Philips Medical Systems North America SRRBV1 Dual SRR Module User Manual ait fm manual en 2011 03 24
Philips Medical Systems North America Co. Dual SRR Module ait fm manual en 2011 03 24
Contents
User Manual

Instructions for Use
IntelliVue Patient Monitor
MX600/MX700/MX800
Release H.0 with Software Revision H.1x.xx
Patient Monitoring

Part Number 453564260091
Printed in Germany 05/11
*453564260091*
3
1Table of Contents
1Introduction 13
Introducing the Monitor 13
Devices for Acquiring Measurements 15
Operating and Navigating 24
Operating Modes 31
Understanding Screens 32
Connecting Additional Displays to the Monitor 33
Using the XDS Remote Display 34
Using the Visitor Screen 34
Understanding Profiles 34
Understanding Settings 36
Changing Wave Speeds 37
Freezing Waves 38
Using Labels 39
Entering Measurements Manually 42
Changing Monitor Settings 42
Checking Your Monitor Revision 43
Getting Started 43
Disconnecting from Power 45
Networked Monitoring 45
Using the Integrated PC 46
Using the X2 or MP5 with a Host Monitor 47
2Alarms 49
Visual Alarm Indicators 50
Audible Alarm Indicators 51
Acknowledging Alarms 53
Pausing or Switching Off Alarms 54
Alarm Limits 56
Reviewing Alarms 60
Latching Alarms 61
Testing Alarms 62
Alarm Behavior at Power On 62
Alarm Recordings 63
3Patient Alarms and INOPs 65
Patient Alarm Messages 65
Technical Alarm Messages (INOPs) 70
4
4Managing Patients 95
Admitting a Patient 95
Quick Admitting a Patient 96
Editing Patient Information 97
Discharging a Patient 97
Transferring Patients 98
Data Upload from an MMS 102
Care Groups 105
5ECG, Arrhythmia, ST and QT Monitoring 111
Skin Preparation for Electrode Placement 111
Connecting ECG Cables 111
Selecting the Primary and Secondary ECG Leads 112
Checking Paced Status 112
Understanding the ECG Display 112
Monitoring Paced Patients 113
Changing the Size of the ECG Wave 114
Changing the Volume of the QRS Tone 115
Changing the ECG Filter Settings 115
Selecting Positions of Va and Vb Chest Leads (for 6-lead placement) 116
Choosing EASI or Standard Lead Placement 116
About ECG Leads 116
ECG Lead Fallback 117
ECG Lead Placements 117
Capture 12-Lead 123
EASI ECG Lead Placement 125
ECG and Arrhythmia Alarm Overview 126
Using ECG Alarms 127
ECG Safety Information 128
About Arrhythmia Monitoring 129
Switching Arrhythmia Analysis On and Off 130
Choosing an ECG Lead for Arrhythmia Monitoring 130
Understanding the Arrhythmia Display 132
Arrhythmia Relearning 134
Arrhythmia Alarms 135
About ST Monitoring 139
Switching ST On and Off 140
Understanding the ST Display 141
Updating ST Baseline Snippets 142
Recording ST Segments 142
About the ST Measurement Points 143
ST Alarms 145
Viewing ST Maps 146
About QT/QTc Interval Monitoring 149
QT Alarms 152
Switching QT Monitoring On and Off 153

5
6Monitoring Pulse Rate 155
Entering the Setup Pulse Menu 155
System Pulse Source 155
Switching Pulse On and Off 156
Using Pulse Alarms 156
7Monitoring Respiration Rate (Resp) 159
Lead Placement for Monitoring Resp 159
Understanding the Resp Display 160
Changing Resp Detection Modes 160
Changing the Size of the Respiration Wave 161
Changing the Speed of the Respiration Wave 162
Using Resp Alarms 162
Changing the Apnea Alarm Delay 162
Resp Safety Information 162
8Monitoring SpO2 165
SpO2 Sensors 165
Applying the Sensor 165
Connecting SpO2 Cables 166
Measuring SpO2 166
SpO2 Signal Quality Indicator (Fast SpO2 only) 167
Assessing a Suspicious SpO2 Reading 168
Changing the Averaging Time 168
Understanding SpO2 Alarms 168
Pleth Wave 171
Perfusion Numeric 171
Perfusion Change Indicator 171
Setting SpO2/Pleth as Pulse Source 172
Setting Up Tone Modulation 172
Setting the QRS Volume 172
Calculating SpO2 Difference 172
9Monitoring NBP 173
Introducing the Oscillometric NBP Measurement 173
Preparing to Measure NBP 175
Starting and Stopping Measurements 176
Enabling Automatic Mode and Setting Repetition Time 178
Enabling Sequence Mode and Setting Up The Sequence 178
Choosing the NBP Alarm Source 178
Switching Pulse from NBP On/Off 179
Assisting Venous Puncture 179
Calibrating NBP 179
10 Monitoring Temperature 181
Making a Temp Measurement 181
6
Calculating Temp Difference 182
11 Monitoring Invasive Pressure 183
Setting up the Pressure Measurement 183
Zeroing the Pressure Transducer 184
Adjusting the Calibration Factor 186
Displaying a Mean Pressure Value Only 187
Changing the Pressure Wave Scale 187
Optimizing the Waveform 187
Using the Wave Cursor 187
Non-Physiological Artifact Suppression 188
Choosing the Pressure Alarm Source 188
Calibrating Reusable Transducer CPJ840J6 189
Calculating Cerebral Perfusion Pressure 191
Calculating Pulse Pressure Variation 191
Measuring Pulmonary Artery Wedge Pressure 192
Editing the Wedge 193
Identifying the Pressure Analog Output Connector 193
12 Monitoring Cardiac Output 195
Hemodynamic Parameters 195
Using the C.O. Procedure Window 196
Accessing the Setup C.O. and Setup CCO Menus 197
Entering the HemoCalc Window 198
Measuring C. O. Using the PiCCO Method 198
Measuring C.O. Using the Right Heart Thermodilution Method 203
Documenting C.O. Measurements 206
C.O. Injectate Guidelines 206
C.O./CCO Curve Alert Messages 207
C.O./CCO Prompt Messages 209
C.O./CCO Warning Messages 209
C.O./CCO Safety Information 210
13 Monitoring Carbon Dioxide 213
Measurement Principles 214
Measuring CO2 using M3014A or X2 214
Measuring Mainstream CO2 using M3016A 218
Measuring Microstream CO2 using M3015A/B 220
Setting up all CO2 Measurements 222
14 Monitoring Airway Flow, Volume and Pressure 225
Attaching the Flow Sensor 226
Zero Calibration 228
Automatic Purging 228
Manual Purging 229
Gas Compensation 229
7
Setting up Spirometry 230
15 Monitoring tcGas 233
Identifying tcGas Module Components 233
Setting the tcGas Sensor Temperature 233
Using the tcGas Site Timer 234
Setting the tcGas Barometric Pressure 235
Remembraning the tcGas Transducer 235
Calibrating the tcGas Transducer 235
Applying the tcGas Transducer 237
Finishing tcGas Monitoring 238
TcGas Corrections 238
16 Monitoring Intravascular Oxygen Saturation 241
Selecting a Measurement Label 242
Preparing to Monitor with the M1021A Wide Module 242
Preparing to Monitor with the M1011A Narrow Module 246
Further Information for Both Modules 247
17 Monitoring EEG 249
EEG Monitoring Setup 249
Using the EEG Impedance/Montage Window 250
About Compressed Spectral Arrays (CSA) 252
Changing EEG Settings 253
EEG Reports 254
EEG Safety Information 254
EEG and Electrical Interference 255
18 Monitoring BIS 257
BIS Monitoring Setup 257
BIS Continuous Impedance Check 259
BIS Cyclic Impedance Check 260
BIS Window 260
Changing the BIS Smoothing Rate 261
Switching BIS and Individual Numerics On and Off 262
Changing the Scale of the EEG Wave 262
Switching BIS Filters On or Off 262
BIS Safety Information 262
19 Assigning a Telemetry Device and a Monitor to One Patient 265
How Can You Combine Devices? 265
Functions Available When the Telemetry Data Window is Displayed 267
General Telemetry-related Functions 268
Use Models With Telemetry 269
8
20 Trends 271
Viewing Trends 271
Setting Up Trends 274
Documenting Trends 278
Trends Databases 278
Screen Trends 279
21 Calculations 283
Viewing Calculations 284
Reviewing Calculations 285
Performing Calculations 285
Entering Values for Calculations 286
Documenting Calculations 287
22 High Resolution Trend Waves 289
Changing the Hi-Res Trend Waves Displayed 289
Hi-Res Trend Wave Scales 289
Hi-Res Trend Waves and OxyCRG 289
Printing Hi-Res Trend Wave Reports 290
Hi-Res Trend Wave Recordings 290
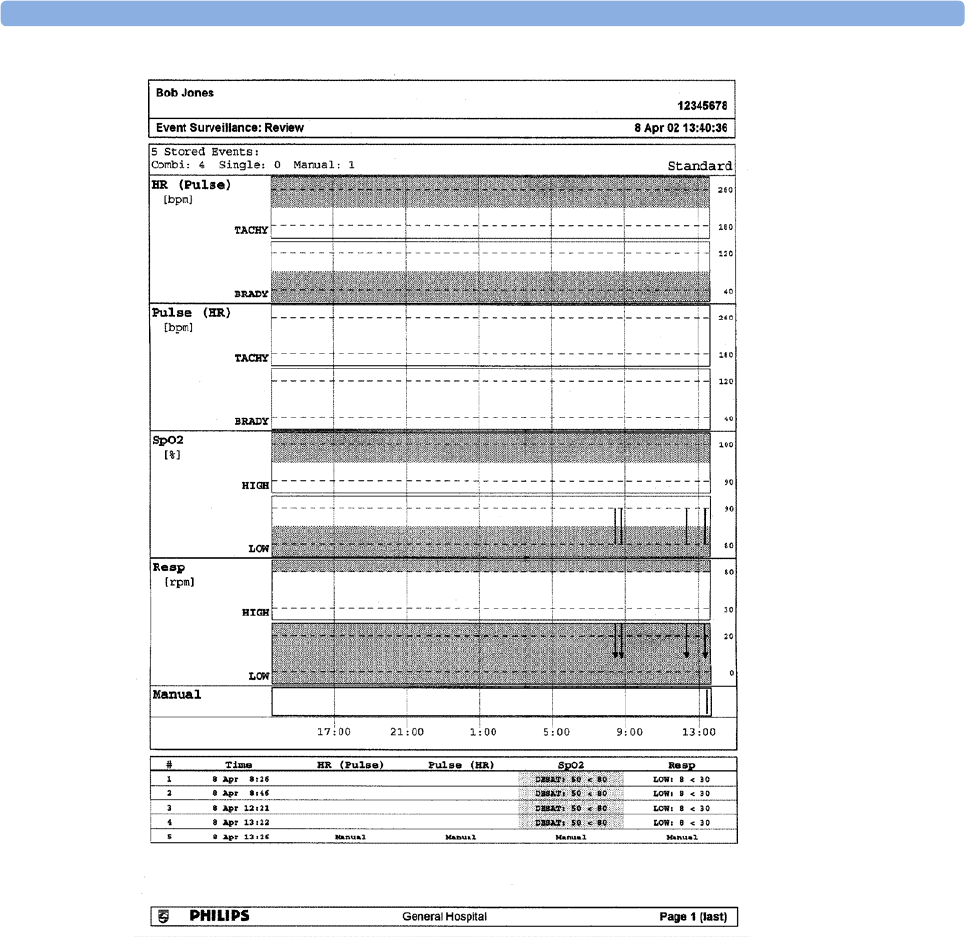
23 Event Surveillance 291
Levels of Event Surveillance 291
Event Groups 292
Event Episodes 292
Events Pop-Up Keys 293
Event Triggers 294
The Events Database 298
Viewing Events 298
Annotating Events 301
Documenting Events 301
24 ProtocolWatch 309
SSC Sepsis Protocol 309
25 Recording 317
Central Recording 317
Starting and Stopping Recordings 317
Overview of Recording Types 319
All ECG Waves Recordings 319
Creating and Changing Recordings Templates 320
Changing ECG Wave Gain 321
Recording Priorities 321
Recording Strip 321
Reloading Paper 323
Recorder Status Messages 323

9
26 Printing Patient Reports 325
Starting Report Printouts 325
Stopping Reports Printouts 326
Setting Up Reports 327
Setting Up Individual Print Jobs 328
Checking Printer Settings 329
Printing a Test Report 329
Switching Printers On Or Off for Reports 329
Dashed Lines on Reports 329
Unavailable Printer: Re-routing Reports 330
Checking Report Status and Printing Manually 330
Printer Status Messages 331
Sample Report Printouts 332
27 Using the Drug Calculator 337
Accessing the Drug Calculator 338
Performing Drug Calculations 338
Charting Infusion Progress 340
Using the Titration Table 341
Documenting Drug Calculations 341
28 IntelliBridge EC10 Module 343
Connecting an External Device 343
Changing Waves and Numerics Displayed 344
Viewing the IntelliBridge Device Data Window 344
Using Screens with External Device Data 344
Alarms/INOPs from External Devices 345
Language Conflict with External Device Drivers 345
29 VueLink Modules 347
Connecting an External Device 348
Changing VueLink Waves and Numerics Displayed 348
Viewing the VueLink Device Data Window 349
Using VueLink Screens 349
Switching VueLink On and Off 349
Alarms/INOPs From External Devices 350
Language Conflict with External Device Drivers 350
30 Using Timers 351
Viewing Timers 351
Timer Setup Pop-up Keys 352
Setting Up Timers 352
Displaying a Timer On The Main Screen 353
Displaying A Clock On The Main Screen 354
10
31 Respiratory Loops 355
Viewing Loops 355
Capturing and Deleting Loops 356
Showing/Hiding Loops 356
Changing Loops Display Size 356
Using the Loops Cursor 356
Changing Loops Type 357
Setting Up Source Device 357
Documenting Loops 357
32 Laboratory Data 359
Viewing Received Data 359
33 Care and Cleaning 361
General Points 361
Cleaning the Monitor 362
Disinfecting the Monitor 362
Sterilizing the Monitor 363
Cleaning, Sterilizing and Disinfecting Monitoring Accessories 363
Cleaning the SO2 Optical Module 363
Cleaning the Recorder Printhead (M1116B only) 363
34 Maintenance and Troubleshooting 365
Inspecting the Equipment and Accessories 365
Inspecting the Cables and Cords 366
Maintenance Task and Test Schedule 366
Troubleshooting 367
Disposing of the Monitor 367
Disposing of Empty Calibration Gas Cylinders 367
35 Accessories 369
ECG/Resp Accessories 369
NBP Accessories 372
Invasive Pressure Accessories 375
SpO2 Accessories 376
Temperature Accessories 380
Cardiac Output (C.O.) Accessories 381
Mainstream CO2 Accessories 382
Sidestream CO2 Accessories 382
Mainstream CO2 Accessories (for M3016A) 383
Microstream CO2 Accessories 383
Spirometry Accessories 384
tcGas Accessories 385
EEG Accessories 385
BIS Accessories 385
SO2 Accessories for M1021A 386
11
SO2 Accessories for M1011A 386
Recorder Accessories 386
Battery Accessories 386
36 Specifications 387
Intended Use 387
Manufacturer's Information 387
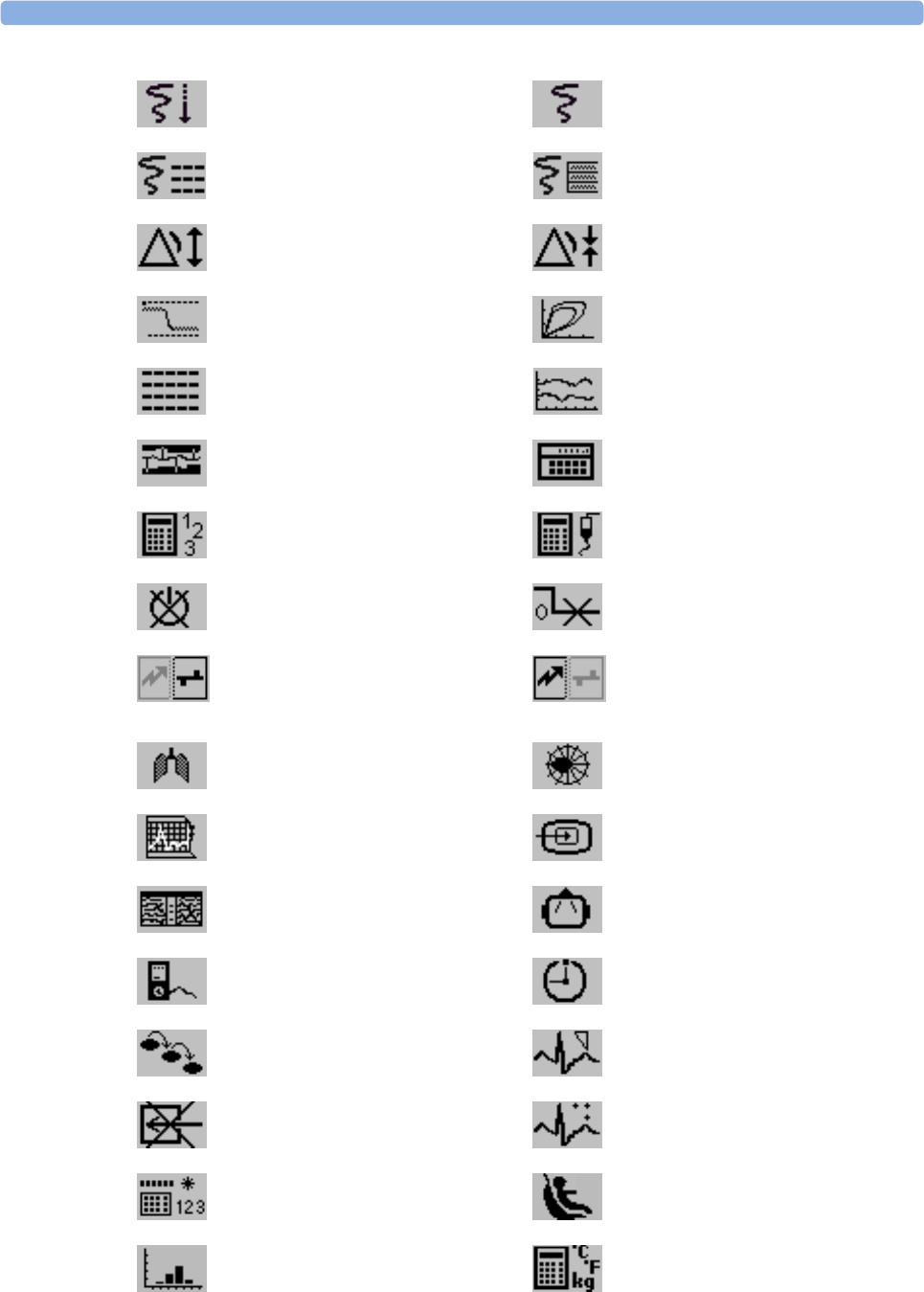
Symbols 389
Installation Safety Information 390
Monitor Mounting Precautions 393
Altitude Setting 393
Monitor Safety Specifications 393
EMC And Radio Regulatory Compliance 393
Physical Specifications 395
Environmental Specifications 397
Performance Specifications 399
Interface Specifications 401
Measurement Specifications 405
Safety and Performance Tests 424
37 Default Settings Appendix 429
Country-Specific Default Settings 429
Alarm and Measurement Default Settings 436
Alarm Default Settings 436
ECG, Arrhythmia, ST and QT Default Settings 437
Pulse Default Settings 438
Respiration Default Settings 439
SpO2 Default Settings 439
NBP Default Settings 440
Temperature Default Settings 440
Invasive Pressure Default Settings 441
Cardiac Output Default Settings 443
CO2 Default Settings 444
Spirometry Default Settings 444
tcGas Default Settings 445
Intravascular Oxygen Saturation 445
SvO2 Default Settings 446
ScvO2 Default Settings 446
EEG Default Settings 446
BIS Default Settings 447
VueLink Default Settings 447
Index 449

12

1
13
1Introduction
These Instructions for Use are for clinical professionals using the IntelliVue MX600/MX700/MX800
patient monitor.
This basic operation section gives you an overview of the monitor and its functions. It tells you how to
perform tasks that are common to all measurements (such as entering data, switching a measurement
on and off, setting up and adjusting wave speeds, working with profiles). The alarms section gives an
overview of alarms. The remaining sections tell you how to perform individual measurements, and
how to care for and maintain the equipment.
Familiarize yourself with all instructions including warnings and cautions before starting to monitor
patients. Read and keep the Instructions for Use that come with any accessories, as these contain
important information about care and cleaning that is not repeated here.
This guide describes all features and options. Your monitor may not have all of them; they are not all
available in all geographies. Your monitor is highly configurable. What you see on the screen, how the
menus appear and so forth, depends on the way it has been tailored for your hospital and may not be
exactly as shown here.
In this guide:
•A warning alerts you to a potential serious outcome, adverse event or safety hazard. Failure to
observe a warning may result in death or serious injury to the user or patient.
•A caution alerts you to where special care is necessary for the safe and effective use of the
product. Failure to observe a caution may result in minor or moderate personal injury or damage
to the product or other property, and possibly in a remote risk of more serious injury.
Introducing the Monitor
The IntelliVue MX600/MX700/MX800 patient monitor offers a monitoring solution optimized for
the high-end surgical, cardiac, medical and neonatal care environments. Combining patient surveillance
and data management, it allows multi-measurement monitoring by linking separate modules. The
MX600 uses the navigation knob as primary input device and the MX700/MX800 use the touch
screen as primary input device. All monitors have a remote control for convenient access to the five
main keys and numeric data input.

1Introduction
14
The monitor stores data in trend, event, and calculation databases. You can see tabular trends (vital
signs) and document them on a printer. You can view measurement trend graphs, with up to three
measurements combined in each graph, to help you identify changes in the patient's physiological
condition. You can view fast-changing measurement trends with beat to beat resolution and see up to
four high resolution trend segments. Event surveillance enhances documentation and review of
physiologically significant events by automatically detecting and storing up to 50 user-defined clinical
events over a 24 hour period.
With the optional Integrated PC, you have computer functionality directly in the monitor. You can use
standard applications (e.g. Web browsers), connect to the hospital network or intranet, and run a
second independent display with content from the patient monitor.
An IntelliVue X2 or MP5 can be connected to your monitor, where it acts as a multi-measurement
module, acquiring measurements for the host monitor. When the X2 or MP5 is disconnected from the
the original host monitor, it continues to monitor the patient as a fully independent, battery powered
patient monitor, eliminating the need for a separate transport monitor. On connection to a new host
monitor, the X2 or MP5 resumes its role as multi-measurement module, ensuring fully continuous
monitoring.
Major Parts and Keys
MX600/700:
1Color coded alarm lamps
2Alarms Off lamp
3Power on/Standby switch with
integrated LED: Green - On/
Standby, Red - Error
4AC power LED
5Mounting quick-release lever
(when this is pressed the
monitor is not fixed on the
mounting)
6Part number and serial number
7Hardkeys (Silence, Alarms Off,
Main Screen)
8Navigation knob

1 Introduction
15
MX800:
Devices for Acquiring Measurements
The patient monitor acquires patient measurements using the devices described in this section. You
can also extend the measurement capabilities of your monitor with such devices. Of these
measurement devices, only the X2 has its own power on/standby switch, and can be powered from an
external power supply or a rechargeable battery when not directly connected to the monitor (refer to
the IntelliVue X2 Instructions for Use for details). All the rest take their power exclusively from the
monitor, and switch on automatically when you turn on the monitor. A green power-on LED indicates
when they are drawing power from the monitor. A permanently illuminated, or flashing, red LED
indicates a problem with the unit that requires the attention of qualified service personnel.
All symbols used on the front panels are explained in “Symbols” on page 389.
WARNING
When connecting devices for acquiring measurements, always position cables and tubing carefully to
avoid entanglement or potential strangulation.
Flexible Module Rack (M8048A)
The 8-slot flexible module rack (FMS-8) lets you use up to eight plug-in physiological measurement
modules. For the MX800, you can connect two FMSs to use up to 10 measurement modules.
The maximum number of specific module types that can be used simultaneously in an FMS-8 is: five
pressure modules, four temperature modules, four VueLink or IntelliBridge modules (any
combination).
1Color coded alarm lamps
2Alarms Off lamp
3Power on/Standby switch with
integrated LED: Green - On/
Standby, Red - Error
4AC power LED
5Mounting quick-release lever
(when this is pressed the
monitor is not fixed on the
mounting)
6Part number and serial number
1Introduction
16
Connect the FMS to the monitor via the measurement link cable (MSL). Use the MSL connector on
the left-hand side to connect an additional MMS. Use the connector on the right to connect to the
monitor.
4-Slot Flexible Module Rack (FMS-4)
The 4-Slot flexible module rack (FMS-4) lets you use up to four plug-in physiological measurement
modules.
The maximum number of specific module types that can be used simultaneously in an FMS-4 is: four
pressure modules, four temperature modules, four VueLink or IntelliBridge modules (any
combination).
Connect the FMS to the monitor via the measurement link cable (MSL). Use the MSL connector on
the left-hand side (if you have the appropriate option) to connect an additional MMS. Use the
connector on the back to connect to the monitor.
Measurement Modules
You can use up to eight measurement modules with the Flexible Module Rack (M8048A). Available
modules are:
• Invasive blood pressure (M1006B)
• Temperature (M1029A)
• Oxygen saturation of arterial blood (SpO2) (M1020B)
• Cardiac output (M1012A), and Continuous cardiac output with M1012A Option #C10
• Transcutaneous gas (M1018A)
• Mixed venous oxygen saturation - SvO2 (M1021A)
• Intravascular Oxygen Saturation - ScvO2 or SvO2 (M1011A)
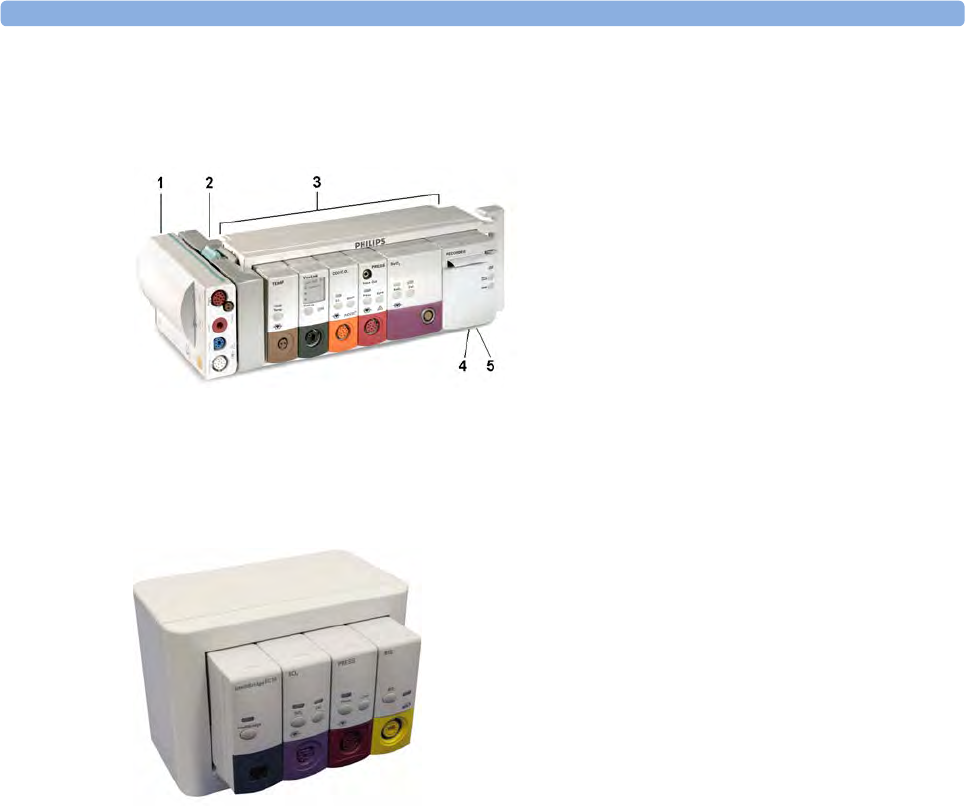
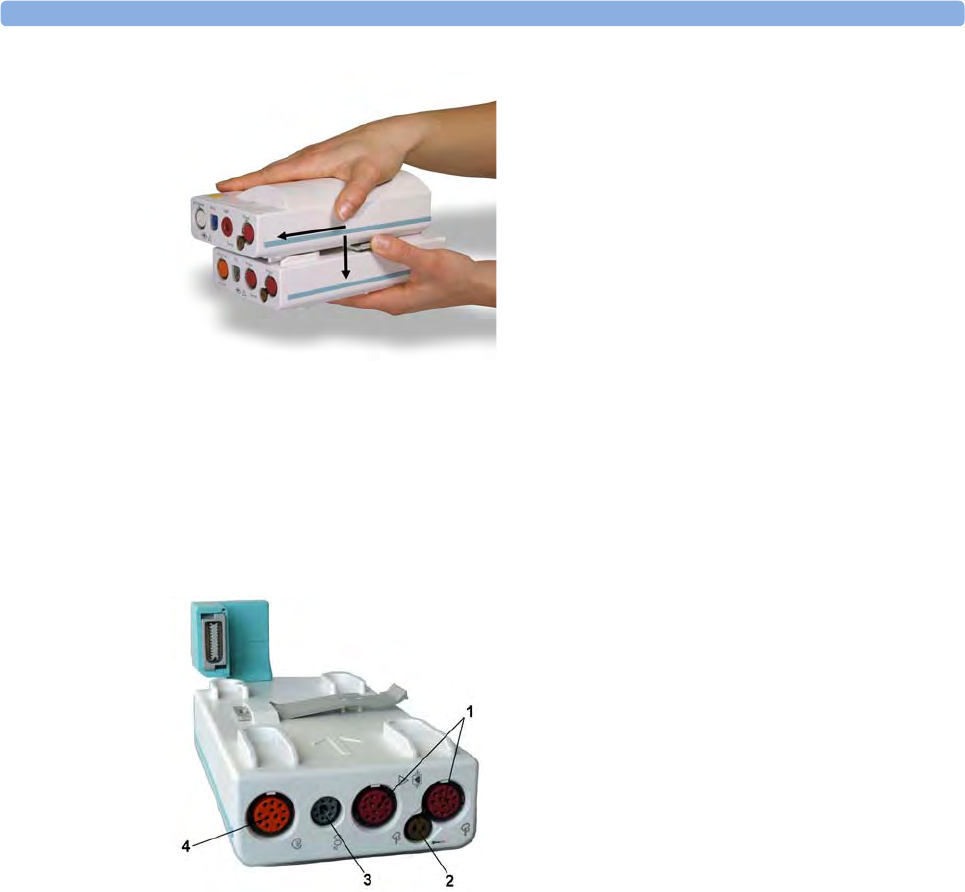
1X1 Multi-Measurement Module
2Multi-Measurement Module
mount
3Flexible Module Rack FMS-8
4Power on LED
5Interruption indicator
1 Introduction
17
• Recorder (M1116B)
• VueLink device interface (M1032A)
• IntelliBridge EC10
• EEG (M1027A)
• Bispectral Index - BIS (M1034A)
• Spirometry (M1014A)
You can plug in and unplug modules during monitoring. Insert the module until the lever on the
module clicks into place. Remove a module by pressing the lever upwards and pulling the module out.
A measurement automatically switches on when you plug the module in, and switches off when you
unplug it. Reconnecting a module to the same monitor restores its label and measurement settings,
such as alarms limits. If you connect it to a different monitor, the module remembers only its label.
The connector socket on the front of each module is the same color as the corresponding connector
plug on the transducer or patient cable.
Press the Setup key on the module's front to display the measurement's setup menu on the monitor
screen. When the setup menu is open, a light appears above the key. Some modules have a second key.
On the pressure module, for example, it initiates a zeroing procedure.
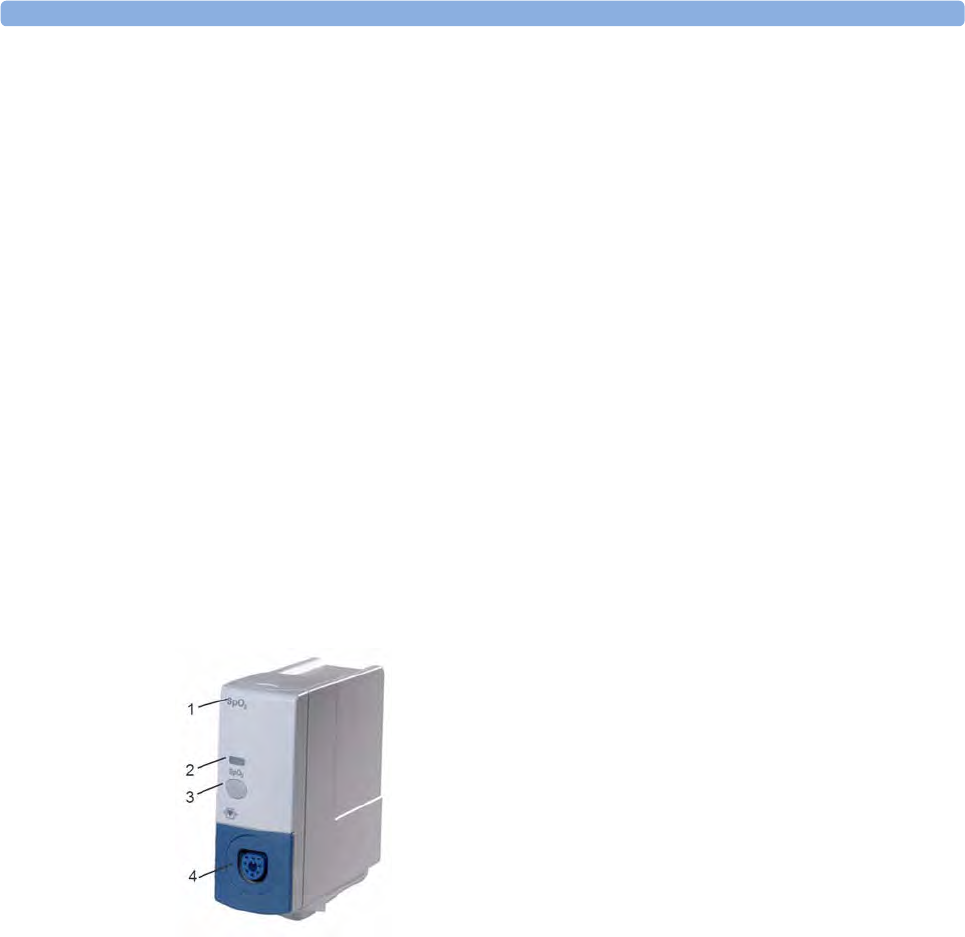
Example Module (SpO2)
X1 Multi-Measurement Module (M3001A)
The X1 Multi-Measurement Module (MMS) can simultaneously monitor 3-, 5-, 6- or 10-lead ECG
(including arrhythmia and ST monitoring), respiration, SpO2, NBP and either invasive pressure or
temperature.
You can connect it to the monitor via a cable or mount it on the left side of the FMS.
1Module name
2Setup key LED
3Setup key to enter setup menu of measurement modules or
external device data window. Some modules have a second
module-specific key next to this one, for example Zero.
4Connector socket for patient cable/transducer

1Introduction
18
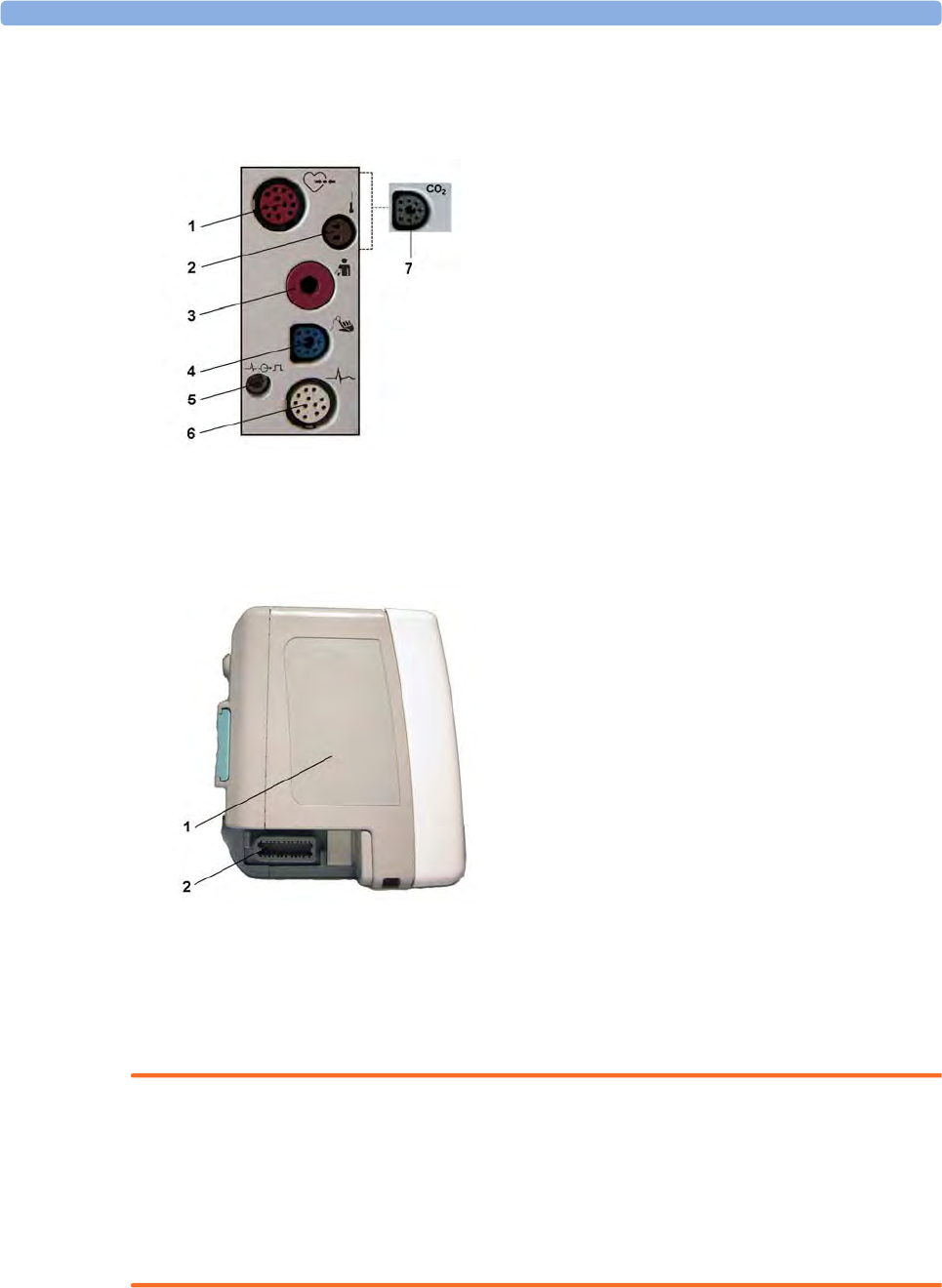
X1 Connectors and Symbols
X2 Multi-Measurement Module (M3002A)
The X2 Multi-Measurement Module (MMS) can simultaneously monitor 3-, 5-, 6- or 10-lead ECG
(including arrhythmia and ST monitoring), respiration, SpO2, NBP and either invasive pressure and
temperature, or CO2. It has a color touchscreen display.
1White ECG/Resp connector
2Blue SpO2 connector
3Red NBP connector
4Combined pressure (red) and temperature
(brown) connector - connect either invasive
pressure transducer or temperature probe.
You might have a version of the MMS that
does not have this connector.
5NBP STAT key - starts NBP STAT series
of measurements
OR
Zero key - initiates a zero procedure for the
connected pressure transducer when
pressed and held for a second
6NBP Start/Stop key - starts or stops NBP
measurements
7Silence: acknowledges all active alarms by
switching off audible alarm indicators and
lamps
1 Introduction
19
The X2 has the added capability to operate as a stand-alone monitor, and can be powered by a
rechargeable battery. This makes it particularly suited to transport situations. When the X2 is
disconnected from the original host monitor, it continues to monitor the patient as a stand-alone
monitor running on battery power, eliminating the need for a separate transport monitor. When the
X2 is connected to a new host monitor, it resumes its role as MMS, ensuring fully continuous
monitoring. For details of using the X2 as a stand-alone monitor, refer to the IntelliVue X2 Instructions
for Use.
When connected to a host monitor (Companion Mode is indicated), the X2 takes power from the
host, including that required for battery charging. The X2 can also be powered by AC mains when not
connected to a host monitor using the optionally available external power supply (M8023A). See the
IntelliVue X2 Instructions for Use for details.
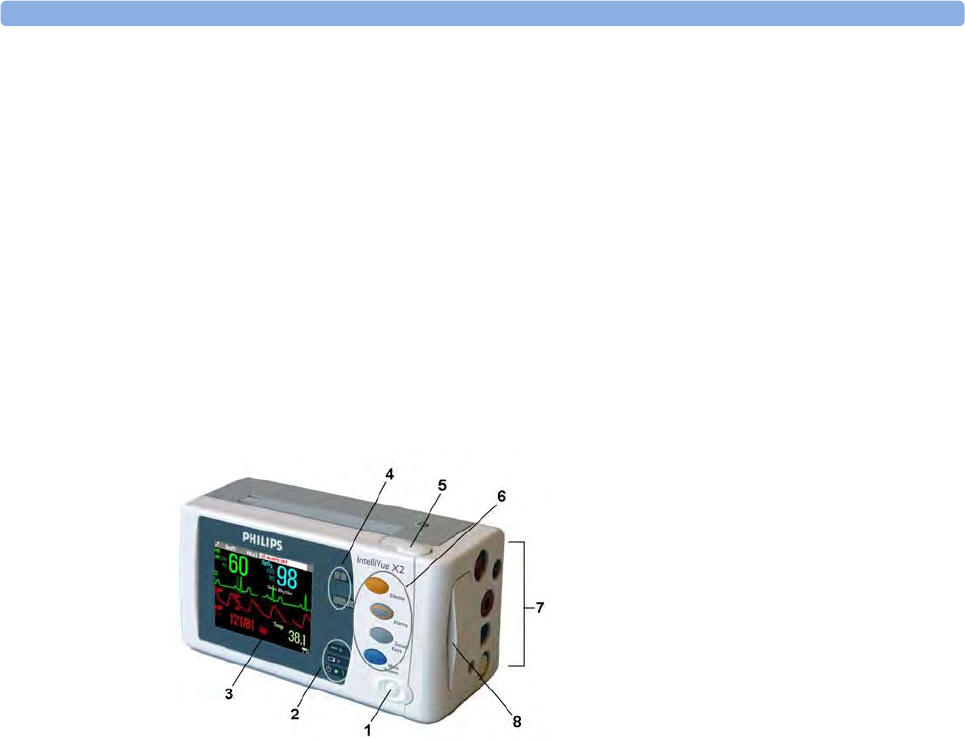
X2 Overview
1On/Standby switch
2Power and battery indicators (see “X2
Controls and Indicators” on page 20)
33.5-inch TFT LCD touchscreen QVGA
display
4Alarm lamps (see “X2 Controls and
Indicators” on page 20)
5Battery eject button
6Hard keys (see “X2 Controls and
Indicators” on page 20)
7Measurement connectors (see “X2 Patient
Connectors, Right Side” on page 21)
8Battery compartment
1Introduction
20
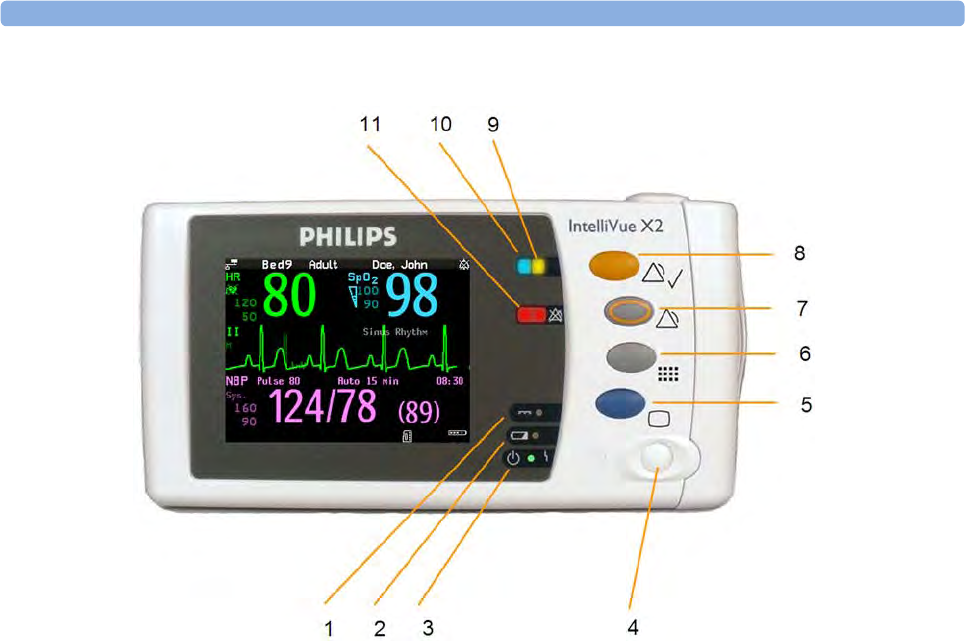
X2 Controls and Indicators
1External power LED. Green when monitor is powered from an external power source.
2Battery status LED. Yellow when charging. Flashing red when battery is empty.
3On/Standby LED. Green when monitor is on. Red indicates an error.
4On/Standby switch. Disabled when X2 is connected to a host monitor
5Main Screen key: closes all open menus/windows and returns to the main screen.
6SmartKeys key: brings up SmartKeys on the screen.
7Alarms key: turns alarms On/Off, or pauses them.
8Silence key
9Active alarm lamp. Red or yellow, depending on alarm level. Blinks until active alarm is
acknowledged.
10 Active INOP alarm lamp in light blue. Blinks until active INOP is acknowledged.
11 Alarms off indicator. When alarms are suspended, the lamp is red, and the alarms off symbol is
shown.
1 Introduction
21
X2 Patient Connectors, Right Side
Showing symbols version (international) - English version has text labels
X2 Left Side
MMS Extensions
The MMS extensions connect to the X1 and X2 MMS and use the MMS settings and power. Trend
data and measurement settings from the measurements in the extensions are stored in the MMS.
WARNING
• The MMS extensions can only function when they are connected to an MMS. If the MMS is
removed during monitoring, the measurements from both the MMS and the extension are lost.
• Measurements from an MMS extension connected to an X2 are not available when the X2 is
running on its own battery power. They are only available when the X2 is powered from AC mains,
when connected to a host monitor or the external power supply (M8023A), or from the Battery
Extension.
To separate an extension from the MMS, press the release lever down, and push the MMS forward.
1Pressure (option)
2Temperature (option)
3Noninvasive blood pressure
4SpO2
5ECG sync pulse output
6ECG/Respiration
7CO2 (option in place of Pressure and Temperature)
1Loudspeaker
2MSL Connector. Connects to the external power
supply or a host monitor via the MSL cable for AC
mains operation, battery charging, and
communication with a network.
1Introduction
22
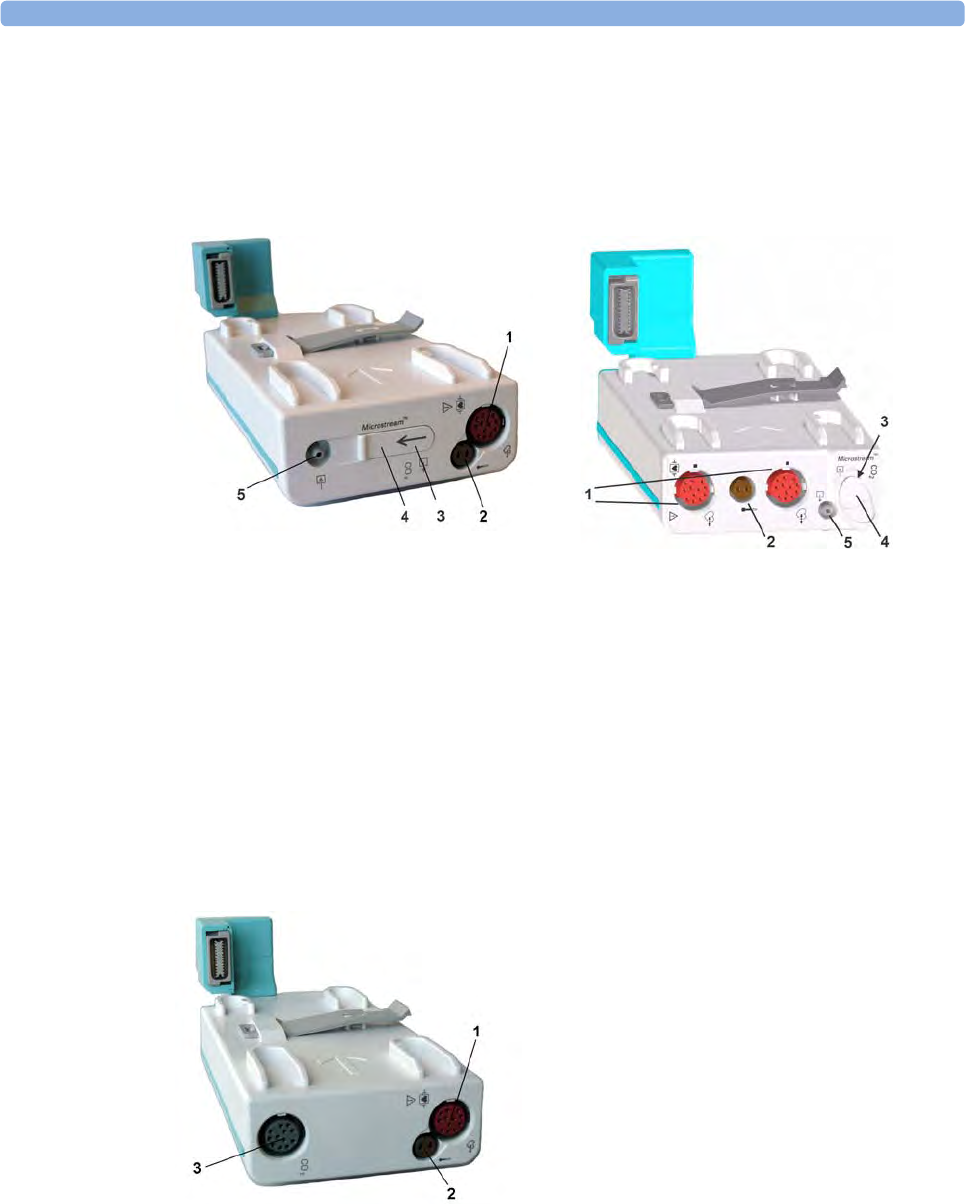
M3014A, M3015A, M3015B and M3016A Capnography MMS Extensions
The optional M3014A Capnography extension adds mainstream capnography or sidestream
capnography, and optionally one pressure plus either a pressure or a temperature, Cardiac Output and
Continuous Cardiac Output to the MMS.
M3014A
1Pressure connectors (red)
2Temperature connector (brown)
3Mainstream/sidestream connector CO2
4Cardiac Output connector
1 Introduction
23
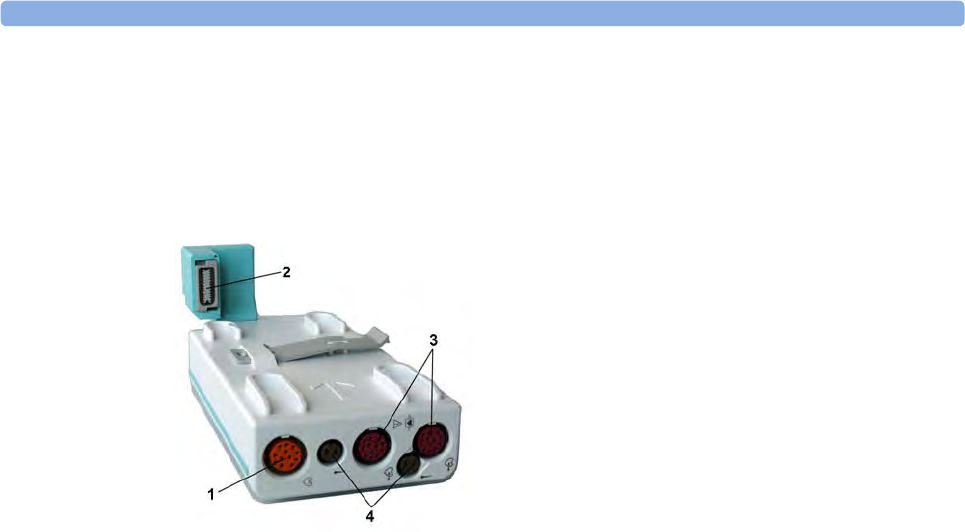
The optional M3015A Microstream CO2 extension adds microstream capnography and optionally
either pressure or temperature to the MMS. The optional M3015B Microstream CO2 extension adds
microstream capnography, two pressures and a temperature to the MMS.
The optional M3016A Mainstream CO2 extension adds mainstream capnography and optionally either
pressure or temperature to the MMS.
When a capnography extension is connected to an X2 MMS with CO2, the CO2 from the extension
will be automatically deactivated in favor of the one in the X2. If you prefer to use the CO2
measurement on the extension, you can activate it via the measurement selection key (see “Resolving
Label Conflicts” on page 40).
M3015A M3015B
1Pressure connectors (red) - M3015A optional
2Temperature connector (brown) - M3015A optional
3Inlet
4Microstream connector CO2
5Gas sample outlet
M3016A
1Pressure connectors (red)
2Temperature connector (brown)
3Mainstream/sidestream connector CO2
(optional)
1Introduction
24
The cardiac output measurement in the M3014A is deactivated when the extension is used with an X2
MMS, even if the X2 is connected to an external power supply. The cardiac output measurement is
only available when the X2 is connected to a host monitor.
M3012A Hemodynamic MMS Extension
The M3012A Hemodynamic extension can be connected to the M3001A Multi-Measurement Module
to provide the following additional measurements: Temperature, Pressure, an additional Pressure or
Temperature, and C.O. and CCO measurements.
The cardiac output measurement is deactivated when the extension is used with an X2 MMS unless the
X2 is connected to a host monitor.
Operating and Navigating
Everything you need to operate the monitor is contained on its screen. Almost every element on the
screen is interactive. Screen elements include measurement numerics, waveforms, screen keys,
information fields, alarms fields and menus.
The configurability of the monitor means that often you can access the same element in different ways.
For example, you might be able to access an item through its on-screen setup menu, via a hard key, or
via a SmartKey.
1Cardiac Output (orange; optional)
2Connection to MMS
3Pressure connectors (red)
4Temperature connectors (brown)
1 Introduction
25
Selecting Screen Elements
Select a screen element to tell the monitor to carry out the actions linked to the element. For example,
select the Patient Identification element to call up the Patient Demographics window, or select the
HR numeric to call up the Setup ECG menu. Select the ECG wave segment to call up the ECG Lead
menu.
Note that the space between each line of a menu may be configured to wide or narrow to facilitate
your most common method of operation, either touch, remote control or a pointing device such as a
mouse.
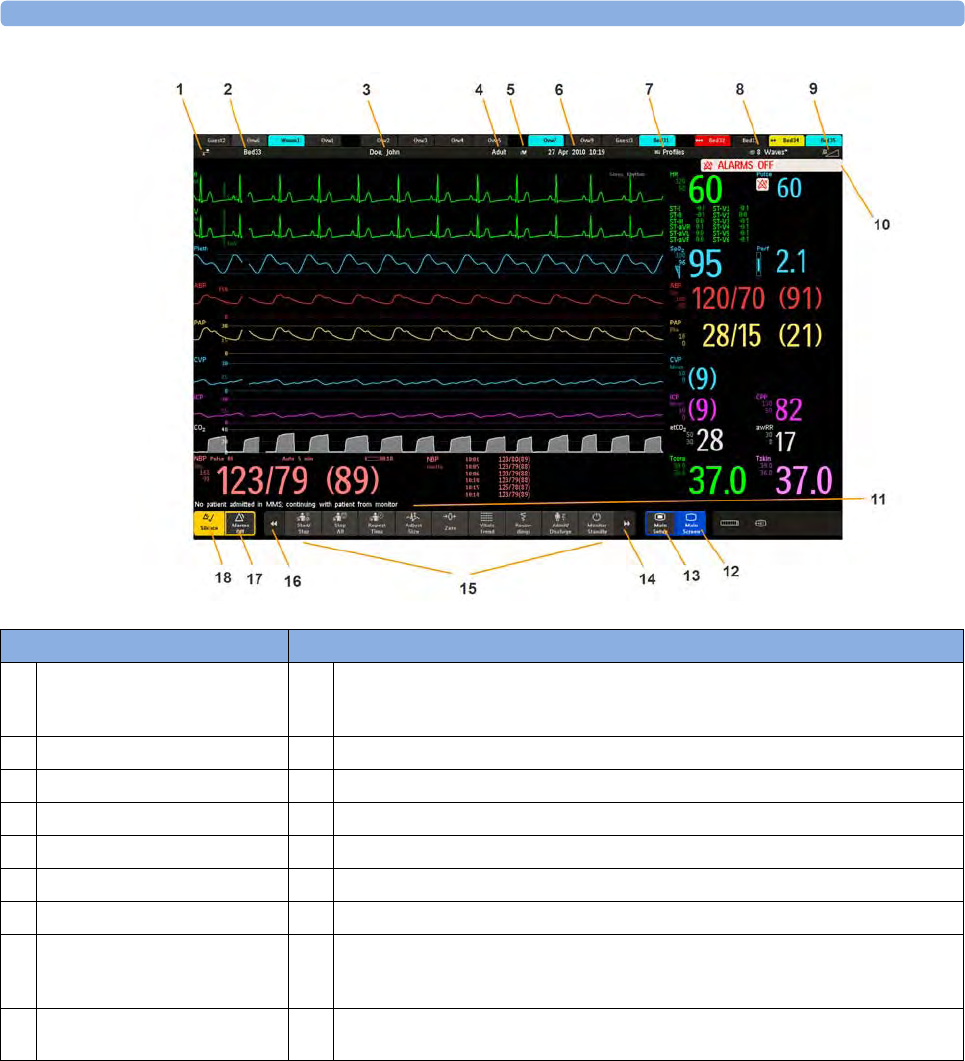
Monitor information line Other screen elements
1network connection indicator
(documented in Information
Center Instructions for Use)
10 alarm status area - shows active alarm messages
2bed label 11 status line - shows information messages and prompting you for action
3patient identification 12 close all open menus and windows and return to main screen
4patient category 13 enter Main Setup menu
5paced status 14 scroll right to display more SmartKeys
6date and time 15 SmartKeys - these change according to your monitor's configuration
7access the Profiles menu 16 scroll left to display more SmartKeys
8current screen name/enter
Change Screen menu 17 Pause Alarms - pauses alarm indicators. Pause duration depends on monitor
configuration. If pause duration is infinite, this key is labeled Alarms Off. Select again
to immediately re-enable alarm indicators.
9adjust alarm volume/level
indicator 18 Silence - acknowledges all active alarms by switching off audible alarm indicators and
lamps permanently or temporarily, if alarm reminder (ReAlarm) is configured on.
1Introduction
26
Using the Touchscreen
Select screen elements by pressing them directly on the monitor's screen.
Disabling Touchscreen Operation
To temporarily disable touchscreen operation of the monitor, press and hold the Main Screen
permanent key. A padlock will appear on the Main Screen permanent key.
Press and hold the Main Screen permanent key again to re-enable the touchscreen operation.
Using a Mouse or Trackball
If you are using a mouse or trackball, select screen elements by clicking on them (press and release the
left mouse button). While you are moving the mouse, a cursor appears and a highlight shows your
current position.
Moving Windows
You can move windows and menus using the Touchscreen or a mouse. To move a window,
1Select the title of the window and keep your finger on the title, or the mouse button pressed.
2Move your finger on the Touchscreen, or move the mouse, to move the window.
3Take your finger off the screen, or release the mouse button, to place the window in the final
position.
The new position is only active until the window or menu is closed. Not all locations on the screen can
be a target position, a window cannot overlap the monitor info line, the alarms and INOPs or the
status line.
Using Keys
The monitor has four different types of keys:
Permanent Keys
A permanent key is a graphical key that remains on the screen all the time to give you fast access to
functions.
Pause Alarms - pauses alarm indicators. Pause duration depends on monitor
configuration. If pause duration is infinite, this key is labeled Alarms Off.
Select again to immediately re-enable alarm indicators.
Silence - acknowledges all active alarms by switching off audible alarm indicators and
lamps.
Main Screen - close all open menus and windows and return to the main screen.
Main Setup - enter main setup menu.
1 Introduction
27
SmartKeys
A SmartKey is a configurable graphical key, located at the bottom of the main screen. It gives you fast
access to functions. The selection of SmartKeys available on your monitor depends on your monitor
configuration and on the options purchased. If you have an integrated PC (iPC) you may also see
Smartkeys generated by applications on the iPC.
enter profile menu, or revert to
default profile
change Screen, or revert to default
screen
show BIS Sensor previous Screen
freeze waves quick admit a patient
set alarm limits enter patient identification menu to
admit/discharge/transfer
change alarm volume end case to discharge a patient
change QRS volume view information for patients in
other beds
enter standby mode - suspends
patient monitoring. All waves and
numerics disappear from the display.
All settings and patient data
information are retained.
change screen brightness (not for
independent displays)
review beat labels (annotate
arrhythmia wave)
re-learn arrhythmia
change amplitude (size) of ECG
wave
enter cardiac output procedure
- start/stop manual NBP
measurement
- start auto series
- stop current automatic
measurement within series
start NBP STAT measurement
stop automatic or STAT NBP
measurement and measurement
series
start NBP measurement and
measurement series
stop current NBP measurement
start veni puncture (inflate cuff to
subdiastolic pressure)
set the NBP repeat time
access patient reports zero invasive pressure transducer
1Introduction
28
start a delayed recording access pop-up recording keys
access Vital Signs recording function access Select Waves recording
function
set wide automatic alarm limits set narrow automatic alarm limits
access wedge procedure window access the Loops window
review vital signs trend review graph trend
access event surveillance access calculations
access the calculator access the Drug Calculator
gas analyzer - exit standby mode suppress zero for all gas
measurements
unpair equipment and continue
central monitoring with the monitor
unpair equipment and continue
central monitoring with the telemetry
device
access the spirometry data window access ST Map application
start 12-Lead Capture (only available
if Information Center is connected)
access remote applications (if
Application Server is connected)
access EEG CSA access the EEG montage
display external device information access timers
access ProtocolWatch set standard or EASI lead placement
switch CO2 pump off new lead setup
enter data manually start/stop car seat assessment record
open the Histogram window open Unit Conversion window

1 Introduction
29
Hardkeys
A hardkey is a physical key on a monitoring device, such as the zero pressure key on the MMS or a
setup key on a module.
Pop-Up Keys
Pop-up keys are task-related graphical keys that appear automatically on the monitor screen when
required. For example, the Confirm pop-up key appears only when you need to confirm a change.
Using the Remote Control
The remote control provides you with direct access to five hard keys, a navigation knob and a numeric
keypad:
Hardkeys
1Silence - acknowledges all active alarms by switching off audible alarm indicators and lamps.
Behavior follows the Silence permanent key configuration.
2Alarms Off/Pause Alarms - pauses alarm indicators. Behavior follows the Pause Alarms
permanent key configuration.
3Main Screen - close all open menus and windows and return to the main screen.
4SmartKeys - display a block of SmartKeys specially configured for remote tasks (see below)
5Back - go back one step to the previous menu.
1Introduction
30
The remote control can be used with a USB cable connection to the monitor or without a cable using
short range radio. When used without a cable, the remote control must be assigned to the monitor.
The assignment is made in Configuration or Service mode.
CAUTION
When using a remote control without a cable, it is important that the user knows which remote control
is assigned to which monitor. Use the tethering cable delivered with the remote control to attach it to a
bed rail or IV pole, or label the remote control with the bed or monitor ID.
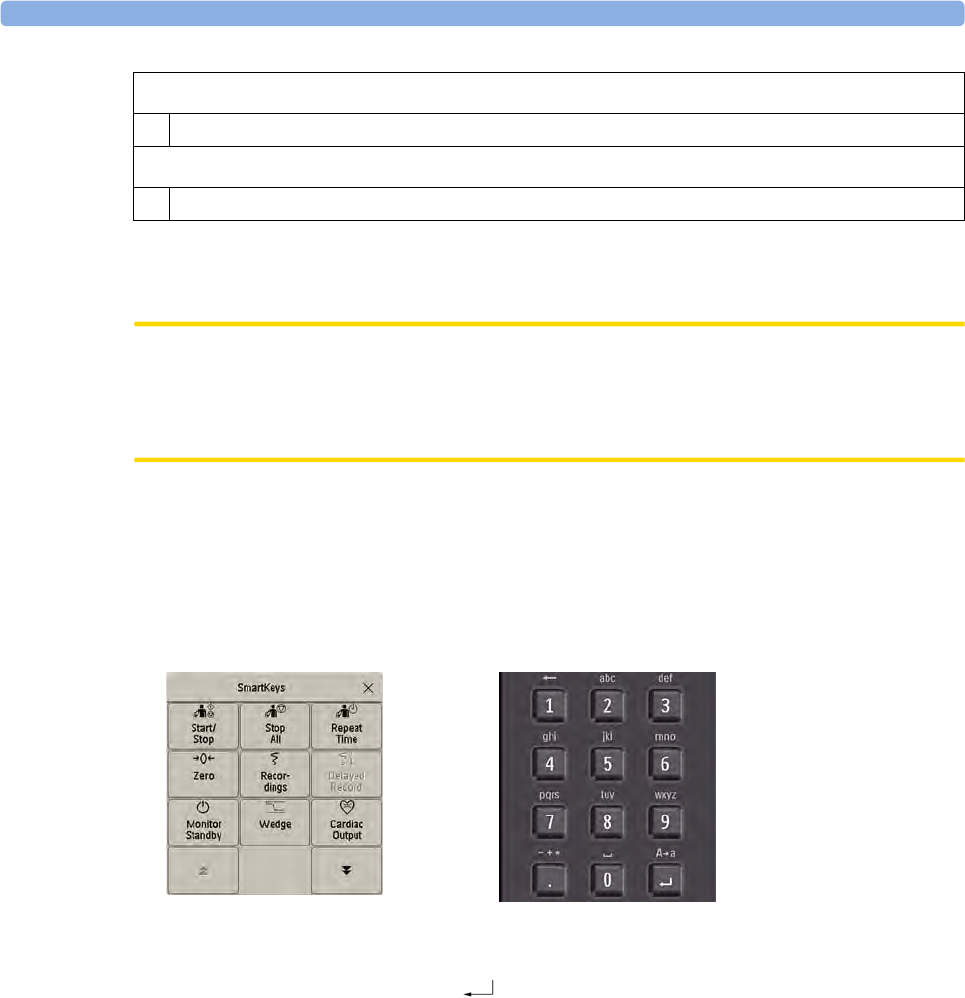
Using the SmartKeys Key
The SmartKeys hard key on the remote control displays a block of SmartKeys on the monitor screen.
Nine SmartKeys appear in a 3 by 3 matrix which corresponds to the layout of the numeric pad on the
remote control.
Pressing the 1 key on the remote control selects the top left SmartKey, pressing the 8 key selects the
bottom center SmartKey. The .and the key can be used to select the arrow keys to page up and
down in the available SmartKeys.
The SmartKeys which appear can be configured so that you have the functions available which you
most often need when using the remote control. If no list of SmartKeys has been configured, the
standard SmartKeys will be displayed and you can page through to the key you want.
Using the On-Screen Keyboard
Use this as you would a conventional keyboard. Enter the information by selecting one character after
another. Use the Shift and capital Lock keys to access uppercase letters. Use the Back key to delete
single characters, or use the Clr key to delete entire entries. Select Enter to confirm what you have
entered and close the on-screen keyboard.
If a conventional keyboard is connected to the monitor, you can use this instead of or in combination
with the on-screen keyboard.
Keypad
6 Type numeric data on the keypad and press the Enter key to enter the data on the monitor.
Navigation knob
7 Rotate the knob to highlight screen elements, then press to select the highlighted element.

1 Introduction
31
Using the On-Screen Calculator
You can use the on-screen calculator to perform any of the standard operations for which you would
normally use a handheld calculator.
• To access the on-screen calculator, select the Calculator SmartKey, or select Main Setup then
Calculations followed by Calculator.
Operating Modes
When you switch the monitor on, it starts up in monitoring mode. To change to a different mode:
1Select the Main Setup menu.
2Select Operating Modes and choose the mode you require.
Your monitor has four operating modes. Some are passcode protected.
•Monitoring Mode: This is the normal, every day working mode that you use for monitoring
patients. You can change elements such as alarm limits, patient category and so forth. When you
discharge the patient, these elements return to their default values. Changes can be stored
permanently only in Configuration Mode. You may see items, such as some menu options or the
altitude setting, that are visible but ‘grayed out’ so that you can neither select nor change them.
These are for your information and can be changed only in Configuration Mode.
•Demonstration Mode: Passcode protected, this is for demonstration purposes only. You must
not change into Demonstration Mode during monitoring. In Demonstration Mode, all stored
trend information is deleted from the monitor’s memory.
•Configuration Mode: Passcode protected, this mode is for personnel trained in configuration
tasks. These tasks are described in the Configuration Guide. During installation the monitor is
configured for use in your environment. This configuration defines the default settings you work
with when you switch on, the number of waves you see and so forth.
• Service Mode: Passcode protected, this is for trained service personnel.
When the monitor is in Demonstration Mode, Configuration Mode, or Service Mode, this is indicated
by a box with the mode name in the center of the Screen and a symbol in the bottom right-hand
corner. Select the mode box in the center of the screen to change to a different mode.
When an X2 or MP5 is connected to a host monitor (Companion Mode is indicated):
• The monitor in companion mode will adopt the operating mode of the host monitor.
• You cannot change the operating mode at the monitor in companion mode.
Standby Mode
Standby mode can be used when you want to temporarily interrupt monitoring.
To enter Standby mode,
• select the Monitor Standby SmartKey or
•select
Main Setup, followed by Monitor Standby.
The monitor enters Standby mode automatically after the End Case function is used to discharge a
patient.
1Introduction
32
Standby suspends patient monitoring. All waves and numerics disappear from the display but all
settings and patient data information are retained. A special Standby screen is displayed. This can be
configured to a moving image or a blank screen. If a patient location is entered at the Information
Center, this will also be displayed on the Standby screen (availability depends on Information Center
revision).
To resume monitoring,
• Select anything on the screen or press any key.
If you connect an X2 or MP5 that is powered on (and not in Standby) to a host monitor in Standby
mode, the host will leave Standby mode. When connected to a host monitor, with both the host and
the monitor in companion mode in Standby mode, leaving Standby on the monitor in companion
mode will also make the host leave Standby.
Understanding Screens
Your monitor comes with a set of pre-configured Screens, optimized for common monitoring
scenarios such as OR adult, or ICU neonatal. A Screen defines the overall selection, size and position
of waves, numerics and other elements on the monitor screen when you switch on. You can easily
switch between different Screens during monitoring. Screens do NOT affect alarm settings, patient
category and so forth.
When you switch from a complex to a less complex Screen layout, some measurements may not be
visible but are still monitored in the background. If you switch to a more complex Screen with, for
example, four invasive pressure waves but you have only two pressures connected to the monitor, the
"missing" two pressures are either left blank or the available space is filled by another measurement.
Switching to a Different Screen
1To switch to a different Screen, select the current Screen name in the monitor info line, or select
the Change Screen SmartKey.
2Choose the new Screen from the pop-up list.
Changing a Screen's Content
If you do not want to change the entire Screen content, but only some parts of it, you can substitute
individual waves, numerics, high-res waves, or trends. Be aware that these changes cannot be stored
permanently in Monitoring Mode.
To change the selection of elements on a Screen,
1Select the element you want to change.
2From the menu that appears, select Change Wave, Change Numeric, or ChangeHiResTrend, and
then select the wave or numeric you want, or select the high-resolution trend wave you want from
the list of available waves.
If you do not see Change Numeric in the menu, this Screen may be configured to always display
the numeric beside its wave. Changing the wave will automatically change the numeric.
The changed Screen is shown with an asterisk in the monitor info line.
In the Change Screen menu, the changed Screen is shown linked to the original Screen and marked
with an asterisk.

1 Introduction
33
Up to three modified Screens can be accessed via the Change Screen menu.
To recall Screens, either
• select the name of the Screen in the Change Screen menu
or
• use the previous/next arrows at the top of the Change Screen menu to move back and forth in
the Screen history. The ten most recently-used Screens including up to three modified Screens can
be accessed.
After a patient discharge, the monitor's default Screen is shown. Modified Screens are still available in
the Change Screen menu.
If the monitor is switched off and then on again, modified Screens are erased from the monitor's
memory and cannot be recalled. If a modified Screen was the last active Screen when the monitor was
switched off, it is retained (unless Automat. Default is configured to Yes).
Connecting Additional Displays to the Monitor
You can connect a second display, showing the same Screen as the main display, to your monitor, for
viewing only.
If you have the optional independent display interface, you can connect a second display which can be
configured and operated individually using standard input devices.
For monitors with multiple displays and multiple input devices, the usage and behavior can be
configured according to specific requirements at installation (for example, use for two independent
operators or tracking of mouse input across two displays). For details refer to the Service Guide.
When two operators are using two displays, the scope of an action depends on the type of operation:
• Patient monitoring operations such as Silence or Pause alarms take effect for the monitor as a
whole, the results will be seen on both displays.
• Display operations such as the Main Screen key and Back hardkey will take effect only on the
display being operated.
If you are operating two displays with one remote control, to navigate from one display to another:
1Move the highlight to the Main Screen key and then turn one click further.
The highlighting moves to a special "jump" field at the edge of the Screen.
2Press the navigation knob on the remote control to confirm; the highlighting will automatically
move to the other display.
The content of each Screen can be changed individually as described in the previous section. If you are
operating two displays, you can choose Screens for both displays from one location:
1Select Profiles in the monitor info line of the first display,
2Select Display 1, or Display 2, then select the Screen you want to appear on that display from the
list of available Screens.
When two displays are mounted next to each other or one above the other, a special Screen can be
assigned which spans across both displays. The Screen content for these Tall and Wide Screens can
then use the increased area available with two displays. These Screens appear in the Screen list with a
special Tall Screen or Wide Screen symbol.

1Introduction
34
Certain windows (for example: cardiac output procedure) can only be shown on one display at a time.
If you try to open one of these windows when it is already shown on another display, you will see a
blank gray window with a cross through it.
Using the XDS Remote Display
Using the IntelliVue XDS solution it is possible to view an independent monitor screen on an external
display. The XDS solution consists of a medical grade PC-based hardware platform, XDS application
software and the XDS connectivity option on the monitor. Depending on the configuration you can
also operate the monitor from the external display. The XDS must be connected to the same Local
Area Network (LAN) as the monitor.
It is also possible to use an existing PC, connected to the same LAN, to host the XDS Application
software.
For more details, including limitations and restrictions, refer to the Instructions for Use for the XDS
Application.
Using the Visitor Screen
If a visitor Screen is configured for your monitor, you can use it to clear the screen of all waves and
numerics but continue to monitor the patient with active alarms and trend storage at the bedside and
Information Center. You can change the name of the visitor Screen in Configuration Mode.
• To activate this Screen, select the Screen name in the monitor info line to open the Change Screen
menu, then select the name of the visitor Screen configured for your monitor from the list of
available Screens.
To select a Screen with waves and numerics again,
• Touch the gray box in the center of the screen, showing the visitor Screen's name, to open the
Change Screen menu and select a different Screen to show waves and numerics again.
Understanding Profiles
Profiles are predefined monitor configurations. They let you change the configuration of the whole
monitor so you can adapt it to different monitoring situations. The changes that occur when you
change a complete profile are more far reaching than those made when you change a Screen. Screens
affect only what is shown on the display. Profiles affect all monitor and measurement settings.
The settings that are defined by Profiles are grouped into three categories. Each category offers a
choice of 'settings blocks' customized for specific monitoring situations. These categories are:
•Display (screens)
Each profile can have a choice of many different predefined screens.
If you are using a second display, each display can have its own individual screen selection.
When you change the profile, the screen selection configured for the new profile becomes active.
•Measurement Settings
Each profile can have a choice of different predefined measurement settings. These relate directly
to individual measurements, for example, measurement on/off, measurement color, alarms limits,
NBP alarm source, NBP repeat time, temperature unit (°F or °C), pressure unit (mmHg or kPa).
1 Introduction
35
•Monitor Settings
Each profile can have a choice of different predefined monitor settings. These relate to the
monitor as a whole; for example, display brightness, alarms off/paused, alarm volume, QRS tone
volume, tone modulation, prompt tone volume, wave speed, resp wave speed, pulse source.
You can change from one complete profile to another or swap individual settings blocks (display/
monitor settings/measurement settings) to change a subset of a profile. Changes you make to any
element within the settings blocks are not saved when you discharge the patient, unless you save them
in Configuration Mode.
Depending on your monitor configuration, when you switch on or discharge a patient the monitor
either continues with the previous profile, or resets to the default profile configured for that monitor.
WARNING
If you switch to a different profile, the patient category and paced status normally change to the setting
specified in the new profile. However some profiles may be set up to leave the patient category and
paced status unchanged. Always check the patient category, paced status, and all alarms and settings,
when you change profiles.
When you leave Demonstration Mode, the monitor uses the default profile.
Swapping a Complete Profile
1Select Profiles in the monitor info line, or select the Profiles SmartKey.
2In the Profiles menu, select Profile.
3Chose a profile from the pop-up list.
4Confirm your selection.
Swapping a Settings Block
1Select Profiles in the monitor info line, or select the Profiles SmartKey.
2In the Profiles menu, select Display or Measmnt.Settings or Monitor Settings to call up a list of
the settings blocks in each category.
3Choose a settings block from the pop-up list.
4Confirm your selection.
Default Profile
Your monitor has a default profile that it uses when you leave Demonstration, or Service modes, or
when you discharge a patient. This profile is indicated by a diamond shaped symbol.

1Introduction
36
Locked Profiles
Understanding Settings
Each aspect of how the monitor works and looks is defined by a setting. There are a number of
different categories of settings, including,
Screen Settings, to define the selection and appearance of elements on each individual Screen
Measurement settings, to define settings unique to each measurement, for example, high and low
alarm limits
Monitor settings, including settings that affect more than one measurement or Screen and define
general aspects of how the monitor works, for example, alarm volume, reports and recordings, and
display brightness.
You must be aware that, although many settings can be changed in Monitoring Mode, permanent
changes to settings can only be done in the monitor's Configuration Mode. All settings are reset to the
stored defaults:
• when you discharge a patient
• when you load a Profile
• when the monitor is switched off for more than one minute (if Automat. Default is set to Yes).
Changing Measurement Settings
Each measurement has a setup menu in which you can adjust all of its settings. You can enter a setup
menu:
• via the measurement numeric - select the measurement numeric to enter its setup menu. For
example, to enter the Setup ECG menu, select the HR (heart rate) numeric.
• via the Setup hardkey (on plug-in modules) - press the Setup hardkey on the module front.
•via the Main Setup permanent key - if you want to setup a measurement when the measurement is
switched off, use the Main Setup permanent key and select Measurements. Then select the
measurement name from the pop-up list. With this permanent key you can access any setup menu
in the monitor.
• via the Measurement Selection key.
This guide always describes the entry method using the setup menu. But you can use any method you
prefer.
Some profiles are locked, so that you cannot change them, even in Configuration Mode.
These are indicated by this lock symbol.

1 Introduction
37
Switching a Measurement On and Off
When a measurement is off, its waves and numerics are removed from the monitor's screen. The
monitor stops data acquisition and alarming for this measurement. A measurement automatically
switches off if you disconnect its module or MMS. If you disconnect a transducer, the monitor
replaces the measurement numeric with question marks. If in this situation alarms are paused or
switched off, the measurement in question may be switched off completely, depending on monitor
configuration.
1Enter the measurement's setup menu and select the measurement.
2Select the measurement name to switch between on and off. The screen display indicates the active
setting.
Switching Numerics On and Off
For some measurements, such as EEG, you can choose which numerics to view on the screen.
In the measurement's setup menu, select the numeric name to toggle between on and off.
For example in the Setup EEG menu, select the EEG numeric name to toggle between on and off.
Adjusting a Measurement Wave
To quickly adjust wave-related measurement settings (such as speed or size), select the measurement
wave itself. This displays the measurement wave menu, which has only wave-related measurement
settings.
Changing Wave Speeds
Lowering the wave speed compresses the wave and lets you view a longer time period. Increasing the
speed expands the waveform, giving you a more detailed view.
The monitor distinguishes three groups of wave speed settings,
•RespiratorySpeed, for all respiratory waves: CO2, anesthetic agents and O2
•EEG Speed, for all EEG and BIS waves
•Global Speed, for all waves not included in the other two groups.
Changing the Wave Group Speed
The wave speed group setting defines the speed of all the waves in the group.
To change the wave speed of a wave speed group,
1Select Main Setup, then select User Interface
2Select Global Speed, RespiratorySpeed, or EEG Speed as required
3Select a value from the list of available speeds.
Changing Wave Speed for a Channel
To change the wave speed of an individual wave channel,
1Enter the Wave menu for a measurement by selecting its wave.
2Select Change Speed.
1Introduction
38
3To set the speed to the wave group speed, select RespiratorySpeed, EEG Speed, or Global Speed.
To set an individual channel speed, select a numeric value from the list of available speeds. This
overrides the wave group speed setting and set the speed for the individual wave channel on the
monitor Screen. The wave channel speed is independent of the wave (label) depicted in the
channel, if you change the wave, the new wave will retain the set channel speed.
Freezing Waves
You can freeze waves on the screen and measure parts of the wave using cursors. The waves are frozen
with a history of 20 seconds so that you can go back and measure what you have seen.
Freezing An Individual Wave
To freeze a wave,
1Enter the Wave menu for the measurement by selecting the wave on the screen.
2Select Freeze Wave.
The realtime wave is replaced with the frozen wave.
Freezing All Waves
To freeze all waves on the screen,
1Select the Freeze Waves SmartKey.
All realtime waves are replaced with frozen waves.
Measuring Frozen Waves
To measure a frozen wave,
1Select the frozen wave.
If you are using touch, this automatically positions the vertical cursor. The cursor can be
repositioned by touching the required point on the wave, or
2Using the SpeedPoint or another pointing device or touch: use the right/left arrow keys to move
the vertical cursor.
The vertical cursor moves through the time axis and the current value is displayed next to the
cursor.
3Use the up/down arrow keys to activate and move the horizontal cursor.
The horizontal cursor measures the wave value, which is displayed above the cursor line. If the
wave is a pressure wave, the cursor value can be stored as a systolic, diastolic or mean pressure
value; if the pressure wave is a PAP wave it can also be stored as a PAWP value; for pressure waves
P, P1 to P8 it can also be stored as an IAP value. The stored value appears in the trend database as
a manually entered value.
Changing The Wave Speed
Lowering the wave speed compresses the wave and lets you view a longer time period. Increasing the
speed expands the waveform, giving you a more detailed view.

1 Introduction
39
To change the wave speed:
1Select the frozen wave.
2Select Change Speed.
3Select a speed from the list.
Updating The Frozen Wave
To update the wave, that is freeze the current wave:
1Select the frozen wave.
2Select Freeze Again.
Releasing Frozen Waves
To release frozen waves,
1Select a frozen wave.
2Select Unfreeze Waves.
All frozen waves are released.
Using Labels
You may have more than one instance of some measurements, for example pressure, being used
simultaneously. The monitor uses labels to distinguish between them. The default settings defined in
the profile (such as measurement color, wave scale, and alarm settings) are stored within each label.
When you assign a label to a measurement, the monitor automatically applies these default settings to
the measurement. The labels assigned are used throughout the monitor, in reports, recordings, and in
trends.
Changing Measurement Labels (e.g. Pressure)
To change a measurement label of a measurement with multiple labels (e.g. invasive pressure or
temperature),
1Enter the wave menu of the measurement.
2Select Label.
3Choose a label from the list.
The monitor automatically applies the scale, color, etc. settings stored in the Profile for the label you
select. You can change scale settings in Monitoring Mode, but color can only be changed in the
monitor's Configuration Mode.
Any labels already being used in the monitor are shown "grayed-out" in the list and cannot be selected.
About Label Sets
Your monitor may be configured to use a Restricted or Full label set. The Full label set provides extra
labels for Pressure and Temp. See the sections on Pressure and Temperature in these Instructions for
Use for more information.
If you connect an MMS from a monitor using a Full label set to an IntelliVue monitor using a
Restricted label set or an M3/M4 monitor, any additional labels switch to labels available in the target
monitor. This may cause a label conflict with other monitored measurements.
1Introduction
40
Be aware that connecting a monitor using the Full label set to an Information Center with certain
software revisions may affect the availability of measurement information from the additional labels on
the Information Center. See the Information Center documentation and your monitor's Configuration
Guide for information on label set compatibility.
Resolving Label Conflicts
Each label must be unique, that is, it can only be assigned once. You cannot monitor two pressures
labeled "ICP" at the same time. If you need to use two identical pressures, you must assign different
labels to them, for example, P and ICP.
Measurement labels are stored in the measurement device (module or MMS). If you try to use two
measurement devices that have identical labels, this causes a label conflict in the monitor.
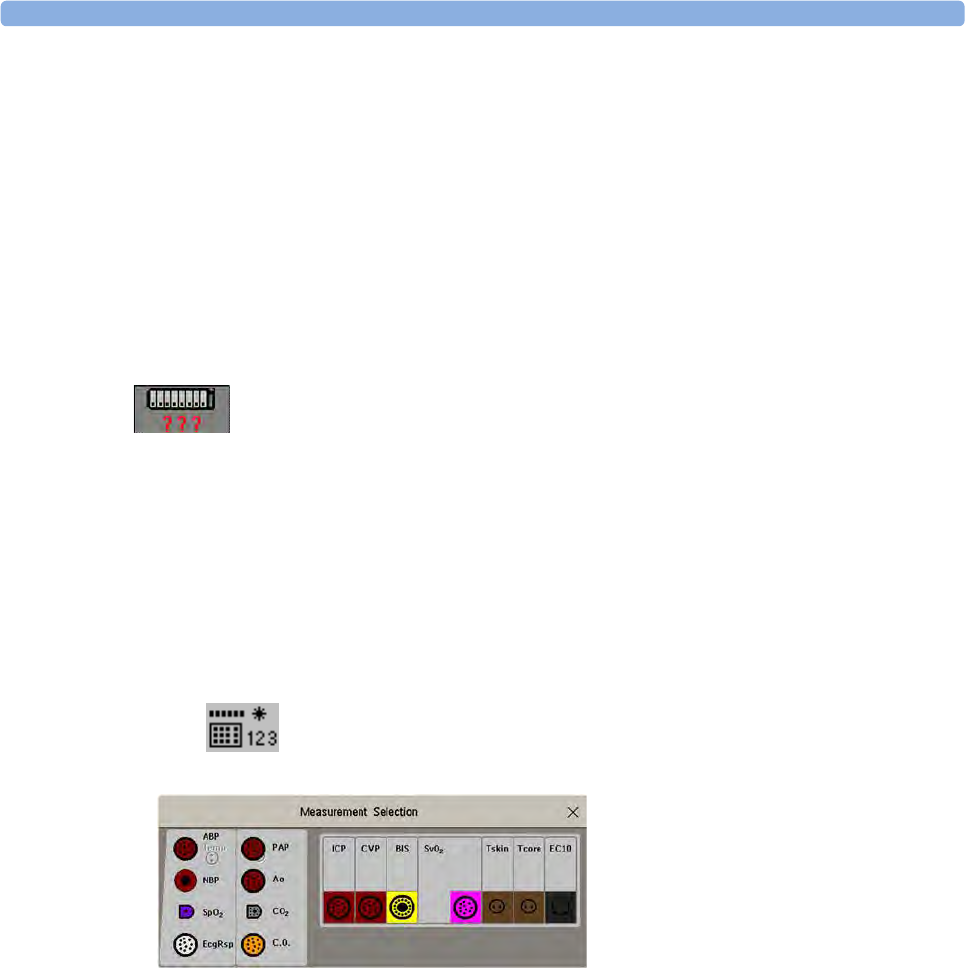
Measurement selection key with question marks indicating a label conflict.
Depending on your configuration, the monitor will either
• resolve the conflict automatically, by assigning a new, generic label to the most recently connected
conflicting label (e.g. a second FAP label could be changed to ABP)
•display the Measurement Selection window automatically for you to resolve the conflict
• take no action, you must enter the Measurement Selection window and resolve the conflict.
All the currently available measurement devices, for example MMSs, MMS extensions, measurement
modules, Gas analyzers, devices connected to a host monitor and manually entered measurements
(marked ), are depicted in the Measurement Selection window.
Any measurement labels causing a label conflict are shown in red. If a measurement device is
connected but currently unavailable, for example, because it was deactivated due to a label conflict, the
device is shown "grayed-out".
De-activated devices are grayed-out (here
the Temp measurement on the left)
1 Introduction
41
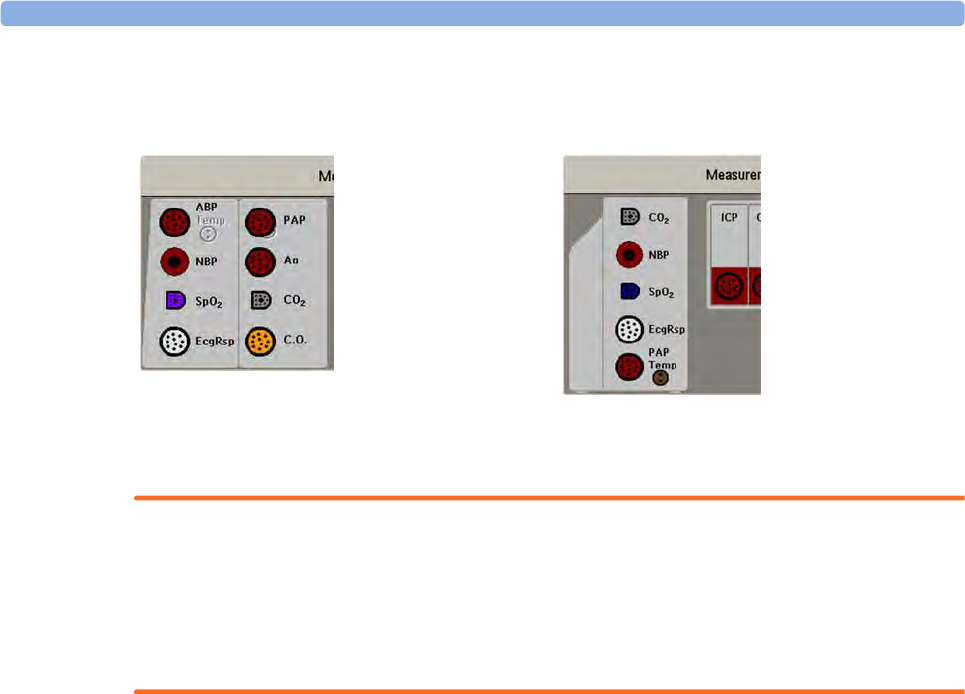
When an X2 or MP5 is connected to a host monitor, the measurement selection window looks like
this:
WARNING
When an X2 or MP5 with an active measurement, say SpO2, is connected to a host monitor with the
same measurement already active, the SpO2 measurement on the X2 or MP5 is deactivated and the
Meas. DEACTIVATED INOP is displayed. The measurement can only be reactivated if the X2 or MP5
is disconnected from the host monitor. The label conflict can be resolved on the host monitor like any
other label conflict.
To resolve a label conflict:
1Select the measurement selection key or select Main Setup, then Meas. Selection to display the
Measurement Selection window.
2Select the device whose label you want to correct.
3Use the measurement selection pop-up keys to resolve the conflict. Select either:
–Change Label: to assign a different label to the conflicting label
–De- Activate: to disable the conflicting device. It retains its label for future use but becomes
invisible to the monitor, as though it had been unplugged. When the device has been
deactivated the question marks under the measurement selection key will be replaced by XXX.
–Setup <Measurement Label>: to enter the Setup menu for the measurement and change the
conflicting device's label to a different label.
–Modify Driver (VueLink/IntelliBridge only): - to modify the device driver setup to disable the
conflicting device's label.
Label Compatibility
When a new measurement is introduced, or new labels for an existing measurement, these labels will
not be shown on older Information Centers, and consequently not on the Overview screen sourced
from the Information Center.
When a patient is transferred from a monitor with these new labels to one with an older software
revision, the labels will be replaced with a generic label for that measurement. The settings for that
generic label will then be used.
X2 connected to host monitor MP5 connected to host monitor

1Introduction
42
If it is critical that the measurement labels are available at the Information Center and after transfers,
the older monitors and the Information Center must be upgraded to the appropriate software revision.
Entering Measurements Manually
You can enter values into the monitor that have been measured with other equipment or manually (for
example, manual temperatures, lab values). These values are then stored in the database, included in
trends and reports, and passed on to the Information Center and central charting systems. There is no
alarm functionality for manually entered measurements.
To enter values,
1Select the Enter Values SmartKey or select Main Setup then select Enter MeasValues.
2Select the measurement you want to enter values for. The Edit window will open.
3If the measurement is switched off, switch it on by selecting the label.
4Select Value and enter the value.
5Select Date/Time to enter the date and time for the value. The default is always the current date
and time.
6For compound labels, for example ABPs, ABPd and ABPm, select the Format field to select
whether all values are required or a single value.
7Select Save.
When a manually entered value has been configured to display as a numeric on the screen, you can also
enter a new value for this measurement by selecting the numeric, then selecting Enter MeasValues.
Manually entered measurement values are marked with a * on the display, in trends, and so forth. Each
measurement has a defined measurement interval after which a value becomes invalid (no value is then
displayed). Values can be entered up to two hours after they have been measured or up to the
measurement interval, if this is shorter.
The list of measurement labels which appears in the Enter Measurement Values window is set in
Configuration Mode.
No values can be entered manually on a monitor in companion mode when it is connected to a host
monitor.
Switching Manually Entered Measurements On and Off
To switch a manually entered measurement on or off,
1Select the Enter Values SmartKey or select Main Setup then select Enter MeasValues.
2Select the measurement you want to switch on or off.
3Select the measurement label field to switch between On and Off.
Changing Monitor Settings
To change monitor settings such as brightness, or QRS tone volume, select the Main Setup permanent
key and then select User Interface to enter a submenu where you can change these settings.
1 Introduction
43
Adjusting the Screen Brightness
1Select the Brightness SmartKey.
2Select the appropriate setting for the screen brightness. 10 is the brightest, 1 is the least bright.
Optimum is suitable for most monitoring locations and optimizes power usage for battery
powered monitors.
Your monitor may be configured with a lower brightness for Standby mode and also (for battery
powered monitors) for transport to conserve battery power. These settings can only be changed in the
monitor's Configuration Mode.
If you are using a monitor with an external display, the Brightness SmartKey does not adjust the
brightness of this display. See the instructions supplied with the external display for instructions.
Setting the Date and Time
1Select the Date, Time screen element from the monitor's info line to enter the Date, Time menu.
2Select, in turn, the Year, Month, Day, Hour (in 24 hour format, only) and Minute as necessary.
Select the correct values from the pop-up list.
3Select Store Date, Time to change the date and time.
If your monitor is connected to an Information Center, the date and time are automatically taken from
this. Once it is set, the internal clock retains the setting even when you switch off the monitor.
WARNING
Changing the date or time will affect the storage of trends and events.
Checking Your Monitor Revision
1Select Main Setup then select Revisions to open the Monitor Revision menu.
2Select the correct device from the device pop-up keys.
3From the Monitor Revision menu, select the monitor component for which you need revision
information.
Getting Started
Once you understand the basic operation principles, you can get ready for monitoring. We also
recommend working through the CBT for self-training before using the monitor (not available in all
languages).
1Introduction
44
Inspecting the Monitor
WARNING
If the monitor is mechanically damaged, or if it is not working properly, do not use it for any
monitoring procedure on a patient. Contact your service personnel.
1Before you start to make measurements, carry out the following checks on the monitor including
all connected MMSs, modules, or MMS extensions.
– Check for any mechanical damage.
– Check all the external cables, plug-ins and accessories.
2Plug the power cord into the AC power source.
3Check all the functions of the instrument that you need to monitor the patient, and ensure that the
instrument is in good working order.
Switching On
Press the power on/standby switch on the monitor for one second. The monitor performs a self test
during which all lamps will light up and a tone will be sounded, and is then ready to use. If you see a
message such as CO₂ SENS.WARMUP wait until it disappears before starting to monitor that
measurement. Connected devices usually take their power from the monitor. External devices such as
gas monitors and those connected via VueLink/IntelliBridge have their own power switches.
Power On/Power Off Behavior
The general rules determining the behavior of the monitor when connected to, or disconnected from
power are as follows:
• A monitor that was switched on prior to a temporary power loss switches on again when power is
restored.
• A monitor that was switched off prior to a temporary power loss remains off when power is
restored.
• An X2 or MP5 switches on automatically when connected to a running host monitor.
• When an X2 or MP5 is disconnected from a running host monitor, the X2 or MP5 continues to
run without interruption on battery power.
Setting up the Modules
1Decide which measurements you want to make.
2Connect the required modules, MMSs, or MMS extensions.
3Check that you have the correct patient cables and transducers plugged in. The connectors are
color-coded to the patient cables and transducers for easy identification.
Starting Monitoring
After you switch on the monitor,
1Admit your patient to the monitor.
2Check that the profile, alarm limits, alarm and QRS volumes, patient category and paced status and
so forth are appropriate for your patient. Change them if necessary.
1 Introduction
45
3Refer to the appropriate measurement chapter for further details of how to perform the
measurements you require.
WARNING
During MR imaging, remove all transducers, sensors and cables from the patient. Induced currents
could cause burns.
Disconnecting from Power
The On/Standby switch does not disconnect the monitor from the ac power source. To disconnect,
unplug the power cable.
Monitoring After a Power Failure
If the monitor is without power for less than one minute, monitoring will resume with all active
settings unchanged. If the monitor is without power for more than one minute, the behavior depends
on your configuration. If Automat. Default is set to Yes, the default profile will be loaded when power
is restored. If Automat. Default is set to No, all active settings are retained, if power is restored within
48 hours. The Automat. Default setting is made in Configuration Mode.
Networked Monitoring
You can connect your monitor to an Information Center on a network, using one of the optional
interfaces:
• Standard wired LAN
• Wireless LAN
• IntelliVue Instrument Telemetry System (IIT).
WARNING
Do not connect patient monitors to the standard hospital network.
Additionally, when an IntelliVue X2 or MP5 is equipped with IIT and declared at the Information
Center as a telemetry device, it allows data continuity when paired to a host monitor. After
disconnection from the host monitor, it continues to monitor the patient during transport and
provides continuous data to the same sector on the Information Center. (See “Assigning a Telemetry
Device and a Monitor to One Patient” on page 265.)
If your monitor is connected to a network, a network symbol is displayed in the upper left corner next
to the bed label. To see details about the Care Group, the monitoring equipment, and technical
information about the network,
• in the monitor info line, select the bed label.
Be aware that some network-based functions may be limited for monitors on wireless networks in
comparison to those on wired networks.
Printout functionality and data export are not guaranteed when using a standard hospital network.
1Introduction
46
Using the Integrated PC
If your monitor has the optional integrated PC (iPC), you can run applications on the iPC. The
applications display data on the monitor's display (or on a second independent display) that is
generated on and retrieved from the iPC or externally.
For details about applications, refer to the XDS/iPC Instructions for Use.
The monitor runs independently of the iPC, and vice versa.
WARNING
• Some clinical applications may show data from another patient. Be aware that some of the data on
your patient monitor display may not always be from your patient.
• Applications running on the iPC cannot act as a primary alarming device and cannot be relied
upon for alarm notification. There may be no audible or visible indications apart from what is
shown on the screen and any data shown may be delayed.
Starting the iPC
Your monitor may be configured to have the iPC start up automatically when the monitor is switched
on. If not:
1Select Main Setup then Internal PC.
2In the Internal PC menu, select Switch PC On to start the iPC.
Viewing the iPC Desktop on the Monitor Display
If the Desktop is not displayed on the monitor display:
1Select the iPC key , or
2Select Main Setup, Internal PC, then Show PC Window.
To hide the Desktop again, select Main Screen.
Adjusting the iPC Audio Volume
The Audio from the iPC is normally configured to be off. However, your monitor may have the iPC
audio configured on for use with specific PC applications.
WARNING
Always minimize the iPC audio volume or mute it completely when it is not needed for an iPC
application. This will avoid iPC tones distracting from or masking tones from the monitor.

1 Introduction
47
Using Input Devices with the iPC and Monitor
You can connect input devices such as a mouse, trackball and keyboard to the rear of the patient
monitor (using the left hand row of USB connectors) and use them for input to the monitor.
Correspondingly you can connect input devices to the rear of the patient monitor (using the right
hand row of USB connectors) or to the front USB connector and use them for the iPC. Input devices
connected to the iPC can also be shared with the patient monitor. Sharing input devices and
touchscreen input requires a specific software application; refer to the IntelliVue XDS Application
Instructions for Use for details.
If the iPC is switched off when input devices are shared, any input devices connected to it will not be
available for use with the monitor.
Shutting the iPC Down
The iPC will be shut down automatically when the monitor is switched off.
If you want to shut down the iPC when the monitor is on,
1Select Main Setup then Internal PC.
2In the Internal PC menu, select Switch PC Off.
If there is a problem with the shutdown, and you need to switch off the iPC manually,
1Select Main Setup then Internal PC.
2In the Internal PC menu, select Force PC Off to force the iPC to power down.
Special Situations at Shutdown
• If you switch the monitor off and then on again immediately, the iPC will continue running and
will not be shut down.
• In some situations, shutting down the iPC can take a little time. The monitor will go into Standby
mode until the shutdown is complete. By touching the touchscreen, you can bring the monitor
back into operating mode. If you do this, the iPC will restart when the shutdown is complete.
• If the shutdown cannot be completed within a certain time, a window will open giving the reason:
for example, that a file has not been saved, or that updates are being installed. You can then decide
whether to wait (for example, in the case of the updates) or to take action (for example by saving
the unsaved file). You will also have the option to force shutdown, if necessary.
Using the X2 or MP5 with a Host Monitor
When you connect an X2 or MP5 in companion mode to a host monitor, an integrated system is
formed for monitoring a single patient. The following general observations and considerations apply to
such a system:
• The host monitor is the "master" of the system, and you have full control over all the system's
operation only via the host monitor.
• Functions you can operate on a monitor in companion mode are restricted to measurements
originating in that device. If you try to operate controls that are disabled, you are prompted by the
message Not available in Companion Mode.

1Introduction
48
• Depending on how it is configured, your host monitor can determine whether the user interface of
a connected monitor in companion mode is completely disabled or not, and what is displayed on
the screen (a standard main screen, or a blank screen indicating Companion Mode).
This is controlled by two monitor settings that are applied to the monitor in companion mode on
connection. You can change the settings in Configuration Mode.
• Global settings such as line frequency, QRS sound and ECG lead colors from the host monitor,
are applied to the monitor in companion mode on connection. When disconnected from the host,
the monitor in companion mode re-applies its own global settings.
• No audible alarms are available on a monitor in companion mode when connected to a host
monitor. The only visual alarm indication is provided by the alarm lamps which are controlled by
the host monitor. Alarms become active again as soon as the monitor in companion mode is
disconnected from the host monitor.
• The host monitor is the master of all ADT information. ADT operations on the monitor in
companion mode are disabled, and any pending actions on the monitor in companion mode (for
example, admit or end case) are canceled.
• The date and time of the monitor in companion mode is synchronized with that of the host
monitor.
• Event surveillance in the monitor in companion mode is disabled. Main Setup menu operations
and SmartKeys are disabled. While connected to a host monitor, no new events are detected in the
monitor in companion mode, and no events are deleted. There is no transfer of stored events from
the monitor in companion mode to the host monitor. After disconnection from the host monitor,
event surveillance is enabled again in the monitor in companion mode, and new events are
detected.

2
49
2Alarms
The alarm information here applies to all measurements. Measurement-specific alarm information is
discussed in the sections on individual measurements.
The monitor has two different types of alarm: patient alarms and INOPs.
Patient Alarms
Patient Alarms are red and yellow alarms. A red alarm indicates a high priority patient alarm such as a
potentially life threatening situation (for example, asystole). A yellow alarm indicates a lower priority
patient alarm (for example, a respiration alarm limit violation). Additionally there are short yellow
alarms, most of which are specific to arrhythmia-related patient conditions (for example, ventricular
bigeminy).
INOPs
INOPs are technical alarms, they indicate that the monitor cannot measure or detect alarm conditions
reliably. If an INOP interrupts monitoring and alarm detection (for example, LEADS OFF), the monitor
places a question mark in place of the measurement numeric and an audible indicator tone will be
sounded. INOPs without this audible indicator indicate that there may be a problem with the reliability
of the data, but that monitoring is not interrupted.
Most INOPs are light blue, however there are a small number of INOPs which are always yellow or
red to indicate a severity corresponding to red and yellow alarms. The following INOPs can also be
configured as red or yellow INOPs to provide a severity indication:
•ECG LEADS OFF
•NBP CUFF OVERPRESS
•CUFF NOT DEFLATED
•OCCLUSION
•TELE DISCONNECTED
•Replace TeleBatt
All monitors in a unit should have the same severity configured for these INOPs.
Alarms are indicated after the alarm delay time. This is made up of the system delay time plus the
trigger delay time for the individual measurement. See the Specifications section for details.
If more than one alarm is active, the alarm messages are shown in the alarm status area in succession.
An arrow symbol next to the alarm message informs you that more than one message is active.
2 Alarms
50
The monitor sounds an audible indicator for the highest priority alarm. If more than one alarm
condition is active in the same measurement, the monitor announces the most severe. Your monitor
may be configured to increase alarm indicator volume automatically during the time when the alarm is
not acknowledged.
Visual Alarm Indicators
WARNING
• No alarms are available on an X2 or MP5 when connected to a host monitor (Companion Mode
is indicated). Alarms become active again as soon as the X2 or MP5 is disconnected from the host
monitor.
• Alarm fields and other visual alarm indicators are disabled on an X2 or MP5 when connected to a
host monitor. The only visual alarm indication is provided by the alarm lamps, which are
controlled by the host monitor.
Alarm Message
An alarm message text appears in the alarm status area at the top of the screen indicating the source of
the alarm. If more than one measurement is in an alarm condition, the message changes every two
seconds, and has an arrow ( ) at the side. The background color of the alarm message matches the
alarm priority: red for red alarms, yellow for yellow alarms, light blue for standard INOPs, red for red
INOPs and yellow for yellow INOPs. The asterisk symbols (*) beside the alarm message match the
alarm priority: *** for red alarms, ** for yellow alarms, * for short yellow alarms. Standard INOPs do
not have a symbol, red and yellow INOPs have exclamation marks beside the alarm message: !!! for
red INOPs and !! for yellow INOPs.
Depending on how your monitor is configured, it may display alarm limit violation messages:
• in text form, for example ** SpO₂ LOW or
• in numeric form, for example **Pulse xxx>yyy where the first number shows the maximum
deviation from the alarm limit, and the second number shows the currently set limit.
Flashing Numeric
The numeric of the measurement in alarm flashes.
Bright Alarm Limits
If the alarm was triggered by an alarm limit violation, the corresponding alarm limit on the monitor
screen is shown more brightly if Show ALarmLimits is enabled and there is sufficient room on the
screen.
Alarm Lamp
A lamp on the monitor's front panel flashes. The alarm lamp is divided into two sections. The right
one flashes for a patient alarm, except for short yellow alarms where the lamp will light for
approximately six seconds. The color is yellow or red corresponding to the highest priority patient
alarm currently present. The left one lights continuously for a light blue INOP and flashes for yellow
or red INOPs as follows:
2 Alarms
51
If only patient alarms are present, and no INOPs, the patient alarms will use both left and right
sections to flash (for red and yellow alarms) or light for approximately six seconds (for short yellow
alarms). If only INOPs are present, and no patient alarms, red and yellow INOPs will use both left and
right sections to flash but light blue INOPs will always light continuously in the left section only.
Nurse Call Systems
If configured to do so, red, yellow and light blue alarms are indicated on any device connected to the
nurse call relay.
Audible Alarm Indicators
The audible alarm indicators configured for your monitor depend on which alarm standard applies in
your hospital. Audible alarm indicator patterns are repeated until you acknowledge the alarm by
switching it off or pausing it, or until the alarm condition ceases (if audible alarm indication is set to
non-latching).
WARNING
• Do not rely exclusively on the audible alarm system for patient monitoring. Adjustment of alarm
volume to a low level or off during patient monitoring may result in patient danger. Remember
that the most reliable method of patient monitoring combines close personal surveillance with
correct operation of monitoring equipment.
• No audible alarm indicators are available on an X2 or MP5 when connected to a host monitor
(Companion Mode is indicated). Alarms become active again as soon as the X2 or MP5 is
disconnected from the host monitor.
Alarm Tone Configuration
The audible alarm indicators of your monitor are configurable. In the monitor's Configuration Mode,
you can:
• increase the alarm volume of unacknowledged alarms at regular intervals
• change the interval between alarm sounds (ISO/IEC Standard alarms only)
• change the base volume of the red and yellow alarm tones and the INOP tones
• change the alarm sound to suit the different alarm standards valid in different countries.
Traditional Audible Alarms (HP/Agilent/Philips/Carenet)
• Red alarms and red INOPs: A high pitched sound is repeated once a second.
• Two-star yellow alarms and yellow INOPs: A lower pitched sound is repeated every two seconds.
• One-star yellow alarms (short yellow alarms): The audible indicator is the same as for yellow
alarms, but of shorter duration.
INOP Lamp Color On Off
Yellow 1.0 seconds 1.0 seconds
Red 0.25 seconds 0.25 seconds
2 Alarms
52
• Standard INOPs: an INOP tone is repeated every two seconds.
ISO/IEC Standard Audible Alarms
• Red alarms and red INOPs: A high pitched tone is repeated five times, followed by a configurable
pause.
• Two-star yellow alarms and yellow INOPs: A lower pitched tone is repeated three times, followed
by a configurable pause.
• One-star yellow alarms (short yellow alarms): The audible indicator is the same as for yellow
alarms, but of shorter duration.
• Standard INOPs: a lower pitched tone is repeated twice, followed by a pause.
Changing the Alarm Tone Volume
• The alarm volume symbol at the top right of the monitor screen gives you an indication of the
current volume.
To change the volume, select the volume symbol and then select the required volume from the
pop-up selection.
• If you want to see a numerical indication of the current alarm volume on a scale from zero to 10,
or change the setting, select the Alarm Volume SmartKey.
The volume scale pops up. The current setting is indented. To change the setting, select the
required number on the scale. Any settings that are inactive ("grayed out") have been disabled in
the monitor's Configuration Mode.
• When the alarm volume is set to zero (off), the alarm volume symbol reflects this.
If you switch the alarm volume off, you will not get any audible indication of alarm conditions.
There is no alarm volume indication on the screen of an X2 or MP5 when connected to a host monitor
(Companion Mode is indicated).
Minimum Volume for No Central Monitoring INOP
If your monitor is connected to an Information Center, and the connection is interrupted, the INOP
message No Central Monit. will appear within 30 seconds, accompanied by an INOP tone. To help
ensure that this INOP, and any other active alarm, is not overlooked, the INOP and alarm tones may
be configured to have a minimum volume. In this case, INOP and alarm tones will sound even if the
monitor alarm volume is set to zero.
Minimum Volume for Severe Yellow or Red INOPs
Severe yellow or red INOPs require action to ensure the well-being of the patient. Therefore the
minimum volume for the INOP tone is set to at least alarm volume 8, irrespective of the current alarm
volume setting. The INOP tone will sound even if the monitor alarm volume is set to zero.
2 Alarms
53
The severe INOPs for which this applies are:
CUFF NOT DEFLATED (configurable to yellow or red)
NBP CUFF OVERPRESS (configurable to yellow or red)
!!INSERT BATTERY - X2 (yellow)
Power Loss Tone
When power is lost - no power is available via the power cable - a buzzer will sound, if so configured.
The tone can be silenced by pressing the On/Off power switch.
Acknowledging Alarms
To acknowledge all active alarms and INOPs, select the Silence permanent key. This switches off the
audible alarm indicators and alarm lamps.
Alternatively, you can acknowledge alarms by pressing the Silence hardkey on the MMS or on the
SpeedPoint. The hardkeys follow the behavior configured for the permanent key.
A check mark beside the alarm message indicates that the alarm has been acknowledged . If the
monitor is configured to re-alarm, a dashed check mark will be shown .
If the condition that triggered the alarm is still present after the alarm has been acknowledged, the
alarm message stays on the screen with a check mark symbol beside it, except for NBP alarms and
alarms from other intermittent measurements. When such an alarm is acknowledged the alarm
message disappears.
If the alarm condition is no longer present, all alarm indicators stop and the alarm is reset.
Switching off the alarms for the measurement in alarm, or switching off the measurement itself, also
stops alarm indication.
Acknowledging Disconnect INOPs
Acknowledging an INOP that results from a disconnected transducer switches off the associated
measurement, unless the monitor is configured to not allow this. The only exception is ECG/Resp:
acknowledging a disconnect INOP for ECG leads does not switch off the ECG and Resp
measurements. Acknowledging a disconnect INOP at the Information Center switches off the audible
INOP indicator but does not switch off the measurement.
Unplugging an MMS or a plug-in module automatically switches off its measurements.
2 Alarms
54
Alarm Reminder
If Alarm Reminder is configured on for your monitor, you will get an audible reminder of alarm
conditions that remain active after you have acknowledged the alarm. This reminder may take the form
of a repetition of the alarm tone for a limited time, or an unlimited repetition of the alarm tone (this is
the same as a new alarm). Alarm Reminder is not available for standard, light blue INOPs but for
yellow and red INOPs.
In Configuration Mode, you can set the interval between silencing the alarm and sounding the
reminder tone to one, two, or three minutes.
The alarm reminder behavior at the Information Center is different to that at the monitor. Refer to the
Information Center Instructions for Use for further information.
Pausing or Switching Off Alarms
If you want to temporarily prevent alarms from sounding, for example while you are moving a patient,
you can pause alarms. Depending on your monitor configuration, alarms are paused for one, two, or
three minutes, or infinitely.
To view the alarm pause setting chosen for your unit,
1Select Main Setup, Alarms, then Alarm Settings
2Check the Alarms Off setting.
This setting can only be changed in Configuration Mode.
To Pause All Alarms
• Select the Pause Alarms permanent key. If your monitor is configured to infinite pause time, the
permanent key is labeled Alarms Off, and selecting it switches alarms off.
• Or press the Alarms hardkey on the SpeedPoint or Navigation Point. The hardkey follows the
behavior configured for the permanent key.
Depending on the configuration, you may need to select Confirm to complete the change.
To Switch All Alarms Off
You can only switch alarms off permanently if your monitor is configured to allow infinite alarms
pause and the permanent key is labeled Alarms Off.
• Select the Alarms Off permanent key.
• Or press the Alarms hardkey on the SpeedPoint or Navigation Point. The hardkey follows the
behavior configured for the permanent key.
Depending on the configuration, you may need to select Confirm to complete the change.
Pausing alarms infinitely is the same as switching them off.
2 Alarms
55
To Switch Individual Measurement Alarms On or Off
1Select the measurement numeric to enter its setup menu.
2Select Alarms to switch between on and off.
The alarms off symbol is shown beside the measurement numeric.
While Alarms are Paused or Off
• The red Alarms Paused lamp on the monitor front panel is lit.
In the alarm field, the monitor displays the message ALARMS PAUSED 1:28 or ALARMS OFF,
together with the alarms paused symbol or the alarms off symbol.
• No alarms are sounded and no alarm messages are shown.
• INOP messages are shown but no INOP tones are sounded.
The only exceptions are the INOPs CUFF NOT DEFLATED, NBP CUFF OVERPRESS and INOPs
relating to empty, missing and malfunctioning batteries.
These INOPs switch the alarms on, and the INOP tones are sounded, even if alarms are paused or
off. You need to remove the INOP condition first before you can switch the alarm tones off again.
• The nurse call relay is not active.
If a disconnect INOP is present and alarms are paused or switched off, the measurement in question
may be switched off, depending on monitor configuration.
Restarting Paused Alarms
To manually switch on alarm indication again after a pause, select the permanent key Pause Alarms (or
Alarms Off) again.
Alarm indication starts again automatically after the pause period expires. If the monitor is configured
to stay paused infinitely, you must select Alarms Off again to restart alarm indication.
Resetting Arrhythmia Alarm Timeouts
To reset the arrhythmia alarm timeout period, select the Alarms Off or Pause Alarms permanent key
and then reselect it.
Extending the Alarm Pause Time
If your monitor has extended alarm pause enabled, you can extend the alarm pause time. Use this to
prevent alarms being indicated, for example, while you are washing a patient or carrying out a
procedure. Only extend the alarm pause time when you are sure that clinical personnel are available to
monitor the patient's condition closely.
Alarms Paused Alarms Off
2 Alarms
56
To extend the alarm pause time to five or 10 minutes,
1Select one of the alarm fields. This calls up the Alarm Messages window.
2Select either the pop-up key PauseAl. 5 Min or the pop-up key PauseAl. 10 Min. Each time you
select one of these pop-up keys, the Alarm Pause Time is reset to five (or 10) minutes.
Alarm Limits
The alarm limits you set determine the conditions that trigger yellow and red limit alarms. For some
measurements (for example, BIS and SpO2), where the value ranges from 100 to 0, setting the high
alarm limit to 100 switches the high alarm off, or setting the low alarm limit to 0 switches it off. In
these cases, the alarms off symbol is not displayed.
WARNING
Be aware that the monitors in your care area may each have different alarm settings, to suit different
patients. Always check that the alarm settings are appropriate for your patient before you start
monitoring.
Viewing Individual Alarm Limits
You can usually see the alarm limits set for each measurement next to the measurement numeric on
the main screen.
If your monitor is not configured to show the alarm limits next to the numeric, you can see them in the
appropriate measurement setup menu. Select the measurement numeric to enter the menu and check
the limits.
Viewing All Alarm Limits
The Alarm Limits overview window lists the currently set alarm limits for all measurements. If an
Apnea alarm delay time is set, this is also shown. The alarms off symbol is shown beside the
measurement label of any measurement whose alarm switched off.
To open the Alarm Limits window, either select any alarm field to open the Alarm Messages window,
then select the Alarm Limits pop-up key, or select the Alarm Limits SmartKey, if configured.
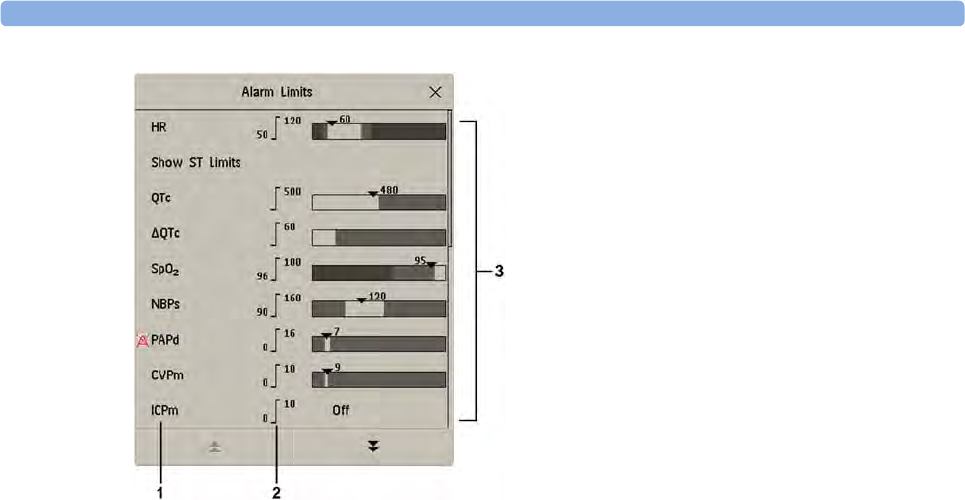
2 Alarms
57
1Measurement labels, with alarms off symbol where appropriate
2Current alarm limits
3Graphic view of current yellow and red alarm limits and currently monitored measurement value.
Off indicates the measurement is switched off
•Select
Show ST Limits to expand the list of ST leads and view the currently set alarm limits.
Selecting Hide ST Limits hides the list again.
You can use the pop-up keys that open with the Alarm Limits window to perform common tasks:
–All Al. On/All Al. Off
–All Lim. Narrow/All Lim. Wide to set narrow or wide alarm AutoLimits for all measurements.
–Print Limits/Record Limits to print a list of all current alarm limit settings on a connected
printer or recorder.
These pop-up keys are not available in the window for changing individual alarm limits which you
access by selecting the measurement label in the Alarm Limits window.
Changing Alarm Limits
To change individual measurement alarm limits using the measurement's Setup Menu,
1In the measurement's setup menu, select the alarm limit you want to change. This calls up a list of
available values for the alarm limit.
2Select a value from the list to adjust the alarm limit.
Alternatively, you can use the keys in the measurement alarm limits window, which you access by
selecting the measurement label in the Alarm Limits window.
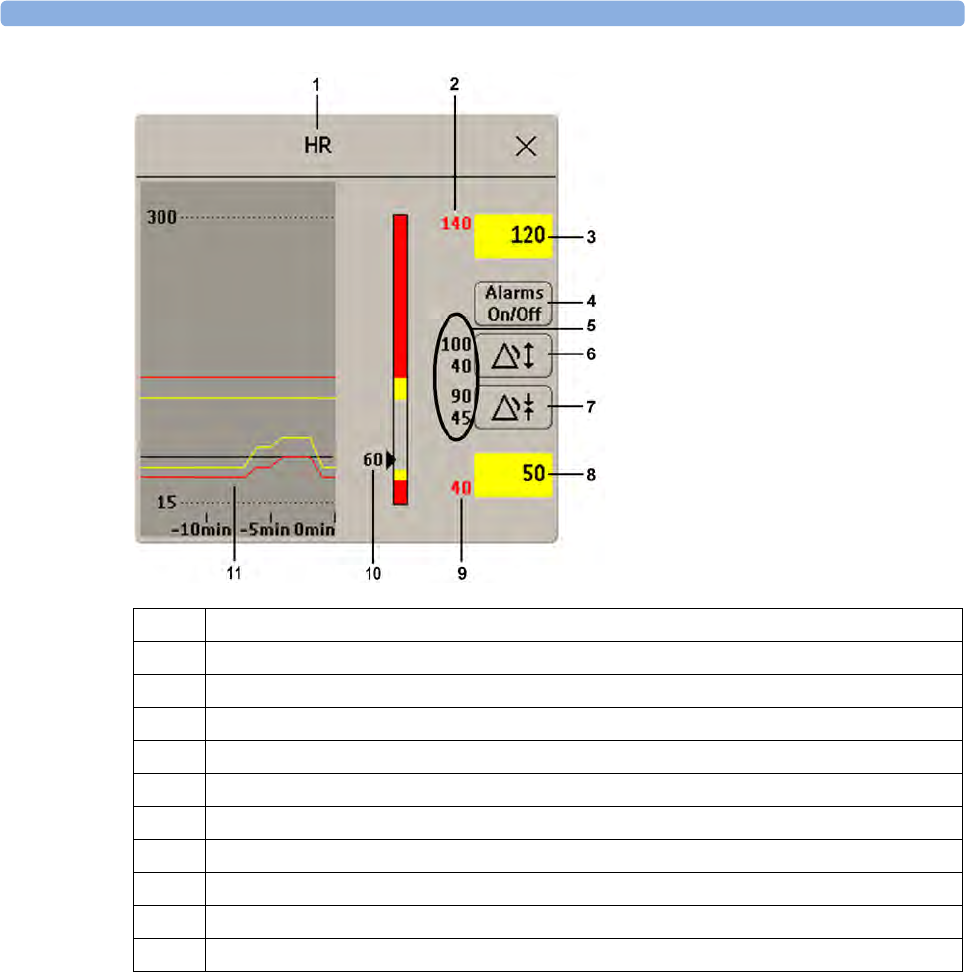
2 Alarms
58
T
To change alarm limits,
1Enter the Alarm Limits window.
2Using touch: to set the high alarm limit, select the high yellow alarm field to open a pop-up list of
high alarm limits. Select a limit from the list. Repeat to set the low yellow alarm field.
Using a SpeedPoint or Navigation Point: position the cursor in the high yellow alarm field,
then press the knob inwards. Rotate the knob to the left or right to adjust the limit. Press the knob
again to set the displayed limit. Repeat to set the low yellow alarm limit.
If you set the yellow alarm limit outside the red alarm limit, the monitor will automatically adapt the
red alarm limit.
When an ST measurement is in the alarm limits window there are also two pop-up keys available
labeled All ST Narrow/All ST Wide. With these keys you can set Auto Limits for all ST Leads.
1Parameter label
2High red alarm (view only)
3High yellow alarm field. Select to open a pop-up list of high alarm limits
4Alarms On/Off key - select to switch between alarms on or off
5Preview Alarm AutoLimits for a measurement before applying
6Select to apply wide AutoLimits
7Select to apply narrow AutoLimits
8Low yellow alarm field. Select to open a pop-up list of low alarm limits
9Low red alarm (view only)
10 Graphic view of alarm limits with currently measured value
11 15-min trend, showing alarm limits and monitored measurement values
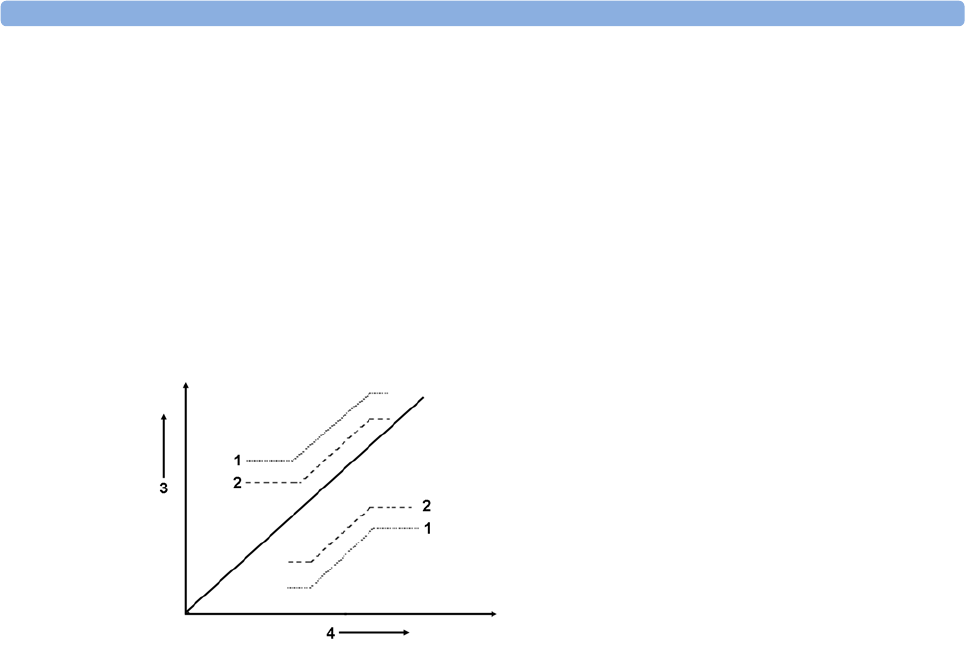
2 Alarms
59
About Automatic Alarm Limits
The monitor can automatically set alarm limits suited to your individual patient, using the Automatic
Alarm Limits function (AutoLimits). This tells the monitor to adapt the alarm limits of selected
measurements to the measured vital signs within a defined safe limit. The monitor calculates safe
AutoLimits for each patient based on the measured values from the last 12 seconds.
The wide and narrow limits have a fixed relationship to the measured value within the non-
pathological range. Outside of this range, no auto limits are calculated. To set values outside of the
non-pathological range, limits must be changed manually, based on the clinician's judgment about the
specific patient.
Limits Narrow sets limits close to the currently measured values for situations where it is critical for
you to be informed about small changes in your patient's vital signs.
Limits Wide sets limits further away from the currently measured values for situations where small
changes are not so critical.
Use the keys in the measurement alarm limits window to apply AutoLimits for individual
measurements. These keys are not available if AutoLimits have been disabled for the measurement in
the monitor's Configuration Mode.
AutoLimits are not available for all measurements. The list of measurements for which AutoLimits can
be used is defined in the monitor's Configuration mode.
Use the measurement alarm limits window to check AutoLimits before you apply them to ensure that
they are appropriate for your individual patient and their clinical condition. Once applied, AutoLimits
are shown on the monitor screen just like manually-set alarm limits. If the AutoLimits are not
appropriate for your patient, you must set alarm limits manually. The limits remain unchanged until
you set them again or change them manually.
About Smart Alarm Delays
The monitor can be configured to apply a delay before announcing limit alarms. The delay is calculated
using an intelligent algorithm. This capability can be used to suppress alarms which occur because a
limit is exceeded for a short time or by a small amount. Currently, Smart Alarm Delays are available
only for SpO2 limit alarms and are not available in the U.S.A. or in clinical environments under FDA
control. See the Monitoring SpO2 chapter for details.
1Wide alarm limits
2Narrow alarm limits
3Alarm Limits
4Measurement value
2 Alarms
60
WARNING
Before using Smart Alarm Delays, make sure that you fully understand how the delay is applied and
what the consequences are.
Documenting Alarm Limits
The alarm limits pop-up keys appear with the Alarm Limits and measurement alarm limits windows.
• Select the Print Limits pop-up key to print an overview of all alarm limits on a connected printer.
• Select the Record Limits pop-up key to send a recording of the alarm limits to a recorder.
Reviewing Alarms
You can see which alarms and INOPs are currently active in the respective alarms and INOPs fields at
the top of the screen.
To see the currently active alarms and INOPs listed in one place, select any of the alarm status areas on
the monitor screen. The Alarm Messages window pops up.
All alarms and INOPs are erased from the Alarm Messages window when you discharge a patient, or
if you change to Demonstration Mode.
Alarm Messages Window
The Alarm Messages window shows all the currently active alarms and INOPs sorted by priority,
beginning at the top with the most recent. INOPs are shown on the left hand side and patient alarms
are shown on the right hand side. Any active red alarms are shown first, followed by yellow alarms.
Acknowledged alarms or INOPs are shown with the check mark symbol.
The Alarm Messages window pop-up keys appear when the window is opened. If alarm pause
extension is disabled, the pause pop-up keys are inactive ("grayed-out"). Selecting the Review Alarms
pop-up key opens the Review Alarms window.
If you do not immediately understand an INOP or alarm message, refer to its help text.
•In the Alarm Messages window, select the INOP message. This calls up a help window with an
explanation of the INOP message and, where appropriate, a suggested solution for the problem.
• If the alarm or INOP was generated in a device other than the monitor (for instance, in an MMS
or FMS), this source is specified at the end of the help text.
Review Alarms Window
The Review Alarms window contains a list of the most recent alarms and INOPs with date and time
information.
If configured to do so, each alarm is shown with the alarm limit active when the alarm was triggered
and the maximum value measured beyond this limit. The Review Alarms window also shows when the
monitor was switched on (after being switched off for longer than 1 minute) and any actions related to
switching alarms on and off, entering or leaving Standby mode, silencing alarms or changing the ECG
source.
2 Alarms
61
When you select an item from the list, you can get additional information about that item. If you select
a high or low limit alarm in the list, the Graphical Trends window will open to provide further data. If
you select an alarm resulting from an event alarm notification, the Event Episode window for that
event will open. If you select an alert other than a high or low alarm, a help text window opens with
more information. This is the same as the help text window that opens in the Alarm Messages
window. Some items in the list are simply log items not related to a patient alert as such (for example,
Alarms On or Alarms Off). You cannot see any further information if you select one of these items.
When you close these windows you will return to the Review Alarms window.
The information in the Review Alarms window is deleted when a patient is discharged, and when you
leave Demonstration Mode.
The Review Alarms window pop-up keys appear when the window is opened. If alarm pause
extension is disabled, the pause pop-up keys are inactive. Selecting the Active Alarms pop-up key
opens the Alarm Messages window.
Latching Alarms
The alarm latching setting for your monitor defines how the alarm indicators behave when you do not
acknowledge them. When alarms are set to non-latching, their indicators end when the alarm condition
ends. Switching alarm latching on means that visual and/or audible alarm indications are still displayed
or announced by the monitor after the alarm condition ends. The indication lasts until you
acknowledge the alarm.
Viewing the Alarm Latching Settings
To see the alarm latching setting for your monitor
1In the monitor's Main Setup menu, select Alarms.
2Select Alarm Settings, and see the Visual Latching and Audible Latching settings.
This setting can only be changed in Configuration Mode. You should be aware of the settings chosen
for your unit. There are three possible choices each for visual and audible latching, red, red and yellow,
and off. These choices can be combined to give the following settings:
Visual Latching Audible Latching
Red&Yellow Red&Yellow
Red&Yellow Red Only
Red&Yellow Off
Red Only Red Only
Red Only Off
Off Off
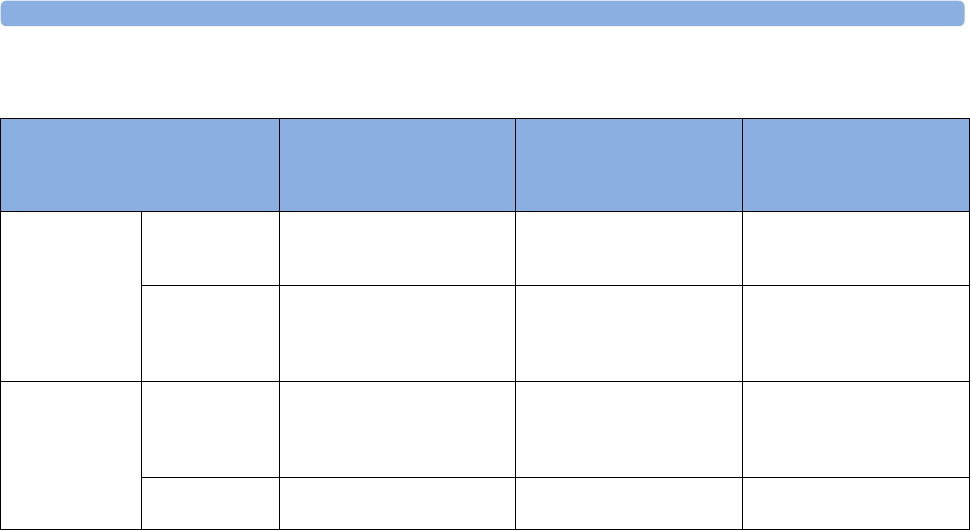
2 Alarms
62
Alarm Latching Behavior
All INOPs are non-latching. See “Yellow Arrhythmia Alarms” on page 136 for information on one-
star yellow alarms latching behavior.
Testing Alarms
When you switch the monitor on, a selftest is started. You must check that the alarms lamps light, one
after the other, and that you hear a single tone. This indicates that the visible and audible alarm
indicators are functioning correctly. For further testing of individual measurement alarms, perform the
measurement on yourself (for example SpO2 or CO2) or use a simulator. Adjust alarm limits and check
that appropriate alarm behavior is observed.
Alarm Behavior at Power On
If the monitor is switched off for longer than one minute and then switched on again (or after a loss of
power lasting longer than one minute, or when a patient is discharged), the monitor can be configured
to:
• restore the alarm settings from the monitor's configured default Profile,
• restore the most recently used alarm settings, or
• switch the alarms off.
After any of these situations, you should check that the alarm settings are appropriate for your patient
and monitoring situation, and if necessary, select the correct Profile and patient category.
If power is lost for less than one minute, the alarm on/off condition prior to the power loss is
restored.
Red & Yellow Measurement
Alarms
Non-latching alarms Visual and audible latching Visual latching, audible
non-latching
Alarm has not
been
acknowledged.
Alarm condition
still present.
Alarm tone on. Alarm lamp on.
Alarm message. Flashing
numerics.
Alarm tone on. Alarm lamp
on. Alarm message. Flashing
numerics.
Alarm tone on. Alarm lamp
on. Alarm message. Flashing
numerics.
Alarm condition
no longer present.
All audible and visual alarm
indicators automatically stop.
Alarm tone on.
Alarm lamp on.
Alarm message.
Flashing numerics.
Alarm message. Flashing
numerics.
Audible alarm indicators
automatically stop.
Alarm has been
acknowledged.
Alarm condition
still present.
Alarm tone off. Alarm lamp off.
Alarm message. Flashing
numerics. Audible alarm
reminder (if configured).
Alarm tone off. Alarm lamp
off. Alarm message. Flashing
numerics. Audible alarm
reminder (if configured).
Alarm tone off. Alarm lamp
off. Alarm message. Flashing
numerics. Audible alarm
reminder (if configured).
Alarm condition
no longer present.
Audible and visual alarm
indicators automatically stop.
Audible and visual alarm
indicators automatically stop.
Audible and visual alarm
indicators automatically stop.

2 Alarms
63
Alarm Recordings
You can set up your monitor so that it automatically triggers alarm recordings at the Information
Center, or if configured, to a printer as a realtime report.
1Press the Main Setup SmartKey.
2Select Alarms from the Main Setup menu.
3Select Alarm Recording from the Alarms menu to open the Alarm Recordings menu.
4Select a measurement from those listed for which you want to change the alarm condition that
triggers an alarm recording. This opens a pop-up list.
5For the desired measurement(s), choose the alarm condition to trigger an alarm recording:
Red Only: an alarm recording will automatically be triggered when the measurement enters a red
alarm condition.
Red&Yellow: both yellow and red alarms will trigger an alarm recording.
Off: disables automatic alarm recording.
Refer to the Recording chapter for details of how to set up a recording.

