Provider Bulletin April 2019
File info: application/pdf · 3 pages · 261.56KB
Provider Bulletin April 2019
Provider, Bulletin, April, 2019
All-Cause Readmission and Potentially Preventable ...
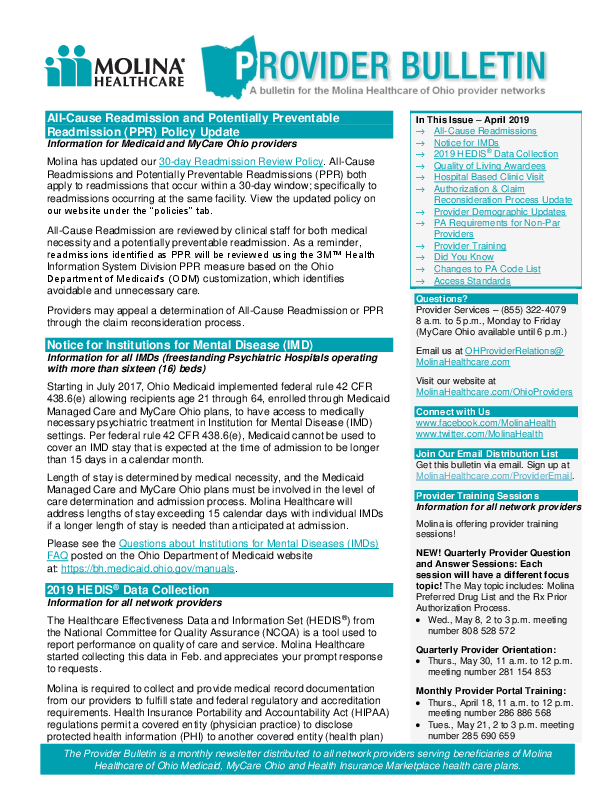
The Provider Bulletin is a monthly newsletter distributed to all network providers serving beneficiaries of Molina Healthcare of Ohio Medicaid, MyCare Ohio and Health Insurance Marketplace health care plans.
Extracted Text
All-Cause Readmission and Potentially Preventable Readmission (PPR) Policy Update Information for Medicaid and MyCare Ohio providers Molina has updated our 30-day Readmission Review Policy. All-Cause Readmissions and Potentially Preventable Readmissions (PPR) both apply to readmissions that occur within a 30-day window; specifically to readmissions occurring at the same facility. View the updated policy on our website under the "policies" tab. All-Cause Readmission are reviewed by clinical staff for both medical necessity and a potentially preventable readmission. As a reminder, readmissions identified as PPR will be reviewed using the 3MTM Health Information System Division PPR measure based on the Ohio Department of Medicaid's (ODM) customization, which identifies avoidable and unnecessary care. Providers may appeal a determination of All-Cause Readmission or PPR through the claim reconsideration process. Notice for Institutions for Mental Disease (IMD) Information for all IMDs (freestanding Psychiatric Hospitals operating with more than sixteen (16) beds) Starting in July 2017, Ohio Medicaid implemented federal rule 42 CFR 438.6(e) allowing recipients age 21 through 64, enrolled through Medicaid Managed Care and MyCare Ohio plans, to have access to medically necessary psychiatric treatment in Institution for Mental Disease (IMD) settings. Per federal rule 42 CFR 438.6(e), Medicaid cannot be used to cover an IMD stay that is expected at the time of admission to be longer than 15 days in a calendar month. Length of stay is determined by medical necessity, and the Medicaid Managed Care and MyCare Ohio plans must be involved in the level of care determination and admission process. Molina Healthcare will address lengths of stay exceeding 15 calendar days with individual IMDs if a longer length of stay is needed than anticipated at admission. Please see the Questions about Institutions for Mental Diseases (IMDs) FAQ posted on the Ohio Department of Medicaid website at: https://bh.medicaid.ohio.gov/manuals. 2019 HEDIS� Data Collection Information for all network providers The Healthcare Effectiveness Data and Information Set (HEDIS�) from the National Committee for Quality Assurance (NCQA) is a tool used to report performance on quality of care and service. Molina Healthcare started collecting this data in Feb. and appreciates your prompt response to requests. In This Issue � April 2019 All-Cause Readmissions Notice for IMDs 2019 HEDIS� Data Collection Quality of Living Awardees Hospital Based Clinic Visit Authorization & Claim Reconsideration Process Update Provider Demographic Updates PA Requirements for Non-Par Providers Provider Training Did You Know Changes to PA Code List Access Standards Questions? Provider Services � (855) 322-4079 8 a.m. to 5 p.m., Monday to Friday (MyCare Ohio available until 6 p.m.) Email us at OHProviderRelations@ MolinaHealthcare.com Visit our website at MolinaHealthcare.com/OhioProviders Connect with Us www.facebook.com/MolinaHealth www.twitter.com/MolinaHealth Join Our Email Distribution List Get this bulletin via email. Sign up at MolinaHealthcare.com/ProviderEmail. Provider Training Sessions Information for all network providers Molina is offering provider training sessions! NEW! Quarterly Provider Question and Answer Sessions: Each session will have a different focus topic! The May topic includes: Molina Preferred Drug List and the Rx Prior Authorization Process. Wed., May 8, 2 to 3 p.m. meeting number 808 528 572 Quarterly Provider Orientation: Thurs., May 30, 11 a.m. to 12 p.m. meeting