter cable M1363A
Foam ECG electrodes, snap-fit, for MECG Adapter Cable (disposable) 40493D/E
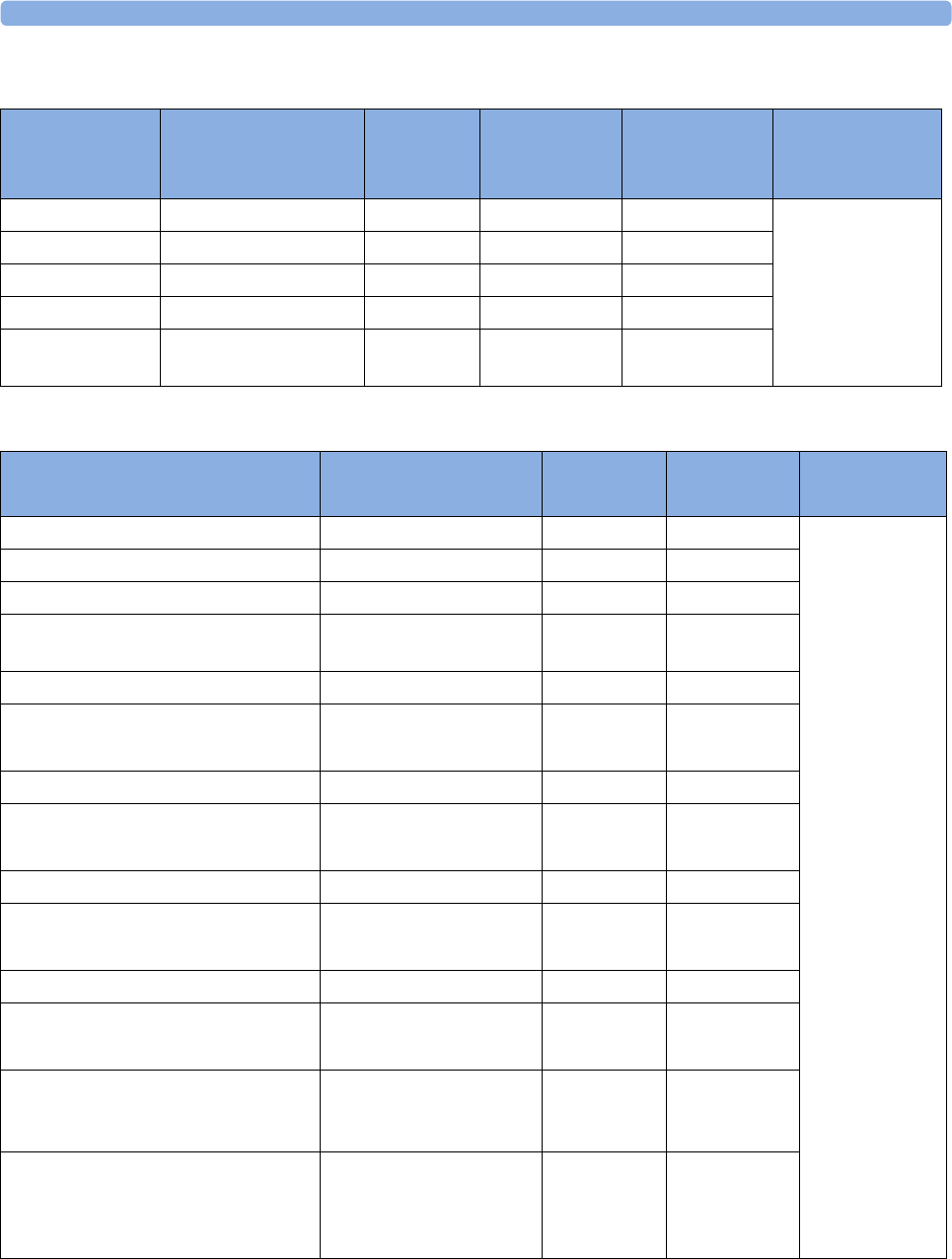
27 Accessories and Supplies
261
Adult Multi-Patient Comfort Cuffs and Disposable Cuffs
Adult EasyCare Reusable Cuffs
Maternal Patient
Category
Limb Circumference Bladder
Width
Disposable
cuff
Part No.
Reusable cuff
Part No.
Tubing
Adult (Thigh) 42.0 - 54.0 cm 20.0 cm M1879A M1576A M1598B (1.5 m)
or
M1599B (3.0 m)
Large Adult 34.0 - 43.0 cm 16.0 cm M1878A M1575A
Adult 27.0 - 35.0 cm 13.0 cm M1877A M1574A
Small Adult 20.5 - 28.0 cm 10.5 cm M1876A M1573A
Cuff kit of 4 adult
sizes
M1578A
Maternal Patient Category (color) Limb Circumference Bladder
Width
Part No. Tubing
Adult Thigh (grey) 45.0 - 56.5 cm 21.0 cm M4559B M1598B (1.5 m)
or
M1599B (3.0 m)
Adult Thigh (grey) pack of 5 cuffs 45.0 - 56.5 cm 21.0 cm M4559B5
Large Adult X-Long (burgundy) 35.5 - 46.0 cm 17.0 cm M4558B
Large Adult X-Long (burgundy) pack
of 5 cuffs
35.5 - 46.0 cm 17.0 cm M4558B5
Large Adult (burgundy) 35.5 - 46.0 cm 17.0 cm M4557B
Large Adult (burgundy)
pack of 5 cuffs
35.5 - 46.0 cm 17.0 cm M4557B5
Adult X-Long (navy blue) 27.5 - 36.5 cm 13.5 cm M4556B
Adult X-Long (navy blue)
pack of 5 cuffs
27.5 - 36.5 cm 13.5 cm M4556B5
Adult (navy blue) 27.5 - 36.5 cm 13.5 cm M4555B
Adult (navy blue)
pack of 5 cuffs
27.5 - 36.5 cm 13.5 cm M4555B5
Small Adult (royal blue) 20.5 - 28.5 cm 10.6 cm M4554B
Small Adult (royal blue)
pack of 5 cuffs
20.5 - 28.5 cm 10.6 cm M4554B5
Cuff kits containing one small adult,
one adult, one large adult and one
thigh cuff.
864288
Cuff kits containing one small adult,
one adult, one adult X-long, one large
adult, one large adult X-long and one
thigh cuff
864291
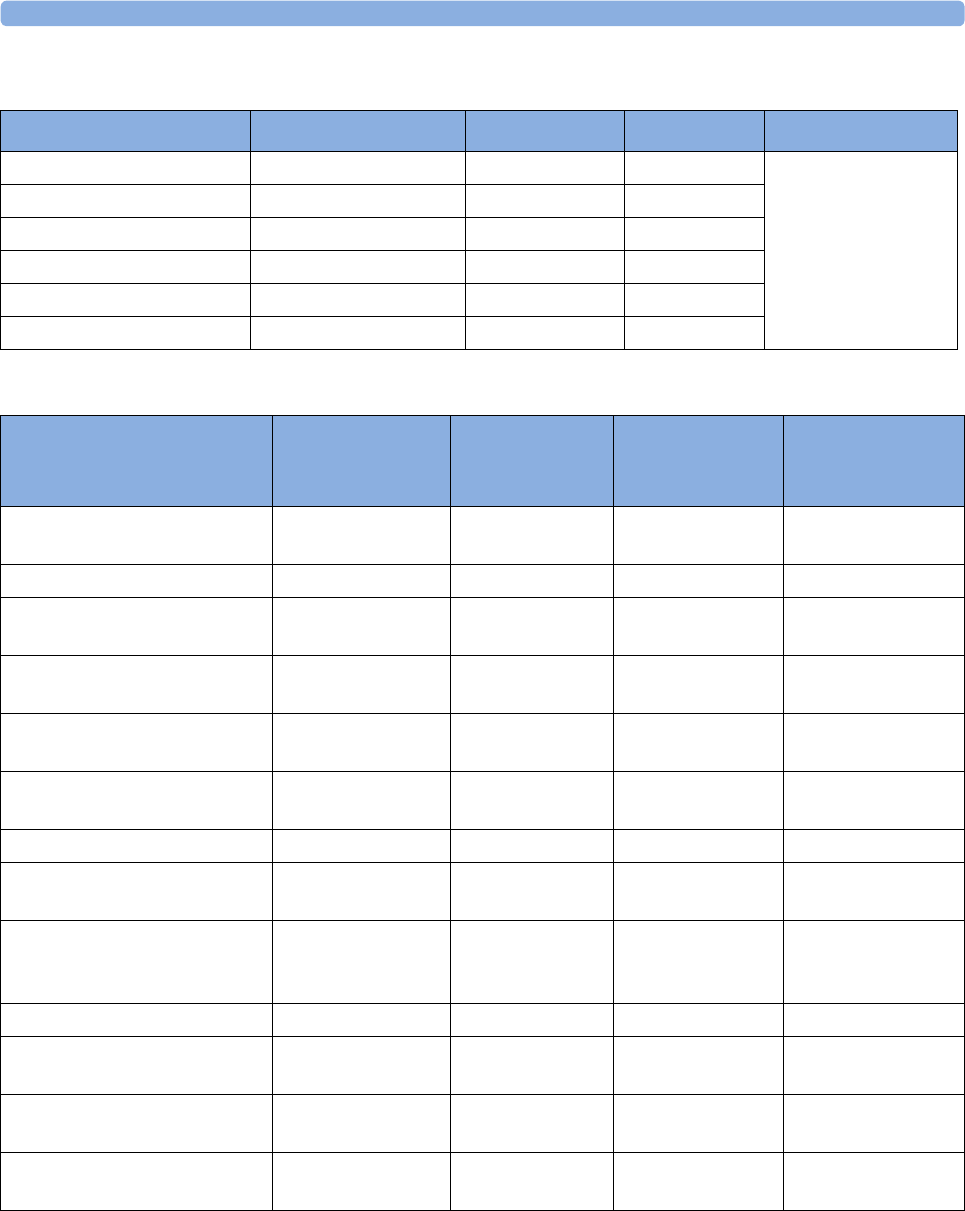
27 Accessories and Supplies
262
Adult Single Patient Soft Cuffs
IntelliVue CL NBP Pod Accessories
Maternal Patient Category Limb Circumference Bladder Width Part No. Tubing
Adult (Thigh) 45.0 - 56.5 cm 20.4 cm M4579B M1598B (1.5 m)
or
M1599B (3.0 m)
Large Adult X-Long 35.5 - 46.0 cm 16.4 cm M4578B
Large Adult 35.5 - 46.0 cm 16.4 cm M4577B
Adult X-Long 27.5 - 36.5 cm 13.1 cm M4576B
Adult 27.5 - 36.5 cm 13.1 cm M4575B
Small Adult 20.5 - 28.5 cm 10.4 cm M4574B
Description Limb
Circumference
Range
Bladder Width Contents Product No.
Mobile CL Reusable Small
Adult Cuff
21 - 27 cm 10.5 cm 1 cuff 989803163171
Mobile CL Reusable Adult Cuff 26.0 - 34.5 cm 13.0 cm 1 cuff 989803163191
Mobile CL Reusable Large
Adult Cuff
33.5 - 45.0 cm 16.0 cm 1 cuff 989803163211
Mobile CL Single-Patient Small
Adult Cuff
21 - 27 cm 10.5 cm 20 cuffs 989803163181
Mobile CL Single-Patient Adult
Cuff
26.0 - 34.5 cm 13.0 cm 20 cuffs 989803163201
Mobile CL Single-Patient Large
Adult Cuff
33.5 - 45.0 cm 16.0 cm 20 cuffs 989803163221
Mobile CL NBP Cradle Kit - - 20 cradles 989803163251
Mobile CL Extension Air Hose,
1.0 m
- - 1 extension air hose 989803163131
Mobile CL NBP Battery Kit - - 1 Battery
1 disassembly tool
1 front housing
989803163261
Telemetry Pouch with window - - 50 pouches 989803137831
Telemetry Pouch with window - - 4 boxes of
50 pouches
989803140371
White Telemetry Pouch with
Snaps; box of 50
- - 50 pouches 989803101971
(9300-0768-050)
White Telemetry Pouch with
Snaps; 4 boxes of 50
--4boxes of
50 pouches
989803101981
(9300-0768-200)
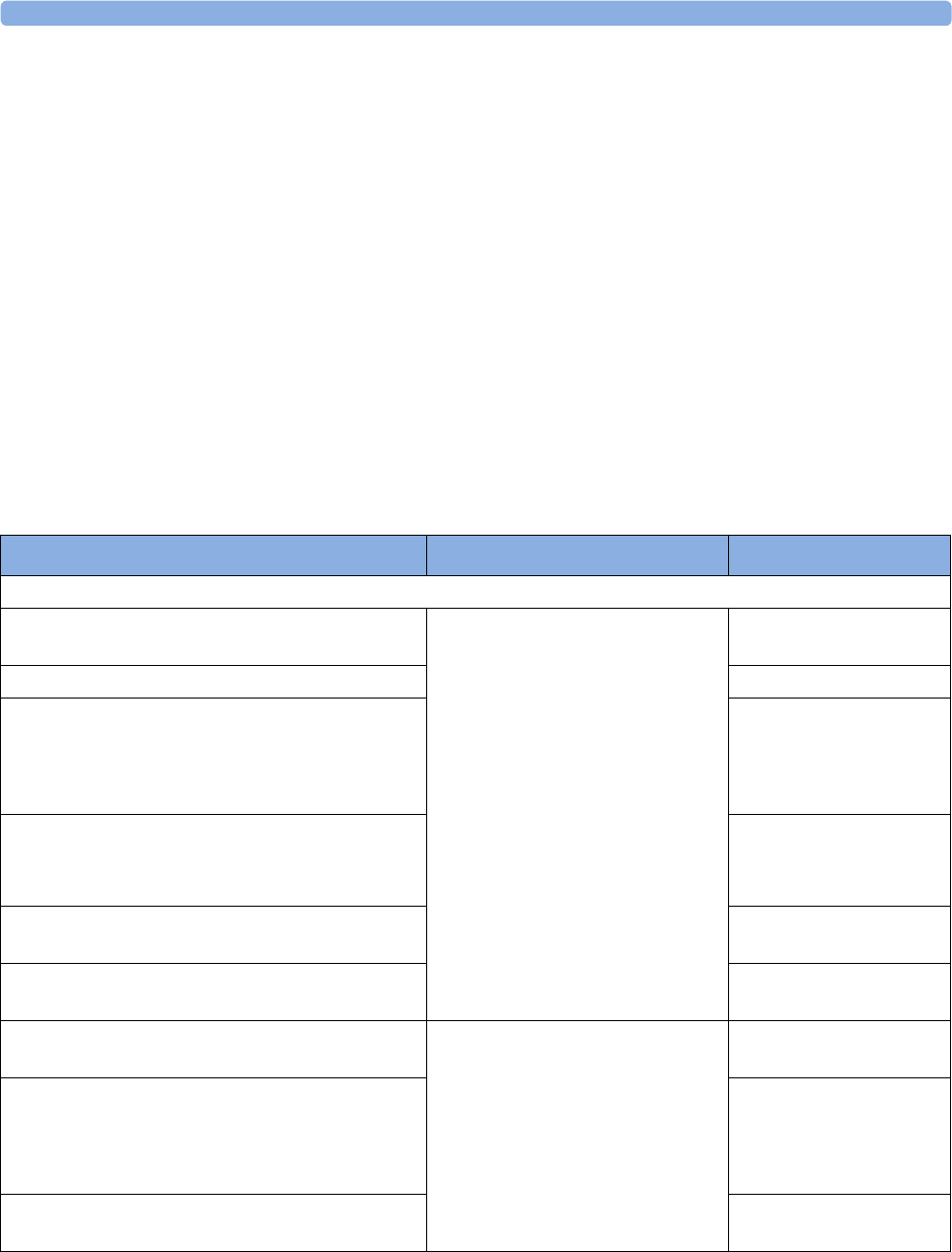
27 Accessories and Supplies
263
SpO2 Accessories
Some Nellcor sensors contain natural rubber latex which may cause allergic reactions. See the
Instructions for Use supplied with the sensors for more information. M1901B, M1903B and M1904B
are not available in USA from Philips. Purchase Nellcor OxiCliq sensors and adapter cables directly
from Tyco Healthcare. Some sensors may not be available in all countries.
Do not use more than one extension cable with any sensors or adapter cables. Do not use an extension
cable with Philips reusable sensors or adapter cables with part numbers ending in -L (indicates "Long"
version).
All listed sensors operate without risk of exceeding 41°C on the skin if ambient temperature is below
37°C.
Make sure that you use only the accessories that are specified for use with this device, otherwise patient
injury can result.
Philips SpO2 Accessories
Description Comments Product Number
Philips reusable sensors
Adult sensor (2.0 m cable), for patients over 50 kg.
Any finger, except thumb.
No adapter cable required. M1191B
M1191A with longer cable (3.0 m) M1191BL
Small adult, pediatric sensor (1.5 m cable) for
patients between 15 kg and 50 kg. Any finger except
thumb.
Use only on adult patients with FM30/40/50.
M1192A
Ear sensor (1.5 m cable) for patients more than
40 kg.
Use only on adult patients with FM30/40/50.
M1194A
Adult clip sensor (3 m cable) for patients over
40 kg. Any finger except thumb.
M1196A
Adult clip sensor (2 m cable) for patients over 40
kg. Any finger except thumb.
M1196S
Adult sensor (0.45 m), for patients over 50 kg. Any
finger except thumb.
Requires M1943A (1.0 m) or
M1943AL (3.0 m) adapter cable.
M1191T
Small adult, pediatric sensor (0.45 m cable) for
patients between 15 kg and 50 kg. Any finger except
thumb.
Use only on adult patients with FM30/40/50.
M1192T
Adult clip sensor (0.9 m cable) for patients over
40 kg. Any finger except thumb.
M1196T
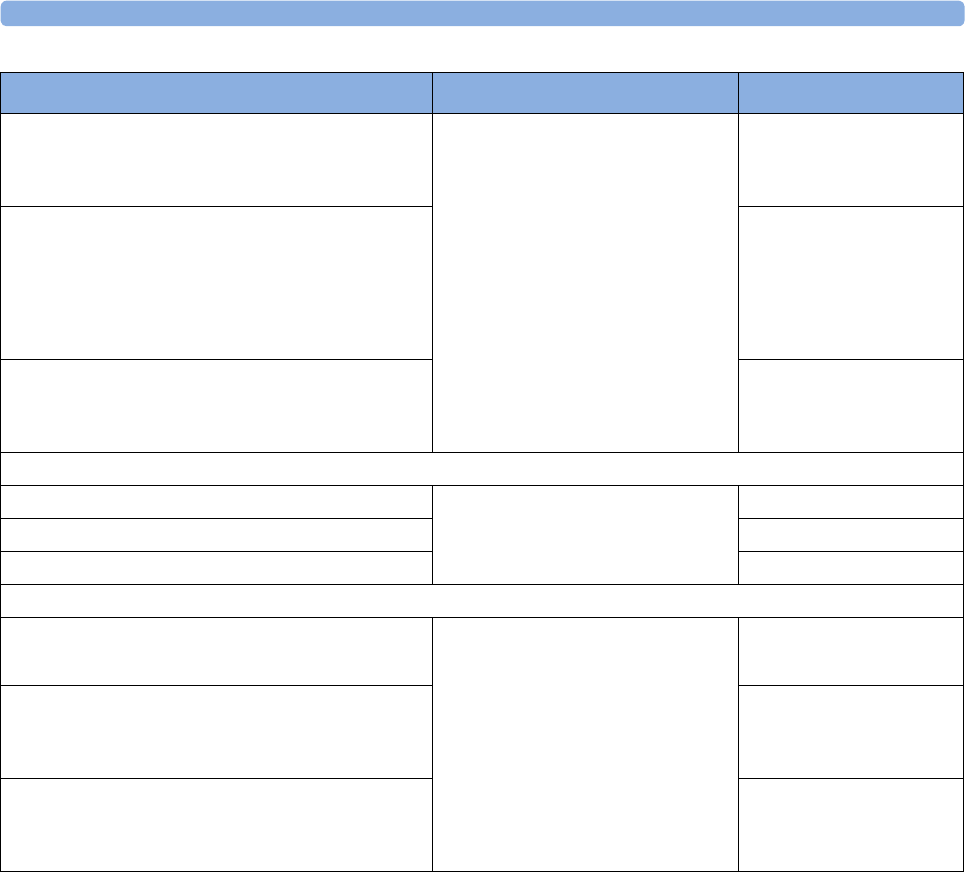
27 Accessories and Supplies
264
Special Edition (SE)
Adult sensor (3 m cable), for patients over 50 kg.
Any finger except thumb.
No adapter cable required.
SE sensors work with FM30/40/50,
as well as with OxiMax-compatible
SpO2 versions of other Philips
monitors.
M1191ANL
Special Edition (SE)
Small adult, pediatric sensor (1.5 m cable) for
patients between 15 kg and 50 kg. Any finger except
thumb.
Use only on adult patients with FM30/40/50.
M1192AN
Special Edition (SE)
Ear sensor (1.5 m cable) for patients more than
40 kg.
M1194AN
Philips disposable sensors. Not available in the USA.
Identical to OxiMax MAX-A Requires M1943A (1.0 m) or
M1943AL (3.0 m) adapter cable
M1904B
Identical to OxiMax MAX-P M1903B
Identical to OxiMax MAX-N M1901B
Philips disposable sensors. Available worldwide.
Adult/Pediatric finger sensor (0.45 m cable)
Use only on adult patients with FM30/40/50.
Requires M1943A (1.0 m) or
M1943AL (3.0 m) adapter cable
M1131A
Adult/Infant/Neonatal (0.9 m cable) for patients
> 40 kg. Any finger except thumb.
Use only on adult patients with FM30/40/50.
M1133A
Adult/Infant/Neonatal (0.9 m cable) for patients
> 40 kg. Any finger except thumb. Adhesive-free
Use only on adult patients with FM30/40/50.
M1134A
Description Comments Product Number
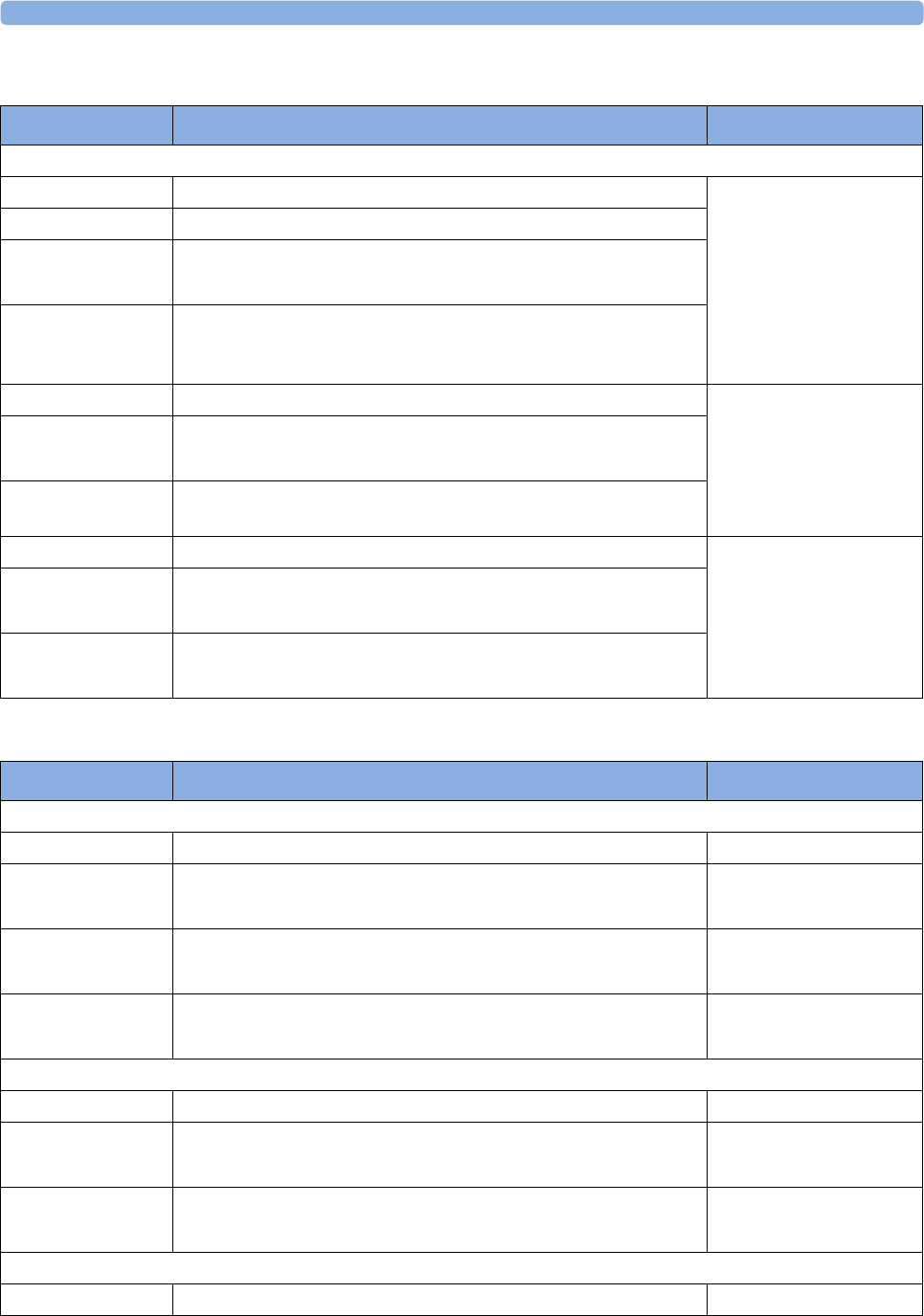
27 Accessories and Supplies
265
Nellcor SpO2 Accessories
Masimo SpO2 Accessories
Product Number Description Comments
NELLCOR disposable sensors (must be ordered from Nellcor)
OxiMax MAX-A Adult finger sensor (patient size > 30 kg) Requires M1943A (1.0 m)
or M1943AL (3.0 m)
adapter cable.