2 Alarms
64

3
65
3Patient Alarms and INOPs
This chapter lists patient alarms alphabetically, and technical alarms (INOPs) arranged by the source of
the INOP and then alphabetically, irrespective of their priority. All alarms and INOPs are listed here;
the ones which can appear on your monitor will depend on the model and the individual options.
For information on alarms and INOPs from the gas modules refer to your Gas Module Instructions
for Use.
Patient Alarm Messages
The measurement labels and abbreviations for pressure, temperature, SpO2, and anesthetic agent
alarms are explained in the individual chapters.
Some alarms may be shown at the Information Center in shortened form, when transferred through
IntelliVue Instrument Telemetry. These shortened alarm texts are included in the list and identified
with the note "at Information Center".
Note that yellow arrhythmia alarms may be shown with one or with two stars, depending on your
monitor configuration and the Information Center revision you are using.
Refer to your IntelliBridge Device Driver Instructions for Use for patient alarms from connected
external devices.
Refer to your Gas Module Instructions for Use for patient alarms and INOPs from the gas modules.
Alarm Message From Condition Indication
* AFIB
** AFIB
ECG/Arrhythmia Atrial fibrillation waveform detected yellow alarm lamp, short yellow
audible alarm
*** APNEA
*** APNEA x:yy
*** APNEA >10min
CO2, Resp,
Spirometry
Respiration has stopped for longer than the
preset apnea time. "x:yy" denotes the Apnea
duration in minutes and seconds
numeric flashes, red alarm lamp,
alarm tone
*** ASYSTOLE ECG No QRS detected for a period greater than the
asystole threshold (in the absence of Vfib or
chaotic ECG)
numeric flashes, red alarm lamp,
alarm tone
** awRR HIGH CO2, Resp, AGM The airway respiration rate has exceeded the
high alarm limit.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** awRR LOW CO2, Resp, AGM The airway respiration rate has dropped below
the low alarm limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
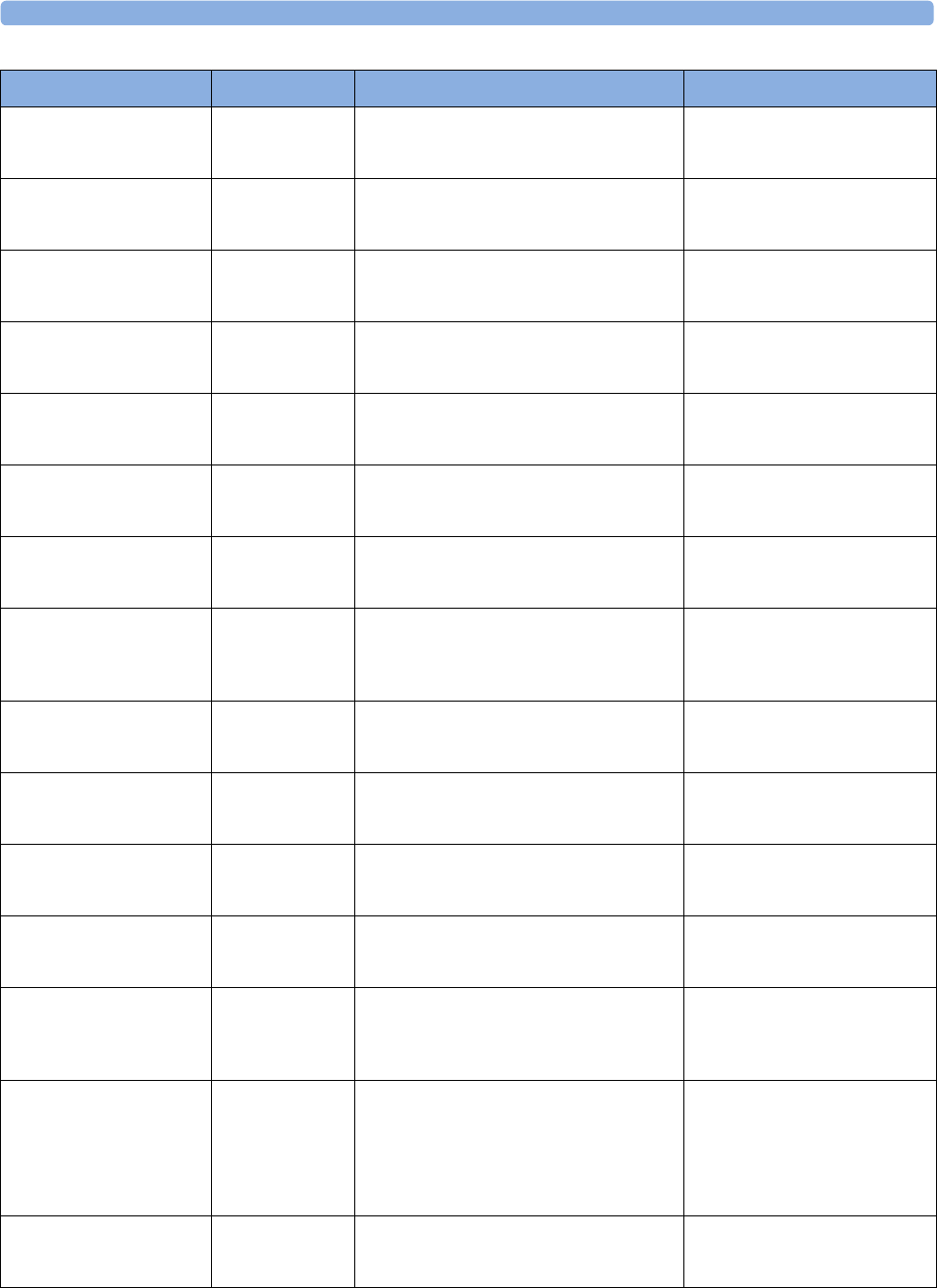
3 Patient Alarms and INOPs
66
** BIS HIGH BIS The Bispectral Index value has exceeded the
high alarm limit.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** BIS LOW BIS The Bispectral Index value has dropped below
the low alarm limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
** CCO HIGH
** CCI HIGH
CCO Continuous Cardiac Output or CC Index is
above the high alarm limit.
numeric flashes and high alarm
limit is highlighted, yellow alarm
lamp, alarm tone
** CCO LOW
** CCI LOW
CCO Continuous Cardiac Output or CC Index is
below the low alarm limit.
numeric flashes and low alarm limit
is highlighted, yellow alarm lamp,
alarm tone
** CPP HIGH CPP The CPP value has exceeded the high alarm
limit.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** CPP LOW CPP The CPP value has fallen below the low alarm
limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
*** DESAT
*** DESAT xx < yy
SpO2The SpO2 value has fallen below the
desaturation alarm limit. xx denotes the lowest
measured value, and yy is the desaturation limit.
numeric flashes, red alarm lamp,
alarm tone
** EC10 ALARM
*** EC10 ALARM
at Information Center
EC10 Intellibridge A yellow (**) or red (***) patient alarm is
present on the IntelliBridge module. Check the
monitor display for more detailed alarm
information.
(on monitor) yellow or red alarm
lamp; the alarm text is defined by
the Intellibridge device driver
** etCO₂ HIGH CO2, Resp, AGM The end tidal CO2 high alarm limit has been
exceeded.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** etCO₂ LOW CO2, Resp, AGM The end tidal CO2 value has fallen below the
low alarm limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
** etO₂ HIGH O2, AGM The end tidal O2 high alarm limit has been
exceeded.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** etO₂ LOW O2, AGM The end tidal O2 value has fallen below the low
alarm limit.
numeric flashes, and low limit is
highlighted, yellow alarm lamp,
alarm tone
* EVENT
** EVENT
*** EVENT
at Information center
Event surveillance An event has occurred and the event
notification is configured to alarm. Check on
the monitor for more details on event group.
(on monitor) event group name
flashes, yellow or red alarm lamp
and alarm tone
* EVENT:<Event
Group>
** EVENT:<Event
Group>
*** EVENT:<Event
Group>
Event surveillance An event has occurred and the event
notification is configured to alarm.
event group name flashes, yellow or
red alarm lamp and alarm tone
*** EXTREME BRADY ECG The bradycardia limit has been exceeded. numeric flashes and alarm limit is
highlighted, red alarm lamp, alarm
tone
Alarm Message From Condition Indication
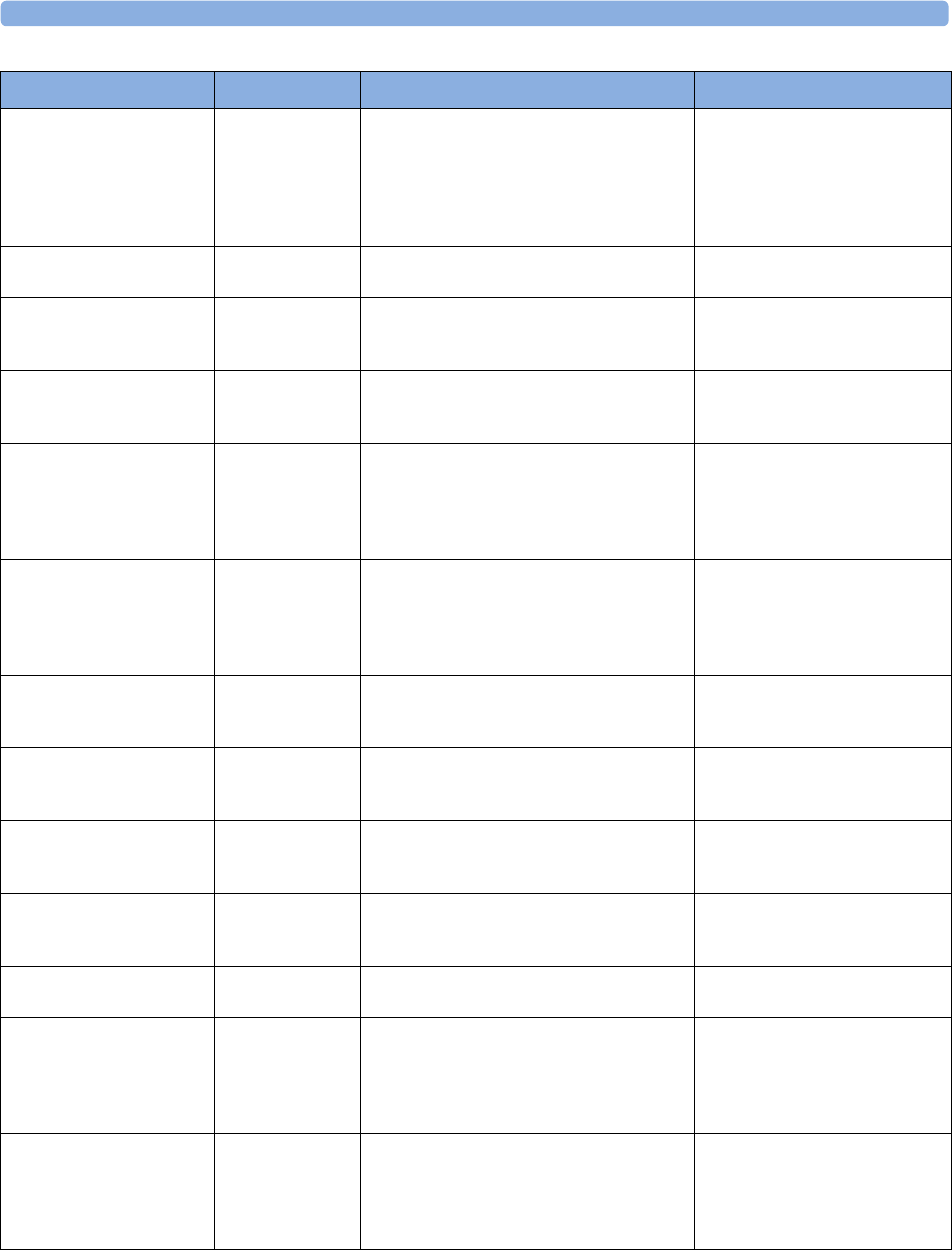
3 Patient Alarms and INOPs
67
** HR LOW ECG The heart rate has fallen below the low alarm
limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone. If configured to short
yellow, the sound switches off after
5 seconds if Arrhythmia is switched
on.
* IRREGULAR HR
** IRREGULAR HR
ECG/Arrhythmia Consistently irregular heart rhythm. numeric flashes, yellow alarm lamp,
short yellow audible alarm
* MISSED BEAT
** MISSED BEAT
ECG/Arrhythmia No beat detected for 1.75*R-R interval, or if
HR>120bpm no beat detected for one second
(non-paced patients only).
numeric flashes, yellow alarm lamp,
short yellow audible alarm
* MULTIFORM PVCs
** MULTIFORM PVCs
ECG/Arrhythmia Two differently shaped Vs detected, each
occurring at least twice within the last 300 beats
and at least once within the last 60 beats.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
** NBP HIGH NBP The measured NBP value is above the high
alarm limit.
s, d, or m after the label indicates whether the
systolic, diastolic or mean pressure has crossed
the limit.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** NBP LOW NBP The measured NBP value is below the low
alarm limit.
s, d, or m after the label indicates whether the
systolic, diastolic or mean pressure has crossed
the limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
* NON-SUSTAIN VT
** NON-SUSTAIN VT
ECG/Arrhythmia A run of Vs having a ventricular HR>V-Tach
HR limit, but lasting for less than the V-Tach
Run limit has been detected.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
* PACER NOT CAPT
** PACER NOT CAPT
ECG/Arrhythmia
(paced patients
only)
A missed beat with a pace pulse was detected. numeric flashes, yellow alarm lamp,
short yellow audible alarm
* PACER NT PACING
** PACER NT PACING
ECG/Arrhythmia
(paced patients
only)
A missed beat without a pace pulse was
detected.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
* PAIR PVCs
** PAIR PVCs
ECG/Arrhythmia A non-ventricular contraction, followed by two
ventricular contractions, followed by a non-
ventricular contraction has been detected.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
* PAUSE
** PAUSE
ECG/Arrhythmia No beat detected for a period greater than the
pause threshold.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
*** <Press Label> HIGH PRESS The measured pressure value is above the
extreme high alarm limit.
s, d, or m after the label indicates whether the
systolic, diastolic or mean pressure has crossed
the limit.
numeric flashes, high limit is
highlighted, red alarm lamp, alarm
tone
** <Press Label> HIGH PRESS The measured pressure value is above the high
alarm limit.
s, d, or m after the label indicates whether the
systolic, diastolic or mean pressure has crossed
the limit.
numeric flashes, high limit is
highlighted, yellow alarm lamp,
alarm tone
Alarm Message From Condition Indication
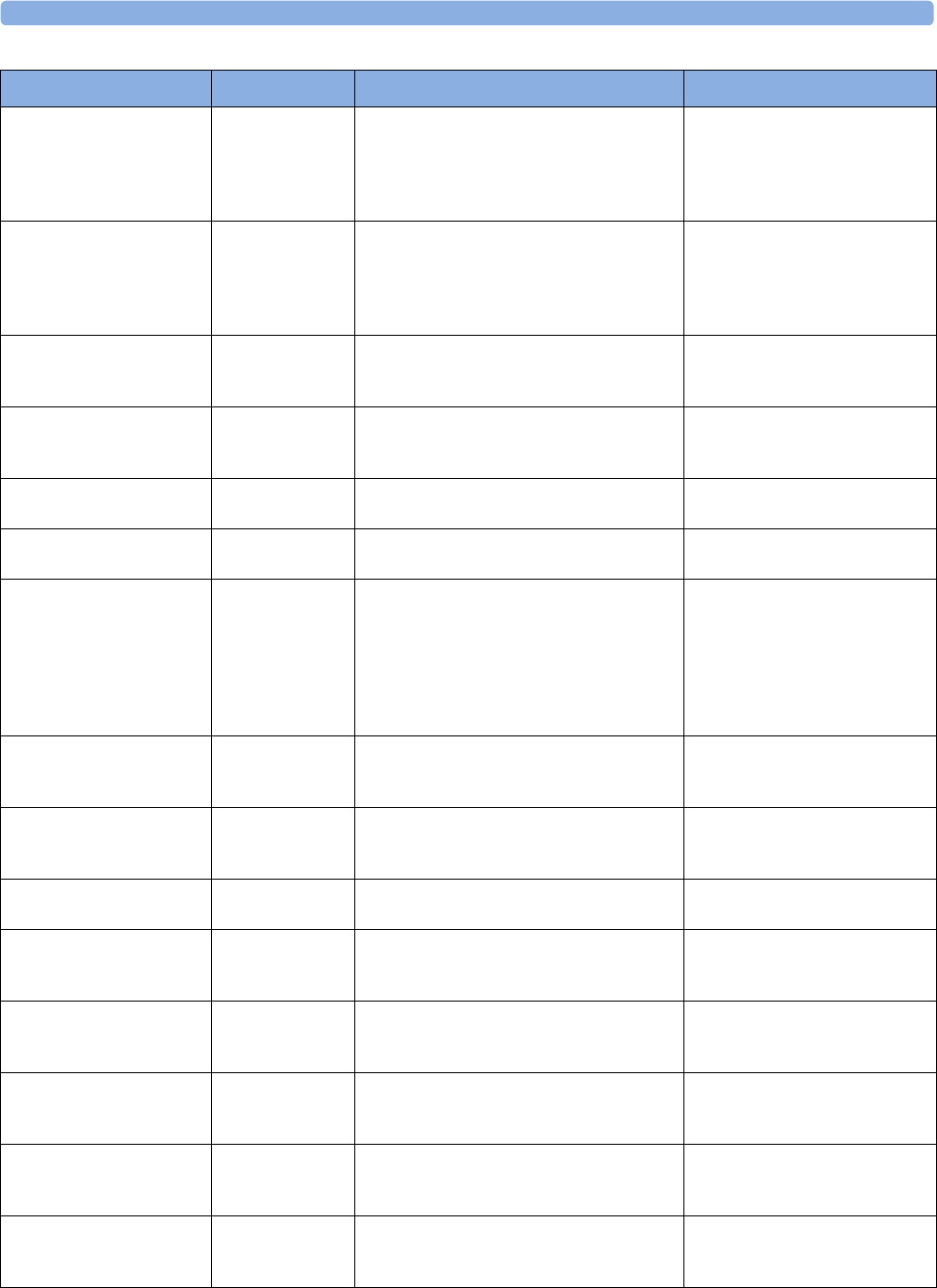
3 Patient Alarms and INOPs
68
*** <Press Label> LOW PRESS The measured pressure value is below the
extreme low alarm limit.
s, d, or m after the label indicates whether the
systolic, diastolic or mean pressure has crossed
the limit.
numeric flashes and low limit is
highlighted, red alarm lamp, alarm
tone
** <Press Label> LOW PRESS The measured pressure value is below the low
alarm limit.
s, d, or m after the label indicates whether the
systolic, diastolic or mean pressure has crossed
the limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
** Pulse HIGH PRESS, SpO2The pulse rate has exceeded the high alarm
limit.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** Pulse LOW PRESS, SpO2The pulse rate has dropped below the low
alarm limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
* PVCs/min HIGH
** PVCs/min HIGH
ECG/Arrhythmia More premature ventricular contractions have
been detected in a minute than the limit.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
** QTc HIGH ECG/QT QTc value has exceeded the QTc high limit for
more than 5 minutes
numeric flashes, yellow alarm lamp,
alarm tone
* R-ON-T PVCs
** R-ON-T PVCs
ECG/Arrhythmia For HR <100, a PVC with R-R interval < 1/3
the average interval followed by a
compensatory pause of 1.25 x average R-R
interval or two such Vs without compensatory
pause occurring within 5 minutes of each other.
(When HR >100, 1/3 R-R interval is too short
for detection.).
numeric flashes, yellow alarm lamp,
short yellow audible alarm
** RR HIGH RESP The respiration rate has exceeded the high
alarm limit.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** RR LOW RESP The respiration rate has dropped below the low
alarm limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
* RUN PVCs HIGH
** RUN PVCs HIGH
ECG/Arrhythmia A run of PVCs greater than 2 was detected. numeric flashes, yellow alarm lamp,
short yellow audible alarm
** <SO₂ Label> HIGH SvO2/SO2The the measured intravascular oxygen
saturation has exceeded the high limit.
numeric flashes and high alarm
limit is highlighted, yellow alarm
lamp, alarm tone
** <SO₂ Label> LOW SvO2/SO2The measured intravascular oxygen saturation
has fallen below the low limit.
numeric flashes and low alarm limit
is highlighted, yellow alarm lamp,
alarm tone
** <SpO₂ Label> HIGH SpO2The arterial oxygen saturation has exceeded the
high alarm limit.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** <SpO₂ Label> LOW SpO2The arterial oxygen saturation has fallen below
the low alarm limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
** ST-<n> HIGH ECG/ST The ST elevation in lead <n> is higher than the
limit.
numeric flashes and high alarm
limit is highlighted, yellow alarm
lamp, alarm tone
Alarm Message From Condition Indication
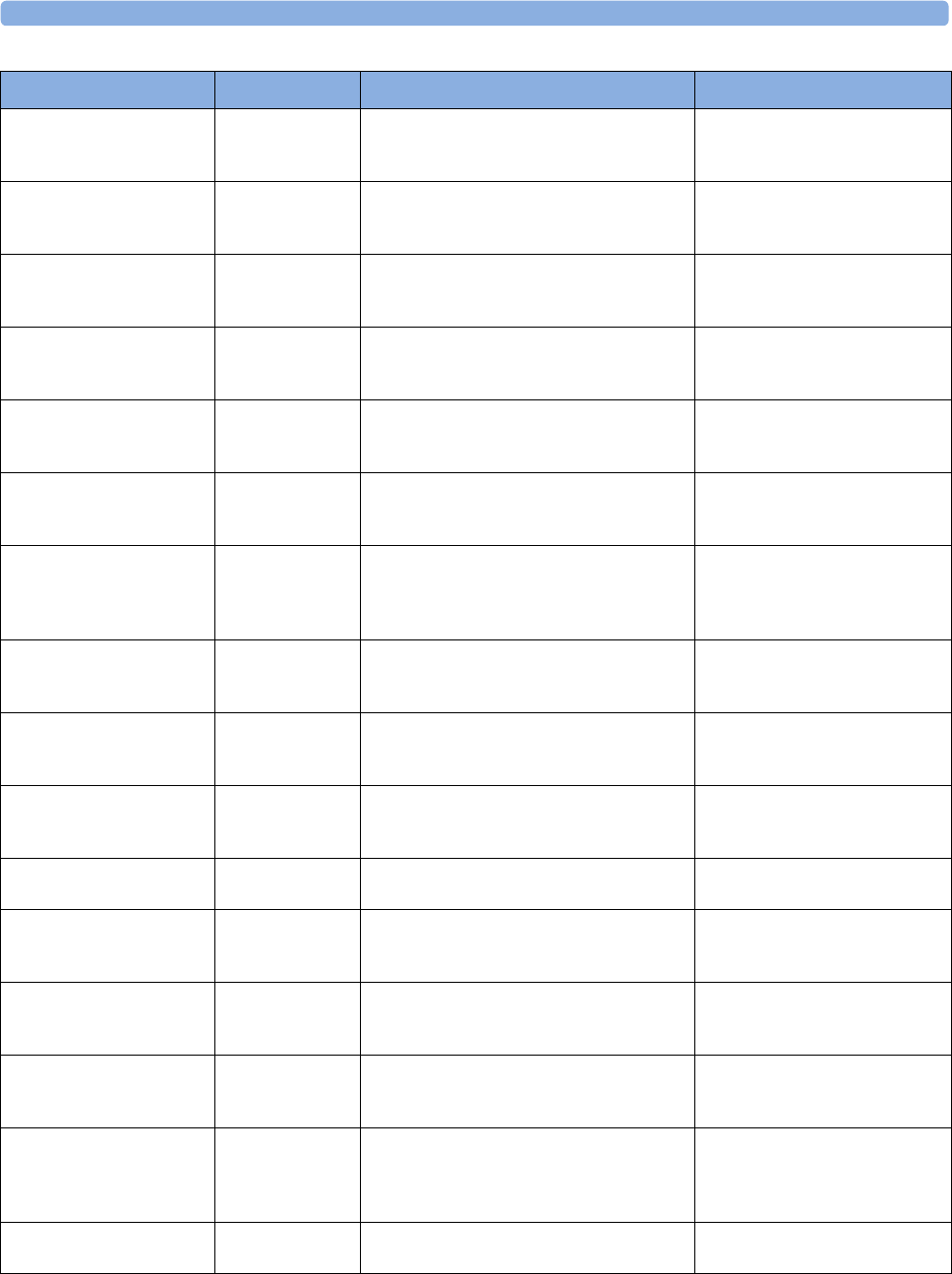
3 Patient Alarms and INOPs
69
** ST-<n> LOW ECG/ST The ST depression in lead <n> is lower than
the limit.
numeric flashes and low alarm limit
is highlighted, yellow alarm lamp,
alarm tone
* SVT
** SVT
ECG/Arrhythmia A run of supraventricular beats greater than the
SVT run limit has been detected and the HR
has exceeded the SVT HR limit.
numeric flashes, yellow alarm lamp,
alarm tone
** Tblood HIGH C.O. The blood temperature value has exceeded the
high alarm limit.
numeric flashes, high alarm limit is
highlighted, yellow alarm lamp,
alarm tone
** Tblood LOW C.O. The blood temperature value has fallen below
the low alarm limit.
numeric flashes, low alarm limit is
highlighted, yellow alarm lamp,
alarm tone
** tcpO₂ HIGH
** tcpCO₂ HIGH
tcGas The tcpO2 or tcpCO2 value has exceeded the
high alarm limit.
numeric flashes, high alarm limit is
highlighted, yellow alarm lamp,
alarm tone
** tcpO₂ LOW
** tcpCO₂ LOW
tcGas The tcpO2 or tcpCO2 value has fallen below
the low alarm limit.
numeric flashes, low alarm limit is
highlighted, yellow alarm lamp,
alarm tone
* TELE ALARM
** TELE ALARM
*** TELE ALARM
Telemetry This is a generic alarm from the telemetry
system. The specific alarm cause is indicated in
the alarm message in the Telemetry Data
Window.
yellow or red alarm lamp and alarm
tone
** <Temp Label> HIGH TEMP The temperature has exceeded the high alarm
limit.
numeric flashes and high limit is
highlighted, yellow alarm lamp,
alarm tone
** <Temp Label> LOW TEMP The temperature has fallen below the low alarm
limit.
numeric flashes and low limit is
highlighted, yellow alarm lamp,
alarm tone
* VENT BIGEMINY
** VENT BIGEMINY
ECG/Arrhythmia A dominant rhythm of N, V, N, V (N =
supraventricular beat, V = ventricular beat) was
detected.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
*** VENT FIB/TACH ECG A fibrillatory waveform for 4 consecutive
seconds was detected.
numeric flashes, red alarm lamp,
alarm tone
* VENT RHYTHM
** VENT RHYTHM
ECG/Arrhythmia A dominant rhythm of adjacent Vs > vent
rhythm limit and ventricular HR < VTach HR
limit was detected.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
* VENT TRIGEMINY
** VENT TRIGEMINY
ECG/Arrhythmia A dominant rhythm of N, N, V, N, N, V (N =
supraventricular beat, V = ventricular beat) was
detected.
numeric flashes, yellow alarm lamp,
short yellow audible alarm
*** VTACH ECG, Arrhythmia Ventricular tachycardia has been detected
(Consecutive PVCs exceed V-Tach Run limit
and HR exceeds V-Tach HR limit).
numeric flashes, red alarm lamp,
alarm tone
** VueLink ALARM
*** VueLink ALARM
at Information Center
VueLink A yellow (**) or red (***) patient alarm is
present on the VueLink module. Check the
monitor display for more detailed alarm
information.
(on monitor) yellow or red alarm
lamp; the alarm text is defined by
the VueLink device driver
** ΔQTc HIGH ECG/QT ΔQTc value has exceeded the ΔQTc high limit
for more than 5 minutes
numeric flashes, yellow alarm lamp,
alarm tone
Alarm Message From Condition Indication
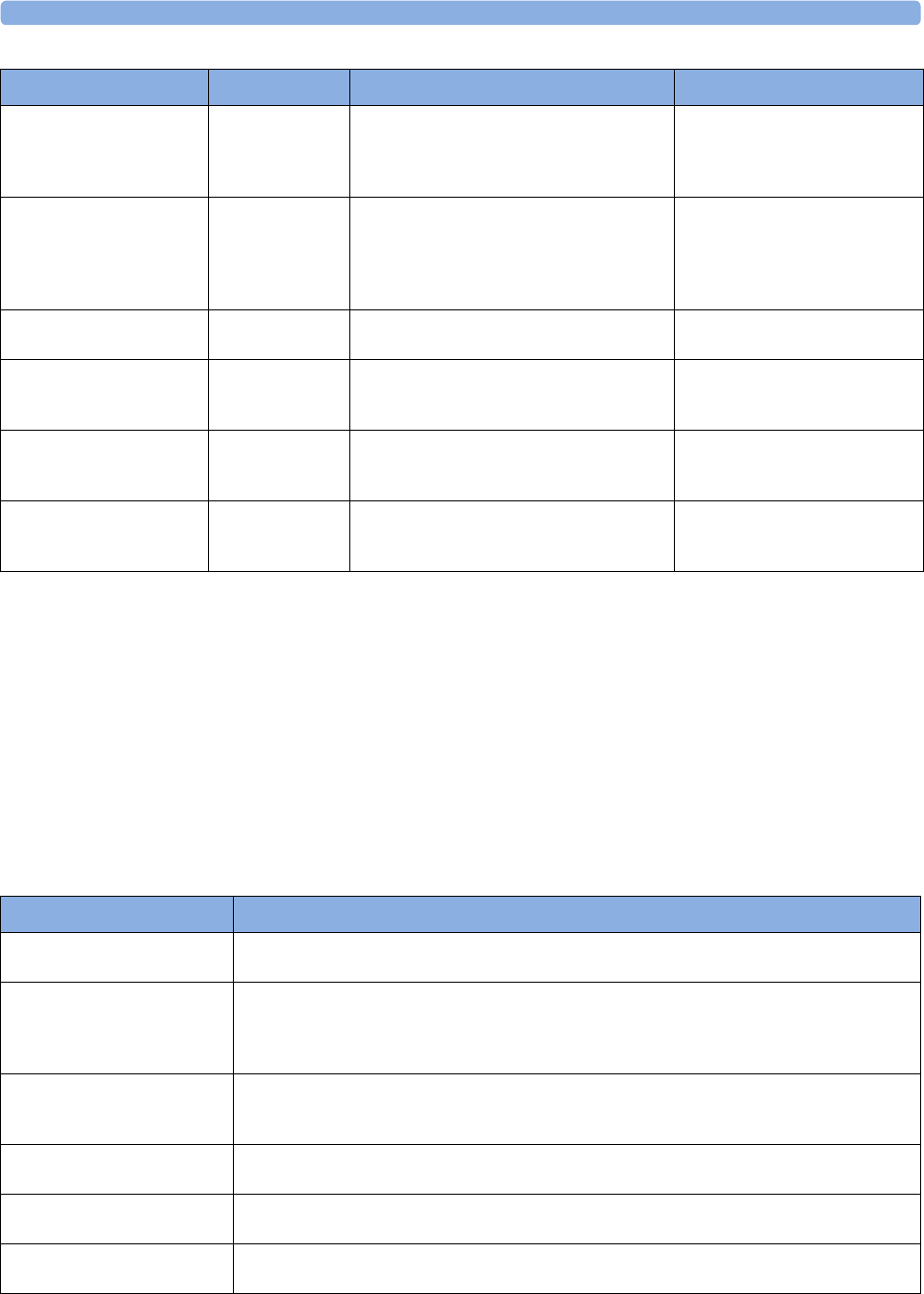
3 Patient Alarms and INOPs
70
Technical Alarm Messages (INOPs)
If an INOP interrupts monitoring and alarm detection, the measurement numeric will be replaced
by -?-. If an INOP may lead to unreliable measurement values, a ?appears next to the numeric.
The measurement labels and abbreviations for pressure, temperature, SpO2, and VueLink INOP
messages are explained in the individual measurement chapters.
Monitor INOPs
***BRADY/P xxx<yyy
***BRADY xxx < yyy
Press, SpO2The heart rate from the Pulse signal has fallen
below the bradycardia limit. xxx denotes the
lowest measured value; yyy is the bradycardia
limit.
numeric flashes and alarm limit is
highlighted, red alarm lamp, alarm
tone
***<Pressure>
DISCONNECT
PRESS The pressure is non-pulsatile and the mean
pressure is continuously less than 10mmHg
(1.3kPa). This alarm occurs only with arterial
pres su re s (P, AB P, ART, A o, BA P, FA P, PA P,
UAP, P1, P2, P3, P4).
numeric flashes, red alarm lamp,
alarm tone
**ST MULTI <n>,<n> ECG/ST The ST depression or elevation is outside of
the limit in two or more leads <n> and <n>.
numeric flashes, yellow alarm lamp,
alarm tone
**ST MULTI
at Information Center
ECG/ST The ST depression or elevation is outside of
the limit in two or more leads. Check on the
monitor
(on monitor) numeric flashes,
yellow alarm lamp, alarm tone
***TACHY xxx > yy ECG The tachycardia limit has been exceeded numeric flashes and alarm limit is
highlighted, red alarm lamp, alarm
tone
***TACHY/P xxx>yy
or
***TACHY xxx > yy
Press, SpO2, ECG The tachycardia limit has been exceeded. xxx
denotes the highest measured value; yy is the
tachycardia limit.
numeric flashes, alarm limit is
highlighted, red alarm lamp, alarm
tone
Alarm Message From Condition Indication
INOP Message, Indication What to do
!! CHECK PAIRING
INOP tone
There is a problem with device pairing. Check that the monitor and telemetry device are correctly
paired.
Bad Server Link
INOP tone
1) An MMS with an incompatible software revision is connected to the monitor. This combination
does not allow monitoring, OR
2) You cannot use this combination of monitor, MMS and cable. Switch off the monitor and contact
your service personnel.
CENTRAL: TELE ONLY
INOP tone
System connectivity via telemetry device is limited (No alarms, only local numerics) when in
companion mode and host monitor does not have system connectivity. Only telemetry device
parameters can be displayed at central station.
Check Alarm Lamps
INOP tone
Perform a visual check of the alarm lamp to establish whether there is a problem. Contact your service
personnel to check the internal connections to the alarm lamps.
Check DrugSettings
INOP tone
There was a problem loading the drug settings. Check that the settings are complete and correct.
!!CHECK ECG SOURCE
INOP tone
The telemetry device and the monitor both have valid ECG signals. Unpair the telemetry device and
the monitor if they are no longer used for the same patient.
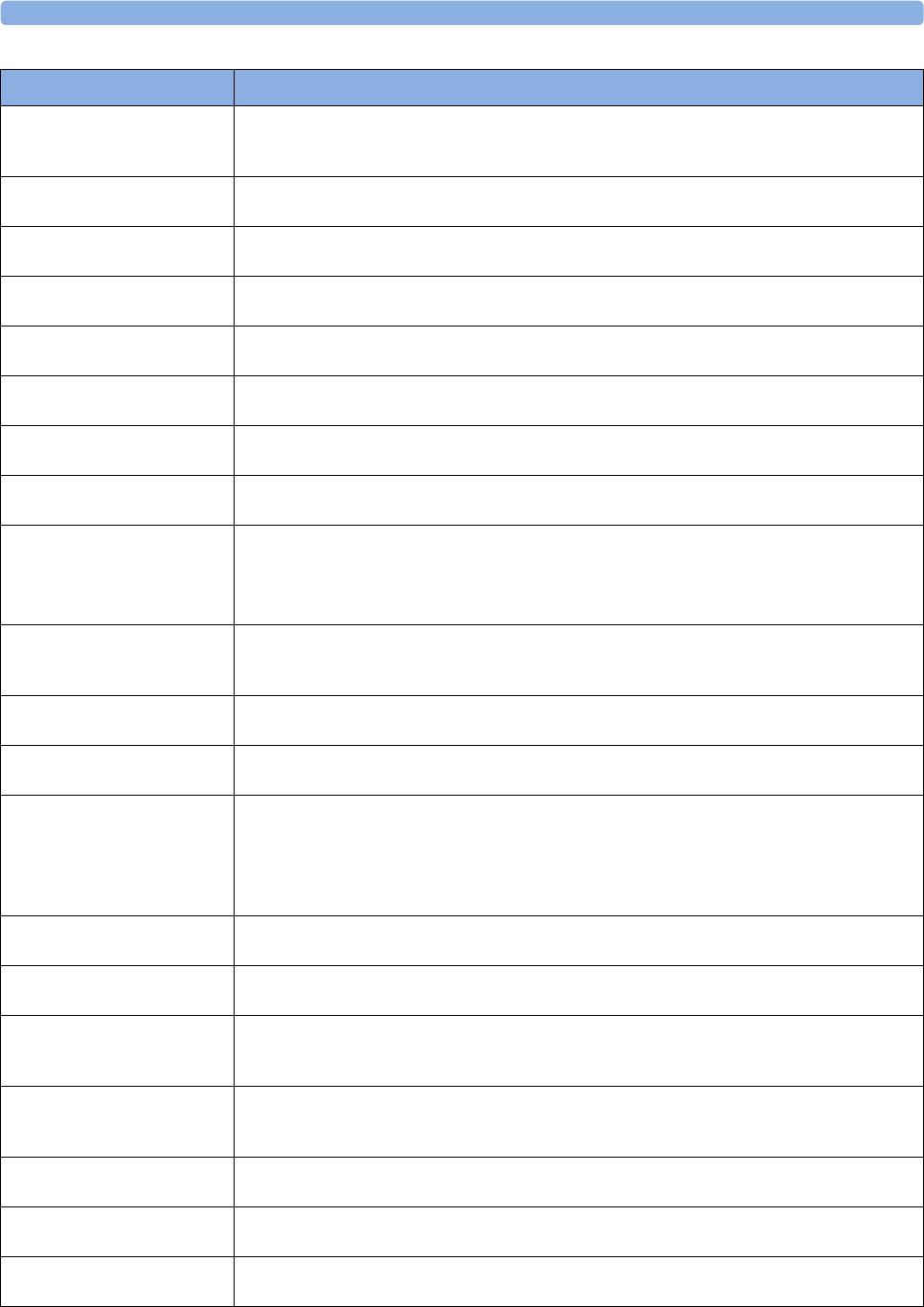
3 Patient Alarms and INOPs
71
Check Flex Texts
INOP tone
Check the names of the monitor menus, for example the labels for screens, profiles, event or trend
group names, before you resume monitoring. If they are unexpected, there may be a problem with the
monitor software. Contact your service personnel.
Check Keyboard
INOP tone
Perform a visual and functional check of the keyboard. Contact your service personnel.
Check Main Board 2
INOP tone
There is a problem with the second main board in the monitor. Contact your service personnel.
Check Monitor Func
INOP tone
Potential problem with alarm lamps, display or interfaces detected. Contact your service personnel.
Check Monitor Temp
INOP tone
The temperature inside the monitor is too high. Check that the monitor ventilation is not obstructed.
If the situation continues, contact your service personnel.
Check Mouse Device
INOP tone
Perform a visual and functional check of the mouse input device. Contact your service personnel.
Check MSL Voltage
INOP tone
There is a problem with the voltage of the Measurement Link (MSL). Contact your service personnel.
Check Network Conf
INOP tone
The monitor is receiving network topology information from more than one source, e.g. the Database
Server and an Application Server. Contact your service personnel.
Check Screen Res.
INOP tone
The Screen you have selected uses a resolution which is not supported by the display. The monitor will
show a generic Screen instead until you select a different Screen.
Contact your service personnel if you want the Screen deleted from the Profile(s) to avoid this in
future.
Check Settings
INOP tone
If this INOP appears, check the monitor and patient settings before you resume monitoring. If the
settings are unexpected, there may be a problem with the monitor software. Contact your service
personnel.
Check SpeedPoint
INOP tone
Perform a visual and functional check of the SpeedPoint input device. Contact your service personnel.
Check Touch Input
INOP tone
Perform a visual and functional check of the touch input device. Contact your service personnel.
Check Waves
INOP tone
The options purchased with this monitor may not support the number of waves required to show the
selected Screen, so some waves or high resolution trends are missing from the Screen. Select a
different Screen with fewer waves.
Contact your service personnel if you want the Screen deleted from the Profile(s) to avoid this in
future.
CHK ECG Sync Cable
INOP tone
The ECG Sync is detecting an invalid signal, or the ECG Sync cable is disconnected.
Chk IndepDsp Cable The monitor cannot communicate with the D80 Intelligent Display. Check the MSL coupling cable.
The end with the gray connector must be connected to the Intelligent Display.
Chk MSL Connection
INOP tone
Check that the MSL cable is properly connected. If this is the case, try using another MSL cable, to
check if your cable is defective. If this does not help, the device connected via the MSL cable may be
defective, contact your service personnel.
ECG EQUIP MALF T
Numeric is displayed with a -?-
INOP tone
Contact your service personnel.
The ECG in the Telemetry device is faulty.
Internal.Comm.Malf
INOP tone
There is a problem with I2C Bus communication in the monitor. Contact your service personnel.
MCC Reversed
INOP tone
The MSL coupling cable is reversed. Connect the end with the gray connector to the Intelligent
Display.
MCC Unsupported
INOP tone
An MSL coupling cable has been connected to a device which does not support MSL coupling.
INOP Message, Indication What to do
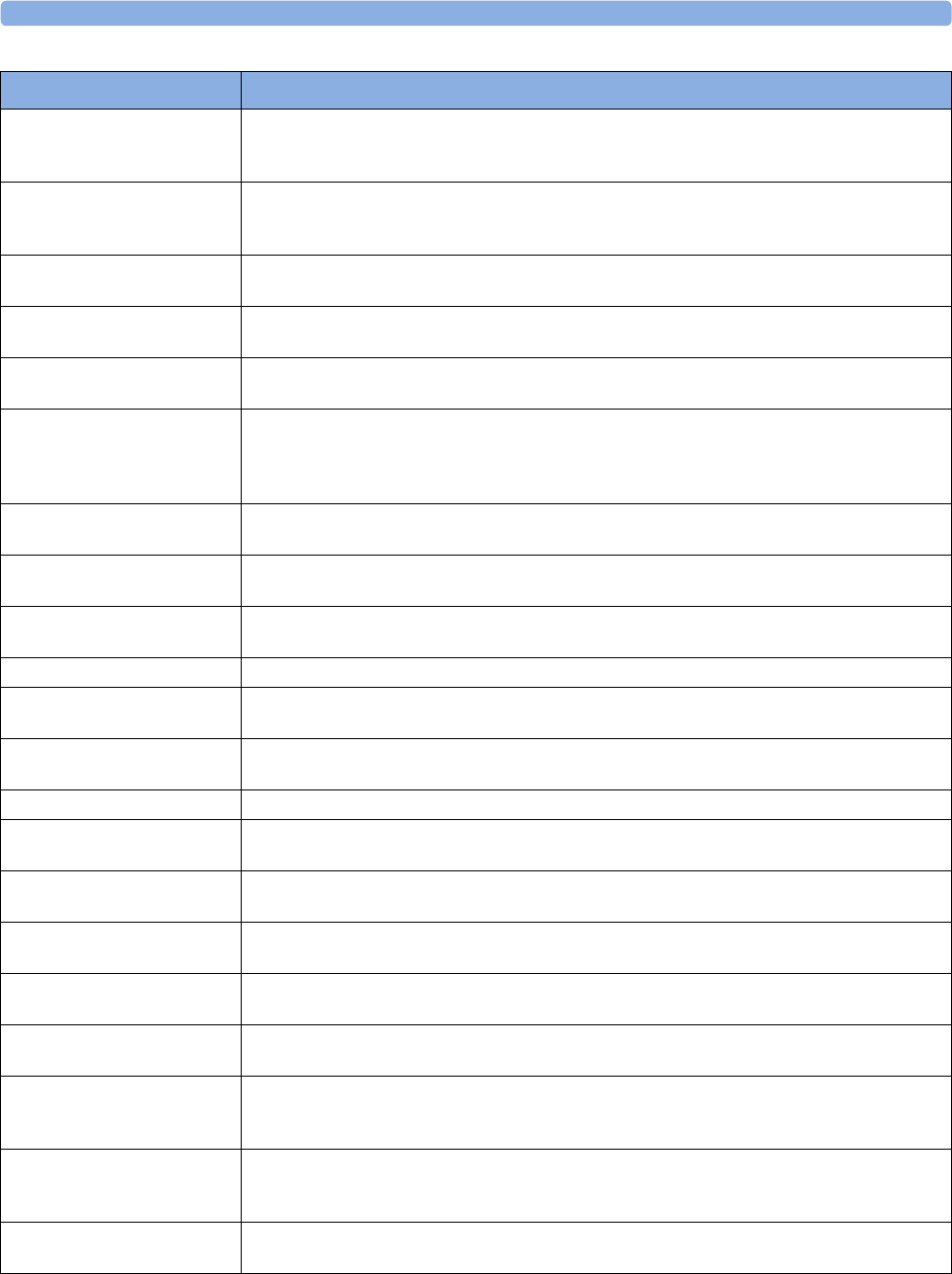
3 Patient Alarms and INOPs
72
Meas. DEACTIVATED An X2 or MP5 has been connected to a host monitor (companion mode) and all derived
measurements have been deactivated and/or measurements with a label conflict. The measurements
can only be reactivated by disconnecting the measurement device from the host monitor.
!!MORE BED ALARMS
!!!MORE BED ALARMS
at Information Center
The monitor is associated with a telemetry device and is sending data to the Information Center via
the telemetry device. There are currently more alarms at the bedside than can be transmitted to the
Information Center.
MSL Power High The power consumption of the devices connected to the Measurement Link (MSL) cable is too high.
If this situation continues, the MSL will be switched off. Contact your service personnel.
MSL Power Off
INOP tone
The power consumption of the devices connected to the Measurement Link (MSL) cable was too high
for too long and the MSL has been switched off. Contact your service personnel.
MSL Power Overload
INOP tone
The power consumption of the devices connected to the Measurement Link (MSL) cable is much too
high or there has been a short circuit. The MSL has been switched off. Contact your service personnel.
No Central Monit.
INOP tone
There is a problem with the communication to the network. Central monitoring is currently not
possible (no patient alarms or information). Check the connection. In case the connection is via a
telemetry device, the current telemetry use model does not support central monitoring. Contact your
service personnel.
NO ECG AT CENTRAL The ECG measured with the monitor ECG is not being sent to the Information Center via the
telemetry device.
Rem.AlarmDev.Malf.
INOP tone
There is a problem with the connection to the remote alert device. Contact your service personnel to
check the remote alert device and its connections.
Settings Malfunc.
INOP tone
The monitor cannot use the predefined settings for monitoring. Contact your service personnel.
Speaker Malfunct. Contact your service personnel to check the speaker and the connection to the speaker.
SRR INTERFERENCE
INOP tone
The short range radio connection has interference from another device. Try using another channel.
SRR INVALID CHAN
INOP tone
The channel configuration of the Short Range Radio is invalid. Check channel and channel mask
configuration.
SRR MALFUNCTION Malfunction in the short range radio device. If the INOP persists contact your service personnel.
TAAP DISABLED
INOP tone
The currently selected telemetry configuration on the monitor does not allow connection of telemetry
devices to the monitor.
TELE CONFIG UNSUPP
INOP tone
Telemetry device not supported (companion mode)
TELE EQUIP MALF
INOP tone
The telemetry device has a malfunction. Disconnect and reconnect the telemetry device. If the INOP
reappears, replace the telemetry device.
TELE INCOMPATIBLE SRR-enabled telemetry device is not supported by this central software revision. Please check
configuration.
TELE UNSUPPORTED
INOP tone
This telemetry device is not supported for direct connection to the monitor.
TimeExpired:<Timer
Label>
INOP tone
The time has expired for the timer indicated in the INOP text. Clearing the timer clears the INOP.
Unsupported LAN
INOP tone
There is a problem with the communication to the network and central monitoring is currently not
possible. Check the connection. If the INOP persists, switch off the monitor and contact your service
personnel.
User I/F Malfunct.
INOP tone
Perform a visual and functional check of all the monitor input devices. Contact your service personnel.
INOP Message, Indication What to do
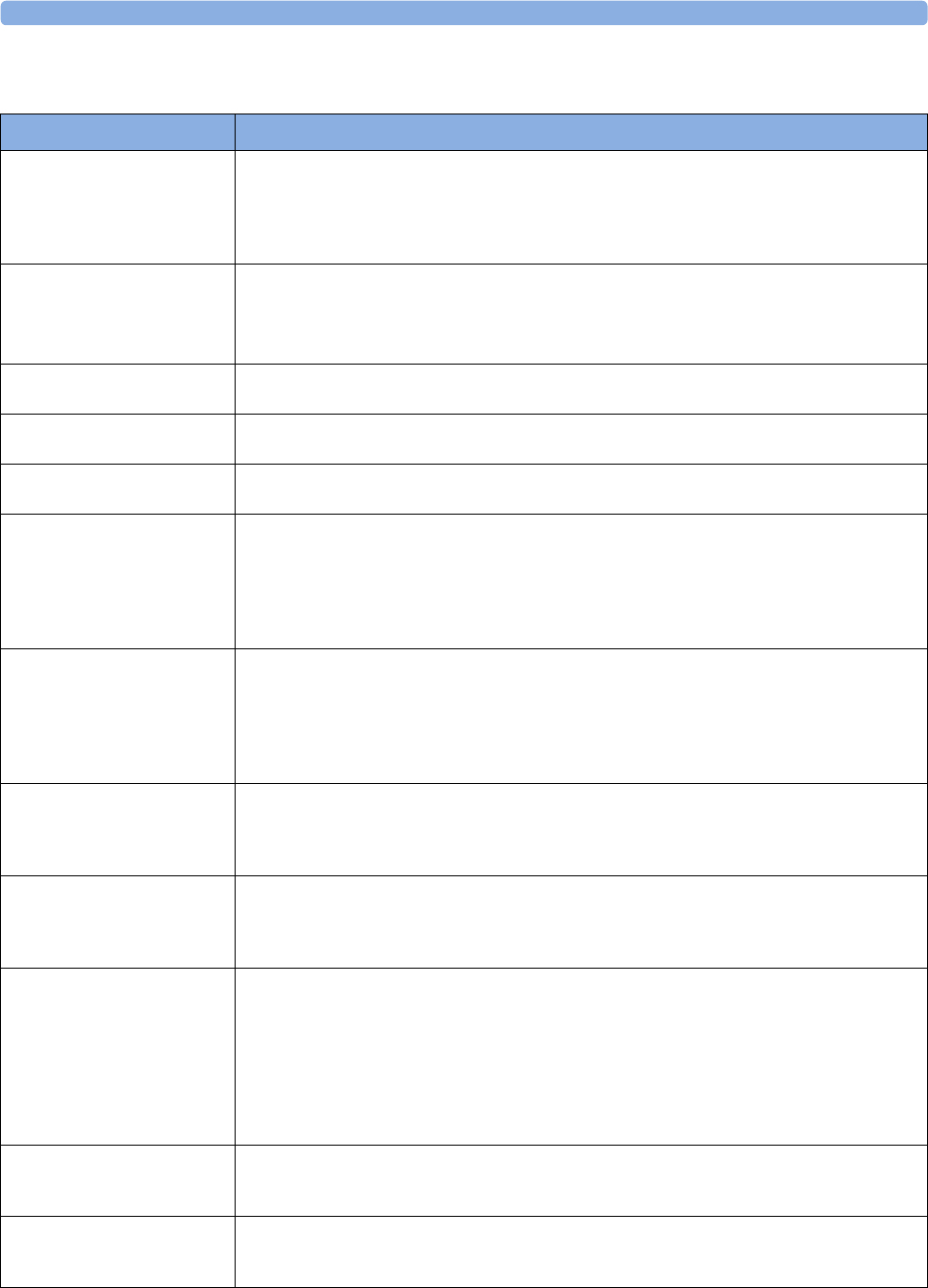
3 Patient Alarms and INOPs
73
Battery INOPs
INOP Message, Indication What to do
Batt 1 MISSING
Batt 2 MISSING
INOP tone
During this INOP, alarms cannot
be paused or switched off.
The monitor requires two batteries but can detect only one battery. Insert the missing battery
immediately.
Batt EMPTY
INOP tone, battery LED flashes
During this INOP, alarms cannot
be paused or switched off.
The estimated remaining battery-powered operating time is less than 10 minutes. Replace the battery
immediately.
If the condition persists and the monitor is not connected to mains power, this INOP is re-issued two
minutes after you acknowledge it.
BATT EXTENSN MALF
INOP tone
There is a hardware error in the Battery Extension. Contact your service personnel.
Batt INCOMPAT.
INOP tone
The battery cannot be used with this monitor. Replace with the correct battery (M4607A).
Batt LOW
INOP tone
The estimated battery-powered operating time remaining is less than 20 minutes.
Batt MALFUNCTION
INOP tone, battery LED flashes
During this INOP, alarms cannot
be paused or switched off unless
the monitor is connected to
mains power.
The monitor cannot determine the battery status. If this INOP persists, replace the faulty battery. If
the condition persists and the monitor is not connected to mains power, this INOP is re-issued two
minutes after you acknowledge it.
Place the battery in a different monitor or in a battery charger. If the same INOP is shown, contact
your service personnel.
BATTERIES EMPTY
Batt 1 EMPTY
Batt 2 EMPTY
INOP tone, battery LED flashes
During this INOP, alarms cannot
be paused or switched off.
The estimated remaining battery-powered operating time of the indicated battery or batteries is less
than 10 minutes. Replace the batteries immediately.
If the condition persists and the monitor is not connected to mains power, this INOP is re-issued two
minutes after you acknowledge it.
BATTERIES INCOMPAT
Batt 1 INCOMPAT.
Batt 2 INCOMPAT.
INOP tone
The indicated battery or batteries cannot be used with this monitor. Replace with the correct battery or
batteries as specified in this book.
BATTERIES LOW
Batt 1 LOW
Batt 2 LOW
INOP tone
The estimated battery-powered operating time remaining is less than 20 minutes.
BATTERIES MALFUNC.
Batt 1 MALFUNCTION
Batt 2 MALFUNCTION
INOP tone, battery LED flashes
During this INOP, alarms cannot
be paused or switched off unless
the monitor is connected to
mains power.
The monitor cannot determine the battery status. If this INOP persists, replace the faulty battery or
batteries. If the condition persists and the monitor is not connected to mains power, this INOP is re-
issued two minutes after you acknowledge it.
Place the batteries in a different monitor or in a battery charger. If the same INOP is shown, contact
your service personnel.
Charge Batt 1 Now
Charge Batt 2 Now
INOP tone
Battery must be charged. Connect the monitor to mains power or exchange the battery.
CHARGER MALFUNC.
INOP tone, battery LED may
flash
There is a problem with the battery charger in the monitor. Connect the monitor to mains power and
contact your service personnel.
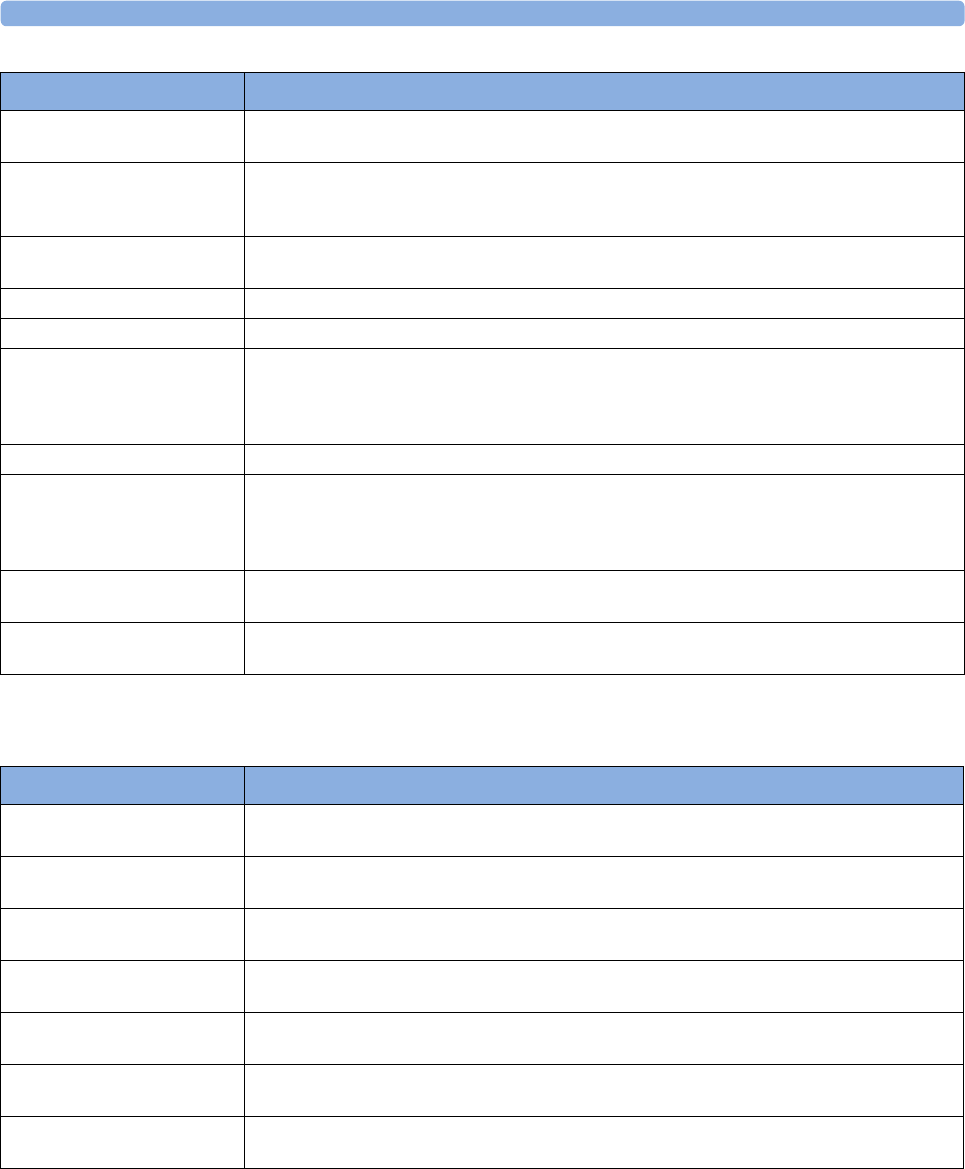
3 Patient Alarms and INOPs
74
MMS, MMS Extensions and FMS INOPs
CHECK BATT TEMP
INOP tone
The temperature of one or both batteries is too high. Check that ventilation openings (if applicable)
are not blocked and monitor is not exposed to heat.
Chk MSL Connection Check the MSL connection between X2/MP2 and the battery extension for damage or loose
connections. Check also if a second X1 or X2 has been connected accidentally (e.g. in companion
mode).
ExtBat EMPTY The estimated battery-powered operating remaining time is less than 10 minutes. Replace the battery in
the battery extension immediately.
ExtBat INCOMPAT. The battery in the battery extension cannot be used.
ExtBat LOW The estimated battery-powered operating time remaining is less than 20 minutes.
ExtBat MALFUNCTION The monitor cannot determine the status of the battery in the battery extension. If this INOP persists,
replace the faulty battery in the battery extension. If the condition persists and the monitor is not
connected to mains power or a host monitor, this INOP is re-issued two minutes after you
acknowledge it.
ExtBat MISSING There is no battery in the Battery Extension
!!INSERT BATTERY
Severe yellow INOP tone
During this INOP, alarms cannot
be paused or switched off.
X2/MP2 only: There is no battery in the battery compartment. You cannot operate the monitor on
AC mains while the battery compartment is open (not sealed with a battery). Load a battery
immediately.
MSL Power High The power consumption of the devices connected to the Battery Extension is too high. If this
situation continues, the Battery Extension will be switched off. Contact your service personnel.
MSL Power Off The power consumption of the devices connected to the Battery Extension was too high for too long.
The Battery Extension has been switched off. Contact your service personnel.
INOP Message, Indication What to do
INOP Message, Indication What to do
FMS UNPLUGGED
INOP tone
Make sure that the Flexible Module Rack is connected to the monitor. All FMS measurements are off
while the FMS is unplugged.
FMS UNSUPPORTED
INOP tone
The Flexible Module Rack is not supported by your monitor. Contact your service personnel.
MEASSRV UNSUPPORTD
INOP tone
The Multi-Measurement module is not supported by the monitor. Contact your service personnel.
MMS Ext. UNPLUGGED
INOP tone
The MMS extension has been disconnected from the Multi-Measurement Module.
MMS Ext. Unpowered
INOP tone
The MMS extension cannot operate while the Multi-Measurement Module is running on battery
power.
MMS Ext.EQUIP MALF
INOP tone
Loss of communication between the Multi-Measurement Module and the MMS extension. Contact
your service personnel.
MMS UNPLUGGED
INOP tone
Make sure that the Multi-Measurement Module is connected to the monitor. All MMS measurements
are off while the MMS is unplugged.
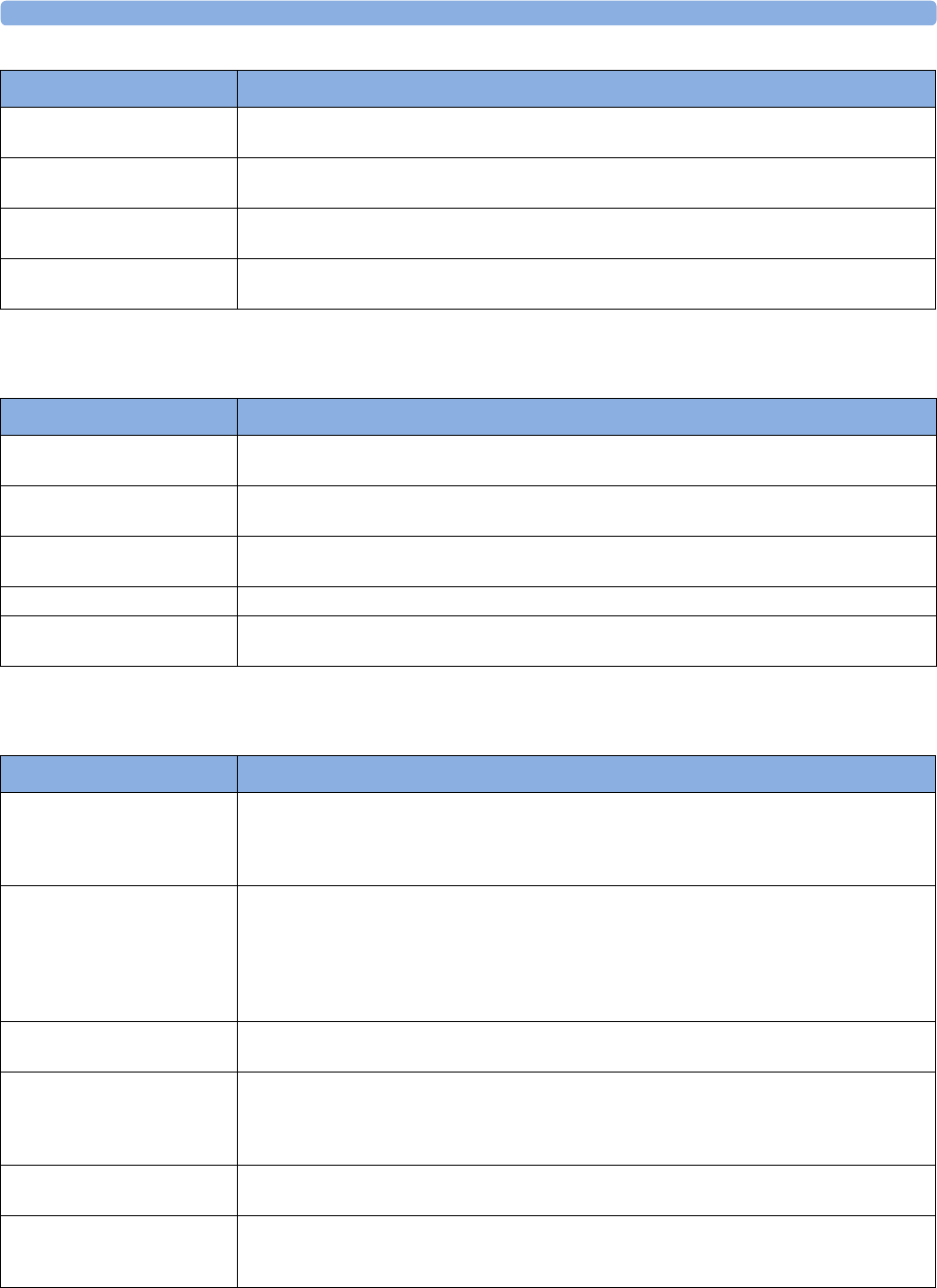
3 Patient Alarms and INOPs
75
Display INOPs
ECG, Arrhythmia, QT and ST INOPs
MMS UNSUPPORTED
INOP tone
The Multi-measurement Module is not supported by your monitor. Contact your service personnel.
MMSExt.Unsupported
INOP tone
The MMS extensions not supported by your monitor. Contact your service personnel.
NO PPV FROM FMS The measurement device does not supply a beat-to-beat arterial pressure value. Contact your service
personnel.
NO PPV FROM MMS The measurement device does not supply a beat-to-beat arterial pressure value. Contact your service
personnel.
INOP Message, Indication What to do
INOP Message, Indication What to do
Indep.Dsp Malfunc. There is a problem with the Independent Display. Check the MSL coupling cable then contact your
service personnel.
Indep.Dsp NotSupp. The monitor does not support a second main display. The monitor software is incompatible. Contact
your service personnel.
Intell.Dsp Malf. There is a problem with the Intelligent Display. Check the MSL coupling cable then contact your
service personnel.
Intell.Dsp Missing The monitor has lost contact with the connected Intelligent Display. Contact your service personnel.
Intell.Dsp Unsupp. The monitor does not support the connected Intelligent Display. The monitor software is
incompatible.
INOP Message, Indication What to do
C LEAD OFF
HR Numeric is replaced by -?-
for 10 seconds.
INOP tone
The C electrode (AAMI: V electrode) has become detached from the patient or the lead set has been
changed. Reattach the electrode or select New Lead Setup in the Setup ECG menu to confirm the
new lead set.
CANNOT ANALYZE ECG The arrhythmia algorithm cannot reliably analyze the ECG data. Check the ECG signal quality of the
selected primary and secondary leads. If necessary, improve lead position or reduce patient motion.
If you have arrhythmia analysis on, and you are not getting a reliable HR because the signal is below a
minimum amplitude, unstable, or contains artifact, and you have tried to improve the system
performance by choosing another lead and changing electrodes, you should consider turning
arrhythmia analysis off.
CANNOT ANALYZE QT The QT algorithm cannot generate a valid QT value for more than 10 minutes, or 1 minute in the
initial phase.
CANNOT ANALYZE ST The ST algorithm cannot generate a valid ST value. Possible causes are large variations in the measured
ST values for consecutive beats, or ventricular paced beats. Review the ECG signal quality and the ST
measurement points.
If the patient has a ventricular pacemaker, ST analysis is not possible.
ECG EL. NOISY <ECG
Lead>
The ECG signal from the named ECG electrodes [RA, LA, LL, RL, V (or C)] is noisy. Check the ECG
connections and make sure that the electrode indicated is attached.
ECG EQUIP MALF
Numeric is replaced by -?-
INOP tone
Contact your service personnel.
The ECG hardware is faulty.
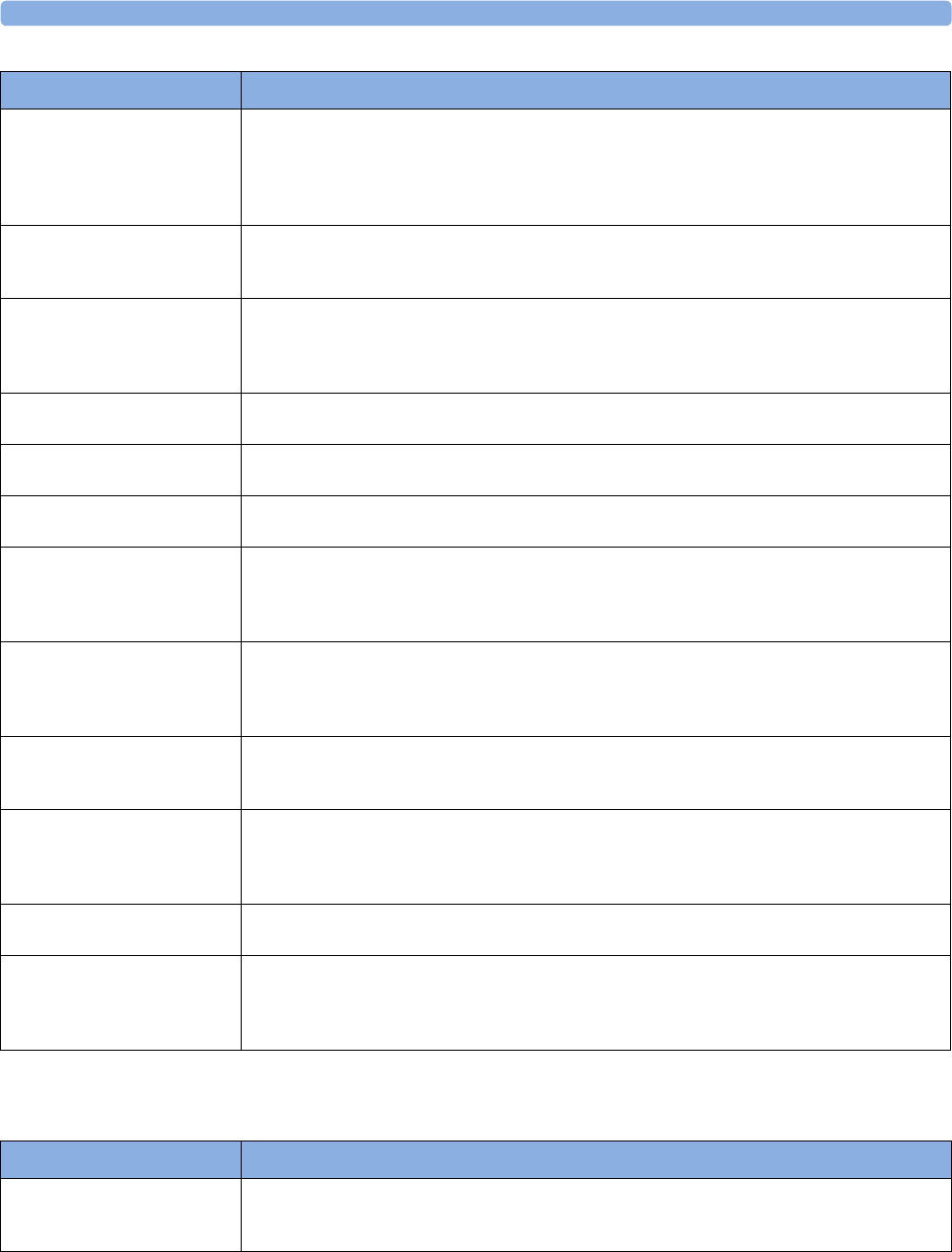
3 Patient Alarms and INOPs
76
Pulse INOPs
<ECG Lead> LEAD OFF
!! <ECG Lead> LEAD OFF
!!! <ECG Lead> LEAD OFF
Numeric is replaced by -?-
INOP tone
Not all the required leads for ECG monitoring are connected. Check the ECG connections and make
sure that the electrode indicated by <ECG lead> [RA, LA, LL, RL, V or C] electrodes is attached. In
EASI mode, all 5 electrodes must be connected.
ECG LEADS OFF
!! ECG LEADS OFF
!!!ECG LEADS OFF
Check that all of the required ECG leads are attached, and that none of the electrodes have been
displaced.
ECG NOISY SIGNAL
INOP tone
The ECG signal is too noisy. Check that the electrodes are properly placed and have not dried out.
Remove any possible sources of signal noise (such as power cords) from the area around the cable and
the patient.
The ECG signal may be saturated or overloaded.
!!ECG/AR ALARM OFF All ECG alarms have been switched off, or the HR alarm source is not ECG. To resume ECG alarm
generation, switch ECG alarms on or select ECG as the alarm source.
ECG/ARRH ALARM OFF
!!ECG/AR ALARM OFF
All ECG alarms have been switched off, or the HR alarm source is not ECG. To resume ECG alarm
generation, switch ECG alarms on or select ECG as the alarm source.
EcgOut EQUIP MALF
INOP tone
There is a problem with the device connected to the ECG Out connector. Contact your service
personnel.
LA LEAD OFF
Numeric is replaced by -?- for 10
seconds.
INOP tone
The LA electrode has become detached from the patient or the lead set has been changed. Reattach
the electrode or select New Lead Setup in the Setup ECG menu to confirm the new lead set.
LL LEAD OFF
Numeric is replaced by -?- for 10
seconds.
INOP tone
The LL electrode has become detached from the patient or the lead set has been changed. Reattach the
electrode or select New Lead Setup in the Setup ECG menu to confirm the new lead set.
RA LEAD OFF
Numeric is replaced by -?-
INOP tone
The RA electrode has become detached from the patient or the lead set has been changed. Reattach
the electrode or select New Lead Setup in the Setup ECG menu to confirm the new lead set.
RL LEAD OFF
Numeric is replaced by -?- for 10
seconds.
INOP tone
The RL electrode has become detached from the patient or the lead set has been changed. Reattach
the electrode or select New Lead Setup in the Setup ECG menu to confirm the new lead set.
SOME ECG ALRMS OFF This message appears (if configured to do so) when the on/off settings of the yellow arrhythmia
alarms differ from the current Profile.
V LEAD OFF
Numeric is replaced by -?- for 10
seconds.
INOP tone
The V electrode (IEC: C electrode) has become detached from the patient or the lead set has been
changed. Reattach the electrode or select New Lead Setup in the Setup ECG menu to confirm the
new lead set.
INOP Message, Indication What to do
INOP Message, Indication What to do
PULSE NO ALARMING
Numeric is replaced by -?-
INOP tone
Pulse has no alarming because the system pulse is measured by an external device. Select another pulse
source to enable pulse alarming.
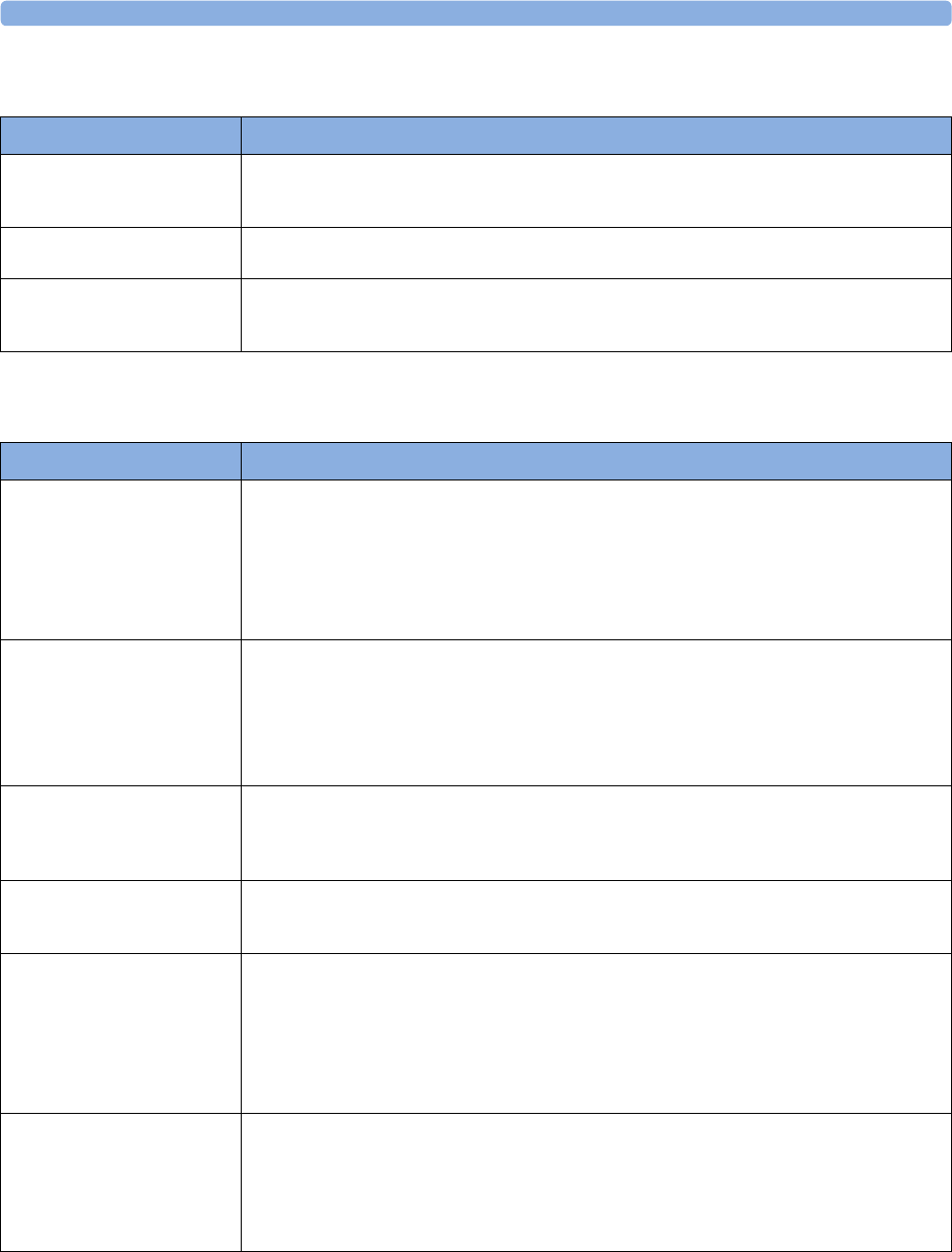
3 Patient Alarms and INOPs
77
Resp INOPs
NBP INOPs
INOP Message, Indication What to do
Resp EQUIP MALF
Numeric is replaced by -?-
INOP tone
Contact your service personnel. The RESP hardware is faulty.
Resp ERRATIC
Numeric is replaced by -?-
The monitor has detected too many artifacts in the measured Resp signal. Check that the RA and LL
electrodes are correctly attached and have not dried out.
Resp LEADS OFF
Numeric is replaced by -?-
INOP tone
Not all the required leads for Resp monitoring are attached. Make sure that the RA and LL leads are
attached.
INOP Message, Indication What to do
!! CUFF NOT DEFLAT
!!!CUFF NOT DEFLAT
Numeric is displayed with a -?-
Severe yellow/red INOP tone
During this INOP, alarms cannot
be paused or switched off.
Remove the cuff from the patient. Make sure that the tubing is not kinked or twisted and that the
correct patient category is selected. Try repeating the measurement.
You can silence the INOP, but the INOP message remains visible until the next NBP measurement is
started or the Stop All SmartKey is selected.
[Adult or pediatric patients: The NBP cuff pressure has exceeded 15 mmHg (2kPa) for more than 3
minutes.
Neonatal patients: The NBP cuff pressure has exceeded 5mmHg (0.7kPa) for more than 90 seconds.]
!! CUFF OVERPRESS
!!!CUFF OVERPRESS
Numeric displayed with -?-
Severe yellow/red INOP tone
During this INOP, alarms cannot
be paused or switched off.
The NBP cuff pressure exceeds the overpressure safety limits. Remove the cuff from the patient. Make
sure that the tubing is not kinked or twisted and that the correct patient category is selected. Try
restarting the measurement.
You can silence this INOP, but the INOP message remains visible until the next measurement is
started or the Stop All SmartKey is selected.
NBP DEACTIVATED
INOP tone
The NBP measurement label in the measurement device has been deactivated by deactivating the label
in the Measurement Selection window. The measurement automatically disappears from the
display. To switch the measurement on again, reactivate the measurement label in the Measurement
Selection window.
NBP EQUIP MALF
Numeric is replaced by -?-
INOP tone
Remove the cuff from the patient. The NBP hardware is faulty. Contact your service personnel.
You can silence this INOP, but the INOP message remains visible until the next measurement is
started or the Stop All SmartKey is selected.
NBP INTERRUPTED
Numeric is replaced by -?-
INOP tone
Check the tubing and cuff for leakages or kinks. Check that you are using the correct cuff size and
placement, and that the correct patient category is selected. Try restarting the measurement.
If the INOP occurs repeatedly, contact your service personnel.
You can silence this INOP, but the INOP message remains visible until the next measurement is
started or the Stop All SmartKey is selected.
This INOP arises when the measurement needed longer than the maximum time for inflation,
deflation or the total measurement.
NBP MEASURE FAILED
Numeric may be displayed with a
-?-
INOP tone
Check that you are using the correct cuff size and placement, and that the correct patient category is
selected. Try restarting the measurement.
You can silence this INOP, but the INOP message remains visible until the next measurement is
started or the Stop All SmartKey is selected.
Check the condition and suitability of the patient for NBP monitoring. Use another cuff to continue
measuring.
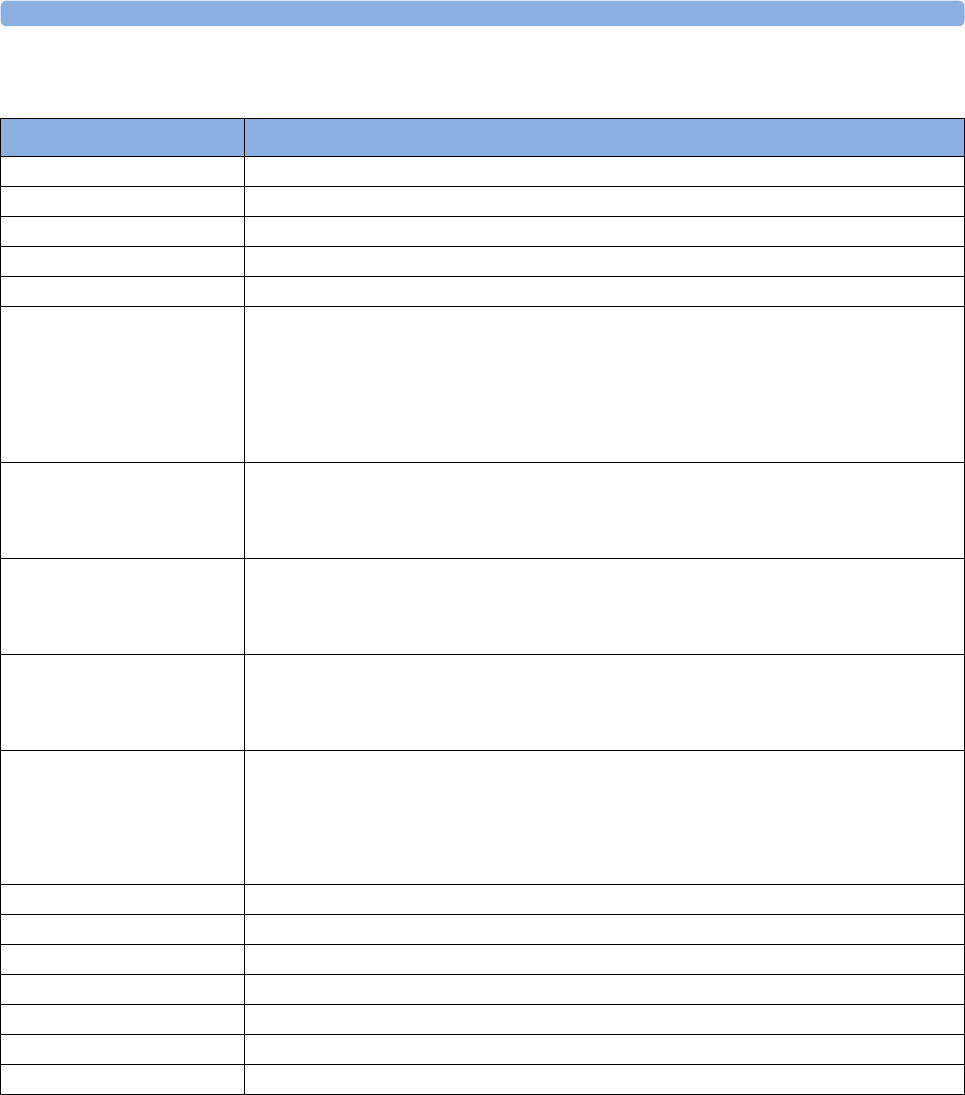
3 Patient Alarms and INOPs
78
Temperature INOPs
INOP Message, Indication What to do
T1, T2, T3, T4 INOPs See <Temp Label> INOPs
Tamb INOPs See <Temp Label> INOPs
Tart INOPs See <Temp Label> INOPs
Tcereb INOPs See <Temp Label> INOPs
Tcore INOPs See <Temp Label> INOPs
<Temp Label>
DEACTIVATED
INOP tone
A Temp measurement label in the measurement device has been deactivated, either by connecting a
Pressure transducer in the shared Press/Temp socket, or by deactivating the label in the
Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either reconnect a Temp transducer or reactivate the
measurement label in the Measurement Selection window.
<Temp Label> EQUIP
MALF
Numeric is replaced by -?-
INOP tone
Contact your service personnel.
The temperature hardware is faulty.
<Temp Label> NO
TRANSDUC
Numeric is replaced by -?-
INOP tone
Make sure the TEMP probe is connected to the MMS or module.
If you silence this INOP, the measurement will be switched off.
<Temp Label>
OVERRANGE
Numeric is replaced by -?-
INOP tone
Try changing the application site of the transducer.
[The temperature is less than -1°C, or greater than 45°C.]
<Temp Label>
UNPLUGGED
INOP tone
A Temp measurement label has been deactivated, either by unplugging a module, or by deactivating
the label in the Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either replug the module or reactivate the measurement label in
the Measurement Selection window.
Tesoph INOPs See <Temp Label> INOPs
Tnaso INOPs See <Temp Label> INOPs
Trect INOPs See <Temp Label> INOPs
Tskin INOPs See <Temp Label> INOPs
Ttymp INOPs See <Temp Label> INOPs
Tven INOPs See <Temp Label> INOPs
Tvesic INOPs See <Temp Label> INOPs
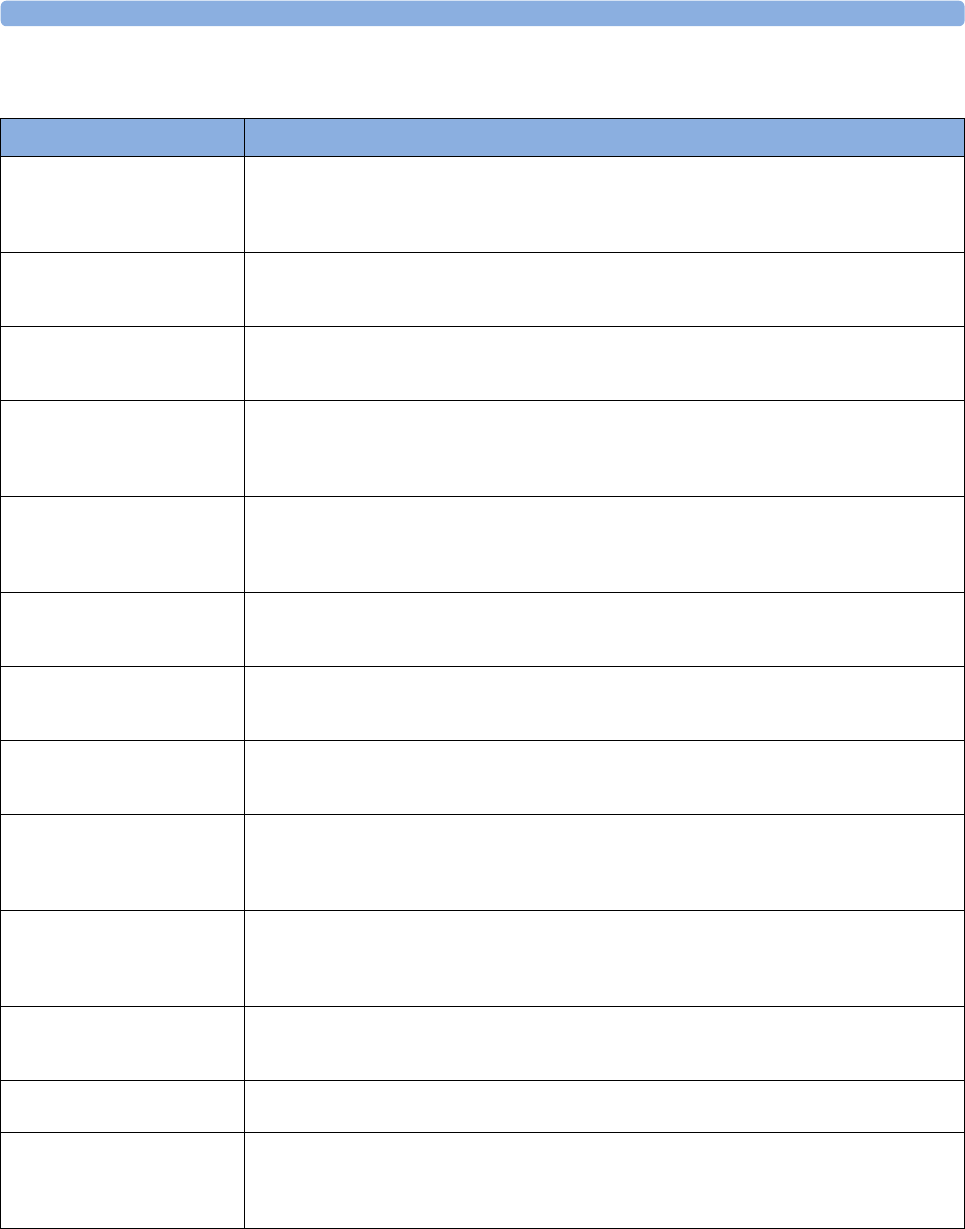
3 Patient Alarms and INOPs
79
SpO2 INOPs
INOP Message, Indication What to do
<SpO₂ Label>
DEACTIVATED
INOP tone
The SpO2 measurement label in the measurement device has been deactivated by deactivating the label
in the Measurement Selection window. The measurement automatically disappears from the
display. To switch the measurement on again, reactivate the measurement label in the Measurement
Selection window.
<SpO₂ Label> EQUIP MALF
Numeric is replaced by -?-
INOP tone
The MMS or module is faulty. Unplug and replug the MMS or module. If the INOP persists, contact
your service personnel.
<SpO₂ Label> ERRATIC
Numeric is replaced by -?-
INOP tone
Check the sensor placement. Try another adapter cable and sensor. If the INOP persists, contact your
service personnel.
<SpO₂ Label>
EXTD.UPDATE
Numeric is replaced by -?-
(questionable numeric)
The update period of displayed values is extended due to an NBP measurement on the same limb or
an excessively noisy signal.
<SpO₂ Label>
INTERFERNCE
Numeric is replaced by -?-
INOP tone
There is too much interference, caused by a high level of ambient light and/or electrical interference.
Cover the sensor to minimize ambient light. If the INOP persists, make sure that the sensor cable is
not damaged or positioned too close to power cables.
<SpO₂ Label> LOW PERF
Numeric is replaced by -?-
(questionable numeric)
Accuracy may be compromised due to very low perfusion. Stimulate circulation at sensor site. If INOP
persists, change the measurement site.
<SpO₂ Label> NO SENSOR
Numeric is replaced by -?-
INOP tone
Make sure the SpO2 sensor is connected. If the INOP persists, try another adapter cable and sensor. If
you silence this INOP, the measurement will be switched off.
<SpO₂ Label> NOISY SIGN.
Numeric is replaced by -?-
INOP tone
Excessive patient movement or electrical interference is causing irregular pulse patterns. Try to reduce
patient movement or to relieve the cable strain on the sensor.
<SpO₂ Label> NON-
PULSAT.
Numeric is replaced by -?-
INOP tone
Check the perfusion at measurement site. If necessary, stimulate circulation or change measurement
site. If the INOP is due to NBP measurement on the same limb, wait until the NBP measurement is
finished.
<SpO₂ Label> POOR
SIGNAL
Numeric is replaced by -?-
(questionable numeric)
The signal condition of the SpO2 measurement is poor and measurement accuracy may be
compromised.
<SpO₂ Label> PULSE?
Numeric is replaced by -?-
INOP tone
The detectable pulsations of the SpO2 signal are outside the specified pulse rate range.
<SpO₂ Label> SEARCHING
Numeric unavailable
SpO2 is analyzing the patient signal to derive Pulse, SpO2 and Perf values. Please wait until the search
analysis is complete.
<SpO₂ Label> SENSOR
MALF
Numeric is replaced by -?-
INOP tone
The SpO2 sensor or adapter cable is faulty. Try another adapter cable and sensor. If the INOP persists,
contact your service personnel.
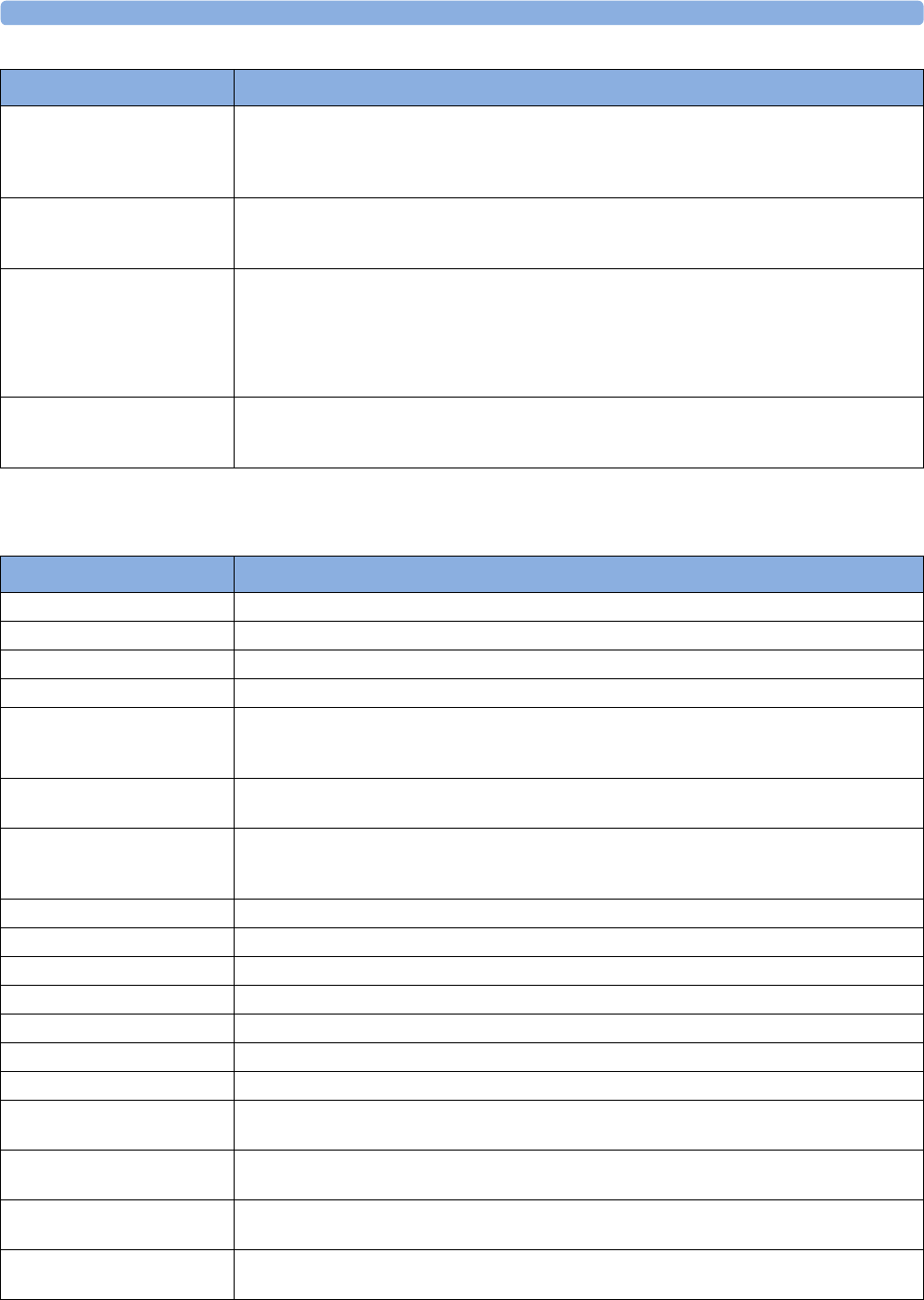
3 Patient Alarms and INOPs
80
Pressure INOPs
<SpO₂ Label> SENSOR
OFF
Numeric is replaced by -?-
INOP tone
The SpO2 sensor is not properly applied to the patient. Apply the sensor following the instructions
supplied by the manufacturer.
<SpO₂ Label>
UNKN.SENSOR
Numeric is replaced by -?-
The connected sensor or adapter cable is not supported by the SpO2 measurement. Use only specified
sensors and cables.
<SpO₂ Label>
UNPLUGGED
Numeric is replaced by -?-
INOP tone
An SpO2 measurement label has been deactivated, either by unplugging a module, or by deactivating
the label in the Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either replug the module or reactivate the measurement label in
the Measurement Selection window.
<SpO₂ Label> UPGRADE
Numeric is replaced by -?-
Numeric is unavailable
The SpO2 measurement is currently in upgrade mode. Monitoring is not possible in this mode.
INOP Message, Indication What to do
INOP Message, Indication What to do
ABP INOPs See <Press Label> INOPs
Ao INOPs See <Press Label> INOPs
ART INOPs See <Press Label> INOPs
BAP INOPs See <Press Label> INOPs
CPP CHK SOURCES
Numeric is replaced by -?-
INOP tone
Not all measurements or values required to perform the calculation are available. Check the
measurement sources.
CPP CHK UNITS
Numeric is replaced by -?-
The monitor has detected a conflict in the units used for this calculation. Check the unit settings.
CPP UNPLUGGED With the default profile settings, the CPP measurement is disabled in the adult profile and enabled in
the pediatric and neonatal profiles. When changing from a pediatric or neonatal profile to an adult
profile, this INOP can occur. Enable CPP in the adult profile to clear the INOP.
CVP INOPs See <Press Label> INOPs
FAP INOPs See <Press Label> INOPs
IC1 / IC2 INOPs See <Press Label> INOPs
ICP INOPs See <Press Label> INOPs
LAP INOPs See <Press Label> INOPs
P / P1 / P2 / P3 / P4 INOPs See <Press Label> INOPs
PAP INOPs See <Press Label> INOPs
PPV BAD <Press Label>
SIGNAL
The arterial pressure source selected for PPV is not providing a pulsatile signal.
PPV BAD SIGNAL
at Information Center
The arterial pressure source selected for PPV is not providing a pulsatile signal.
PPV CHK SOURCES The arterial pressure source selected for PPV is unplugged or switched off. When this INOP has
displayed for 1 minute PPV will be switched off.
<Press Label> ARTIFACT
Numeric questionable
A non-physiological event (flush or blood sample) is detected. A resulting limit alarm or non-pulsatile
INOP will be suppressed.
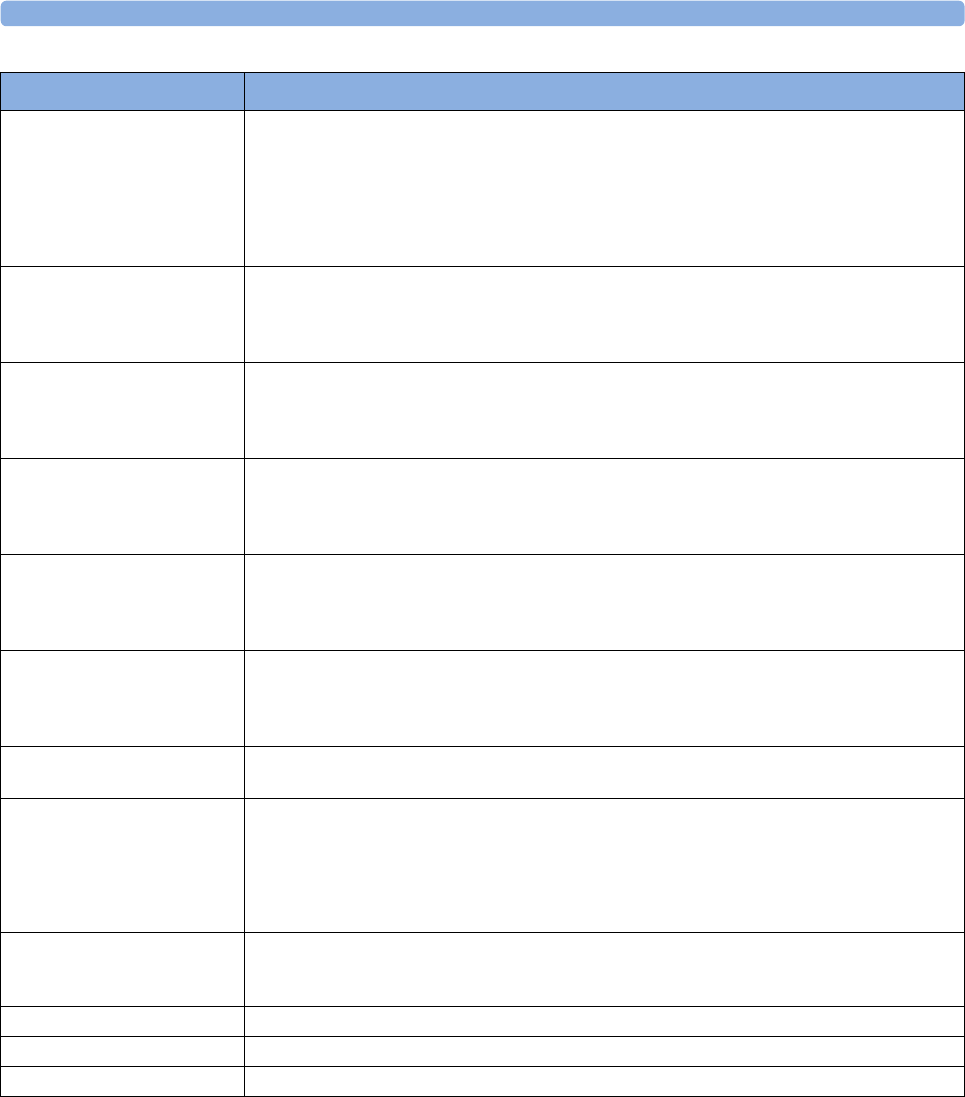
3 Patient Alarms and INOPs
81
<Press Label>
DEACTIVATED
INOP tone
A Pressure measurement label in the measurement device or extension has been deactivated, either by
connecting a Temp transducer in the shared Press/Temp socket, or by deactivating the label in the
Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either reconnect a Pressure transducer or reactivate the
measurement label in the Measurement Selection window.
<Press Label> EQUIP
MALF
Numeric is replaced by -?-
INOP tone
Contact your service personnel.
The pressure hardware is faulty.
<Press Label> NO
TRANSDUCER
Numeric is replaced by -?-
INOP tone
Make sure that the pressure transducer is connected to the measurement device or module.
If you silence this INOP, the measurement will be switched off.
<Press Label> NOISY
SIGNAL
Pulse numeric is replaced by -?-
INOP tone
This INOP can only arise when a pressure is selected as the pulse source. It occurs when the pulse
detector finds a pulse rate above 350bpm. This is usually caused by movement artifact or electrical
interference.
<Press Label> NON-
PULSATILE
Pulse numeric is replaced by -?-
INOP tone
This INOP can only arise when a pressure is selected as the pulse source. It occurs when the pulse rate
being measured is less than 25 beats per minute or the amplitude is less than three mmHg.
Check the catheter and connections to the patient.
<Press Label>
OVERRANGE
Numeric is replaced by -?-
INOP tone
Make sure that the measurement has been properly prepared and zeroed, and that the transducer is
level with the heart. If this INOP persists, try another transducer.
Possible causes are a measured pressure outside the allowed pressure range, or a broken wire to the
transducer.
<Press Label> REDUCE
SIZE
Increase the scale for the pressure wave.
<Press Label>
UNPLUGGED
INOP tone
A Pressure measurement label has been deactivated, either by unplugging a module, or by deactivating
the label in the Measurement Selection window.
The measurement automatically disappears from the display.
To switch the measurement on again, either replug the module or reactivate the measurement label in
the Measurement Selection window.
<Press Label>
ZERO+CHECK CAL
Numeric is replaced by -?-
Perform a zero and check the calibration of the transducer.
RAP INOPs See <Press Label> INOPs
UAP INOPs See <Press Label> INOPs
UVP INOPs See <Press Label> INOPs
INOP Message, Indication What to do
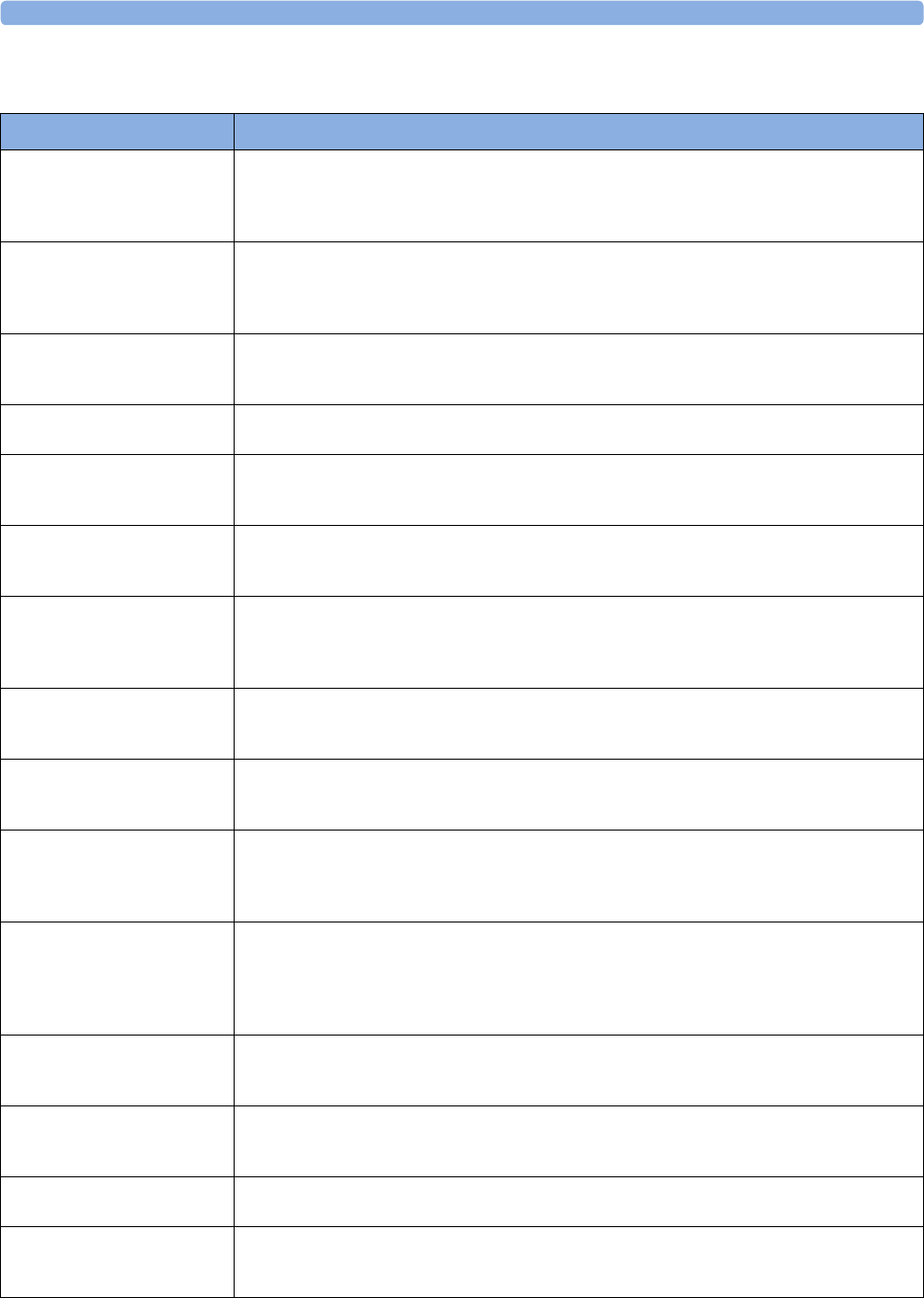
3 Patient Alarms and INOPs
82
CO2 INOPs
INOP Message, Indication What to do
!! CO₂ OCCLUSION
!!! CO₂ OCCLUSION
Numeric is replaced by -?-
INOP tone
The sample line or exhaust tube is blocked. Check the tubing, then disconnect and reconnect the
sample line. If the INOP persists, connect a new sample line.
CO₂ AUTO ZERO
Numeric is replaced by -?-
if the Autozero lasts >15 sec,
INOP tone sounds.
The automatic zero calibration is in progress. This typically takes 10 seconds. During this time the CO2
values may not be updated, or they may be replaced by -?-. Wait until the zero calibration is complete
to resume monitoring.
CO₂ CAL MODE
CO2 numeric displays current
CO2 value for accuracy check
Currently no calibration is running. Accuracy can be checked by placing the transducer on the two cells
of the calstick and starting calibration. To start monitoring, leave Cal. Mode.
CO2 CAL RUNNING
Numeric is replaced by -?-
Wait until calibration is finished.
CO₂ CHECK CAL
Numeric is replaced by -?-
INOP tone
The CO2 value is outside the measurement range. Perform an accuracy check for both calstick cells
and, if necessary, recalibrate the transducer.
CO₂ CHK ADAPTER
Numeric is replaced by -?-
INOP tone
Check that the sensor is connected to the airway adapter, clean the airway adapter, if necessary.
Perform a zero calibration. If the INOP persists, contact your service personnel.
CO₂ DEACTIVATED
INOP tone
The CO2 measurement label in the measurement device has been deactivated by deactivating the label
in the Measurement Selection window. The measurement automatically disappears from the
display. To switch the measurement on again, reactivate the measurement label in the Measurement
Selection window.
CO₂ EQUIP MALF
Numeric is replaced by -?-
INOP tone
The Measurement Extension is faulty. Unplug and replug the Multi-Measurement Module with
Extension. If you are using the mainstream method, unplug and replug the transducer or try another
transducer. If the INOP persists, contact your service personnel.
CO₂ FAILED CAL
Numeric is replaced by -?-
INOP tone
Make sure that the Cal cell was changed between CAL1 and CAL2. Repeat the calibration. If the
INOP reappears, try another transducer. If the INOP persists, contact your service personnel.
CO₂ NO SENSOR
from M3014A
Numeric is replaced by -?-
INOP tone
There is no CO2 sensor connected. If you silence this INOP the CO2 measurement will be switched
off.
CO₂ NO TRANSDUC
from mainstream CO2 (except
M3014A)
Numeric is replaced by -?-
INOP tone
There is no CO2 transducer connected. If you replace the transducer, the new transducer must be
calibrated. If you silence this INOP the CO2 measurement will be switched off.
CO₂ NO TUBING
Numeric is replaced by -?-
INOP tone
Either the sample line is disconnected, or an incorrect line is attached. Check the connection. If
necessary, connect another sample line (Use only the approved accessories).
If you silence this INOP, the measurement will be switched off.
CO₂ OVERRANGE
Numeric is replaced by -?-
INOP tone
The CO2 value is higher than the measurement range. If you suspect a false high value, contact your
service personnel.
CO₂ PUMP OFF
Numeric is replaced by -?-.
The pump has been switched off for fifteen minutes. To switch it on again, select Pump On in the
Setup CO₂ menu.
CO₂ PURGING
Numeric is replaced by -?-
INOP tone
The Filterline is being purged to remove an occlusion in the line or airway adapter. If the occlusion is
removed, the INOP will disappear. If not, the INOP CO₂ OCCLUSION is displayed.
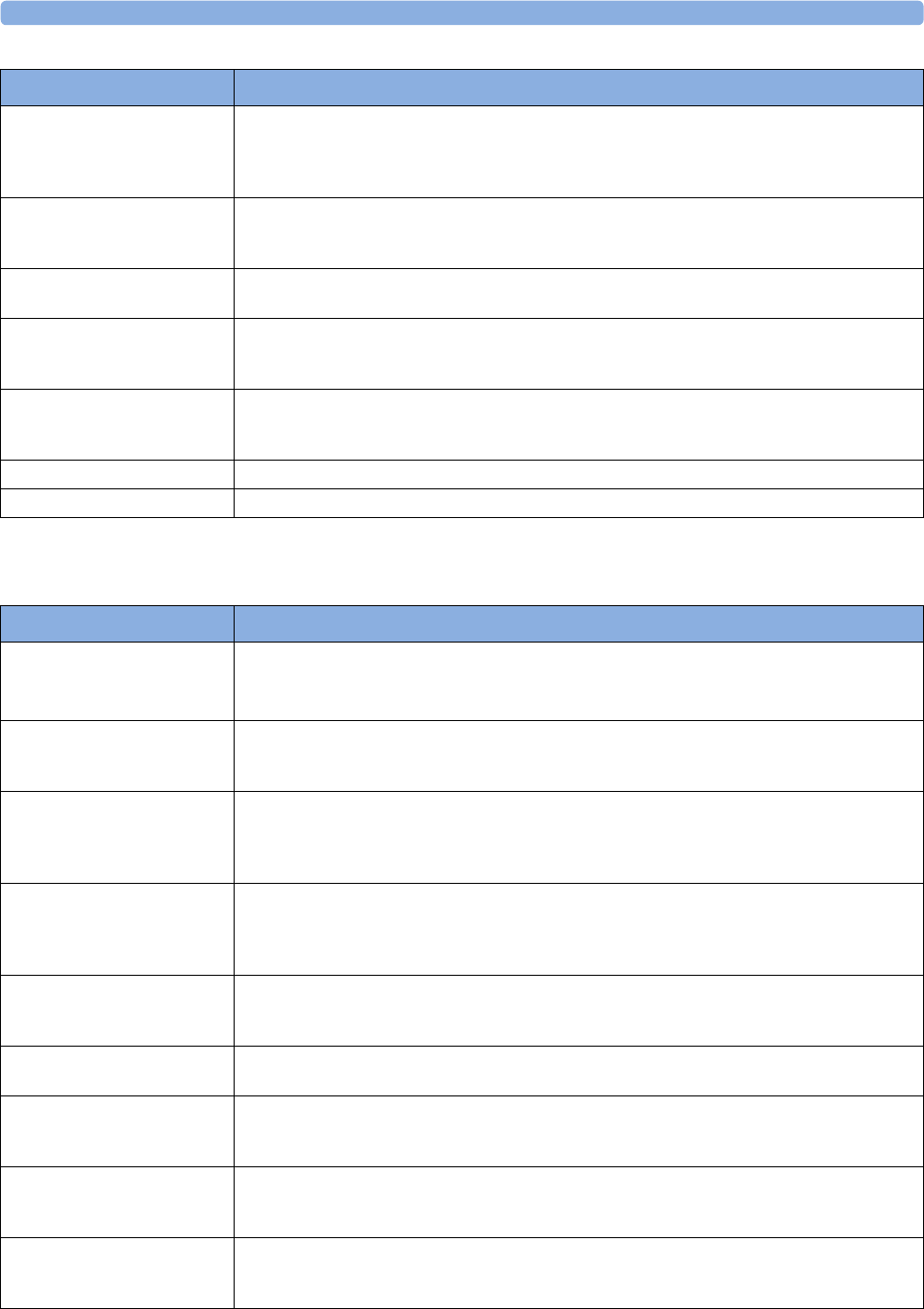
3 Patient Alarms and INOPs
83
SO2 INOPs
CO₂ SENS.WARMUP
Numeric is replaced by -?-
Microstream CO2: INOP tone
Mainstream CO2: no INOP tone
Wait until the sensor reaches operating temperature and the INOP disappears.
CO₂ UPDATE FW
Numeric is replaced by -?-
INOP tone
The software in the Measurement Extension does not match the software in the MMS. Contact your
service personnel.
CO₂ WAIT CAL2
Numeric is replaced by -?-
Calibration on the first calstick cell is complete. Place the transducer on the other calstick cell and start
the CAL2 calibration cycle.
CO₂ ZERO FAILED
Numeric is replaced by -?-
INOP tone
An error occurred during the last zero calibration. Check the airway adapter and clean, if necessary.
Perform another zero calibration. If the INOP persists, contact your service personnel.
CO₂ ZERO REQU'D
Numeric is replaced by -?-
INOP tone
Perform zero calibration for the CO2 sensor. If the INOP persists, contact your service personnel.
CO₂CHANGE SCALE The CO2 wave is clipped. Select a more appropriate wave scale to display the whole wave.
CO₂ZERO RUNNING Wait until zero calibration is finished.
INOP Message, Indication What to do
INOP Message, Indication What to do
<SO₂ Label> CAL FAILED
Numeric is replaced by -?-
INOP tone
The calibration failed. Check the catheter-to-Optical-Module connection. Manually restart the
calibration. Try another catheter and Optical Module. If the catheter is already inserted, perform an in-
vivo calibration.
<SO₂ Label> CAL MODE
Numeric is replaced by -?-
INOP tone
Pre-insertion calibration is complete, but the catheter tip is still inside the optical reference. The
catheter is now ready for insertion.
<SO₂ Label> CANNOT
MEAS
Numeric is replaced by -?-
INOP tone
The signal is out of the normal range, and no oxygen saturation can be derived. Perform an in-vivo
calibration. If the INOP persists, try another Optical Module and catheter.
<SO₂ Label> CONN
OPTMOD
Numeric is replaced by -?-
INOP tone
The Optical Module was disconnected during data storage. Reconnect the Optical Module for at least
20 seconds.
<SO₂ Label> EQUIP MALF
Numeric is replaced by -?-
INOP tone
The SO2/SvO2 Module or Optical Module is faulty. Unplug and replug the Optical Module and SO2/
SvO2 module. Exchange the modules. If the INOP persists, contact your service personnel.
<SO₂ Label> INCOMPAT.
INOP tone
The SO2 Module or Optical Module is not supported. Contact your service personnel.
<SO₂ Label> IN-VIVO CAL The in-vivo calibration is not yet complete. Lab values must be stored to the Optical Module to
complete the calibration. Either continue with the next steps of the current calibration or recall the
previous calibration.
<SO₂ Label> LOW LIGHT
Numeric is replaced by -?-
INOP tone
The optical signal levels are too low. Check that the catheter is either in the optical reference or
inserted into the patient. Check the catheter-to-Optical Module connection. If INOP persists, try
another catheter and Optical Module.
<SO₂ Label> NO OPTMOD
Numeric is replaced by -?-
INOP tone
Connect the Optical Module. If the INOP persists, try another Optical Module. Silencing this INOP
switches the measurement off.
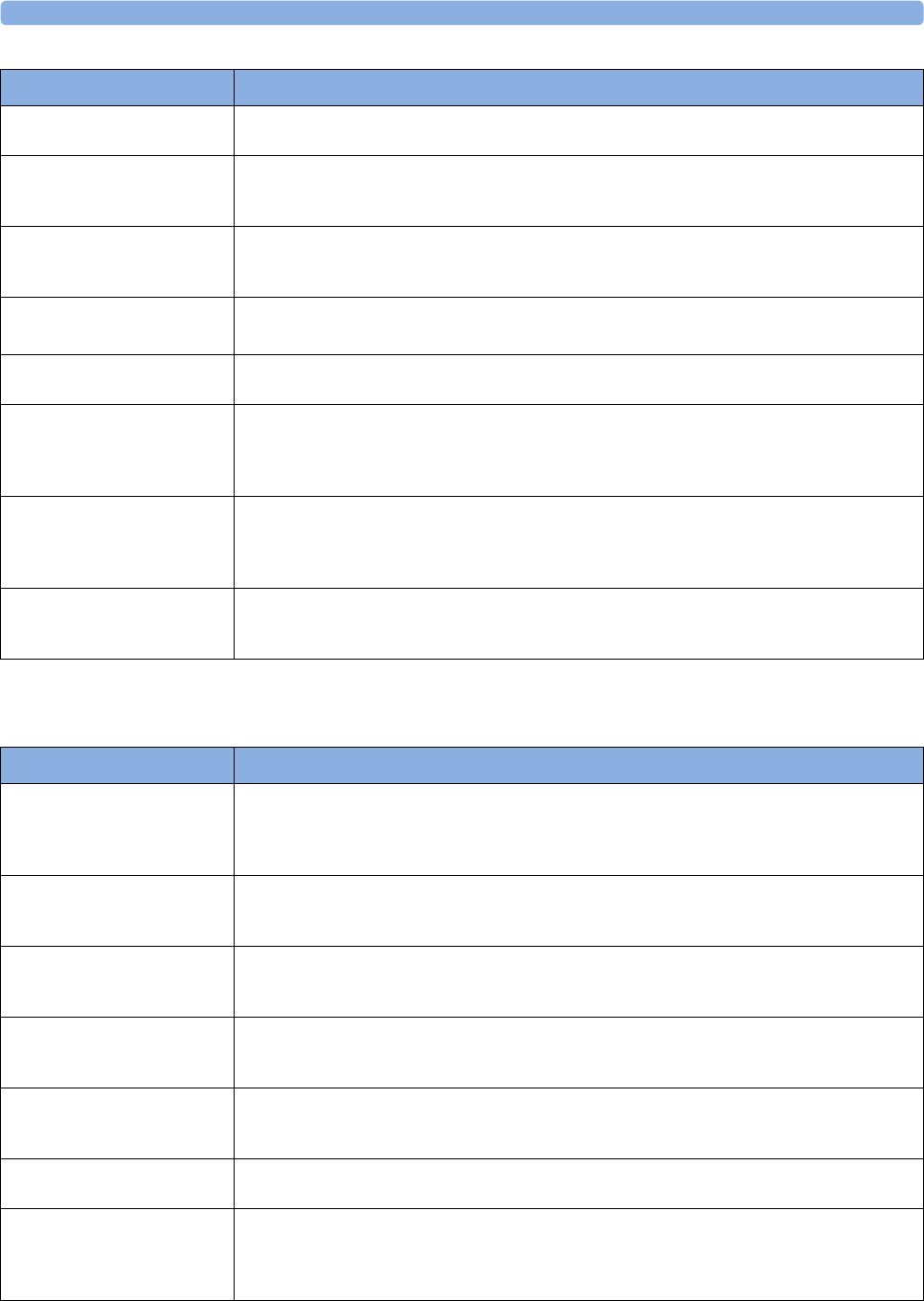
3 Patient Alarms and INOPs
84
C.O. INOPs
<SO₂ Label> OPTMOD
MALF
The Optical Module memory is faulty, and calibration data cannot be stored for transport or during
power failure. If this capability is needed, use another Optical Module.
<SO₂ Label> PRE-INS CAL
Numeric is replaced by -?-
INOP tone
The pre-insertion calibration is running. This typically takes one minute. During this time alarms are
switched off. Wait until the calibration is complete.
<SO₂ Label> UNPLUGGED
Numeric is replaced by -?-
INOP tone
Measurement switched on and SO2/SvO2 module unplugged from the rack.
<SO₂ Label> UPGRADE
INOP tone
The SO2 module is currently in upgrade mode.
Monitoring is not possible in this mode.
<SO₂ Label> WARMUP
Numeric is replaced by -?-
The Optical Module has not yet reached the operating temperature. Wait a few minutes until warm-up
is finished.
<SO₂ Label>CAL
REQUIRED
Numeric is replaced by -?-
INOP tone
There is no valid calibration data in the Optical Module. Perform either a pre-insertion or an in-vivo
calibration.
<SO₂ Label>CONFIG
ERROR
Numeric is replaced by -?-
INOP tone
The Optical Module has been configured to SaO2 Mode. Use Change to Venous in the setup
menu to reconfigure to venous saturation mode.
<SO₂ Label>LIGHT INTENS
Numeric is replaced by -?-
INOP tone
The intensity changed considerably since the last light intensity calibration. This may indicate that the
catheter tip is positioned against a blood vessel wall or that there is low blood flow. Reposition the
catheter (and perform a Light Intensity Calibration).
INOP Message, Indication What to do
INOP Message, Indication What to do
C.O. DEACTIVATED
INOP tone
The Cardiac Output measurement label in the measurement device has been deactivated by
deactivating the label in the Measurement Selection window. The measurement automatically
disappears from the display. To switch the measurement on again, reactivate the measurement label in
the Measurement Selection window.
C.O. EQUIP MALF
Numeric is replaced by -?-
INOP tone
There is a problem with the C.O. hardware. Contact your service personnel.
C.O. UNPLUGGED
Numeric is replaced by -?-
INOP tone
Plug in the C.O. module. Silencing this INOP switches off the measurement.
CCI NO BSA
CCI numeric unavailable
INOP tone
CCI cannot be calculated because the patient's body surface area is unknown. Enter the patient weight
and height to provide the BSA for CCI calculation.
CCO BAD PRESS SIGN
Numeric is replaced by -?-
INOP tone
The arterial pressure wave can currently not be used for pulse contour calculation for CCO or CCI
measurement. Possible causes are air bubbles in the tubing or a physiological condition, for example
severe arrhythmia.
CCO NO CALIBRATION
Numeric is replaced by -?-
The CCO measurement is currently not calibrated.
CCO NO <Press Label>
Numeric is replaced by -?-
INOP tone may sound
CCO/CCI cannot be calculated. Make sure that the pressure chosen in the Setup CCO menu under
CCO From matches the pressure measured with the arterial catheter for CCO measurement. A
pressure from an external device cannot be used. Select another pressure label, either ABP, Ao, ART,
BA P, FA P, or UAP.
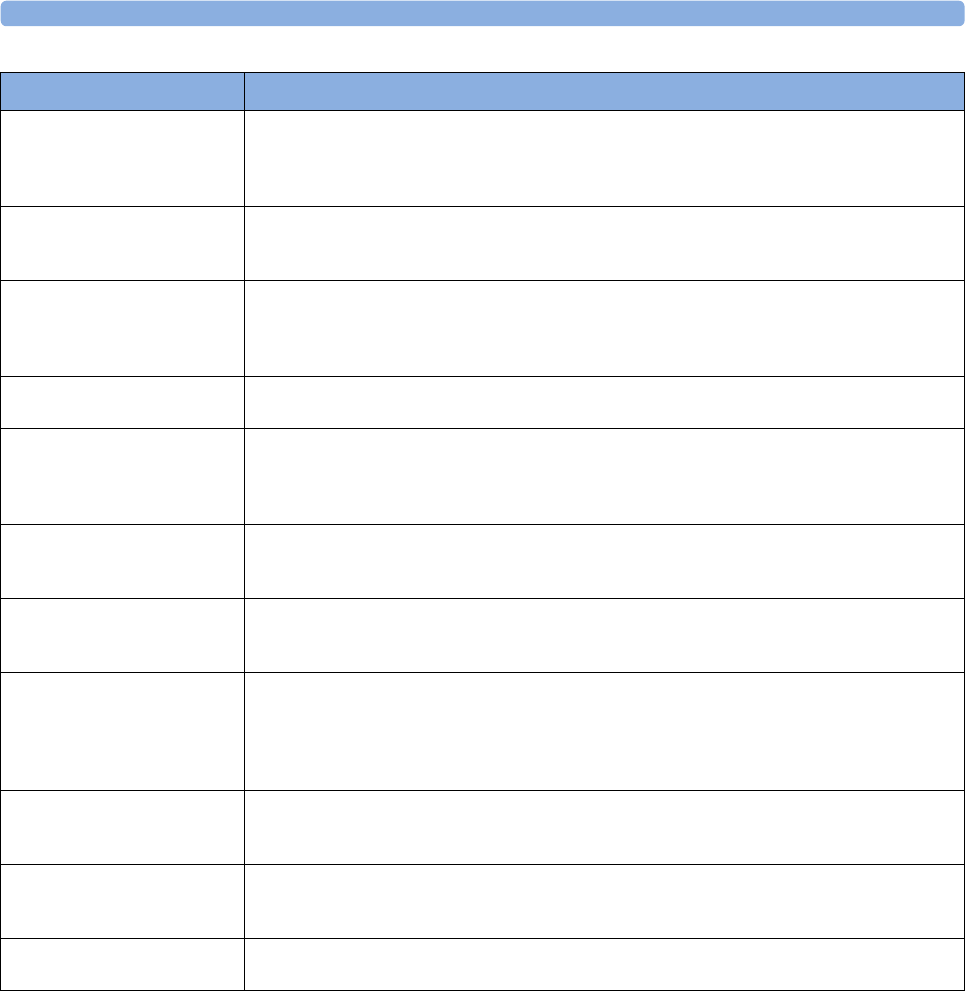
3 Patient Alarms and INOPs
85
CCO NO PRESS
at Information Center
CCO/CCI cannot be calculated. Make sure that the pressure chosen in the Setup CCO menu under
CCO From matches the pressure measured with the arterial catheter for CCO measurement. A
pressure from an external device cannot be used. Select another pressure label, either ABP, Ao, ART,
BA P, FA P, or UAP.
CCO NOT SUPPORTED
Numeric is replaced by -?-
INOP tone
A catheter for transpulmonary C.O. measurements has been unplugged and replaced with a Right
Heart C.O. catheter, or the measurement mode has been changed manually. Silencing this INOP
switches the measurement off.
CCO OVERRANGE
CCI OVERRANGE
Numeric is replaced by -?-
INOP tone
The measured CCO or CCI value is not within the specified range for CCO/CCI measurement.
CCO PRESS INVALID
at Information Center
The arterial pressure selected for pulse contour calculation for CCO is available but currently invalid.
Make sure the pressure transducer is connected and the zero calibration is valid.
CCO <Press Label>
INVALID
Numeric is replaced by -?-
INOP tone may sound
The arterial pressure selected for pulse contour calculation for CCO is available but currently invalid.
Make sure the pressure transducer is connected and the zero calibration is valid.
CCO PRESS OVERRANG
Numeric is replaced by -?-
INOP tone
The mean value of the arterial pressure values used for pulse contour calculation for CCO is below 0
mmHg or above 300 mmHg.
CCO PULSE OVERRANG
Numeric is replaced by -?-
INOP tone
The pulse rate of the pressure used for pulse contour calculation for CCO is below 30 bpm or above
240 bpm.
CCO RECALIBRATE
Numeric is replaced by -?-
The most recent CCO or CCI calibration was made over 8 hours ago or the arterial pressure
measurement used for CCO calculation has been zeroed after the CCO calibration was performed.
You should recalibrate CCO or CCI with transpulmonary C.O. measurements at least every 8 hours or
when the hemodynamic condition of the patient has changed. The pressure measurement must be
zeroed before a CCO calibration.
CCO/Tbl NO TRANSD.
Numeric is replaced by -?-
INOP tone
No transducer attached to the module or catheter disconnected.
Tblood NO TRANSDUC
Numeric is replaced by -?-
INOP tone
No transducer attached to the module or catheter disconnected.
Tblood OVERRANGE
Numeric is replaced by -?-
Tblood out of range 17°C - 43°C.
INOP Message, Indication What to do
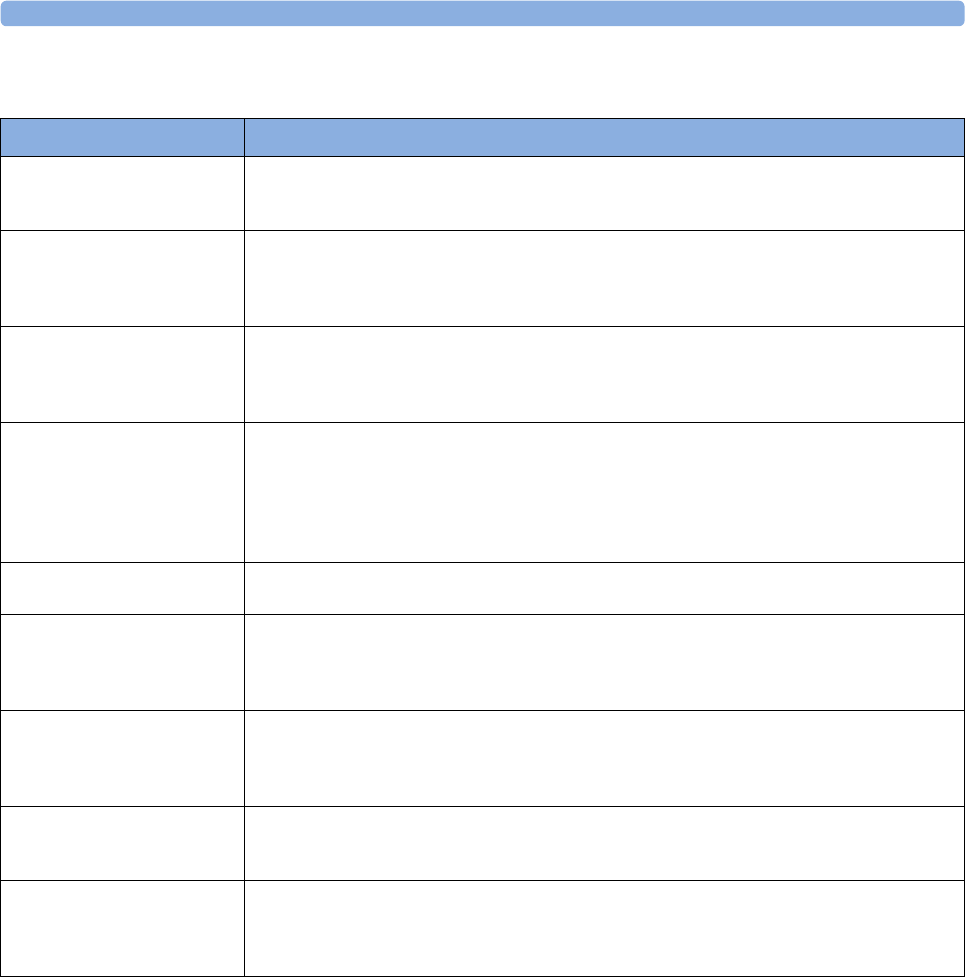
3 Patient Alarms and INOPs
86
tcGas INOPs
INOP Message, Indication What to do
<tcGas Label> CAL FAILED
Numeric is replaced by -?-
INOP tone
A calibration failed. Check the calibration unit, gas pressure, and tubing connections, then restart the
calibration. If the calibration has failed more than once, remembrane the transducer and restart the
calibration. If this INOP persists, contact your service personnel.
<tcGas Label> CAL
REQUIRD
Numeric is replaced by -?-
INOP tone
Calibration is required before applying the transducer to the patient.
Insert a membraned transducer into the calibration chamber on the module, connect the calibration
unit to the calibration chamber, open the gas valve and start the calibration. If this INOP occurs
during a calibration, there may be a module or transducer malfunction: contact your service personnel.
<tcGas Label> CAL
RUNNING
Numeric displays first -?-, then
numeric is displayed with a ?
Wait until the tcpO2/tcpCO2 calibration is finished.
<tcGas Label> CHANGE
SITE
If Heat Switch Off is
configured to Yes, numeric is
replaced by -?-
INOP tone
Site Timer has timed out. Change the application site to avoid skin burns. To reset the Site Timer,
either calibrate and change the measurement site, or change the measurement site and reset the Site
Timer manually by selecting the appropriate site time from the Setup tcGas menu.
<tcGas Label> CHECK
TIME
Site Timer due to time out in 15 minutes or less.
<tcGas Label> EQUIP
MALF
Numeric is replaced by -?-
INOP tone
There is a malfunction in the transducer or module. Connect another transducer. If this INOP persists,
contact your service personnel.
<tcGas Label> NO
TRANSDUC
Numeric is replaced by -?-
INOP tone
No transducer is connected to the tcpO2/tcpCO2 module. Silencing the alarm switches off the
measurement.
<tcGas Label>
STABILIZING
Numeric is replaced by ?
The transducer has not yet reached the selected temperature and/or skin hyperemization is not yet
finished. This INOP will disappear within three minutes.
<tcGas Label>
UNPLUGGED
Numeric is replaced by -?-
INOP tone
The measurement is switched on but the module is unplugged.
The measurement automatically disappears from the display. Silencing this INOP switches off the
measurement.
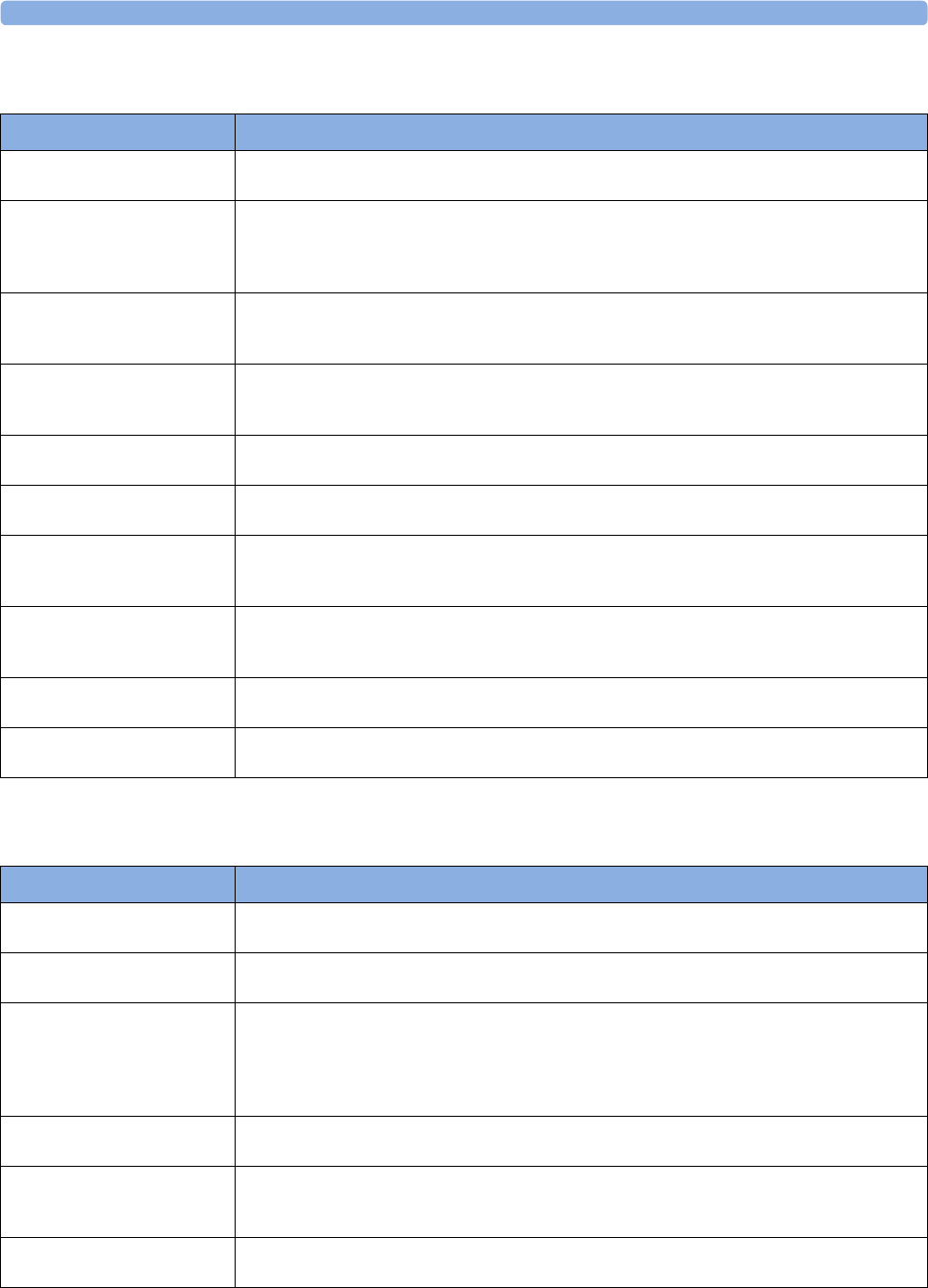
3 Patient Alarms and INOPs
87
EEG INOPs
BIS INOPs
INOP Message, Indication What to do
EEG EQUIP MALF
INOP tone
The EEG hardware is faulty. Contact your service personnel.
EEG IMPEDANCE HIGH
EEG1 IMPED. HIGH
EEG2 IMPED. HIGH
The signal electrode in one or both channels exceeds the user-selected impedance limit, or the
impedance of a single electrode exceeds the limit. Check the impedance. If the impedance is too high,
reconnect the electrodes according to the EEG monitoring setup guidelines. If the INOP persists,
contact your service personnel.
EEG LINE NOISE
EEG1 LINE NOISE
EEG2 LINE NOISE
Excessive line noise has been detected in either channel EEG1 or EEG2, or in both EEG channels.
Keep all cables together and away from metallic bodies, other cables & radiated fields.
EEG MUSCLE NOISE
EEG1MUSCLE NOISE
EEG2MUSCLE NOISE
Too much power above 30 Hz has been detected in channel EEG1 or EEG2, or both.
Check the Electrode-to-Skin Impedance and reposition the electrode away from possible muscle
activity, if necessary.
EEG NO TRANSDUC
INOP tone
The trunk cable is disconnected from the EEG plug-in module. Reconnect the trunk cable. Silencing
this INOP switches the measurement off.
EEG UNPLUGGED
INOP tone
Plug in module. Silencing this INOP switches off the measurement.
EEG1 LEAD OFF <n>
EEG2 LEAD OFF <n>
[n = electrode]
Reconnect specified electrode.
EEG1 LEAD OFF
EEG2 LEAD OFF
at Information Center
One or more electrodes are not connected. Check in the EEG Impedance / Montage window on
the monitor which electrode(s) are affected and reconnect the electrodes.
EEG1 LEADS OFF
EEG2 LEADS OFF
Two or more electrodes are not connected. Check in the EEG Impedance / Montage window
which electrodes are affected and reconnect the electrodes.
EEG1 OVERRANGE
EEG2 OVERRANGE
Input signal is too high in one or both channels. This is usually caused by interfering signals such as
line noise or electrosurgery.
INOP Message, Indication What to do
BIS CABLE INCOMPAT
INOP tone
The semi-reusable sensor cable connected is unknown or not supported by your software revision.
Replace it with a Philips-supported sensor cable.
BIS CABLE USAGE
INOP tone
The semi-reusable sensor cable has exceeded the maximum number of uses. Replace the cable.
BIS DSC DISCONN
INOP tone
DSC is not properly connected OR either DSC or BIS engine may be faulty.
Make sure that the DSC is properly connected to the BIS Engine. If INOP persists, replace DSC with
a known good one of the same type.
If INOP persists replace BIS engine.
Silencing this INOP switches the measurement off.
BIS DSC INCOMPT
INOP tone
DSC is not supported by the BIS engine or new DSC connected to an old BIS engine. A software
upgrade may be required. Contact your service personnel.
BIS DSC MALFUNC Electrocautery used during self-test OR malfunction in the DSC hardware.
Make sure not to use electrocautery during the self-test procedure. Disconnect and reconnect the DSC
to the BIS engine. If the INOP persists, replace the DSC or contact your service personnel.
BIS DSC UPDATE
INOP tone
DSC update currently being carried out. This INOP will disappear when the DSC update is finished.
Do not disconnect the DSC during the update. No action is needed.
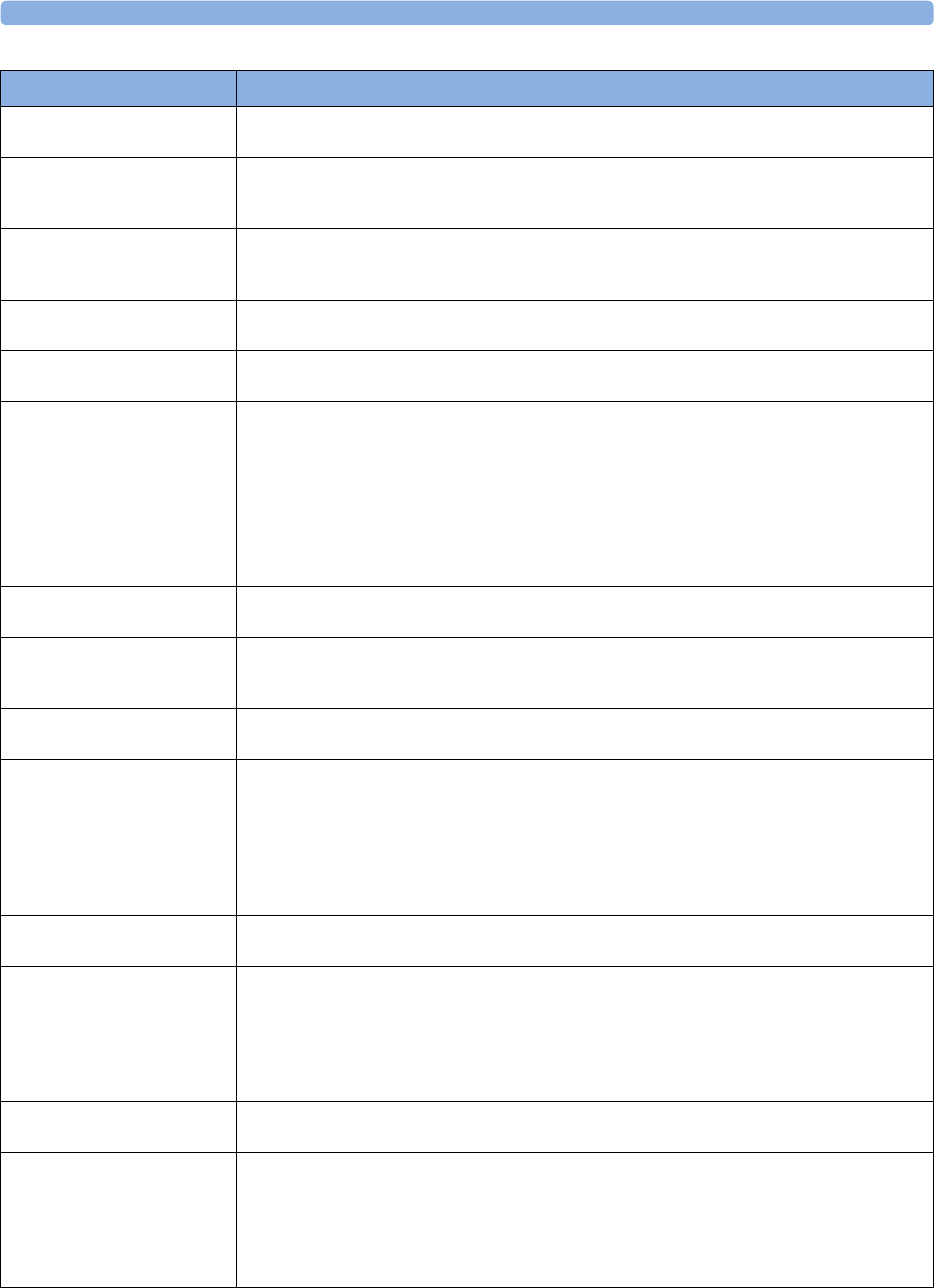
3 Patient Alarms and INOPs
88
BIS ELECTR. DISC.
INOP tone
One or more electrodes are not connected to the semi-reusable sensor cable. Check all electrode
connections.
BIS ENGINE DISCONN
INOP tone
BIS engine not connected OR Module Cable defective.
Make sure that the Module Cable is properly connected. If INOP persists, replace the Module Cable.
Silencing this INOP switches the measurement off.
BIS ENGINE INCOMPT
INOP tone
BIS engine software is not supported. A software upgrade may be required. Contact your service
personnel.
MP20/30 - BIS engine not supported.
BIS ENGINE MALFUNC
INOP tone
Malfunction in the BIS engine hardware. Disconnect and reconnect the BIS engine. If the INOP
persists, replace BIS engine.
BIS EQUIP MALF
INOP tone
There is a malfunction in the BIS hardware. Unplug and replug the BIS module. If the INOP persists,
contact your service personnel.
BIS HIGH IMPEDANCE
INOP tone may sound
Impedance of one or more electrode(s) is above the valid range, most often caused by bad skin
preparation. Check the sensor montage and press the electrode pads firmly. If this INOP persists,
replace the sensor(s) in question using correct skin preparation.
If INOP persists, contact your service personnel.
BIS IMPEDANCE CHCK
INOP tone may sound
The Cyclic Impedance check is running. It will stop automatically if all impedances are within the valid
range. If any electrodes do not pass the impedance test, check the sensor montage and press the
electrode pads firmly.
To manually stop the Cyclic Impedance Check, select Cyclic Check off in the Setup BIS menu.
BIS ISOELECTRC EEG No discernible EEG activity is detected for longer than one minute.
Check the patient. Check that the electrodes are properly connected.
BIS LEAD OFF
INOP tone may sound
One or more electrodes have no skin contact and therefore impedances cannot be measured. Check
the sensor montage and press the electrode pads firmly.
If this INOP persists, replace the sensor(s) in question, using correct skin preparation.
BIS OVERCURRENT
INOP tone
Unplug and replug the BIS module or, f or the MP20/MP30, disconnect and reconnect the BISx from
the Interface board. If the INOP persists, contact your service personnel.
BIS SENSOR DISCONN
INOP tone
The sensor is not properly connected to the patient interface cable (PIC) and/or the PIC is not
properly connected to the DSC or BISx, or the sensor or PIC or DSC or BISx may be faulty.
Check all the connections.
Disconnect and reconnect the sensor, PIC, DSC, BISx.
If the INOP persists, replace the sensor.
If the INOP persists, replace PIC. If INOP persists, contact your service personnel.
Silencing this INOP switches the measurement off.
BIS SENSOR INCOMPT
INOP tone
Unsupported sensor connected or sensor type unknown or not supported by your software revision.
Replace the sensor, using only Philips supported sensors.
BIS SENSOR MALFUNC
INOP tone
Malfunction in the sensor hardware, most often caused by liquids permeating into the connectors OR
patient interface cable (PIC) or DSC or BISx may be faulty.
Replace the sensor. Manually initiate a Cyclic Impedance Check. Make sure all electrodes pass the test.
Make sure that the both sides of the PIC connector (between PIC and sensor) are dry. If you are not
sure that the connector is dry, replace the PIC until it has dried. If this INOP persists, contact your
service personnel.
BIS SENSOR USAGE
INOP tone
Excessive sensor usage. Replace sensor.
A Cyclic Impedance Check will start automatically.
BIS SQI < 15% (INOP tone)
OR
BIS SQI < 50% (no INOP
tone)
If the signal quality is below 50%, BIS numerics cannot be reliably derived.
If the signal quality is below 15%, no BIS numerics can be derived.
This may occur as a result of artifacts such as those generated from motion or the presence of
electrocautery devices. Make sure the sensor is properly attached to the patient. Manually initiate a
Cyclic Impedance Check. Make sure all electrodes pass the test. Make sure the patient is completely
relaxed (even small motions of the facial muscles affect the signal quality).
INOP Message, Indication What to do
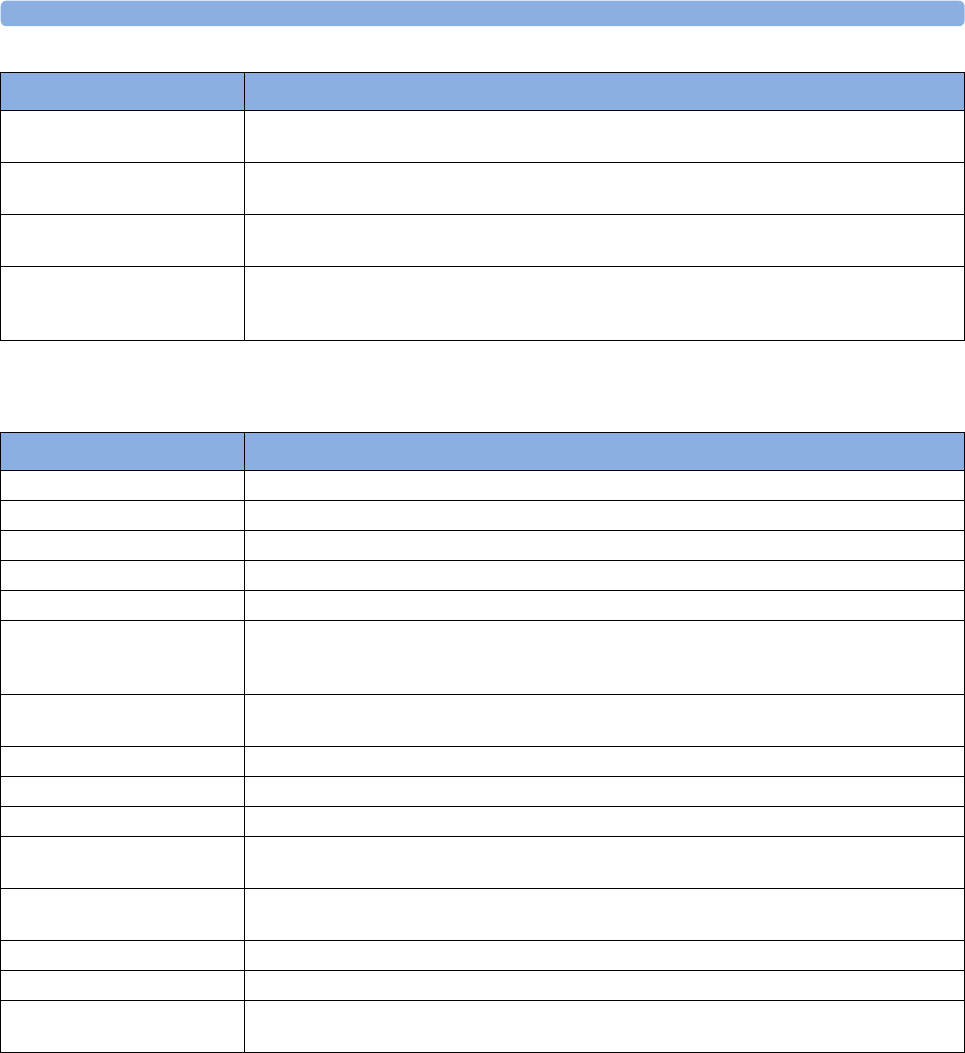
3 Patient Alarms and INOPs
89
Spirometry INOPs
BIS UNPLUGGED
INOP tone
Plug in the BIS module. Silencing this INOP switches off the measurement.
BISx DISCONNECTED
INOP tone
The BISx is not connected to the BIS module or the BIS interface board. Silencing this INOP switches
the measurement off.
BISx INCOMPATIBLE
INOP tone
The BISx software is not compatible with the BIS module or with the MP20/MP30 monitor software.
A software upgrade may be required. Contact your service personnel.
BISx MALFUNCTION
INOP tone
The BISx is faulty. Disconnect and reconnect it to the module or BIS interface board. If the INOP
persists, replace the BISx.
MP20/MP30 - Malfunction on interface board. If the INOP persists, contact your service personnel.
INOP Message, Indication What to do
INOP Message, Indication What to do
AWFCHANGE SCALE Airway flow signal exceeds range of selected scale. Adjust scale to display complete wave.
AWPCHANGE SCALE Airway pressure signal exceeds range of selected scale. Adjust scale to display complete wave.
AWVCHANGE SCALE Airway volume signal exceeds range of selected scale. Adjust scale to display complete wave.
SPIRO ALARMS SUPPR Alarming is suppressed for the spirometry module.
SPIRO CANNOT MEAS Measurement is at its limit, e.g. ambient pressure out of range.
SPIRO GAS COMPENS? Gas compensation is set to Gas Analyzer but not all gases necessary for compensation are
measured by a gas monitor. Some of the fall-back values provided by the user are used. Measurement
accuracy might be reduced.
SPIRO INCOMPATIBLE Module revision not compatible with the host monitor software revision. Contact your service
personnel.
SPIRO MALFUNCTION Module failure detected. Contact your service personnel.
SPIRO NO BREATH No breath was detected for more than 25 seconds. Breath derived numerics are not available.
SPIRO NO SENSOR No sensor detected. Make sure the correct sensor is attached to the breathing circuit.
SPIRO PATIENT CAT. Mismatch of patient size configured in the host monitor and sensor type plugged into the module.
Check the instructions on selecting the correct sensor in the chapter on Spirometry.
SPIRO PURGE FAILED The purge operation could not be completed successfully. Check for kinked sensor tubings, hard
occlusions and make sure that the pump is running and all valves are switching.
SPIRO PURGING A purge operation is in progress - no data update on the screen. Wait until purge is complete.
SPIRO UNKN. SENSOR An unknown sensor ID code was detected. Use only the sensors listed in the Accessories chapter.
SPIRO UPGRADE The module is running a firmware upgrade. Wait until upgrade is completed before resuming
monitoring.
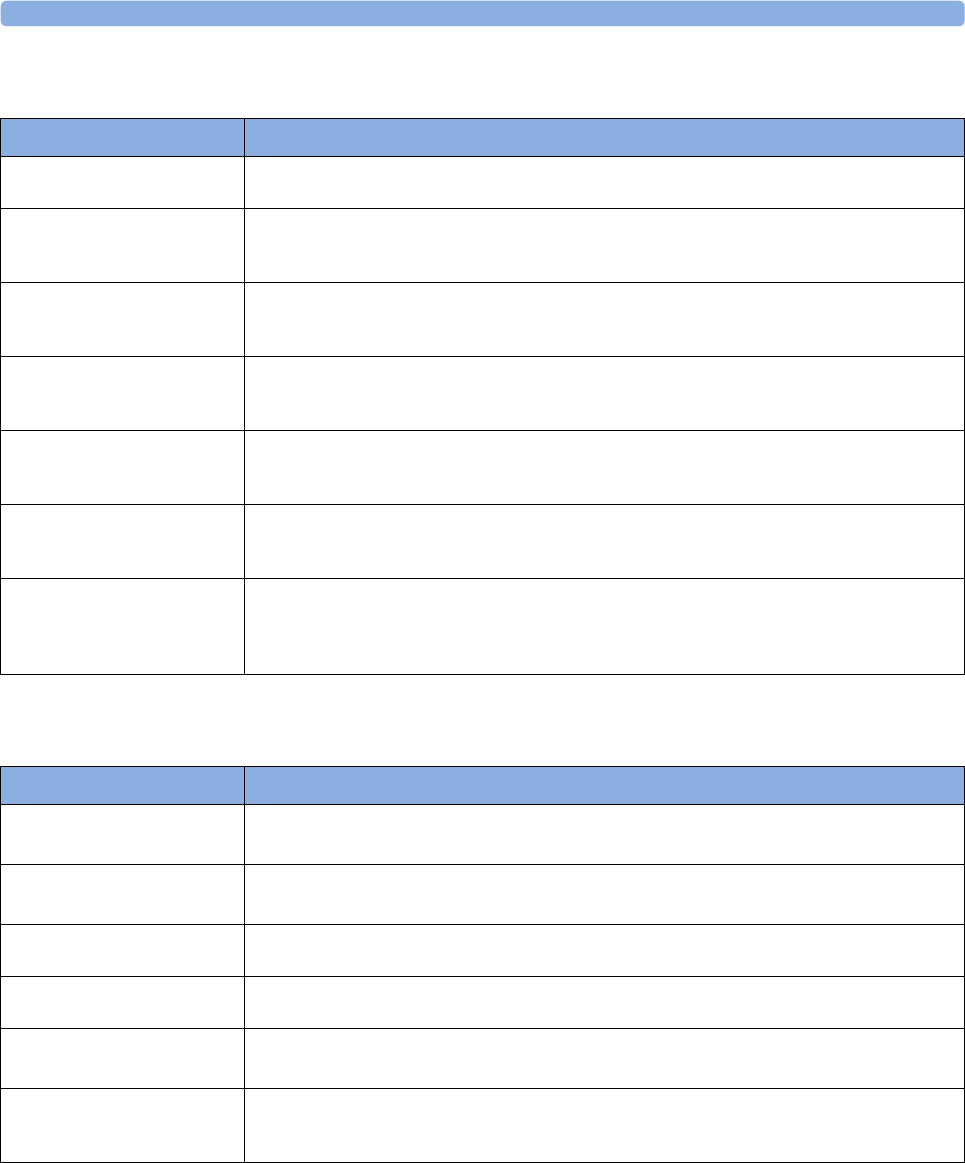
3 Patient Alarms and INOPs
90
VueLink INOPs
IntelliBridge INOPs
INOP Message, Indication What to do
VueLink ALARM
at Information Center
A technical alarm is present on the VueLink module. The INOP text on the monitor is defined by the
VueLink device driver.
<VueLink Option> CHECK
SETUP
INOP tone
No information was received from the external device. The device may be switched off or
disconnected.
VueLink INOP abbreviations may differ slightly depending on the device category.
<VueLink Option> CHK
CABLE
INOP tone
No cable or the wrong cable connected to the VueLink module, or incorrect device selected. Silencing
this INOP switches the measurement off.
VueLink INOP abbreviations may differ slightly depending on the device category.
<VueLink Option> CHK
CONF.
INOP tone
The wrong external device has been selected on the VueLink module, or the external device has not
been correctly setup, or the wrong cable has been used to connect the device to the VueLink module.
VueLink INOP abbreviations may differ slightly depending on the device category.
<VueLink Option> EQUIP
MALF
INOP tone
Malfunction in the VueLink module. If this message appears repeatedly, the module must be replaced.
Contact your service personnel.
VueLink INOP abbreviations may differ slightly depending on the device category.
<VueLink Option> NO
CONFIG
INOP tone
The VueLink module has not been configured during installation. The installation process should be
completed by either your biomedical engineering department or the Philips service engineer.
VueLink INOP abbreviations may differ slightly depending on the device category.
<VueLink Option>
UNPLUGGED
INOP tone
The VueLink module has been unplugged from the rack, or the whole rack has been disconnected.
The measurement automatically disappears from the display. Silencing this INOP switches off the
measurement.
VueLink INOP abbreviations may differ slightly depending on the device category.
INOP Message, Indication What to do
DEVICE CHECK CONF.
INOP tone
Device identification completed, but communication could not be established due to error.
IntelliBridge INOP abbreviations may differ slightly depending on the device category.
DEVICE CHECK SETUP
INOP tone
Device identification completed, but communication could not be established due to timeout.
IntelliBridge INOP abbreviations may differ slightly depending on the device category.
DEVICE DEMO DATA
INOP tone
The device connected to the IntelliBridge module reports demo data but the monitor is not in DEMO
mode.
DEVICE REAL DATA
INOP tone
The monitor is in DEMO mode but the device connected to the IntelliBridge module reports data that
are not flagged as demo data.
DEVICE UNSUPPORTED
INOP tone
Device identification completed, but no appropriate device driver installed.
IntelliBridge INOP abbreviations may differ slightly depending on the device category.
<EC10 / EC40> EQUIP
MALF
INOP tone
Malfunction in the IntelliBridge module. If this message appears repeatedly, the module must be
replaced. Contact your service personnel.
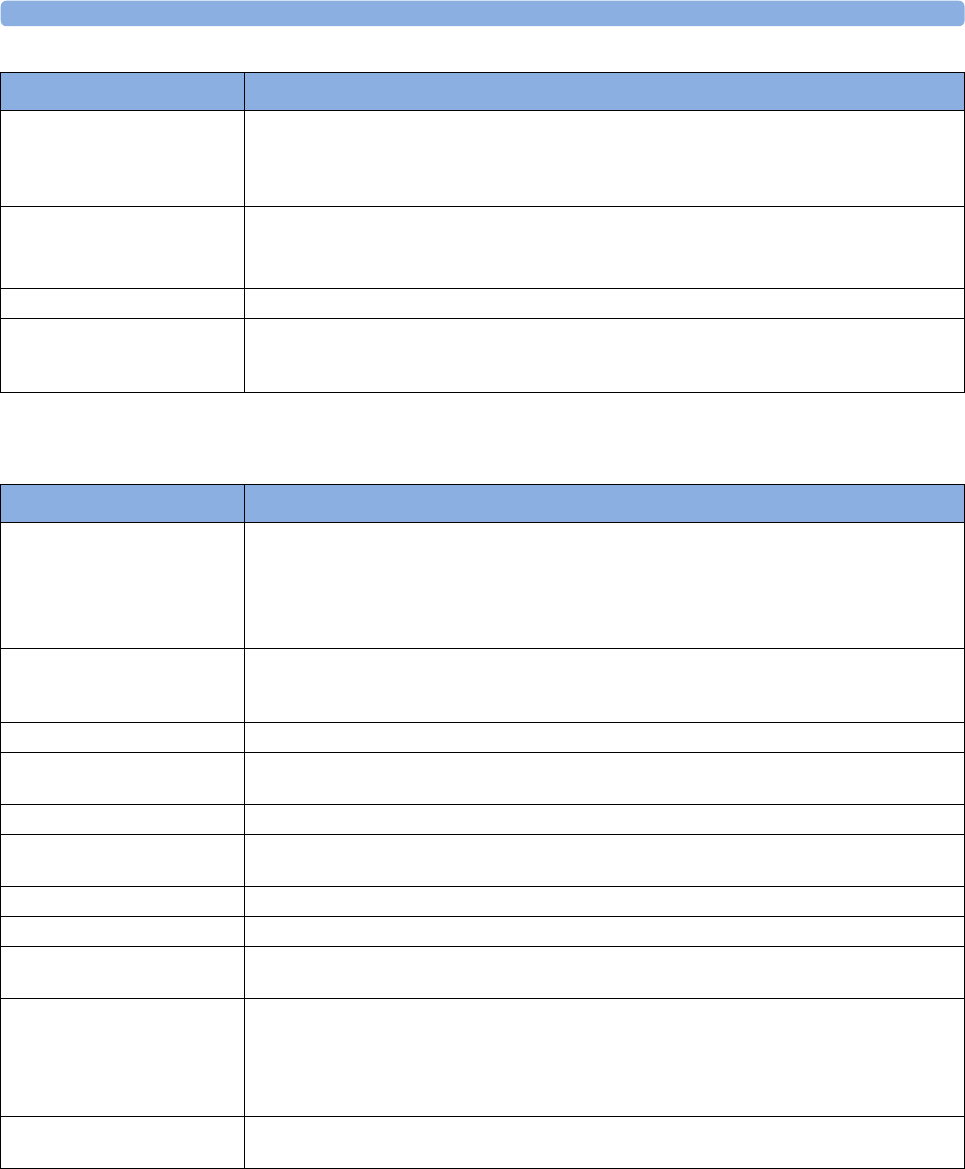
3 Patient Alarms and INOPs
91
Telemetry INOPs
EC10 INOP
!! EC10 INOP
!!! EC10 INOP
at Information Center
A technical alarm is present on the IntelliBridge EC10 module.
On the monitor the indication is a red (!!!), yellow (!!) or cyan alarm lamp (as appropriate) and an INOP
text that is defined by the IntelliBridge EC10 device driver.
<External Device>
UNPLUGGED
INOP tone
The IntelliBridge module has been unplugged from the rack, or the whole rack has been disconnected.
Silencing this INOP switches off the measurement.
IntelliBridge INOP abbreviations may differ slightly depending on the device category.
NO DEVICE DATA Communication with connected device has been lost.
TEXT UPLOAD FAILED
INOP tone
Incoming text from the IntelliBridge modules exceeds the maximum limit. Try unplugging one of the
IntelliBridge modules. If the INOP occurs repeatedly contact your service personnel; a software
upgrade may be necessary.
INOP Message, Indication What to do
INOP Message, Indication What to do
!! REPLACE BATT. T
!!!REPLACE BATT. T
Severe yellow/red INOP tone
During this INOP, alarms cannot
be paused or switched off.
The battery in the telemetry device is almost empty and must be replaced.
!! TELE INOP
!!! TELE INOP
Severe yellow/red INOP tone
Check for further details at the Information Center or in the Telemetry Data window on the monitor.
BATTERY LOW T The battery in the Telemetry device is low and must be replaced soon.
Check ECG Settings
INOP tone
Synchronization of ECG settings between the monitor and Information Center has failed. Check that
the ECG settings in use are appropriate.
!!CHECK ECG SOURCE Both the telemetry device and the monitor have valid ECG signals
Chk SpO₂T Settings
INOP tone
Synchronization of SpO2T settings between the monitor and Information Center has failed. Check
that the SpO2T settings in use are appropriate.
INVALID LEADSET The leadset plugged in cannot be used with the telemetry device.
LEADSET UNPLUGGED The leadset has been unplugged from the telemetry device.
NO ECG SOURCE A telemetry device is paired with the monitor but the Information Center is not detecting a valid ECG
signal from either of them.
!!TELE DISCONNECT
!!!TELE DISCONNECT
INOP tone
Telemetry transceiver was disconnected or short range radio link was lost.
For cable connections; check Telemetry interface, cable connection and setup.
For short range radio connections: if the telemetry transceiver has not moved out-of-range, check for
interference sources close to the monitor (bluetooth devices, DECT phones, cellular phones,
microwaves, etc.). If this INOP persists, ask your service personnel to survey the interference sources.
Tele Sync Unsupp.
INOP tone
The MMS in use does not support synchronization of ECG and SpO2 settings between the monitor
and central station after a telemetry device has been paired. Use an MMS with revision E.0 or above.
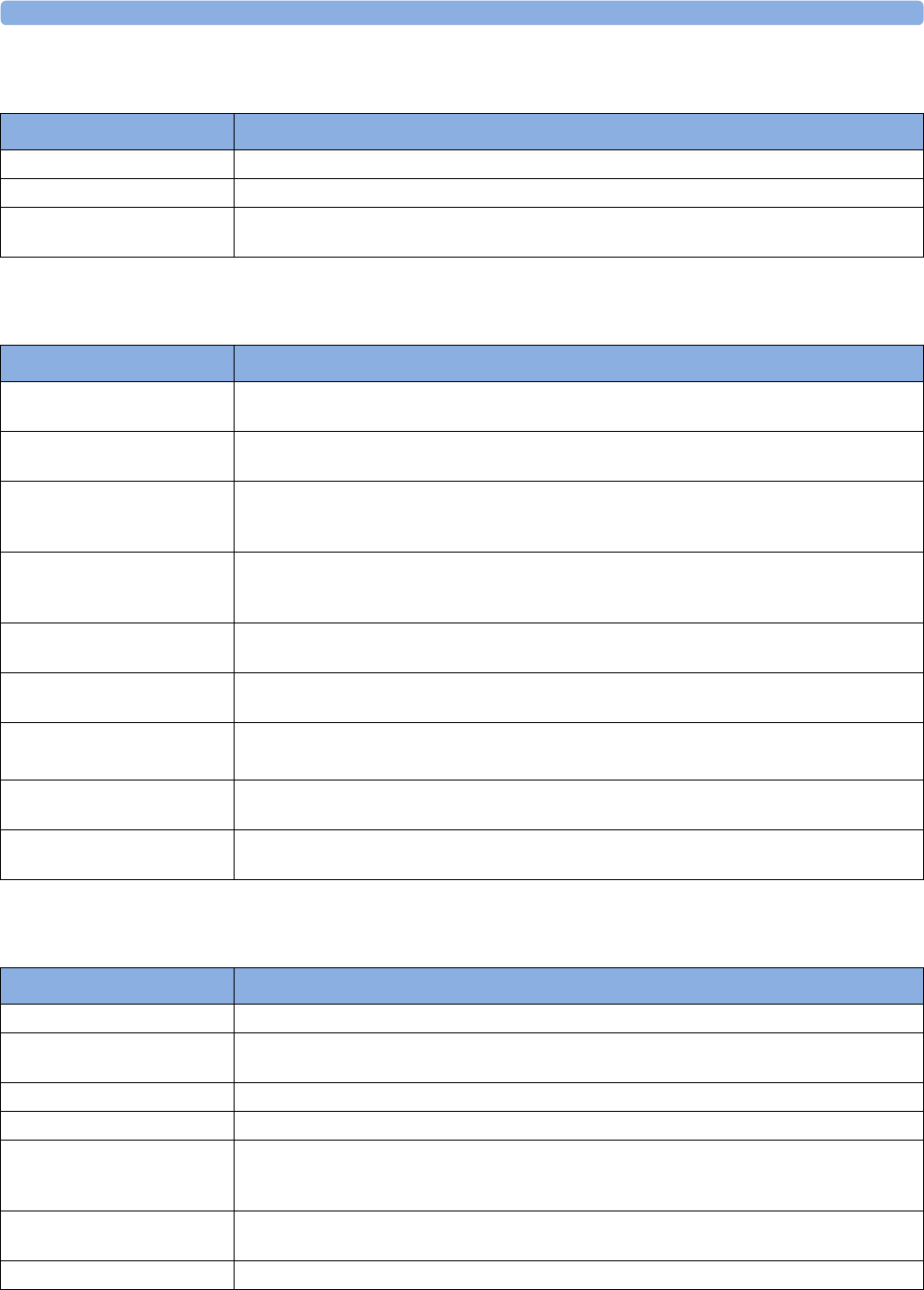
3 Patient Alarms and INOPs
92
ProtocolWatch INOPs
Calculated Values INOPs
Cableless Measurement Device INOPs
INOP Message, Indication What to do
PW In Conflict There is a patient information mismatch which has not yet been resolved (>15 minutes).
PW: Check Settings Contact your service personnel. Settings could not be loaded or interpreted correctly.
PW:Action Required The protocol currently running requires a user response. Check which pop-up window is displayed and
provide the appropriate response.
INOP Message, Indication What to do
Sp-vO₂ CHK SOURCES
Numeric is replaced by -?-
Not all measurements or values required to perform the calculation are available. Check measurement
sources.
Sp-vO₂ CHK UNITS
Numeric is replaced by -?-
The monitor has detected a conflict in the units used for this calculation. Check the unit settings.
SVR CHK SOURCES
SVRI CHK SOURCES
Numeric is replaced by -?-
Not all measurements or values required to perform the calculation are available. Check measurement
sources.
SVR CHK UNITS
SVRI CHK UNITS
Numeric is replaced by -?-
The monitor has detected a conflict in the units used for this calculation. Check the unit settings.
SVR SET CVP USED
SVRISET CVP USED
A CVP value is required for this calculation, but is not currently being measured. The monitor is using
the CVP value preset in the Setup SVR menu.
ΔSpO₂ CHK SOURCES
Numeric is replaced by -?-
Not all measurements or values required to perform the calculation are available. Check measurement
sources.
ΔSpO₂ CHK UNITS
Numeric is replaced by -?-
The monitor has detected a conflict in the units used for this calculation. Check the unit settings.
ΔTemp CHK SOURCES
Numeric is replaced by -?-
Not all measurements or values required to perform the calculation are available. Check measurement
sources.
ΔTemp CHK UNITS
Numeric is replaced by -?-
The monitor has detected a conflict in the units used for this calculation. Check the unit settings.
INOP Message, Indication What to do
cl NBP Batt Empty The remaining battery time of the NBP Pod is below 30 minutes. Change the battery.
cl NBP Batt Incomp The battery in use with the NBP Pod is incompatible. Replace it with one approved for use with the
NBP Pod.
cl NBP Batt Low The remaining battery time of the NBP Pod is below 2 hours.
cl NBP Batt Malf There is a malfunction in the NBP Pod's battery system. Contact your service personnel.
cl NBP Batt Temp The temperature of the battery in the NBP Pod is critically high. Check that the Pod is not covered or
exposed to a heat source. If the INOP persists, remove the Pod from the patient and contact your
service personnel.
cl NBP Check Batt The battery in the NBP Pod is nearing the end of its useful life. Only 50 charge/discharge cycles
remain. Contact your service personnel to replace the battery.
cl NBP Disconnect The NBP Pod has lost the connection to the monitor.
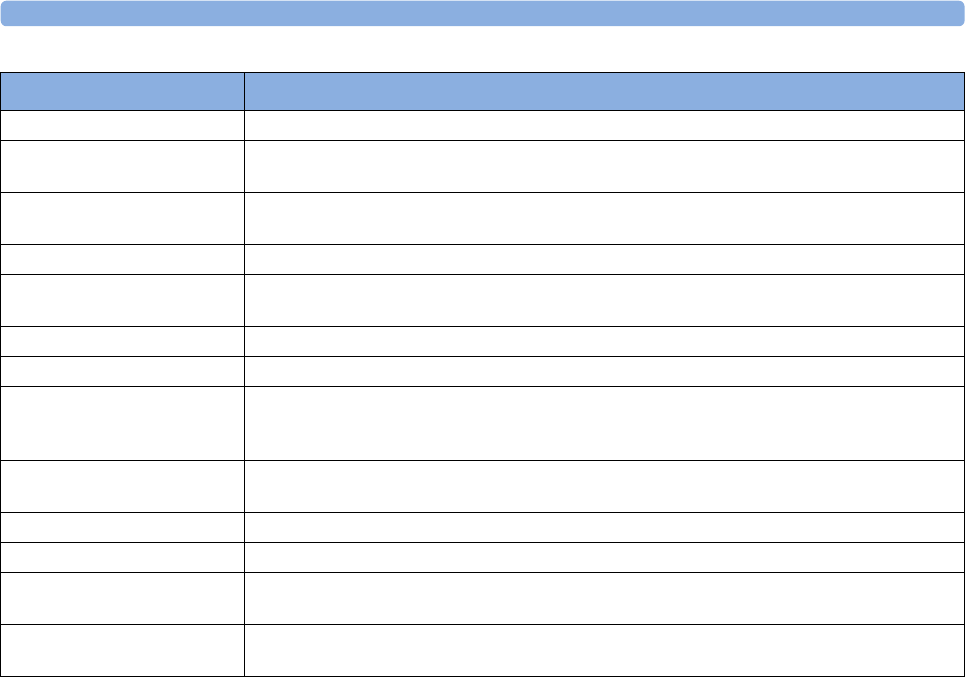
3 Patient Alarms and INOPs
93
cl NBP No Cradle The NBP Pod is not in its cradle.
cl NBP Remove The temperature of the battery in the NBP Pod is too high. Remove the Cableless Measurement
Device from the patient and contact service personnel.
cl NBP Serv Batt The battery in the NBP Pod has reached the end of its useful life. It can no longer be charged. Contact
your service personnel to replace the battery.
cl SpO₂ Batt Empty The remaining battery time of the SpO2 Pod is below 30 minutes. Change the battery.
cl SpO₂ Batt Incmp The battery in use with the SpO2 Pod is incompatible. Replace it with one approved for use with the
SpO2 Pod.
cl SpO₂ Batt Low The remaining battery time of the SpO2 Pod is below 2 hours.
cl SpO₂ Batt Malf There is a malfunction in the SpO2 Pod's battery system. Contact your service personnel.
cl SpO₂ Batt Temp The temperature of the battery in the SpO2 Pod is critically high. Check that the Pod is not covered or
exposed to a heat source. If the INOP persists, remove the Pod from the patient and contact your
service personnel.
cl SpO₂ Check Batt The battery in the SpO2 Pod is nearing the end of its useful life. Only 50 charge/discharge cycles
remain. Contact your service personnel to replace the battery.
cl SpO₂ Disconnect The SpO2 Pod has lost the connection to the monitor.
cl SpO₂ No Cradle The SpO2 Pod is not in its cradle.
cl SpO₂ Remove The temperature of the battery in the SpO2 Pod is too high. Remove the SpO2 Pod from the patient
and contact service personnel.
cl SpO₂ Serv Batt The battery in the SpO2 Pod has reached the end of its useful life. It can no longer be charged. Contact
your service personnel to replace the battery.
INOP Message, Indication What to do

3 Patient Alarms and INOPs
94

4
95
4Managing Patients
Use the Patient Demographics window and its associated pop-up keys to admit, discharge, and
transfer (ADT) patients.
All patient demographic and ADT information is shared between the patient monitor and the
Information Center, for example, patients admitted to the monitor are automatically admitted to a
connected Information Center.
Note that when an X2 or MP5 monitor is connected to a host monitor, its ability to admit or discharge
a patient is disabled, and the host monitor controls patient demographic and ADT information.
Admitting a Patient
The monitor displays physiological data and stores it in the trends as soon as a patient is connected.
This lets you monitor a patient who is not yet admitted. It is however important to admit patients
properly so that you can identify your patient on recordings, reports, and networked devices.
During admission you enter data that the monitor needs for safe and accurate operation. For example,
the patient category setting determines the algorithm the monitor uses to process and calculate some
measurements, the safety limits that apply for some measurements, and the alarm limit ranges.
NOTE
It is strongly recommended that the same patient data fields be configured to be mandatory at the
monitor and the Information Center.
To admit a patient,
1Select the patient name field or select the Admit/Dischrg SmartKey to open the Patient
Demographics window.
2Clear any previous patient data by selecting the Dischrge Patient or End Case pop-up key and
then Confirm.
If you do not discharge the previous patient, you will not be able to distinguish data from the
previous and current patients, for example, in the trend database.
3Select Admit Patient.
4Enter the patient information: select each field and use the on-screen keyboard or choose from the
pop-up list of alternatives to input information.
If a conventional keyboard or a barcode scanner is connected to the monitor you can use this to
enter patient information.
–Last Name: Enter the patient's last name (family name), for example Doe.
–First Name: Enter the patient's first name, for example Doe, John.

4 Managing Patients
96
–Middle Name (if configured to appear): Enter the patient's middle name.
–Lifetime Id, Encounter Id: Whether these fields appear and how they are labeled can be
configured for your hospital. One or both fields may be displayed and the labels may read:
MRN, Case Id, Visit Id, or other alternatives. Enter the appropriate data for the fields
displayed.
–Patient Cat.: Choose the patient category, either Adult, Pedi, or Neo.
–Paced: Choose Yes or No (You must use Yes if your patient has a pacemaker).
–Height: Enter the patient's height.
–Weight: Enter the patient's weight.
–BSA: The monitor calculates the body surface area automatically.
–Date Of Birth: Enter the patient's date of birth. Enter this in the form dd/mm/yyyy.
–Age: The monitor calculates the patient age automatically.
–Gender: Choose Male or Female.
–Notes (1) / Notes (2): Enter any extra information about the patient or treatment.
Select Confirm. The patient's name appears on the monitor info line at the top of the screen.
Patient Category and Paced Status
The patient category setting determines the algorithm the monitor uses to process and calculate some
measurements, the safety limits that apply for some measurements, and the alarm limit ranges.
The paced setting determines whether the monitor shows pacemaker pulses or not. When Paced is set
to No, pace pulses are filtered and therefore do not show in the ECG wave.
WARNING
Patient Cat. and Paced status will always contain a value, regardless of whether the patient is fully
admitted or not. If you do not specify settings for these fields, the monitor uses the default settings
from the current profile, which might not be correct for your patient.
Patient category
Changing the patient category may change the arrhythmia and NBP alarm limits. Always check alarm
limits to make sure that they are appropriate for your patient.
Paced status
For paced patients, you must set Paced to Yes. If it is incorrectly set to No, the monitor could mistake
a pace pulse for a QRS and fail to alarm during asystole.
Admitting a Centrally-Monitored Patient
You can admit a patient at either the bedside or the Information Center. When you admit a patient, the
patient's name appears on the bedside monitor and the Information Center.
If you do not fill in all patient information required by the Information Center, the Information Center
may reject the admission. Complete all the required fields and try again to admit the patient.
Quick Admitting a Patient
Use Quick Admit only if you do not have the time or information to fully admit a patient. Complete
the rest of the patient demographic details later.
4 Managing Patients
97
1Select the Quick Admit SmartKey.
2Enter the required data (ID fields or last name depending on configuration) with the keyboard or a
barcode scanner.
3Select Enter.
4In the confirmation window, select Confirm to discharge the previous patient (if confirmation is
configured).
5Check that patient category and paced status are correct for the new patient.
If the monitor is connected to an Information Center and only the ID field is entered, the patient name
is set to - - - at the Information Center. Complete the rest of the demographic details as soon as
possible to fully identify the patient on the network, on the monitor and on printed reports. To
complete the details, select Admit Patient again and complete all required fields.
Editing Patient Information
To edit the patient information after a patient has been admitted, select the patient name field on the
Main Screen to open the Patient Demographics window, and make the required changes.
Discharging a Patient
WARNING
Always perform a discharge before starting monitoring for a new patient, even if your previous patient
was not admitted. Failure to do so can lead to data being attributed to the wrong patient.
A discharge:
– clears the information in the Patient Demographics window
– erases all patient data (such as trend, event, and calculation data) from the monitor,
measurement modules and Information Center. This ensures that data from a previous patient
are not mixed with data from the new patient.
– resets patient category and paced settings to the settings defined in the default Profile
– resets all monitor and measurement settings as well as the active Screen to the settings defined
in the default Profile
– discharges the patient from the Information Center.
When a patient is discharged from the monitor or from an Information Center, all patient data is
deleted. Make sure that you have printed out any required reports before discharging. Check that a
functioning local or central printer is available before you use End Case.
To Discharge a Patient
1Select the patient name field or select the Admit/Dischrg SmartKey to open the Patient
Demographics window and associated pop-up keys.
2Select the pop-up key for either:

4 Managing Patients
98
–End Case - to print any configured end case reports or vital signs recording, discharge the
patient and clear the patient database, then enter standby mode. If an End Case SmartKey is
configured for your monitor, you can also select this instead and then confirm.
To see which end case reports are set up for your monitor, select Main Setup, Reports, then
Auto Reports. For each auto report, if End Case Report is set to On, this report will be
printed when you select End Case. See “Setting Up Auto Reports” on page 327 for
information on setting up end case reports.
–Dischrge Patient - to discharge the patient without printing any reports.
New Patient Check
The monitor can be configured to ask you in certain situations:
• after a specified power-off period
• after a specified standby period
• when no basic vitals (HR, RR, Pulse, SpO2, NBP) have been measured for a specified period
whether a new patient is now being monitored. The pop-up window is entitled Is This A New
Patient?. The monitor offers a Yes key to discharge the previous patient and begin monitoring a new
patient and a No key to continue monitoring with the current patient data and settings.
The time periods for the three conditions can be configured independently.
Transferring Patients
To save you from having to enter the same patient data multiple times and enable patient transfer
without loss of data, information can be shared between Multi-Measurement Modules (MMS), patient
monitors, and Information Centers.
– patient demographic information is shared between connected MMSs, patient monitors, and
Information Centers
– measurement settings and calibration data can be uploaded from an MMS to a patient
monitor, if configured
– trend information can be uploaded from an MMS to a patient monitor, if configured.
Different sets of patient and measurement-related data are stored in the monitor and the Multi-
Measurement Module. Understanding this will help you to understand what happens to patient data
when you transfer patients.
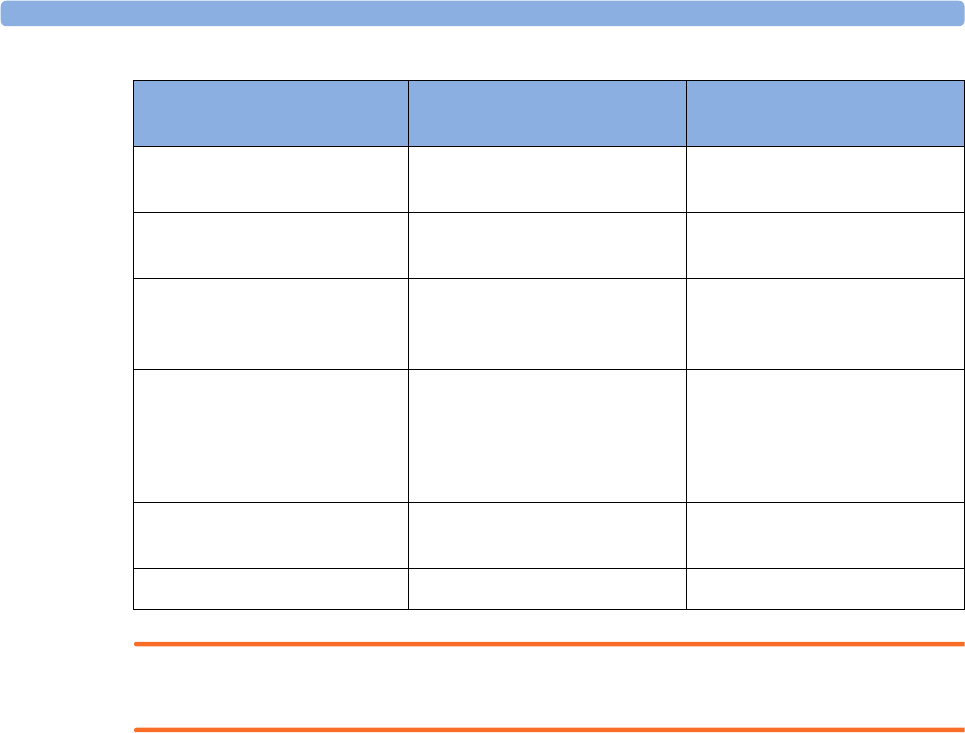
4 Managing Patients
99
WARNING
If the monitor is not battery-powered, you cannot monitor during transport.
Transferring a Centrally-Monitored Patient
Scenario: A centrally-monitored patient is moved to another monitoring location on the same
Information Center database server without interrupting the collection of patient trend information.
1Before you disconnect the MMS from the monitor, select the patient name field or select the
Admit/ Dischrge SmartKey to open the Patient Demographics window, then select the Transfer
pop-up key. If the patient is not admitted or not monitored by an Information Center, the
Transfer key is inactive ("grayed-out").
This step preserves the patient's demographic data during the transfer.
2Remove the MMS and any connected extensions from the monitor.
3Connect the MMS to the transfer monitor and monitor your patient during the move.
4At the new location, connect the MMS to the monitor. If the monitor detects a patient mismatch,
a window will open showing your patient's data and asking whether to Complete Transfer Of
This Patient?.
5Select Yes to complete the transfer. This re-admits the patient from the transfer list to the new
monitor. This will upload the patient demographics, and, if configured, the measurement settings
and trend data stored in the MMS to the receiving monitor.
6Verify that the settings for patient category and paced mode are correct.
Patient Information Stored in Monitor Stored in MMS and
extensions
Patient demographics (name,
DOB, patient IDs)
yes yes
Monitor settings (alarm
pause time, alarm volume)
yes no
Measurement settings for all
measurements (alarm limits,
measurement on/off, etc.)
yes yes, for all MMS and extensions
measurements
Trend data yes, for all MMS and extensions
measurements (up to a
maximum of 16 or 32,
depending on your database
configuration)
most recent 8 hours of
information, for all MMS and
extensions measurements
Calculation data (HemoCalc
data)
yes no
Events data yes no
4 Managing Patients
100
Transferring a Centrally-Monitored Patient with X2 or MP5
WARNING
Measurements from a MMS extension connected to an X2 are not available when the X2 is running on
battery power. They are only available when the X2 is running on external power, either when
connected to a host monitor or the external power supply (M8023A).
Scenario: A centrally-monitored patient is moved to another monitoring location on the same
Information Center database server without interrupting the collection of patient trend information.
1Before you disconnect the X2/MP5 from the host monitor, select the patient name field or select
the Admit/ Dischrge SmartKey to open the Patient Demographics window, then select the
Transfer pop-up key. If the patient is not admitted or not monitored by an Information Center,
the Transfer key is inactive ("grayed-out").
This step preserves the patient's demographic data during the transfer.
2Remove the X2/MP5 and any connected extensions from the monitor.
3Move the patient using the X2/MP5 as the transport monitor.
4At the new location, connect the X2/MP5 to the new host monitor. If the monitor detects a
patient mismatch, a window will open showing your patient's data and asking Complete Transfer
Of This Patient?.
5Select Yes to complete the transfer. This re-admits the patient from the transfer list to the new
monitor. This will upload the patient demographics, and, if configured, the measurement settings
and trend data stored in the X2/MP5 to the receiving monitor.
6Verify that the settings for patient category and paced mode are correct.
Transferring a Centrally-Monitored Patient with X2 or MP5 using IIT
WARNING
Measurements from a MMS extension connected to an X2 are not available when the X2 is running on
battery power. They are only available when the X2 is running on external power, either when
connected to a host monitor or the external power supply (M8023A).
Scenario: A centrally-monitored patient is moved with an X2 or MP5 to another monitoring location
on the same Information Center database server without interrupting the collection of patient trend
information. The X2/MP5 has an IntelliVue Instrument Telemetry interface (IIT), is connected to a
host monitor, and is declared as a telemetry device at the Information Center.
NOTE
The Transfer key is not available while the X2/MP5 is connected to a host monitor (Companion
Mode is indicated).
1Remove the X2/MP5 and any connected extensions from the host monitor.
2Move the patient using the X2/MP5 as the transport monitor.
3At the new location, just before connecting the X2/MP5 to the new host monitor:
–open the Patient Demographics window.
– select the Transfer pop-up key.

4 Managing Patients
101
–wait until the transfer has completed.
4Connect the X2/MP5 to the new host monitor. The monitor detects a patient mismatch and a
window will open showing your patient's data and asking Complete Transfer Of This Patient?.
5Select Yes to complete the transfer. This re-admits the patient from the transfer list to the new
monitor. This will upload the patient demographics, and, if configured, the measurement settings
and trend data stored in the X2/MP5 to the receiving monitor.
6Verify that the settings for patient category and paced mode are correct.
If you accidentally transfer a patient, use Re-Admit to restore this patient's data to the Information
Center. If you are not connected to the network, select Clear Transfer to leave transfer mode. The
patient data remains in the monitor.
Transferring a Patient with an X1 (no Information Center)
Scenario: A patient is moved to another monitoring location using a transport monitor and re-admitted
at the new monitor.
1Disconnect the X1 from the original monitor and silence the resulting UNPLUGGED INOP.
If you are sure that the patient will not be returning to this monitor, you should perform a
discharge or end-case. This prevents data from the next patient accidentally being mixed up with
your current patient's data.
2Connect the X1 to the transport monitor and move the patient.
3At the new monitoring location, remove the X1 from the transport monitor and connect it to the
new monitor.
4If prompted, re-admit the patient to the new monitor: in the Select Patient window, select the
patient in the X1 to retain the data in the X1. This will upload the patient demographics, and, if
configured, the measurement settings and trend data stored in the X1 to the monitor. Verify that
the settings for patient category and paced mode are correct.
Transferring a Patient with an X2 or MP5 (no Information Center)
WARNING
Measurements from a MMS extension connected to an X2 are not available when the X2 is running on
battery power. They are only available when the X2 is powered from AC mains, either when connected
to a host monitor or the external power supply (M8023A).
Scenario: A patient is moved to another monitoring location using the X2 or MP5 and re-admitted at
the new monitor.
1Disconnect the X2/MP5 from the original host monitor and silence the resulting UNPLUGGED
INOP.
If you are sure that the patient will not be returning to this monitor, you should perform a
discharge or end-case. This prevents data from the next patient accidentally being mixed up with
your current patient's data.
2Move the patient using the X2/MP5 as the transport monitor.
3At the new monitoring location, connect the X2/MP5 to the new host monitor.
4If prompted, re-admit the patient to the new monitor: in the Select Patient window of the new
monitor, select the patient in the X2/MP5 to retain the data in the X2/MP5. This will upload the
4 Managing Patients
102
patient demographics, and, if configured, the measurement settings and trend data stored in the
X2/MP5 to the monitor. Verify that the settings for patient category and paced mode are correct.
Data Upload from an MMS
The Multi-Measurement Module stores eight hours of patient trend data at one-minute resolution. It
also stores patient demographic information and the measurement settings (including the ST baseline)
and calibration data for the measurements carried out by the MMS and any connected extensions. This
data can be uploaded to an IntelliVue patient monitor, if your monitor is configured to do so and if at
least five minutes of trend information is stored in the MMS.
Your monitor's data upload settings are defined in Configuration Mode to suit your patient transfer use
model.
How data is uploaded to the host monitor depends on the configuration mode settings MMS Trend
Upload and MMS Sett. Upload.
If there is a patient mismatch and you select Continue Monitor, no data will be uploaded from the
MMS.
Data Exchange Between Information Centers
You can transfer demographic data and trend data from one IIC to another by selecting Transfer on
the patient monitor. Trend data is not shared between Information Centers and monitors.
Resolving Patient Information Mismatch
When you connect together devices which store patient demographic data, for example:
• an MMS and a monitor,
• an X2 or MP5 and a host monitor,
• a monitor and an Information Center,
the system compares patient category, paced status, and unique patient identification in order to
synchronize this information. If configured to do so, the monitor indicates a mismatch if the
information is not identical.
Depending on your monitor's configuration, this mismatch may be automatically resolved or you may
have to resolve it manually. If your monitor is configured to resolve mismatches automatically,
depending on the configuration, either the monitor or the Multi-Measurement Module data is
automatically retained.
WARNING
1When a monitor is connected to an Information Center by the wireless IntelliVue Instrument
Telemetry interface, the patient data will automatically be merged in the case of a transfer. This
means there is no patient discharge at the monitor and settings and trend data will be retained. You
will see a message on the monitor and the Patient Demographics window will automatically
appear so that you can check the data and change it if necessary.
2It is important to resolve the mismatches as soon as they are identified. Failure to do so could
result in using incorrect/confusing data to make clinical decisions. Certain settings, for example
Paced and Patient Cat., may not match between the Information Center and the monitor. If the
Paced status is set incorrectly, the system could mistake a pace pulse for a QRS and fail to alarm in
4 Managing Patients
103
the case of asystole. It is important that the patient category is set correctly so the ECG can be
analyzed correctly and initial arrhythmia alarm limits set.
In the case where an MP5 or X2 with an IntelliVue Instrument Telemetry interface is declared as a
"telemetry device" at the Information Center and is connected to a host monitor, it is important to
resolve an existing mismatch between the monitor and the Information Center before
disconnecting the MP5/X2. Failure to do so discharges the MP5/X2 and synchronizes the
demographics and settings to the Information Center.
Manually Resolving Patient Mismatch
The patient mismatch is indicated by question marks (???) beside the questionable fields in the Monitor
Info Line and in the Select Patient window. The monitor displays a message such as Different
patients in Central and Monitor.
The Select Patient window automatically opens so you can decide which patient data to use. You do
not have to resolve the mismatch immediately, but the indicators remain until you do.
For some common mismatch situations, the monitor will simplify the resolution by suggesting a
solution for the mismatch. For example, when a patient arrives after transport and the Transfer key
has been selected, the monitor will show this patient's data and ask Complete Transfer Of This
Patient?. You can then select Yes to complete the transfer. If you select No you will go to the Select
Patient window.
There can be up to three sets of demographic data in the Select Patient window if the patient is
different in the Information Center, monitor, and MMS.
After you resolve the mismatch, the monitor displays a confirmation window that shows the patient
that has been selected and where data will be erased, if applicable. Confirm your choice. The monitor
automatically displays the Patient Demographics window after confirmation. Verify that the settings
shown are correct for the patient.
Gender, date of birth, height, weight, and nursing notes do not generate a mismatch. If these fields are
different on different devices, the monitor resolves them itself. For example, it may take date of birth
from the Information Center, whilst taking gender from the MMS. Always check the Patient
Demographics after combining patients, to ensure that you are satisfied with the results. Change them
if necessary.
WARNING
After resolving a patient mismatch, check that the monitor settings (especially patient category, paced
status and alarm limits) are correct for the patient.
Patient Mismatch - If One Set of Patient Data is Correct
If there is a mismatch between an Information Center and a monitor, or a monitor and an MMS,
choose the data set you want to continue using for this patient by selecting one of the sectors in the
Select Patient window.
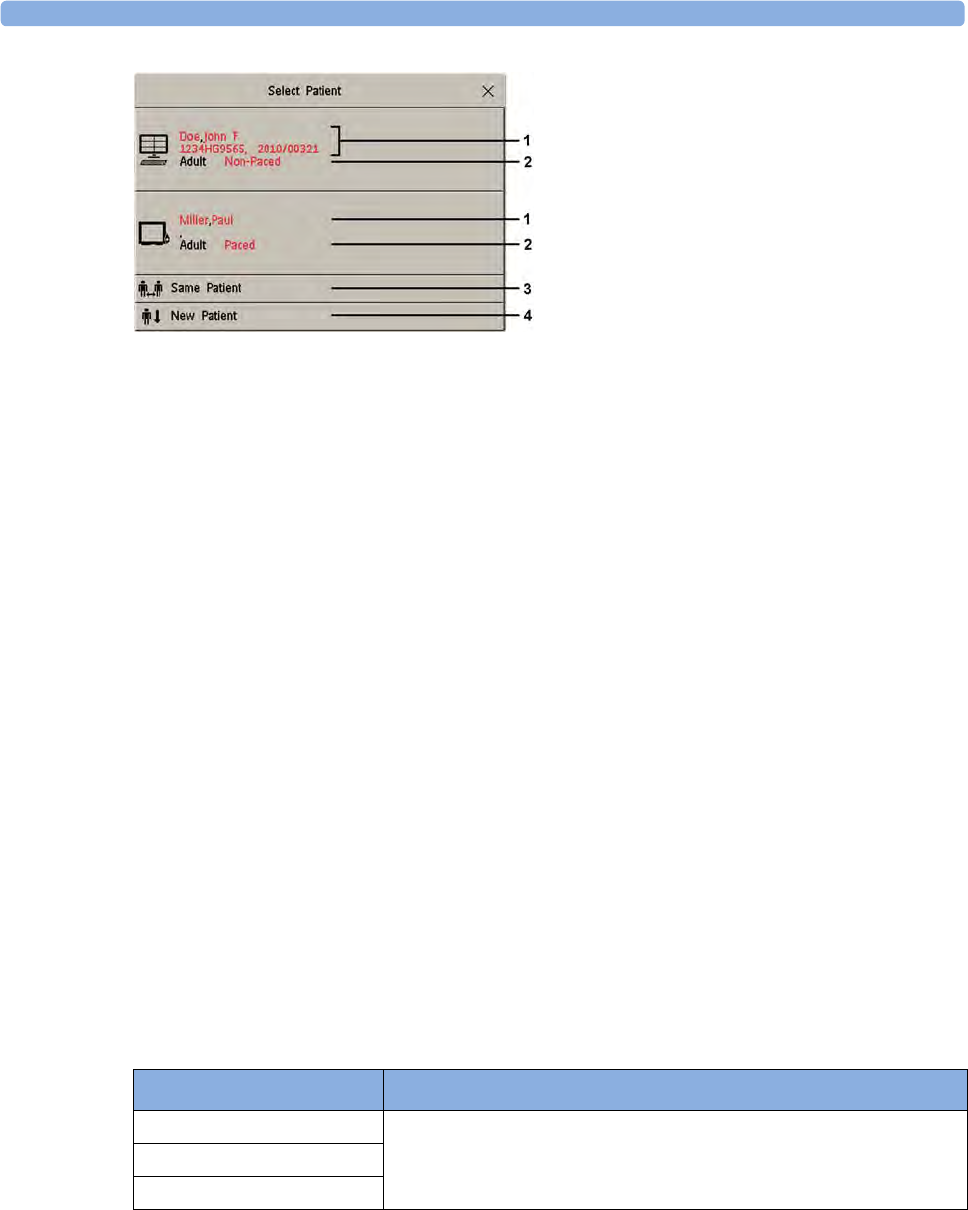
4 Managing Patients
104
1Patient demographics
2Patient category and paced status
3Same Patient - see “Patient Mismatch - If Both Patient Data Sets Are Correct” on page 104.
4New Patient - see “Patient Mismatch - If Neither Patient Data Set is Correct” on page 104.
After you resolve the mismatch, the monitor displays a confirmation window that shows the patient
that has been selected and where data will be erased, if applicable. Confirm your choice. The monitor
automatically displays the Patient Demographics window after confirmation. Verify that the settings
shown are correct for the patient.
Patient Mismatch - If Neither Patient Data Set is Correct
A patient mismatch where neither set of patient data is correct might occur if you connect a new MMS
to a monitor in order to prepare for a new patient, before you actually start measuring.
Select New Patient if you are sure that none of the information is correct. This discharges all patients,
erases all data in both the monitor and MMS, resets all settings to the default Profile, and lets you
admit a new patient.
Patient Mismatch - If Both Patient Data Sets Are Correct
A patient mismatch where both sets of patient data are correct might occur if you admit a new patient
at the monitor (or Information Center) before the patient arrives at your unit and then connect the
MMS that was used during the patient transport to the monitor.
Select Same Patient if the patient information is different, but you are sure it is the same patient. This
merges the demographics and updates them in the Information Center, monitor, and MMS, according
to this table. Be aware that your monitor may be configured to merge trend data from the MMS and
the monitor, and to upload measurement settings from the MMS to the monitor.
Patient Information This information is taken from...
Patient name the monitor, if the patient was admitted there. For centrally-admitted
patients, this information is taken from the Information Center.
Patient IDs
Screen Notes
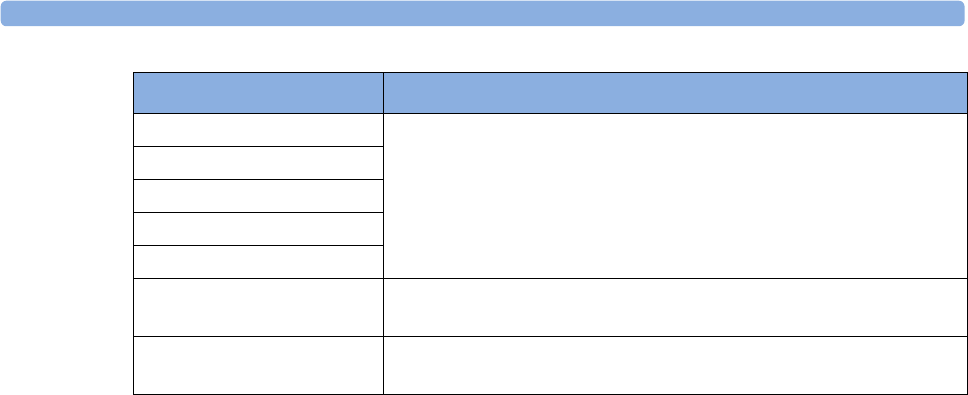
4 Managing Patients
105
Automatically Resolving Patient Mismatch
Your monitor can be configured to automatically resolve mismatches in one of two ways.
• continue using the patient in the MMS, and delete the old data in the monitor. This is suitable for
transport monitors.
• continue with the patient in the monitor, and delete the data in the MMS.
Care Groups
If your monitor is connected to an Information Center, you can group bedside monitors into Care
Groups. This lets you:
• view information on the monitor screen from another bed in the same or in a different Care
Group.
• be notified of yellow or red alarm conditions at the other beds in the Care Group.
• see the alarm status of all the beds in the Care Group on each monitor screen.
There are two main types of Care Groups:
• standard care group (Bed-based Care Group) - up to 12 patients monitored by up to 4
Information Centers
• unit group (Unit-based Care Group) - for a complete unit with up to 64 patients monitored by
up to 4 Information Centers
Monitors must be assigned to these Care Groups at the Information Center. There is a third care
group which can be assigned locally at the bedside. This is the My Central care group which includes
all beds (up to 16) from the Information Center your bed is connected to. This care group setting is
typically used in facilities with only one Information center. The selection of beds is automatic and
cannot be changed.
The functions available with Care Groups depend on the Information Center revision your monitors
are connected to. See your Information Center Instructions for Use for further details.
Patient Category the Multi-Measurement Module, if connected, otherwise the data is
taken from the monitor.
Date of Birth
Height
Weight
Gender
Paced Status Paced status is always set to Yes where there is a mismatch in patient
information.
Trend data if there is newer trend data stored in the MMS, it is uploaded to the
monitor.
Patient Information This information is taken from...
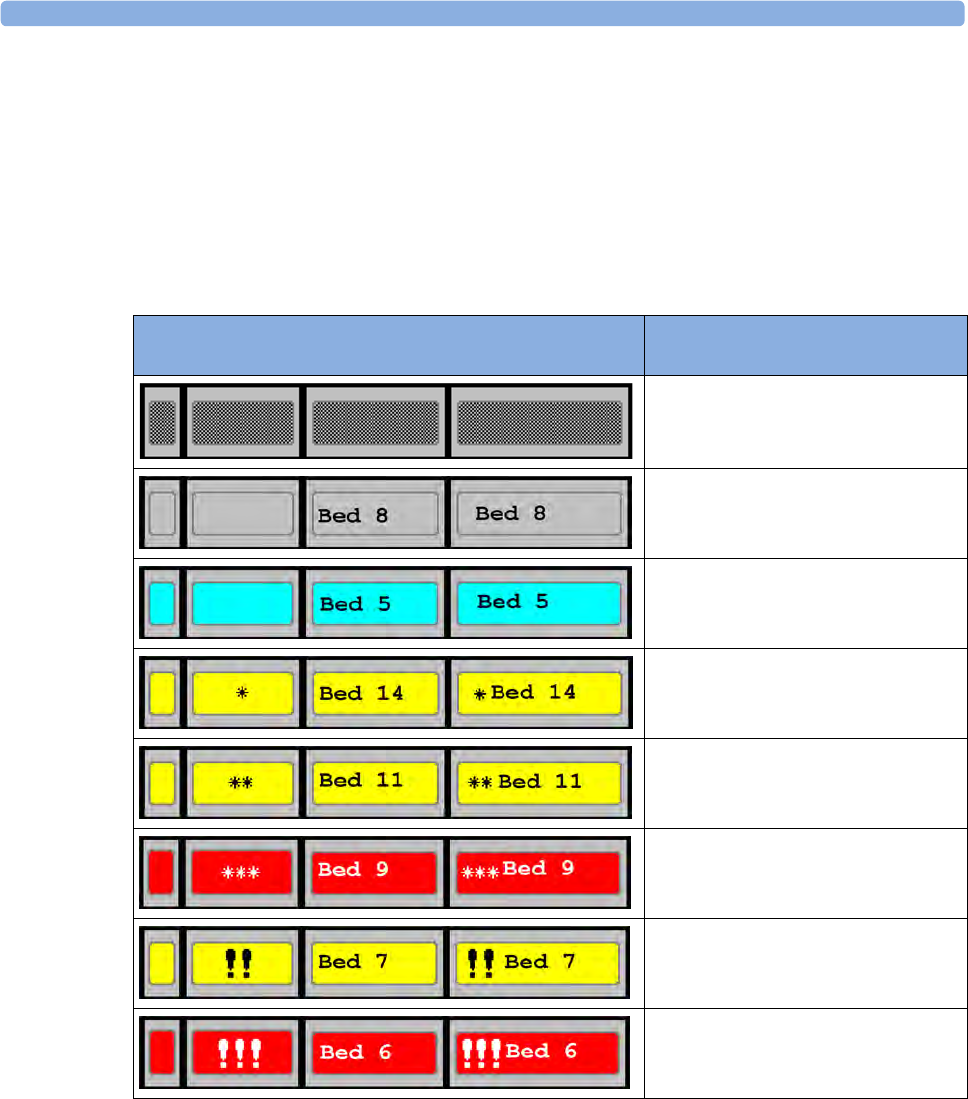
4 Managing Patients
106
Understanding the Care Group Overview Bar
The Care Group monitors' status is shown in symbol form in the Care Group overview bar. Flashing
symbols indicate active alarms, symbols that are not flashing indicate alarms that have been
acknowledged. Selecting a bed symbol calls up the window for that bed or a setup window to select
this.
The Care Group overview bar must be configured to display on the monitor Screen. If it is not visible
on your monitor, select a Screen which has been configured to show the bar. Some screens may show
the Care Group monitors grouped together in a tabular format on the right hand side of the screen.
Care Group Symbols (four alternative display possibilities
depending on space available)
No data from this bed
The alarms are on but there are no currently
active alarms at this monitor
The highest priority alarm at this monitor is a
standard INOP
The highest priority alarm at this monitor is a
short yellow alarm
The highest priority alarm at this monitor is a
yellow alarm
The highest priority alarm at this monitor is a
red alarm
The highest priority alarm at this bed is a
yellow INOP
The highest priority alarm at this bed is a red
INOP
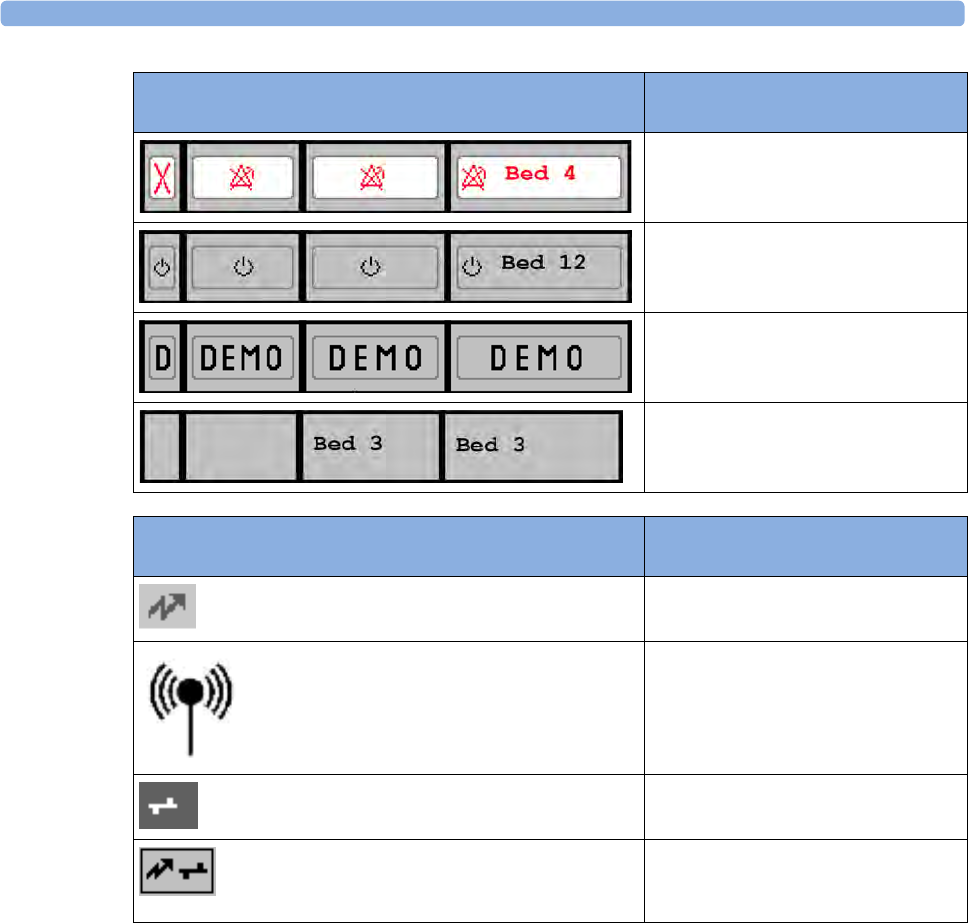
4 Managing Patients
107
Viewing the My Care Group Window
This window shows the alarm status, bed name, and patient name for every bed in the Care Group.
The window for the Unit group shows first the beds of the Information Center this bed is connected
to. By selecting the Information Center name at the top of the list, you can display a list of all
Information Centers associated with the Unit group, and select another Information Center to view.
To enter the My Care Group window,
• select the Other Patients SmartKey, if configured, or
•in the Main Setup menu, select My Care Group.
The alarms at this monitor are suspended
The monitor is in standby mode
The monitor is in Demonstration mode
The current monitor
Care Group Symbols (used in the Care Group overview bar and
the My Care Group window)
This is a telemetry bed
This bed is on a wireless network.
This bed is on a wired network.
This is a "paired" bed, with a bedside
monitor and a telemetry transmitter
assigned.
Care Group Symbols (four alternative display possibilities
depending on space available)
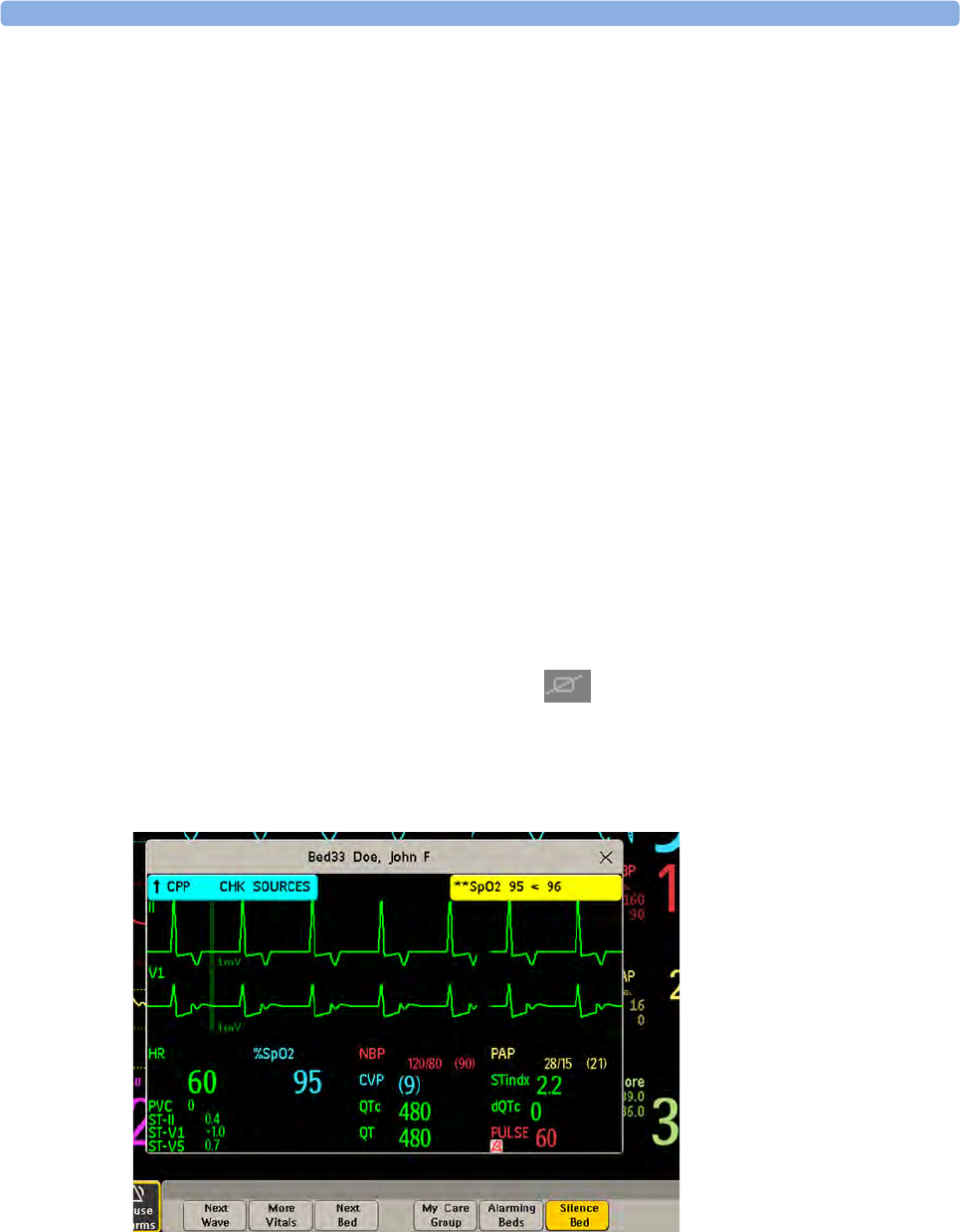
4 Managing Patients
108
Use the My Care Group pop-up keys to navigate through the Care Groups:
My Unit lets you view a list of all the Information Centers in your Care Unit. Select an Information
Center to see a list of the monitors connected to it. Select any monitor to see the Other Patient
window for that bed.
Other Units lets you view a list of all the Care Units in your Care Domain. Select any Care Unit to
view a list of the Information Centers connected to it. Select an Information Center to see a list of
the monitors connected to it. Select any monitor to see the Other Bed window for that bed.
Alarming Beds lets you view a list of all beds in your care group with an unacknowledged alarm.
The beds are listed in order of alarm severity.
Viewing the Other Bed Window
The Other Bed window lets you view a subset of the waveform and numeric information from another
bed on the same network. Waves and numeric information from another bed are delayed. If
configured, Other Bed information is displayed in color, using the colors defined by the Information
Center.
The Other Bed window can be configured to pop-up automatically when an alarm occurs at another
bed. To avoid too many windows appearing (for example, in large care groups) and covering the
monitor's own bed data on the screen, you can temporarily disable this automatic pop-up:
1Select Main Setup then Network followed by Auto Window
2Select Disabled
When automatic pop-up is disabled in this way, an icon will appear as a reminder in the Care Group
Overview Bar next to the monitor's own bed label . Depending on the configuration, the
automatic pop-up is disabled for five minutes or until you set it to Enabled again.
• To open the Other Bed window, select the required bed label or patient name in the Care Group
Overview Bar. If you are in a Unit Group with many beds, the My Care Group window may open
for you to select the bed.
The Other Bed window may be configured to display embedded in a specially designed Screen.
• To display the embedded Other Bed screen element, in the Change Screen menu, select a Screen
designed to show the Other Bed information permanently.
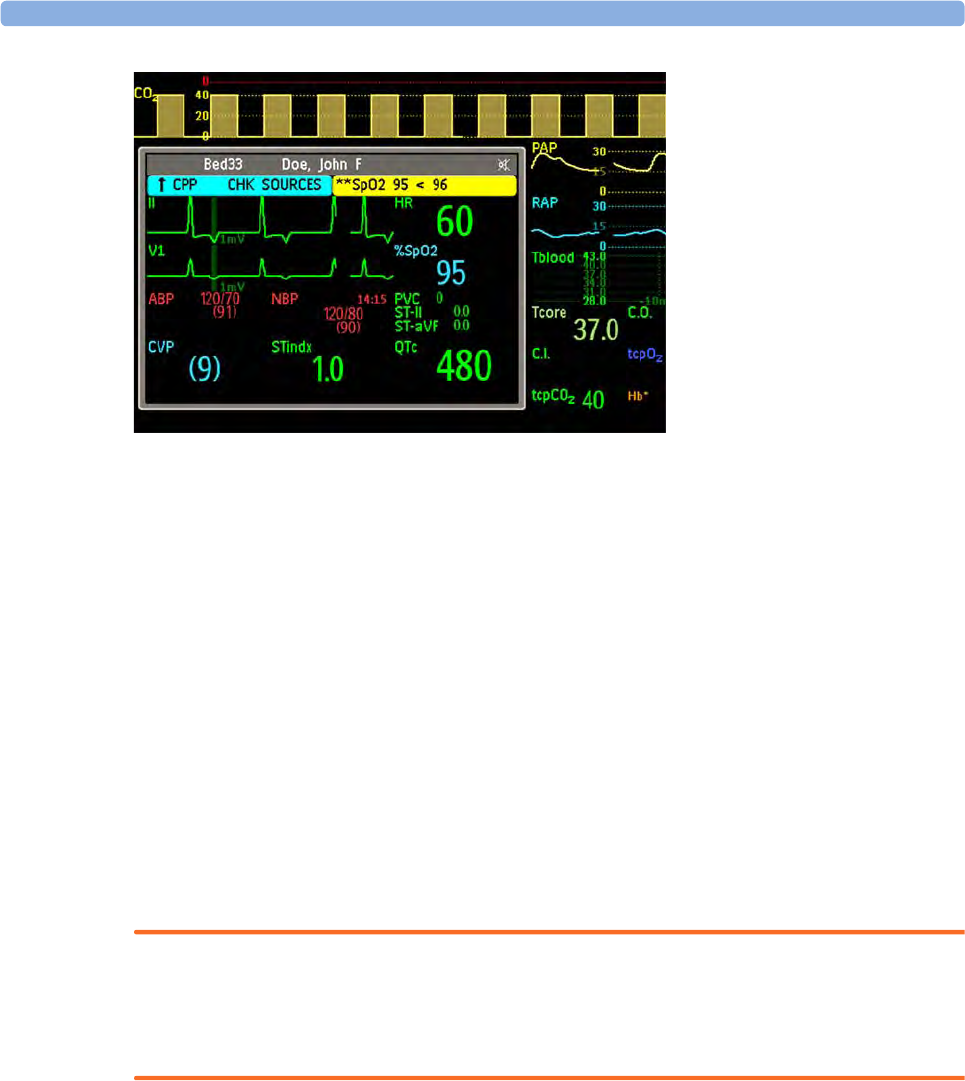
4 Managing Patients
109
Note that a Screen with an embedded Other Bed screen element cannot be displayed on the D80
Intelligent Display.
Changing the Screen may automatically change the bed shown in the other bed window. If you switch
to a different Screen, you should check that the correct other bed is displayed.
Other Bed Pop-Up Keys
Select the Other Patients SmartKey or the Other Bed window or embedded screen element to access
the associated pop-up keys:
Next Wave lets you view waveforms not currently shown in the other bed window.
More Vitals lets you view more numerics not currently shown in the other bed window.
Next Bed lets you view waveforms and numerics from the next available bed in the Care Group.
My Care Group lets you call up the Care Group window to select another bed.
Alarming Beds lets you view a list of all beds in your care group with an unacknowledged alarm.
The beds are listed in order of alarm severity.
Silence Bed lets you silence active alarms at the other bed. (Whether you see this key depends on
the revision and configuration of the Information Center your monitors are connected to.)
WARNING
The Silence Bed pop-up key in the Other Bed window silences alarms at a remote bed. Be aware that
accidental use of this key could silence alarms for the wrong patient.
To silence own bed alarms use the Silence permanent key on screen.
Visual Alarm Status Information in the Other Bed Window
• If individual alarms are switched off at the other bed, this is indicated by the crossed alarm symbol
beside the measurement numeric.
• If alarms are switched off at the other bed, the message Alarms Off is shown in the other bed
window.
• In the embedded Other Bed window, the crossed speaker symbol in the upper right hand indicates
that the volume of the audible alarm status change notification for the other beds in the care group
is set to zero at the overview monitor.