number 281 154 853 Molina is required to collect and provide medical record documentation from our providers to fulfill state and federal regulatory and accreditation requirements. Health Insurance Portability and Accountability Act (HIPAA) regulations permit a covered entity (physician practice) to disclose protected health information (PHI) to another covered entity (health plan) Monthly Provider Portal Training: Thurs., April 18, 11 a.m. to 12 p.m. meeting number 286 886 568 Tues., May 21, 2 to 3 p.m. meeting number 285 690 659 The Provider Bulletin is a monthly newsletter distributed to all network providers serving beneficiaries of Molina Healthcare of Ohio Medicaid, MyCare Ohio and Health Insurance Marketplace health care plans. PROVIDER BULLETIN MOLINA HEALTHCARE OF OHIO without enrollees' consent for the purpose of facilitating health care operations. Molina will reach out to providers via phone and fax with collection instructions and a corresponding member list. The following options are available for record submission: Fax, mail or secure email An onsite visit by Molina; based on the volume of records Providers may allow Molina access to their Electronic Health Records (EHR) for quick access to records pertaining to the specific HEDIS� project. o For EHR setup email RegionB_EMRSupport@MolinaHealthCare.com Thank you for your continued collaboration. Molina Quality Living Program Awardees Information for all network providers Molina is proud to announce the most recent quarter's performance for nursing facilities in the Molina Quality Living Program. Gold Level Mason Health Care Center Pinnacle Point Nursing Rehab Silver Level Bethany Village Country View of Sunbury Crown Pointe Care Center Diversicare of Bradford Place Eastland Health Care & Rehabilitation Center Judson Care Center Masonic Health Care Mother Angelina McCrory Manor Mt Healthy Christian Village Mt Washington Care Center Quaker Heights Care Community Tri County Extended Care Center About the Molina Quality Living Program: This program recognizes and awards nursing facility partners that meet or exceed select Centers for Medicare and Medicaid Services (CMS) quality measures when providing care to Molina MyCare Ohio members in custodial care. Hospital-Based Clinic Visit Facility Fees Information for providers in the Marketplace network Effective April 1, 2019, Molina will not separately reimburse a clinic fee or any other facility fee associated with space used to provide Evaluation and Management (E&M) services in the event they are billed on a UB-04 claim form (`facility fee'), regardless of the office location and/or uses the hospital tax identification number for the Molina Marketplace product. The following are conditions under which claims will be denied: Type of Bill: 13X Revenue Code: 51X E&M Procedure Codes: 99201-99205, 99211-99215 or G0463 Review the Molina Hospital-Based Clinic Visits Payment Policy on our Marketplace website, under the "Policies" tab. APRIL 2019 Monthly Claim Submission Training: Thurs., April 11, 2 to 3 p.m. meeting number 801 480 015 Thurs., May 16, 1 to 2 p.m. meeting number 282 775 074 To join WebEx, call (866) 499-0396 and follow the instructions. To view sessions, log into WebEx.com, click on "Join" and follow the instructions. Did You Know? Molina offers a variety of electronic and mobile resources to give our members 24-hour access to their health plan. Some of the electronic resources Molina offers include: My Molina: Online member portal used to request a new ID card, print a temporary ID card, find or change Primary Care Providers (PCPs) and pharmacies, view health records, benefits and eligibility. o Marketplace members can use this option to pay their premiums. Molina HealthInHand App: IOS and Android App that is used to access the member portal and has the ability to call the Nurse Advice Line, schedule transportation, contact Member Services or other support services. o Prenatal Care Card: Part of HealthInHand App for pregnant or new moms that provides