OxiMax MAX-AL OxiMax MAX-A with long cable
OxiMax MAX-P Pediatric foot/hand sensor (patient size 10-50 kg)
Use only on adult patients with FM30/40/50.
OxiMax MAX-N Adult finger or neonatal foot/hand sensor
(patient size > 40 kg or < 3 kg)
Use only on adult patients with FM30/40/50.
Oxisensor II D-25 Adult sensor (patient size > 30 kg) Requires M1943A (1.0 m)
or M1943AL (3.0 m)
adapter cable.
Oxisensor II D-20 Pediatric sensor (patient size 10-50 kg)
Use only on adult patients with FM30/40/50.
Oxisensor II N-25 Neonatal/Adult sensor (patient size < 3 kg or > 40 kg) Use only on
adult patients with FM30/40/50.
OxiCliq A See OxiMax MAX-A Requires M1943A (1.0 m)
or M1943AL (3.0 m)
adapter cable together
with OC3 adapter cable.
OxiCliq P See OxiMax MAX-P
Use only on adult patients with FM30/40/50.
OxiCliq N See OxiMax MAX-N
Use only on adult patients with FM30/40/50
Product Number Description Philips Part Number
MASIMO LNOP reusable sensors (No adapter cable required)
LNOP DC-I Adult Finger Sensor (> 30 kg) 989803140321
LNOP DC-IP Pediatric Finger Sensor (10 - 50 kg)
Use only on adult patients with FM30/40/50
989803140331
LNOP YI Multi-Site Sensor (> 1kg)
Use only on adult patients with FM30/40/50
n/a
LNOP TC-I Ear Sensor (> 30 kg)
Use only on adult patients with FM30/40/50
989803140341
MASIMO LNCS reusable sensors (No adapter cable required)
LNCS DC-I Adult Finger Sensor (> 30 kg) 989803148281
LNCS DC-IP Pediatric Finger Sensor (10 - 50 kg)
Use only on adult patients with FM30/40/50
989803148291
LNCS TC-I Ear Sensor (> 30 kg)
Use only on adult patients with FM30/40/50
989803148301
MASIMO LNOP disposable adhesive sensors
LNOP Adt Adult Sensor (> 30 kg) 989803140231
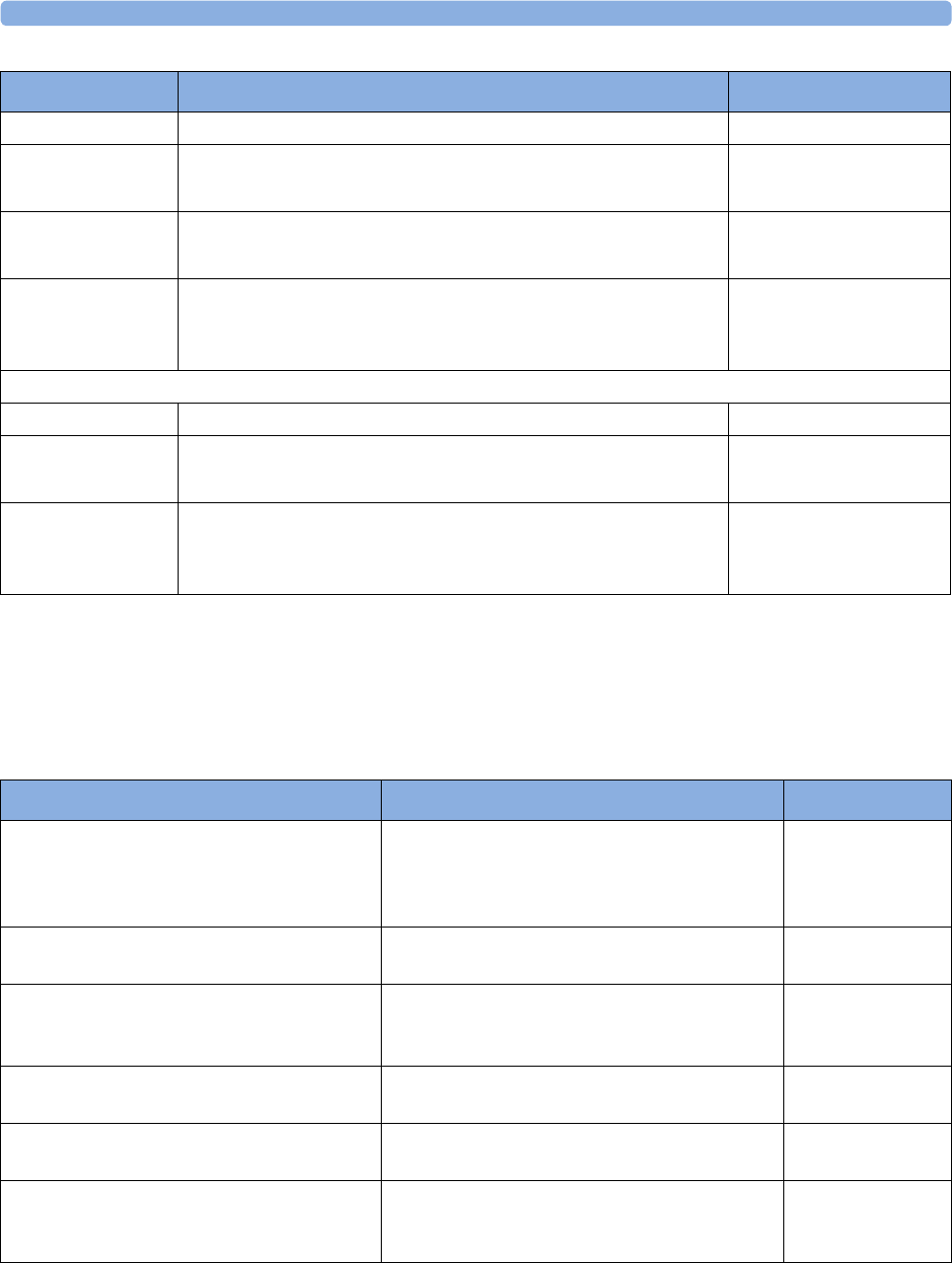
27 Accessories and Supplies
266
IntelliVue CL SpO2 Pod Accessories
All listed sensors operate without risk of exceeding 41°C on the skin, if the initial skin temperature
does not exceed 35°C.
Ensure that you use only the accessories that are specified for use with this device, otherwise patient
injury can result.
1 May not be available in all geographies
LNOP Adtx Adult Sensor (> 30 kg) n/a
LNOP Pdt Pediatric Sensor (10 - 50 kg)
Use only on adult patients with FM30/40/50
989803140261
LNOP Pdtx Pediatric Sensor (10 - 50 kg)
Use only on adult patients with FM30/40/50
n/a
LNOP Neo-L Neonatal Sensor (< 3kg)
or Adult adhesive Sensor (> 40 kg)
Use only on adult patients with FM30/40/50
989803140291
MASIMO LNCS disposable adhesive sensors (No adapter cable required)
LNCS Adtx Adult Sensor (> 30 kg) 989803148231
LNCS Pdtx Pediatric Finger Sensor (10 - 50 kg)
Use only on adult patients with FM30/40/50
989803148241
LNCS Neo-L Neonatal Foot Sensor (<3 kg)
or Adult Finger Sensor (>40 kg)
Use only on adult patients with FM30/40/50
989803148271
Product Number Description Philips Part Number
Description Contents Product No.
Mobile CL 20 single patient SpO2 Sensors
and Cradles for use on adult patients >10 kg
20 Single-Patient Mobile CL DSpO2-1A Sensors
20 Single-Patient Wristbands
20 Single-Patient Cradles
pre-assembled
989803165941
Mobile CL 20 single patient SpO2 Sensors
for use on adult patients > 10 kg
20 Single-Patient Mobile CL DSpO2-1A Sensors 989803165921
Mobile CL reusable SpO2 sensor and Cradles
for use on adult patients > 15 kg
1 Reusable Mobile CL RSpO2-1A Sensor
20 Single-Patient Cradles with pre-attached
Wristbands
9898031659311
Mobile CL 20 SpO2 Cradles (single patient) 20 Single-Patient Cradles with pre-attached
Wristbands
989803165951
Mobile CL 50 SpO2 Wristbands (single
patient)
50 Single-Patient Wristbands 989803165961
Mobile CL SpO2 Battery Kit 1 Battery
1 disassembly tool
1 front housing
989803168861
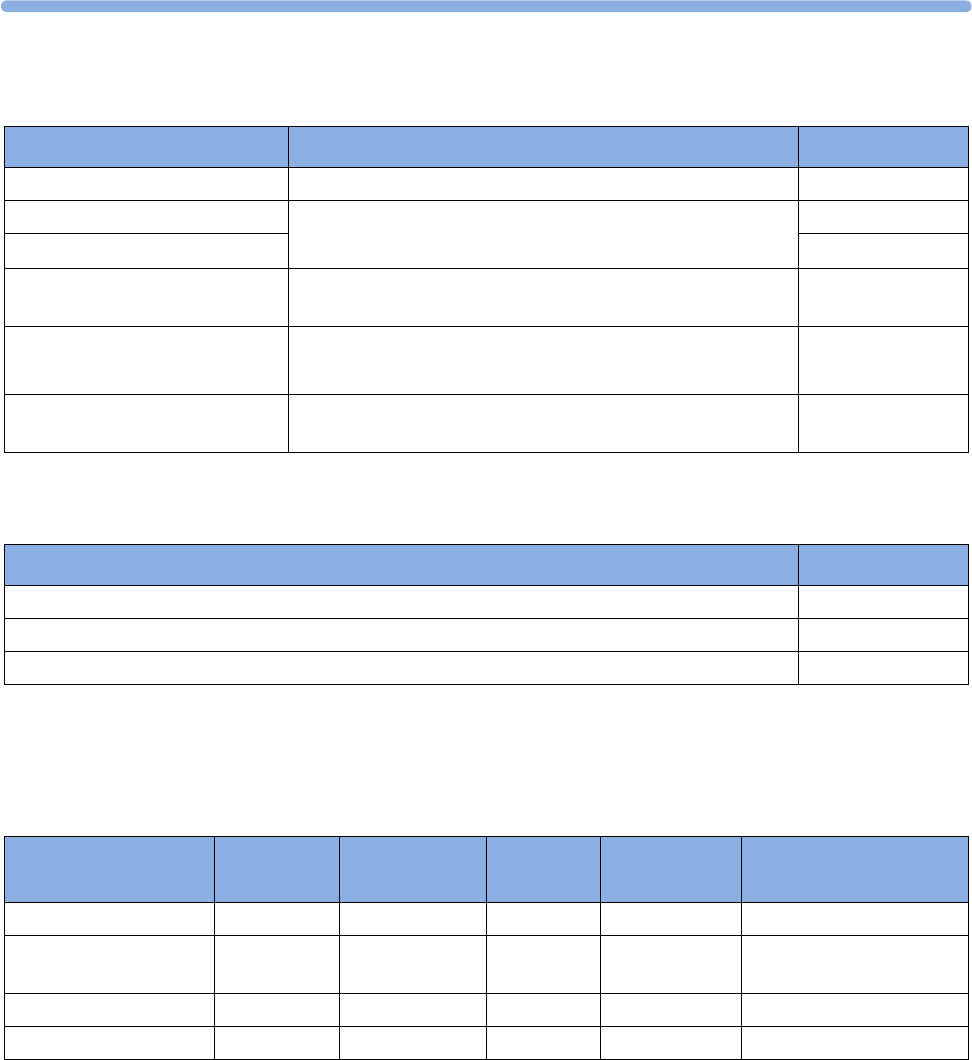
27
267
Extension / Adapter Cables
Tympanic Temperature Accessories
Recorder Paper
Supplied in cases of 40 packs. Each pack has 150 numbered pages. Single use. Use the paper specified
here.
* Bradycardia and tachycardia alarm ranges are shaded.
Description Comments Product No.
Extension cable (2 m) For use with Philips reusable sensors and adapter cables. M1941A
Adapter cable (1.1 m cable) Adapter cable for Philips/Nellcor disposable sensors. M1943A
Adapter cable (3 m cable) M1943AL
Adapter Cable for OxiCliq
sensors
Available from Nellcor. OC 3
LNOP MP12 LNOP MP Series Patient Cable (3.6 m) Adapter Cable for
Masimo LNOP sensors
M1020-61102
LNC MP10 LNCS MP Series Patient Cable (3.0 m) Adapter Cable for
Masimo LNCS sensors
989803148221
Description Part No.
Temperature probe 989803180831
Disposable probe cover with CE marking (22 boxes @ 96) 989803179611
Disposable probe cover (22 boxes @ 96) 989803179381
Geography FHR Scale Grid Color Scale
Units
Highlighted
3cm Lines?
Product No.
USA/Canada and Asia 30 - 240 Red/Orange mmHg Yes M1910A
Europe/Japan 50 - 210 Green mmHg and
kPa
No M1911A
Japan 50 - 210 Green mmHg Yes M1913A
Japan 50 - 210 Green*mmHg Yes M1913J
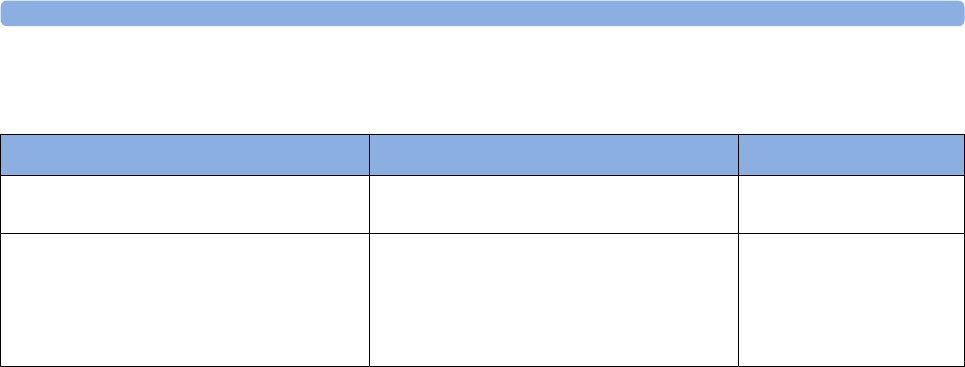
27 Accessories and Supplies
268
Batteries
Description Comment Product No.
Smart Battery 10.8 V, 6000 mAh, Lithium
Ion
For Avalon FM20 or Avalon FM30 with
battery option #E25
M4605A
Avalon CL Cableless Smart transducer
Battery Replacement Kit
Consists of one Philips Lithium Ion Battery
(Part No. 453564107871), a tool to open
and close the cableless transducer for
battery replacement and two replacement
O-ring seals.
989803184861
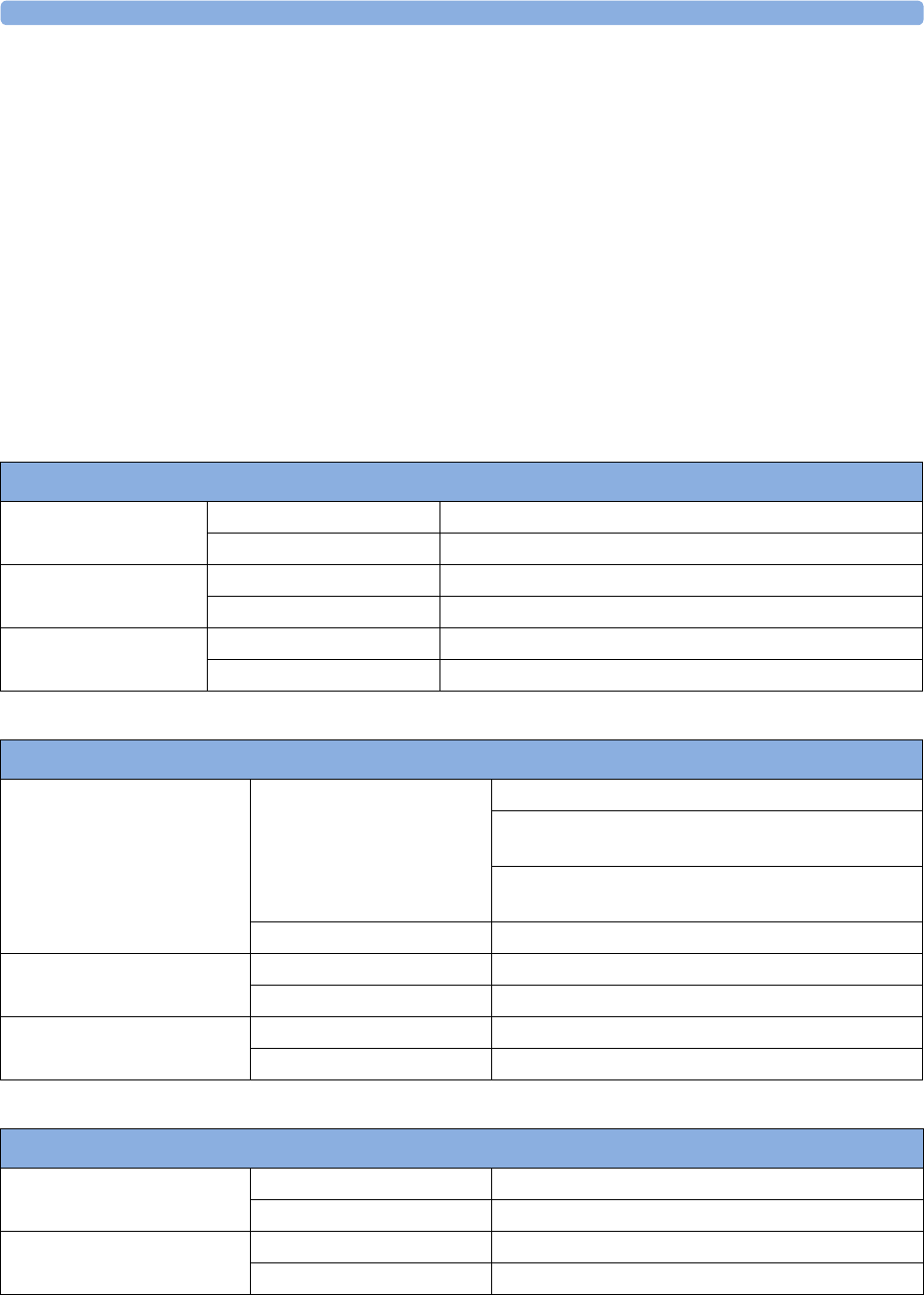
28 Specifications and Standards Compliance
269
28Specifications and Standards
Compliance
The monitors are intended to monitor a mother and her fetus(es), which from an electrical safety point
of view, are one person.
Environmental Specifications
The monitor may not meet the given performance specifications if stored and used outside the
specified temperature and humidity ranges.
Avalon CL Base station 866074
Temperature Range Operating 0°C to 45°C (32°F to113°F)
Storage/Transportation -20°C to 60°C (-4°F to 140°F)
Humidity Range Operating <95% relative humidity @ 45°C/113°F
Storage/Transportation <90% relative humidity @ 60°C/140°F
Altitude Range Operating -500 to 3000 m/-1640 to 9840 ft.
Storage/Transportation -500 to 13100 m/-1640 to 43000 ft.
Monitor (M2702A/M2703A); Interface Cable for Avalon CTS (M2731-60001 and M2732-60001)
Temperature Range Operating Without battery option: 0°C to 45°C (32°F to 113°F)
With battery option/charging: 0°C to 35°C (32°F to
95°F)
With battery option/fully charged: 0°C to 40°C (32°F
to 104°F)
Storage/Transportation -20°C to 60°C (-4°F to 140°F)
Humidity Range Operating <95% relative humidity @ 40°C/104°F
Storage/Transportation <90% relative humidity @ 60°C/140°F
Altitude Range Operating -500 to 3000 m/-1640 to 9840 ft.
Storage/Transportation -500 to 13100 m/-1640 to 43000 ft.
Transducers (M2734A/M2734B/M2735A/M2736A/M2738A)
Temperature Range Operating 0°C to 40°C (32°F to 104°F)
Storage/Transportation -20°C to 60°C (-4°F to 140°F)
Humidity Range Operating <95% relative humidity @ 40°C/104°F
Storage/Transportation <90% relative humidity @ 60°C/140°F
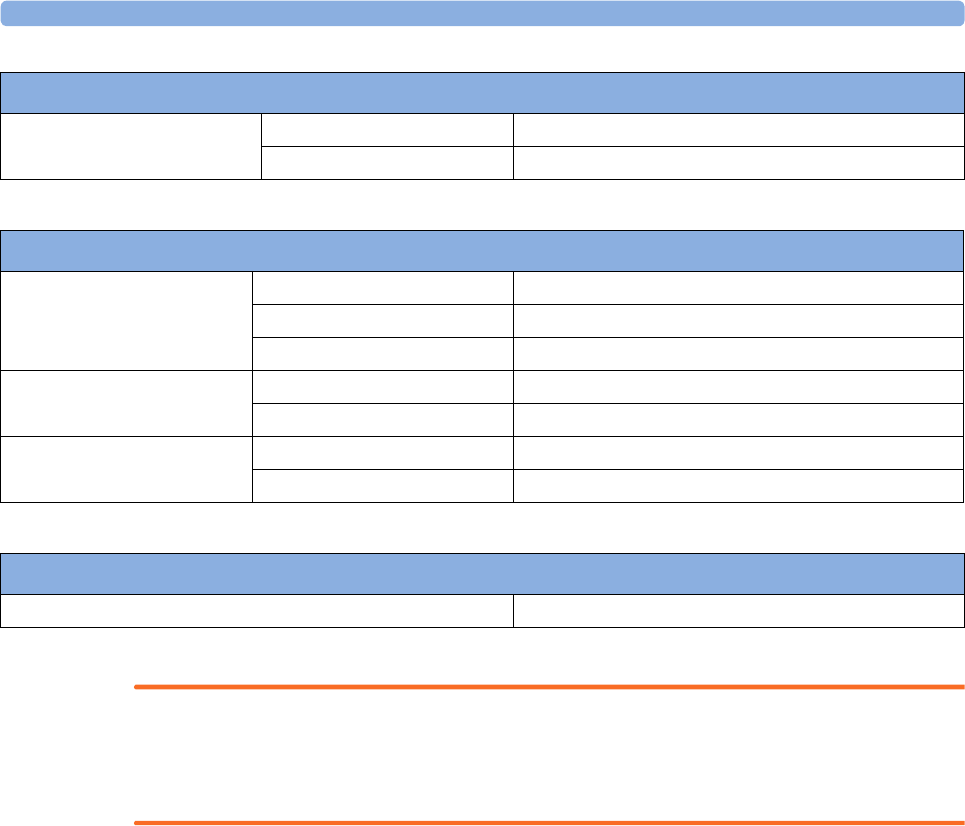
28 Specifications and Standards Compliance
270
WARNING
Explosion Hazard: Do not use in the presence of flammable anesthetics, such as a flammable
anesthetic mixture with air, oxygen, nitrous oxide, or in oxygen rich environment. Use of the devices in
such an environment may present an explosion hazard.
Altitude Range Operating -500 to 3000 m/-1640 to 9840 ft.
Storage/Transportation -500 to 13100 m/-1640 to 43000 ft.
Transducers (M2734A/M2734B/M2735A/M2736A/M2738A)
Avalon CL Transducers (866075/866076/866077)
Temperature Range Operating 0°C to 40°C (32°F to 104°F)
Charging 0°C to 35°C (32°F to 95°F)
Storage/Transportation -20°C to 60°C (-4°F to 140°F)
Humidity Range Operating <95% relative humidity @ 40°C/104°F
Storage/Transportation <90% relative humidity @ 60°C/140°F
Altitude Range Operating -500 to 3000 m/-1640 to 9840 ft.
Storage/Transportation -500 to 13100 m/-1640 to 43000 ft.