4 Managing Patients
110
Care Group Alarms
Changes in the alarm status of beds in a Care Group are announced visually and audibly at all other
beds in the same Care Group. The visual and audible indicators used depend on the monitor and
Information Center configuration.
When an alarm is detected at another bed in the Care Group,
• the alarm status is shown in the Care Group overview bar as an icon.
• a message informing you about the care group alarm is shown in the monitor status line.
• if configured, the Other Bed window, the Alarming Beds window or the My Care Group window
may pop up on the Screen (if automatic alarm notification is enabled at the bedside monitor and at
the Information Center). The automatic alarm notification is suppressed when a window, menu or
pop-up keys are active.
• if configured, an audible status change notification is issued. The tone type and volume can be
configured.
Automatic alarm notification can be switched off permanently in the monitor's Configuration Mode or
at the Information Center. To temporarily disable and re-enable automatic alarm notification at the
bedside monitor, for example if you want to carry out a procedure, in Monitoring Mode:
1Select the network symbol on the monitor screen to call up the Network menu.
2Select Auto Window to toggle between the settings Enabled and Disabled.
This setting resets to the default at discharge and when the monitor is switched on. Always re-enable
the Auto Window as soon as possible.

5
111
5ECG, Arrhythmia, ST and QT
Monitoring
The electrocardiogram (ECG) measures the electrical activity of the heart and displays it on the
monitor as a waveform and a numeric. This section also tells you about arrhythmia monitoring (see
“About Arrhythmia Monitoring” on page 129), ST monitoring (see “About ST Monitoring” on
page 139) and QT monitoring (see “About QT/QTc Interval Monitoring” on page 149).
Skin Preparation for Electrode Placement
Good electrode-to-skin contact is important for a good, noise-free ECG signal, as the skin is a poor
conductor of electricity.
1Select sites with intact skin, without impairment of any kind.
2Clip or shave hair from sites as necessary.
3Wash sites thoroughly with soap and water, leaving no soap residue.
We do not recommend using ether or pure alcohol, because this dries the skin and increases the
resistance.
4Dry skin thoroughly.
5Gently abrade the skin using ECG skin preparation paper to remove dead skin cells to improve the
conductivity of the electrode site.
Connecting ECG Cables
1Attach the clips or snaps to the electrodes before placing them. If you are not using pre-gelled
electrodes, apply electrode gel to the electrodes before placement.
2Place the electrodes on the patient according to the lead placement you have chosen.
3Attach the electrode cable to the patient cable.
4Plug the patient cable into the white ECG connector. An ECG waveform and numeric appears on
the monitor display.
5 ECG, Arrhythmia, ST and QT Monitoring
112
CAUTION
To protect the monitor from damage during defibrillation, for accurate ECG information and to
protect against noise and other interference, use only ECG electrodes and cables specified by Philips.
Selecting the Primary and Secondary ECG Leads
The monitor uses the primary and secondary lead to compute HR and to analyze and detect cardiac
arrhythmias. They are also available for recordings and for display on the Information Center.
The secondary lead is only used if your monitor is configured for multi-lead (instead of single-lead)
arrhythmia analysis.
You should choose a lead as primary or secondary lead that has the following characteristics:
To select a lead as primary or secondary lead:
•In the Setup ECG menu, select Primary or Secondary, then select the appropriate lead. You can
assign any available lead whether it is currently displayed or not.
Checking Paced Status
It is important to set the paced status correctly when you start monitoring ECG.
• To change the paced status in the Setup ECG menu, select Paced to toggle between Yes or No.
WARNING
Pace pulse rejection must be switched on for paced patients by setting Paced to Yes. Switching pace
pulse rejection off for paced patients may result in pace pulses being counted as regular QRS
complexes, which could prevent an asystole event from being detected. When changing profiles, and at
admission/discharge, always check that paced status is correct for the patient.
Some pace pulses can be difficult to reject. When this happens, the pulses are counted as a QRS
complex, and could result in an incorrect HR and failure to detect cardiac arrest or some arrhythmias.
Make sure that pace pulses are detected correctly by checking the pace pulse markers on the display.
Keep pacemaker patients under close observation.
Understanding the ECG Display
Your display may be configured to look slightly different.
• the QRS complex should be either completely above or
below the baseline and it should not be biphasic
• the QRS complex should be tall and narrow
• the P-waves and T-waves should be less than 0.2 mV
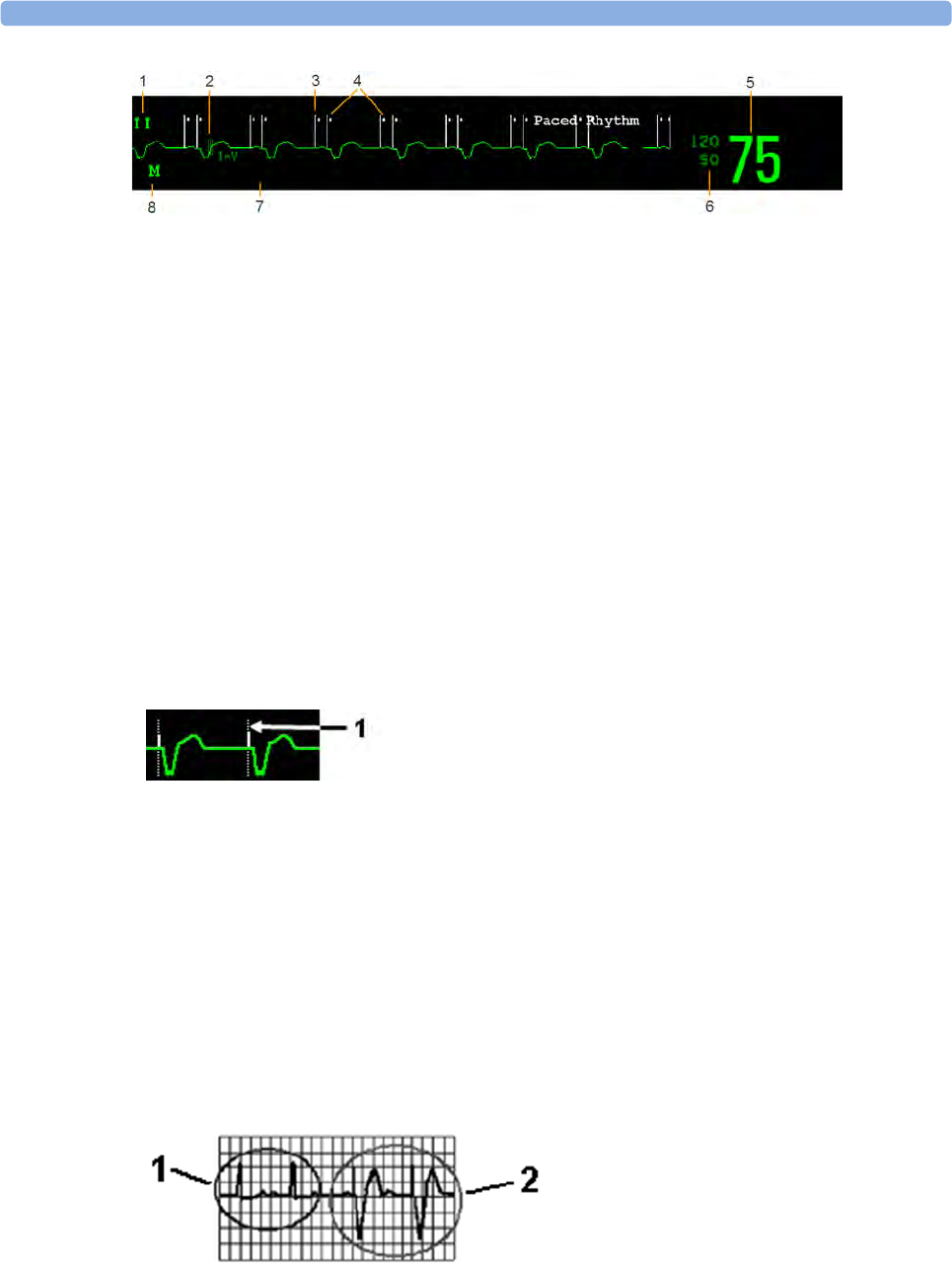
5 ECG, Arrhythmia, ST and QT Monitoring
113
1Lead label of the displayed wave
21 mV calibration bar
3Pacer spikes
4Pace pulse markers
5Current heart rate
6Current heart rate alarm limits
7EASI lead placement label (located here when present)
8ECG Filter label
ECG HR numeric: This is the heart rate derived from the monitored ECG.
Pace pulse markers: These are shown if the Paced status has been set to Yes, the pacer spikes are not
configured to have a fixed size, and the patient has a paced signal.
Pacer Spikes: The pacer spikes are shown in white, unless the ECG wave is white, then they will be
green. If the pacer spikes have been configured to have a fixed size, they will be displayed in the
background as a dotted line.
Defibrillator synchronization marks: If an HP/Agilent/Philips defibrillator is connected, or the 2nd
Sync Out channel is configured to ECG SyncPuls and a sync cable is plugged in, the synchronization
marks (vertical lines on the ECG wave) are shown on the ECG wave. The synchronization marks will
be shown in yellow, unless the ECG wave is yellow, then they will be green.
ST numerics in ECG wave: ST numerics can be configured to show underneath the ECG wave on
the left side.
Monitoring Paced Patients
An ECG optimized for monitoring a paced patient should look like this:
You should choose a lead as primary or secondary lead that has these characteristics:
1Pacer spikes configured to have a fixed size
1Normal Beats
2Pace Pulses/Pace Beats
5 ECG, Arrhythmia, ST and QT Monitoring
114
• the normal QRS complex should be either completely above or below the baseline and it should
not be biphasic. For paced patients, the QRS complexes should be at least twice the height of pace
pulses.
• the QRS complex should be tall and narrow
• the P-waves and the T-waves should be less than 0.2 mV.
For ease of identification on the screen, the pacer spikes can be configured to have a fixed size. They
are then shown in the background as a dotted lines. The length of the dotted line is fixed to the wave
channel height and is independent of the actual pacer amplitude.
Setting the Paced Status (Pace Pulse Rejection)
Avoiding Pace Pulse Repolarization Tails
Some unipolar pacemakers display pace pulses with repolarization tails. These tails may be counted as
QRSs in the event of cardiac arrest or other arrhythmias.
If you note a visible repolarization tail, choose a lead that decreases the size of the repolarization tail.
Changing the Size of the ECG Wave
If any of the displayed ECG waves is too small or clipped, you can change the size of one or all of the
ECG waves on the screen.
Changing the adjustment factor only changes the visual appearance of the ECG wave on the screen. It
does not affect the ECG signal analyzed by the monitor.
In the Setup ECG menu, select Paced to toggle between Yes and No.
You can also change the paced status in the Patient Demographics window.
When Paced is set to Yes:
– Pace Pulse Rejection is switched on. This means that pacemaker
pulses are not counted as extra QRS complexes.
– pace pulse marks are shown on the ECG wave as a small dash (only
when the pacer spikes are not configured to have a fixed size).
– The paced symbol is displayed on the main screen.
When Paced is set to No, pacer spikes are not shown in the ECG wave. Be
aware that switching pace pulse rejection off for paced patients may result in
pace pulses being counted as regular QRS complexes, which could prevent an
asystole event from being detected.
Paced
Non-Paced
1Repolarization tail (note width)

5 ECG, Arrhythmia, ST and QT Monitoring
115
Comparing the wave size to the 1 mV calibration bar on the ECG wave segment can help you to get an
idea of the true ECG signal strength. If you choose a fixed adjustment factor, the 1 mV calibration bar
will be the same size for all the displayed ECG waves. If you choose Auto Size, or an individual size
using the Size Up/Size Down keys, the calibration bar may be a different size for each wave.
To Change the Size of an Individual ECG Wave
1Select the wave segment you want to change. This calls up the lead menu for this segment.
2In the lead menu, select Size Up to increase wave size or Size Down to decrease the size.
Selecting Auto Size lets the monitor choose the optimal adjustment factor for all available ECG
waves.
To Change the Size of all the ECG Waves
To change the size of all the ECG waves on the screen by a fixed adjustment factor,
1In the Setup ECG menu, select Adjust Size.
2Select the required adjustment factor from the line of pop-up keys.
–Size X0.5 to halve the wave size
–Size X1 to display the wave without zoom
–Size X2 to double the wave size
–Size X4 to multiply the wave size by four
–Previous Size: to return one step to the previous size
–Auto Size: to let the monitor choose the optimal adjustment factor for all the ECG waves.
Changing the Volume of the QRS Tone
The QRS tone is derived from either the HR or Pulse, depending on which is currently selected as the
alarm source. The QRS volume can be set from 0 to 10 (0 means off).
To change the QRS volume, in the Setup ECG menu select QRS Volume and then select the
appropriate volume from the pop-up list.
Changing the ECG Filter Settings
The ECG filter setting defines how ECG waves are smoothed. An abbreviation indicating the filter
type is shown underneath the lead label on the monitor display. Filter settings do not affect ST
measurement.
To change the filter setting, in the Setup ECG menu, select Filter and then select the appropriate
setting.
–Monitor: Use under normal measurement conditions.
–Ext. Monitor: Use when diagnostic quality is required but low frequency interference or a
wandering baseline may be expected. The upper edge frequency is the same as the Diag setting
and the lower edge frequency is the same as the Monitor setting.
–Filter: The filter reduces interference to the signal. It should be used if the signal is distorted
by high frequency or low frequency interference. High frequency interference usually results in
large amplitude spikes making the ECG signal look irregular. Low frequency interference
usually leads to a wandering or rough baseline. In the operating room, the Filter reduces
artifacts and interference from electrosurgical units. Under normal measurement conditions,

5 ECG, Arrhythmia, ST and QT Monitoring
116
selecting Filter may suppress the QRS complexes too much and thus interfere with the clinical
evaluation of the ECG displayed on the monitor. This does not affect the ECG analysis
performed by the monitor.
If AutoFilter is set to On in Configuration Mode, the filter setting will automatically be set to
Filter if electromagnetic interference is detected.
–Diag: Use when diagnostic quality is required. The unfiltered ECG wave is displayed so that
changes such as R-wave notching or discrete elevation or depression of the ST segments are
visible.
The setting Diag selects the highest available ECG bandwidth which is 0.05 to 150 Hz for the
Adult, Pedi and Neo patient category. The term "diagnostic" relates only to the ECG
bandwidth requirements for diagnostic electrocardiographic devices as outlined in the ANSI/
AAMI standard EC11-1991.
Selecting Positions of Va and Vb Chest Leads (for
6-lead placement)
The two chest leads for the 6-lead placement can be positioned at any two of the V1 to V6 positions.
Select the positions you have used in the Setup ECG menu, so that the chest leads will be correctly
labeled.
1In the Setup ECG menu, select Va Lead.
2Select the position used from the list.
3Select Vb Lead and select the position used from the list.
Choosing EASI or Standard Lead Placement
You must enable either standard lead placement or EASI lead placement.
•In the Setup ECG menu, select Lead Placement and then Standard or EASI.
EASI is shown beside the 1 mV calibration bar on the ECG wave on the display, and EASI is marked on
any recorder strips and printouts.
See the section on “EASI ECG Lead Placement” on page 125 for electrode placement diagrams.
About ECG Leads
To make it possible to compare measured ECG signals, the electrodes (or lead sets) are placed in
standardized positions, forming so-called "leads". To obtain ECG signals optimized for use in
diagnosis and patient management in different care environments, different lead sets in varying lead
placements can be used. You can use either standard lead placements or EASI lead placements with
this monitor.
When placing electrodes, choose a flat, non-muscular site where the signal will not be interfered with
by either movement or bones. Correct lead placement is always important for accurate diagnosis.
Especially in the precordial leads, which are close to the heart, QRS morphology can be greatly altered
if an electrode is moved away from its correct location.
5 ECG, Arrhythmia, ST and QT Monitoring
117
ECG Leads Monitored
Changing Lead Sets
To change the ECG lead set,
•When adding leads: place the additional electrodes as required - the monitor automatically
recognizes the new lead placement.
•When removing leads: there are two possibilities - removing the complete chest leads block or
removing individual leads. If you unplug the chest lead block from the trunk cable connector, the
monitor will automatically recognize the new lead placement. Remove individual leads by
removing the electrodes. The monitor will issue a LEAD OFF INOP message; select New Lead
Setup in the Setup ECG menu and the INOP message will disappear.
ECG Lead Fallback
If fallback is configured on and there is a leads off INOP in the primary lead (and in the secondary
lead, if you are using multi-lead monitoring) for longer than 10 seconds, and if another lead is available,
this available lead automatically becomes the primary lead. This is known as lead fallback. When the
Leads Off condition is corrected, the leads are automatically switched back.
This setting can only be changed in Configuration Mode.
ECG Lead Placements
The labels and colors of the ECG electrodes differ according to the standards that apply for your
hospital. The electrode placement illustrations in this chapter use the AAMI labels and colors.
If you are using these leads are available: Resp is measured
between electrodes:
a 3-electrode set I, II, III RA and LL
a 5-electrode set I, II, III, aVR, aVL, aVF, V and MCL RA and LL
a 6-electrode set I, II, III, aVR, aVL, aVF, Va, Vb RA and LL
a 10-electrode set I, II, III, aVR, aVL, aVF, V1, V2, V3, V4, V5, V6 RA and LL
an EASI 5-electrode set I, II, III, aVR, aVL, aVF, V1, V2, V3, V4, V5, V6 I and A
Electrode labels Electrode colors
AAMI EASI IEC AAMI IEC
RA I R White Red
LA S L Black Yellow
LL A F Red Green
RL N N Green Black
VECBrown White
V1 C1 Brown/Red White/Red
V2 C2 Brown/Yellow White/Yellow
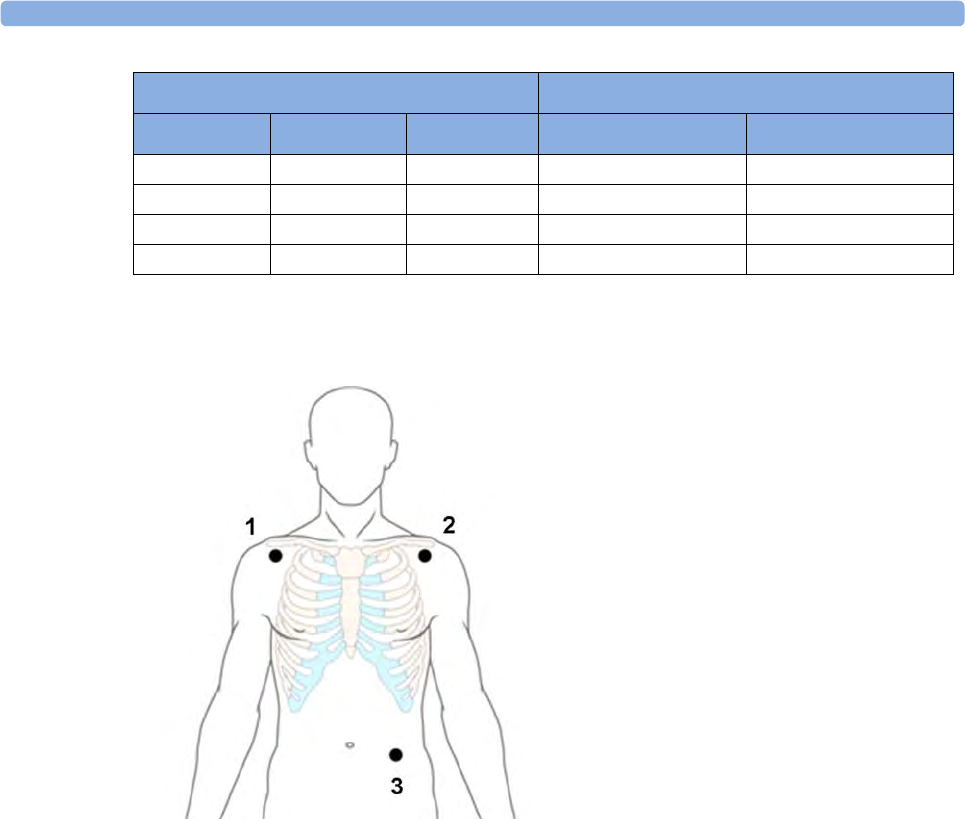
5 ECG, Arrhythmia, ST and QT Monitoring
118
Standard 3-Lead Placement
V3 C3 Brown/Green White/Green
V4 C4 Brown/Blue White/Brown
V5 C5 Brown/Orange White/Black
V6 C6 Brown/Violet White/Violet
Electrode labels Electrode colors
AAMI EASI IEC AAMI IEC
1RA placement: directly below the clavicle and
near the right shoulder
2LA placement: directly below the clavicle and
near the left shoulder
3LL placement: on the left lower abdomen
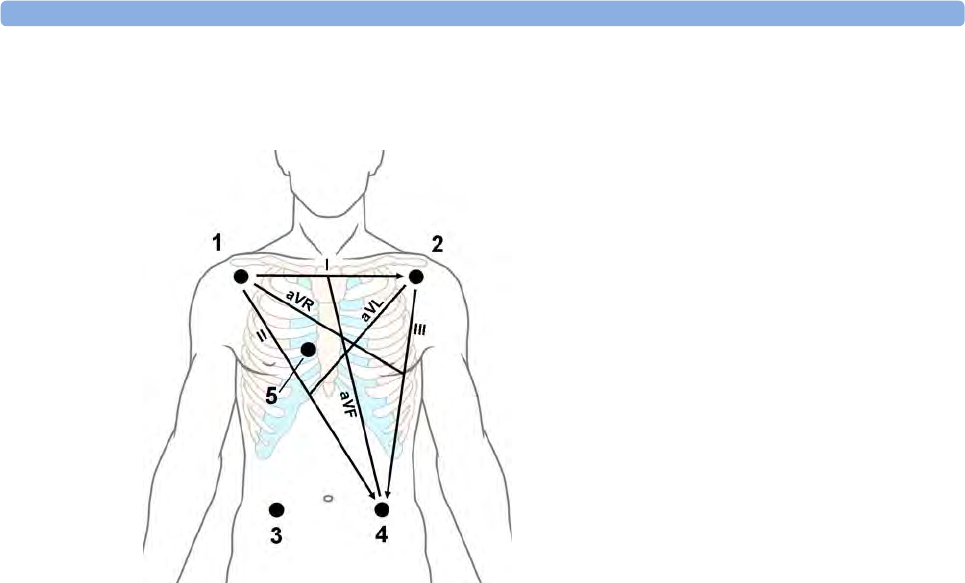
5 ECG, Arrhythmia, ST and QT Monitoring
119
Standard 5-Lead Placement
6-Lead Placement
For a 6-lead placement use the positions from the 5-lead diagram above but with two chest leads. The
two chest leads, Va and Vb, can be positioned at any two of the V1 to V6 positions shown in the chest
electrode diagram below. The Va and Vb lead positions chosen must be selected in the Setup ECG
Menu to ensure correct labeling.
1RA placement: directly below the clavicle and
near the right shoulder
2LA placement: directly below the clavicle and
near the left shoulder
3RL placement: on the right lower abdomen
4LL placement: on the left lower abdomen
5V placement: on the chest, the position
depends on your required lead selection
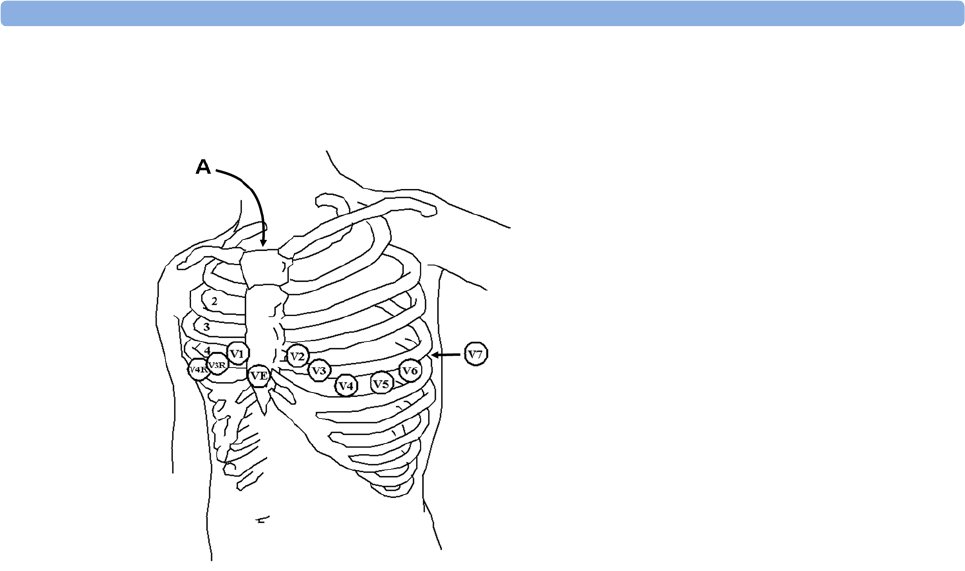
5 ECG, Arrhythmia, ST and QT Monitoring
120
Chest Electrode Placement
For accurate chest electrode placement and measurement, it is important to locate the fourth
intercostal space.
1Locate the second intercostal space by first palpating the Angle of Lewis (the little bony
protuberance where the body of the sternum joins the manubrium). This rise in the sternum is
where the second rib is attached, and the space just below this is the second intercostal space.
2Palpate and count down the chest until you locate the fourth intercostal space.
10-Lead Placement
When monitoring 12-leads of ECG, using a 10-Electrode Lead Placement, it is important to correctly
place electrodes and to label all 12-lead ECG reports with the correct lead placement.
V1 on the fourth intercostal space at the right
sternal border
V2 on the fourth intercostal space at the left
sternal border
V3 midway between the V2 and V4 electrode
positions
V4 on the fifth intercostal space at the left
midclavicular line
V5 on the left anterior axillary line, horizontal
with the V4 electrode position
V6 on the left midaxillary line, horizontal with the
V4 electrode position
V3R -V6R on the right side of the chest in
positions corresponding to those on the left
VE over the xiphoid process
V7 on posterior chest at the left posterior axillary
line in the fifth intercostal space
V7R on posterior chest at the right posterior
axillary line in the fifth intercostal space
A - Angle of Lewis
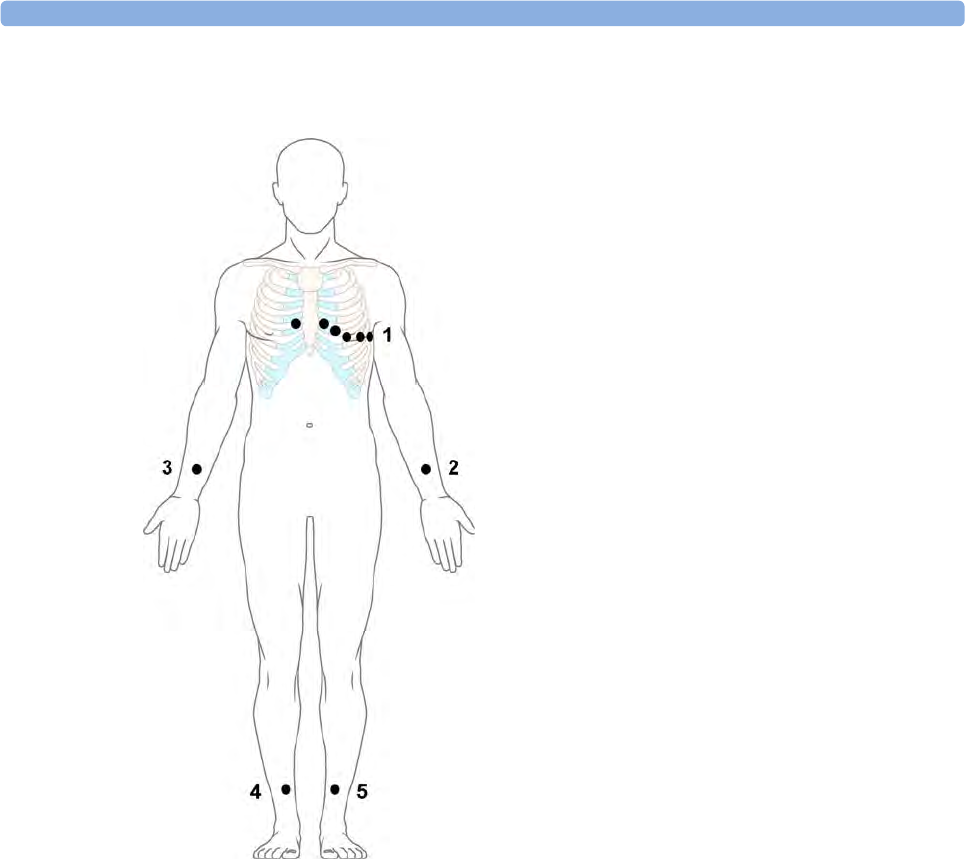
5 ECG, Arrhythmia, ST and QT Monitoring
121
Conventional 12-Lead ECG
In conventional 12-Lead ECG using 10 electrodes, an electrode is placed on the right arm, left arm,
right leg, and left leg. Six V- electrodes are placed on the chest. The right leg electrode is the reference
electrode.
Limb electrodes:
– Place arm electrodes on the inside of each arm, between the wrist and the elbow.
– Place leg electrodes inside of each calf, between the knee and the ankle.
Chest electrodes:
V1 - on the 4th intercostal space at the right sternal border
V2 - on the 4th intercostal space at the left sternal border
V3 - midway between the V2 and V4 electrode positions
V4 - on the 5th intercostal space at the left midclavicular line
V5 - on the left anterior axillary line, horizontal with the V4 electrode position
V6 - on the left midaxillary line, horizontal with the V4 electrode position
1V1 - V6
2LA
3RA
4RL
5LL
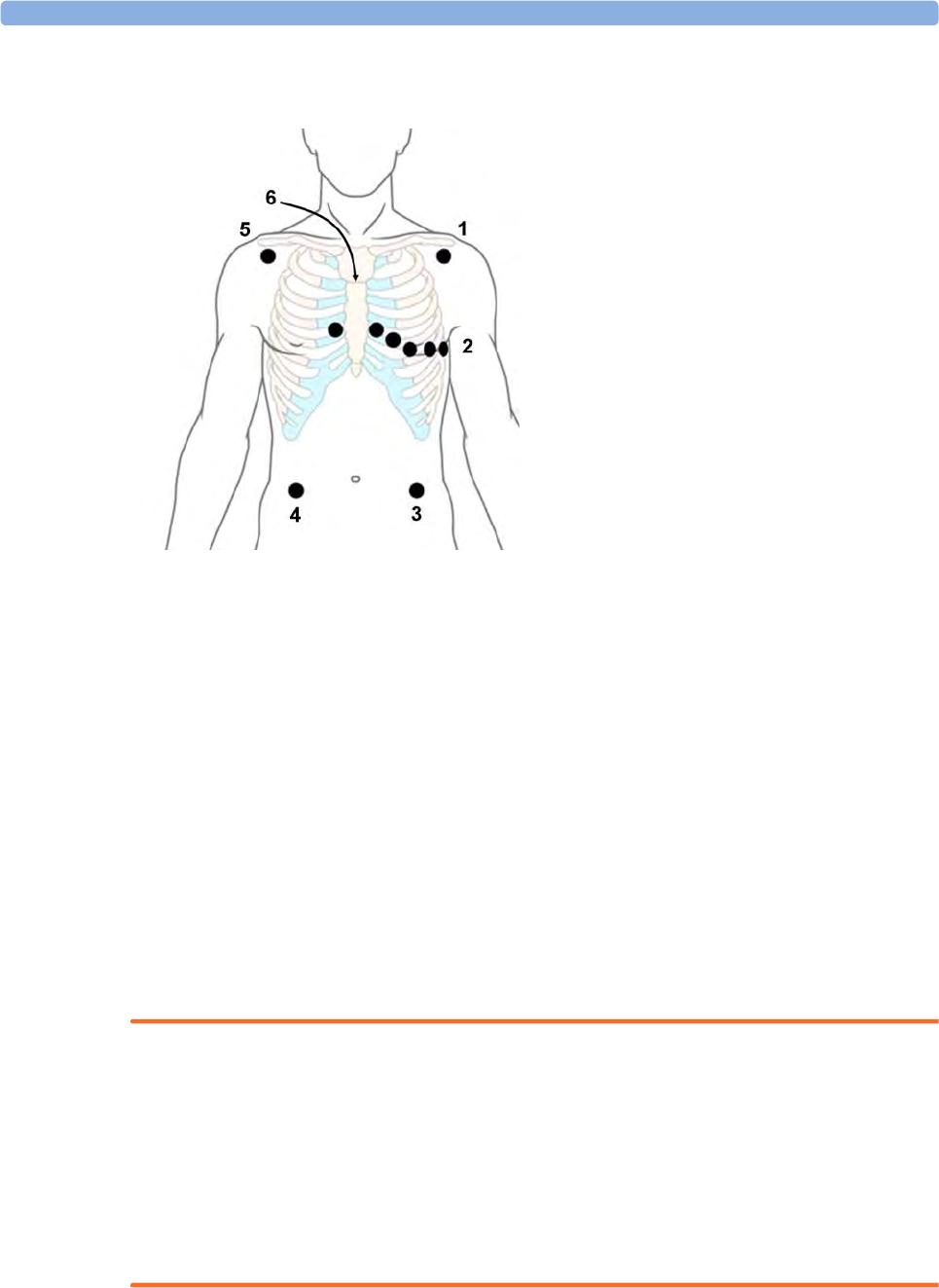
5 ECG, Arrhythmia, ST and QT Monitoring
122
Modified 12-Lead ECG
If your institution uses modified 10 Lead ECG electrode placement (the Mason-Likar Lead System),
place the four limb electrodes close to the shoulders and lower abdomen.
The six V electrodes are placed on the chest in the same position as the conventional 12-lead
placement.
Choosing Standard or Modified Electrode Placement
If your institution uses modified 10 Lead ECG electrode placement (the Mason-Likar Lead System),
you must switch Mod.LeadPlacment to On in the monitor. To do this,
•in the Setup ECG menu, select Mod.LeadPlacment to toggle between On and Off.
– When Mod.LeadPlacment is set to On, 12 Lead ECG Reports will be labeled 12 Lead ECG
Report (Mason-Likar), and captured 12-lead ECGs will be labeled Mason-Likar to the right
of the bandwidth annotation at the Information Center.
– When Mod.LeadPlacment is set to Off, 12 Lead ECG Reports will be labeled 12 Lead ECG
Report (Standard), and captured 12-lead ECGs will not be annotated at the Information
Center.
WARNING
Do not use ECG analysis interpretation statements and measurements for 12-lead ECGs obtained
using the modified (Mason-Likar) limb electrode placement. This may lead to misdiagnosis since the
modified (Mason-Likar) limb electrode placement does not look the same as the conventional 12-lead
ECG and may mask inferior infarction due to calculated axis, R, P and T wave magnitudes shifts and
ST slope.
Do not export 12-lead ECGs obtained using the modified (Mason-Likar) limb electrode placement.
Captured 12-Lead ECGs using the modified (Mason-Likar) limb electrode placement exported from
the Information Center are not annotated with the Mason-Likar label.
1LA
2V1-V6
3LL
4RL
5RA
6Angle of Lewis

5 ECG, Arrhythmia, ST and QT Monitoring
123
Capture 12-Lead
You can view a 12-Lead ECG on the screen, capture a 12-Lead ECG episode, preview the captured
ECG data and then store it and send it to a connected Information Center for analysis. You can also
print a 12-Lead report.
The monitor can store one 12-Lead ECG episode at any time.
Viewing the Realtime 12-Lead ECG
To open the 12-Lead ECG window and view the realtime ECG waves,
• Select the Capture 12 Lead SmartKey, or
•Select
Main Screen, then Capture 12 Lead.
If a previously viewed 12-Lead ECG was not stored, a window will pop up asking whether you want to
keep it or not. The title bar of the window shows the date and time when this 12-Lead ECG was
captured. If you do not need the ECG, select No to discard it, otherwise, select Yes and then select
Store & Send to store that 12-Lead ECG and send it to an Information Center (if one is connected).
If your patient is not admitted, you will be prompted to enter at least the age and gender of the patient.
This information is needed for analysis of the 12-Lead ECG at the Information Center but is not
essential if you only want to capture the 12-Lead ECG without sending it for analysis. To enter this
information:
1Select the Admit Patient pop-up key, then
2Enter the information in the Patient Demographics window.
3Open the 12-Lead ECG window again as described above.
The age and gender will now be displayed in the title bar of the pop-up keys.
To change the way the realtime waves are displayed, select the Change View pop-up key or select the
wave area. You can switch between a one or two column display. The two column display lets you see
a larger representation of the waves.
While the realtime 12-Lead waves are being viewed in the window, the ECG filter mode (see
“Changing the ECG Filter Settings” on page 115) is changed to the 12-Lead filter setting (see “Setting
Up the 12-Lead ECG” on page 124).
Capturing the 12-Lead ECG
To capture the last 10 seconds of ECG data, select the Capture Waves pop-up key. The pop-up key is
active as soon as enough wave data is available; until then a progress bar is displayed in the title bar of
the pop-up keys. A preview of the captured data appears on the screen (unless your monitor is
connected to an Information Center with software release earlier than Revision M — then the
captured data is automatically stored and sent to the Information Center).
The title bar of the pop-up keys will now show the current filter setting and, if you are using EASI lead
placement, an EASI indicator (see “EASI ECG Lead Placement” on page 125).
You can at any time return to the realtime 12-Lead ECG view by selecting the Show Waves pop-up
key. From there, you return to the preview window by selecting the Show Preview pop-up key.
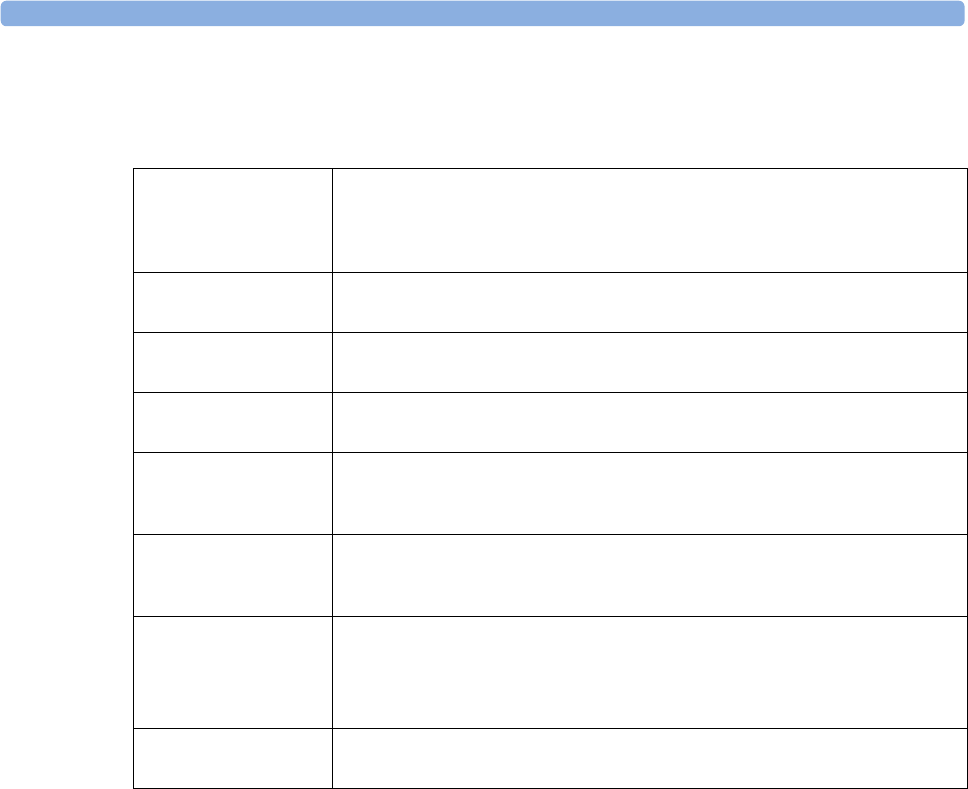
5 ECG, Arrhythmia, ST and QT Monitoring
124
Setting Up the 12-Lead ECG
In the Preview window, select the Setup 12 Lead pop-up key to choose settings for filter, gain, etc., if
changes are needed. All changes apply to both the display and the printed 12-Lead report.
Storing and Sending the 12-Lead ECG
You can enter an order number that will then be associated with the 12-Lead ECG. To enter an order
number, select the Enter OrderNo. pop-up key. The order number will be displayed in the title bar of
the pop-up keys.
To store the previewed data on the monitor and send it to a connected Information Center for storage
and analysis, select the Store & Send pop-up key. If the monitor is connected to an Information
Center, use the Store & Send function before patient transport to store the 12-Lead ECG centrally, as
the 12-Lead ECG data will not be uploaded from the MMS to another monitor after transport.
If the connection to the Information Center is not active while storing, the 12-Lead ECG will be
automatically sent as soon as the connection is established or restored. If a previously stored 12-Lead
ECG is waiting to be sent to the Information Center, it will be overwritten when a new 12-Lead ECG
is stored and can then not be sent to the Information Center.
Printing the 12-Lead ECG
Print a dedicated 12-Lead ECG report by selecting the Print Report pop-up key.
Filter Applies a filter to the waveforms.
Choices are 0.05-150Hz D, 0.5-150Hz eM, 0.5-40Hz M (or 0.5-55Hz M for
pediatric and neonatal patient categories), 0.5-20Hz F. The selected filter will be
displayed in the title bar of the pop-up keys.
Gain Defines the gain used for the waveforms.
Choices are 2.5 mm/mV, 5 mm/mV, 10 mm/mV and 20 mm/mV.
Chest Gain Defines the gain for the chest leads relative to the standard gain setting.
Choices are Full and Half.
Paper Speed Defines the waveform speed.
Choices are 25 mm/sec and 50 mm/sec.
Format Defines the page layout.
Choices are 12X1, 6X2, 3X4, 3X4 1R and 3X4 3R. 1R and 3R refer to 1 or 3 rhythm
leads.
Time Defines whether all leads show simultaneous or sequential intervals of time, when
displaying or printing 2 or more columns.
Choices are Sequential and Simultaneous.
Rhythm Lead 1
Rhythm Lead 2
Rhythm Lead 3
Defines which lead will be used as rhythm lead 1, 2 or 3.
Choices are Primary, Secondary, I, II, III, aVR, aVL, aVF, V1, V2, V3, V4, V5, V6,
V, MCL.
This setting is only relevant when 3X4 1R or 3X4 3R is selected as Format.
Lead Sequence Defines the sequence in which the leads are presented.
Choices are Cabrera and Internat.
5 ECG, Arrhythmia, ST and QT Monitoring
125
Capture 12-Lead Pop-up Keys
Here is a summary of all the pop-up keys available during 12-Lead ECG procedure:
EASI ECG Lead Placement
Using a standard 5-electrode set in EASI lead placement you can monitor up to 12 standard ECG leads
simultaneously and continuously at the bedside. EASI provides a monitoring method for trending ST
segment changes that can provide an early indication of ischemia.
WARNING
EASI-derived 12-lead ECGs and their measurements are approximations to conventional 12-lead
ECGs. As the 12-lead ECG derived with EASI is not exactly identical to the 12-lead conventional
ECG obtained from an electrocardiograph, it should not be used for diagnostic interpretations.
Respiratory monitoring is also possible with the EASI placement; respiration is measured between the
I and A electrodes.
Place the electrodes as accurately as possible to obtain the best quality EASI measurements.
When EASI lead placement is selected, EASI is shown beside the 1mV calibration bar on the ECG
wave on the display, and EASI is marked on any recorder strips and printouts.
EASI Monitoring During INOP Conditions
If one of the derived EASI leads has an INOP condition (for example, LEAD OFF), a flat line is
displayed. After 10 seconds, the directly acquired EASI AI, AS, or ES lead (depending on which is
available) is displayed with the corresponding lead label. This causes an arrhythmia relearn.
Pop-up Keys Selecting this pop-up key lets you
Admit Patient enter the age and gender for the patient in the Patient Demographics
window, to allow analysis of the 12-Lead ECG.
Change View switch between the single column and two-column display of the realtime
wave data.
Capture Waves capture the current ECG waves and open the preview window.
Show Waves return to the realtime 12-Lead ECG view.
Show Preview show the preview of the captured 12-Lead wave data.
Setup 12 Lead choose settings for filter, gain, display layout, etc.
Enter OrderNo. enter an order number that is stored with the capture and displayed in the
title bar of the pop-up keys.
Print Report print a 12-Lead report.
Store & Send store the captured 12-Lead ECG in the monitor and send it to the
Information Center.
Show Stored view a previously stored 12-Lead ECG, allowing a visual comparison
between the current and the stored data.
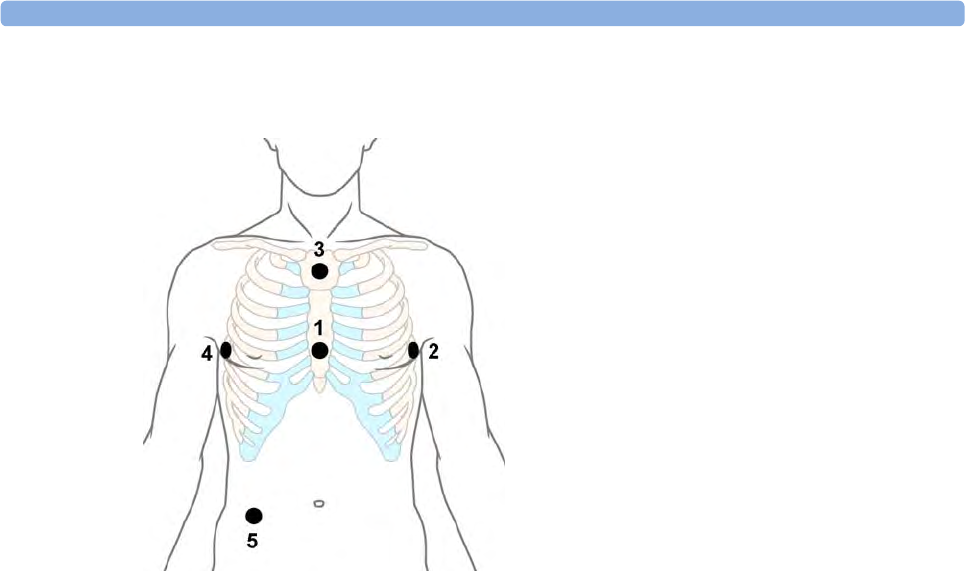
5 ECG, Arrhythmia, ST and QT Monitoring
126
EASI Electrode Placement
ECG and Arrhythmia Alarm Overview
The ECG and arrhythmia alarms available depend on which measurements are switched on, and the
arrhythmia option enabled for your monitor.
• Cardiotach alarms are available when HR is on and the active alarm source is ECG, but arrhythmia
is switched off
• Basic arrhythmia alarms are available when Arrhythmia is switched on
• Advanced arrhythmia alarms are available when Arrhythmia is switched on and the Advanced
Arrhythmia option has been enabled for your monitor
1E (V) - on the lower sternum at the level of
the fifth intercostal space
2A (LL) - on the left midaxillary line at the
same level as the E electrode
3S (LA) - on the upper sternum
4I (RA) - on the right midaxillary line at the
same level as the E electrode
5N - reference electrode - can be anywhere,
usually below the sixth rib on the right hip
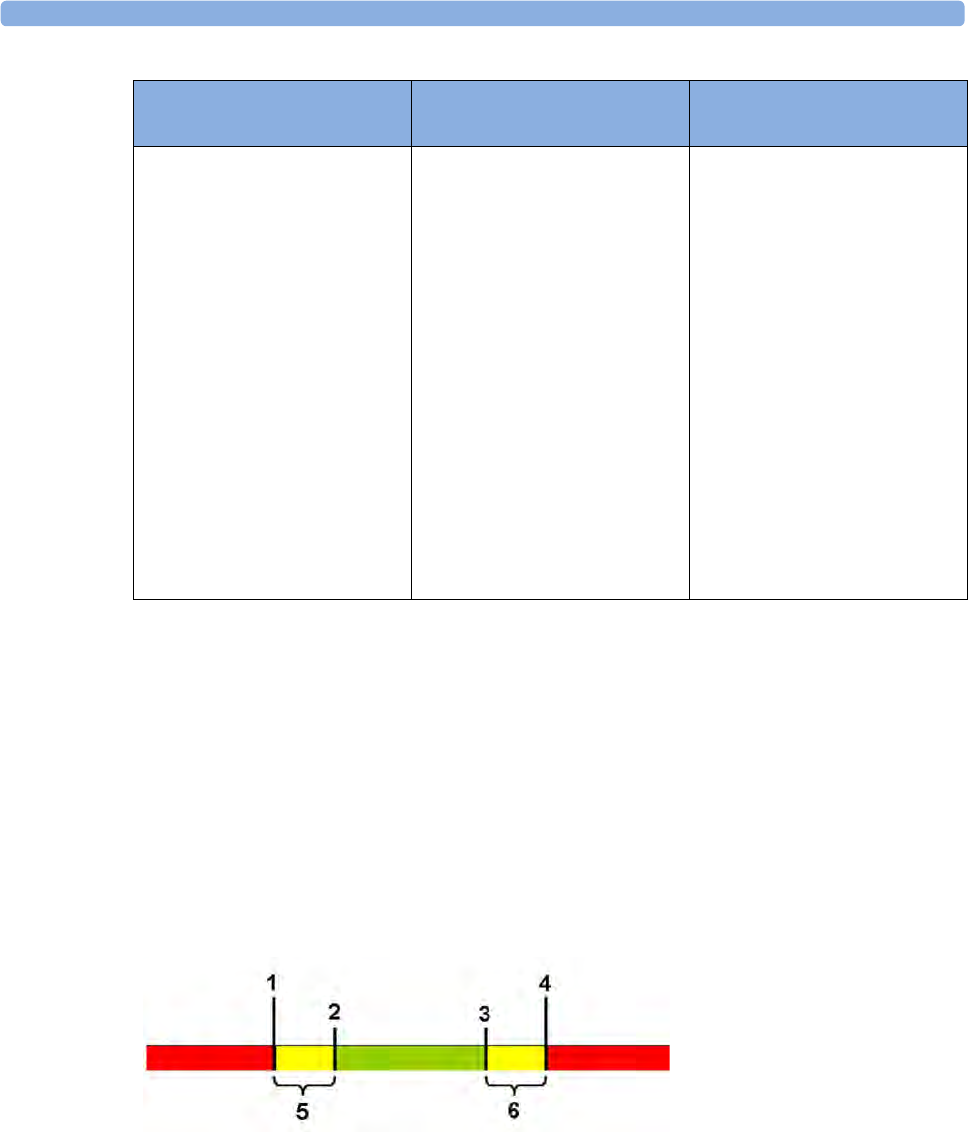
5 ECG, Arrhythmia, ST and QT Monitoring
127
Using ECG Alarms
ECG alarms can be switched on and off and the high and low alarm limits changed just like other
measurement alarms, as described in the Alarms chapter. Special alarm features which apply only to
ECG are described here.
Extreme Alarm Limits for Heart Rate
The extreme rate alarms, Extreme Tachy and Extreme Brady, generated by the active alarm source,
either HR or Pulse, are set in Configuration Mode by adding a set value (the Δ value) to the high and
low alarm limits.
You need to know which value has been configured for your monitor. Changing the high and low
alarm limits automatically changes the extreme alarm limits within the allowed range.
To see the extreme rate alarms set for your monitor, in the Setup ECG menu, see the menu items Δ
ExtrTachy and Δ ExtrBrady.
Cardiotach Alarms Additional Alarms with Basic
Arrhythmia Option
Additional Alarms with
Enhanced Arrhythmia Option
***Asystole
***Ventricular Fibrillation/
Tachycardia
***Extreme Bradycardia
***Extreme Tachycardia
**High heart rate
**Low heart rate
***Ventricular Tachycardia
**Pacer Not Capture
**Pacer Not Pacing
**PVCs/min HIGH (PVC >
limit/min)
**Afib
**Supraventricular Tach
**Missed Beat
**Pause
**Irregular HR
**Ventricular Rhythm
**Run PVCs High
**Pair PVCs
**R-on-T PVCs
**Ventricular bigeminy
**Ventricular trigeminy
**Non-sustain VT
**Multiform PVCs
1Extreme Brady Limit
2Low Limit
3High Limit
4Extreme Tachy Limit
5Δ Extreme Brady
6Δ Extreme Tachy
5 ECG, Arrhythmia, ST and QT Monitoring
128
ECG Alarms Off Disabled
Be aware that your hospital department may have decided to disable the Alarms Off setting for ECG
in the monitor's Configuration Mode. In this case, HR alarms cannot be switched off in Monitoring
Mode. If you try to switch off the HR alarms, you will see the message To activate enter Config and
enable Alarms Off.
HR Alarms When Arrhythmia Analysis is Switched Off
When arrhythmia analysis is switched off, only these HR-related alarms will be detected:
• the asystole alarm
• the ventricular fibrillation/tachycardia alarm
• the extreme tachycardia and extreme bradycardia alarms
• the high heart rate and low heart rate alarms.
Enhanced Asystole Detection
In order to improve alarming on asystole under certain conditions, you can set Asystole Detect. in
Configuration Mode to Enhanced. In enhanced mode an asystole alarm will be suppressed for up to
five seconds if a valid beat-to-beat Pulse is detected from a Pressure.
ECG Safety Information
CAUTION
Interference from instruments near the patient and ESU interference can cause problems with the
ECG wave. See the monitor specifications for more information.
WARNING
Defibrillation and Electrosurgery:
Do not touch the patient, or table, or instruments, during defibrillation.
After defibrillation, the screen display recovers within 10 seconds if the correct electrodes are used and
applied in accordance with the manufacturers instructions.
ECG cables can be damaged when connected to a patient during defibrillation. Check cables for
functionality before using them again.
According to AAMI specifications the peak of the synchronized defibrillator discharge should be
delivered within 60 ms of the peak of the R wave. The signal at the ECG output on the IntelliVue
patient monitors is delayed by a maximum of 30 ms. Your biomedical engineer should verify that your
ECG/Defibrillator combination does not exceed the recommended maximum delay of 60 ms.
When using electrosurgical (ES) equipment, never place ECG electrodes near to the grounding plate of
the ES device, as this can cause a lot of interference on the ECG signal.
General:
When you are connecting the electrodes or the patient cable, make sure that the connectors never
come into contact with other conductive parts, or with earth. In particular, make sure that all of the
ECG electrodes are attached to the patient, to prevent them from contacting conductive parts or earth.

5 ECG, Arrhythmia, ST and QT Monitoring
129
During surgery:
Use the appropriate orange electrode ECG safety cable, or lead cable with an orange connector, for
measuring ECG in the operating room. These cables have extra circuitry to protect the patient from
burns during cautery, and they decrease electrical interference. This also reduces the hazard of burns in
case of a defective neutral electrode at the HF device. These cables cannot be used for measuring
respiration.
Pacemaker failure:
During complete heart block or pacemaker failure to pace/capture, tall P-waves (greater than 1/5 of
the average R-wave height) may be erroneously counted by the monitor, resulting in missed detection
of cardiac arrest.
Patients exhibiting intrinsic rhythm:
When monitoring paced patients who exhibit only intrinsic rhythm, the monitor may erroneously
count pace pulses as QRS complexes when the algorithm first encounters them, resulting in missed
detection of cardiac arrest.
The risk of missing cardiac arrest may be reduced by monitoring these patients with low heart rate limit
at or slightly above the basic/demand pacemaker rate. A low heart rate alarm alerts you when the
patient's heart rate drops to a level where pacing is needed. Proper detection and classification of the
paced rhythm can then be determined.
Filtered ECG signal from external instruments:
Instruments such as defibrillators or telemetry units produce a filtered ECG signal. When this signal is
used as an input to the bedside monitor, it is filtered again. If this twice-filtered signal is passed to the
arrhythmia algorithm, it may cause the algorithm to fail to detect pace pulses, pacemaker non-capture,
or asystole, thus compromising paced patient monitoring performance.
External pacing electrodes:
When a pacemaker with external pacing electrodes is being used on a patient, arrhythmia monitoring is
severely compromised due to the high energy level in the pacer pulse. This may result in the arrhythmia
algorithm's failure to detect pacemaker noncapture or asystole.
Fusion beat pacemakers:
Pacemakers that create fusion beats (pace pulse on top of the QRS complex) cannot be detected by the
monitor's QRS detector.
Rate adaptive pacemakers:
Implanted pacemakers which can adapt to the Minute Ventilation rate may occasionally react on the
Impedance measurement used by patient monitors for the determination of the Resp value and
execute pacing with the maximum programmed rate. Switching off the Resp measurement can prevent
this.
About Arrhythmia Monitoring
Arrhythmia analysis provides information on your patient's condition, including heart rate, PVC rate,
rhythm, and ectopics. The monitor uses the user-selected primary and secondary ECG leads for single-
lead or multi-lead arrhythmia analysis. During arrhythmia analysis, the monitor continuously

5 ECG, Arrhythmia, ST and QT Monitoring
130
• optimizes ECG signal quality. This is important for arrhythmia analysis. The monitor continuously
filters the ECG signal to remove baseline wander, muscle artifact, and signal irregularities. Also, if
the Patient Paced status is set to Yes, pace pulses are filtered out to avoid processing them as QRS
beats.
• detects beats, for example, QRS complexes, identifying them for further analysis.
• measures signal features such as R-wave height, width, and timing.
• creates beat templates, and classifies and labels beats to aid in rhythm analysis and alarm detection.
• examines the ECG signal for ventricular fibrillation, asystole, and noise.
Arrhythmia Options
Your monitor has either the basic or the enhanced arrhythmia option. Both options provide rhythm
and ectopic status messages and beat labeling. The number of rhythms being classified, events being
detected, and alarms generated differs according to the option. The alarms available with the different
options are listed in the section “ECG and Arrhythmia Alarm Overview” on page 126, the rhythm and
ectopic messages detected are listed in “Arrhythmia Status Messages” on page 132.
Where Can I Find More Information?
See the Application Notes on ST and Arrhythmia supplied on your documentation DVD for detailed
information on the arrhythmia algorithm and its clinical application.
Switching Arrhythmia Analysis On and Off
1In the Setup Arrhythmia menu, select Arrhythmia to toggle between On and Off.
2Select the Confirm pop-up key which appears at the bottom of the screen.
Be aware that when arrhythmia analysis is switched off,
– the message Arrhythmia Off appears beside the ECG wave, if configured to do so
– only the HR-related alarms are detected (the asystole alarm, the ventricular fibrillation/
tachycardia alarm, the extreme tachycardia and extreme bradycardia alarms, the high heart rate
and low heart rate alarms)
– HR High and HR Low alarms behave like normal yellow alarms, no timeout periods are active.
Choosing an ECG Lead for Arrhythmia Monitoring
It is important to select a suitable lead for arrhythmia monitoring.
Guidelines for non-paced patients are:
– QRS complex should be tall and narrow (recommended amplitude > 0.5 mV)
– R-Wave should be above or below the baseline (but not bi-phasic)
– T-wave should be smaller than 1/3 R-wave height
– the P-wave should be smaller than 1/5 R-wave height.
For paced patients, in addition to the above, the pace pulse should be:
– not wider than the normal QRS
– the QRS complexes should be at least twice the height of pace pulses
– large enough to be detected, with no re-polarization.

5 ECG, Arrhythmia, ST and QT Monitoring
131
To prevent detection of P-waves or baseline noises as QRS complexes, the minimum detection level
for QRS complexes is set at 0.15 mV, according to AAMI-EC 13 specifications. Adjusting the ECG
wave size on the monitor display (gain adjustment) does not affect the ECG signal which is used for
arrhythmia analysis. If the ECG signal is too small, you may get false alarms for pause or asystole.
Aberrantly-Conducted Beats
As P-waves are not analyzed, it is difficult and sometimes impossible for the monitor to distinguish
between an aberrantly-conducted supraventricular beat and a ventricular beat. If the aberrant beat
resembles a ventricular beat, it is classified as ventricular. You should always select a lead where the
aberrantly-conducted beats have an R-wave that is as narrow as possible to minimize incorrect calls.
Ventricular beats should look different from these 'normal beats'. Instead of trying to select two leads
with a narrow R-wave, it may be easier to just select one lead and use single lead arrhythmia
monitoring. Extra vigilance is required by the clinician for this type of patient.
Atrial Fibrillation Alarm
The monitor performs atrial fibrillation analysis using information about the RR irregularity, PR
interval variability and P wave variability.
In order to generate an Afib alarm the following criteria must be detected for 1 minute:
• normal beat RR intervals must be irregular
• PR interval deviation must be large
• P-wave region must not match well
Atrial fibrillation analysis is only available for adult patients and atrial fibrillation detection cannot be
performed on PVCs or Paced beats.
Since most atrial flutters have regular RR intervals, they cannot be detected by the atrial fibrillation
algorithm.
An Afib alarm can be falsely detected in the presence of:
• sinus arrhythmia,
• muscle noise, or
• electrode motion artifact.
If you also have monitors with earlier software revisions, the Afib alarm will not be generated after a
transfer to one of these monitors. Always leave the Irregular HR alarm switched on, so that this alarm
can be generated in such situations.
See the Application Note on Arrhythmia/ST supplied on your documentation DVD for detailed
information on the arrhythmia algorithm and ECG analysis.
Intermittent Bundle Branch Block
Bundle branch and the other fascicular blocks create a challenge for the arrhythmia algorithm. If the
QRS during the block changes considerably from the learned normal, the blocked beat may be
incorrectly classified as ventricular, causing false PVC alarms. You should always select a lead where
the bundle branch block beats have an R-wave that is as narrow as possible to minimize incorrect calls.
Ventricular beats should look different from these 'normal beats'. Instead of trying to select two leads
with a narrow R-wave, it may be easier to just select one lead and use single lead arrhythmia
monitoring. Extra vigilance is required by the clinician for this type of patient.
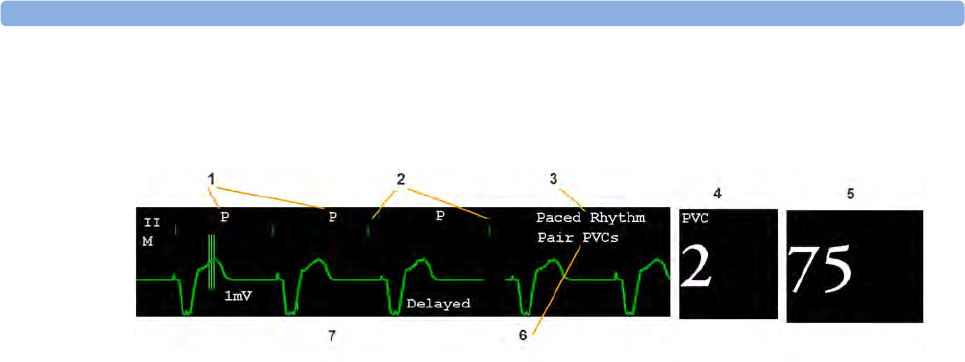
5 ECG, Arrhythmia, ST and QT Monitoring
132
Understanding the Arrhythmia Display
Your monitor screen may look slightly different from the illustration.
1Beat label
2Pace pulse marks
3Rhythm status message
4PVC Numeric
5HR Numeric
6Ectopic status message
7Delayed arrhythmia wave
Viewing Arrhythmia Waves
To review arrhythmia beat labels, in the Setup Arrhythmia menu, select Annotate Arrhy.
The wave showing the primary ECG lead will be delayed by six seconds and shown on a gray
background. Beat labels will be annotated above the ECG wave and Delayed will be written beside it.
To return to the normal ECG primary lead display, select Annotate Arrhy again.
Arrhythmia Beat Labels
Arrhythmia beat labels tell you how the monitor is classifying beats.
N = Normal
V = Ventricular Ectopic
S = Supra-ventricular Premature
P = Paced
' = Pacer spike
" = Biventricular Pacer Spike
L = Learning patient's ECG
A = Artifact (noisy episode)
? = Insufficient information to classify beats
I = Inoperative condition (e.g., LEADS OFF)
M = Pause or missed beat
Arrhythmia Status Messages
The monitor displays two types of status messages:
5 ECG, Arrhythmia, ST and QT Monitoring
133
• Rhythm Status Messages -- to indicate the patient's rhythm.
• Ectopic Status Messages -- to indicate the presence of ectopic beats.
These status messages are shown on the right hand side of the primary ECG wave. They are updated
every second, with the exception of the Sinus and Supraventricular (SV) rhythm messages.
The Sinus and SV rhythm messages are updated based on the current heart rate, taking into account
the patient category (adult, pediatric, or neonatal). For the message to change from one rhythm status
to another, the HR must be in the new range for five beats.
If you have basic arrhythmia capability, you will get only messages for the alarms provided with this
level.
Rhythm Status Messages
The label B or E indicates basic (B) or enhanced (E) arrhythmia capability.
Ectopic Status Messages
The label B or E indicates basic (B) or enhanced (E) arrhythmia capability.
Rhythm Status Message Description B or E
Asystole No QRS for 4 consecutive seconds in absence of vent fib or
chaotic signal
B, E
Vent Fib/Tach A fibrillatory wave for 4 consecutive seconds B, E
Vtach A dominant rhythm of adjacent Vs and a HR > the V-Tach
Heart Rate Limit
B, E
Sustained VT Ventricular tachycardia rhythm for more than 15 seconds E
Vent Rhythm A dominant rhythm of adjacent PVCs and a HR ≤ the V-Tach
HR Limit
E
Vent Bigeminy A dominant rhythm of N, V, N, V E
Vent Trigeminy A dominant rhythm of N, N, V, N, N, V E
Paced Rhythm A dominant rhythm of paced beats B, E
Irregular HR Consistently irregular rhythm E
Sinus Brady
Sinus Rhythm
Sinus Tach
A dominant rhythm of SV beats preceded by P-waves B, E
SV Brady
SV Rhythm
SV Tach
A dominant rhythm of SV beats not preceded by P-waves B, E
Unknown ECG Rhythm Rhythm cannot be determined B, E
Learning ECG Algorithm is learning the ECG beat morphology B, E
Learning Rhythm Algorithm is learning the rhythm of the classified beats B, E
CANNOT ANALYZE ECG ECG signal is predominantly invalid and therefore cannot be
analyzed
B, E
5 ECG, Arrhythmia, ST and QT Monitoring
134
Arrhythmia Relearning
During a learning phase:
• Alarm timeout periods are cleared
• Stored arrhythmia templates are cleared
• Asystole, Vfib, and HR alarms (when there are enough beats to compute the HR) are active. No
other alarms are active.
Initiating Arrhythmia Relearning Manually
To initiate relearning manually, in the Setup Arrhythmia menu, select Relearn Arrhy.
– While the monitor is learning, the delayed arrhythmia wave displays the beat label L and the
rhythm status message Learning ECG.
– Next, the monitor determines the dominant rhythm. The beats are labeled N, and the rhythm
status message changes to Learning Rhythm.
After relearning is complete, you should check the delayed arrhythmia wave to ensure that the
algorithm is labeling the beats correctly.
If beats are still not classified correctly, check that the ECG is optimized for arrhythmia monitoring.
You may need to select a different lead or change the electrodes or electrode positions if there is
excessive noise, unstable voltage, low amplitude, or large P- or T-waves.
Ectopic Status Message Explanation B or E
(No message displayed) No ectopic activity within the last minute
Run PVCs More than 2 consecutive PVCs within the last minute E
Pair PVCs Pair PVCs within the last minute E
Pacer Not Capt Pause with pace pulse (paced patient only) within the last
minute
B, E
Pacer Nt Pacing Pause without pace pulse (paced patient only) within the last
minute
B, E
Pause No beat detected for 1.75 x average R-R interval for HR <120,
or
No beat for 1 second with HR >120 (non-paced patient only),
or
No beat detected for more than the set pause threshold.
E
R-On-T PVCs R-ON-T detected within the last minute E
Multiform PVCs Multiform PVCs detected within the last minute E
Frequent SVPBs SVPB count within last minute is greater than 5 E
SVPBs 1-5 SVPBs in the last minute with a sinus rhythm and no Vs E
SV Beats SV count within last minute and rhythm status is paced B, E
Paced Beats Paced beat count within last minute and rhythm status is not
paced
B, E
5 ECG, Arrhythmia, ST and QT Monitoring
135
Automatic Arrhythmia Relearn
Arrhythmia relearning is initiated automatically whenever:
• ECG monitoring is switched on
• The ECG Lead or Lead Label of the primary/secondary lead is changed manually, or when
fallback occurs
• A Leads Off INOP condition (that has been active for > 60 seconds) ends.
If you are monitoring multi-lead arrhythmia and there is a change in one lead only, relearning happens
only in the affected lead. During this learning phase, the system will continue monitoring using the
other lead. Therefore, the delayed arrhythmia wave is not labeled L and there is no Learning ECG
rhythm status message. In addition, alarm timeout periods are maintained, stored arrhythmia templates
are maintained for the operative lead, and all alarms switched on are active.
Arrhythmia Relearn and Lead Fallback
Lead fallback triggers an automatic arrhythmia relearn.
WARNING
If arrhythmia learning takes place during ventricular rhythm, the ectopics may be incorrectly learned as
the normal QRS complex. This may result in missed detection of subsequent events of V-Tach and V-
Fib.
For this reason you should:
• take care to initiate arrhythmia relearning only during periods of predominantly normal rhythm
and when the ECG signal is relatively noise-free
• be aware that arrhythmia relearning can happen automatically
• respond to any INOP messages (for example, if you are prompted to reconnect electrodes)
• be aware that a disconnected EASI electrode triggers an arrhythmia relearn on all leads
• always ensure that the arrhythmia algorithm is labeling beats correctly.
Arrhythmia Alarms
Arrhythmia alarms can be switched on and off and the alarm settings changed just like other
measurement alarms, as described in the Alarms section. Special alarm features which apply only to
arrhythmia are described here.
The different alarms detected and generated by the monitor depend on the level of arrhythmia analysis
that is enabled. For a complete list of arrhythmia alarms and INOPs, see the Alarms chapter.
The monitor detects arrhythmia alarm conditions by comparing ECG data to a set of pre-defined
criteria. An alarm can be triggered by a rate exceeding a threshold (for example, HR >xx), an abnormal
rhythm (for example, Ventricular Bigeminy), or an ectopic event (for example, Pair PVCs).
5 ECG, Arrhythmia, ST and QT Monitoring
136
Yellow Arrhythmia Alarms
Yellow arrhythmia alarms are short yellow alarms specific to arrhythmia-related patient conditions.
Depending on your monitor and Information Center configuration, they may be shown with one or
two stars. The heart rate alarms (High HR and Low HR) can be configured as short yellow or standard
yellow alarms. When they are standard yellow alarms they exist independently of the other arrhythmia
alarms and no timeout periods apply.
WARNING
When arrhythmia analysis is on, all yellow ECG and arrhythmia alarms are short yellow alarms (one-
star). This means that the yellow alarm lamp and the tones are active for six seconds only, after which
the blinking numeric and the alarm message remain for up to three minutes. The only exception to this
are the HR High and Low alarms which can be configured as standard yellow alarms. Red alarms
behave as usual.
Arrhythmia Alarms and Latching
When using arrhythmia analysis, Visual Latching and Audible Latching should be on for red alarms,
or at least Visual Latching should be on. Because of the transient nature of arrhythmia alarms, many
arrhythmia conditions may go unnoticed if alarm latching is off. This setting can only be changed in
Configuration Mode.
Switching Individual Arrhythmia Alarms On and Off
Some arrhythmia alarms can be individually switched on or off:
Non-Sustain, Vent Rhythm, Run PVCs, Pair PVCs, R-On-T PVCs, V.Bigeminy, V.Trigeminy,
Multif.PVCs, Pause, SVT, IrregularHR, Missed Beat, PVCs/min and Afib.
To switch individual alarms on or off, in the Setup Arrhythmia menu, select the alarm from the list to
toggle between On and Off. The monitor displays the INOP message SOME ECG ALRMS OFF, if
configured, when more alarms are switched off than configured in your active profile.
Switching All Yellow Arrhythmia Alarms On or Off
All yellow arrhythmia alarms can be switched on and off together. To do this,
•In the Setup Arrhythmia menu, select All Yellow Off or All Yellow On.
Adjusting the Arrhythmia Alarm Limits
Some arrhythmia alarms have limits which can be individually adjusted:
VTach HR, VTach Run, PVCs/min, Vent Rhythm, SVT HR, SVT Run, Asystole Thresh., Pause
Threshold
1To adjust alarm limits, in the Setup Arrhythmia menu, select the alarm to be adjusted.
2Select the appropriate setting from the pop-up list.
Arrhythmia Alarm Timeout Periods
Normally, an arrhythmia alarm is announced when an alarm condition is detected. However, there are
certain situations that can inhibit the audible and visible indications of the alarm even though the alarm
condition was detected. These include:
5 ECG, Arrhythmia, ST and QT Monitoring
137
• if a more serious alarm condition is active in the same chain
• if a timeout period is in effect for a particular alarm
• if a timeout period is in effect for a higher alarm in that chain.
See “Arrhythmia Alarm Chaining” on page 138 for more details on alarm chains.
What is a Timeout Period?
Timeout periods are automatically started when a yellow arrhythmia alarm is detected. During this
period, the same alarm condition will not generate another alarm. Alarm conditions further down the
same arrhythmia alarm chain will also not generate an alarm, but alarms further up the chain will: see
“Arrhythmia Alarm Chaining” on page 138.
To view the timeout period configured for your monitor, in the Setup Arrhythmia menu, see the
menu items TimeOut 1st and TimeOut 2nd.
This setting can only be changed in Configuration Mode.
Resetting the Timeout Period
To reset the timeout period, select the Alarms Off or Pause Alarms permanent key and then reselect
it.
How are Yellow Arrhythmia Alarms Indicated?
When a yellow arrhythmia alarm is generated, it triggers visual and audible indicators. Yellow
arrhythmia alarms are always set to latch visually for three minutes except HR High/Low alarms, if
configured to standard yellow. Depending on the alarm condition, audible and visual alarm indicators
will appear as follows:
If you silence a yellow arrhythmia alarm and the alarm condition still exists, the visual indicators
continue until the condition stops. You will get an alarm reminder every time the configured timeout
period has expired.
If you silence a yellow arrhythmia alarm and the alarm condition has stopped, the visual
indicators are immediately cleared. Silencing an alarm does not reset its timeout period, so you will not
get a realarm for the same condition or lower on the chain until the timeout expires.
Alarm Condition Example Short yellow alarm tone sounds Alarm message
displayed
Single alarm
instance
Non-sustained V-
tach
when alarm condition is initially
detected
for 3 minutes (latching
time)
Continuous alarm
condition
PVCs/min HIGH when alarm condition is initially
detected and - as an alarm
reminder - every time the
configured timeout period has
expired
until the alarm
condition stops, plus a
maximum of three
minutes latching time
Same intermittent
alarm condition
Pair of PVCs each time the alarm condition is
detected, provided that the
configured timeout period has
expired
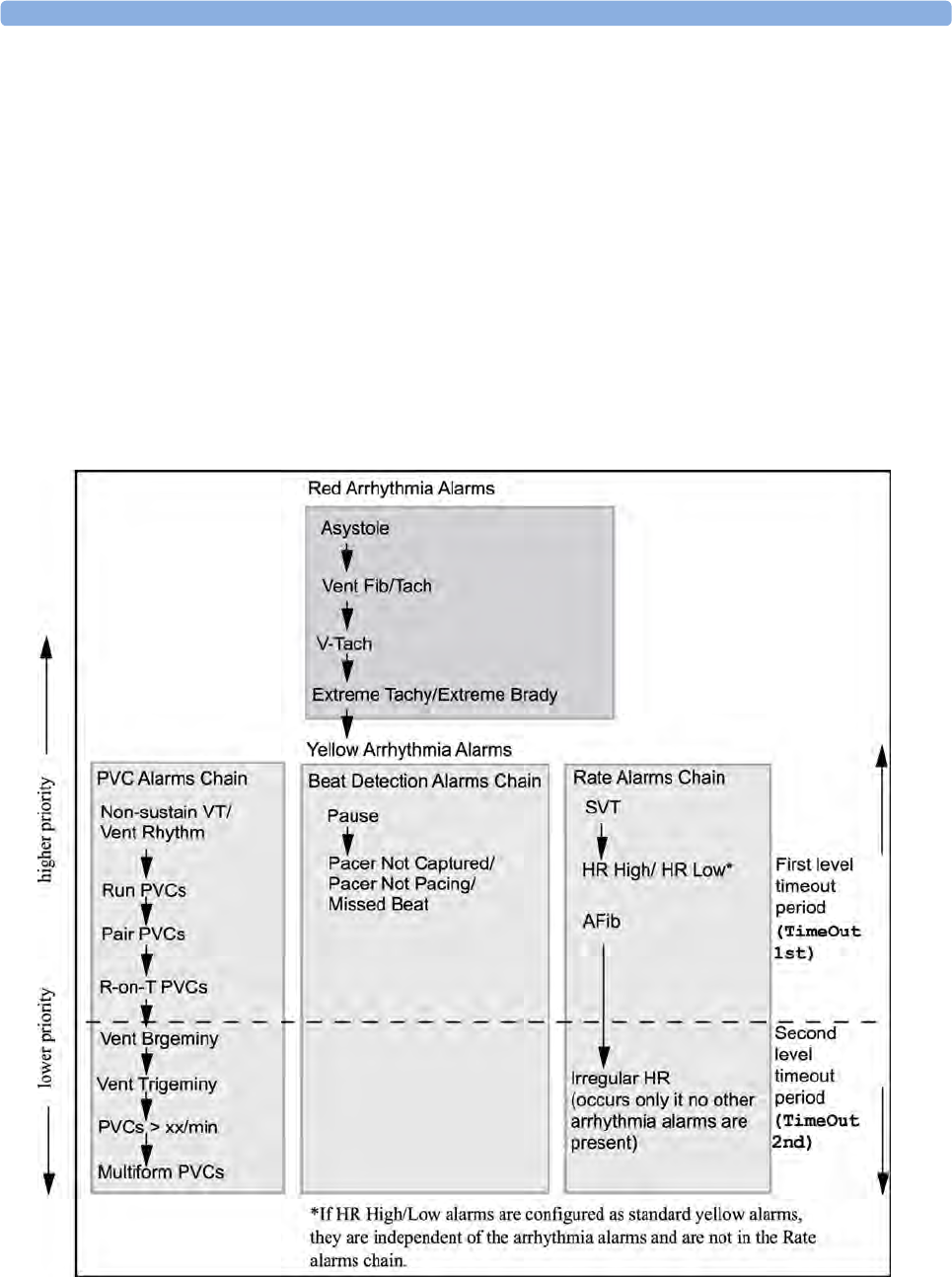
5 ECG, Arrhythmia, ST and QT Monitoring
138
Arrhythmia Alarm Chaining
When arrhythmia analysis is switched on, multiple alarm conditions may be present. Announcing all of
the detected alarm conditions would be confusing, and might hide a more serious condition. For this
reason, arrhythmia alarms are prioritized in three alarm "chains": PVC Alarms; Beat Detection Alarms,
and Rate Alarms.
Only the highest priority alarm condition in each chain is announced. Lower priority alarms in the
same chain will not be announced while an alarm is active or during the configured timeout period. If
alarm conditions of equal severity from different chains are detected, the alarm condition that occurred
most recently is announced. The exception is Irregular HR, which only occurs if no other alarms are
occurring.
See “ECG and Arrhythmia Alarm Overview” on page 126 for information on which alarms are
included in the different arrhythmia options. See “Arrhythmia Alarm Timeout Periods” on page 136
for an explanation of how alarm timeouts work.
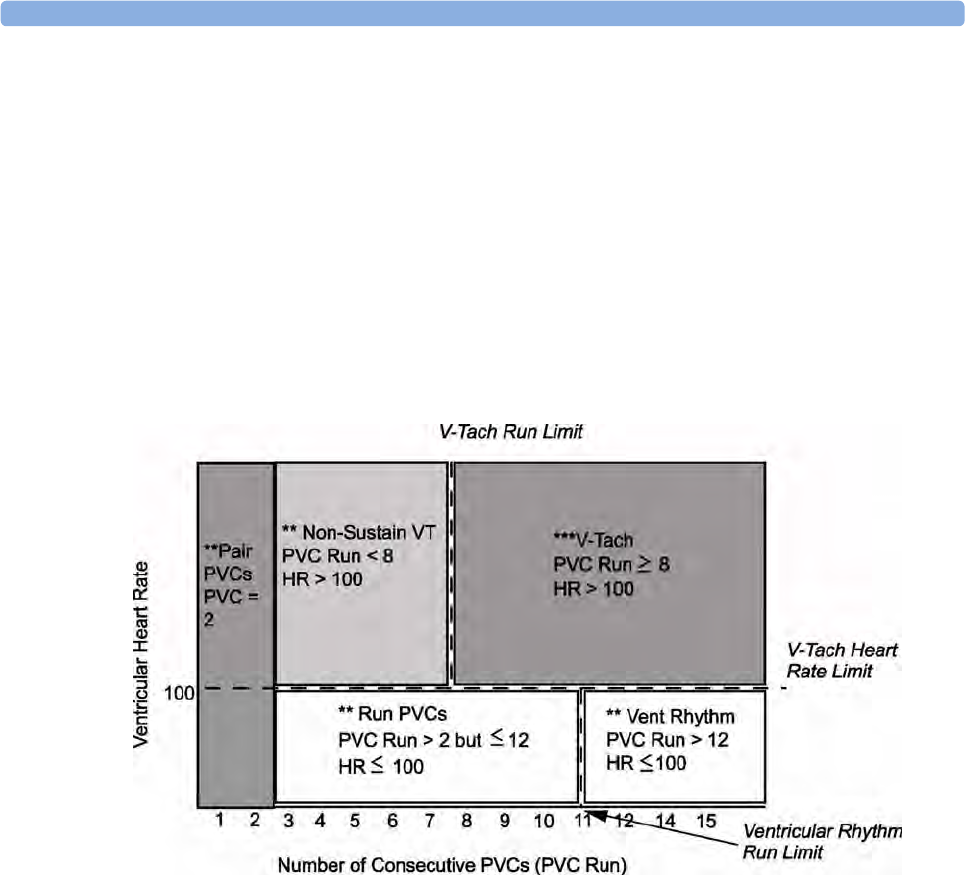
5 ECG, Arrhythmia, ST and QT Monitoring
139
– If there is an active Vent Bigeminy alarm, a PVCs > xx/min will not be triggered because it is
lower on the same chain. However, a high HR alarm will become active because it is on a
different chain.
– Higher priority alarms supersede previous alarms. For example, if a Vent Trigeminy alarm is
active and a Pair PVCs occurs, the Pair alarm will be activated.
Understanding PVC-Related Alarms
PVC-related alarms are detected on the basis of the current ventricular heart rate and the number of
consecutive PVCs counted (referred to as PVC Runs).
Example:
This diagram illustrates the conditions under which PVC alarms would be generated if the Vent
Rhythm Run limit is set to 12, the V-Tach Run Limit is set to 8, and the V-Tach HR Limit is set to 100.
You will see that
• if both the V-Tach Heart Rate Limit and the V-Tach Run Limit are exceeded, a red V-Tach alarm is
generated
• if the ventricular heart rate exceeds the V-Tach Heart Rate Limit but not the V-Tach Run Limit, a
yellow Non-Sustain VT alarm is generated.
About ST Monitoring
The monitor performs ST segment analysis on normal and atrially paced beats and calculates ST
segment elevations and depressions. This information can be displayed in the form of ST numerics and
snippets on the monitor.
All available leads can be monitored continuously. The ECG waveform does not need to be displayed
on the monitor for ST Segment analysis.
ST analysis is always performed using a dedicated filter which ensures diagnostic quality. If you are
monitoring ECG using an ECG filter mode other than Diagnostic, the ST segment of the ECG wave
may look different from the ST segment of the ST snippet for the same wave. For diagnostic
evaluation of the ST segment, always switch to Diagnostic filter mode or use the ST snippet.
5 ECG, Arrhythmia, ST and QT Monitoring
140
WARNING
Some clinical conditions may make it difficult to achieve reliable ST monitoring, for example:
• if you are unable to get a lead that is not noisy
• if arrhythmias such as atrial fib/flutter are present, which may cause an irregular baseline
• if the patient is continuously ventricularly paced
• if the patient has left bundle branch block.
You should consider switching ST monitoring off if these conditions are present.
This monitor provides ST level change information; the clinical significance of the ST level change
information should be determined by a physician.
ST segment monitoring is intended for use with adult patients only and is not clinically validated for
use with neonatal and pediatric patients. For this reason, the recommended - and default - setting for
ST monitoring in neonatal and pediatric modes is ST Analysis: Off.
Switching ST On and Off
To switch all ST monitoring on or off, in the Setup ST Analysis menu, select ST Analysis to toggle
between On and Off.
Selecting Leads for ST Analysis
You select which leads to use for ST analysis in the Setup ST Analysis menu.
To see the current list of leads selected for ST analysis:
1Enter the Setup ST Analysis menu.
2Select Setup ST Leads. This opens the Setup ST Leads pop-up window. Leads chosen for ST
monitoring are listed here. There are two pop-up keys at the bottom of the screen, Add and
Delete. If all leads are already selected, the Add pop-up key is disabled.
To choose a lead for ST monitoring:
1Select the Add key at the bottom of the Setup ST Leads window. This opens the Choices pop-up
window.
2Choose a lead from the list for ST monitoring. This closes the Choices window and adds the
selected lead to the list of chosen leads.
To disable ST monitoring for a lead:
1Choose a lead from the list in the Setup ST Leads window.
2Select the Delete key. This removes this lead from the list.
NOTE
The order in which ST leads are listed in the Setup ST Leads menu determines the order in which ST
leads are displayed on the monitor screen.
To change the order in which ST leads are displayed,
1In the Setup ST Leads menu, choose a lead from the list.
2Select the Sort Up or Sort Down key to move the lead up or down in the list.
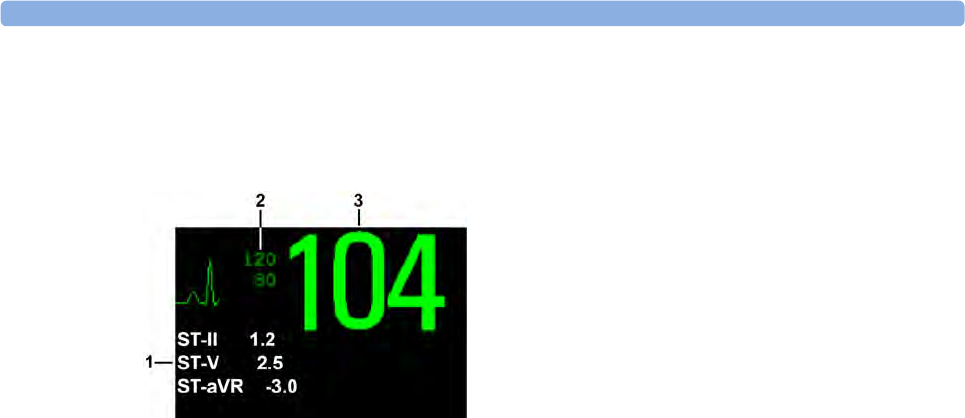
5 ECG, Arrhythmia, ST and QT Monitoring
141
Understanding the ST Display
Your monitor screen may be configured to look slightly different from the illustrations.
ST Numerics
Up to 12 ST numerics plus the ST index can be displayed on the monitor screen. They can be
configured to show beside the measurement numerics, beside the ECG wave, or beside the ST snippet.
A positive ST value indicates ST segment elevation; a negative value indicates depression.
ST numerics are displayed in the order in which you select ST leads for analysis. If there is additional
space in the field assigned to ST numerics, the monitor will display extra numerics in the order in
which they appear in the list in Setup ST Leads, in the Setup ST Analysis menu. Any ST leads
switched on for analysis that do not fit in the assigned numerics field are shown in succession in place
of the last ST numeric.
ST Index
The ST index numeric (STindx) is the sum of the absolute values for the ST leads V2, V5, aVF.
Because it is based on absolute values, it is always a positive number. If you haven't selected one of the
leads V2, V5, and aVF for ST analysis, the ST index numeric will display a question mark "?".
To switch the ST index numeric on or off for display, in the Setup ST Analysis menu, select ST-Index
to toggle between On and Off.
ST Snippets
ST snippets show a one second wave segment for each measured ST lead. The most recent snippet is
drawn in the same color as the ECG wave, usually green, superimposed over the stored baseline
snippet, drawn in a different color. The comparison shows any deviation in the measurement since the
baseline snippet was stored, for example as a result of a procedure carried out on the patient.The
information is updated once per minute.
If you do not see ST snippets on the Screen, select the Screen name in the Monitor Info Line and
select a Screen configured to show snippets from the pop-up list of available Screens.
ST Baseline Window
The ST Baseline Window shows an ST snippet drawn on a grid. The current ST numeric and the ST
numeric stored with the baseline are shown, as well as the difference between these two numerics.
A "?" in front of the difference numeric indicates that the ST measurement points were adjusted since
the baseline snippet was stored.
The Baseline Window opens with the ST pop-up keys Update Baseline, Record ST, Change ST Lead,
Adjust ST Points, ST Map and arrow keys for scrolling through the available leads.
To view the ST Baseline window, select any snippet on the Screen.
1ST numerics
2Current HR alarm limits
3Current heart rate
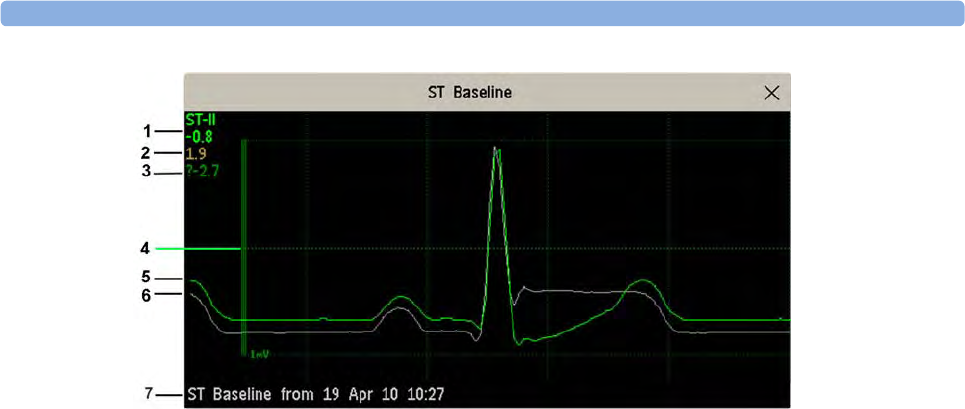
5 ECG, Arrhythmia, ST and QT Monitoring
142
1ST label and numeric
2Baseline ST numeric
3Difference between current values and baseline values
41 mV calibration bar
5Current snippet
6ST baseline
7Timestamp of most recently stored baseline snippet
Updating ST Baseline Snippets
ST analysis requires valid samples to measure and store a snippet. ST Snippets and ST values are
updated every minute. If there is artifact in the signal, it may take longer for an ST snippet and an ST
value to appear.
The first baseline is stored automatically after ST monitoring is started, or when a new patient is
admitted. To update ST baselines,
1Select an ST snippet to open the ST Baseline window.
2In the ST Baseline window, select Update Baseline to store all current snippets as baselines. This
deletes all previously-stored baselines.
An ST baseline copy is also stored in the MMS, for transport purposes.
Recording ST Segments
To record all currently available ST snippets and baselines, in the ST Baseline window, select the pop-
up key Record ST.
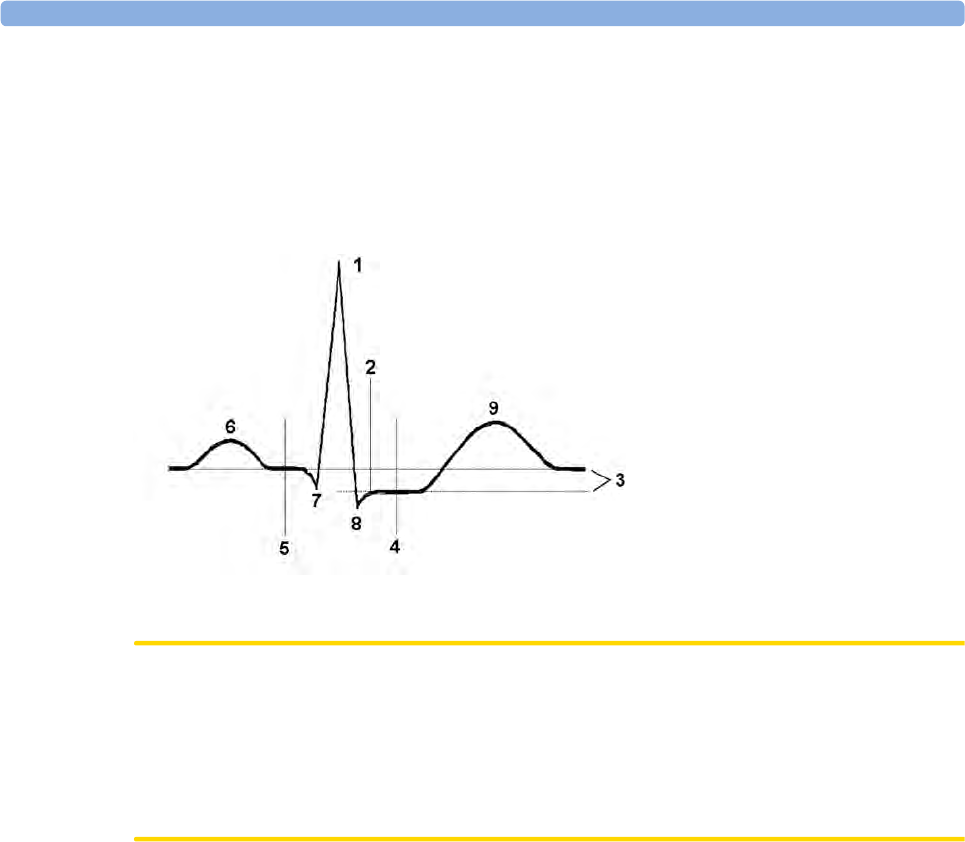
5 ECG, Arrhythmia, ST and QT Monitoring
143
About the ST Measurement Points
The ST value for each beat complex is the vertical difference between the ISO point and the ST point,
as shown in the diagram below. The isoelectric (ISO) point provides the baseline, the ST point is at the
midpoint of the ST segment. The J point is where the QRS complex changes its slope; as it is a fixed
distance away from the ST point, it can be useful to help you position the ST point correctly.
CAUTION
The ST measurement points need to be adjusted when you start monitoring, and if the patient's heart
rate or ECG morphology changes significantly, as this may affect the size of the QT interval and thus
the placement of the ST point. Artifactual ST segment depression or elevation may occur if the
isoelectric point or the ST point is incorrectly set.
Always ensure that ST measurement points are appropriate for your patient.
Adjusting ST Measurement Points
Depending on your monitor's configuration, the ST point can be positioned either
• relative to the J-point.
In the Adjust ST Points window, the pop-up keys ISO Point, J Point and ST Point are visible and
can be adjusted.
or
• directly by selecting a numeric value for the ST point.
In the Adjust ST Points window, you can adjust the ISO and ST point.
The ST Uses setting can only be changed in Configuration Mode.
To adjust the ST measurement points,
1In the Setup ST Analysis menu, select Adjust ST Points to open the Adjust ST Points window.
Alternatively, you can use the Adjust ST Points pop-up key in the ST Baseline window.
2Select a suitable ECG lead for ST measurement, with a visible J-point and a visible P wave. Use the
up and down arrow keys to scroll through the ST snippets for the other ECG leads.
1R-wave peak at 0 msec
2J point, for example, 48 msec
3Difference = ST value
4ST measurement point, for
example, J + 60 msec
5Isoelectric point set to -80 msec
6P
7Q
8S
9T
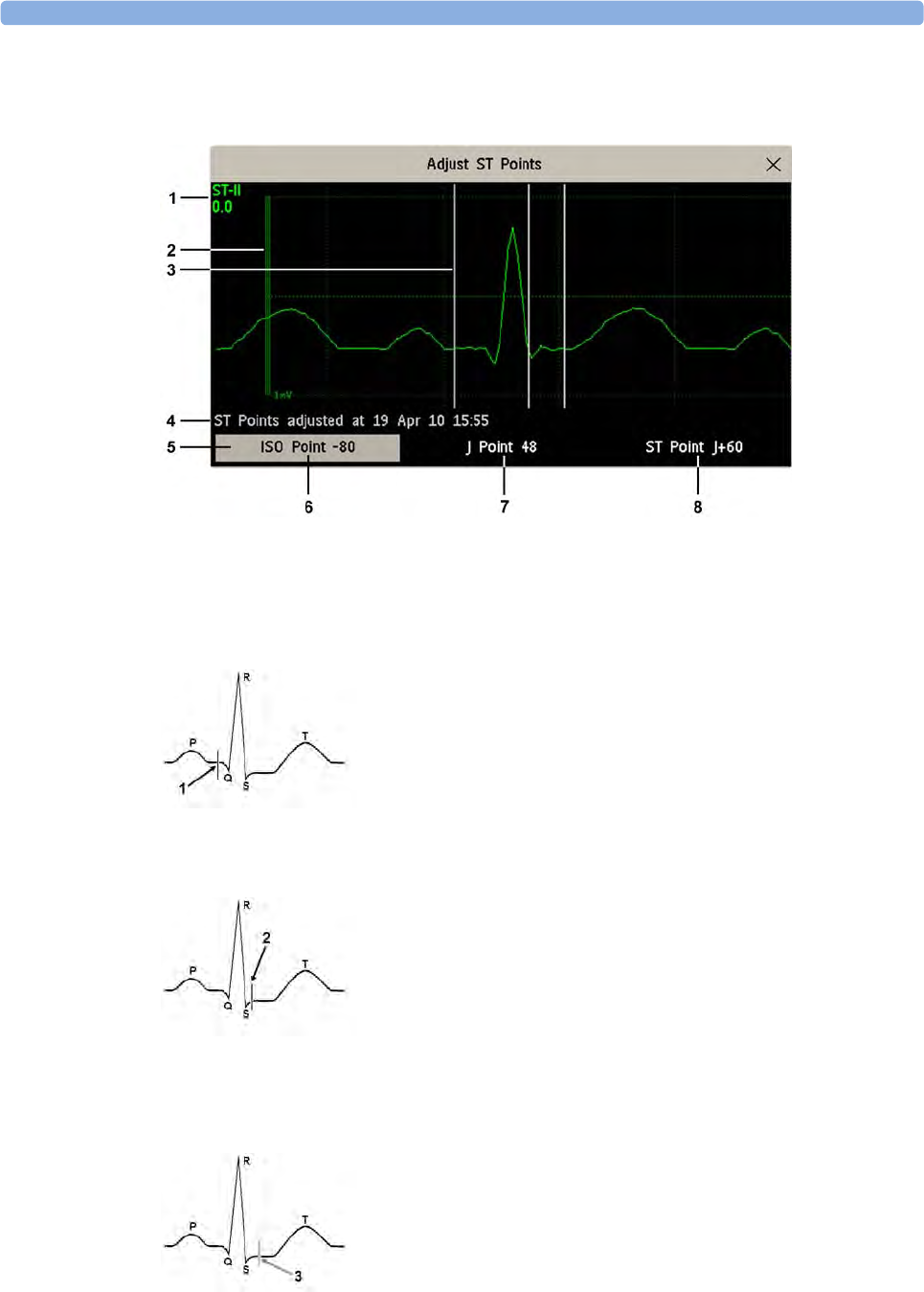
5 ECG, Arrhythmia, ST and QT Monitoring
144
3Use the Select Point pop-up key to scroll through the points and activate the point you need to
adjust, then use the left and right arrow keys to move the measurement point. Each point is
highlighted while active.
1 ST label and the ST numeric that would apply using the current points
2 1mV calibration bar
3 Cursors for adjusting ST points
4 Timestamp of most recent ST point adjustment
5 Highlighted ST point
The ISO-point cursor (1) positions the isoelectric point relative to the R-wave peak. The relation is
shown beside the ISO-point in milliseconds. Position the ISO-point in the middle of the flattest
part of the baseline (between the P and Q waves or in front of the P wave).
The J-point cursor (2) positions the J-point relative to the R-wave peak. It helps you to correctly
position the ST-point. Position the J-point at the end of the QRS complex and the beginning of
the ST segment.
The J-point cursor is not available if your monitor is configured to let you set the ST point directly.

5 ECG, Arrhythmia, ST and QT Monitoring
145
To position the ST-point (3) relative to the J-point:
select either J+60 or J+80. Select J Point and use the arrow keys to move the J-Point and position
the ST-point at the midpoint of the ST segment.
To position the ST-point directly:
select ST Point and use the left and right arrow keys to position the ST point at the midpoint of the
ST segment.
4Select the Apply Changes pop-up key to activate the new ST measurement points and recalculate
all ST values.
The most recent ST Points adjustment time is displayed in the Adjust ST Points window. This
information is cleared when a patient is discharged or when a new Profile is loaded into the
monitor.
5To update the ST snippet shown in the Adjust ST Points window, select the Update pop-up key.
ST Alarms
ST alarms are yellow alarms. Each ST lead has its own alarm limit. ST alarms are triggered when an ST
value exceeds its alarm limit for more than one minute. Switching ST alarms off switches off alarms for
all ST leads.
If more than one ST measurement is in alarm, the monitor only displays the alarm message of the ST
lead which is currently furthest from its set alarm limits.
Single- or Multi-lead ST Alarming
Be aware that if multi-lead ST alarming is switched on, only alarms involving more than one ST lead
will be announced.
To choose individual or multi-lead ST alarming,
•In the Setup ST Analysis menu, select ST Alarm Mode and select either Single ST or Multi ST.
Changing ST Alarm Limits
The monitor can detect alarms on each ST lead separately, so you can set high and low ST alarm limits
individually for each ST lead. You can also set separate alarm limits for single-lead and multi-lead ST
monitoring. Set the high and low alarm limits based on your assessment of the patient's clinical
condition, unit protocols, physician orders or medication specified limits. A good guideline is + 1.0
mm or - 1.0 mm from the patients's ST, or follow your hospital protocol.
1In the Setup ST Analysis menu, select ST Alarm Mode and select Single ST or Multi ST.
2Select the alarm to be adjusted.
3Select the appropriate setting.

5 ECG, Arrhythmia, ST and QT Monitoring
146
Viewing ST Maps
The monitor can derive a multi-axis portrait (map) from the ST analysis to help you detect changes in
ST values. It displays two planes obtained from a multilead ECG in a multi-axis diagram, where each
axis represents a lead. The ST value at the J point is given. The position of the axes within the diagram
correspond to the placement of the ECG leads. Each ST value is assigned to either a limb lead, or to a
chest lead. Every axis shows the polarity of the lead it represents. By joining adjacent ST values, the
monitor obtains the ST map. The contour line, and the map shading, is shown in the same color as the
ECG parameter.
Current View
In current view, the monitor displays an ST map that corresponds to the current ST values. Three or
more leads per plane are necessary to display a map.
The left of the following diagram shows leads I, II, III, aVR, aVL, and aVF on the limb leads. On the
right, the V-leads (V1, V2, V3, V4, V5, and V6) are on the chest leads.
1Alarm status indicator
2EASI Limb Leads
3EASI Chest Leads
4ST index (for EASI)
5ST label, value and polarity of corresponding lead
6ST map
If an ST lead is switched off, its axis is not shown in the map.
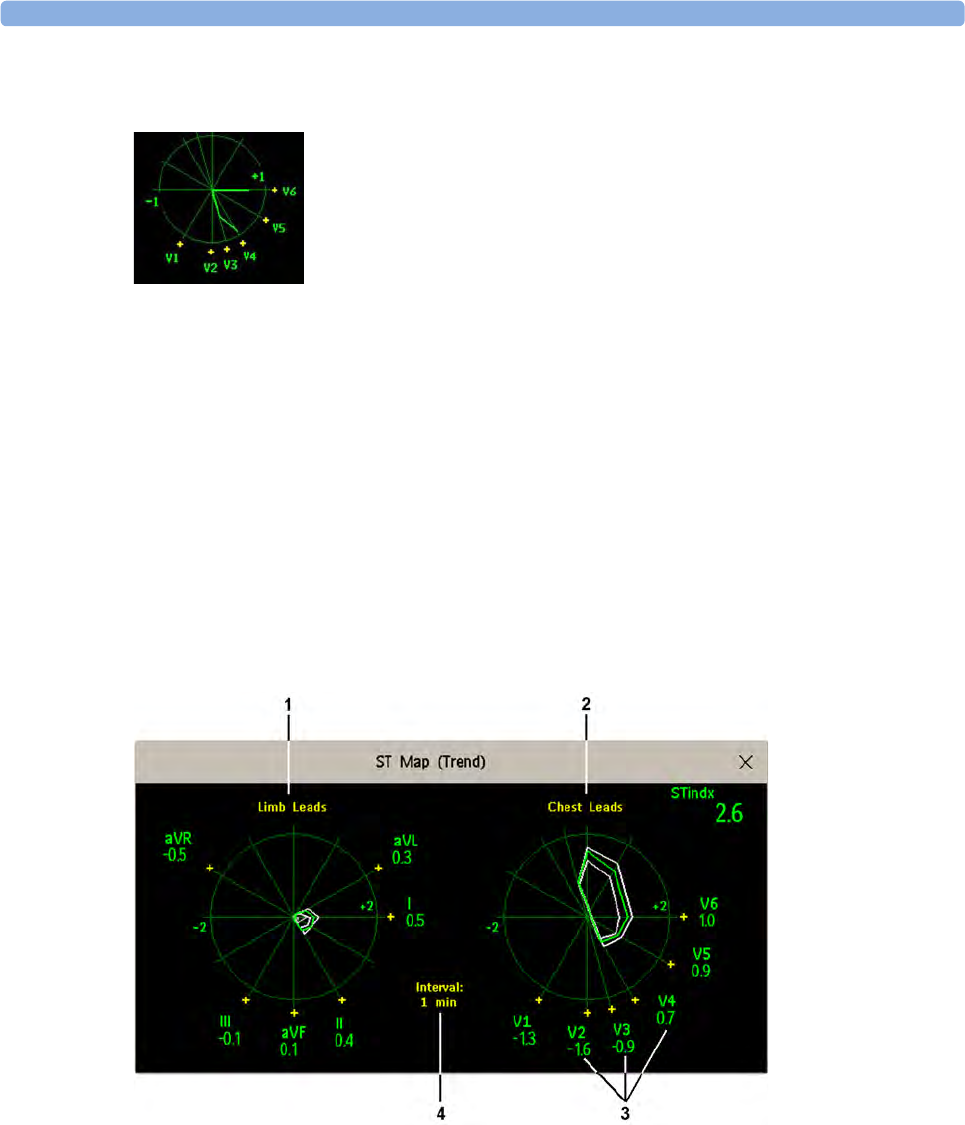
5 ECG, Arrhythmia, ST and QT Monitoring
147
If a lead is in INOP (the value is being measured but is invalid or unavailable because, for example, the
corresponding ECG electrode is off), the area formed by the remaining ST leads is left open.
If there is insufficient information (for example, there are less than three chest leads) for a second ST
map to be displayed, the currently available ST values are displayed in place of the second ST map.
Trend View
In trend view, you can see up to four trended ST maps, and the current ST map, simultaneously. You
can configure the time interval between trended samples. The most recent map is shown in the same
color as the parameter itself. Past values change from white through dark gray. In the diagram below,
the time interval between trends is 12 seconds. The first trended sample is white and is 12 seconds old.
The second trended sample corresponds to the ST values 24 seconds ago and so forth. The ST values
on the diagrams show the current ST values.
If a lead is turned off, its axis is no longer shown. This has no impact on the presentation of trended
values that were recorded while the lead was still on. In the diagram below, lead V4 was switched off
20 seconds ago. The current ST values and the first trended value reflect this change in the lead setup.
All other maps are displayed the way in which they were recorded.
1Limb Leads
2Chest Leads
3current ST values
4trending interval
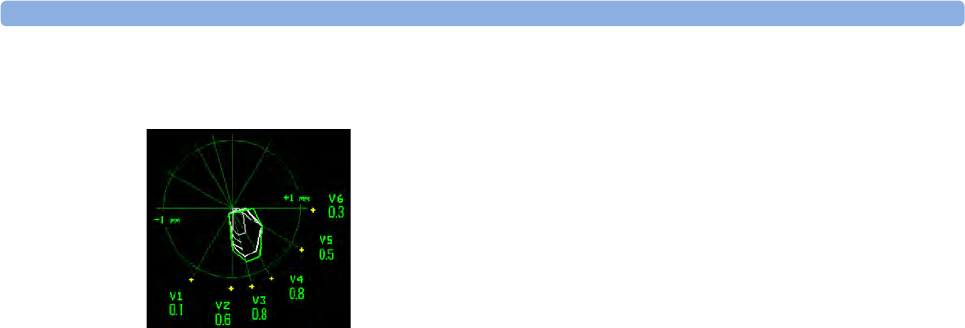
5 ECG, Arrhythmia, ST and QT Monitoring
148
Viewing an ST Map
To display an ST map,
•In the Main Setup menu, select ST Map.
Working in the ST Map Task Window
You may need to activate the ST map task window to see all the data, and to access the pop-up keys.
Select the map view on screen to activate its task window. Once you activate it, you can perform the
tasks detailed here.
Switching Between ST Map Views
To switch between views,
•Select
Current View or Trend View to toggle between views.
If your trend view is empty, you need to adjust the priority of this measurement in the trending priority
list. See “Trend Priority” on page 276.
Displaying an ST Reference Baseline
You can display an ST reference baseline for the current view, or for the trended view. The baseline is
shown in yellow. However, if the ECG color is yellow, the baseline is shown in green. Use this baseline
to detect ST changes. The baseline is derived automatically whenever the monitor relearns arrhythmia
and also on user request.
Select Show Baseline/Hide Baseline to toggle between baseline display on and off.
Updating an ST Map Reference Baseline
To update the baseline,
•In the Setup ST Analysis menu, select ST Baseline then select Update Baseline.
Changing the Scale of the ST Map
To change scale,
•Select
Size Up or Size Down to alter the size at which monitor displays the map.
In this diagram, V4 was either temporarily switched off, or in INOP,
for around 30 seconds. No data was recorded. Consequently, the
affected maps are not closed.
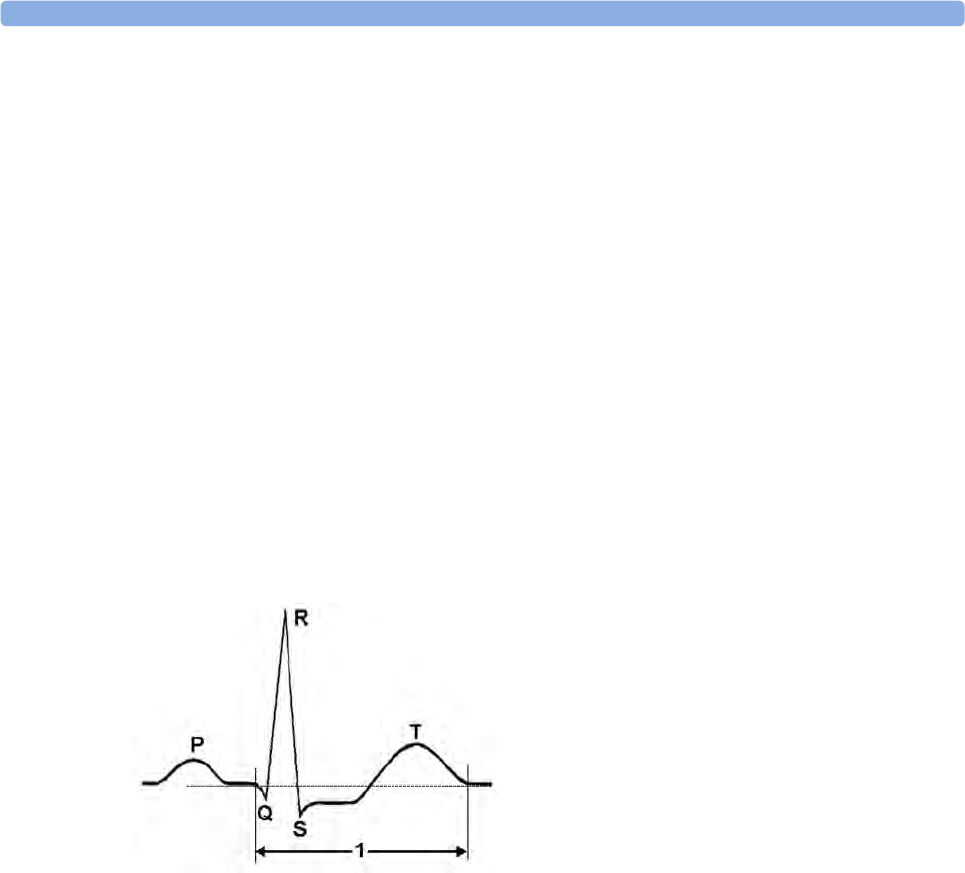
5 ECG, Arrhythmia, ST and QT Monitoring
149
Changing the Trending Interval
To determine how frequently the monitor displays a trended sample,
1In Trend view, select Select Interval.
2Select the required interval from the menu. The interval ranges between 12 seconds to 30 minutes.
Printing an ST Map Report
To print the most recently viewed (current or trend) window,
1Select Main Setup then select Reports.
2Select ST Map.
3Press Print.
About QT/QTc Interval Monitoring
The QT interval is defined as the time between the beginning of the Q-wave and the end of the T-
wave. It measures the total duration of the depolarization (QRS duration) and repolarization (ST-T)
phases of the ventricular action potential. QT interval monitoring can assist in the detection of
prolonged QT interval syndrome.
The QT interval (1) has an inverse relationship to heart rate. Faster heart rates shorten the QT interval
and slower heart rates prolong the QT interval. Therefore there are several formulas used to correct
the QT interval for heart rate. The heart rate corrected QT interval is abbreviated as QTc. The monitor
uses as a default the Bazett correction formula and the alternative Fridericia formula can be selected in
Configuration Mode.
For QT interval monitoring to be effective, basic or enhanced arrhythmia monitoring should be turned
on.
QT Measurement Algorithm
The QT values are updated every five minutes except in the initial phase (first five minutes) where they
are updated once per minute. Normal or atrial paced beats and beats with a similar morphology are
averaged to form a representative waveform for further processing. Normal beats followed by a
premature QRS will be excluded from the measurements to prevent the premature beat from
obscuring the end of the T-wave. If the algorithm cannot form a representative waveform, for example
because the morphology of the beats is too varied, a CANNOT ANALYZE QT INOP will be generated
after 10 minutes. This is also the case if normal beats have been falsely labeled so that the algorithm
does not have enough valid beats to make QT measurements. No QT value is calculated if the QT-HR
is >150 bpm (Adult) or >180 bpm (Pedi/Neo).
5 ECG, Arrhythmia, ST and QT Monitoring
150
Because of the different algorithm approaches, a QT/QTc measurement from a diagnostic 12-lead
program may differ from the realtime measurement on the monitor.
Where Can I Find More Information?
See the Application Note on QT/QTc Interval Monitoring and the QT Interval Monitoring Quick
Guide supplied on your documentation DVD for detailed information on the QT algorithm and
performance.
Indications For Use Of QT Interval Monitoring
Of special concern for QT monitoring is the administration of QT prolonging drugs to patients
identified with risk factors for Torsade de Pointe. Females, older patients and patients with
bradycardia, impaired left ventricular function (ischemia, left ventricular hypertrophy), hypokalemia
and hypomagnesemia are in this increased risk category.
Limitations For Use Of QT Interval Monitoring
Some conditions may make it difficult to achieve reliable QT monitoring, for example:
• the T-wave is very flat
• T-waves are not well defined due to atrial flutter or atrial fibrillation
• the end of the T-wave is difficult to define because of the presence of U-waves
• a high heart rate causes the P-wave to encroach on the end of the previous T-wave
• noise or high QRS morphology variation
For these cases you should select a lead with a good T-wave amplitude and no visible flutter activity,
and without a predominant U-wave or P-wave.
Some conditions such as left or right bundle branch block or hypertrophy can lead to a widened QRS
complex. If a long QTc is observed you should verify it to ensure that it is not caused by QRS
widening.
Because normal beats followed by ventricular beats are not included in the analysis, no QT
measurement will be generated in the presence of a bigeminy rhythm.
If the heart rate is extremely high (over 150 bpm for adults and over 180 bpm for pediatrics and
neonates) QT will not be measured.
When the heart rate changes, it can take several minutes for the QT interval to stabilize. For reliable
QTc calculation it is important to avoid a region where the heart rate is changing.
WARNING
QT/QTc measurements should always be verified by a qualified clinician.
Selecting The QT Leads
For QT Monitoring you can select one of the following three modes:
• All Leads mode - all available leads (I, II, III, V, MCL, V1 - V6) are used to produce a global QT
measurement. For EASI lead placement, directly acquired AI, AS and ES leads are used.
• Primary-Lead mode - the primary lead will be used for QT measurement. If the original primary
lead becomes unavailable or is changed, QT measurement will continue with the new primary lead.
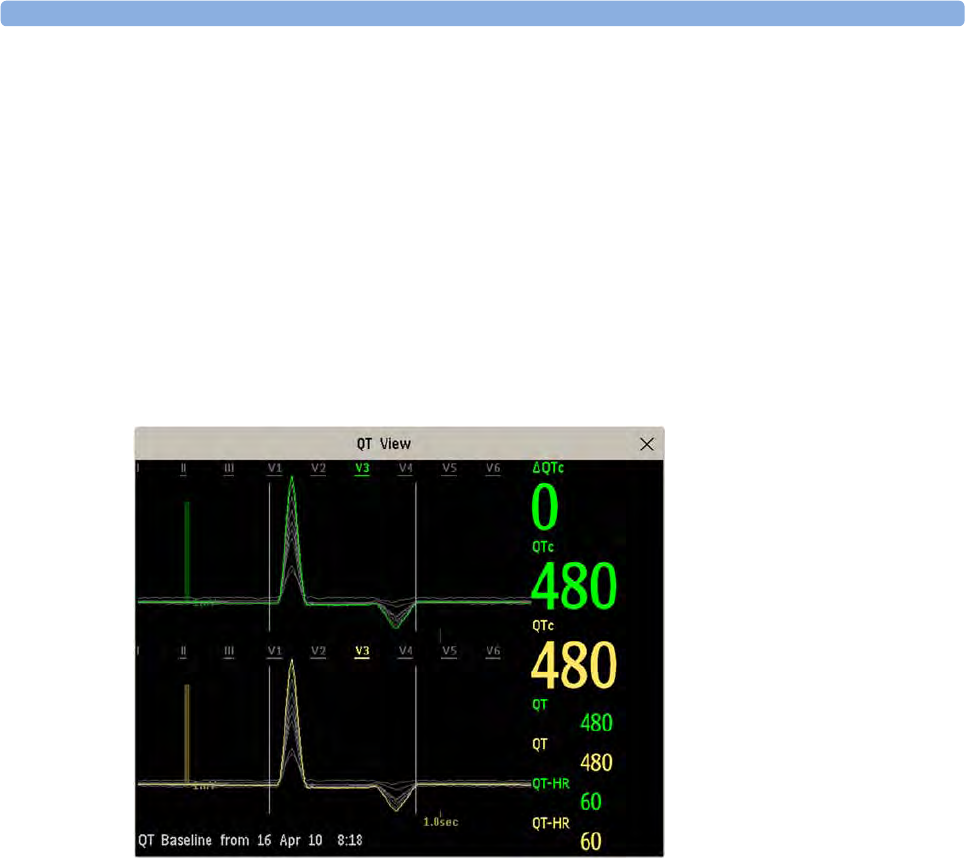
5 ECG, Arrhythmia, ST and QT Monitoring
151
• Single-Lead mode - a single lead selected from all available leads (except the augmented leads) will
be used for QT measurement. QT measurement will stop if the selected lead becomes unavailable.
To select the mode,
1Select the QT numeric to enter the Setup QT Analysis window.
2Select QT Lead and select All, Primary Lead or one of the available single leads.
When using the All Leads mode, make sure when you compare QT values that they are based on the
same set of leads.
Changing the lead(s) used for QT measurements will not cause the baseline to be reset.
QT View
In the QT View window you can verify that the QT algorithm detects correct Q and T points.
The current waves are shown in the upper half of the window and the baseline waves in a different
color below. The Q and T points are marked with a vertical line. By selecting one of the lead labels at
the top of the window you can highlight the corresponding wave; the other waves are shown in gray.
The underlined lead labels are the leads used for the QT calculation. By selecting the numeric area you
can highlight all underlined leads.
Changing The View To A Single Wave Set
To view one set of waves in a larger scale, you can cycle through the different views,
1Select Current view to see the set of current waves.
2Select Baseline view to see the set of baseline waves.
3Select Split view to return to the combined view with current and baseline waves.
Setting The QT Baseline
In order to quantify changes in the QTc value, you can set a QTc baseline. For example to assess the
effect of medication on the QT interval you can set the current value as the baseline before you begin
medication. This baseline will then be used to calculate the ΔQTc value.
5 ECG, Arrhythmia, ST and QT Monitoring
152
To set the baseline,
•Select
Set Baseline and set the value.
If no baseline has been set for this patient, the first five minute value after the start of monitoring is
automatically set as baseline. If you set a new baseline the previous baseline is discarded. As the ΔQTc
alarm is based on the difference between the baseline and the current value, setting an inappropriate
new baseline may prevent a ΔQTc alarm from being generated. Discharging a patient clears the
baseline.
Printing The QT Waves
To start a printout,
•Select
Print QT.
Recording The QT Waves
To start a recording,
•Select
Record QT.
QT Alarms
There are two QT alarms, QTc high limit alarm and ΔQTc high alarm. The QTc high limit alarm is
generated when the QTc value exceeds the set limit for more than 5 minutes. The ΔQTc alarm is
generated when the difference between the current value and the baseline value exceeds the set limit
for more than 5 minutes.
The CANNOT ANALYZE QT INOP and the -?- will be displayed when no QT measurement could be
calculated for 10 minutes. Up to this time the previous valid value will be displayed. The following
additional messages on the cause of the invalid measurements may also be displayed.
Additional Message Cause of Invalid QT Measurement
QT Startup QT monitoring was just turned on or has been reset
Asystole or Leads Off 1Not all specified leads needed to perform QT analysis are
available, or
2Asystole condition is detected
Insufficient Valid Leads Not enough valid QRS complexes to generate a QT measurement
Invalid Rhythm for QTc Not enough valid RR intervals to generate QT-HR, the averaged HR
used for QTc calculation
High QT-HR QT-HR exceeds the specified upper limit of 150 bpm (for adults) or
180 bpm (for neonates and pediatrics)
Small R Wave R-wave of the signal is too small
Small T Wave T-wave of the signal is too small
5 ECG, Arrhythmia, ST and QT Monitoring
153
Switching Individual QTc Alarms On and Off
Each QTc alarm can be switched off individually.
To switch an alarm on or off, in the Setup QT Analysis menu, select QTc High Alarm or ΔQTc High
Alarm to toggle between On and Off.
Changing QTc Alarm Limits
Set the high alarm limits based on your assessment of the patient's clinical condition, unit protocols,
physician orders or medication specified limits.
1In the Setup QT Analysis menu, select QTc High Limit.
2Select the appropriate setting.
3Select ΔQTc High Limit.
4Select the appropriate setting.
Switching QT Monitoring On and Off
To switch all QT monitoring on or off, in the Setup QT Analysis menu, select QT Analysis to switch
between On and Off.
End of T not Detected End of the T-Wave cannot be accurately detected
QT out of Range QT measurement is outside the specified range of valid QT values
(200-800 msec)
QTc out of Range QTc measurement is outside the specified range of valid QTc values
(200-800 msec)
QTc Erratic QTc measurements are not stable
Additional Message Cause of Invalid QT Measurement

5 ECG, Arrhythmia, ST and QT Monitoring
154

6
155
6Monitoring Pulse Rate
The pulse numeric counts the arterial pulsations that result from the mechanical activity of the heart in
beats per minute (bpm). You can display a pulse from any measured SpO2 signal (pleth wave), or any
arterial pressure (P, ABP, ART, Ao, PAP, UAP, FAP, BAP: see the Monitoring Invasive Pressure
chapter for an explanation of the pressure labels). The displayed pulse numeric is labeled and color-
coded to match its source wave. If the pulse numeric is not displayed, see the Setup Pulse menu to
check whether it is switched on.
Entering the Setup Pulse Menu
If a pulse numeric is displayed on the screen, select it to enter the setup menu for that pulse source. If
no pulse numeric is visible, in the Setup SpO₂ menu or the setup menu from an arterial pressure, select
pulse with the correct source, e.g. Pulse (HR).
System Pulse Source
The currently selected system pulse source is shown in the setup menus of the pulse source
measurements. The pulse rate chosen as system pulse:
• is monitored as system pulse and generates alarms when you select pulse as the active alarm source
• is sent via the network to the Information Center, if available
• is trended in the HighRes Trends and stored in the monitor's databases.
To define which pulse rate is used as system pulse,
1In the Setup Pulse menu, select System Pulse.
2Select one of the SpO2 or arterial pressure labels from the pop-up list, or select Auto.
If you select Auto, the monitor automatically chooses a pulse rate to be used as system pulse. It
looks through the list from top to bottom and activates the first pulse rate that is switched on and
available.
If your selected pulse source measurement becomes unavailable or is switched off, the monitor will use
the next measurement from the list as system pulse until the selected pulse source measurement
becomes available again.

6 Monitoring Pulse Rate
156
Switching Pulse On and Off
To switch a particular pulse numeric on or off, enter the Setup Pulse menu via the measurement setup
menu or wave menu of the pulse source. For example, to switch an SpO2 pulse numeric on or off,
1Enter the Setup Pulse menu by selecting the Pulse numeric or by selecting Pulse in the Setup
SpO₂ menu.
2In the Setup Pulse menu, select the correct pulse label, e.g. Pulse (SpO₂), to toggle between On
and Off.
Using Pulse Alarms
You can change pulse rate alarm limits in the ECG/Pulse Alarms menu which can be accessed from
the Setup Pulse menu or the Setup ECG menu by selecting Alarm Source. Changing the alarm limits
for a specific Pulse numeric changes the alarm limits for all pulse rate alarms and heart rate alarms.
Pulse alarms are only generated when the active alarm source is set to Pulse, a pulse source is set as
system pulse and pulse alarms are switched on.
Selecting the Active Alarm Source: ECG or Pulse?
In most cases the HR and Pulse numerics are identical. In order to avoid simultaneous alarms on HR
and Pulse, the monitor uses either ECG or Pulse as its active alarm source. To change the alarm
source, select Alarm Source in the ECG/Pulse Alarms menu, then select
•ECG/Arrhythm: if you want the HR to be the alarm source for HR/Pulse.
•Pulse: If you select Pulse as the active alarm source, the monitor will prompt you to confirm your
choice. Be aware that if you select Pulse as the alarm source, all arrhythmia and ECG HR alarms
are switched off.
•Auto: If the alarm source is set to Auto, the monitor will use the heart rate from the ECG
measurement as the alarm source whenever the ECG measurement is switched on and at least one
ECG lead can be measured without an INOP condition.
The monitor will automatically switch to Pulse as the alarm source if:
– a valid ECG lead can no longer be measured
and
– a Pulse source is switched on and available,
The monitor then uses the pulse rate from the measurement currently active as system pulse.
While Pulse is the alarm source, all arrhythmia and ECG HR alarms are switched off. If an ECG
lead becomes available again, the monitor automatically uses HR as alarm source.
Note:
If ECG is switched off, the monitor will always change to Pulse as alarm source, if a Pulse is available.
One exception to this rule can arise when you have a telemetry device paired with your monitor. The
monitor ECG is then deactivated but the monitor may be configured to allow only ECG as the active
alarm source. In this case the monitor will not switch to Pulse as alarm source and Pulse will not be
available as a selection in the ECG/Pulse Alarms menu.
6 Monitoring Pulse Rate
157
WARNING
Selecting Pulse as the active alarm source for HR/Pulse switches off the arrhythmia alarms listed in the
section “ECG and Arrhythmia Alarm Overview” on page 126, including Asystole, Vfib and Vtach
alarms, and the heart rate alarms. This is indicated by the message ECG/ARRH ALARM OFF (unless this
has been configured off for your monitor), and the crossed-out alarm symbol beside the ECG heart
rate numeric. The message ECG/ARRH ALARM OFF can be configured off, or to switch to a yellow
(medium severity) INOP after a fixed number of hours.
High and low pulse rate and extreme bradycardia and extreme tachycardia alarms from pulse are active.
Alarm Source Selection Disabled
If you cannot change the alarm source, selection of the alarm source may be disabled. If you try to
change the source, the monitor displays the message To activate enter Config and enable Alarm
Source Selection. This setting can only be changed in Configuration Mode.
Changing HR/Pulse Alarm Limits
As Pulse and HR share the same high and low alarm limits, if you change the alarm limit in the Setup
Pulse menu, the high or low alarm limits for HR in the Setup ECG menu change automatically, and
vice versa. The only exceptions are caused by a low limit clamp for each measurement: the lowest value
for Pulse when derived from SpO2 is 30 bpm; from HR 15 bpm, and from Pressure 25 bpm.
Extreme Alarm Limits for Heart Rate
The extreme rate alarms, *** EXTREME TACHY and *** EXTREME BRADY, generated by the active
alarm source, either HR or Pulse, are set in Configuration Mode by adding a set value to the high and
low alarm limits. You need to know what value has been configured for your monitor. Changing the
high and low alarm limits automatically changes the extreme alarm limits within the allowed range.
• To see the values added to the high and low limit alarms to create the extreme rate alarms for your
monitor, in the Setup ECG menu, see the menu items Δ ExtrTachy and Δ ExtrBrady.
QRS Tone
The active alarm source is also used as a source for the QRS tone. You can change the tone volume in
the Setup SpO₂ and Setup ECG menus and the QRS tone modulation in the Setup SpO₂ menu.
WARNING
The audible QRS tone might be influenced by external interference and is not intended to be used as a
substitute for ECG based arrhythmia analysis.
If arrhythmia detection is needed, do not rely on the audible QRS tone.

6 Monitoring Pulse Rate
158

7
159
7Monitoring Respiration Rate
(Resp)
For the respiratory measurement (Resp), the monitor measures the thoracic impedance between two
ECG electrodes on the patient's chest. Changes in the impedance due to thoracic movement produce
the Resp waveform on the monitor screen. The monitor counts the waveform cycles to calculate the
respiration rate (RR).
Lead Placement for Monitoring Resp
Correct patient skin preparation techniques for electrode placement are important for Resp
measurement: you will find this information in the chapter on ECG.
The Resp measurement uses the standard ECG cable sets and lead placements. You can use any of the
different types of ECG cable sets - 3-lead, 5-lead, 6-lead or 10-lead, using either standard or EASI™
placement - to measure Resp, as long as you use ICU ECG cables.
The Resp signal is always measured between two of the ECG electrodes. If you are using standard
ECG electrode placement, Resp is measured between the RA and LL electrodes. If you are using
EASI™ ECG electrode placement, Resp is measured between the I and A electrodes.
Optimizing Lead Placement for Resp
If you want to measure Resp and you are already measuring ECG, you may need to optimize
placement of the two electrodes between which Resp will be measured for some patients.
Repositioning ECG electrodes from standard positions, especially when you are using EASI™ ECG
electrode placement, results in changes in the ECG waveform and may influence ST and arrhythmia
interpretation.
Cardiac Overlay
Cardiac activity that affects the Resp waveform is called cardiac overlay. It happens when the Resp
electrodes pick up impedance changes caused by the rhythmic blood flow. Correct electrode
placement can help to reduce cardiac overlay: avoid the liver area and the ventricles of the heart in the
line between the respiratory electrodes. This is particularly important for neonates.
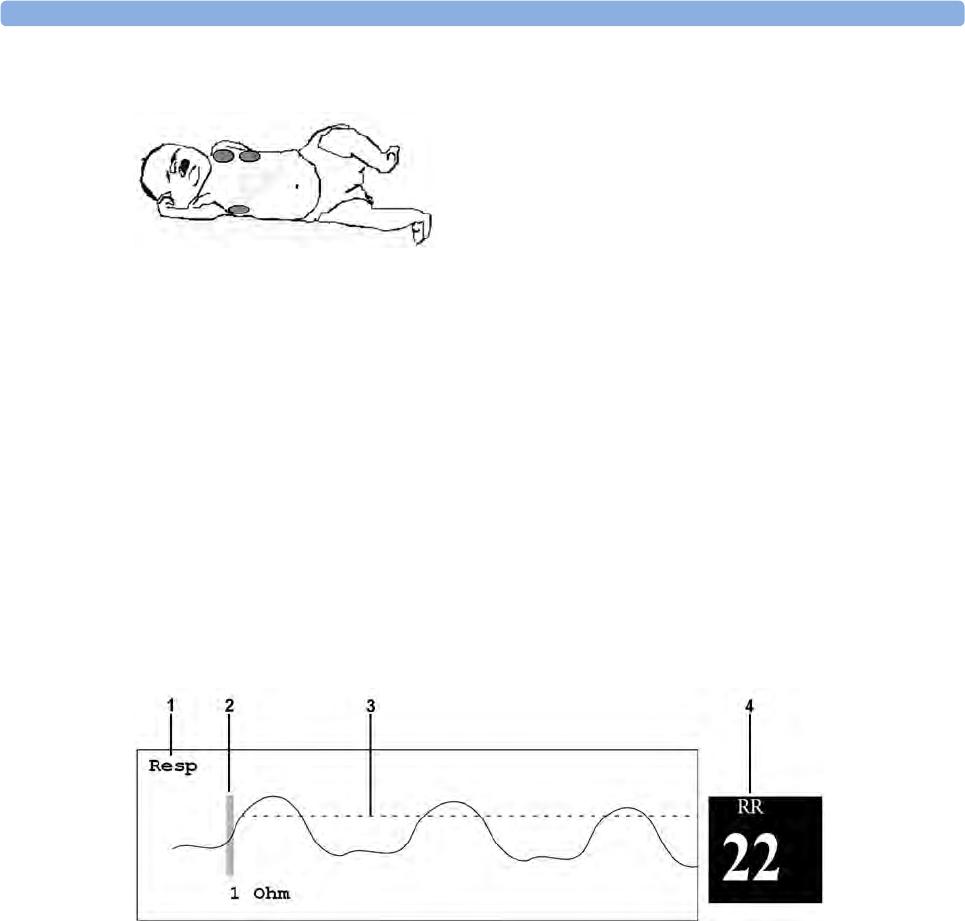
7 Monitoring Respiration Rate (Resp)
160
Lateral Chest Expansion
Some patients, especially neonates, expand their chests laterally. In these cases it is best to place the
two respiratory electrodes in the right midaxillary and left lateral chest areas at the patient's maximum
point of breathing movement to optimize the respiratory wave.
Abdominal Breathing
Some patients with restricted chest movement breathe mainly abdominally. In these cases, you may
need to place the left leg electrode on the left abdomen at the point of maximum abdominal expansion
to optimize the respiratory wave.
Understanding the Resp Display
The Resp measurement is displayed on the monitor as a continuous wave and a numeric respiration
rate. If the detected respiration rate is close to the heart rate, this is indicated by the text HR = RR next
to the respiration wave if you are in manual monitoring mode. Your monitor screen may look slightly
different from the illustration.
1Resp wave label
2One Ohm calibration bar
3Manually-set Resp detection level
4Resp numeric and label
Changing Resp Detection Modes
The Resp detection level can be set either automatically or manually.
• To change the resp detection mode, in the Setup Resp menu, select Detection to toggle between
the settings.
Auto Detection Mode
In Auto Detection Mode, the monitor adjusts the detection level automatically, depending on the wave
height and the presence of cardiac artifact. Note that in Auto Detection Mode,

7 Monitoring Respiration Rate (Resp)
161
• the detection level (a dotted line) is not displayed on the waveform,
• the algorithm expects a heart rate and therefore needs at least 3 electrodes attached to the patient.
If you are monitoring respiration with only two electrodes, the detection algorithm becomes less
sensitive which may result in reduced breath detection performance.
Use Auto Detection Mode for situations where:
• the respiration rate is not close to the heart rate
• breathing is spontaneous, with or without continuous positive airway pressure (CPAP)
• patients are ventilated, except patients with Intermittent Mandatory Ventilation (IMV).
Manual Detection Mode
In Manual Detection Mode you must set the Resp detection level.
•In the Setup Resp menu, select Manual Up or Manual Down. Use the dotted detection level line
in the Resp waveform to determine when the desired level is reached.
Once set, the detection level will not adapt automatically to different respiration depths. It is important
to remember that if the depth of breathing changes, you may need to change the detection level.
Use Manual Detection Mode for situations where:
• the respiration rate and the heart rate are close.
• patients have Intermittent Mandatory Ventilation.
• respiration is weak. Try repositioning the electrodes to improve the signal.
Resp Detection Modes and Cardiac Overlay
In Auto Detection Mode:
If you are monitoring Resp and the ECG is switched off, the monitor cannot compare the ECG and
Resp rates to detect cardiac overlay. The respiration detection level is automatically set higher to
prevent the detection of cardiac overlay as respiration.
In Manual Detection Mode:
Cardiac overlay can in certain situations trigger the respiration counter. This may lead to a false
indication of a high respiration rate or an undetected apnea condition. If you suspect that cardiac
overlay is being registered as breathing activity, raise the detection level above the zone of cardiac
overlay. If the Resp wave is so small that raising the detection level is not possible, you may need to
optimize the electrode placement as described in the section “Lateral Chest Expansion” on page 160.
Changing the Size of the Respiration Wave
WARNING
When monitoring in Manual Detection Mode, make sure to check the respiration detection level after
you have increased or decreased the size of the respiration wave.
•In the Setup Resp menu, select Size Up to increase the size of the wave or Size Down to decrease
it.
7 Monitoring Respiration Rate (Resp)
162
Changing the Speed of the Respiration Wave
Resp waveforms are usually viewed at a slower speed than other waveforms. For this reason, the Resp
measurement has its own speed control and is not affected by the wave speed settings of the other
measurements.
• Select the Resp wave to enter the Resp Wave menu, then select Change Speed. Choose the
required speed from the pop-up list. This defines the speed at which the wave is drawn across the
screen in millimeters per second (mm/s).
Using Resp Alarms
Resp alarms can be switched on and off and the high and low alarm limits can be changed just like
other measurement alarms, as described in the Alarms chapter.
Changing the Apnea Alarm Delay
The apnea alarm is a high priority red alarm used to detect apneas. The apnea alarm delay time defines
the time period between the point where the monitor cannot detect any respiration activity and the
indication of the apnea alarm.
1In the Setup Resp menu, select Apnea Time.
2Select the appropriate setting.
Resp Safety Information
WARNING
Respiration detection level
If you do not set the detection level for the respiration correctly in manual detection mode, it may not
be possible for the monitor to detect apnea. If you set the detection level too low, the monitor is more
likely to detect cardiac activity, and to falsely interpret cardiac activity as respiratory activity in the case
of apnea.
Apnea
The respiration measurement does not recognize obstructive and mixed apneas - it only indicates an
alarm when a pre-adjusted time has elapsed since the last detected breath.
The safety and effectiveness of the respiration measurement method in the detection of apnea,
particularly the apnea of prematurity and apnea of infancy, has not been established.
Interference
If operating under conditions according to the EMC Standard EN 60601-1-2 (Radiated Immunity 3V/
m), field strengths above 1V/m may cause erroneous measurements at various frequencies. Therefore
it is recommended to avoid the use of electrically radiating equipment in close proximity to the
respiration measurement unit.
Resp Accessories
7 Monitoring Respiration Rate (Resp)
163
To monitor respiration, use only the non-OR ECG accessories listed in the Resp section of the
accessories chapter. You cannot measure respiration if you are using an orange OR ECG cable set.
This is because of the higher internal impedance of the OR cable set, required for use if electrosurgery
is being performed.
Rate adaptive pacemakers
Implanted pacemakers which can adapt to the Minute Ventilation rate may occasionally react on the
Impedance measurement used by patient monitors for the determination of the Resp value and
execute pacing with the maximum programmed rate. Switching off the Resp measurement can prevent
this.