members with weekly education during pregnancy, prenatal and post-partum list of to do care and notification reminders. Teladoc: Members can visit with a certified health care provider and be treated for backaches, sinus problems, asthma, skin conditions, respiratory infections, colds, flus and more. Members are able to get short-term prescriptions. o Go to Teladoc.com/Molina-oh o Call (800) 835-2362 24-Hour Nurse Advice Line: Access to a registered nurse who can advise on where to go for care, make recommendations for home care and answer questions about pregnancy, child care, prescriptions, injuries and more. Members can find out if they need urgent or emergency care and locate a doctor by calling (888) 275-8750. WWW.MOLINAHEALTHCARE.COM 2 (855) 322-4079 PROVIDER BULLETIN MOLINA HEALTHCARE OF OHIO Authorization and Claim Reconsideration Process Updates Information for all network providers Effective Jan. 1, 2019, Molina updated the Authorization and Claim Reconsideration processes. Please review these updates in the Authorization and Claim Reconsideration Guides available on our website, under the "Forms" tab on the Marketplace website, and under the "Manual" tab on all other lines of business. These guides are specific to each line of business. Please confirm the line of business the member is eligible under and reference the correct guide for the reconsideration process and appeal rights. Provider Demographic Update on Provider Portal Information for all network providers Molina has updated the Provider Portal to include a feature enabling providers to report demographic information data corrections. Submissions are limited to one update per provider at a time. To update provider information select "Account Tools" on the Provider Portal at https://Provider.MolinaHealthcare.com and under "View/Update Profile" click "Report data change in the Provider Directory: Submit Here." Behavioral Health (BH) provider types 84 and 95 for Community Mental Health Center (CMHC) and Substance Use Disorder (SUD) agencies will still need to send Molina updates via the CMHC-SUD BH Rendering Provider Template. This universal roster is used to report information about the organization, as well as practitioners rendering services on behalf of the organization. Email BHProviderServices@MolinaHealthcare.com to request a copy of the template. Prior Authorization Requirements for Non-Par Providers Information for non-par providers in all networks As a reminder, if a provider is non-par for a line of business, all nonemergent services rendered by non-contracted providers require prior authorization (PA), unless otherwise specified. For additional questions, please view the "Non-Contracted Provider Billing Guidelines" or the "Molina Healthcare Prior Authorization Request Form and Instructions" available at MolinaHealthcare.com/OhioProviders. APRIL 2019 Notice of Changes to Prior Authorization (PA) Requirements Molina posts new comprehensive PA Code Lists to our website quarterly. However; changes can be made to the lists between quarterly comprehensive updates. Always use the lists posted to our website under the "Forms" tab instead of printing hard copies. This practice ensures you are accessing the most up-to-date versions of Molina's PA requirements. Access Standards Information for all network providers Find Molina's appointment availability standards in our Provider Manual, available on our website. Based on industry and National Committee for Quality Assurance (NCQA) guidelines, our standards are approved by our Quality Improvement Committee. We conduct an annual survey to measure compliance and perform targeted education and corrective action plans with providers that do not meet standards. Fighting Fraud, Waste & Abuse Do you have suspicions of member or provider fraud? The Molina Healthcare AlertLine is available 24 hours a day, 7 days a week, even on holidays at (866) 606-3889. Reports are confidential, but you may choose to report anonymously. WWW.MOLINAHEALTHCARE.COM 3 (855) 322-4079