SpO2 Sensors
Operating Temperature Range 0°C to 37°C (32°F to 98.6°F)
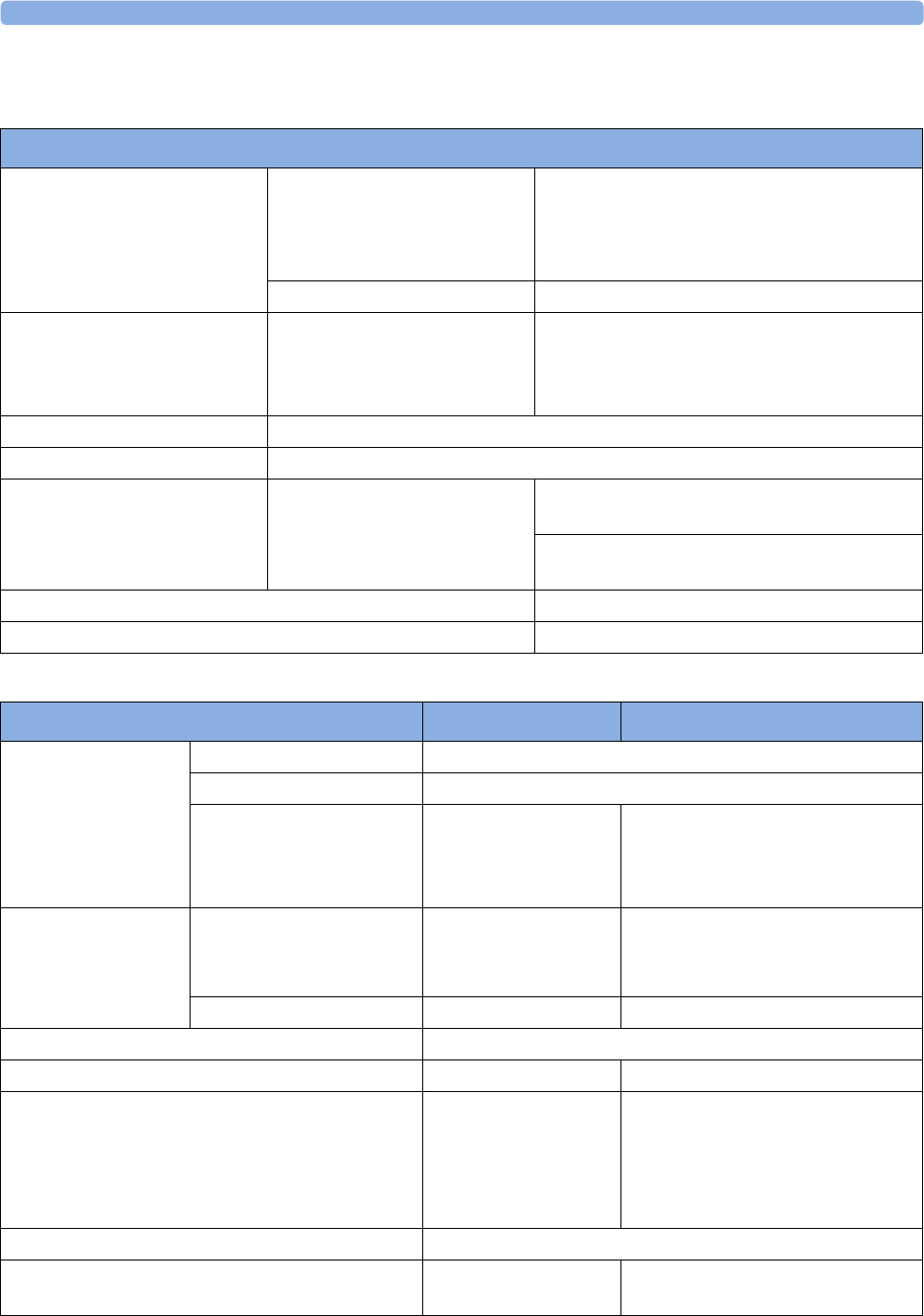
28 Specifications and Standards Compliance
271
Physical Specifications
Avalon CL Base Station
Dimension and Weight Size mm/(in):
width x height x depth
349 x 74 x 183 mm
(349 mm-5% max. width 350 mm)
(13.7 x 2.9 x 7.2 in
13.7 in -5% max. width 13.8 in)
Weight 0.985 kg /2.2 lbs
Electrical Class When connected to M2702A/
M2703A/M2704A/M2705A
Class II equipment using a red
connector at the fetal sockets.
When connected to M2704A/M2705A Class I
equipment using a black connector in the
telemetry socket.
Electrical Power Source External (powered by fetal monitor)
Mode of Operation Continuous operation
Interface cable connector type Connector color Red for FM20/30 left side or FM40/50 front
fetal connector socket
Black for FM40/50 rear telemetry connector
socket
Interface cable length 1,5 m /4.11 ft
Ingress Protection IP31
Monitor Physical Specifications M2702A/M2703A M2704A/M2705A
Power Supply Voltages 100 VAC to 240 VAC ±10%
Supply Frequency Range 50 Hz/60 Hz
Power Consumption
(current)
0.7 - 0.4 A (M2702A/
M2703A)
1.3 - 0.7 A
(M8023A#E25)
1.3 - 0.7 A
Dimensions and
Weight
Size (without options) mm/
(in):
width x height x depth
286 x 133 x 335 ±1%
(11.3 x 5.2 x 13.2 in
±1%)
420 x 172 x 370 ±5%
(16.5 x 6.8 x 14.6 in ±5%)
Weight < 5.1 kg/11.2 lbs < 9.0 kg/19.8 lbs
Degree of Protection Against Electrical Shock Type CF
Electrical Class Class II equipment Class I equipment
Electrical Power Source External (AC) without
battery option #E25
Internal (LiIo battery) if
with battery option
#E25
External (AC)
Mode of Operation Continuous operation
Water Ingress Protection Code - IP X1 (provided recorder drawer is
shut)
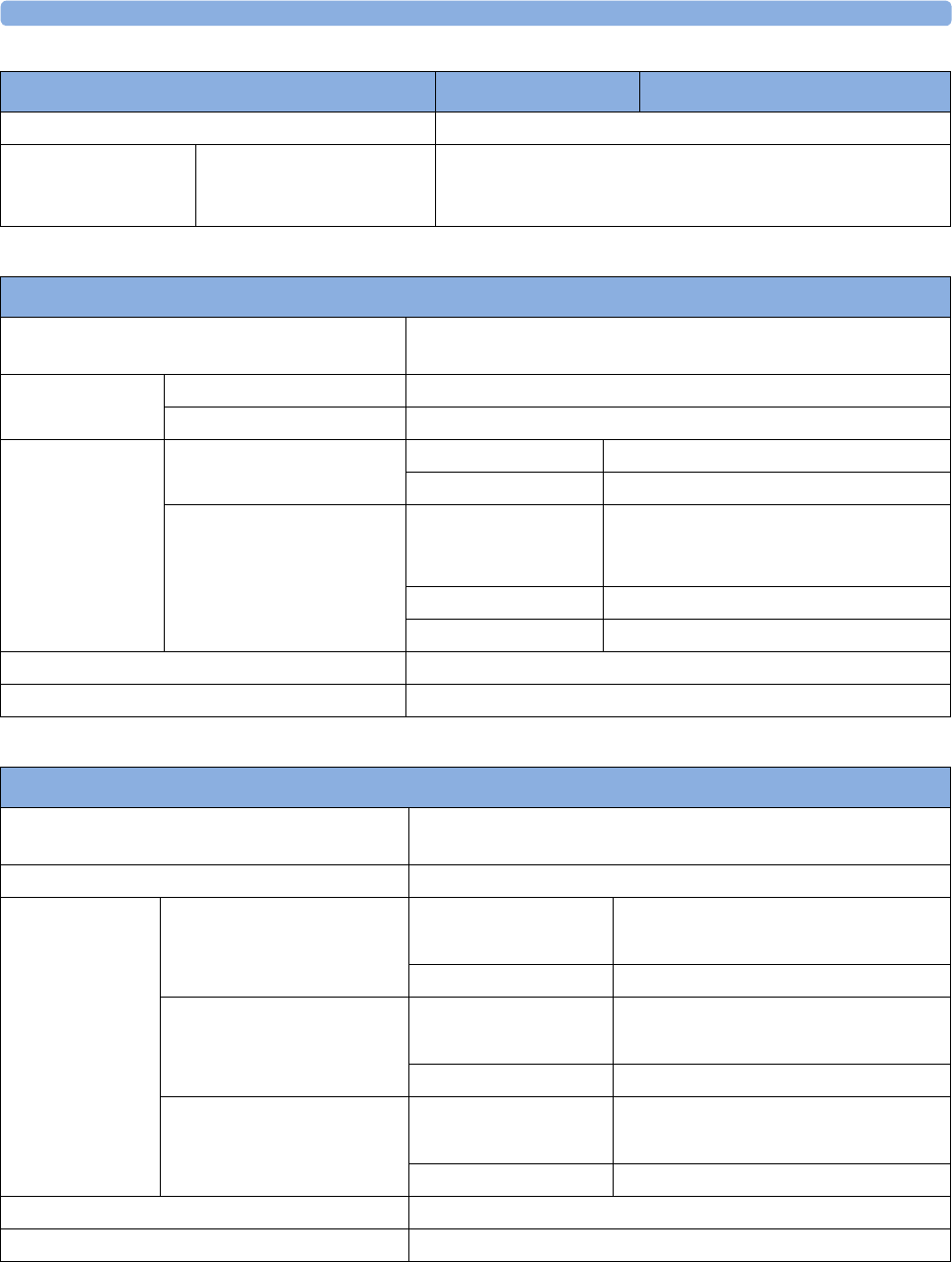
28 Specifications and Standards Compliance
272
Global Speed 6.25 mm/sec, 12.5 mm/sec, 25 mm/sec, 50 mm/sec
Startup Time Time taken from switching
on the monitor to seeing the
first parameter labels
< 30 seconds
Monitor Physical Specifications M2702A/M2703A M2704A/M2705A
Transducers (M2734A/M2734B/M2735A/M2736A/M2738A)
Shock Resistance Withstands a 1 m drop to concrete surface with possible cosmetic
damage only
Water Ingress
Protection Code
M2734A&B/35/36A IP 68 (immersion up to 1 m water depth for 5 hours)
M2738A IP 67 (immersion up to 0.5 m water depth for 30 minutes)
Dimensions and
Weight
M2734A&B/35/36A Size (diameter) 83 mm/3.27 in
Weight (without cable) < 220 g/7.8 oz.
M2738A Maximum size mm/
(in): width x height x
depth
50 x 28 x 135 (2.0 x 1.1 x 5.3 in)
Cable length 2.5 m
Weight < 150 g/5.3 oz.
Degree of Protection Against Electrical Shock Type CF
Transducer Identification Optical Signal Element (Finder LED). Not M2738A
Avalon CL Transducers (866075/866076/866077)
Shock Resistance Withstands a 1.5 m drop to concrete surface with possible
cosmetic damage only.
Water Ingress Protection Code IP 68 (immersion up to 1 m water depth for 5 hours)
Dimensions and
Weight
Avalon Cableless Toco+MP
Transducer 866075
Size (diameter/height) 75.5 mm/ 36.6 mm
2.9 / 1.4 in
Weight 123 g ±10%/4.3 oz ±10%
Avalon Cableless US
Transducer 866076
Size (diameter/height) 75.5 mm/ 36.6 mm
2.9 / 1.4 in
Weight 131 g ±10%/4.6 oz ±10%
Avalon Cableless ECG/IUP
Transducer 866077
Size (diameter/height) 75.5 mm/ 36.6 mm
2.9 / 1.4 in
Weight 121 g ±10%/4.2 oz ±10%
Degree of Protection Against Electrical Shock Type CF
Transducer Identification Optical Signal Element (Finder LED).
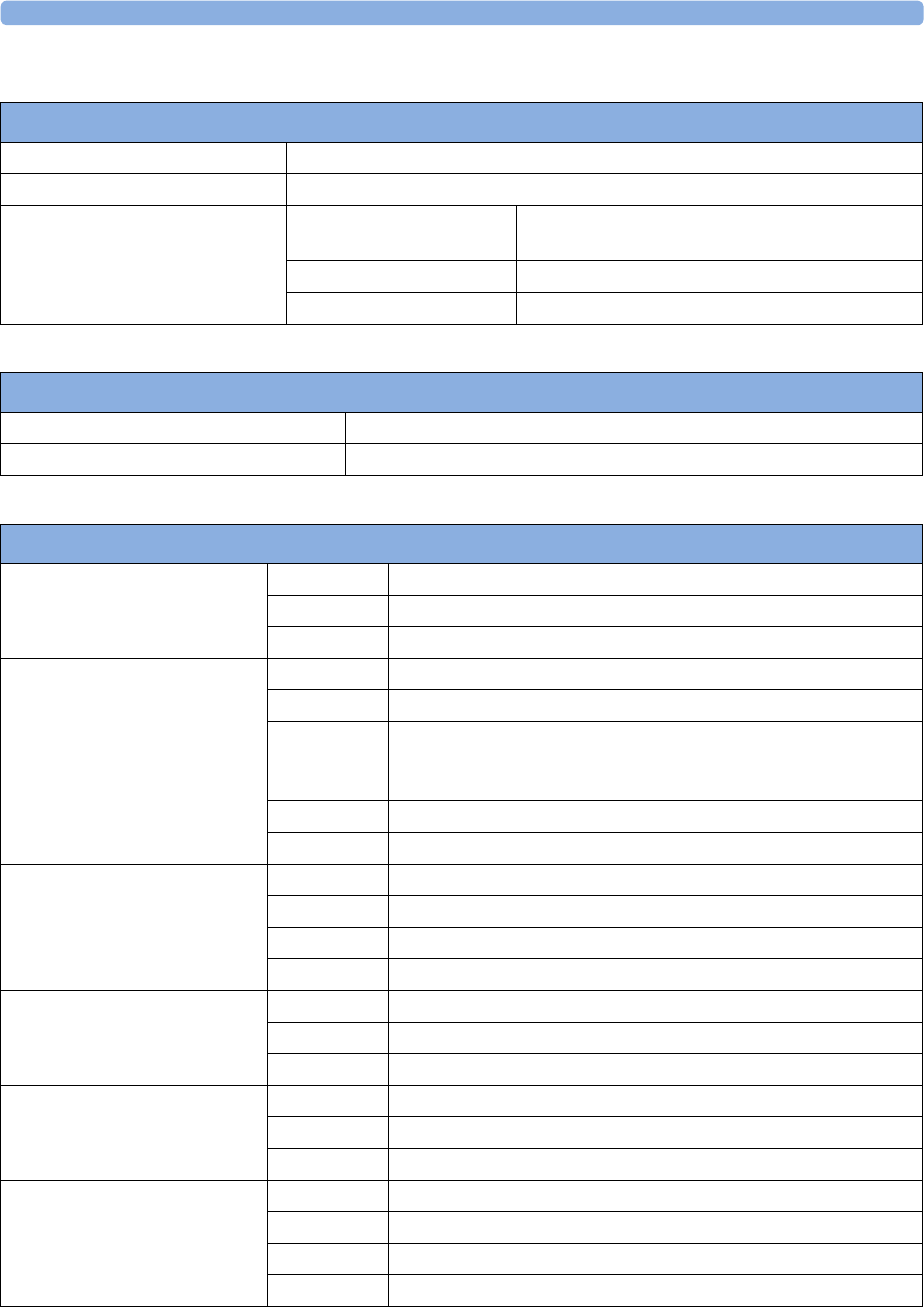
28 Specifications and Standards Compliance
273
Interface Cable for Avalon CTS (M2731-60001 and M2732-60001)
Shock Resistance Withstands a 1m drop to concrete surface with possible cosmetic damage only
Water Ingress Protection Code IP X1
Dimensions and Weight Maximum size mm/(in):
width x height x depth
55 x 28 x 50 (2.2 x 1.1 x 2.0 in)
Cable length 2.5 m
Weight < 200 g/7.0 oz.
M8023A (Option #E25) External Power Supply Weight and Dimensions
Maximum Weight 700 g ±10% (1.5 lb ±10%)
Size (W x H x D) 207 x 70 x 113 mm / 8.1 x 2.8 x 4.4 in
Interface Specifications
Network Standard 100-Base-TX (IEEE 802.3 Clause 25)
Connector RJ45 (8 pin)
Isolation Basic insulation (reference voltage: 250 V; test voltage: 1500 V)
MIB/RS232 Standard IEEE 1073-3.2-2000
Connectors RJ45 (8 pin)
Mode Software-controllable
BCC (RxD/TxD cross over) or
DCC (RxD/TxD straight through
Power 5 V ±5 %, 100 mA (max.)
Isolation Basic insulation (reference voltage: 250 V; test voltage: 1500 V)
USB Interface Standard USB 2.0 full-speed (embedded host)
Connectors USB series "Standard A" receptacle
Power Low power port 4.4V min; max. load for all ports together 500 mA
Isolation none
RS232 (Standard) Connectors RJ45 (8-pin)
Power none
Insulation Basic insulation (reference voltage: 250 V; test voltage: 1500 V)
RS232 (Independent display
interface option)
Connectors RJ45 (8-pin)
Power none
Isolation none
Basic Nurse Call Relay Connectors Modular Jack 6P6C, active open and closed contact
Contact <=100 mA, <=24 V DC
Isolation Basic insulation (reference voltage: 250 V; test voltage: 1500 V)
Delay <[Configured Latency +0.5] sec
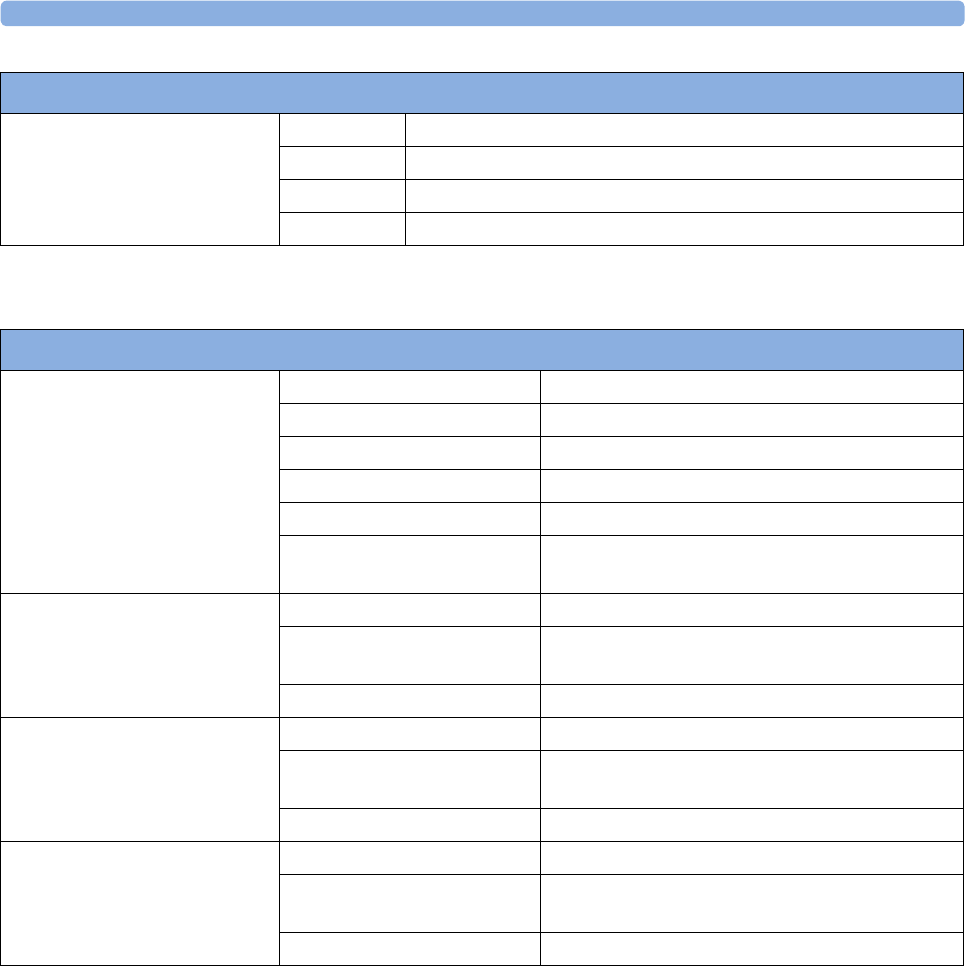
28 Specifications and Standards Compliance
274
1 The power loss indication functionality of the Nurse Call Relay board is not supported with fetal
monitors.
Flexible Nurse Call Relay1Connectors 20 pin MDR (Mini D-Ribbon), active open and closed contacts
Contact <=100 mA, <=24 V DC
Isolation Basic insulation (reference voltage: 250 V; test voltage: 1500 V)
Delay <[Configured Latency +0.5] sec
Interface Specifications
Avalon CL Radio Interface Specifications
Short Range Radio Interface Type Internal SRR interface
Technology IEEE 802.15.4
Frequency Band 2.4 GHz ISM (2.400 - 2.483 GHz)
Modulation Technique DSSS (O -QPSK)
Effective radiated power max. 0 dBm (1 mW)
Range ca. 5 m without any physical obstructions as walls
and doors
OBR (WMTS) Frequency Band 608 - 614 MHz
Effective radiated power <20 mW (Base Station)
<1 mW (CL transducers)
Range min. 70 m
OBR (ISM) Frequency Band 433.05 -434.79 MHz
Effective radiated power <10 mW (Base Station)
<1 mW (CL transducers)
Range min. 70 m
OBR (T108) Frequency Band 920.6 - 923.4 MHZ
Effective radiated power <20 mW (Base Station)
<10 mW (CL transducers)
Range min. 70 m
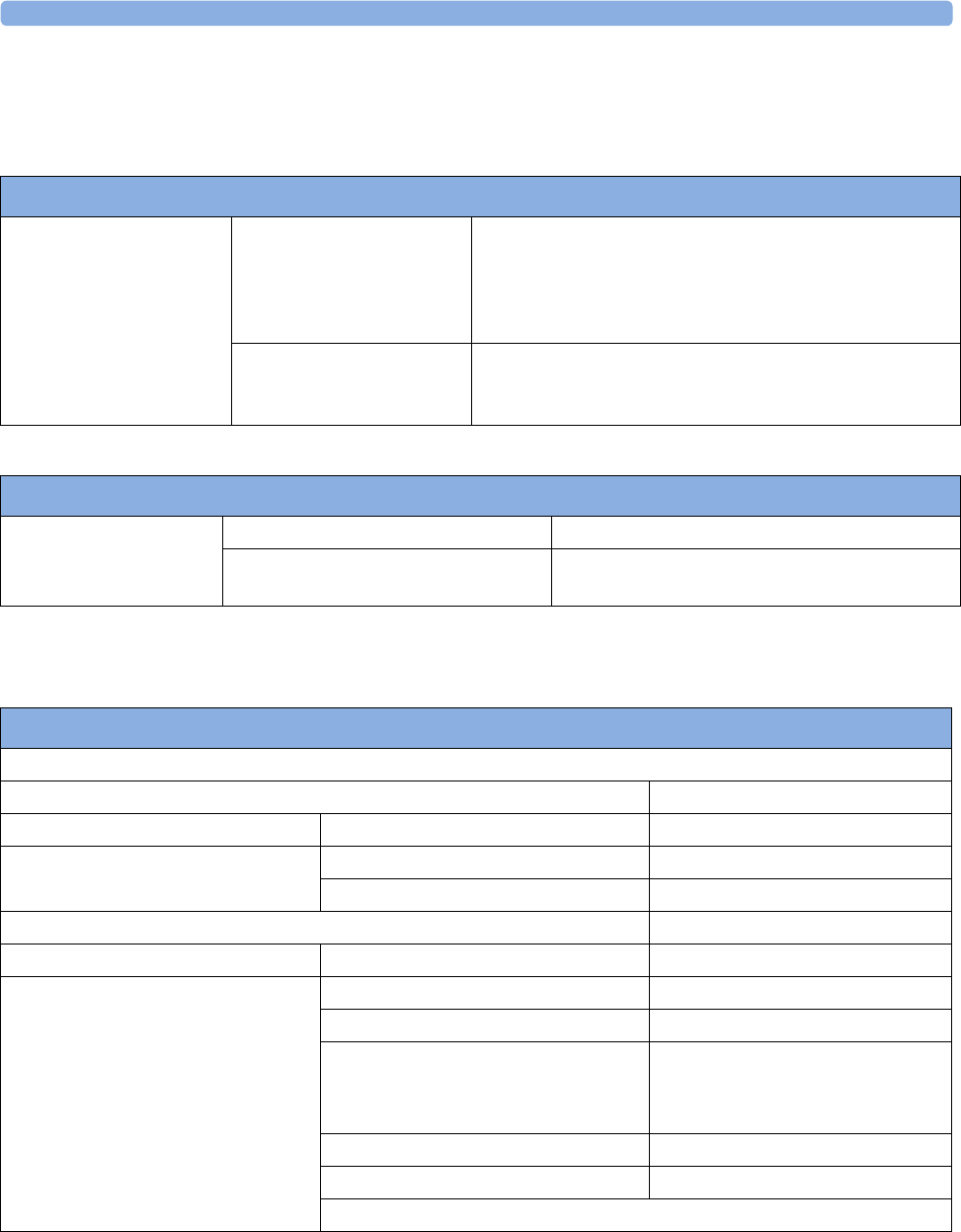
28 Specifications and Standards Compliance
275
Performance Specifications
Battery Specifications
Fetal / Maternal Specifications
Performance Specifications
Avalon FM20/30 Battery
Option #E25
Operating Time
(with new, fully charged
battery)
Basic monitoring configuration: >2 hours
(Display Brightness: 70%, Recorder: "On" at 3cm/min,
NBP: Auto Mode at 15min, 2 US Transducers, 1 Toco+
with MECG, 1 Patient Module with DECG)
Charge Time When monitor is off: approx. 6 hours
When monitor is in use: more than 10 hours (depending on
monitor configuration).