7 Monitoring Respiration Rate (Resp)
164
8
165
8Monitoring SpO2
Philips pulse oximetry uses a motion-tolerant signal processing algorithm, based on Fourier artifact
suppression technology (FAST). It provides four measurements:
• Oxygen saturation of arterial blood (SpO2) - percentage of oxygenated hemoglobin in relation to
the sum of oxyhemoglobin and deoxyhemoglobin (functional arterial oxygen saturation).
• Pleth waveform - visual indication of patient's pulse.
• Pulse rate (derived from pleth wave) - detected pulsations per minute.
• Perfusion indicator - numerical value for the pulsatile portion of the measured signal caused by
arterial pulsation.
The monitors are also compatible with SpO2 technologies from other manufacturers. Please refer to
the instructions for use provided with these devices for further information.
SpO2 Sensors
Depending on the purchased SpO2 option, different sensors and adapter cables can be used. The
sensors for the different options are color-coded to match the connectors. See the Accessories chapter
for a compatibility table.
Familiarize yourself with the instructions for use supplied with your sensor before using it. In
particular, check that the sensor being used is appropriate for your patient category and application
site.
CAUTION
Do not use OxiCliq disposable sensors in a high humidity environment, such as in neonatal
incubators or in the presence of fluids, which may contaminate sensor and electrical connections
causing unreliable or intermittent measurements. Do not use disposable sensors when there is a
known allergic reaction to the adhesive.
Always use the MAX-FAST forehead sensor with the foam headband provided by Nellcor.
Applying the Sensor
1Follow the SpO2 sensor's instructions for use, adhering to all warnings and cautions.
2Remove colored nail polish from the application site.
8 Monitoring SpO2
166
3Apply the sensor to the patient. The application site should match the sensor size so that the
sensor can neither fall off, nor apply excessive pressure.
When using the M1195A Infant Finger Sensor, select a finger or toe with a diameter of between 7
and 8 mm (0.27" and 0.31"). When applying a M1193A neonatal sensor do not overtighten the
strap.
4Check that the light emitter and the photodetector are directly opposite each other. All light from
the emitter must pass through the patient's tissue.
WARNING
Proper Sensor Fit: If a sensor is too loose, it might compromise the optical alignment or fall off. If it
is too tight, for example because the application site is too large or becomes too large due to edema,
excessive pressure may be applied. This can result in venous congestion distal from the application site,
leading to interstitial edema, hypoxemia and tissue malnutrition. Skin irritations or lacerations may
occur as a result of the sensor being attached to one location for too long. To avoid skin irritations and
lacerations, periodically inspect the sensor application site and change the application site regularly.
Venous Pulsation: Do not apply sensor too tightly as this results in venous pulsation which may
severely obstruct circulation and lead to inaccurate measurements.
Ambient Temperature: At elevated ambient temperatures be careful with measurement sites that are
not well perfused, because this can cause severe burns after prolonged application. All listed sensors
operate without risk of exceeding 41°C on the skin if the initial skin temperature does not exceed
35°C.
Extremities to Avoid: Avoid placing the sensor on extremities with an arterial catheter, an NBP cuff
or an intravascular venous infusion line.
Connecting SpO2 Cables
Connect the sensor cable to the color-coded socket on the measurement device (MMS or module).
You can connect some Philips sensors directly to the measurement device. For other sensors, use the
corresponding adapter cable.
CAUTION
Extension cables: Do not use more than one extension cable (M1941A). Do not use an extension
cable with Philips reusable sensors or adapter cables with part numbers ending in -L (indicates "long"
cable version).
Electrical Interference: Position the sensor cable and connector away from power cables, to avoid
electrical interference.
Humidity: For neonatal patients, make sure that all sensor connectors and adapter cable connectors
are outside the incubator. The humid atmosphere inside can cause inaccurate measurements.
Measuring SpO2
1Select the correct patient category setting (adult/pediatric and neonatal), as this is used to optimize
the calculation of the SpO2 and pulse numerics.
8 Monitoring SpO2
167
2During measurement, ensure that the application site:
– has a pulsatile flow, ideally with a perfusion indicator value above 1.0.
– has not changed in its thickness (for example, due to edema), causing an improper fit of the
sensor.
WARNING
• For fully conscious pediatric or adult patients, who have a normal function of perfusion and
sensory perception at the measurement site:
To ensure skin quality and correct optical alignment of the sensor, inspect the application site
when the measurement results are suspicious or when the patient complains about pressure at
the application site, but at least every 24 hours. Correct the sensor alignment if necessary.
Move the sensor to another site, if the skin quality changes.
• For all other patients:
Inspect the application site every two to three hours to ensure skin quality and correct optical
alignment. Correct the sensor alignment if necessary. If the skin quality changes, move the
sensor to another site.
Change the application site at least every four hours.
• Injected dyes such as methylene blue, or intravascular dyshemoglobins such as methemoglobin
and carboxyhemoglobin may lead to inaccurate measurements.
• Inaccurate measurements may result when the application site for the sensor is deeply pigmented
or deeply colored, for example, with nail polish, artificial nails, dye or pigmented cream.
• Interference can be caused by:
– High levels of ambient light (including IR warmers) or strobe lights or flashing lights (such as
fire alarm lamps). (Hint: cover application site with opaque material.)
– Another SpO2 sensor in close proximity (e.g. when more than one SpO2 measurement is
performed on the same patient). Always cover both sensors with opaque material to reduce
cross-interference.
– Electromagnetic interference, especially at perfusion indicator values below 1.0 or signal
quality indicator below medium.
– Excessive patient movement and vibration.
SpO2 Signal Quality Indicator (Fast SpO2 only)
The SpO2 numeric is displayed together with a signal quality indicator (if configured and enough space
is available) which gives an indication of the reliability of the displayed values.
The level to which the triangle is filled shows the quality of the signal; the indicator below shows a
medium signal quality, the signal quality is at a maximum when the triangle is completely filled.
8 Monitoring SpO2
168
Assessing a Suspicious SpO2 Reading
Traditionally, pulse rate from SpO2 was compared with heart rate from ECG to confirm the validity of
the SpO2 reading. With newer algorithms, such as FAST-SpO2, this is no longer a valid criteria because
the correct calculation of SpO2 is not directly linked to the correct detection of each pulse.
When pulse rate is very low, or strong arrhythmia is present, the SpO2 pulse rate may differ from the
heart rate calculated from ECG but this does not indicate an inaccurate SpO2 value.
If you doubt the measured SpO2, use the signal quality indicator (if available) or the pleth wave and
perfusion indicator instead to assess the signal quality.
WARNING
With pulse oximetry, sensor movement, ambient light (especially strobe lights or flashing lights) or
electromagnetic interference can give unexpected intermittent readings when the sensor is not
attached. Especially bandage-type sensor designs are sensitive to minimal sensor movement that might
occur when the sensor is dangling.
Changing the Averaging Time
Depending on the monitor configuration, you may be able to change the averaging time for the SpO2
values.
The averaging time represents the approximate time period used for the calculation. The exact
averaging algorithm depends on the SpO2 technology (option) used and on the signal conditions. The
longer the averaging time, the longer the time needed until the SpO2 value reflects the physiological
event. Fast averaging is useful for situations where an extremely fast measurement is required or few
artifacts are expected. Use slow averaging where you expect the number of artifacts to be relatively
high.
1In the Setup SpO₂ menu, select Average.
2Select the required averaging time from the list.
Understanding SpO2 Alarms
This refers to SpO2 specific alarms. See the Alarms chapter for general alarm information. SpO2 offers
high and low limit alarms, and a high priority desat alarm. You cannot set the low alarm limit below the
desat alarm limit.
CAUTION
If you measure SpO2 on a limb that has an inflated noninvasive blood pressure cuff, a non-pulsatile
SpO2 INOP can occur. If the monitor is configured to suppress this alarm there may be a delay of up
to 60 seconds in indicating a critical status, such as sudden pulse loss or hypoxia.
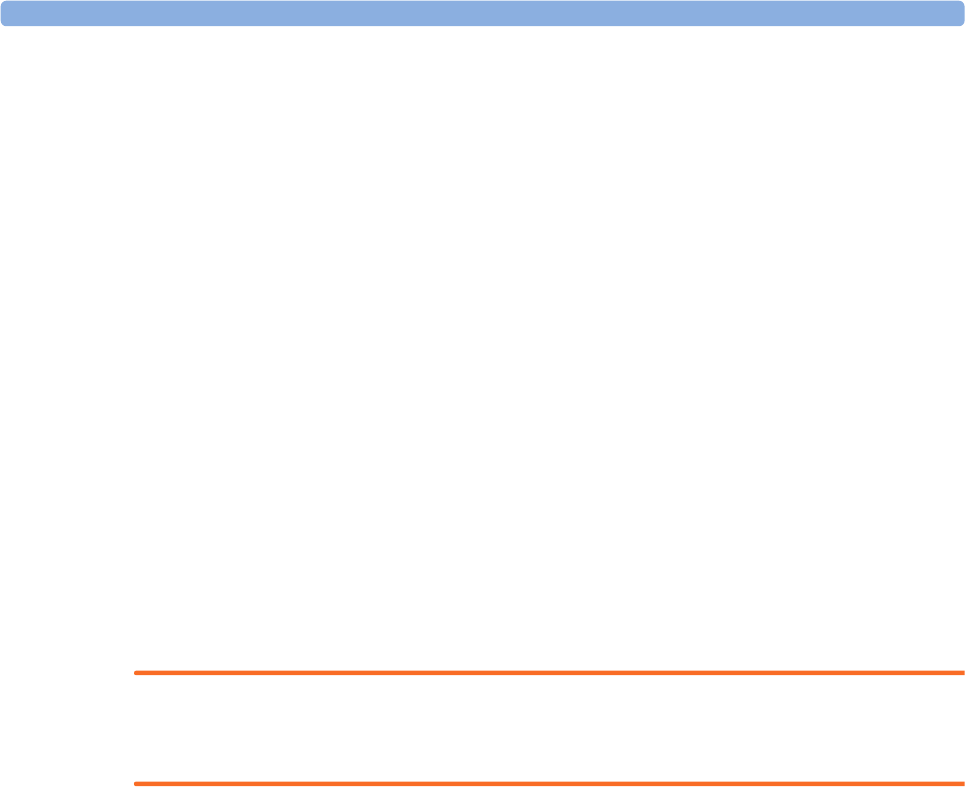
8 Monitoring SpO2
169
Alarm Delays
There is a delay between a physiological event at the measurement site and the corresponding alarm at
the monitor. This delay has two components:
• The general system delay time is the time between the occurrence of the physiological event and
when this event is represented by the displayed numerical values. This delay depends on the
algorithmic processing and the configured averaging time. The longer the averaging time
configured, the longer the time needed until the numerical values reflect the physiological event.
• The time between the displayed numerical values crossing an alarm limit and the alarm indication
on the monitor. This delay is the combination of the configured alarm delay time plus the general
system alarm signal delay time.
The alarm delay time can be configured to a fixed value (between 0 and 30 seconds) or the monitor can
be configured to apply a delay based on an intelligent algorithm. See “About Smart Alarm Delays” on
page 169 for details on how this works.
See “Performance Specifications” on page 399 for delay specifications.
About Smart Alarm Delays
The Smart Alarm Delay functionality is currently not available in the U.S.A. or in clinical environments under FDA control.
The monitor can be configured to apply a delay before announcing SpO2 limit alarms. The delay is
calculated using an intelligent algorithm. This capability can be used to suppress alarms which occur
because a limit is exceeded for a short time or by a small amount.
WARNING
Before using Smart Alarm Delays, make sure that you fully understand how the delay is applied and
what the consequences are.
The following factors are considered when calculating the delay:
• the amount by which a limit is exceeded
• the time it is exceeded for, and hence
•the speed with which the values change when a limit is exceeded
If the measured value rises, or falls, very quickly, an alarm will be announced with only a short delay. If
the value changes slowly, the delay will be longer before an alarm is announced. And if the value
changes slowly and only for a short time, an alarm may not be announced at all. Here are some specific
examples to illustrate this.
Examples
In the examples, the SpO2 low alarm limit is set to 90%, and the Smart Alarm Delay is configured on.
The measured SpO2 signal is represented by the dotted curve. The vertical axis (V) shows the change
in the SpO2 value and the horizontal axis (T) shows the time.
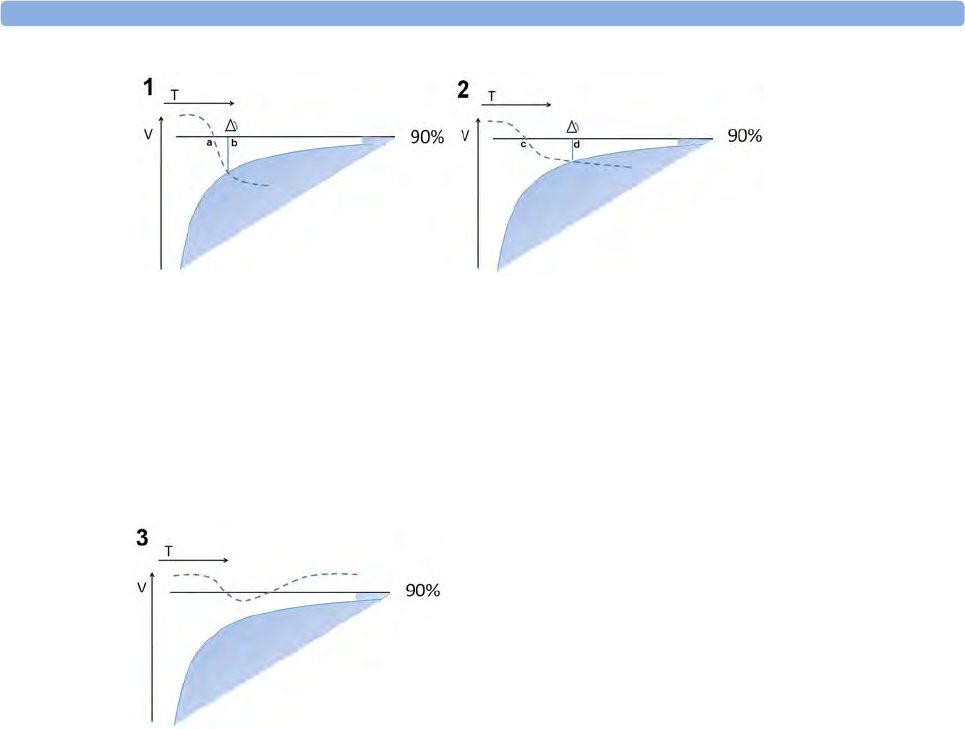
8 Monitoring SpO2
170
In example 1, the SpO2 value is dropping quickly and goes below the low alarm limit at the point
marked a. At the point marked b it also crosses into the shaded area which represents the Smart Alarm
Delay criteria - the low limit alarm is announced. The delay between the limit being crossed and the
alarm being announced, the distance between a and b, is short.
In example 2, the SpO2 value is dropping more slowly and goes below the low alarm limit at the point
marked c. At the point marked d it also crosses into the shaded area which represents the Smart Alarm
Delay criteria - the low limit alarm is announced. The delay between the limit being crossed and the
alarm being announced, the distance between c and d, is this time longer.
In example 3, the SpO2 value drops slowly below the low alarm limit and after a short time increases
again above the limit. As the value never crosses into the shaded area which represents the Smart
Alarm Delay criteria, no alarm is announced.
However, if a limit is exceeded by a small amount for a very long time, an alarm will be announced. For
this case there is a maximum delay time after which an alarm will always be announced.
Configuration
To accommodate different levels of patient stability, there are three different Smart Alarm Delay
settings: Short, Medium and Long, which correspond to three different sets of criteria (three different
shaded areas). The appropriate setting for the treatment area where the monitor is to be used is
decided during monitor configuration. The Short setting ensures a quick response to changing
conditions for less stable patients. The Medium and Long settings extend the delay to avoid
unnecessary alarms for more stable patients. For detailed numeric information about the different
settings, see the SpO2 section in the Specifications chapter. For background information as a basis for
the decision for a specific setting, see the Configuration Guide.
Adjusting the Alarm Limits
In the Setup SpO₂ menu:
•Select
High Limit then choose the high alarm limit.
•Select
Low Limit then choose the low alarm limit.
8 Monitoring SpO2
171
WARNING
High oxygen levels may predispose a premature infant to retrolental fibroplasia. If this is a
consideration do NOT set the high alarm limit to 100%, which is equivalent to switching the high
alarm off.
Adjusting the Desat Limit Alarm
The Desat alarm is a high priority (red) alarm notifying you of potentially life threatening drops in
oxygen saturation.
1In the Setup SpO₂ menu, select Desat Limit.
2Adjust the limit.
Pleth Wave
The Pleth wave is autoscaled to maximum display size. It decreases only when the signal quality
becomes marginal. It is NOT directly proportional to the pulse volume. If you need an indication of
change in pulse volume, use the perfusion indicator.
1 Minimum size for reliable SpO2 value
Perfusion Numeric
The perfusion numeric (Perf) gives a value for the pulsatile portion of the measured signal caused by
the pulsating arterial blood flow.
As pulse oximetry is based on the pulsatile nature of the signal, you can also use the perfusion numeric
as a quality indicator for the SpO2 measurement. Above 1 is optimal, between 0.3-1 is acceptable.
Below 0.3 is marginal; reposition the sensor or find a better site.
Perfusion Change Indicator
The perfusion change indicator is a graphic symbol which shows the change in the perfusion value,
relative to a reference value which you can set.
To set the current perfusion value as the reference value:
•In the Setup SpO₂ menu, select Set Perf Ref..
When a reference value has been set, the perfusion change indicator is displayed next to the perfusion
numeric.
8 Monitoring SpO2
172
Setting SpO2/Pleth as Pulse Source
1In the Setup SpO₂ menu, select Pulse (SpO₂) to enter the Setup Pulse menu.
2In the Setup Pulse menu, select System Pulseand select the correct SpO2 label from the pop-up
list.
Setting Up Tone Modulation
If tone modulation is on, the QRS tone pitch lowers when the SpO2 level drops. Remember, the QRS
tone is derived from either heart rate or pulse depending on which is currently selected as the active
alarm source.
In the Setup SpO₂ menu, select Tone Modulation to switch between Yes (for on) and No (for off).
Tone modulation is licensed under US patent US 4.653.498 from Nellcor Puritan Bennett
Incorporated.
Setting the QRS Volume
In the Setup SpO₂ menu, select QRS Volume and set the appropriate QRS tone volume.
Calculating SpO2 Difference
When a second SpO2 measurement is present (either through the SpO2 module or through an external
device), the monitor displays both SpO2 values, and calculates the difference between them. The
second value is subtracted from the first.
1From the Main Setup menu, select Measurements.
2From the Setup ΔSpO₂menu, select First SpO₂.
3Choose the first measurement source.
4Select Second SpO₂.
5Choose the second measurement source.
9
173
9Monitoring NBP
This monitor uses the oscillometric method for measuring NBP. In adult and pediatric mode, the
blood pressure measurements determined with this device comply with the American National
Standard for Electronic or Automated Sphygmomanometers (ANSI/AAMI SP10-1992) in relation to
mean error and standard deviation, when compared to intra-arterial or auscultatory measurements
(depending on the configuration) in a representative patient population. For the auscultatory reference,
the fifth Korotkoff sound was used to determine the diastolic pressure.
In neonatal mode, the blood pressure measurements determined with this device comply with the
American National Standard for Electronic or Automated Sphygmomanometers (ANSI/AAMI SP10-
1992) in relation to mean error and standard deviation, when compared to intra-arterial measurements
in a representative patient population.
The NBP measurement is suitable for use in the presence of electrosurgery and during the discharge of
a cardiac defibrillator according to IEC 601-2-30:1999/EN 60601-2-30:2000.
A physician must determine the clinical significance of the NBP information.
Introducing the Oscillometric NBP Measurement
Oscillometric devices measure the amplitude of pressure changes in the occluding cuff as the cuff
deflates from above systolic pressure. The amplitude suddenly increases as the pulse breaks through
the occlusion in the artery. As the cuff pressure decreases further, the pulsations increase in amplitude,
reach a maximum (which approximates to the mean pressure), and then diminish.
Studies show that, especially in critical cases (arrhythmia, vasoconstriction, hypertension, shock),
oscillometric devices are more accurate and consistent than devices using other noninvasive measuring
techniques.
WARNING
Patient Category: Select the correct patient category setting for your patient. Do not apply the higher
adult inflation, overpressure limits and measurement duration to neonatal patients.
Intravenous infusion: Do not use the NBP cuff on a limb with an intravenous infusion or arterial
catheter in place. This could cause tissue damage around the catheter when the infusion is slowed or
blocked during cuff inflation.
Skin Damage: Do not measure NBP in cases of sickle-cell disease or any condition where skin
damage has occurred or is expected.
9 Monitoring NBP
174
Unattended measurement: Use clinical judgement to decide whether to perform frequent
unattended blood pressure measurements in cases of severe blood clotting disorders because of the
risk of hematoma in the limb fitted with the cuff.
CAUTION
If you spill liquid onto the equipment or accessories, particularly if there is a chance that it can get
inside the tubing or the measurement device, contact your service personnel.
Measurement Limitations
Measurements are impossible with heart rate extremes of less than 40 bpm or greater than 300 bpm, or
if the patient is on a heart-lung machine.
The measurement may be inaccurate or impossible:
• with excessive and continuous patient movement such as shivering or convulsions
• if a regular arterial pressure pulse is hard to detect
• with cardiac arrhythmias
• with rapid blood pressure changes
• with severe shock or hypothermia that reduces blood flow to the peripheries
• with obesity, where a thick layer of fat surrounding a limb dampens the oscillations coming from
the artery
• on an edematous extremity.
The effectiveness of this sphygmomanometer has not been established in pregnant, including pre-
eclamptic patients.
Measurement Modes
There are four modes for measuring NBP:
•Manual - measurement on demand.
•Auto - continually repeated measurements (between one minute and 24 hours adjustable interval).
•Sequence - up to four measurement cycles which will run consecutively, with number of
measurements and interval between them configurable for each cycle.
•STAT - rapid series of measurements over a five minute period, then the monitor returns to the
previous mode. Use only on supervised patients.
Reference Method
The measurement reference method can be Auscultatory (manual cuff) or Invasive (intra-arterial). For
further information, see the Application Note supplied on the monitor documentation DVD.
In Neonatal mode, to comply with safety standards, invasive is always used as the reference method.
This setting cannot be changed and is not visible in any operating mode.
In Adult and Pediatric mode, to check the current setting, select Main Setup then Measurements
followed by NBP, and check whether the Reference setting is set to Auscultatory or Invasive. This
setting can only be changed in Configuration Mode.
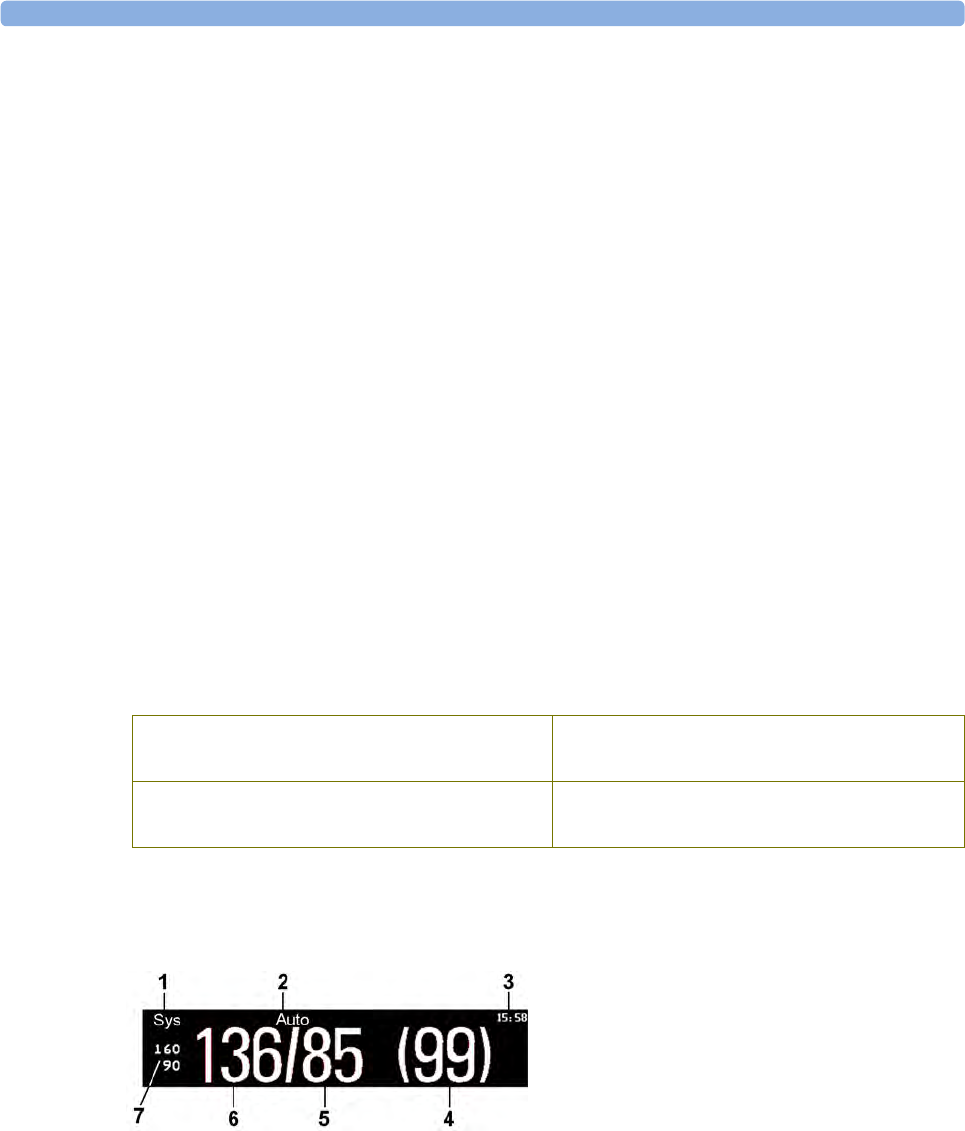
9 Monitoring NBP
175
Preparing to Measure NBP
1Connect the cuff to the air tubing.
2Plug the air tubing into the red NBP connector. Avoid compression or restriction of pressure
tubes. Air must pass unrestricted through the tubing.
3Make sure that you are using a Philips-approved correct sized cuff and that the bladder inside the
cover is not folded or twisted.
A wrong cuff size, and a folded or twisted bladder, can cause inaccurate measurements. The width
of the cuff should be in the range from 37% to 47% of the limb circumference. The inflatable part
of the cuff should be long enough to encircle at least 80% of the limb.
4Apply the cuff to a limb at the same level as the heart. If it is not, you must use the measurement
correction formula to correct the measurement.
The marking on the cuff must match the artery location. Do not wrap the cuff too tightly around
the limb. It may cause discoloration, and ischemia of the extremities. Inspect the application site
regularly to ensure skin quality and inspect the extremity of the cuffed limb for normal color,
warmth and sensitivity. If the skin quality changes, or if the extremity circulation is being affected,
move the cuff to another site or stop the blood pressure measurements immediately. Check more
frequently when making automatic or stat measurements.
Correcting the Measurement if Limb is not at Heart Level
To correct the measurement if the limb is not at heart level, to the displayed value
Understanding the NBP Numerics
Depending on the NBP numeric size, not all elements may be visible. Your monitor may be configured
to display only the systolic and diastolic values.
add 0.75 mmHg (0.10 kPa) for each centimeter
higher or
deduct 0.75 mmHg (0.10 kPa) for each
centimeter lower or
add 1.9 mmHg (0.25 kPa) for each inch higher. deduct 1.9 mmHg (0.25 kPa) for each inch
lower.
1Alarm source
2Measurement Mode
3Timestamp/Timer
4Mean pressure
5Diastolic
6Systolic
7Alarm limits
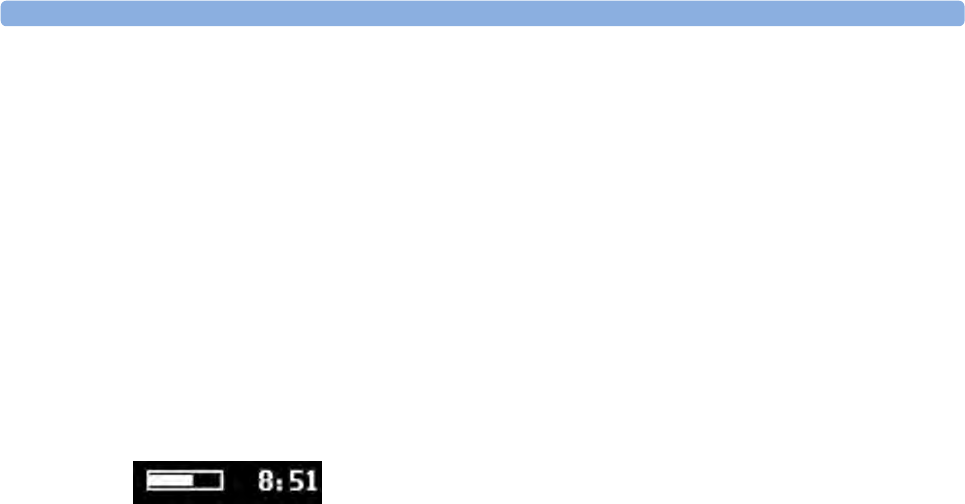
9 Monitoring NBP
176
The measured NBP value, together with the corresponding pulse rate if this is switched on, will be
displayed for one hour. After that the values are regarded as invalid and are no longer displayed. In
Auto mode the measurement values may disappear more quickly (to be replaced by new measurement
values), if the repeat time is set to less than one hour.
Alarm Sources
If you have parallel alarm sources, the sources are displayed instead of the alarm limits.
NBP Timestamp
Depending on your configuration, the time shown beside the NBP numeric can be:
– the time of the most recent NBP measurement, also known as the "timestamp", or
– the time until the next measurement in an automatic series, displayed with a graphic
representation of the remaining time, as shown here.
The NBP timestamp will normally show the completion time of the NBP measurement. Only under
the following conditions the timestamp shows the beginning of the measurement:
•when in Auto or Sequence mode, and
• the monitor is configured to synchronize the measurements in a measurement series to an "easy-
to-document" time. For example, if you start the first measurement at 08:23, and the Repeat Time
is set to 10 minutes, the monitor automatically performs the next measurement at 8:30, then 8:40
and so on.
During Measurements
The cuff pressure is displayed instead of the units and the repeat time. An early systolic value gives you
a preliminary indication of the systolic blood pressure during measurement.
Starting and Stopping Measurements
Use the Setup menu, SmartKeys or the MMS hardkey to start and stop measurements.
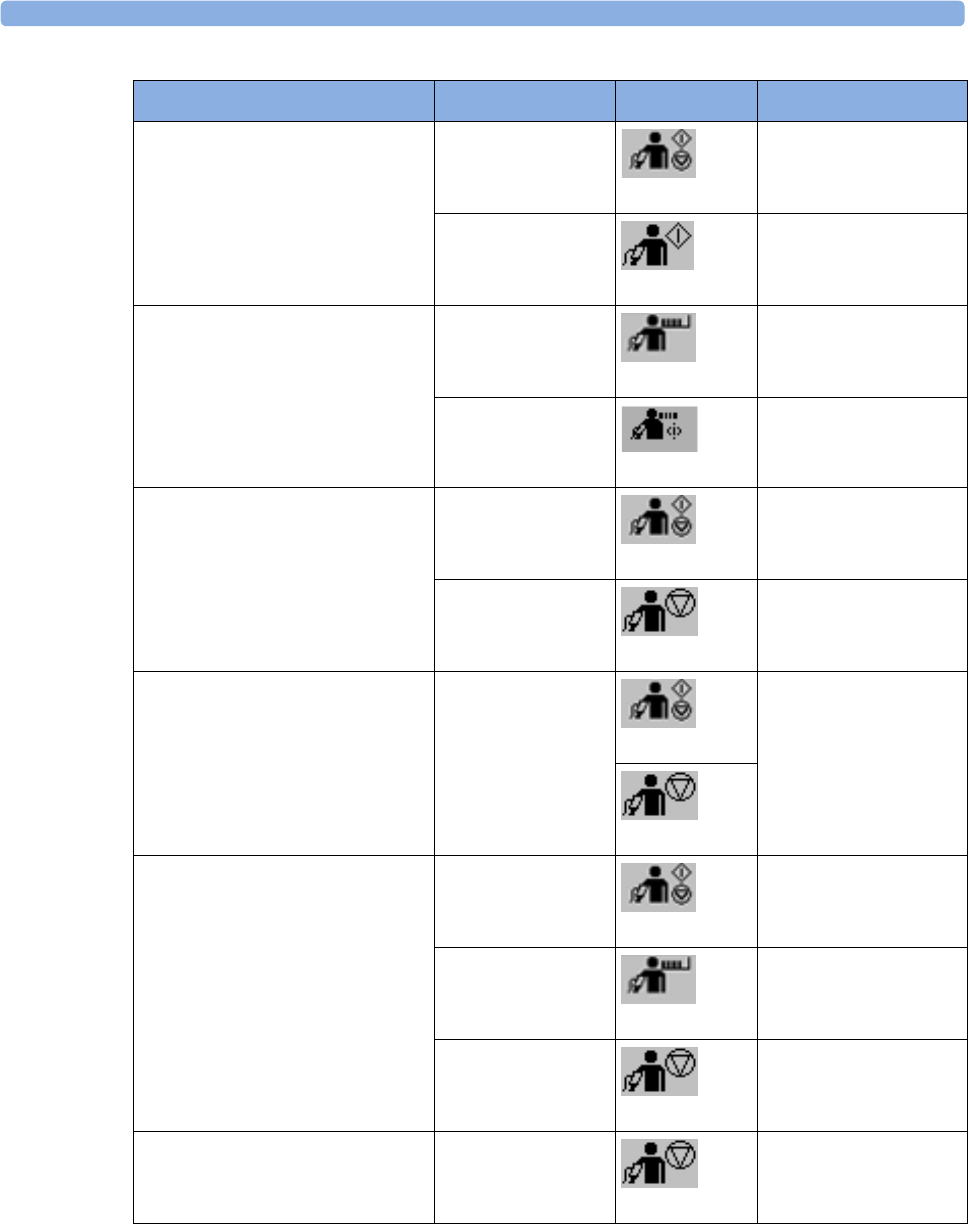
9 Monitoring NBP
177
Action to be performed NBP Setup menu SmartKeys MMS hardkey
Start manual measurement
Start Auto series
Start/Stop
Start/ Stop
Start/Stop
Start NBP
---
Start STAT measurement NBP STAT
NBP STAT
STAT (for MMS
without Pressure/Temp
measurement)
Start STAT
Stop Manual measurements Start/Stop
Start/ Stop
Start/Stop
Stop NBP
Stop current Auto measurement Start/Stop
Start/ Stop
Start/Stop
Stop NBP
Stop current STAT
measurement and end series
Start/Stop
Start/ Stop
Start/Stop
NBP STAT
NBP STAT
STAT (for MMS
without Pressure/Temp
measurement)
Stop NBP
Stop Auto, Manual or STAT
measurement AND series
Stop All
Stop All
9 Monitoring NBP
178
CAUTION
Use clinical judgment to decide whether to perform repeated series of STAT measurements because of
the risk of purpura, ischemia and neuropathy in the limb with the cuff.
Enabling Automatic Mode and Setting Repetition
Time
1In the Setup NBP menu, select Mode and select Auto from the pop-up menu.
2For an automatic measurement, select Repeat Time and set the time interval between two
measurements.
Enabling Sequence Mode and Setting Up The
Sequence
1In the Setup NBP menu, select Mode and select Sequence from the pop-up menu.
2Select Setup Sequence to open the Setup Sequence window.
Up to four measurement cycles can be setup which will run consecutively. For each cycle you can
set the number of measurements and the interval between them. If you want to run less than four
cycles in a sequence, you can set the number of measurements for one or more cycles to Off.
3Select each sequence in turn and select the number of measurements and the time interval between
the measurements.
4To have measurements continue after the sequence, set the number of measurements for your last
cycle to Continuous and this cycle will run indefinitely.
CAUTION
Be aware that, if none of the cycles are set to Continuous, NBP monitoring will end after the last
measurement of the cycle.
When the NBP measurement mode is set to Sequence, the repetition time for Auto mode cannot be
changed.
Choosing the NBP Alarm Source
You can monitor for alarm conditions in systolic, diastolic and mean pressure, either singly or in
parallel. Only one alarm is given, with the priority of mean, systolic, diastolic.
In the Setup NBP menu, select Alarms from and choose from:
9 Monitoring NBP
179
If Mean is not selected as alarm source (Sys., Dia., or Sys & Dia selected), but the monitor can only
derive a mean value, mean alarms will nevertheless be announced using the most recent mean alarm
limits. Check that the mean alarm limits are appropriate for the patient, even when not using mean as
the alarm source. When no value can be derived an NBP MEASURE FAILED INOP will be displayed.
Switching Pulse from NBP On/Off
In the process of making the NBP measurement, a pulse value can be derived and displayed. The pulse
value is displayed together with the time the measurement was made. After one hour the value
becomes invalid. There are no alarms associated with pulse from NBP.
To switch the display of the pulse value on or off:
•In the Setup NBP menu select Pulse (NBP).
Assisting Venous Puncture
You can use the NBP cuff to cause sub-diastolic pressure. The cuff deflates automatically after a set
time (adult/pediatric 170 seconds, neonatal 85 seconds) if you do not deflate it.
1In the Setup NBP menu select VeniPuncture.
2Puncture vein and draw blood sample.
3Reselect VeniPuncture to deflate the cuff.
During measurement, the NBP display shows the inflation pressure of the cuff and the remaining time
in venous puncture mode.
NOTE
Performing a venous puncture while automatic or sequence NBP measurements are being made
suspends the measurement series for the duration of the venous puncture inflation and for three
minutes afterwards.
Calibrating NBP
NBP is not user-calibrated. Cuff-pressure transducers must be verified at least once every two years by
a qualified service professional, and calibrated, if necessary. See the Service Guide for details.
Menu option Pressure value monitored
Sys. systolic
Dia. diastolic
Mean mean
Sys & Dia systolic and diastolic in parallel
Dia & Mean diastolic and mean in parallel
Sys & Mean systolic and mean in parallel
Sys&Dia&Mean all three pressures in parallel

9 Monitoring NBP
180
10
181
10Monitoring Temperature
WARNING
Measurements from an MMS extension connected to an X2 are not available when the X2 is running
on its own battery power. They are only available when the X2 is powered by external power: when
connected to a host monitor, to the external power supply (M8023A) or to the Battery Extension
(865297).
You can measure temperature using an X1 or X2 Multi-Measurement Module (MMS), one of the
MMS extensions, or the temperature plug-in module.
Temp measurement automatically switches on when you connect a probe. You can switch the
measurement off manually.
Making a Temp Measurement
1Select the correct type and size of probe for your patient.
2If you are using a disposable probe, connect the probe to the temperature cable.
3Plug the probe or temperature cable into the temperature connector socket.
4Apply the probe to the patient. You are advised to use a protective rubber cover on rectal probes.
5Select an appropriate temperature label.
6Check that the alarm settings (on or off, high and low limits) are appropriate for this patient and
this type of temperature measurement.
WARNING
Make sure you set alarm limits for the correct label. The alarm limits you set are stored for that
particular label only. Changing the label may change the alarm limits.
Selecting a Temperature for Monitoring
Tell the monitor which temperature you want to monitor by selecting its temperature label. The label is
a unique identifier for each type of temperature. When you choose a label, the monitor uses that label's
stored color and alarm settings.
1In the Setup <Temp Label> menu, select Label.
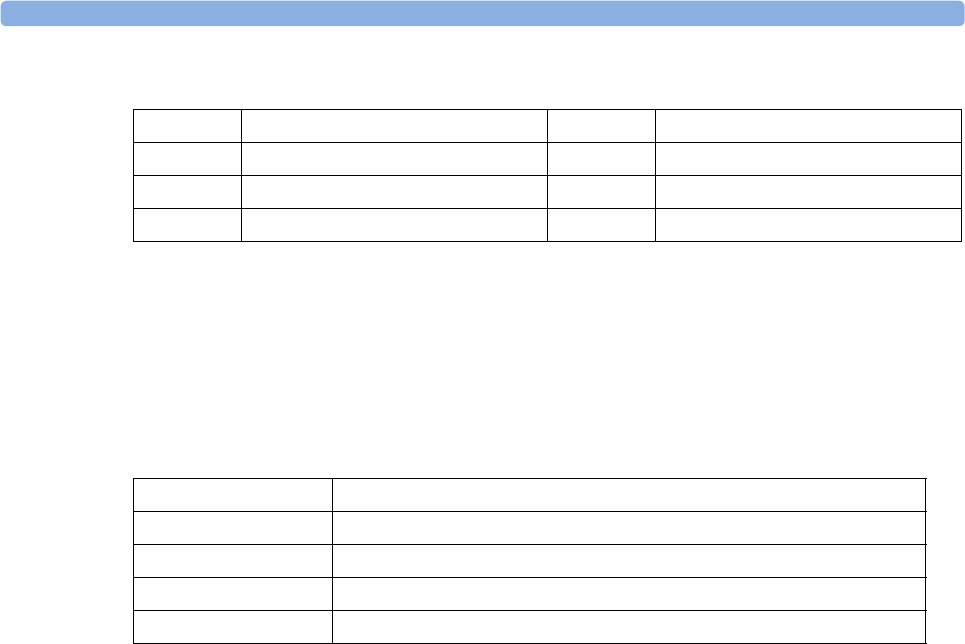
10 Monitoring Temperature
182
2Select the appropriate label from the list.
Extended Temperature Label Set
The following additional labels are available if Label Set is set to Full. This setting can only be changed
in Configuration Mode.
Note that if your monitor is connected to an Information Center, the additional labels in the extended
label set may not be correctly displayed. See the Configuration Guide for your monitor for more
information.
Calculating Temp Difference
The monitor can calculate and display the difference between two temperature values by subtracting
the second value from the first. The difference is labeled ΔTEMP.
1In the Main Setup menu, select Measurements.
2In the Setup ΔTemp menu, select First Temp.
3Label the measurement source as appropriate.
4Select Second Temp.
5Label the measurement source as appropriate.
Temp non-specific temperature label Trect rectal temperature
Tart arterial temperature Tskin skin temperature
Tcore core temperature Tven venous temperature
Tesoph esophageal temperature Tnaso nasopharyngeal temperature
T1, T2, T3, T4 Non-specific temperature labels
Tamb ambient temperature
Tcereb cerebral temperature
Ttymp tympanic temperature
Tvesic vesical temperature
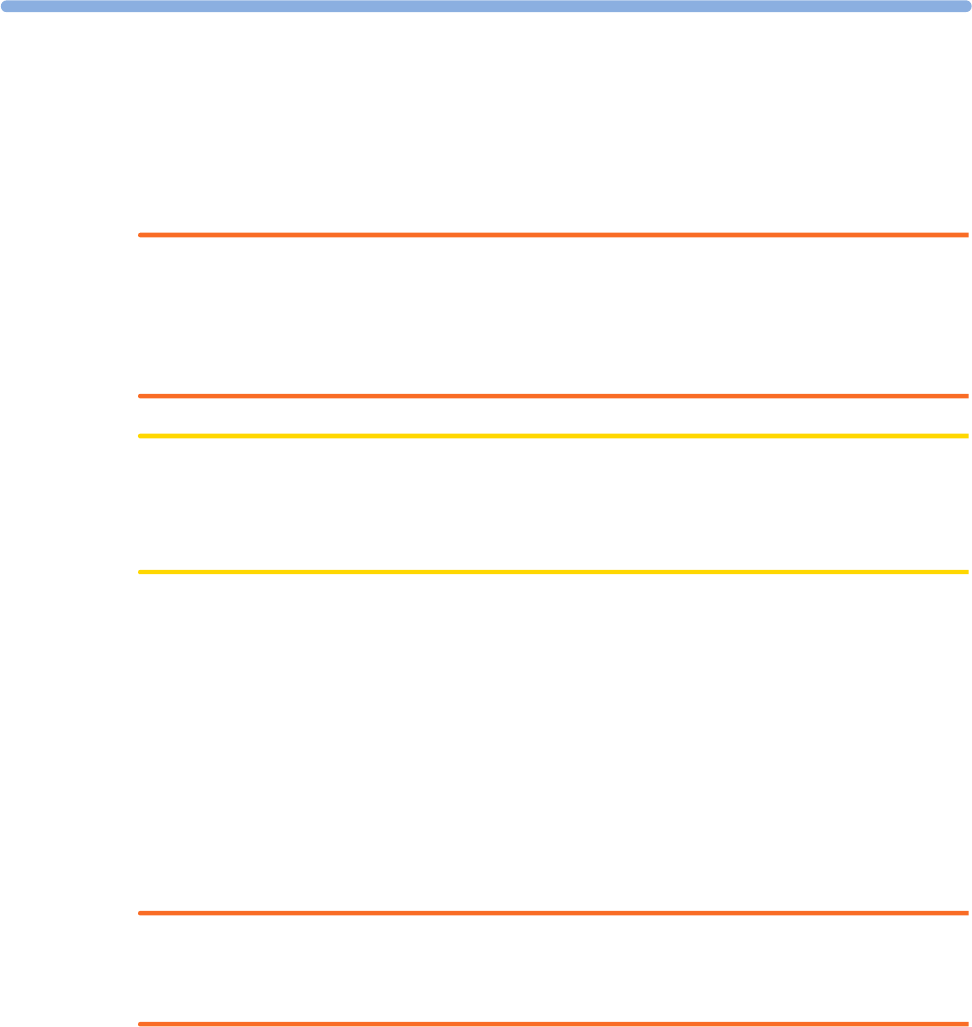
11
183
11Monitoring Invasive Pressure
WARNING
Measurements from an MMS extension connected to an X2 are not available when the X2 is running
on its own battery power. They are only available when the X2 is powered by external power: when
connected to a host monitor, to the external power supply (M8023A) or to the Battery Extension
(865297).
CAUTION
Do not use the X2 in combination with monitors using an M1006A pressure module and the
HP1290A pressure transducer. This may cause interference on the respiration or invasive pressure
signals.
You can measure pressure using an X1 or X2 Multi-Measurement Module (MMS), one of the MMS
extensions or the pressure plug-in module. With the plug-in module you may see a wave channel
before the pressure cable is plugged in - with the MMS this will not be the case.
Setting up the Pressure Measurement
1Plug in the pressure cable.
2Prepare the flush solution.
3Flush the system to exhaust all air from the tubing. Ensure that the transducer and stopcocks are
free of air bubbles.
WARNING
If air bubbles appear in the tubing system, flush the system with the infusion solution again. Air
bubbles may lead to a wrong pressure reading.
1Connect the pressure line to the patient catheter.
2If you are using an infusion pressure cuff with the pressure line, attach the pressure cuff to the
fluid to be infused. Inflate it according to your standard hospital procedure, then start the infusion.
3Position the transducer so that it is level with the heart, approximately at the level of the
midaxillary line.
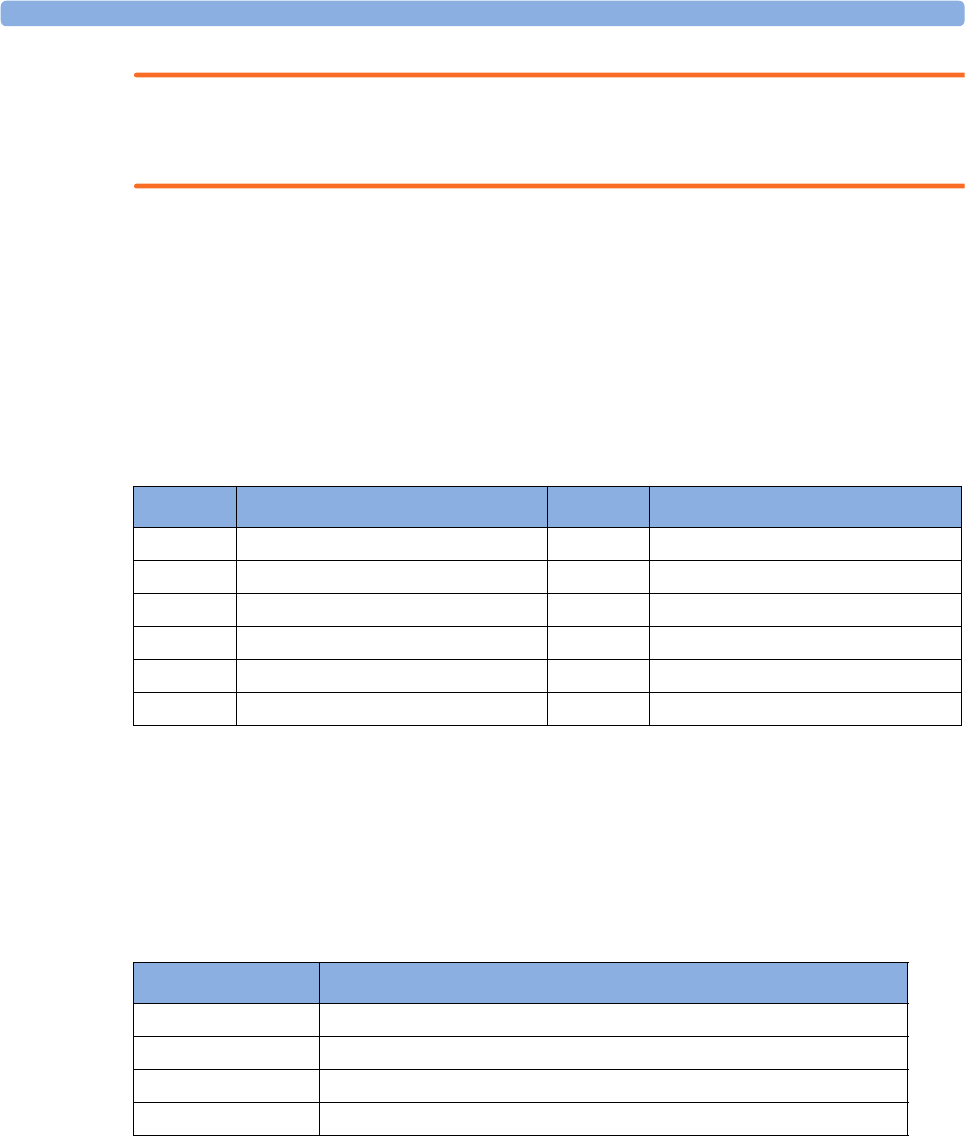
11 Monitoring Invasive Pressure
184
WARNING
If measuring intracranial pressure (ICP, IC1 or IC2) with a sitting patient, level the transducer with the
top of the patient's ear. Incorrect leveling may give incorrect values.
Selecting a Pressure for Monitoring
Tell the monitor which pressure you want to monitor by selecting its pressure label. The label is a
unique identifier for each type of pressure. When you choose a label, the monitor uses that label's
stored settings, for example color, wave scale and alarm settings. The label also determines which
algorithm is used to process the pressure signal, so an incorrect label can lead to incorrect pressure
values.
1In the Setup <Press Label> menu, select Label.
2Select the appropriate label from the list.
Extended Pressure Label Set
The following additional labels are available if Label Set is set to Full. This setting can only be changed
in Configuration Mode.
Note that if your monitor is connected to an Information Center, the additional labels in the extended
label set may not be correctly displayed. See the Configuration Guide for your monitor for more
information.
Zeroing the Pressure Transducer
To avoid inaccurate pressure readings, the monitor requires a valid zero. Zero the transducer in
accordance with your hospital policy. You must perform a zero:
• when you use a new transducer or tubing
• every time you reconnect the transducer cable to the monitor
Label Description Label Description
ABP Arterial blood pressure PNon-specific pressure label
ART Arterial blood pressure (alternative) PAP Pulmonary artery pressure
Ao Aortic pressure RAP Right atrial pressure
CVP Central venous pressure UAP Umbilical arterial pressure
ICP Intracranial pressure UVP Umbilical venous pressure
LAP Left atrial pressure
Label Description
BAP Brachial arterial pressure
FAP Femoral arterial pressure
IC1, IC2 Alternative intracranial pressures
P1, P2, P3, P4 Alternative non-specific pressure labels
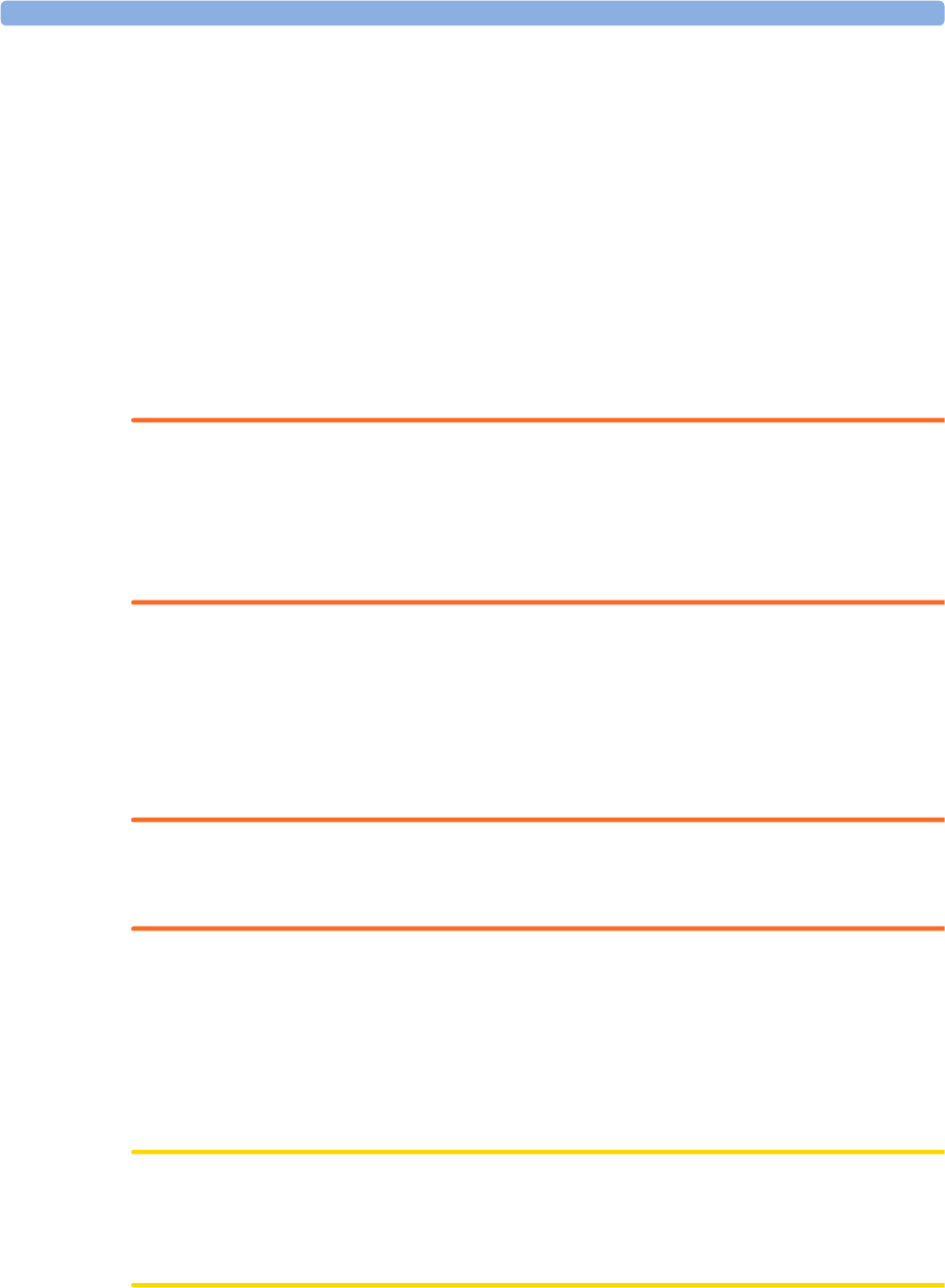
11 Monitoring Invasive Pressure
185
• if you think the monitor's pressure readings are not correct.
When using a pressure module, the zero information is stored in the module. When a pressure module,
with the transducer connected, is plugged into the monitor, the monitor will use the Zero stored in the
module.
Zeroing ICP (or IC1/IC2)
Your hospital guidelines may require you to zero the ICP transducer less frequently than other
transducers, due to the need for aseptic conditions. When you zero an ICP transducer, the zero values
are automatically stored and you will not be prompted to repeat the zero procedure.
If you want to simultaneously zero all pressures except ICP, disconnect the ICP transducer from the
Multi-Measurement module or pressure module while zeroing. Reconnecting the transducer recalls the
stored values.
WARNING
If you select the label ICP (or IC1/IC2), the measurement device uses the most recently stored zero.
Therefore, make sure you zeroed the transducer correctly in accordance with the transducer
manufacturer's instructions and your hospital policy. When you use a transducer that you cannot
rezero after placement, ensure that you keep the measuring device with the patient so that you are
certain you have the correct zero data for this patient.
Determining a Pressure's Most Recent Zero
The monitor displays the most recent zero on the status line. If this has "timed-out" after you have
performed a zero, redisplay the information in the status line by entering the pressure's setup menu.
Zeroing a Pressure Measurement
WARNING
Invasive pressure alarms (and pulse alarms, if derived from invasive pressure) are temporarily
suppressed until 30 seconds after the transducer finishes zeroing.
1Turn off the stopcock to the patient.
2Vent the transducer to atmospheric pressure, to compensate for the static and atmospheric
pressure exerted on the transducer.
3In the setup menu for the pressure, select Zero <Press Label>.
4When you see the message <Press Label> zero done at <date and time> on the status line,
close the stopcock to atmospheric pressure, and open the stopcock to the patient.
CAUTION
When using high frequency ventilation, ensure that the tubing from the ventilator does not touch the
arterial line, or connect with it indirectly, while zeroing the pressure. This could cause small pressure
variations which can interfere with the zero procedure.
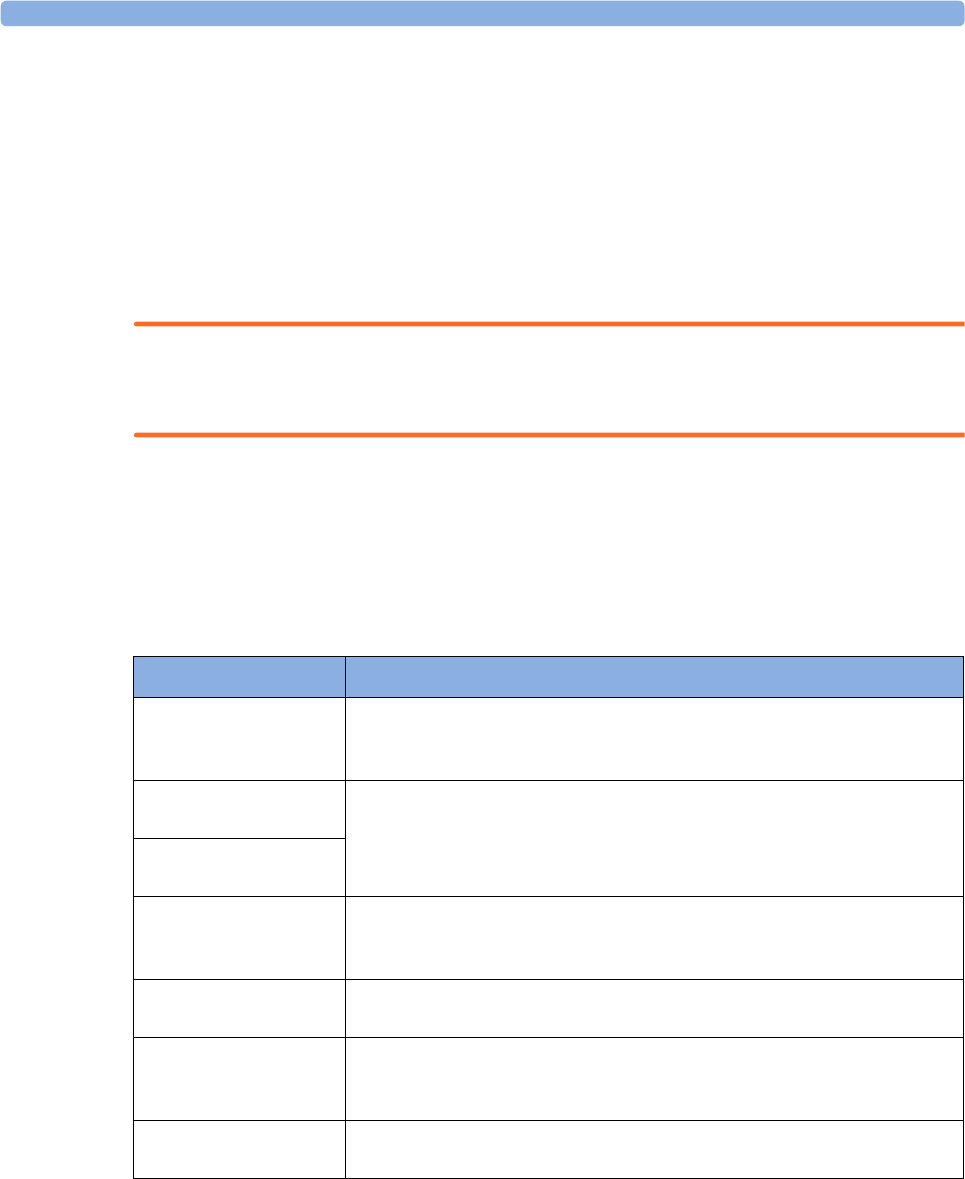
11 Monitoring Invasive Pressure
186
Using the Zero Hardkey
Pressing the Zero hardkey for two seconds on the M1006B Pressure module starts a zero for the
pressure currently measured with the module.
Pressing the Zero hardkey for two seconds on the M3001A Multi-Measurement module zeros the
pressure being measured by the Multi-Measurement module and the pressures from any connected
MMS extensions.
Zeroing All Pressures Simultaneously
WARNING
Before zeroing all pressures, make sure that all pressure transducers are vented to atmospheric
pressure.
If you are measuring pressures with more than one measuring device, using the Zero Press SmartKey
to initiate the zeroing calls up a list of all active pressures. Select the pressure you want to zero or select
All Press to zero all pressures simultaneously.
Troubleshooting the Zero
The status line lists the probable cause of an unsuccessful zero:
Adjusting the Calibration Factor
Each time you use a reusable transducer, compare the calibration factor written on your transducer
with the calibration factor shown on the monitor. To ensure accurate measurement, they must be the
same.
Message Corrective Action
unable to zero -
equipment
malfunction
The hardware is faulty. Contact your service personnel.
unable to zero -
excessive offset
Make sure the transducer is vented to air and try again. If this fails, the
hardware may be faulty. Replace the adapter cable and try again. If it fails,
replace the transducer and try again. If it still fails, contact your service
personnel.
unable to zero -
unstable signal
unable to zero - no
transducer
Make sure that the transducer is connected and try again. If this fails,
exchange the adapter cable and try again. If this fails, exchange the
transducer.
unable to zero -
pulsatile pressure
Make sure that the transducer is vented to air, not to the patient, and try
again.
unable to zero - timed
out
Try pressing the Zero hardkey or Zero <Press Label> key again. If this
fails, replace the transducer and adapter cable and contact your service
personnel.
Switch on first Pressure measurement is switched off. To switch it on, in the Setup <Press
Label> menu, select the pressure's label.

11 Monitoring Invasive Pressure
187
1In the Setup <Press Label> menu, select Cal. Factor.
If the value here does not match that on the transducer, select the corresponding value from the
list now in accordance with your hospital's procedure.
2To confirm you want to use the new calibration factor, select the Confirm pop-up key.
Displaying a Mean Pressure Value Only
Use this when you want to see only the mean pressure.
In the pressure's setup menu, select Mean only. Toggle between On to display mean pressure value
only, and Off to display all pressure values (systolic, diastolic and mean).
Changing the Pressure Wave Scale
1Select the label of the pressure wave whose scale you want to set to enter the Setup <Press
Label> menu.
2In the Setup <Press Label> menu, (for example ABP) select Scale.
3Select a value from the pop-up list:
– a positive value sets the top gridline. The bottom gridline is set at zero.
– a negative value sets the bottom gridline. The middle gridline is set at zero.
Optimizing the Waveform
In the Setup <Press Label> menu, select Optimum Scale to let the monitor select the best minimum
and maximum scales for the current wave.
Using the Wave Cursor
When the pressure wave is selected, you can display a cursor in the wave. It appears as a white
horizontal line in the wave. Using the pop-up keys you can move the cursor up or down to the
required position and store the corresponding value. The cursor value can be stored
• as a systolic, diastolic or mean pressure value,
• as an IAP (intra-abdominal pressure) value - for the waves P, P1 to P8, if IAP is configured as a
measurement which can be manually entered
• as a PAWP value - if the pressure wave is a PAP wave
The stored value appears in the trend database as a manually entered value.
To display and position the cursor
1Select the pressure wave.
2Select Activate Cursor.
3Use the pop-up arrow keys to position the cursor.
Using the pop-up keys you can also change the scale or the speed for the wave, freeze the wave or start
a printout or recording.
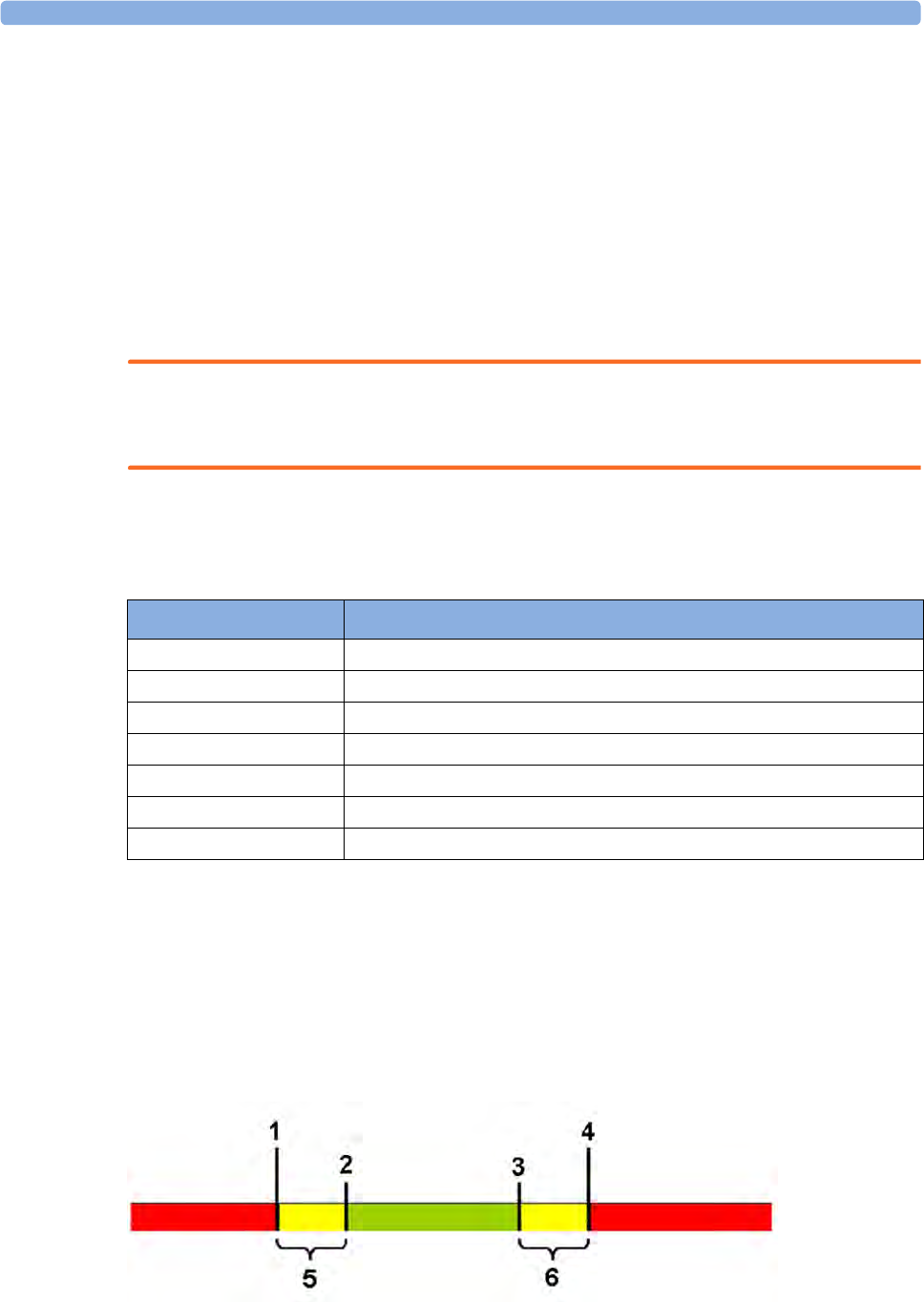
11 Monitoring Invasive Pressure
188
Non-Physiological Artifact Suppression
Some clinical procedures may affect blood pressure, for example, a flush procedure or a blood sample.
Your monitor may be configured to suppress these non-physiological artifacts for a specified duration
(Artifact Suppr. is configured to 30 sec, 60 sec, or 90 sec). During artifact suppression, the monitor
shows the INOP message <Press Label> ARTIFACT, and a question mark is shown beside the
pressure numerics. Pressure alarms and the <Press Label> NON-PULSATILE INOP are suppressed
during the configured period. The CPP alarms are not suppressed.
Choosing the Pressure Alarm Source
WARNING
Make sure you set alarm limits for the correct label. The alarm limits you set are stored for that
particular label only. Changing the label may change the alarm limits.
You can monitor for alarm conditions in systolic, diastolic and mean pressure, either singly or in
parallel. Only one alarm is given at a time, in this order of priority: mean, systolic, diastolic.
In the Setup <Press Label> menu, select Alarms from and choose the source.
Select and set the High Limit and Low Limit for the pressure(s) you have selected.
Extreme Alarm Limits for Pressure
The extreme pressure alarms, Extreme High and Extreme Low, can be made available for your
monitor in Configuration Mode and are additional to the standard High and Low limit alarms. They
are generated by the active pressure alarm source, and are setup in Configuration Mode by adding a set
value (the Δ value) to the high and low alarm limits. This value can be set for each pressure label
individually.
Menu option Pressure value monitored
Sys. systolic
Dia. diastolic
Mean mean
Sys & Dia systolic and diastolic in parallel
Dia & Mean diastolic and mean in parallel
Sys & Mean systolic and mean in parallel
Sys&Dia&Mean all three pressures in parallel
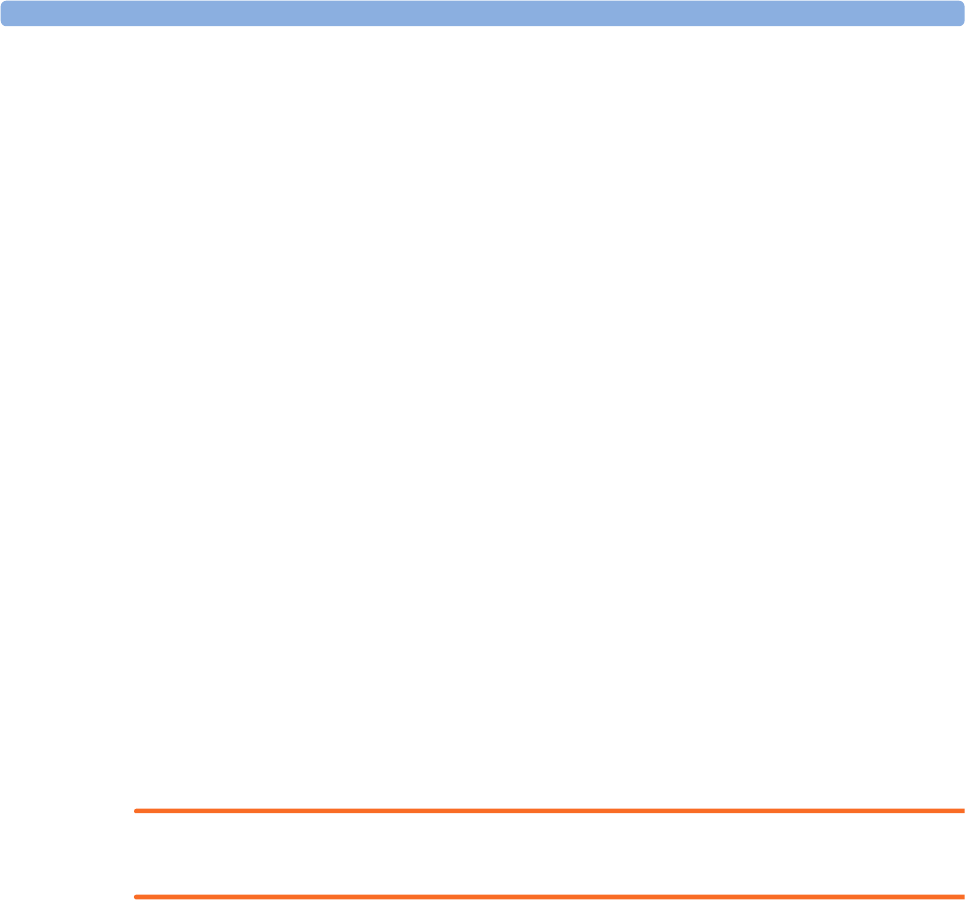
11 Monitoring Invasive Pressure
189
1Extreme Low Limit
2Low Limit
3High Limit
4Extreme High Limit
5Δ Extreme Low
6Δ Extreme High
You need to know which values have been configured for your monitor. Changing the high and low
alarm limits automatically changes the extreme alarm limits within the allowed range.
• To see the extreme pressure alarms set for your monitor, in the Setup <Press Label> menu, see
the menu items Δ Extreme High and Δ Extreme Low.
The extreme pressure alarms are high priority, red alarms, marked *** in the alarm message.
Calibrating Reusable Transducer CPJ840J6
Depending on your monitor's configuration, you may be able to perform a calibration in monitoring
mode. Perform a mercury calibration when you use a new transducer, and at regular intervals
according to your hospital policy. You require:
• standard sphygmomanometer.
• sterile 10cc syringe with heparinised solution.
•3-way stopcock.
• approximately 25cm of tubing.
Making the Pressure Calibration
WARNING
Never perform the invasive pressure calibration while a patient is being monitored.
1Zero the transducer.
2Connect the syringe and manometer.
a. Attach the tubing to the manometer.
b. Connect the 3-way stopcock to the stopcock that is not connected to the patient catheter
when you measure a patient.
c. Attach the syringe to one port and the manometer tubing to the other port.

11 Monitoring Invasive Pressure
190
d. Open the port to the manometer.
1 Tubing to manometer
2 Syringe with heparinised solution
3 To pressure connector on monitor
4 Patient connection stoppered
5 Off
3Move the syringe barrel in and raise the mercury to 200 mmHg (30 kPa). 200 mmHg is the
recommended calibration pressure.
4In the Setup <Press Label> menu, select Cal. Press.
5Select the calibration pressure from the list, for example 200 mmHg.
6Select Confirm to recalculate the calibration factor using the applied pressure.
7When the monitor displays <Press Label> mercury calibr. done at <date and time>, remove
the manometer tubing, syringe and extra stopcock. We recommend you replace the transducer
dome and tubing with sterile ones.
8Label the transducer with the calibration factor shown in the Cal. Factor field in the pressure's
setup menu.
9Reconnect the patient and start measuring again.
Troubleshooting the Pressure Calibration
The status line lists the probable cause of an unsuccessful calibration.
Message Corrective Action
unable to calibrate - equipment
malfunction
Contact your service department. The pressure hardware is
faulty.
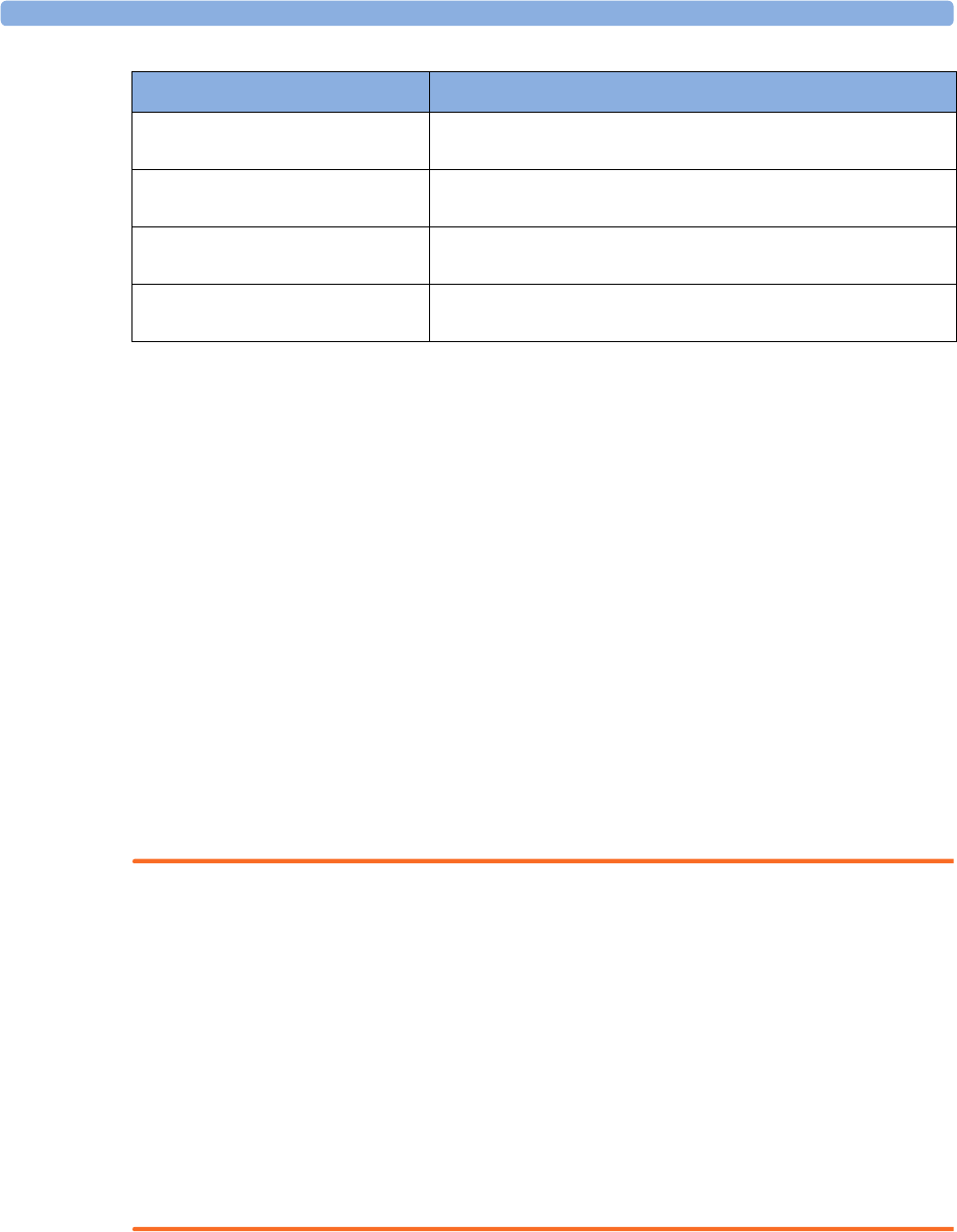
11 Monitoring Invasive Pressure
191
Calculating Cerebral Perfusion Pressure
The monitor can calculate the difference between mean arterial pressure and the intracranial pressure.
The difference is labeled CPP.
1In the Main Setup menu, select Measurements.
2In the Setup CPP menu, select one of the listed pressures as the arterial pressure source.
Calculating Pulse Pressure Variation
Note: Pulse Pressure Variation can be calculated in two different ways on this monitor - directly from
the pressure measurement or in conjunction with the CCO measurement. Refer to the Cardiac Output
chapter for information on PPV from CCO. Only one PPV can be active at a time.
Pulse Pressure Variation (PPV) is calculated from beat-to-beat arterial pressure values. Pulse pressure
is the difference between the systolic and the diastolic pressure values for a single beat. Pulse pressure
variation is defined as the maximal pulse pressure less the minimum pulse pressure divided by the
average of the two. The average variation in pulse pressure is calculated over periods of 32 seconds.
WARNING
• This monitor can calculate PPV from beat-to-beat values of any arterial pulsatile pressure. The
circumstances under which the calculation of a PPV value is clinically meaningful, appropriate and
reliable must be determined by a physician.
• The clinical value of the derived PPV information must be determined by a physician. According
to recent scientific literature, the clinical relevance of PPV information is restricted to sedated
patients receiving controlled mechanical ventilation and mainly free from cardiac arrhythmia.
• PPV calculation may lead to inaccurate values in the following situations:
– at respiration rates below 8 rpm
– during ventilation with tidal volumes lower than 8 ml/kg
– for patients with acute right ventricular dysfunction ("cor pulmonale").
• The PPV measurement has been validated only for adult patients
To select an arterial pressure as PPV source:
1In the Main Setup menu, select Measurements.
2In the Setup PPV menu, select ABP, ART, Ao, BAP, P or FAP as the arterial pressure source.
unable to calibrate - out of range Make sure that you have selected the value for Cal. Press that
you are applying to the transducer, and repeat the calibration.
unable to calibrate - no
transducer
Make sure that the transducer is connected and try again.
unable to calibrate - unstable
signal
Make sure there are no disturbances to the transducer, and
repeat the calibration.
unable to calibrate - perform
zero first
No valid zero. Zero the transducer.
Message Corrective Action
11 Monitoring Invasive Pressure
192
CAUTION
Older Multi-Measurement modules cannot supply a beat-to-beat arterial pressure value. In this case the
monitor shows a NO PPV FROM MMS or NO PPV FROM FMS INOP.
Measuring Pulmonary Artery Wedge Pressure
Pulmonary Artery Wedge Pressure (PAWP) values, used to assess cardiac function, are affected by:
• Fluid status
• Myocardial contractility
• Valve and pulmonary circulation integrity
Obtain the measurement by introducing a balloon-tipped pulmonary artery flotation catheter into the
pulmonary artery. When the catheter is in one of the smaller pulmonary arteries, the inflated balloon
occludes the artery allowing the monitor to record changes in the intrathoracic pressures that occur
throughout the respiration cycle. The pulmonary wedge pressure is the left ventricular end diastolic
pressure (preload).
The most accurate PAWP values are obtained at the end of the respiration cycle when the intrathoracic
pressure is fairly constant. You can use the respiration waveform as a reference when assessing the
PAWP waveform, to ensure constant measurement timing relative to the respiratory cycle. The
monitor displays the PAWP value for up to 24 hours or until you admit a new patient.
WARNING
The pressure receptor in the catheter records pressure changes that occur only in front of the
occlusion. Even though the catheter tip is in the pulmonary artery, the receptor records pressure
changes transmitted back through the pulmonary circulation from the left side of the heart.
While performing the wedge procedure, the monitor switches off the pressure alarms for pulmonary
artery pressure (PAP).
Due to a slight measurement delay, you should not use sidestream CO2 as a direct reference for
determining the end expiratory point in the pressure curve.
To start the Wedge procedure,
1In the Main Setup menu, select Wedge to display the wedge procedure window.
2Prepare and check the pressure line according to your hospital policy.
3Use the Refernce Wave 1 and Refernce Wave 2 pop-up keys to select any ECG or respiratory
wave as reference waves.
4Select Change Speed if you want to change the speed of the displayed wave. The speed can also
be changed in the screen for editing the wedge.
5Select Change Scale to change the wave scale of the PAP. The same scale will be used in the
screen for editing the wedge. If the setting Optimum Scale is used, the wave scale will be
optimized when a wedging waveform is recognized and will revert to the previous scale when the
wedge procedure window is closed.
6Inflate the balloon when the monitor prompts you: Ready for balloon inflation. The waveform
changes from the PAP to the PAWP wave. The measurement takes approximately 12 seconds. On
11 Monitoring Invasive Pressure
193
completion, the monitor stores the PAWP waveform display and prompts you to deflate the
balloon. If the monitor cannot detect a wedging waveform you must use Store Trace to store the
wedge and two reference waves manually.
7Deflate the balloon when the monitor prompts you: Ready for balloon deflation and verify that
the waveform returns to pulmonary artery shape.
8If you need to start a new measurement, select Restart Wedge.
Editing the Wedge
1Select the Edit Wedge pop-up key to see the stored waveforms.
2The monitor displays a cursor in the waveform at the PAWP mean value. It also displays any
previously stored value and the time it was stored.
3Select Change Speed if you want to change the speed (resolution) of the displayed wave.
4Move the cursors up, down, right and left to set them on the correct wedge position.
5Select Store Wedge to store the PAWP value.
6Select Print Wedge to print the PAWP waveform and any reference waves or Record Wedge to
record them. While recording or printing, you cannot perform any more Wedge tasks.
WARNING
Prolonged inflation can cause pulmonary hemorrhage, infarction or both. Inflate the balloon for the
minimum time necessary to get an accurate measurement.
If the pulmonary artery flotation catheter drifts into the wedge position without inflation of the
balloon, the pulmonary artery pressure waveform assumes a wedged appearance. Take appropriate
action, in accordance with standard procedures, to correct the situation.
If the PAWP (mean) is greater than the PAP (systolic), deflate the balloon and report the incident in
accordance with hospital policy, because the pulmonary artery could be accidentally ruptured, and the
wedge value derived will not reflect the patient's hemodynamic state, but will merely reflect the
pressure in the catheter or balloon.
Identifying the Pressure Analog Output Connector
1Analog output (module M1006B, option C01 only)

11 Monitoring Invasive Pressure
194

12
195
12Monitoring Cardiac Output
The Cardiac Output (C.O.) measurement invasively measures cardiac output and other hemodynamic
parameters using a technique called thermodilution. This can be used to determine the flow rate of a
system by introducing a cold solution into the system and measuring the resulting drop in temperature
at a downstream site. The temperature change is displayed as a curve in the C.O. procedure window,
and the monitor calculates the C.O. value from this curve. The C.O. value is inversely proportional to
the area under the curve. As cardiac output varies continuously, a series of measurements must be
carried out to achieve a reliable C.O. average value. Always use the average of multiple thermodilution
measurements for therapy decisions.
The measurements can be carried out using the right heart thermodilution method or the PiCCO
method (transpulmonary thermodilution).
• The right heart method is available with
– C.O. module M1012A, standard and option #C10
– M3012A Hemodynamic Measurement Extension Module, options #C05 and #C10
– M3014A Capnography Measurement Extension Module, option #C05 and #C10
• The PiCCO method is available with
– C.O. module M1012A, option #C10
– M3012A Hemodynamic Measurement Extension Module, option #C10
– M3014A Capnography Measurement Extension Module, option #C10
The PiCCO method additionally lets you measure Continuous Cardiac Output (CCO) by performing
pulse contour analysis on the blood pressure waveform.
Hemodynamic Parameters
This table illustrates the hemodynamic parameters available with each method, whether they are
measured continuously, and whether they can be shown on the monitor's main screen or in the
Hemodynamic Calculations window.
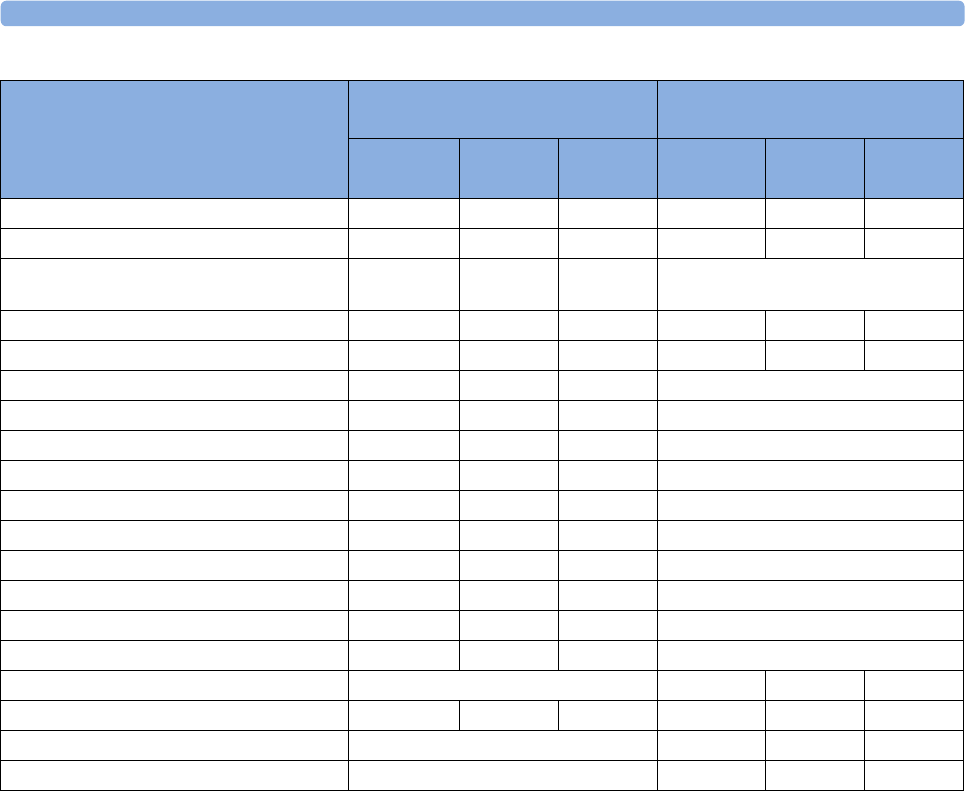
12 Monitoring Cardiac Output
196
* currently not available in the U.S.A. or in clinical environments under FDA control.
Using the C.O. Procedure Window
The procedure window displays up to six trials (measurement curves) with the trial number and the
C.O. value under the thermodilution curve. When you open the window, a line of pop-up keys
automatically appears to let you carry out C.O.-related tasks. This example shows the procedure
window for the transpulmonary (PiCCO) Method. The window may be configured to look slightly
different on your monitor.
To open the procedure window,
•Select
Cardiac Output in the Setup C.O. or Setup CCO menu, or
• Select the Cardiac Output SmartKey on the Screen, if configured, or
• Press the START hardkey on the front of the C.O. plug-in module, if available, or
• Press a remote start switch, if you are using one.
Measured and Calculated Hemodynamic
Parameters and Indexes
PiCCO Method (Transpulmonary
Thermodilution)
Right Heart Thermodilution
Continuous? Main
Screen
HemoCalc
Window Continuous? Main
Screen
HemoCalc
Window
Blood Temperature (Tblood) Y Y N Y Y N
C.O./C.I.: Cardiac Output N YYN YY
CCO/CCI: Continuous Cardiac Output Y Y Y (in the
C.O. field)
Not available
SVR/SVRI: Systemic Vascular Resistance N and Y Y Y N N Y
SV/SI: Stroke Volume/SV Index N and Y Y Y N N Y
SVV: Stroke Volume Variation Y Y Y Not available
*dPmax: Left Ventricular Contractility Index Y Y Y Not available
CFI: Cardiac Function Index N Y Y Not available
PPV: Pulse Pressure Variation Y Y Y Not available
ITBV/ITBVI: Intrathoracic Blood Volume N Y Y Not available
EVLW/EVLWI: Extravascular Lung Water N Y Y Not available
GEDV/GEDVI: Global End-Diastolic Volume N Y Y Not available
*PVPI: Pulmonary Vascular Permeability Index N Y Y Not available
*GEF: Global Ejection Fraction N Y Y Not available
*RLShnt: Right-Left-Shunt Fraction N N N Not available
PVR/PVRI: Pulmonary Vascular Resistance Not available N N Y
LCW/LCWI: Left Cardiac Work N N Y N N Y
RCW/RCWI: Right Cardiac Work Not available N N Y
RVSW/RVSWI: Right Ventricular Stroke Work Not available N N Y
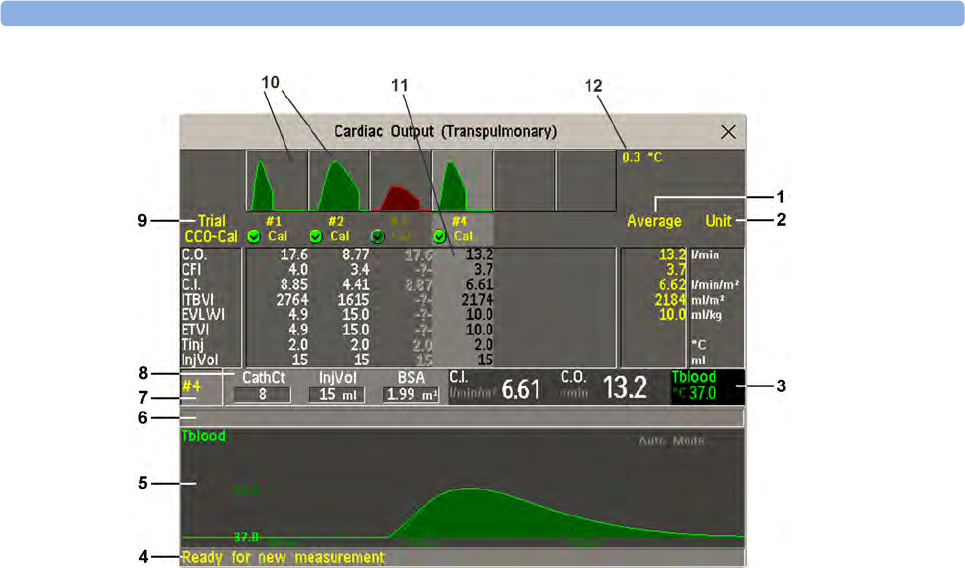
12 Monitoring Cardiac Output
197
1Average - column of averaged values
2Unit column
3Continuously measured numeric
4Prompt message field
5Thermodilution curve of current trial
6Curve alert message field
7Current trial number
8Setup information
9Trial numbers for the trial curves
10 Trial curves
11 Results table of current trial
12 Trial curve scale
• To change the measurement parameters shown in the results table of the procedure window, select
the Table Contents pop-up key and choose from the list of available parameters.
• To view the currently-used temperature unit, see the "grayed-out" setting Temperature Unit in the
Setup C.O. menu. This setting can only be changed in Configuration Mode.
• The Cardiac Output screen element may be configured to display permanently on a specially
designed Screen. Selecting the screen element opens the cardiac output pop-up keys.
Accessing the Setup C.O. and Setup CCO Menus
C.O. settings can be changed in the Setup C.O. menu. To access this menu,
• press the C.O. hard key on the C.O. module, or
• select any of the discontinuous C.O. numerics (for example, C.O., C.I.) on the screen.

12 Monitoring Cardiac Output
198
CCO/CCI settings can be changed in the Setup CCO menu. To access this menu,
• select any of the continuously measured hemodynamic numerics (CCO, CCI.) on the screen.
Entering the HemoCalc Window
From the procedure window, select the pop-up key Hemo Calc to open the Hemo Calculations
window.
Measuring C. O. Using the PiCCO Method
The PiCCO method combines transpulmonary thermodilution and pulse contour analysis on the
blood pressure waveform. A fluid with a known volume and temperature is injected into the right
atrium through a CVP catheter. The injectate bolus mixes with the blood in the heart and the change in
blood temperature is measured with a thermistor at the distal end of an arterial catheter placed in one
of the bigger systemic arteries, for example, the femoral or the axillary artery.
The PiCCO Method requires a pressure measurement made using either the M1006B Pressure
module, or a M3001A/M3002A MMS, or a measurement extension module M3015A, M3014A, or
M3012A. (A pressure from an external device may not be used.) You will also need a conventional
central venous (CVP) line and an arterial catheter from PULSION Medical Systems. You must use the
approved catheters and puncture locations.
Measuring Continuous Cardiac Output
Every time C.O. is measured with the PiCCO method, the monitor uses this C.O. value and the result
of the pulse contour analysis to calculate a patient-specific calibration factor. The monitor uses this
value to compute CCO and the other continuous hemodynamic parameters. CCO values are calculated
on a beat-to-beat basis and then averaged over a 12-second time frame. The calculated values are
displayed as numerics on the monitor screen.
Measuring Systemic Vascular Resistance
The monitor uses CCO, an arterial pressure, and CVP to calculate a continuous SVR value. If a
continuously measured CVP value is not available, the monitor uses a preset, static CVP value to
calculate the SVR (you will see the INOP message SVR SET CVP USED). If the BSA is available, the
monitor uses the CCI to calculate the SVRI. A CCO or CCI from an external device can also be used
for the SVR/SVRI calculation.
SVR/SVRI settings can be changed in the corresponding setup menu. To enter the menu, select Main
Setup then Measurements followed by SVR or SVRI.
To display a SVR/SVRI numeric on the Screen, select any numeric, then select Change Numeric and
select SVR or SVRI from the list of available numerics.
Measuring Pulse Pressure Variation
Note: Pulse Pressure Variation can be calculated in two different ways on this monitor - in conjunction
with CCO or directly from the pressure measurement. Refer to the Invasive Pressure chapter for
information on PPV from pressure. Only one PPV can be active at a time.
12 Monitoring Cardiac Output
199
Pulse Pressure Variation (PPV) is calculated from beat-to-beat arterial pressure values. Pulse pressure
is the difference between the systolic and the diastolic pressure values for a single beat. Pulse pressure
variation is defined as the maximal pressure less the minimum pressure divided by the average of these
two pressures.
WARNING
• The monitor calculates PPV from beat-to-beat values of the arterial pressure selected for CCO.
The circumstances under which the calculation of a PPV value is clinically meaningful, appropriate
and reliable must be determined by a physician.
• The clinical value of the derived PPV information must be determined by a physician. According
to recent scientific literature, the clinical relevance of PPV information is restricted to sedated
patients receiving controlled mechanical ventilation and mainly free from cardiac arrhythmia.
• PPV calculation may lead to inaccurate values in the following situations:
– at respiration rates below 8 rpm
– during ventilation with tidal volumes lower than 8 ml/kg
– for patients with acute right ventricular dysfunction ("cor pulmonale").
• The PPV measurement has been validated only for adult patients
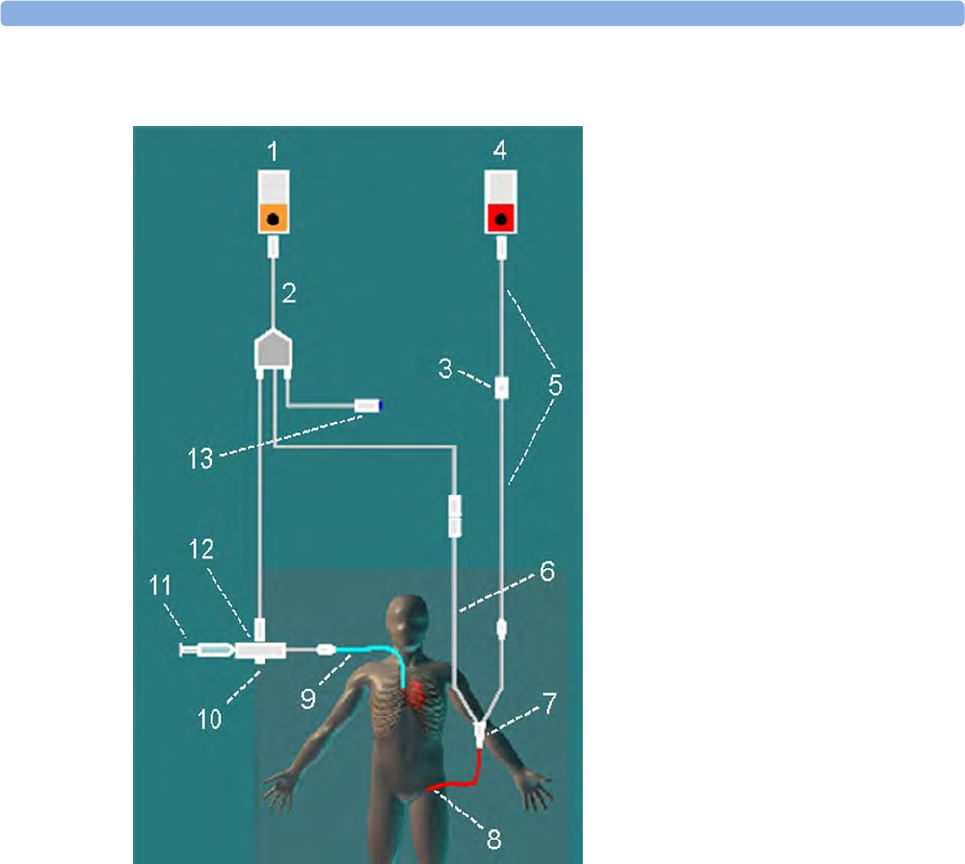
12 Monitoring Cardiac Output
200
Setting Up the PiCCO C.O. Measurement
1Set up the arterial line using the arterial catheter (transpulmonary catheter) and the transducer kit
from PULSION Medical Systems. It must be placed in one of the bigger systemic arteries, for
example, the femoral or the axillary artery. You must use the approved catheters and puncture
locations.
2Set up the central venous line.
3Connect the injectate temperature probe housing to the venous line.
4Plug the C.O. interface cable into the C.O. module or measurement extension module and connect
the following devices to the C.O. interface cable:
– Injectate temperature probe
– Thermistor connector
– Remote start switch (if used).
Follow your hospital standards to avoid unintentional extraction of the C.O. catheter. Secure the
cable using the mounting clip shipped with each C.O. interface cable. You may also find it helpful
to loop the C.O. interface cable, tape the loop, and attach it to the undersheet of the patient's bed
using a safety pin.
1C.O.Module
2 C.O. Interface Cable
3 PULSION Pressure Transducer
4 Press Module
5 Pressure Adapter Cable
6 Thermistor Connection Cable
7 Thermistor Connection
8 PULSION Arterial Catheter
9CVP Line
10 Injectate Temperature Probe
Housing
11 Injectate Syringe
12 Injectate Temperature Probe
13 Remote Switch

12 Monitoring Cardiac Output
201
5If you are measuring CCO, set up the pressure measurement now. The CCO measurement requires
a minimally dampened invasive pressure setup. You must ensure that there are no air bubbles in
the pressure line or dome and use only specified accessories.
6Check that the correct measurement method is selected.
If a catheter is already connected to the Cardiac Output Interface Cable, the monitor automatically
recognizes the method used. If not, in the Setup C.O. menu, select Method and then select
Transpulmnry.
7Check that you are using the correct probe - the M1646. This is the only probe supported for use;
it can be used with room temperature injectate or with cold injectate.
8Check that the correct arterial catheter constant is selected.
If the catheter is recognized by the monitor, the catheter constant is automatically displayed and
cannot be changed manually. If it is not recognized, in the procedure window, select CathCt and
use the pop-up keypad to enter the correct value. The catheter constant is usually written either on
the catheter or on the catheter packaging.
9Make sure that the injectate volume setting matches the injectate volume you will use. To change
the volume, in the procedure window, select InjVol and select the correct injectate volume from
the pop-up list.
If there is a problem with the volume or temperature you have chosen, the monitor will issue a
curve alert message to inform you of this.
10 If you are measuring CCO or CCI, check that the correct pressure source is selected in the Setup
CCO menu. The pressure label under CCO From must match the pressure measured with the
arterial catheter. To change the pressure source, select CCO From to call up a list of available
pressure labels and select the correct label.
11 If you are measuring CCO or CCI, verify that the correct alarm source is selected in the menu item
Alarms From. To change the alarm source, select Alarms From and choose either CCO or CCI.
Performing PiCCO C.O. Measurements
Always wait for the monitor to indicate readiness for the next step before proceeding.
If you are measuring CCO, all measurements should be conducted within 15 minutes. Older
measurements "expire" for CCO calibration.
1Enter the procedure window.
2When you see the message Ready for new measurement, start the measurement by selecting the
pop-up key Start C.O. or pressing the Start hardkey on the C.O. module, or pressing the remote
start switch. If the measuring mode is set to Auto the Start C.O. key will also enable the automatic
start of consecutive measurements.
3When you hear the ready tone and see the message Stable baseline, inject now!, inject the
solution into the CVP catheter.
At the end of the measurement the thermodilution curve, cardiac output, index values, ITBV and
EVLW values and any curve alerts are displayed and a message will appear Wait before starting
new measurement or in Auto mode Prepare for next injection or press Stop.
4When you see the Stable baseline, inject now! message, repeat the procedure until you have
completed the measurements you want to perform. You can perform a maximum of 6
measurements before editing. If you perform more than 6 measurements without rejecting any, the
oldest will automatically be deleted when a 7th curve is stored.
12 Monitoring Cardiac Output
202
Editing PiCCO C.O. Measurements
It is important to identify and reject erroneous trials, as the monitor uses all the measurement trial
values you do not reject to calculate the averaged cardiac output.
1Review the trials. Irregular trials or trials marked with a "?" should be reviewed carefully. Consider
the similarity of the values and the shape of the C.O. curve. A normal C.O. curve has one smooth
peak and returns to the temperature baseline level after the peak.
2Reject unsatisfactory trials: use the Select Trial pop-up key to move between trials, then select the
Accept Reject pop-up key to accept or reject trials. If you are using a touch screen you can accept
or reject trials directly by tipping on the trial curve. Discard conspicuously different values. The
background of rejected trials is red and the background of accepted trials is green. The monitor
recalculates the average values after you reject or accept trials.
If all values are different from each other, there may be true hemodynamic instability caused, for
example, by severe cardiac arrhythmia.
Saving and Calibrating PiCCO C.O. Measurements
When you have finished editing the trials, you must save the results. This closes the measurement
series, sends the average C.O. numeric to be displayed on the main screen, and stores the averaged
values in the trends and calculations databases.
Before the monitor can calculate CCO, you must calibrate the measurement. You should also calibrate
CCO every eight hours, or if the hemodynamic condition of the patient changes consistently in the
same direction over 15 minutes, or if there are large or sudden changes in the patient's condition.
The monitor only uses C.O. measurements from within the last 15 minutes for calibrating CCO.
To save and calibrate,
• In the procedure window, select the pop-up key SaveC.O. &Cal CCO to use the averaged
C.O. value to calibrate Continuous Cardiac Output (CCO).
Your monitor may be configured to have two separate pop-up keys, Save C.O. and Cal CCO, instead
of the combined SaveC.O. &Cal CCO.
WARNING
CCO calibration is patient-specific. When the C.O. module or measurement extension module is
plugged in after the patient has changed, make sure that the correct CCO calibration is used. When in
doubt perform a new CCO calibration first.
CCO Calibration Status Indicators
Each measurement trial is tagged with a calibration status indicator next to its trial number. Reflecting
the quality of the pressure signal during the thermodilution measurement, this tag indicates each trial's
validity to be used in a CCO calibration.
12 Monitoring Cardiac Output
203
For a trial to be eligible for calibration, the pressure signal must be continuously available and
undisturbed starting 30 seconds before the first C.O. measurement of the series. Do not zero the
pressure measurement, change the pressure label, or disturb the pressure signal in any other way during
this time.
Measuring C.O. Using the Right Heart
Thermodilution Method
In the right heart thermodilution method, a fluid of known volume and temperature is injected into the
right atrium through the proximal port of a pulmonary artery (PA) (Swan-Ganz) catheter. The injectate
bolus mixes with the blood in the right ventricle and the change in blood temperature is measured with
a thermistor at the distal end of the catheter in the pulmonary artery.
Cal A pressure signal for CCO was available during the measurement (valid for calibration)
?Cal A disturbed pressure signal for CCO was available during the measurement (valid for
calibration)
N/A No adequate pressure signal for CCO was available during the measurement (no valid
calibration data)
Exp This trial is more than 15 minutes older than the most recent trial and has expired for
CCO calibration (no valid calibration data)
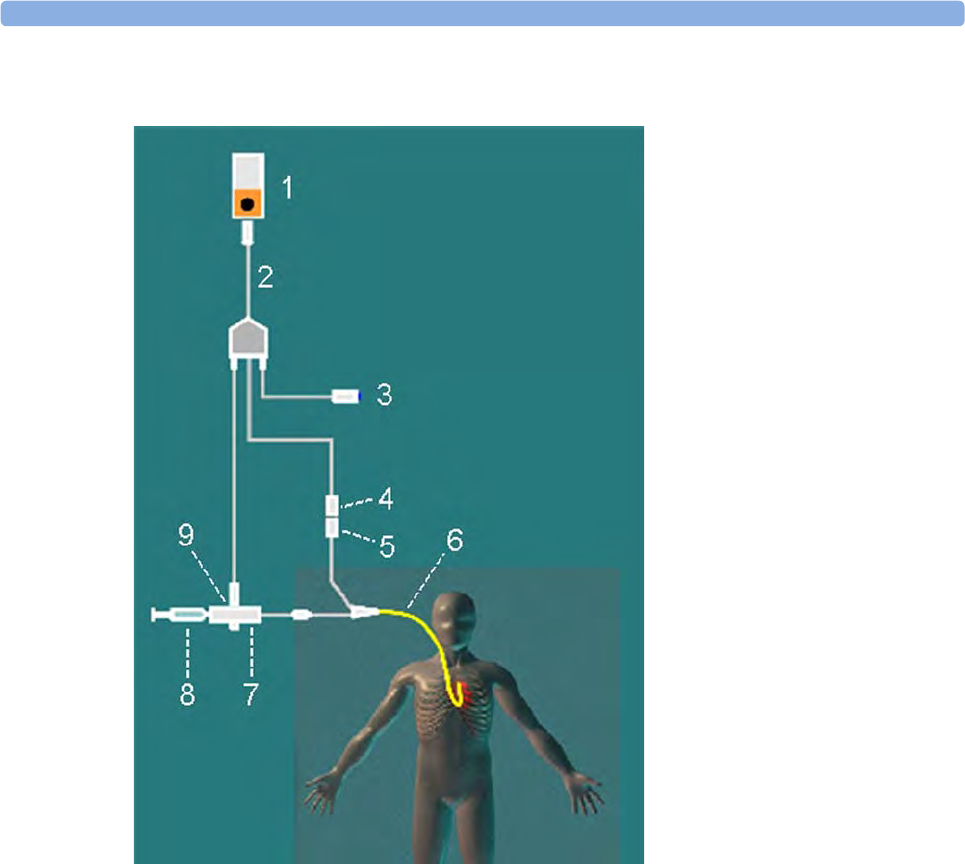
12 Monitoring Cardiac Output
204
Setting up RH C.O. Measurements
1Set up the PA line using a PA catheter.
2Attach the injectate temperature probe housing to the PA line.
3Plug the C.O. interface cable into the C.O. module or measurement extension module and connect
the following devices into the C.O. interface cable:
– injectate temperature probe
– remote start switch (if used).
Follow your hospital standards to avoid unintentional extraction of the C.O. catheter. Secure the
cable using the mounting clip shipped with each C.O. interface cable. You may also find it helpful
to loop the C.O. interface cable, tape the loop, and attach it to the undersheet of the patient's bed
using a safety pin.
4Plug the thermistor connection cable of the PA catheter into the thermistor connector.
5Connect the injectate temperature probe to the injectate temperature probe housing.
6Check that the correct measurement method is selected.
If a catheter is already connected to the Cardiac Output Interface Cable, the monitor automatically
recognizes the method used. If not, in the Setup C.O. menu, select Method and then select Right
Heart.
1C.O.Module
2 C.O. Interface Cable
3 Remote Start Switch
4 Thermistor Connector
5 Thermistor Connection Cable
6 PA Catheter
7 Injectate Temperature Probe
Housing
8 Injectate Syringe
9 Injectate Temperature Probe

12 Monitoring Cardiac Output
205
Ice-Bath Setup for RH Thermodilution C.O. Measurements
If you are using the flow-through method illustrated above, the injectate temperature is measured at
the time of injection by the temperature probe in the injectate temperature probe housing.
If you are using the ice-bath setup, the injectate temperature probe and the injectate are both placed in
an ice-bath and the probe measures the temperature of the contents of the ice bucket.
Setting the Computation Constant
Check that the correct Computation Constant is entered in the procedure window. This can be found
in the documentation supplied with the catheter and is based on the injectate volume, injectate
temperature and catheter type. To change the value, in the procedure window, select Computation
Constant and use the pop-up keypad to enter the correct value.
Performing RH C.O. Measurements
1Enter the procedure window.
2When you see the message Ready for new measurement, select the pop-up key Start C.O.. If the
measuring mode is set to Auto the Start C.O. key will also enable the automatic start of
consecutive measurements.
3When you hear a ready tone and see the message Inject now!, inject the solution into the right
atrial port of the Swan-Ganz catheter. The optimal injection rate is 2.5 ml/second.
At the end of the measurement the thermodilution curve, cardiac output, index values and curve
alerts (if necessary) are displayed and a message will appear Wait before starting new
measurement or in Auto mode Prepare for next injection or press Stop.
4When you see the Inject now! message, repeat the procedure until you have completed the
measurements you want to perform. You can perform a maximum of six measurements before
editing. If you perform more than six measurements without rejecting any, the oldest will
automatically be deleted when a seventh curve is stored.
Editing and Saving RH C.O. Measurements
It is important to identify and reject erroneous measurements (called "trials"), as the monitor uses all
the measurement trial values you do not reject to calculate the averaged cardiac output.
1Review the trials. Irregular trials or trials marked with a "?" should be reviewed carefully. Consider
the similarity of the values and the shape of the C.O. curve. A normal C.O. curve has one smooth
peak and returns to the temperature baseline level after the peak.
2Reject unsatisfactory trials: use the Select Trial pop-up key to move between trials, then select the
Accept Reject pop-up key to accept or reject trials. If you are using a touch screen you can accept
or reject trials directly by tipping on the trial curve. Discard conspicuously different values. The
background of rejected trials is red and the background of accepted trials is green. The monitor
recalculates the average values after you reject or accept trials.
If all values are different from each other, there may be true hemodynamic instability caused, for
example, by severe cardiac arrhythmia.
3Save average C.O. values. To close a measurement series, you must save the average values by
selecting the pop-up key Save C.O.. This sends the average C.O. numeric to be displayed on the
main screen, and stores the averaged values in the trends and calculations databases.

12 Monitoring Cardiac Output
206
Documenting C.O. Measurements
You can document C.O. measurements on the default printer or recorder.
1In the procedure window, select the pop-up key Print/ Record.
2From the pop-up list, choose:
–Print Results to print the contents of the procedure window
–Record Results to record the contents of the procedure window
–Record Trial to send an individual trial curve to the recorder.
C.O. Injectate Guidelines
The greater the injectate volume and the colder the temperature, the more accurate the measurement.
Reduced injectate volume or higher injectate temperature may reduce the specified accuracy.
For adult patients, to ensure the greatest measurement accuracy, use a cold injectate (< 8°C) of 10 ml
volume, if not contra-indicated by the patient's condition. Your choice of injectate volume should be
based on the injectate temperature and the patient's cardiac output.
Guidelines for Right Heart Thermodilution C.O. Injectate
If you are using the right heart thermodilution method, the use of injectate with a temperature less than
8°C lower than the blood temperature may cause incorrect values for the thermodilution.
Guidelines for PiCCO C.O. Injectate
If you are using the PiCCO method, the use of injectate with a temperature that is not at least 12°C
lower than the blood temperature may cause incorrect values for the thermodilution and CCO
calibration.
Injectate Volume, Patient Weight and ETVI Values (PiCCO Only)
When deciding on an injectate volume and temperature, you must consider your patient's weight and
extra-vascular thermal volume index (ETVI).
High ETVI
The dilution of injectate is influenced by extravascular tissue and fluid. The accuracy of the PiCCO
method may be reduced in patients with high extra-vascular thermal volume index (ETVI) values. Use
the table below as a guide in selecting the correct injectate temperature. As shown in the table, if your
patient has an ETVI > 10, you must use cold injectate.
Weight
Use the table below as a guide in choosing an injectate volume appropriate for the patient weight.
12 Monitoring Cardiac Output
207
C.O./CCO Curve Alert Messages
After each measurement trial, the monitor analyzes the thermodilution curve. If the curve appears
abnormal, a curve alert message appears in the procedure window. A question mark symbol ("?") may
appear next to the cardiac output numeric if any of these messages appear. The curve alert messages
are not error messages and do not necessarily mean that the measured values are invalid.
Patient
Weight
Cold Injectate Room Temperature Injectate
ETVI < 10 ETVI ≥ 10 ETVI < 10 ETVI ≥ 10
< 3 kg 2 ml 2 ml 3 ml Use cold injectate
< 10 kg 2 ml 3 ml 3 ml
< 25 kg 3 ml 5 ml 5 ml
< 50 kg 5 ml 10 ml 10 ml
< 100 kg 10 ml 15 ml 15 ml
≥ 100 kg 15 ml 20 ml 20 ml

12 Monitoring Cardiac Output
208
C.O./CCO Curve Alert
Messages
Possible Causes
Tinj off scale The Tinjectate is out of the range -1°C and 30°C. Cool down or
heat up the injectate or change the injectate solution and repeat the
measurement.
Noisy baseline A blood temperature baseline drift that could not be compensated
was detected during the C.O. measurement. Possible causes are:
- Interference may be caused by a ventilator.
- Interference may be caused by an infusion pump: infusions of
significant volume through the central line should be paused at
least 30 seconds before the first thermodilution measurement in a
series and should not recommence until the measurement series is
completed.
- Do not administer injections through the central line during a
measurement series.
- Electrical devices in the vicinity can cause interference: check for
infusion pumps connected to the central catheter, cables parallel to
the thermodilution cable, electrocautery. Make sure all devices are
properly grounded.
- Wait until measurement results are displayed before moving the
patient or catheter.
- Close the stopcock to the injectate syringe after the injection.
- Do not rinse the catheter during measurement, to avoid
temperature fluctuations.
Temperature baseline drift May occur if patient is recovering from open heart surgery, or if
patient was cooled down for surgery and is in the process of
regaining normal body temperature when the measurement is
made.
Small signal, more indicator
required
The peak of the transpulmonary thermodilution curve was below
0.1ºC. Increase injectate volume and/or lower injectate
temperature.
Injectate temperature too high The difference between the blood and injectate temperatures is too
small. The calculated value for C.O. may not be accurate.
High ETVI, use cold injectate
or greater inj. volume
The ETVI value is too high. The accuracy of the transpulmonary
thermodilution measurement may be reduced. Increase injectate
volume and/or lower injectate temperature following the guidelines
given in the section Guidelines for PiCCO C.O. Injectate
(“Guidelines for PiCCO C.O. Injectate” on page 206).
Disturbed injection The injection should be performed quickly and with a steady
pressure. Shaking, unsteady pressure, or injections that take longer
than six seconds may cause this message to appear; you should bear
this in mind if you are using a large injectate volume (> 10 ml).
Check Injectate Temperature
Probe Type
The recorded Tinj signal is uncharacteristic for the M1646 injectate
temperature probe. An incorrect probe type may have been used.
12 Monitoring Cardiac Output
209
If you have followed all of these guidelines, your measurement values should be valid, even if you still
see a curve alert message. Ensure that at least three subsequent measurements within the current series
do no differ by more than 15%. If the difference exceeds 15%, use your clinical judgment to determine
the appropriate intervention.
C.O./CCO Prompt Messages
Prompt messages appear in the procedure window if a C.O. measurement trial must be terminated.
C.O./CCO Warning Messages
Warning messages contain important information about the C.O. measurement.
Unsteady baseline There is a noisy baseline, and thermal baseline drift.
Multiple peaks Caused by faulty injection technique.
Abnormal decay time May be caused by low cardiac output. Calculated value for
C.O. may not be accurate.
Very long curve The decay time of the curve is longer than 15 seconds.
Very short curve Decay time of the curve is less than 0.5 seconds. If there is a noisy
baseline, part of the baseline may have been mistaken for a
thermodilution curve. Calculated value for C.O. may not be
accurate.
Irregular curve Any combination of curve alert messages.
Delayed injection Injection is given more than 15 seconds after Start C.O. is selected.
Calculated value for C.O. may not be accurate.
C.O./CCO Curve Alert
Messages
Possible Causes
C.O./CCO Prompt Messages Possible Causes
Curve below baseline,
measurement terminated
May be caused by thermal baseline drift. No C.O. value
calculated.
Excessive curve height,
measurement terminated
The curve exceeds the upper limit. This may be caused by an
injectate that was too cold. No C.O. value calculated.
Unstable baseline, injection not
recommended!
The baseline is unstable. Wait until the baseline is stable before
injecting. If this does not occur within a reasonable time,
injection is possible but the accuracy of the measured values
may be reduced.
Excessive baseline drift, don't
inject now!
No measurement is possible. Measured values are incorrect.
12 Monitoring Cardiac Output
210
C.O./CCO Safety Information
WARNING
Catheter constant - Make sure that the arterial catheter constant for the measurement is appropriate
to the catheter used.
Computation Constant - Make sure that the computation constant for the measurement is
appropriate to the injectate volume, injectate temperature and catheter type used.
IABP - Do not perform transpulmonary thermodilution measurements on patients undergoing IABP
treatment.
CCO accuracy - Accuracy of the CCO measurement and all the derived values may be influenced by
patients with valve diseases or artificial valves.
C.O. and MRI - Do not use the Cardiac Output Interface Cable in Magnetic Resonance Imaging
(MRI) Applications.
Aortic graft patients - Do not use an arterial catheter in the arteria femoralis when it is contra
indicated, for example, with patients who have an aortic graft.
C.O./CCO Warning Messages Possible Causes
Next measurement erases older
curve
Six curves are stored, this is the maximum possible. If another
measurement is stored, the oldest thermodilution curve will be
erased.
Previous C.O. setup data replaced A C.O. module or measurement extension module has been
plugged in with different C.O. setup data from the previous
data. The new C.O. setup data is read from the new C.O. device,
and replaces the current data. The message disappears when the
Start C.O. pop-up key is pressed.
Verify C.O. setup data A new transpulmonary thermodilution catheter has been
connected to the C.O. Interface Cable.
Check arterial pressure, CCO cal
currently not possible
Poor or invalid pressure signal, for example if pressure was not
zeroed.
Verify the Computation Constant A new catheter has been plugged in, or the computation
constant has been changed and Start C.O. has not been
selected.
Previous Comp. Constant
replaced
A new C.O. module or measurement extension module with a
different computation constant from the current one has been
connected. The new computation constant is read from the new
C.O. device, and replaces the current one. The message
disappears when Start C.O. is selected.
12 Monitoring Cardiac Output
211
CAUTION
During the cardiac output measurement procedure the blood temperature alarms are inactive. This is
indicated by a crossed-out alarm symbol next to the temperature numeric. Making alarms inactive
during this procedure prevents false alarms. The alarms are automatically reactivated when you have
completed the measurement procedure.

12 Monitoring Cardiac Output
212
13
213
13Monitoring Carbon Dioxide
WARNING
Measurements from an MMS extension connected to an X2 are not available when the X2 is running
on its own battery power. They are only available when the X2 is powered by external power: when
connected to a host monitor, to the external power supply (M8023A) or to the Battery Extension
(865297).
Only one CO2 measurement at a time is supported.
Use the CO2 measurement to monitor the patient's respiratory status and to control patient ventilation.
There are two methods for measuring carbon dioxide in the patient's airway:
• Mainstream measurement uses a CO2 sensor attached to an airway adapter directly inserted into
the patient's breathing system. This method is available using the M3014A Capnography
Extension and the M3016A Mainstream CO2 Extension, or the X2 with the optional CO2
measurement.
• Sidestream measurement takes a sample of the respiratory gas with a constant sample flow from
the patient's airway and analyzes it with a remote CO2 sensor built into the measurement system.
Philips offers the sidestream CO2 measurement in the M3014A Capnography Extension or the X2
with the optional CO2 measurement, and the Microstream method of sidestream CO2
measurement in the M3015A/B Microstream CO2 Extension.
Refer to your Gas Module Instructions for Use, if you are using a Gas Module to monitor CO2.
WARNING
Correlation: The etCO2 readings do not always correlate closely with paCO2, especially in neonatal
patients and patients with pulmonary disease, pulmonary embolism or inappropriate ventilation.
Pharmaceuticals in aerosols: Do not measure CO2 in the presence of pharmaceuticals in aerosols.
Explosion Hazard: Do not use in the presence of flammable anesthetics or gases, such as a
flammable anesthetic mixture with air, oxygen or nitrous oxide. Use of the devices in such an
environment may present an explosion hazard.
Failure of operation: if the measurement or a sensor fails to respond as described, do not use it until
the situation has been corrected by qualified personnel.

13 Monitoring Carbon Dioxide
214
Low etCO2 values: Leakages in the breathing system or sampling system may cause the displayed
etCO2 values to be significantly too low. Always connect all components securely and check for leaks
according to standard clinical procedures. Displacement of the nasal or combined nasal oral cannulas
can cause lower than actual etCO2 readings. Even with combined nasal oral cannulas, the etCO2
readings may be slightly lower than actual in patients breathing through the mouth only.
Measurement Principles
For both mainstream and sidestream measurements, the measurement principle is infrared
transmission, where the intensity of infrared light passing the respiratory gas is measured with a photo
detector. As some of the infrared light is absorbed by the CO2 molecules, the amount of light passing
the gas probe depends on the concentration of the measured CO2.
When using a wet ventilator circuit, monitor mainstream CO2 if available, in preference to sidestream
CO2.
The partial pressure is calculated from the gas concentration by multiplying the concentration value
with the ambient pressure.
The measurement provides:
•a CO
2 waveform.
•an end tidal CO
2 (etCO2) value: the CO2 value measured at the end of the expiration phase.
• an inspired minimum CO2 (imCO2): the smallest value measured during inspiration.
• an airway respiration rate (awRR): the number of breaths per minute, calculated from the CO2
waveform.
Depending on the Max Hold setting configured for your monitor, the etCO2 numeric shows either the
highest CO2 value measured within the configured time period (Max Hold set to 10 sec or 20 sec) or
the etCO2 numeric shows breath-to-breath value (Max Hold set to Off).
Measuring CO2 using M3014A or X2
The M3014A Capnography Extension or the X2 with the CO2 option measures partial pressure of
carbon dioxide in a patient's expired gas using the mainstream method or the sidestream method.
The mainstream CO2 measurement can be used, with appropriate accessories, with intubated adult,
pediatric and neonatal patients. The sidestream CO2 measurement can be used, with appropriate
accessories, with intubated and non-intubated adult, pediatric, infant and neonatal patients. With
intubated patients, a sample of the respiratory gas is drawn from the patient's breathing circuit through
an airway adapter and a gas sampling tube. With non-intubated patients, the gas sample is drawn
through a nasal or oral-nasal cannula.
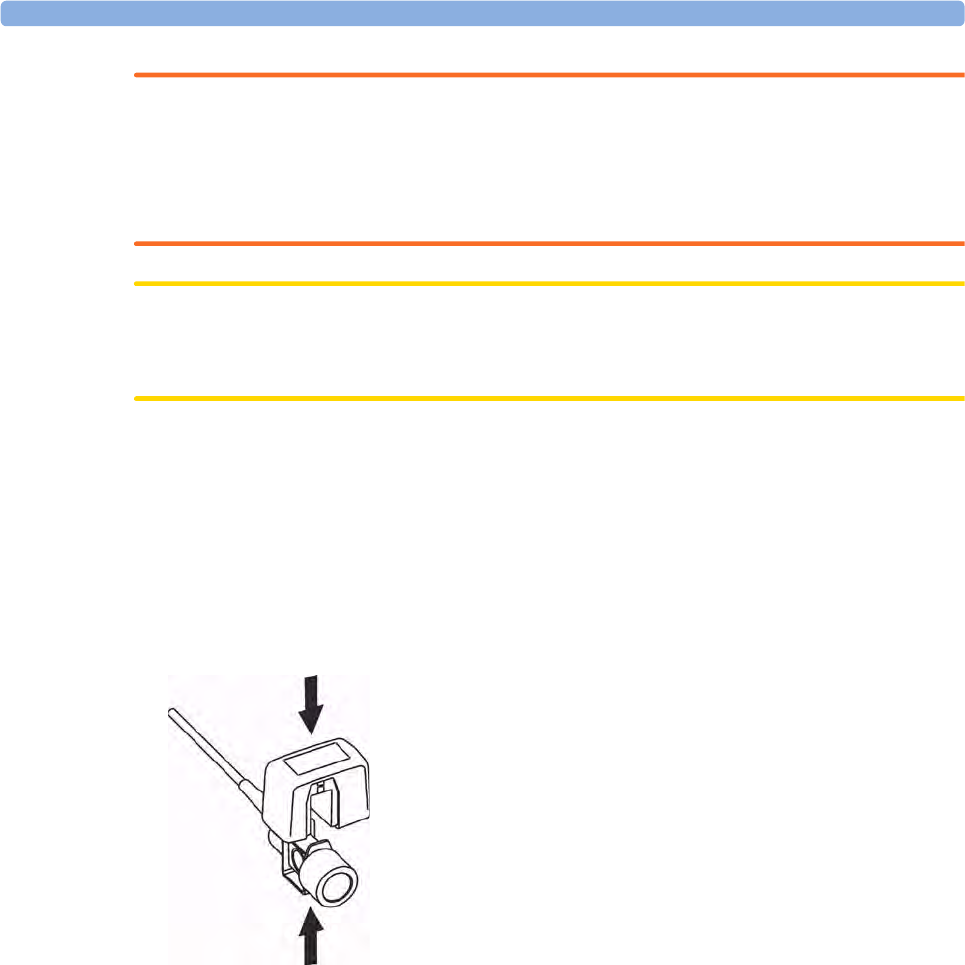
13 Monitoring Carbon Dioxide
215
WARNING
Altitude Setting: The monitor is not equipped with automatic barometric pressure compensation.
Before the CO2 measurement is used for the first time, the altitude must be set to the correct value. An
incorrect altitude setting will result in incorrect CO2 readings. The CO2 readings will typically deviate
5% for every 1000m difference.
CAUTION
Use the CO2 measurement with Philips approved accessories only. Refer to the instructions for use
provided with the accessory.
Preparing to Measure Mainstream CO2
You must perform a zero as described in this procedure each time you use a new airway
adapter.
1Attach the sensor connector to the CO2 connector on the MMS extension, or on the X2 (when
the optional CO2 measurement is integrated).
2Wait 2 minutes, allowing the sensor to reach its operating temperature and a stable thermal
condition.
3Choose the appropriate airway adapter and connect it to the sensor head. The airway adapter clicks
into place when seated correctly. To zero the sensor:
– expose the sensor to room air and keep it away from all sources of CO2 including the
ventilator, the patient's breath and your own.
– in the setup menu for the CO2, select Start Zero Cal.
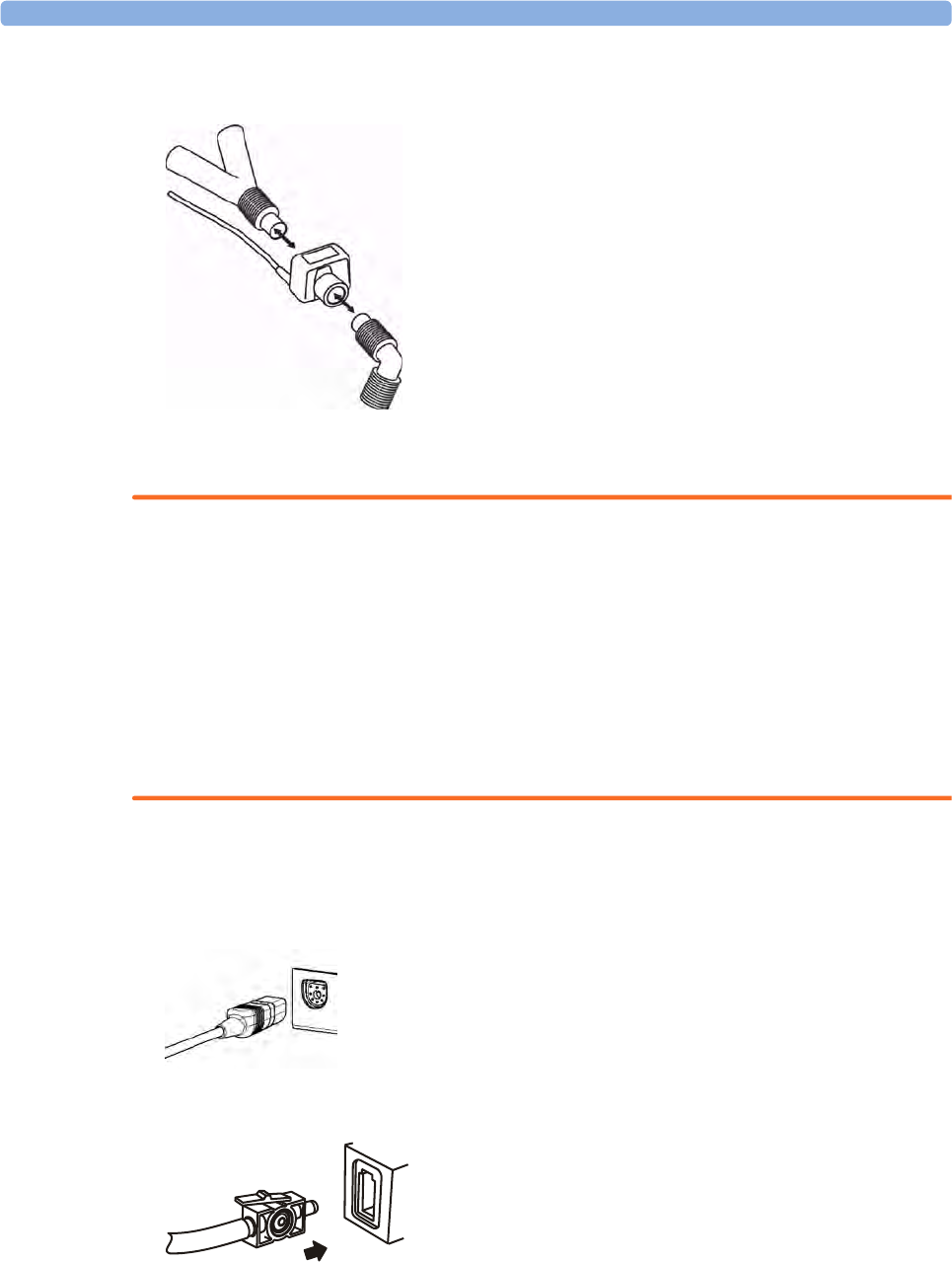
13 Monitoring Carbon Dioxide
216
– When you see the message CO₂ calibration done at <date and time> on the status line, the
zero calibration is finished and you can begin monitoring.
4Install the airway adapter at the proximal end of the circuit between the elbow and the ventilator Y-
section.
WARNING
To prevent stress on the endotracheal tube, support the sensor and airway adapter.
Position sensor cables and tubing carefully to avoid entanglement or potential strangulation. Do not
apply excessive tension to any cable.
Replace the airway adapter, if excessive moisture or secretions are observed in the tubing or if the
CO2 waveform changes unexpectedly without a change in patient status.
To avoid infection, use only sterilized, disinfected or disposable airway adapters.
Inspect the airway adapters prior to use. Do not use if airway adapter appears to have been damaged
or broken. Observe airway adapter color coding for patient population.
Preparing to Measure Sidestream CO2
1Plug the sensor cable into the monitor's CO2 input connector. Allow the sensor two minutes warm
up time
2Connect the cannula, airway adapter, or sample line as appropriate, to the sensor. It will click into
place when seated correctly.
3To zero the sensor:
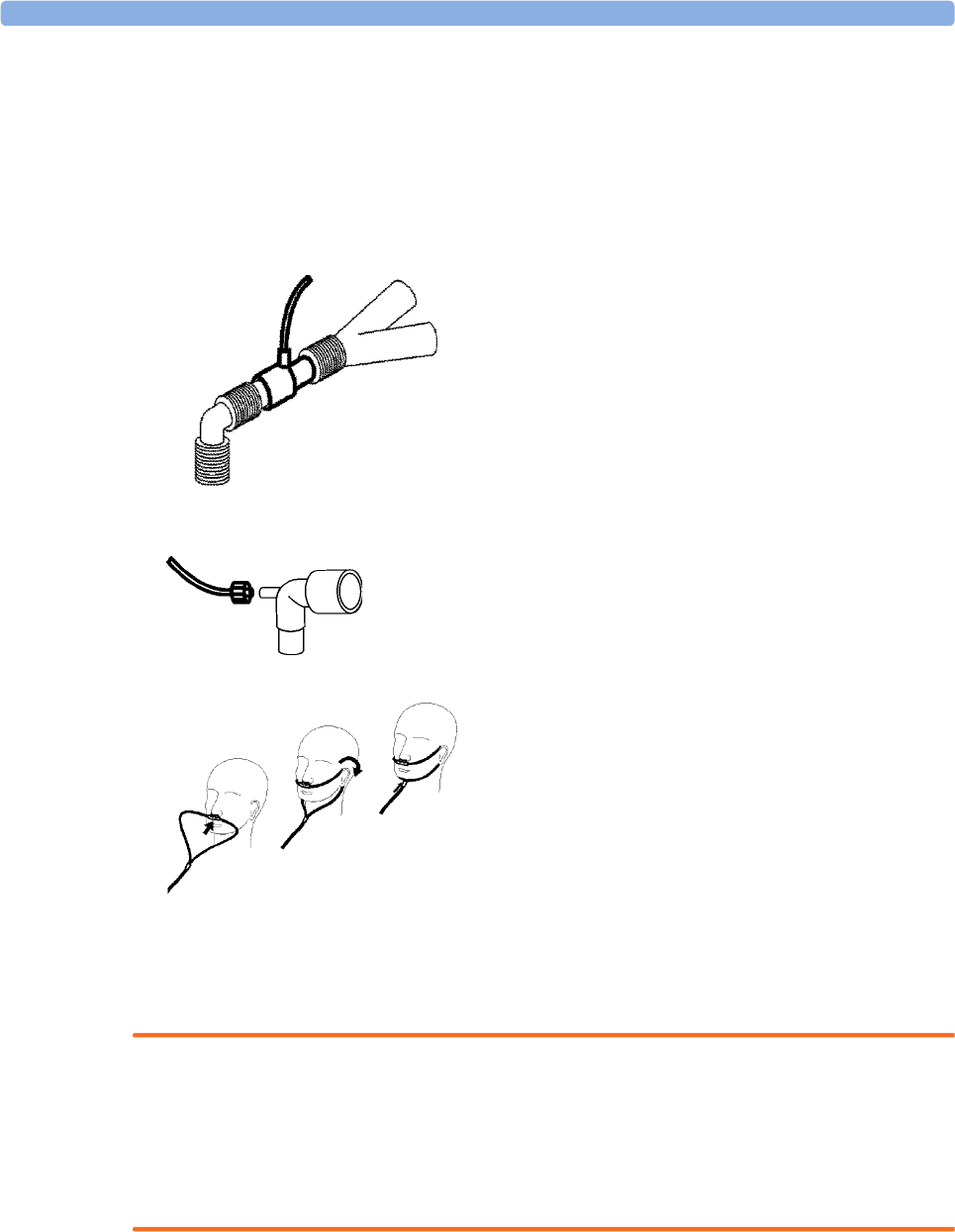
13 Monitoring Carbon Dioxide
217
– expose the sensor to room air and keep it away from all sources of CO2 including the
ventilator, the patient's breath and your own.
– in the setup menu for the CO2, select Start Zero Cal.
– when you see the message CO₂ calibration done at <date and time> on the status line, the
zero calibration is finished and you can begin monitoring.
4For intubated patients requiring an airway adapter: Install the airway adapter at the proximal end of the
circuit between the elbow and the ventilator Y-section.
For intubated patients with an integrated airway adapter in the breathing circuit.: Connect the male luer
connector on the straight sample line to the female port on the airway adapter.
For non-intubated patients: Place the nasal cannula onto the patient.
For patients prone to mouth breathing use an oral-nasal cannula.
For nasal or oral-nasal cannulas with oxygen delivery, place the cannula on the patient as shown then
attach the oxygen supply tubing to the oxygen delivery system and set the prescribed oxygen flow.
WARNING
Always connect the airway adapter to the sensor before inserting the airway adapter into the breathing
circuit. In reverse, always remove the airway adapter from the breathing circuit before removing the
sensor.
Make sure that you do not accidentally connect the luer connector of the gas sample line to an infusion
link or any other links in the patient vicinity.
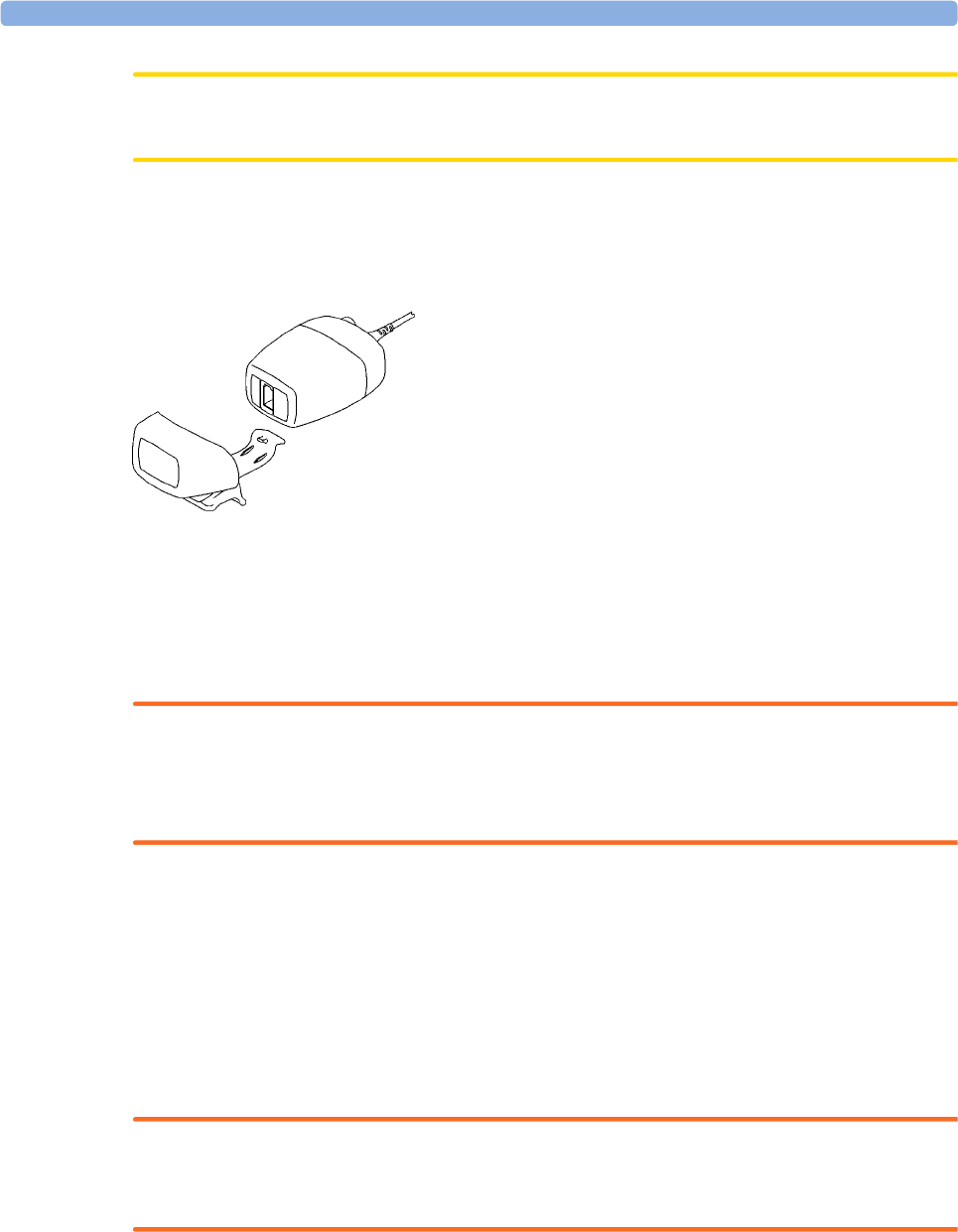
13 Monitoring Carbon Dioxide
218
CAUTION
Always disconnect the cannula, airway adapter or sample line from the sensor when not in use.
Using the Sidestream Sensor Holder
The holder delivered with the sensor can be used to clamp the sensor onto an IV pole or a shelf.
1Push the sensor into the holder until it clicks into position.
2Clamp the holder onto an IV pole, a shelf or another appropriate location.
To remove the sensor from the holder, release the clip and pull the sensor out of the holder.
Removing Exhaust Gases from the System
WARNING
Anesthetics: When using the sidestream CO2 measurement on patients who are receiving or have
recently received anesthetics, connect the outlet to a scavenging system, to avoid exposing medical
staff to anesthetics.
Use an exhaust tube to remove the sample gas to a scavenging system. Attach it to the sidestream
sensor at the outlet connector.
Measuring Mainstream CO2 using M3016A
The M3016A Mainstream CO2 Extension measures partial pressure of carbon dioxide in a patient's
expired gas using the mainstream method. When using the appropriate accessories you can use the
mainstream CO2 measurement with ventilated adults, pediatric and neonatal patients.
WARNING
Infra-red radiation: Do not expose the airway adapter or M1460A transducer to infra-red radiation
during use. This may cause incorrect readings.
Preparing to Measure Mainstream CO2
1Attach the transducer connector to the CO2 connector on the M3016A extension.
13 Monitoring Carbon Dioxide
219
2Wait 20 minutes, allowing the transducer to reach its operating temperature and a stable thermal
condition.
3Perform an accuracy check and then, if necessary, calibrate the transducer.
Checking Transducer Accuracy
WARNING
Check transducer accuracy at least once a week or if you doubt the CO2 readings.
1In Setup CO₂ menu, select Cal. Mode to switch on calibration mode.
2Look at the calibration value displayed in the Setup CO₂ menu next to Start CAL1. Is it the same
as the value on the calstick? If not, calibrate the transducer now.
3Place the transducer on the low cell of the calstick (labeled 0.0 mmHg or "ZERO"). The reading
on the screen should be zero within ±1 mmHg within one minute.
4Place the transducer on the high cell of the calstick. The reading on the screen should be within ±1
mmHg of the value on the calstick within one minute.
5If both readings are in range, you can leave calibration mode and begin monitoring. If either of the
readings is out of range, calibrate the transducer.
Calibrating the Transducer
1Check that the windows on the calstick are clean and clear.
2Place the transducer on one of the calstick cells and select Start CAL1.
3Enter the calibration value printed on the calstick then press Confirm to start calibration.
4When the message CO₂ CAL1 calibration done -- Start CAL2 calibration appears, put the
transducer on the other cell and select Start CAL2 then press Confirm.
5When you see the message CO₂ calibration completed - leave Cal. Mode, calibration is
complete.
6Select Cal. Mode to switch calibration mode off. You cannot monitor in calibration mode.
Attaching and Removing the CO2 Transducer
1Open the latch and place the transducer (B) onto the airway adapter (A). Place the airway adapter
in the patient's breathing circuit between the endotracheal tube and the Y-piece. You may see the

13 Monitoring Carbon Dioxide
220
CO₂ SENS.WARMUP message until the transducer reaches operating temperature. Wait until this
disappears before starting the measurement.
2To remove the transducer from the airway adapter, open the latch and pull out the airway adapter.
WARNING
To prevent stress on the endotracheal tube, support the transducer and airway adapter.
To avoid infection, use only sterilized airway adapters.
Measuring Microstream CO2 using M3015A/B
The M3015A/B Microstream CO2 Extension measures the partial pressure of carbon dioxide in a
patient's expired gas using Microstream technology.
The measurement is equipped with an automatic barometric pressure compensation.
13 Monitoring Carbon Dioxide
221
Preparing to Measure Microstream CO2
Use appropriate accessories for:
• the patient type (adult, pediatric or neonatal),
• the ventilation situation (including humidification)
• the duration - short term use, up to 24 hours (typically OR), or long term use (typically ICU).
All accessories are for single patient use only.
Using Microstream Accessories
The Microstream measurement can be operated with the special Microstream accessories only. Refer
to the instructions for use provided with the accessory.
For intubated patient with non-humidified ventilation, you can use a Microstream FilterLine set. For
humidified ventilation, use a FilterLine H Set.
For non-intubated patients, the gas sample is taken through a Nasal FilterLine, or a Smart CapnoLine
(which is a combined oral-nasal FilterLine). In parallel to the measurement of the CO2, oxygen (O2)
may be delivered to the patient to support gas exchange. This is done by using an O2/CO2 FilterLine,
or a Smart CapnoLine O2 (a combined oral-nasal O2/CO2 FilterLine).
Using the FilterLine and Airway Adapter
WARNING
Make sure that you do not accidentally connect the luer connector of the gas sample line to an infusion
link or any other links in the patient vicinity.
1Attach the female Luer connector to the CO2 inlet connector by pushing the socket cover aside
and screwing the connector into place.
2Check that the FilterLine is not kinked.
3Change the FilterLine if a CO₂ OCCLUSION INOP appears on the monitor or if the readings
become extremely erratic.
Disconnect the FilterLine during suctioning and nebulizing therapies or suppress sampling by turning
off the pump as described in Suppressing Sampling (“Suppressing Sampling (not Mainstream CO2)”
on page 223).
Check the table in the Microstream CO2 Accessories section of the Accessories chapter for typical
usage times for the different Microstream accessories.
CO2 values for non-intubated patients using Microstream accessories will always tend to be lower than
for intubated patients. If values appear extremely low, check whether the patient is breathing through
the mouth or whether one nostril is blocked.
13 Monitoring Carbon Dioxide
222
Removing Exhaust Gases from the System
WARNING
Anesthetics: When using the Microstream CO2 measurement on patients who are receiving or have
recently received anesthetics, connect the outlet to a scavenging system, or to the anesthesia machine/
ventilator, to avoid exposing medical staff to anesthetics.
Use an exhaust tube to remove the sample gas to a scavenging system. Attach it to the MMS Extension
at the outlet connector.
Suppressing Zero Calibration
To prevent an automatic zero calibration from being started in the next five minutes,
•in the Setup CO₂ menu, select No Zero For 5Min, or select the Suppress CO₂ Zero SmartKey, if
configured.
Selecting No Zero For 5Min or selecting the Suppress CO₂ Zero SmartKey again before the timer has
timed out resets the timer to five minutes, unless an AutoZero became due during the previous
suppression.
Setting up all CO2 Measurements
These tasks are common to all CO2 measurements except where otherwise noted.
Adjusting the CO2 Wave Scale
1In the CO₂ Wave menu or the Setup CO₂ menu, select Scale.
2Choose a suitable scale range from the pop-up list.
Setting up CO2 Corrections
Temperature, water vapor in the patient's breath, barometric pressure, and the proportions of O2, N2O
and Helium in the mixture all influence CO2 absorption. If values seem inaccurately high or low, check
that the monitor is using the appropriate corrections.
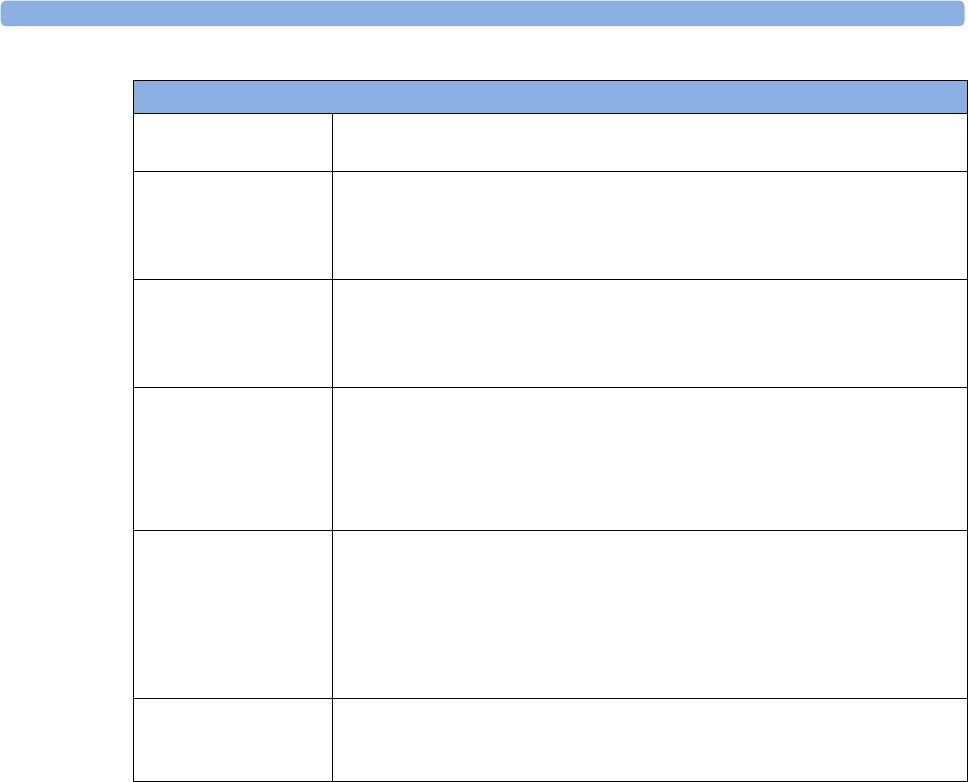
13 Monitoring Carbon Dioxide
223
Suppressing Sampling (not Mainstream CO2)
To temporarily stop sampling, in the Setup CO₂ menu, select Pump 15Min Off or use the CO₂ Pump
Off SmartKey if available.
Selecting Pump 15Min Off again before fifteen minutes have passed resets the timer to fifteen
minutes.
To re-start the pump, in the Setup CO₂ menu, select Pump On.
Changing CO2 Alarms
This refers to CO2 specific alarms. See theAlarms section for general alarm information.
1In the Setup CO₂ menu, select etCO₂ High or imCO₂ High and choose the high alarm limit.
2Select etCO₂ Low and choose the low alarm limit.
Changing the Apnea Alarm Delay
This determines the time limit after which the monitor alarms if the patient stops breathing.
1In the Setup CO₂ menu, select awRR.
2In Setup awRR menu, select Apnea Time.
3Choose the apnea alarm delay time.
Correction
Altitude
(M3014A only)
Altitude is set during installation. The monitor automatically applies an
appropriate correction.
O2
(M3014A only)
In the Setup CO₂ menu, select Oxy. Corr and select a value between 20%
and 100%, the default value is 20%. If you are not measuring the expired O2,
estimate it by subtracting 5% from the inspired O2 then select the nearest
value from the list.
Humidity At installation, the monitor is configured to automatically apply either Body
Temperature Pressure Saturated (BTPS) or Ambient Temperature Pressure
Dry (ATPD). To see which, go to the Setup CO₂ menu, and scroll down to
look at Hum. Corr or Humidity Corr..
N2O
(M3016A mainstream
and M3015A/B
microstream only)
In the Setup CO₂ menu, select N₂O Corr. and turn on or off. If N2O is
present in the ventilation gas mixture, you must turn this on.
If the N2O correction is not available in the Setup CO₂ menu, the CO2
measurement in your MMS Extension does not require N2O correction or it
is setup with Gas Corr. (see below).
Gas
(M3014A only)
In the Setup CO₂ menu, select Gas Corr. and select Helium, N₂O or turn off.
If Helium or N2O is present in the ventilation gas mixture, you must make
the appropriate selection.
If the Gas correction is not available in the Setup CO₂ menu, the CO2
measurement in your MMS Extension does not require N2O or Helium
correction or the N2O correction is setup with N₂O Corr. (see above).
Agent
(M3014A only)
In the Setup CO₂ menu, select Agt. Corr and select the concentration of the
anesthetic agent (between 0.0% and 20.0%). If an anesthetic agent is present
in the ventilation gas mixture, you must select the appropriate concentration.
13 Monitoring Carbon Dioxide
224
WARNING
Safety and effectiveness of the respiration measurement method in the detection of apnea,
particularly the apnea of prematurity and apnea of infancy, has not been established.
Prolonged delay: The selected apnea alarm delay may be prolonged by up to 17 seconds, if an apnea
occurs during the automatic zero process. This applies to the Microstream (M3015A/B) measurement
only.
Deriving Alarms From awRR
1In the Setup CO₂ menu, select awRR.
2In the Setup awRR menu, select Alarms.
3Choose On to derive alarms from the airway respiration signal or Off to disable them.
Changing awRR Alarm Limits
1In the Setup CO₂ menu, select awRR.
2Select High Limit to set the upper alarm limit.
Select Low Limit to set the lower alarm limit.
3Select the appropriate setting.

14
225
14Monitoring Airway Flow,
Volume and Pressure
The M1014A Spirometry Module is designed to be used in combination with Philips-branded airway
flow sensors and combined CO2/airway flow sensors. It produces a real time wave for flow, volume
and pressure of respiratory gases together with numerics for analysis of ventilatory mechanics.
The measurement provides:
• Airway flow, airway volume and airway pressure waveform.
•Numerics for:
– respiratory rate
– tidal volume
– minute volume
– PEEP (positive end-expiratory pressure)
– PIP (peak inspiration pressure)
– dynamic compliance
– airway resistance
• Numerics for: (only visible in SpirometryValues Window, no alarming, no trending)
– peak inspiratory flow
– peak expiratory flow
– negative inspiratory pressure
– mean airway pressure
– plateau pressure numeric
–I:E ratio
The measurement also provides pressure-volume loops, flow-volume loops and pressure-flow loops.
Please see “Respiratory Loops” on page 355 for details on loops.
When using combined CO2/Flow sensors you can also perform mainstream capnography with
intubated adult, pediatric and neonatal patients. See the Monitoring Carbon Dioxide chapter for details
on the CO2 measurement and the Accessories chapter for a list of compatible accessories.
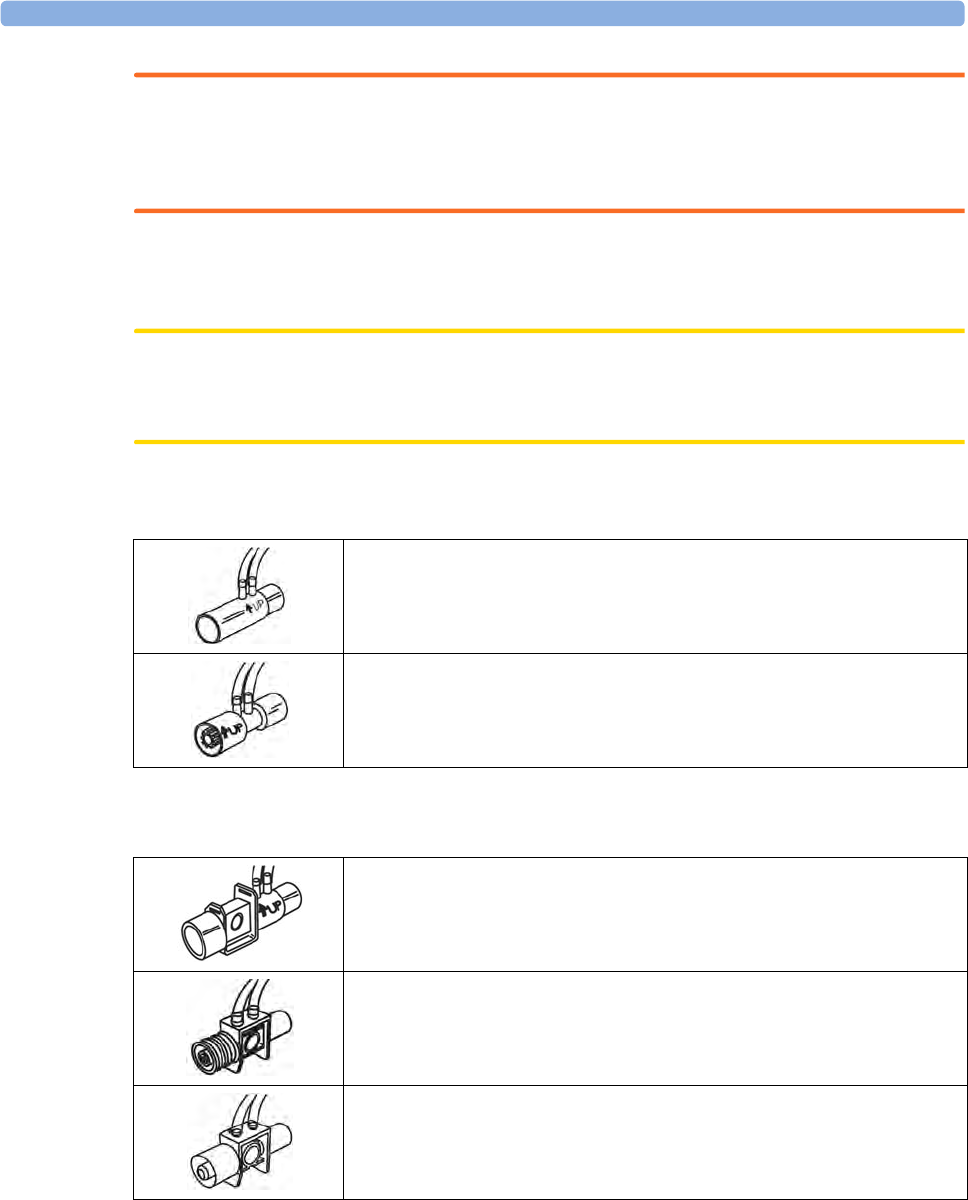
14 Monitoring Airway Flow, Volume and Pressure
226
WARNING
Electrical Shock Hazard: Do not open the module. Contact with exposed electrical components
may cause electrical shock. Always turn off and remove power before cleaning the module. Refer
servicing to qualified service personnel.
Attaching the Flow Sensor
CAUTION
Use the M1014A Spirometry Module with Philips approved accessories only. Refer to the instructions
for use provided with the accessory.
1Select the appropriate flow sensor. Make sure that you are using the correct sensor for the
respective patient category. Otherwise accuracy may be reduced.
You can also use combined CO2/flow sensors. Note that the M3014A Capnography Extension is
required to measure CO2.
1If you are using a combined CO2/Flow sensor, connect it to the CO2 sensor head first. The airway
adapter clicks into place when seated correctly.
2Click the connector into place in the flow sensor receptacle on the monitor before connecting to
the breathing circuit.
Pediatric/Adult Flow Sensor (M2785A). Color: clear
For intubated patients with endotracheal tube diameters >4 mm. Adds
approximately 6.5 cc of deadspace.
Infant/Neonatal Flow Sensor (M2786A) Color: violet
For intubated patients with endotracheal tube diameters ≤ 4mm. Adds less
than 1 cc of deadspace.
Pediatric/Adult Combined CO2/Flow Sensor (M2781A). Color: clear
For intubated patients with endotracheal tube diameters >5.5 mm. Adds
8 cc of deadspace.
Pediatric Combined CO2/Flow Sensor (M2783A): Color: green
For intubated patients with endotracheal tube diameters of 3.5 - 6 mm.
Adds less than 4 cc of deadspace.
Infant/Neonatal Combined CO2/Flow Sensor (M2782A).
Color: violet
For intubated patients with endotracheal tube diameters of 2.5 -4 mm. Adds
less than 1 cc of deadspace.
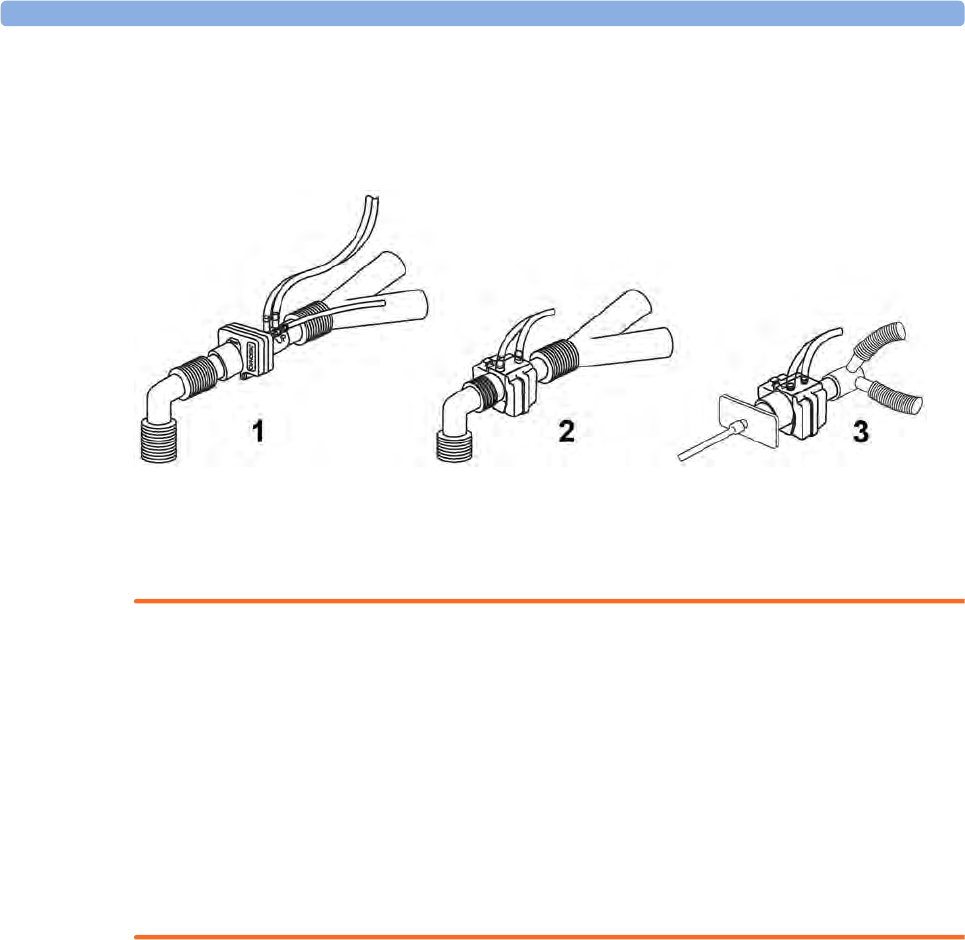
14 Monitoring Airway Flow, Volume and Pressure
227
3Install the flow sensor or the combined CO2/Flow sensor at the proximal end of the breathing
circuit between the elbow and the ventilator Y-piece. Make sure that the spirometry sensor is in a
horizontal position with its tubing pointing upwards. The correct position is also indicated by an
arrow on some of the sensors. (Graphic shows combined CO2/Flow Sensors).
1 Pediatric/adult sensor
2 Pediatric sensor
3 Infant/Neonatal sensor
WARNING
To prevent stress on the endotracheal tube, support the sensor and airway adapter.
Position sensor cables and tubing carefully to avoid entanglement or potential strangulation. Do not
apply excessive tension to any cable or tubing.
Replace the sensor, if excessive moisture or secretions are observed in the tubing and cannot be
removed by a purge cycle.
Reuse poses a patient hazard. Do not disassemble, clean, disinfect or sterilize the sensor.
A system leak may significantly affect readings of flow, volume, pressure and other respiratory
mechanics parameters.
Do not leave the sensor in the patient circuit when not connected to the monitor.
NOTE
• Do NOT place the airway adapter between the endotracheal tube and the elbow (pediatric/adult
circuit), as this may allow patient secretions to block adapter windows.
• The striped tubing of the flow sensor should always be proximal to the patient.
• Position the airway adapter with the spirometry tubing pointing upwards.
• To prevent "rain-out" and moisture from draining into the airway adapter, do NOT place the
airway adapter in a gravity dependent position.
• Periodically check the flow sensor and tubing for excessive moisture or secretion build up.
Perform a purge cycle if droplets are visible within the sensor or tubing. Repeat if necessary. If
purging does not remove the droplets, replace the sensor.
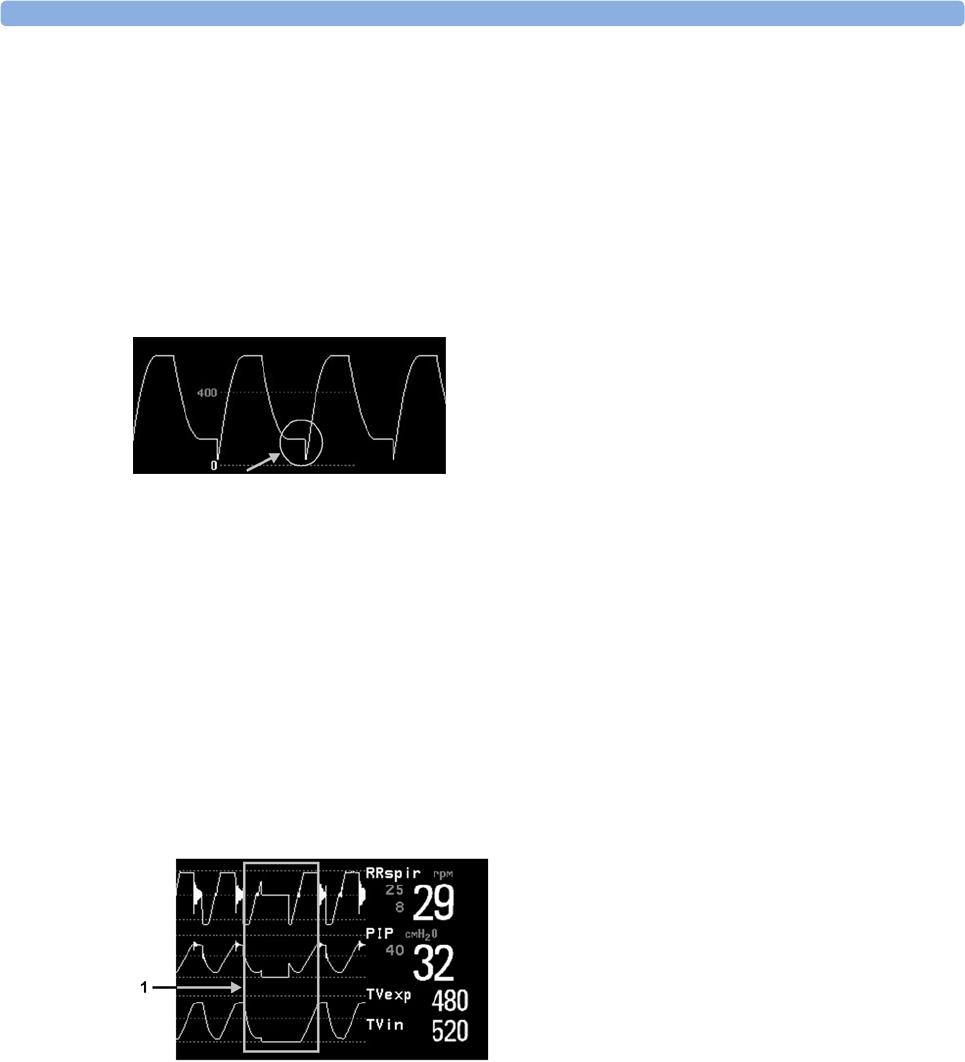
14 Monitoring Airway Flow, Volume and Pressure
228
• For routine performance of airway care, separate the system between the endotracheal tube and
the airway adapter (neonatal circuit), or between the endotracheal tube and elbow (pediatric/adult
circuit). Lavage and suctioning of the airway can then be performed without fluids and mucous
accumulating on the airway adapter windows.
• Measurement values provided by a ventilator may differ significantly from the values provided by
the spirometry module, due to different locations of the flow sensor.
• Incorrect entry of gas compensation parameters (i.e. temperature, gas composition) may reduce
the accuracy of the measured values.
• An abnormal volume waveform as displayed below may be an indicator of an air leak:
In general, if MVexp or TVexp are significantly smaller than MVin or TVin, the tubing should be
checked for leaks.
Zero Calibration
The zero calibration maintains the accuracy of the spirometry waves and numerics by regularly
compensating for drifts within the measurement section. It is performed automatically without user
interaction and takes about 2 seconds to complete. The automatic zero calibration is normally carried
out every ten minutes. During warm-up or when the ambient pressure changes, this interval may be
reduced to two minutes.
During the zero calibration the waveform is flat but the numerics remain on the screen. Typically, a
zero calibration is started at the beginning of a respiration cycle, therefore a waveform may begin
normally and then immediately become flat for the time of the zero calibration.
1 Zero Calibration
Automatic Purging
A double lumen connecting line (tubing) connects the flow sensors to the patient monitor. The
M1014A Spirometry Module includes an automatic and manual purge feature which provides a flush
of room air to keep the sensor tubing free from water condensation and patient secretions. This
feature is available for the adult, pediatric, and neonatal modes. The purge will begin with the
exhalation portion of the ventilator cycle.
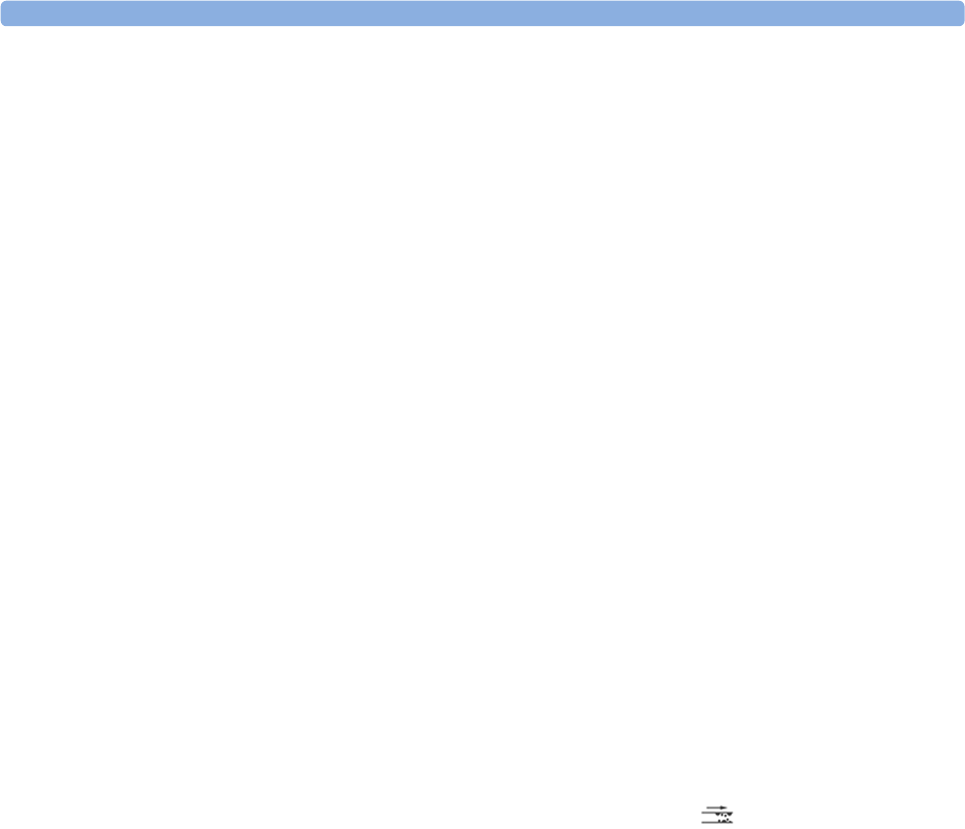
14 Monitoring Airway Flow, Volume and Pressure
229
NOTE
• During the purge cycle the pump will be heard
• If the purge does not sufficiently clear the flow tubing lines, the flow sensor should be replaced
• With each purge cycle, a zero calibration is automatically performed
Adult Mode
The system automatically purges the sensor tubing every ten minutes or less, depending on system
conditions. In adult mode, the system will purge both sides of the line, one at a time, during each purge
cycle. The higher the pressure, the more frequent the purging. This action anticipates increased
moisture migration into the sensor tubing due to the increase in circuit pressure.
Neonatal and Pediatric Modes
The automatic purge cycles used in the neonatal or pediatric mode is fixed at every three minutes
regardless of circuit pressure. Only one side of the sensor tubing will be purged during each purge
cycle.
Unlike the adult purge mode, the neonatal or pediatric purge mode does not use the full force of the
internal pump, but rather pressurizes an internal reservoir which is used for the purge. This minimizes
the pressure delivered to the ventilator circuit, but does deliver a sufficient pressure to purge the sensor
tubing.
Manual Purging
Occasionally, purging may be required in between the automatic purge cycles. The manual purge may
be used as often as needed. Check the orientation of the flow sensor if repeated manual purge cycles
become necessary.
To manually purge, press the Purge button on the module (marked by on international versions of
the module) or select Purge in the Setup Spirometry window to initiate a combined purge and zero
cycle.
Gas Compensation
Temperature and the proportions of individual gases influence the flow measurement. If values seem
inaccurately high or low, check that the monitor is using the appropriate gas compensation. Gas
compensation can be done using either manually entered gas concentrations or gas concentrations
from the gas analyzer.
NOTE
If you unintentionally switch the gas compensation to the incorrect setting, the accuracy of the
measured flow and volume values may be significantly reduced. The tables below show examples of
incorrect gas compensation settings and the resulting inaccuracies:
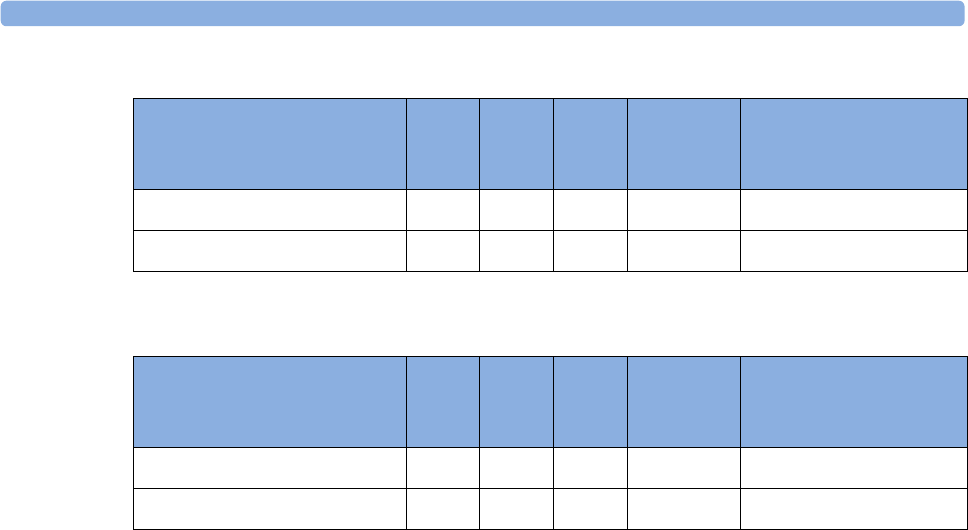
14 Monitoring Airway Flow, Volume and Pressure
230
Incorrect Balance Gas Setting (N2O instead of N2)
Incorrect Agent Percentage Setting
Setting up Spirometry
The following settings can be accessed through the Setup Spirometry menu.
Optimizing Scale Settings
In the Setup Spirometry menu, select Optimize Scales. The scale settings for all three spirometry
waves (AWF, AWP, AWV) will be optimized.
Spirometry Values Window
You can view all spirometry measurement data in the spirometry data window. In the Setup
Spirometry menu, select Show All Values.
Alarms and Alarm Limits
Alarms can be derived from PEEP, PIP, MV and RRspir. In the Setup Spirometry menu you can set
the alarm limits. Please refer to the Alarms chapter of this manual for details on alarm settings.
Changing the Apnea Alarm Delay
This determines the time limit after which the monitor alarms if the patient stops breathing.
1In the Setup Spirometry menu, select RRspir.
2In Setup RRspir menu, select Apnea Time.
3Choose the apnea alarm delay time.
N2O2N2OAgent Difference between
measured and actual
values
Actual Gas Composition 60 40
Gas Compensation Setting 40 60 15%
N2O2N2OAgent Difference between
measured and actual
values
Actual Gas Composition 55 40 5
Gas Compensation Setting 60 40 0 15%
14 Monitoring Airway Flow, Volume and Pressure
231
WARNING
Safety and effectiveness of the respiration measurement method in the detection of apnea,
particularly the apnea of prematurity and apnea of infancy, has not been established.
WARNING
If an apnea occurs during a zero calibration or purge, the time delay between the start of apnea and the
activation of the apnea alarm could be up to 10 seconds plus the configured apnea delay time.
Automatic Alarm Suppression
If the automatic alarm suppression is switched on, all spirometry alarms are suppressed until breathing
activity has been detected. This setting must be made in configuration mode.
Choosing Measured AWV Components
1In the Setup Spirometry menu, select AWV.
2Select MV to choose the measured components for Minute Volume (inspiratory and/or expiratory
or off).
Select TV to choose the measured components for Tidal Volume (inspiratory and/or expiratory or
off).
NOTE
If MV and TV are set to off, there will be no alarming for these parameters.
Setting the Gas Compensation Mode
1In the Setup Spirometry menu, select Gas Compensation.
2Select Mode to choose the Gas Compensation mode:
– select Manual for manually entered gas concentrations or
– select Gas Analyzer for gas concentrations from the gas analyzer.
NOTE
• Gas concentrations from the gas analyzer are only available for Philips gas analyzers, not for
devices connected via a Vuelink/IntelliBridge module.
• If gas concentrations from the gas analyzer are selected but not all data is available, the missing
data is taken from manually entered values. In case of invalid data or no data at all, the INOP
message SPIRO GAS COMPENS? is displayed.
Changing the Type of Balance Gas
1In the Setup Spirometry menu, select Gas Compensation.
2Select Balance Gas to change the type of balance gas.
3Select the appropriate setting (N2 or N2O).

14 Monitoring Airway Flow, Volume and Pressure
232
Changing the Concentration of Inspired O2 and the Inspired Agents
1In the Setup Spirometry menu, select Gas Compensation.
2Select Inspired O₂ to change the concentration of inspired O2.
Select Inspired Agent to change the concentration of the inspired agent(s).
3Select the appropriate setting.
Changing the Temperature of the Inspired Gas
Depending on the type of ventilator environment (e.g. if you are using a Heat Moisture Exchanger)
you may want to change the temperature setting of the inspired gas:
1In the Setup Spirometry menu, select Gas Compensation.
2Select Inspired Temp to change the temperature of the inspired gas.
3Select the appropriate temperature setting.
NOTE
Changing the temperature setting unintentionally will result in approximately 3% reduced accuracy per
10°C (18°F) temperature setting change.
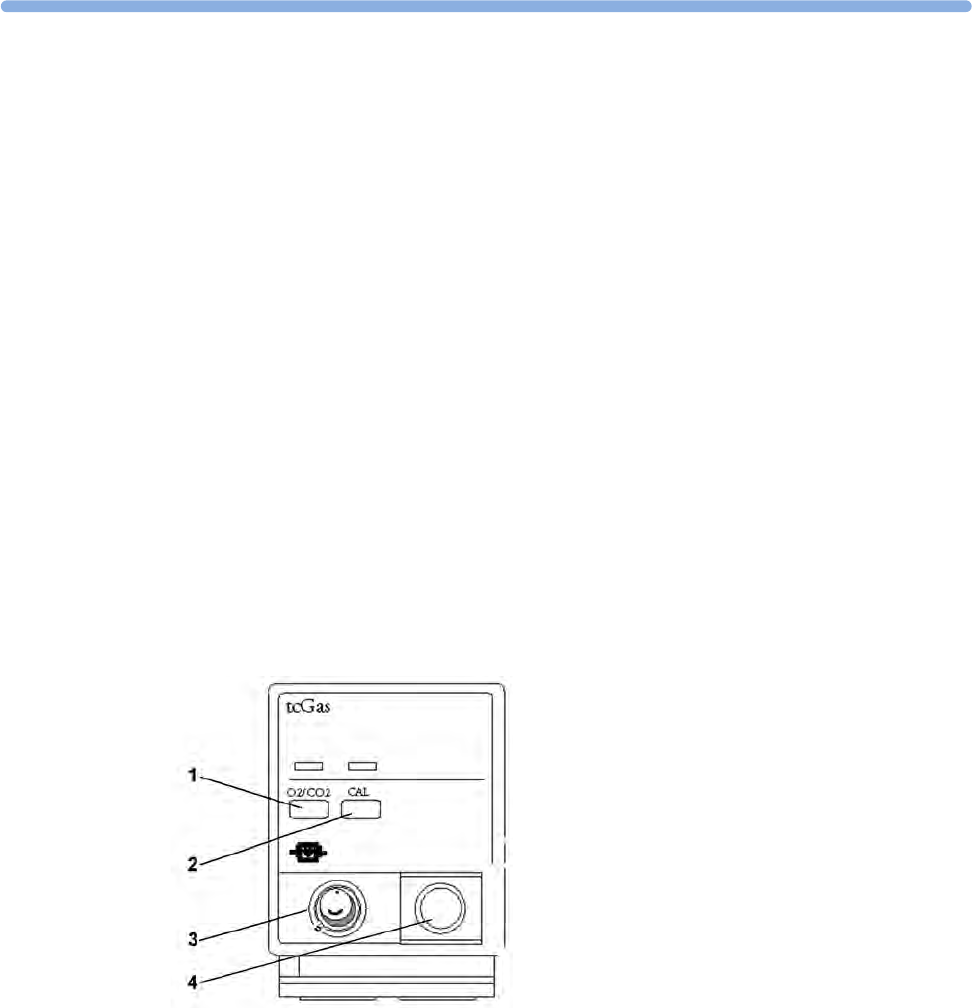
15
233
15Monitoring tcGas
The tcGas module measures the partial pressure of the oxygen and carbon dioxide that diffuses
through the skin, thereby providing a measure of these gases in the capillary blood.
The monitor's settings for altitude and barometric pressure influence the measurement. The tcpO2/
tcpCO2 measurement is valid for an infant patient not under gas anesthesia. Anesthetic agents, such as
halothane, can cause incorrect or drifting readings.
Transcutaneous measurements cannot replace arterial blood gas monitoring. However, you can use
transcutaneous monitoring to reduce the frequency of arterial sampling. The values at tissue level will
not be the same as those measured arterially because the measurement is transcutaneous. They
correlate with (track closely) the arterial values. For example, a drop in transcutaneous values usually
indicates a corresponding drop in arterial values.
Transcutaneous values will not always correlate with blood samples taken from the capillary blood of
the heel (heelsticks or astrups).
Identifying tcGas Module Components
Setting the tcGas Sensor Temperature
1In the Setup tcGas menu, select Transducer Temp..
1Press to enter Setup tcGas menu
2Press to start calibration
3Calibration chamber
4Transducer connector
15 Monitoring tcGas
234
2Choose a temperature value appropriate for your patient's age, weight and physical condition in
accordance with your hospital policy.
Usually, a higher transducer temperature gives a better correlation and a quicker response time.
However, higher temperatures also increase the risk of skin burns. Most physicians prefer a
temperature between 42°C (107°F) and 44°C (111°F), and a site time of four hours or less. Usually,
the higher the transducer temperature, the less the site time should be. Whenever you change the
temperature setting, the monitor forces you to make a new calibration.
Using the tcGas Site Timer
Availability and behavior of the site timer depend on your monitor's configuration.
WARNING
Prolonged continuous monitoring may increase the risk of undesirable changes in skin characteristics,
such as irritation, reddening, blistering or burns. If the site timer is disabled, the transducer will heat
indefinitely while on a patient. Change the site regularly, in accordance with medical procedures in your
hospital.
Setting the tcGas Site Timer
The site timer helps reduce the risk of skin burn by ensuring that the transducer is used at one site for
no longer than a predefined period. It reminds you when this period expires.
1In the Setup tcGas menu, select Site Time.
2Choose the time you want the transducer to remain on the measurement site. The optimum time
depends on the transducer temperature and your patient's skin sensitivity.
The site timer starts automatically when you remove the calibrated transducer from the calibration
chamber. If you return the transducer to the chamber and then remove it again, the site time continues
to count down the remaining time; it does not start a new time period. The time remaining before the
site timer expires appears in the status line which is visible as long as the Setup tcGas menu is open.
When the time expires, the monitor sounds a tone and a displays a change site INOP. The monitor
either switches off the transducer heating or continues monitoring, depending on its configuration.
Although you can reuse the transducer for up to two hours after the heating is switched off, without
making a new calibration, you are recommended to recalibrate before applying it to a patient. After two
hours without heat, you must recalibrate.
During the initial few minutes of use, the monitor eliminates false alarms by temporarily suppressing
tcGas alarms. It displays the <tcGas Label> STABILIZING INOP. After you apply the transducer to
the skin, the instrument reading slowly assumes a steady value. The reading stabilizes when the
measurement site is warm and local hyperemization is complete. This takes 10 to 20 minutes for the
tcpO2 reading and three to seven minutes for tcpCO2.
Restarting the tcGas SiteTimer
To restart the site timer without recalibration (for example, after the site time has elapsed):
1In the Setup tcGas menu, select Site Time.
2Enter and confirm your desired time.

15 Monitoring tcGas
235
Disabling the tcGas Site Timer
Depending on your monitor's configuration, you might be able to disable the site timer. Remember,
this means that the transducer heats indefinitely while on a patient.
1In Setup tcGas menu, select Site Timer and switch this to Disabled.
2Select the Confirm pop-up key.
Setting the tcGas Barometric Pressure
Altitude and barometric pressure affect tcGas values. The monitor derives barometric pressure from
its altitude setting. If you want to set the true barometric pressure you must do this before starting a
calibration - changes after calibration do not influence tcGas values. The monitor remembers this
pressure setting until you enter a new one.
1In the Setup tcGas menu, select Ambient Pressure.
2Enter the current barometric pressure reading indicated by your barometer.
3Select the Confirm pop-up key.
Remembraning the tcGas Transducer
Follow the instructions supplied with the transducer.
New/Dried Out Transducers
Remembrane all new or dried out transducers twice before using. After the first remembraning, unplug
the transducer from the module and leave it for 24 hours with the cap on. Remembrane again before
calibrating.
Storing tcGas Transducers
If you need to store a sensor for more than 24 hours, protect it for up to 28 days by putting two drops
of electrolyte solution into the cap. Screw the cap on the sensor. Remembrane if it dries out or after 28
days.
Calibrating the tcGas Transducer
You can use either a Philips (15210B) or a Radiometer TCC3 calibration unit and a gas cylinder whose
pressure indicator is above the 'out-of-gas' zone (black on 15210B, red on TCC3). To maintain
accuracy, it is recommended to calibrate the transducer every four hours, even if the monitor does not
prompt you to do so. You MUST calibrate when:
• you remembrane the transducer
• you change the transducer heat setting
• you doubt the measurement accuracy
• you start a new monitoring period or use a new site
• the monitor displays the Calibration required INOP message.
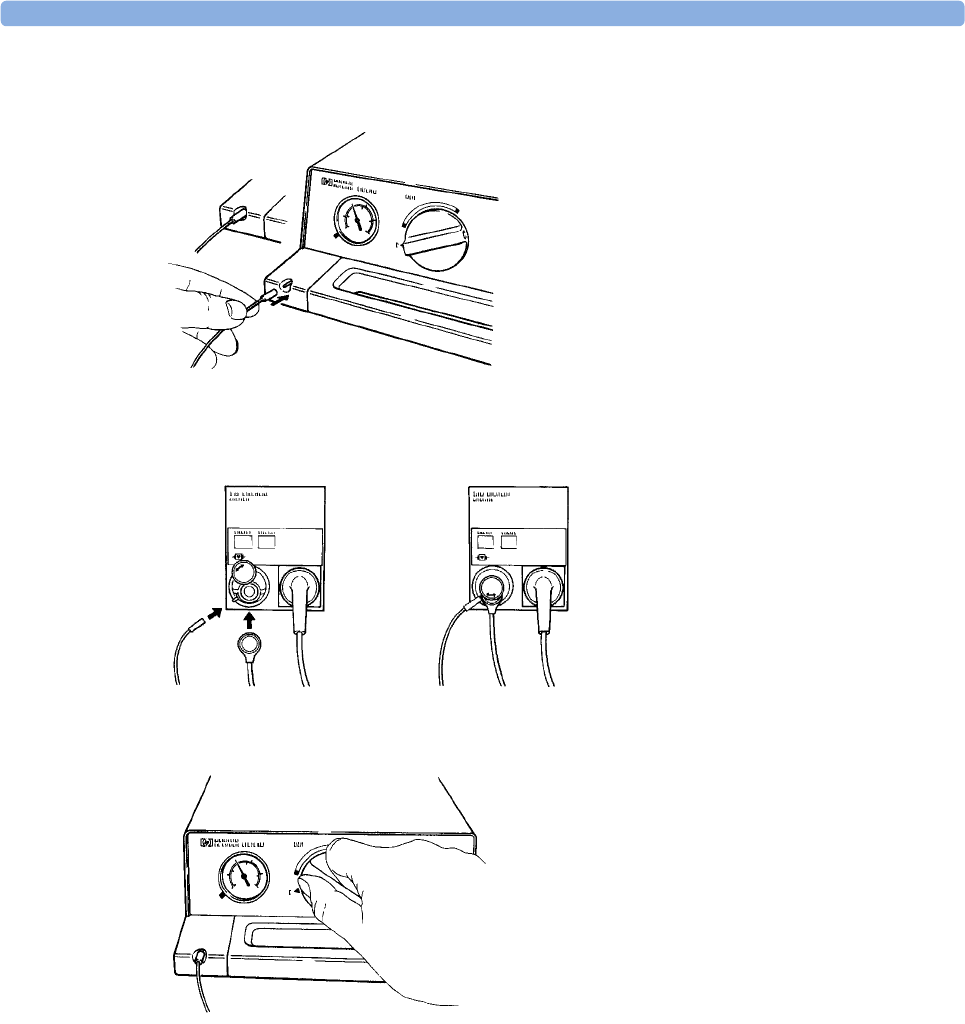
15 Monitoring tcGas
236
1Connect the calibration unit to the inlet on the side of the module's calibration chamber using the
recommended gas tubing. Different tubing will cause inaccurate measurements.
2Plug the transducer cable into the module. Swing the calibration chamber cover open and insert
the transducer into the chamber. Close the cover to secure the transducer. Set the transducer
temperature at the monitor now.
3On the 15210B calibration unit, turn the timer control clockwise as far as you can. On the
Radiometer calibration unit, press the button with the green arrow once.
4Press CAL on the module until the light above the key comes on and wait (three - 20 minutes) for
the completion message to appear on the monitor. Alternatively, in the Setup tcGas menu, select
StartCalibration. To save gas on 15210B, if the timer control dial is not in the start position when
the monitor displays the completion message, turn the dial counter-clockwise to the start position.
For TCC3, if the green light is still flashing when INOP <tcGas Label> CAL RUNNING
disappears, press the green arrow button again.
Calibration Failure
If calibration fails, the monitor displays <tcGas Label> transducer or cal. unit malfunction and the
<tcGas Label> CAL FAILED INOP for the measurement.
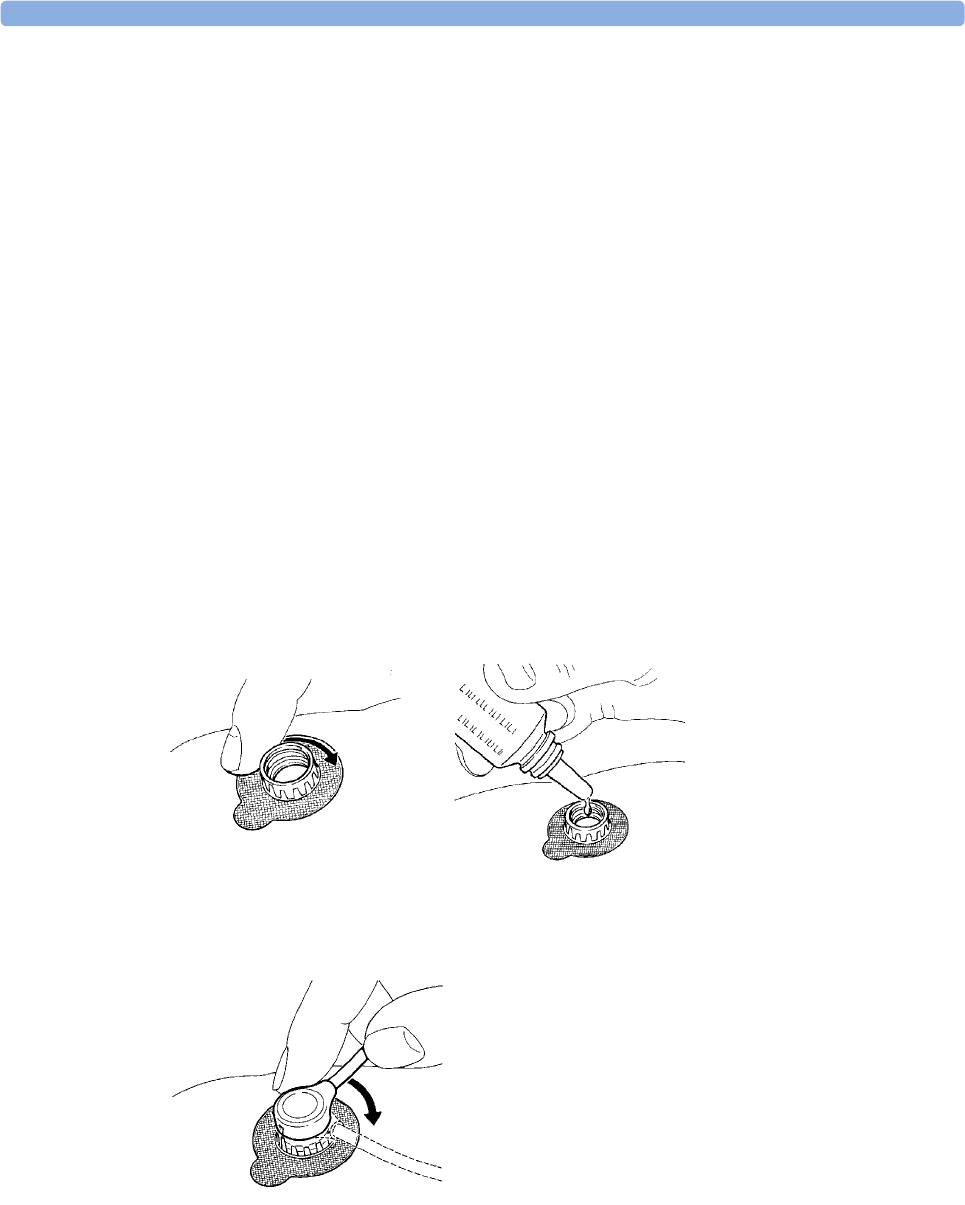
15 Monitoring tcGas
237
Troubleshooting tcGas Calibration
Perform each of the following steps, in order, until calibration is successful.
1Check the calibration unit, then recalibrate, remembering to turn on the gas supply on the
calibration unit. If the pressure indicator reading is in the out of gas zone, there is insufficient gas
in the cylinder. Connect the gas tubing firmly to the calibration unit and to the module's
calibration chamber.
2If Step 1 fails, check whether you need to activate the transducer (necessary if the electrolyte has
dried out or if you have a new transducer). Remembrane the transducer, removing the old
membranes, and cleaning the transducer head thoroughly.
3Calibrate a second time.
4If Step 2 is unsuccessful, calibrate again. This calibration may be required to stabilize the
electrochemical system in the transducer.
5Only if the above steps are unsuccessful (you have activated and remembraned the transducer and
calibration has still failed twice), replace the transducer.
Applying the tcGas Transducer
1Peel protection film from fixation ring. Using a finger, press the sticky side of the ring on to clean,
dry skin. Press around the outside to ensure a good seal. Apply three to five drops of contact fluid
in the ring's center. Remove transducer from chamber.
2Align the arrow on the transducer with the tab on the ring and fasten by turning a quarter-turn
clockwise. Wait 10-20 minutes for readings to stabilize.
3Apply the transducer as soon as possible after you see the message indicating that calibration is
complete. If you wait longer than 30 minutes, the heat supply to the transducer switches off to
prevent the electrolyte from drying out and a new calibration is necessary.
Optimize the measurement by selecting a site with high capillary density and blood flow, thin
epidermis and no cardiovascular disorders. Most physicians use the abdomen, chest and back.
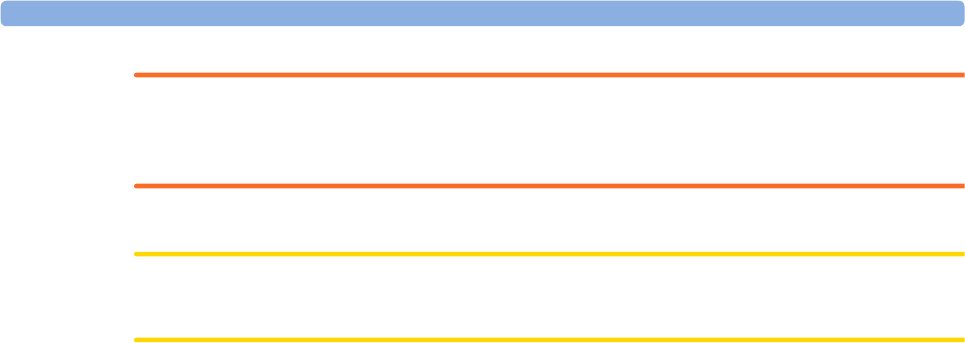
15 Monitoring tcGas
238
WARNING
You must either remove the transducer before defibrillating, or remembrane and calibrate the
transducer after defibrillating.
CAUTION
To avoid transducer damage, remove it from the patient during high frequency surgical procedures.
Selecting the tcGas HeatPowerDisplay Mode
The heat power display gives an indication of the skin's perfusion below the transducer and of the
transducer's contact with the skin. If the transducer loses contact, the heat power value drops
significantly. When perfusion is poor you need less heat power to maintain the transducer temperature.
•In the Setup tcGas menu, select HeatPowerDisplay and then Relative or Absolute. Choose
Relative when the skin temperature is stable (the <tcGas Label> STABILIZING INOP disappears).
This indicates subsequent changes in the relative heat power (and therefore changes in perfusion
or transducer contact) since the last zeroing.
Zeroing the tcGas Relative Heat Power
When you start a calibration, the HeatPowerDisplay is set to Absolute. When you switch to Relative,
it automatically zeros. Zero again if you change application site.
Finishing tcGas Monitoring
Replace the transducer in the calibration chamber.
When changing the application site after a measuring period, some users leave the fixation rings in
position to allow them to quickly move the transducer from site to site. Always unscrew the transducer
from the fixation ring before removing the fixation ring from the skin.
TcGas Corrections
Transcutaneous pCO2 values tend to be higher than arterial values due to the metabolic processes of
the skin and the effect of heating on the blood under the transducer. Depending on your monitor's
configuration, one or both of these corrections may automatically apply.
Temperature Correction for tcpCO2
The transducer temperature causes an increase in partial CO2 pressure. Your monitor may be
configured to correct this.
•In the Setup tcGas menu, look at the menu item CO₂ Correction. If correction is enabled, it is set
to On.