Performance Specification
Avalon CL Transducer
Battery
Operating time With a new and fully charged battery min. 8 hours
Charge time From a "low battery" indication to a "fully
charged" indication min. 3 hours
Performance Specifications
Ultrasound
Measurement Method Ultrasound Pulse Doppler
Measurement Range US 50 to 240 bpm
Resolution Display 1 bpm
Printer 1/4 bpm
Jitter @ 200 bpm ≤ 3 bpm
Display Update Rate 1 / second
US Intensity (M2736A/AA) Average output power P = (7.4 ± 0.4) mW
Peak-negative acoustic pressure p_ = (40.4 ± 4.3) kPa
Output beam intensity (Iob)
(= spatial average - temporal average
intensity)
Isata = (2.38 ± 0.59) mW/cm2
Spatial-peak temporal average intensity Ispta = (15.0 ± 3.2) mW/cm2
Effective radiating area @ -12 dB (3.11 ± 0.74) cm2
Thermal index (TI) and mechanical index (MI) are always below 1.0.
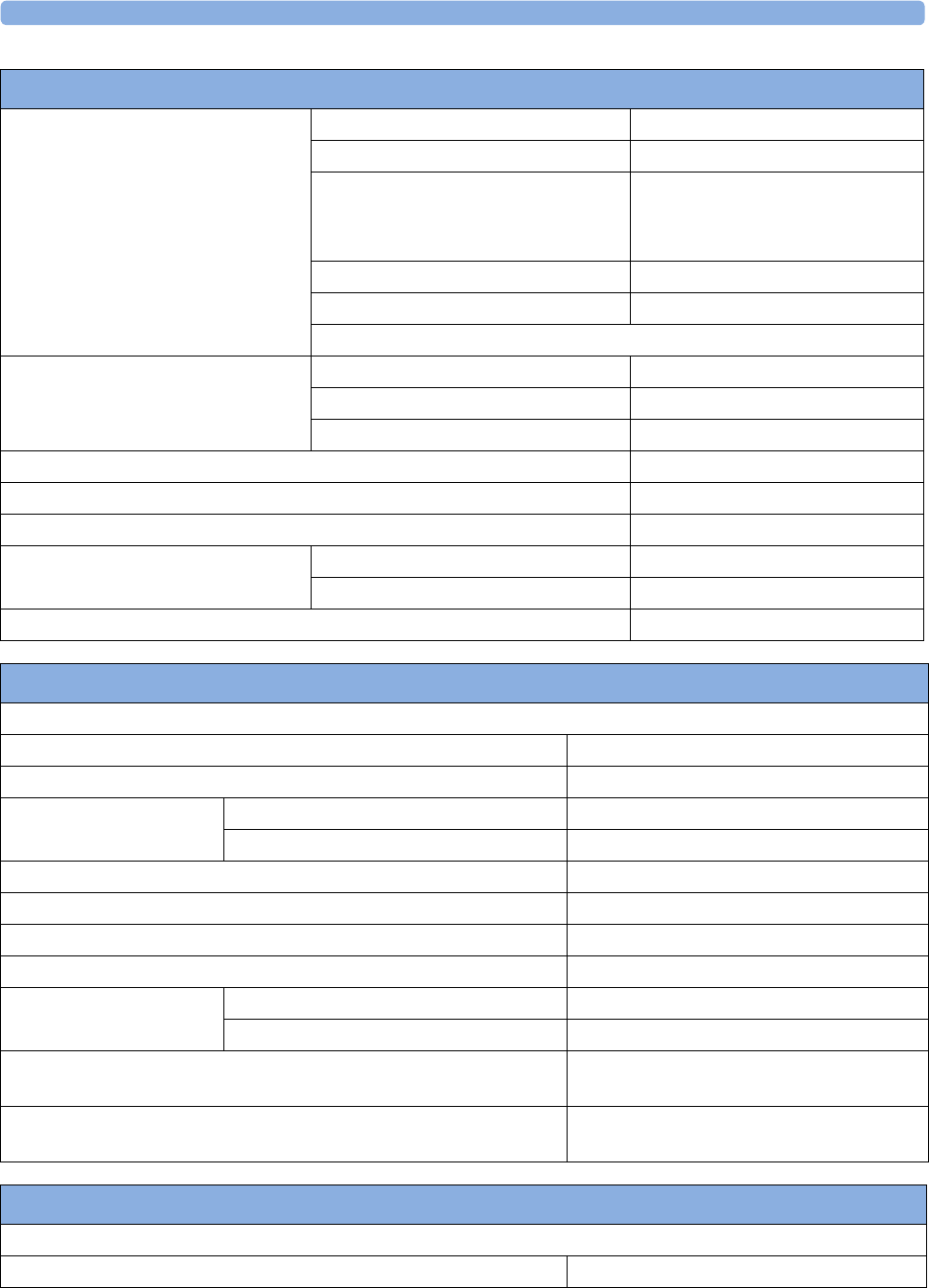
28 Specifications and Standards Compliance
276
US Intensity CL (866076) Average output power P = (12.4 ± 0.4) mW
Peak-negative acoustic pressure p_ = (49.1 ± 5.2) kPa
Output beam intensity (Iob)
(= spatial average - temporal average
intensity)
Isata = (2.77 ± 0.56) mW/cm2
Spatial-peak temporal average intensity Ispta = (21.1 ± 5.1) mW/cm2
Effective radiating area @ -12 dB A-12dB = (4.47 ± 0.89) cm2
Thermal index (TI) and mechanical index (MI) are always below 1.0.
Signal Quality Indication Poor Quality empty
Acceptable Quality half-full
Good Quality full
Beat-to -Beat (max.) for Ultrasound 28bmp
US Frequency 1 MHz ± 100 Hz
US Signal range 3.5 µVpp to 350 µVpp @ 200 Hz
US Burst Repetition Rate 3.0 kHz
Duration ≤ 100 µs
FMP Signal Range @ 33 Hz 200 µVpp to 40 µVpp
Performance Specifications
Performance Specifications
Toco
Measurement Method Strain Gauge Sensor Element
Sensitivity 1 unit = 2.5 g
Resolution Display 1 unit
Printer 1/4 unit
Measurement Range 400 units
Signal Range 0 to 127 units
Maximum Offset Range -300 units
Baseline Setting 20 units
Update Rate Display 1 / second
Printer ~4 / seconds
Auto Offset Correction 3 seconds after connecting the transducer,
the Toco value is set to 20 units
Auto Zero Adjust Toco value is set to zero following a negative
measurement value for 5 seconds
Performance Specifications
Maternal Pulse from Toco
Emitted Light Energy ≤ 15 mW
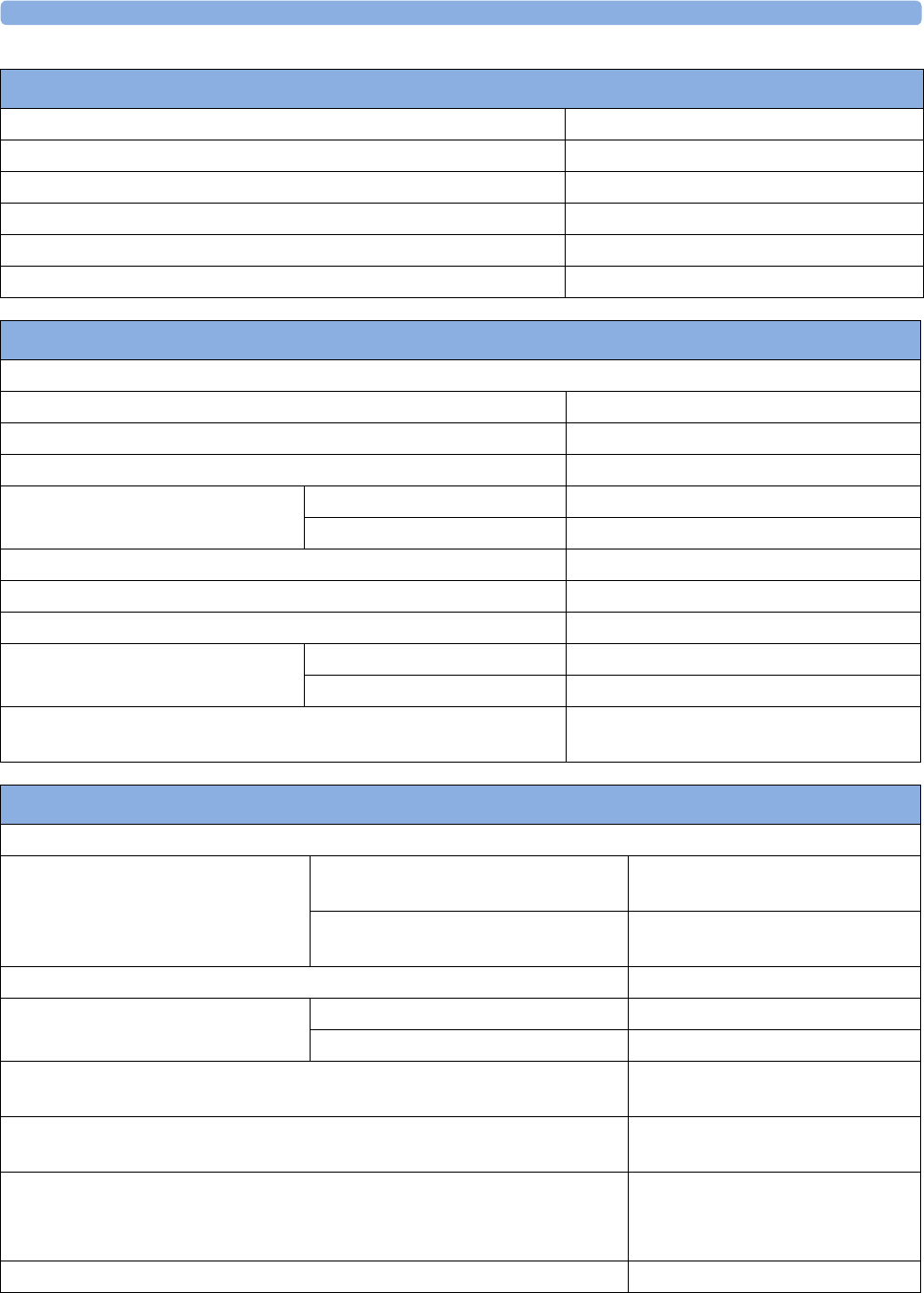
28 Specifications and Standards Compliance
277
Wavelength Range 780 to 1100 nm
Range 40 to 240 bpm
Resolution 1 bpm
Display Update Rate 1 / s
Accuracy ± 2% or 1 bpm, whichever is greater
Update Rate every 4 seconds
Performance Specifications
Performance Specifications
IUP
Measurement Method Passive Resistive Strain Gauge Elements
Measurement Range -100 to +300 mmHg
Signal Range -99 to 127 mmHg or -13.2 to 16.9 kPa
Resolution Display 1 mmHg
Printer 1/4 mmHg
Sensitivity 5 µV/V/mmHg
Offset Compensation +100 to -200 mmHg
Accuracy (not including sensor accuracy) ± 0.5% per 100 mmHg
Update Rate Display 1 / second
Printer ~4 / seconds
Auto Offset Correction 3 seconds after connecting the transducer,
the IUP value is set to 0 mmHg
Performance Specifications
ECG
Performance Specifications Type DECG Single Lead ECG (derived from
Fetal Scalp Electrode)
MECG Single Lead ECG (derived from RA
and LA electrodes)
Measurement Range 30 to 240 bpm
Resolution Display 1 bpm (display update rate 1/s)
Recorder 1/4 bpm
Wave Speed 6.25 mm/sec, 12.5 mm/sec, 25
mm/sec, 50 mm/sec
Accuracy ± 1 bpm or 1%, whichever is greater
(non-averaging)
Beat-to -Beat (max.) MECG: 28 bpm
DECG: 28 bpm (with Artifact
Suppression On)
Differential Input Impedance > 15MΩ
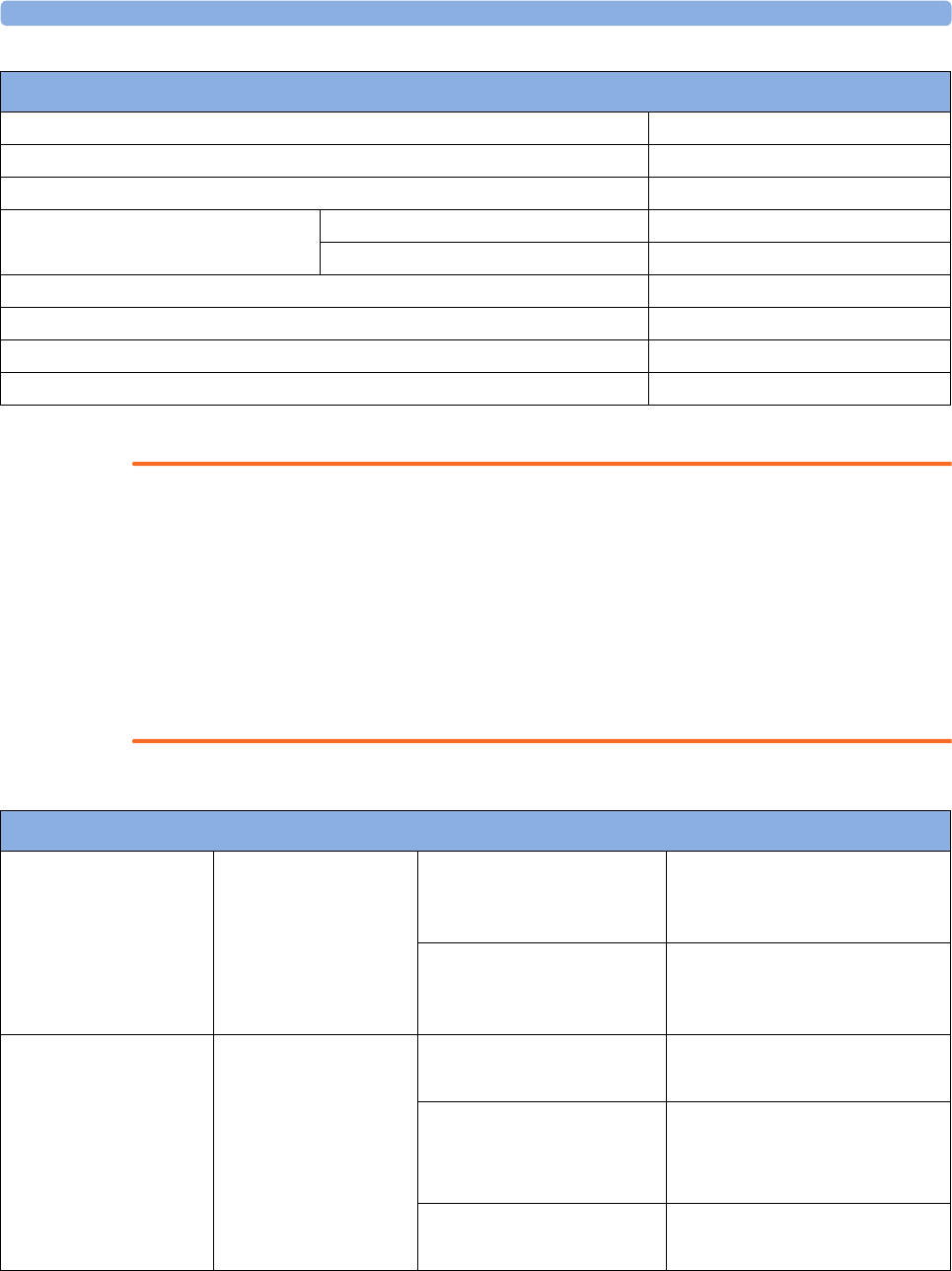
28 Specifications and Standards Compliance
278
WARNING
The fetal/maternal monitor is not a diagnostic ECG device. In particular, the display of fetal/maternal
ECG is intended only for evaluating signal quality for fetal/maternal heart rate as derived from the
ECG waveform.
When in doubt, it can be used to identify sources of compromised signal quality, such as noise or
muscle artifacts. It can subsequently be used to verify the result of measures taken to resolve them
(e.g., checking ECG cable connections or adapting the fetal ArtifactSuppress configuration).
The safety and effectiveness of the displayed fetal/maternal ECG waveform (i.e., P, QRS and T
segments) for evaluation of fetal/maternal cardiac status during labor have not been evaluated.
Electrode Offset Potential Tolerance ± 400 mV
Filter Bandwidth 0.8 to 80 Hz
INOP Auxiliary Current (Leads Off Detection) < 100 µA
Input Signal Range DECG 20 µVpp to 6 mVpp
MECG 150 µVpp to 6 mVpp
Dielectric Strength 1500 Vrms
Defibrillator Protection None
ESU Protection None
Pace pulse detection None
Performance Specifications
Fetal Heart Rate (Ultrasound/DECG) Alarm Specifications
FHR Alarm Limits Range Bradycardia
(low limit)
60 to 200 bpm
adjustable in 10 bpm steps
Default: 110 bpm
Tachycardia
(high limit)
70 to 210 bpm
adjustable in 10 bpm steps
Default: 170 bpm
FHR Alarm Delay Range Bradycardia
(low limit) Delay
10 to 300 seconds in steps of 10s
Default: 240s
Tachycardia
(high limit) Delay
10 to 300 seconds
in steps of 10s
Default: 300s
Signal Loss Delay 10 to 30 seconds
in steps of 10s
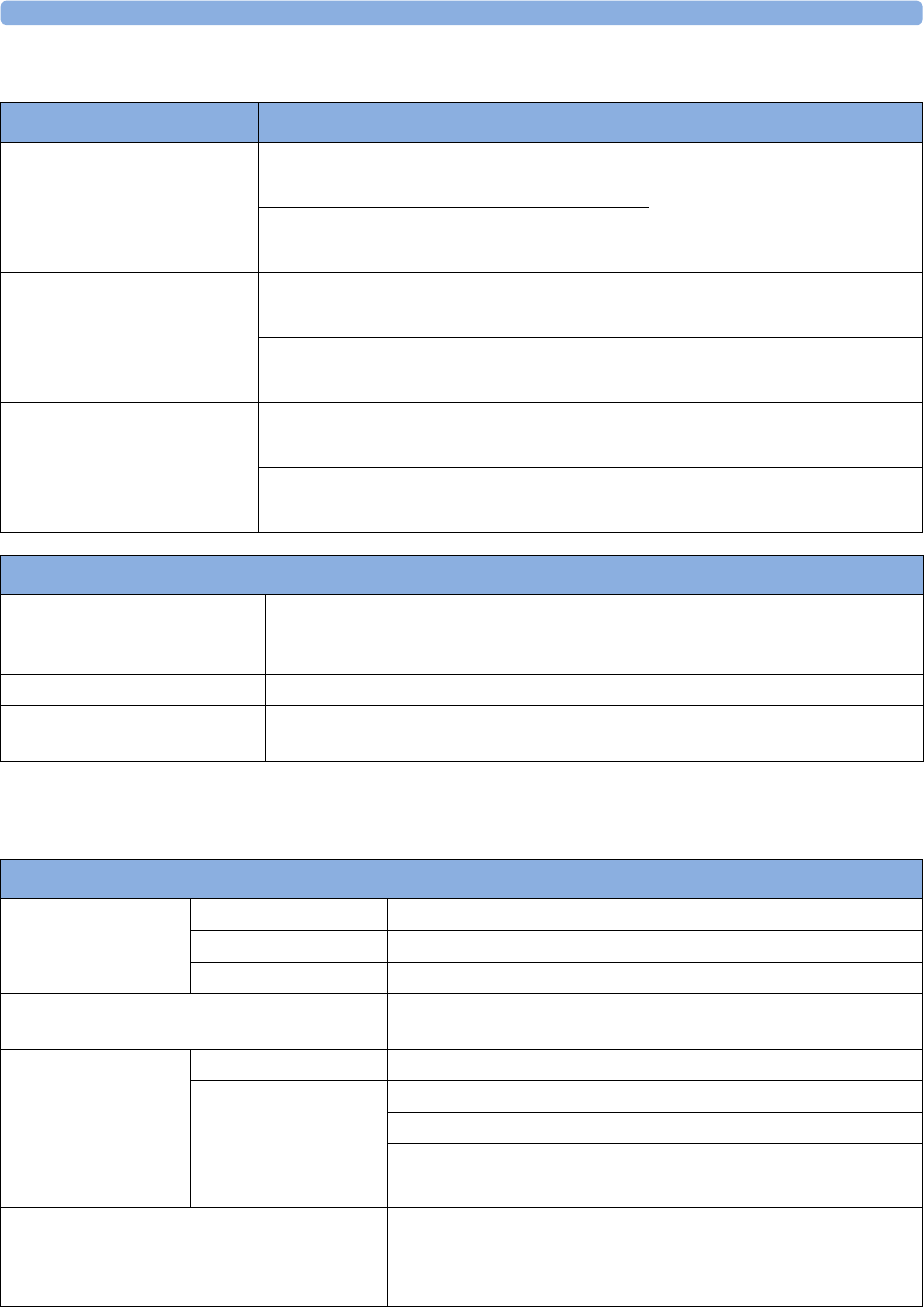
28 Specifications and Standards Compliance
279
Noninvasive Blood Pressure
Complies with IEC 80601-2-30:2010/EN 80601-2-30:2010.
MECG Alarm Specifications Range Adjustment
MECG Alarm Limits High Range: 31 to 240
Default: 120 bpm
1 bpm steps (30 to 40 bpm)
5 bpm steps (40 to 240 bpm)
Low Range: 30 to 235
Default: 50 bpm
Tachycardia Difference to high limit: 0 to 50 bpm
Default: 20 bpm
5 bpm steps
Clamping at: 150 to 240 bpm
Default: 200 bpm
5 bpm steps
Bradycardia Difference to low limit: 0 to 50 bpm
Default: 20 bpm
5 bpm steps
Clamping at: 30 to 100 bpm
Default: 40 bpm
5 bpm steps
Maternal ECG Supplemental Information as required by IEC 60601-2-27
Heart Rate Averaging Method The maternal heart rate is computed by averaging the 12 most recent RR intervals.
If each of 3 consecutive RR intervals is greater than 1200 ms (i.e. rate less than 50
bpm), then the 4 most recent RR intervals are averaged to compute the HR.
Display Update Rate 2 s
Response Time of Heart Rate
Meter to Change in Heart Rate
HR change from 80 to 120 bpm: 10 sec.
HR change from 80 to 40 bpm: 14 sec.
Performance Specifications
Measurement
Ranges
Systolic 30 to 270 mmHg (4 to 36 kPa)
Diastolic 10 to 245 mmHg (1.5 to 32 kPa)
Mean 20 to 255 mmHg (2.5 to 34 kPa)
Accuracy Max. Std. Deviation:8 mmHg (1.1 kPa)
Max. Mean Error: ±5 mmHg (±0.7 kPa)
Pulse Rate Range 40 to 300 bpm
Accuracy
(average over
noninvasive blood
pressure measurement
cycle)
40 to 100 bpm: ±5 bpm
101 to 200 bpm: ±5% of reading
201 to 300 bpm: ±10% of reading
Measurement Time Typical at HR > 60bpm
Auto/manual: 30 seconds (adult)
Maximum time: 180 seconds (adult)
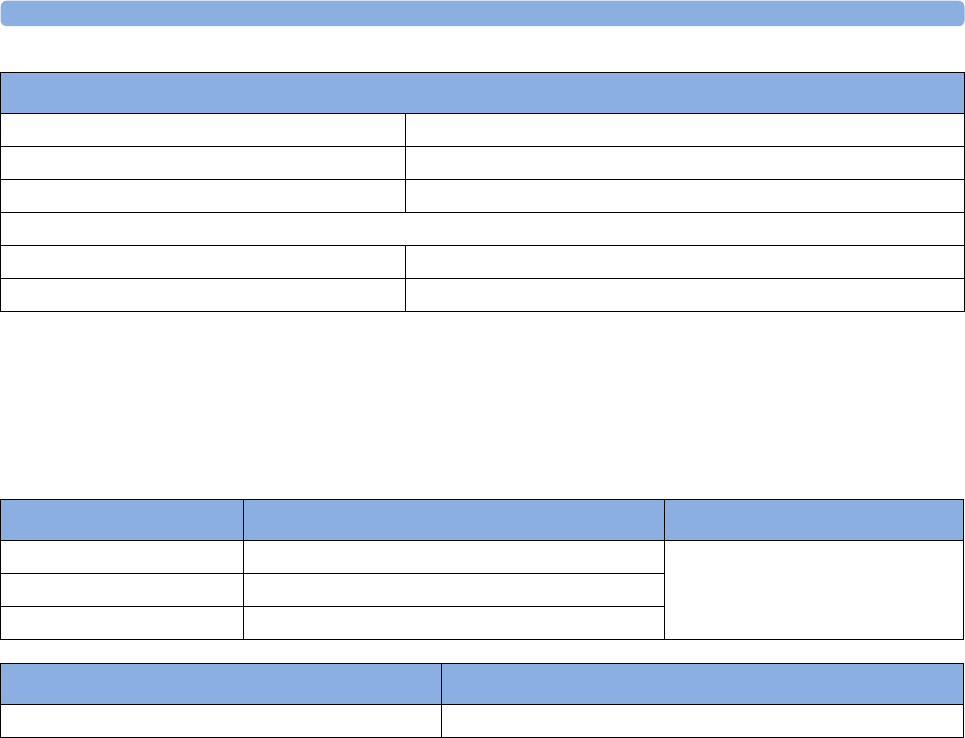
28 Specifications and Standards Compliance
280
Measurement Validation: In adult mode, the blood pressure measurements determined with this
device comply with the American National Standard for Electronic or Automated
Sphygmomanometers (ANSI/AAMI SP10:2002/A1:2003) in relation to mean error and standard
deviation, when compared to intra-arterial or auscultatory measurements (depending on the
configuration) in a representative population. For the auscultatory reference the 5th Korotkoff sound
was used to determine the diastolic pressure.
SpO2
Complies with EN/ISO 80601-2-61 2011 (except alarm system; alarm system complies with IEC
60601-1-8:2006).
Measurement Validation: The SpO2 accuracy has been validated in human studies against arterial
blood sample reference measured with a CO-oximeter. Pulse oximeter measurements are statistically
distributed, only about two-thirds of the measurements can be expected to fall within the specified
accuracy compared to CO-oximeter measurements.
Cuff Inflation Time Typical for normal adult cuff: Less than 10 seconds
Initial Cuff Inflation Pressure 165 ±15 mmHg
Auto Mode Repetition Times 1, 2, 2.5, 3, 5, 10, 15, 20, 30, 45, 60 or 120 minutes
Venipuncture Mode Inflation
Inflation Pressure 20 to 120 mmHg (3 to 16 kPa)
Automatic deflation after 170 seconds
Performance Specifications
Alarm Specifications Range Adjustment
Systolic Adult: 30 to 270 mmHg (4 to 36 kPa) 10 to 30 mmHg: 2 mmHg (0.5 kPa)
> 30 mmHg: 5 mmHg (1 kPa)
Diastolic Adult: 10 to 245 mmHg (1.5 to 32 kPa)
Mean Adult: 20 to 255 mmHg (2.5 to 34 kPa)
Overpressure Settings Adjustment
> 300 mmHg (40 kPa) > 2 sec not user adjustable
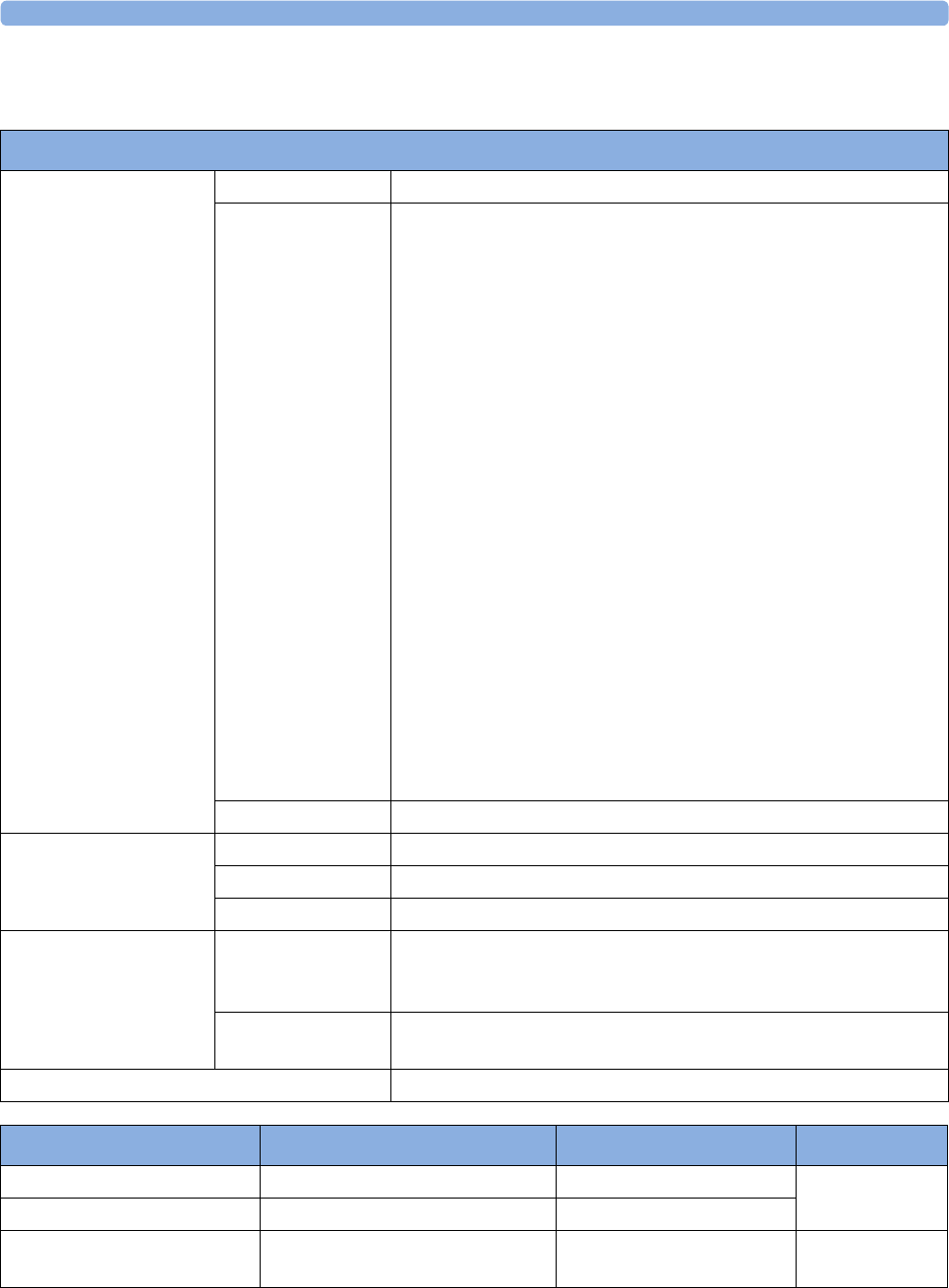
28 Specifications and Standards Compliance
281
Display Update Period: Typical: 2 seconds, Maximum: 30 seconds. Max. with noninvasive blood
pressure INOP suppression on: 60 seconds.
SpO2 Performance Specifications
SpO2
The specified accuracy is
the root-mean-square
(RMS) difference
between the measured
values and the reference
values
Range 0 to 100%
Accuracy Philips Reusable Sensors:
M1191A/B, M1191AL/BL, M1191ANL, M1192A, M1192AN =
2% (70% to 100%)
M1191T, M1192T, M1194A, M1194AN, M1196A, M1196T = 3%
(70% to 100%)
Philips Disposable Sensors with M1943A(L):
M1131A, M1901B, M1903B, M1904B = 3% (70% to 100%)
M1133A, M1134A = ±2% (70% to 100%)
NellcorPB® Sensors with M1943A(L):
MAX-A, MAX-AL, MAX-P, MAX-N, D-25, D-20, N-25, OxiCliq A,
P, N = 3% (70% to 100%)
Masimo Reusable Sensors® with LNOP MP12 or LNC MP10:
LNOP DC-I, LNOP DC-IP, LNOP YI, LNCS DC-I, LNCS DC-IP:
2% (70% to 100%)
LNOP TC-I, LNCS TC-I: 3.5% (70% to 100%)
Masimo Disposable Sensors® with LNOP MP12 or LNC
MP10:
LNOP Adt, LNOP Adtx, LNOP Pdt, LNOP Pdtx, LNCS Adtx,
LNCS Pdtx: 2% (70% to 100%)
LNOP Neo-L, LNCS Neo-L: 3% (70% to 100%)
Resolution 1%
Pulse Range 30 to 300 bpm
Accuracy ±2% or 1 bpm, whichever is greater
Resolution 1 bpm
Sensors Wavelength range 500 to 1000 nm.
Information about the wavelength range can be especially useful to
clinicians (for instance, when photodynamic therapy is performed).
Emitted Light
Energy
≤ 15mW
Pulse Oximeter Calibration Range 70% - 100%
SpO2 Alarm Specifications Range Adjustment Delay
SpO250 to 100% 1% steps (0, 1, 2, 3,... 30) +
4 seconds
Desat 50 to Low alarm limit 1% steps
Pulse 30 to 300 bpm 1 bpm steps (30 to 40 bpm)
5 bpm steps (40 to 300 bpm)
max. 14 seconds
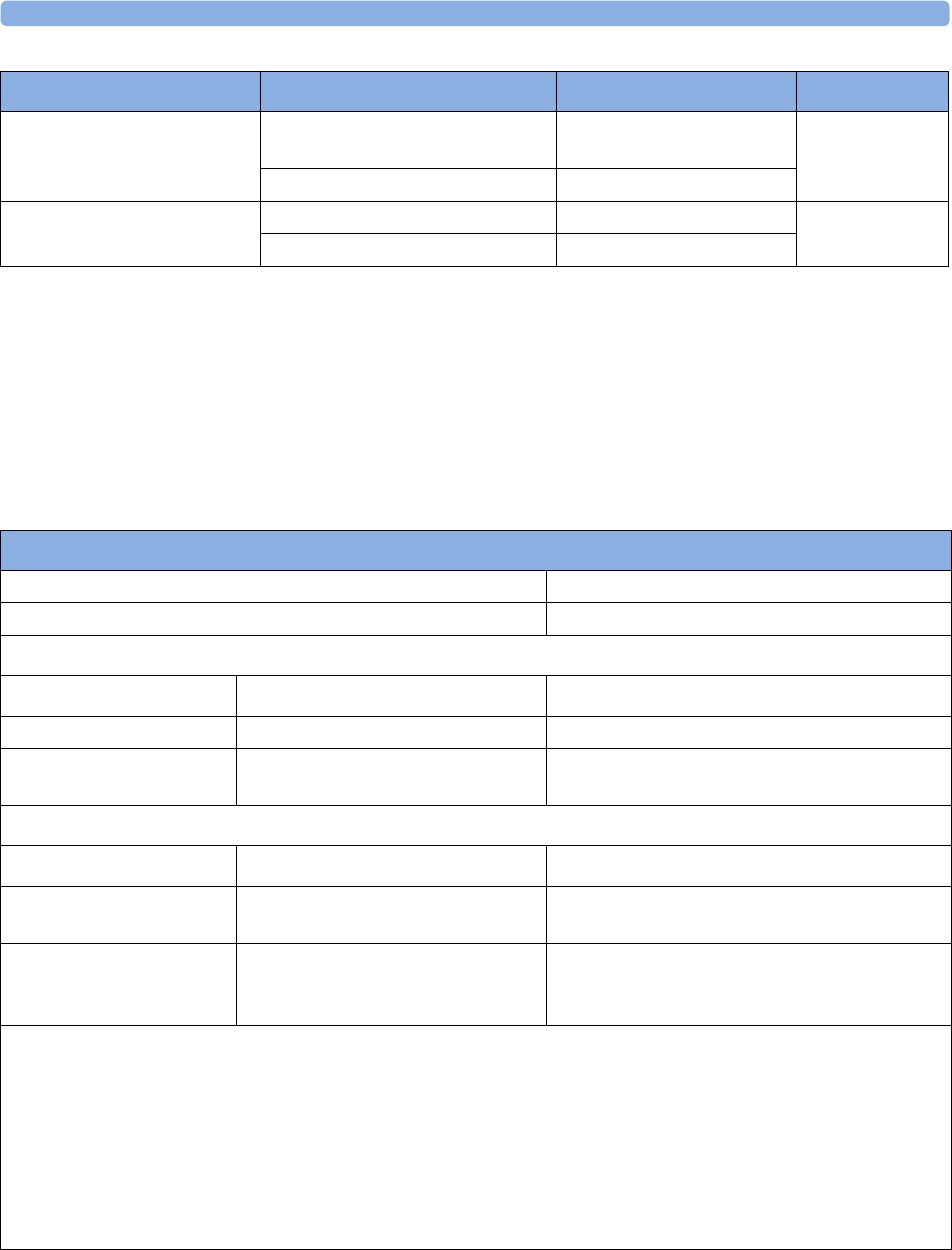
28 Specifications and Standards Compliance
282
Tympanic Temperature
Complies with:
• EN 12470-5 (Clinical thermometers - Part 5:2003: Performance of infra-red thermometers)
• ASTM E1965-98 (Infrared Thermometers for Intermittent Determination of Patient
Temperature)
with minor exceptions as noted below.
Performance Specifications
Tachycardia Difference to high limit 0 to 50
bpm
5 bpm steps max. 14 seconds
Clamping at 150 to 300 bpm 5 bpm steps
Bradycardia Difference to low limit 0 to 50 bpm 5 bpm steps max. 14 seconds
Clamping at 30 to 100 bpm 5 bpm steps
SpO2 Alarm Specifications Range Adjustment Delay
Performance Specifications
Temperature Resolution 0.1 °C or 0.1 °F
Response Time less than 2 seconds
Temperature Calibrated Accuracy Specifications (out of the Factory)
Ambient Temperature Target Temperature Accuracy
25°C (77°F) 37.7°C to 38.9°C (98.4°F to 102°F) ±0.1°C (±0.2°F)
16°C to 33°C (60.8° to
91.4°F)
33°C to 42°C (91.4°F to 107.6°F) ±0.2°C (±0.4°F)
Temperature Calibrated Accuracy Specifications (after recalibration using Genius 2 Checker/Calibrator)
Ambient Temperature Target Temperature Accuracy
16°C to 33°C (60.8° to
91.4°F)
36°C to 39°C (96.8°F to 102.2°F) ±0.2°C (±0.4°F)
16°C to 33°C (60.8° to
91.4°F)
Less than 36°C or greater then 39°C
(Less than 96.8°F or greater than
102.2°F)
±0.3°C (±0.5°F)
ASTM laboratory requirement for IR thermometers in the display range 37°C to 39°C (98°F to 102°F) is ±0.2°C
(±0.4°F), whereas for mercury-in-glass and electronic thermometers, the requirement per ASTM standards E667-86
and E1112-86 is ±0.1°C (±0.2°F).
Clinical accuracy characteristics and procedures are available from Covidien llc on request. To verify the accuracy, use
a certified black body as specified in EN 12470-5:2003, Annex C, or use a Genius 2 Checker/Calibrator - available
from Covidien llc under part number 303097.
Clinical repeatability: meets section A.5 of EN 12470-5:2003 (E) per Covidien llc technical report. Data is available
from Covidien llc on request.
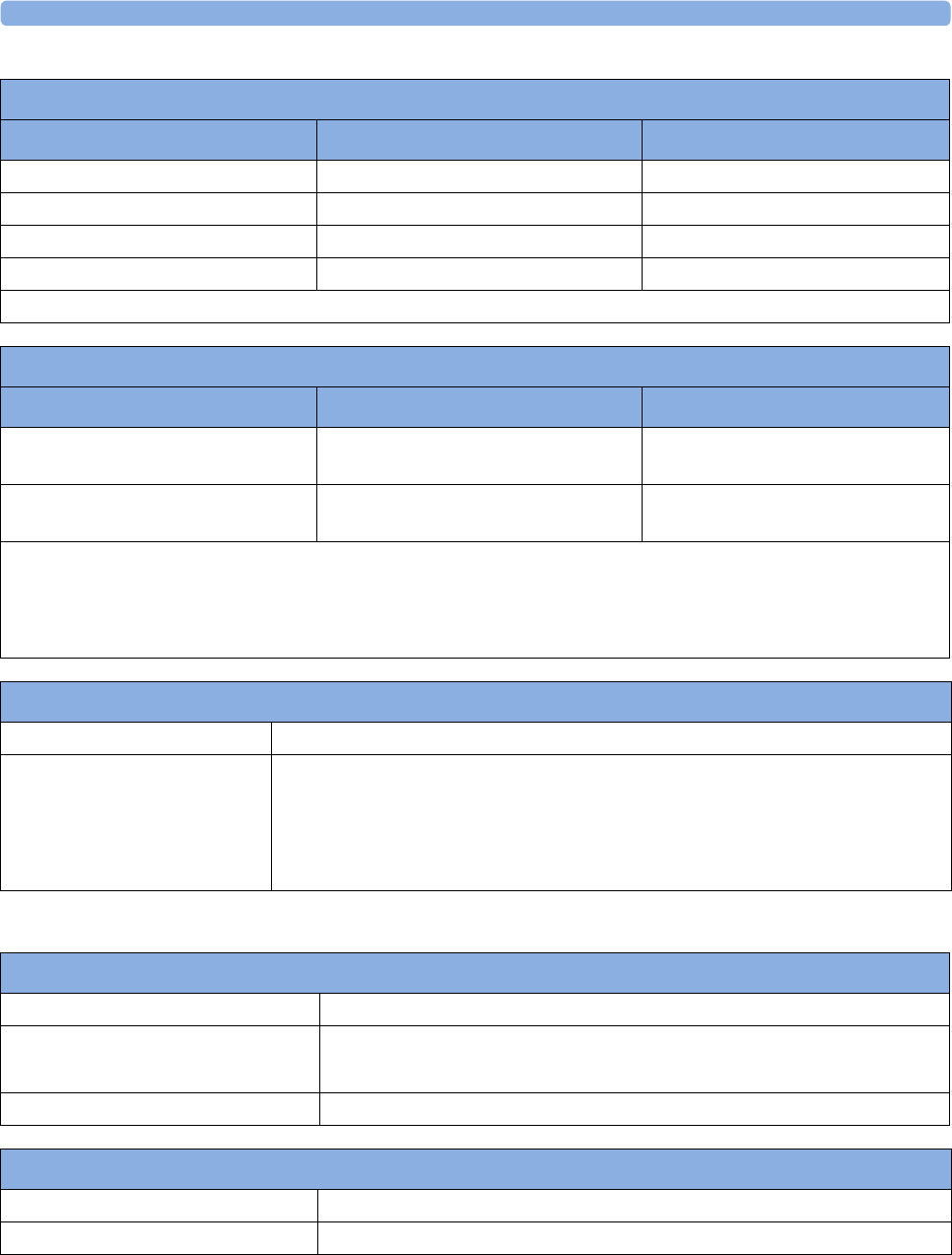
28 Specifications and Standards Compliance
283
Physical Specifications
Displayed Temperature Measurement Range
Mode Range °C Range °F
Ear 33.0 to 42.0 91.4 to 107.6
Oral (ear + 0.6. °C) 33.6 to 42.0 92.5 to 107.6
Core (ear + 1.04 °C) 34.0 to 42.0 93.2 to 107.6
Rectal (ear + 1.16 °C) 34.2 to 42.0 93.6 to 107.6
Caution: ASTM E1965-98 specifies 34.4°C to 42.2°C (94°F to 108°F)
Ambient Temperature Range
Mode Range °C Range °F
Operating 10 to 95% RH, non-
condensing
16 to 33 60.8 to 91.4
Storage up to 95% RH, non-
condensing
-25 to 55.0 -13 to 131
Caution: EN12470-5 specifies 16.0°C to 35.0° C (60.8° F to 95° F), 10 to 95% RH, non-condensing
ASTM E1965-98 specifies 16.0°C to 40.0° C (60.8° F to 104° F), up to 95% RH, non-condensing
Storing the thermometer outside the specified temperature/humidity range might adversely affect measurement
accuracy. Check the calibration after storage in uncertain conditions.
Tympanic Temperature Alarm Specifications
Range 33.0°C to 42.0° C (91° F to 108° F)
Adjustment 0.5° C steps (33° C to 35° C)
0.1° C steps (35° C to 42° C)
1.0° F steps (91° F to 95° F)
0.2° F steps (95° F to 108° F)
Thermometer
Dimensions 190 mm x 43 mm x 55 mm (±3 mm)
Cable length 60 ±5 cm (spiral cable relaxed)
250 ±15 cm (spiral cable extended)
Weight (including cable) 180 ±10 g
Base Station
Dimensions 205 mm x 65 mm x 75 mm (±3 mm)
Weight (excluding cable) 400g ±10 mm
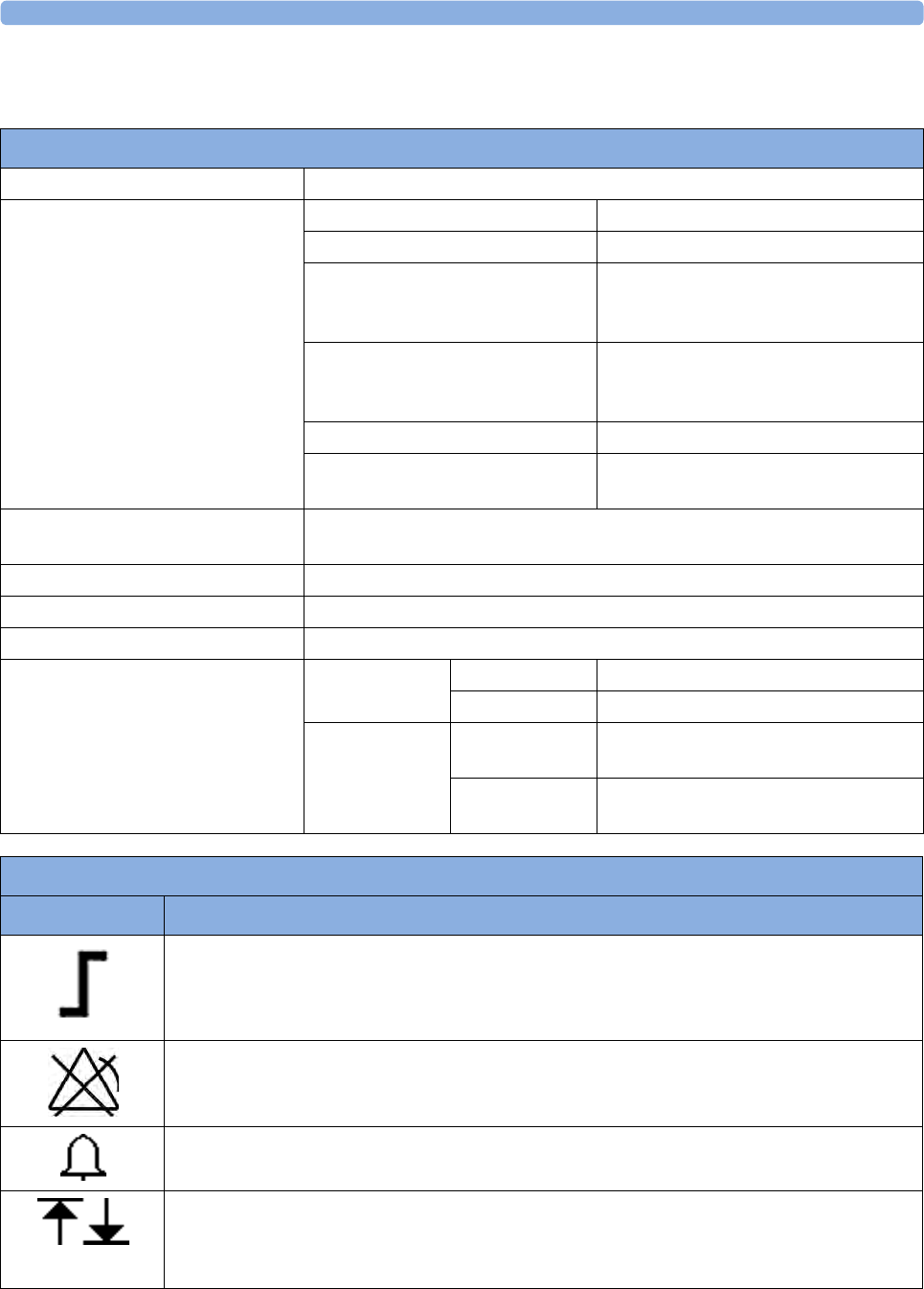
28 Specifications and Standards Compliance
284
Recorder Specifications
Built-in Thermal Array Fetal Trace Recorder
Mechanism Thermal Array Recorder
Paper & Printing Type Standard Z-fold paper
Standard Speeds (real-time traces) 3 cm/min, 2 cm/min, 1cm/min
Fast Print Speed (stored traces) Max. 20 mm/s
Print speed is variable and depends on
the print load
ECG Wave Print Speed
(not real-time)
Emulated 25 mm/s
Print speed is variable and depends on
the print load
Paper Advance 20 mm/s
Sensing Optical Reflex Sensor for black page
marks
Accuracy @ 3 cm/min, 2 cm/min,
1 cm/min
±5 mm/page
Usable Print Width 128 mm
Resolution 8 dots/mm (200 dpi)
Time Delay to see trace on paper <30s @ 1 cm/min
Trace Separation Offset for FHR
(Ultrasound and DECG)
Twin Standard FHR2 +20 bpm
Classic FHR1 +20 bpm
Triplet Standard FHR2 +20 bpm
FHR3 -20 bpm
Classic FHR1 +20 bpm
FHR3 -20 bpm
Recorder Symbols
Symbol Description
Parameter is capable of alarming and alarms were enabled at the time of printing the annotation.
Low / high limit are printed surrounding the symbol.
Parameter is capable of alarming but alarms were disabled at the time of printing the annotation.
(Note: There is no alarm related annotation at all if a parameter does not have alarming
capability.)