15 Monitoring tcGas
239
Metabolism Correction for tcpCO2
CO2 production in the epidermis increases the CO2 value. Your monitor may be configured to
automatically deduct a metabolism factor (only applies when CO₂ Correction is on).
In the Setup tcGas menu, look at the value shown for the menu item MetabolismFactor. This is
deducted from the CO2 value.

15 Monitoring tcGas
240
16
241
16Monitoring Intravascular
Oxygen Saturation
Depending on the probe or catheter used and the measurement location, the two modules, M1011A
and M1021A, measure the central venous oxygen saturation or mixed venous oxygen saturation
continuously and invasively.
The two modules can be differentiated by their size and their labeling. The M1011A is a single-width
module (narrow) and is labeled SO2. The M1021A is a double-width module (wide) and is labeled
SvO2.
WARNING
Injected dyes, such as methylene blue, or intravascular dyshemoglobin may lead to inaccurate
measurements.
Do not monitor oxygen saturation during infusion of I.V. fat emulsion or other turbid substances
through the distal lumen of the OptiCath catheter. These liquids might temporarily modify the blood
scattering and absorption characteristics at the catheter tip. This interferes with the optical
measurement of oxygen saturation. After infusion is complete, you can again monitor oxygen
saturation accurately.
During injection of the bolus for thermodilution cardiac output measurements, the SvO2
measurement might be disturbed.
Explosion Hazard: Do not use in the presence of flammable anesthetics or gases, such as a
flammable anesthetic mixture with air, oxygen or nitrous oxide. Use of the devices in such an
environment may present an explosion hazard.
1 M1011A
2 M1021A
16 Monitoring Intravascular Oxygen Saturation
242
Do not use probes/catheters when they, or the packaging, are damaged.
Always select the correct label for the measurement location and the catheter/probe in use. This is
especially important when Protocol Watch is in use, to ensure that the correct limits are used for the
criteria applied.
CAUTION
Use the modules with Philips approved accessories only. Refer to the instructions for use provided
with the accessory.
Selecting a Measurement Label
Always select a measurement label before inserting a catheter/probe.
Use the SvO2 label when the catheter/probe will be located in the pulmonary artery (measuring mixed
venous oxygen saturation). This is the only label which allows the measurement value to be used to
calculate oxygen extraction (see “Calculating Oxygen Extraction” on page 247) and in the standard
oxygen calculations.
Use the ScvO2 label when the catheter/probe will be located in a central vein (measuring central
venous oxygen saturation.
Use the SO2 label in all other cases.
To select a measurement label:
1Select Main Setup then Measurements followed by <SO₂ Label>
2Select Label.
3Select the appropriate label for the catheter/probe location.
Preparing to Monitor with the M1021A Wide
Module
In addition to the measurement module, you need a Hospira OptiCath catheter, and 50131 Optical
Module. Use only the Hospira accessories listed in the Accessories section.
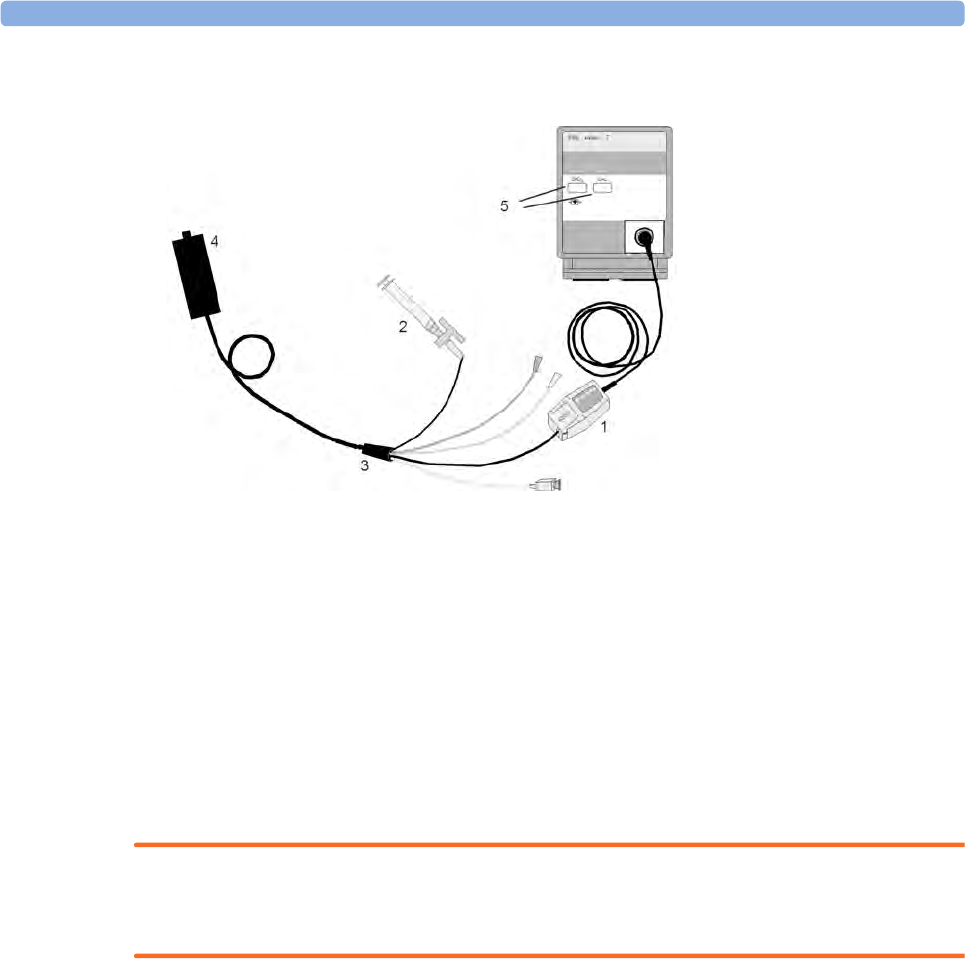
16 Monitoring Intravascular Oxygen Saturation
243
Connect the optical module (Hospira 50131) to the measurement module. Allow the optical module to
warm up before you perform a calibration. Although the warm up message disappears from the screen
after one minute, Hospira recommends letting the optical module warm up for 15 minutes for best
accuracy. Please refer to the instructions for the optical module.
To avoid false alarms during the pre-insertion calibration and insertion of the catheter into the patient,
the monitor automatically suspends alarms during the pre-insertion calibration, for up to three minutes
after you remove the catheter tip from the optical reference. After light intensity calibration, or after
three minutes (whichever comes first), the monitor returns to the alarm state it was in prior to pre-
insertion calibration.
Carrying out a Pre-insertion Calibration
WARNING
It is strongly recommended to carry out a pre-insertion calibration prior to all insertions. If this is not
possible, you must perform an in-vivo calibration after insertion.
Refer to the instructions for use that accompany the catheter. Do not use the catheter if the packaging
is damaged. If you have to disconnect the monitor from the patient (for example, when transferring
the patient from one location to another), you must disconnect at the SvO2 module. The catheter
should remain in the optical module, otherwise you need to recalibrate.
1Remove outer wrapping from catheter tray to uncover optical connector.
2Place the optical module on the catheter tray in the space provided and open the lid.
3Place the optical connector into the optical module (with the label "TOP" facing upwards) and
close the lid.
4In the Setup <SO₂ Label> menu, select Start Pre-InsCal. Ensure that the tip of the catheter is
still in the optical reference.
5Insert the catheter when you see the message <SO₂ Label> calibration completed - catheter
ready for insertion. If the calibration fails, repeat the calibration before inserting the catheter. If it
fails a second time, replace the optical module.
1Optical module
2Balloon inflation stopcock
3Hospira fiber optic catheter
4Optical reference
5Enter setup/calibration
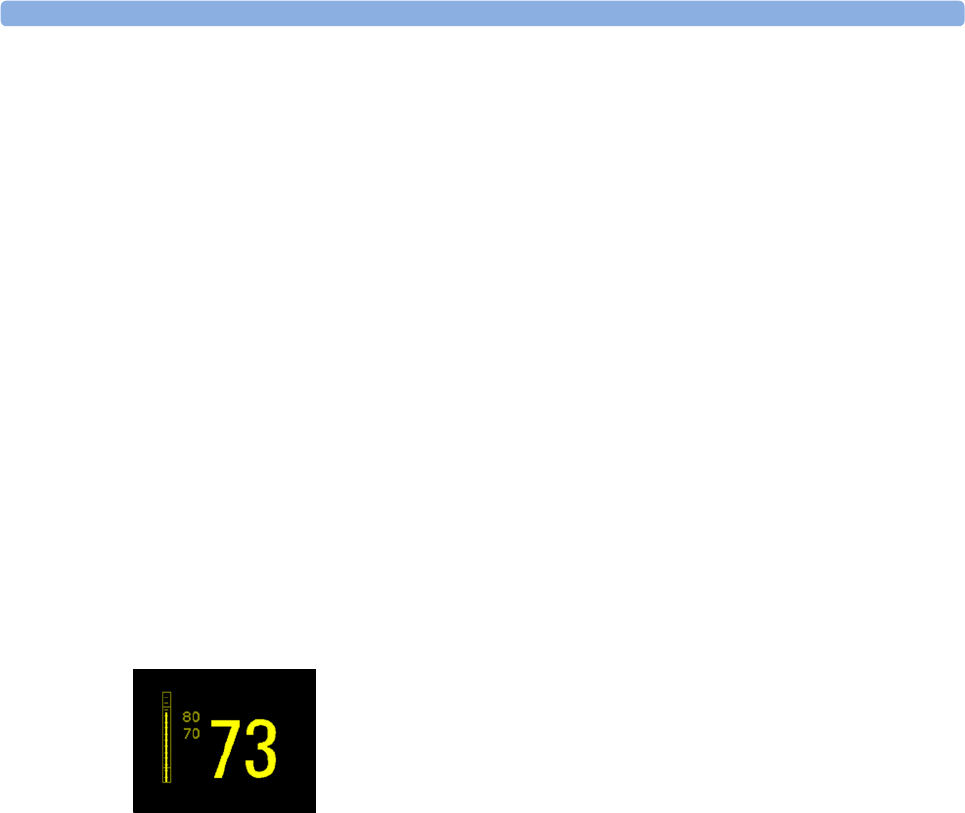
16 Monitoring Intravascular Oxygen Saturation
244
Inserting the Catheter
1Remove the inner cover of the catheter tray.
2Remove the catheter tip from the optical reference. Check the catheter's proper operation (for
example: the balloon tip).
3Prepare and insert the catheter in accordance with standard hospital practice.
The SvO2 catheter is thin and flexible, treat it carefully. Avoid kinking, bending or grasping the
catheter with forceps or a hemostat. Damage to the fiber results in low intensity light and sudden
decrease in intensity readings. Refer to the documentation provided with the fiber-optic catheter,
paying special attention to any precautions, warnings or contraindications.
Secure the optical module directly or in close proximity to the patient, to avoid placing excessive
tension on the catheter, which would result in movement of the catheter tip from the optimal position
in the patient. Position the optical module to avoid contact with liquids, because fluid entering the
catheter-optical module connection may impair light transmission.
If you place the catheter in the patient without performing the pre-insertion calibration, you must
perform an in-vivo calibration once the catheter is in place.
Performing a Light Intensity Calibration
Perform a light intensity calibration after the catheter is in its proper position. When the catheter is
positioned properly, the light intensity indicator must cover at least two small divisions above the
midpoint.
•In the Setup <SO₂ Label> menu, select Start Light Cal.
Calibration is complete after a few seconds. If you doubt existing light intensity readings, recalibrate.
Performing In-Vivo Calibration
Perform an in-vivo calibration:
• if you place the catheter in a patient without performing a pre-insertion calibration.
• if the catheter was disconnected from the optical module.
• when the catheter has been in the patient for 24 hours.
• if any significant change in light intensity occurs that the monitor cannot correct automatically.
Setting Up the In-Vivo Calibration
Check for:
• proper positioning of the catheter in the patient.
• relatively stable oxygen saturation in patient.
• that the SvO2 light intensity indicator covers at least two divisions above the midpoint.

16 Monitoring Intravascular Oxygen Saturation
245
Making the In-Vivo Calibration
1Be prepared to draw a blood sample from the patient.
2In the Setup <SO₂ Label> menu, select Start In-VivoCal.
3To clear the distal lumen, draw off and discard at least 2 ml of blood before taking the sample.
4Draw a blood sample from the distal port of the catheter and flush the line according to standard
hospital practice.
5Obtain laboratory analysis of the sample using direct measurements.
6Select CalibrationValue and select from the list the value received from the lab.
7Complete the calibration by selecting Store In-VivoCal (even if the stored calibration value did not
change) and select Confirm. This updates the data stored in the optical module.
Selecting Recall Last Cal recalls the previously stored calibration value.
If the calibration fails, check that the light intensity indicator is indicating a stable medium to high level.
Repeat the calibration.
Setting Up the In-Vivo Calibration
Check for:
• proper positioning of the probe/catheter in the patient.
• relatively stable oxygen saturation in patient.
• that the light intensity indicator is indicating a stable medium to high level.
Depending on the probe/catheter in use you may need to enter a catheter correction factor. This will
be indicated in the table in the Accessories chapter or in the catheter documentation.
1In the Setup <SO₂ Label> menu, select Catheter Factor.
2Enter the correction factor.
Making the In-Vivo Calibration
1Be prepared to draw a blood sample from the patient.
2In the Setup <SO₂ Label> menu, select Start In-VivoCal.
3To clear the distal lumen, draw off and discard at least 2 ml of blood before taking the sample.
4Draw a blood sample from the distal port of the catheter and flush the line according to standard
hospital practice.
5Obtain laboratory analysis of the sample using direct measurements.
6Select CalibrationValue and select from the list the value received from the lab.
7Select Hct [%] (or Hb [mmol/l] or Hb [g/dl] depending on the set up) and enter the corresponding
value from the laboratory analysis.
To change the setup for entering the Hb/Hct, see “Changing the Lab Value Required for Entry”
on page 246 below.
8Complete the calibration by selecting Store In-VivoCal (even if the stored calibration value did not
change) and select Confirm. This updates the data stored in the optical module.
Selecting Recall Last Cal recalls the previously stored calibration value.
If the calibration fails, check that the light intensity indicator is indicating a stable medium to high level.
Repeat the calibration.
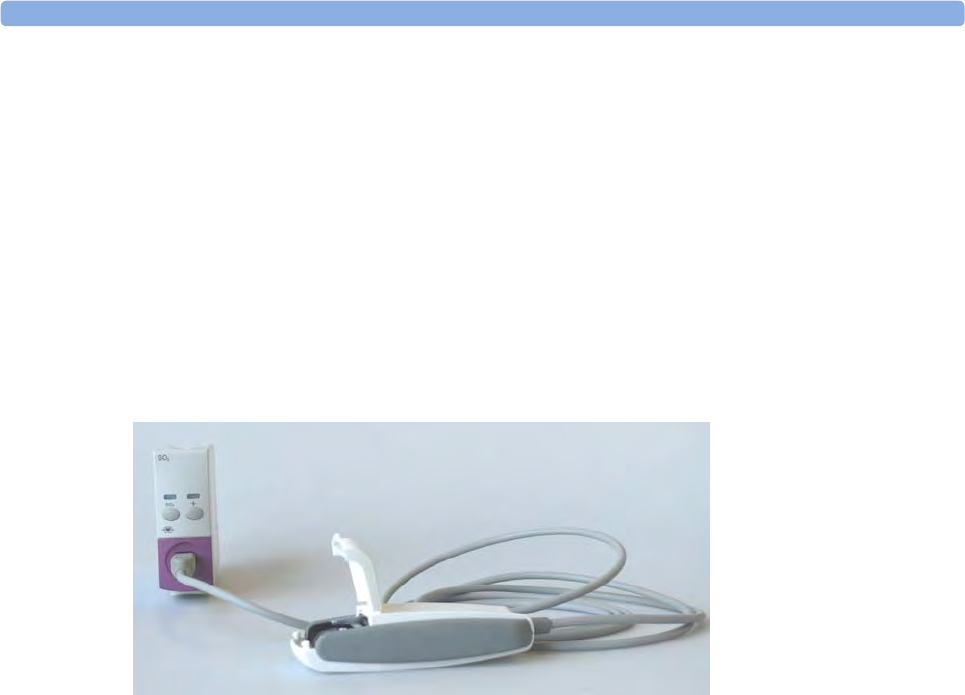
16 Monitoring Intravascular Oxygen Saturation
246
Changing the Lab Value Required for Entry
You can change the lab value required to be entered: Hb [g/dl], Hb [mmol/l] or Hct [%].
1In the Setup <SO₂ Label> menu, select Hb/Hct Entry.
2Select your preferred lab value and unit.
Preparing to Monitor with the M1011A Narrow
Module
In addition to the module, you need a Philips SO2 Optical Module and a compatible fiber optic probe
or catheter. Use only the accessories listed as applicable for the intended measurement location in the
Accessories section.
Connecting the Optical Module
1Connect the optical module to the SO2 module. Allow the optical module to warm up before you
insert the probe/catheter and perform a calibration.
Although the warmup message disappears from the screen after one minute, it is preferable to let
the optical module warm up for 10 minutes for best accuracy.
2Position the optical module to avoid contact with liquids. Fluid entering the catheter-optical
module connection will impair measurement performance.
3Place the optical module on the catheter tray in the space provided and open the lid.
4For instructions on the placement of fiber optic catheters/probes, refer to the documentation
provided with the accessory.
After Insertion
The SO2 probe/catheter is thin and flexible, treat it carefully. Avoid kinking, bending or grasping the
probe/catheter with forceps or a hemostat. Damage to the fiber results in low intensity light and a
sudden decrease in intensity readings. Refer to the documentation provided with the fibre-optic
probe/catheter, paying special attention to any precautions, warnings or contraindications.
Secure the optical module directly attached or in close proximity to the patient, to avoid placing
excessive tension on the catheter, which would result in movement of the catheter tip from the optimal
position in the patient.
You must perform an in-vivo calibration once the probe/catheter is in place.
The probe/catheter should be replaced after it has been in place for 72 hours.
16 Monitoring Intravascular Oxygen Saturation
247
CAUTION
Do not apply excessive tension to any sensor cable or part of the catheter.
Performing In-Vivo Calibration
Perform an in-vivo calibration:
• when you place the catheter in a patient.
• if the catheter was disconnected from the optical module.
• when the catheter has been in the patient for 24 hours.
• if any significant change in light intensity occurs that the monitor cannot correct automatically.
Further Information for Both Modules
Checking Suspicious Values
If you have any doubts about the correctness of the measurement value, take a blood sample and have
it analyzed using standard laboratory procedures.
Calculating Oxygen Extraction
Oxygen extraction is the difference between the measured SpO2 and SvO2 values. If you are
monitoring SpO2 and SvO2, the monitor can calculate this value and display it as a numeric.
• To switch oxygen extraction calculation on or off, in the Setup Sp-vO₂ menu, select Sp-vO₂ and
toggle between On and Off.
•If more than one SpO
2 value is available, you must choose which value is used in the calculation.
In the Setup Sp-vO₂ menu, select SpO₂ Source and select the required source.
If one of the calculation sources becomes unavailable, the monitor displays the INOP Sp-vO₂ CHK
SOURCES for one minute. After this time, the calculation automatically switches off. If the missing
source becomes available again, the calculation automatically switches on again.

16 Monitoring Intravascular Oxygen Saturation
248

17
249
17Monitoring EEG
The Electroencephalograph (EEG) module monitors the patient's cerebral function by measuring the
electrical activity of the brain. It provides the monitor with two channels of realtime EEG waves, EEG
trend information in the form of Compressed Spectral Arrays (CSA), and up to eight of the following
numerics:
Spectral Edge Frequency - The SEF is the frequency below which a defined percentage of the Total
Power lies. The percentage is set in Configuration Mode.
Mean Dominant Frequency (MDF) - The MDF is the mean value of the frequency which
dominates the measured EEG.
Peak Power Frequency (PPF) - The PPF is the frequency with the highest measured amplitude.
Total Power (TP) - The TP numeric indicates the power in the measured frequency band.
Percentage of total power in each frequency band:
–Alpha waves (8 to 13 Hz)
–Beta waves (13 to 30 Hz)
–Theta waves (4 to 8 Hz)
–Delta waves (0.5 to 4 Hz).
EEG Monitoring Setup
1Plug the trunk cable into the EEG module.
2Prepare the patient's skin prior to placing the electrodes. Good electrode-to-skin contact is
important for a good EEG signal, as the skin is a poor conductor of electricity.
– Shave hair from sites, if necessary.
– Wash sites thoroughly with soap and water. We do not recommend using ether or pure
alcohol, because this dries the skin and increases the resistance.
– Use a skin preparation paste to remove skin cells and oil before placing the electrodes.
3Select the desired electrode montage in the Setup EEG menu or in the EEG Impedance / Montage
window.
4Attach the reference electrode first.
5Place the electrodes on the patient's head according to the selected montage. Use electrode gel if
you are not using pre-gelled electrodes. Remember to select a site where the signal will not be
interfered with by muscle artifacts.
6Connect the electrode connector end to the trunk cable.
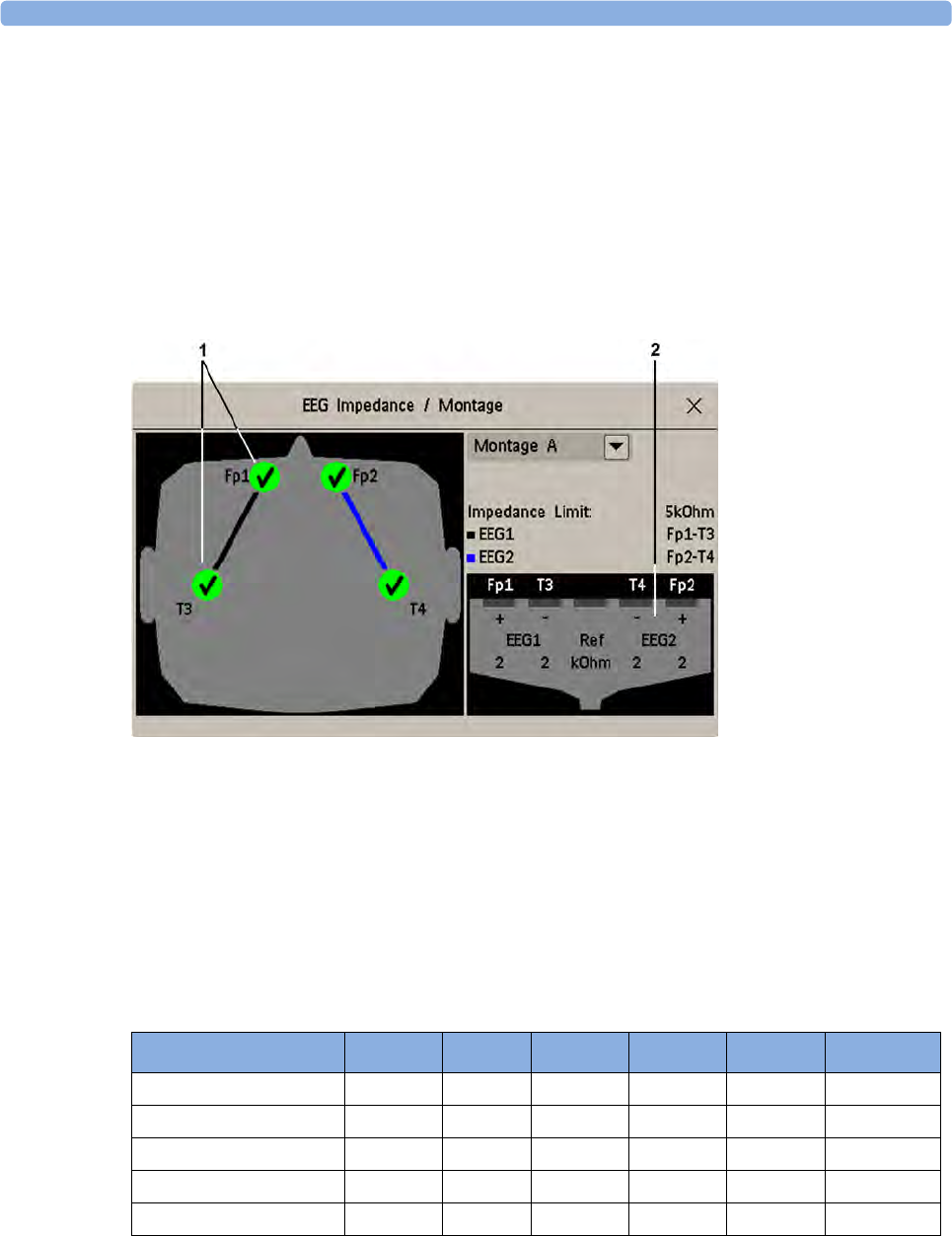
17 Monitoring EEG
250
7Check the electrode-to-skin impedance in the EEG Impedance / Montage window.
8For good signal quality, keep all lead wires together and away from other electric devices and
metallic bodies.
Using the EEG Impedance/Montage Window
To open the window, in the Setup EEG menu, select Show Montage, or select the EEG Montage
SmartKey.
The window may be configured to look slightly different on your monitor.
1Electrode locations on the patient's head. The symbols represent the electrode-to-skin impedance.
2Wiring and impedance values for the selected montage
Choosing an EEG Electrode Montage
1To activate one of the five pre-configured electrode montages, select the arrow beside the label in
the EEG Impedance / Montage window and choose a montage from the list.
2Attach the electrodes as illustrated in the EEG Impedance / Montage window.
The five default electrode montage configurations can be modified and renamed in Configuration
Mode.
The electrode locations are labeled according to the international 10-20 electrode placement system.
Montage Name EEG1+ EEG1- Label1 EEG2+ EEG2- Label2
Montage A Fp1 T3 Fp1-T3 Fp2 T4 Fp2-T4
Montage B O1 T3 O1-T3 O2 T4 O2-T4
Montage C F3 C3 F3-C3 F4 C4 F4-C4
Montage D C3 P3 C3-P3 C4 P4 C4-P4
Montage E Fp1 T5 Fp1-T5 Fp2 T6 Fp2-T6
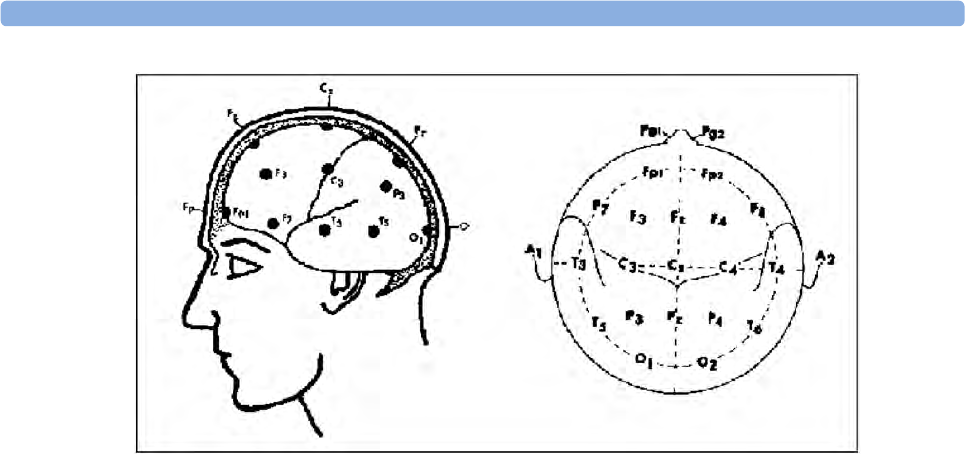
17 Monitoring EEG
251
Changing the Impedance Limit
The impedance limit can be set for all electrodes simultaneously in the Setup EEG menu, or in the EEG
Impedance / Montage window using the pop-up keys. If the limit is exceeded during monitoring, an
INOP will appear and the graphic impedance indicator will change.
To change the impedance limit, either
• use the pop-up keys that appear with the EEG Impedance / Montage window, or
•in the Setup EEG menu, select Impedance Limit to call up a list of selections between 1 and
30 kOhm, then select the required limit from this list.
About Electrode-to-Skin Impedance
Electrode-to-skin impedance is the main quality indicator for the measured EEG signal. During
normal EEG monitoring, electrode-to-skin impedance is measured continuously and disconnected
electrodes are detected. The impedance value for each single, independent signal electrode is displayed
in the EEG Impedance / Montage window. If the measured electrode-to skin impedance of one or
more electrodes is above the limit, an INOP will be issued.
For impedance measurement at least two electrodes, plus the reference electrode, must be connected.
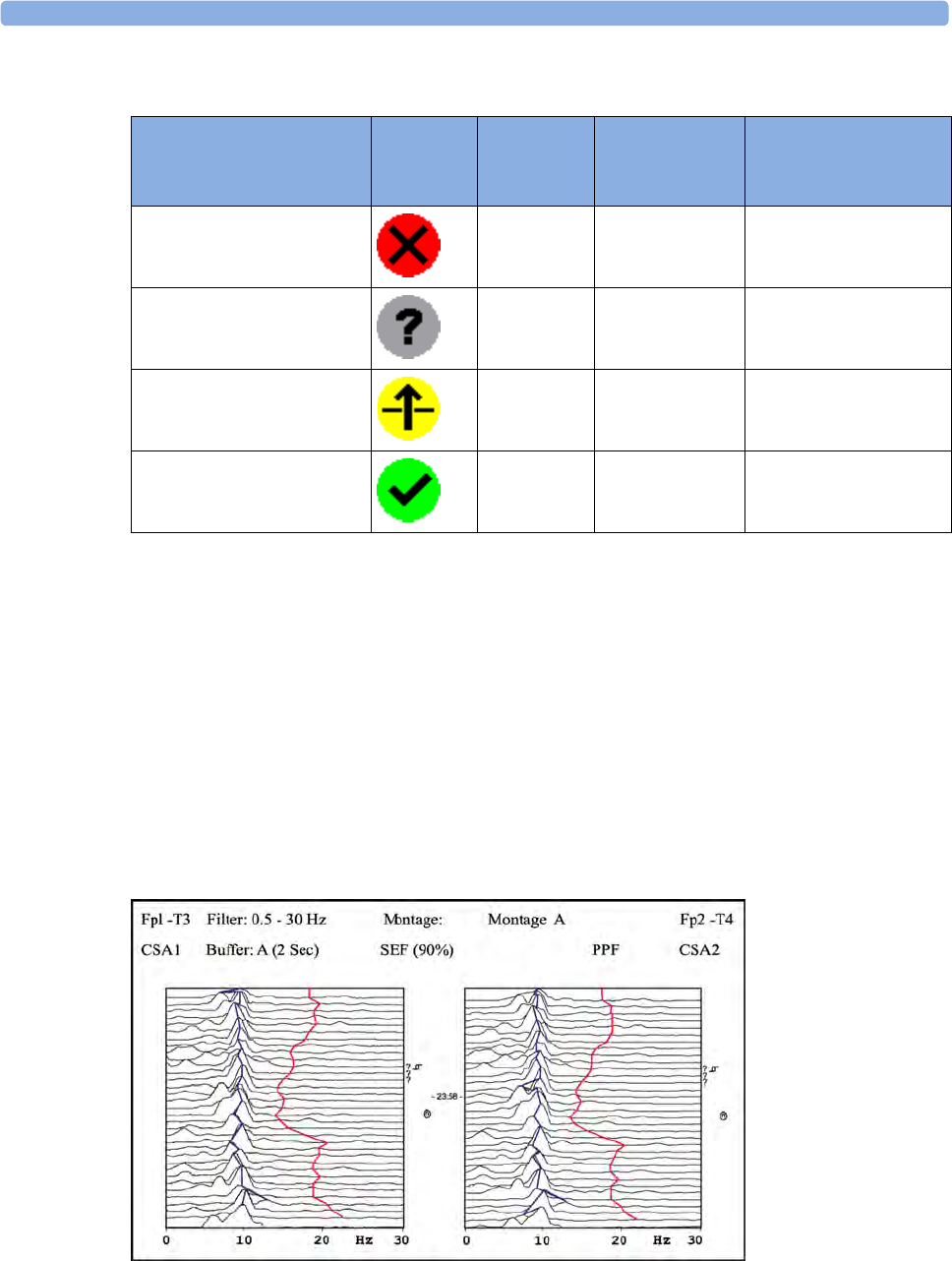
17 Monitoring EEG
252
Impedance Indicators
About Compressed Spectral Arrays (CSA)
The continuous EEG signal is sampled periodically and this value is stored in a frame. Each frame is
processed using Fast Fourier Transformation (FFT) to provide a frequency spectrum displayed as a
compressed spectral array (CSA).
The CSA window provides an overview of the patient's EEG values over time. It may be configured to
look slightly different on your monitor.
• To view the CSA window permanently embedded on a Screen, select a Screen configured to
display the CSA window.
• To view the CSA window over the current Screen, select the EEG CSA SmartKey, if configured, or
select Setup EEG or Main Setup then Show CSA.
Electrode/Skin
Impedance
Symbol Color Displayed
Impedance
Value
Action
Electrode not connected red no value connect electrode
Noisy signal gray 60 kΩ (fixed) check electrode-to-skin
connections
Electrode connected,
impedance above limit
yellow measured value
(e.g. 15 kΩ)
check limit, check
electrode-to-skin
contact
Electrode connected,
impedance at or below limit
green measured value
(e.g. 3 kΩ)
no action necessary
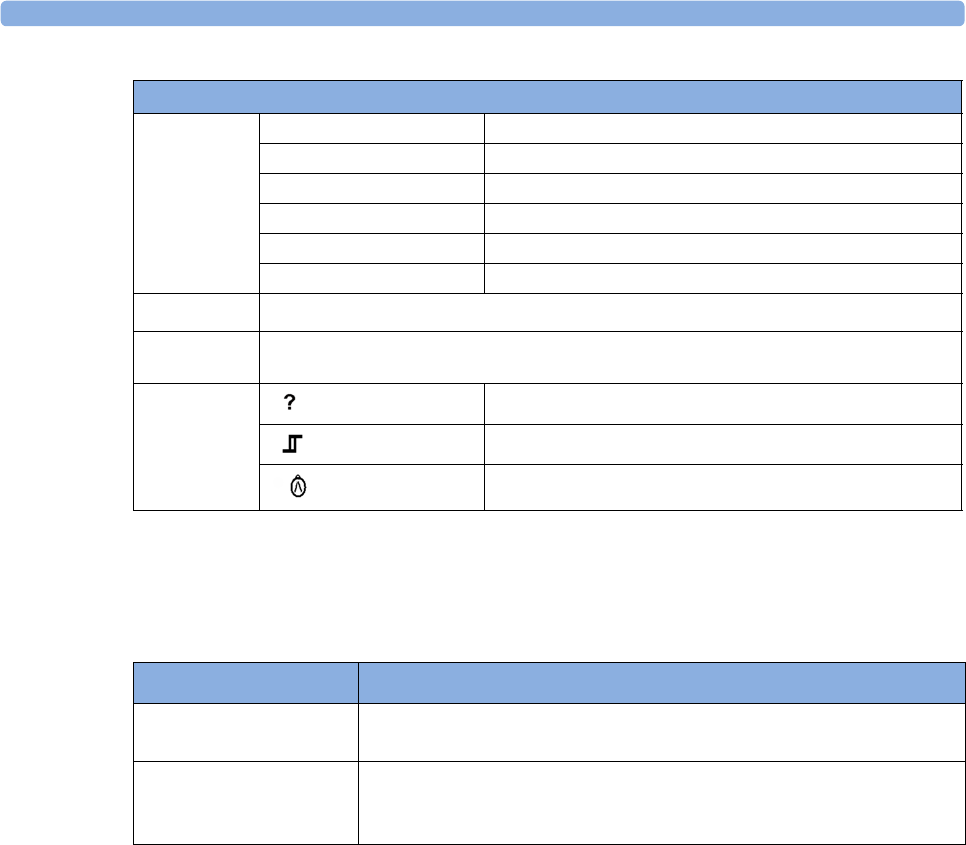
17 Monitoring EEG
253
Changing CSA Settings
When CSAs are shown embedded on the Main Screen, select the CSA to show the pop-up keys. When
the CSA is shown in a window over the current screen, the pop-up keys are always displayed.
Changing EEG Settings
Be aware that any changes made to EEG settings apply to both EEG channels.
Switching EEG Numerics On and Off
Each EEG numeric can be individually switched on or off in the Setup EEG menu.
1In the Setup EEG menu, select the numeric label.
2Select On or Off to switch between the settings.
Changing the Scale of the EEG Waves for Display
This only changes the visual appearance of the wave. It does not affect the signal analyzed by the
monitor or printed in reports or recordings.
1In the Setup EEG menu, select Wave Scale to call up a list of wave scales.
2Select the required scale from this list.
Scaling information is displayed with each EEG wave.
The CSA contains the following information
Status line
Lead label for example, Fp1-T3, Fp2-T4
CSA label CSA1 or CSA2 according to EEG channel
Montage label for example, Montage A
Filter settings for example, 1-30 Hz
Buffer label and time the buffer and interval between spectral lines on the CSA
Current SEF Threshold can only be changed in Configuration Mode
Spectral lines The energy at each frequency is computed and displayed as a spectral line
Trendlines EEG values are sampled at configured time intervals and displayed as color-coded trendlines.
Trendlines are available for the three frequency numerics (SEF, PPF, MDF)
Annotations:
INOP marker
Filter change marker
Montage change marker
Setup CSA Window This menu entry lets you
Buffer choose one of the three pre-configured buffers. A buffer defines the
interval between the spectral lines displayed in the CSA.
On/Off SEF
On/Off MDF
On/Off PPF
switch the trendline of the specific numeric on or off
17 Monitoring EEG
254
•If Show Gridlines is set to On in Configuration Mode, gridlines and the current wave scale values
are shown with the EEG wave.
•If
Show Gridlines is set to Off in Configuration Mode, the current wave scale is indicated by a size
bar beside the EEG wave.
Changing Filter Frequencies
The low and high pass filters screen out undesirable interference from the raw EEG wave display. The
current EEG filter frequency settings are shown in the header of the CSA. Changing filter settings
affects the EEG wave and all the EEG numerics. Whenever the filter setting is changed, a filter change
marker appears next to the spectral lines.
To change the filter settings:
1In the Setup EEG menu, select Low Filter or High Filter to call up a list of available frequencies.
2Select the required frequency from this list.
Changing the Speed of the EEG Wave
The EEG measurement has its own speed control and is not affected by the wave speed settings of the
other measurements.
In the Setup EEG menu, select EEG Speed. Choose the required speed from the pop-up list. This
defines the speed at which the wave is drawn across the screen in millimeters per second (mm/s).
EEG Reports
The content of EEG Reports is always the same and does not need to be configured.
To print an EEG Report, in the Setup EEG menu, select Print Report.
Alternatively, you can select the CSA and use the Print Report pop-up key to start the report.
To modify the buffer and trendline settings on the CSA Report, in the Reports menu, select CSA On
EEG Rep.. If you do not change these settings, the monitor will use the default settings with the
trendlines for the SEF numeric on and the buffer time from Buffer C.
EEG Safety Information
WARNING
Do not touch the patient, or table, or instruments during defibrillation.
When connecting electrodes and/or patient cables, ensure that the EEG leads and connectors do not
come into contact with other conductive parts or earth.
CSA On EEG Rep. This menu entry lets you
Buffer choose one of the three pre-configured buffer times
Trend SEF
Trend MDF
Trend PPF
switch the trendline of the specific numeric on or off
17 Monitoring EEG
255
High-frequency Surgery - To reduce the hazard of burns in the high-frequency surgical neutral
electrode connection, the EEG electrodes should not be located between the surgical site and the
electrosurgical unit return electrode.
EEG and Electrical Interference
CAUTION
Interference from a non-grounded instrument near the patient and electrosurgery interference can
cause problems with the waveform and the CSA.
Radiated field strengths above 1 V/m and patient signals ≤ 50 µV may cause noise on the EEG waves
at various frequencies. Therefore, it is recommended to avoid the use of electrical radiating equipment
in close proximity to the patient monitor. The noise does not influence the measurement accuracy.
Interference from ECG can be eliminated by adjusting the low filter settings.

17 Monitoring EEG
256

18
257
18Monitoring BIS
Bispectral Index monitoring helps to monitor the level of consciousness of a patient under general
anesthesia or sedation in the OR and ICU. The BIS sensor is placed on the patient's forehead to
capture electroencephalographic (EEG) signals from which several numerics are derived, including a
single BIS value representing the level of consciousness. See the chapter on Specifications for the BIS
intended use statement.
The BIS Module provides the monitor with an EEG wave and the following numerics:
Bispectral Index (BIS). The BIS numeric reflects the patient’s level of consciousness. It ranges from
100 (fully awake) to 0 (suppression; no electrical brain activity).
Signal Quality Index (SQI). The SQI numeric reflects signal quality and provides information about
the reliability of the BIS, SEF, TP, SR, and Bursts numerics during the last minute.
It ranges from 0 to 100%:
SQI < 15%: the numerics cannot be derived
SQI 15% to 50%: the numerics cannot be reliably derived
SQI 50% to 100%: the numerics are reliable.
Electromyographic Activity (EMG). The EMG numeric reflects the electrical power of muscle
activity and high frequency artifacts.
EMG < 55 dB: this is an acceptable EMG
EMG ≤ 30 dB: this is an optimal EMG
(note that the minimum possible EMG is approximately 25 dB).
Suppression Ratio (SR). The SR is the percentage of time over the last 63-second period during
which the EEG is considered to be in a suppressed state.
Spectral Edge Frequency (SEF). The SEF is the frequency below which 95% of the Total Power is
measured.
Total Power (TP). The TP numeric indicates the power in the frequency band 0.5 to 30 Hz. The
useful range is 30 - 100 dB.
Bursts (BISx used with the Extend sensor only). The Bursts numeric helps you quantify suppression
by measuring the number of EEG bursts per minute, where an EEG burst is defined as a period of
activity followed and preceded by inactivity (at least 0.5 second).
BIS Monitoring Setup
There are two BIS solutions available for use with the M1034A BIS module: using the Digital Signal
Converter (DSC) and BIS Engine or using the BISx.
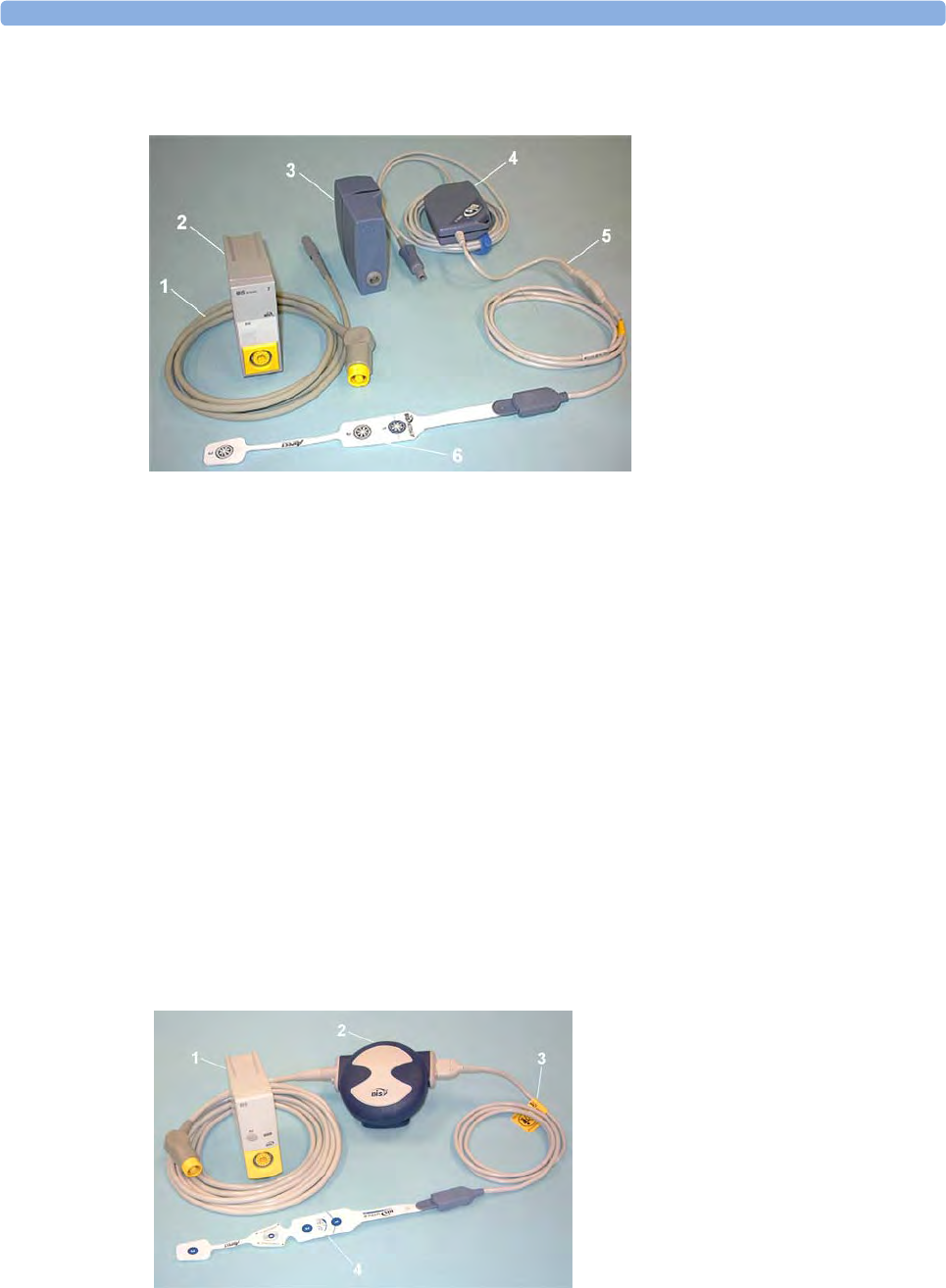
18 Monitoring BIS
258
Monitoring BIS Using the DSC and BIS Engine
1If you are monitoring BIS with the DSC and BIS Engine,
a. Connect the BIS Engine to the BIS module using the BIS Engine Cable.
b. Connect the digital signal converter (DSC) to the digital signal converter port on the front of
the BIS Engine. Use the attachment clip to secure the digital signal converter near, but not
above the patient's head.
c. Attach the patient interface cable (PIC) to the digital signal converter (DSC).
2Attach the BIS sensor to the patient following the instructions supplied with the sensor.
Make sure that the patient's skin is dry. Be aware that a wet sensor or a salt bridge may cause
erroneous BIS and impedance values.
A variety of sensors are available for use in the OR and ICU environments.
3Connect the BIS sensor to the patient interface cable.
As soon as a valid sensor is detected, the impedances of all electrodes are measured automatically
and the results are shown in the BIS window.
Monitoring BIS using the BISx
1BIS Engine Cable
2BIS Module
3BIS Engine
4Digital Signal Converter (DSC)
5Patient Interface Cable
6BIS Sensor
1BIS Module
2BISx
3Patient Interface Cable
4BIS Sensor
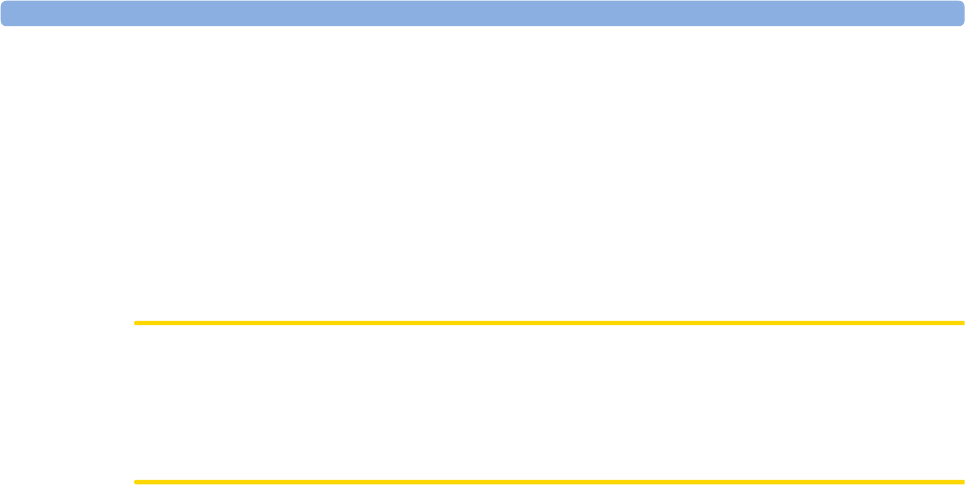
18 Monitoring BIS
259
1If you are monitoring BIS using the BISx,
a. Connect the BISx to the BIS module
b. Use the clip on the rear of the BISx to affix it in a position convenient for your patient, not
above the patient's head.
2Attach the BIS sensor to the patient following the instructions supplied with the sensor.
Make sure that the patient's skin is dry. Be aware that a wet sensor or a salt bridge may cause
erroneous BIS and impedance values.
A variety of sensors are available for use in the OR and ICU environments.
CAUTION
Ensure that the BISx does not come into prolonged contact with your patient's skin, as it may
generate heat and cause discomfort.
The BISx may remain connected to a patient during defibrillation as long as the sensor is not
located between the defibrillator pads.
3Attach the patient interface cable (PIC) to the BISx.
4Connect the BIS sensor to the PIC.
As soon as a valid sensor is detected, the impedances of all electrodes are measured automatically and
the results are shown in the BIS window.
Manufacturer's Information
BIS Engine, DSC, BISx, the Patient Interface Cable and the BIS Sensors are manufactured by Aspect
Medical Systems.
BIS Continuous Impedance Check
This checks:
• the combined impedance of the signal electrodes plus the reference electrode.
This is done continuously and does not affect the EEG wave. As long as the impedances are
within the valid range, there is no notification of this check or its results.
• the impedance of the ground electrode.
This is done every ten minutes and takes approximately 4 seconds. It causes an artifact in the EEG
wave, and the message Ground Check is shown on the monitor screen during the check. If the
ground electrode does not pass this check, another check is started. This continues until the
ground electrode passes the check.
If the Continuous Impedance Check interferes with other measurements, it can be switched off. To do
this:
1In the Setup BIS menu, select Cont. Imp. Check.
2Select On or Off as required.
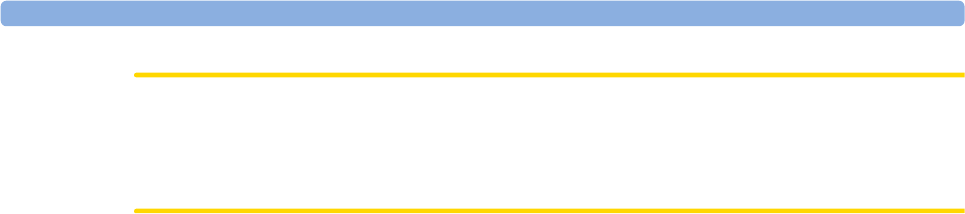
18 Monitoring BIS
260
CAUTION
Switching the continuous impedance check off will disable automatic notification to the user of
impedance value changes, which may lead to incorrect BIS values. Therefore, this should only be done
if the check interferes with or disturbs other measurements.
BIS Cyclic Impedance Check
This measures the exact impedance of each individual electrode. It causes a disturbed EEG wave, and
the INOP BIS IMPEDANCE CHCK is shown on the monitor screen during the check.
Starting a Cyclic Impedance Check
The Cyclic Impedance Check is automatically started when a sensor is connected. To manually start a
Cyclic Impedance Check:
•select
Cyclic Check in the Setup BIS menu to toggle between On and Off, or
•select
StartCyclicCheck in the BIS window.
Stopping a Cyclic Impedance Check
The Cyclic Impedance Check stops automatically if the impedances of all electrodes are within the
valid range. To manually stop a Cyclic Impedance Check:
•select
Cyclic Check in the Setup BIS menu to toggle between On and Off, or
•select
Stop CyclicCheck in the window.
If you stop a Cyclic Impedance Check before the ground electrode has passed, a ground electrode
impedance check will be started automatically. This cannot be switched off.
BIS Window
To open the BIS window, in the Setup BIS menu, select Show Sensor.
The window may look slightly different on your monitor. The graphic in the BIS Window
automatically adapts to show the type of sensor you are using, showing three or four electrodes as
required. Each symbol in the graphic represents an electrode and illustrates the most recently-
measured impedance status of the electrodes. Although BIS may still be measured when the electrode
status is red or yellow, for best performance, all electrodes should be green.
In addition, if the measured electrode-to skin impedance of any electrode or electrode combination is
above the limit, or if disconnected electrodes are detected, an INOP will be issued, either BIS HIGH
IMPEDANCE or BIS LEAD OFF.
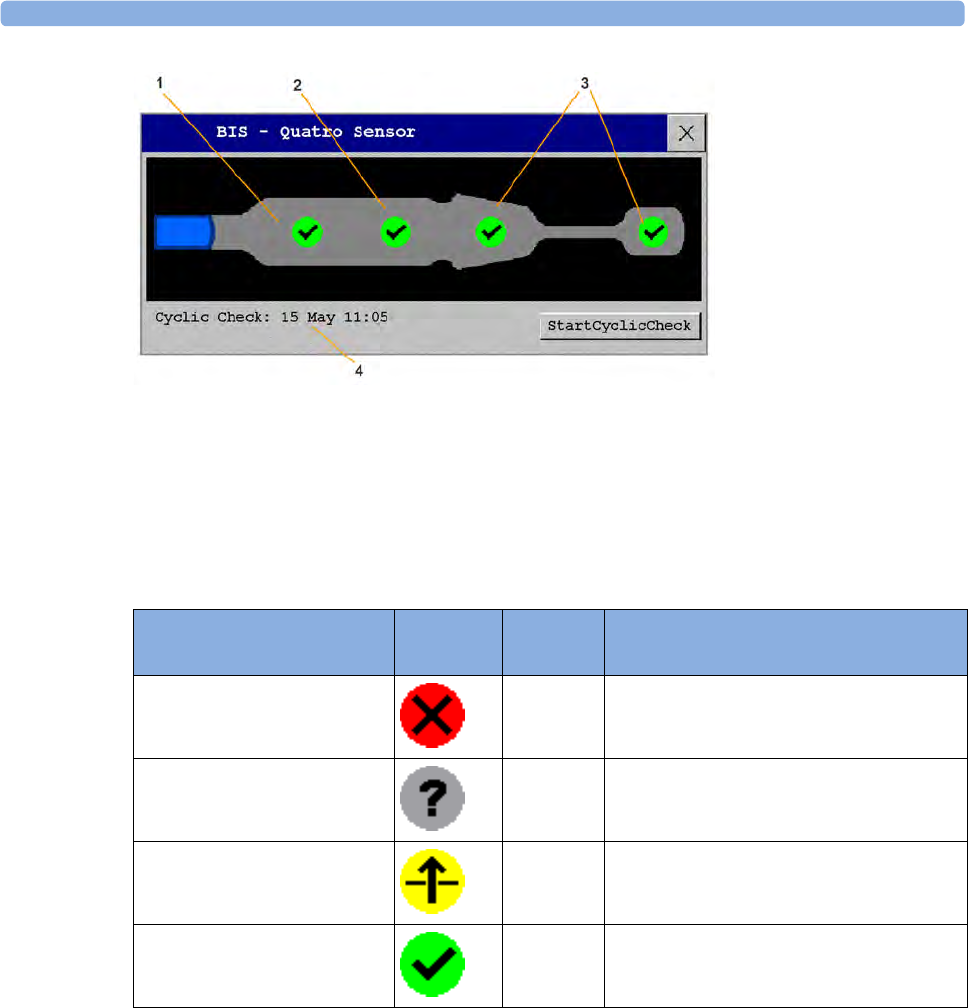
18 Monitoring BIS
261
1Reference Electrode
2Ground Electrode
3Signal Electrode(s)
4Time of the most recent cyclic check
BIS Impedance Indicators
In addition to the symbols, the impedance value in kOhm is also displayed.
Changing the BIS Smoothing Rate
The smoothing rate defines how the monitor averages the BIS value.
To change the smoothing rate, in the Setup BIS menu, select Smoothing Rate then choose either:
–15 sec: this provides increased responsiveness to changes in the patient's state.
–30 sec: this provides a smoother BIS trend with decreased variability and sensitivity to
artifacts.
Electrode-to-Skin
Impedance
Symbol Color Action
Electrode has no skin contact red Reconnect electrode, or check the sensor-
to-skin contact. If necessary, clean and dry
skin.
Too much signal noise,
impedance cannot be
measured
gray Check sensor-to-skin contact. Press sensor
more firmly to skin. If necessary, clean and
dry skin.
Impedance above limit yellow Check sensor-to-skin contact. Press sensor
more firmly to skin. If necessary, clean and
dry skin.
Impedance within valid range green No action necessary

18 Monitoring BIS
262
Switching BIS and Individual Numerics On and Off
To switch the BIS measurement on or off:
•In the Setup BIS menu, select BIS and then On or Off as required.
To switch individual numerics provided by the BIS Module on or off:
•In the Setup BIS menu, select SQI, TP, SEF, SR, EMG, or Bursts and then On or Off as required.
Changing the Scale of the EEG Wave
Changing the scale only changes the visual appearance of the wave. It does not affect the signal
analyzed by the monitor or printed in reports or recordings.
The scale information shown depends on whether gridlines are switched on or off for display. This
setting can only be changed in Configuration Mode.
1In the Setup BIS menu, select Scale to call up a list of wave scales.
2Select the required scale from this list.
– When gridlines are switched off, you can choose from the available scale values: 50 µV,
100 µV, 200 µV, and 500 µV. Scaling information is displayed as a vertical bar on the EEG
wave together with its height equivalent in mV.
– When gridlines are switched on, scales are defined as a range, either ± 25 µV, ± 50 µV, ±
100 µV, or ± 250 µV. Scaling information is shown in the form of gridlines.
Switching BIS Filters On or Off
The low and high pass filters screen out undesirable interference from the raw EEG wave display. The
notch filter removes line frequency interference. Filter settings affect the EEG wave and the SEF and
TP values, but they do not affect the BIS, EMG, SR, and SQI values.
The filter settings are set in Configuration Mode. You can switch all the filters on or off together in
Monitoring Mode.
1In the Setup BIS menu, select Filters.
2Select On or Off as required.
BIS Safety Information
For information on the use of BIS in specific monitoring situations and on pharmacological responses
to the anesthetic agents Nitrous Oxide (when used as the sole anesthetic agent), Ketamine, and
Etomidate, please contact Aspect Medical Systems to request a copy of their publication "A Clinician's
Guide to the Bispectral Index®".
Considerations for Use
Due to limited clinical experience in the following applications, BIS values should be interpreted
cautiously in patients with known neurological disorders, those taking psychoactive medications, and
in children below the age of 1.
18 Monitoring BIS
263
WARNING
Conductive Parts: The conductive parts of sensors and connectors should not contact other
conductive parts, including earth.
High-frequency Surgery: To reduce the hazard of burns in the high-frequency surgical neutral
electrode connection, the BIS sensor should not be located between the surgical site and the electro-
surgical unit return electrode.
Defibrillation: The BIS sensor must not be located between defibrillator pads when a defibrillator is
used on a patient connected to the patient monitor.
Securing Cables: To minimize the risk of patient strangulation, the patient interface cable (PIC) must
be carefully placed and secured.
CAUTION
Revisions: The system will only function if all component revisions are compatible. Otherwise, an
incompatibility INOP is displayed.
If the DSC has an older software revision than the BIS Engine, the DSC will automatically be
upgraded by the BIS Engine. Do not disconnect the DSC from the BIS Engine, or disconnect the BIS
module from the monitor, or switch the monitor power off within the first ten seconds after
connection, as this will disrupt a possible software upgrade and cause damage to the DSC.
Impedance Checks: Impedance checks may influence data acquisition of other
electroencephalographic devices.

18 Monitoring BIS
264

19
265
19Assigning a Telemetry
Device and a Monitor to One
Patient
It is possible to assign a monitor and a telemetry device to the same patient, resulting in the
information from both devices being combined in one sector at the Information Center. This is called
"pairing" and when a telemetry device and a monitor are paired, the measurement data from the
telemetry device will be displayed on the monitor screen.
A telemetry device can be:
• any Philips telemetry device (only for indirect connections, see below).
• a TRx/TRx+ Intellivue Telemetry system transceiver.
• an MP5 monitor or X2 Multi measurement module with a telemetry interface, declared as a
telemetry device and with a telemetry equipment label.
For complete user information, including accessory listings and specifications, for the M4841A/
M4851A TRx/TRx+ IntelliVue Telemetry Transceiver, refer to the Instructions for Use provided with
the device.
How Can You Combine Devices?
•With an indirect connection, using standard telemetry transmission - the data are sent to the
monitor via the Information Center and arrive with a delay of several seconds at the monitor.
•With a direct connection to the monitor
– an MP5 or X2 is connected via MSL cable to the monitor, or
– a telemetry transceiver with a short range radio adapter is assigned to an MP5 or X2 which is
connected (Companion Mode) to a an MX600/700/800 host monitor
the data arrive with a minimal delay on the monitor screen.
Indirect Connection - Manual Pairing
The telemetry device can be paired with the monitor at the Information Center or at the monitor. For
detailed information regarding pairing and configuration at the Information Center, see the
Information Center Instructions for Use.
To pair the monitor with a telemetry device at the monitor:
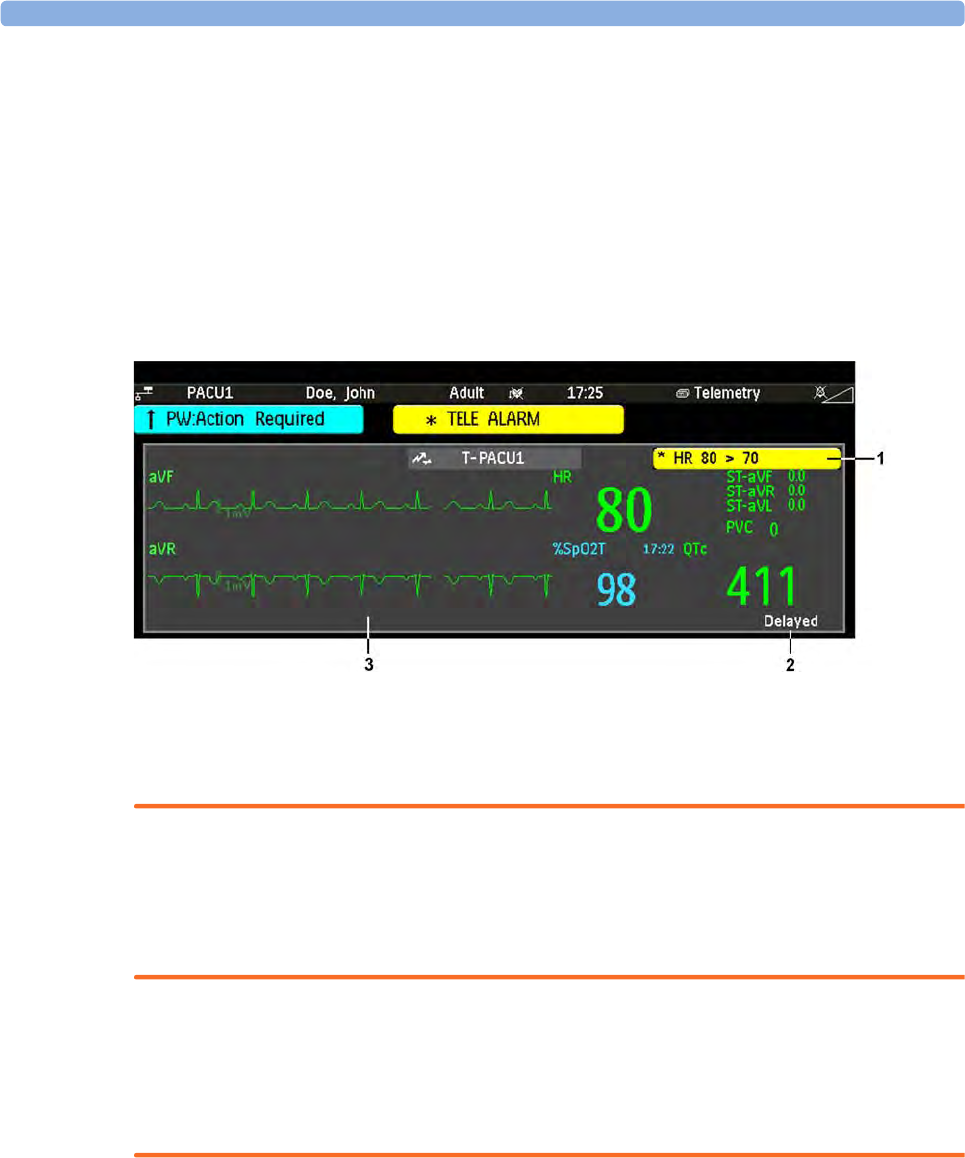
19 Assigning a Telemetry Device and a Monitor to One Patient
266
1Select Main Setup then Measurements
2Select Telemetry
The Setup Telemetry menu will appear with only one entry Paired Equipment.
3Enter here the equipment label of the telemetry device to be paired.
Pairing at the monitor is only possible when the monitor already has a connection to the Information
Center and the Information Center software version allows pairing at the monitor.
Telemetry Data Window
The measurements from the telemetry device are shown in the telemetry data window on the monitor.
1A current alarm generated by the telemetry device.
2Delayed - indication that data in the window is delayed
3Telemetry data window
WARNING
All data presented in the telemetry data window are delayed for several seconds.
If you need realtime data, for example for defibrillation, always use the monitor ECG instead of
telemetry. As long as the ECG is being measured with the telemetry device there will be no ECG signal
available at the ECG analog output.
Direct Connection - Automatic Pairing
The following direct connections are possible:
• an MP5 or X2, declared as a telemetry device, and connected with an MSL cable to a monitor.
WARNING
• When ECG is being measured with a telemetry device directly connected to the monitor, there will
be no ECG signal available at the ECG analog output or ECG Sync Pulse output and no
synchronization marks on the ECG wave. A No ECG Out message will appear in the ECG wave
channel.
• When a telemetry device is connected to the monitor, arrhythmia relearning is initiated, and again
when the telemetry device is disconnected.

19 Assigning a Telemetry Device and a Monitor to One Patient
267
• Controls on the Telemetry Device (e.g. nurse call) will be inactive when the device is directly
connected to the monitor except in the case when the monitor has no network connection and
data are transferred via the telemetry device.
Pairing an X2 or MP5 With a Telemetry Interface to a Host Monitor
An X2 Multi-measurement module or an MP5 using an IntelliVue Instrument Telemetry interface will
be automatically paired when it is connected to a host monitor and it has been declared as a "telemetry
device" at the Information Center.
When the X2 or MP5 is disconnected from the host monitor it will remain paired and the
measurement data will appear at the host monitor in the Telemetry Data window. After the X2 or MP5
is disconnected from the monitor it may take over 15 seconds until their data is displayed at the
Information Center.
Pairing of a host monitor and a telemetry device, with all the related functionality, is only possible
when the host monitor is using a wired LAN connection or a wireless LAN interface (but not using
the IntelliVue Instrument Telemetry interface).
The X2 or MP5 can also be manually paired to a host monitor without a direct connection, as
described in “Indirect Connection - Manual Pairing” on page 265.
Refer also to “Use Models With Telemetry” on page 269 for further related use modes.
Functions Available When the Telemetry Data
Window is Displayed
Controlling the Telemetry Device from the Bedside
You can change settings for a paired telemetry device at the monitor:
1Select the telemetry data screen element
2Select the Setup Tele pop-up key
The Setup Telemetry menu will appear with the settings available for the telemetry device. These will
normally include: adjusting heart rate alarms, ECG size control, selecting primary/secondary lead,
relearning arrhythmia, and selecting the arrhythmia analysis mode. The Equipment label of the paired
device is also shown here.
Viewing and Silencing Telemetry Alarms at the Bedside
When a telemetry device is paired with the monitor, telemetry alarms will also be indicated on the
monitor, in addition to the main indication at the Information Center.
If configured, a generic * TELE ALARM message will appear in the alarm status area with standard alarm
tones. The * TELE ALARM message will have the color and * or ! coding corresponding to the severity
of the alarm. The specific alarm message (for example ** HR LOW) will appear in the telemetry data
window.
If configured, alarms generated from a paired telemetry device can be silenced at the bedside. Either
the monitor Silence key is configured to silence both monitor and telemetry alarms (must be
configured at the Information Center) or the Silence Bed pop-up key will be available:
1Select the telemetry screen element.
19 Assigning a Telemetry Device and a Monitor to One Patient
268
2Select the Silence Bed pop-up key.
Depending on your Information Center configuration, the Silence Bed key may silence both telemetry
alarms and bedside alarms.
WARNING
Even when the telemetry data is not visible on the screen, you may be silencing telemetry and monitor
alarms, if the Information Center and monitor are so configured.
Suspending Telemetry Alarms
When you select Pause Alarms or Alarms Off at the monitor, the alarms are off or paused for the
bedside measurements. When you switch alarms off or pause alarms at the Information Center, both
telemetry and monitor alarms are affected.
Refer to the Information Center Instructions for Use for more details on the Suspend/Pause alarms
behavior of the Information Center and telemetry device.
Using Standby
When you select Standby mode at the monitor, the bedside goes into Standby mode but the telemetry
device will continue monitoring.
Refer to the Information Center Instructions for Use for details on the Standby behavior of the
Information Center and telemetry device.
General Telemetry-related Functions
The following functions are valid for directly and indirectly connected telemetry devices.
ECG Source Tracking at the Information Center
The Information Center continuously checks whether a valid ECG signal is coming from the monitor
or the telemetry device. If you unplug the ECG patient cable from the monitor and plug it into the
telemetry device, the Information Center will automatically switch to monitoring the ECG from the
telemetry device. At the monitor, its own ECG measurement will be deactivated and the Setup ECG
menu will no longer be accessible.
When you unplug the patient cable from the telemetry device and plug it back into the monitor again,
the Information Center will switch back to monitoring the ECG from the monitor. The ECG
measurement will be activated again at the monitor. Note that in this case, as the screen switches back
to the monitor's own measurements, the SpO2T measurement (if present) will no longer be displayed.
In the same way the source is tracked when a telemetry device is directly connected to a monitor, then
disconnected and vice versa.
In case of ambiguity, a yellow INOP message !!CHECK ECG SOURCE indicates that more than one
valid ECG source is active.
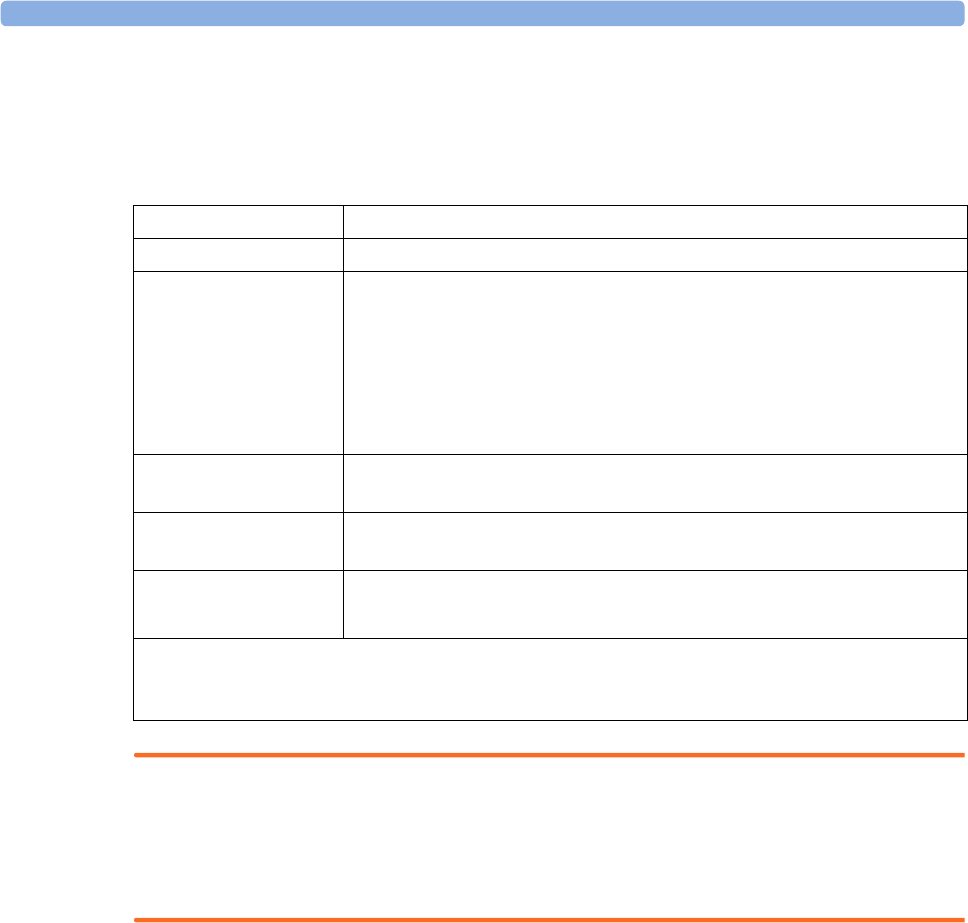
19 Assigning a Telemetry Device and a Monitor to One Patient
269
Synchronized Settings
If ECG is measured at the monitor, and then the patient is connected to a telemetry device for
monitoring, the Information Center will use the monitor settings for the telemetry device. In general,
the following settings will be synchronized:
WARNING
• Not all settings are synchronized; after changing the ECG source, always check that the settings
are appropriate.
• Va and Vb leads are reset to default (V2, V5) if the configured Va or Vb lead for the telemetry
device is not one of V1 through V6
If later the patient is disconnected from the telemetry device, and reconnected to the monitor again,
any changes in the settings made in the meantime will be passed on to the monitor. In this way,
settings continuity is preserved when the ECG source changes.
Settings synchronization can only take place when there is no patient information mismatch between
the monitor and the Information Center. If a Check ECG Settings or !! CHECK PAIRING INOP
appears always check that the ECG settings, especially the paced setting, are appropriate for your
patient.
Use Models With Telemetry
The standard use model combining a monitor and a telemetry device involves pairing the two devices
so that the data measured by the telemetry device appears on the monitor screen - and at the
Information Center in the same patient sector as the monitor data. The following variations are
possible:
1The monitor is paired with a telemetry transceiver - indirect connection
Heart Rate HR/Pulse Alarm On/Off, Heart Rate High/Low Limit,
ECG Primary Lead, Secondary Lead, Va Lead1, Vb Lead1, Lead Placement
Arrhythmia Analysis Mode, Asystole Threshold, Pause Threshold, VTach HR, VTach
Run, PVCs/min, Vent. Rhythm, SVT HR, SVT Run, PVCs/min On/Off,
Pacer not capture On/Off, Pacer not pace On/Off, Non-Sustain On/Off,
Vent. Rhythm On/Off, Run PVCs On/Off, Pair PVCs On/Off, Missed
Beat On/Off, Pause On/Off, R-on-T PVCs On/Off, Vent. Bigeminy On/
Off, Vent. Trigeminy On/Off, Multiform PVCs On/Off, Irregular HR
On/Off, SVT On/Off, Afib On/Off
ST ST Analysis On/Off, ST Alarm On/Off, ISO Point, J point, ST point, ST
Priority List, Single ST Alarm Limit, Multi ST Alarm Limit
QT QT analysis On/Off, QT Lead, QTc High Alarm On/Off, ΔQTc Alarm
On/Off, QTc High Limit, ΔQTc High Limit, QTc Formula2, QT Baseline
SpO2TSpO
2 Alarms on/off, SpO2 Alarm limits
NBP Alarm Suppression On/Off, Pulse(SpO2) On/Off
1Va and Vb leads are reset to default (V2, V5) if the configured Va or Vb lead for the telemetry device is not one of V1
through V6.
2This setting will only be synchronized when the Information Center supports QT Analysis for Telemetry

19 Assigning a Telemetry Device and a Monitor to One Patient
270
– telemetry data appear on the monitor
2An MP5 or X2 is declared as a telemetry device and paired with an MX600/700/800 monitor -
direct or indirect connection
– MP5/X2 measurement data appear on the monitor it is paired with
– a telemetry transceiver cannot be used with the MP5/X2
3A telemetry transceiver directly connected (SRR or for MP5 cable) to an MP5 or X2, that is
connected (Companion Mode) to an MX600/700/800 monitor - direct connection
– telemetry data appear on the host monitor
– telemetry transceiver is paired with the host monitor but is assigned to the MP5 or X2
–the MP5 or X2 must have no equipment label
The different variations require different configuration settings; refer to the Configuration Guide for
details.
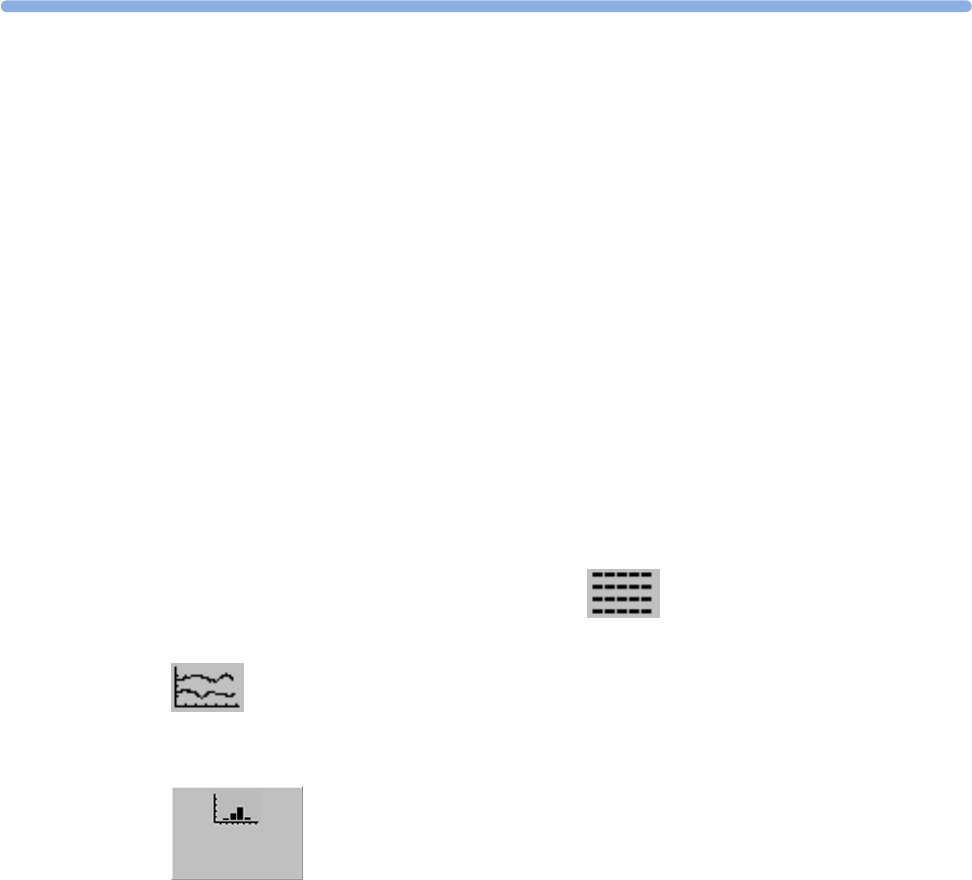
20
271
20Trends
Trends are patient data collected over time and displayed in graphic, tabular or histogram form to give
you a picture of how your patient's condition is developing. Trend information is stored in the trends
database for continuously-monitored measurements, such as ECG, as well as for aperiodically-
measured parameters, such as Cardiac Output.
Viewing Trends
Trend information can be viewed embedded as a screen element on specially-designed Screens, or you
can open a trend window over the current Screen.
• To view trends embedded as a screen element, enter the Change Screen window, then select a
Screen designed to show an embedded trend window.
• To open the tabular trends window over the current Screen, select Main Setup, Trends, then
Vitals Trend, or select the Vitals Trend SmartKey .
• To open the graphic trends window over the current Screen, select the Graph Trend SmartKey
.
• To open the histogram trend window over the current screen, select Main Setup, Trends, then
Histogram, or select the Histo- gram SmartKey.
The trend windows open displaying the most recent data and are updated as new data is stored. A
timescale along the bottom or the top of the screen shows you where you are in the trends database.
The preview column on the right-hand side shows the latest available measurement value. The preview
column is updated every five minutes or whenever an NBP or other aperiodic measurement is
completed.
A question mark (?) beside a value means that the data may not be reliable, due perhaps to an INOP
condition in the measurement.
Your monitor screen may look slightly different to the examples shown in this chapter.
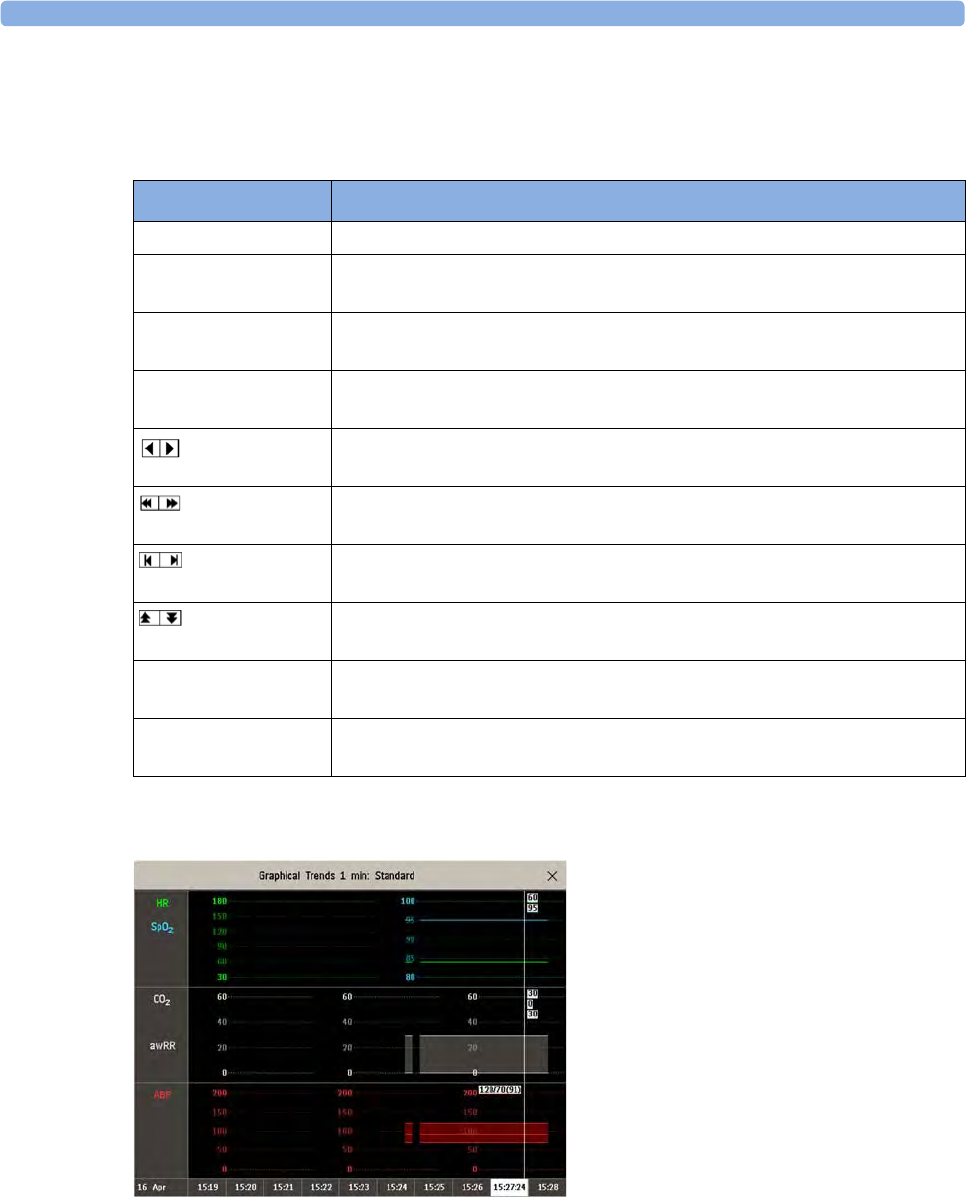
20 Trends
272
Trends Pop-Up Keys
When you open the graphic or tabular trends window, a selection of pop-up keys appears to let you
navigate through the stored trend data and carry out trends-related tasks.
Viewing Graphic Trends
A cursor spanning all measurements in the trend group helps you to navigate through the trends
database and shows you your current position in the database. When the cursor is moved across the
time line, the values measured at the cursor time are shown in the right hand column.
In graphical trends, aperiodic measurement trends are shown as an asterisk, NBP has a special symbol.
To use the trend cursor to navigate in time through the trends database,
Pop-Up Keys Selecting this pop-up key lets you....
Select Group see a pop-up list of trend groups and select a group for viewing.
Select Interval see a pop-up list of available data resolution settings and select the level of
detail shown in the trend view.
Print/ Record print a tabular trends report or make a tabular trend recording of the data in
the current window. The report will use the current trend interval settings.
Print print a graphic trends report of the data in the current window. The report
will use the current trend interval settings.
move the cursor one step to the left or right to navigate through the trends
database timeline.
move the cursor one page to the left or right to navigate through the trends
database timeline.
jump to the beginning or the end of the trends database to see the most
recent or oldest trend information stored.
scroll up and down the screen to see measurement trends that do not fit in
the current view.
Vital Signs open the current trend view in tabular form. The displayed time period and
resolution stay the same.
Graph Trend open the current trend view in graphic form. The displayed time period and
resolution stay the same.
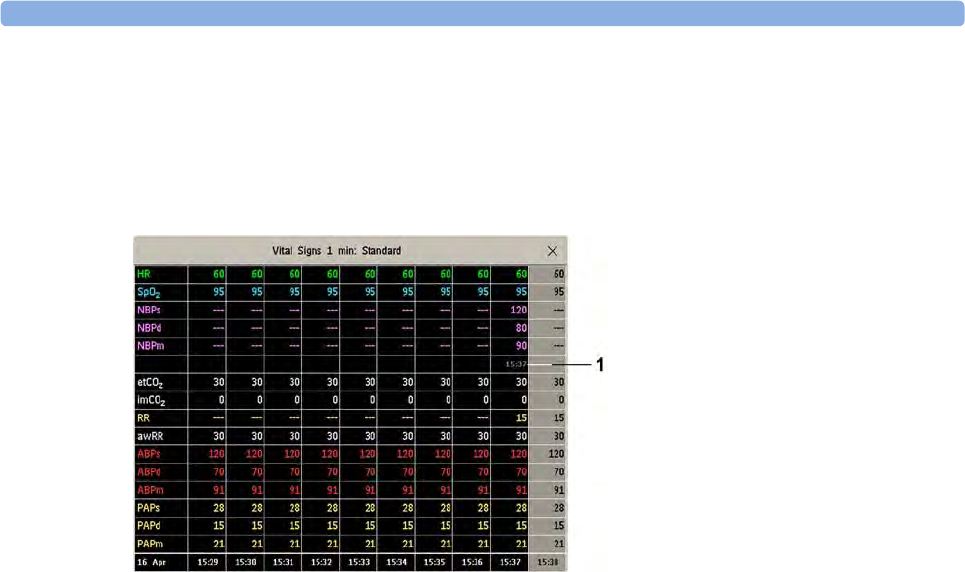
20 Trends
273
1Select the graphical trend or the arrow pop-up keys to activate the cursor.
2Use the arrow pop-up keys to move the trend cursor backwards and forwards in time, or
3Place the cursor at a specific time by touching the graph.
Viewing Vital Signs Trends
1Aperiodic values are shown with a timestamp
The currently-selected column is highlighted. The values can be configured to display in the same
colors as the waves and numerics on the realtime display.
Any values available for display before the next scheduled update are shown in the right hand column,
with a timestamp in brackets.
If more than one value is available for an aperiodic trend for a certain trend period, all measured values
are stored in the database and the value closest to the timestamp is shown in the Vital Signs display
marked with an arrow.
To view the Vital Signs trend with one column for each NBP measurement (see “Defining the Column
Interval Using the NBP Measurement” on page 277):
1With the Vital Signs trend open, select Interval.
2Select NBP from the pop-up list.
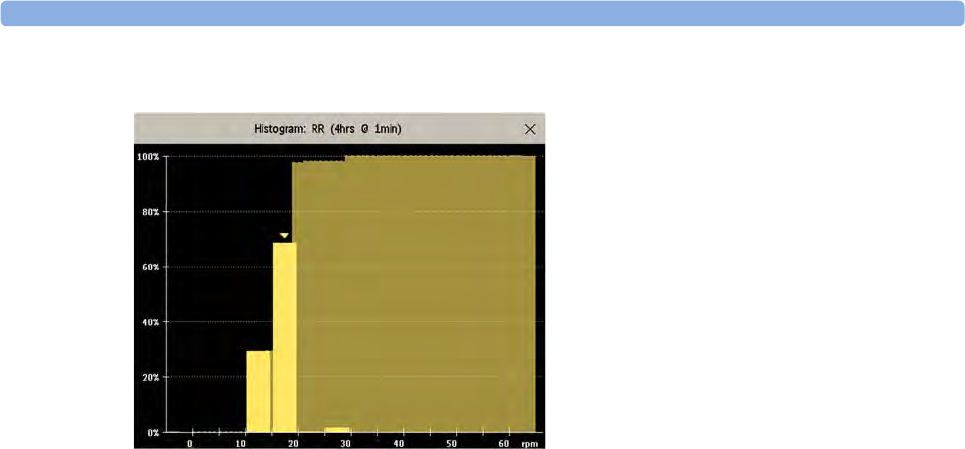
20 Trends
274
Viewing Histogram Trends
The title line of the window shows the label of the trended measurement and the resolution of the
data; in the RR histogram above, 1 minute trend samples.
The horizontal axis shows the range and unit of the displayed measurement. The vertical axis shows
the percentage of time.
The columns in the foreground show how much of the time the measured values fell into this range on
the scale. For example, in the histogram above, the RR value was between 15 and 20 rpm during 70%
of the last four hours. The arrow mark over that column shows that the currently measured value is
also in this range. These columns are displayed in the same color as the measurement data.
The columns in the background show the cumulative percentage value: each of the foreground
columns is added to the sum of those columns to the left of it.
A question mark is displayed if less than two-thirds of the data are valid samples.
The pop-up keys in the window can be used to change the measurement, the time period and the
range. You can also print out a histogram report.
The SpO2 histograms can be trend histograms or realtime histograms with 1 second samples. For
SpO2 realtime histograms, the range cannot be changed.
Setting Up Trends
Trends are set up in Configuration Mode. You can make temporary changes to trends settings such as
trend groups, priorities, or scales in Monitoring Mode. The general settings for all Trends are under
Main Setup, Trends.
Settings for a single segment in graphical trends or for the corresponding trend group can be made
more easily in that segment menu.
Making Segment Settings
The Graphical Trends window is divided into measurement segments, each of which has its own
settings.
To enter the segment menu,
• select the left hand column of the segment, where the measurement label is displayed.

20 Trends
275
Expanded View
To expand the segment to fill the Graphical Trends window,
•in the Segment menu, select Expand to have that segment enlarged to fill the window.
In the expanded view, you can also highlight a measurement to make it more easily visible (for example
when multiple ST trends are in one segment). To highlight a measurement,
•in the Segment menu, select Highlight repeatedly until the highlight is on the required
measurement.
To return the segment to its original size,
•in the Segment menu, select Expand again.
Trend Scales for Segment Measurements
To change the trend scales for a measurement in the current segment:
1In the Segment menu, select the measurement label
2Select Upper to change the upper limit of the scale or Lower to change the lower limit of the scale.
Optimum Scale
To have the monitor automatically select an optimum scale for viewing, based on current values,
•in the Segment menu, select Optimum Scale.
This scale change is temporary. When the graphical trend window is closed the scale reverts back to
the setting in Parameter Scales.
To switch off automatic optimum scaling,
•in the Segment menu, select Optimum Scale again.
Trend Group
To add or remove measurements for this trend group or change the order of the existing
measurements:
1In the Segment menu, select Change Group.
2Use the Add, Change, Sort Up and Sort Down pop-up keys to change or re-order the group as
required.
No. of Segments
In an embedded graphical trend window, you can select the number of segments to be displayed in the
Segment menu:
•In the Segment menu, select No. Of Segments.
Trend Groups
The measurements grouped in trend groups define the trends displayed together in the Vital Signs or
Graphical Trends windows and printed in trends reports and recordings. The sequence of the
measurements in the group defines the order in which they are displayed. Measurements listed
between dotted line separators are displayed overlapping. The trend group All contains all available
measurements, you cannot change the order or selection of this group.

20 Trends
276
To change the selection of measurements in a trend group, either use the Change Group setting in the
Segment menu or:
1Select Main Setup, Trends, then Trend Groups.
2Select the Trend Group you want to change and use the pop-up keys to Add, Change, or Delete
the selection of measurements trended.
To temporarily change the order in which the measurements are displayed in a group,
1Select Main Setup, Trends, then Trend Groups.
2Select the Trend Group and then the measurement you want to move and use the Sort Up/Sort
Down pop-up keys.
Trend Interval
The trend interval defines the resolution of trend data shown on the Screen. High-resolution data is
especially suited for neonatal applications, where the clinical situation may change very quickly. In
adult monitoring, where the patient's status typically changes more gradually, a longer trend may be
more informative.
To set the trend resolution, in the Vital Signs or Graphical Trends window,
• Select the Select Interval pop-up key and then select the required interval from the list.
Trend Priority
The monitor stores trend information for all monitored measurements, if configured to do so. (Data
from VueLink or IntelliBridge modules cannot be included in trends when the label is a free-text label.)
If your configuration restricts the number of measurements trended, you must choose which
measurements will be included. A priority list is used to select the trended measurements.
To see the measurement priority list for trending,
1In the Main Setup menu, select Trends.
2Select Trend Priority.
To add measurements to the priority list,
1Select the pop-up key Add and choose from the pop-up list of available measurements.
2Use the Sort Up and Sort Down pop-up keys to change the priority order.
Trend Parameter Scales
Parameter scales define how the trend waveform will appear on the screen and in trend reports.
Separate scales can be set for adult, pediatric, and neonatal patient trends.
To change the trend parameter scales settings, either use the Scale setting in the Segment menu or:
1In the Main Setup menu, select Trends.
2Select Parameter Scales.
3Select the measurement or parameter you want to change from the list.
4Select the pop-up key Change to call up the Scale menu.
5In the Scale menu, select the parameter label you want to define settings for. Select Adult, Pedi,
and Neo and use the pop-up keypad to enter new upper and lower scale definitions.
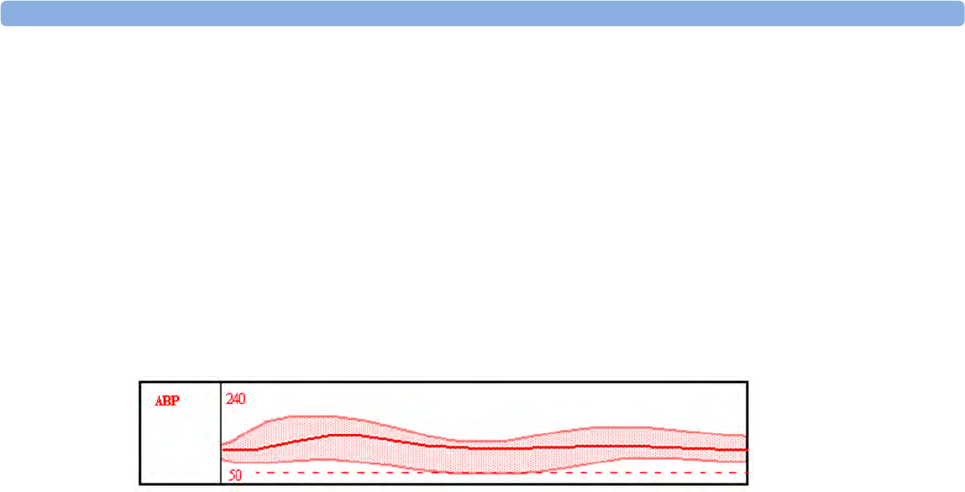
20 Trends
277
Graphical Trend Presentation
Graphical trends and screen trends for measurements with compound values (for example ABP or
CO2) can be viewed in line or band form.
To change the presentation style,
1Select Main Setup then select Trends.
2Select Global Style and choose
•Line to display the trends as a continuous line
•Band to fill the area between the trend lines, for example, between the systolic and diastolic
pressures, with color.
This sample ABP trend shows the continuously-measured values for the systolic, diastolic and mean
pressures displayed in band form.
Defining the Column Interval Using the NBP Measurement
You can have the NBP measurement determine the interval between the columns on the Vital Signs
trend. Each NBP measurement will generate a column in the trend table. The values for the other
measurements are added to the column to provide a complete vital signs set for the NBP measurement
time.
To use the NBP measurement to determine the column interval:
1Select Main Setup then Trends.
2In the Trends menu, select Setup VitalSigns.
3In the Vital Signs menu, select Column and then NBP from the pop-up menu.
Setting Measurement and Period for Histograms
To set the default for the measurement data to be used in the histogram,
1Select Main Setup then select Trends.
2Select Setup Histogram.
3Select Data Source.
4Select either a realtime SpO2 or Trended Data. From the trended data list select the required
measurement.
To set the default period for the histogram,
1Select Main Setup then select Trends.
2Select Histogram.
3Select Select Period and select the required time period from the list.
When viewing a histogram, the data source, the period and the range can be changed using the pop-up
keys.
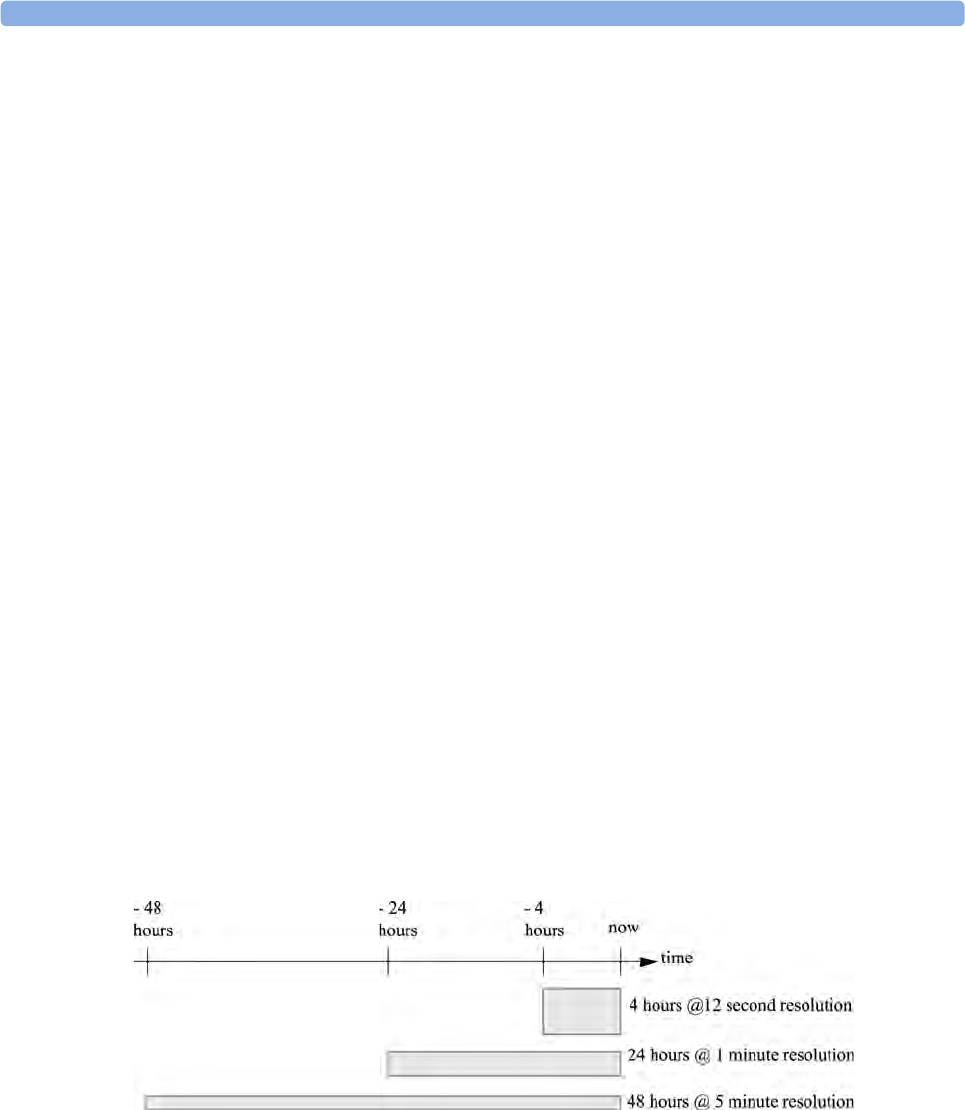
20 Trends
278
Documenting Trends
To print a Vital Signs or Graphical Trends report,
•in the Vital Signs or Graph Trends window, select the pop-up key Print to print a report for the
trend group currently on the monitor screen.
Reports include the most recent information in the trends database and extend backwards in time
according to the selected trend interval and your monitor's configuration. Trends reports can be
printed on central or local printers.
To make a Vital Signs recording,
•in the Vital Signs window, select the Print/ Record pop-up key, then select the Record Vitals pop-
up key.
Vital Signs recordings print the trend data for the current group and trend period shown in the Vital
Signs window.
Trends Databases
Depending on the purchased options and the monitor's configuration, the trends databases store
information for up to 32 measurements for up to 72 hours.
The values in the trends database are stored as measured by the monitor, they are not averaged values.
The trend resolution defines how often a value is stored. In general, if more than one value is available
for storage in the trends database, the most recent value is used. Some values in the trends are marked
with arrows. This indicates that for this time period, more values were available and the most recent
one is shown.
Example database configuration
In this example, we see that the monitor stores the most recent data at the highest resolution, older
data are stored at a lower resolution.
"4 hours @ 12 second resolution" means that the monitor stores trend data every 12 seconds, for the
most recent four hours.
Aperiodic Trends Database
Aperiodic trends do not count toward the maximum number of trends allowed by the trend
configuration. Trend data for aperiodic measurements is stored in a separate database and
timestamped with the measurement time.

20 Trends
279
Trending Multiple-Value Measurements
Some measurements generate multiple values, for example invasive pressure measurements can
provide systolic, diastolic, and mean values. These values are trended as separate measurements.
Screen Trends
Trends configured to display permanently on special monitor Screens are called screen trends. The
selection and number of measurement waves in the Screen Trend segment depends on your monitor
configuration. Screen trends are color-coded to match the measurement wave and numerics, and they
can be viewed in graphical, tabular, histogram or horizon format.
If you do not see screen trends on the monitor Screen, select a different Screen, one that is configured
to show screen trends. Screen trends are only available on specially designed Screens.
Screen Trend information is taken from the Trends database. If you do not see a Screen Trend for a
particular measurement on the Screen, check the trend priority list to ensure that this measurement is
being trended.
Setting the Screen Trend Time
To set the ScreenTrend Time for all graphical, histogram and horizon screen trends ("global" trend
time),
1Select a screen trend then select Setup Trend, or select Main Setup then select Trends.
2Select ScreenTrend Time and select the required time: 30 minutes, one, two, four, eight, or twelve
hours.
This is now the Global screen trend time and defines the period of trend information shown for
all screen trends.
To set a different ScreenTrend Time for a screen trend or a group of aligned screen trends,
1Select a screen trend.
2Select Change TrendTime
3Select the required trend time.
Selecting Global leaves the trend time set to the global screen trend time.
Changing the Selection of Screen Trends Displayed
1Select the screen trend.
2Select Change Trend and select the required trend from the list of available trends.
Select Blank to remove the selected trend from the Screen.
If you do not see Change Trend in the screen trend menu, the trend is aligned to display with the
measurement wave. Changing the wave automatically changes the trend.
To display two or more screen trends overlapping,
1Select the screen trend to open the screen trend menu,
2Select Change Trend followed by Add Trend and select a screen trend from the pop-up list.
Activating the Cursor for Screen Trends
To activate the cursor for Screen Trends:
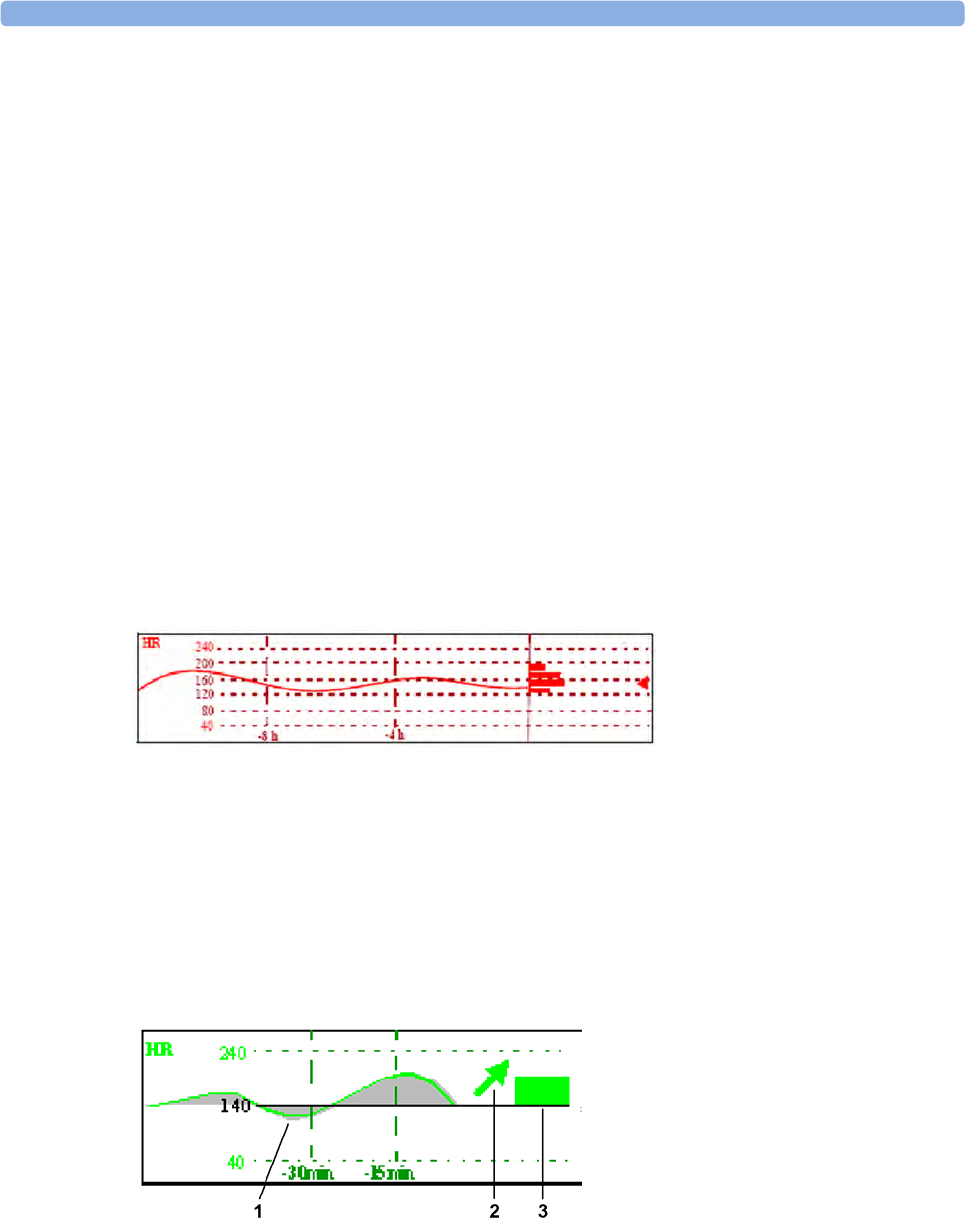
20 Trends
280
1Select the screen trend.
2Select Activate Cursor.
You can now use the arrow keys to move the cursor across the time line. The values measured at the
cursor time are shown next to the cursor.
To de-activate the cursor,
•Select
Main Screen.
Changing the Screen Trend View
To switch between tabular, graphic, histogram and horizon views, select the screen trend then select
Change View and select the required view.
Tabular View
Aperiodic measurements such as NBP, C.O., C.I., and Wedge can be viewed as a screen trend in
tabular form. The measured values and their timestamps are shown, with the measurement label.
The trend time for tabular screen trends depends on the space available on the Screen. Up to 30
measurements or 12 hours information can be shown.
Histogram View
The histogram view presents a combination of graphical trend and histogram. The histogram is on the
right hand side in a horizontal presentation with vertical gridlines representing 25%, 50%, 75% and
100%. Each column shows the percentage of time that the measurement values were in a specific
range. This range is represented by the column's position in the graphical trend gridlines. The arrow
mark next to a column shows that the currently measured value is in the range covered by that column.
If less than two-thirds of the samples are valid, a question mark will be displayed with the histogram,
except when the histogram consists of intermittently measured data.
Horizon View
The horizon view presents trend information superimposed over a defined baseline or base range. This
helps you visualize changes in your patient's condition since the baseline was set.
The horizon view is made up of:

20 Trends
281
• a horizon, drawn in white, as a reference point or baseline to help you visualize changes in your
patient's condition. The horizon can be set to represent your patient's current condition, or a
target condition and can be a single value or a range.
• a graphical trend, displaying patient data for the set TrendTime (1).
• a trend indicator arrow, indicating how the patient trend has developed in the set time period
(10minutes, 5minutes or 2minutes) (2).
• a deviation bar, showing how the currently measured value deviates from the set horizon (3). The
height of the deviation bar is an indication of the extent of the change in your patient's condition
relative to the (horizon) baseline.
Your monitor may not be configured to show all elements of the screen trend horizon view.
Setting the Horizon
The horizon is the reference value to which deviations in the measurements are compared.
1To set the horizon, select the horizon trend.
2Select
–Set High Horizon to select the upper horizon value. If the high and low horizon values are the
same, the horizon is a baseline - if the values are different the horizon is a range.
–Set Low Horizon to select the lower horizon value.
–Auto Horizon to set the horizon for the selected horizon trend to the currently-measured
value.
–Auto All to reset the horizon for all horizon screen trends to the currently-measured values.
–Set Horizon to set the horizon to a specific value from a pop-up list.
Setting the Horizon Trend Scale
The horizon trend scale is defined with respect to the horizon. If your horizon is set to 100 and you
select 20 as the horizon scale delta, the upper limit of the horizon scale will be 120 and lower limit 80.
To set the horizon trend scale delta,
1Select the horizon trend.
2Select Set Scale Delta and select a value to define the distance between the horizon and the upper
and lower scale limits.
Be aware that changing the horizon trend scale can change the angle of the trend indicator, without the
patient's condition having changed.
If a measurement exceeds the outer limits of the scale, the wave will be clipped and you must either
reset the horizon or the horizon trend scale to display the values outside the scale limits.
Setting the Time Period for the Trend Indicator Arrow
The time period for which the trend indicator arrow is displayed can be set in the Trends window.
1Select Main Setup then select Trends.
2Select HorizonArrowTime.
3Select 10, 5 or 2 minutes.

20 Trends
282
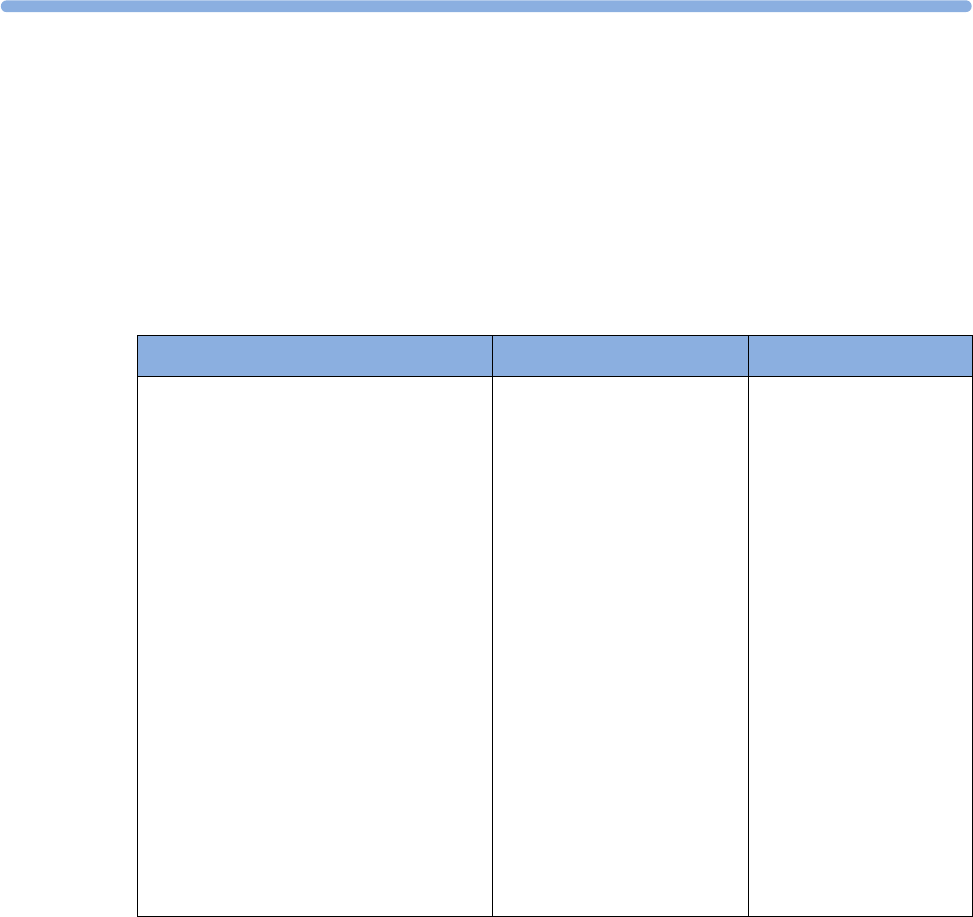
21
283
21Calculations
Calculations are patient data that is not directly measured but calculated by the monitor when you
provide it with the appropriate information.
Your monitor can perform the following hemodynamic, oxygenation, and ventilation calculations.
The hemodynamic calculations available depend on the Cardiac Output measurement method being
used and the regulatory standards that apply for your hospital: see the Monitoring Cardiac Output
chapter for availability details.
Hemodynamic Oxygenation Ventilation
Cardiac Index (C.I.)
Stroke Volume (SV)
Stroke Index (SI)
Systemic Vascular Resistance (SVR)
Systemic Vascular Resistance Index (SVRI)
Pulmonary Vascular Resistance (PVR)
Pulmonary Vascular Resistance Index (PVRI)
Left Cardiac Work (LCW)
Left Cardiac Work Index (LCWI)
Left Ventricular Stroke Work (LVSW)
Left Ventricular Stroke Work Index (LVSWI)
Right Cardiac Work (RCW)
Right Cardiac Work Index (RCWI)
Right Ventricular Stroke Work (RVSW)
Right Ventricular Stroke Work Index (RVSWI)
Extra Vascular Lung Water Index (EVLWI)
Intrathoracic Blood Volume Index (ITBVI)
Global End Diastolic Volume Index (GEDVI)
Arterial Oxygen Content (CaO2)
Venous Oxygen Content (CvO2)
Arteriovenous Oxygen Content
(CavO2)
Oxygen Availability Index (DO2I)
Oxygen Consumption (VO2)
Oxygen Consumption Index
(VO2I)
Oxygen Extraction Ratio (O2ER)
Alveolar-Arterial Oxygen
Difference (AaDO2)
Percent Arteriovenous Shunt
(Qs/Qt)
Minute Volume (MINVOL)
Compliance (COMP)
Dead Space (Vd)
Dead Space/Tidal Volume
Ratio (Vd/Vt)
Alveolar Ventilation
(ALVENT)
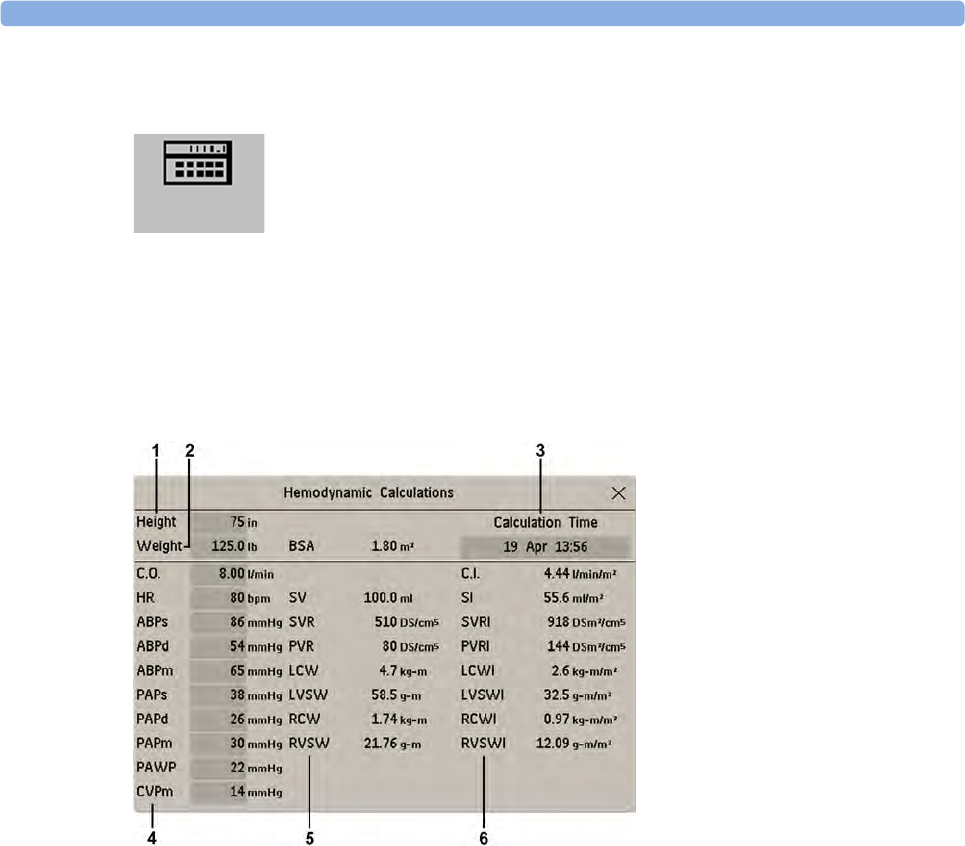
21 Calculations
284
Viewing Calculations
• Select the Calcs SmartKey to open the Calculations window.
• Select the Calc Type field and select the required calculation type for display.
Calculations Windows
This example calculations window shows the Hemodynamic Calculations window. The ventilation
and oxygenation windows are similar.
1Height used for the calculations
2Weight used for the calculations
3Calculation Time
4Calculations input values
5Output values
6Indexed calculation values
Calculations Pop-Up Keys
Depending on the calculations group you choose, a selection of pop-up keys will appear to let you
navigate through the stored events and carry out calculations-related tasks.
21 Calculations
285
Reviewing Calculations
To enter the calculations review window, select the Oxygen Review, Vent Review, or Hemo Review
pop-up key as required.
The review window lists all the input and output values for each measurement in the calculations
group. The timeline in the review window lists the times the calculations were performed.
To review individual calculations, select the calculation in the review window and then select the
Original Calc pop-up key.
The storage time for calculations is the same as the trend database storage time configured for the
monitor. So if trends are stored for 48 hours, the calculations will also be stored for 48 hours.
Performing Calculations
You must check that all input values are appropriate for your patient before performing calculations.
1Select the Calcs SmartKey to open the Calculations window.
2Check the calculation time in the Calc Time field.
When you enter the calculation window, this field will show either the current time or the time of
the most recent available C.O. measurement, depending on your monitor configuration.
– To choose a different calculation time, select the Calc Time field. This calls up a list showing
the timestamps of calculations performed earlier. Select a time from this list, or select Select
Time to enter a time of your choice. The values from the Vital Signs database from the 30
minute period before the selected time will be used.
– To enter the current time, select the Resample Vitals pop-up key. If you choose the current
time, the monitor will resample all the required values that are monitored.
3Enter any values that must be entered or edited manually. Select the value field and then use the
pop-up keypad to enter the required values. Select Enter to confirm each entered value. Manually-
entered values are marked with an asterisk (*).
Pop-Up Keys Selecting this pop-up key lets you....
Resample Vitals use the most recent monitored values. Resampling sets the calculation time to
the current time, and displays the corresponding values for the previous
second.
Perform Calc perform the displayed calculation using the currently-input values and store the
calculation in the calculations database
Print/Record print or record the displayed calculation.
On/Off DateTime toggle between showing the date and time or the units for the calculation input
values.
On/Off Ranges toggle between showing the normal ranges or the units for the calculation
output values.
Cardiac Output access the C.O. procedure window.
Hemo Review open the hemodynamic calculations review window.
Vent Review open the ventilation calculations review window.
Oxygen Review open the oxygenation calculations review window.

21 Calculations
286
Entering Values for Calculations
The monitor automatically enters any available values for calculations. For aperiodically-measured
values such as C.O., the monitor will re-use the most recent value in the calculation database until a
new value becomes available. If the calculation time is the last C.O. time, values will be used from up
to and including 30 minutes before the C.O. time, except for height and weight where the last available
value will be used.
• To enter calculations values manually or edit automatically-entered values, select the value field to
open the on-screen keyboard and use this to enter the correct value. Values edited manually are
marked with an asterisk (*).
If you enter a value that has more decimal places than allowed for a particular input, the value you
enter will be rounded off after you select Enter. If you enter a value which cannot be stored, the
message Value out of range will appear. Enter a new value.
In hemodynamic calculations, if the systolic and diastolic pressures are manually entered, the mean
pressure is calculated and marked with an asterisk (*). The formula used to estimate the mean pressure
is [systolic + (diastolic x 2)] / 3.
Automatic Value Substitution
If the monitor cannot find a value required for calculation, it automatically tries to find an equivalent
source for this value. For example, if C.O. is required but unavailable, the monitor automatically looks
for CCO as a alternative source of C.O. values, or an alternative Pressure label may be used instead of
ABP. The label of the value in the Calculations window does not change. Substituted values are
marked with an asterisk (*).
Automatic Unit Conversion
The monitor needs consistent units for performing calculations. It automatically converts units where
necessary before it performs the calculation, for example, pressures sourced in kPa, cmH2O, or mbar
are automatically converted to mmHg, or to cmH2O for ventilation calculations.
Manual Unit Conversion
If you need to convert units for other purposes you can use the Unit Conversion window:
1Select Main Setup then select Calculations.
2Select Unit Conversion.
3Select the field under the unit you know and use the on-screen keypad to enter the known value.
The converted value automatically appears in the adjacent field.
BSA Formula
Your monitor provides both the Boyd and Dubois formulas for the calculation of body surface area
(BSA). For calculations, the monitor uses the setting defined in the Patient Demographics menu. All
calculation results that use BSA are indexed to the selected formula.
• To check the current setting, select the patient name to enter the Patient Demographics menu.
BSA(B) indicates that the Boyd formula is used; BSA(D) indicates that the Dubois formula is used.
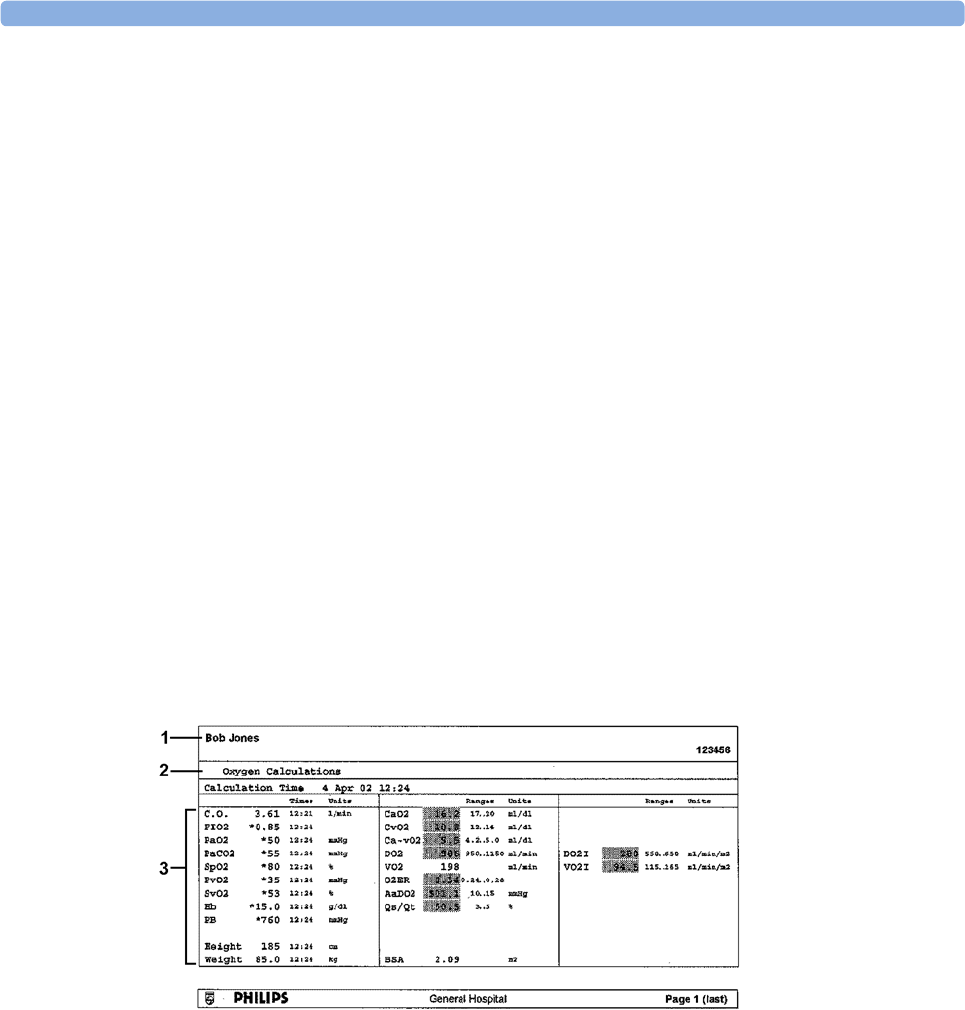
21 Calculations
287
Comparing Dynamic Compliance Values
If you compare the dynamic compliance value (COMP) from the ventilation calculations with the
value from the Spirometry measurement you may see a difference. This comes from the different
sampling methods:
• The algorithm in the ventilation calculations takes into account only two sets of paired AWP/
AWV data: those from complete expiration and complete inspiration, when AWF is zero.
• The algorithm in the Spirometry application takes into account all sets of paired AWP/AWV data
(125Hz sampling rate), over one complete breath cycle, and calculates an "averaged" compliance
using a least square method.
Documenting Calculations
To send a Calculations recording to a connected recorder, in the Calculations window, select the
Print/ Record pop-up key, then select the Record Calc pop-up key.
Calculations recordings print the patient demographic information and the content of the current
Calculations window on the recorder strip.
To print a report for the calculation group currently on the monitor screen, select the pop-up key Print
Calc. To print the review window, select the pop-up key Print in the review window. All the
calculations in the current group will be printed in the report.
Calculation reports can be printed on central or local printers.
This example report shows the oxygen calculation group. Ventilation and hemodynamic calculation
reports are similar.
1Patient information
2Calculation group
3Three columns of calculations input and output values, with times, units and ranges, where
appropriate

21 Calculations
288

22
289
22High Resolution Trend Waves
High resolution (hi-res) trend waves provide information for fast-changing parameters at a glance.
They can help you to recognize trend patterns and to find interrelationships between measurements,
by comparing changes in your patient's condition across different hi-res trend waves.This can aid in the
early detection of cardiorespiratory and hemodynamic problems.
The amount of data you can show on a screen depends on the display size and resolution: for example,
on an eight inch (20 cm) wave trace on your monitor screen, you can view approximately six minutes
of hi-res trend wave trace. The hi-res waves are drawn at a speed of 3 cm/minute.
The availability of hi-res trend waves depends on your monitor configuration and on the options
purchased for your monitor.
Changing the Hi-Res Trend Waves Displayed
To change the selection of hi-res trend waves on the Screen:
1Select a displayed hi-res trend wave.
2Select the required hi-res trend wave from the pop-up list.
If there are no hi-res trend waves on the Screen, you must change to a Screen with hi-res trend waves.
Hi-Res Trend Wave Scales
Hi-res trend waves are either compressed realtime waves or fast numeric trends.
• Hi-res trend waves from compressed realtime waves include: Resp, CO2, AB P, PAP, CV P, ICP,
AWP, anesthetic agents.
• Hi-res trend waves from fast numeric trends include: btbHR, SpO2, tcpO2, tcpCO2, Pulse, Perf,
CPP, BIS, CCO, inO2, Delta SpO2.
Hi-res trend waves from realtime waves use the wave scale as their display scale. Changing the wave
scale changes the hi-res trend wave scale.
Hi-res trend waves from numerics use a pre-defined display scale dependent on the patient category.
Hi-Res Trend Waves and OxyCRG
OxyCRG is a combination of three hi-res trend waves, btbHR, SpO2, and Resp, mainly used in
neonatal monitoring.
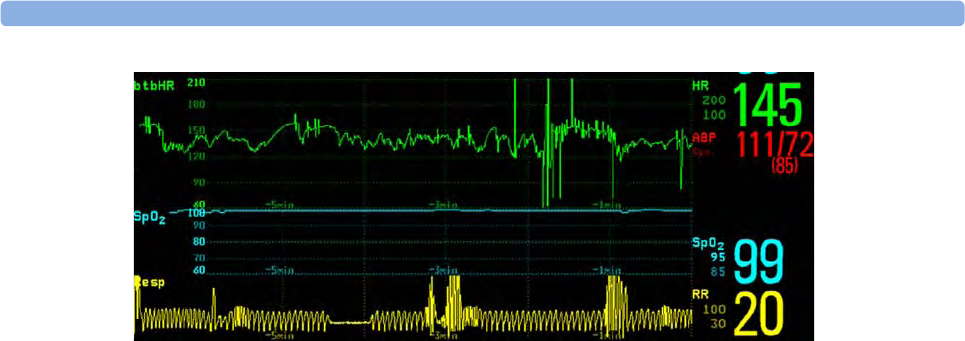
22 High Resolution Trend Waves
290
Printing Hi-Res Trend Wave Reports
To print hi-res trend waves on reports, you can choose to print either
• all VisibleWaves - prints all waves and hi-res trend waves currently displayed
•All Waves - prints realtime waves and hi-res trend waves for all currently-monitored measurements
•HiRes Waves - prints hi-res trend waves for the currently-monitored measurements
•OxyCRG Waves - prints hi-res trend waves for btbHR, SpO2, and Resp.
For each hi-res trend wave, a maximum of six minutes of measurement data will be printed.
See the Printing Patient Reports chapter for more information on setting up reports.
Hi-Res Trend Wave Recordings
The selection of waves in hi-res trend wave recordings and the recording speed are defined by the pre-
configured HiResTrd recording template. See the Recording chapter for more information.
To start a hi-res trend waves recording,
1select the Recor- dings SmartKey, if configured, or select Main Setup then select Recordings.
2select the HiRes Recordng pop-up key.

23
291
23Event Surveillance
Events are electronic records of episodes in your patient's condition. You can trigger them manually,
or set them to trigger automatically during pre-defined clinical situations.
Depending on the level of event surveillance available on your monitor, the information stored for
each event episode can include:
• waveforms for up to four measurements of your choice (depending on episode type, see “Events
Pop-Up Keys” on page 293 for more details)
• numeric vital signs for all the measurements monitored
• any alarm conditions active when the event episode was triggered
• any annotations connected with the event.
You can navigate through the event database to view events retrospectively, and you can document
events on a recording or report marked with the patient name, bed label, and the data and time.
When an MP5 is connected to a host monitor, event surveillance will be disabled. No new events will
be detected and no existing events will be deleted. There is no data exchange between the host monitor
and the MP5 for event surveillance. When the MP5 is disconnected from the host monitor event
surveillance will resume and new events will be detected.
Levels of Event Surveillance
The appearance of the Events windows and menus and the settings you can select for events depends
on the event surveillance option purchased for your monitor: basic event surveillance, advanced event
surveillance, or neonatal event review (NER). This table lists the differences between the options.
To determine which level of event surveillance your monitor has, select Main Setup then Event
Surveill. followed by Setup Events and select the trigger group to see the available event groups.
• if the only event group listed is NER, your monitor has the Neonatal Event Review option
• if there is one event group and it is not NER, your monitor has the Basic Event Surveillance option
• if you see six event groups, your monitor has the Advanced Event Surveillance option.
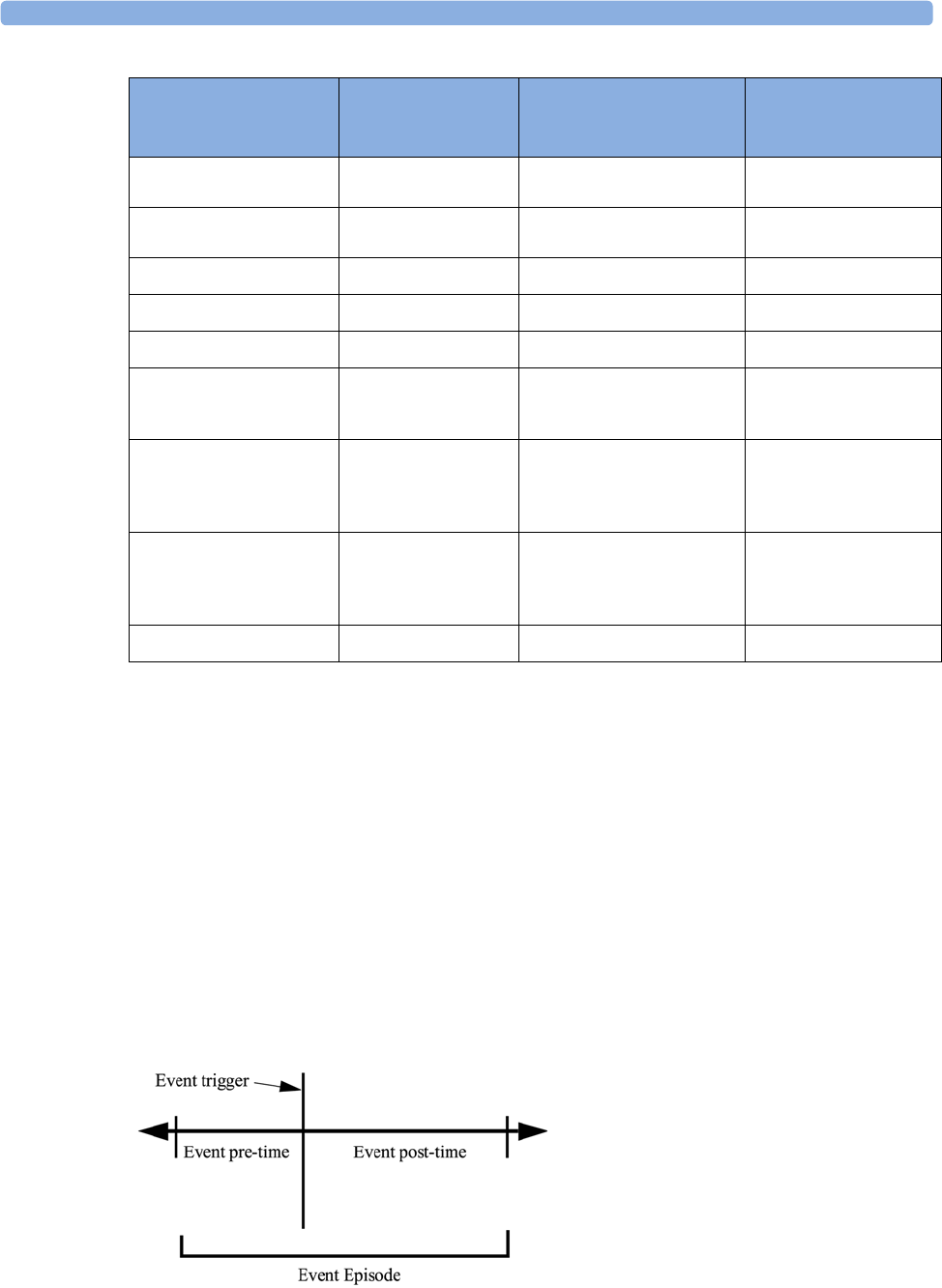
23 Event Surveillance
292
Event Groups
The event group
• monitors the patient's signals to detect event triggers
• defines which waveforms are recorded in the event data.
In basic event surveillance only one event group can be active at a time, with Advanced Event
Surveillance all six groups can be active simultaneously. Active event groups monitor for event triggers.
Event groups are defined in Configuration Mode. In monitoring mode the groups can be adapted to
current conditions, for example episode types and threshold levels can be changed.
Event Episodes
Event Functionality
Basic Event
Surveillance
Option C06
Advanced Event Surveillance
Option C07
Neonatal Event Review
(NER)
Option C04
Event groups 1 6 (one group can be configured
to NER)
NER
Measurements per group 3 4 3 (plus 1 for episode
recording)
Triggers per measurement 12 1
Trigger types Simple ("at least one") Combined ("at least two") Simple ("at least one")
Annotation no yes yes
Types of event episode
Average trend
Snapshot events
Average trend
High resolution trend
Snapshot events
High Resolution Trend
Event views
Graphic Event Review
window, Graphic Event
Episode window
Summary view, graphic and
tabular Event Review window,
graphic and tabular Event
Episode window
Graphic and tabular Event
Review window, graphic
and tabular Event Episode
window
Database capability
25 events for 24 hours 25 events for 24 hours
25 events for 8 hours
50 events for 8 hours
50 events for 24 hours
25 events for 24 hours
25 events for 8 hours
50 events for 8 hours
50 events for 24 hours
Event Notification no yes no
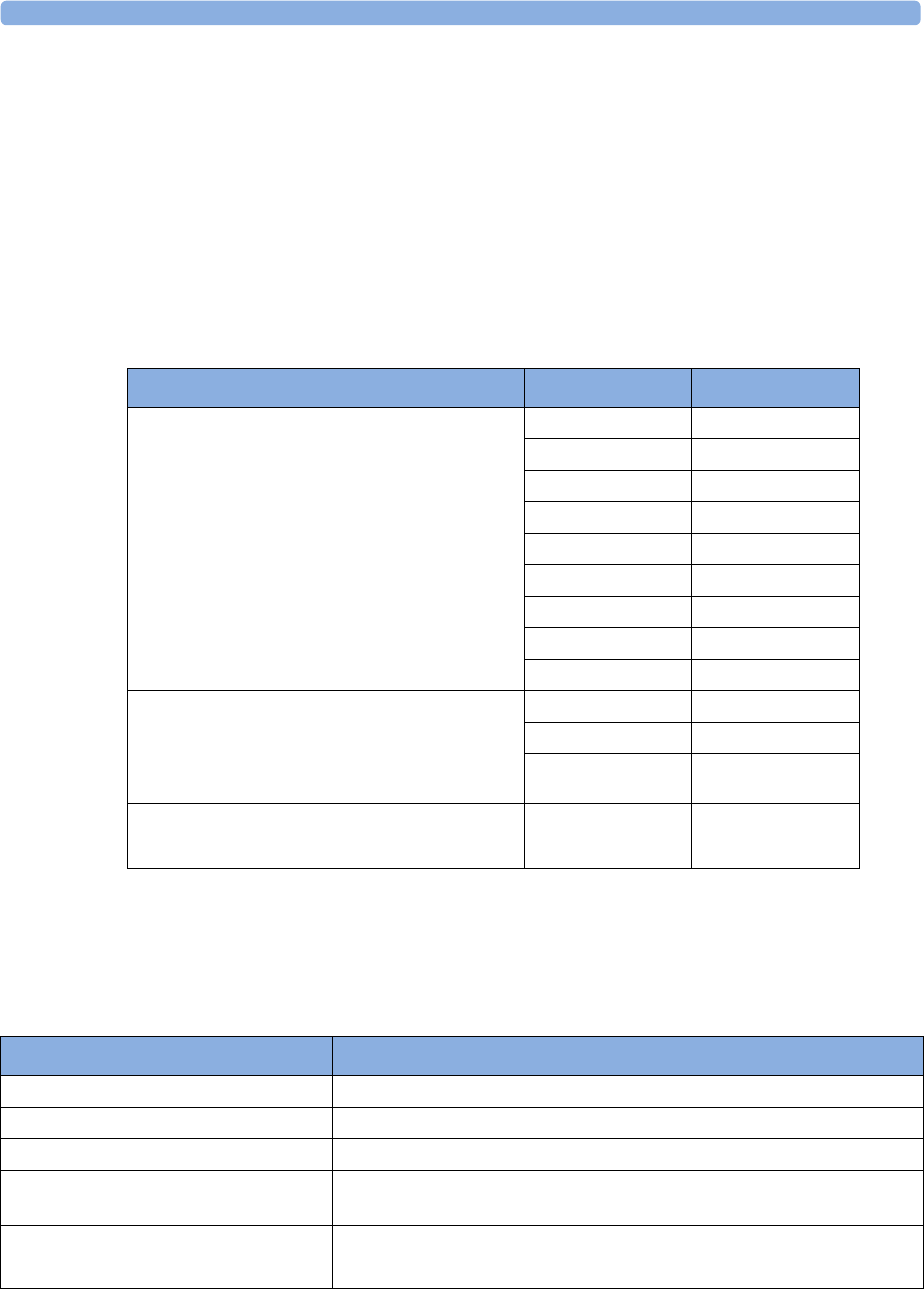
23 Event Surveillance
293
When an event occurs, information for a predefined duration is stored. This is the event episode. It
includes information from a defined period before the trigger, called the event pre-time. The episode
time after the event is called the event post-time. If a further event occurs during the event post-time it
changes a single event to a combined event (combi-event).
Manually-triggered event episodes document patient information from the time leading up to the event
trigger; they do not have a post-time.
The episode type defines the level of detail captured in an event episode. The higher the data
resolution, the shorter the period that the monitor can store in its memory. High-resolution data is
suited for neonatal applications, where the clinical situation may change very quickly. In adult
monitoring, where the patient's status typically changes more gradually, a longer trend may be more
informative.
Events Pop-Up Keys
Depending on the events view you choose, a selection of the events pop-up keys let you navigate
through the stored events and carry out events-related tasks.
Event Episode Types Pre-time Post-time
Average trend
20 minutes, five samples per minute
2 minutes 18 minutes
4 minutes 16 minutes
6 minutes 14 minutes
8 minutes 12 minutes
10 minutes 10 minutes
12 minutes 8 minutes
14 minutes 6 minutes
16 minutes 4 minutes
18 minutes 2 minutes
HiResTrend
Four minutes, four samples per second.
Neonatal Event Review (NER) is a type of
HiResTrend
1 minute 3 minutes
2 minutes 2 minutes
3 minutes 1 minute
Realtime Wave Snapshot
15 seconds
5 seconds 10 seconds
10 seconds 5 seconds
Pop-Up Keys Selecting this pop-up key lets you....
Event Setup open the Event Setup menu.
Show Episode open the Event Episode window to review the selected event in detail.
Show Review open the Event Review window.
Review Group choose a different event group for reviewing in the Event Review window
(Advanced Event Surveillance only).
Show Summary open the Event Summary window.
Manual Event start a manually-triggered event capture.
23 Event Surveillance
294
Event Triggers
You can trigger event capture manually, for example, if you want to record a patient's condition before
a procedure. You can also set events to trigger automatically, when the patient's values cross a
predefined threshold value, or when a particular measurement or procedure is carried out.
If more than one trigger is available for the measurements in the active event group, the trigger
condition may be At Least One Param., At Least Two Param., At Least Three Par., or All Four
Parameter. If the trigger is At Least One Param. (this is short for "at least one measurement
parameter"), the monitor starts an event capture if a trigger occurs in any of this event group's
measurements. If the trigger is At Least Three Par., the monitor captures events when three or more
trigger thresholds from this event group's measurements are violated. With Enhanced Condition you
can not only select a minimum number of triggers to trigger an event but define which specific
measurement triggers these must be. For example, At Least Two Param. will cause an event to be
captured if a trigger occurs in any two of this event group's measurements - with Enhanced Condition
you can select that only when triggers are in HR and SpO2 an event will be captured.
Start CAR Stop CAR open the Start CAR window to start a Car seat Assessment Record (CAR)
period or stop a currently running CAR.
CAR Histogrm open the window showing the CAR SpO2 histogram
move the cursor left or right to the next event to navigate through the
events database. Placing the cursor over an event highlights it and shows
the event values for the selected event.
jump to the first or last event in the event database.
Vitals View Graphic
View
toggle between a tabular and graphic version of the Event Episode window
currently viewed.
Table
Review
Graphic
Review
CAR
Review
toggle between a tabular and graphic version of the Event Review window
currently viewed.
Delete Event delete the currently-selected event from the database. The monitor asks
you to confirm this deletion. You cannot retrieve deleted events.
Select Annotatn access the list of available annotations to add a nursing note for the current
event episode (Advanced Event Surveillance only).
Print/ Record access the printing and recording pop-up keys to document events.
Pop-Up Keys Selecting this pop-up key lets you....
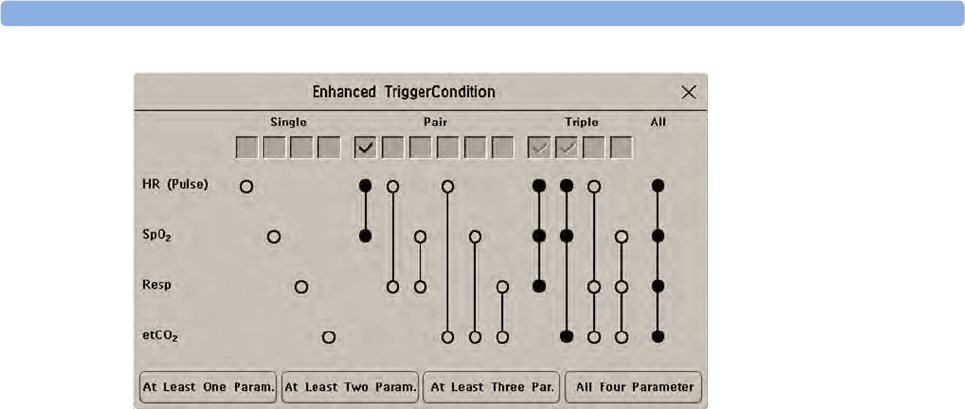
23 Event Surveillance
295
The trigger condition for event groups is set in the monitor's Configuration Mode.
If You Use Alarm Limits As Event Triggers
The event capture is triggered automatically when your patient's values violate set alarm limits, or when
a specified alarm condition, such as apnea, occurs. No events of this kind are triggered if alarms are
switched off. Changing alarm limits changes the event trigger definitions.
The asterisk symbols beside the trigger tell you about the alarm triggers:
*** indicates a high priority (red) alarm
** indicates a lower priority (yellow) alarm. This category includes short yellow arrhythmia alarms,
which may be configured to be shown as one star alarms (*) on your monitor.
Triggers without asterisk symbols are user-defined triggers.
If You Set User-defined Threshold Triggers
You can define event triggers that are independent of alarm limits. You must set a threshold value and
a threshold time for the trigger. If you set the trigger threshold time to 12 seconds, the monitor triggers
an event if the threshold is violated for more than 12 seconds.
If You Set "On Measurement" Triggers
You can set aperiodic measurements (such as NBP) or procedures (such as Cardiac Output) to trigger
an event whenever they start.
If You Set Use-defined Deviation Triggers
You can define event triggers that are independent of specific limits and based instead on deviations
from the current values. You must set a deviation and a period of time in which the deviation occurs.
There are three types of deviation available: ANY Deviation, UP Deviation where only changes in a
positive direction are detected and DOWN Deviation where only changes in a negative direction are
detected. The deviation can be defined either in relative terms as a percentage, for example 10%, or as
an absolute value, such as 10 bpm.
Event Retriggering
If a condition that triggered an event persists and the values remain beyond the trigger threshold, a
new event will not be triggered.
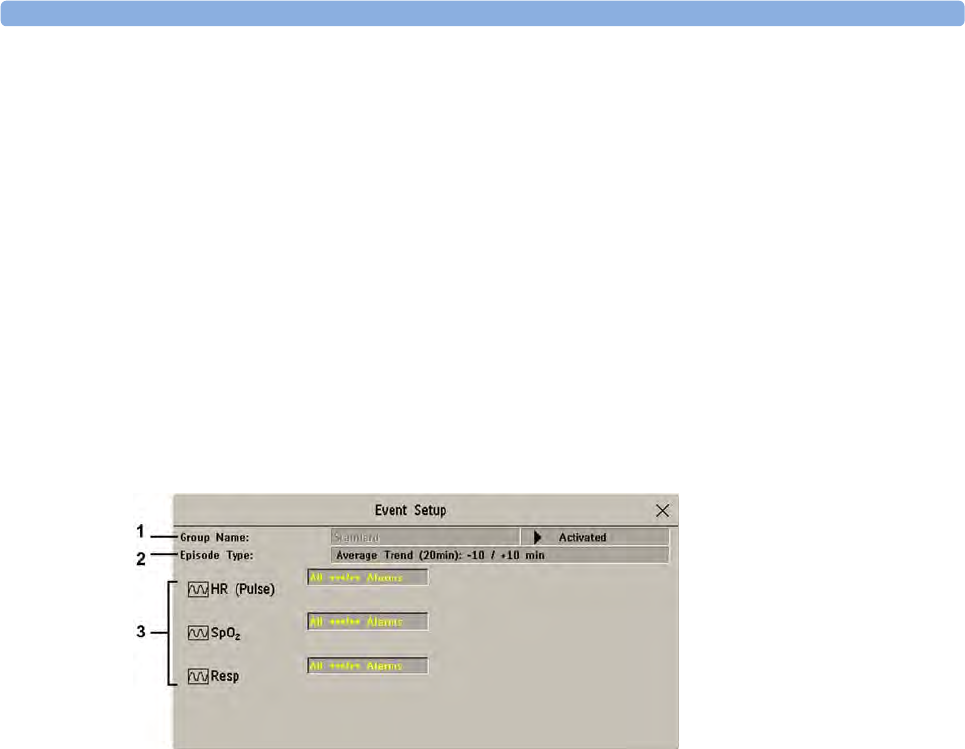
23 Event Surveillance
296
For a new event to be triggered by the same condition, the measured values for at least one of the
triggers must cross back into the normal range and then recross the trigger threshold.
Event Notification
(Advanced Event Surveillance Only). You can be notified when an event is detected. For each event
group you can define a type of notification depending on the severity of the event conditions. The
notification can be a status message with a prompt tone or a standard *, **, or *** alarm notification.
These event alarms are handled exactly like measurement alarms; they can be silenced and are also
suspended when all alarms are suspended. You should only use alarm notification for events which are
comparable in severity to standard measurement alarms to avoid potential confusion due to too many
alarms. Notification in the form of an alarm is not available when the trigger condition is At Least One
Param.. Selecting None switches event notification off.
Setting the type of notification, or switching notification off, is done in Configuration Mode.
Setting Triggers for NER and Basic Event Surveillance
1Group Name
2Episode Type
3Measurements used as event triggers
1Select Main Setup then Event Surveill. followed by Setup Events to enter the Event Setup
window.
2Select the name of the current episode type to set the episode pre/post time.
3Set the event trigger for each measurement. Select each trigger name and select, if available, either
an alarm trigger, or a user-defined trigger from the pop-up trigger list. If you select a user-defined
trigger, set the required threshold level and delay time.
4Set the trigger status to Activated to start event triggering. If the status is Deactivated event
surveillance is effectively switched off.
5Select Confirm to confirm your changes.

23 Event Surveillance
297
Setting Triggers and Notification for Advanced Event Surveillance
1Group Name
2Group Type
3Notification Type
4Episode Type
5Trigger Condition
6Measurements used as event triggers
1Select the group name to enter the setup window for that group.
2Set the trigger status to Activated, to have this event group trigger events, or Deactivated.
3Set the episode type.
Select the name of the current episode type and select an episode type from the pop-up list. The
pre/post episode time for the selected episode type is displayed.
4Set the trigger for each measurement. Select each trigger name and select either an alarm trigger or
a user-defined trigger from the pop-up trigger list. If you select a user-defined trigger, set the
required threshold level and delay time. If a deviation trigger is configured, set the deviation and
duration.
5Select Confirm to confirm your changes.
Triggering Events Manually
To manually trigger an event, select the SmartKey Manual Event and (for Advanced Event
Surveillance) select the group in which the event will be triggered.
For manually-triggered events, patient information for the time leading up to the trigger moment is
stored using the settings of the assigned event group.
Running a Car Seat Assessment Record
In the NER group you can run a Car Seat Assessment Record (CAR). This is a special period of event
surveillance using the current setup of the NER group.
To start a CAR period:
1Select the Start CAR pop-up key or SmartKey.

23 Event Surveillance
298
2Select the required time period for the assessment.
3Select Confirm to start the CAR.
If the NER group was not active it will be activated automatically.
During the CAR period an SpO2 histogram is also generated with 1 second samples. For general
information about the presentation of data in a histogram, see “Viewing Histogram Trends” on
page 274. The CAR SpO2 histogram is unique: it can only be accessed from the events function. It is
generated from the beginning of the CAR period (contrary to the non-SpO2 histograms which are
generated from trended data retrospectively at the end of a time period). Settings are fixed for this
histogram and cannot be changed when viewing it.
The Events Database
The maximum number of events that can be stored in the event database depends on the database
configuration and the level of event surveillance used. The event database is set up in the monitor's
Configuration Mode. Events are stored in the monitor's event database for the configured lifetime,
either 8 hours or 24 hours. Deleted events cannot be retrieved. Events are automatically deleted when:
• their configured lifetime is over
• the storage capacity of the database is exceeded (storing a further event deletes the oldest event in
the memory)
• a patient is discharged.
As the event database is cleared when you discharge a patient, you should ensure that you have
documented any events you require for the patient records before you confirm the discharge.
Viewing Events
• To see a summary of all the events in every group in the event database, use the Event Summary
window.
• To review all the events in a particular event group, use the Event Review window.
• To review individual event episodes in detail, use the Event Episode window.
To start viewing events, either:
•in the Main Setup menu, select Event Surveill. and then select the event view you require from the
list, or
• select the Event Surveill SmartKey
and then select the event view you require from the list.
Event Summary and Event Counter
Vertical bars mark events in the Event Summary window. The timeline shows the position of the
stored events in the event database. Selecting this view activates a cursor that lets you navigate across
the timeline. Use the Show Episode pop-up key to select individual events for review in the Event
Episode window. It also calls up the events pop-up keys.
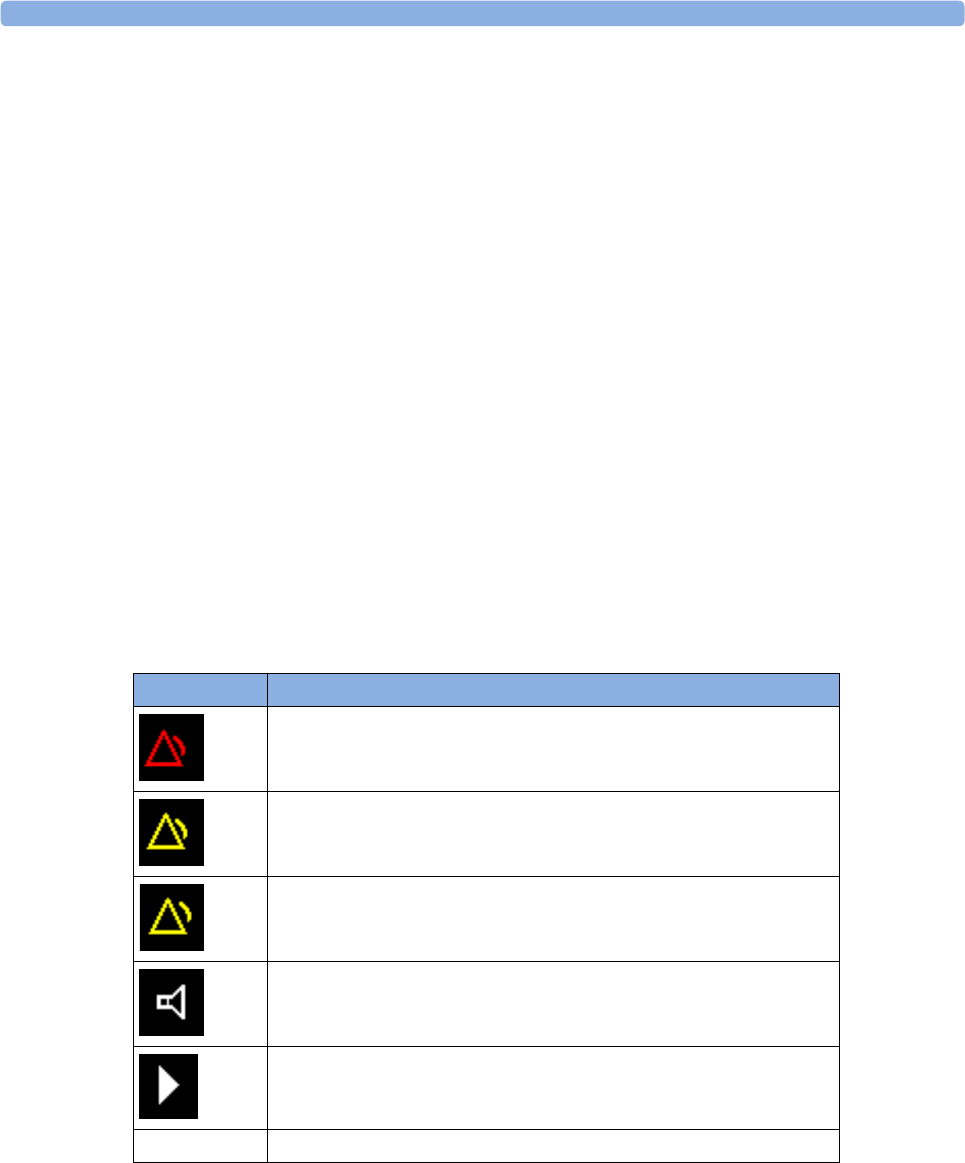
23 Event Surveillance
299
The event counter counts the total number of events in the database. If more than one event group
was set to trigger events within the event history, the event counter also counts the event group totals.
Counting Combi-Events
If one or more events occur during the same Episode Time, the monitor combines them and displays
them as distinct events in one event episode, called a combi-event. The first event is the trigger event,
and the others are follow-up events. For example, if an apnea event is followed 40 seconds later by a
brady event, the brady event is not counted as a single event but as part of the apnea event.
Counting Neonatal Event Review (NER) Events
For neonatal events (NER, formerly "OxyCRG"), apnea events (A), bradycardia events (B), and
combinations of these events are counted and classified by the event counter in the Event Summary. If
they are associated with a Desaturation (D), this is also marked. Manual events (M) are counted
separately. For example, A(D):2(1) indicates that two apnea events occurred and one of them was
associated with a desaturation.
Event Summary Window
(Advanced Event Surveillance only). The Event Summary window shows the number of stored events
in each event group and the total number of events in the database. Vertical bars mark events on a
timeline showing the position of the stored events in the event database. The symbol next to the group
name indicates the activation and notification status:
Selecting the Event Summary window calls up the events pop-up keys.
Parts of the Event Summary window can also be embedded in Screens so that they are always visible,
for example the Total row showing the total number of events with the bars on the timeline or the
column showing all the groups with the activation and notification status.
symbol meaning
group activated, notification set to ***alarm
group activated, notification set to **alarm
group activated, notification set to *alarm
group activated, notification set to screen prompt
group is activated, notification is switched off
no symbol group not activated
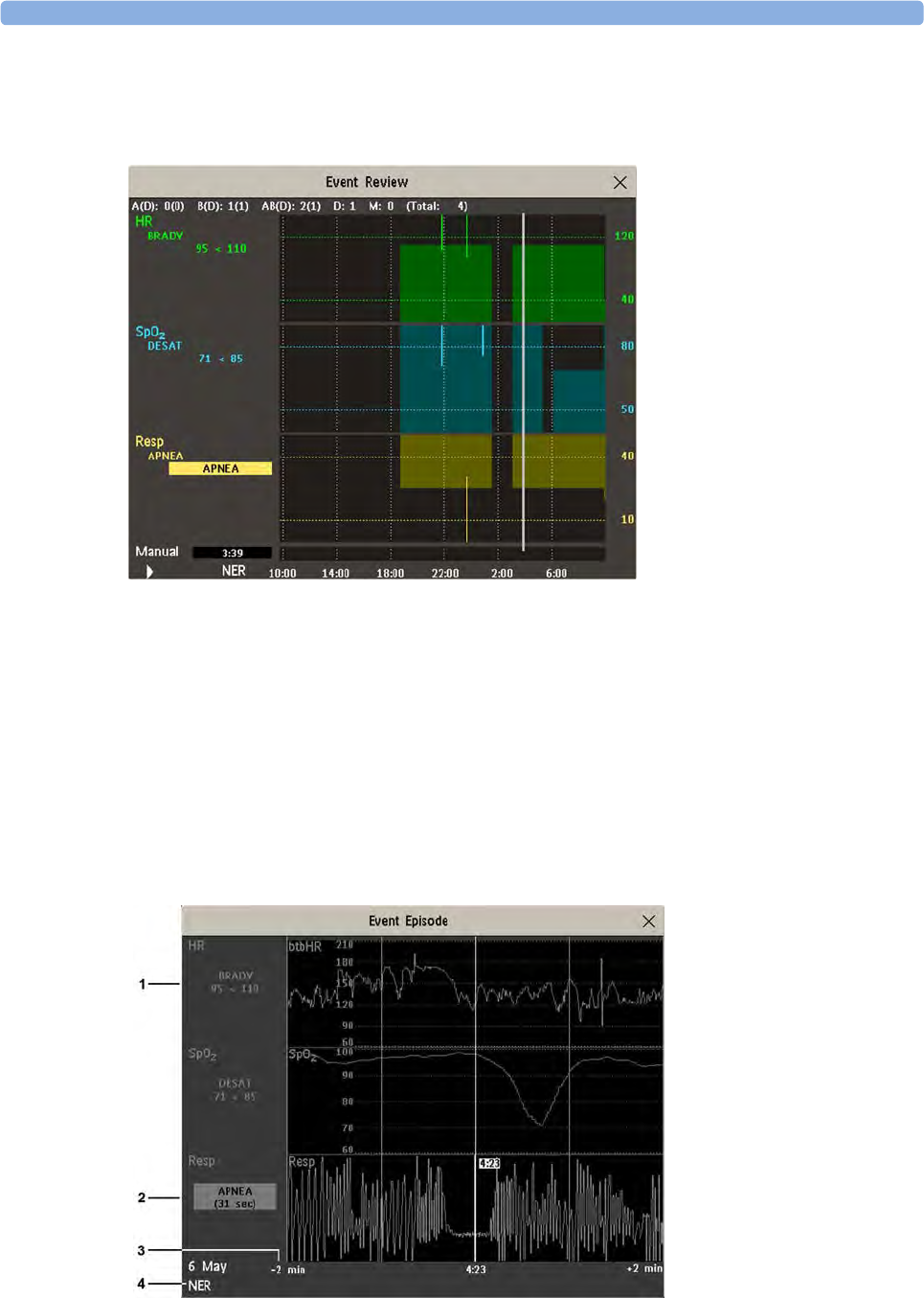
23 Event Surveillance
300
Event Review Window
To enter the Event Review window, select the graphic event summary, if available, or select the events
pop-up key Show Review.
When you open the Event Review window, it automatically shows the event group with the most
recent event.
• To view other event groups, select the pop-up key Review Group and select the group from the
list.
Event Episode Window
To enter the Event Episode window, select the pop-up key Show Episode.
Depending on the event group settings, the Event Episode window shows either 20 minutes of
average trend event information, four minutes of high-resolution event information, or 15 seconds of
realtime wave information.
1Follow-on event values
2Trigger event values,
highlighted
3Timeline, showing
episode Pre/Post-time
4Active event group

23 Event Surveillance
301
The event values to the left of the measurement channels show the trigger threshold set and the
maximum amount by which this limit was exceeded. In this example, Desat 71<85 tells you that 71
was the lowest SpO2 value measured during the event time and that the Desat trigger threshold was set
to 85 when the event was triggered. If the event was manually triggered, the event value boxes display
"manual".
Annotating Events
1To annotate an event, in the Event Episode window, select the pop-up key Select Annotatn.
2Select the required annotation from the pop-up list of available annotations for the currently active
event group.
Up to 20 annotations can be configured to let you add commonly-used clinical notes to event episodes
for documentation purposes. To see the complete list of available annotations, in the Event Setup
menu, select Event Annotation.
Documenting Events
You can print a report or make a recording of the events history stored in the database or of individual
event episodes or a Car Seat Assessment Record.
Documenting Event Review
1In the Event Review window, select the pop-up key Print/ Record. This calls up the event
documentation pop-up keys.
2For a graphic Event Review recording, select the Record Graphic pop-up key.
For a tabular Event Review recording, select the Record Tabular pop-up key.
For a CAR review report, select the Print CAR pop-up key
To print an Event Report, select the Print Review pop-up key.
Documenting an Event Episode
1In the Event Episode window, select the pop-up key Print/ Record. This calls up the event
documentation pop-up keys.
2To make an Event Episode recording, select the Record pop-up key.
To print an Event Episode, select the Print Episode pop-up key.
Event Recordings
Event recordings can be sent to a locally-connected M1116B recorder module.
Event Review Recordings
Each event review recording strip begins with a summary of the events stored in the event database.
Recording strip annotation is explained in the Recording chapter.
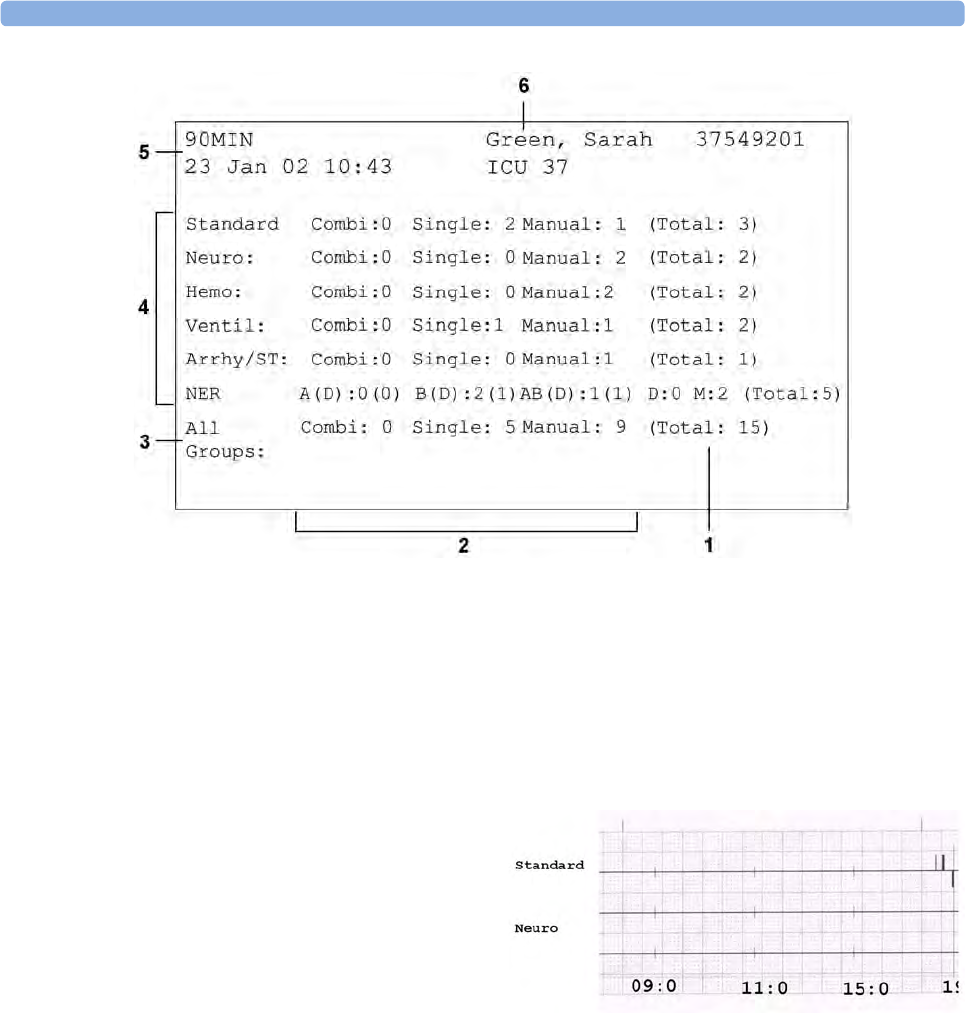
23 Event Surveillance
302
1Event total per event group
2Event types
3Total events in database
4Event groups
5Recording strip code
6Patient information and medical record no.
In graphic event review recordings,
events are represented by bars, and each
event group is printed on a separate
channel.
The timeline reflects the period stored
in the database, either 24 hours (divided
into 4 hour sections) or 8 hours (divided
into one-hour sections).
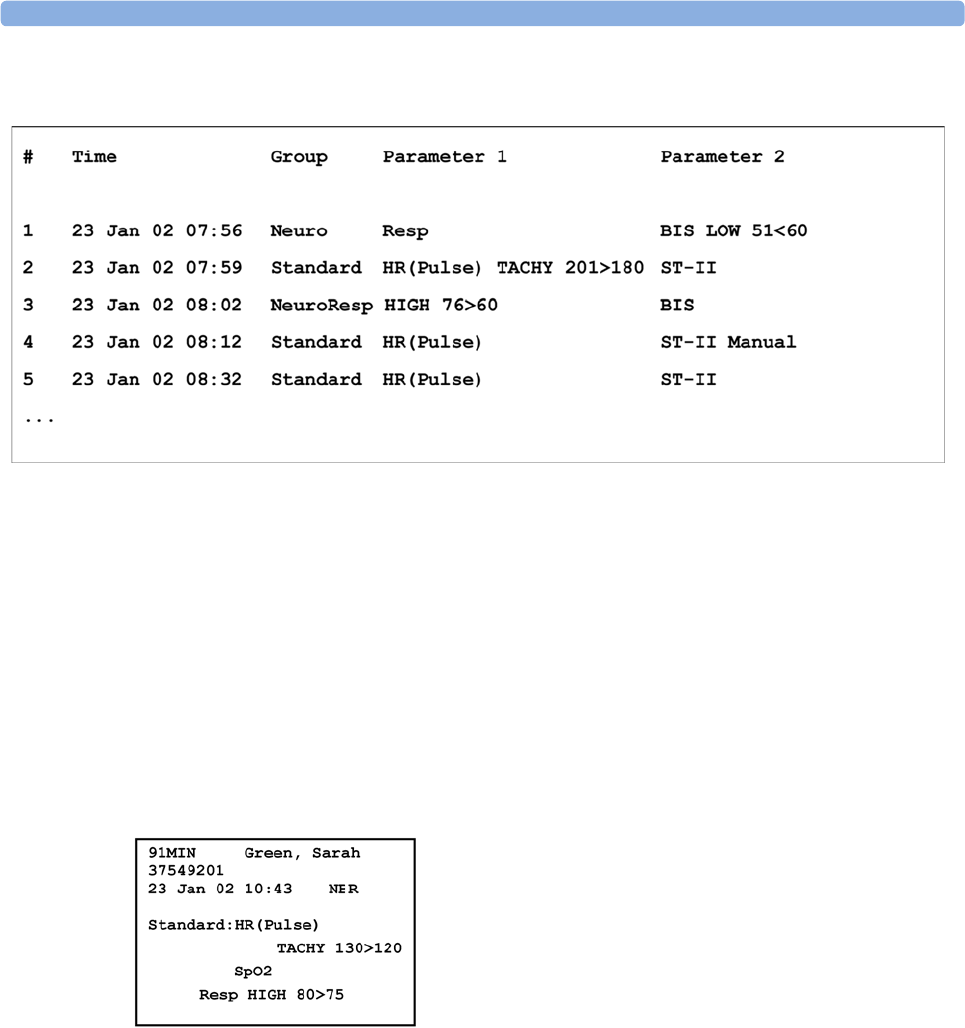
23 Event Surveillance
303
In tabular event review recordings, the events stored in the event database are shown in chronological
order, with a number and time-stamp.
The measurements in the event group are shown in the next columns, marked "Parameter 1, Parameter
2...", along with the event values measured at the time of the event. For each event, the trigger values
are shown.
This section of the recording is A4 or letter size, so that it fits in a patient file.
Event Episode Recordings
Event episode recordings are divided into four sections.
The first section shows the patient information and the event group of the episode with the event
values for the group measurements. The trigger symbol marks the event trigger.
The second section (2 below) shows the waveforms recorded during the episode. The trigger moment
is marked with a triangle and divides the episode into the pre/post time. Any calibration marks and
grid marks on the screen are automatically printed on the recording.
If there are four measurements in the event group being recorded, two waveforms will be recorded in
two separate waveforms segments.
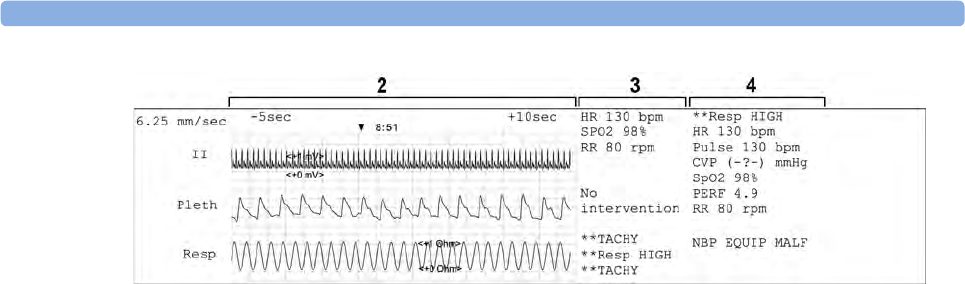
23 Event Surveillance
304
The third section (3 above) shows the most important vital signs information, including numerics,
active alarms, and any annotations made on the event episode.
The fourth section (4 above) shows the numerics for all the currently monitored vital signs and any
alarm conditions or INOPs active at the time the event was triggered.
Event Reports
Event reports can be printed on A4 and letter size paper on a printer connected locally or centrally to
your monitor.
Event Review Reports
The event review report documents all the events stored in the event database for a selected group.
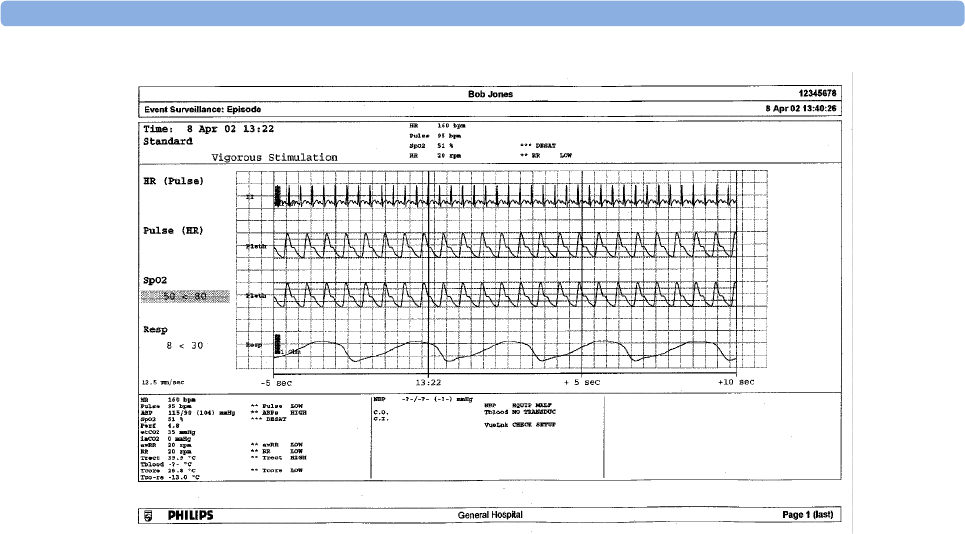
23 Event Surveillance
306
Event Summary Reports
(Advanced Event Surveillance only). The event summary report shows a graphical view and a tabular
view of all events in the database for all groups.
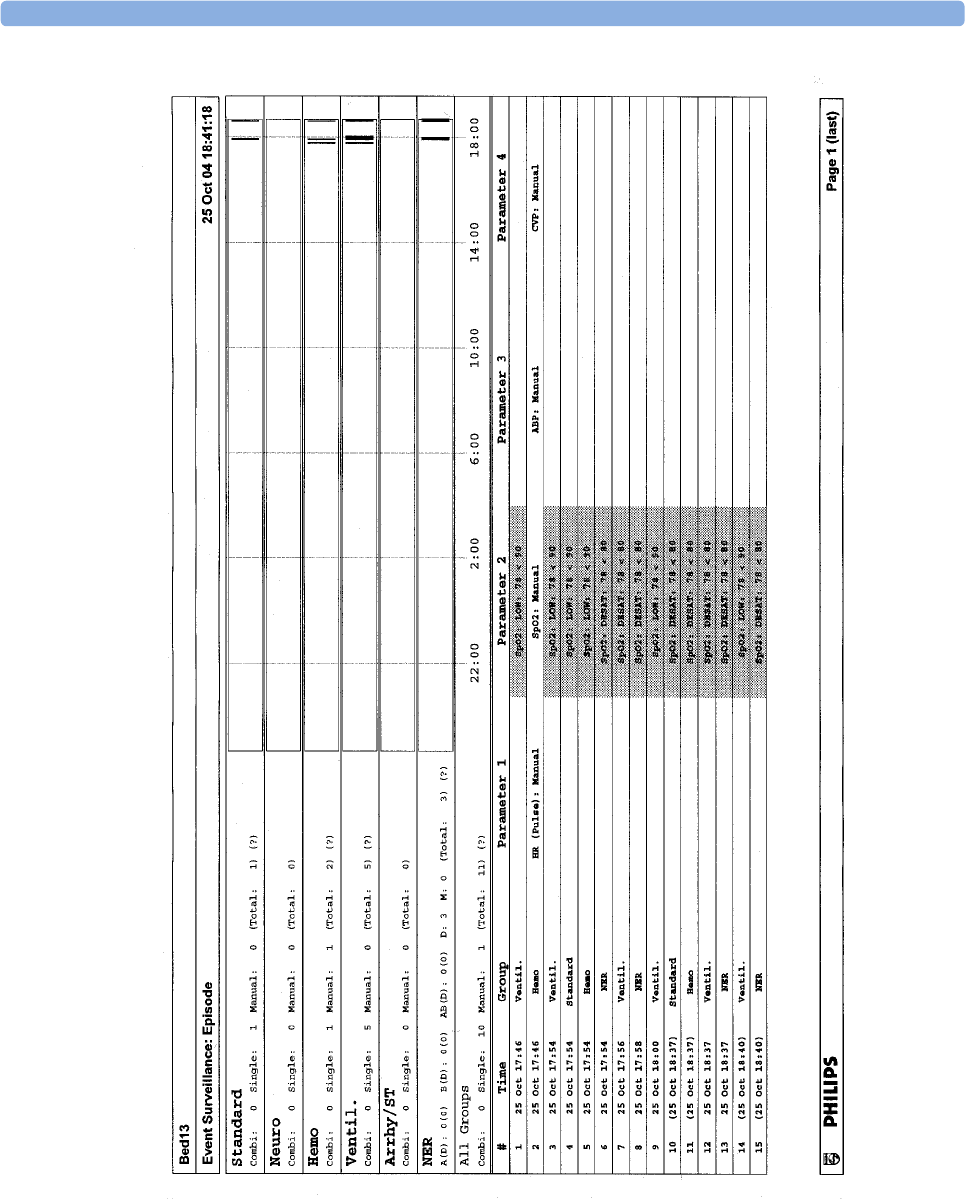
23 Event Surveillance
307

23 Event Surveillance
308

24
309
24ProtocolWatch
ProtocolWatch (PW) is a clinical decision support tool. It allows you to run a clinical protocol which
can monitor developments in the patient's condition, taking into account:
• measured values from the monitor
• values manually entered by you (for example manual temperature measurements, lab values)
• your assessment of patient status
ProtocolWatch notifies you when certain conditions or combinations of conditions occur and it
documents developments in a log which can be printed.
SSC Sepsis Protocol
The SSC (Surviving Sepsis Campaign) Sepsis Protocol is a protocol implemented for the
ProtocolWatch application. The SSC Sepsis Protocol is for use in screening for severe sepsis and
monitoring of its treatment. It is a computerized implementation of the January 2008 Surviving Sepsis
Campaign Guidelines for Management of Severe Sepsis and Septic Shock. Philips does not make any
claims about their effectiveness to reduce the morbidity or mortality associated with severe sepsis.
The SSC Sepsis Protocol assists you in recognizing the early signs and symptoms of sepsis by
comparing the state of your patient to the defined criteria and then guides you through the
recommended treatment protocol. Use of the SSC Sepsis Protocol requires thorough knowledge of the
complete SSC Guidelines for Management of Severe Sepsis and Septic Shock. Due to space limitations
on the screen, the recommendations cannot always be reproduced in the full detail available in the
printed and on-line guidelines. The SSC Sepsis Protocol is not a diagnostic or therapeutic tool and is
not intended to replace the competent judgment of a clinician.
The SSC Sepsis Protocol consists of three separate consecutive phases:
Severe Sepsis Screening - measurement values and patient status are compared to the Severe Sepsis
Screening criteria. When these criteria have been met, the clinician confirms the presence of infection
and sepsis-related organ dysfunction and can authorize entering the Sepsis Resuscitation Bundle.
Sepsis Resuscitation Bundle - the recommendations for sepsis resuscitation are listed and can be
checked off as they are implemented. After achievement of all the sepsis resuscitation goals, or at the
latest after 6 hours, the Sepsis Resuscitation Bundle is completed and the Sepsis Management Bundle
begins.
Sepsis Management Bundle - the recommendations to maintain patient status are listed and can be
checked off as they are implemented. The Sepsis Management Bundle ends when 24 hours have
passed since the Sepsis Resuscitation Bundle began.
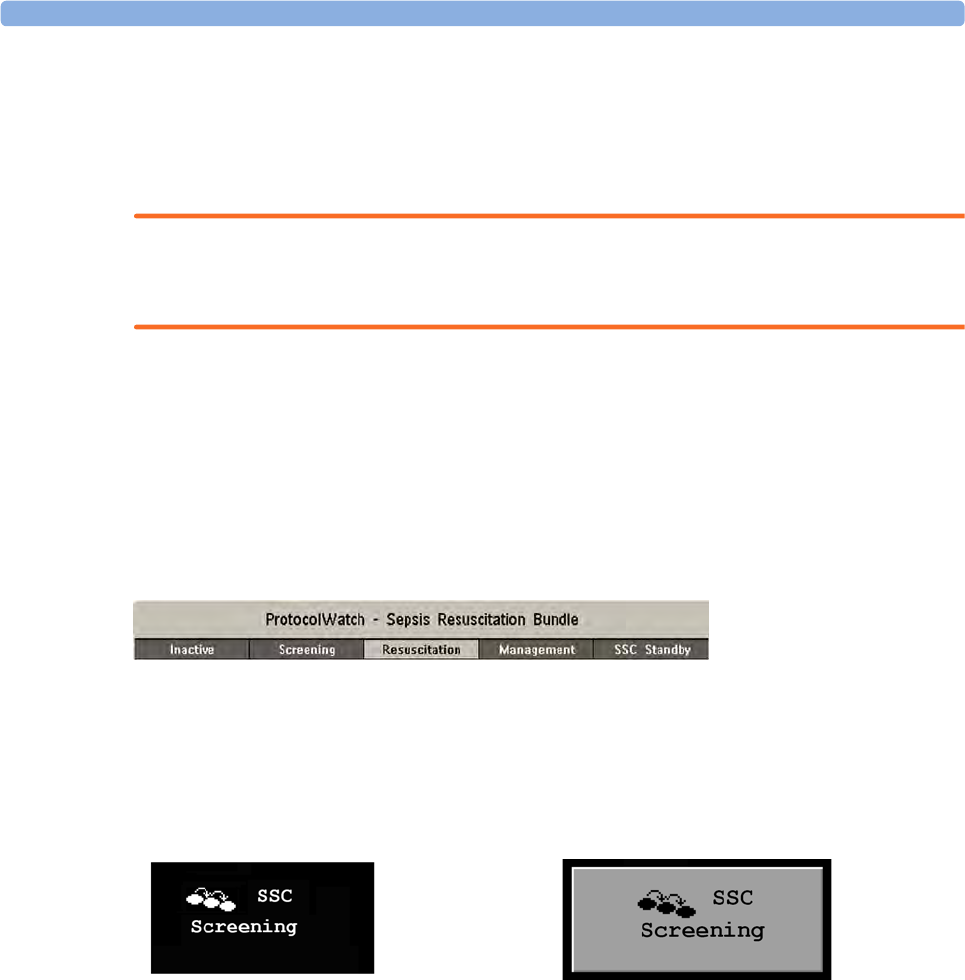
24 ProtocolWatch
310
Depending on the option your monitor has, it may be that only the Severe Sepsis Screening phase is
implemented. If, at the end of this phase sepsis has been confirmed, and the patient is transferred for
treatment in the resuscitation and management phases, you can transfer the current state, the settings
and the log from the SSC Sepsis Protocol in the MMS to another monitor with the full version of the
SSC Sepsis Protocol. The transfer of data and settings must be enabled in Configuration mode.
WARNING
Always consider the specific clinical context for your patient, before following SSC Sepsis Protocol
treatment recommendations.
The SSC Sepsis Protocol and this description are based on the SSC Guidelines for Management of
Severe Sepsis and Septic Shock from January 2008 and the SSC Bundle definitions from January 2005.
To check the version of the Guidelines and Bundle definitions on the monitor,
•Select
Main Setup then Revision then ProtocolWatch followed by SSC Sepsis
Orientation On The Screen
At the top of each window there is an orientation line showing the phases available on your monitor,
with the currently active phase highlighted.
You can also place the ProtocolWatch symbol, together with the currently active phase, on the main
screen, in one of the numeric positions. This allows you to see at a glance which phase is currently
active, even when no SSC Sepsis Protocol window is currently displayed.
If you need to enter data or perform an action in an SSC Sepsis Protocol window, the symbol will turn
into a SmartKey.
Transferring Patients And Moving Manually Between Phases
If a patient has already been diagnosed as having severe sepsis before connecting them to the monitor,
you can select Main Setup then ProtocolWatch followed by Manual Transition to go directly to the
Sepsis Resuscitation Bundle to monitor treatment. Direct entry to the Sepsis Management Bundle is
also possible using the Manual Transition function and the time into the selected bundle can be set.
If a patient has been screened on arrival, for example in the emergency department, then transferred to
Intensive Care when Sepsis is confirmed, the current state, the settings and the log from the SSC Sepsis
Protocol will be transferred with the MMS to the new monitor. Should it be necessary, you can select
the phase at the new monitor manually with Main Setup then ProtocolWatch followed by Manual
Transition. The transfer of data and settings must be enabled in Configuration mode.
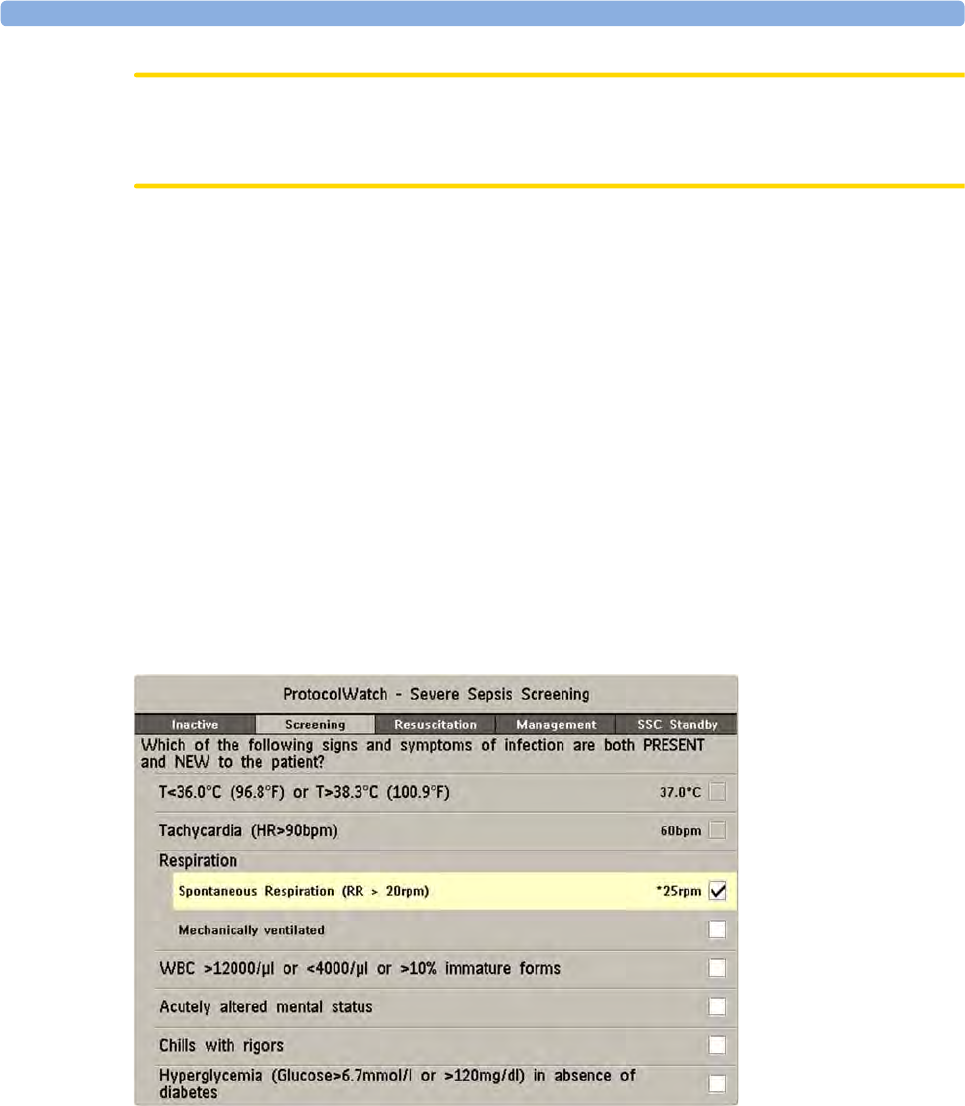
24 ProtocolWatch
311
CAUTION
It is not possible to transfer SSC Sepsis Protocol data from a monitor with release F.0 software to
another monitor with release G.0 software or above, and vice versa.
Suspending the Protocol for 24 Hours
To suspend the protocol for 24 hours:
1Select Main Setup then ProtocolWatch followed by Suspend for 24 hours.
2Select Confirm.
The protocol will resume activity after 24 hours with Severe Sepsis Screening.
Severe Sepsis Screening
As soon as an adult patient is connected to the monitor, and heart rate or pulse is being measured, the
protocol begins to observe heart rate, temperature and respiration rate values in the background. If
temperature or respiration rate is not being measured continuously, a pop-up window appears at 4-
hour intervals to ask for manually measured values. These values are all compared to the screening
criteria: HR above 90, Temp above 38.3°C (100.9°F) or below 36.0°C (96.8°F), RR above 20.
If any one of the values fulfills the screening criteria, the first Severe Sepsis Screening window
appears:
The measured value which has fulfilled the criteria is shown highlighted (in the example above it is
respiration). There is a check box for the infection signs and symptoms listed,
• if the monitor has measured values which meet the screening criteria, and
• for all signs and symptoms which cannot be measured by the monitor.
Check the box if you can confirm that this sign or symptom is present and new. If the patient is
mechanically ventilated, the Mechanically ventilated box must be checked. If you have manually
measured temperature or respiration rate, you can enter the values using the Enter RR and Enter Temp
keys.

24 ProtocolWatch
312
Select Confirm when the check boxes reflect the current patient status.
Select Remind 15 min if you want to delay filling out this screen. (When you enter the screen manually
this key will be a Cancel key, as no action is required in this case.)
Changing Conditions
The window reappears if:
• a previously fulfilled criteria is again fulfilled
• a new HR or RR criteria is fulfilled,
• the HR or RR value which previously fulfilled the criteria now triggers a ** RR HIGH, ** HR HIGH
alarm or a ***TACHY xxx > yy alarm,
• after 8 hours (configurable to 12 hours) if at least one infection sign is still present.
Two Or More Infection Signs Or Symptoms Confirmed
If you have confirmed two or more infection signs in the first Severe Sepsis Screening window, a new
pop-up window appears asking Is the patient history suggestive of a new infection?.
If you select Yes, the next screen appears requesting a lactate measurement.
If you select No, the screening phase continues and the first Severe Sepsis Screening window reappears
in the situations described in Changing Conditions above.
Lactate Measurement
To enter the Lactate value, select the Enter Lact key. If the value entered is > 4 mmol/l the check box
is automatically checked.
Select Confirm when a value has been entered. What follows depends on the Lactate value:
•If Lactate is > 4 mmol/l: the value meets the criteria for severe sepsis and a window appears
recommending authorized clinician review before entering the Sepsis Resuscitation Bundle.
•If Lactate is ≤ 4 mmol/l: a further window appears requiring your input to determine on the
basis of blood pressure values whether the patient meets the criteria for severe sepsis.
Hypotension Evaluation
If the Lactate value was not above 4 mmol/l, the next window asks whether the patient has persistent
hypotension.
The protocol defines Hypotension as:
• SBP < 90mmHg (12.0kPa), or
• MAP < 65mmHg (9.0kPa), or
• SBP decrease > 40mmHg (5.0kPa) below baseline.
You can see this definition in the window by selecting Show Details.
If the patient has persistent hypotension as defined, select Yes. This acknowledges that the patient
meets the criteria for severe sepsis and a final window appears recommending authorized clinician
review before entering the Sepsis Resuscitation Bundle.
If the patient does not have persistent hypotension, select No. After an hour a screen appears asking Is
the previously acknowledged infection still present?.

24 ProtocolWatch
313
If you select Yes, the window for the Lactate measurement will reappear. If you select No, screening
continues - comparing heart rate, temperature and respiration rate values against the screening criteria.
Authorized Clinician Review
To review the protocol, select Protocol Log. You can also print out the log to document the screening
phase.
Select Confirm to complete the screening phase and, if you have the appropriate monitor option,
continue to the Sepsis Resuscitation Bundle phase.
Sepsis Resuscitation Bundle
The treatment recommendations from the Sepsis Resuscitation Bundle are presented and the
implementation of the recommendations is monitored.
When the Sepsis Resuscitation Bundle phase begins, the ProtocolWatch Screen automatically appears
on the monitor (if configured and available on the monitor).
The lower area of the screen contains:
• a reminder list of the treatment recommendations - recommendations which have been fulfilled
are shown in gray, overdue recommendations are shown in orange
• a timer showing the time already passed in this phase
• three horizon trends for MAP, CVP and ScvO2 or SvO2, if these measured values are available
• a list of the latest manually entered values - if you select this list you will open the Manual Entry
Log window where the last 24 manually entered values are shown for reference
If ScvO2 or SvO2 and CVP are not being continuously measured, a pop-up window appears at hourly
intervals to ask for a manually measured value.
Monitoring the Sepsis Resuscitation Bundle Recommendations
When you select the lower area of the ProtocolWatch Screen, the Sepsis Resuscitation Bundle
window appears. If you do not have the ProtocolWatch Screen displayed, the Sepsis Resuscitation
Bundle window appears automatically once an hour.

24 ProtocolWatch
314
Select the Enter Lact key to enter a lactate value. When you have entered a value, or if a lactate value
had previously been entered, the box is checked.
Check the Take Blood Cultures box when you have taken blood cultures.
Check the Administer Intravenous Antibiotics box when you have started broad-spectrum antibiotic
therapy.
The remaining three recommendations are automatically compared to the Sepsis Resuscitation Bundle
criteria, if the measurements are available on the monitor. A box is checked when the corresponding
recommendation has been fulfilled.
Depending on your configuration, continuously measured CVP values may be disregarded if they
exceed a set limit. Whether this is so, and which limit is applied, is set in the monitor's Configuration
mode.
If you have manually measured ScvO2 or CVP, you can enter the values using the Enter ScvO2 and
Enter CVP keys. The box is checked automatically if the value fulfills the recommendation.
The boxes for MAP, ScvO2/SvO2 and CVP can also be checked manually (for cases where the
monitor does not measure them) but only when the timer has reached 4 hours to ensure that these
values are achieved and maintained mid-term. Check these boxes if the recommendation has been
fulfilled.
To see more details about the recommendations, select the Show Details key.
Select Confirm when the check boxes reflect the current treatment status.
Checking The Sepsis Resuscitation Bundle Window
During the Sepsis Resuscitation Bundle you can open the Sepsis Resuscitation Bundle window at any
time to check the status or to make entries. The recommendations are shown as follows:
• Recommendations which are not yet fulfilled are shown in black. They also appear in the list on
the lower area of the ProtocolWatch Screen.
• Recommendations which are overdue are shown in orange.
• Recommendations which have been fulfilled and confirmed are shown in gray. They no longer
appear in the list on the lower area of the ProtocolWatch Screen.
Previewing the Sepsis Management Bundle
At any time during the Sepsis Resuscitation Bundle you can preview the Management Bundle in order
to see which recommendations will follow there.
• Select the Preview Managmnt key.
Ending The Sepsis Resuscitation Bundle
When all recommendations have been fulfilled and confirmed, or when 6 hours have passed since the
bundle started, the Sepsis Resuscitation Bundle is ended.
You are asked to confirm with the Yes key that the Sepsis Management Bundle should now be started.
If you select No, the Sepsis Resuscitation Bundle is extended for 1 hour.
Sepsis Management Bundle
The stabilization recommendations from the Sepsis Management Bundle are presented and the
implementation of the recommendations is monitored.
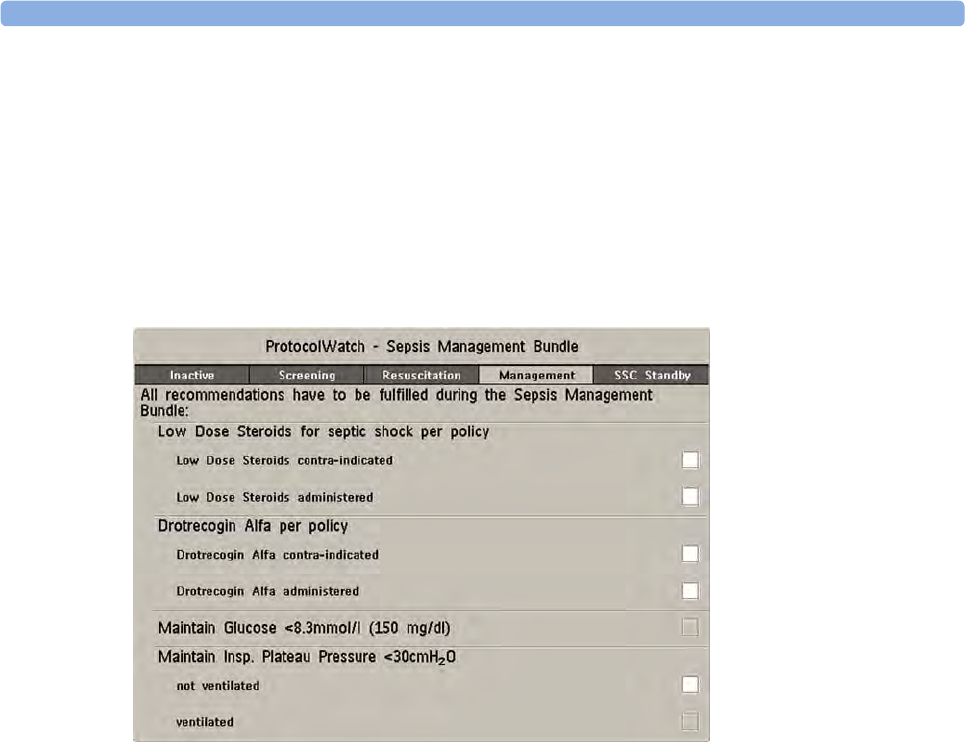
24 ProtocolWatch
315
When the Sepsis Management Bundle phase begins, the ProtocolWatch Screen is automatically
updated (if configured and available on the monitor). In the lower area of the Screen, the list of
recommendations for the Sepsis Management Bundle replaces the list for the Sepsis Resuscitation
Bundle. The timer shows the combined time for both phases.
Monitoring the Sepsis Management Bundle Recommendations
When you select the lower area of the ProtocolWatch Screen, the Sepsis Management Bundle
window appears. If you do not have the ProtocolWatch Screen displayed, the Sepsis Management
Bundle window appears automatically once every six hours.
The Low Dose Steroids for septic shock per policy recommendation and/or the Drotrecogin Alfa
per policy recommendation may not appear if they have been configured not to do so for your
hospital.
Check the Low Dose Steroids administered box when you have started steroid therapy or the Low
Dose Steroids contra-indicated box if this treatment is contra-indicated for your patient.
Check the Drotrecogin Alfa administered box when you have started recombinant human activated
protein C therapy or the Drotrecogin Alfa contra-indicated box if this treatment is contra-indicated
for your patient.
The boxes for Maintain Glucose <8.3mmol/l (150 mg/dl) and Maintain Insp. Plateau Pressure
<30cmH₂O can only be checked when the timer has reached 20 hours to ensure that the stabilization
of these values is achieved long-term. Check these boxes if the recommendation has been fulfilled.
Recommendations which have been fulfilled are shown in gray with the time fulfillment was entered.
To see more details about the recommendations, select the Show Details key.
Select Confirm when the check boxes reflect the current treatment status.
Ending The Sepsis Management Bundle
The Sepsis Management Bundle normally ends 24 hours after the Sepsis Resuscitation Bundle started,
as documented by the bundle timer on the ProtocolWatch screen. You are asked to confirm with the
Yes key that routine monitoring should now resume. By selecting No you can extend the Sepsis
Management Bundle phase by an additional 6 hours.

24 ProtocolWatch
316
After completion of the Sepsis Management Bundle a sepsis standby phase begins which allows time
for further patient stabilization and recovery. During this phase Severe Sepsis Screening is suspended.
The standby phase is by default 7 days but the length can be adjusted in Configuration Mode.
Viewing And Printing The Protocol Log
The Protocol Log stores all user interactions, alarms and phase transitions while the SSC Sepsis
Protocol is running.
To view the Log select Main Setup then ProtocolWatch followed by Protocol Log
You can choose between three different views of the Protocol Log:
•Summary View - a short form which does not include when the windows were triggered
•Full View - a complete log of all user interactions, alarms and phase transitions
•Phase View - you can view log entries for one phase by selecting that phase on the orientation line
When the Log consists of several pages, you can move through the pages with the Previous Page and
Next Page keys.
To start a Protocol Log printout, select Print.
The log is cleared whenever a patient is discharged.
Always Discharge Patients
It is essential that patients are discharged when monitoring ends. As a reminder, the monitor can be
configured to display a pop-up window when the monitor has been switched off, in Standby mode, or
not monitoring basic vitals for a certain time. The window asks whether a new patient is being
monitored and offers a pop-up key to discharge the previous patient if this is the case. The window
must be configured in Configuration Mode.
When the previous patient is discharged, this clears the protocol log, resets the timers and deletes
manually entered measurement values.
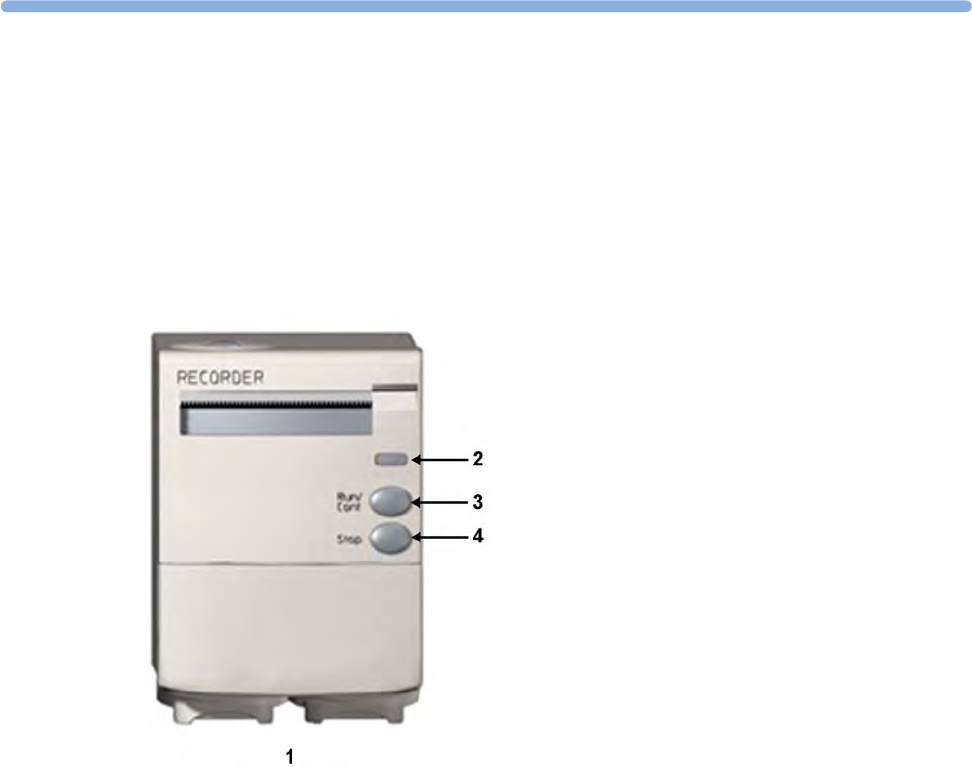
25
317
25Recording
The M1116B plug-in recorder records numerics for all active measurements and up to three
waveforms. You can use it for local recording mounted in the monitor's FMS.
Central Recording
For central recording from the bedside, your monitor must be connected via a network to an
Information Center. You can use either the M1116B 2-Channel Recorder or the standalone M3160A
4-Channel Recorder. Recordings made on the M3160A may look slightly different to those described
here. See the documentation supplied with the Information Center for information on the 4-Channel
Recorder.
Starting and Stopping Recordings
The recordings pop-up keys let you start and stop recordings. Select the Recor- dings SmartKey to
call up the line of pop-up keys. Scroll right or left to see any pop-up keys not displayed.
The selection of pop-up keys available depends on the monitor you are using.
1M1116B Plug-in Recorder
2Continue LED - flashes if a continuous recording is
ongoing
3RUN/CONT key - starts a delayed recording or
makes the current recording continuous
4STOP key - stops the current recording
25 Recording
318
Quickstarting Recordings
To quickstart any type of recording using a pre-configured recordings template,
• Select the Recor- dings SmartKey and then select the pop-up key of the recording type you want
to start.
Alternatively, you can
• Select the Main Setup SmartKey, select Recordings, then select the recording type.
To quickstart a delayed recording,
• Select the SmartKey Delayed Record to immediately start a delayed recording.
M1116B only
• You can also start a delayed recording by pressing the Run/Cont key on the recorder module.
Extending Recordings
Timed (non-continuous) recordings stop when their runtime is over. Continuous recordings continue
until stopped manually or by an INOP condition.
• To extend an ongoing recording by its runtime, reselect its Start pop-up key once.
• To make an ongoing recording continuous, reselect its Start pop-up key twice within 5 seconds.
M1116B
only • You can also make an ongoing recording continuous by pressing the Run/Cont key on the
recorder module.
Stopping Recordings
Recordings stop automatically when the preset runtime is over, when the recorder runs out of paper,
when you open the recorder door or when the recorder has an INOP condition.
• To manually stop a recording, select the Recor- dings SmartKey and then select the pop-up key
Stop All Recordng.
M1116B
only • You can also stop a recording by pressing the Stop key on the recorder module.
Recording Without a Template
To record without a pre-configured template, selecting the waves you require,
1Either: Select the Recor- dings SmartKey then select the pop-up key Select Waves.
Or: Select the SmartKey Record Waves.
Delayed Recordng Vital Signs
RT A Recordng Alarm Limits
RT B Recordng ST Segments
RT C Recordng ECG QT
Select Waves Setup Recordng
HiRes Recordng Stop All Recordng
All ECG Waves
25 Recording
319
2Use the pop-up keys to choose up to three measurement waves to be printed on the recording. If
you want fewer than three waves on the recording, select the waves you want then select the
Continue pop-up key.
3Select one of the recording speed pop-up keys to set the required recording speed.
4Select the Start pop-up key to start the recording.
Select Waves recordings use default values for any recorder settings not defined: runtime is
continuous, overlapping is set to non-overlapping.
Overview of Recording Types
This table details settings for local recordings. For details on recordings made on the central recorder,
see your Information Center Instructions for Use.
All ECG Waves Recordings
An All ECG Waves recording shows a 4 second recording of each lead with a calibration bar preceding
each ECG lead. All available leads are recorded sequentially in the standardized lead order. The
recording is realtime, that is, the information recorded is not simultaneous.
Delayed Alarm Realtime (RT) All ECG
Waves HiRes Trend Procedure or
Context
Type of
recording
manual automatic, triggered by
defined alarm conditions
manual manual manual manual, use the
context
window's pop-
up keys to start
Recording
Destination
local recorder and
central
local recorder and
central
printer local recorder and
central
local recorder
only
local recorder
only
local recorder
only
Information
recorded
from the start
trigger minus the
delay time
from the start
trigger minus the
delay time
n/a from the start
trigger
from the start
trigger, in
realtime
from the start
trigger minus
delay time
defined by the
context
Number of
waves
up to 3 up to 3 n/a up to 3 all ECG waves
currently
monitored and
available
up to 3 high-
resolution trends
(beat-to-beat)
waves
up to 3 waves,
or specific to
the context, e.g.
a wedge
procedure
Speed 50, 25, 12.5, 6.25,
2.5 mm/sec
50, 25, 12.5, 6.25,
2.5 mm/sec
n/a 50, 25, 12.5, 6.25,
2.5 mm/sec
25 mm/sec 1, 2, 2.5, 3, 6 cm/
min
defined by the
context
Runtime 15, 20, 25, or 30
seconds
15, 20, 25, or 30
seconds
n/a 6, 8, 10, 15
seconds or
continuously
4 seconds per
wave
10 minutes, or
continuously
defined by the
context
Stops automatically automatically n/a automatically if
limited, manually
if continuous
automatically automatically if
limited, manually
if continuous
defined by the
context
Delay Time 10, 15 seconds 10, 15 seconds n/a none none 6, 5, 4, 3, 2, 1
minutes
defined by the
context
Overlap up to 3 waves up to 3 waves n/a up to 3 waves none up to 3 waves defined by the
context
n/a = not applicable

25 Recording
320
Creating and Changing Recordings Templates
To save you defining recording settings each time you start a recording, you can create templates for
commonly-used types of recordings in the Setup Recording menu. You can create templates for one
delayed recording, one alarm recording, three realtime recordings (two for MP20/30), and one high
resolution recording. All ECG Waves recordings do not need to be configured, they always use the
same format.
Changing recordings templates changes the settings that will be used each time a recording of this
name is triggered.
1Select the Main Setup permanent key to call up the Main Setup menu.
2Select Recordings to enter the Setup Recording menu.
3Select the name of the template you want to create or change. Each recording name is linked to a
recording type, delayed, alarm, realtime, and hi-res trends. Recording names can be changed in the
monitor's Configuration Mode.
4Design the template by selecting each menu item and entering the information for the template.
•Recorder: choose which recorder the recording will print to (Local, Central 2-Ch, or Central 4-
Ch recorder, or Printer (for realtime reports in alarm recording only)).
•Channel 1, Channel 2, etc.: choose which waveform to record in each channel. If the wave
assigned to a recording channel in a particular template is not available when a recording is
triggered, the channel is left blank on the recording strip. The pop-up list of available (currently
monitored) waves differs according to the recording type:
– Realtime, delayed and alarm recordings: the list shows all the currently available waves.
– High-resolution recordings: the list shows all the available high-resolution waves.
In addition to the currently available waves, you can choose from several other settings which
make an automatic allocation when the recording starts:
–Alarm Par will always record the measurement in alarm in the chosen recorder channel
–Primary Lead will always record the current primary lead in the chosen recorder channel
–SecondryLead will always record the current secondary lead in the chosen recorder channel
–Any Agent will always record the currently selected anesthetic agent.
For high-resolution recordings only the Any Agent setting is available.
•Overlap: define whether the recorded waveforms will be printed overlapping or beside each other.
•Speed: choose the recording print speed.
•Delay Time: Delayed recordings start documenting on the recorder strip from a pre-set time
before the recording is started. This interval is called the "Delay Time" and can be set as specified
in “Overview of Recording Types” on page 319. This setting can only be changed in Configuration
Mode.
•Run Time: see how long this type of recording is configured to run. This setting can only be
changed in Configuration Mode. Continuous recordings run indefinitely.
Central Config: if available in the General menu, select this setting to use the recording settings made
for the centrally-connected recorder.

25 Recording
321
Changing ECG Wave Gain
The ECG Gain setting in the General Recording Setup window defines how every recorded ECG
wave, irrespective of template or recording type, will appear on the recorder strip. This does not affect
the displayed ECG wave, or printed ECG reports. To change the ECG gain setting for recordings,
1In the Setup Recording menu select General.
2Select ECG Gain.
3Select the required setting:
–Auto: the wave recording will use the same scale as the ECG wave on the monitor screen
–5 mm/mV, 10 mm/mV, 20 mm/mV: the wave recording will use a scale of 5, 10, or 20
millimeters per millivolt.
Recording Priorities
Manually-started recordings have priority over automatically-started recordings. If an
automatically-triggered alarm recording is running, and a realtime or delayed recording is manually
started, the alarm recording is stopped and the manually-requested recording is started.
More recent manually-started recordings have priority over older manually-started recordings.
If a manually-started recording is running, and another manually-started recording is triggered, then
the older recording is stopped and the more recent manually-started recording is started.
Alarm recordings are prioritized according to alarm priority. If an alarm recording triggered by a
yellow alarm is running and a new alarm recording is triggered by a red alarm, the yellow alarm
recording is stopped and the red alarm recording is started.
Recording Strip
The information printed on the recording strip includes the patient name and MRN, bed number, date
and time of recording, recording speed, and recording code. Active alarm and INOP messages as well
as numerics for all currently monitored measurements are also printed.
Recording strip annotations are printed at the beginning of the recording strip and updated at regular
intervals, every 15 minutes for recordings made at speeds lower than 6.25 mm/s, and every 60 seconds
for recordings made at speeds greater or equal to 6.25 mm/s.
Recording Strip Code
The recording strip code printed in the first line of the initial annotation has up to seven characters,
specifying recording type, operating mode, application area, patient category, and delay time, if
applicable.
25 Recording
322
Recorded Waveforms
A selection of up to three waveforms is recorded, marked with wave labels and wave scale information.
Wave scale information can be in the form of a calibration bar, like the 1 mV calibration bar for ECG,
or calibration steps before the waveform starts.
Maintaining Recording Strips
Recording ink sometimes fades when covered with transparent tape. Avoid covering any part of a
recording that is clinically relevant (annotation or waveforms) when taping a recording strip to a
patient record or other patient documentation.
Code Meaning
Recording type 90
8A
0B
91
Realtime
Delayed
Alarm
Context (Procedures)
Operating mode M
D
C
S
Monitoring
Demo
Configuration
Service
Application area I
O
C
N
ICU
OR
CCU
NICU
Patient category A
P
N
Adult
Pediatric
Neonatal
25 Recording
323
Reloading Paper
M1116B
Recorder Status Messages
1Use the latch on the right side of the recorder door to pull the door
open.
2Remove the empty core.
3Insert a new roll so that it fits snugly into its housing and the paper
end is feeding from the top. Recommended paper: 40477A and
40477B.
4Pull out some paper and fold along the front edge at a 45° angle. This
makes it easier to feed the paper under the roller as shown.
5Feed the paper through and pull some paper out from the top of the
roller.
6Close the recorder door.
7To test if paper is loaded correctly, start a recording. If no printing
appears, paper may be loaded backwards. Try reloading the paper.
Recorder Status Messages Explanation
For example:
Local alarm recording running
The named recording is currently running.
No Central alarm recording available
No local alarm recording available
No alarm recording can be made on the selected
recorder. Try selecting another recorder. If a local
recorder was selected, the monitor will try to reroute the
recording to a central recorder. Recordings configured
to a central recorder cannot be rerouted to a local
recorder. Alarm recordings may be lost. Try configuring
Printer as the alarm recording destination.
No alarm recording available No recorder available. Alarm recordings will be lost.
Try configuring Printer as the alarm recording
destination.
Central Recorder out of paper
Local Recorder out of paper
The named recorder is out of paper.
Central Recorder door open
Local Recorder door open
The door of the specified recorder is open.
<Recorder name> not supported The M1116A recorder is not supported. Connect a
M1116B plug-in recorder.

25 Recording
324

26
325
26Printing Patient Reports
Starting Report Printouts
Most patient reports can be printed by selecting Main Setup then Reports (or the Print Reports
SmartKey) and then selecting the report name in the top half of the Reports menu. Report names are
shown only for reports that have been correctly set up.
Data from the time of the print request is printed, even if the print job is delayed in the printer queue.
Your monitor can also be set up to automatically print all reports when a matching printer is available.
To set this up
1Select Main Setup then select Reports
2Select Auto Print Dbs.
–Always will print all reports when a matching printer is available.
–Host Only will print the reports stored on the host monitor when a matching printer is
available. Reports stored in the companion database (shown in gray on the Reports Job List)
must be manually sent to the printer. See “Checking Report Status and Printing Manually” on
page 330.
–Never will print no reports automatically; all reports stored in the host or companion database
must be manually sent to the printer. See “Checking Report Status and Printing Manually” on
page 330.
Printout Location
Depending on availability, reports can be printed on locally connected printers, printers connected to
the Information Center or the Application server, an external PC-based print server with Philips server
software or into the print database.
Print jobs stored in the database are automatically printed when a print device with a matching paper
size becomes available.
Print jobs in the print database are not deleted after a patient discharge. A new patient can be
admitted and their reports are saved in addition to the previous reports. Always admit your patient so
that reports can be clearly assigned to a patient.
When an X2 or MP5 is connected to a host monitor, reports requested or stored on the X2 or MP5
can be printed via the host monitor. Reports requested on the X2 or MP5 when connected to a host
monitor will not show any patient alarms or INOPs. In order to see alarms, reports should be
requested on the host monitor.
26 Printing Patient Reports
326
Starting the Different Types of Report
Stopping Reports Printouts
• To stop Reports printing, in the Reports menu, select
–Delete Report to stop the current print job
–Delete All Repts to cancel all queued report printouts
Report types Report contents How to start printing reports
Vital Signs Report depends on selected trend group, data
resolution, and period.
In the Vital Signs window, select Print/ Record, then select
Print.
Graphic Trends
Report
In the Graphical Trends window, select Print.
Events Reports Event Episode In the Event Episode or Event Review window, select the
pop-up key Print/ Record, then select Print Review or Print
Episode.
Graphic or tabular Event Review
EEG Report EEG Waves, numerics, CSAs, montage
information and impedance values
In the Setup EEG menu, select Print Report.
ECG Reports Depends on format selected Select the ECG Report A or ECG Report B Smartkeys, if
configured, or the Print Reports SmartKey followed by ECG
Report A or ECG Report B.
ST Map Report ST data in a transversal and/or horizontal
multiaxis diagram,
In the ST Map (Current) or ST Map (Trend) window, select
Print.
Cardiac Output
Report
Trial curves and numerics In the Cardiac Output (Right Heart) or Cardiac Output
(Transpulmonary) window, select the pop-up key Print/
Record.
Wedge Report Wedge numerics and reference wave In the Wedge window, select the Print Wedge pop-up key.
Calculations Report Hemodynamic, Oxygenation, or Ventilation
Review
In the Calculations windows, select the Print/ Record pop-
up key.
Drug Calculator
Report
Titration Table In the Titration Table window, select the Print Titr.Tbl pop-
up key.
Drip Table In the Drip Table window, select the Print Drip Tbl pop-up
key.
Alarm Limits Report Graphic and numeric report of all current
alarm limits
In the Alarm Limits window, select Print Limits.
Realtime Reports,
including oxyCRG
Reports
patient data and numerics, and either:
all displayed waves OR all measured waves
OR all measured RT waves Or all measured
HiRes waves, OR oxyCRG waves (RT waves:
ECG Primary lead, Pleth, Resp; HiRes
waves: btbHR, HiRes SpO2, HiRes Resp)
Select the Realtime Report SmartKey, if configured.
Loops Report Individual Loops diagram with timestamp,
currently measured numerics
In the Loops window, select Print Loop.
Battery Report Battery serial numbers, information on the
currently-measured and potential charge
status of the battery or batteries
In the Battery Status window, select Print Status.
Central Report A/B/C These are reports configured at the
Information Center. Monitors connected via
the IntelliVue Instrument Telemetry wireless
network can have these reports available.
In the Main Setup select Reports then Central Report A,
Central Report B or Central Report C.

26 Printing Patient Reports
327
–Scheduled Rep. to select Off and switch off scheduled reports.
Setting Up Reports
As the content of context-linked reports, such as Cardiac Output, Calculations, and Wedge, is defined
by the content of the procedure window these reports do not need to be set up, however a target
printer can be configured in the Setup Reports menu.
The content you define in the individual Setup Reports menus will be used in all reports of this type:
for example, if you set a print speed of 50 mm/sec in the ECG Reports menu, every ECG report will
be printed at this speed, irrespective of format.
ECG report layout and Auto Reports settings must be defined in Configuration Mode.
Setting Up ECG Reports
The settings you choose in the ECG Reports menu apply for all ECG reports printed. To set up ECG
Reports,
1Select Main Setup, Reports, then ECG Reports. Note the report layout configured for your
monitor, either Internat or Cabrera. This setting is inactive ("grayed-out") in Monitoring Mode
and can only be changed in Configuration Mode.
2Select ECG Gain and set the required ECG gain to define how ECG waves will appear on the ECG
report printouts.
3Select Speed and select the report print speed.
4Select Annotation and switch to On if the printed ECG wave should be annotated with beat labels.
See the ECG, Arrhythmia, ST and QT Monitoring chapter for a list of beat labels. Pace pulse
marks are automatically printed beside the wave for paced patients.
Setting Up Vital Signs and Graphic Trend Reports
The settings you choose in the Vital Signs Report and Graphical Trend Report menus apply for all
Vital Signs and Graphic Trend reports printed.
To set up Vital Signs and Graphic Trend reports,
Select Main Setup, Reports, then Vital Signs Rep. or Graph Trend Rep..
1Select Trend Group and select the group you want to print on the report. The groups available
depend on your monitor's trend configuration.
2Select Period and select the period of time for which trend data should be printed on the report. If
Automatic Period is configured to On, all trend data for the current patient will be printed,
irrespective which trend period is selected.
3Select Interval (Vital Signs Reports only) and select the resolution of the trend data printed on the
report,
Setting Up Auto Reports
Auto Reports print automatically when a specified trigger occurs. There are two types of Auto Reports:
Scheduled Reports, which print at predefined intervals, and End Case Reports, which print when a
patient is discharged using the End Case function. An Auto Report can be both a Scheduled Report
and an End Case report.
To set up Auto Reports,

26 Printing Patient Reports
328
1Select Main Setup, Reports, then Auto Reports and select the Auto Report you want to set up (A,
B, C, or D).
2Select Report and assign a report type to the Auto Report.
3Select End Case Report and switch to On if you want the selected report to print automatically
when you select End Case to discharge a patient.
Switch End Case Report to Off if the report is a Scheduled Report only.
4Select Scheduled Rep. and toggle to On if you want the selected report to print at predefined
intervals, starting at a predefined time of day. The start time you set applies for every following day.
For example, if you set a start time of 07:00 and a repeat time of six hours, the first report will print
at 07:00 every day, the next at 13:00 and so on.
– To set the time of day at which you want the report to print every day: select Start Hour and
Start Minute and select the required time from the pop-up list
– To set the time interval in minutes between two scheduled reports: select Rep. Freq. (hrs) and
Rep. Freq. (min) and select the time interval from the pop-up list.
If you are setting up an end case report, these settings will be inactive ("grayed-out").
Switch Scheduled Rep. to Off if the report is an End Case Report only.
5Repeat the procedure for all Auto Reports you want to set up.
All Auto Reports or Scheduled Reports set to On print automatically at the predefined trigger.
Be aware that the monitor's memory for reports is limited. If the memory is full, Auto Reports cannot
be printed and the information may be lost.
Setting Up Individual Print Jobs
To adjust the appearance of individual print jobs, in the Reports menu,
Select Main Setup, Reports, then Setup Reports to enter the Setup Reports menu.
1Select Report and then select the report you want to set up.
2Select Report Type and then select the reports template you want the report selected in Step 2 to
use. The selection of templates listed depends on the report type selected.
Each template includes patient demographic data, and each Realtime Report also includes alarm
and INOP information. In addition, the templates include:
VisibleWaves: all waves currently visible, in the order they appear on the screen.
All Waves: all measured waves.
RT Waves: all currently measured realtime waves, according to the monitor's priority list.
HiRes Waves: all measured HiRes waves.
OxyCRG Waves: the OxyCRG/Neonatal Event Review waves.
Vital Signs: trend information in tabular form.
Graph Trend: trend information in graphic form.
ECG reports: ECG3X4, ECG6X2, ECG12X1, ECG4X2, ECG8X1,ECG12X1 (2P)
EEG reports: EEG Report.
Episode: a single patient event episode.
Review: an overview of patient events
Alarm Limits: a list of all currently set alarm limits.

26 Printing Patient Reports
329
3Select Report Size to set the paper size to be used for the report: Unspecified to use the default
size for the template chosen, Universal, A4, Letter, LrgUniversal, A3, or Ledger. The list of
available sizes depends on the report type selected.
4Select Orientation to set the orientation of the report printout: Unspecified to use the default size
for the template chosen, Landscape or Portrait.
5Select Target Device and choose which printer the print job will be sent to: Unspecified to use
the default printer, or choose from the list of printer names defined at the Information Center or
in the monitor's Configuration Mode (for example, Remote 1 or Database).
Some settings may be inactive ("grayed-out") in this menu for reports that can only be started in a
special window.
Checking Printer Settings
The printer settings for your monitor are defined in Configuration Mode. The printer settings Paper
Size, Resolution, Color Support, and Duplex Option for the active printer are visible but inactive
("grayed-out") in the Setup Printers menu. When Print Database is selected as active printer only the
Paper Size setting will be shown.
To enter the Setup Printers menu, in the Reports menu, select Setup Printers.
Printer names for locally-connected printers can be defined in Configuration Mode. You can see
whether a specified printer is centrally or locally connected in the Setup Printers menu under Port. If
"Local" is included in the port name, e.g. Local 2, that indicates locally-connected printers, and
"Remote", e.g.Remote 1, indicates centrally-connected printers.
Printing a Test Report
A test report can be printed in Configuration mode, refer to the Service Guide for details.
Switching Printers On Or Off for Reports
You can enable or disable printer status to switch individual printers on or off for report printouts.
1In the Setup Printers menu, select Printer and then select the name of the device you want to
switch on or off for Reports printing from the pop-up list.
2Select Printer Status to toggle between the settings Enabled and Disabled. If you set this to
Disabled, no reports will be printed to the named printer.
If the monitor detects that no printer of a particular type is available, the Printer Status setting will
automatically be set to Disabled and "grayed out".
Dashed Lines on Reports

26 Printing Patient Reports
330
If a section of a wave on a report is drawn with dashed lines, this tells you that a setting that affects the
appearance of the wave on the screen was changed while the report was printing.
For example, if you change the wave scale while a report is printing, the wave scale and wave size are
changed immediately on the monitor screen and on the report. To indicate that the scale information
printed at the beginning of the report no longer matches the currently used scale, the wave will be
printed using dashed lines, starting from the moment the change took place.
Some examples of settings that cause dashed lines in reports if changed during printing are: Filter
mode, ECG lead placement, wave scale, measurement unit, paced/non-paced setting, and
measurement mode. Note that as ECG waves are drawn with a fixed gain on reports (either 10 mm/
mV or 20 mm/mV), changing the ECG wave scale will not cause dashed-line reports.
To avoid dashed lines on reports, wait 15 seconds after changing a setting before you trigger a report.
Unavailable Printer: Re-routing Reports
If you send a report to be printed on a printer that is not available, for example, because it has run out
of paper, this print job is suspended and stored in the monitor's memory.
If the target device of this print job was set to Unspecified, the monitor will periodically try to resend
the print job to the first printer listed in the Setup Printers menu under Printer that is set to Enabled
and that has paper of the correct size.
To allow the report to print, you must either solve the problem with the target printer, or re-route the
print job to another printer with paper of the correct size. To re-route a print job,
• Enable the new target printer by selecting it in the Setup Printers menu and toggling to Enabled.
As the monitor tries to send the report to the printers in the order they are listed, you must make
sure that all the printers above the new target printer are disabled.
If the target device of the print job was set to a specific printer, re-routing is not possible.
Checking Report Status and Printing Manually
A list of all print requests which are waiting, printing or stored can be viewed in the Reports Job List.
To view the list, in the Reports menu, select Reports Job List.
The following information is displayed for each print request:
• Report title
• Patient name (except for system reports such as the battery status report)
• Request date and time
• Report paper format
•Job status: Preparing, Printing, Waiting, In Database, In Companion, Retry, Cancelling, Error.
Individual reports can be deleted from the list with the Delete Report key, and all reports with the
Delete All Repts key.
CAUTION
The Reports Job List includes privacy information, in the form of the patient name with the related
report title and date. It is advisable to provide controlled access to this data to ensure confidentiality.
26 Printing Patient Reports
331
If an MP5 or an X2 is connected to a host monitor, all print requests which are stored in the print
database are shown "grayed out" on the Reports Job List and will not be deleted with the Delete All
Repts key.
Printing Manually
Those jobs shown in black will be printed automatically when a matching printer is available. If the
Auto Print Dbs setting is Host Only or Never, some or all reports will not be printed automatically and
will be shown in gray. Any jobs shown in gray must be printed manually; to do this,
1In the Reports Job List, select the required report
2Select Print Report.
Selecting Print All Reps will send all reports to the printer.
Printer Status Messages
Printer Status Message Possible causes and suggested action
Print job queued for <Printer
Name>
The report has been placed in the queue for the named printer.
Print job could not be queued
(insufficient resources)
Print job could not be queued
(queue is full)
Print job could not be queued (no
matching printer found)
The printer queue is full and the monitor cannot accept another report request.
Wait until some more reports have been printed, then try again, OR
A report has been triggered that uses a paper size unavailable with the target
printer. Try another printer, if available, or change the paper size of the print
request.
Cancelling all print jobs Delete All Reps has been selected in the Reports menu, OR
The Operating Mode has been changed from Monitoring Mode to
Demonstration or Service Mode.
Cancelling the active print job The current report is being canceled as the result of a user request.
Cancelling print jobs due to
patient discharge
When a patient is discharged, all queued reports are canceled except those
stored in the print database.
Cancelling # print jobs due to
hotstart
The monitor has restarted and all report requests have been canceled except
those stored in the print database. "#" is the number of reports canceled.
Printing failed: No report
configured!
A report has been triggered which has not been correctly set up. Enter the setup
menu for the report type to set up the report.
Printing on <Printer Name>... A report is in progress, or the monitor is waiting for the central printer to accept
the print job.
26 Printing Patient Reports
332
Sample Report Printouts
Each report header contains the patient's bed label, last name and first name, middle name (if there is
enough space) the patient ID, the date and time, and the name of the report. The report footer
contains the hospital label and page number, and the last page contains a note to mark the report end.
The monitor may be configured to leave a space on the top left or right of the report printout to enable
you to stick a patient address label on it. This setting is called the Addressograph and it can only be
changed in the monitor's Configuration Mode.
Printer <Printer Name>
unavailable -> job suspended
The chosen device is unavailable. Check that the printer is properly connected
and that paper is available. The requested report will start printing when the
printer becomes available.
Print database full -> job
suspended
The requested report does not fit into the print database. You can select another
printer to print the report (see “Unavailable Printer: Re-routing Reports” on
page 330). Alternatively you can delete another report from the Reports Job
List (using the Delete Report key) to create space for your report.
Job on <Printer Name> failed
(data unavailable)
Job on <Printer Name> failed
(printer unavailable)
Job on <Printer Name> failed
(data requisition error)
A report cannot be started on the requested printer.
One of three reasons is shown in the status message:
• data unavailable - the connected X2 or MP5 has been removed before the
data for the report was transferred.
• printer unavailable - make sure the printer is plugged in, switched on, and
has paper loaded.
• data requisition error - an internal error has caused data required for the
report to be unavailable, try starting the report again.
Print job on <Printer Name>
done
The report has been printed.
Printer Status Message Possible causes and suggested action
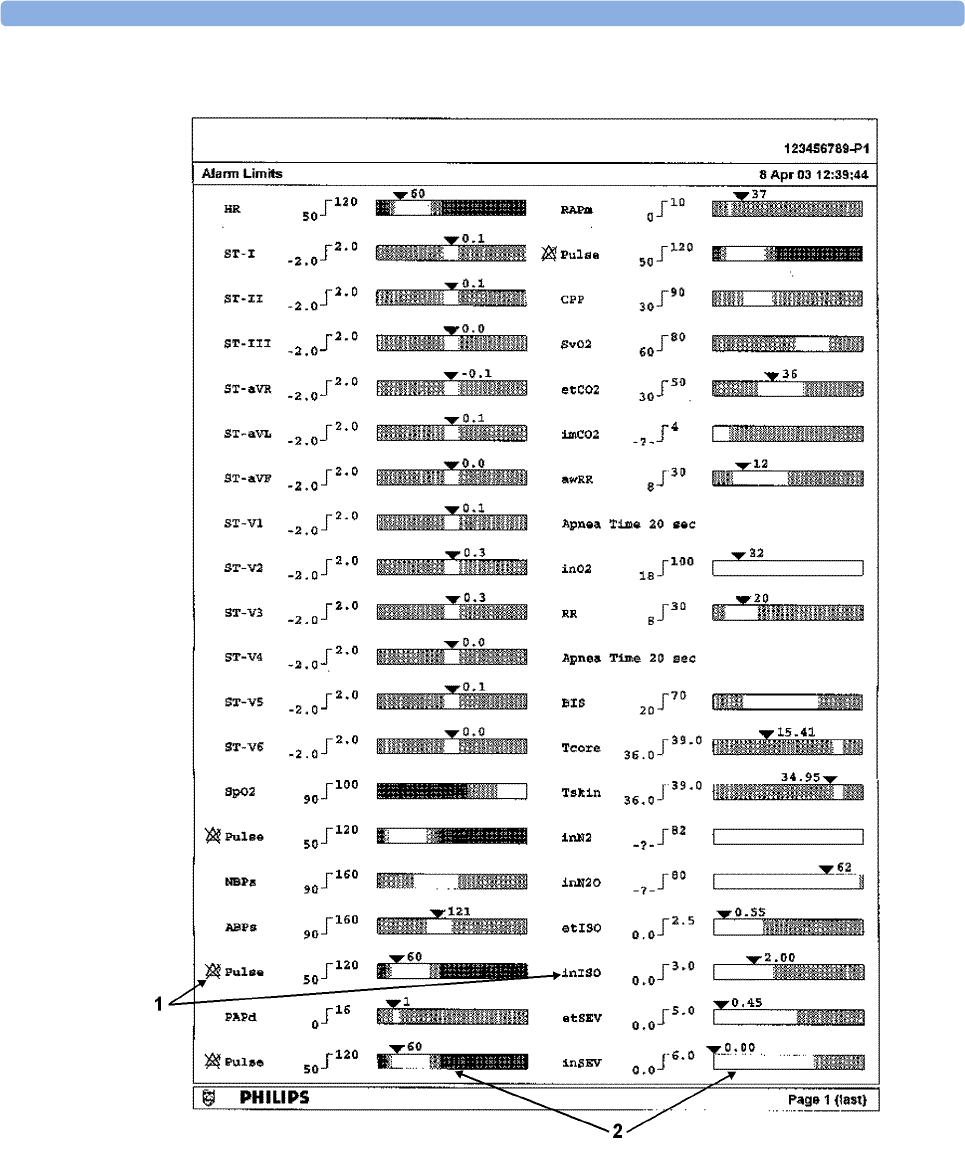
26 Printing Patient Reports
333
Alarm Limits Report
1Measurement labels, with alarms off symbol where alarms are switched off
2Graphic view of current alarm limits in relation to currently monitored measurement value
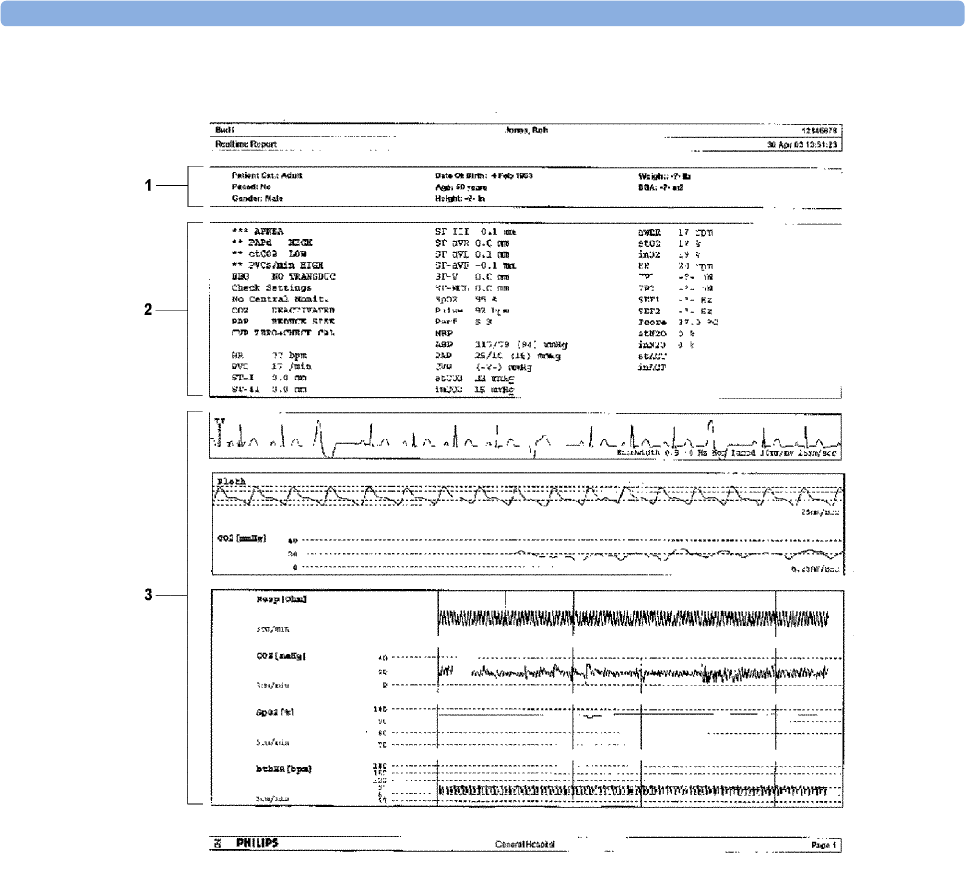
26 Printing Patient Reports
334
Realtime Report
1Patient demographic information, time stamp
2Active Alarms and INOPs, followed by vital signs
3Measurement waves section
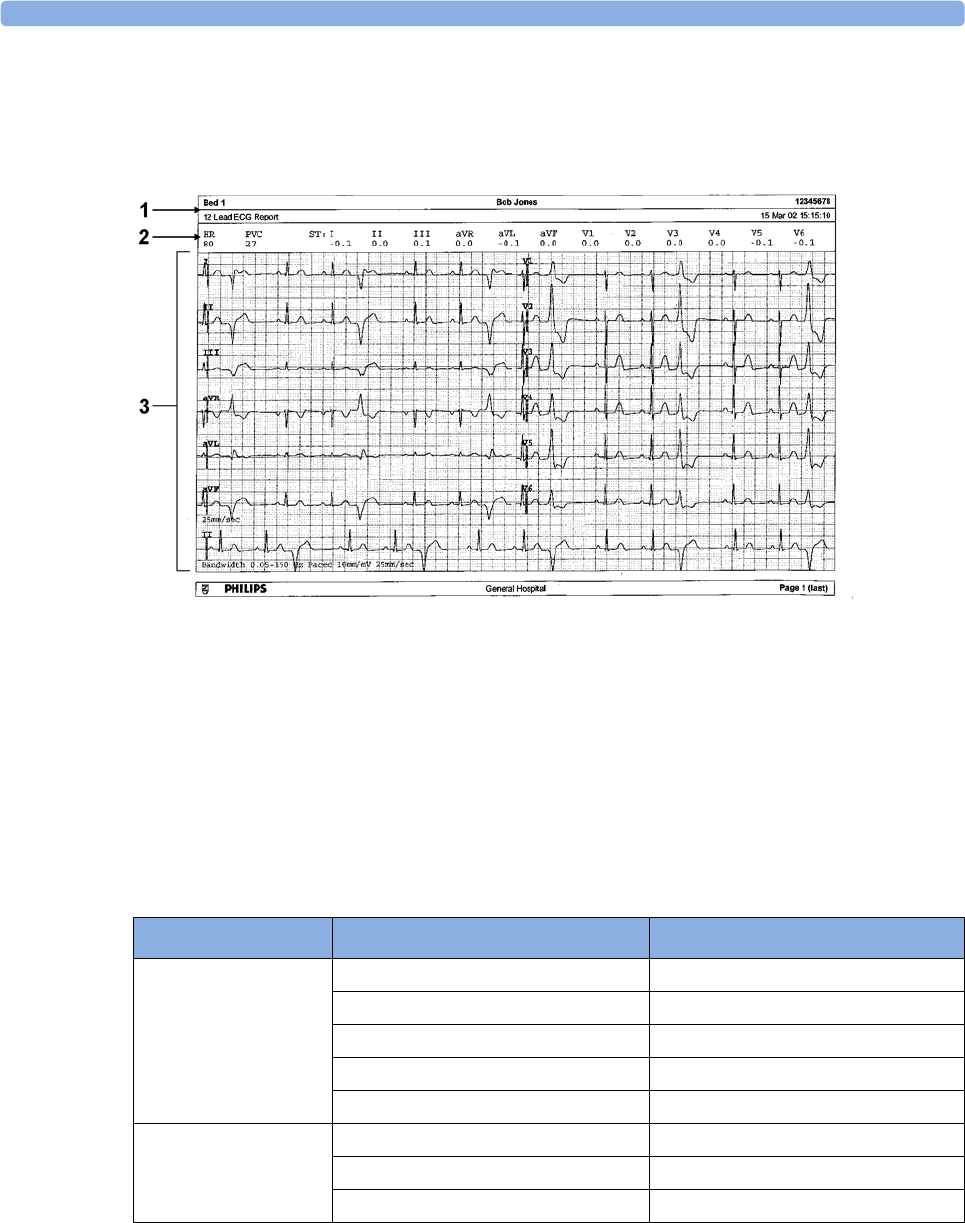
26 Printing Patient Reports
335
Cardiac Output Report
ECG Reports
1Patient information
2Numeric block
3Wave area
Below the header on ECG Reports, the numeric block shows the current HR, PVC, and ST values.
The wave area shows the printed waves for all available ECG leads. A 1 mV calibration bar is printed
at the beginning of each wave. With the 3X4, 6X2, and 2X4 formats, a rhythm stripe prints a longer
section of the ECG wave from the primary ECG lead for ECG rhythm evaluation. The ECG signal
bandwidth, the patient's paced status, the ECG gain, and the print speed are printed at the bottom of
the wave area. Pace pulse marks are automatically printed beside the wave for paced patients. Beat
labels can be set to print on the rhythm stripe. The 12X1 (2P) format prints the report over two pages.
Other Reports
See the sections on Trends and Calculations and the chapter on Event Surveillance for other example
reports.
ECG Report type Available Formats Available Paper Sizes
12-Lead ECG 3X4 landscape A4, letter, A3, ledger
6X2 landscape A4, letter, A3, ledger
12X1 portrait A4 and letter only
12X1 landscape A4, letter, A3, ledger
12X1 (2P) landscape A4, letter (2 pages)
Multi-lead ECG 2X4 landscape A4, letter, A3, ledger
8X1 portrait A4 and letter only
8X1 landscape A4, letter, A3, ledger

26 Printing Patient Reports
336
27
337
27Using the Drug Calculator
Drug mixtures for intravenous (IV) drug infusions combine information on drug dose, rate, amount,
volume, concentration, and standardized rate. The Drug Calculator helps you to manage infusions by
calculating one of these values at a time.
*Be aware that your hospital may use either 'µg' or 'mcg' as an abbreviation for microgram. These
abbreviations are equivalent.
WARNING
Before you administer any drug, always check that the correct calculation units and patient category are
selected. Consult your pharmacy if you have questions.
Decisions on the choice and dosage of drugs administered to patients must always be made by the
physician in charge. The Drug Calculator performs calculations based on the values input during use, it
does not check the plausibility of the calculations performed.
Ter m Definition Units
Dose total quantity of drug to be delivered to
the patient over time
amount units per time or per kg/
time, if the drug is weight-
dependent
Rate volume of the mixture to be delivered to
the patient over time
ml/hour
Amount amount of drug to be added to diluent
to make up a mixture
ng, mcg*, mg, g, mUnit, Unit,
where g stands for gram
Volume quantity of mixture of diluent and drug ml
Concentration ratio of the amount of drug to the
solution volume
amount units per ml
Standardized Rate 1ml volume of the mixture to be
delivered to the patient per hour
ml/hr
27 Using the Drug Calculator
338
Accessing the Drug Calculator
To access the Drug Calculator, select Main Setup then Calculations followed by Drug Calculator, or
select the Drug Calc SmartKey, if configured.
Performing Drug Calculations
Using the service Support Tool, a list of drugs can be configured for the monitor containing pre-
defined dosage recommendations and unit settings. Selecting the arrow beside the drug name in the
Drug Calculator window opens a list of configured drugs. Contact your pharmacist if you have any
questions about the drugs in the list.
If ANY DRUG is the only entry in the list of drugs, no drugs have been pre-configured for your
monitor. Drug calculations can be performed for non-specific drugs.
You must have a Support Tool to add additional drugs to the Drug Calculator.
About the Rule of Six
If the Rule of Six has been enabled for use with individual drugs in your Drug Calculator, you can use
the formula in crisis situations to quickly calculate the amount of a drug needed to yield a target dose
for continuous infusion for neonatal or pediatric patients (the drug amount is given in "mg", the
patient weight in "kg"). The Rule of Six can only be used with the dose unit mcg/kg/min.
CAUTION
JCAHO recommends disabling the Rule of Six. The configuration is not JCAHO-compliant if Rule of
Six is enabled.
The Drug Calculator uses the following formula for Rule of Six calculations, based on the patient's
weight:
• For a target dose of 0.1 mcg/kg/min, the Drug Calculator multiplies 0.6 x patient weight to
calculate the amount you need to add to the IV solution to equal a total of 100 ml.
• For a target dose of 1.0 mcg/kg/min, the Drug Calculator multiplies 6.0 x patient weight to
calculate the amount you need to add to the IV solution to equal a total of 100 ml.
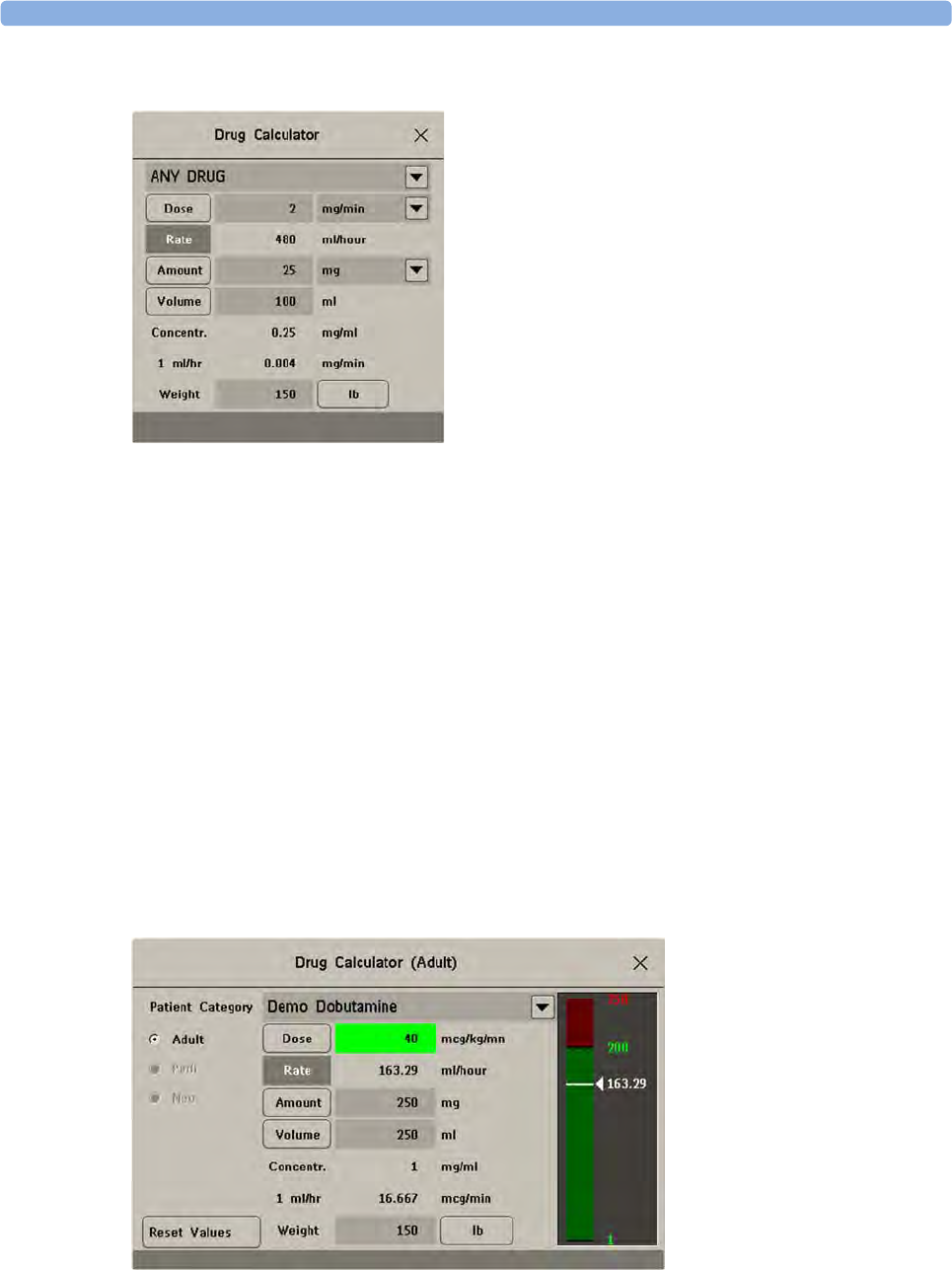
27 Using the Drug Calculator
339
Performing Calculations for a Non-Specific Drug
If a list of drugs has not been configured for your monitor, you can use the Drug Calculator to
calculate drug doses for a single, generic drug called ANY DRUG. Selecting the arrow beside the drug
name in the Drug Calculator window shows that are no other drugs configured.
1Enter three of these four values: dose, amount, volume, rate of the infusion solution.
To enter values, select the correct unit, then select each value field and use the pop-up keypad to
enter the correct value.
2If you have chosen a weight-dependent dose unit, you must enter the patient weight now or
choose a different unit.
If available, the patient weight from the Patient Demographics window is entered automatically in
the Drug Calculator window when the Drug Calculator is accessed. To change the patient weight,
select the Weight key then use the on-screen keypad to enter the correct value. This will not
change the patient weight stored in the patient demographic information.
3When you have entered three values, the Drug Calculator automatically calculates the unknown
fourth value and shows it in the highlighted field. Standardized rate and concentration are also
calculated.
Performing Calculations for a Specific Drug
1Select the arrow beside ANY DRUG, then select the required drug from the list of drugs. This
opens the window for the selected drug.
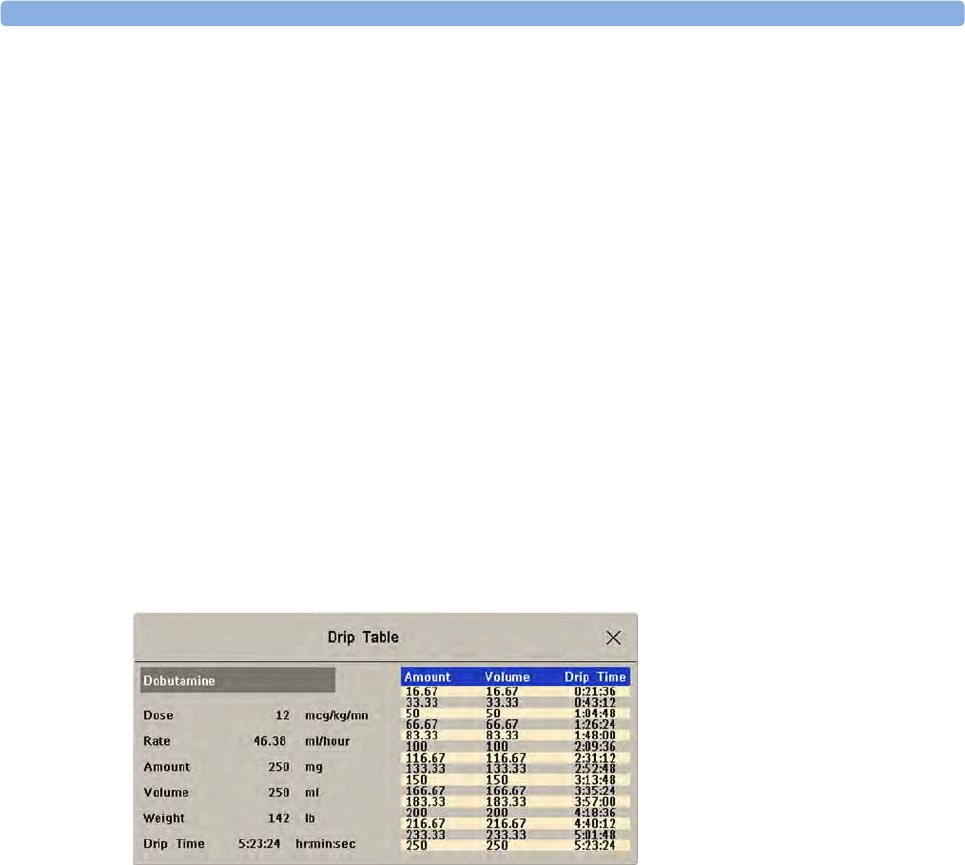
27 Using the Drug Calculator
340
2Select the correct patient category for your patient.
If you have a neonatal or pediatric patient, the Rule Of 6 choice may be available. Select if required.
3Enter the patient weight, if necessary.
If available, the patient weight from the Patient Demographics window is entered automatically in
the Drug Calculator window. To change the patient weight, select the Weight key then use the on-
screen keypad to enter the correct value. This will not change the patient weight stored in the
patient demographic information. Select the weight unit shown to change between lb and kg.
4When a specific drug is selected, the initial values for Dose, Amount and Volume are the
configured Start values for this drug. The Rate is then calculated. If other values are required you
can calculate any value by entering the remaining three values as described in “Performing
Calculations for a Non-Specific Drug” on page 339.
The column on the right of the window shows either drug dose or dosage rate, whichever is the
calculated value. The current calculated value is shown on a scale with the recommended range in
green. If the current calculated value lies outside the recommended range it is shown in red.
If you have changed values in the Drug Calculator and you want to revert to the configured values,
select Reset Values key at any time.
Charting Infusion Progress
The Drip Table shows you at a glance how much of the infusion has been administered to your patient
and how much time is left.
• To see the Drip Table, in the Drug Calculator window, select the Drip Table pop-up key.
If the Drip Time exceeds 24 hours, the Drip Time timestamp shows - - :- - : - - .
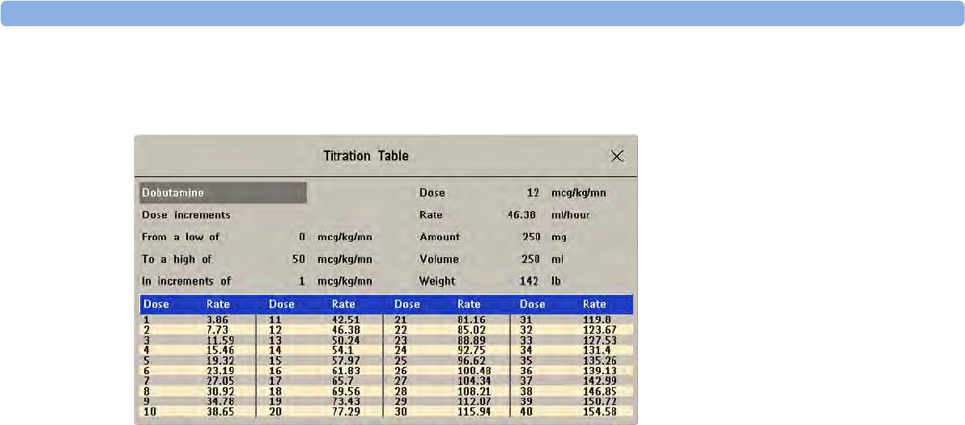
27 Using the Drug Calculator
341
Using the Titration Table
Use the Titration Table to see at a glance what dose your patient would receive of a drug at different
infusion rates. By clicking on the title row of the table you can switch between the Dose increments
and Rate increments view.
Values outside of the recommended range are shown in red.
To see the Titration Table,
•in the Drug Calculator window, select the pop-up key Titr. Table.
The Titration Table is configured with the service Support Tool.
Documenting Drug Calculations
•In the Drug Calculator window, select the pop-up key Record DrugCalc to immediately start a
recording of the current drug calculation.
•In the Titration Table window, select the pop-up key Print Titr.Tbl to print a report of the current
Titration Table.
•In the Drip Table window, select the pop-up key Print Drip Tbl to print a report of the current
Drip Table.

27 Using the Drug Calculator
342
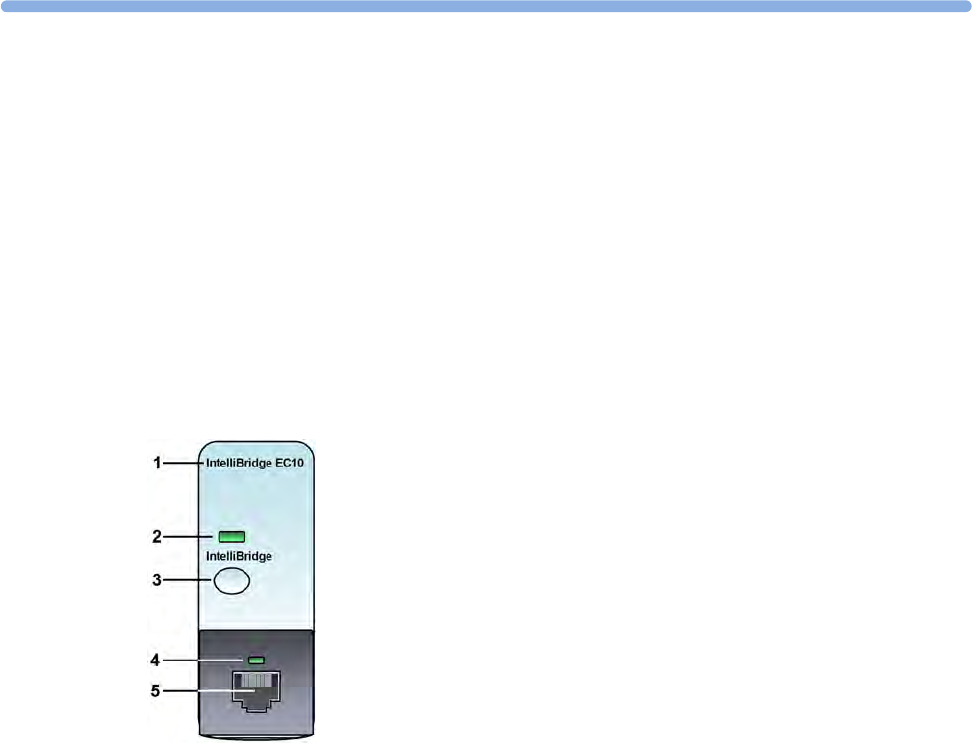
28
343
28IntelliBridge EC10 Module
An IntelliBridge EC10 module transmits information from a connected external device to your
monitor. The IntelliBridge EC5 ID module is used to provide identification information from the
external device. Data imported from the external device, for example waveforms, measurement
numerics, settings and alarms, can be displayed on the monitor, passed on to an Information Center
and included in trends as appropriate. The external device may show more information than is
available on the monitor. Data from IntelliBridge EC10 modules cannot be included in monitor trends
when the label is a free-text label.
See the documentation supplied with the IntelliBridge module for a list of supported devices and
accessories, and for configuration information.
Connecting an External Device
1Insert the module into the FMS or integrated module slot.
2Check that you have the correct EC5 ID module for the external device - indicated on the EC5
label.
3Connect the EC5 ID module to the external device.
4Connect the EC5 to the EC10 module using the supplied cable.
5Switch the external device on.
6The connection status LED (4) will flash green until it has correctly identified the external device
and started communication. Check that the connection status LED then lights green continuously
indicating that communication has been established.
1module name
2setup indicator LED
3setup/data viewing key
4connection status LED
5external device cable connector
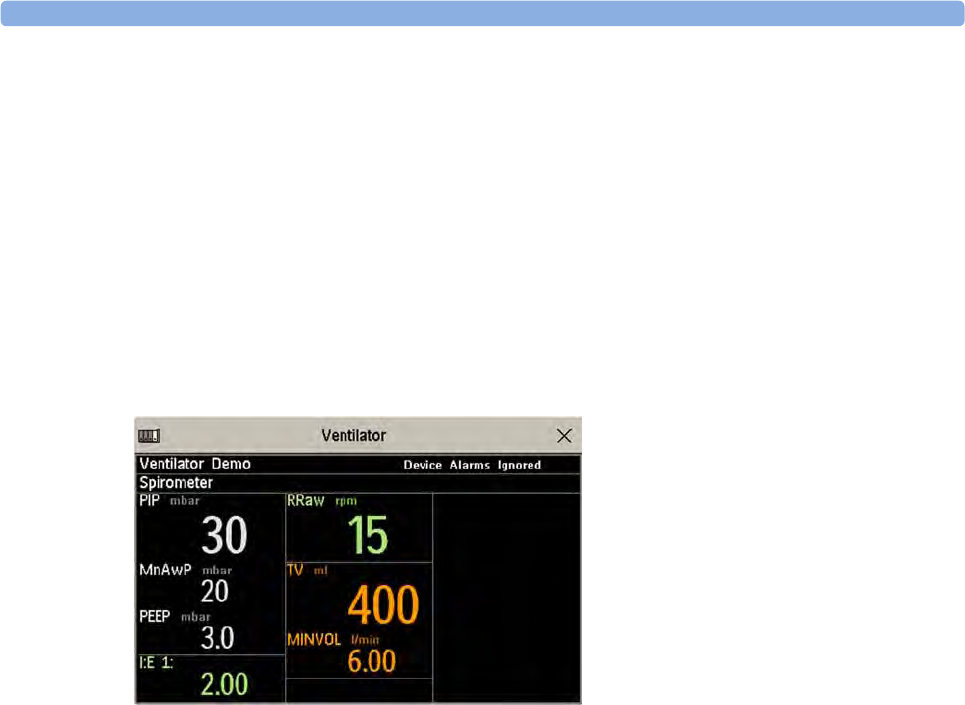
28 IntelliBridge EC10 Module
344
Changing Waves and Numerics Displayed
To change the waves and numerics from the IntelliBridge module displayed on the Screen,
1Select Main Setup, Measurements, then <External Device> to enter the setup menu for the
connected device.
2Select Setup Driver.
3Select Setup Wavesor Setup Numerics and make the changes required.
4Close the setup menu. The monitor takes a few seconds to activate the change.
Viewing the IntelliBridge Device Data Window
To view the IntelliBridge device data window, either
• select the setup key on the IntelliBridge module, or
• select the External Devices SmartKey and then select the pop-up key with the device name on it,
or
•in the Setup <External Device> menu, select Show Device Data.
Check that the correct external device ID is shown in the window title.
Select the device data window then Setup Device to open the setup menu for the connected device.
With the More Data key you can page through additional data which does not fit on the first screen.
When an infusion system is connected the data is presented differently. The data from each pump is
displayed in a horizontal frame in the window. Data from several infusion pumps can be displayed.
To see a detailed information window for one of the pumps, you can select data for that pump on the
Screen or select the More Data pop-up key.
Using Screens with External Device Data
Your monitor may be configured to show external device data permanently on the Screens.
Select the device data window to display the pop-up keys that let you access the setup menu and make
changes.
28 IntelliBridge EC10 Module
345
Alarms/INOPs from External Devices
The IntelliBridge module itself generates INOPs, but does not generate alarms. If the external device's
alarms are on, the module transmits these to the monitor. A message in the External Device Data
window tells you either Device Alarms Ignored or Device Alarms Accepted or No Alarms Available.
External device alarms status symbols precede some, but not all, measurement labels.
Alarms from external devices are transmitted to the monitor. For all numerics configured in the setup
menu, an alarm condition is announced at the monitor. For one or more measurements not configured
in the setup menu, an alarm is announced as a text message for the highest priority alarm. Priority is
determined at the external device.
Refer to the documentation supplied with the IntelliBridge module for details of how alarms are
announced on the monitor and the Information Center.
INOPs from the IntelliBridge Module
Language Conflict with External Device Drivers
You should avoid language conflicts between the IntelliBridge module device driver and the monitor.
Be aware that if you connect an IntelliBridge module with a different operating language to the
monitor, the monitor will show:
• measurement labels in the monitor language
• alarm and INOP texts in the IntelliBridge module device driver language.
the monitor is configured to accept external device alarms, but the alarms are
switched off at the external device.
INOP Text INOP Condition
!!NO DEVICE DATA
!!!NO DEVICE DATA
Communication has been lost to a connected device when
– !! a medium priority INOP or patient alarm was present
– !!! a high priority INOP or patient alarm was present
NO DEVICE DATA Communication has been lost to a connected device with no (or
only low priority) INOPs/physical alarms.
DEVICE UNSUPPORTED Device identification completed but no appropriate device driver
installed
DEVICE CHECK CONF. Device identification completed but communication could not be
established due to errors
DEVICE CHECK SETUP Device identification completed but communication could not be
established due to timeout

28 IntelliBridge EC10 Module
346
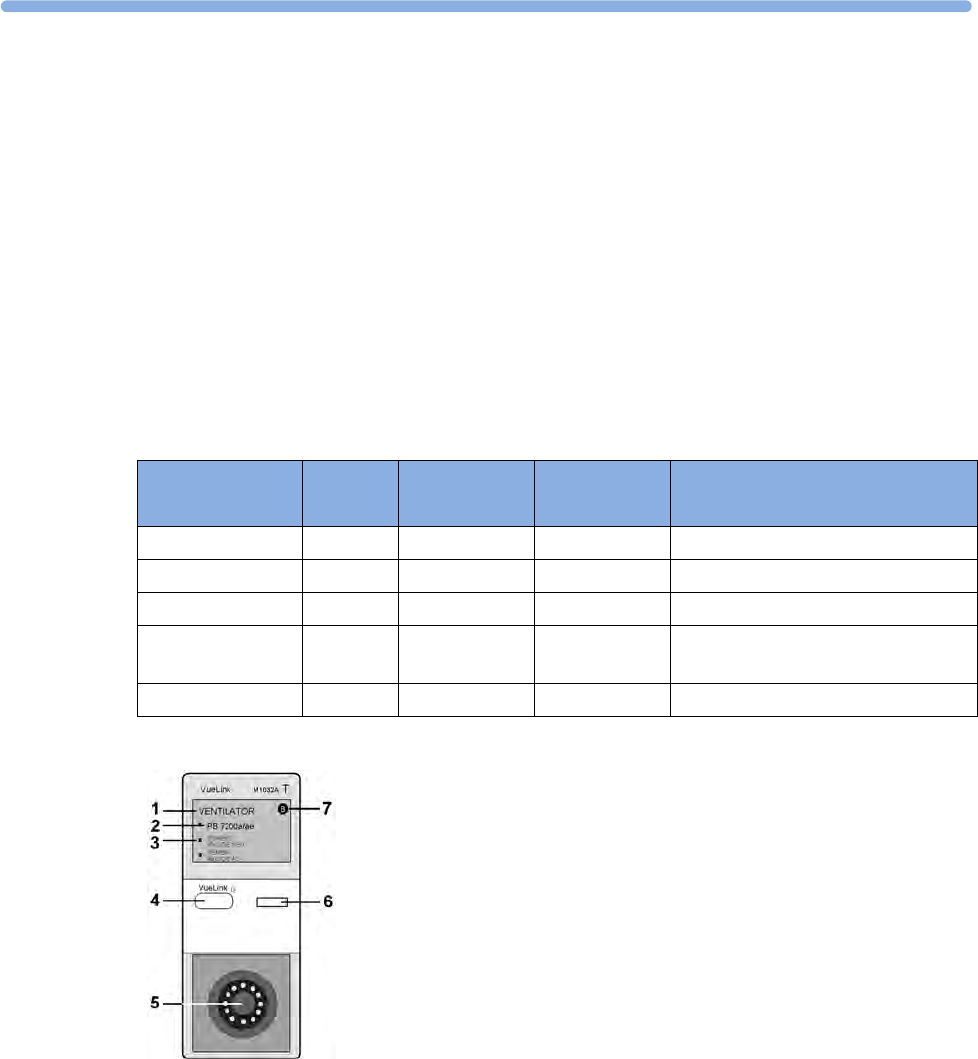
29
347
29VueLink Modules
A VueLink module transmits information from a connected external device to your monitor. Each
module can be connected to one of up to three preselected external devices, and supports alarms from
the external device. Data from VueLink modules cannot be included in monitor trends when the label
is a free-text label.
The external device may show more information than is available on the monitor. The number of
waves and numerics you can view simultaneously on your monitor's main screen depends on the
module type. Type A modules support one wave and two numerics, type B modules support two
waves and six numerics.
The device labels (2) on the module indicate for which external devices the module is configured. The
selection LED (3) shows which device is currently active. The device label text may differ slightly from
the labels on the external devices.
Module Type Max. Wave Max.
Numeric
External Devices
Auxiliary A 1 2 standalone measurement module
Ventilator B 2 6 ventilators
Gas Analyzer B 2 6 gas analyzers
Anesthesia
Machine
B 2 6 anesthesia machines
Auxiliary Plus B 2 6 external multi-measurement devices
1module name
2device label
3selection LED
4setup key
5external device cable connector
6setup indicator LED
7module type (A or B)
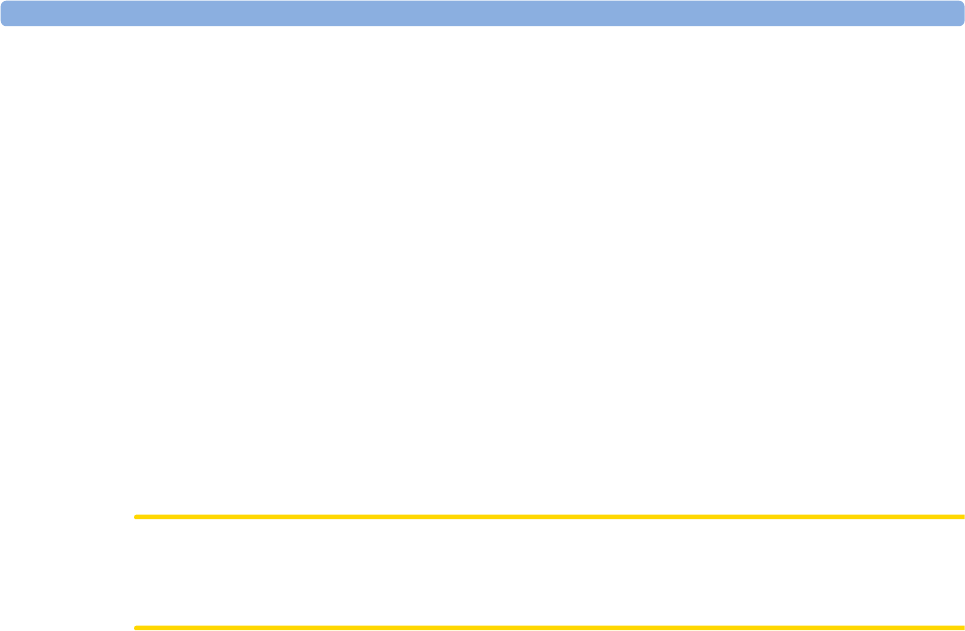
29 VueLink Modules
348
See the documentation supplied with the VueLink module for a list of supported devices and
accessories, and for configuration information.
Connecting an External Device
1Insert the module into the FMS or integrated module slot.
2Check that the device selection LED (3) lights to show that it has correctly identified the external
device. If not, select Main Setup, Measurements and then the name of the external device to
enter the setup menu for the connected device.
3In the device setup menu, select Device, select the correct device from the list, and confirm the
selection.
4Connect the external device to the module and switch it on.
Once the VueLink device has been correctly connected, you can select the External Devices
SmartKey and then select the Setup Device pop-up key to access the setup menu for the connected
device.
CAUTION
Selecting the wrong device can cause unpredictable system behavior. Rectify this by switching off the
external device when it is safe to do so, and selecting the correct device.
Changing VueLink Waves and Numerics Displayed
To change the waves and numerics from the VueLink module displayed on the Screen,
1Select Main Setup, Measurements and then the name of the connected device to enter its setup
menu.
2Select the item you want to change, then select the new item from the pop-up list,
or
Select Show Device Data to view the device data window.
3Close the setup menu. The monitor takes a few seconds to activate the change.
29 VueLink Modules
349
Viewing the VueLink Device Data Window
1Mode information from external device
2Name of external device
3Type of external device
4Device Alarms Accepted
To view the VueLink device data window, either
• select the setup hardkey on the VueLink module or the External Devices SmartKey, and then
select the pop-up key for the device, or
•in the Setup <External Device> menu, select Show Device Data.
Select the device data window then the Setup Device key to open the setup menu for the connected
device.
Using VueLink Screens
Your monitor may be configured to show VueLink device data permanently on the Screens.
Select the device data window to display the external device pop-up keys that let you access the setup
menu and carry out external device tasks.
Switching VueLink On and Off
• To switch VueLink measurements on and off, in the setup menu for the external device, select
Device Interface to toggle between the settings On and Off.
29 VueLink Modules
350
Alarms/INOPs From External Devices
The VueLink module itself generates INOPs, but does not generate alarms. If the external device's
alarms are on, the module transmits these to the monitor. A message in the VueLink info window tells
you, depending on the configuration setting, either Device Alarms Ignored or Device Alarms
Accepted or, when the external device is not supplying alarm data, No Alarms Available. When
Device Alarms Ignored is set, alarms from the external device will not be displayed on the monitor
and will not be transmitted to the Information Center. External device alarms status symbols precede
some, but not all, measurement labels.
Alarms from external devices are:
• transmitted to the monitor. For all numerics configured in the setup menu, an alarm condition is
announced at the monitor. For one or more measurements not configured in the setup menu, an
alarm is announced as a text message for the highest priority alarm. Priority is determined at the
external device.
• always non-latching on the monitor.
• announced as a flashing numeric while the alarm condition persists.
• announced audibly and visibly at the Information Center.
Language Conflict with External Device Drivers
You should avoid language conflicts between the VueLink module device driver and the monitor. Be
aware that if you connect a VueLink module with a different operating language to the monitor, the
monitor will show:
• measurement labels in the monitor language
• alarm and INOP texts in the VueLink module device driver language.
the monitor is configured to accept external device alarms, but the alarms
are switched off at the external device.
!alarms status of this external measurement is unknown
30
351
30Using Timers
With the Timers function you can set timers to notify you when a specific time period has expired.
CAUTION
Do not use the timers to schedule critical patient-related tasks.
Viewing Timers
You can view currently active timers in the Timers window or directly on the Main Screen (if a timer
has been substituted for a numeric).
To open the Timers window:
• Select the Timer SmartKey
or
•Select
Main Setup then select Timer
The maximum number of timers which can be active depends on your monitor model.
For a timer with a defined run time a progress bar is shown with the run time for that timer. Next to
the progress bar the elapsed time or the remaining time is shown, depending on whether the timer is
counting up or down. On the left, the label of the timer and a symbol indicating the type of expiry
notification is shown.
Timer Types
There are four types of timer: Basic, Enhanced, Cyclic and No Limit. A Basic timer has a single,
defined run time and progress is shown in the progress bar. An Enhanced timer is like a Basic timer
but the progress bar shows progress beyond the end of the run time. A Cyclic timer is like a Basic
timer but restarts automatically when the run time is expired. A No Limit timer has no run time or
progress bar and shows the time elapsed since the timer was started.
The type of timer is set in the monitor's Configuration Mode and is associated with the timer label.
30 Using Timers
352
Timer Setup Pop-up Keys
When you open the Timers window and select a timer, then select the setup key, the setup window
opens and a selection of pop-up keys appear to let you activate and control the timers.
Setting Up Timers
The timer type, display color of the timer and whether a window automatically pops up on expiry are
settings made in Configuration Mode for each timer label.
The remaining timer settings can be made in Monitoring Mode. If you change settings when a timer is
running it will not be stopped. The timer will continue to count but the new settings will be applied.
To display the setup window for a timer,
•in the Timers window, select the required timer, then select the setup key or
• select a timer on the Screen then select Setup Timers.
Timer Label
You can select from a variety of specific labels, for example Tourniquet, Infus, Docu or from four
non-specific labels TimerA, TimerB, TimerC, and TimerD. When you assign a label to a timer, the
monitor automatically applies the associated configuration settings to this timer, but the timer
continues counting and is not reset.
To select a label, in the Timers window:
1Select the required timer and display the Setup window.
2Select Label.
3Select a specific or non-specific label from the list.
Run Time
The run time can be set between 1 minute and 96 hours. No Limit timers have no run time.
To set the run time, in the Timers window:
1Select the required timer and display the Setup window.
2Select Run Time.
3Select a run time from the list.
Pop-Up Keys Selecting this pop-up key lets you....
Start start the timer.
Stop stop the timer, allowing either restarting after a pause (Start key) or clearing
(Clear key).
Clear clear the timer, ending this timer episode.
Timers return to the timer window showing all active timers

30 Using Timers
353
Timer Counting Direction
Timers can count up or down, showing elapsed time or remaining time. No Limit timers automatically
count up.
To change the direction, in the Timers window:
1Select the required timer and display the Setup window.
2Select Direction to switch between Up and Down.
Notification
When a timer expires (except a No Limit timer), the color changes to red and a message appears in the
status line on the Main Screen. Be aware that if a timer has been configured to display in light red, the
color will not visibly change when the timer expires.
Additional notification is also available and can be set to:
Alarm: An INOP alarm indicates the expiry of the timer
Sound: A single tone indicates the expiry of the timer
No Sound: No additional notification
To set the additional notification, in the Timers window:
1Select the required timer and display the Setup window.
2Select Notification and select the notification level required from the list.
If an MP5 is connected to a host monitor, and notification is set on the MP5 to Alarm, the INOP
alarm will appear on the host monitor TimeExpired:MMS.
Timer Volume
For all Timers with the notification setting Sound, you can set the volume of the tone.
To set the volume, in the Timers window:
1Select the required timer and display the Setup window.
2Select Timer Volume and select a volume setting from the list.
Displaying a Timer On The Main Screen
If you want to have a timer displayed on the Main Screen, you can substitute it for a numeric which is
not directly associated with a wave. If limited space is available, some of the timer display elements
may not be displayed. The minimum information displayed is the label and the elapsed or remaining
time.
30 Using Timers
354
To display a timer on the Main Screen:
1Select the numeric you want to substitute.
2Select Change Numeric.
3Select Any Timer.
Main Screen Timer Pop-up Keys
When you select a timer displayed on the Main Screen, additional pop-up keys become available:
Displaying A Clock On The Main Screen
In the same way that you can substitute a timer for a numeric, you can also substitute a larger clock
display for a numeric.
To display a clock on the Main Screen:
1Select the numeric you want to substitute.
2Select Change Numeric.
3Select Clock.
When you select the clock on the Main Screen you can select Date, Time in the menu to set the date
and time.
Pop-Up Keys Selecting this pop-up key lets you....
Setup <Timer Label> enter the setup screen for the currently selected timer.
Change Timer select a different timer for display.
Timers enter the Timers window.
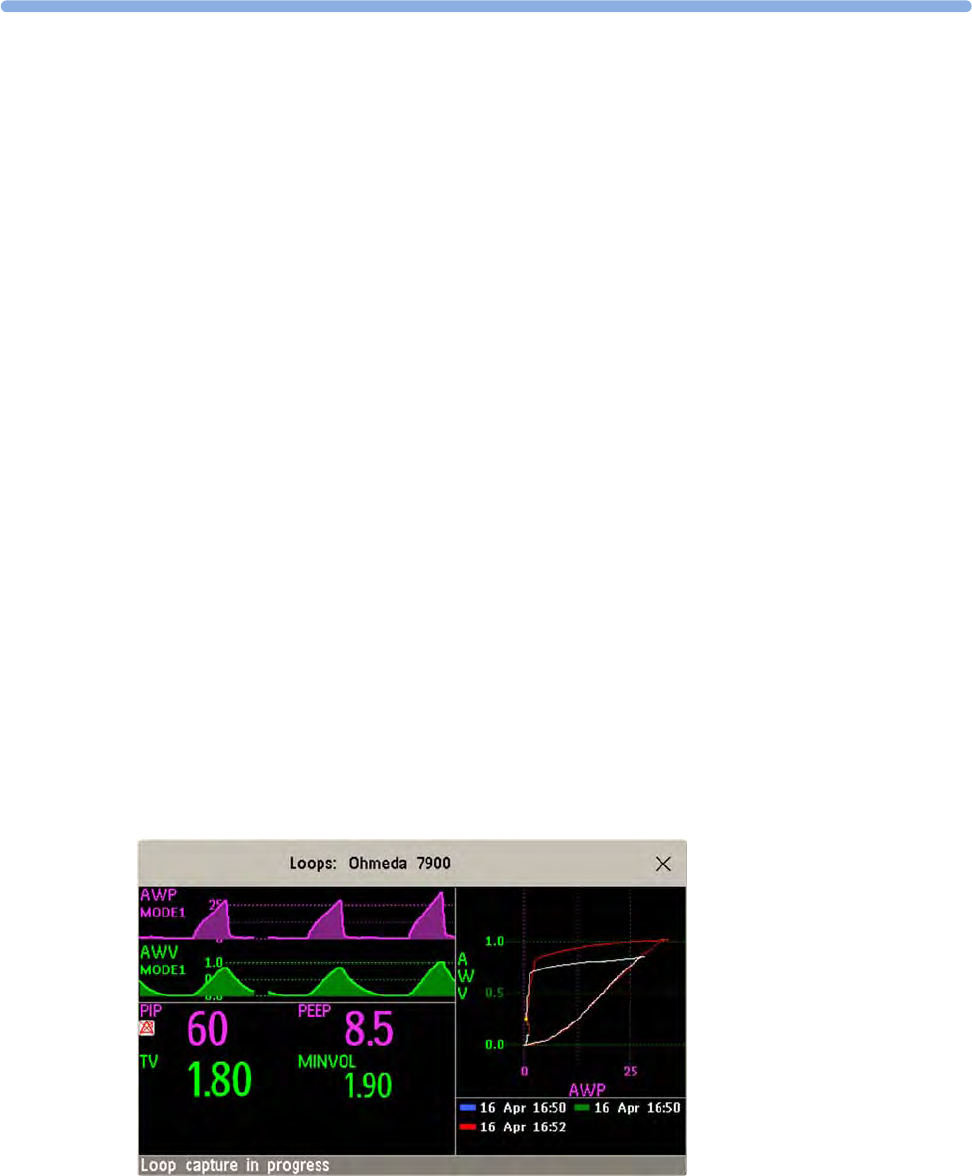
31
355
31Respiratory Loops
Using a Spirometry module or a VueLink/IntelliBridge module connected to a ventilator, you can
measure and store graphic representations of realtime respiratory loops. Respiratory loops can help
you recognize changes in your patient's lung function, and they can also indicate a fault in the airway
tubing (for example, if the respiratory loop does not close).
You can measure:
• Pressure-volume loops
• Pressure-flow loops
•Volume-flow loops.
Note that you cannot store loops from different patients and different source devices in the same list
as they are patient and device specific. This prevents you from inadvertently comparing information
from different patients.
Viewing Loops
In the loops display, the current loop is drawn in white, and up to six stored loops are color-coded to
match their timestamps. The currently-used source device is shown in the window title.
To view respiratory loops permanently on your Screen,
• select the current Screen name to open the Change Screen menu, then select a Screen configured
to display the loops screen element.
Select the loops screen element to access the loops pop-up keys.

31 Respiratory Loops
356
To open the Loops window, and its associated pop-up keys,
•select
Main Setup then Loops, or select the Loops SmartKey, if configured.
In the Loops window, in addition to the stored loops, two realtime airway waves and up to nine
available numerics from the source device can be shown.
Capturing and Deleting Loops
Up to six loops of each kind can be stored for reference.
To capture the current Loop and display it in the Loops window,
• select the Capture Loop pop-up key.
The monitor will prompt you to save the loop for reference, either in addition to or in place of
previously stored loops.
Status messages at the bottom of the window provide information on the loop capture process.
To delete Loops from the reference list,
• Select the Select Loop pop-up key to view the list of stored loops and delete the loops from the
list.
Showing/Hiding Loops
Colored rectangles beside the loops timestamps and color-coded with the loops tell you whether each
loop is currently displayed or not:
– A filled-in rectangle marks loops currently shown in the Loops window
– A rectangle outline marks loops not currently shown.
Selecting the timestamp of the currently-displayed loop hides it and shows the next in the list; selecting
the timestamp of a currently hidden loop displays it.
Changing Loops Display Size
To change the loops display size, in the Loops window, select the pop-up key Select Size then select
•Size X0.5 to display loops at half the usual size
•Size X1 to display loops at the usual size
•Size X2 to display loops at twice the usual size
This does not affect the size of loops printed in reports.
Using the Loops Cursor
To view the coordinates for any point on a stored loop,
1Select the pop-up key Select Loop.
2Select the required loop from the list of available loops.
3Use the arrow pop-up keys to move the cursor around the loop. The values for both loop axes are
shown for every point on the loop.
Select the X at the top of the loop list to exit the cursor.

31 Respiratory Loops
357
Changing Loops Type
To change the loop type, in the Loops window, select the Loop Type pop-up key (only available if the
source device delivers three waves), then select
•Press/Volume to display Pressure/Volume loops
•Flow/Volume to display Volume/Flow loops
•Press/Flow to display Pressure/Flow loops.
or, if the source device only delivers two waves,
1In the Loops window, select the Setup Device pop-up key to enter the setup window for the
external device.
2Select Wave 1 and select pressure, flow, or volume waves as required. Repeat for Wave 2.
Setting Up Source Device
The source device for the loops is indicated in the Loops window title.
• Select the Setup Device pop-up key to view the settings of the current source device.
If the source device is changed, all reference loops from a previous device are cleared from the
reference list when the first loop from the new source device is captured. Reconnecting the previous
device recalls its reference list.
Documenting Loops
1In the Loops window, select the pop-up key Print Loop
2From the list of available loops, select an individual loop, or select Print All to print a report of all
For each loop, the report prints
• the currently-displayed loop, with the loop capture timestamp
• up to six realtime numerics provided by the loop source device
•SpO
2, etCO2, PO2, and PCO2 numerics from the patient monitor, if available.

31 Respiratory Loops
358

32
359
32Laboratory Data
Laboratory data can be entered manually at the Information Center or at the monitor. For details on
manual entry at the monitor, see “Entering Measurements Manually” on page 42. Selected laboratory
data can be integrated on the monitor - values are then stored in the database and included in trends
and reports and can be displayed as a numeric on the main screen. Which data can be stored and used
on the monitor in this way is selected in Configuration Mode.
Viewing Received Data
When new data has been received from the Information Center a New Lab Data received. Check Lab
Results Window. message will appear with the arrival time. To view the data, select Main Setup then
select Lab Results or the Lab Results SmartKey.
The Lab Results window shows the most recent set of data received. The data is grouped into
categories:
•Blood Gases
•Electrolytes
•Hematology
•Metabolites
•Chemistry
•Enzymes/Markers
•Coagulation
•Urine Diagnostics
If no results are available for a particular category, that category will not be shown. Values which were
entered manually at the Information Center will be marked with an asterisk (*).

32 Laboratory Data
360
33
361
33Care and Cleaning
Use only the Philips-approved substances and methods listed in this chapter to clean or disinfect your
equipment. Warranty does not cover damage caused by using unapproved substances or methods.
Philips makes no claims regarding the efficacy of the listed chemicals or methods as a means for
controlling infection. Consult your hospital's Infection Control Officer or Epidemiologist. For
comprehensive details on cleaning agents and their efficacy refer to "Guidelines for Prevention of
Transmission of Human Immunodeficiency Virus and Hepatitis B Virus to Health Care and Public-
Safety Workers" issued by the U.S. Department of Health and Human Services, Public Health Service,
Centers for Disease Control, Atlanta, Georgia, February 1989. See also any local policies that apply
within your hospital, and country.
General Points
Keep your monitor, modules, Multi-Measurement Module, MMS extensions, Flexible Module Rack,
cables and accessories free of dust and dirt.
After cleaning and disinfection, check the equipment carefully. Do not use if you see signs of
deterioration or damage. If you need to return any equipment to Philips, decontaminate it first.
Observe the following general precautions:
• Always dilute according to the manufacturer's instructions or use lowest possible concentration.
• Do not allow liquid to enter the case.
• Do not immerse any part of the equipment or any accessories in liquid.
• Do not pour liquid onto the system.
• Never use abrasive material (such as steel wool or silver polish).
• Never use bleach.
WARNING
If you spill liquid on the equipment, battery, or accessories, or they are accidentally immersed in liquid,
contact your service personnel or Philips service engineer. Do not operate the equipment before it has
been tested and approved for further use.
The general care and cleaning information given here meets the requirements of Aspect Medical
Systems for their BIS measurement devices.
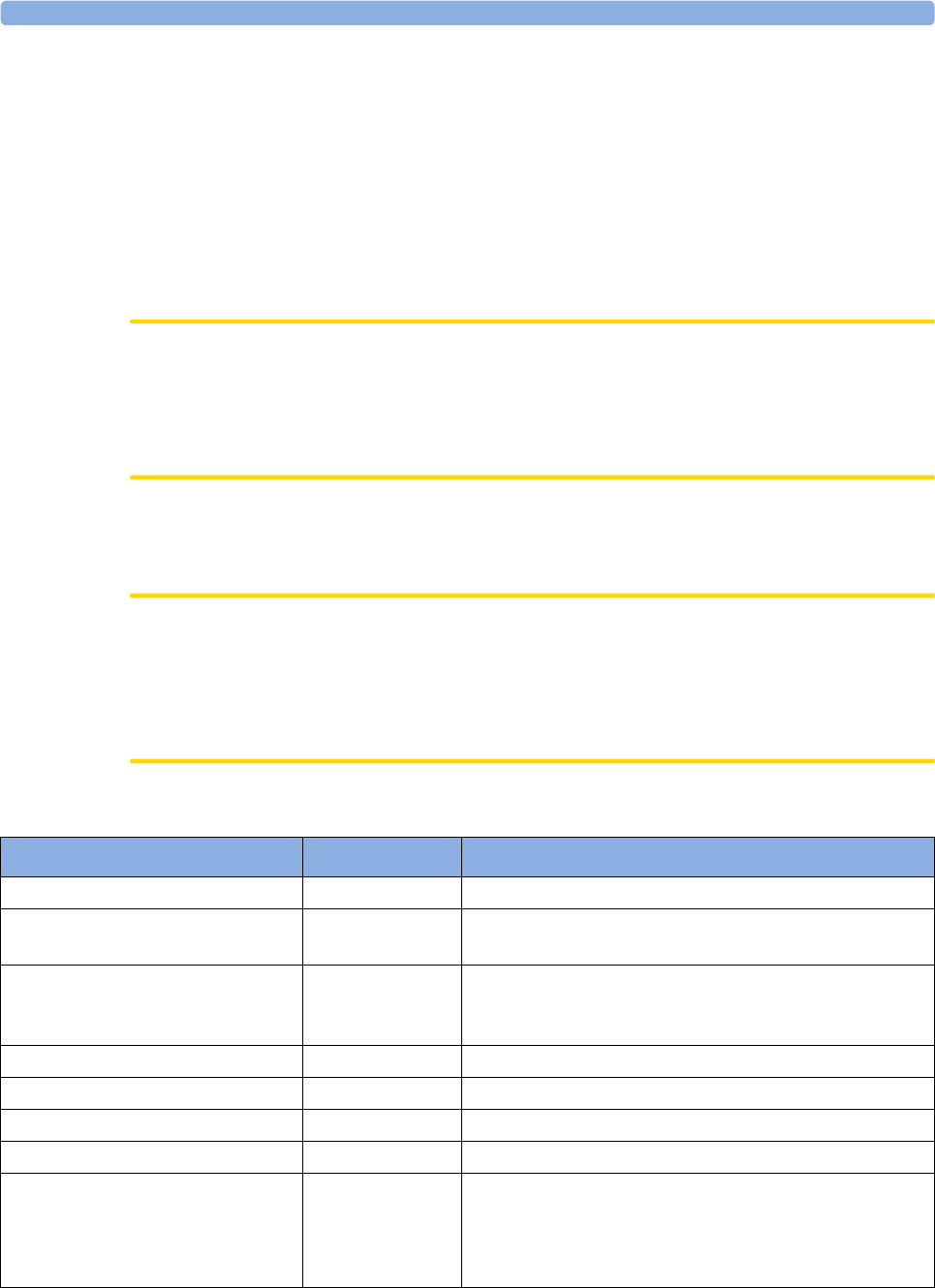
33 Care and Cleaning
362
Cleaning the Monitor
Clean with a lint-free cloth, moistened with warm water (40°C/104°F maximum) and soap, a diluted
non-caustic detergent, tenside, ammonia- or alcohol-based cleaning agent. Do not use strong solvents
such as acetone or trichloroethylene.
Take extra care when cleaning the screen of the monitor because it is more sensitive to rough cleaning
methods than the housing. Do not permit any liquid to enter the monitor case and avoid pouring it on
the monitor while cleaning. Do not allow water or cleaning solution to enter the measurement
connectors. Wipe around, not over, connector sockets.
CAUTION
To clean the touch-enabled display, disable the touch operation by switching off the monitor during
the cleaning procedure, or by selecting and holding the Main Screen key until the padlock symbol
appears on it, indicating that touch operation is disabled. Select and hold again to re-enable touch
operation.Unplug a mouse, keyboard or other connected device before cleaning it.
Disinfecting the Monitor
CAUTION
Solutions: Do not mix disinfecting solutions (such as bleach and ammonia) as hazardous gases may
result.
Hospital policy: Disinfect the product as determined by your hospital's policy, to avoid long term
damage to the product.
Clean equipment before disinfecting. Recommended types of disinfecting agents are:
Product Name Product Type Ingredients
Isopropanol liquid Isopropanol 80%
Bacillol® AF liquid, spray 100 g concentrate contains:
Propan-1-ol 45.0 g; Propan-2-ol 25.0 g; Ethanol 4.7 g
Bacillol®25 liquid Ethanol 100 mg/g
Propan-2-ol (= 2-Propanol) 90 mg/g; Propan-1-ol (= 1-
Propanol) 60 mg/g
Meliseptol®spray 50% 1-Propanol
Accel TB RTU liquid 0.5% accelerated hydrogen peroxide
Oxivir® Tb Cleaner Disinfectant spray 0.5% accelerated hydrogen peroxide
Oxivir® Tb Wipes wipes 0.5% accelerated hydrogen peroxide
Carpe DiemTM/MC Tb
Ready-to-Use General Virucide,
Bactericide, Tuberculocide,
Fungicide, Sanitizer
spray 0.5% accelerated hydrogen peroxide
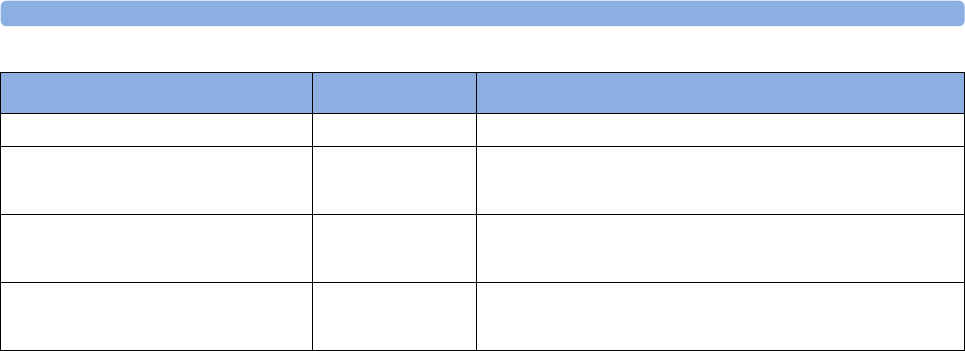
33 Care and Cleaning
363
Sterilizing the Monitor
Sterilization is not recommended for this monitor, related products, accessories or supplies unless
otherwise indicated in the Instructions for Use that accompany the accessories and supplies.
Cleaning, Sterilizing and Disinfecting Monitoring
Accessories
To clean, disinfect and sterilize reusable transducers, sensors, cables, leads, and so forth, refer to the
instructions delivered with the accessory.
Cleaning the SO2 Optical Module
The outside of the optical module can be cleaned as described under “Cleaning the Monitor” on
page 362. The compartment with the fiber-optic connection can only be cleaned with a dry cloth. Do
not introduce any moisture into this compartment.
Cleaning the Recorder Printhead (M1116B only)
If you run recordings at low speed (1 or 2cm/min) for extended periods, deposits of paper debris may
collect on the print head making recordings unevenly fainter in horizontal stripes.
1Remove the recorder.
2Open the recorder door and un-thread the paper from behind the rubber roller.
3Tear off or roll up the excess paper into the roll chamber to get it out of your way.
Carpe DiemTM/MC Tb Wipes wipes 0.5% accelerated hydrogen peroxide
Super Sani-Cloth
Germicidal Disposable Wipes
wipes isopropanol 55%
quaternary ammonium chlorides 0.5%
SANI-CLOTH® PLUS
Germicidal Disposable Wipes
wipes isopropanol 15%
quaternary ammonium chlorides 0.25%
SANI-CLOTH® HB Germicidal
Germicidal Disposable Wipes
wipes isopropanol < 0.15%
quaternary ammonium chlorides 0.14%
Product Name Product Type Ingredients
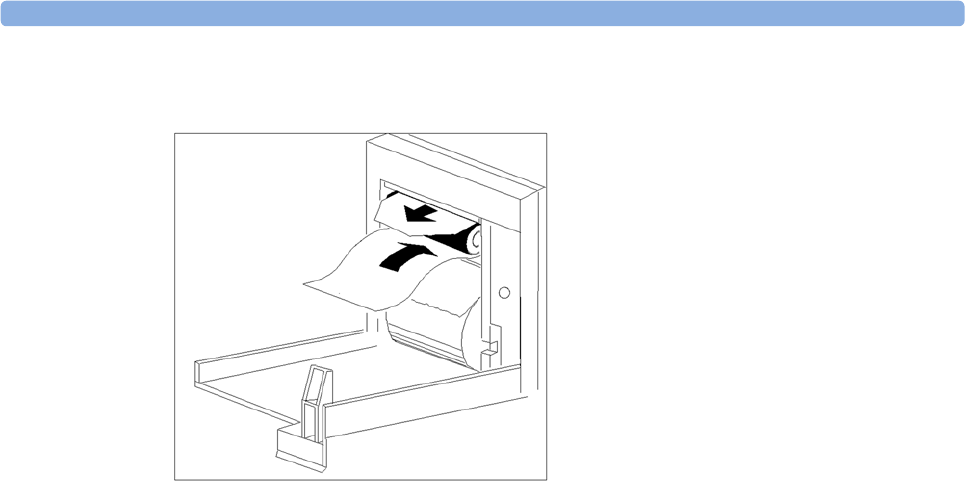
33 Care and Cleaning
364
4Thread the cloth cleaning strip instead of paper around the rubber roller until approximately two
inches of the strip come out from the top of the roller.
5Close the recorder door, aligning both ends of the strip over the top of the door.
6Holding the top end of the cleaning strip between your thumb and forefinger, pull the strip
through and out of the recorder.
7Open the door and ensure that the paper cavity is dust-free. Re-thread the paper and replace the
recorder.
34
365
34Maintenance and
Troubleshooting
WARNING
Schedule: Failure on the part of the responsible individual hospital or institution employing the use of
this equipment to implement a satisfactory maintenance schedule may cause undue equipment failure
and possible health hazards.
Contact: If you discover a problem with any of the equipment, contact your service personnel, Philips,
or your authorized supplier.
Inspecting the Equipment and Accessories
You should perform a visual inspection before every use, and in accordance with your hospital's policy.
With the monitor switched off:
1Examine unit exteriors for cleanliness and general physical condition. Make sure that the housings
are not cracked or broken, that everything is present, that there are no spilled liquids and that there
are no signs of abuse.
2Inspect all accessories (cables, transducers, sensors and so forth). If any show signs of damage, do
not use.
3Switch the monitor on and make sure the backlight is bright enough. Check that screen is at its full
brightness. If the brightness is not adequate, contact your service personnel or your supplier.
4If the MMS and MMS Extensions are mounted on the monitor, make sure that they are locked
into place and do not slide out without releasing the locking mechanism.
WARNING
Electrical Shock Hazard: Do not open the monitor or measurement device. Contact with exposed
electrical components may cause electrical shock. Always turn off and remove power before cleaning
the sensor, monitor or measurement device. Do not use a damaged sensor or one with exposed
electrical contacts. Refer servicing to qualified service personnel.
34 Maintenance and Troubleshooting
366
Inspecting the Cables and Cords
1Examine all system cables, the power plug and cord for damage. Make sure that the prongs of the
plug do not move in the casing. If damaged, replace it with an appropriate Philips power cord.
2Inspect the Measurement Link cable and ensure that it makes good connection with the MMS and
the FMS. Make sure that there are no breaks in the insulation.
3Inspect the cable connecting the MMS to the monitor. Make sure the connectors are properly
engaged.
4Inspect the patient cables, leads and their strain reliefs for general condition. Make sure there are
no breaks in the insulation. Make sure that the connectors are properly engaged at each end to
prevent rotation or other strain.
5Apply the transducer or electrodes to the patient, and with the monitor switched on, flex the
patient cables near each end to make sure that there are no intermittent faults.
Maintenance Task and Test Schedule
The following tasks are for Philips-qualified service professionals only. All maintenance tasks and
performance tests are documented in detail in the service documentation supplied on the monitor
documentation DVD.
Ensure that these tasks are carried out as indicated by the monitor's maintenance schedule, or as
specified by local laws. Contact a Philips-qualified service provider if your monitor needs a safety or
performance test. Clean and disinfect equipment to decontaminate it before testing or maintaining it.
Maintenance and Test Schedule Frequency
Monitor Tests
Safety checks. Selected tests on the
basis of IEC 60601-1
At least once every two years, or as needed, after any repairs
where the power supply is removed or replaced, or if the
monitor has been dropped.
Monitor Maintenance
Check ECG synchronization of the
monitor and defibrillator (only if
hospital protocol requires use of
monitor during defibrillation)
At least once every two years, or as needed.
Replace backlight
(integrated displays only)
25,000 - 30,000 hours (about three years) of continuous
usage, or as needed.
Multi-measurement Module and Module Tests
Performance assurance for all
measurements not listed below.
At least once every two years, or if you suspect the
measurement values are incorrect.
Multi-measurement Module and Module Maintenance
NBP calibration At least once every two years, or as specified by local laws.
Microstream CO2 calibration and
performance test
At least once a year or after 4000 operating hours.
Mainstream and sidestream CO2
calibration check (M3014A)
At least once a year, or if you suspect the measurement
values are incorrect.
34 Maintenance and Troubleshooting
367
Troubleshooting
If you suspect a problem with an individual measurement, read the Instructions for Use and double-
check that you have set up the measurement correctly.
If you suspect an intermittent, system-wide problem call your service personnel. You may be asked for
information from the status log. To view the status log,
1In the Main Setup menu, select Revisions.
2Select the pop-up key corresponding to the status log you want to consult, for example, for the
MMS or the monitor.
3View the status log by selecting Status Log from the Monitor Revision window.
Disposing of the Monitor
WARNING
To avoid contaminating or infecting personnel, the environment or other equipment, make sure you
disinfect and decontaminate the monitor appropriately before disposing of it in accordance with your
country's laws for equipment containing electrical and electronic parts. For disposal of parts and
accessories such as thermometers, where not otherwise specified, follow local regulations regarding
disposal of hospital waste.
You can disassemble the monitor, MMS, FMS and modules as described in the Service Guide.
You will find detailed disposal information on the following web page:
http://www.healthcare.philips.com/main/about/Sustainability/Recycling/pm.wpd
The Recycling Passports located there contain information on the material content of the equipment,
including potentially dangerous materials which must be removed before recycling (for example,
batteries and parts containing mercury or magnesium).
Do not dispose of waste electrical and electronic equipment as unsorted municipal waste. Collect it
separately, so that it can be safely and properly reused, treated, recycled, or recovered.
Disposing of Empty Calibration Gas Cylinders
1Empty the cylinder completely by pushing in the pin of the regulator valve or by pulling out the
pin of the fill valve using a tire valve stem wrench or a pair of needle nose pliers.
2When the cylinder is empty, either remove the valve stem from the fill (or regulator) hole, or drill a
hole in the cylinder.
3Write "Empty" on the cylinder and dispose of it appropriately for scrap metal.
34 Maintenance and Troubleshooting
368
WARNING
Ensure that the cylinder is completely empty before trying to remove the valve stem or drill a hole in
the cylinder.
35
369
35Accessories
You can order parts and accessories from Philips supplies at www.medical.philips.com or consult your
local Philips representative for details.
WARNING
Reuse: Never reuse disposable transducers, sensors, accessories and so forth that are intended for
single use, or single patient use only. Reuse may compromise device functionality and system
performance and cause a potential hazard.
Philips' approval: Use only Philips-approved accessories. Using non-Philips-approved accessories
may compromise device functionality and system performance and cause a potential hazard.
Packaging: Do not use a sterilized accessory if its packaging is damaged.
ECG/Resp Accessories
This symbol indicates that the cables and accessories are designed to have special protection
against electric shocks (particularly regarding allowable leakage currents), and are defibrillator proof.
The following cables may not all be available in all countries. Please check availability with your local
Philips supplier.
Recommended Cables
Trunk Cables
3-Electrode Cable
Set
5-Electrode Cable
Set
6-Electrode Cable
Set
10-Electrode
Cable set
(5+5)
10-Electrode
Cable set
(6+4)
Part No. M1669A M1668A M1667A M1663A M1665A
Length 2.7 m 2.7 m 2.7 m 2.0 m 2.7 m
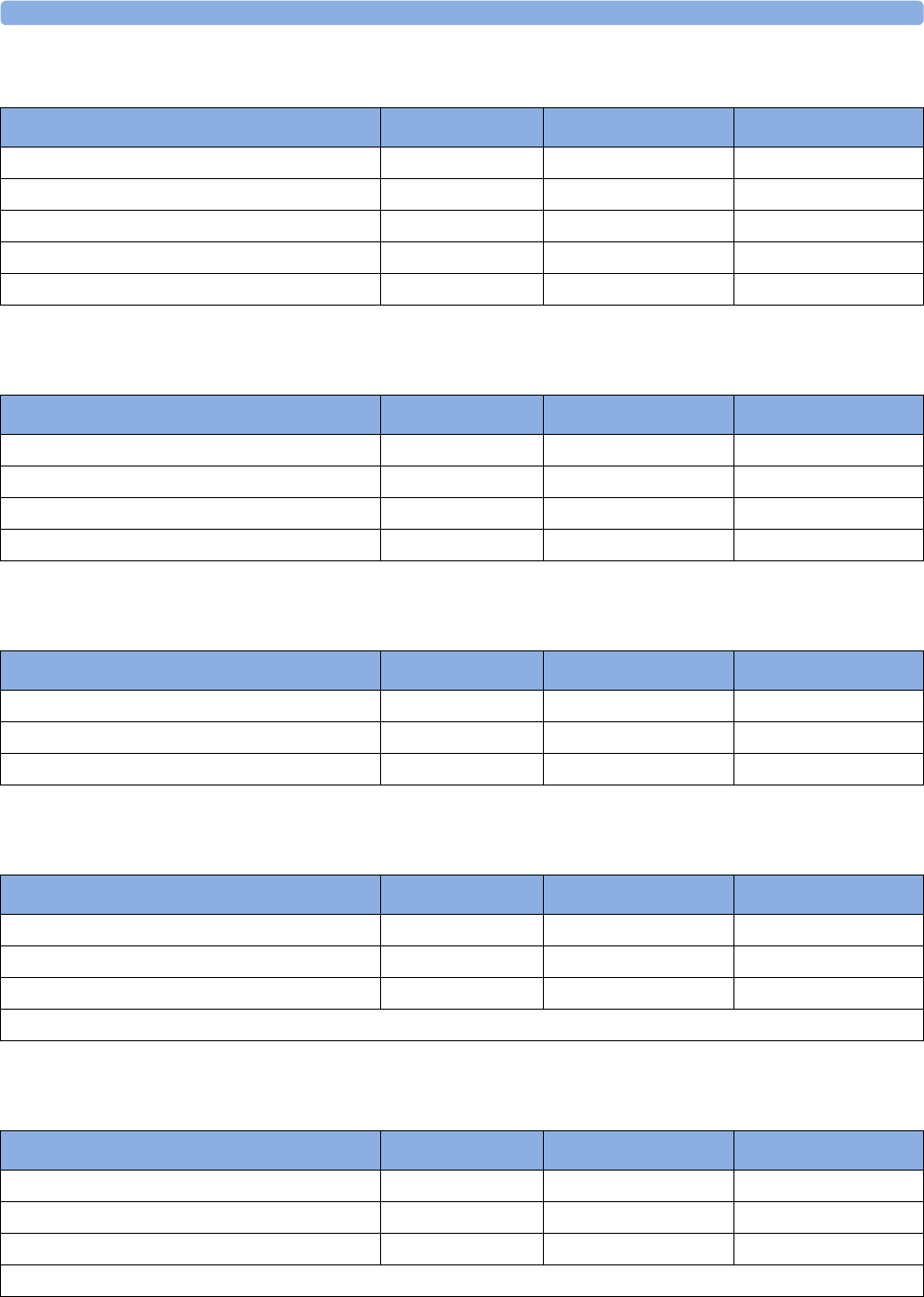
35 Accessories
370
3-Electrode Cable Sets
5-Electrode Cable Sets
6-Electrode Cable Sets
10-Electrode (5+5)Cable Sets
10-Electrode (6+4)Cable Sets
Description Length AAMI Part No. IEC Part No.
OR Grabber shielded 1.0 m M1675A M1678A
ICU Grabber shielded 1.0 m M1671A M1672A
ICU snap shielded 1.0 m M1673A M1674A
ICU Clip non-shielded 0.45 m M1622A --
ICU Clip non-shielded 0.7 m M1624A M1626A
Description Length AAMI Part No. IEC Part No.
OR Grabber shielded 1.0 m/1.6 m M1973A M1974A
ICU Grabber shielded 1.0 m/1.6 m M1968A M1971A
ICU Snap shielded 1.0 m/1.6 m M1644A M1645A
ICU Miniclip non-shielded 0.7 m/1.3 m M1647A M1648A
Description Length AAMI Part No. IEC Part No.
OR Grabber 1.0 m/1.6 m M1684A M1685A
ICU Grabber 1.0 m/1.6 m M1680A M1681A
ICU Snap 1.0 m/1.6 m M1682A M1683A
Description Length AAMI Part No. IEC Part No.
ICU Grabber, chest, shielded 1.0 m M1976A M1978A
ICU Snap, chest, shielded 1.0 m M1602A M1604A
OR Grabber, chest, shielded 1.0 m M1979A M1984A
For Limb Leads see 5-electrode cable sets
Description Length AAMI Part No. IEC Part No.
ICU Grabber, chest, shielded 1.0 m M1532A M1533A
ICU Snap, chest, shielded 1.0 m M1537A M1538A
OR Grabber, chest, shielded 1.0 m M1557A M1558A
For Limb Leads see 6-electrode cable sets
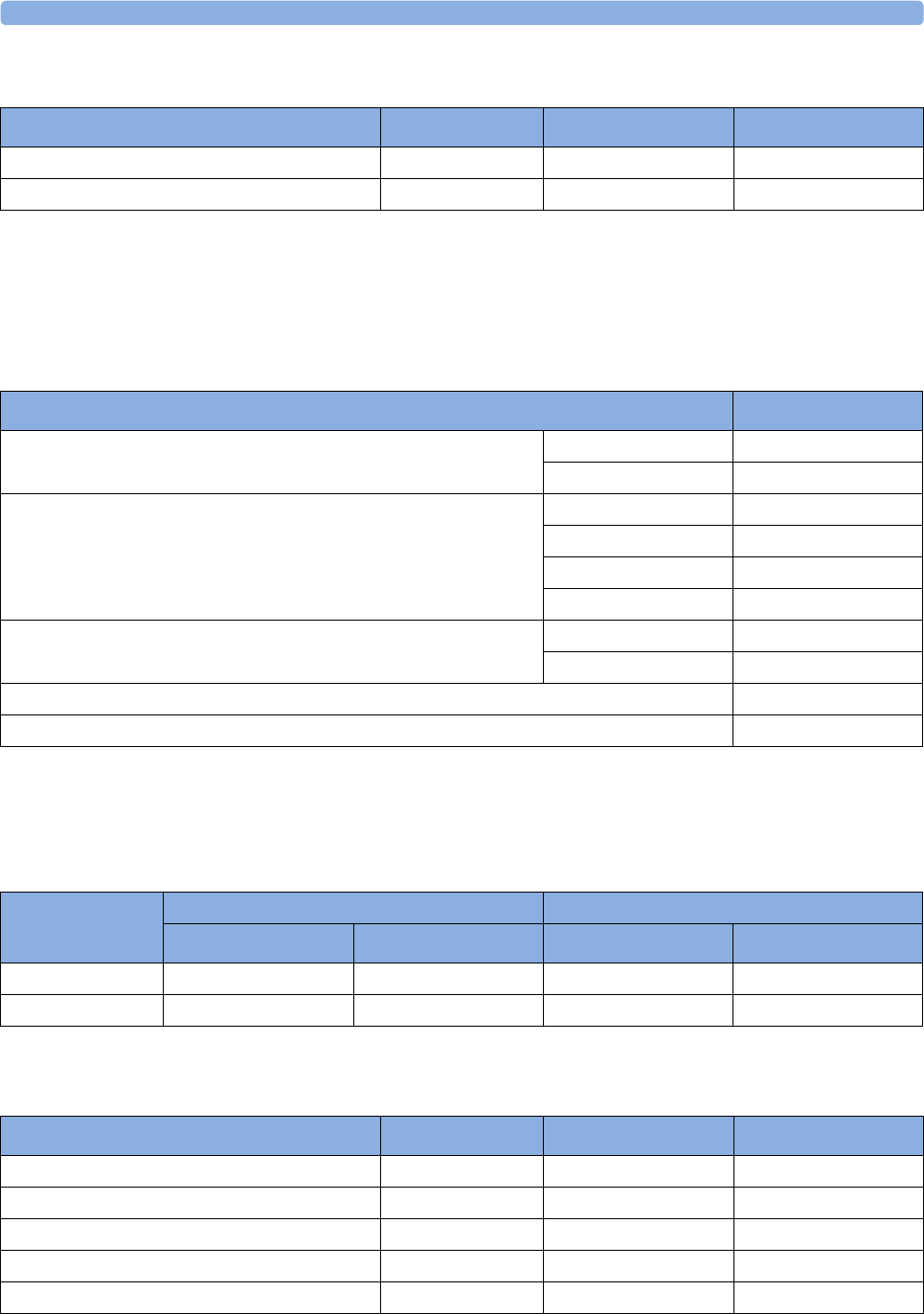
35 Accessories
371
One-piece Cables
Radio-translucent Cables
Pack of five single wires, radio-translucent, 0.9 m, M1649A
Set Combiners and Organizers
Supported Cables
Trunk Cables
3-Electrode Cable Sets
Description Length AAMI Part No. IEC Part No.
3-lead Grabber, ICU 1.0 m 989803143181 989803143171
5-lead Grabber, ICU 1.0 m 989803143201 989803143191
Set combiners and organizers Part No.
Set combiner 3-electrode M1501A
5-electrode M1502A
Set organizer for shielded leadsets - grabber and snap 3-electrode M1503A
4-electrode M1664A
5-electrode M1504A
6-electrode M1679A
Set organizer for non-shielded lead sets - miniclip 3-electrode M1636A
5-electrode M1638A
Bedsheet clip M1509A
Replacement red cover for trunk cable (for 5-electrode cable sets) 989808148861
Length 3-Electrode Cable Set 5-Electrode Cable Set
AAMI Part No. IEC Part No. AAMI Part No. IEC Part No.
0.9 m M1540C M1550C M1560C M1570C
2.7 m M1500A M1510A M1520A M1530A
Description Length AAMI Part No. IEC Part No.
OR 1.0 m M1601A M1611A
ICU Grabber shielded 1.0 m M1603A M1613A
ICU snap shielded 1.0 m M1605A M1615A
ICU Clip non-shielded 0.45 m M1608A M1618A
ICU Clip non-shielded 0.7 m M1609A M1619A
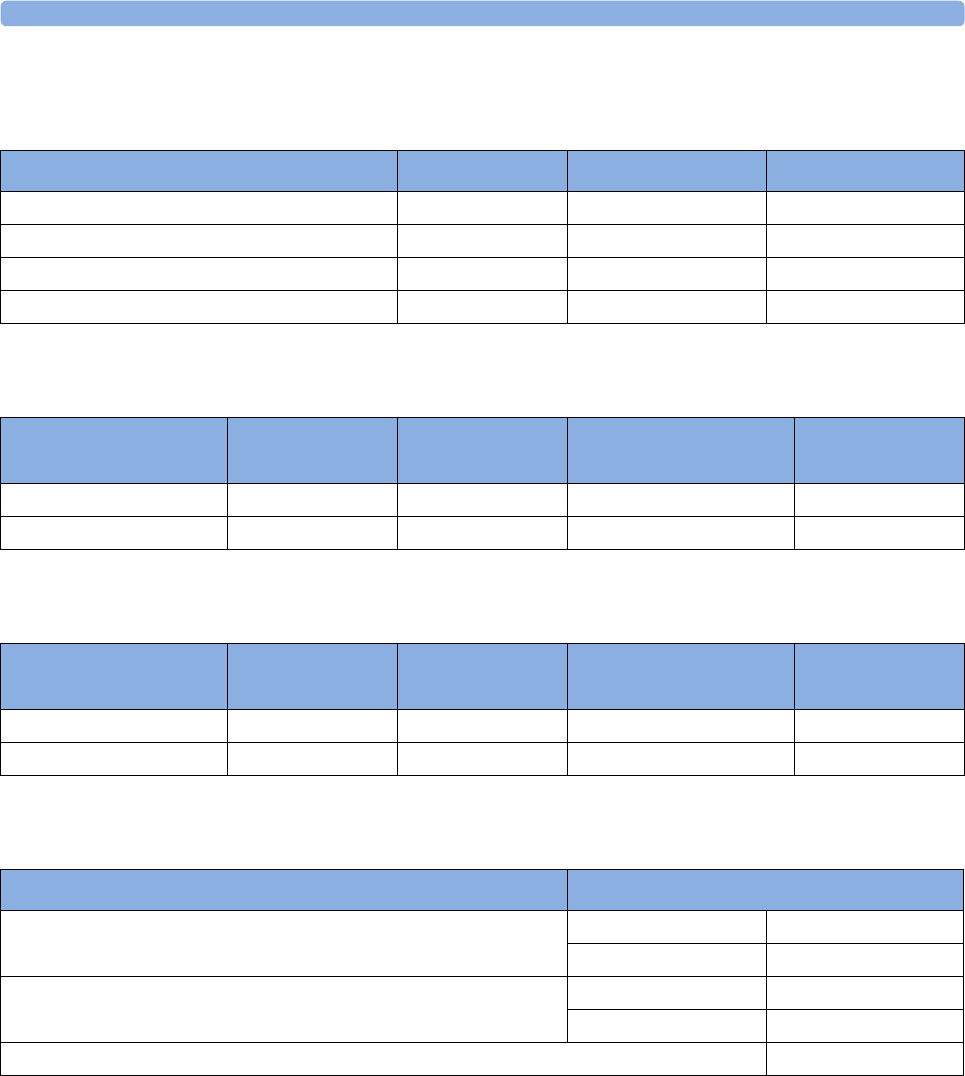
35 Accessories
372
5-Electrode Cable Sets
3-Electrode One Piece Cables
5-Electrode One Piece Cables
Set Combiners and Organizers
Description Length AAMI Part No. IEC Part No.
OR Grabber shielded 1.0 m/1.6 m M1621A M1631A
ICU Grabber shielded 1.0 m/1.6 m M1623A M1633A
ICU Snap shielded 1.0 m/1.6 m M1625A M1635A
ICU Clip non-shielded 0.7 m/1.3 m M1629A M1639A
AAMI 3-Electrode One
Piece Cables
Length AAMI Part No. IEC 3-electrode One
Piece Cables
IEC Part No.
OR Grabber 1.9 m M1970A OR Grabber M1980A
ICU Snap 1.9 m M1972A ICU Grabber M1981A
AAMI 5-electrode One
Piece Cables
Length AAMI Part No. IEC 5-electrode One
Piece Cables
IEC Part No.
OR Grabber 2.5 m M1975A OR Grabber M1985A
ICU Snap 2.5 m M1977A ICU Grabber M1986A
Set combiners and organizers Part No.
Set combiner 3-electrode M1501A
5-electrode M1502A
Set organizer Shielded 3-electrode M1503A
Shielded 5-electrode M1504A
Bedsheet clip M1509A
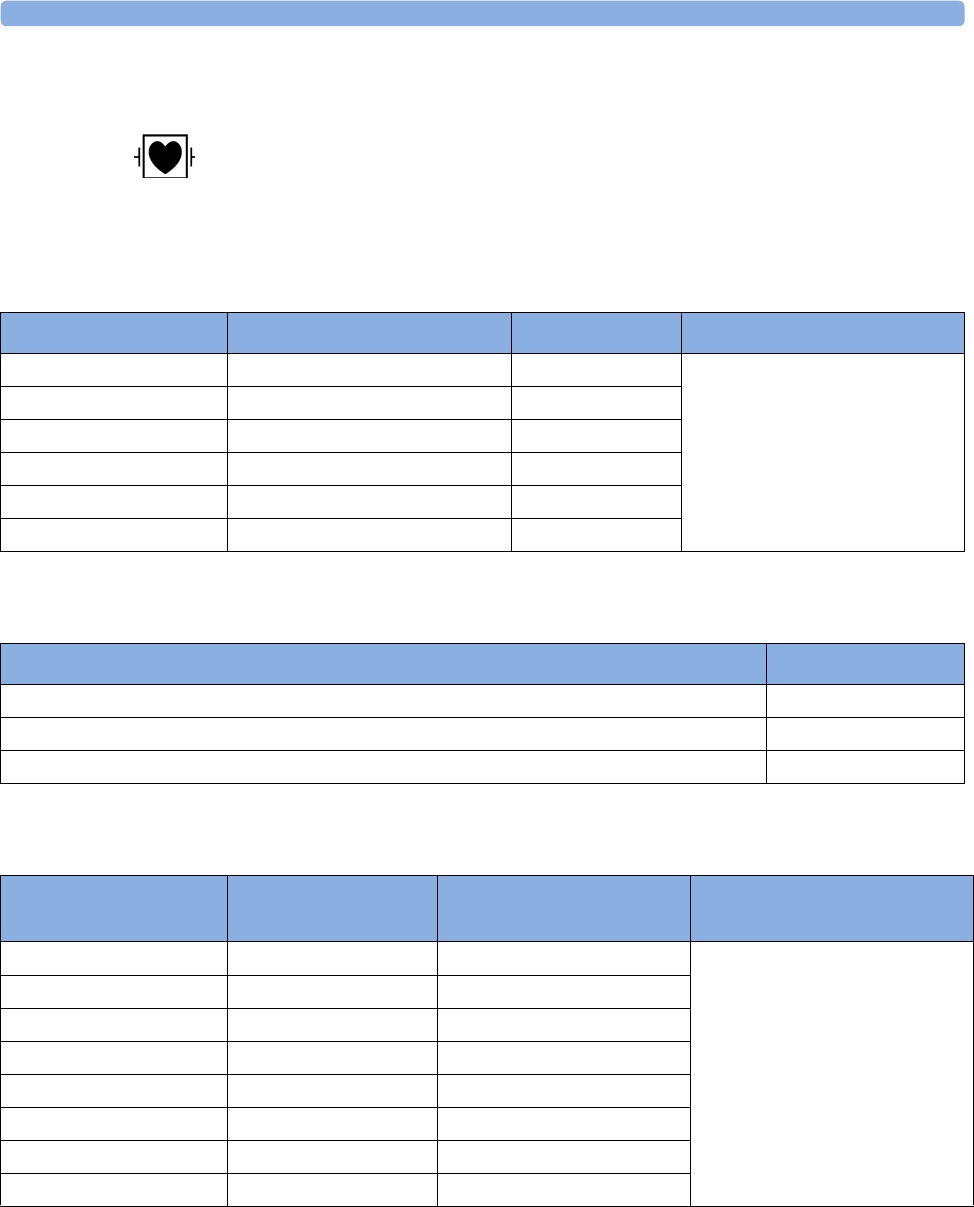
35 Accessories
373
NBP Accessories
These cuffs and tubings are designed to have special protection against electric shocks
(particularly regarding allowable leakage currents), and are defibrillator proof. You can use them during
electrosurgery.
Adult/Pediatric Reusable Comfort Cuffs
Adult/Pediatric Reusable Comfort Cuff Kits
Adult/Pediatric Reusable EasyCare Cuffs
Patient Category Limb Circumference Part No. Tubing
Adult (Thigh) 42 to 54 cm M1576A M1598B (1.5 m)
or
M1599B (3 m)
Large Adult 34 to 43 cm M1575A
Adult 27 to 35 cm M1574A
Small Adult 20.5 to 28 cm M1573A
Pediatric 14 to 21.5 cm M1572A
Infant 10 to 15 cm M1571A
Cuff Kits Part No.
Infant, pediatric, small adult, adult M1577A
Small adult, adult, large adult, thigh M1578A
Infant, pediatric, small adult, adult, large adult, thigh M1579A
Patient Category Limb Circumference Part No.
(Pack of five)
Tubing
Adult Thigh 44 - 56 cm M4559B (M4559B5) M1598B (1.5 m)
or
M1599B (3 m)
Large Adult X-Long 35 - 45 cm M4558B (M4558B5)
Large Adult 35 - 45 cm M4557B (M4557B5)
Adult X-Long 27.5 - 36 cm M4556B (M4556B5)
Adult 27.5 - 36 cm M4555B (M4555B5)
Small Adult 20.5 - 28.5 cm M4554B (M4554B5)
Pediatric 14 - 21.5 cm M4553B (M4553B5)
Infant 10 - 15 cm M4552B (M4552B5)
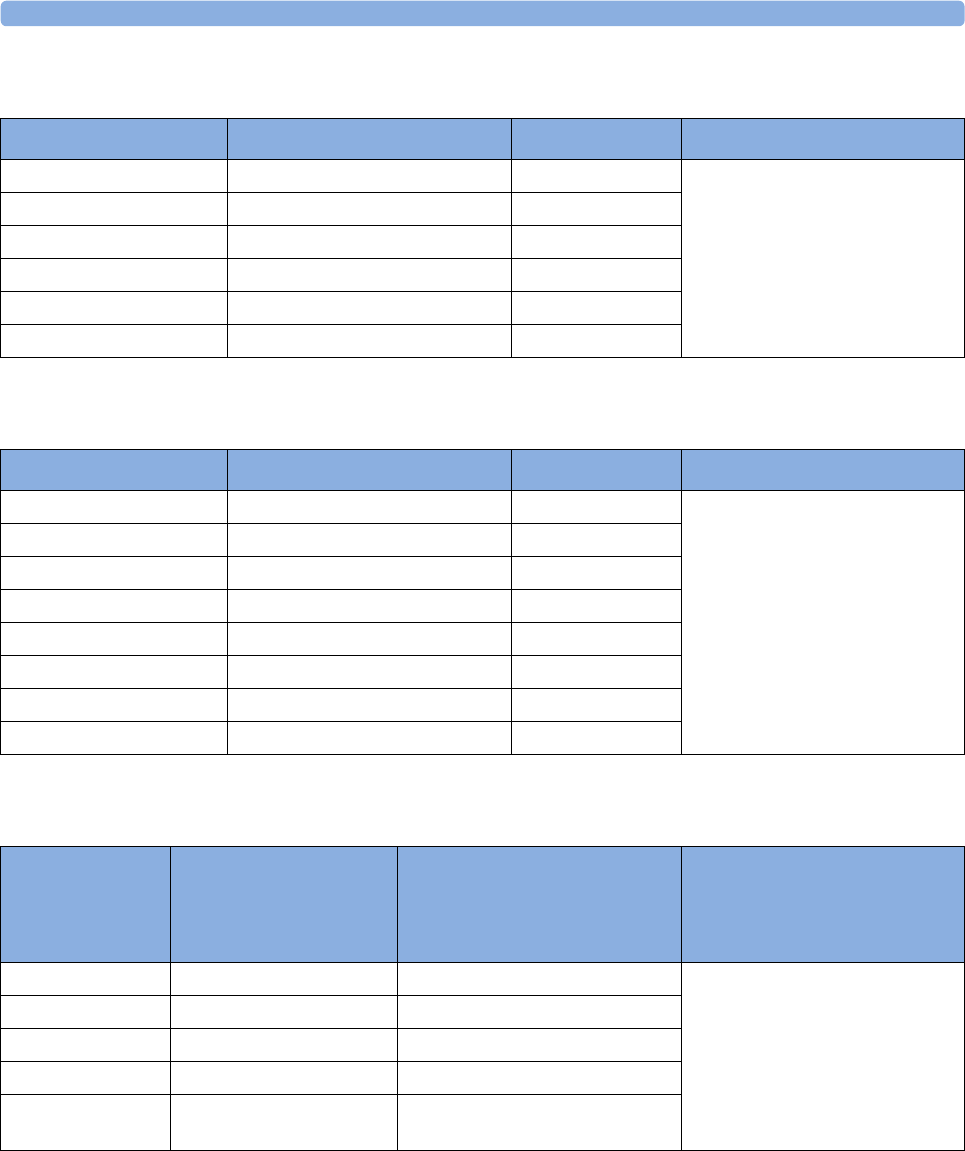
35 Accessories
374
Adult/Pediatric Single Patient Cuffs
Adult/Pediatric Single Patient, Soft Cuffs
Neonatal/Infant Single Patient Cuffs
Patient Category Limb Circumference Part No. Tubing
Adult (Thigh) 42 to 54 cm M1879A M1598B (1.5 m)
or
M1599B (3 m)
Large Adult 34 to 43 cm M1878A
Adult 27 to 35 cm M1877A
Small Adult 20.5 to 28 cm M1876A
Pediatric 14 to 21.5 cm M1875A
Infant 10 to 15 cm M1874A
Patient Category Limb Circumference Part No. Tubing
Adult (Thigh) 44 - 56 cm M4579B M1598B (1.5 m)
or
M1599B (3 m)
Large Adult X-Long 35 - 45 cm M4578B
Large Adult 35 - 45 cm M4577B
Adult X-Long 27.5 - 36 cm M4576B
Adult 27.5 - 36 cm M4575B
Small Adult 20.5 - 28.5 cm M4574B
Pediatric 14.0 - 21.5 cm M4573B
Infant 10 - 15 cm M4572B
Cuffs Limb Circumference Part No.
A - Luer connector
B - ISO 80369-1 compliant
connector
Tubing
Size 1 3.1 to 5.7 cm M1866A/B For A-version cuffs:
M1596B (1.5 m) or M1597B
(3 m)
For B-version cuffs:
M1596C (1.5 m) or M1597C
(3 m)
Size 2 4.3 to 8.0 cm M1868A/B
Size 3 5.8 to 10.9 cm M1870A/B
Size 4 7.1 to 13.1 cm M1872A/B
Size 5 (Infant) 10 to 15 cm M1873B
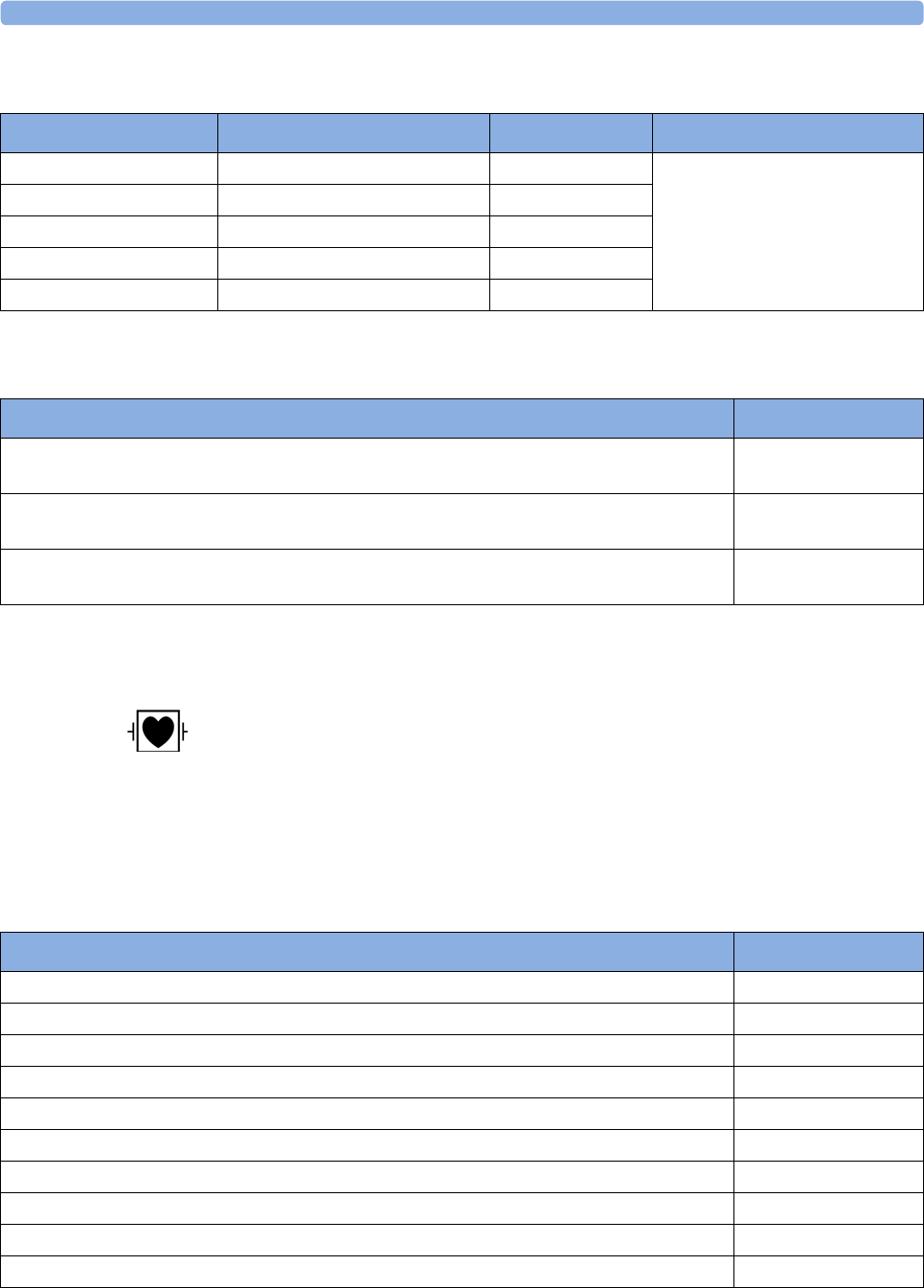
35 Accessories
375
Neonatal/Infant Single Patient, Soft Cuffs
Neonatal/Infant Cuff Kits
Invasive Pressure Accessories
These transducers and accessories are designed to have special protection against electric
shocks (particularly regarding allowable leakage currents), and are defibrillator proof.
If you are using the M3012A Hemodynamic MMS Extension, and you want to measure temperature
and invasive pressure at the same time, we recommend that you use the pressure transducer CPJ840J6,
with a round module connector piece, and not a transducer with a square connector. Pressure
transducers with square connectors may make it difficult to connect the adjacent Temperature
connector at the same time.
Cuffs Limb Circumference Part No. Tubing
Size 1 3.1 to 5.7 cm M1866S M1596C (1.5 m)
or
M1597C (3 m)
Size 2 4.3 to 8.0 cm M1868S
Size 3 5.8 to 10.9 cm M1870S
Size 4 7.1 to 13.1 cm M1872S
Size 5 (Infant) 10 to 15 cm M1873S
Cuff Kits Part No.
Standard, Single Patient, Luer connector: 10 x M1866A, 10 x M1868A, 10 x M1872A,
and 20 x M1870A
M1820-60020
Standard, Single Patient, ISO 80369-1 compliant connector: 5 x M1866B, 10 x M1868B,
20 x M1870B, 10 x M1872B, and 5 x M1873B
989803167541
Soft, Single Patient, ISO 80369-1 compliant connector: 5 x M1866S, 10 x M1868S,
20 x M1870S, 10 x M1872S, 5 x M1873S
989803167551
Transducer, accessories, sensor kits Part No.
Reusable pressure transducer 5 µV/V/mmHg sensitivity CPJ840J6
Sterile disposable pressure domes for CPJ840J6 (pack of 50) CPJ84022
Transducer holder for CPJ840J6 (pack of 4) CPJ84046
IV pole mount for CPJ840J6 CPJ84447
Monitoring Line Set for CPJ840J6 CPJ84026
Single channel disposable sensor kit (20) - (EU/EFTA only) M1567A
Dual channel disposable sensor kit (20) (EU/EFTA only) M1568A
Transducer holder for M1567/8A (EU/EFTA only) M2271A
IV pole mount for M1567/8A (EU/EFTA only) M2272C
Adapter cable for disposable sensor kit 3,0m for M1567/8A M1634A
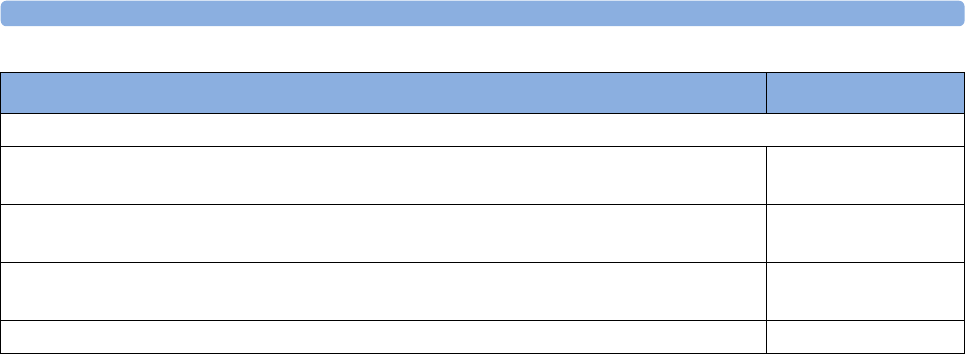
35 Accessories
376
SpO2 Accessories
This section lists accessories for use with Philips SpO2 technology. For accessory lists for other SpO2
technologies, refer to the instructions for use provided with these devices.
Some Nellcor sensors contain natural rubber latex which may cause allergic reactions. See the
Instructions for Use supplied with the sensors for more information. M1901B, M1902B, M1903B and
M1904B disposable sensors are not available in USA from Philips. Purchase Nellcor sensors and
adapter cables directly from Tyco Healthcare.
Do not use more than one extension cable with any sensors or adapter cables. Do not use an extension
cable with:
• Masimo adapter cables,
• Philips reusable sensors or adapter cables with part numbers ending in -L (indicates "Long"
version) or with a cable longer than 2 m.
All listed sensors operate without risk of exceeding 41°C on the skin, if the initial skin temperature
does not exceed 35°C.
Make sure that you use only the accessories that are specified for use with this device, otherwise patient
injury can result.
Always use the MAX-FAST forehead sensor with the foam headband provided by Nellcor.
Option A01 is the Philips FAST-SpO2 version; Option A02 is the Nellcor OxiMax-compatible
version.
The SpO2 Option A02 may not be available in all countries. Some sensors may not be available in all
countries.
Pressure transducer kits
PiCCO monitoring kit, 30cm pressure line, includes PV4046 injectate temperature sensor
housing for M1646A
PV8103
PiCCO monitoring kit, 150cm pressure line, includes PV4046 injectate temperature sensor
housing for M1646A
PV8115
PiCCO monitoring kit, 150cm pressure line, includes PV4046 injectate temperature sensor
housing for M1646A and central venous pressure line
PV8115CVP
PULSION Pressure Interface Cable for disposable pressure transducer PMK 206
Transducer, accessories, sensor kits Part No.
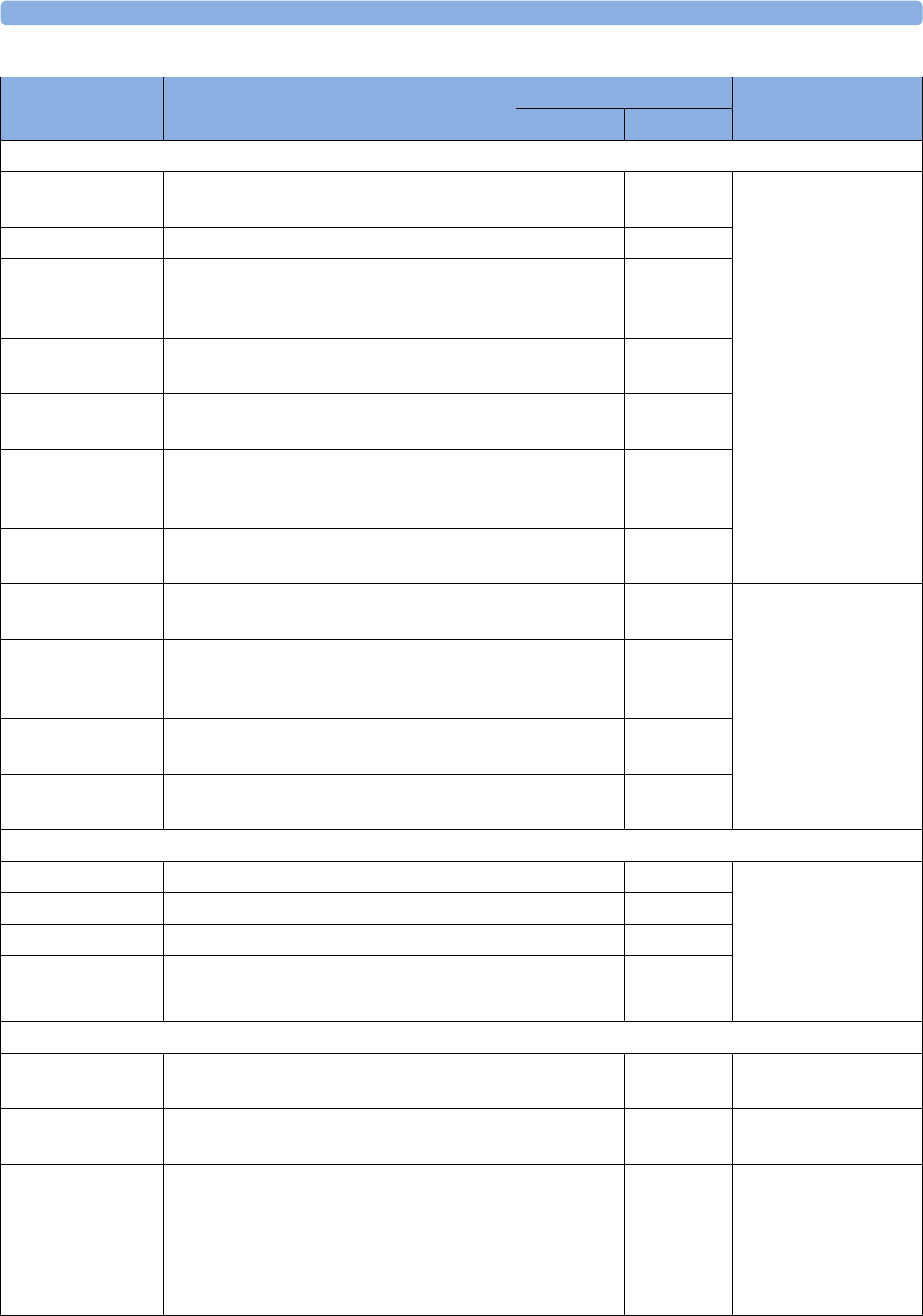
35 Accessories
377
Product Number Description Compatible with Comments
Opt. A01 Opt. A02
Philips reusable sensors.
M1191A/B Adult sensor (2 m cable), for patients over
50 kg. Any finger, except thumb.
yes no No adapter cable
required.
M1191AL/BL M1191A/B with longer cable (3 m) yes no
M1192A Small adult, pediatric sensor (1.5 m cable)
for patients between 15 kg and 50 kg. Any
finger except thumb.
yes no
M1193A Neonatal sensor (1.5 m cable) for patients
between 1kg and 4 kg. Hand or foot.
yes no
M1194A Ear sensor (1.5 m cable) for patients more
than 40 kg.
yes no
M1195A Infant sensor (1.5 m cable) for patients
between 4kg and 15 kg. Any finger except
thumb.
yes no
M1196A Adult clip sensor (3 m cable) for patients
over 40 kg. Any finger except thumb.
yes no
M1191T Adult sensor (0.45 m cable), for patients
over 50 kg. Any finger, except thumb.
yes no Requires M1943 (1 m)
or M1943AL (3 m)
adapter cable
M1192T Small adult, pediatric sensor (0.45 m cable)
for patients between 15 kg and 50 kg. Any
finger except thumb.
yes no
M1193T Neonatal sensor (0.9 m cable) for patients
between 1 kg and 4 kg. Hand or foot.
yes no
M1196T Adult clip sensor (0.9 m cable) for patients
over 40 kg. Any finger except thumb.
yes no
Philips disposable sensors. Not available in the USA.
M1904B Identical to OxiMax MAX-A yes yes Option A01: Use
adapter cable M1943A
or M1943AL.
Option A02: Must use
adapter cable
M1943NL.
M1903B Identical to OxiMax MAX-P yes yes
M1902B Identical to OxiMax MAX-I yes yes
M1901B Identical to OxiMax MAX-N yes yes
Philips disposable sensors. Available worldwide.
M1131A Adult/Pediatric finger sensor, 0.45 m cable
(patient size > 20 kg)
yes no Use adapter cable
M1943A or M1943AL.
M1132A Infant finger or toe sensor, 0.9 m cable
(patient size 3 - 10 kg)
yes no Use adapter cable
M1943A or M1943AL.
M1133A Adult/Infant/Neonatal, 0.9 m cable
Foot or hand for neonates < 3 kg
Big toe or thumb for patients between 10 kg
and 20 kg
Any finger except thumb for patients > 40
kg
yes no Use adapter cable
M1943A or M1943AL.
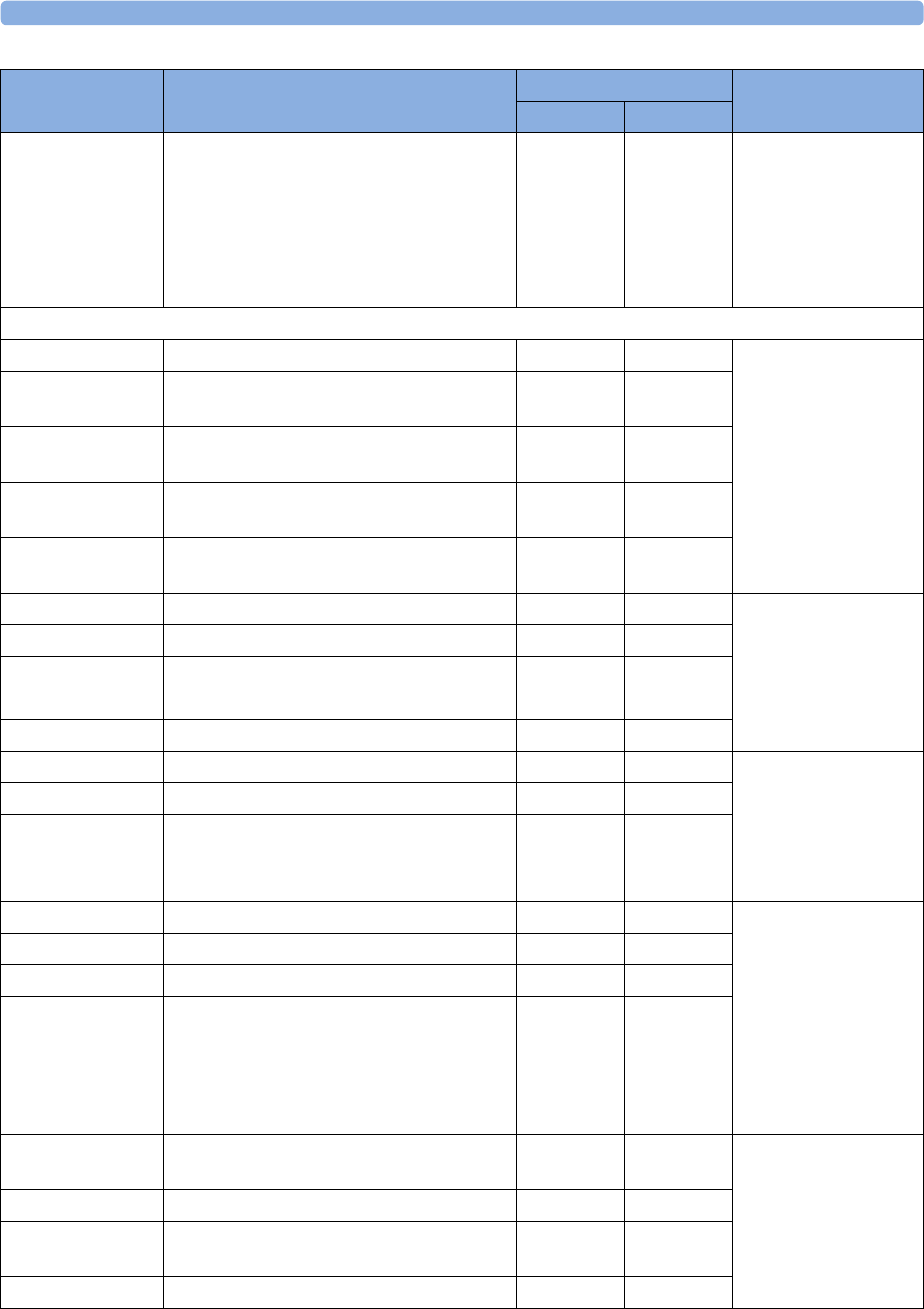
35 Accessories
378
M1134A Adhesive-free, Adult/Infant/Neonatal, 0.9
m cable
Foot or hand for neonates < 3 kg
Big toe or thumb for patients between 10 kg
and 20 kg
Any finger except thumb for patients > 40
kg
yes no Use adapter cable
M1943A or M1943AL.
NELLCOR disposable sensors (must be ordered from Nellcor)
OxiMax MAX-A Adult finger sensor (patient size > 30 kg) yes yes Option A01: Use
adapter cable M1943A
or M1943AL.
Option A02: Must use
adapter cable
M1943NL.
OxiMax
MAX-AL
OxiMax MAX-A with long cable yes yes
OxiMax MAX-P Pediatric foot/hand sensor (patient size 10-
50 kg)
yes yes
OxiMax MAX-I Infant foot/hand sensor (patient size 3-20
kg)
yes yes
OxiMax MAX-N Adult finger or neonatal foot/hand sensor
(patient size > 40 kg or < 3 kg)
yes yes
MAX-FAST Forehead sensor no yes Must use M1943NL
adapter cable.
OxiMax MAX-R Adult nasal sensor no yes
OxiMax SC-A Adult SoftCare sensor no yes
OxiMax SC-NEO Neonatal SoftCare sensor no yes
OxiMax SC-PR Pre-term infant SoftCare sensor no yes
Oxisensor II D-25 Adult sensor (patient size > 30 kg) yes no Must use M1943A or
M1943 AL adapter
cable.
Oxisensor II D-20 Pediatric sensor (patient size 10-50 kg) yes no
Oxisensor II I-20 Infant sensor (patient size 3-20 kg) yes no
Oxisensor II N-25 Neonatal sensor (patient size < 3 kg or > 40
kg)
yes no
OxiCliq A See OxiMax MAX-A yes yes Option A01: Use
adapter cable M1943A
or M1943AL together
with OC-3 adapter
cable.
Option A02: Must use
adapter cables
M1943NL and OC-3
adapter cable.
OxiCliq P See OxiMax MAX-P yes yes
OxiCliq I See OxiMax MAX-I yes yes
OxiCliq N See OxiMax MAX-N yes yes
Oxiband OXI-A/
N
Adult / neonatal sensor no yes Must use M1943NL
adapter cable.
Oxiband OXI-P/I Pediatric / infant sensor no yes
Durasensor
DS100A
Adult finger clip sensor no yes
Dura-Y D-YS Y-sensor no yes
Product Number Description Compatible with Comments
Opt. A01 Opt. A02
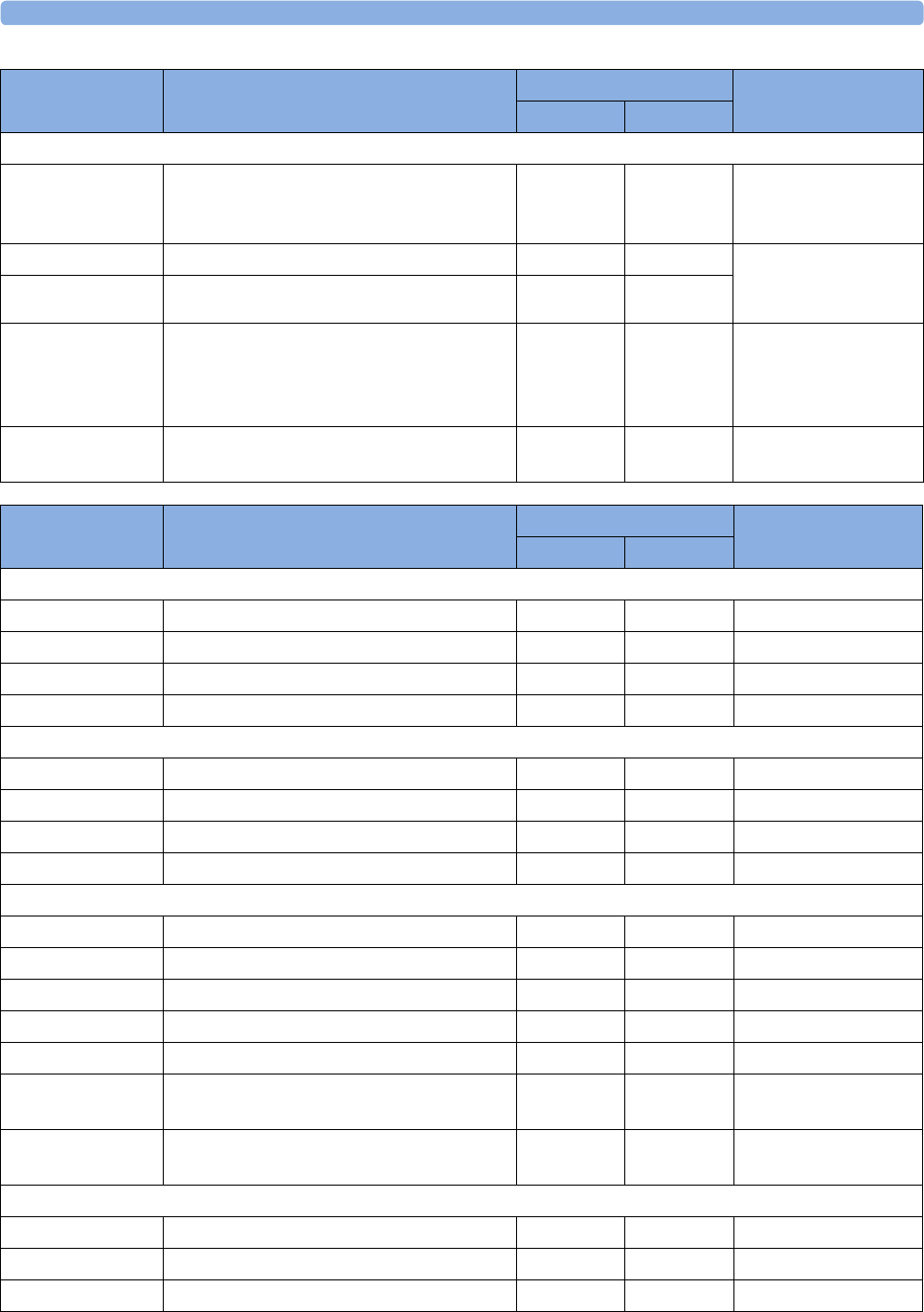
35 Accessories
379
Extension / Adapter Cables for Philips and Nellcor Sensors
M1941A Extension cable (2 m) yes yes For use with Philips
reusable sensors and
M1943A adapter cable.
M1943A Adapter cable (1.1 m cable) yes no Adapter cable for
Philips/Nellcor
disposable sensors.
M1943AL Adapter cable (3 m cable) yes no
M1943NL OxiMax adapter cable (3 m cable) no yes Adapter cable for
Philips disposable/
Nellcor disposable and
reusable sensors.
OC-3 Adapter Cable for OxiCliq sensors yes yes Available from Nellcor
only.
Product Number Description Compatible with Comments
Opt. A01 Opt. A02
Product Number Description Compatible with Philips Part Number
Opt. A01 Opt. A02
MASIMO LNOP® reusable sensors.
LNOP DCI Adult Finger Sensor (> 30 kg) yes no n/a
LNOP DCIP Pediatric Finger Sensor (10 - 50 kg) yes no n/a
LNOP YI Multi-Site Sensor (> 1kg) yes no n/a
LNOP TC-I Ear Sensor (> 30 kg) yes no n/a
MASIMO LNCS® reusable sensors.
LNCS DCI Adult Finger Sensor (> 30 kg) yes no n/a
LNCS DCIP Pediatric Finger Sensor (10 - 50 kg) yes no n/a
LNCS YI Multi-Site Sensor (> 1kg) yes no n/a
LNCS TC-I Ear Sensor (> 30 kg) yes no n/a
MASIMO LNOP® disposable adhesive sensors.
LNOP Adt Adult Sensor (> 30 kg) yes no n/a
LNOP Adtx Adult Sensor (> 30 kg) yes no n/a
LNOP Pdt Pediatric Sensor (10 - 50 kg) yes no n/a
LNOP Pdtx Pediatric Sensor (10 - 50 kg) yes no n/a
LNOP Inf-L Infant Toe Sensor (3 - 20 kg) yes no n/a
LNOP Neo-L Neonatal Sensor (< 3 kg)
or Adult adhesive Sensor (> 40 kg)
yes no n/a
LNOP NeoPt-L Neonatal Pre-Term Sensitive Skin Sensors
(< 1 kg)
yes no n/a
MASIMO LNCS® disposable adhesive sensors.
LNCS Adtx Adult Finger Sensor, 18 inch (> 30 kg) yes no n/a
LNCS Adtx-3 Adult Finger Sensor, 3 feet (> 30 kg) yes no n/a
LNCS Pdtx Pediatric Finger Sensor, 18 inch (10 - 50 kg) yes no n/a
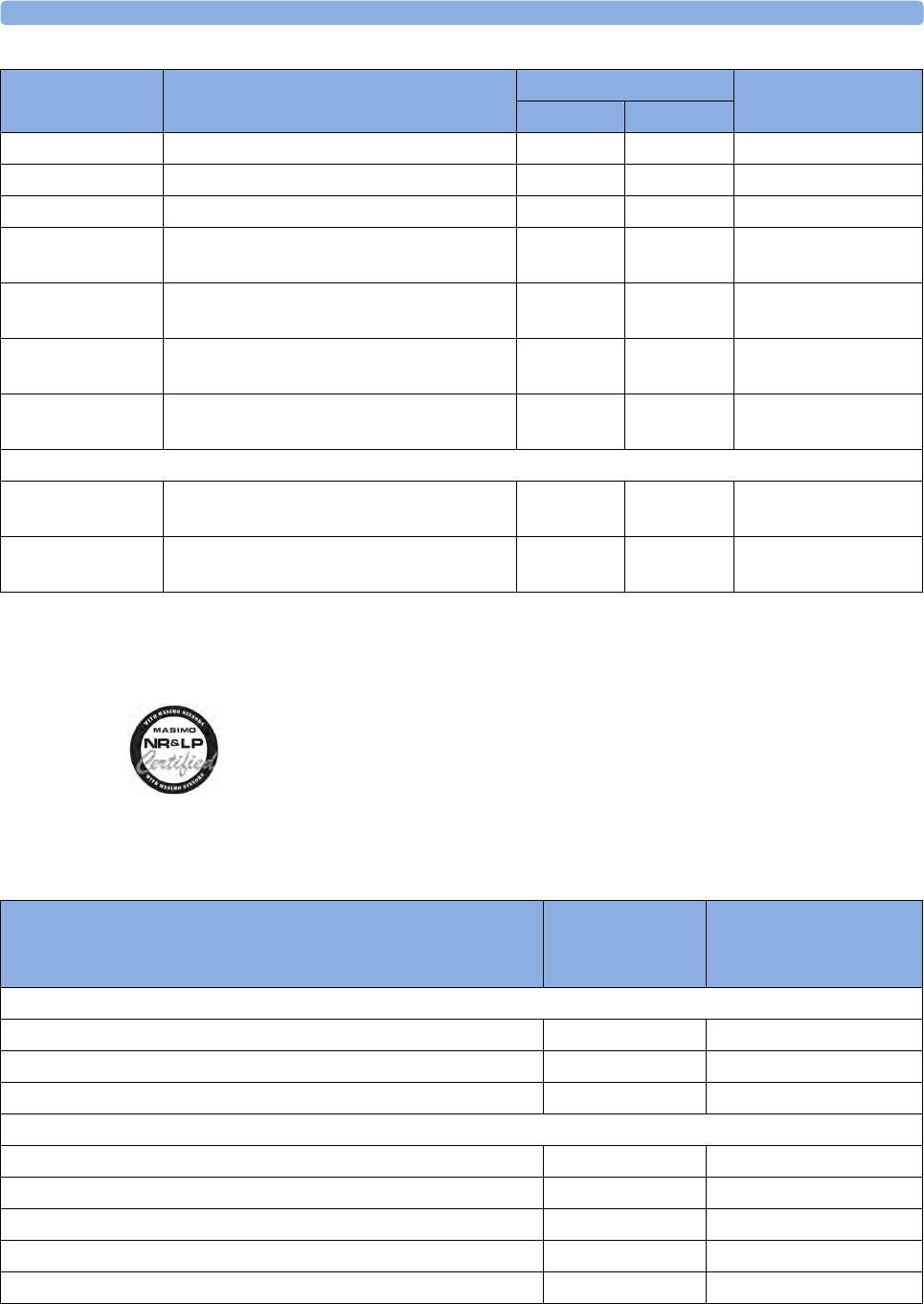
35 Accessories
380
The Philips M3001A/M3002A option A01 and the M1020B option A01 SpO2 Module use Masimo
certified pulse oximetry for reduced noise and low perfusion performance with Masimo Sensors under
the Masimo NR&LP protocol available from Masimo.
Temperature Accessories
LNCS Pdtx-3 Pediatric Finger Sensor, 3 feet (10 - 50 kg) yes no n/a
LNCS Inf Infant Toe Sensor, 18 inch (3 - 20 kg) yes no n/a
LNCS Inf-3 Infant Toe Sensor, 3 feet (3 - 20 kg) yes no n/a
LNCS Neo Neonatal Foot Sensor, 18 inch (< 3 kg)
or Adult Finger Sensor 18 inch(> 40 kg)
yes no n/a
LNCS Neo-3 Neonatal Foot Sensor, 3 feet (< 3 kg)
or Adult Finger Sensor, 3 feet(> 40 kg)
yes no n/a
LNCS NeoPt Neonatal pre-term sensitive skin Sensor
18 inch (< 1 kg)
yes no n/a
LNCS NeoPt-3 Neonatal pre-term sensitive skin Sensor
3 feet (< 1 kg)
yes no n/a
Adapter Cable for MASIMO sensors.
LNOP MP12 LNOP MP Series Patient Cable (3.6 m)
Adapter Cable for Masimo LNOP Sensors
yes no 451261000761
LNC MP10 LNCS MP Series Patient Cable (3.0 m)
Adapter Cable for Masimo LNCS Sensors
yes no 989803148221
Product Number Description Compatible with Philips Part Number
Opt. A01 Opt. A02
Temperature Probes Part No. Minimum measurement
time for accurate
readings
Reusable
General purpose probe 21075A 90 sec
Small flexible vinyl probe (Infant/Pediatric) 21076A 60 sec
Attachable surface probe 21078A 60 sec
Disposable
General purpose probe M1837A 90 sec
Skin probe 21091A 60 sec
Esophageal/Stethoscope Probe (French 12) 21093A 180 sec
Esophageal/Stethoscope Probe (French 18) 21094A 210 sec
Esophageal/Stethoscope Probe (French 24) 21095A 310 sec
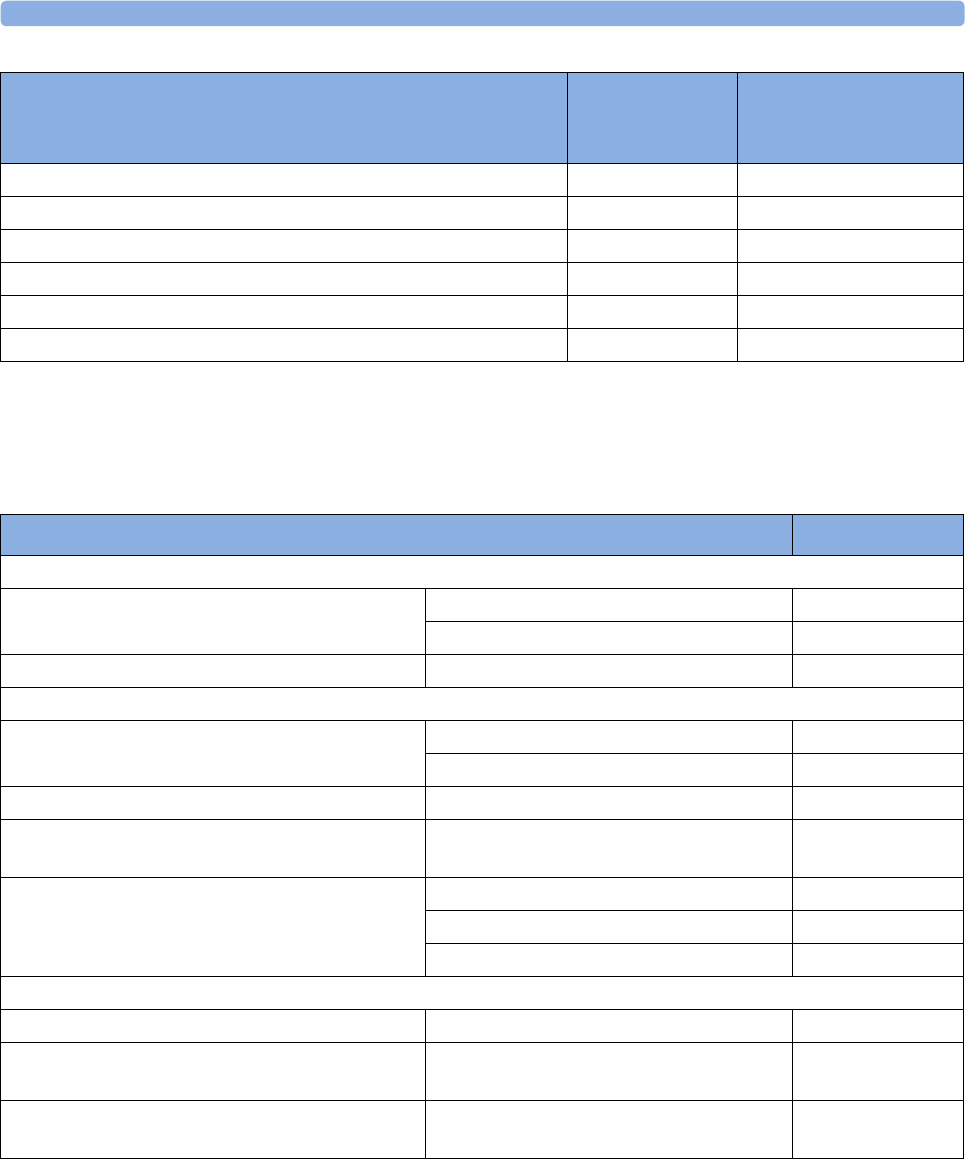
35 Accessories
381
Cardiac Output (C.O.) Accessories
See Pressure accessories for PULSION continuous cardiac output accessories.
Esophageal/Rectal Probe (French 12) 21090A 90 sec
Foley Catheter Probe (12 French) M2255A 180 sec
Foley Catheter Probe (16 French) 21096A 180 sec
Foley Catheter Probe (18 French) 21097A 180 sec
Adapter cable 1.5m 21082B
Adapter cable 3.0m 21082A
Temperature Probes Part No. Minimum measurement
time for accurate
readings
Description Part No.
Accessories common to both methods
Accessories Set of ice buckets 14455A
Remote handswitch 15244A
PiCCO inline temperature probe Latex free M1646A
Right Heart Thermodilution
C.O. Interface Cables 2.7 meter cable M1642A
2.4 m + 2.4 m cable M1643A
Right heart catheter for thermodilution (from Edwards Lifesciences) 831HF75
Edwards CO-Set+ (only with 23001A/B) contact Edwards Lifesciences for
information
Injectate Probes 2.4m injectate temp. probe (reusable) 23001A
0.5m injectate temp. probe (reusable) 23001B
Ice bath temp. probe 23002A
Transpulmonary Thermodilution
C.O. Interface Cables 2.4 m + 2.4 m cable M1643A
PULSION Pressure Transducer Kits (pressure line
available in various lengths)
Contact PULSION for information
Pressure Interface Cable for disposable pressure
transducer
PULSION PMK 206
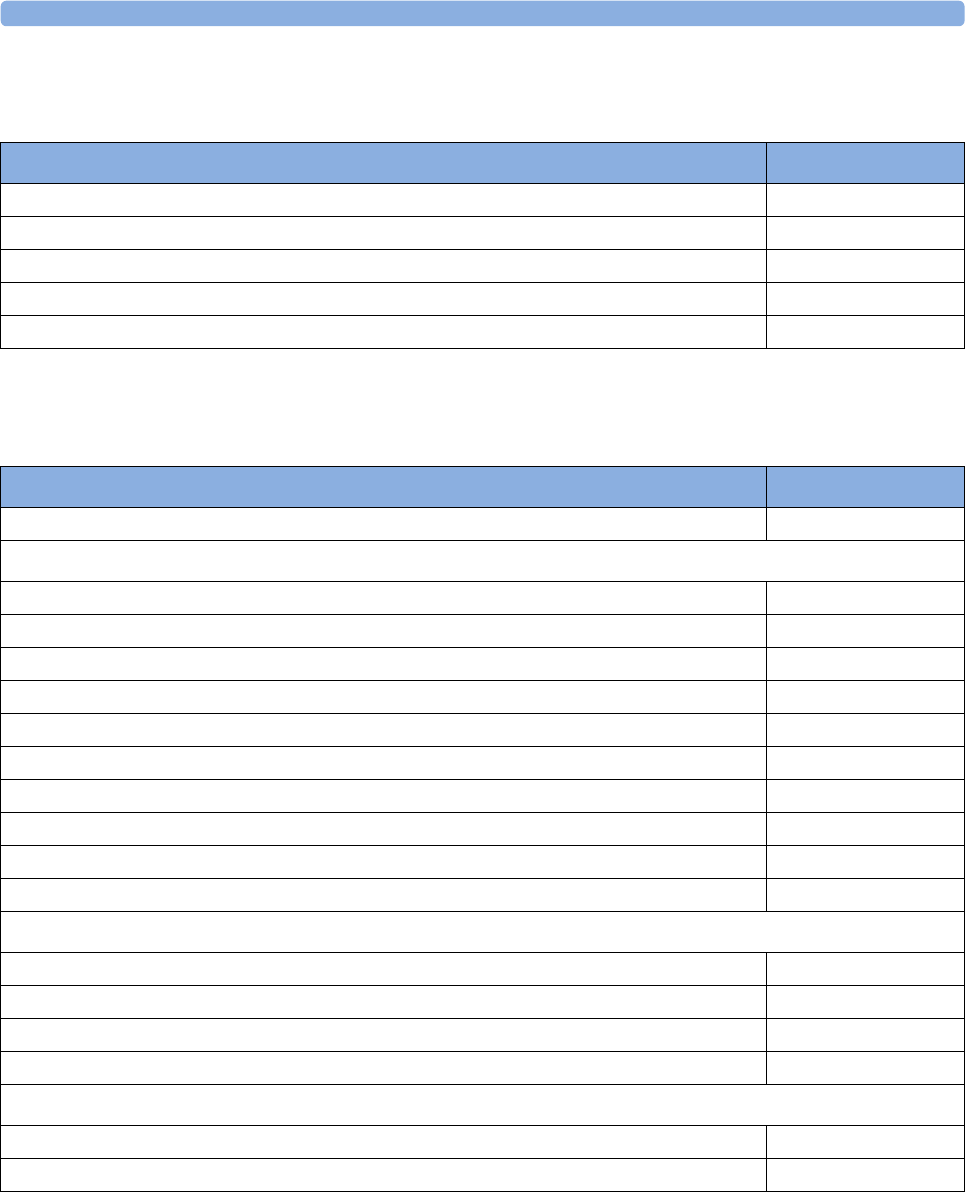
35 Accessories
382
Mainstream CO2 Accessories
Sidestream CO2 Accessories
Description Part No.
CO2 Sensor M2501A
Adult/Pediatric Airway Adapter (reusable) M2513A
Infant Airway Adapter (reusable) M2516A
Adult Airway Adapter (single-patient use) M2533A
Infant Airway Adapter (single-patient use) M2536A
Description Part No.
CO2 Sensor M2741A
Nasal and Oral-Nasal Cannulas
CO2 Nasal Cannula, Adult M2744A
CO2 Nasal Cannula, Pediatric M2745A
CO2 Nasal Cannula, Infant M2746A
CO2 / O2 Nasal Cannula, Adult M2750A
CO2 / O2 Nasal Cannula, Pediatric M2751A
CO2 / O2 Nasal Cannula, Infant 989803144471
CO2 Oral-Nasal Cannula, Adult M2756A
CO2 Oral-Nasal Cannula, Pediatric M2757A
CO2 / O2 Oral-Nasal Cannula, Adult M2760A
CO2 / O2 Oral-Nasal Cannula, Pediatric M2761A
Airway Adapters
Airway Adapter Set, ET > 4.0 mm M2768A
Airway Adapter Set, ET =< 4.0 mm 989803144531
Airway Adapter Set H, ET > 4.0 mm M2772A
Airway Adapter Set H, ET =< 4.0 mm M2773A
Straight Sample Lines
Straight Sample Line M2776A
Straight Sample Line H M2777A
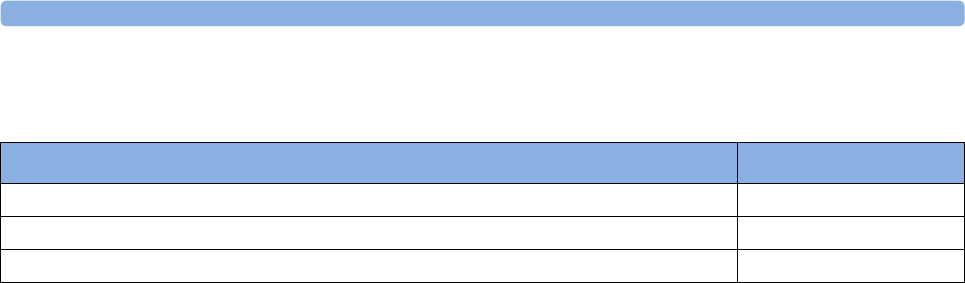
35 Accessories
383
Mainstream CO2 Accessories (for M3016A)
Microstream CO2 Accessories
• "FilterLine Set" is a combination of a FilterLine with an Airway Adapter.
• "H" in the accessory name indicates suitability for humidified ventilation and longer usage due to
the active removal of humidity from the sample line.
• "Smart CapnoLine" is a combined oral-nasal FilterLine.
• "Smart CapnoLine O2" is a combined oral-nasal-O2-CO2 FilterLine.
• "NIV Line" is a nasal FilterLine suitable for mask ventilation (for example, C-PAP).
• The accessories are supplied in packs of 25.
• Extension is not compatible with the M2786A Infant/Neonatal Flow Sensor for the spirometry
measurement (M1014A).
Description Part No.
CO2 Sensor M1460A
Standard Airway Adapter (reusable) M1465A
Small Airway Adapter (reusable) 14363A
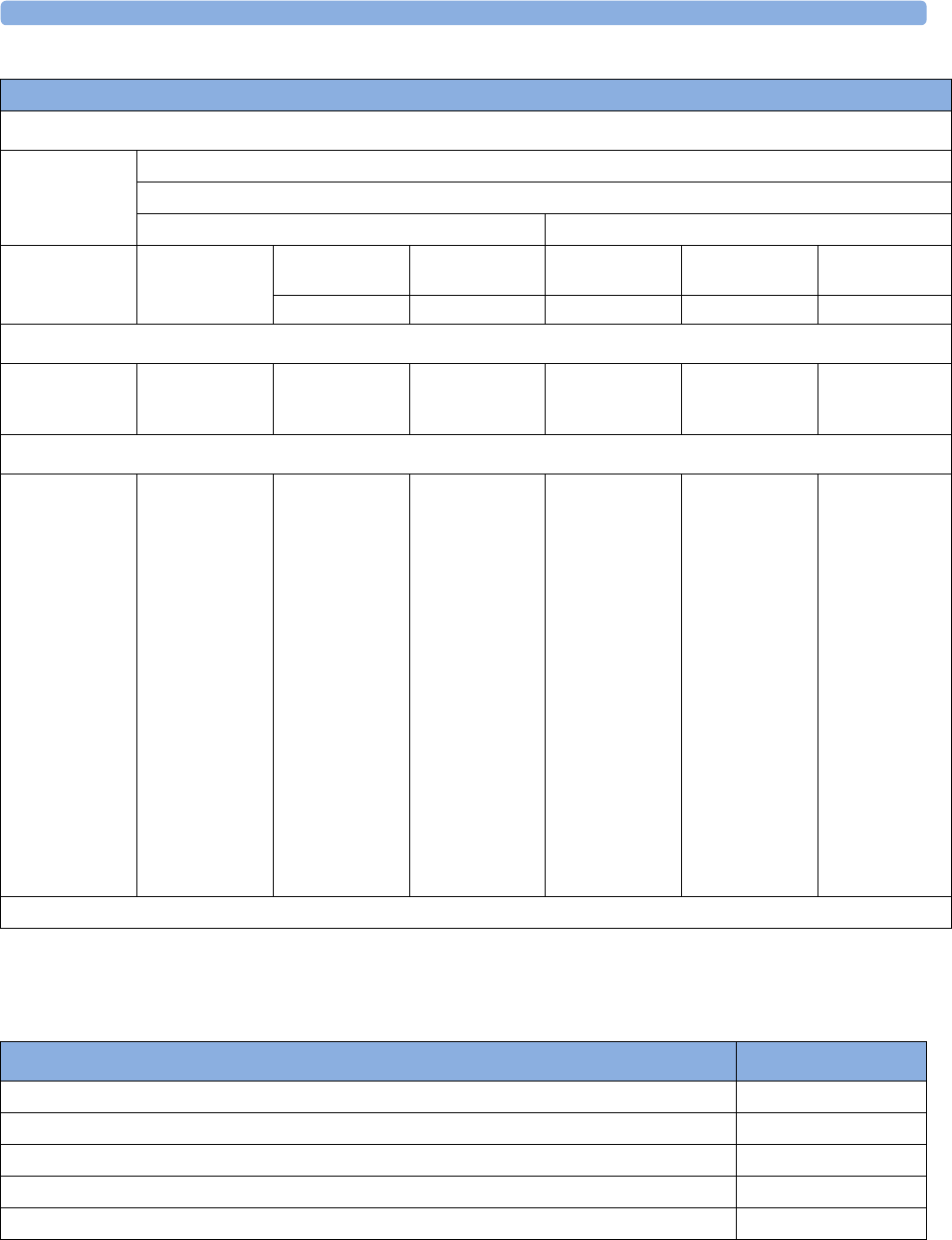
35 Accessories
384
Spirometry Accessories
Microstream accessory selection flowchart
Is the patient intubated?
Yes No
Does the patient need oxygen?
Yes No
Short-term
(up to 6 hours)
Long-term
(up to 72 hours)
Short-term
(up to 8 hours)
Long-term
(up to 24 hours)
Long-term
(up to 24 hours)
Short-term
(up to 8 hours)
Short-term
(up to 8 hours)
Oral/Nasal Nasal Nasal Oral/Nasal Nasal
Key Applications
Critical Care OR, EMS, ED Procedural
Sedation, Critical
Care, EMS, ED
Critical Care, Sleep
Lab, Long-term
Pain Management
Critical Care, Sleep
Lab
Procedural
Sedation, Critical
Care, EMS, ED
EMS, ED
Philips part numbers (A = Adult, P= Pediatric, I = Infant, N = Neonate)
FilterLine Set:
A/P: M1920A
FilterLine Set
Long:
A/
P:989803160241*
FilterLine:
M1925A*
FilterLine H Set:
A/P: M1921A
I/N: M1923A
FilterLine H Set
Long
A/
P:989803160251*
I/
N:989803160261*
VitaLine H Set:
A/
P:989803159571*
I/N:
989803159581*
FilterLine H:
M1926A*
Smart CapnoLine
O2:
A: M2522A
P: M2520A
Smart CapnoLine
O2 Long
A:989803160281*
P:989803160271*
CapnoLine HO2:
A: M4680A
P: M4681A
CapnoLine H:
A: M4689A
P: M4690A
I/N: M4691A
Smart CapnoLine:
A: M2526A
P: M2524A
Smart CapnoLine
Plus Long
A:989803160301*
NIV Line:
A: 4686A
P: M4687A
*Not available in all geographies.
Description Part No.
Adult/Pediatric Flow Sensor M2785A
Neonatal Flow Sensor M2786A
Adult/Pediatric CO2/Flow Sensor M2781A
Neonatal CO2/Flow Sensor M2782A
Pediatric CO2/Flow Sensor M2783A
35 Accessories
385
Measurement of CO2 and Spirometry with Neonates
For measurement of CO2 and Spirometry with neonates, the use of the M3014A Mainstream CO2
Extension, the M1014A Spirometry Module and the M2782A Combined CO2/Flow Sensor is
recommended.
The M1923A Filterline H Set Infant/Neonatal used for Microstream CO2 measurement with the
M3015A Extension is not compatible with the M2786A Infant/Neonatal Flow Sensor for the
spirometry measurement (M1014A).
tcGas Accessories
This symbol indicates that the specified transducer (but not its membranes) is designed to have
special protection against electric shocks (particularly regarding allowable leakage currents), and is
defibrillator proof.
1May not be available in all countries due to pending regulatory clearance
EEG Accessories
Description Part No.
tcpO2/CO2 transducer M1918A
Accessory Kit for M1918A (O-ring remover, absorbent paper, electrolyte solution, 12
replacement membranes)
15209-60010
Application Kit for M1918A (4x25 disposable fixation rings, contact fluid) 15209-60020
tcpO2/CO2 transducer M1918B1
Accessory Kit for M1918B (10 replacement membranes, electrolyte solution) 9898031519511
Application Kit for M1918B (4x25 disposable fixation rings, contact fluid) 9898031519611
Calibration gas - 6 gas bottles 15210-60010
Calibration gas - 6 gas bottles (Europe and Japan only) 15210-64010
Replacement tubing (5 tubes) M2205A
Calibration unit 15210B
Radiometer TCC3 calibration unit (available from Radiometer) n/a
Description Part No.
Trunk Cable 2.7 m M2268A
Trunk Cable, 1.0 m M2269A
Reusable 80-cm-long 5-lead cables with 10 mm silver/silverchloride leadwired cup electrodes
(Adult)
M1931A
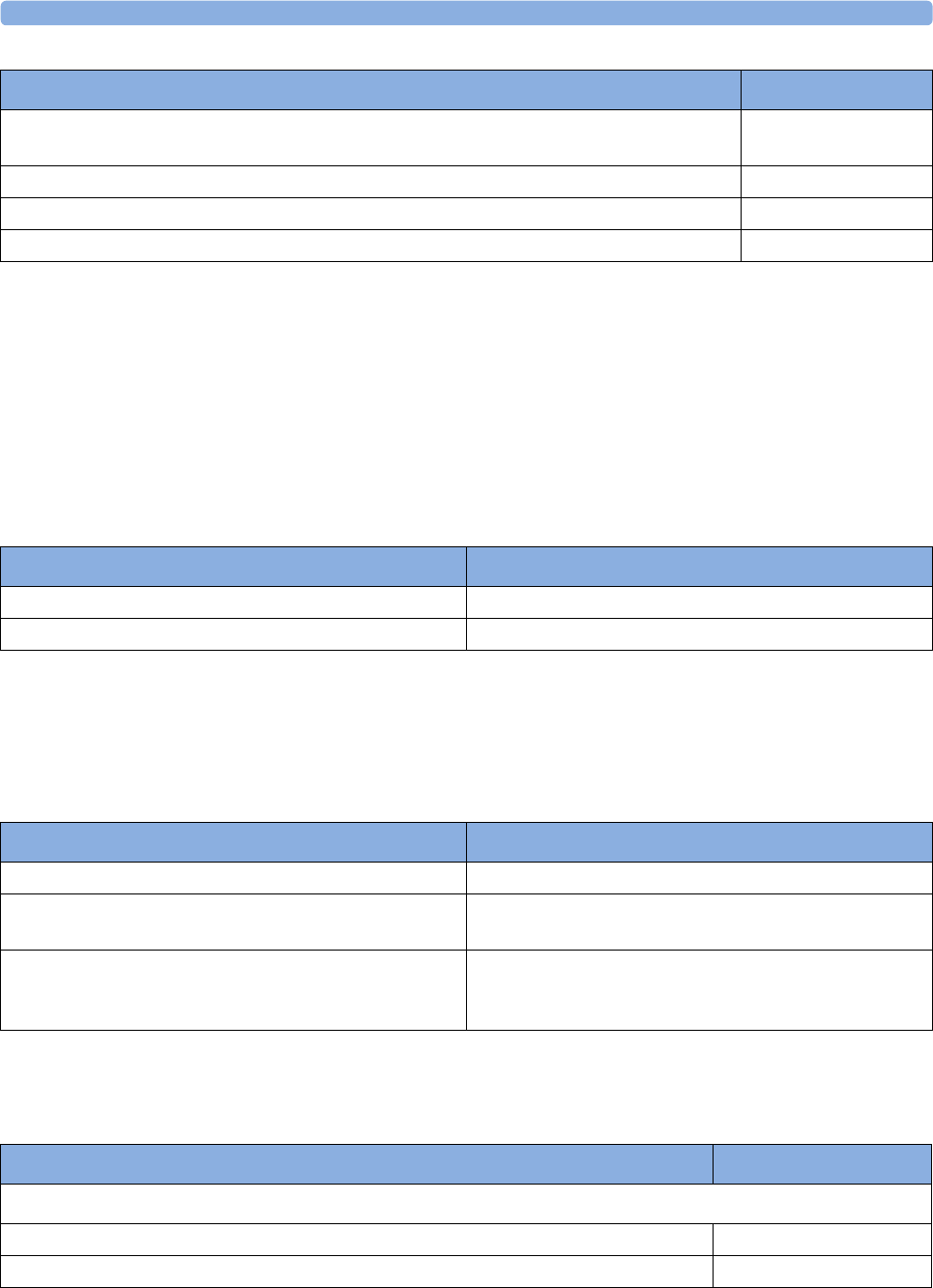
35 Accessories
386
BIS Accessories
To re-order sensors, contact Aspect Medical Systems. BIS sensors are not available from Philips.
SO2 Accessories for M1021A
Contact your local Hospira representative for information on accessories. They are not available from
Philips.
SO2 Accessories for M1011A
Contact your local PULSION or Edwards representative for information on accessories. They are not
available from Philips.
Recorder Accessories
Reusable 80 cm 5-lead cables with 6 mm silver/silverchloride leadwired cup electrodes
(Pediatric/Neonatal)
M1932A
Reusable 80 cm 5-lead cables with clip M1934A
Disposable EEG electrodes M1935A
EC2™ Electrode Cream (conductive paste) M1937A
Description Part No.
Description Hospira Part No.
Optical Module 50131
Hospira Opticath® Catheter family (SvO2, ScvO2) Contact Hospira for part numbers of compatible catheters
Description Product Number (Order Number)
Philips SO2 Optical Module 989803151591
Pulsion: CeVOX Fiberoptic Probe family (ScvO2) Contact PULSION for part numbers of compatible
probes
Edwards: Philips-compatible versions of the PreSep
Catheter (ScvO2) or Swan-Ganz Oximetry Catheter
(SvO2) families
Contact Edwards for part numbers of compatible
catheters
Description Part No.
For M1116B recorder:
10 rolls of paper 40477A
80 rolls of paper 40477B
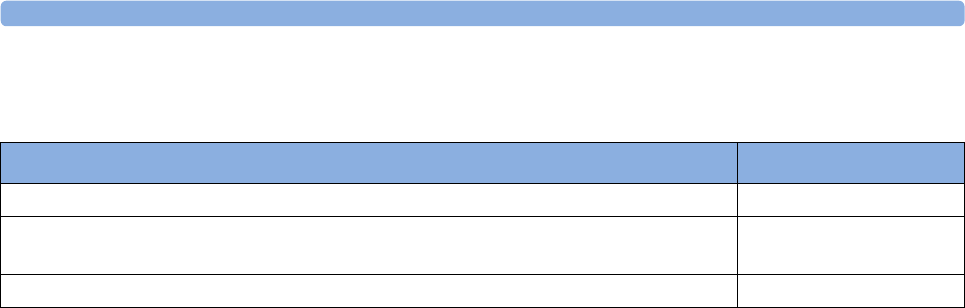
35 Accessories
387
Battery Accessories
Description Part No.
Lithium Ion Smart Battery 1Ah (internal battery for X2) M4607A
Battery Charger and Conditioner (requires size adapter 4512 610 17451 to charge
M4607A battery)
865432
Size adapter for M4607A battery 4512 610 17451