Alarm is on (printed next to measurement label)
Upper and lower alarm limit (printed next to measurement label)
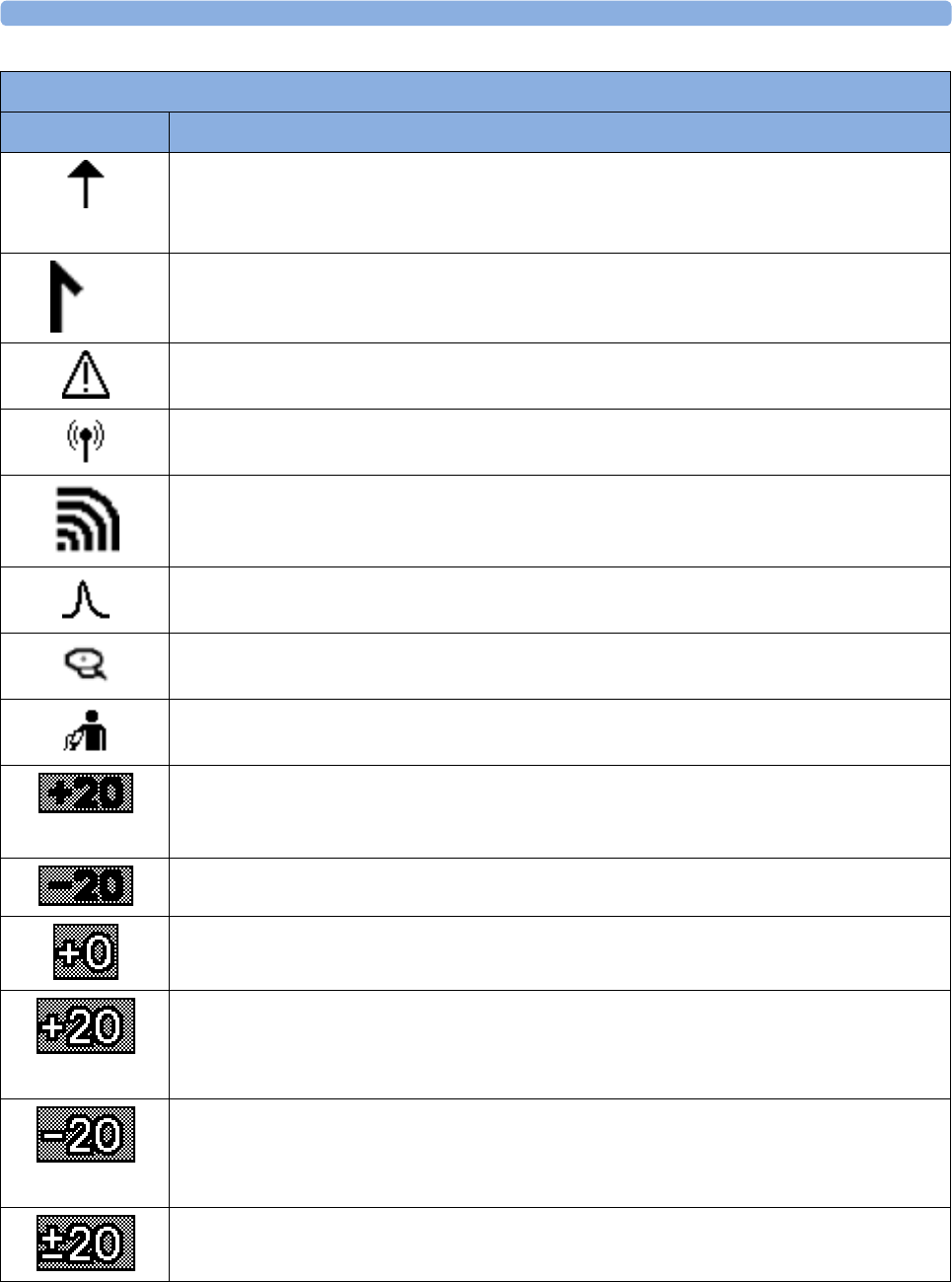
28 Specifications and Standards Compliance
285
FMP detection is on
Beginning of the date/time annotation
Warning (INOP)
Measurement from a cableless transducer (printed next to measurement label)
Measurement from a cableless maternal measurement Pod (SpO2 or NBP)
Pulse from SpO2
Pulse from Toco MP
Pulse from NBP
Trace separation +20 bpm (in label)
Trace separation -20 bpm (in label)
Trace separation Off (in trace)
Trace separation +20 bpm (in trace)
Trace separation -20 bpm (in trace)
Trace separation +20 bpm and -20 bpm (in trace)
Recorder Symbols
Symbol Description
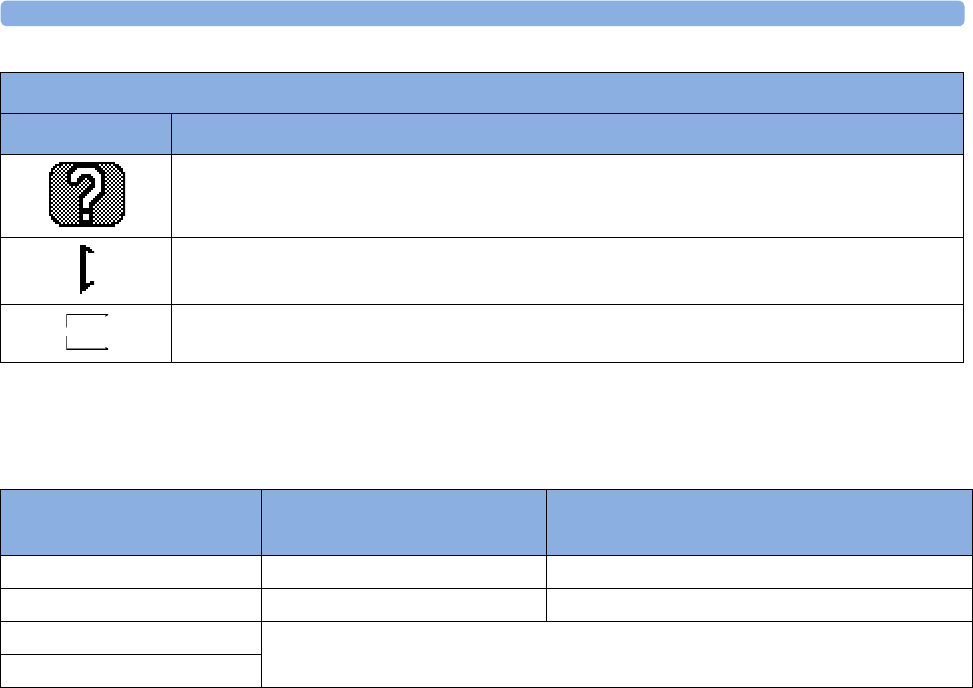
28 Specifications and Standards Compliance
286
Compatible External Displays: FM40/FM50 Only
External displays can be connected with a maximum cable run of 10 m.
* The video output of the Avalon FM40/FM50 has VGA resolution.
Manufacturer's Information
You can write to Philips at this address:
Philips Medizin Systeme Boeblingen GmbH
Hewlett-Packard-Str. 2
71034 Boeblingen
Germany
Visit our website for local contact information at: www.healthcare.philips.com
© Copyright 2013. Koninklijke Philips N.V. All Rights Reserved.
Trademark Acknowledgment
OxisensorTM II, Oxi-CliqTM, and OxiMaxTM are trademarks of Tyco Healthcare Group LP, Nellcor
Puritan Bennett Division.
Coincidence of heart rates is detected
Marker
Special wave, with different speed and scale (for example, fast printout of MECG wave on
FM30)
Recorder Symbols
Symbol Description
Compatible Display
Specifications
External XGA Display
(M8031B)
External SXGA Display (M8033C)
Resolution* 1024 x 768 1280 x 1024 pixel
Refresh frequency 60 Hz or 75 Hz 60 Hz
Useful screen Depends on size of display
Pixel size
28 Specifications and Standards Compliance
287
Regulatory and Standards Compliance
The monitor is in conformity with the requirements of the European Medical Devices Directive 93/
42/EEC and bears the CE marking:
The monitor is classified into Class IIb to Annex IX rule 10.
Safety and Performance
The monitor complies with the following major international safety and performance standards:
• IEC 60601-1:2005+A1:2012 / EN 60601-1:2006+AC:2010
• IEC 60601-1-6:2010 / EN 60601-1-6:2010
• IEC 60601-1-8:2006 / EN 60601-1-8:2007+AC:2010
• IEC 60601-2-27:2011+AC:2012 / EN 60601-2-27:2006+AC:2006
• IEC 80601-2-30:2009+C1:2010 / EN 80601-2-30:2010
• IEC 60601-2-37:2007 / EN 60601-2-37:2008
• IEC 60601-2-49:2011 / EN 60601-2-49:2001
• ISO 80601-2-61:2011 / EN 80601-2-61:2011
• ANSI/AAMI ES60601-1+C1:2009+A2:2010
• CAN/CSA C22.2#60601-1-08+TC2:2011
• JIS T 1303 2005
• AS/NZS 3200.1.0-1998
The possibility of hazards arising from hardware and software errors was minimized in compliance
with ISO 14971:2012, IEC 60601-1:2005+A1:2012 / EN 60601-1:2006+AC:2010.
Alarm sounds are compliant with Standard ISO/IEC 9703-2 and IEC 60601-1-8:2006 / EN 60601-1-
8:2007+AC:2010.
28 Specifications and Standards Compliance
288
Safety Tests Fetal Monitor
All the safety tests and procedures required after an installation or an exchange of system components
are described in your monitor's Service Guide. These safety tests are derived from international
standards but may not be sufficient to meet local requirements.
WARNING
• Do not use additional AC mains extension cords or multiple portable socket-outlets. If a multiple
portable socket-outlet is used, the resulting system must be compliant with IEC/EN 60601-1 A1:
2012.
• Do not connect any devices that are not supported as part of a system.
• Do not use a device in the patient vicinity if it does not comply with IEC/EN 60601-1-1. The
whole installation, including devices outside of the patient vicinity, must comply with IEC/EN
60601-1 A1: 2012. Any non-medical device, including a PC running an OB TraceVue/IntelliSpace
Perinatal system, placed and operated in the patient's vicinity must be powered via a separating
transformer (compliant with IEC/EN 60601-1 A1: 2012) that ensures mechanical fixing of the
power cords and covering of any unused power outlets.
• Do not use USB devices with own power supplies unless an appropriate separation device is used
(either between USB interface and device or between device and power).
During the installation the fetal monitor is configured for your environment. This configuration
defines your custom default settings you work with when you switch on your fetal monitor. See the
Fetal Monitor's Service Guide and the Configuration Guide for details on how to configure your fetal
monitor.
Electromagnetic Compatibility (EMC)
The device and its accessories, listed in the accessories section, comply with the following EMC
standards:
• EN 60601-1-2+AC:2010 (IEC 60601-1-2:2007)
Take special precautions regarding electromagnetic compatibility (EMC) when using medical electrical
equipment. You must operate your monitoring equipment according to the EMC information
provided in this book. Before using the device, assess the electromagnetic compatibility of the device
with surrounding equipment.
This ISM device complies with Canadian ICES-003:2012. Cet appareil ISM est conforme à la norme
NMB-003 du Canada.
CAUTION
•FM20/FM30 only: Although this is an electrical Class II device, it has a protective earth
conductor which is needed for EMC purposes.
• Always use the supplied power cord with the three-prong plug to connect the monitor to AC
mains. Never adapt the three-prong plug from the power supply to fit a two-slot outlet.
28 Specifications and Standards Compliance
289
CAUTION
The use of accessories, transducers and cables other than those specified may result in increased
electromagnetic emissions or decreased electromagnetic immunity of the device.
WARNING
Do not use cordless/mobile phones or any other portable RF communication system within the
patient vicinity, or within a 1.0 m radius of any part of the fetal monitoring system.
WARNING
For paced patients: The radiated SRR power of the CL SpO2 and CL NBP Maternal Cableless
Measurement Devices, and other sources of radio-frequency energy, when used in very close proximity
of a pacemaker, might be sufficient to interfere with pacemaker performance. Due to shielding effects
of the body, internal pacemakers are somewhat less vulnerable than external pacemakers. However,
caution should be exercised when monitoring paced patients.
In order to minimize the possibility of interference, avoid positioning and wearing the Cableless
Measurement Devices in very close proximity to a pacemaker. Consult the pacemaker manufacturer
for information on the RF susceptibility of their products
EMC Testing
CAUTION
Fetal parameters, especially ultrasound and ECG, are sensitive measurements involving small signals,
and the monitoring equipment contains very sensitive high gain front-end amplifiers. Immunity levels
for radiated RF electromagnetic fields and conducted disturbances induced by RF fields are subject to
technological limitations. To ensure that external electromagnetic fields do not cause erroneous
measurements, it is recommended to avoid the use of electrically radiating equipment in close
proximity to these measurements.
28 Specifications and Standards Compliance
290
Reducing Electromagnetic Interference
CAUTION
The device should not be used adjacent to, or stacked with, other equipment unless otherwise
specified.
The product and associated accessories can be susceptible to interference from continuous, repetitive,
power line bursts, and other RF energy sources, even if the other equipment is compliant with EN
60601-1-2 emission requirements. Examples of other sources of RF interference are other medical
electrical devices, cellular products, information technology equipment, and radio/television
transmissions.
When electromagnetic interference (EMI) is encountered, for example, if you can hear spurious noises
on the fetal monitor's loudspeaker, attempt to locate the source. Assess the following:
• Is the interference due to misplaced or poorly applied transducers? If so, re-apply transducers
correctly according to directions in this book or in the Instructions for Use accompanying the
accessory.
• Is the interference intermittent or constant?
• Does the interference occur only in certain locations?
• Does the interference occur only when in close proximity to certain medical electrical equipment?
Once the source is located, there are a number of things that can be done to mitigate the problem:
1Eliminating the source. Turn off or move possible sources of EMI to reduce their strength.
2Attenuating the coupling. If the coupling path is through the patient leads, the interference may be
reduced by moving and/or rearranging the leads. If the coupling is through the power cord,
connecting the system to a different circuit may help.
3Adding external attenuators. If EMI becomes an unusually difficult problem, external devices such
as an isolation transformer or a transient suppressor may be of help. Your service provider can be
of help in determining the need for external devices.
Where it has been established that electromagnetic interference is affecting physiological parameter
measurement values, a physician, or a suitably qualified person authorized by a physician, should
determine if it will negatively impact patient diagnosis or treatment.
System Characteristics
The phenomena discussed above are not unique to this system but are characteristic of fetal patient
monitoring equipment in use today. This performance is due to very sensitive high gain front end
amplifiers required to process the small physiological signals from the patient. Among the various
monitoring systems already in clinical use, interference from electromagnetic sources is rarely a
problem.
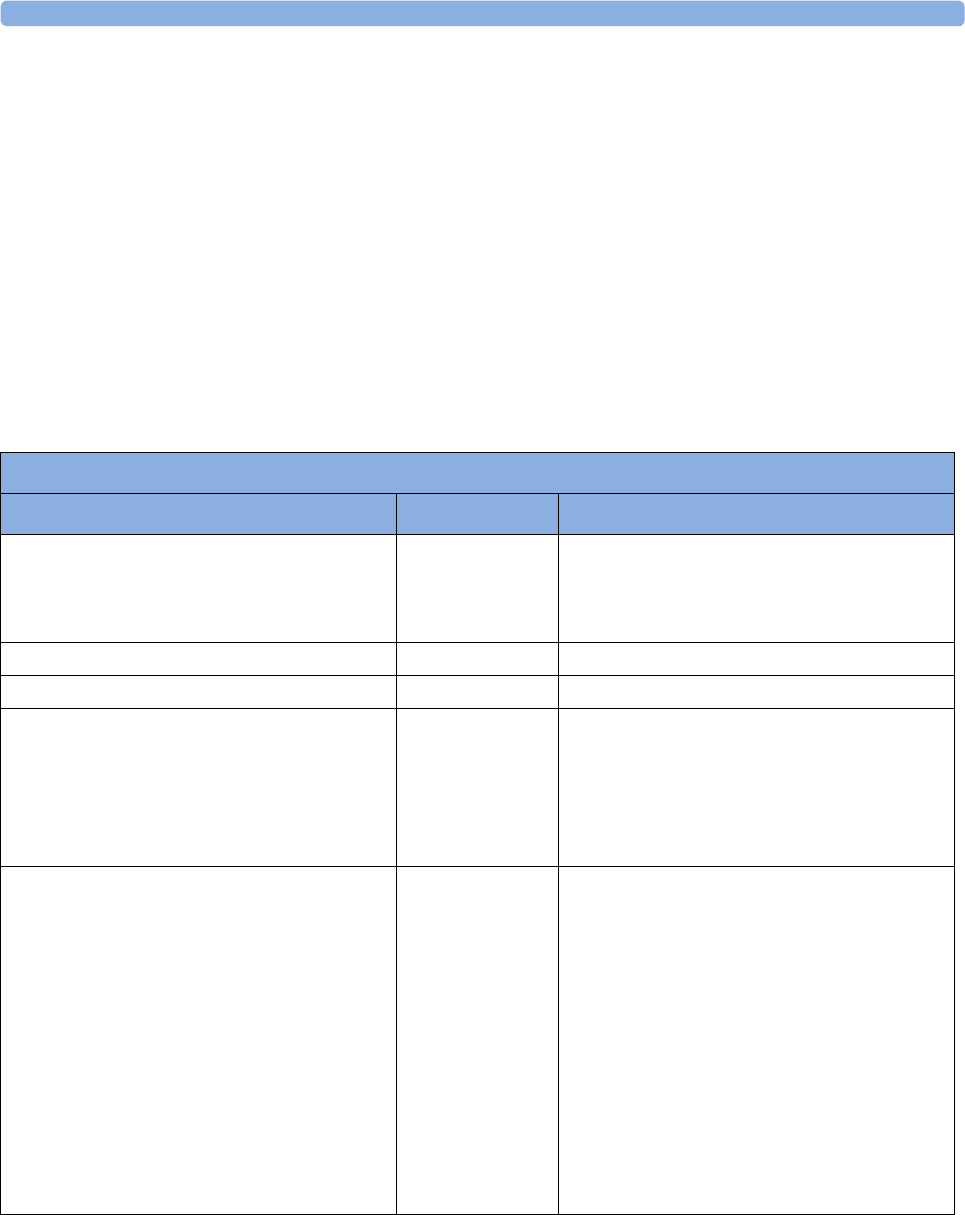
28 Specifications and Standards Compliance
291
Electromagnetic Emissions and Immunity
The EMC standards state that manufacturers of patient-coupled equipment must specify immunity
levels for their systems. See Tables 1 to 4 for this detailed immunity information. See Table 5 for
recommended minimum separation distances between portable and mobile communications
equipment and the product.
Immunity is defined in the standard as the ability of a system to perform without degradation in the
presence of an electromagnetic disturbance.
Caution should be exercised in comparing immunity levels between different devices. The criteria used
for degradation are not always specified by the standard and can therefore vary with the manufacturer.
In the table below, the term "device" refers to the Avalon FM20/30/40/50 fetal monitor together with
its accessories. The table gives details of the electromagnetic emissions, and how these are classified,
for the device, and the electromagnetic environments in which the device is specified to technically
function.
1 Note that the device is not intended for home use.
Electromagnetic Immunity
The monitor is suitable for use in the specified electromagnetic environment. The user must ensure
that it is used in the appropriate environment as described below.
Table 1 - Guidance and Manufacturer's Declaration: Electromagnetic Emissions
Emissions Test Compliance Avoiding Electromagnetic Interference
Radiofrequency (RF) emissions Group 1 The device uses RF energy only for its internal
function. Therefore, its RF emissions are very
low and are not likely to cause any interference
in nearby electronic equipment.
Harmonic emissions IEC 61000-3-2 Class A
Voltage fluctuations and flicker IEC 61000-3-3 complies
RF emissions CISPR 11
For the Avalon FM20/30 fetal monitor with all
accessories except the IUP/ECG patient
module M2738A.
Class B The device is suitable for use in all
establishments, including domestic
establishments and those directly connected to
the public low-voltage supply network that
supplies buildings used for domestic purposes
1.
RF emissions CISPR 11
For the Avalon FM40/FM50 with all
accessories.
For the Avalon FM20/30 fetal monitor
whenever used with the IUP/ECG patient
module M2738A.
For the Avalon CTS Interface Cable (M2731-
60001/M2732-60001) whenever used with the
Avalon CTS Cableless Fetal Transducer System.
For the Avalon CL Base Station with cableless
transducers whenever used with the fetal
monitors.
Class A The device is suitable for use in all
establishments other than domestic
establishments and those directly connected to
the public low-voltage supply network that
supplies buildings used for domestic purposes.
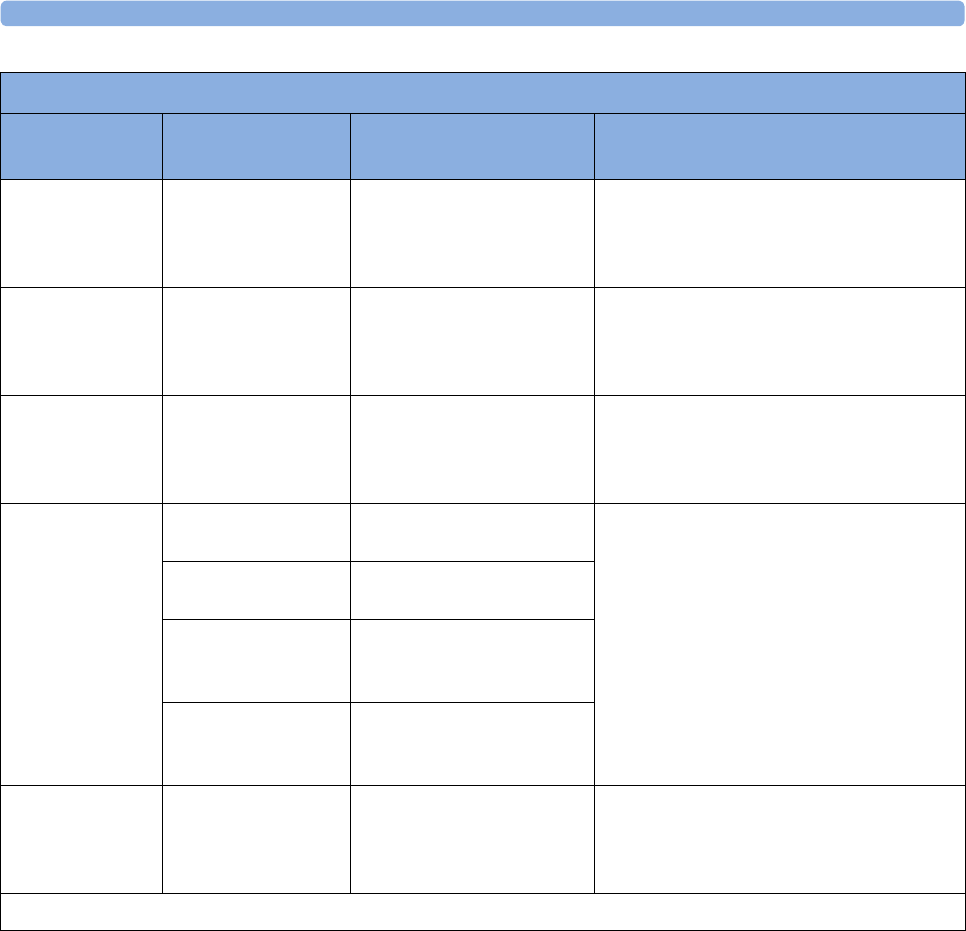
28 Specifications and Standards Compliance
292
Table 2 - Guidance and Manufacturer's Declaration: Electromagnetic Immunity
Immunity Test IEC 60601-1-2
Test Level
Compliance Level Electromagnetic Environment
Guidance
Electrostatic
discharge (ESD)
IEC 61000-4-2
± 6 kV contact
± 8kV air
± 6 kV contact
± 8kV air
Floors should be wood, concrete, or ceramic
tile. If floors are covered with synthetic
material, the relative humidity should be at
least 30%.
Electrical fast
transient/burst
IEC 61000-4-4
± 2 kV for power
supply lines
± 1 kV for input/
output lines
± 2 kV for power supply
lines
± 1 kV for input/output
lines
Mains power quality should be that of a
typical commercial and/or hospital
environment
Surge
IEC 61000-4-5
± 1 kV differential
mode
± 2 kV common
mode
± 1 kV differential mode
± 2 kV common mode
Mains power quality should be that of a
typical commercial and/or hospital
environment
Voltage dips, short
interruptions and
voltage variations
on power supply
input lines
IEC 61000-4-11
<5% UT (> 95% dip
in UT) for 0.5 cycles
<5% UT (> 95% dip in UT)
for 0.5 cycles
Mains power quality should be that of a
typical commercial and/or hospital
environment. If the user of the device
requires continued operation during power
mains interruptions, it is recommended that
the device is powered from an
uninterruptible power supply.
40% UT (60% dip in
UT) for 5 cycles
40% UT (60% dip in UT) for
5 cycles
70% UT
(30% dip in UT) for
25 cycles
70% UT (30% dip in UT) for
25 cycles
< 5% UT
(> 95% dip in UT) for
5 sec
< 5%UT (> 95% dip in UT)
for 5 sec
Power frequency
(50/60 Hz)
magnetic field
IEC 61000-4-8
3 A/m 3 A/m Power frequency magnetic fields should be
at levels characteristic of a typical location in
a typical commercial and/or hospital
environment
Key: UT is the AC mains voltage prior to application of the test level.

28 Specifications and Standards Compliance
293
Radio Compliance Notice
Avalon CL with WMTS
Operation of this equipment requires the prior coordination with a frequency coordinator designated
by the FCC for the Wireless Medical Telemetry Service.
This device complies with Part 15 of the FCC Rules and RSS-210 of Industry Canada. Operation is
subject to the following two conditions: (1) this device may not cause harmful interference, and (2) this
device must accept any interference received, including interference that may cause undesired
operation. Any changes or modifications to this equipment not expressly approved by Philips Medical
Systems may cause harmful radio frequency interference and void your authority to operate this
equipment.