35 Accessories
388

36 Specifications
389
36Specifications
The specifications in this section apply to the MX600, MX700 and MX800 patient monitors.
The monitors are not user installable. They must be installed by qualified service personnel.
Intended Use
The monitor is intended to be used for monitoring and recording of, and to generate alarms for,
multiple physiological parameters of adults, pediatrics, and neonates in health care facilities. The
monitor is to be used by trained health care professionals.
The monitor is only for use on one patient at a time. It is not intended for home use. Rx only:
U.S. Federal Law restricts this device to sale by or on the order of a physician. Not a therapeutic
device.
The transcutaneous gas measurement (tcGas) is restricted to neonatal patients only.
ST segment monitoring is intended for use with adult patients only and is not clinically validated for
use with neonatal and pediatric patients.
The ECG measurement is intended to be used for diagnostic recording of rhythm and detailed
morphology of complex cardiac complexes (according to AAMI EC 11).
BIS is intended for use under the direct supervision of a licensed health care practitioner or by
personnel trained in its proper use. It is intended for use on adult and pediatric patients within a
hospital or medical facility providing patient care to monitor the state of the brain by data acquisition
of EEG signals. The BIS may be used as an aid in monitoring the effects of certain anesthetic agents.
Use of BIS monitoring to help guide anesthetic administration may be associated with the reduction of
the incidence of awareness with recall in adults during general anesthesia and sedation.
The SSC Sepsis Protocol, in the ProtocolWatch clinical decision support tool, is intended for use with
adult patients only.
The derived measurement Pulse Pressure Variation (PPV) is intended for use with sedated patients
receiving controlled mechanical ventilation and mainly free from cardiac arrhythmia. The PPV
measurement has been validated only for adult patients.
The monitor is indicated for use by health care professionals whenever there is a need for monitoring
the physiological parameters of patients.
WARNING
The monitor is not intended for use in an MRI environment or in an oxygen-enriched environment
(for example, hyperbaric chambers).
Manufacturer's Information
You can write to Philips at this address

36 Specifications
390
Philips Medizin Systeme Boeblingen GmbH
Hewlett-Packard-Str. 2
71034 Boeblingen
Germany
Visit our website at: www.healthcare.philips.com/us/.
© Copyright 2011. Koninklijke Philips Electronics N.V. All Rights Reserved.
BIS Manufacturer's Information
BISx, the BIS Engine, the DSC, the Patient Interface Cable and the BIS Sensor are manufactured by
Aspect Medical Systems:
Aspect Medical Systems, Inc
141 Needham St
Newton,
MA 02464
USA
1-617-559-7000
Free call:
1-888-BIS_INDEX
1-888-247-4633
Email: bis_info@aspectms.com
Web: www.aspectmedical.com
Address of the EU Authorized Representative:
Aspect Medical Systems International B.V.
Rijnzathe 7d2
3454 PV De Meern
The Netherlands
Phone: +31.30.662.9140
Email: amsint@aspectms.com
Trademark Acknowledgement
PiCCOTM is a trademark of PULSION Medical Systems AG.
Bispectral Index and BIS are trademarks of Aspect Medical Systems Inc, and are registered in the USA,
EU and other countries.
Microstream®, FilterLine®, and Smart CapnoLine® are trademarks or registered trademarks of
Oridion Systems Ltd.
Citrix® and ICA® (Independent Computing Architecture) are registered trademarks of Citrix Systems,
Inc.
The following are trademarks of Nellcor Puritan Bennett Incorporated: Nellcor®, Durasensor®, Dura-
Y®, Oxiband®, Oxicliq®, OxiMax®. MAX-FAST® is a trademark of Mallinckrodt Inc.
Masimo®, Masimo SET®, and LNOP are federally registered trademarks of the Masimo Corporation.
Other product and company names mentioned in this book may be trademarks of their respective
owners.
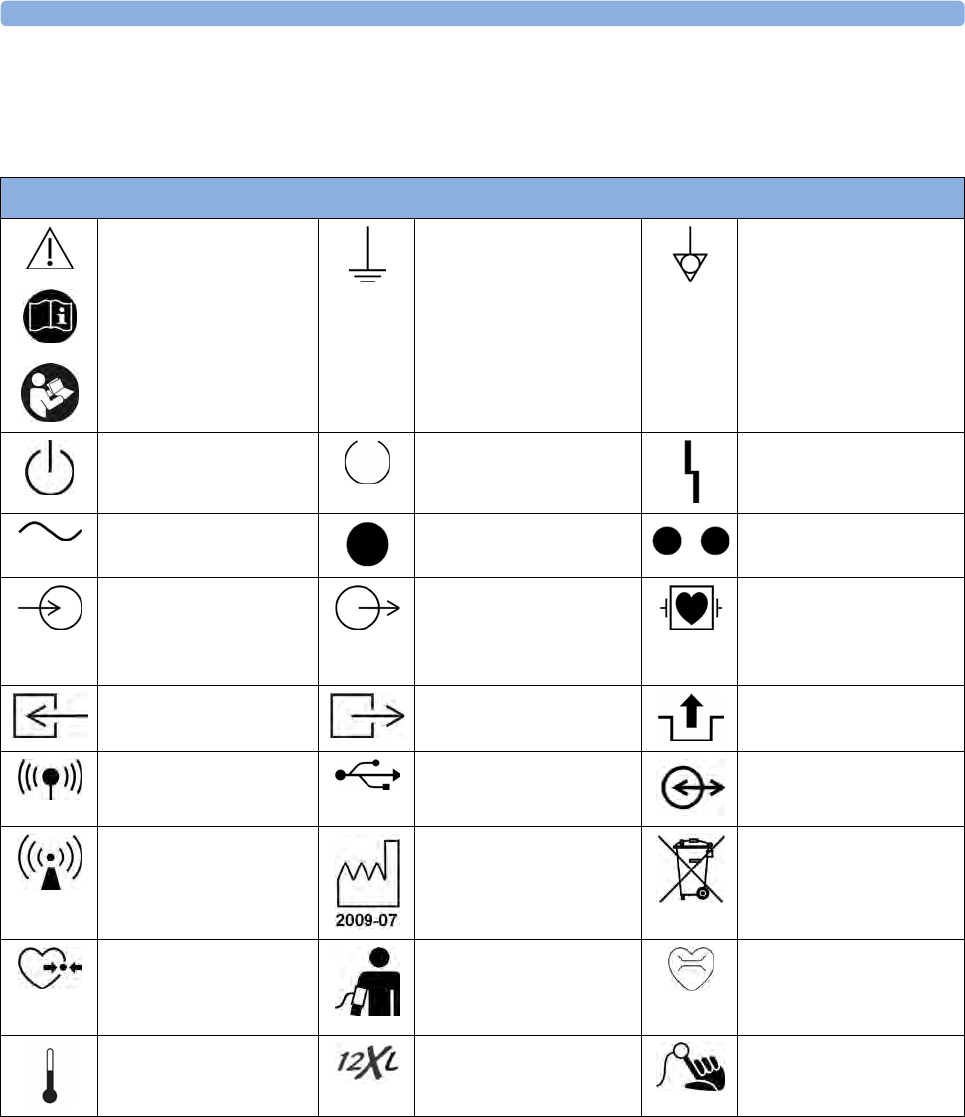
36 Specifications
391
Symbols
These symbols can appear on the monitor and its associated equipment.
Symbols
Refer to accompanying
documents
Protective earth Equipotential grounding
Standby FMS power-on indicator Error LED
Alternating current Connection direction
indicator
Connection direction
indicator
Electrical input indicator
(In some cases gas input
indicator)
Electrical output indicator
(In some cases gas output
indicator)
Connector has special
protection against electric
shocks and is defibrillator
proof
Gas input indicator Gas output indicator Quick mount release
built-in wireless network USB interface Data input/output symbol
Non-ionizing radiation
symbol
Identifies year and month
of manufacture
Always use separate
collection for waste
electrical and electronic
equipment (WEEE)
Pressure connector NBP connector Cardiac Output connector
Temperature connector Monitor supports 12-lead
ECG
SpO2 connector
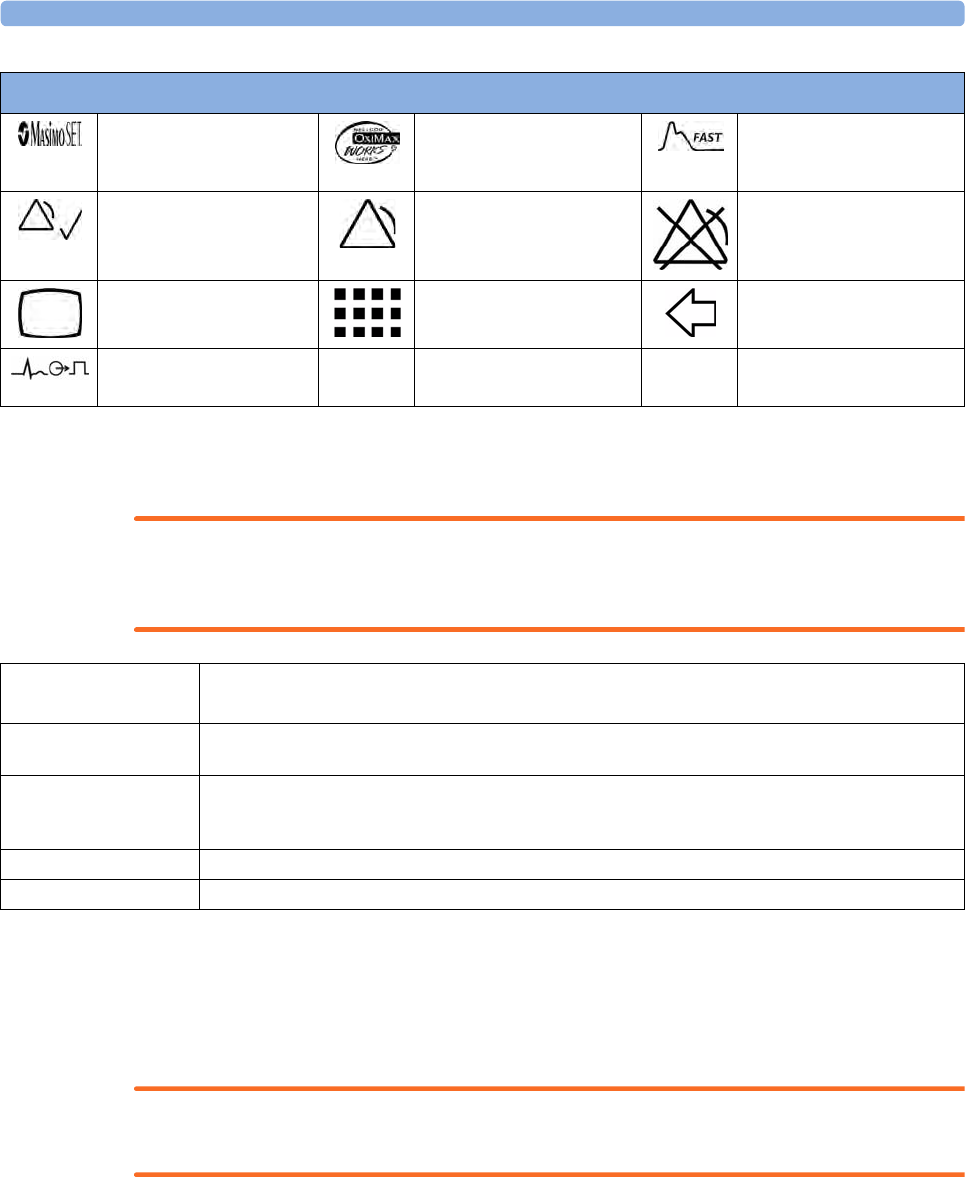
36 Specifications
392
Installation Safety Information
WARNING
If multiple instruments are connected to a patient, the sum of the leakage currents may exceed the
limits given in IEC/EN60601-1, IEC60601-1-1, UL60601-1. Consult your service personnel.
Connectors
The actual placement of boards and configuration of connections for your monitor depends on how
your hardware has been configured. See the symbols table (“Symbols” on page 389) to see which
symbols are used to mark the connections.
WARNING
Connect only medical devices to the ECG output connector socket.
Masimo SET technology Nellcor OxiMax
compatible
Uses FAST SpO2
algorithm
Silence Alarms Alarms On/Off Alarms Switched Off
Main Screen SmartKeys Back key
ECG Sync Output/
Analog ECG Output
Symbols
Grounding The monitor must be grounded during operation. If a three-wire receptacle is not available, consult the
hospital electrician. Never use a three-wire to two-wire adapter.
Equipotential Grounding If the monitor is used in internal examinations on the heart or brain, ensure that the room incorporates an
equipotential grounding system to which the monitor has a separate connections.
Combining equipment Combinations of medical equipment with non-medical equipment must comply with IEC 60601-1-1. Never
use a multiple portable socket-outlet or extension cord when combining equipment unless the socket outlet is
supplied specifically for use with that equipment.
Fusing The monitor uses double fusing (line and neutral).
Network Cables All network cables must be unshielded.
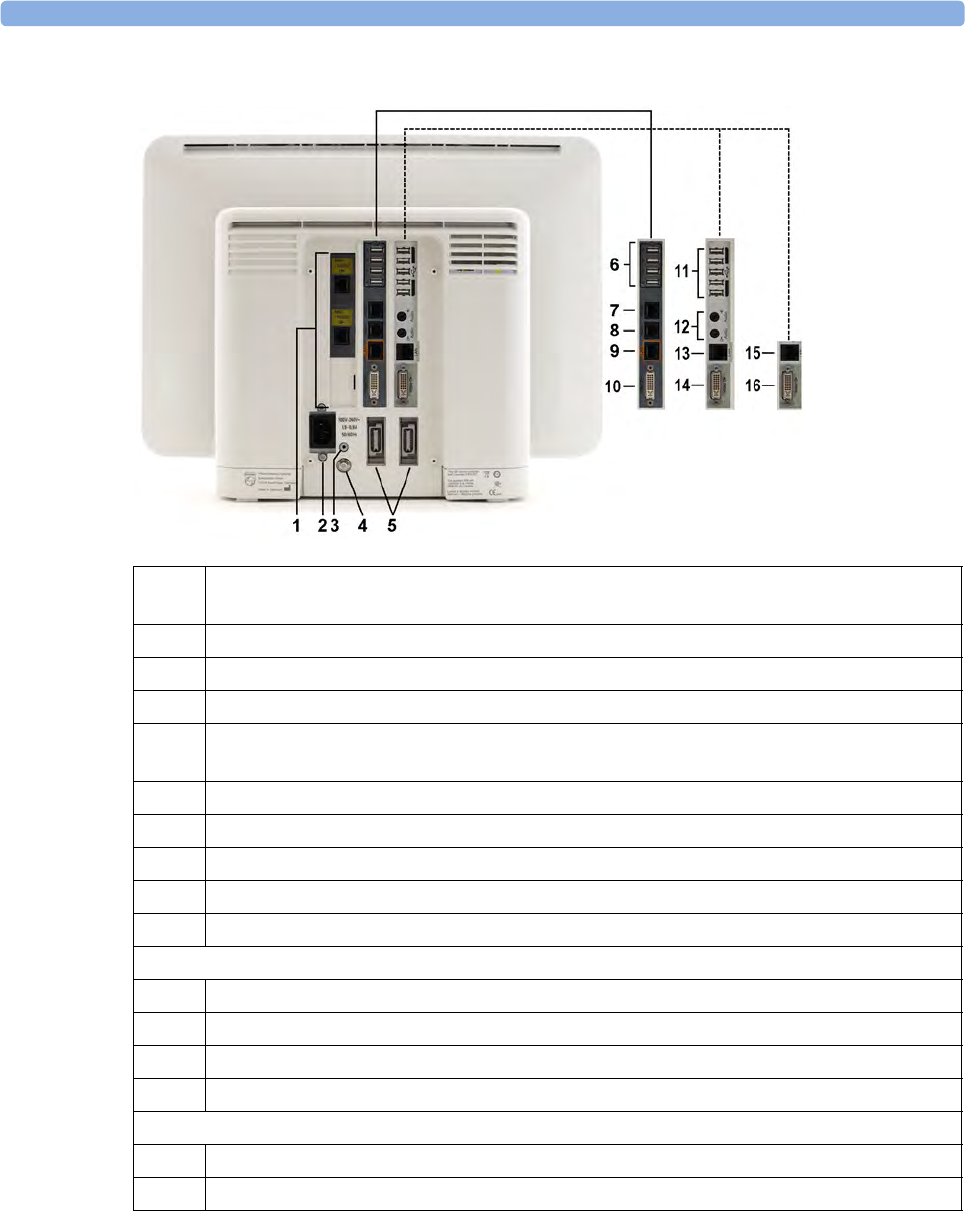
36 Specifications
393
Rear of the Monitor
1 Serial/MIB (RS232) interface cards, type RJ45 or Flexible Nurse Call interface card or
combination of both (optional)
2 AC power input
3 Protective earth screw hole
4 Equipotential ground connector
5 Measurement link connectors (MSL)
(Two standard in MX800, one standard in MX600/700)
6 USB rear connectors (for remote control, keyboard, pointing devices, printer)
7 Serial RS232 connector
8 Nurse Call
9 Wired network connector
10 Video out connector (digital/analog)
The following connectors are only present with the iPC
11 USB rear connectors (for keyboard, pointing devices, printer)
12 Audio in/out
13 Local Area Network
14 Video out connector (digital/analog)
The following connectors are only present with the Independent Display Interface
15 Serial RS232 connector for touch
16 Video out connector (digital/analog)

36 Specifications
394
Left side of the Monitor
Right side of the Monitor
1ECG Sync Output/Analog ECG output connector
1 USB side connector (only present with the iPC)
36 Specifications
395
Monitor Mounting Precautions
Mount the monitor using either the Philips Quick Mount or Fix Mount solution or another approved
mounting solution. Select the mounting equipment and the mounting position so that no patient,
operator or other person can be harmed by a monitor removed intentionally or released accidentally
from the mount. When using the Quick Mount, be aware of the danger of accidental activation of the
Quick Mount release button when lifting or moving items located under the monitor, such as pole
mounts, etc. If in doubt, use the Philips Fix Mount solution to avoid such situations. Refer to the
respective IntelliVue Monitor Service Manual, Installation Instructions chapter, for more details.
Altitude Setting
Altitude affects tcGas and CO2 measurements. The monitor must be configured at installation to the
correct altitude.
Monitor Safety Specifications
The monitors, together with the Multi-Measurement Modules (M3001A/M3002A), and the Flexible
Module Rack (M8048A), all modules and MMS extensions, comply with the Medical Device Directive
93/42/EEC.
Aspect BISx, Aspect BIS Engine and Aspect DSC comply with the requirements of the Council
Directive 93/42/EEC of 14 June 1993 (Medical Device Directive).
In addition, the product complies with:
IEC 60601-1:1988 + A1:1991 + A2:1995; EN60601-1:1990 + A1:1993 + A2:1995; UL 60601-1:2003;
CAN/CSA C22.2#601.1-M90 +Suppl. No. 1-94 + Am. 2; IEC 60601-1-1:2000; EN 60601-1-1:2001;
IEC 60601-1-2:2001 + A1:2004; EN 60601-1-2:2001 + A1:2006.
The possibility of hazards arising from software errors was minimized in compliance with ISO
14971:2007, EN60601-1-4:1996 + A1:1999 and IEC 60601-1-4:1996 + A1:1999.
Classification (according to IEC 60601-1): Class 1, Type CF, Continuous Operation. The BIS
measurement uses a Type BF applied part.
EMC And Radio Regulatory Compliance
This ISM device complies with Canadian ICES-001. Cet appareil ISM est conforme à la norme NMB-
001 du Canada.
36 Specifications
396
IntelliVue 802.11 Bedside Adapter (Option J35 Wireless Network
Adapter)
FCC and Industry Canada Radio Compliance: This device complies with Part 15 of the FCC Rules and
RSS-210 of Industry Canada. Operation is subject to the following two conditions: (1) this device may
not cause harmful interference, and (2) this device must accept any interference received, including
interference that may cause undesired operation. Any changes or modifications to this equipment not
expressly approved by Philips Medical Systems may cause harmful radio frequency interference and
void your authority to operate this equipment.
The maximum antenna gain permitted (for devices in the 5250-5350 MHz and 5470-5725 MHz bands)
complies with the e.i.r.p. limits as stated in RSS-210.
The maximum antenna gain permitted (for devices in the 5725-5825 MHz band) complies with the
e.i.r.p. limits specified for point-to-point operation, as stated in RSS-210.
The device for the band 5150-5250 MHz is only for indoor usage to reduce potential for harmful
interference to co-channel mobile satellite systems.
The OEM radio device used in this product is in compliance with the essential requirements and other
relevant provisions of Directive 1999/5/EC. This product is intended to be connected to the Publicly
Available Interfaces (PAI) and used throughout the EEA.
CAUTION
High power radars are allocated as primary users (meaning they have priority) of 5250-5350 MHz and
5650-5850 MHz and these radars could cause interference and /or damage to LE-LAN devices.
IntelliVue 802.11 Bedside Adapter CE compliances:
This device is compliant to Council Directive 73/23/EEC (Low voltage directive) & 89/336/
EEC (EMC directive) & 1999/5/EC (Radio Equipment and Telecommunications Terminal
Equipment Directive)
The radio component contained in this device is compliant to Council Directive 1999/5/
EC (Radio Equipment and Telecommunications Terminal Equipment Directive)
IntelliVue Instrument Telemetry ISM (2.4GHz)
FCC and Industry Canada Radio Compliance: This device complies with Part 15 of the FCC Rules and
RSS-210 of Industry Canada. Operation is subject to the following two conditions: (1) this device may
not cause harmful interference, and (2) this device must accept any interference received, including
interference that may cause undesired operation. Any changes or modifications to this equipment not
expressly approved by Philips Medical Systems may cause harmful radio frequency interference and
void your authority to operate this equipment.
The radio device used in this product is in compliance with the essential requirements and
other relevant provisions of Directive 1999/5/EC (Radio Equipment and Telecommunications
Terminal Equipment Directive). Class 2 radio equipment. Member states may apply restrictions on
putting this device into service or placing it on the market. This product is intended to be connected to
the Publicly Available Interfaces (PAI) and used throughout the EEA.
36 Specifications
397
IntelliVue Instrument Telemetry WMTS (US only)
FCC Radio Compliance: This device complies with Part 15 of the FCC Rules. Operation is subject to
the following two conditions: (1) this device may not cause harmful interference, and (2) this device
must accept any interference received, including interference that may cause undesired operation.
Operation of this equipment requires the prior coordination with a frequency coordinator designated
by the FCC for the Wireless Medical Telemetry Service.
Short Range Radio Interface (MX600/700/800 and 865244 Remote
Control)
FCC and Industry Canada Radio Compliance: This device complies with Part 15 of the FCC Rules and
RSS-210 of Industry Canada. Operation is subject to the following two conditions: (1) this device may
not cause harmful interference, and (2) this device must accept any interference received, including
interference that may cause undesired operation. Any changes or modifications to this equipment not
expressly approved by Philips Medical Systems may cause harmful radio frequency interference and
void your authority to operate this equipment.
The radio component contained in this device is in compliance with the essential requirements
and other relevant provisions of Council Directive 1999/5/EC (Radio Equipment and
Telecommunications Terminal Equipment Directive)
In addition the product complies with: ETSI EN 300 328; AS/NZS 4771+A1; ARIB STD-T66.
Class 1 radio equipment.
Physical Specifications
Product Maximum Weight W x H x D Comments
MX800 Monitor <12 kg (<26.4 lb) <478 x 364 x 152 mm
<18.82 x 14.33 x 5.98 in
without cable
management
MX600/MX700 Monitor <9.5 kg (<20.9 lb) <392 x 321 x 163 mm
<15.43 x 12.64 x 6.42 in
without cable
management
M3001A
Multi-Measurement Module (MMS)
<650 g (<1.4 lb) 188 x 96.5 x 51.5 mm
7.4 x 3.8 x 2 in
M3002A
Multi-Measurement Module (MMS)
<1.25 kg (<2.8 lb) 188 x 99 x 86 mm
7.4 x 3.9 x 3.4 in
including battery,
without handle or
options
M3012A
Hemodynamic MMS Extension
<550 g (<1.2 lb) <190 x 98 x 40 mm
<7.5 x 4 x 1.6 in
M3014A
Capnography MMS Extension
<500 g (<0.99 lb) <190 x 98 x 40 mm
<7.5 x 4 x 1.6 in
M3015A
Microstream CO2 MMS Extension-
<550 g (<1.21 lb) <190 x 98 x 40 mm
<7.5 x 4 x 1.6 in
M3016A
Mainstream CO2 MMS Extension
<450 g (<0.99 lb) <190 x 98 x 40 mm
<7.5 x 4 x 1.6 in
M8048A
8-Slot Flexible Module Rack (FMS-8)
<3500 g (<7.7 lb) <320 x 135 x 120 mm
12.6 x 5.3 x 4.7 in
without plug-in
modules
865243
4-Slot Flexible Module Rack (FMS-4)
<950 g (<2.09 lb) <194 x 139 x 110 mm
<7.64 x 5.47 x 4.33 in
without MMS Mount
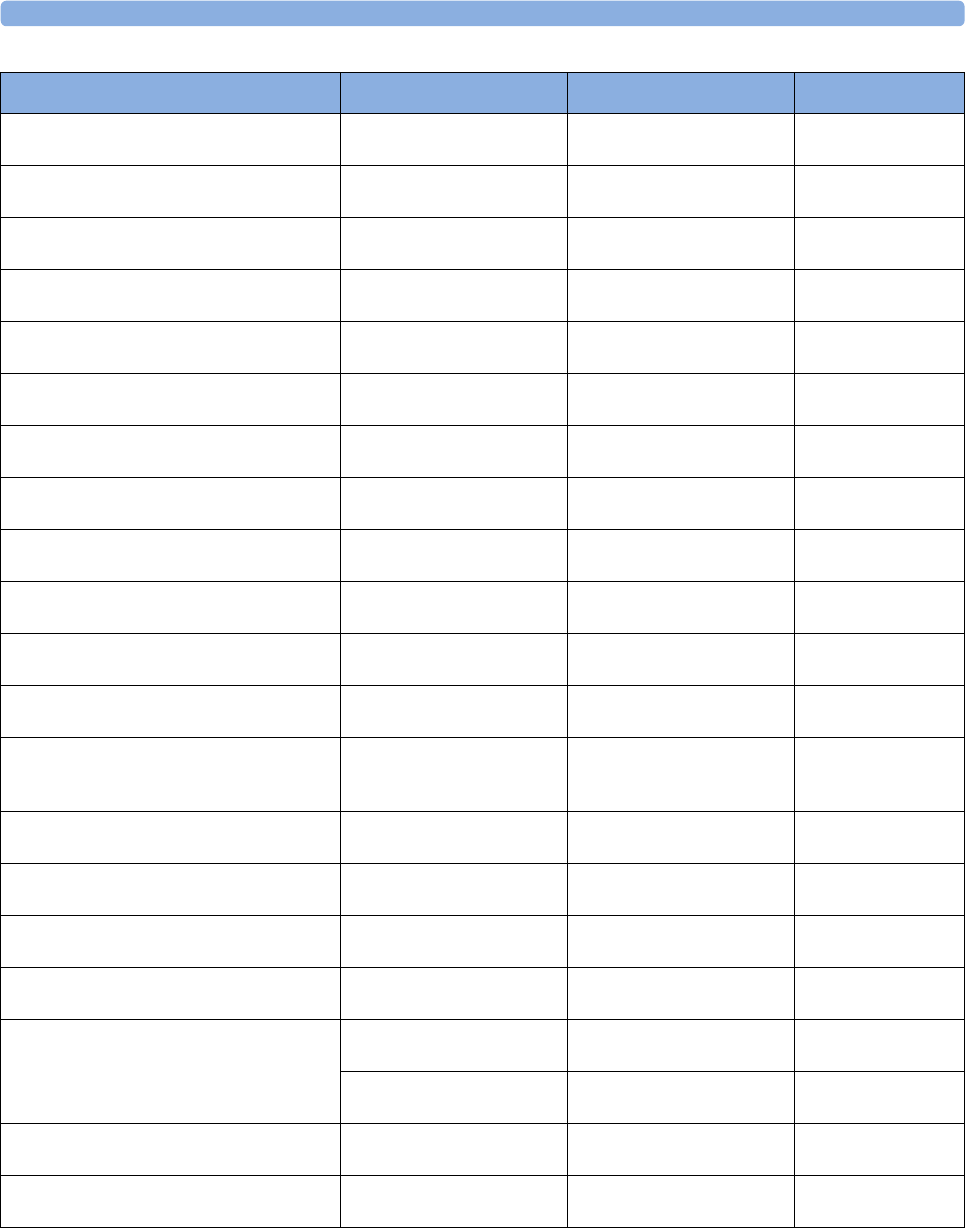
36 Specifications
398
M8025A
Remote Alarm Device
<300 g (<0.7 lb) 62 x 125 x 63 mm
2.4 x 5 x 2.5 in
M1006B
Invasive Press Module
190 g (6.7 oz)
Option #C01: 225 g (7.9 oz)
36 x 99.6 x 97.5 mm
1.4 x 3.9 x 3.8 in
M1029A
Temperature Module
215 g (7.6 oz) 36 x 99.6 x 97.5 mm
1.4 x 3.9 x 3.8 in
M1012A
Cardiac Output Module
225 g (7.9 oz) 36 x 99.6 x 97.5 mm
1.4 x 3.9 x 3.8 in
M1014A
Spirometry Module
250 g (8.8 oz) 36 x 99.6 x 97.5 mm
1.4 x 3.9 x 3.8 in
M1018A
Transcutaneous Gas Module
350 g (11.3 oz) 72.5 x 99.6 x 97.5 mm
2.9 x 3.9 x 3.8 in
M1020B
SpO2 Module
<250 g (<0.55 lb) 36 x 99.6 x 97.5 mm
1.4 x 3.9 x 3.8 in
M1021A
Mixed Venous Oxygen Saturation Module
460 g (13.04 oz) 72.5 x 99.6 x 97.5 mm
2.9 x 3.9 x 3.8 in
M1011A
SO2 Module
<200g (<7.1 oz) 36 x 99.6 x 102.5 mm
1.4 x 3.9 x 4.0 in
- Optical Module <200g (<7.1 oz) 50 x 30 x 120 mm
2.0 x 1.2 x 4.7 in
including 2.9m cable
M1027A
Electroencephalograph Module
210 g (7.4 oz) 36 x 99.6 x 97.5 mm
1.4 x 3.9 x 3.8 in
M1034A
BIS Interface Module
215 g (7.6 oz) 36 x 99.6 x 97.5 mm
1.4 x 3.9 x 3.8 in
without cables
BISx 499 g (1.1 lb) diameter x height:
95.3 x 63.5 mm
3.8 x 2.5 in
with PIC Plus Cable
(1.22 m, 4 ft) and cable
to BIS module
- DSC Digital Signal Converter 130 g (4.6 oz) (without cabling) 66 x 25 x 107 mm
2.6 x 1.0 x 4.25 in
with PIC Plus Cable
(1.22 m, 4 ft)
- BIS Engine 170 g (6.0 oz) 43 x 93 x 95 mm
1.7 x 3.7 x 3.7 in
M1032A
Vuelink Module
240 g (8.4 oz) 36 x 99.6 x 97.5 mm
1.4 x 3.9 x 3.8 in
865115
IntelliBridge EC10 Module
200 g (7.0 oz) 36 x 99.6 x 102.5 mm
1.4 x 3.9 x 4.0 in
865114
IntelliBridge EC5 Module
35 g (1.1 oz) 35 x 17 x 57 mm
1.4 x 0.7 x 2.1 in
with D-Sub 9-pin male
or female connector
25 g (0.8 oz) 21.5 x 17 x 65 mm
0.9 x 0.7 x 2.6 in
without cable and
strain relief
M1116B
Thermal Array Recorder Module
507.5 g (17.9 oz) 73 x 99.6 x 97 mm
2.9 x 3.6 x 3.9 in.
865244
Remote Control
<250 g (<8.8 oz) 53 x 165 x 23 mm
2.1 x 6.5 x 0.9 in
without navigator
knob
Product Maximum Weight W x H x D Comments
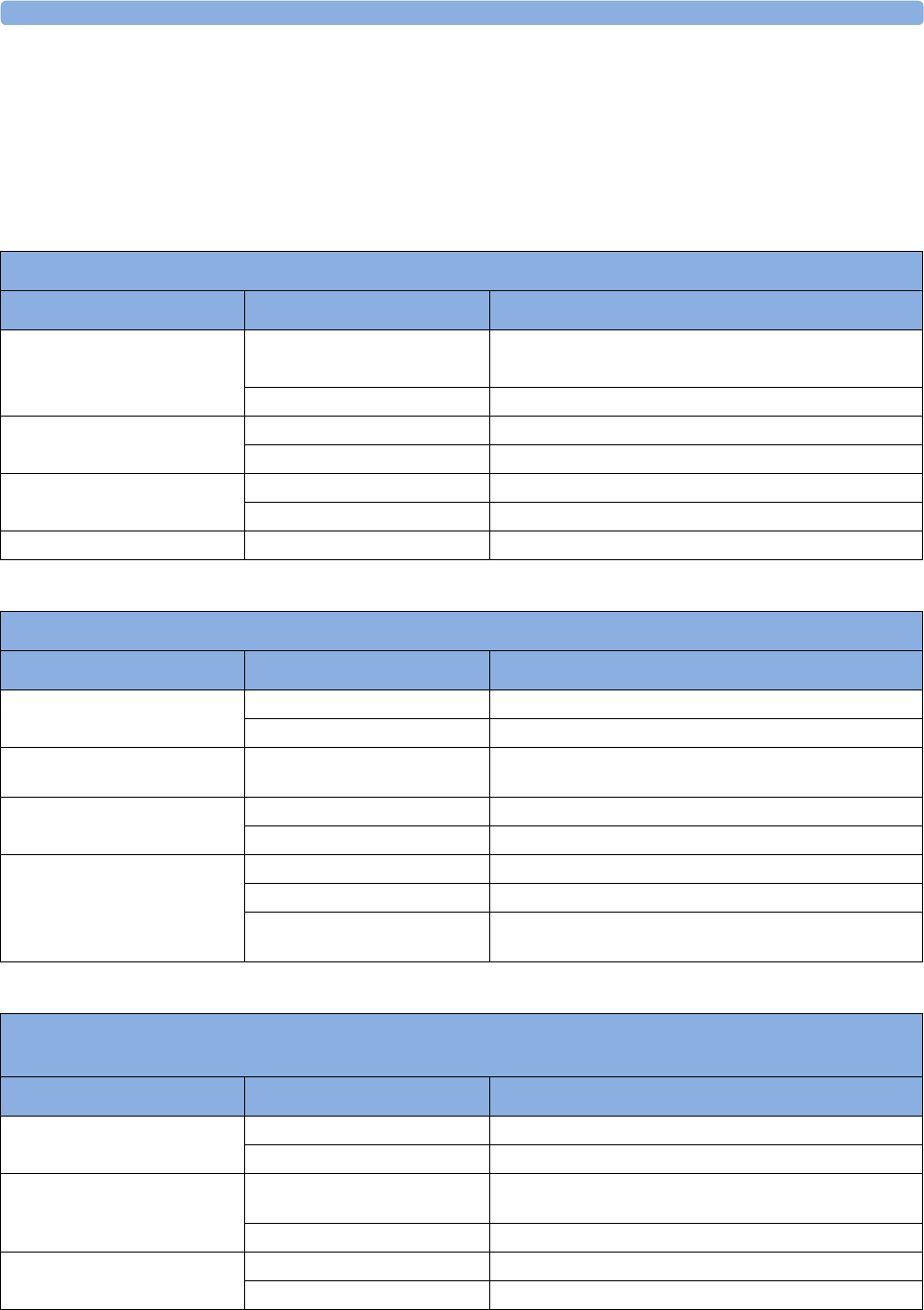
36 Specifications
399
Environmental Specifications
The monitor may not meet the performance specifications given here if stored or used outside the
specified temperature and humidity ranges.
When the monitor and related products have differing environmental specifications, the effective
range for the combined products is that range which is common to the specifications for all products.
MX600/700/800 Monitor
Item Condition Range
Temperature Range Operating 0 to 40°C (32 to 100°F)
0 to 35°C (32 to 95°F) when equipped with the iPC
Storage -20 to 60°C (-4 to 140°F)
Humidity Range Operating 15% to 95% Relative Humidity (RH) (non condensing)
Storage 5% to 95% Relative Humidity (RH)
Altitude Range Operating -500 m to 3000 m (10000 ft)
Storage -500 m to 4600 m (15000 ft)
Ingress Protection IPX1
X2 (M3002A) and External Power Supply (M8023A)
Item Condition Range
Temperature Range Operating 0 to 40°C (32 to 104°F)
Storage including transportation -20 to 60°C (-4 to 140°F)
Temperature Range when
charging the battery
Operating 0 to 35°C (32 to 95°F)
Humidity Range Operating 15% to 95% Relative Humidity (RH)
Storage including transportation 5% to 95% Relative Humidity (RH)
Altitude Range Operating -500 m to 3000 m (10000 ft)
Storage including transportation -500 m to 4600 m (15000 ft)
X2 IP32 (protected against ingress of water when the water is
dripping vertically and the monitor is tilted up to 15°)
Multi-measurement Module M3001A, MMS Extensions M3016A M3015A, M3014A, M3012A, Measurement
Modules, and 8-Slot Flexible Module Rack M8048A
Item Condition Range
Temperature Range Operating 0 to 45°C (32 to 113°F)
Non-operating -40 to 70°C (-40 to 158°F)
Humidity Range Operating 95% Relative Humidity (RH) max. @ 40°C (104°F). M3015A
only non-condensing.
Non-operating 90% Relative Humidity (RH) max. @ 65°C (150°F)
Altitude Range Operating -500 m to 4600 m (-1600 to 15000 ft)
Non-operating -500 m to 15300 m (-1600 to 50000 ft)
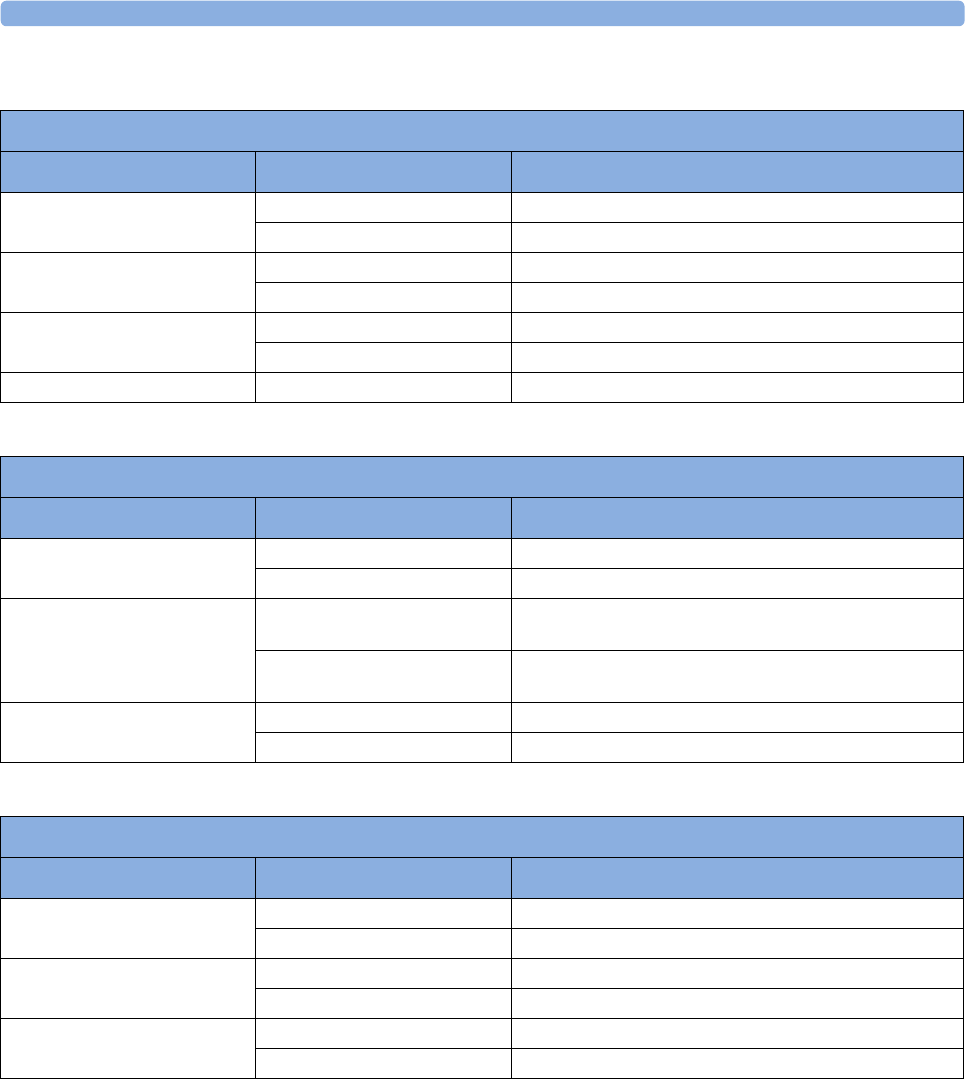
36 Specifications
400
4-Slot Flexible Module Rack 865243
Item Condition Range
Temperature Range Operating 0 to 40°C (32 to 100°F)
Storage -20 to 60°C (-4 to 140°F)
Humidity Range Operating 15% to 95% Relative Humidity (RH) (non condensing)
Storage 5% to 95% Relative Humidity (RH)
Altitude Range Operating -500 m to 3000 m (10000 ft)
Storage -500 m to 4600 m (15000 ft)
Ingress Protection IPX1
Thermal Array Recorder Module M1116B
Item Condition Range
Temperature Range Operating +5 to 45°C (41 to 113°F)
Non-operating -10 to 70°C (14 to 158°F)
Humidity Range Operating 95% Relative Humidity (RH) max. @ 40°C (104°F) (non
condensing)
Non-operating 95% Relative Humidity (RH) max. @ 65°C (150°F) (non
condensing)
Altitude Range Operating up to 3048 m (10000 ft)
Non-operating up to 3048 m (10000 ft)
Remote Control 865244
Item Condition Range
Temperature Range Operating 0 to 40°C (32 to 100°F)
Storage -20 to 60°C (-4 to 140°F)
Humidity Range Operating 15% to 95% Relative Humidity (RH) (non condensing)
Storage 5% to 95% Relative Humidity (RH)
Altitude Range Operating -500 m to 3000 m (10000 ft)
Storage -500 m to 4600 m (15000 ft)
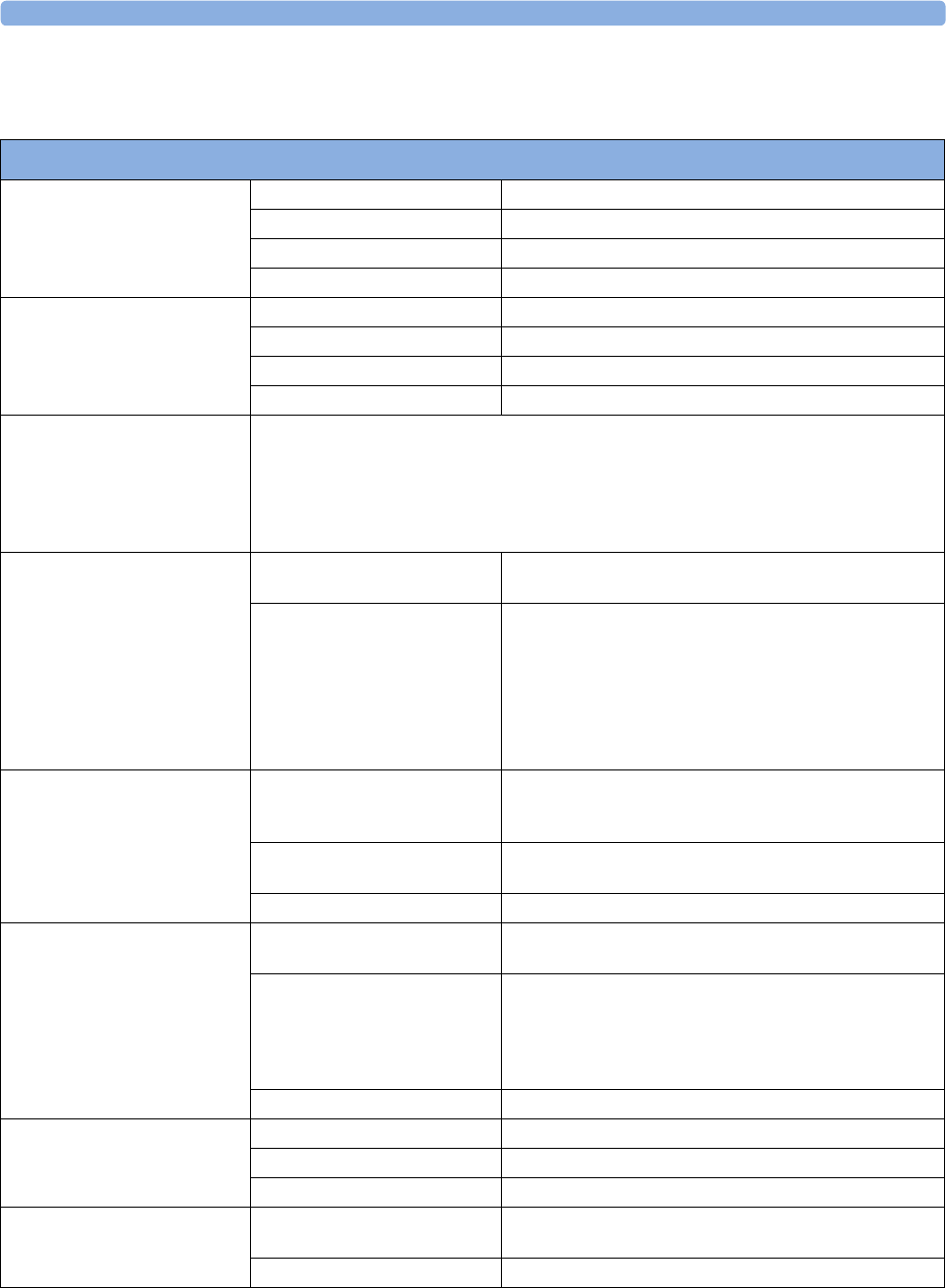
36 Specifications
401
Performance Specifications
MX600/700/800 Performance Specifications
Power Specifications Power Consumption <200 W average
Line Voltage 100 to 240 V
Current 1.9 to 0.9 A
Frequency 50/60 Hz
Indicators Alarms Off red (crossed out alarms symbol) LED
Alarms red/yellow/light blue (cyan) LED
On/Standby/Error green/red LED integrated in power switch
External Power green LED
Sounds Audible feedback for user input
Prompt tone
QRS tone, or SpO2 modulation tone
4 different alarm sounds
Remote tone for alarms on other beds in network
Tone for Timer expired
Trends Resolution 12, 16, 24 or 32 numerics @ 12 sec, 1 minute, 5 minute
resolution
Information Multiple choices of number of numerics, resolution and
duration depending on trend option and application area.
For example:
neonatal extended 12 numerics, 24 hours @ 12 secs or
32 numerics 32 hours @ 1 minute
intensive care extended: 16 numerics 120 hours @ 5 minutes
anesthesia extended 32 numerics 9 hours @ 12 seconds
High Res Trend Waves Measurements available HR, SpO2, Resp, tcpO2, Pulse, Perf, tcpO2, CO2, ABP, PAP,
CVP, ICP, CPP, BIS, CCO, AWP, Anesthetic Agents, Delta
SpO2, inO2
Resolution Measurement samples are taken at a resolution of four samples
per second
Update speed waves are drawn at a speed of 3 cm/minute
Events Information trigger condition and time, event classification and associated
detailed view of episode data
Episode data configurable, either:
4 minutes of high resolution trend or
20 minutes of numerics trend @ 12 sec. resolution or
15 seconds of 4 waves @ 125 samples/sec. (Snapshot)
including all current numerics, alarms and inops
Capacity (max.) 25 or 50 events for either 8 or 24 hours
Alarm Signal System delay less than 3 seconds
Pause duration 1,2,3 minutes or infinite, depending on configuration
Extended alarm pause 5 or 10 minutes
Review Alarms Information all alarms / inops, main alarms on/off, alarm silence and time
of occurrence
Capacity 300 items
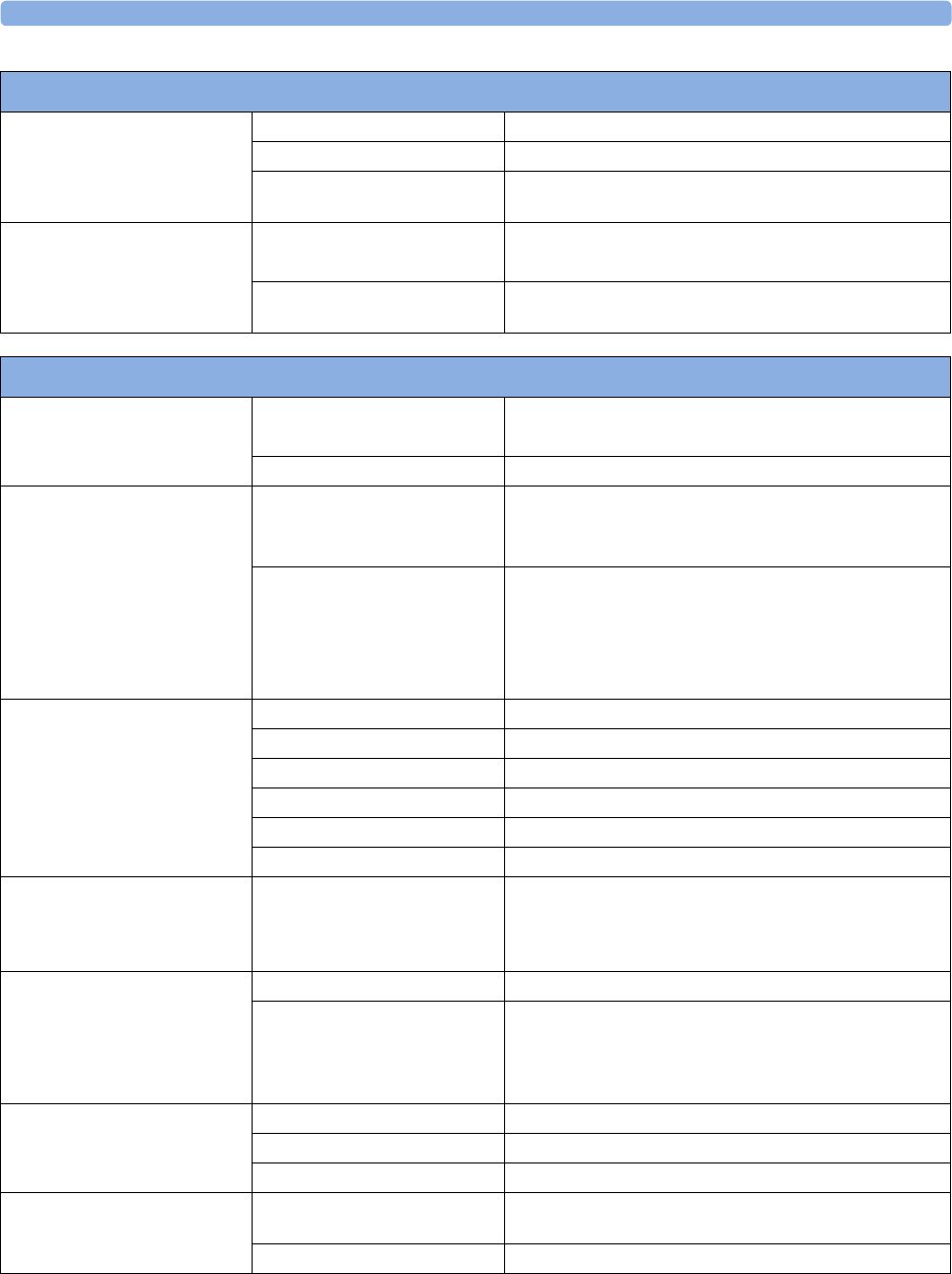
36 Specifications
402
Real Time Clock Range from: January 1, 1997, 00:00 to: December 31, 2080, 23:59
Accuracy better than 4 seconds per day
Hold Time infinite if powered by AC; otherwise at least 48 hours (typical:
>72 hours)
Buffered Memory Hold Time if powered by AC: infinite
without power: at least 8 hours
Contents Active settings, trends, patient data, realtime reports, events,
review alarms
MX600/700/800 Performance Specifications
X2 (M3002A) Performance Specifications
Power Specifications Power consumption <12 W average
<30 W while battery is loading
Operating Voltage 36 to 60 V DC floating
Battery Specifications Operating Time
(with new, fully charged battery at
25°C)
Basic monitoring configuration: 2.5 hours
(Brightness set to optimum, ECG/Resp, SpO2 measurements
in use, NBP measurement every 15 minutes)
Charge Time When X2 is off: 2 hours
When X2 is in use, and connected to a monitor, without
extensions: 12 hours approx.
When X2 is in use, and connected to the external power supply
(M8023A), without extensions: 12 hours approx.
Indicators Alarms Off red (crossed-out alarm symbol) LED
Alarms red/yellow/light blue (cyan) LED
On/Standby / Error green / red LED
AC Power green LED
Battery yellow (charging)/red blinking (empty) LED
External Power green LED
Sounds Audible feedback for user input
Prompt tone
QRS tone, or SpO2 modulation tone
4 different alarm sounds
Trends Resolution 12 or 16 numerics @ 12 sec, 1 minute, 5 minute resolution.
Information Multiple choices of number of numerics, resolution and
duration depending on trend option and application area.
For example:
For neonatal, you can choose between 12 and 16 numerics.
Alarm signal System delay less than 3 seconds
Pause duration 1,2,3 minutes or infinite, depending on configuration
Extended alarm pause 5 or 10 minutes
Review Alarms Information all alarms / inops, main alarms on/off, alarm silence and time
of occurrence
Capacity 300 items
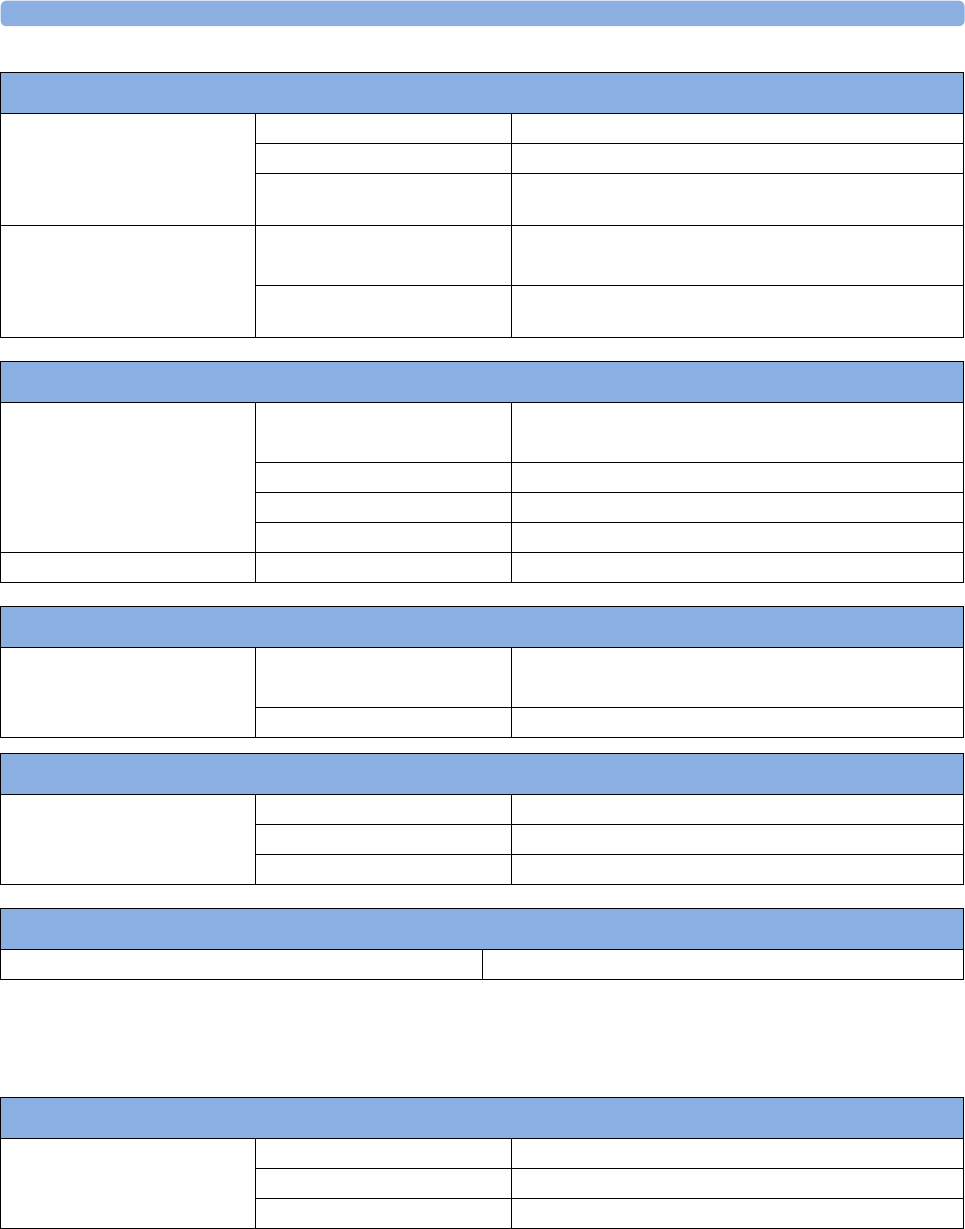
36 Specifications
403
Interface Specifications
Real Time Clock Range from: January 1, 1997, 00:00 to: December 31, 2080, 23:59
Accuracy <4 seconds per day (typically)
Hold Time infinite if powered by host monitor or external power supply;
otherwise at least 48 hours
Buffered Memory Hold Time if powered by host monitor or external power supply: infinite
without power: at least 48 hours (typical: >72 hours)
Contents Active settings, trends, patient data, realtime reports, review
alarms
X2 (M3002A) Performance Specifications
M8023A External Power Supply (for M3002A) Performance Specifications
Power Specifications Power consumption <12 W average
<30 W peak
Line Voltage 100 to 240 V ~
Current 1.3 to 0.7 A
Frequency 50/60 Hz ~
Indicators Power green LED
M3001A MMS Performance Specifications
Trends Trend Data Buffered Memory if powered by monitor mains connection via MSL: infinite
without power applied: at least 6 hours
Contents trend data, patient identification and all active settings
Integrated PC (iPC) Performance Specifications
PC Components Processor Intel Core 2 Duo SP9300/SP9400
Solid-state drive 100 GB or above
RAM 4 GB
865244 Remote Control Performance Specifications
Power (when not connected to the USB interface of the monitor) Two AA primary cells
MX600/700/800 Interface Specifications
Network Standard 100-Base-TX (IEEE 802.3 Clause 25)
Connector RJ45 (8 pin)
Isolation basic insulation (reference voltage: 250 V; test voltage: 1500 V)
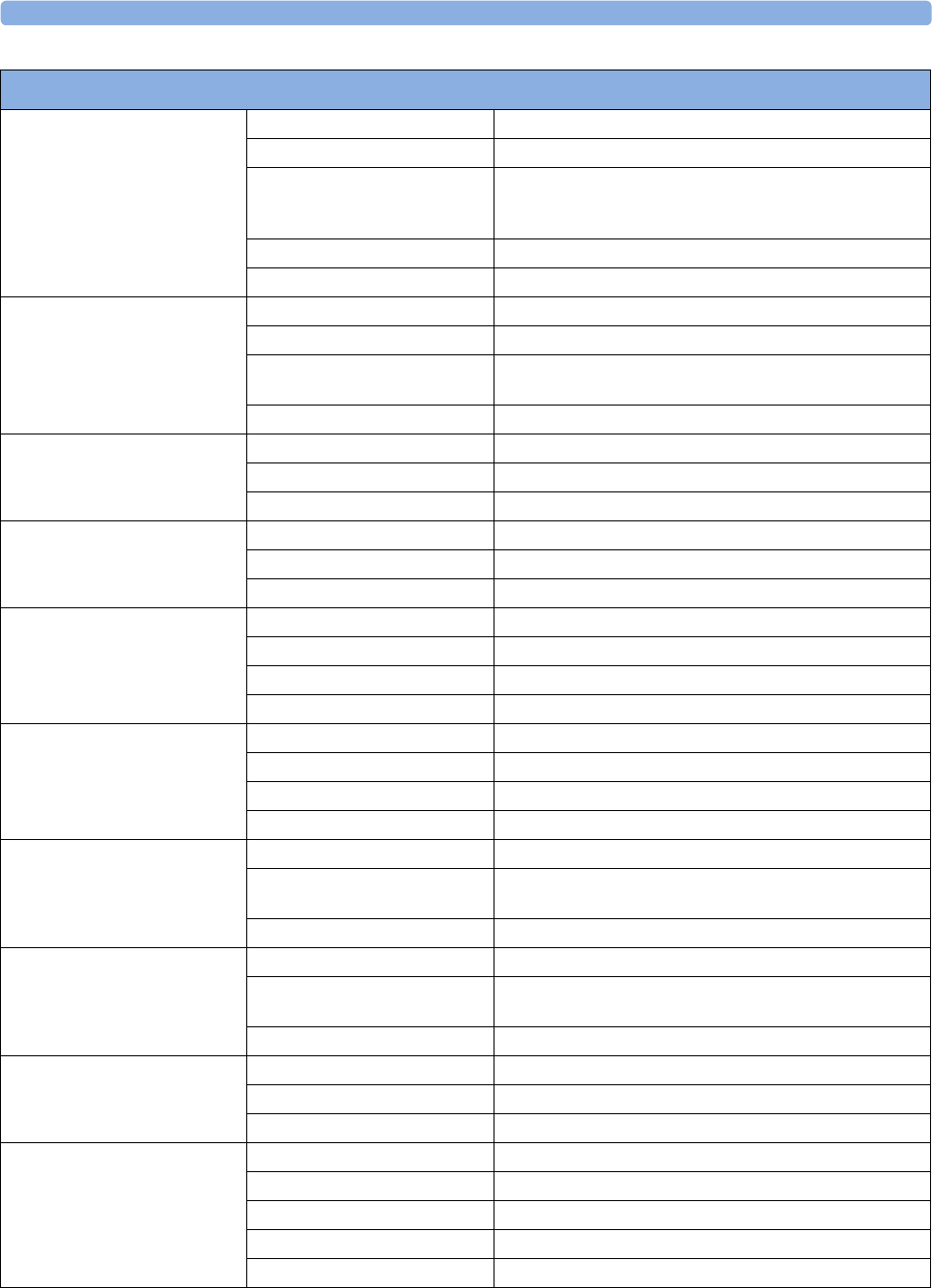
36 Specifications
404
MIB/RS232 Standard IEEE 1073-3.2-2000
Connectors RJ45 (8 pin)
Mode Software-controllable
BCC (RxD/TxD cross over) or
DCC (RxD/TxD straight through)
Power 5 V ±5 %, 100 mA (max.)
Isolation basic insulation (reference voltage: 250 V; test voltage: 1500 V)
USB Interface (4 ports) Standard USB 2.0 full-speed (embedded host)
Connector USB series "Standard A" receptacle
Power Low power port 4.4V min; max. load for all ports together
500 mA
Isolation none
RS232 (Standard) Connector RJ45 (8-pin)
Power none
Isolation basic insulation (reference voltage: 250 V; test voltage: 1500 V)
RS232 (Independent display
interface option)
Connector RJ45 (8-pin)
Power none
Isolation none
Basic Nurse Call Relay Connector modular Jack 6P6C, active open and closed contact
Contact <=100 mA, <=24 V DC
Isolation basic insulation (reference voltage: 250 V; test voltage: 1500 V)
Delay <[Configured Latency +0.5] sec
Flexible Nurse Call Relay Connector 20 pin MDR (Mini D-Ribbon), active open and closed contacts
Contact <=100 mA, <=24 V DC
Isolation basic insulation (reference voltage: 250 V; test voltage: 1500 V)
Delay <[Configured Latency +0.5] sec
IntelliVue Instrument
Telemetry Wireless Network
(USA only)
Type Internal WMTS Adapter
Technology compatible with Philips IntelliVue Telemetry System (ITS),
cellular infrastructure
Frequency Band WMTS, 1395-1400 MHz and 1427-1432 MHz
IntelliVue Instrument
Telemetry Wireless Network
(except USA)
Type Internal ISM Adapter
Technology compatible with Philips IntelliVue Telemetry System (ITS),
cellular infrastructure
Frequency Band 2.4 GHz ISM
IntelliVue 802.11 Bedside
Adapter (Wireless Network
Adapter)
Type Internal Wireless Adapter
Technology IEEE 802.11a/b/g
Frequency Band 2.4GHz and 5GHz ISM Band
Short Range Radio Interface Type Internal SRR interface
Technology IEEE 802.15.4
Frequency band 2.4 GHz ISM (2.400 - 2.483 GHz)
Modulation technique DSSS (O -QPSK)
Effective radiated power max. 0 dBm (1 mW)
MX600/700/800 Interface Specifications
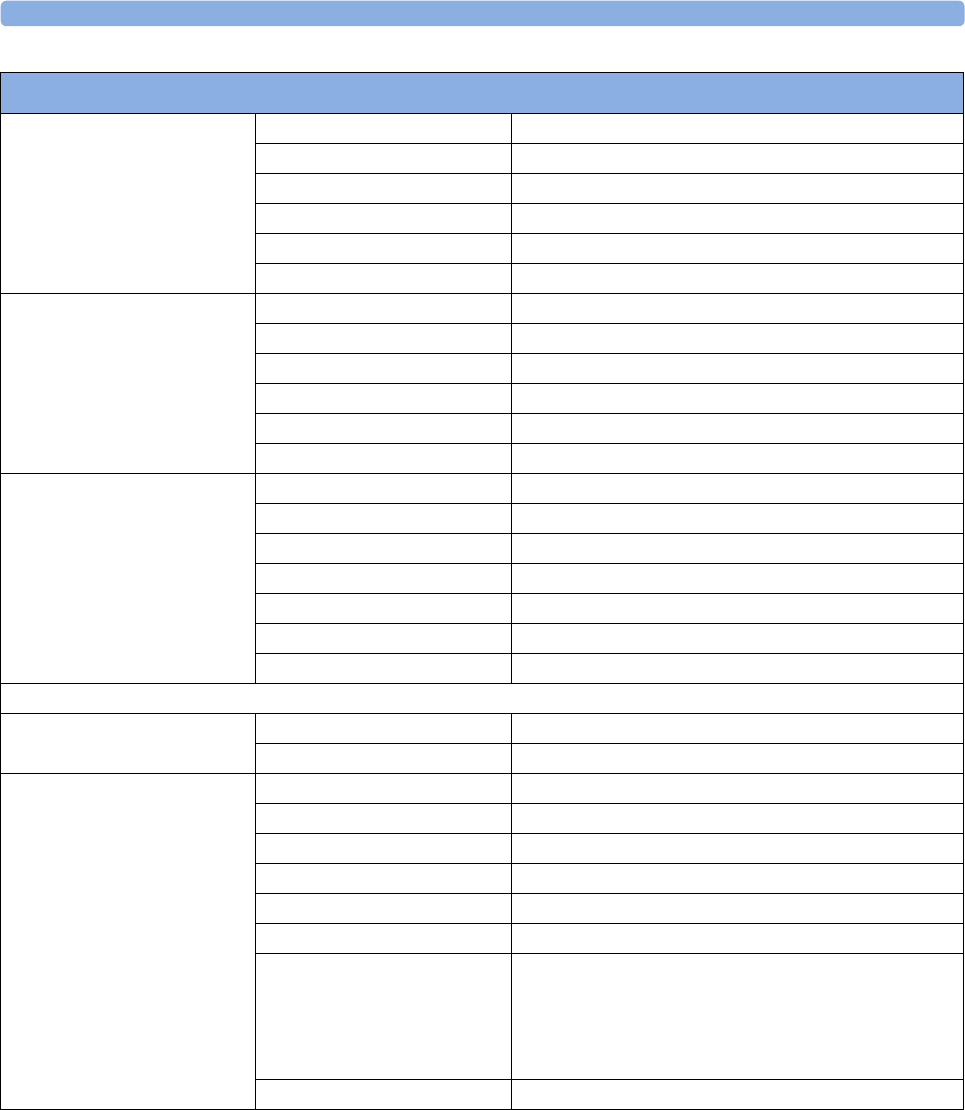
36 Specifications
405
Measurement Link (MSL) Connectors ODU out (Proprietary)
Voltage 56 V ±10 %
Power 45 W
Power Sync. 5 V CMOS Level; 78.125 kHz (typ.)
LAN signals IEEE 802.3 10-Base-T compliant
Serial signals RS-422 compliant
Video Interface (standard) Connector DVI (digital and analog, single link)
Digital video signals single link TMDS
Analog video signals 0.7 Vpp@75 Ohm
HSYNC/VSYNC signals TTL
DDC signals none
DDC power 5 V +/-5% @0-55 mA
Video Interface (Independent
display interface option)
Connector DVI (digital and analog, single link)
Pixel clock frequency 31,5 MHz - 119 MHz
Digital video signals single link TMDS
Analog video signals 0.7 Vpp@75 Ohm
HSYNC/VSYNC signals TTL
DDC signals none
DDC power 5 V +/-5% @0-55 mA
ECG Sync Output/Analog ECG Output (1/4" stereo phone jack with tip, ring, sleeve)
General Connector 1/4" phone with tip, ring, sleeve
Isolation functional isolation
Analog ECG Output
(ring, tip)
Full scale on display signal gain x measured ECG voltage
Gain error <15 %
Baseline offset <100 mV
Bandwidth 1 to 100 Hz
Output voltage swing ±4 V (min)
Signal delay <22 ms
Signal delay with older versions of
the M3001A MMS
[identifiable with the serial number
prefix DE227 or DE441 and
option string #A01]
<30 ms
Pacemaker Pulse filtered and included in ECG output signal
MX600/700/800 Interface Specifications
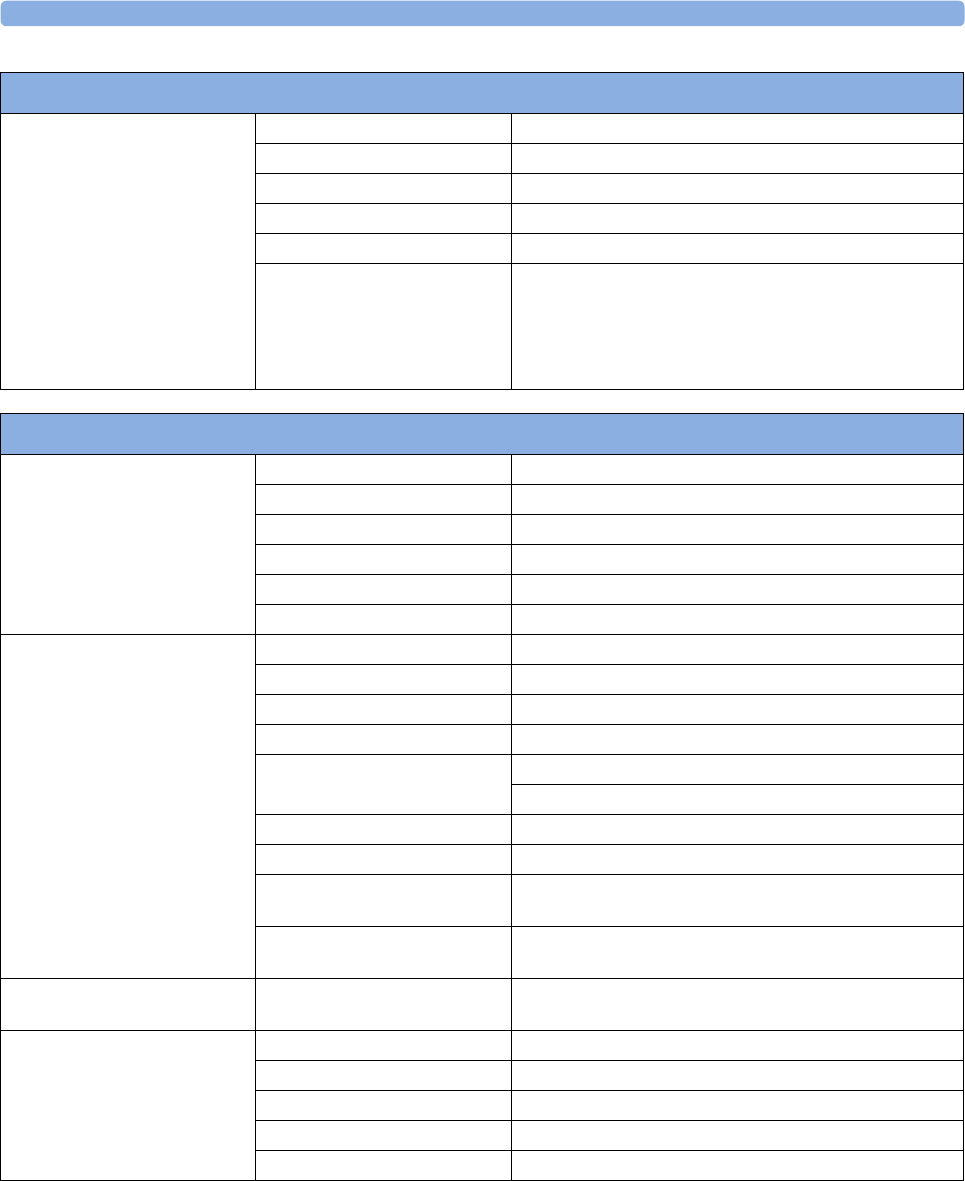
36 Specifications
406
1 The short range radio interface is compatible with the following telemetry devices: TRx4841A/TRx4851A Intellivue
Telemetry System Transceiver
Digital Pulse Output
(ring)
Output low voltage level <0.4 V @ I=-1 mA
Output high voltage level >2.4 V @ I=1 mA
Pulse Width 100 ms±10 ms (active high)
Pulse Rise Time <1 ms (from 0.4 V to 2.4 V)
Signal delay < 25ms per AAMI EC13
Signal delay with older versions of
the M3001A MMS
[identifiable with the serial number
prefix DE227 or DE441 and
option string #A01]
< 35ms per AAMI EC13
MX600/700/800 Interface Specifications
X2 (M3002A) Interface Specifications
Measurement Link (MSL) Connectors Female ODU (Proprietary)
Power 30 V to 60 V input
Power Sync. RS-422 compliant input 78.125 kHz (typical)
LAN signals IEEE 802.3 10-Base-T compliant
Serial signals RS-422 compliant
Local signals Provided for connecting MMS extensions
ECG Sync Pulse Output
(rectangular pulse)
Cable detection Yes
Marker In No
Wave Output No
Connector Binder Series 709/719
Output levels Output low <0.8 V @ I = -4 mA
Output high >2.4 V @ I = 4 mA
Isolation None
Pulse Width 100 +/- 10 ms (high)
Delay from R-wave peak to start of
pulse
20 ms maximum per AAMI EC13
Minimum required R-wave
amplitude
0.5 V
Wireless Network Device
Interface
Signals RD+/-, TD+/-: IEEE 802.3 10Base-T, PWR, GND
12.5 V ±20%, 3.5 W continuous
Short Range Radio Interface1Type Internal SRR interface
Technology IEEE 802.15.4
Frequency Band 2.4 GHz ISM (2.400 - 2.483 GHz)
Modulation Technique DSSS (O -QPSK)
Effective radiated power max. 0 dBm (1 mW)
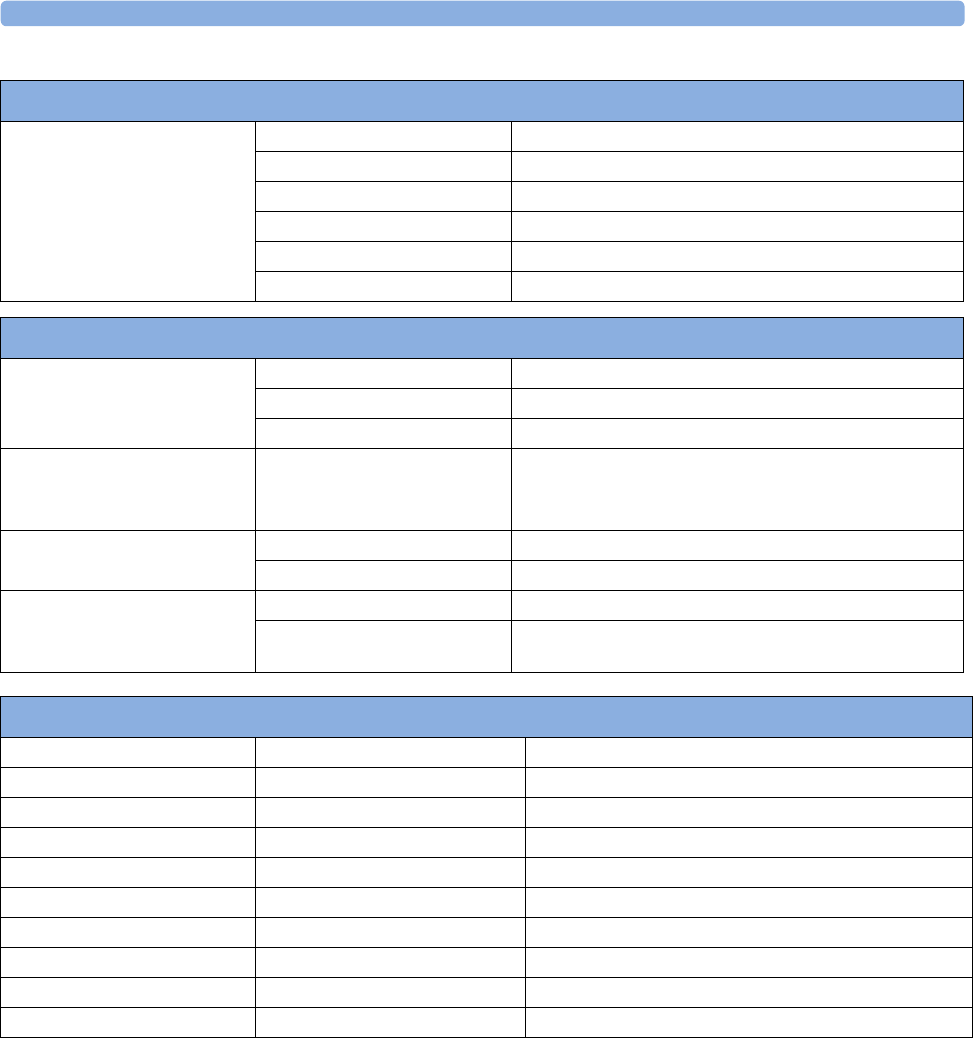
36 Specifications
407
Measurement Specifications
See the Appendix on Default Settings for a list of the settings the monitor is initially shipped with.
ECG/Arrhythmia/ST/QT
Complies with IEC 60601-2-25:1993 + A1:1999 /EN60601-2-25:1995 + A1:1999, IEC 60601-2-
27:2005/EN60601-2-27:2006, IEC 60601-2-51:2003 /EN 60601-2-51:2003 and AAMI EC11/
EC13:1991/2002.
M8023A External Power Supply (for M3002A) Interface Specifications
Measurement Link (MSL) Connectors Male ODU (Proprietary)
Power 48 V output
Power Sync. RS-422 compliant output 78.125 kHz (typical)
LAN signals IEEE 802.3 10-Base-T compliant
Serial signals RS-422 compliant output 78.125 kHz (typical)
Local signals Not connected
Integrated PC (iPC) Interface Specifications
Ethernet LAN (external) Connector RJ-45
LAN Signals IEE 802.3 1000-Base-T compliant
Reinforced insulation IEC60601-1 A-k compliant
USB 6 external ports (5 rear, 1 right
side)
Type A connectors
USB 2.0 supporting high speed mode
Audio microphone input stereo 3.5 mm audio jack
headphone output stereo 3.5 mm audio jack
DVI Video with DVI-I
connector
DVI supports resolutions up to 1920x1200
VGA supports resolutions up to 2048x1536
Display Specifications
19" WSXGA+ Type 482 mm active matrix color LCD (TFT)
Resolution 1680 x 1050 (WSXGA+)
Refresh frequency 58 Hz
Useful screen 409,5 mm x 255.9 mm
Pixel size 0.244 mm x 0.244 mm
15" WXGA Type 389 mm active matrix color LCD (TFT)
Resolution 1280 x 768 (WXGA)
Refresh frequency 59.9 Hz
Useful screen 334.1 mm x 200.5 mm
Pixel size 0.261 mm x 0.261 mm
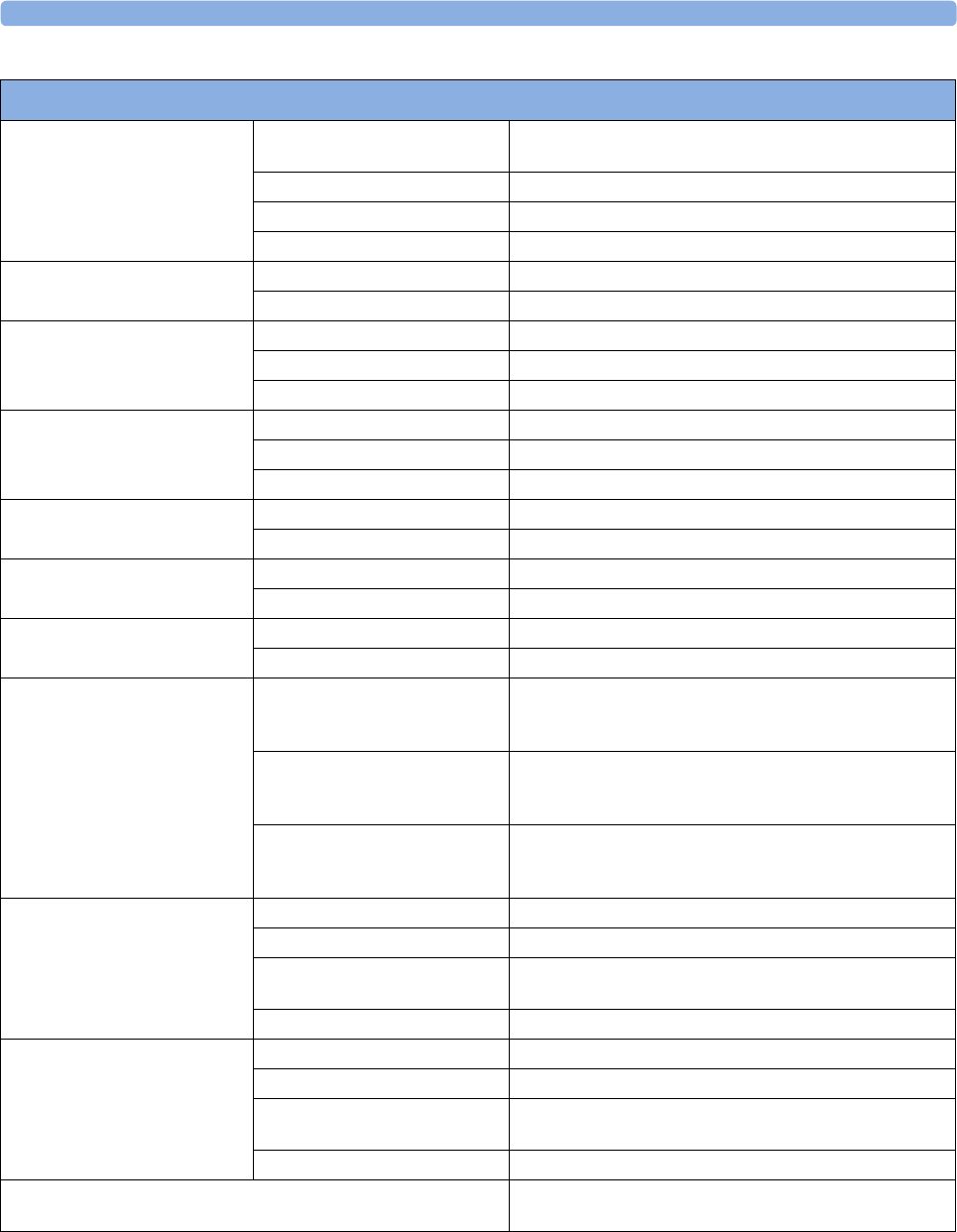
36 Specifications
408
ECG/Arrhythmia/ST Performance Specifications
Cardiotach Range Adult/pedi: 15 to 300 bpm
Neo range: 15 to 350 bpm
Accuracy ±1% of range
Resolution 1 bpm
Sensitivity ≥200 µVpeak
PVC Rate Range 0 to 300 bpm
Resolution 1 bpm
ST Numeric Range -20 to +20 mm
Accuracy ±0.5 mm or 15%, whichever is greater
Resolution 0.1 mm
QT Numeric Range 200 to 800 ms
Accuracy ±30 ms
Resolution 8 ms
QTc Numeric Range 200 to 800 ms
Resolution 1 ms
ΔQTc Numeric Range -600 to +600 ms
Resolution 1 ms
QT-HR Numeric Range - adult 15 to 300 bpm
Range - pediatric and neonatal 15 to 350 bpm
Sinus and SV Rhythm Ranges Brady Adult: 15 to 59 bpm
Pedi: 15 to 79 bpm
Neo: 15 to 89 bpm
Normal Adult: 60 to 100 bpm
Pedi: 80 to 160 bpm
Neo: 90 to 180 bpm
Tachy Adult: >100 bpm
Pedi: >160 bpm
Neo: >180 bpm
Bandwidth Diagnostic Mode Adult/neo/pedi: 0.05 to 150 Hz
Extended Monitoring Mode Adult/neo/pedi: 0.5 to 150 Hz
Monitoring Mode Adult: 0.5 to 40 Hz
Neo/pedi: 0.5 to 55 Hz
Filter Mode Adult/neo/pedi: 0.5 to 20 Hz
Bandwidth
when the ECG is transmitted from
a telemetry device via short range
radio
Diagnostic Mode Adult/neo/pedi: 0.05 to 40 Hz
Extended Monitoring Mode Adult/neo/pedi: 0.5 to 40 Hz
Monitoring Mode Adult: 0.5 to 40 Hz
Neo/pedi: 0.5 to 40 Hz
Filter Mode Adult/neo/pedi: 0.5 to 20 Hz
Differential Input Impedance >2 MΩ RA-LL leads (Resp)
>5 MΩ at all other leads (at 10 Hz including patient cable)
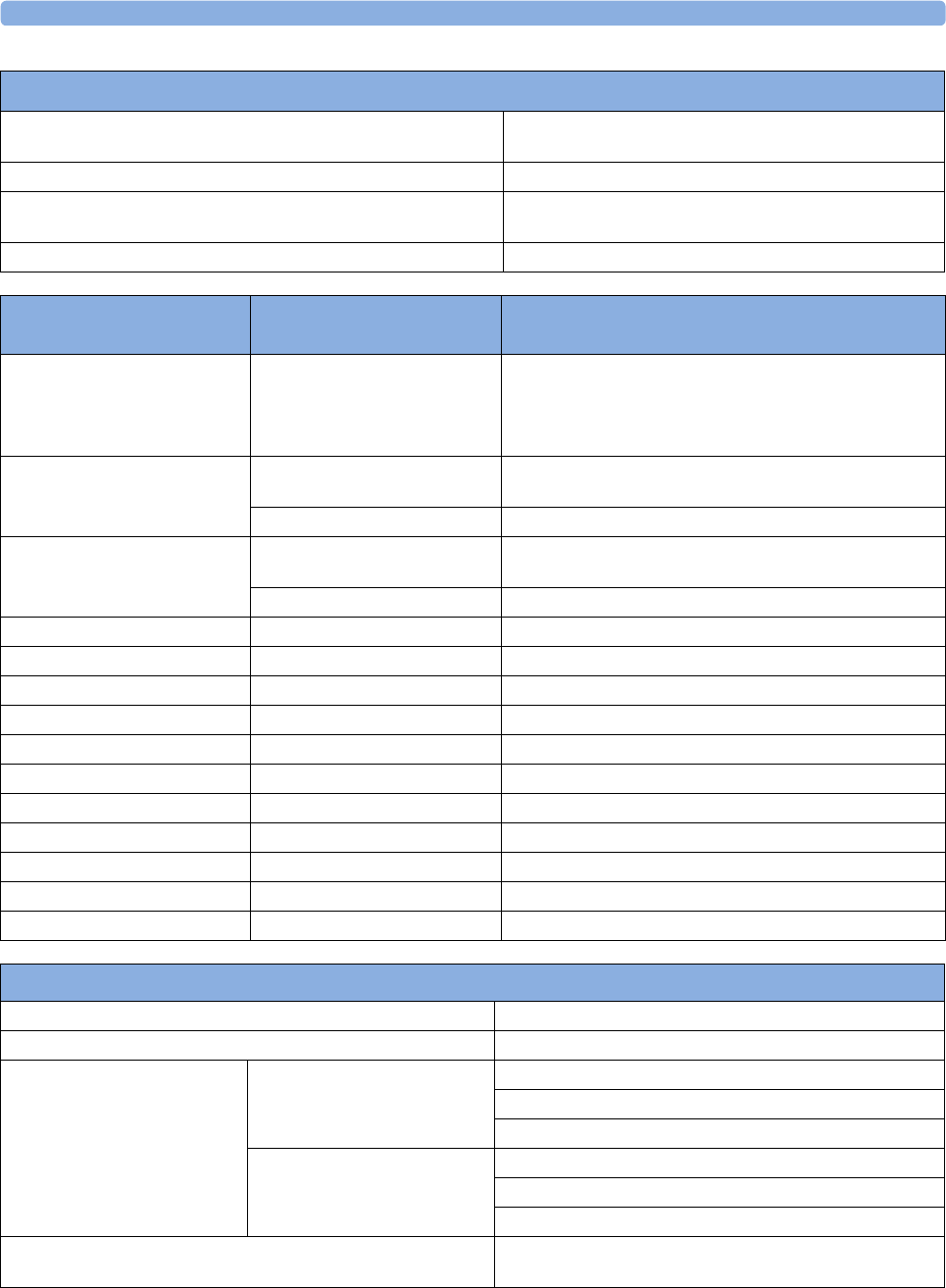
36 Specifications
409
Common Mode Rejection Ratio Diagnostic mode: >86 dB (with a 51 kΩ/47 nF imbalance).
Filter mode: >106 dB (with a 51 kΩ/47 nF imbalance).
Electrode Offset Potential Tolerance ±500 mV
Auxiliary Current
(Leads off Detection)
Active electrode: <100 nA
Reference electrode: <900 nA
Input Signal Range ±5 mV
ECG/Arrhythmia/ST Performance Specifications
ECG/Arrhythmia/ST/QT
Alarm Specifications Range Adjustment
HR 15 to 300 bpm
maximum delay: 10 seconds
according to AAMI EC 13-1992
standard
Adult:1 bpm steps (15 to 40 bpm)
5 bpm steps (40 to 300 bpm)
Pedi/Neo:1 bpm steps (15 to 50 bpm)
5 bpm steps (50 to 300 bpm)
Extreme Tachy Difference to high limit 0 to
50 bpm
5bpm steps
Clamping at 150 to 300 bpm 5 bpm steps
Extreme Brady Difference to low limit 0 to
50 bpm
5bpm steps
Clamping at 15 to 100 bpm 5 bpm steps
Run PVCs None, fixed setting 2 PVCs Not adjustable by user
PVCs Rate 1 to 99 PVCs/minute 1 PVC
Vent Tach HR 20 to 300 bpm 5 bpm
Vent Tach Run 3 to 99 PVCs/minute 1 PVC
Vent Rhythm Run 3 to 99 PVCs/minute 1 PVC
SVT HR 120 to 300 bpm 5 bpm
SVT Run 3 to 99 SV beats 1 SV beat
ST High -19.8 to +20 mm 0.2 mm
ST Low -20 to +19.8 mm 0.2 mm
QTc High 200 ms to 800 ms 10 ms steps
ΔQTc High 30 ms to 200 ms 10 ms steps
ECG/Arrhythmia/ST Supplemental Information as required by AAMI EC11/13, IEC 60601-2-27
Respiration Excitation Waveform Sinusoidal signal, 260 μA, 40.5 kHz
Noise Suppression RL drive gain 44 dB max., max. voltage 1.8 Vrms
Time to Alarm for Tachycardia Vent Tachycardia
1mV
pp,206 bpm
Gain 0.5, Range 6.5 to 8.4 seconds, Average 7.2 seconds
Gain 1.0 Range 6.1 to 6.9 seconds, Average 6.5 seconds
Gain 2.0, Range 5.9 to 6.7 seconds, Average 6.3 seconds
Vent Tachycardia
2mV
pp,195 bpm
Gain 0.5, Range 5.4 to 6.2 seconds, Average 5.8 seconds
Gain 1.0, Range 5.7 to 6.5 seconds, Average 6.1 seconds
Gain 2.0, Range 5.3 to 6.1 seconds, Average 5.7 seconds
Tall T-Wave Rejection Capability Exceeds ANSI/AAMI EC 13 Sect. 3.1.2.1(c) minimum
recommended 1.2 mV T-Wave amplitude
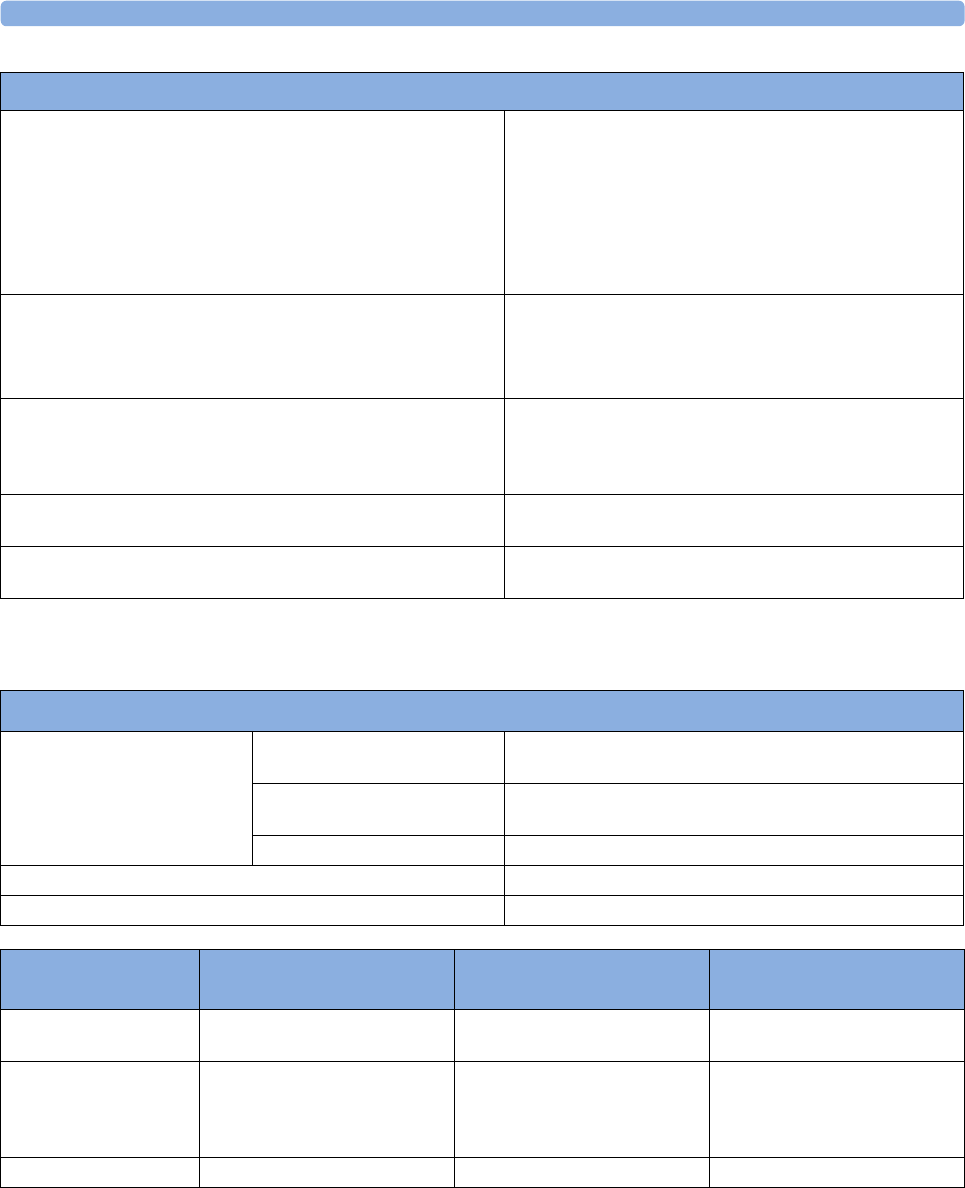
36 Specifications
410
Respiration
Heart Rate Averaging Method Three different methods are used:
Normally, heart rate is computed by averaging the 12 most
recent RR intervals.
For runs of PVCs, up to 8 RR intervals are averaged to compute
the HR.
If each of 3 consecutive RR intervals is greater than 1200 ms
(that is, rate less than 50 bpm), then the 4 most recent RR
intervals are aver\-aged to compute the HR.
Response Time of Heart Rate Meter to Change in Heart Rate HR change from 80 to 120 bpm:
Range: [6.4 to 7.2 seconds] Average: 6.8 seconds
HR change from 80 to 40 bpm:
Range: [5.6 to 6.4 sec] Average: 6.0 seconds
Heart Rate Meter Accuracy and Response to Irregular Rhythm Ventricular bigeminy: 80 bpm
Slow alternating ventricular bigeminy: 60 bpm
Rapid alternating ventricular bigeminy: 120 bpm
Bidirectional systoles: 90 bpm
Accuracy of Input Signal Reproduction Methods A and D were used to establish overall system error
and frequency response.
Pacemaker Pulse Rejection Performance Rejection of pacemaker pulses with amplitudes from ±2 mV to
±700 mV and widths from 0.1 ms to 2.0 ms (Method A)
ECG/Arrhythmia/ST Supplemental Information as required by AAMI EC11/13, IEC 60601-2-27
Respiration Performance Specifications
Respiration Rate Range Adult/pedi: 0 to 120 rpm
Neo: 0 to 170 rpm
Accuracy at 0 to 120 rpm ±1 rpm
at 120 to 170 rpm ±2 rpm
Resolution 1 rpm
Bandwidth 0.3 to 2.5 Hz (-6 dB)
Noise Less than 25 mΩ (rms) referred to the input
Respiration Alarm
Specifications Range Adjustment Delay
High Adult/pedi: 10 to 100 rpm
Neo: 30 to 150 rpm
under 20 rpm: 1 rpm steps
over 20 rpm: 5 rpm steps
max. 14 seconds
Low Adult/pedi: 0 to 95 rpm
Neo: 0 to 145 rpm
under 20 rpm: 1 rpm steps
over 20 rpm: 5 rpm steps
for limits from 0 to 20 rpm:
max. 4 seconds
for limits above 20 rpm: max.
14 seconds
Apnea Alarm 10 to 40 seconds 5 second steps