Installation of this telemetry device is permitted in hospitals and health care facilities only. This device
shall not be operated in mobile vehicles (including ambulances and other vehicles associated with
health care facilities). The installer/user of this device shall ensure that it is at least 80 km from the
Dominion Radio Astrophysical Observatory (DRAO) near Penticton, British Columbia. The
coordinates of DRAO are: latitude N 49E 19' 15", longitude W 119° 37′ 12″. For medical telemetry
systems not meeting this 80 km separation (e.g. the Okanagan Valley, British Columbia) the installer/
user must coordinate with, and obtain the written concurrence of, the Director of DRAO before the
equipment can be installed or operated. The Director of DRAO may be contacted at 250-497-2300
(telephone) or 250-497-2355 (fax). (Alternatively, the Manager, Regulatory Standards, Industry Canada,
may be contacted.)
Le présent appareil est conforme aux CNR d'Industrie Canada applicables aux appareils radio exempts
de licence. L'exploitation est autorisée aux deux conditions suivantes: (1) l'appareil ne doit pas produire
de brouillage, et (2) l'utilisateur de l'appareil doit accepter tout brouillage radioélectrique subi, même si
le brouillage est susceptible d'en compromettre le fonctionnement.
L'utilisation de cet appareil de télémesure est permise seulement dans les hôpitaux et établissements de
soins de santé. Cet appareil ne doit pas être mis en marche dans des véhicules (y compris les
ambulances et autres véhicules associés aux établissements de santé). La personne qui installe/utilise
cet appareil doit s’assurer qu’il se trouve à au moins 80 km de l’Observatoire fédéral de
radioastrophysique (OFR) de Penticton en Colombie-Britannique. Les coordonnées de l’OFR sont :
latitude N 49° 19’ 15», longitude O 119° 37 12 ′′. La personne qui installe/utilise un système de
télémesure médicale ne pouvant respecter cette distance de 80 km (p. ex. dans la vallée de l’Okanagan
(Colombie-Britannique), doit se concerter avec le directeur de l’OFR et obtenir de sa part une
autorisation écrite avant que l’équipement ne puisse être installé ou mis en marche. Le directeur de l’
OFR peut être contacté au 250-497-2300 (tél.) ou au 250-497-2355 (télécopieur). (Le Directeur des
Norm es réglementaires d’Industrie Canada peut également être contacté).
Avalon CL with T108
Japanese Radio Law and Japanese Telecommunications Business Law Compliance.
This device should not be modified (otherwise the granted designation number will become invalid).
28 Specifications and Standards Compliance
294
Finding Recommended Separation Distances
In the following table, P is the maximum output power rating of the transmitter in watts (W) according
to the transmitter manufacturer, and d is the recommended separation distance in meters (m).
Portable and mobile RF communications equipment should be used no closer to any part of the
device, including cables, than the recommended separation distance calculated from the equation
appropriate for the frequency of the transmitter.
Field strengths from fixed RF transmitters, as determined by an electromagnetic site survey, should be
less than the compliance level in each frequency range.
Interference may occur in the vicinity of equipment marked with this symbol:
Table 3 - Guidance and Manufacturer's Declaration: Electromagnetic Immunity
Conducted RF Immunity Test EN/IEC 61000-4-6
IEC 60601-1-2 Test Level
over 150 kHz to 80 MHz Compliance Level
Electromagnetic Environment Guidance:
Recommended Separation Distance (d)
(in Meters, at Frequency Range Tested)
for Ultrasound and ECG Measurements
3.0 VRMS 3.0 VRMS d = 1, 2√P
Key: d = Recommended separation distance in meters (m)
P = maximum output power rating of the transmitter in watts (W) according to the transmitter manufacturer
V1 = Tested compliance level (in Volts) for the Conducted RF Immunity test IEC 61000-4-6
The device meets the compliance level of 3.0 VRMS according to IEC 60601-1-2 over the specified test frequency
range. Over the frequency range 150 kHz to 80 MHz, the recommended separation distance in meters (d) is found by
the following equation:
For a compliance level of 3.0 VRMS:d = 1, 2√P
Table 4 - Guidance and Manufacturer's Declaration: Electromagnetic Immunity
Radiated RF Immunity Test EN/IEC 61000-4-3
IEC 60601-1-2 Test Level
over 80 MHz to 2.5 GHz Compliance Level
Electromagnetic Environment Guidance:
Recommended Separation Distance (d)
(in Meters, at Frequency Range Tested)
for Ultrasound and ECG Measurements
3.0 V/m 3.0 V/m Over 80 MHz to 800 MHz:d = 1, 2√P
Over 800 MHz to 2.5 GHz:d = 2, 3√P
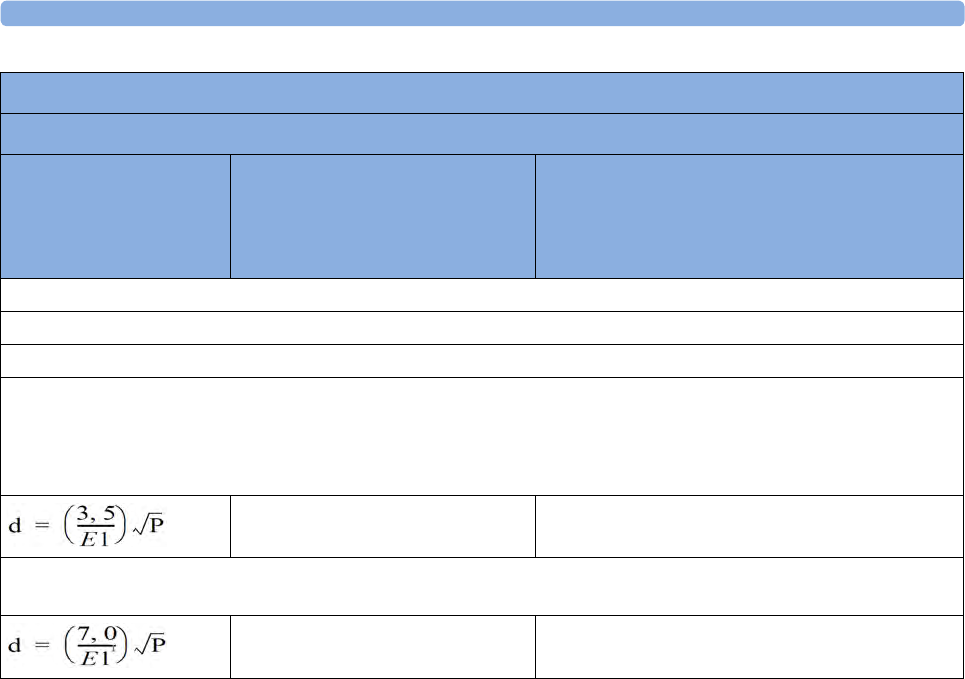
28 Specifications and Standards Compliance
295
Field strengths from fixed transmitters, such as base stations or radio (cellular, cordless) telephones
and land mobile radios, amateur radio, AM and FM radio broadcast and TV broadcast cannot be
predicted theoretically with accuracy. To assess the electromagnetic environment due to fixed RF
transmitters, an electromagnetic site survey should be considered. If the measured field strength in the
location in which the device is used exceeds the applicable RF compliance level above, it should be
observed to verify normal operation. If abnormal performance is observed, additional measures may
be necessary, such as reorienting or relocating the device.
These guidelines may not apply in all situations. Electromagnetic propagation is affected by absorption
and reflection from structures, objects, and people.
If you require further information or assistance, please contact Philips Support.
Key: d = Recommended separation distance in meters (m)
P = maximum output power rating of the transmitter in watts (W) according to the transmitter manufacturer
E1 = Tested compliance level (in Volts/meter) for the Radiated RF Immunity test IEC 61000-4-3
The device meets the compliance level of 3.0 VRMS according to IEC 60601-1-2 over the specified test frequency
range.
Over the frequency range 80 kHz to 800 MHz, the recommended separation distance in meters (d) is found by the
following equation:
For a compliance level of 3.0 VRMS:d = 1, 2√P
Over the frequency range 800 kHz to 2.5 GHz, the recommended separation distance in meters (d) is found by the
following equation:
For a compliance level of 3.0 VRMS:d = 2, 3√P
Table 4 - Guidance and Manufacturer's Declaration: Electromagnetic Immunity
Radiated RF Immunity Test EN/IEC 61000-4-3
IEC 60601-1-2 Test Level
over 80 MHz to 2.5 GHz Compliance Level
Electromagnetic Environment Guidance:
Recommended Separation Distance (d)
(in Meters, at Frequency Range Tested)
for Ultrasound and ECG Measurements
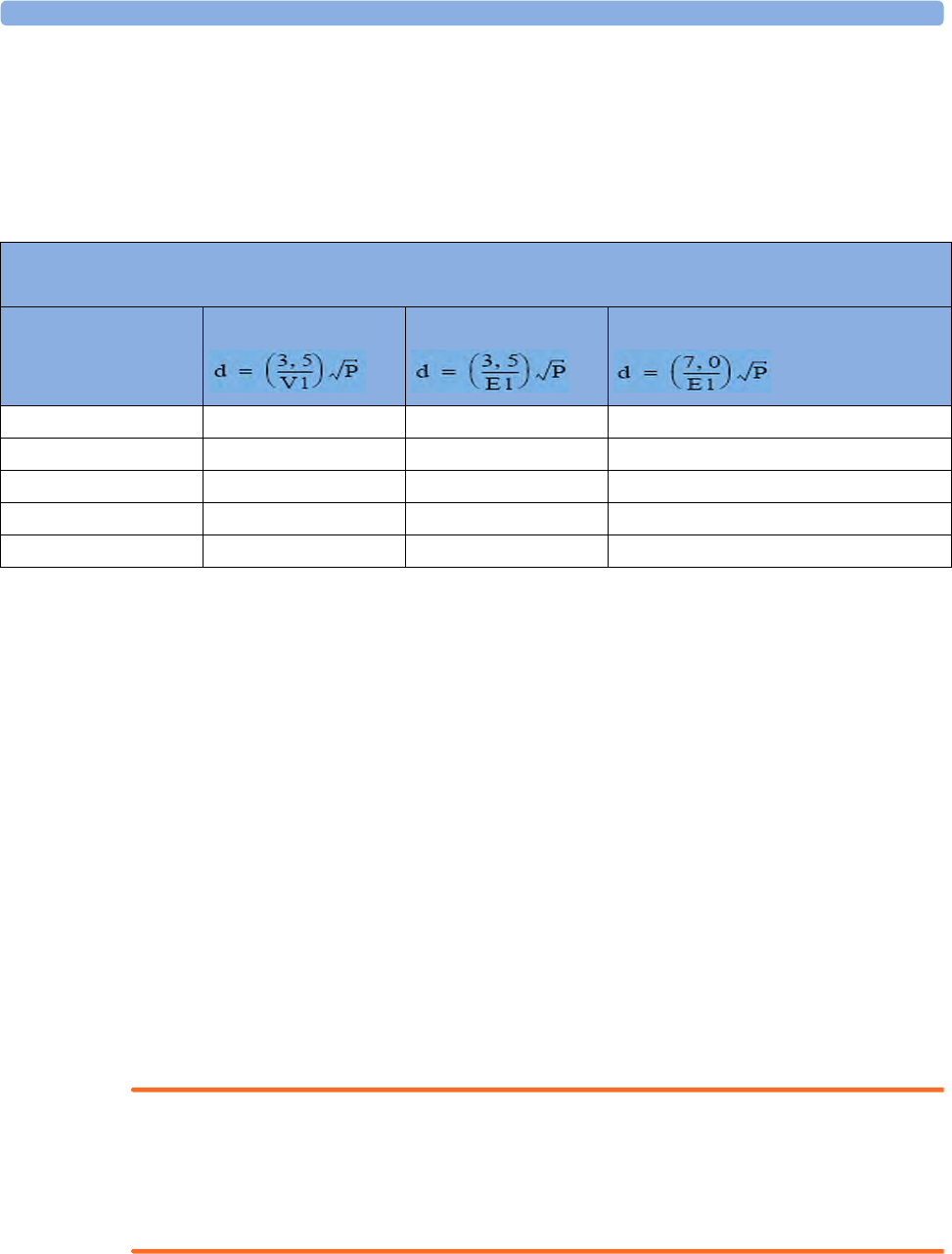
28 Specifications and Standards Compliance
296
Recommended Separation Distances from Other RF Equipment
The device is intended for use in an electromagnetic environment in which radiated RF disturbances
are controlled. The customer or user of the device can help prevent electromagnetic interference by
maintaining a minimum distance between portable and mobile RF communications equipment and the
device as recommended below, according to the maximum output power of the communications
equipment.
Radio Frequency Radiation Exposure Information
The radiated output power of the device is far below the FCC radio frequency exposure limits.
Nevertheless, the device shall be used in such a manner that the potential for human contact during
normal operation is minimized.
Environment
Before operation, make sure that the fetal monitor is free from condensation. This can form when
equipment is moved from one building to another, and is exposed to moisture and differences in
temperature.
Use the monitor in an environment which is reasonably free from vibration, dust, corrosive or
explosive gasses, extremes of temperature, humidity, and so forth. It operates within specifications at
ambient temperatures between 0 and +45°C (32°F to 113°F). Ambient temperatures that exceed these
limits can affect the accuracy of the system, and can damage the components and circuits.
Ambient temperature ranges for storage are -20°C to +60°C (-4°F to 140°F) for the monitor, and -
40°C to +60°C (-40°F to 140°F) for transducers.
The transducers are watertight to a depth of 1.0 m for at least five hours (rated IP 68).
WARNING
•Leakage currents: If several items of equipment used to monitor a patient are interconnected,
the resulting leakage current may exceed allowable limits.
•ECG electrodes: NEVER allow ECG electrodes to contact other electrical conductive parts,
including earth.
Table 5 - Separation Distance (d) in Meters According to Frequency of Transmitter at IEC 60601-1-2 Test
Compliance Level
Rated Maximum Output
Power (P) of Transmitter
(in Watts)
150 kHz to 80 MHz 80 MHz to 800 MHz 800 MHz to 2.5 GHz
0.01 W 0.1 m 0.1 m 0.23 m
0.1 W 0.4 m 0.4 m 0.7 m
1 W 1.2 m 1.2 m 2.3 m
10 W 3.8 m 3.8 m 7.3 m
100 W 12.0 m 12.0 m 23.0 m
28 Specifications and Standards Compliance
297
Monitoring After a Loss of Power
If the monitor is without power for less than one minute, monitoring will resume with all active
settings unchanged. If the monitor is without power for more than one minute, the behavior depends
on your configuration. If Automat. Default is set to Yes, the User Defaults will be loaded when power
is restored. If Automat. Default is set to No, all active settings are retained, if power is restored within
48 hours. The Automat. Default setting is made in Configuration mode.
FM20/30
with
Battery
Option,
FM40/50
When power is lost - no power is available from the AC power source or from the battery - a beeper
will sound. The tone can be silenced by pressing the On/Standby switch.
ESU, MRI and Defibrillation
WARNING
The fetal/maternal monitors are NOT intended for use during defibrillation, electro-surgery, or MRI.
Remove all transducers, sensors, and accessories before performing electro-surgery, defibrillation, or
MRI, otherwise harm to the patient or the user can result.
Cardiac Pacemakers and Electrical Stimulators
WARNING
The fetal/maternal monitors are not intended for use for ECG measurements on patients connected
to external electrical stimulator or with cardiac pacemakers.
Fast Transients/Bursts
The equipment will return to the previous operating mode within 10 seconds without loss of any
stored data.
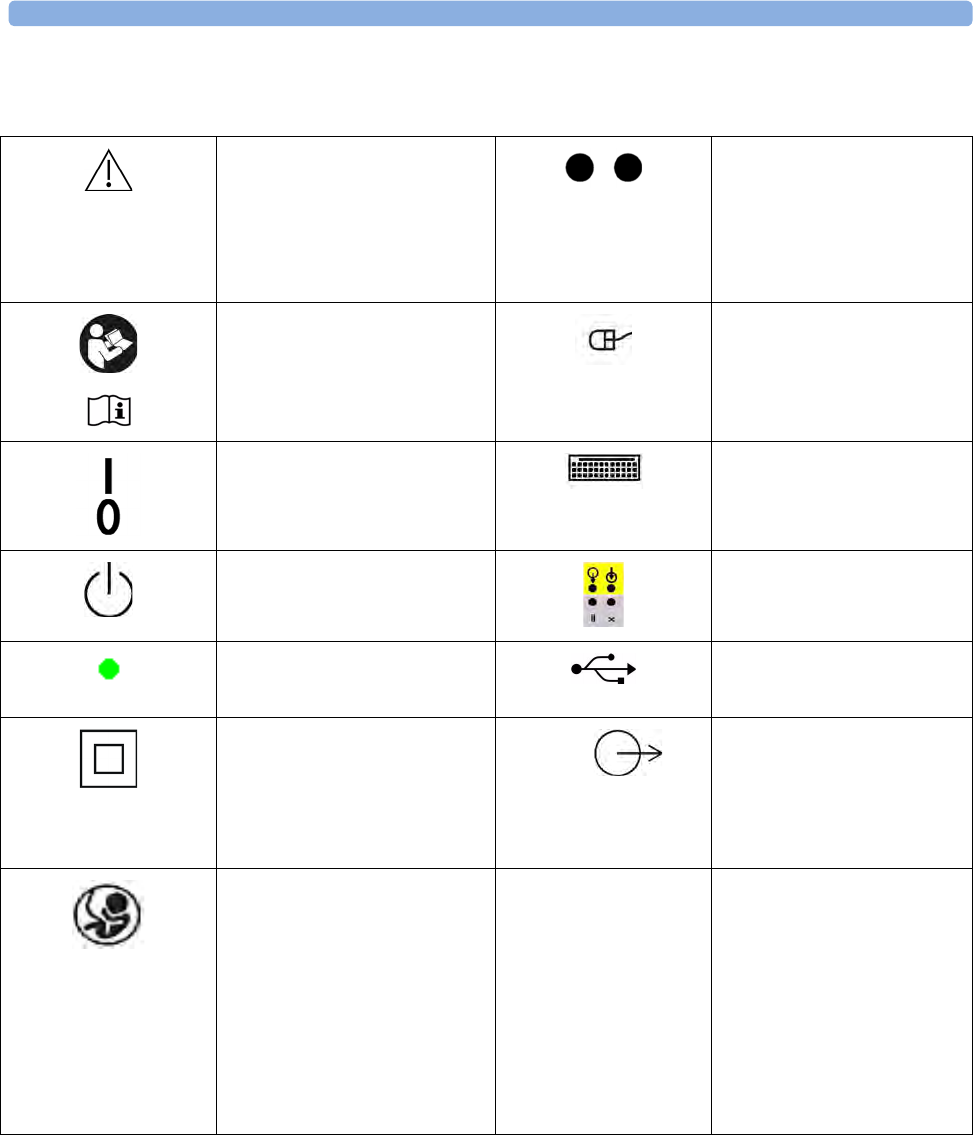
28 Specifications and Standards Compliance
298
Symbols on the System
This caution/warning symbol
indicates that you should
consult the Instructions for
Use (this document), and
particularly any warning
messages.
Connection direction
indicator
FM20/FM30 with battery
option
This symbol indicates that you
should consult the Instructions
for Use (this document).
Mouse connection indicator
(optional)
Power-On/Off Switch -
FM20/FM30 without Battery
Option
Keyboard connection
indicator
(optional)
Power-On/StandBy Switch -
FM40/FM50 and FM20/30
with Battery Option
Serial/MIB connector
(optional)
Power-On LED USB interface
(optional)
Electrical Class II equipment,
in which the protection against
electric shock relies on double
or reinforced insulation
(FM20/FM30).
Video
Analog interface indicator
for connection to any analog
video display (VGA
resolution)
FM40/FM50
Fetal Sensor Socket symbol. IP 67 Ingress Protection code
according to IEC 60529. The
IUP/ECG patient module
(M2738A) is rated IP 67
(protection against dust,
access to hazardous parts,
and the effects of continuous
immersion in water to a
depth of 0.5 meter for 30
minutes).
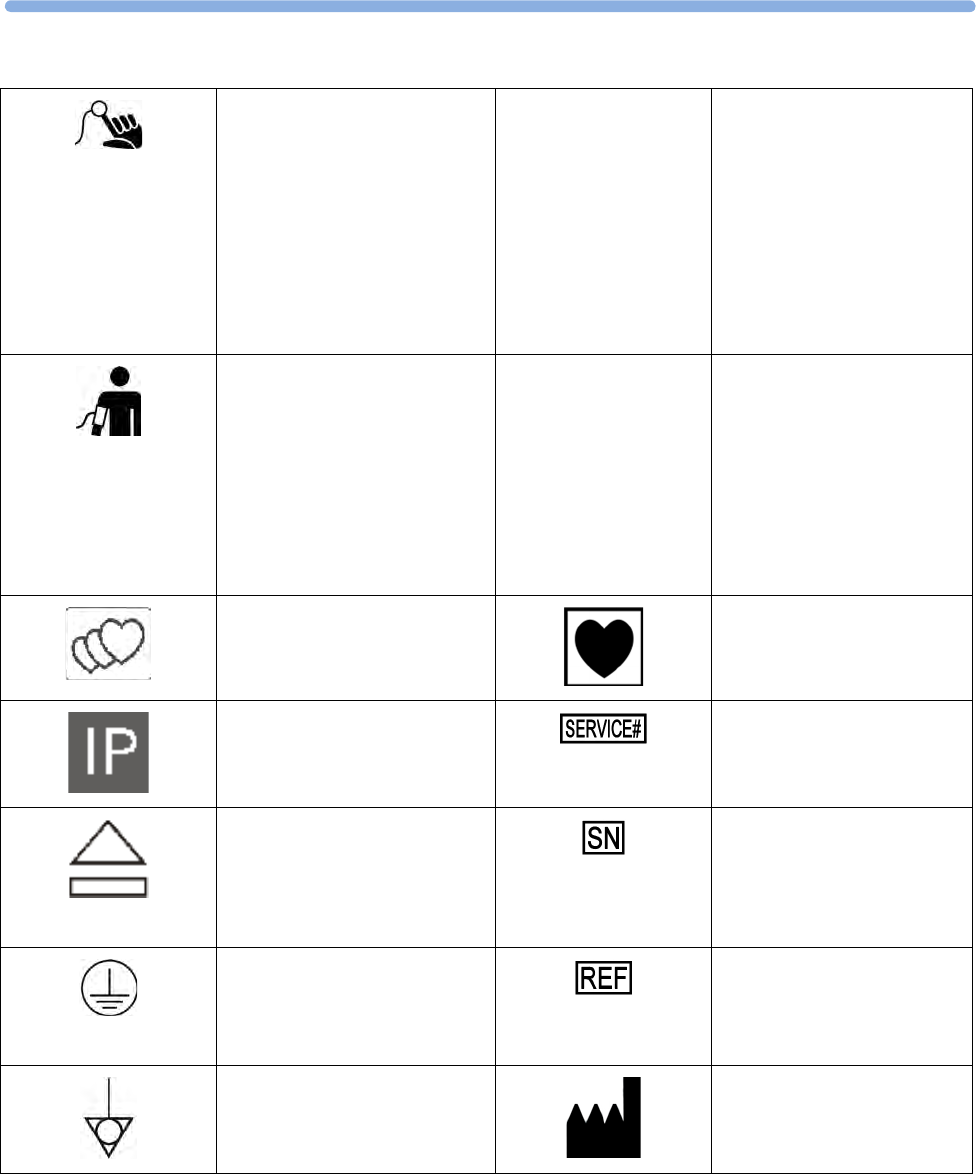
28
299
SpO2 Socket symbol. IP 68 Ingress Protection code
according to IEC 60529. All
transducers (excluding
M2738A) are rated IP 68
(protection against dust,
access to hazardous parts,
and the effects of continuous
immersion in water to a
depth of 1.0 meter for five
hours).
Noninvasive Blood Pressure
Socket symbol.
IP X1 Ingress Protection code
according to IEC 60529. The
monitors and interface cable
for the Avalon CTS
(M2731-60001/
M2732-60001) are rated
IP X1 (protection against
water dripping vertically
only).
Symbol indicating the monitor
has the triplets option.
Type CF equipment, not
defibrillation proof.
Symbol indicating the monitor
is capable of intrapartum
monitoring.
Indicates location of service
number
Button to open paper drawer/
paper eject. (FM40/FM50).
Indicates location of serial
number
Protective earth terminal
(FM40/FM50).
Indicates location of catalog
number
Equipotential grounding point
(FM40/FM50).
Indicates location of the date
of manufacture and/or name
and address of manufacturer
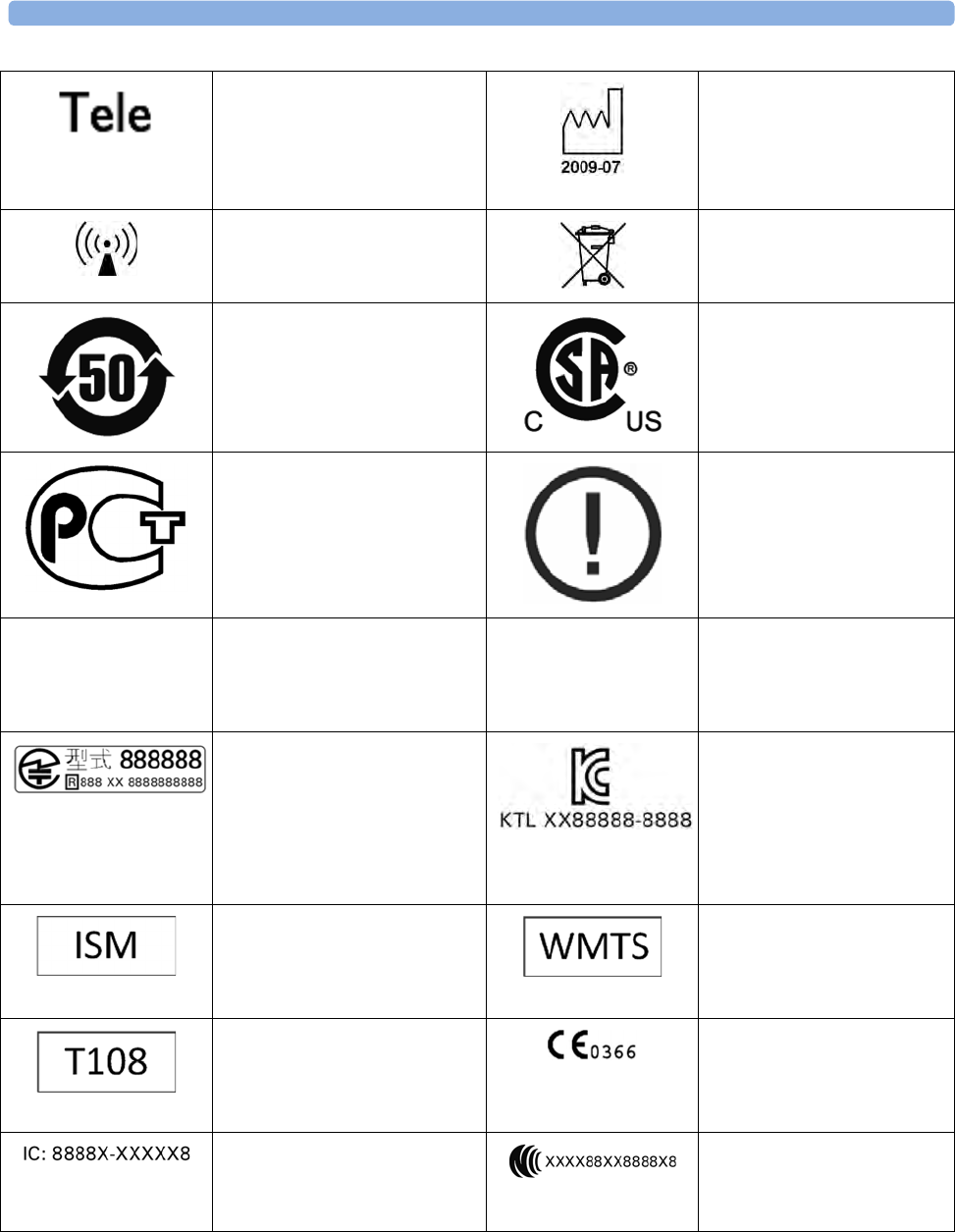
28 Specifications and Standards Compliance
300
Socket for connecting
Avalon CTS interface cable
M2732-60001 or Avalon CL
interface cable (with black
connector, FM40/FM50)
Identifies the year and
month of manufacture.
Symbol indication for non-
ionizing radiation.
Symbol indicating separate
collection for waste electrical
and electronic equipment.
China ROHS CSA US mark
GOST-R mark R&TTE Compliance
Association: "Class 2
Device" Mark
FCC ID Federal Communications
Commission: FCC ID xxxx
CMIIT ID Chinese Radio marking:
CMIIT ID (China Ministry
of Industry and Information
Technology)
Japanese Radio marking: Radio
mark + "PMS Japan" (in
Japanese) + Prod. No. + [R]-
symbol + ID
"Taiwan Radio Label" (NCC
Logo) + ID
Korea radio mark: KC logo,
KCC ID number, and
Conformity assessment
information
Industrial, Scientific, & Medical
radio frequency band (Avalon
CL frequency band used e.g. in
the EU)
Wireless Medical Telemetry
Service (Avalon CL
frequency band used e.g. in
North America)
Association Of Radio
Industries And Businesses
T108 (Avalon CL frequency
band used e.g. in Japan)
CE marking accompanied by
the VDE NB number 0366
IC-ID (Industry Canada ID)
One IC-ID labeling for each
built in radio: OBR, SRR
Taiwan Radio Label (NCC
Logo) + ID
29 Default Settings Appendix
301
29Default Settings Appendix
This appendix documents the most important default settings of your fetal monitor and the Avalon CL
Base Station with the cableless transducers as they are delivered from the factory. For a comprehensive
list and explanation of default settings see the Configuration Guide supplied with your fetal monitor.
The monitor's default settings can be permanently changed in Configuration Mode.
Alarm and Measurement Default Settings
Alarm Defaults Settings
Alarm Setting Choice Default
Alarm Mode INOP only, All INOP only
Alarm Volume 0..10 5
Alarms Off 1 min, 2 min, 3 min, Infinite 3 min
Alarm Text Standard/Enhanced Standard
Visual Latching Red&Yellow/Red/Off Off
Audible Latching Red Only/Off Off
Alarm Sounds Traditional/ISO Traditional
Alarm Low 0..10 4
Fetal / Maternal Defaults Settings
FHR (Ultrasound/DECG) Alarms On/Off Default On
Default Color for FHR Numeric Orange
Toco Default color for Toco numeric Green
IUP Default IUP Scale Unit mmHg
Default color for IUP numeric Green
Maternal Heart Rate HR
Measurement
Default Color for MECG Numeric Red
29 Default Settings Appendix
302
Coincidence Default Settings
NBP Default Settings
CL NBP Default Settings
Coincidence Default Settings
Coincidence Tone immediately
Factory Default Settings
Mode Manual
Repeat Time 15 min
Alarms from Sys.
Low Limit 90 / 50 (60)
High Limit 160 / 90 (110)
VP Pressure mmHg
Done Tone Off
Veni Puncture 60 mmHg
Start Time Synchronized
NBP On
Alarms On
Color Red
Reference Auscultatory
NBP Setting Factory Defaults
Mode Auto
Repeat Time 10 min
NBP On
VP Pressure 60 mmHg
Reference Auscultatory
Unit mmHg
Done Tone Off
Start Time Synchronized
Aging Time 10 min
Color Red
29 Default Settings Appendix
303
SpO2 Default Settings
CL SpO2 Default Settings
SpO2 Factory Default Settings
Desat Limit 80
Low Limit 90
Low Limit 100
High Limit 20 seconds
Desat Delay 10 seconds
Low Alarm Delay 10 seconds
High Alarm Delay 10 seconds
NBP Alarm Suppr. On
Alarms On
Color Cyan
Pulse Default Settings
Pulse (SpO₂)On
High Limit 120 bpm
Low Limit 50 bpm
Bradycardia: Difference to Low
Limit
20 bpm
Bradycardia: Clamp 40 bpm
Tachycardia: Difference to High
Limit
20 bpm
Tachycardia: Clamp 200 bpm
SpO2 Settings Factory Defaults
Repeat Time 15 min
Signal Quality On
NBP Alarm Suppr. On
Color
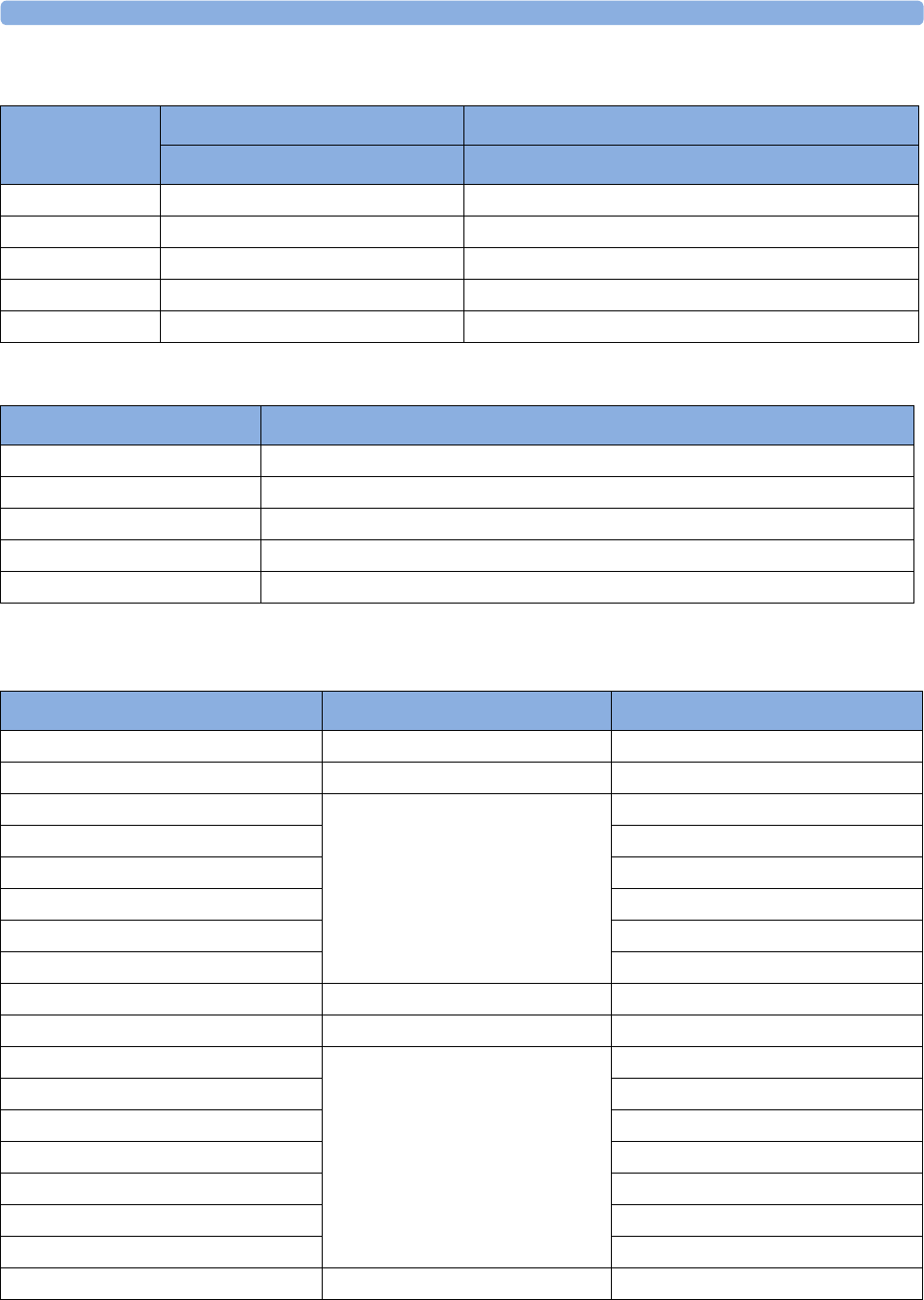
29 Default Settings Appendix
304
Tympanic Temperature Default Settings
Manually Entered Values Default Settings
Recorder Default Settings
pTemp Settings Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Adult
Low Limit 36°C (96.8°F)
High Limit 39°C (102.2°F)
Unit °C
Alarms On
Color Green
Manual Entered Values Default Settings
Label Temp
Unit ºC
Color white
Interval 1h
Msmt off
Setting Choice Default
Recorder Speed 1, 2, or 3 cm/min 3 cm/min
Scale Type US, Internat'l US
Trace Style FHR1 Thin, Medium, Thick, Extra Thick Thick
Trace Style FHR2 Medium
Trace Style FHR3 Extra Thick
Trace Style Toco Thick
Trace Style HR Thin
Wave Style ECG Thin
ECG Wave printing choice Separate, Overlap Separate
Notes Recording Along, Across Along
Auto Start Off, On Off
Confirmed Stop Off
Bridge Paperout On
Paper Save Mode Off
NST Autostart On
NST Autostop Off
Trace Separation Off
Separation Order Standard, Classic Standard
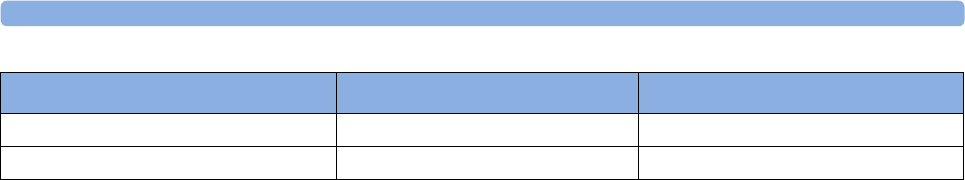
29 Default Settings Appendix
305
Intensity 4 (medium) n/a
Cal. Offset 5 n/a
Setting Choice Default

29 Default Settings Appendix
306
317
1Index
A
accessories 267, 268, 270, 271, 272, 273, 277
cl NBP pod accessories 272
cl SpO2 pod accessories 276
fetal accessories 268
fetal recorder accessories 277
latex information 267
MECG accessories 270
noninvasive blood pressure
accessories 270, 271, 272
adult cuffs 272
multi-patient comfort cuff kits 271
reusable cuffs 271
single-hose disposable cuffs 272
SpO2 accessories 273
Philips sensors (disposable) 273
Philips sensors (reusable) 273
transducer accessories 268
ACOG technical bulletin 80
actions after monitoring 98
active alarms 109
adjusting brightness 66
adjusting display 68
adjusting screen brightness 66
admitting a patient 137, 138
editing information 138
aging numerics 213
alarms 109, 110, 111, 113, 114, 115, 116, 117,
118, 120, 121, 123, 191, 216, 230, 285, 289,
290, 311
acknowledging alarms 114
active alarms 109
alarm behavior at on/off 121
alarm latching 119
alarm limit delay 285
alarm reminder 114
alarm standards 111
audible alarm indicators 111
yellow alarms 109
artifact suppression 208
artifact suppression and fetal
arrhythmia 208
explanation of artifact suppression 208
switching on and off artifact
suppression 208
automatic noninvasive blood pressure
repeat time 215
B
baseline measurement 177, 184, 194
Battery Option 101
using batteries 101
belt actions 70, 72
belt fastening 70
belt fixing button 70
C
Cableless Monitoring 91
Avalon CL 40
configuration cableless system 92
important considerations 159
LED indication 53
TELE window 93
Telemetry 94
Underwater monitoring 97
calibration 216, 260
calibrating noninvasive blood
pressure 260
cautions 9
changing FHR alarm delays 191
changing FHR alarm limits 191
cleaning monitor actions 255, 256, 257, 265
cleaning method 256
cleaning monitoring accessories 257
general cleaning requirements 255
infection control 255
printhead cleaning 265
configuration mode 63
configuring alarm tone 111
confirming fetal life 10, 158, 175, 183
connecting power 12
cross-channel verification 10, 175, 183, 234
CCV and triplets 183
CCV and twins 175
D
data recovery 251
date from OB TraceVue 66
date setting 66
DECG 205, 209, 285
DECG INOPs 209
DECG specifications 285
DECG testing 209
DECG troubleshooting 209
default alarm settings 311
default IUP settings 285
default settings 285
FHR default settings 285
IUP default settings 285
MECG default settings 285
Toco default settings 285
user defaults 65
defibrillation precautions 238, 267, 307
demo mode 63
disabling touchscreen 63
discharging a patient 138
disinfecting 255, 256, 257
infection control 255
recommended substances 257
display 68, 213, 285
adjusting display 68
display noninvasive blood pressure 213
fetal display specifications 285
disposal of electronic waste 266
disposal of monitor 266
dyshemoglobins 228
intravascular dyshemoglobins 228
E
early systolic blood pressure 213
ECG 205, 235, 285
ECG specifications 285
electrical safety tests 298
electrical surgery precautions. See ESU 228,
238, 267, 307
electrodes 237
applying electrodes 237
EMC 298
electromagnetic compatibility 298
electromagnetic emissions 301
electromagnetic interference 300
how to reduce electromagnetic
interference 300
EMC and compliant accessories 298
EMC precautions 298
EMC standards 298
entering notes 61
ESU precautions 238, 267, 307
event marker remote 80
extension cable for SpO2 228
external monitoring 157, 176, 184, 194
external monitoring - Toco 194
external monitoring - triplets 184
external monitoring - twins 176
external monitoring - ultrasound 157
318
F
factory defaults 289, 290, 294
noninvasive blood pressure factory
defaults 289
recorder factory defaults 294
SpO2 factory defaults 290
FAST 227
Fourier Artifact Suppression
Technology 227
fetal accessories 268
fetal arrhythmia 208
fetal demise 10
fetal display specifications 285
IUP - fetal display specifications 285
Toco - fetal display specifications 285
US - fetal display specifications 285
fetal heart rate alerting. See FHR 191
fetal heart rate. See FHR 157
fetal movement 163
fetal movement profile. See FMP 157
FHR 10, 158, 165, 175, 177, 183, 184, 191, 192,
234, 285
alerting 191
cross-channel verification 234
misidentification 10
trace separation 177, 184
FHR alarms 285
finder LED 45, 73, 175, 183
finding monitor revision 67
flexible nurse call 30, 42, 44
FMP 163, 164
FMP and twins 163
FMP statistics 163
functional arterial oxygen saturation 227
G
global settings 65
H
high priority alarms 109
I
infection control 255
infection and sterilizing 255
INOPs 109, 114
CCV INOP 33
coincidence tone 30
disconnect INOPs 114
INOP alarms 109
INOPs indicators 109
silencing INOPs 114
interference 298, 300
how to reduce interference 300
interference from RF equipment 298
internal monitoring 177, 199, 201
intrauterine pressure. See IUP 197
intravascular dyshemoglobins 228
intravascular dyshemoglobins effects on
(SpO2) 228
ISO/IEC standard 9703-2 111
IUP 197, 199, 285
IUP specifications 285
L
latching alarms 118, 119
latching alarm behavior 119
M
mains power (AC) 12, 99
connecting to mains power 12
disconnecting from mains power 99
maintenance 259, 260
maintenance schedule 259, 260
visual inspection 259
maternal ECG 208, 238, 240
electrode position 238
printing waveform 208, 240
viewing waveforms 238
maternal heart rate 233, 234, 235
maternal heart rate and cross-channel
verification 234
maternal heart rate and priorities 233
maternal heart rate from MECG 235
sources of maternal heart rate 233
maternal puls from Toco 32
Maternal Temperature 30
measurement settings 65
changing measurement settings 65
entering setup menu 65
measurements 64, 65, 285
setting up measurements 65
switching on and off measurements 64
MECG 208, 235, 237, 238, 240, 242, 243, 270,
285
accessories 270
alarm limits 285
connection illustration 235
default settings 285
electrodes 237
specifications 285
waveform printing 208, 240
MECG alarm limits 285
methemoglobin (SpO2) 228
MHR 158, 233, 235, 237
MHR from MECG 235
MHR priorities 233
MHR sources 233
monitor settings 10, 40, 66, 68, 98, 251
changing monitor settings 66
major parts and keys 40
power on/off behavior 99
Standby 98
switching on 68
monitoring mode 63
monitoring triplets and FHR 183
monitoring twins and FHR 175
MR imaging and the SpO2 transducer 228
MRI precautions 238, 267, 307
N
NBP. See noninvasive blood pressure 211
NIBP. See noninvasive blood pressure 211
Noninvasive Blood Pressure (NBP) 211,
212, 213, 214, 215, 216, 217, 242, 260, 270,
271, 272, 289
calibration interval 260
comfort cuff kits 271
factory defaults 289
how the measurement works 211
measurement 212, 214
limitations 212
methods 212
starting 214
stopping 214
NBP accessories 270
NBP adult cuffs 272
NBP automatic mode 215
NBP numerics 213
NBP pediatric cuffs 272
NBP performance specifications 289
NBP reusable cuffs 271
NBP single-hose disposable cuffs 272
NBP site inspection 212
NBP troubleshooting 217
NBP venous puncture 216
preparing to measure NBP 212
non-medical devices 298
non-medical devices in patient
vicinity 298
Non-Stress Test timer. See NST timer 143
NST Report
NST analysis 32
Trace Interpretation 145, 148
NST timer 141, 142, 143
O
OB TraceVue 38, 39, 252
connection to OB TraceVue 38, 39
LAN connection 252
operating modes 63
configuration mode 63
demo mode 63
monitoring mode 63
service mode 63
operating temperatures 306
319
oscillometric measurement method 211
P
Paging Patient 97
paper 80, 81, 82, 83, 85, 264, 277
default paper speed 80
loading paper 83, 85
paper out INOP 82
paper speed 80
changing 80
default 80
defaults 80
setting 80
paper, when to reload 82
recorder paper 277
removing paper 83, 85
storing paper 264
tearing off a trace 81
Paper Advance key 61
Paper-Out indication 82
passcode protection 63
patient alarms 123
Patient Demographics window 137
patient module 205, 235
paused alarms 115, 116
restarting paused alarms 116
pausing alarms 115
performance specifications 285, 289, 290
noninvasive blood pressure
specifications 289
SpO2 specifications 290
physiological alarms 109
pop-up keys 95
power 12, 99
connecting power 12
disconnecting from 99
power connection 12
power failure 99
pulse 242
pulse from noninvasive blood
pressure 242
pulse rate 233
R
recorder 76, 100, 264, 265, 277, 294
factory defaults 294
paper storage 264
printhead cleaning 265
recorder paper 277
recorder specifications 294
recorder speed 33
recorder troubleshooting 100
Recorder Elements 79
recording stored data 61
recovering traces 251
trace recovery printout 251
recycling 266
red alarms 109
regulatory compliance 297
remote event marker 80
restarting paused alarms 116
reviewing alarms 118
reviewing alarms window 118
S
safety 260, 297
maintenance interval 260
safety standards 297
screen layouts 64
selftest 68, 76, 120
sensor 227
disposable SpO2 sensors 227
selecting SpO2 sensors 227
separating FHR traces 177, 184
separating triplet traces 184
separating twin traces 177
service mode 63
settings 64, 65, 66
active settings 64
changing settings 66
global settings 65
monitor settings 66
user default settings 65
signal loss delay 192
signal quality 90, 230
signal quality during monitoring 90
signal quality of SpO2 230
silencing alarms 114
specifications 279, 281, 285, 294
built-in recorder specifications 294
DECG specifications 285
ECG specifications 285
environmental specifications 279
monitor 279
SpO2 sensors 279
transducers 279
IUP specifications 285
measurement specifications 285
MECG specifications 285
performance specifications 285
Toco specifications 285
transducer specifications 281
US specifications 285
SpO2 227, 228, 230, 273, 290
accessories 273
alarm specifications 290
connecting the cables 228
disposable sensors 227
factory defaults 290
FAST technology 227
performance specifications 290
Philips sensors (disposable) 273
Philips sensors (reusable) 273
signal quality 230
SpO2 alarms 230, 290
standards 297, 298
EMC standards 298
safety standards 297
standards compliance 297
Standby 61
sterilizing 255, 258
infection control 255
storage temperatures 306
stored data recording 61
suppressing artifacts 208
suspended alarm 116
suspicious SpO2 reading 230
switching on and off 164
switching on and off alarms 116
switching on monitor 68
switching on recorder 76
symbols on the system 308
T
technical alarm messages. See INOPs 126
temperatures 306
operating temperatures 306
storage temperatures 306
testing 120, 209, 242, 298
DECG testing 209
MECG testing 242
safety testing 298
testing alarms 120
time 66
setting time 66
time from OB TraceVue 66
Toco 193, 194, 195, 205, 237, 285
default Toco settings 285
testing a Toco transducer 195
Toco baseline 194
Toco display specifications 285
Toco monitoring 193
Toco sensitivity 195
Toco specifications 285
Toco MP transducer 193, 233
Toco+ transducer 193
touch tone volume 66
touchscreen operation 56, 63
trace actions 81, 251, 252
separation on/off 33
tearing off traces 81
trace recovery on OB TraceVue 252
trace recovery on paper 251
transducer 45, 70, 73, 173, 175, 183, 193, 195,

320
281
connecting transducer to monitor 73
fixing transducer to belt 70
repositioning transducers 73
Toco transducer 193
Toco+ transducer 193
transducer belt clip 70
transducer specifications 281
transducer testing 173, 195
Toco 195
ultrasound 173
triplets 183, 184, 185, 188
cross-channel verification 183
external monitoring 184
importance of monitoring MHR 183
monitoring triplets 183
offsetting baselines 184
troubleshooting 100, 165, 181, 188, 195, 199,
209, 217, 240
DECG 209
FHR 165
IUP 199
MECG 240
troubleshooting FHR 165
twins 163, 175, 176, 177, 178, 179, 181
cross-channel verification 175
external monitoring 176
importance of monitoring MHR 175
invasive monitoring 177
monitoring FHR 175
monitoring twins 175
offsetting baselines 177
twins and FMP 163
U
ultrasound 157, 160, 173, 285
applying gel 160
testing a transducer 173
ultrasound display specifications 285
ultrasound monitoring 157
ultrasound specifications 285
understanding screens 64
USB 30
using the adapter cable 205
uterine activity 193, 194, 195, 197, 199, 205,
237
external monitoring 193
internal monitoring 197
monitoring uterine activity 194, 197, 199,
205, 237
troubleshooting uterine activity 195, 199
V
velcro belt 72
venous puncture 216
visual alarm indicators 110
voltage setting 12
volume 66, 113
alarm volume 113
IUP, zeroing 199
touch tone volume 66
warnings 9

Part Number xxxxxxxxxxx
Printed in Germany 06/13
*453564405521*