36 Specifications
411
SpO2
Unless otherwise specified, this information is valid for SpO2 measured using the M3001A and
M3002A Multi-measurement modules and the M1020B measurement module. The SpO2 Performance
Specifications in this section apply to devices with Philips SpO2 technology. For SpO2 Performance
Specifications valid for other SpO2 technologies, refer to the instructions for use provided with these
devices.
Complies with ISO 9919:2005 / EN ISO 9919:2009 (except alarm system; alarm system complies with
IEC 60601-2-49:2001).
Measurement Validation: The SpO2 accuracy has been validated in human studies against arterial
blood sample reference measured with a CO-oximeter. Pulse oximeter measurements are statistically
distributed, only about two-thirds of the measurements can be expected to fall within the specified
accuracy compared to CO-oximeter measurements.
Display Update Period: Typical: 2 seconds, Maximum: 30 seconds. Maximum with NBP INOP
suppression on: 60 seconds.
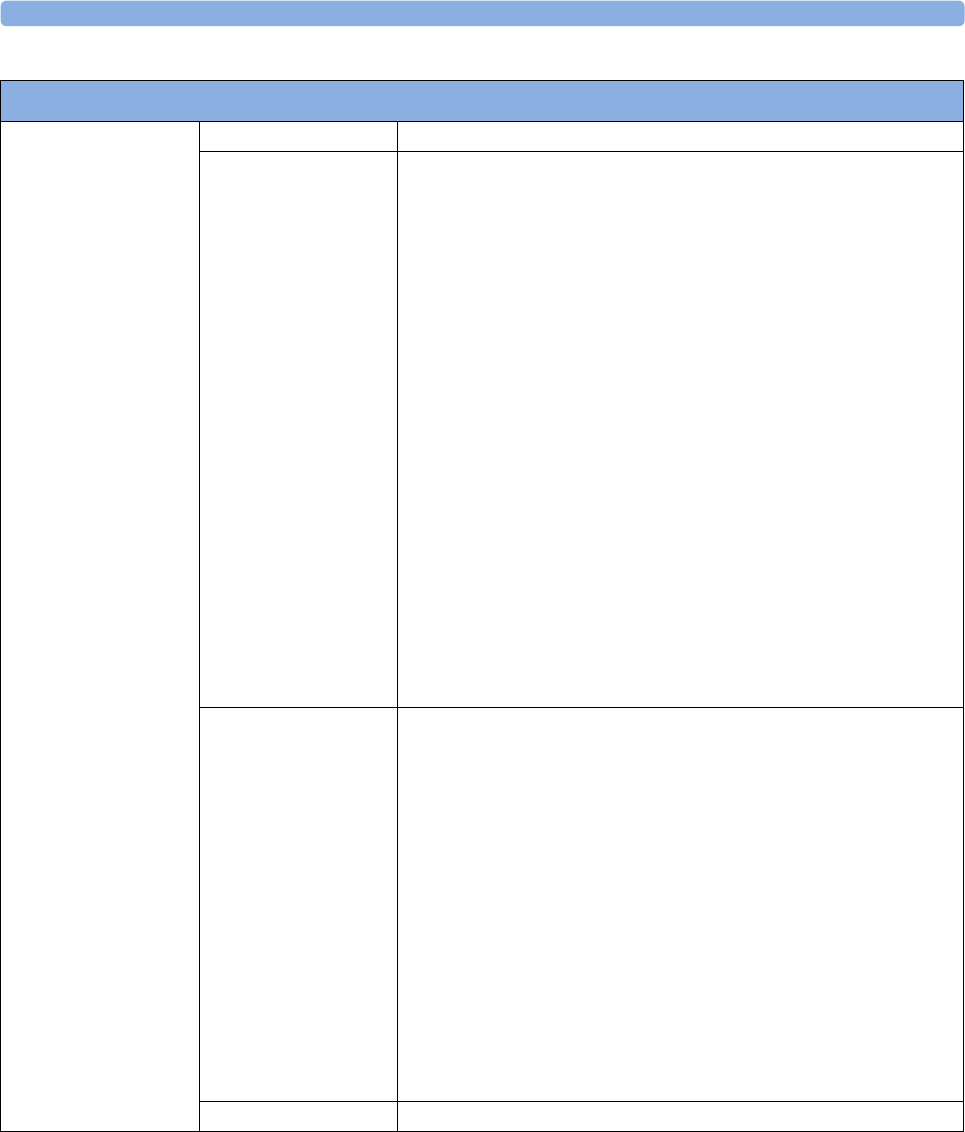
36 Specifications
412
SpO2 Performance Specifications
SpO2
The specified accuracy is
the root-mean-square
(RMS) difference between
the measured values and
the reference values
Range 0 to 100%
Option #A01
Accuracy
Philips Reusable Sensors:
M1191A, M1191AL, M1191B, M1191BL, M1192A, = 2 % (70 % to 100 %)
M1193A, M1194A, M1195A, M1196A = 3 % (70 % to 100 %)
M1191T, M1192T, M1193T (Adult), M1196T = 3% (70% to 100%)
M1193T (Neonate) = 4 % (70 % to 100 %)
Philips Disposable Sensors with M1943A(L):
M1132A, M1133A (adult/infant), M1134A (adult/infant) = 2 %
M1901B, M1902B, M1903B, M1904B, M1131A, M1133A (neonate), M1134A
(neonate) = 3 % (70 % to 100 %)
NellcorPB® Sensors with M1943A(L):
MAX-A, MAX-AL, MAX-P, MAX-I, MAX-N, D-25, D-20, I-20, N-25, OxiCliq
A, P, I, N = 3 % (70 % to 100 %)
Masimo Reusable Sensors® with LNOP MP12 or LNC MP10:
LNOP DC-I, LNOP DC-IP, LNOP YI (adult/pedi/infant), LNCS DC-1,
LNCS DC-IP, LNCS YI (adult/pedi/infant) = 2% (70% to 100%)
LNOP YI (neonate), LNCS YI (neonate) = 3% (70% to 100%)
LNOP TC-I, LNCS TC-I: 3.5 % (70 % to 100 %)
Masimo Disposable Sensors® with LNOP MP12 or LNC MP10:
LNOP DC-I, LNOP DC-IP, LNOP YI (adult/pedi/infant, LNCS DC-1, LNCS
DC-IP, LNCS YI (adult/pedi/infant) = 2% (70% to 100%)
LNOP Neo-L, LNOP NeoPt-L, LNCS Neo-L, LNCS NeoPt-L: 3 % (70 % to
100 %)
Option #A02
Accuracy
Philips Reusable Sensors
M1193AN = 3 % (70 % to 100 %)
Philips Disposable Sensors with M1943NL:
M1901B (Adult), M1902B, M1903B, M1904B = 2 % (70 % to 100 %)
M1901B (Neonate) = 3 %
NellcorPB® Sensors with M1943NL:
MAX-FAST, MAX-A, MAX-AL, MAX-P, MAX-I, MAX-N (Adult) = 2 %
(70 % to 100 %)
SC-A, OxiCliq A, P, I, N (Adult) = 2.5 % (70 % to 100 %)
MAX-N (Neonate), Dura-Y D-YS (Infant to Adult), DS-100A,Oxiband OXI-
A/N (Adult), OXI-P/I = 3 % (70 % to 100 %)
MAX-R, OxiCliq N (Neonate), SC-NEO (Neonate), SC-PR (Neonate), Dura-Y
D-YS with D-YSE or D-YSPD clip = 3.5 % (70 % to 100 %)
Dura-Y D-YS (Neonate), Oxiband OXI-A/N (Neonate) = 4 % (70 % to
100 %)
Resolution 1%
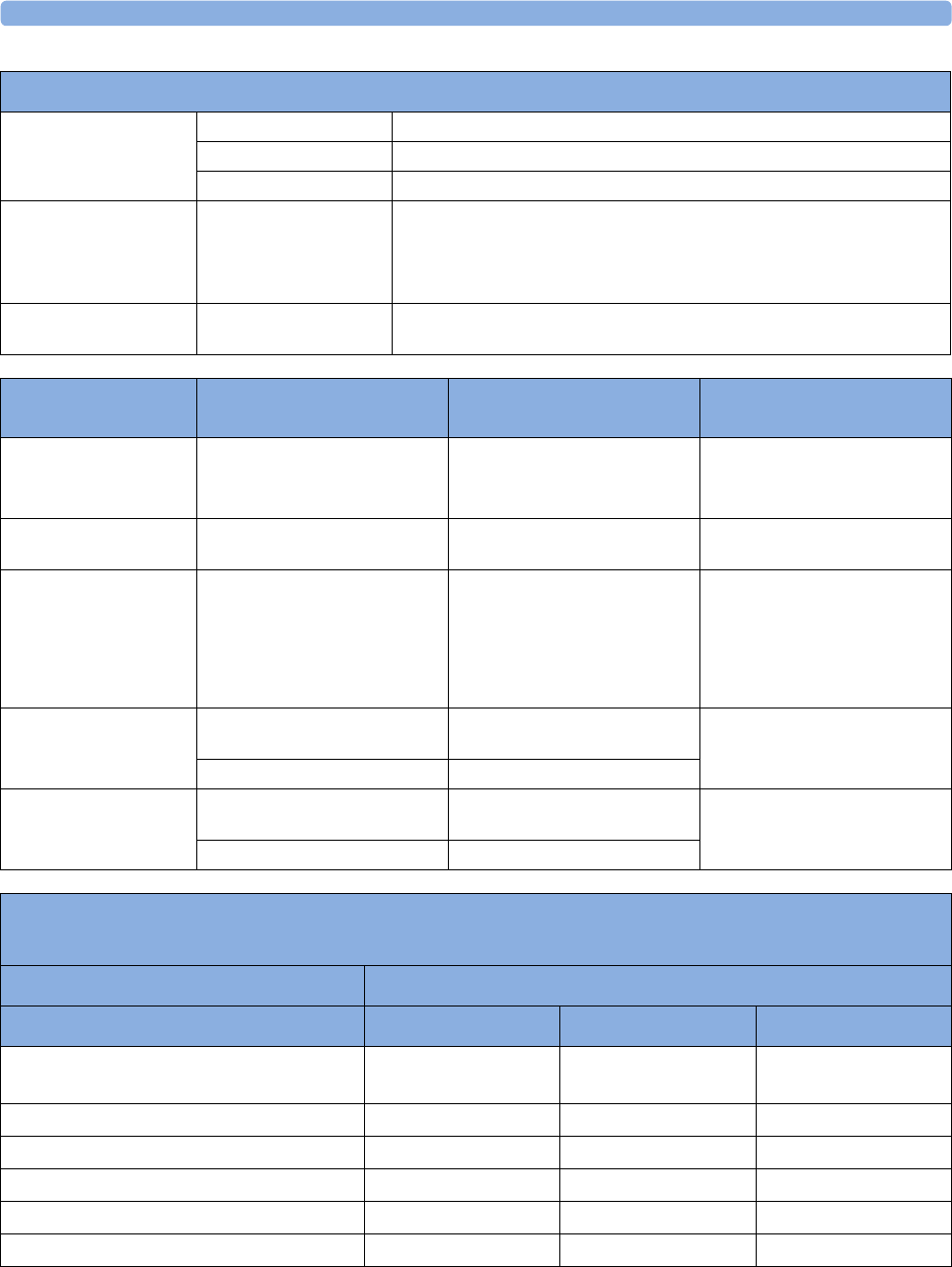
36 Specifications
413
Pulse Range 30 to 300 bpm
Accuracy ±2% or 1 bpm, whichever is greater
Resolution 1 bpm
Sensors Wavelength range: 500 to 1000 nm
Emitted Light Energy: ≤15 mW
Information about the wavelength range can be especially useful to clinicians
(for instance, when photodynamic therapy is performed)
Pulse Oximeter
Calibration Range
70% to 100%
SpO2 Performance Specifications
SpO2 Alarm
Specifications Range Adjustment Delay
SpO2Adult: 50 to 100%
Pedi/Neo: 30 to 100%
1% steps (0, 1, 2, 3,... 30) +4 seconds
or Smart Alarm Delay (see table
below)
Desat Adult: 50 to Low alarm limit
Pedi/Neo: 30 to Low alarm limit
1% steps (0, 1, 2, 3,... 30) +4 seconds
Pulse 30 to 300 bpm Adult:
1 bpm steps (30 to 40 bpm)
5 bpm steps (40 to 300 bpm)
Pedi/Neo:
1 bpm steps (30 to 50 bpm)
5 bpm steps (50 to 300 bpm)
max. 14 seconds
Tachycardia Difference to high limit 0 to
50 bpm
5 bpm steps max. 14 seconds
Clamping at 150 to 300 bpm 5 bpm steps
Bradycardia Difference to low limit 0 to
50 bpm
5 bpm steps max. 14 seconds
Clamping at 30 to 100 bpm 5 bpm steps
SpO2 Smart Alarm Delay Specifications
The Smart Alarm Delay functionality is currently not available in the U.S.A. or in clinical environments under FDA control.
Deviation from violated alarm limit Resulting alarm delay
Short Medium Long
1% 25 sec
(maximum delay)
50 sec
(maximum delay)
100 sec
(maximum delay)
2% 12 sec 25 sec 50 sec
3% 10 sec 16 sec 33 sec
4% 10 sec 12 sec 25 sec
5% 10 sec 10 sec 20 sec
6% 10 sec 10 sec 16 sec
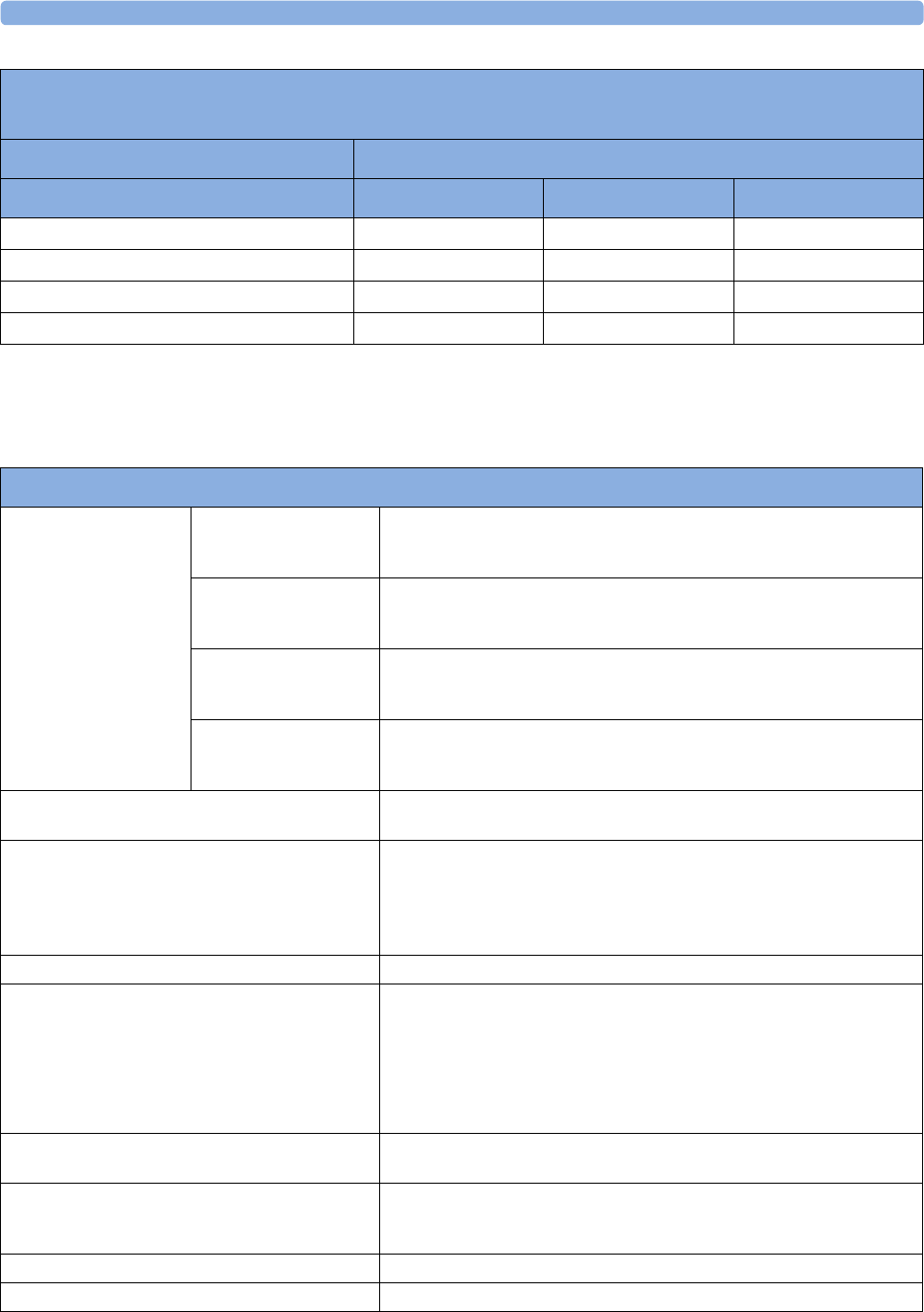
36 Specifications
414
NBP
Complies with IEC 60601-2-30:1999/EN60601-2-30:2000.
7% 10 sec 10 sec 14 sec
8% 10 sec 10 sec 12 sec
9% 10 sec 10 sec 11 sec
>9% 10 sec 10 sec 10 sec
SpO2 Smart Alarm Delay Specifications
The Smart Alarm Delay functionality is currently not available in the U.S.A. or in clinical environments under FDA control.
Deviation from violated alarm limit Resulting alarm delay
Short Medium Long
NBP Performance Specifications
Measurement Ranges Systolic Adult: 30 to 270 mmHg (4 to 36 kPa)
Pedi: 30 to 180 mmHg (4 to 24 kPa)
Neo: 30 to 130 mmHg (4 to 17 kPa)
Diastolic Adult: 10 to 245 mmHg (1.5 to 32 kPa)
Pedi: 10 to 150 mmHg (1.5 to 20 kPa)
Neo: 10 to 100 mmHg (1.5 to 13 kPa)
Mean Adult: 20 to 255 mmHg (2.5 to 34 kPa)
Pedi: 20 to 160 mmHg (2.5 to 21 kPa)
Neo: 20 to 120 mmHg (2.5 to 16 kPa)
Pulse Rate Adult: 40 to 300
Pedi: 40 to 300
Neo: 40 to 300
Accuracy Max. Std. Deviation: 8mmHg (1.1kPa)
Max. Mean Error: ±5 mmHg (±0.7 kPa)
Pulse Rate Measurement Accuracy 40 to 100 bpm: ±5 bpm
101 to 200 bpm: ±5% of reading
201 to 300 bpm: ±10% of reading
(average over NBP measurement cycle)
Pulse Rate Range 40 to 300 bpm
Measurement Time Typical at HR >60 bpm
Auto/manual/sequence: 30 seconds (adult)
25 seconds (neonatal)
Stat: 20 seconds
Maximum time: 180 seconds (adult/pediatric)
90 seconds (neonates)
Cuff Inflation Time Typical for normal adult cuff: Less than 10 seconds
Typical for neonatal cuff: Less than 2 seconds
Initial Cuff Inflation Pressure Adult: 165 ±15 mmHg
Pedi: 130 ±15 mmHg
Neo: 100 ±15 mmHg
Auto Mode Repetition Times 1, 2, 2.5, 3, 5, 10, 15, 20, 30, 45, 60 or 120 minutes
STAT Mode Cycle Time 5minutes
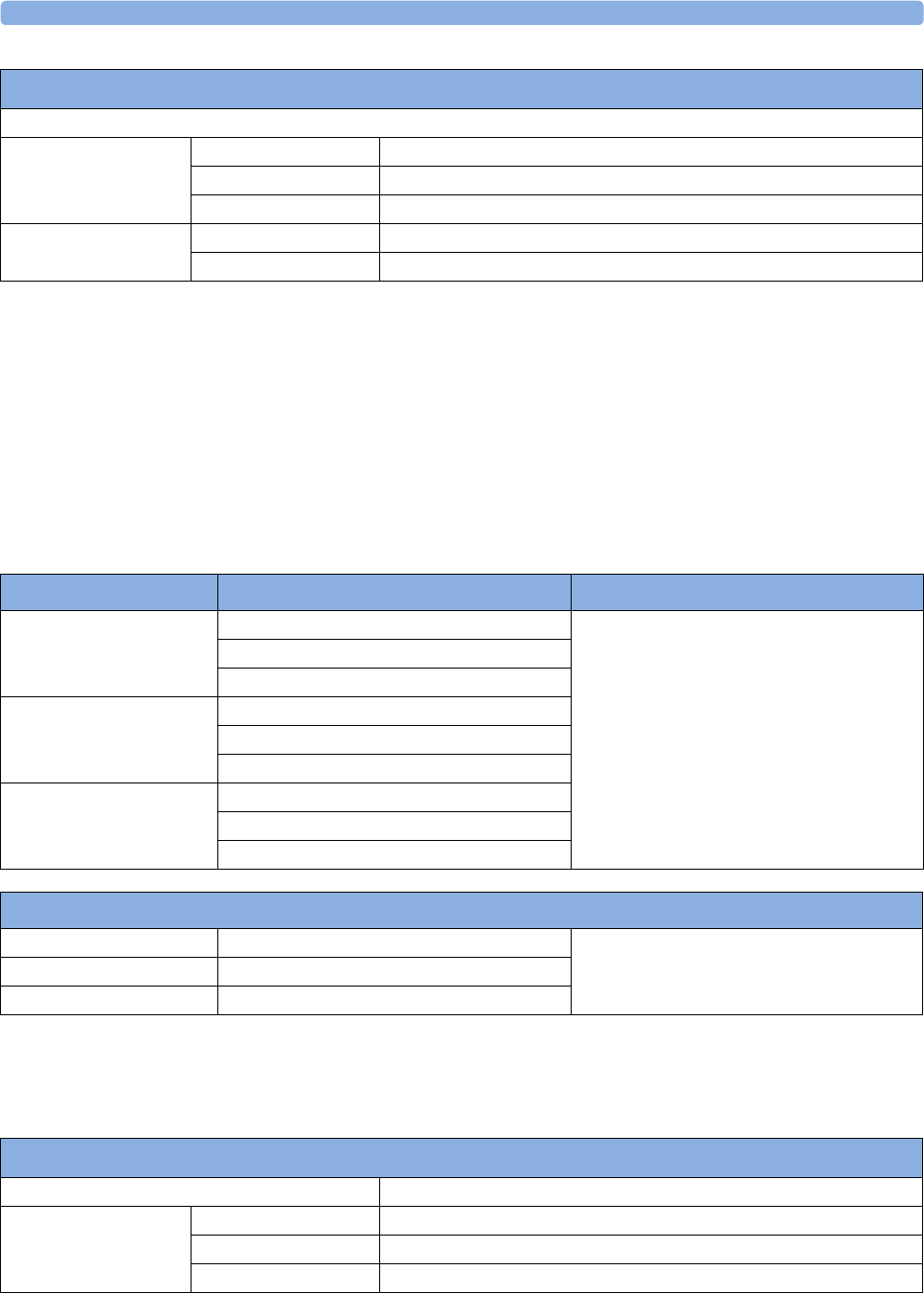
36 Specifications
415
Measurement Validation: In adult and pediatric mode, the blood pressure measurements determined
with this device comply with the American National Standard for Electronic or Automated
Sphygmomanometers (ANSI/AAMI SP10 - 1992) in relation to mean error and standard deviation,
when compared to intra-arterial or auscultatory measurements (depending on the configuration) in a
representative patient population. For the auscultatory reference the 5th Korotkoff sound was used to
determine the diastolic pressure.
In neonatal mode, the blood pressure measurements determined with this device comply with the
American National Standard for Electronic or Automated Sphygmomanometers (ANSI/AAMI SP10 -
1992 and AAMI/ANSI SP10A -1996) in relation to mean error and standard deviation, when
compared to intra-arterial measurements in a representative patient population.
Invasive Pressure and Pulse
Complies with IEC 60601-2-34:2000/EN60601-2-34:2000.
Venipuncture Mode Inflation
Inflation Pressure Adult 20 to 120 mmHg (3 to 16 kPa)
Pediatric 20 to 80 mmHg (3 to 11 kPa)
Neonatal 20 to 50 mmHg (3 to 7 kPa)
Automatic deflation
after
Adult/pediatric 170 seconds
Neonatal 85 seconds
NBP Performance Specifications
NBP Alarm Specifications Range Adjustment
Systolic Adult: 30 to 270 mmHg (4 to 36 kPa) 10 to 30 mmHg: 2 mmHg (0.5 kPa)
>30 mmHg: 5 mmHg (1 kPa)
Pedi: 30 to 180 mmHg (4 to 24 kPa)
Neo: 30 to 130 mmHg (4 to 17 kPa)
Diastolic Adult: 10 to 245 mmHg (1.5 to 32 kPa)
Pedi: 10 to 150 mmHg (1.5 to 20 kPa)
Neo: 10 to 100 mmHg (1.5 to 13 kPa)
Mean Adult: 20 to 255 mmHg (2.5 to 34 kPa)
Pedi: 20 to 160 mmHg (2.5 to 21 kPa)
Neo: 20 to 120 mmHg (2.5 to 16 kPa)
NBP Overpressure Settings
Adult >300 mmHg (40 kPa) >2 sec not user adjustable
Pediatric >300 mmHg (40 kPa) >2 sec
Neonate >150 mmHg (20 kPa) >2 sec
Invasive Pressure Performance Specifications
Measurement Range -40 to 360 mmHg
Pulse Rate Range 25 to 350 bpm
Accuracy ±1% Full Range
Resolution 1 bpm
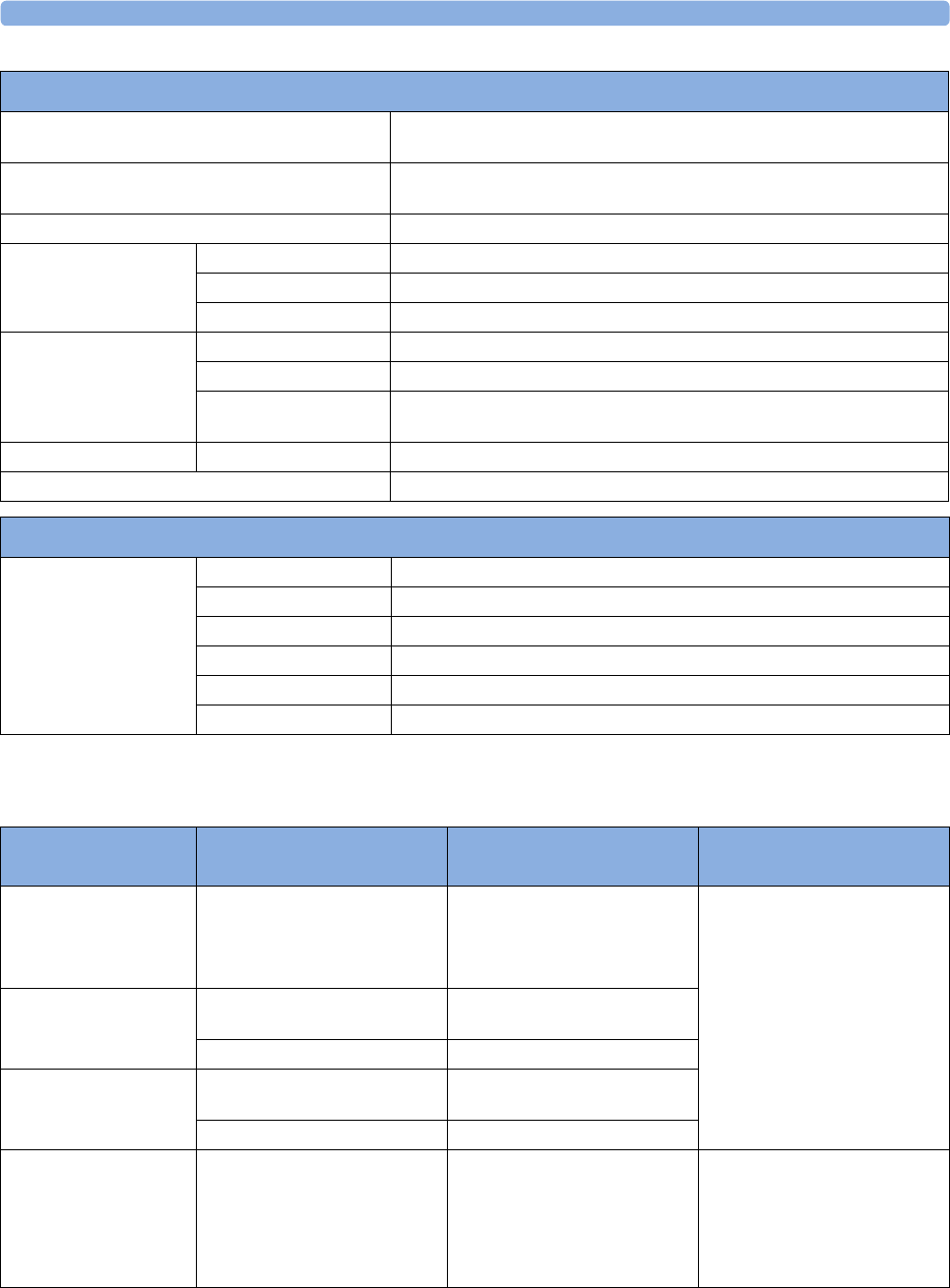
36 Specifications
416
Invasive Pressure Alarm Specifications
Input Sensitivity Sensitivity: 5 µV/V/mmHg (37.5 µV/V/kPa)
Adjustment range: ±10%
Transducer Load Impedance: 200 to 2000 Ω (resistive)
Output Impedance: ≤3000 Ω (resistive)
Frequency Response dc to 12.5 Hz or 40 Hz
Zero Adjustment Range ±200 mmHg (±26 kPa)
Accuracy ±1 mmHg (±0.1 kPa)
Drift Less than 0.1 mmHg/°C (0.013 kPa/°C)
Gain Accuracy Accuracy ±1%
Drift Less than 0.05%/°C
Non linearity and
Hysteresis
Error of ≤0.4 %FS (@CAL 200 mmHg)
Overall Accuracy (including transducer) ±4% of reading or ±4 mmHg (±0.5 kPa), whichever is greater
Volume displacement of CPJ840J6 0.1 mm3 /100 mmHg
Analog output Specifications
Analog Output
available only with
M1006B #C01 (@ CAL
200 mmHg)
Range -0.4 V to 3.6 V
Level 1 V / 100 mmHg
Accuracy ±3% full scale
Offset ±30 mV
Resolution 8 Bit (@ 5 V range)
Signal delay 20 ms
Invasive Pressure Performance Specifications
Invasive Pressure Alarm
Specifications Range Adjustment Delay
Pressure -40 to 360 mmHg
(-5.0 to 48 kPa)
-40 to 50 mmHg
2mmHg (0.5kPa)
>50 mmHg
5mmHg (1kPa)
max. 12 seconds
Extreme High Difference to high limit 0 to
25 mmHg
5 mmHg steps (0.5 kPa)
Clamping at -40 to 360 mmHg 5 mmHg steps (1.0 kPa)
Extreme Low Difference to low limit 0 to
25 mmHg
5 mmHg steps (0.5 kPa)
Clamping at -40 to 360 mmHg 5 mmHg steps (1.0 kPa)
Pulse 25 to 300 bpm Adult:
1 bpm steps (25 to 40 bpm)
5 bpm steps (40 to 300 bpm)
Pedi/Neo:
1 bpm steps (25 to 50 bpm)
5 bpm steps (50 to 300 bpm)
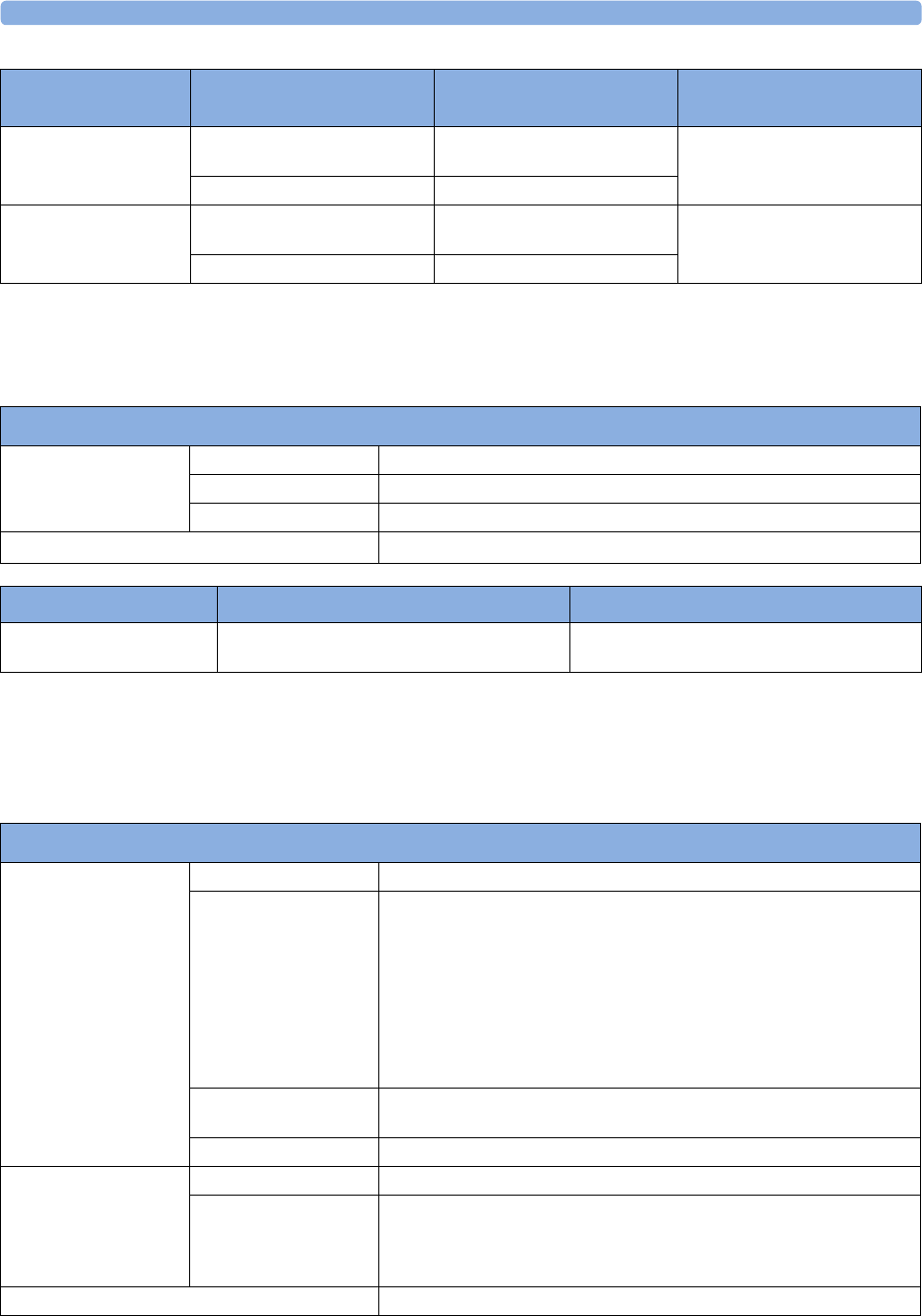
36 Specifications
417
Temp
Complies with EN 12470-4:2000. Specified without transducer.
CO2
The CO2 measurement in M3014A and M3015A complies with EN ISO 21647:2004 + Cor.1:2005
(except alarm system; alarm system complies with IEC 60601-2-49:2001).
Tachycardia Difference to high limit 0 to
50 bpm
5 bpm steps max. 14 seconds
Clamping at 150 to 300 bpm 5 bpm steps
Bradycardia Difference to low limit 0 to
50 bpm
5 bpm steps max. 14 seconds
Clamping at 25 to 100 bpm 5 bpm steps
Invasive Pressure Alarm
Specifications Range Adjustment Delay
Temp Performance Specifications
Temp Range -1 to 45°C (30 to 113°F)
Resolution 0.1°C (0.2°F)
Accuracy ±0.1°C (±0.2°F)
Average Time Constant Less than 10 seconds
Temp Alarm Specifications Range Adjustment
Temp High/Low Alarms -1 to 45°C (30 to 113°F) -1 to 35°C (30 to 95°F), 0.5°C (1.0°F) steps
35 to 45°C (95 to 113°F), 0.1°C (0.2°F) steps
M3015A Microstream CO2 Performance Specifications
CO2 Range 0 to 150 mmHg (0 to 20 kPa), or 20% CO2, whichever is lower
Accuracy Up to 5 minutes during warmup: ±4 mmHg or 12%, whichever is greater
After 5 minutes warmup:
0 to 40 mmHg (0 to 5.3 kPa):±2.2 mmHg (±0.3 kPa)
Above 40 mmHg (5.3 kPa):±(5.5% + (0.08%/mmHg above 40 mmHg)) of
reading
These specifications are valid for 21% O2 and N2 balance, up to 35°C ambient
temperature, up to 60 rpm in adult mode and 100 rpm in neonatal mode.
Outside of these conditions the accuracy reaches at a minimum ±4 mmHg or
±12% of the reading, whichever is greater.
Resolution Numeric: 1.0 mmHg (0.1 kPa)
Wave: 0.1 mmHg (0.01 kPa)
Stability Included in Accuracy specifications
awRR Range 0 to 150 rpm
Accuracy 0 to 40 rpm: ±1 rpm
41 to 70 rpm: ±2 rpm
71 to 100 rpm: ±3 rpm
>100 rpm: ±5% of reading
Warm-up Time 5 minutes for full accuracy specification
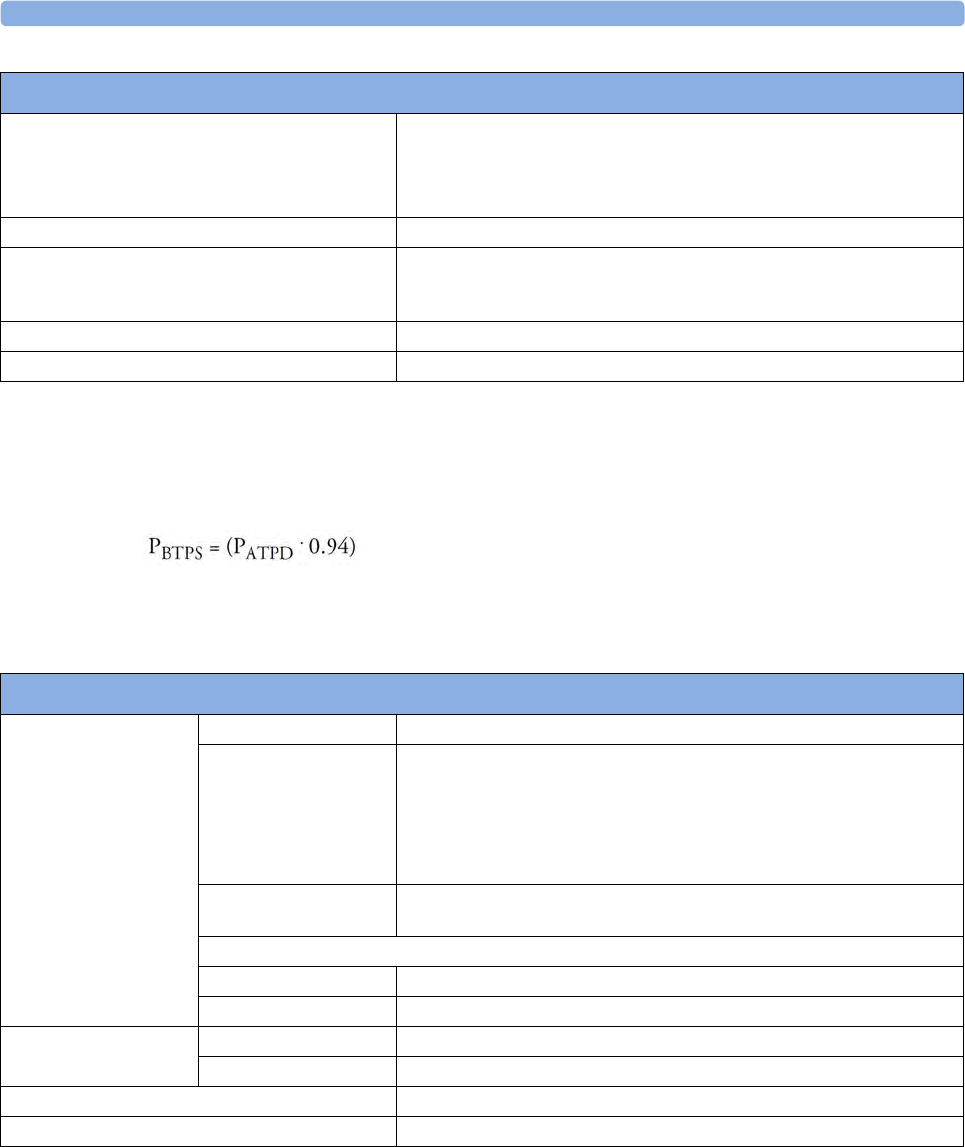
36 Specifications
418
Microstream CO2 Humidity Correction Factor
Either BTPS or ATPD can be selected as the humidity correction factor for the Microstream CO2
readings. The formula for the correction calculation is:
Rise Time 190 ms for neonatal mode
(measured with FilterLine H for neonatal)
240 ms for adult mode
(measured with FilterLine H for adult)
Sample Flow Rate 50 + 15/-7.5 ml/minute
Gas Sampling Delay Time Maximum:
3 seconds (2m sample lines)
6 seconds (4m sample lines)
Sound Pressure Acoustic noise: <45 dBA
Total System Response Time The total system response time is the sum of the delay time and the rise time.
M3015A Microstream CO2 Performance Specifications
where:
PBTPS = partial pressure at body temperature and pressure, saturated
PATPD = partial pressure at ambient temperature and pressure, dry
M3014A Mainstream CO2 Performance Specifications
CO2 Range 0 to 150 mmHg (0 to 20.0 kPa)
Accuracy after 2 minutes warmup:
For values between 0 and 40 mmHg: ±2.0 mmHg (±0.29 kPa)
For values from 41 to 70 mmHg: ±5% of reading
For values from 71 to 100 mmHg: ±8% of reading
The specifications are valid for standard gas mixtures, balance air, fully hydrated
at 35°C, Pabs = 760 mmHg, flow rate = 2 l/min.
Resolution Numeric: 1.0 mmHg (0.1 kPa)
Wave: 0.1 mmHg (0.01 kPa)
Stability:
Short term drift ±0.8 mmHg over four hours
Long term drift Accuracy specification will be maintained over a 120 hour period
awRR Range 2 to 150 rpm
Accuracy ±1 rpm
Warm-up Time 2minutes with CO
2 transducer attached for full accuracy specification
Response Time Less than 60 ms (with adult or infant reusable or disposable adapter)
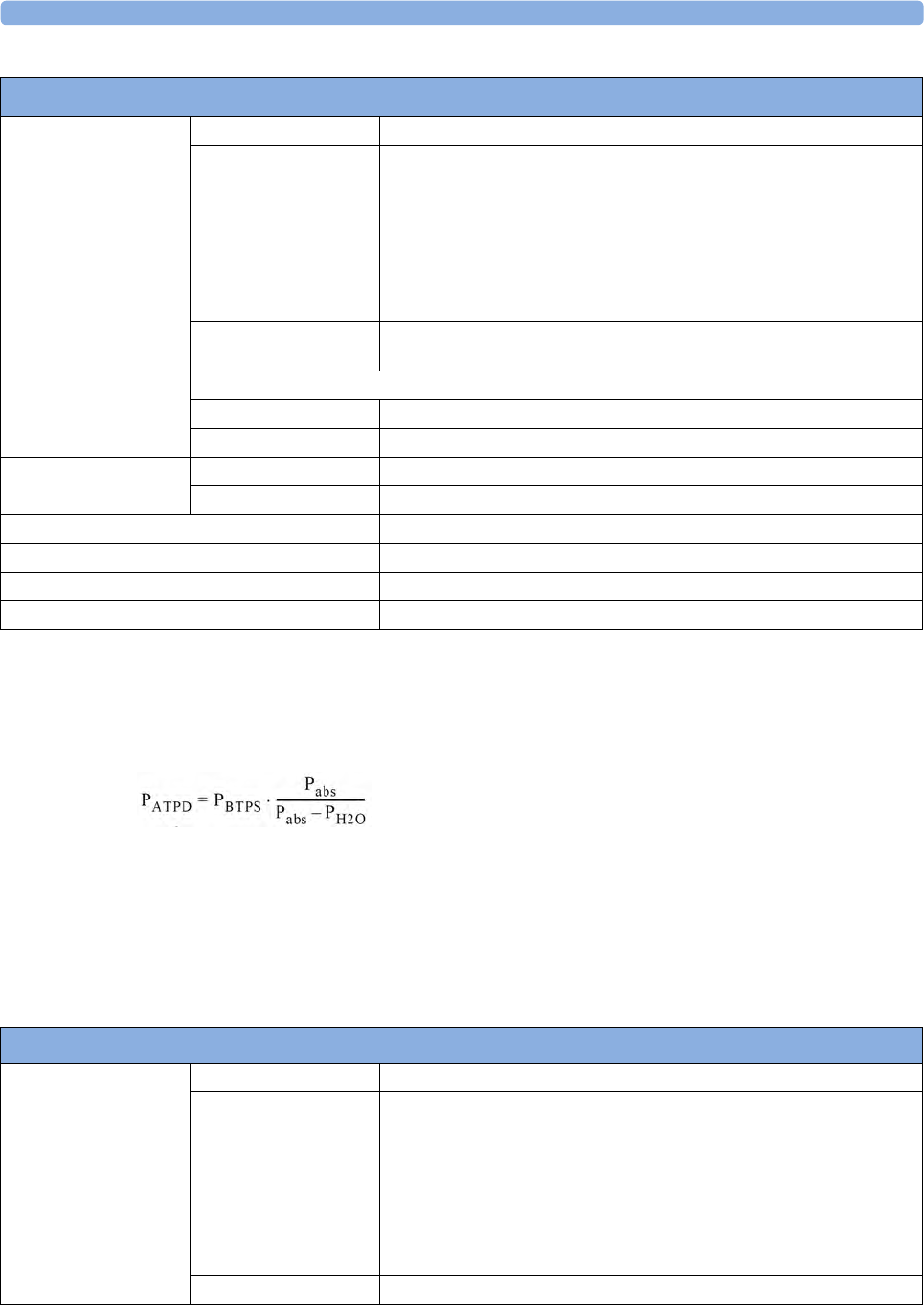
36 Specifications
419
M3014A Mainstream and Sidestream CO2 Humidity Correction Factor
Either BTPS or ATPD can be selected as the humidity correction factor for the CO2 readings. The
formula for the correction calculation is:
M3014A Sidestream CO2 Performance Specifications
CO2 Range 0 to 150 mmHg (0 to 20.0 kPa)
Accuracy after 2 minutes warmup:
For values between 0 and 40 mmHg: ±2.0 mmHg (±0.29 kPa)
For values from 41 to 70 mmHg: ±5% of reading
For values from 71 to 100 mmHg: ±8% of reading
For values from 101 to 150 mmHg: ±10% of reading
At respiration rates above 80 rpm, all ranges are ±12% of actual. The
specifications are valid for gas mixtures of CO2, balance N2, dry gas at
760 mmHg within specified operating temperature range.
Resolution Numeric: 1.0 mmHg (0.1 kPa)
Wave: 0.1 mmHg (0.01 kPa)
Stability:
Short term drift ±0.8 mmHg over four hours
Long term drift Accuracy specification will be maintained over a 120 hour period
awRR Range 2 to 150 rpm
Accuracy ±1 rpm
Warm-up Time 2minutes with CO
2 sensor attached for full accuracy specification
Sample Flow Rate 50 ±10 ml/minute
Total System Response Time 3seconds
Operating Temperature 0 to 40°C (32 to 100°F)
where:
PBTPS = partial pressure at body temperature and pressure,
saturated
PATPD = partial pressure at ambient temperature and pressure,
dry
Pabs = absolute pressure
PH2O = 42 mmHg @35°C and 100% RH
M3016A Mainstream CO2 Performance Specifications
CO2 Range -4 to 150 mmHg (-0.5 to 20.0 kPa)
Accuracy after 20 minutes warmup and calibration:
For values between 0 and 40 mmHg: ±2.2 mmHg (±0.29 kPa)
For values between 40 and 76 mmHg: ±5.5% of reading
The specifications are valid for 45% O2 and N2 or N2O balance. Outside these
conditions the accuracy reaches at a minimum the requirements of EN864/
ISO9918.
Resolution Numeric: 1.0 mmHg (0.1 kPa)
Wave: 0.1 mmHg (0.01 kPa)
Stability ±1.0 mmHg over a 7 day period
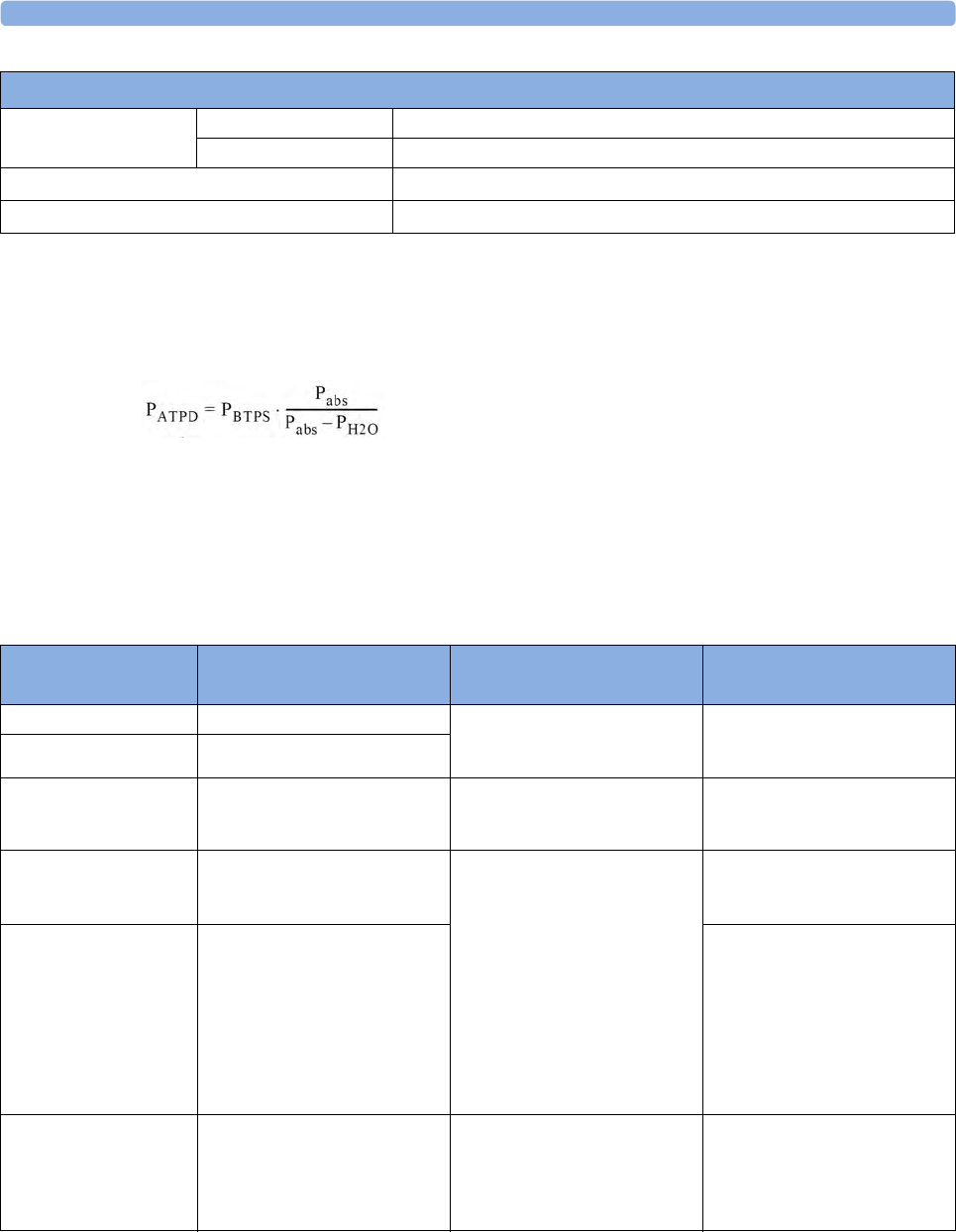
36 Specifications
420
Mainstream CO2 Humidity Correction Factor
Either BTPS or ATPD can be selected as the humidity correction factor for the Mainstream CO2
readings. The formula for the correction calculation is:
Interfering Gas and Vapor Effects On CO2 Measurement Values
The specified deviations for M3002A/M3014A are valid when the appropriate corrections are switched on and set
correctly.
awRR Range 0 to 150 rpm
Accuracy ±2 rpm
Warm-up Time 20 minutes with CO2 transducer attached for full accuracy specification
Response Time Less than 125 ms (for step from 10% to 90%)
M3016A Mainstream CO2 Performance Specifications
where:
PBTPS = partial pressure at body temperature and pressure,
saturated
PATPD = partial pressure at ambient temperature and pressure,
dry
Pabs = absolute pressure
PH2O = 42 mmHg @35°C and 100% RH
CO2 Alarm
Specifications Range Adjustment Delay
etCO2 High 20 to 95 mmHg (2 to 13 kPa) 1 mmHg (0.1 kPa) M3002A/M3014A/M3016A: less
than 14 seconds
M3015A: less than 21 seconds.
etCO2 Low 10 to 90 mmHg (1 to 12 kPa)
imCO2 High 2 to 20 mmHg
(0.3 to 3.0 kPa)
steps of 1 mmHg (0.1 kPa) M3002A/M3014A/M3016A: less
than 14 seconds
M3015A: less than 21 seconds.
awRR High Adult/pedi: 10 to 100 rpm
Neo: 30 to 150 rpm
under 20 rpm: 1 rpm steps
over 20 rpm:5 rpm steps
M3002A/M3014A/M3016A: less
than 14 seconds
M3015A: less than 21 seconds.
awRR Low Adult/pedi: 0 to 95 rpm
Neo: 0 to 145 rpm
M3015A:
settings <20 rpm: less than
8seconds
>20 rpm: less than 21 seconds
M3002A/M3014A/M3016A
settings <20 rpm: less than
4seconds
>20 rpm: less than 14 seconds
Apnea delay 10 to 40 seconds 5 second steps set apnea delay time + 4 seconds
(M3002A/M3014A/M3016A) or
8 seconds (M3015A with 2 m
sample lines) or 11 seconds
(M3015A with 4 m sample lines).
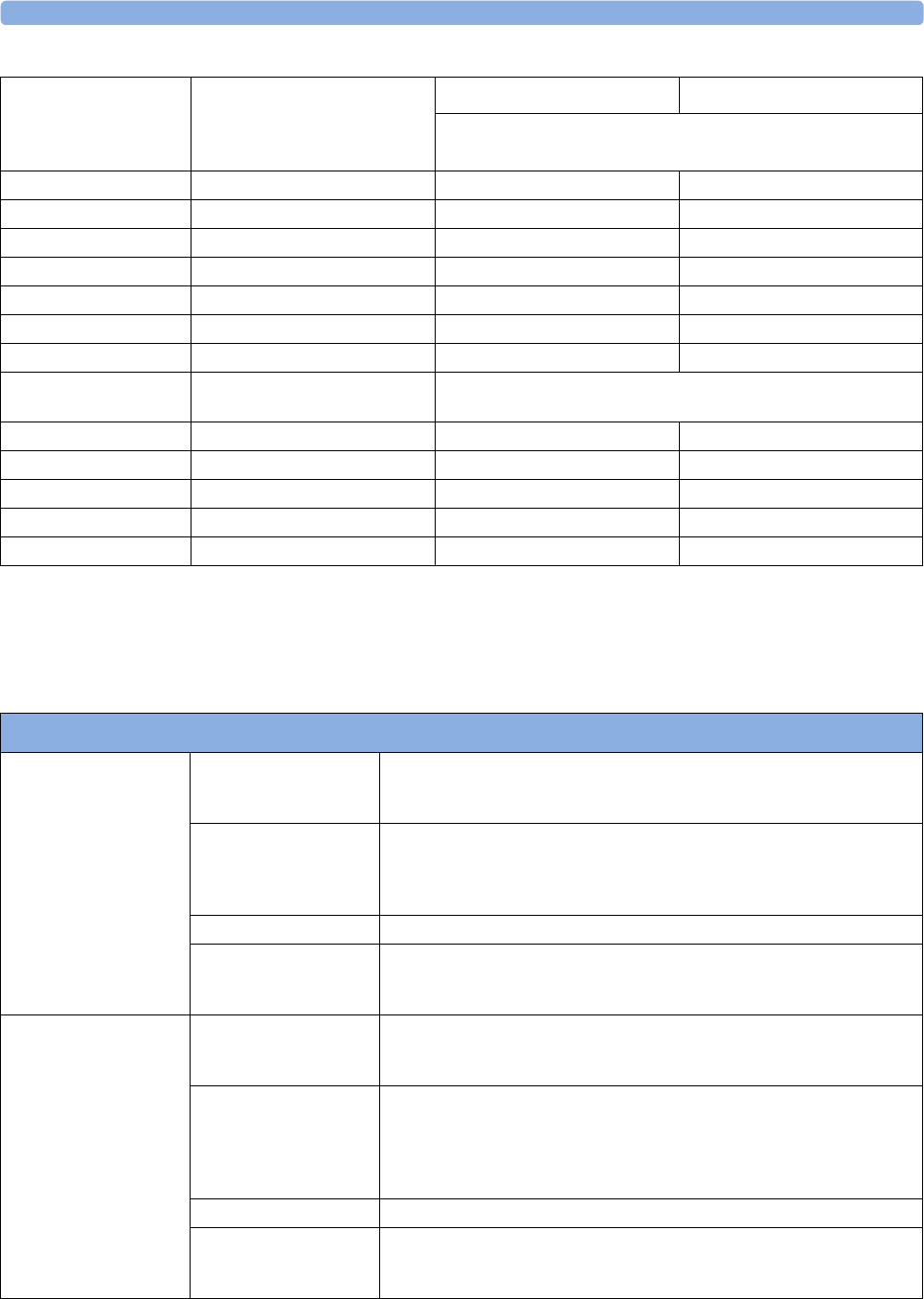
36 Specifications
421
Spirometry
The following specifications apply for 760 mmHg ambient pressure and patient gas: room air at 35°C,
unless otherwise noted
Gas or Vapor Gas Level
(% volume fraction)
M3002A/M3014A M3015A
Additional deviation due to gas interference, measured at 0 -
40 mmHg CO2
Nitrous Oxide 60% ±1 mmHg ±5%
Halothane 4% ±2 mmHg ±5%
Enflurane 5% ±2 mmHg ±5%
Isoflurane 5% ±2 mmHg ±5%
Sevoflurane 5% ±2 mmHg ±5%
Xenon 80% -5 mmHg ±5%
Helium 50% ±1 mmHg ±5%
Metered dose inhaler
propellants
- not specified for use
Desflurane 15% +5 mmHg ±5%
Ethanol 0.1% ±1 mmHg ±5%
Isopropanol 0.1% ±1 mmHg ±5%
Acetone 0.1% ±1 mmHg ±5%
Methane 1.0% ±1 mmHg ±5%
Spirometry Performance Specifications
Flow Wave (AWF) Range ±25 l/min (neonatal)
±100 l/min (pediatric)
±180 l/min (adult)
Accuracy ±3% or
0.125 l/min (neonatal)
0.25 l/min (pediatric)
0.5 l/min (adult)
Scales ±10, ±20, ±40, ±60, ±80, ±100, ±120, ±150 l/min
Scale Default ±20 l/min (neonatal)
±100 l/min (pediatric)
±150 l/min (adult)
Volume Wave (AWV) Range 0 to 100 ml (neonatal)
0 to 400 ml (pediatric)
0 to 3000 ml (adult)
Accuracy ±5% or
±3 ml (neonatal)
±12 ml (pediatric)
±90 ml (adult),
whichever is greater
Scales 50, 100, 200, 600, 800, 1000, 2000, 3000 ml
Scale Default 50 ml (neonatal)
200 ml (pediatric)
800 ml (adult)
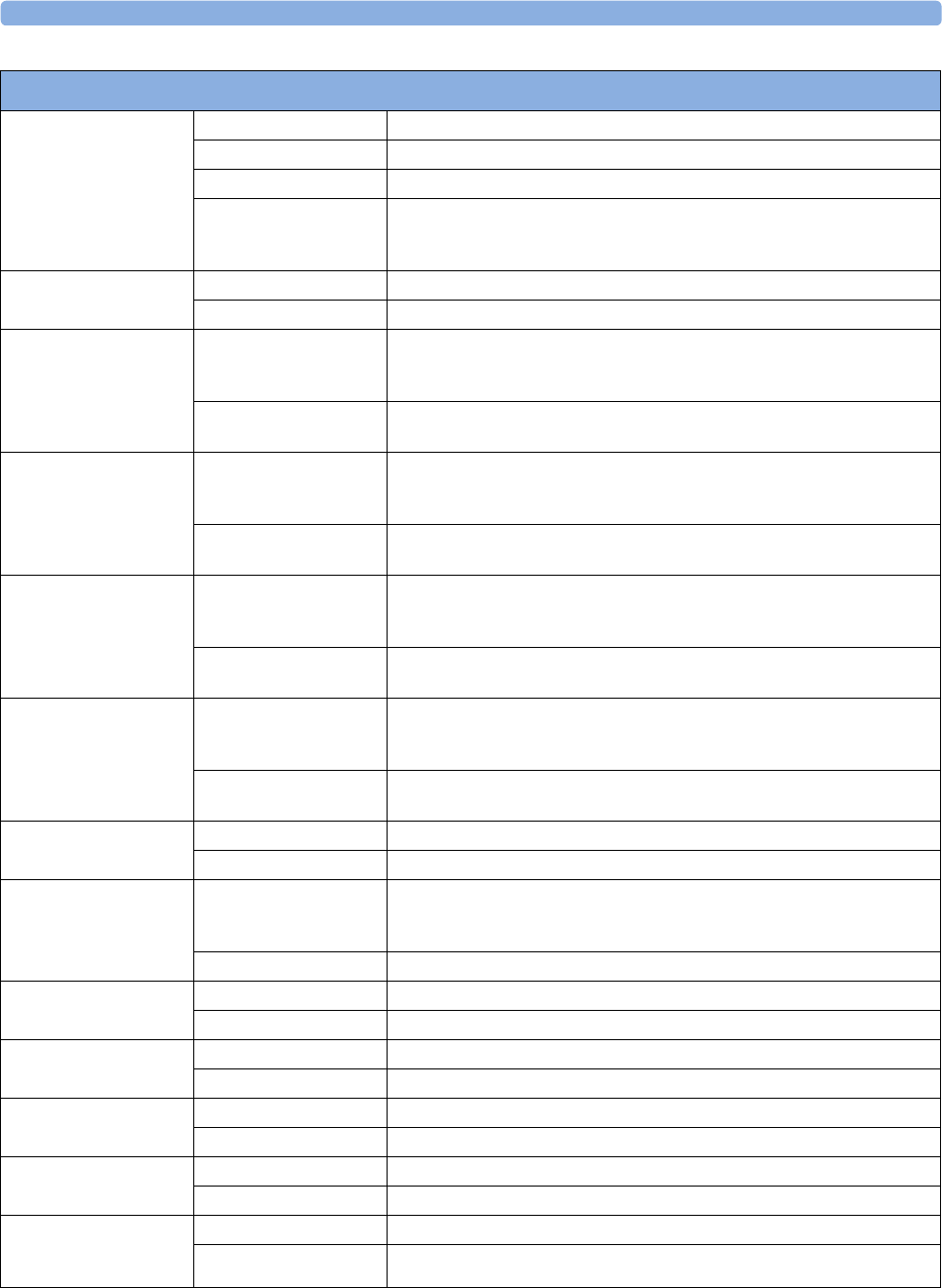
36 Specifications
422
Pressure Wave (AWP) Range -20 to 120 cmH2O
Accuracy ±2% or ±0.5 cmH2O whichever is greater
Scales 10, 20, 40, 60, 80, 100, 120 cmH2O
Scale Default 20 cmH2O (neonatal)
40 cmH2O (pediatric)
40 cmH2O (adult)
Respiration Rate
numeric (RRspir)
Range 2 to 120 breaths/min
Resolution 1 breath/min
Inspired Minute Volume
numeric (MVin)
Range 0.01 to 5 l/min (neonatal)
0.06 to 30 l/min (pediatric)
0.4 to 60 l/min (adult)
Resolution 0.01 l/min (neonatal/pediatric)
0.1 l/min (adult)
Expired Minute Volume
numeric (MVexp)
Range 0.01 to 5 l/min (neonatal)
0.06 to 30 l/min (pediatric)
0.4 to 60 l/min (adult)
Resolution 0.01 l/min (neonatal/pediatric)
0.1 l/min (adult)
Inspired Volume
numeric (TVin)
Range 5 to 100 ml (neonatal)
30 to 400 ml (pediatric)
200 to 3000 ml (adult)
Resolution 1 ml (neonatal/pediatric)
10 ml (adult)
Expired Volume
numeric (TVexp)
Range 5 to 100 ml (neonatal)
30 to 400 ml (pediatric)
200 to 3000 ml (adult)
Resolution 1 ml (neonatal/pediatric)
10 ml (adult)
Lung Compliance
numeric
Range 0 to 500 ml/cmH2O
Resolution 1 ml/cmH2O
Airway Resistance
numeric
Range 0 to 500 cmH2O/l/s (neonatal)
0 to 250 cmH2O/l/s (pediatric)
0 to 100 cmH2O/l/s (adult)
Resolution 1 cmH2O/l/s
Peak Inspiratory
Pressure numeric (PIP)
Range 0 to 120 cmH2O
Resolution 1 cmH2O
Negative Inspiratory
Pressure numeric
Range -20 to 0 cmH2O
Resolution 1 cmH2O
Mean Airway Pressure Range 0 to 120 cmH2O
Resolution 1 cmH2O
Plateau Pressure
numeric
Range 0 to 120 cmH2O
Resolution 1 cmH2O
Positive End-Expiratory
Pressure numeric
(PEEP)
Range 0 to 99 cmH2O
Resolution 1 cmH2O
Spirometry Performance Specifications
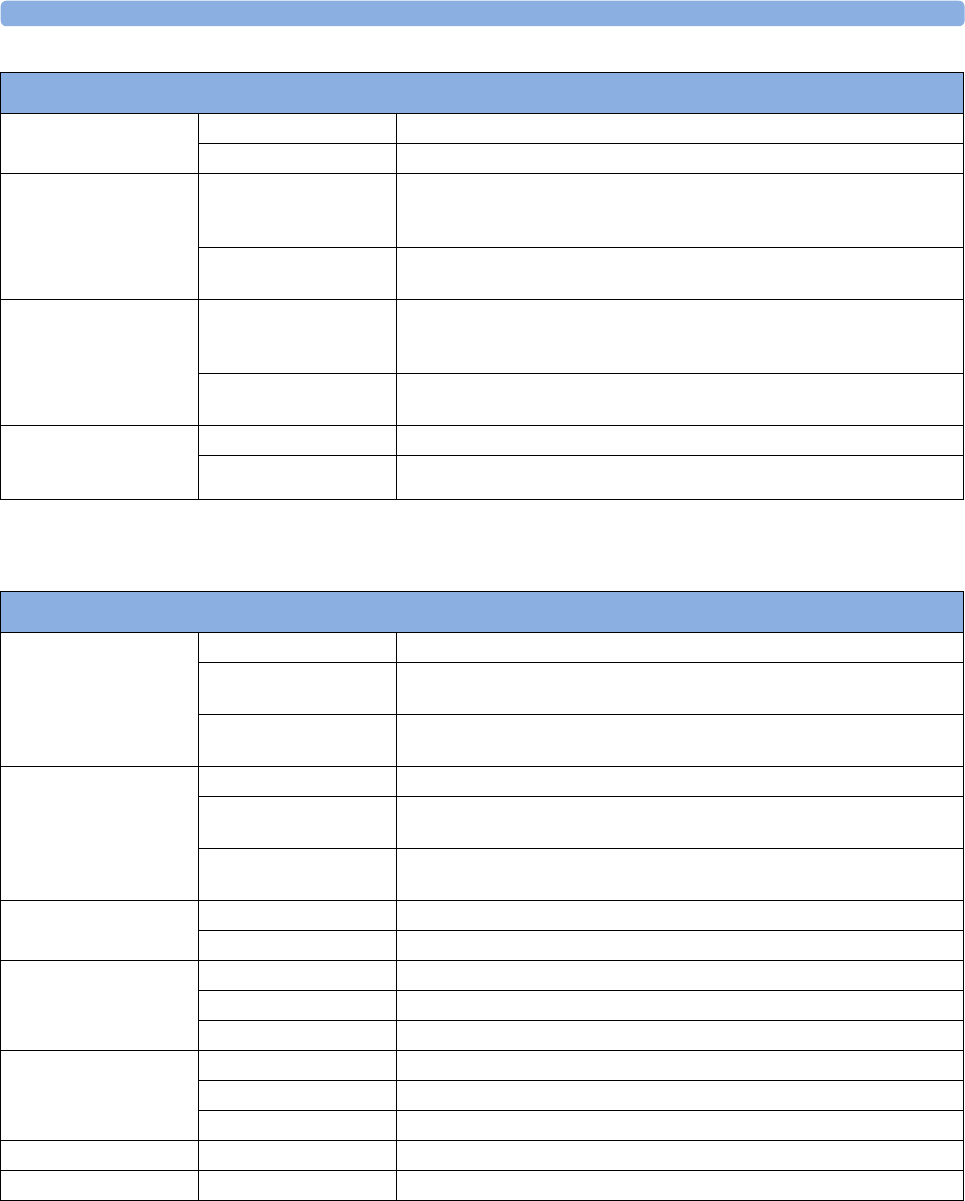
36 Specifications
423
Cardiac Output / Continuous Cardiac Output
Barometric Pressure
numeric (PB)
Range 400 to 800 mmHg
Resolution 1 mmHg
Peak Inspiratory Flow
numeric (PIF)
Range 0.3 to 25 l/min (neonatal)
1 to 100 l/min (pediatric)
2 to 180 l/min (adult)
Resolution 0.1 l/min (neonatal)
1 l/min (pediatric/adult)
Peak Expiratory Flow
numeric (PEF)
Range 0.3 to 25 l/min (neonatal)
1 to 100 l/min (pediatric)
2 to 180 l/min (adult)
Resolution 0.1 l/min (neonatal)
1 l/min (pediatric/adult)
Inspiration to
Expiration ratio numeric
(I:E)
Range 1: 0.2 ... 9.9
Resolution 0.1
Spirometry Performance Specifications
C.O./CCO Performance Specifications
C.O. (right heart) Range 0.1 to 20.0 l/min
Accuracy Instrument Specification (electrical): ±3% or 0.1 l/min
System Specification: ±5%.or 0.2 l/min
Repeatability Instrument Specification (electrical): ±2% or 0.1 l/min
System Specification: ±3%.or 0.1 l/min
C.O. (transpulmonary) Range 0.1 to 25.0 l/min
Accuracy Instrument Specification (electrical): ±4% or 0.15 l/min
System Specification: ±5% or 0.2 l/min
Repeatability Instrument Specification (electrical): ±2% or 0.1 l/min
System Specification: ±3% or 0.1 l/min
EVLW Range 10 to 5000 ml
Standard Deviation 10% or 1 ml/kg
ITBV Range 50 to 6000 ml
Accuracy ±10% or 30 ml
Repeatability ±5% or 20 ml
CCO Range 0.1 to 25.0 l/min
Standard Deviation 10% or 0.3 l/min
Display Update 2 seconds nominal
Blood Temperature Range 17.0 to 43°C (62.6 to 109,5°F)
Injectate Temperature Range -1 to 30°C (30.2 to 86.0°F)
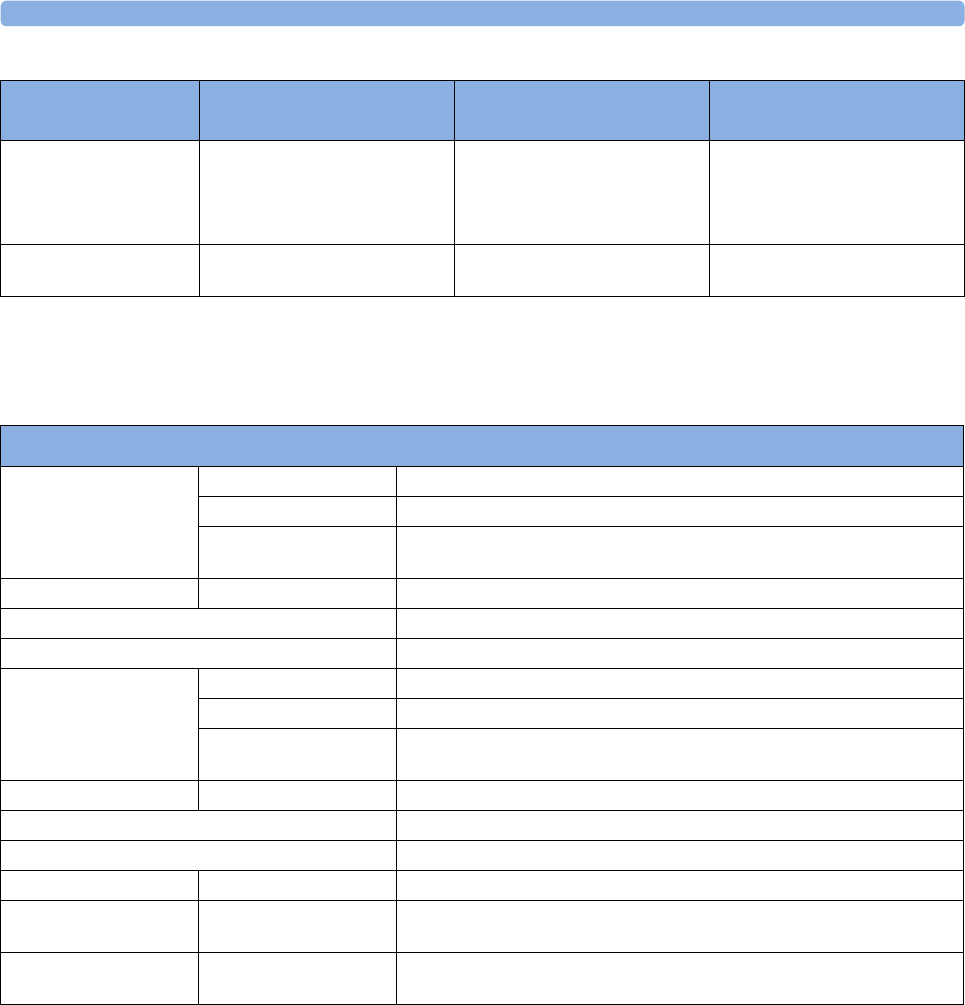
36 Specifications
424
tcGas
Complies with IEC 60601-2-23:1999/EN60601-2-23:2000.
C.O./CCO Alarm
Specifications Range Adjustment Delay
TBlood 17 to 43°C Steps of 0.5°C (17 to 35°C)
Steps of 0.1°C (35 to 43°C)
Steps of 1°F (63 to 95°F)
Steps of 0.2°F (95 to 109°F)
10 seconds after the value exceeds
the set limit range
CCO 0.1 to 25.0 l/min 0.1 l/min (0.1 to 10.0 l/min)
0.5 l/min (10.0 to 25.0 l/min)
10 seconds after the value exceeds
the set limit range
tcGas Performance Specifications
tcpO2 Range 0 to 750 mmHg (0 to 100 kPa)
Resolution 1 mmHg (0.1 kPa)
Overall Accuracy
(incl. transducer)
0 to 20.9% O2 better than +5 mmHg (+0.7 kPa)
Above 20.9% O2 better than +10% of reading
tcpO2 Test Signal 60 mmHg (8.0 kPa)
tcpO2 Drift, including transducer Typically 1.25%/h
tcpO2 response time, including transducer Typically 30 s
tcpCO2 Range 5 to 200 mmHg (0.7 to 26.7 kPa)
Resolution 1 mmHg (0.1 kPa)
Overall Accuracy
(incl. transducer)
5 to 76 mmHg (0.7 to 10.1 kPa) better than +5 mmHg(+0.7 kPa)
Above 76 mmHg (10.1 kPa) better than +10% of reading
tcpCO2 Test Signal 40 mmHg (5.3 kPa)
tcpCO2 Drift, including transducer Typically 2.5%/h
tcpCO2 response time, including transducer Typically 60 s
Warm-up Time <3 minutes
Site Timer 0.5, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 7, or 8 hours. Change Site alarm when site time is
expired and configurable automatic heating switch-off
Transducer Heating Available Temperatures -
37.0°C, 41.0 to 45°C in steps of 0.5°C
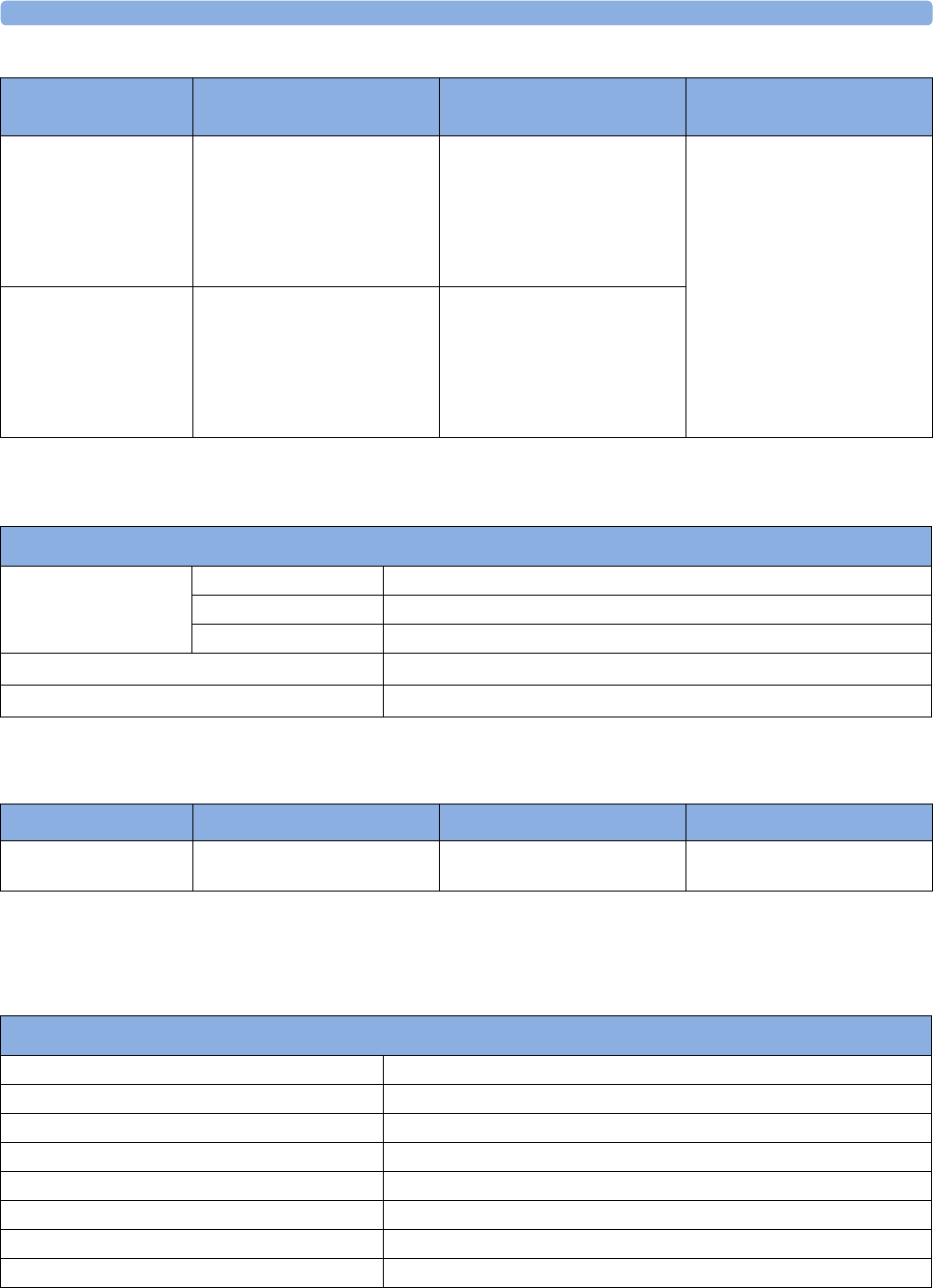
36 Specifications
425
Intravascular Oxygen Saturation
1 The accuracy specification for Edwards Lifesciences’ Philips-compatible catheters has been verified
in the saturation range 40%-95%.
EEG
Complies with IEC 60601-2-26:1994/EN60601-2-26:1994.
tcGas Alarm
Specifications Range Adjustment Alarm Delay
tcpO2 10 to 745 mmHg
1.0 to 99.5 kPa
10 to 30 mmHg: 1 mmHg
1.0 to 4.0 kPa: 0.1 kPa
32 to 100 mmHg: 2 mmHg
4.2 to 13 kPa: 0.2 kPa
105 to 745 mmHg: 5 mmHg
13.5 to 99.5 kPa: 0.5 kPa
10 seconds after the value exceeds
the set limit range.
tcpCO2 10 to 195 mmHg
1.0 to 26 kPa
10 to 30 mmHg: 1 mmHg
1.0 to 4.0 kPa: 0.1 kPa
32 to 100 mmHg: 2 mmHg
4.2 to 13 kPa: 0.2 kPa
105 to 195 mmHg: 5 mmHg
13.5 to 26 kPa: 0.5 kPa
Performance Specifications
SO2, SvO2, ScvO2 Range 10% to 100%
Accuracy ±2% (i.e. ±2 units), 1 standard deviation over 40% to 100%1 range.
Resolution 1%
Stability (system) Drift <2% over 24 hours
Response Time (10 % to 90 %) 5seconds
Alarm Specifications Range Adjustment Delay
SO2, SvO2, ScvO2 10% to 100% 1% max. 15 +4 seconds after value
exceeds the set limit range
EEG Performance Specifications
Leakage Current <=10 mA @ 110 Vac
Input Signal Range 1mVp-p
Differential Input Impedance >15 MΩ @ 10 Hz
Max. DC Input Offset Voltage ±320 mV
Input Protection Against defibrillation (5 kV) and electrosurgery
Common Mode Rejection >105 dB @ 5 kΩ imbalance and 60 Hz
Noise <0.4 mVRMS (1 to 30 Hz)
Electromagnetic Susceptibility <10 mVp-p @ 3 V/m, 26-1000 MHz
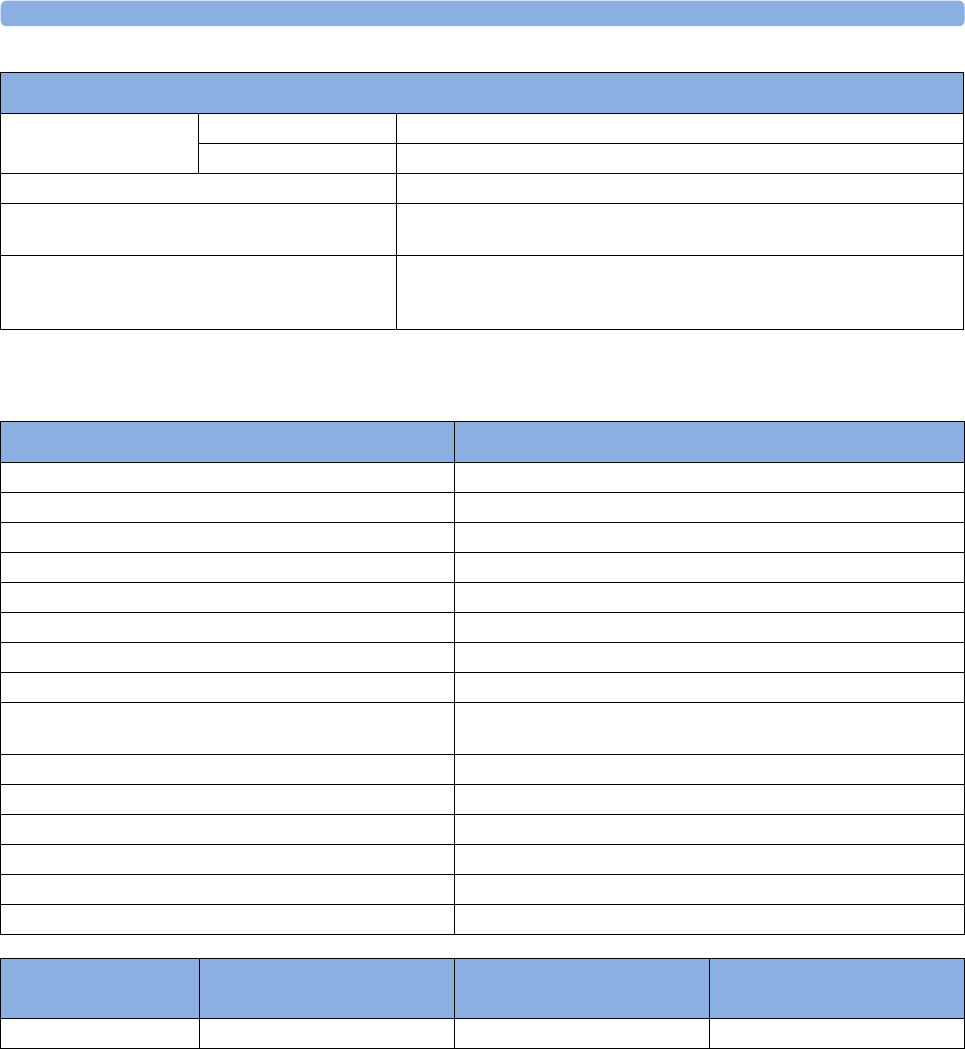
36 Specifications
426
BIS
Safety and Performance Tests
You must observe any national regulations on the qualification of the testing personnel and suitable
measuring and testing facilities. See the maintenance section for a list of required tests. Safety and
performance tests, and what to do if the instrument does not meet these specifications, are described
in the Service Guide.
Electrode Impedance
Measurement
Range 0 to 30 kΩ
Accuracy ±1 kΩ
Bandwidth 0.5 Hz to 50 Hz (-3 dB)
Low Filter Cut-Off Frequencies 0.5, 1.0, 2.0, and 5.0 Hz
(12 dB/octave)
High Filter Cut-Off Frequencies 15 Hz (65 dB/octave)
30 Hz (75 dB/octave)
50 Hz (85 dB/octave)
EEG Performance Specifications
BIS Performance Specifications BIS, BISx M1034A
Bispectral Index (BIS) Range 0 - 100
Signal Quality Index (SQI) Range 0 - 100%
EMG Range 0 - 100 dB
Suppression Ratio (SR) 0 - 100%
Spectral Edge Frequency (SEF) 0.5 - 30.0 Hz
Total Powe r (TP) 0 - 100 dB
Bursts (BISx only) 0 - 30 /minute
Noise <0.3 µV RMS (2.0 µV peak-to-peak)
Wave Scale With gridlines on: ±25 µV, ± 5 0 µV, ± 1 0 0 µV, ± 2 5 0 µV
With gridlines off: 50 µV, 1 0 0 µV, 2 0 0 µV, 5 0 0 µV
Update Frequency (BIS Numeric) 2048 ms
Bandwidth 0.25 - 100 Hz (-3 dB)
High Pass Filters 0.25 Hz, 1 Hz, 2 Hz (-3 dB)
Low Pass Filters 30 Hz, 50 Hz, 70 Hz, 100 Hz (-3 dB)
Notch Filters (for line frequency) 50 Hz, 60 Hz
Impedance Measurement Range 0 to 999 kΩ
BIS Alarm
Specifications Range Adjustment Alarm Delay
BIS High/Low Alarm 0 - 100 1 Max. 2 seconds
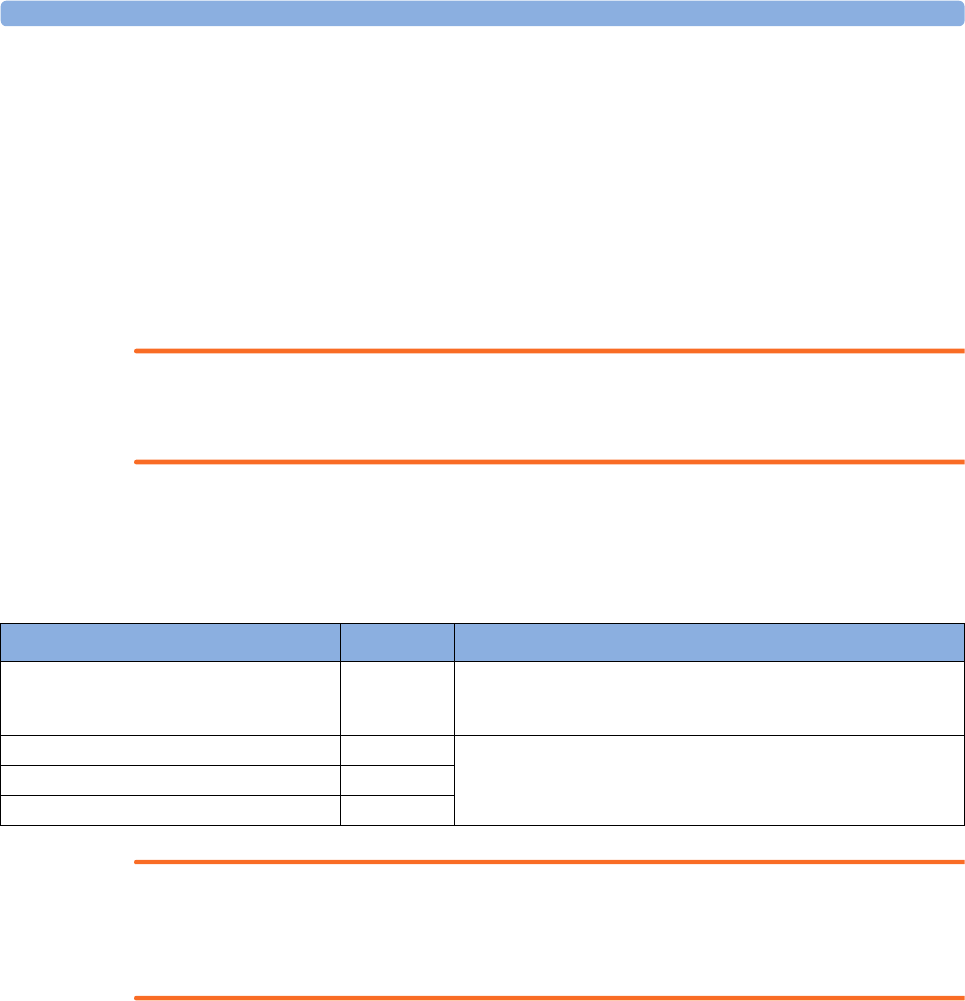
36 Specifications
427
Electromagnetic Compatibility (EMC) Specifications
Take special precautions regarding electromagnetic compatibility (EMC) when using medical electrical
equipment. You must operate your monitoring equipment according to the EMC information
provided in this book. Portable and mobile radio frequency (RF) communications equipment can
affect medical electrical equipment.
Accessories Compliant with EMC Standards
All accessories listed in the accessories section comply, in combination with the patient monitor, with
the requirements of IEC 60601-1-2:2001 + A1:2004.
WARNING
Using accessories other than those specified may result in increased electromagnetic emission or
decreased electromagnetic immunity of the monitoring equipment.
Electromagnetic Emissions
The monitor is suitable for use in the electromagnetic environment specified in the table below. You
must ensure that it is used in such an environment.
WARNING
The monitor should not be used next to or stacked with other equipment. If you must stack the
monitor, you must check that normal operation is possible in the necessary configuration before you
start monitoring patients.
Avoiding Electromagnetic Interference (Resp and BIS)
The respiration (Resp) and BIS measurements are very sensitive measurements that measure very small
signals. Technological limitations do not allow higher immunity levels than 1 V/m for radiated RF
electromagnetic fields and 1 Vrms for conducted disturbances induced by RF fields. Electromagnetic
fields with field strengths above 1 V/m and conducted disturbances above 1 Vrms may cause
erroneous measurements. Therefore Philips recommends that you avoid using electrically radiating
equipment in the close proximity of these measurements.
Electromagnetic Immunity
The monitor is suitable for use in the specified electromagnetic environment. The user must ensure
that it is used in the appropriate environment as described below.
Emissions test Compliance Avoiding Electromagnetic Interference
Radio Frequency (RF) emissions Group 1 The monitor uses RF energy only for its internal function. Therefore, its
RF emissions are very low and are not likely to cause any interference in
nearby electronic equipment
RF emissions CISPR 11 Class A The monitor is suitable for use in all establishments other than domestic
and those directly connected to the public low-voltage power supply
network that supplies buildings used for domestic purposes
Harmonic emissions IEC 61000-3-2 n/a
Voltage fluctuations IEC 61000-3-3 n/a
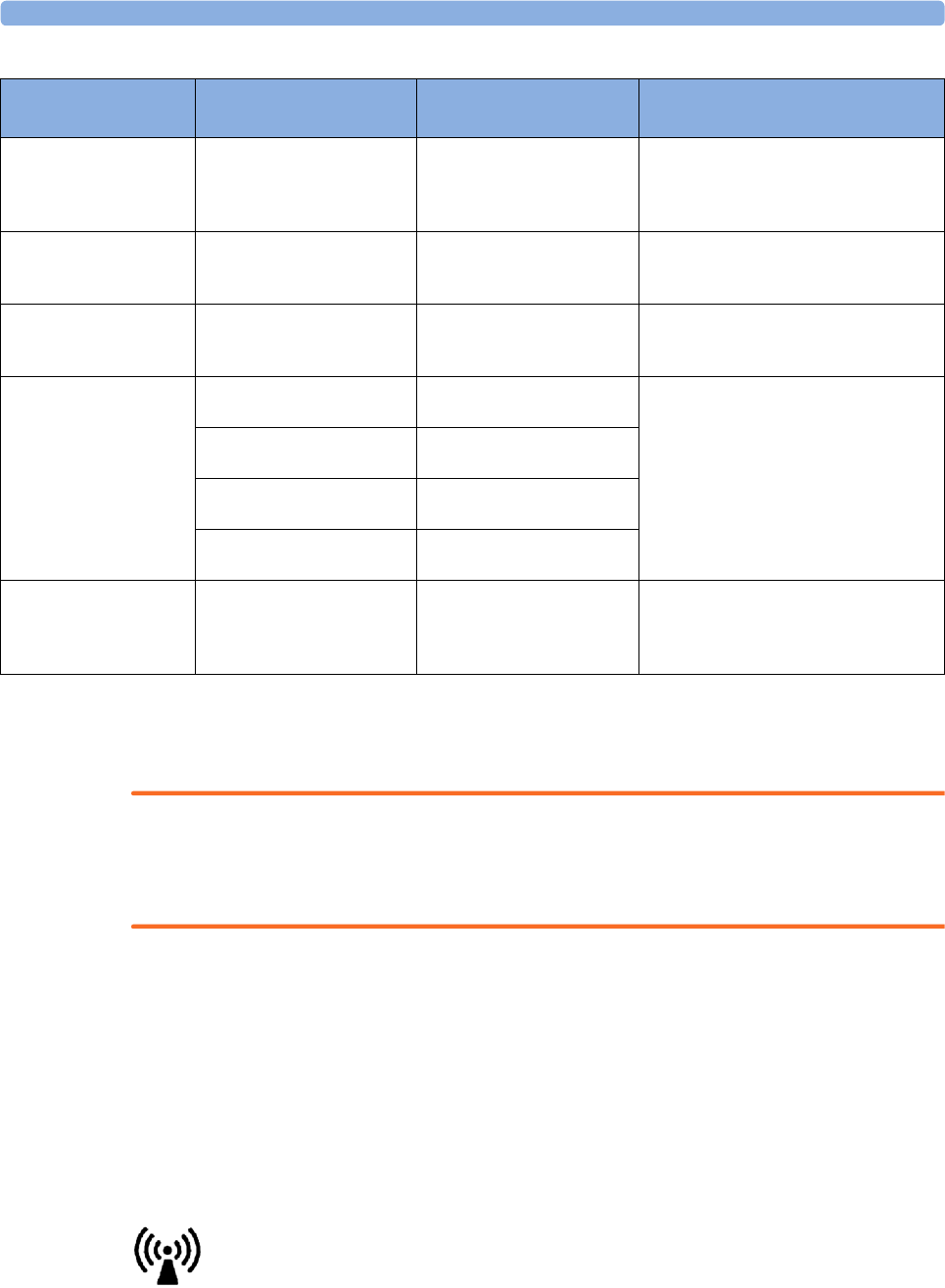
36 Specifications
428
In this table, UT is the a.c. mains voltage prior to application of the test level.
Recommended Separation Distance
WARNING
The monitor, equipped with a wireless network interface, intentionally receives RF electromagnetic
energy for the purpose of its operation. Therefore, other equipment may cause interference, even if
that other equipment complies with CISPR emission requirements.
In the following table, P is the maximum output power rating of the transmitter in watts (W) according
to the transmitter manufacturer and d is the recommended separation distance in meters (m). The
values given in brackets are for respiration and BIS.
Portable and mobile RF communications equipment should be used no closer to any part of the
monitor, including cables, than the recommended separation distance calculated from the equation
appropriate for the frequency of the transmitter.
Field strengths from fixed RF transmitters, as determined by an electromagnetic site survey, should be
less than the compliance level in each frequency range.
Interference may occur in the vicinity of equipment marked with this symbol:
Immunity test IEC 60601-1-2
test level Compliance level Electromagnetic environment guidance
Electrostatic discharge
(ESD)
IEC 61000-4-2
±6 kV contact
±8 kV air
±6 kV contact
±8 kV air
Floors should be wood, concrete, or
ceramic tile. If floors are covered with
synthetic material, the relative humidity
should be at least 30%.
Electrical fast transient/
burst
IEC 61000-4-4
±2 kV for power supply lines
±1 kV for input/output lines
±2 kV for power supply lines
±1 kV for input/output lines
Mains power quality should be that of a
typical commercial and/or hospital
environment
Surge
IEC 61000-4-5
±1 kV differential mode
±2 kV common mode
±1 kV differential mode
±2 kV common mode
Mains power quality should be that of a
typical commercial and/or hospital
environment
Voltage dips, short
interruptions and voltage
variations on power supply
input lines
IEC 61000-4-11
<5% UT (>95% dip in UT) for
0.5 cycles
<5% UT (>95% dip in UT) for
0.5 cycles
Mains power quality should be that of a
typical commercial and/or hospital
environment. If the user of the monitor
requires continued operation during power
mains interruptions, it is recommended
that the monitor is equipped with an
internal battery or is powered from an
uninterruptible power supply.
40% UT (60% dip in UT) for
5cycles
40% UT (60% dip in UT) for
5 cycles
70% UT (30% dip in UT) for
25 cycles
70% UT (30% dip in UT) for
25 cycles
<5% UT (>95% dip in UT) for
5sec
<5% UT (>95% dip in UT) for
5sec
Power frequency (50/
60 Hz) magnetic field
IEC 61000-4-8
3 A/m 3 A/m Power frequency magnetic fields should be
a t levels characteristic of a typical location
in a typical commercial and/or hospital
environment
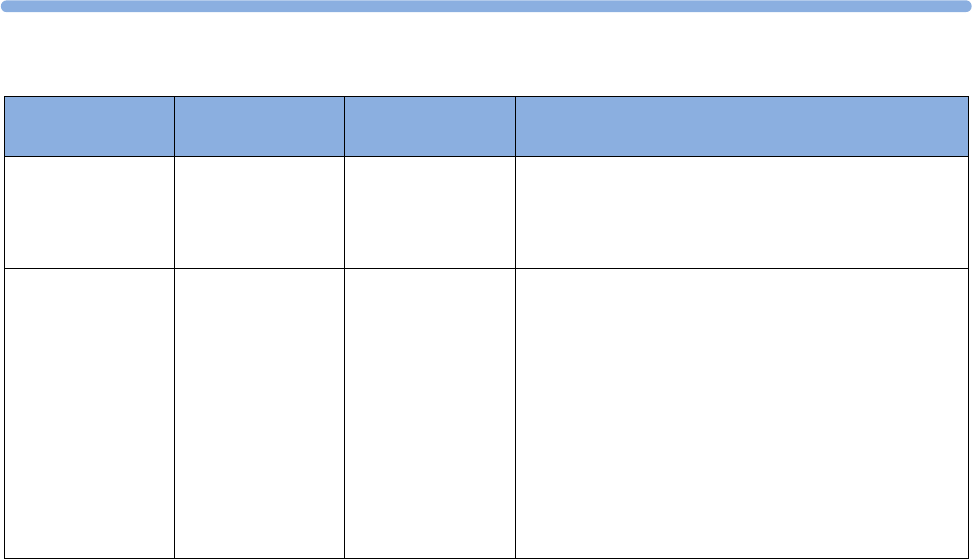
36
429
Field strengths from fixed transmitters, such as base stations for radio (cellular, cordless) telephones
and land mobile radios, amateur radio, AM and FM radio broadcast and TV broadcast cannot be
predicted theoretically with accuracy. To assess the electromagnetic environment due to fixed RF
transmitters, an electromagnetic site survey should be considered. If the measured field strength in the
location in which the monitor is used exceeds the applicable RF compliance level above, the monitor
should be observed to verify normal operation. If abnormal performance is observed, additional
measures may be necessary, such as reorienting or relocating the monitor.
These guidelines may not apply in all situations. Electromagnetic propagation is affected by absorption
and reflection from structures, objects, and people.
Recommended separation distances from portable and mobile RF
communication equipment
The monitor is intended for use in an electromagnetic environment in which radiated RF disturbances
are controlled. The customer or user of the monitor can help prevent electromagnetic interference by
maintaining a minimum distance between portable and mobile RF communications equipment and the
monitor as recommended below, according to the maximum output power of the communications
equipment.
In the following table, P is the maximum output power rating of the transmitter in watts (W) according
to the transmitter manufacturer and d is the recommended separation distance in meters (m). The
values given in brackets are for respiration and BIS.
Immunity test IEC 60601-1-2
test level Compliance level Electromagnetic environment guidance
Conducted RF
IEC 61000-4-6
3VRMS
150 kHz to 80 MHz
3VRMS
(1 VRMS for
respiration and BIS)
Recommended separation distance:
d = 1.2√P
for respiration and BIS:
d = 3.5√P
Radiated RF
IEC 61000-4-3
3V/m
80 MHz to 2.5 GHz
3V/m
(1 V/m for respiration
and BIS)
Recommended separation distance:
80 MHz to 800 MHz
d = 1.2√P
80 MHz to 800 MHz for respiration and BIS
d = 3.5√P
800 MHz to 2,5 GHz
d = 2.3√P
800 MHz to 2,5 GHz for respiration and BIS
d = 7.0√P
2.0 to 2,3 GHz for short range radio
d = 7.0√P
36 Specifications
430
Electrosurgery Interference/Defibrillation/Electrostatic Discharge
The equipment returns to the previous operating mode within 10 seconds without loss of any stored
data. Measurement accuracy may be temporarily decreased while performing electrosurgery or
defibrillation. This does not affect patient or equipment safety. Do not expose the equipment to x-ray
or strong magnetic fields (MRI).
Fast Transients/Bursts
The equipment will return to the previous operating mode within 10 seconds without loss of any
stored data (M1032 within 30 seconds). If any user interaction is required, the monitor indicates this
with a technical alarm (INOP).
Restart time
After power interruption, an ECG wave will be shown on the display after 30 seconds maximum.
Frequency of transmitter 150 kHz to 80 MHz 80 MHz to 800 MHz 800 MHz to 2,5 GHz
Equation
d = 1.2√P
for respiration and BIS:
d = 3.5√P
d = 1.2√P
for respiration and BIS:
d = 3.5√P
d = 2.3√P
for respiration and BIS:
d = 7.0√P
Rated max. output
power of transmitter Separation distance Separation distance Separation distance
0.01 W 0.1 (0.4) m 0.1 (0.4) m 0.2 (0.7) m
0.1 W 0.4 (1.1) m 0.4 (1.1) m 0.7 (2.2) m
1 W 1.3 (3.5) m 1.3 (3.5) m 2.3 (7.0) m
10 W 3.8 (11.1) m 3.8 (11.1) m 7.3 (22.1) m
100 W 12.0 (35.0) m 12.0 (35.0) m 23.0 (70.0) m
37 Default Settings Appendix
431
37Default Settings Appendix
This appendix documents the most important default settings of your monitor as it is delivered from
the factory. For a comprehensive list and explanation of default settings, see the Configuration Guide
supplied with your monitor. The monitor's default settings can be permanently changed in
Configuration Mode.
Note: If your monitor has been ordered pre-configured to your requirements, the settings at delivery
will be different from those listed here.
Country-Specific Default Settings
Certain default settings are specific to a particular country. These are listed here for all countries
alphabetically.
Country-Description Line Frequency Units
Weight
Units
Height
ECG Cable Color
50/60 [Hz] kg, lb in, cm IEC, AAMI
Afghanistan 50 kg cm AAMI
Åland Islands 50 kg cm IEC
Albania 50 kg cm IEC
Algeria 50 kg cm IEC
American Samoa 60 lb in AAMI
Andorra 60 lb in AAMI
Angola 50 kg cm IEC
Anguilla 60 lb in AAMI
Antarctica 60 lb in AAMI
Antigua and Barbuda 50 kg cm AAMI
Argentina 50 kg cm AAMI
Armenia 50 kg cm IEC
Aruba 60 kg cm AAMI
Australia 50 kg cm AAMI
Austria 50 kg cm IEC
Azerbaijan 50 kg cm IEC
Bahamas, The 60 kg cm AAMI
Bahrain 50 kg cm AAMI
Bangladesh 60 lb in AAMI
Barbados 50 kg cm AAMI
Belarus 50 kg cm IEC
Belgium 50 kg cm IEC
37 Default Settings Appendix
432
Belize 60 lb in AAMI
Benin 60 lb in AAMI
Bermuda 60 kg cm AAMI
Bhutan 60 lb in AAMI
Bolivia 50 kg cm AAMI
Bosnia and Herzegovina 50 kg cm IEC
Botswana 50 kg cm IEC
Bouvet Island 60 lb in AAMI
Brazil 60 kg cm AAMI
British Indian Ocean Territory 60 lb in AAMI
Brunei 50 kg cm IEC
Brunei Darussalam 50 kg cm AAMI
Bulgaria 50 kg cm IEC
Burkina Faso 50 kg cm IEC
Burundi 50 kg cm IEC
Cambodia 50 kg cm IEC
Cameroon 50 kg cm IEC
Canada 60 kg cm AAMI
Cape Verde 60 lb in AAMI
Cayman Islands 60 kg cm AAMI
Central African Republic 50 kg cm IEC
Chad 60 lb in AAMI
Chile 50 kg cm AAMI
China 50 kg cm IEC
Christmas Islands 60 lb in AAMI
Cocos Keeling Islands 60 lb in AAMI
Colombia 60 kg cm AAMI
Comoros 60 lb in AAMI
Congo 50 kg cm IEC
Congo, Democratic Republic of
the
50 kg cm IEC
Cook Islands 60 lb in AAMI
Costa Rica 60 kg cm AAMI
Côte d'Ivoire 50 kg cm IEC
Croatia 50 kg cm IEC
Cuba 60 kg cm IEC
Cyprus 50 kg cm IEC
Country-Description Line Frequency Units
Weight
Units
Height
ECG Cable Color
37 Default Settings Appendix
433
Czech Republic 50 kg cm IEC
Denmark 60 lb in AAMI
Djibouti 50 kg cm IEC
Dominica 50 kg cm AAMI
Dominican Republic 60 kg cm AAMI
Ecuador 60 kg cm AAMI
Egypt 50 kg cm IEC
El Salvador 60 kg cm AAMI
Equatorial Guinea 50 kg cm IEC
Eritrea 50 kg cm IEC
Estonia 50 kg cm IEC
Ethiopia 50 kg cm IEC
Falkland Islands, Malvinas 60 lb in AAMI
Faroe Islands 60 lb in AAMI
Fiji 60 lb in AAMI
Finland 50 kg cm IEC
France 50 kg cm IEC
French Guiana 50 kg cm IEC
French Polynesia 60 lb in AAMI
French Southern Territories 60 lb in AAMI
Gabon 50 kg cm IEC
Gambia, The 50 kg cm IEC
Georgia 60 lb in AAMI
Germany 50 kg cm IEC
Ghana 50 kg cm IEC
Gibraltar 60 lb in AAMI
Greece 50 kg cm IEC
Greenland 60 lb in AAMI
Grenada 50 kg cm AAMI
Guadeloupe 50 kg cm IEC
Guam 60 lb in AAMI
Guatemala 60 kg cm AAMI
Guernsey 50 kg cm IEC
Guinea 60 lb in AAMI
Guinea-Bissau 60 lb in AAMI
Guyana 60 kg cm AAMI
Haiti 60 kg cm AAMI
Country-Description Line Frequency Units
Weight
Units
Height
ECG Cable Color
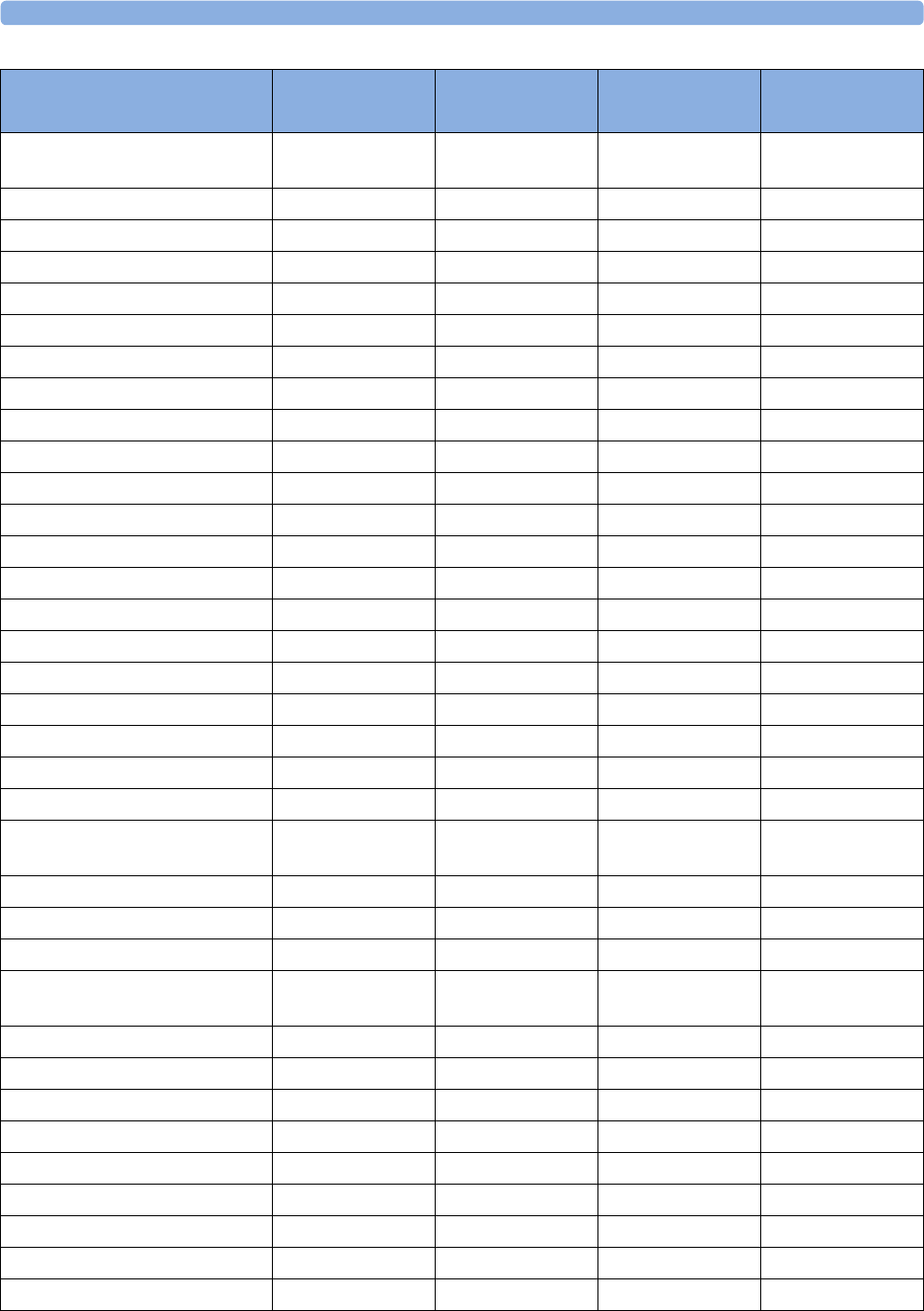
37 Default Settings Appendix
434
Heard Island and McDonald
Islands
60 lb in AAMI
Holy See, Vatican City State 60 lb in AAMI
Honduras 60 kg cm AAMI
Hong Kong 50 kg cm IEC
Hungary 50 kg cm IEC
Iceland 50 kg cm IEC
India 50 kg cm IEC
Indonesia 50 kg cm IEC
Iran, Islamic Republic of 50 kg cm AAMI
Iraq 50 kg cm AAMI
Ireland 50 kg cm IEC
Isle of Man 50 kg cm IEC
Israel 50 kg cm IEC
Italy 50 kg cm IEC
Jamaica 50 kg cm AAMI
Japan 60 kg cm IEC
Jersey 50 kg cm IEC
Jordan 50 kg cm AAMI
Kazakhstan 50 kg cm IEC
Kenya 50 kg cm IEC
Kiribati 60 lb in AAMI
Korea, Democratic People's
Republic of
60 lb in AAMI
Korea, Republic of 60 kg cm AAMI
Kuwait 50 kg cm AAMI
Kyrgyzstan 60 lb in AAMI
Lao People's Democratic
Republics
50 kg cm IEC
Latvia 50 kg cm IEC
Lebanon 50 kg cm AAMI
Lesotho 50 kg cm IEC
Liberia 50 kg cm IEC
Libyan Arab Jamahiriya 60 lb in AAMI
Liechtenstein 60 lb in AAMI
Lithuania 50 kg cm IEC
Luxembourg 50 kg cm IEC
Macao 60 lb in AAMI
Country-Description Line Frequency Units
Weight
Units
Height
ECG Cable Color
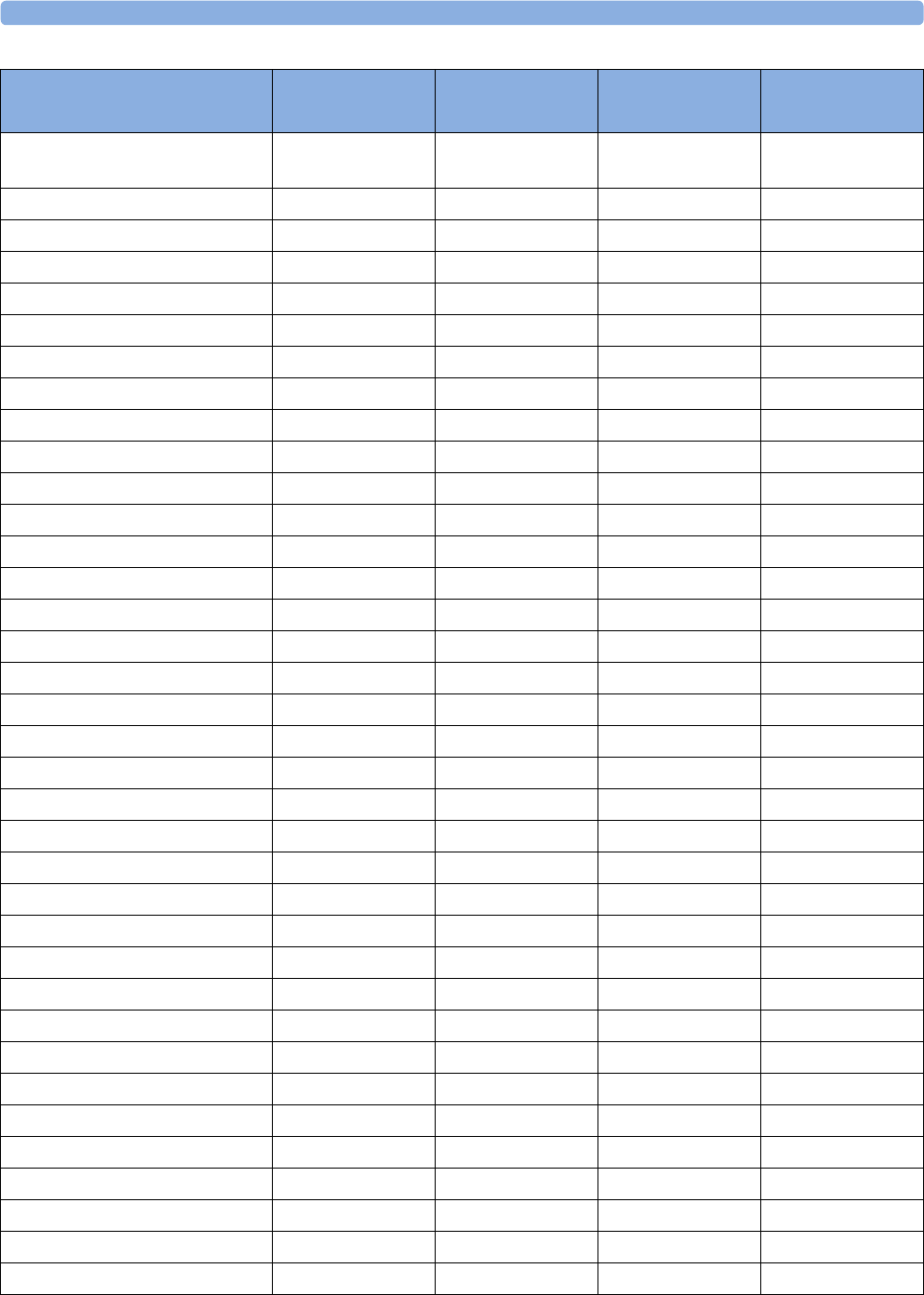
37 Default Settings Appendix
435
Macedonia, The former
Yugoslavian Republic of
50 kg cm IEC
Madagascar 50 kg cm IEC
Malawi 50 kg cm IEC
Malaysia 50 kg cm IEC
Maldives 60 lb in AAMI
Mali 50 kg cm IEC
Malta 50 kg cm IEC
Marshall Islands 60 lb in AAMI
Martinique 60 kg cm IEC
Mauritania 50 kg cm IEC
Mauritius 60 lb in AAMI
Mayotte 60 lb in AAMI
Mexico 60 kg cm AAMI
Micronesia, Federal States of 60 lb in AAMI
Moldova, Republic of 60 lb in AAMI
Monaco 60 lb in AAMI
Mongolia 60 lb in AAMI
Montenegro 50 kg cm IEC
Montserrat 50 kg cm AAMI
Morocco 50 kg cm IEC
Mozambique 50 kg cm IEC
Myanmar 60 lb in AAMI
Namibia 50 kg cm IEC
Nauru 60 lb in AAMI
Nepal 60 lb in AAMI
Netherlands 50 kg cm IEC
Netherlands Antilles 50 kg cm AAMI
New Caledonia 60 lb in AAMI
New Zealand 50 kg cm AAMI
Nicaragua 60 kg in AAMI
Niger 50 kg cm IEC
Nigeria 50 kg cm IEC
Niue 60 lb in AAMI
Norfolk Islands 60 lb in AAMI
Northern Mariana Islands 60 lb in AAMI
Norway 50 kg cm IEC
Country-Description Line Frequency Units
Weight
Units
Height
ECG Cable Color
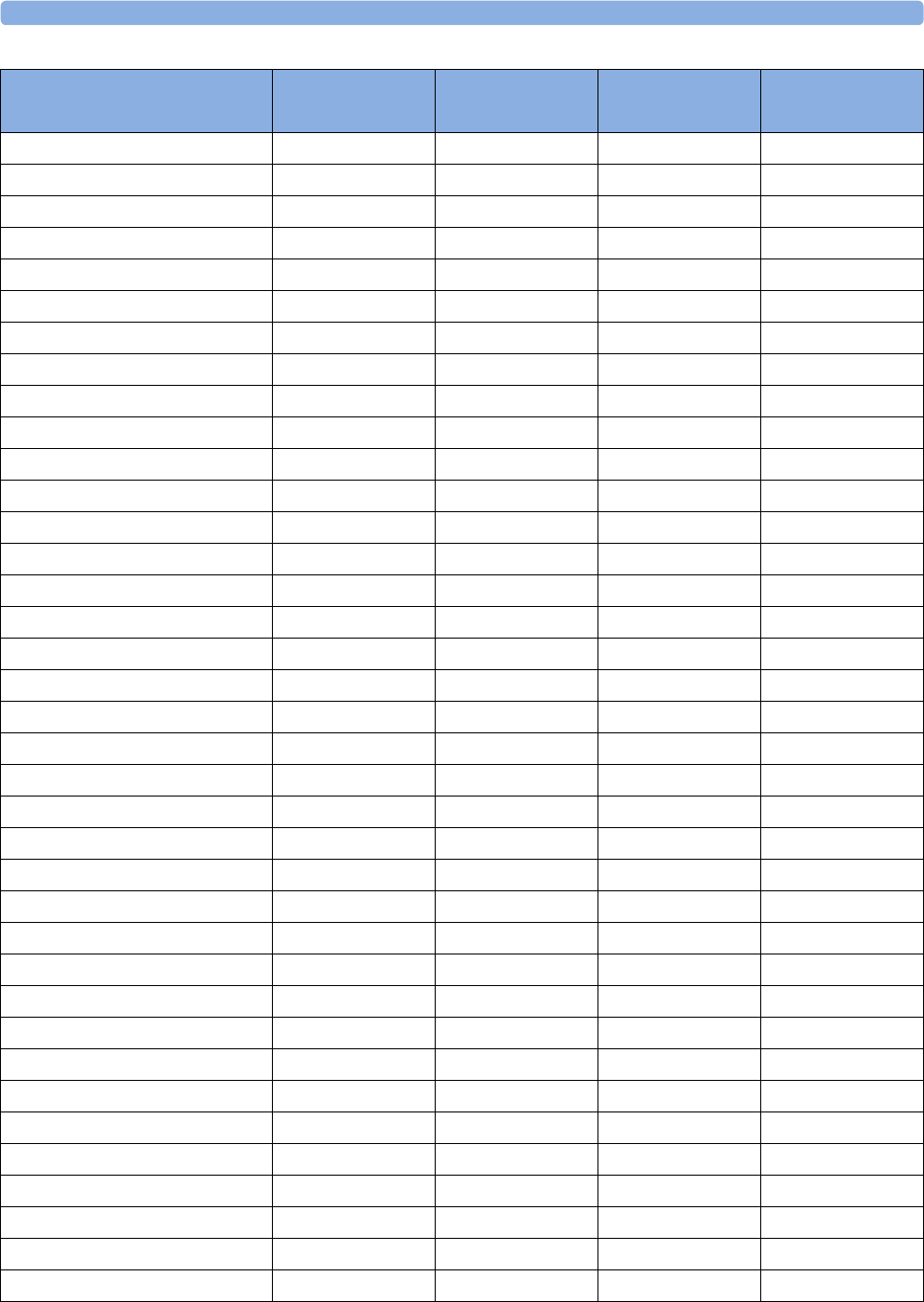
37 Default Settings Appendix
436
Oman 50 kg cm AAMI
Pakistan 50 kg cm IEC
Palau 60 lb in AAMI
Palestinian Territory 50 kg cm AAMI
Panama 60 lb in AAMI
Papua New Guinea 60 lb in AAMI
Paraguay 50 kg cm AAMI
Peru 60 kg cm AAMI
Philippines 60 kg cm AAMI
Pitcairn 60 lb in AAMI
Poland 50 kg cm IEC
Portugal 50 kg cm IEC
Puerto Rico 60 lb in AAMI
Qatar 50 kg cm AAMI
Reunion 60 lb in AAMI
Romania 50 kg cm IEC
Russian Federation 50 kg cm IEC
Rwanda 50 kg cm IEC
Saint Helena 60 lb in AAMI
Saint Kitts and Nevis 60 kg cm AAMI
Saint Lucia 50 kg cm AAMI
Saint Pierre and Miquelon 60 lb in AAMI
Saint Vincent and the Grenadines 50 kg cm AAMI
Samoa 60 lb in AAMI
San Marino 60 lb in AAMI
Sao Tome and Principe 60 lb in AAMI
Saudi Arabia 50 kg cm AAMI
Senegal 50 kg cm IEC
Serbia 50 kg cm IEC
Serbia & Montenegro 50 kg cm IEC
Seychelles 60 lb in AAMI
Sierra Leone 50 kg cm IEC
Singapore 50 kg cm IEC
Slovakia 50 kg cm IEC
Slovenia 50 kg cm IEC
Solomon Islands 60 lb in AAMI
Somalia 50 kg cm IEC
Country-Description Line Frequency Units
Weight
Units
Height
ECG Cable Color
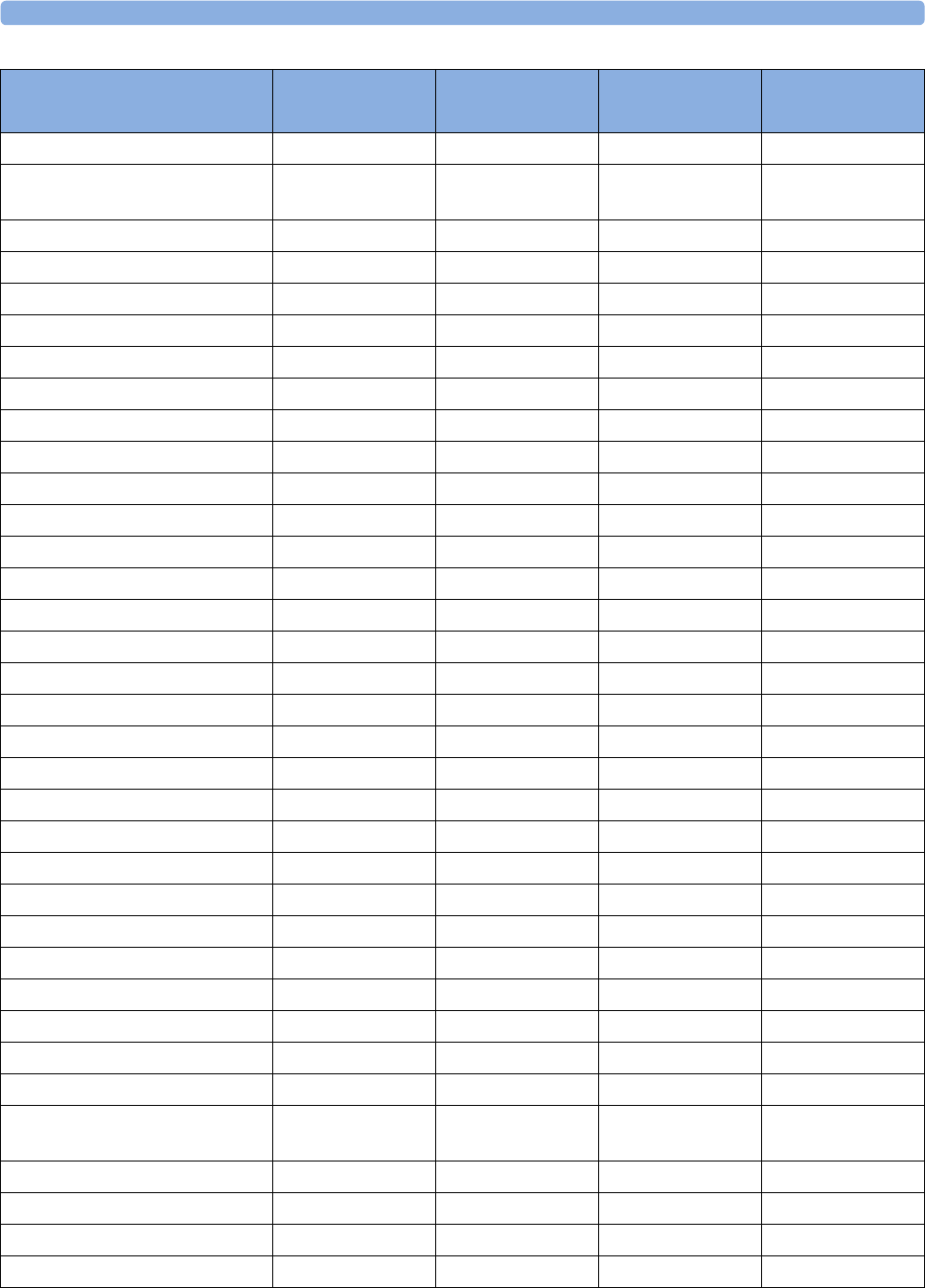
37 Default Settings Appendix
437
South Africa 60 lb in AAMI
South Georgia and the South
Sandwich Islands
60 lb in AAMI
Spain 50 kg cm IEC
Sri Lanka 60 lb in AAMI
Sudan 50 kg cm IEC
Suriname 60 kg cm AAMI
Svalbard and Jan Mayen 60 lb in AAMI
Swaziland 60 lb in AAMI
Sweden 50 kg cm IEC
Switzerland 50 kg cm IEC
Syrian Arab Rep 50 kg cm AAMI
Taiwan, Province of China 60 kg cm AAMI
Tajikistan 60 lb in AAMI
Tanzania, United Republic of 60 lb in AAMI
Thailand 50 kg cm AAMI
Timor-Leste 60 lb in AAMI
Togo 60 lb in AAMI
Tokelau 60 lb in AAMI
Tonga 60 lb in AAMI
Trinidad and Tobago 60 lb in AAMI
Tunisia 50 kg cm IEC
Turkey 50 kg cm IEC
Turkmenistan 60 lb in AAMI
Turks and Caicos Islands 60 kg cm AAMI
Tuvalu 60 lb in AAMI
Uganda 60 lb in AAMI
Ukraine 60 lb in AAMI
United Arab Emirates 50 kg cm AAMI
United Kingdom 50 kg cm IEC
United States 60 lb in AAMI
United States Minor Outlying
Islands
60 lb in AAMI
Uruguay 50 kg cm AAMI
Uzbekistan 60 lb in AAMI
Vanuatu 60 lb in AAMI
Venezuela 60 lb in AAMI
Country-Description Line Frequency Units
Weight
Units
Height
ECG Cable Color
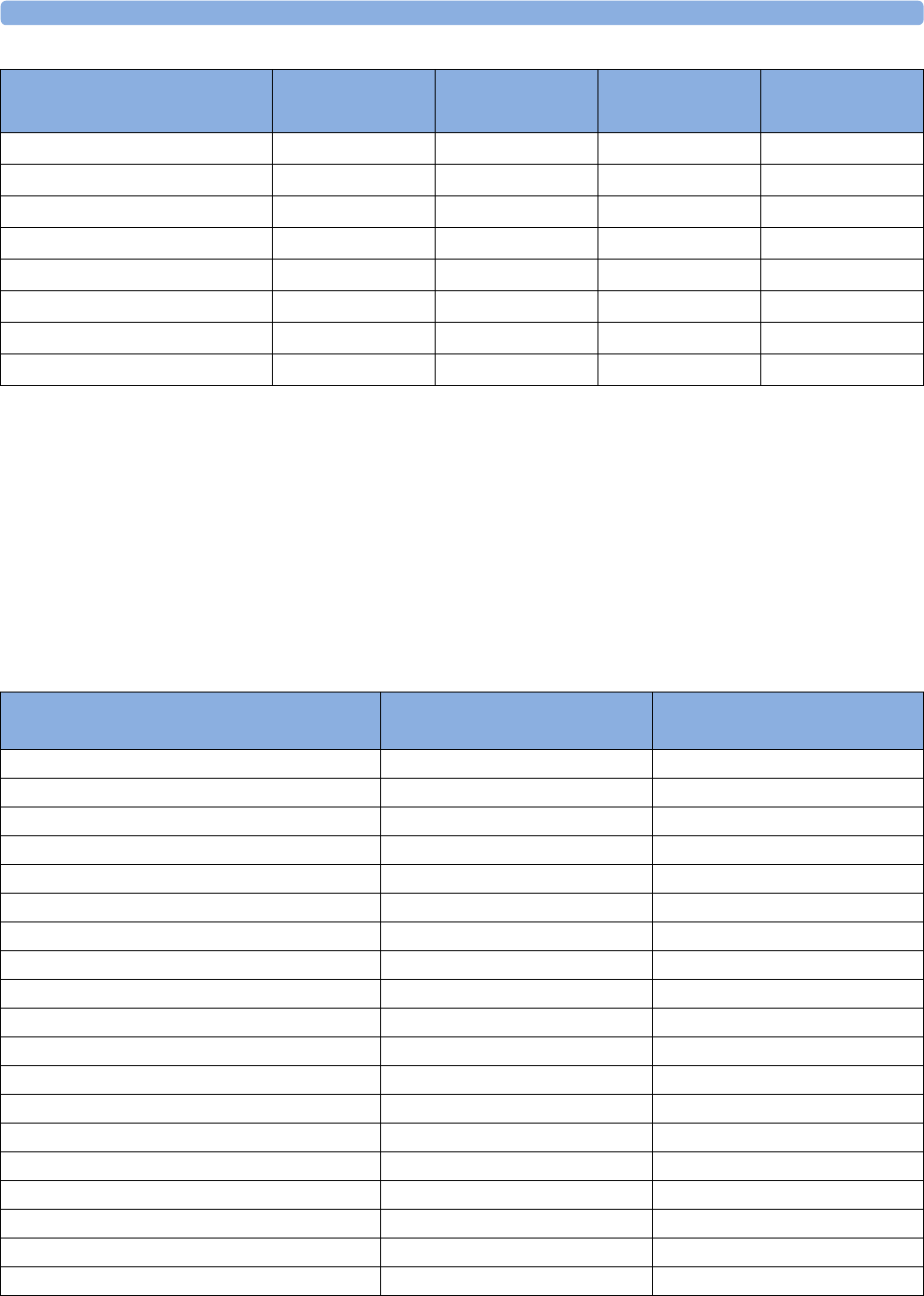
37 Default Settings Appendix
438
Alarm and Measurement Default Settings
The default wave speed for all measurements except Respiration is 25 mm/sec. For Respiration the
default wave speed is 6.25 mm/sec.
In the following tables, settings may be entered only once per table row if they are the same for all
patient categories.
Alarm Default Settings
Viet Nam 50 kg cm IEC
Virgin Islands (British) 50 kg cm AAMI
Virgin Islands (US) 60 lb in AAMI
Wallis and Futuna Islands 60 lb in AAMI
Western Sahara 50 kg cm IEC
Yemen 50 kg cm AAMI
Zambia 60 lb in AAMI
Zimbabwe 60 lb in AAMI
Country-Description Line Frequency Units
Weight
Units
Height
ECG Cable Color
Alarm Settings Factory Default H10/H20/H40 H30 (deviations from H10/H20/
H40)
Alarm Volume 5
Alarms Off 2 min
Pause Al. 5Min Enabled
Pause Al. 10Min Enabled
Auto Alarms Off Off
AlarmOffReminder Off
Visual Latching Red&Yellow Red Only
Audible Latching Red&Yellow Off
Alarm Reminder On
Reminder Time 3 min
Alarm Sounds Traditional
RedAlarmInterval 10 sec
Yel.Al. Interval 20 sec
Alarm Low 42
Red Alarm Volume AlarmVol. +2
Yell.AlarmVolume AlarmVol. +0
Inop Volume AlarmVol. +0
AutoIncrease Vol 2 Steps
IncreaseVolDelay 20 sec
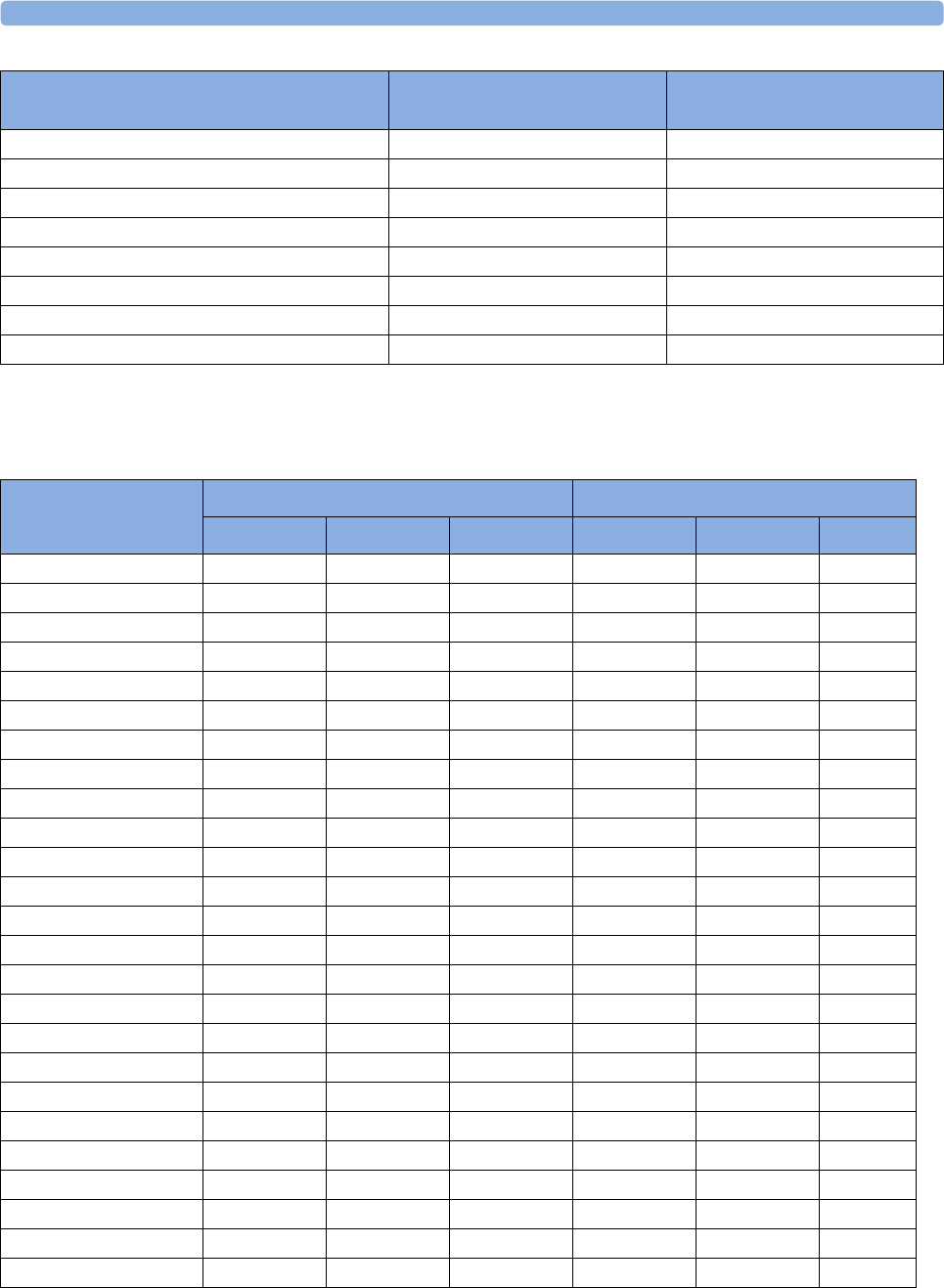
37 Default Settings Appendix
439
ECG, Arrhythmia, ST and QT Default Settings
Keep Blinking No
Relay1 Sensitiv. R&Y&C
Relay2 Sensitiv. Red&Yellow
Relay3 Sensitiv. Red
CyanRelayLatency 5sec
Yel.RelayLatency 2sec
Alarm Text Standard
NoCentrMonMinVol On4
Alarm Settings Factory Default H10/H20/H40 H30 (deviations from H10/H20/
H40)
ECG Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
High Limit 120 bpm 160 bpm 200 bpm
Low Limit 50 bpm 75 bpm 100 bpm
ECG/Arrhy Alarms On On On
Alarm Source Auto Auto Auto Auto
ECG OnOnOn
QRS Volume 111
Primary Lead II II II
Secondary Lead V V V
Analysis Mode Multi Lead Multi Lead Multi Lead
Lead Placement Standard Standard Standard
Mod.LeadPlacment Off Off Off
Filter Monitor Monitor Monitor Filter
AutoFilter Off Off Off
Default ECG Size Size X1 Size X1 Size X1
Color Green Green Green
Asystole Thresh. 4.0 sec 4.0 sec 3.0 sec
Δ ExtrTachy 20 bpm 20 bpm 20 bpm
Tachy Clamp 200 bpm 220 bpm 240 bpm
Δ ExtrBrady 20 bpm 20 bpm 20 bpm
Brady Clamp 40 bpm 40 bpm 50 bpm 40 bpm 60 bpm 80 bpm
ECG AL. OFF Inop Cyan Cyan Cyan
Fallback On On On
Alarms Off Enabled Enabled Enabled
AlarmSource Sel. Enabled Enabled Enabled
Va Lead V2 V2 V2
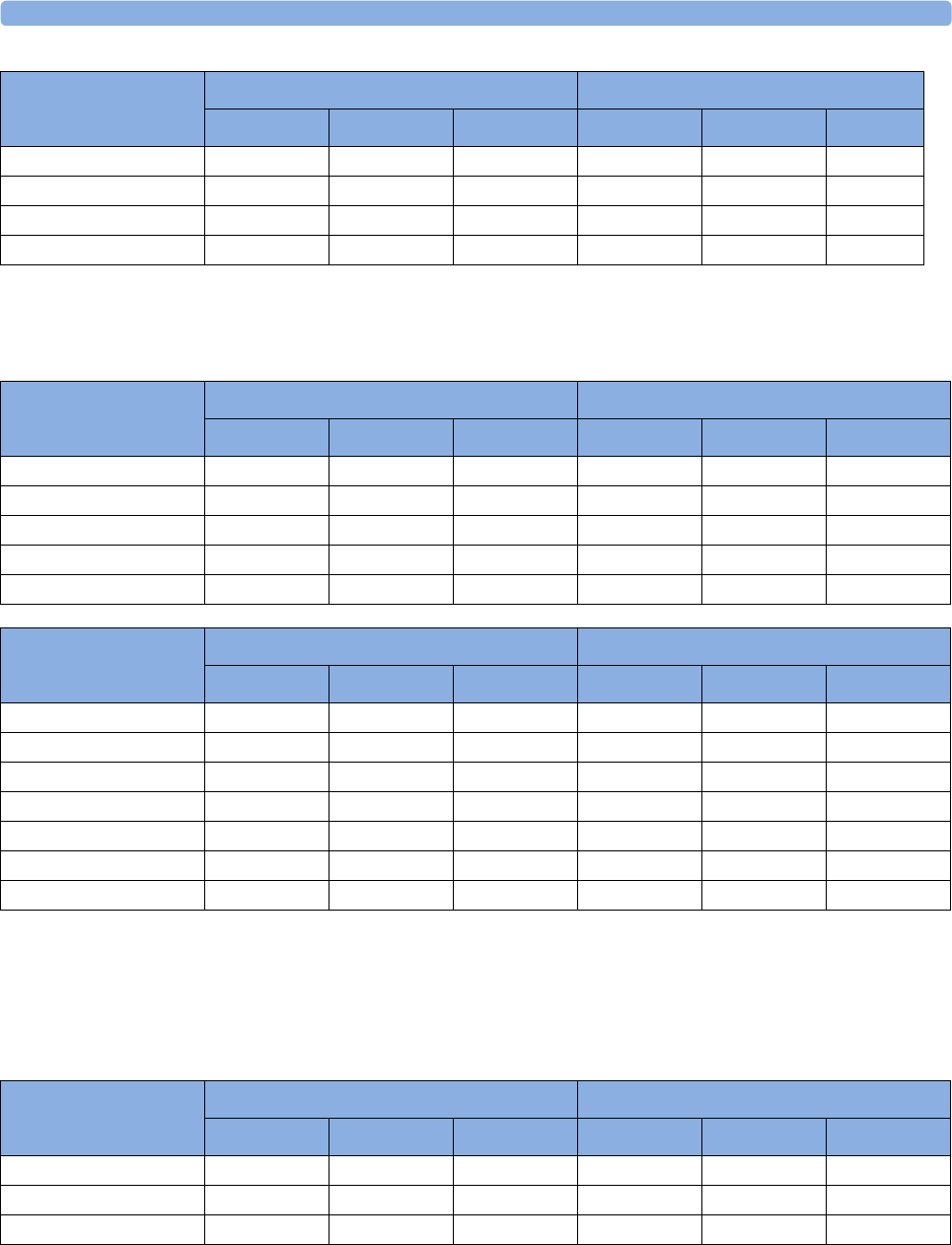
37 Default Settings Appendix
440
Pulse Default Settings
1 When Pulse is not the alarm source, the alarms will be Off.
Pulse alarms use the settings of the currently selected Pulse alarm source.
Respiration Default Settings
Vb Lead V5 V5 V5
SyncPulse Sensit Medium Medium Medium
SyncPulse Marker On On On
PulseAlarms Tele Enabled Enabled Enabled
ECG Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
Pulse Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
Alarm Source Auto Auto Auto Auto Auto Auto
Pulse (source label) On On On
System Pulse SpO₂SpO₂SpO₂Auto Auto Auto
Alarms Off Enabled Enabled Enabled
AlarmSource Sel. Enabled Enabled Enabled
Pulse Alarm Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
Pulse Alarms1On On On
High Limit 120 bpm 160 bpm 200 bpm
Low Limit 50 bpm 75 bpm 100 bpm
Δ ExtrBrady 20 bpm 20 bpm 20 bpm
Brady Clamp 40 bpm40 bpm50 bpm40 bpm60 bpm80 bpm
Δ ExtrTachy 20 bpm 20 bpm 20 bpm
Tachy Clamp 200 bpm 220 bpm 240 bpm
Respiration Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
High Limit 30 rpm 30 rpm 100 rpm
Low Limit 8 rpm 8 rpm 30 rpm
Apnea Time 20 sec 20 sec 20 sec
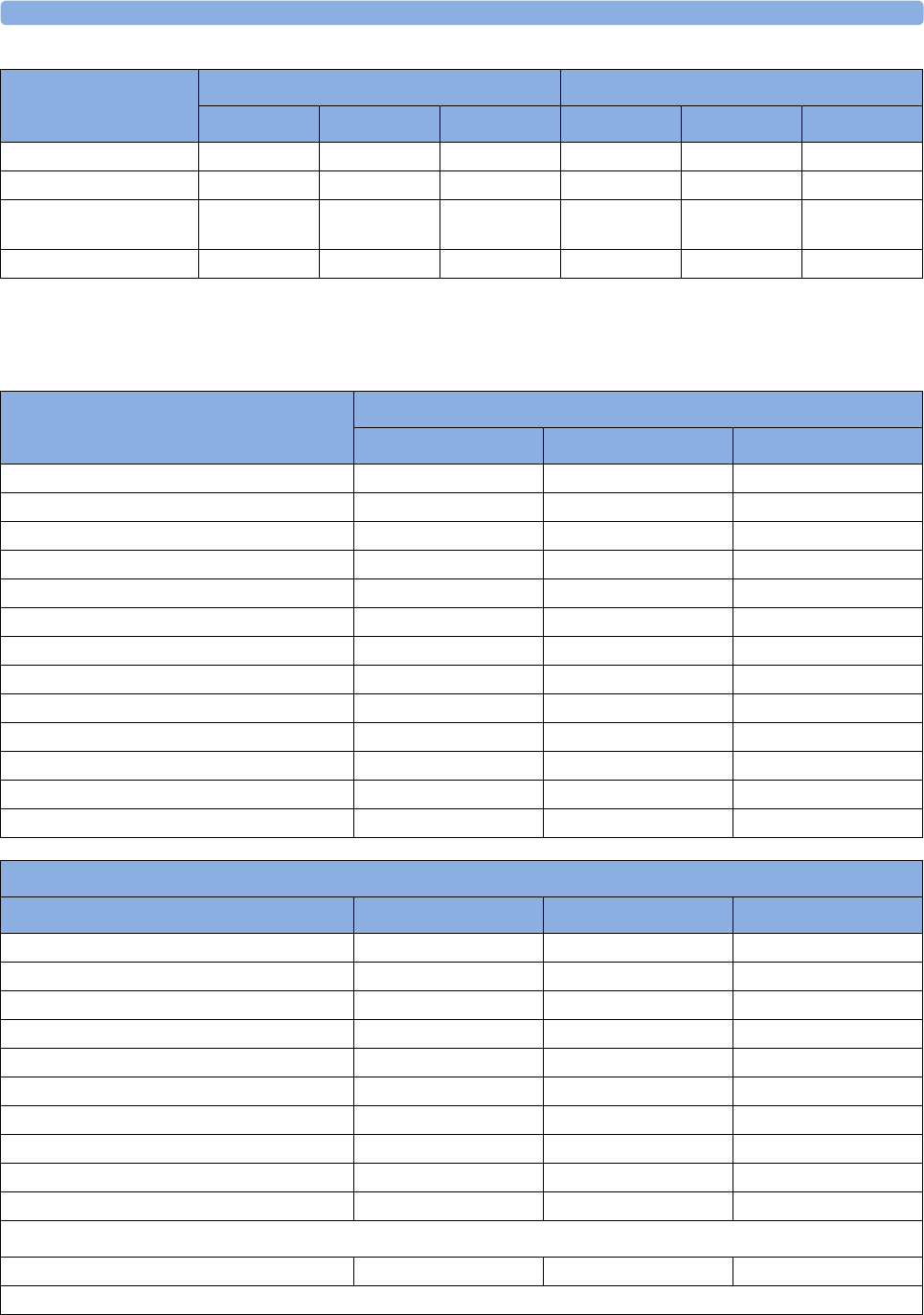
37 Default Settings Appendix
441
SpO2 Default Settings
Alarms On On On
Resp On On On Off Off Off
Detection Auto
(Trigger Mode)
Auto
(Trigger Mode)
Auto
(Trigger Mode)
Color Yellow Yellow Yellow White White White
Respiration Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
SpO2 Settings
Factory Defaults
Adult Pedi Neo
Mode Continuous Continuous Continuous
Repeat Time 15 min 15 min 15 min
Alarms On On On
QRS Volume 111
Tone Modulation Yes Yes Yes
Tone Mod. Type Enhanced Enhanced Enhanced
Perfusion OnOnOn
Average 10 sec 10 sec 10 sec
NBP Alarm Suppr. On On On
Extd. Auto OnOff Disabled Disabled Disabled
Color Cyan (light blue) Cyan (light blue) Cyan (light blue)
Average In Mon. No No No
Signal Quality OnOnOn
SpO2 Alarm Default Settings
Setting Adult Pedi Neo
Desat Limit 80 80 80
Low Limit 90 90 85
High Limit 100 100 95
Desat Delay 20 sec 20 sec 20 sec
High Alarm Delay 10 sec 10 sec 10 sec
Low Alarm Delay 10 sec 10 sec 10 sec
SmartAlarmDelay (SAD) Off Off Off
High Alarm Delay (SAD) Short Short Short
Low Alarm Delay (SAD) Short Short Short
Label SpO₂SpO₂SpO₂
Pulse settings
Pulse (SpO₂) OnOnOn
For all other Pulse default settings, refer to the Pulse Default Settings table.
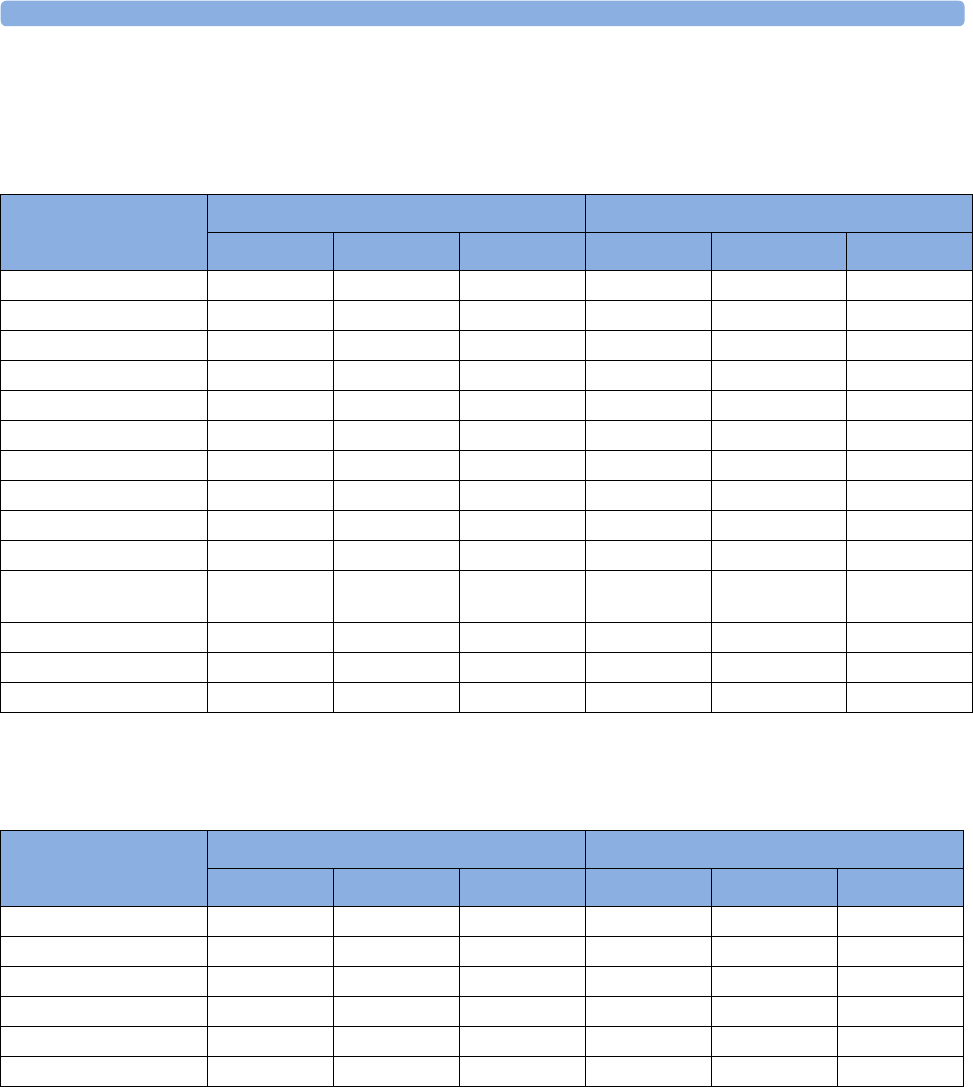
37 Default Settings Appendix
442
NBP Default Settings
Temperature Default Settings
NBP Settings
Factory defaults H10/H20/H30 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
Mode Auto Auto Manual
Alarms from Sys. Sys. Sys.
High Limit 160/90 (110) 120/70 (90) 90/60 (70) 180/90 (110)
Low Limit 90/50 (60) 70/40 (50) 40/20 (24) 70/50 (65)
Alarms On On On
NBP OnOnOn
Repeat Time 10 min 10 min 10 min 3 min 3 min 3 min
Pulse (NBP) OnOnOn
Unit mmHg mmHg mmHg
Done Tone Off Off Off On On
Start Time Synchronize
d
Synchronize
d
Synchronize
d
NotSynchron
.
NotSynchron. NotSynchron
.
VP Pressure 60 mmHg 40 mmHg 30 mmHg
Reference Auscultatory Auscultatory Invasive
Color Red Red Red Magenta Magenta Magenta
Temp Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
Low Limit 36 36 36 35 35 35
High Limit 39 39 39
Alarms On On On
Unit °C °C °C
Range 35...43 35...43 35...43
Color Green Green Green Light Green Light Green Light Green
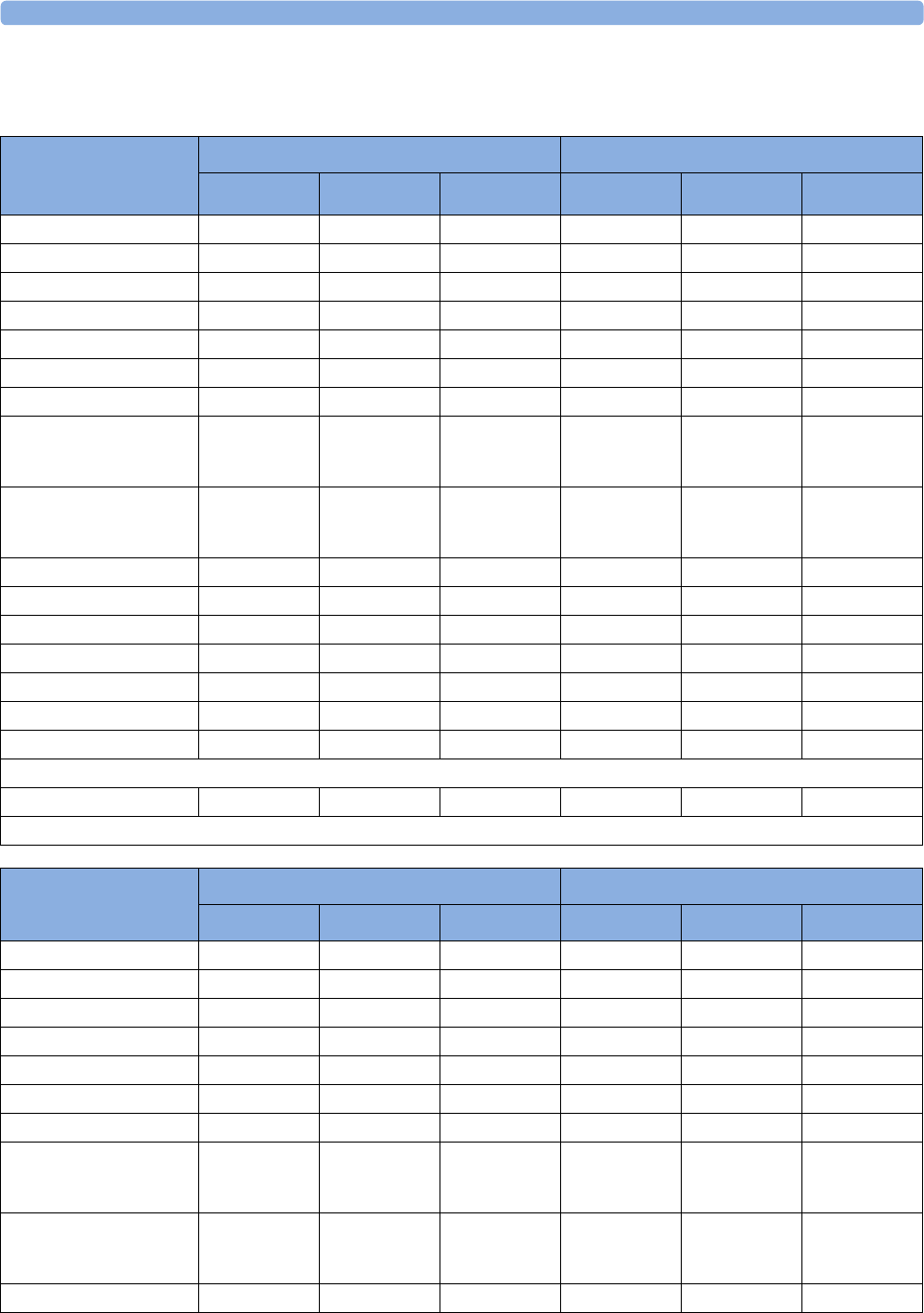
37 Default Settings Appendix
443
Invasive Pressure Default Settings
ABP, P, P1, P2, P3, P4,
UAP, ART, Ao, FAP, BAP
Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
Alarms from Sys. Sys. Sys.
High Limit 160/90 (110) 120/70 (90) 90/60 (70) 180/90 (110)
Low Limit 90/50 (70) 70/40 (50) 55/20 (36) 70/50 (70)
Alarms On On On
Extreme Alarms Disabled Disabled Disabled
Δ Extreme High 15 10 5
Δ Extreme Low 15 10 5
Sys. High Clamp/Dia.
High Clamp (Mean
High Clamp)
190/100 (125) 140/80 (100) 105/75 (75)
Sys. Low Clamp/Dia.
Low Clamp (Mean Low
Clamp)
80/45 (65) 60/35 (45) 45/15 (30) 65/45 (65)
Scale 150 100 100
Mean only No No No
Filter 12 Hz 12 Hz 12 Hz
Mercury Cal Yes Yes Yes
Artifact Suppr. 60 sec 60 sec 60 sec
Unit mmHg mmHg mmHg
Color Red Red Red
Pulse settings for all arterial pressures except P1 to P4
Pulse (Press label) On On On
For all other Pulse default settings, refer to the Pulse Default Settings table.
CVP, RAP, LAP, UVP
Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
Alarms from Mean Mean Mean
High Limit 14/6 (10) 10/2 (4) 10/2 (4)
Low Limit 6/-4 (0) 2/-4 (0) 2/-4 (0)
Alarms On On On
Extreme Alarms Disabled Disabled Disabled
Δ Extreme High 555
Δ Extreme Low 555
Sys. High Clamp/ Dia.
High Clamp (Mean
High Clamp)
20/10 (15) 15/5 (10) 15/5 (10)
Sys. Low Clamp/Dia.
Low Clamp (Mean Low
Clamp)
0/-5 (-5) 0/-5 (-5) 0/-5 (-5)
Scale 30 30 30
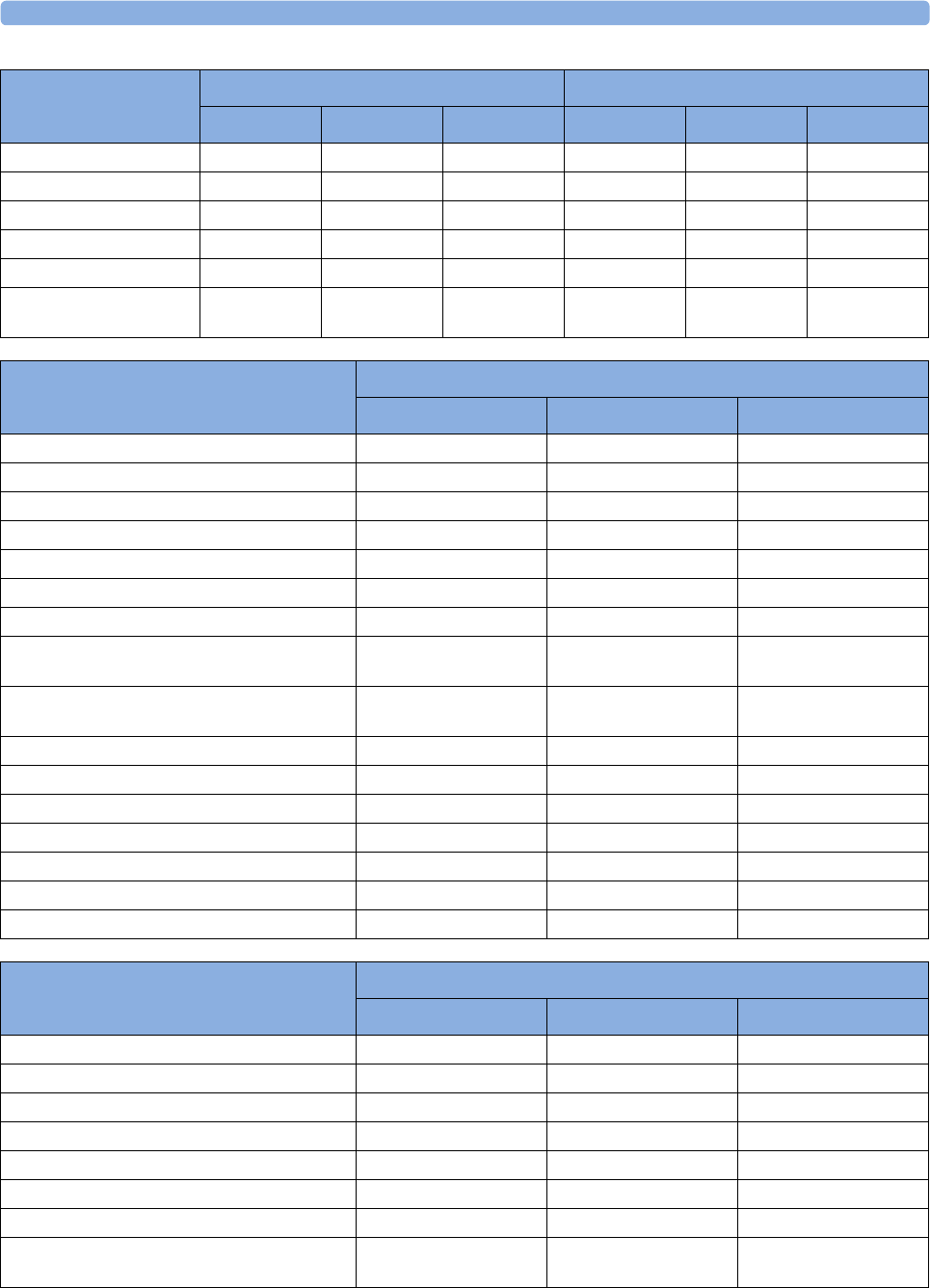
37 Default Settings Appendix
444
Mean only Yes Yes Yes
Filter 12 Hz 12 Hz 12 Hz
Mercury Cal Yes Yes Yes
Artifact Suppr. 60 sec 60 sec 60 sec
Unit mmHg mmHg mmHg
Color Cyan (light
blue)
Cyan (light
blue)
Cyan (light
blue)
Blue Blue Blue
CVP, RAP, LAP, UVP
Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
PAP Settings
Factory Defaults
Adult Pedi Neo
Alarms from Dia. Dia. Dia.
High Limit 34/16 (20) 60/4 (26) 60/4 (26)
Low Limit 10/0 (0) 24/-4 (12) 24/-4 (12)
Alarms On On On
Extreme Alarms Disabled Disabled Disabled
Δ Extreme High 555
Δ Extreme Low 555
Sys. High Clamp/Dia. High Clamp (Mean
High Clamp)
45/20 (25) 65/5 (35) 65/5 (35)
Sys. Low Clamp/Dia. Low Clamp (Mean
Low Clamp)
5/-5 (-5) 15/-5 (5) 15/-5 (5)
Scale 30 30 30
Mean only No No No
Filter 12 Hz 12 Hz 12 Hz
Mercury Cal Yes Yes Yes
Artifact Suppr. 60 sec 60 sec 60 sec
Unit mmHg mmHg mmHg
Color Yellow Yellow Yellow
ICP, IC1, IC2 Settings
Factory Defaults
Adult Pedi Neo
Alarms from Mean Mean Mean
High Limit 14/6 (10) 10/2 (4) 10/2 (4)
Low Limit 6/-4 (0) 2/-4 (0) 2/-4 (0)
Alarms On On On
Extreme Alarms Disabled Disabled Disabled
Δ Extreme High 10 10 10
Δ Extreme Low 10 10 10
Sys. High Clamp/Dia. High Clamp (Mean
High Clamp)
20/10 (15) 15/5 (10) 15/5 (10)
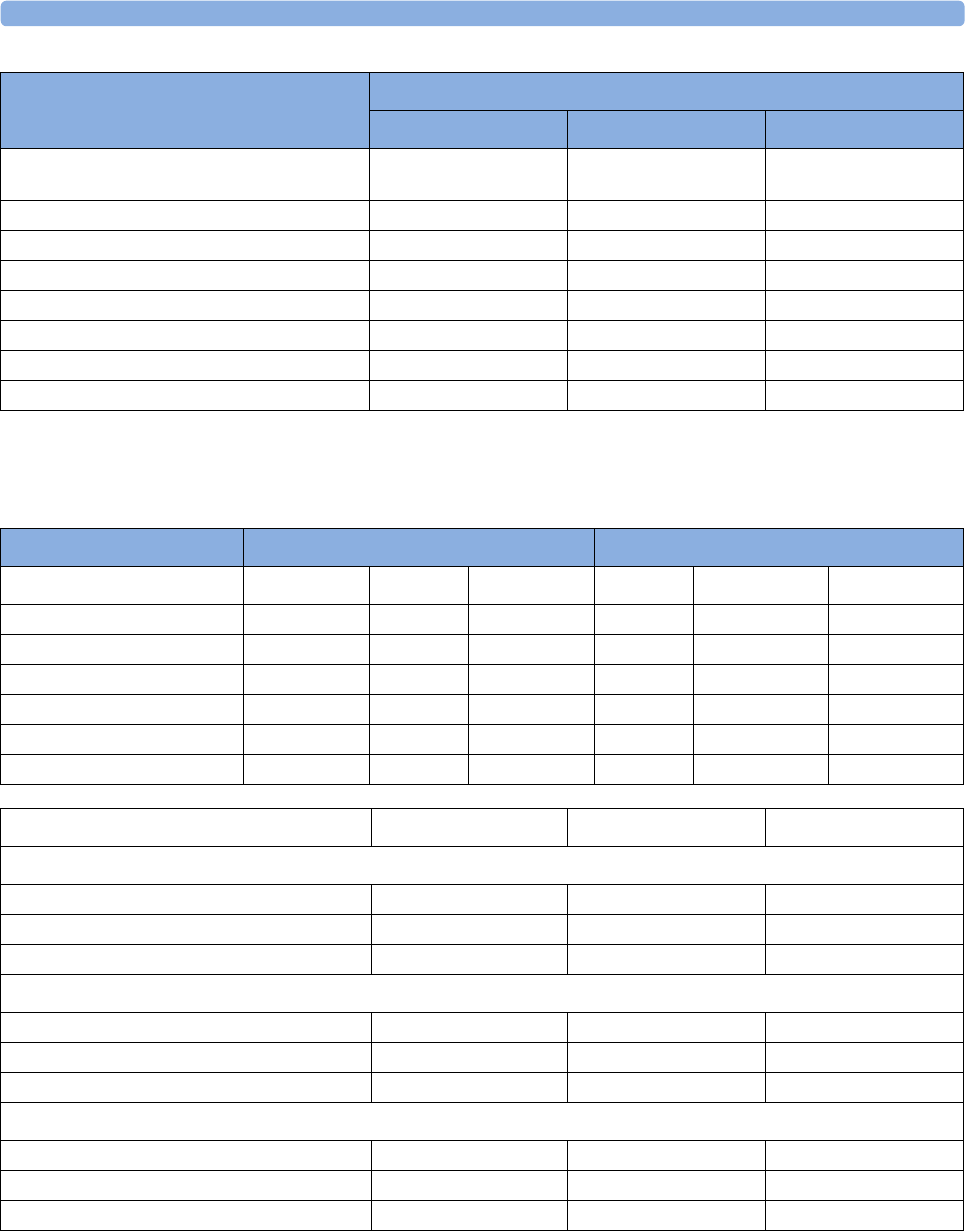
37 Default Settings Appendix
445
Cardiac Output Default Settings
Sys. Low Clamp/Dia. Low Clamp (Mean
Low Clamp)
0/-5 (-5) 0/-5 (-5) 0/-5 (-5)
Scale 30 30 30
Mean only Yes Yes Yes
Filter 12 Hz 12 Hz 12 Hz
Mercury Cal Yes Yes Yes
Artifact Suppr. 60 sec 60 sec 60 sec
Unit mmHg mmHg mmHg
Color Magenta Magenta Magenta
ICP, IC1, IC2 Settings
Factory Defaults
Adult Pedi Neo
C.O. Settings Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
Auto-Calibration On On On
Tblood HighLimit 39.0°C 39.0°C 39.0°C
Tblood Low Limit 36.0°C 36.0°C 36.0°C
Tblood Alarms On On On
Temperature Unit °C °C °C
Color Green Green Green Yellow Yellow Yellow
CCO/CCI Settings Factory Adult Factory Pedi Factory Neo
Settings common to CCO and CCI
Alarms From CCO CCO CCO
CCO From ABP ABP ABP
Color Green Green Green
CCO
Alarms On On On
CCO High Limit 8.5 l/min 3.7 l/min 1.3 l/min
CCO Low Limit 4.0 l/min 2.6 l/min 0.3 l/min
CCI
Alarms On On On
CCI High Limit 4.3 l/min/m2 4.3 l/min/m2 5.2 l/min/m2
CCI Low Limit 2.0 l/min/m2 2.6 l/min/m2 1.2 l/min/m2
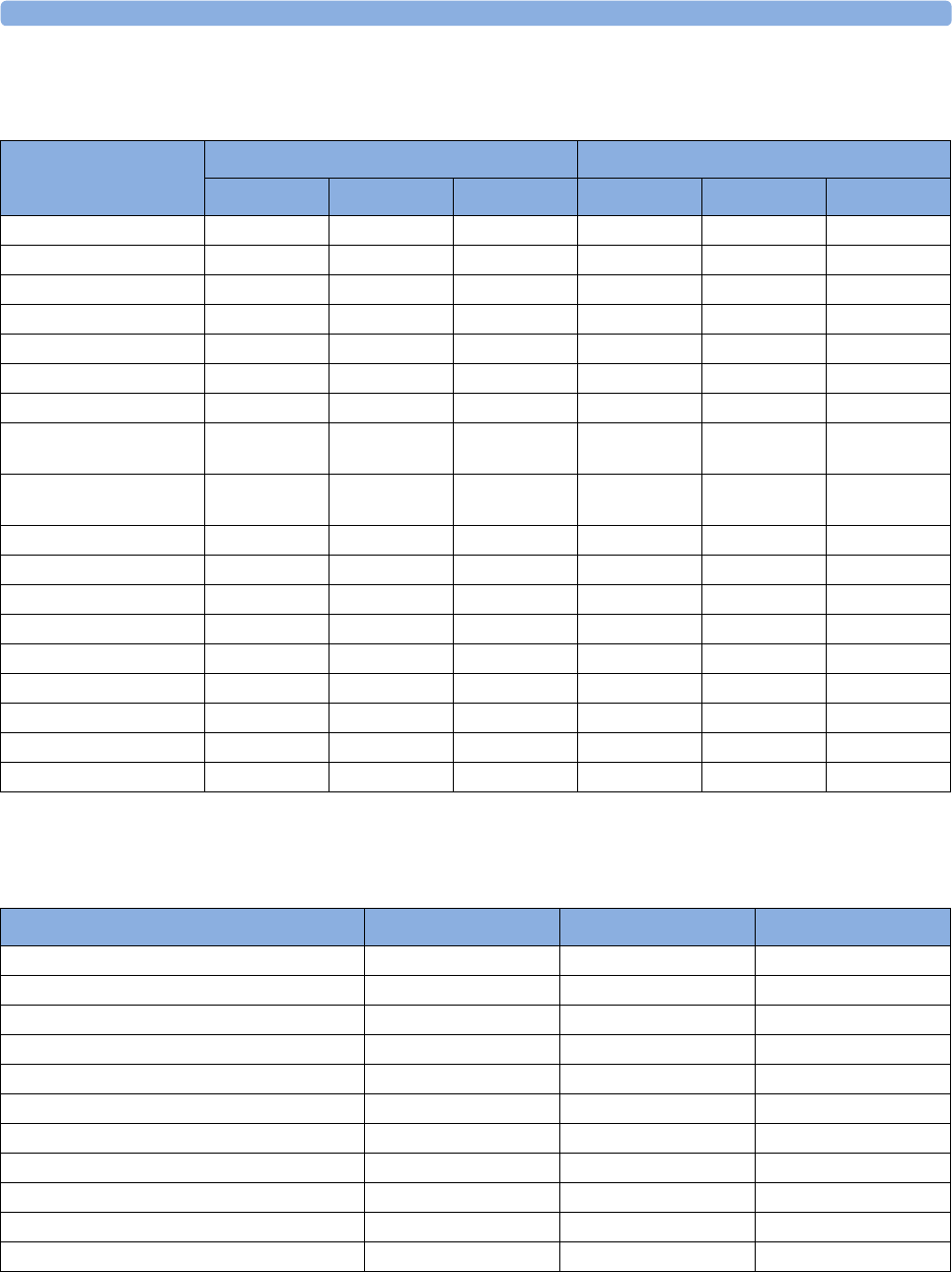
37 Default Settings Appendix
446
CO2 Default Settings
Spirometry Default Settings
CO2 Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
etCO₂ Low 30 30 30 25 25 25
etCO₂ High 50 50 50 60 60 60
imCO₂ High 444
CO₂ Alarms On On On
Unit mmHg mmHg mmHg
Scale 40 mmHg 40 mmHg 40 mmHg 50 50 50
imCO₂On On On Off Off Off
N₂O Corr. (only
M3015A/M3016A)
Off Off Off
Oxygen Corr. (only
M3014A)
16% 16% 16%
Gas Corr. (only M3014A) Off Off Off
Humidity Corr. BTPS BTPS BTPS
Max Hold Off Off Off
awRR On On On
awRR Alarms On On On
High Limit (awRR) 30 30 60
Low Limit (awRR)8830
Apnea Time 20 sec 20 sec 20 sec
Color Yellow Yellow Yellow White White White
Spirometry Settings Factory Adult Factory Pedi Factory Neo
Apnea Time 20 20 20
MVexp Low 4.0 l/min 2.5 l/min 0.4 l/min
MVexp High 8.0 l/min 4.0 l/min 0.8 l/min
PIP High 40 25 20
PEEP Low 000
PEEP High 25 25 25
High Limit (RRspir)8830
Low Limit (RRspir)303060
Scale (AWF) ±150 l/min ±100 l/min ±20 l/min
Scale (AWV) ±800 ml ±200 ml ±50 ml
Scale (AWP) ±40 cmH2O ±40 cmH2O±20 cmH
2O
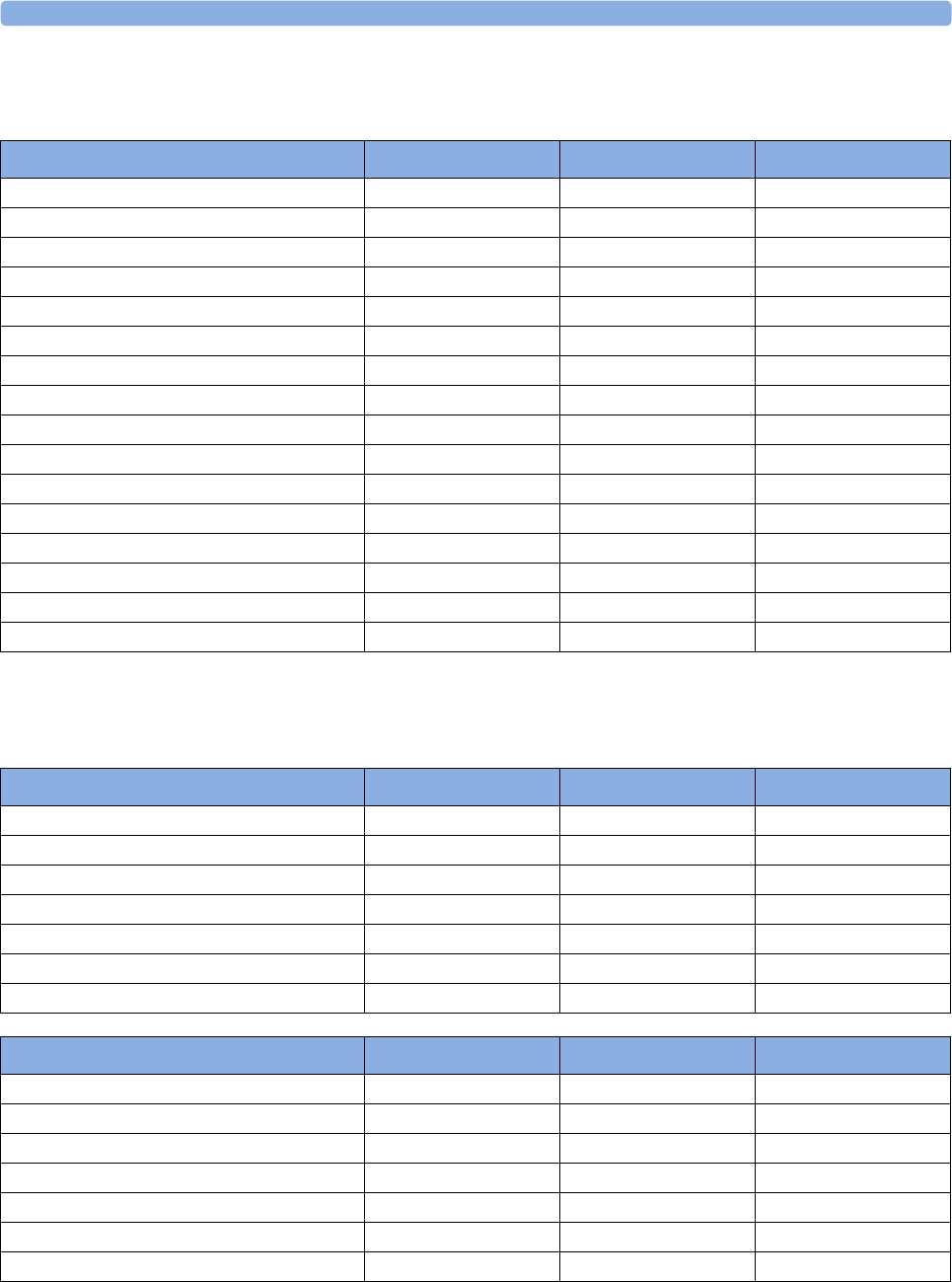
37 Default Settings Appendix
447
tcGas Default Settings
Intravascular Oxygen Saturation
tcGas Settings Factory Adult Factory Pedi Factory Neo
tcpO₂ High Limit 80 mmHg 80 mmHg 80 mmHg
tcpO₂ Low Limit 50 mmHg 50 mmHg 50 mmHg
tcpO₂ Alarms On On On
tcpCO₂ HighLimit 50 mmHg 50 mmHg 50 mmHg
tcpCO₂ Low Limit 30 mmHg 30 mmHg 30 mmHg
tcpCO₂ Alarms On On On
Site Timer 4.0 hours 4.0 hours 4.0 hours
Disable Timer Not Allowed Not Allowed Not Allowed
Heat Switch Off (i.e., after Site Timer elapsed) No No No
Transducer Temp. 43.0°C 43.0°C 43.0°C
CO₂ Correction (Severinghaus) On On On
MetabolismFactor 8 mmHg 8 mmHg 8 mmHg
tcGas Unit mmHg mmHg mmHg
Temperature Unit °C °C °C
tcpO₂ Color Blue Blue Blue
tcpCO₂ Color Green Green Green
SO2 Settings Factory Adult Factory Pedi Factory Neo
Low Limit 70% 70% 70%
HR High Limit 80% 80% 80%
Alarms On On On
Light Intensity On On On
Color Yellow Yellow Yellow
Hb/Hct Entry Hct [%] Hct [%] Hct [%]
Factor Entry Disabled Disabled Disabled
SvO2 Settings Factory Adult Factory Pedi Factory Neo
Low Limit 60% 60% 60%
High Limit 80% 80% 80%
Alarms On On On
Light Intensity On On On
Color Yellow Yellow Yellow
Hb/Hct Entry Hct [%]
Factor Entry Disabled
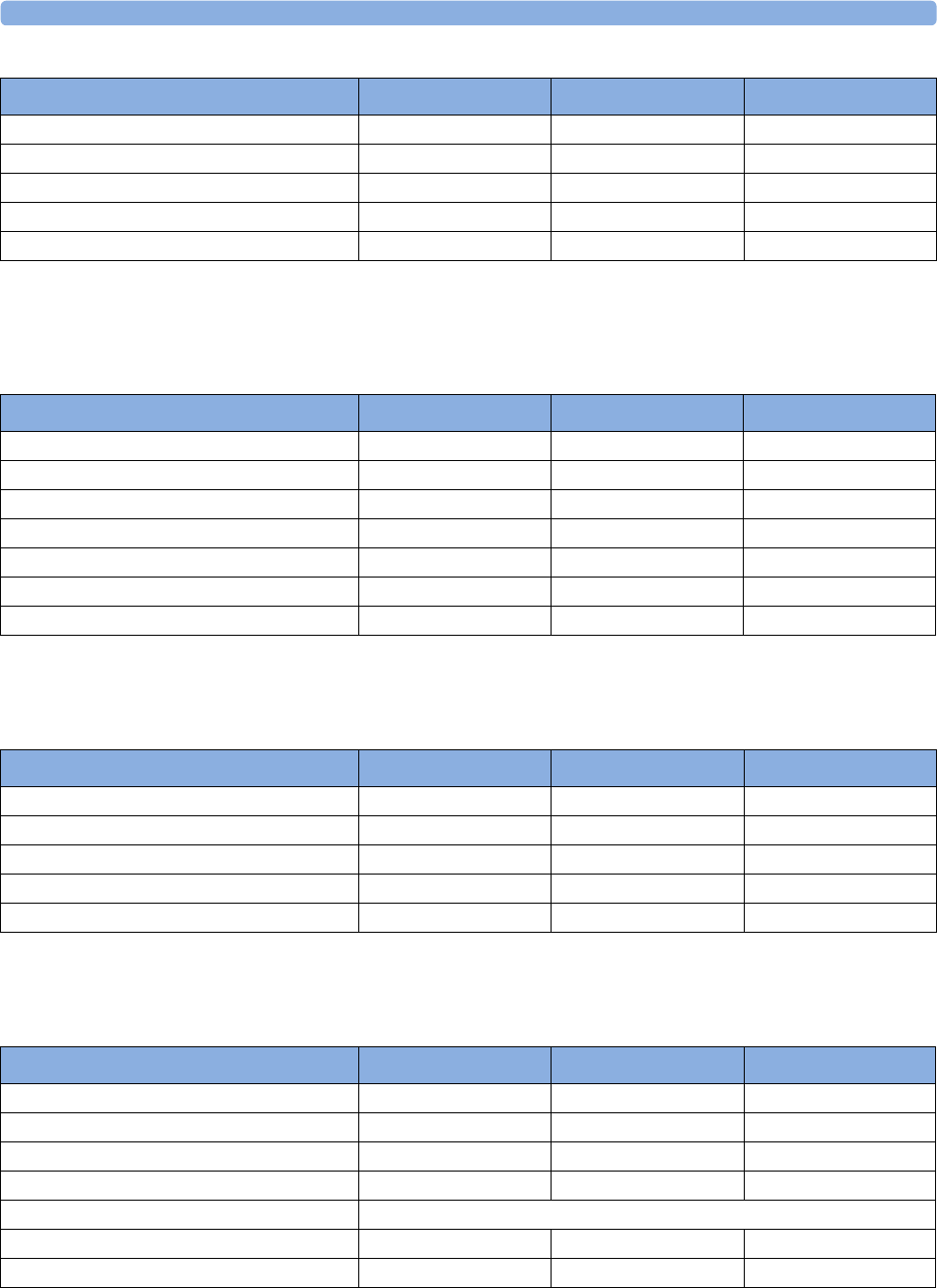
37 Default Settings Appendix
448
SvO2 Default Settings
ScvO2 Default Settings
EEG Default Settings
ScvO2 Settings Factory Adult Factory Pedi Factory Neo
Low Limit 70% 70% 70%
High Limit 80% 80% 80%
Alarms On On On
Light Intensity On On On
Color Yellow Yellow Yellow
SvO2 Settings Factory Adult Factory Pedi Factory Neo
Low Limit 60% 60% 60%
High Limit 80% 80% 80%
Alarms On On On
Light Intensity On On On
Color Yellow Yellow Yellow
Hb/Hct Entry Hct [%]
Factor Entry Disabled
ScvO2 Settings Factory Adult Factory Pedi Factory Neo
Low Limit 70% 70% 70%
High Limit 80% 80% 80%
Alarms On On On
Light Intensity On On On
Color Yellow Yellow Yellow
EEG Settings Factory Adult Factory Pedi Factory Neo
TP, SEF OnOnOn
MDF, PPF, Delta, Theta, Alpha, Beta Off Off Off
SEF Threshold 90% 90% 90%
Numeric Average 8 sec 8 sec 8 sec
Wave Scale 100µV (or +/- 50µV if Show Gridlines is configured to Yes)
Show Gridlines No No No
Low Filter 0.5 Hz 0.5 Hz 0.5 Hz
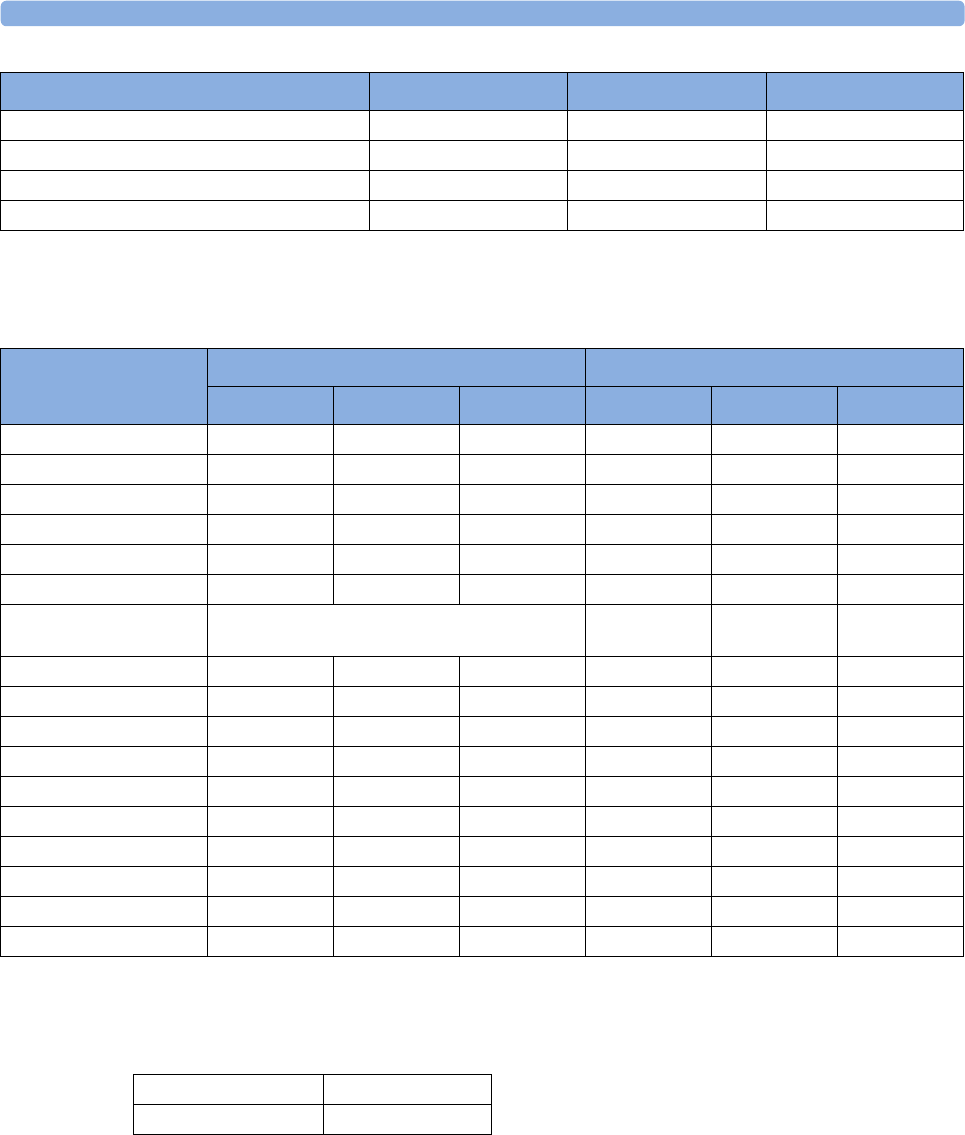
37 Default Settings Appendix
449
BIS Default Settings
VueLink Default Settings
High Filter 30 Hz 30 Hz 30 Hz
Impedance Limit 5 kOhm 5 kOhm 5 kOhm
Smoothing CSA On On On
Color Yellow Yellow Yellow
EEG Settings Factory Adult Factory Pedi Factory Neo
BIS Settings
Factory defaults H10/H20/H40 H30 (deviations from H10/H20/H40)
Adult Pedi Neo Adult Pedi Neo
SQI OnOnOn
EMG OnOnOn
SR On On On
SEF Off Off Off
TP Off Off Off
Bursts On On On Off Off Off
Scale 100µV (or +/- 50µV if Show Gridlines is
configured to Yes)
Show GridlinesNoNoNo
Filters OnOnOn
Low Filter 2 Hz 2 Hz 2 Hz
High Filter 70 Hz 70 Hz 70 Hz
Notch Filter On On On
High Limit 70 70 70
Low Limit 20 20 20
Alarms On On On
Smoothing Rate 30 sec 30 sec 30 sec 15 sec 15 sec 15 sec
Color Yellow Yellow Yellow Magenta Magenta Magenta
Device Alarms Ignored
Color Green
449
1Index
#
10-Electrode (5+5)Cable Sets 370
10-Electrode (6+4)Cable Sets 370
10-Lead Placement 120
3-Electrode Cable Sets 370, 371
3-Electrode One Piece Cables 372
4-Slot Flexible Module Rack (FMS-4) 16
5-Electrode Cable Sets 370, 372
5-Electrode One Piece Cables 372
6-Electrode Cable Sets 370
6-Lead Placement 119
A
Abdominal Breathing 160
Aberrantly-Conducted Beats 131
About Arrhythmia Monitoring 129
About Automatic Alarm Limits 59
About Compressed Spectral Arrays
(CSA) 252
About ECG Leads 116
About Electrode-to-Skin Impedance 251
About Label Sets 39
About QT/QTc Interval Monitoring 149
About Smart Alarm Delays 59, 169
About ST Monitoring 139
About the Rule of Six 338
About the ST Measurement Points 143
Accessing the Drug Calculator 338
Accessing the Setup C.O. and Setup CCO
Menus 197
Accessories 369
Accessories Compliant with EMC
Standards 425
Acknowledging Alarms 53
Acknowledging Disconnect INOPs 53
Activating the Cursor for Screen
Trends 279
Adjusting a Measurement Wave 37
Adjusting ST Measurement Points 143
Adjusting the Alarm Limits 170
Adjusting the Arrhythmia Alarm
Limits 136
Adjusting the Calibration Factor 186
Adjusting the CO2 Wave Scale 222
Adjusting the Desat Limit Alarm 171
Adjusting the iPC Audio Volume 46
Adjusting the Screen Brightness 43
Admitting a Centrally-Monitored
Patient 96
Admitting a Patient 95
Adult Mode 229
Adult/Pediatric Reusable Comfort Cuff
Kits 373
Adult/Pediatric Reusable Comfort
Cuffs 373
Adult/Pediatric Reusable EasyCare
Cuffs 373
Adult/Pediatric Single Patient Cuffs 374
Adult/Pediatric Single Patient, Soft
Cuffs 374
After Insertion 246
Alarm and Measurement Default
Settings 436
Alarm Behavior at Power On 62
Alarm Default Settings 436
Alarm Delays 169
Alarm Lamp 50
Alarm Latching Behavior 62
Alarm Limits 56
Alarm Limits Report 333
Alarm Message 50
Alarm Messages Window 60
Alarm Recordings 63
Alarm Reminder 54
Alarm Source Selection Disabled 157
Alarm Sources 176
Alarm Tone Configuration 51
Alarms 49
Alarms and Alarm Limits 230
Alarms/INOPs From External Devices 350
Alarms/INOPs from External Devices 345
All ECG Waves Recordings 319
Altitude Setting 393
Always Discharge Patients 316
Annotating Events 301
Aperiodic Trends Database 278
Applying the Sensor 165
Applying the tcGas Transducer 237
Arrhythmia Alarm Chaining 138
Arrhythmia Alarm Timeout Periods 136
Arrhythmia Alarms 135
Arrhythmia Alarms and Latching 136
Arrhythmia Beat Labels 132
Arrhythmia Options 130
Arrhythmia Relearn and Lead Fallback 135
Arrhythmia Relearning 134
Arrhythmia Status Messages 132
Assessing a Suspicious SpO2 Reading 168
Assigning a Telemetry Device and a
Monitor to One Patient 265
Assisting Venous Puncture 179
Atrial Fibrillation Alarm 131
Attaching and Removing the CO2
Transducer 219
Attaching the Flow Sensor 226
Audible Alarm Indicators 51
Authorized Clinician Review 313
Auto Detection Mode 160
Automatic Alarm Suppression 231
Automatic Arrhythmia Relearn 135
Automatic Purging 228
Automatic Unit Conversion 286
Automatic Value Substitution 286
Automatically Resolving Patient
Mismatch 105
Avoiding Electromagnetic Interference
(Resp and BIS) 425
Avoiding Pace Pulse Repolarization
Tails 114
B
Battery Accessories 386
Battery INOPs 73
BIS 424
BIS Accessories 385
BIS Continuous Impedance Check 259
BIS Cyclic Impedance Check 260
BIS Default Settings 447
BIS Impedance Indicators 261
BIS INOPs 87
BIS Manufacturer's Information 388
BIS Monitoring Setup 257
BIS Safety Information 262
BIS Window 260
Bright Alarm Limits 50
BSA Formula 286

450
C
C.O. Injectate Guidelines 206
C.O. INOPs 84
C.O./CCO Curve Alert Messages 207
C.O./CCO Prompt Messages 209
C.O./CCO Safety Information 210
C.O./CCO Warning Messages 209
Cableless Measurement Device INOPs 92
Calculated Values INOPs 92
Calculating Cerebral Perfusion
Pressure 191
Calculating Oxygen Extraction 247
Calculating Pulse Pressure Variation 191
Calculating SpO2 Difference 172
Calculating Temp Difference 182
Calculations 283
Calculations Pop-Up Keys 284
Calculations Windows 284
Calibrating NBP 179
Calibrating Reusable Transducer
CPJ840J6 189
Calibrating the tcGas Transducer 235
Calibrating the Transducer 219
Calibration Failure 236
Capture 12-Lead 123
Capture 12-Lead Pop-up Keys 125
Capturing and Deleting Loops 356
Capturing the 12-Lead ECG 123
Cardiac Output (C.O.) Accessories 381
Cardiac Output / Continuous Cardiac
Output 421
Cardiac Output Default Settings 443
Cardiac Output Report 335
Cardiac Overlay 159
Care and Cleaning 361
Care Group Alarms 110
Care Groups 105
Carrying out a Pre-insertion
Calibration 243
CCO Calibration Status Indicators 202
Central Recording 317
Changing a Screen's Content 32
Changing Alarm Limits 57
Changing awRR Alarm Limits 224
Changing CO2 Alarms 223
Changing Conditions 312
Changing CSA Settings 253
Changing ECG Wave Gain 321
Changing EEG Settings 253
Changing Filter Frequencies 254
Changing HR/Pulse Alarm Limits 157
Changing Lead Sets 117
Changing Loops Display Size 356
Changing Loops Type 357
Changing Measurement Labels (e.g.
Pressure) 39
Changing Measurement Settings 36
Changing Monitor Settings 42
Changing QTc Alarm Limits 153
Changing Resp Detection Modes 160
Changing ST Alarm Limits 145
Changing the Alarm Tone Volume 52
Changing the Apnea Alarm Delay 162, 223,
230
Changing the Averaging Time 168
Changing the BIS Smoothing Rate 261
Changing the Concentration of Inspired
O2 and the Inspired Agents 232
Changing the ECG Filter Settings 115
Changing the Hi-Res Trend Waves
Displayed 289
Changing the Impedance Limit 251
Changing the Lab Value Required for
Entry 246
Changing the Pressure Wave Scale 187
Changing the Scale of the EEG Wave 262
Changing the Scale of the EEG Waves for
Display 253
Changing the Scale of the ST Map 148
Changing the Screen Trend View 280
Changing the Selection of Screen Trends
Displayed 279
Changing the Size of the ECG Wave 114
Changing the Size of the Respiration
Wave 161
Changing the Speed of the EEG Wave 254
Changing the Speed of the Respiration
Wave 162
Changing the Temperature of the Inspired
Gas 232
Changing the Trending Interval 149
Changing the Type of Balance Gas 231
Changing The View To A Single Wave
Set 151
Changing the Volume of the QRS
Tone 115
Changing the Wave Group Speed 37
Changing The Wave Speed 38
Changing VueLink Waves and Numerics
Displayed 348
Changing Wave Speed for a Channel 37
Changing Wave Speeds 37
Changing Waves and Numerics
Displayed 344
Charting Infusion Progress 340
Checking Paced Status 112
Checking Printer Settings 329
Checking Report Status and Printing
Manually 330
Checking Suspicious Values 247
Checking The Sepsis Resuscitation Bundle
Window 314
Checking Transducer Accuracy 219
Checking Your Monitor Revision 43
Chest Electrode Placement 120
Choosing an ECG Lead for Arrhythmia
Monitoring 130
Choosing an EEG Electrode Montage 250
Choosing EASI or Standard Lead
Placement 116
Choosing Measured AWV
Components 231
Choosing Standard or Modified Electrode
Placement 122
Choosing the NBP Alarm Source 178
Choosing the Pressure Alarm Source 188
Cleaning the Monitor 362
Cleaning the Recorder Printhead (M1116B
only) 363
Cleaning the SO2 Optical Module 363
Cleaning, Sterilizing and Disinfecting
Monitoring Accessories 363
CO2 415
CO2 Default Settings 444
CO2 INOPs 82
Comparing Dynamic Compliance
Values 287
Configuration 170
Connecting Additional Displays to the
Monitor 33
Connecting an External Device 343, 348
Connecting ECG Cables 111
Connecting SpO2 Cables 166
Connecting the Optical Module 246
Connectors 390
Controlling the Telemetry Device from the
Bedside 267
Conventional 12-Lead ECG 121
Correcting the Measurement if Limb is not
at Heart Level 175
Counting Combi-Events 299
Counting Neonatal Event Review (NER)
Events 299
Country-Specific Default Settings 429
Creating and Changing Recordings
Templates 320

451
Current View 146
D
Dashed Lines on Reports 329
Data Exchange Between Information
Centers 102
Data Upload from an MMS 102
Default Profile 35
Default Settings Appendix 429
Defining the Column Interval Using the
NBP Measurement 277
Deriving Alarms From awRR 224
Determining a Pressure's Most Recent
Zero 185
Devices for Acquiring Measurements 15
Direct Connection - Automatic
Pairing 266
Disabling the tcGas Site Timer 235
Disabling Touchscreen Operation 26
Discharging a Patient 97
Disconnecting from Power 45
Disinfecting the Monitor 362
Display INOPs 75
Displaying A Clock On The Main
Screen 354
Displaying a Mean Pressure Value
Only 187
Displaying a Timer On The Main
Screen 353
Displaying an ST Reference Baseline 148
Disposing of Empty Calibration Gas
Cylinders 367
Disposing of the Monitor 367
Documenting Alarm Limits 60
Documenting an Event Episode 301
Documenting C.O. Measurements 206
Documenting Calculations 287
Documenting Drug Calculations 341
Documenting Event Review 301
Documenting Events 301
Documenting Loops 357
Documenting Trends 278
During Measurements 176
E
EASI ECG Lead Placement 125
EASI Electrode Placement 126
ECG Alarms Off Disabled 128
ECG and Arrhythmia Alarm Overview 126
ECG Lead Fallback 117
ECG Lead Placements 117
ECG Leads Monitored 117
ECG Reports 335
ECG Safety Information 128
ECG Source Tracking at the Information
Center 268
ECG, Arrhythmia, QT and ST INOPs 75
ECG, Arrhythmia, ST and QT Default
Settings 437
ECG, Arrhythmia, ST and QT
Monitoring 111
ECG/Arrhythmia/ST/QT 405
ECG/Resp Accessories 369
Ectopic Status Messages 133
Editing and Saving RH C.O.
Measurements 205
Editing Patient Information 97
Editing PiCCO C.O. Measurements 202
Editing the Wedge 193
EEG 423
EEG Accessories 385
EEG and Electrical Interference 255
EEG Default Settings 446
EEG INOPs 87
EEG Monitoring Setup 249
EEG Reports 254
EEG Safety Information 254
Electromagnetic Compatibility (EMC)
Specifications 425
Electromagnetic Emissions 425
Electromagnetic Immunity 425
Electrosurgery Interference/Defibrillation/
Electrostatic Discharge 428
EMC And Radio Regulatory
Compliance 393
Enabling Automatic Mode and Setting
Repetition Time 178
Enabling Sequence Mode and Setting Up
The Sequence 178
Ending The Sepsis Management
Bundle 315
Ending The Sepsis Resuscitation
Bundle 314
Enhanced Asystole Detection 128
Entering Measurements Manually 42
Entering the HemoCalc Window 198
Entering the Setup Pulse Menu 155
Entering Values for Calculations 286
Environmental Specifications 397
Event Episode Recordings 303
Event Episode Reports 305
Event Episode Window 300
Event Episodes 292
Event Groups 292
Event Notification 296
Event Recordings 301
Event Reports 304
Event Retriggering 295
Event Review Recordings 301
Event Review Reports 304
Event Review Window 300
Event Summary and Event Counter 298
Event Summary Reports 306
Event Summary Window 299
Event Surveillance 291
Event Triggers 294
Events Pop-Up Keys 293
Example Module (SpO2) 17
Examples 169
Expanded View 275
Extended Pressure Label Set 184
Extended Temperature Label Set 182
Extending Recordings 318
Extending the Alarm Pause Time 55
Extreme Alarm Limits for Heart Rate 127,
157
Extreme Alarm Limits for Pressure 188
F
Fast Transients/Bursts 428
Finishing tcGas Monitoring 238
Flashing Numeric 50
Flexible Module Rack (M8048A) 15
Freezing All Waves 38
Freezing An Individual Wave 38
Freezing Waves 38
Functions Available When the Telemetry
Data Window is Displayed 267
Further Information for Both Modules 247
G
Gas Compensation 229
General Points 361
General Telemetry-related Functions 268
Getting Started 43
Graphical Trend Presentation 277
Guidelines for PiCCO C.O. Injectate 206
Guidelines for Right Heart Thermodilution
C.O. Injectate 206
H
Hardkeys 29
Hemodynamic Parameters 195
High ETVI 206
High Resolution Trend Waves 289
452
Hi-Res Trend Wave Recordings 290
Hi-Res Trend Wave Scales 289
Hi-Res Trend Waves and OxyCRG 289
Histogram View 280
Horizon View 280
How are Yellow Arrhythmia Alarms
Indicated? 137
How Can You Combine Devices? 265
HR Alarms When Arrhythmia Analysis is
Switched Off 128
Hypotension Evaluation 312
I
Ice-Bath Setup for RH Thermodilution
C.O. Measurements 205
Identifying tcGas Module
Components 233
Identifying the Pressure Analog Output
Connector 193
If You Set "On Measurement" Triggers 295
If You Set Use-defined Deviation
Triggers 295
If You Set User-defined Threshold
Triggers 295
If You Use Alarm Limits As Event
Triggers 295
Impedance Indicators 252
Indications For Use Of QT Interval
Monitoring 150
Indirect Connection - Manual Pairing 265
Initiating Arrhythmia Relearning
Manually 134
Injectate Volume, Patient Weight and
ETVI Values (PiCCO Only) 206
INOPs from the IntelliBridge Module 345
Inserting the Catheter 244
Inspecting the Cables and Cords 366
Inspecting the Equipment and
Accessories 365
Inspecting the Monitor 44
Installation Safety Information 390
IntelliBridge EC10 Module 343
IntelliBridge INOPs 90
IntelliVue 802.11 Bedside Adapter (Option
J35 Wireless Network Adapter) 394
IntelliVue Instrument Telemetry ISM
(2.4GHz) 394
IntelliVue Instrument Telemetry WMTS
(US only) 395
Intended Use 387
Interface Specifications 401
Interfering Gas and Vapor Effects On CO2
Measurement Values 418
Intermittent Bundle Branch Block 131
Intravascular Oxygen Saturation 423, 445
Introducing the Monitor 13
Introducing the Oscillometric NBP
Measurement 173
Introduction 13
Invasive Pressure Accessories 375
Invasive Pressure Alarm Specifications 414
Invasive Pressure and Pulse 413
Invasive Pressure Default Settings 441
ISO/IEC Standard Audible Alarms 52
L
Label Compatibility 41
Laboratory Data 359
Lactate Measurement 312
Language Conflict with External Device
Drivers 345, 350
Latching Alarms 61
Lateral Chest Expansion 160
Lead Placement for Monitoring Resp 159
Left side of the Monitor 392
Levels of Event Surveillance 291
Limitations For Use Of QT Interval
Monitoring 150
Locked Profiles 36
M
M3012A Hemodynamic MMS
Extension 24
M3014A, M3015A, M3015B and M3016A
Capnography MMS Extensions 22
Main Screen Timer Pop-up Keys 354
Mainstream CO2 Accessories 382
Mainstream CO2 Accessories (for
M3016A) 383
Maintaining Recording Strips 322
Maintenance and Troubleshooting 365
Maintenance Task and Test Schedule 366
Major Parts and Keys 14
Making a Temp Measurement 181
Making Segment Settings 274
Making the In-Vivo Calibration 245
Making the Pressure Calibration 189
Managing Patients 95
Manual Detection Mode 161
Manual Purging 229
Manual Unit Conversion 286
Manually Resolving Patient Mismatch 103
Manufacturer's Information 259, 387
Measurement Limitations 174
Measurement Modes 174
Measurement Modules 16
Measurement of CO2 and Spirometry with
Neonates 384
Measurement Principles 214
Measurement Specifications 405
Measuring C. O. Using the PiCCO
Method 198
Measuring C.O. Using the Right Heart
Thermodilution Method 203
Measuring CO2 using M3014A or X2 214
Measuring Continuous Cardiac
Output 198
Measuring Frozen Waves 38
Measuring Mainstream CO2 using
M3016A 218
Measuring Microstream CO2 using
M3015A/B 220
Measuring Pulmonary Artery Wedge
Pressure 192
Measuring Pulse Pressure Variation 198
Measuring SpO2 166
Measuring Systemic Vascular
Resistance 198
Metabolism Correction for tcpCO2 239
Microstream CO2 Accessories 383
Minimum Volume for No Central
Monitoring INOP 52
Minimum Volume for Severe Yellow or Red
INOPs 52
MMS Extensions 21
MMS, MMS Extensions and FMS
INOPs 74
Modified 12-Lead ECG 122
Monitor INOPs 70
Monitor Mounting Precautions 393
Monitor Safety Specifications 393
Monitoring After a Power Failure 45
Monitoring Airway Flow, Volume and
Pressure 225
Monitoring BIS 257
Monitoring BIS using the BISx 258
Monitoring BIS Using the DSC and BIS
Engine 258
Monitoring Carbon Dioxide 213
Monitoring Cardiac Output 195
Monitoring EEG 249
Monitoring Intravascular Oxygen
Saturation 241
Monitoring Invasive Pressure 183
Monitoring NBP 173
Monitoring Paced Patients 113
Monitoring Pulse Rate 155
Monitoring Respiration Rate (Resp) 159
453
Monitoring SpO2 165
Monitoring tcGas 233
Monitoring Temperature 181
Monitoring the Sepsis Management Bundle
Recommendations 315
Monitoring the Sepsis Resuscitation Bundle
Recommendations 313
Moving Windows 26
N
NBP 412
NBP Accessories 372
NBP Default Settings 440
NBP INOPs 77
NBP Timestamp 176
Neonatal and Pediatric Modes 229
Neonatal/Infant Cuff Kits 375
Neonatal/Infant Single Patient Cuffs 374
Neonatal/Infant Single Patient, Soft
Cuffs 375
Networked Monitoring 45
New Patient Check 98
New/Dried Out Transducers 235
No. of Segments 275
Non-Physiological Artifact
Suppression 188
Notification 353
Nurse Call Systems 51
O
One-piece Cables 371
Operating and Navigating 24
Operating Modes 31
Optimizing Lead Placement for Resp 159
Optimizing Scale Settings 230
Optimizing the Waveform 187
Optimum Scale 275
Orientation On The Screen 310
Other Bed Pop-Up Keys 109
Other Reports 335
Overview of Recording Types 319
P
Pairing an X2 or MP5 With a Telemetry
Interface to a Host Monitor 267
Patient Alarm Messages 65
Patient Alarms and INOPs 65
Patient Category and Paced Status 96
Patient Mismatch - If Both Patient Data
Sets Are Correct 104
Patient Mismatch - If Neither Patient Data
Set is Correct 104
Patient Mismatch - If One Set of Patient
Data is Correct 103
Pausing or Switching Off Alarms 54
Performance Specifications 399
Performing a Light Intensity
Calibration 244
Performing Calculations 285
Performing Calculations for a Non-Specific
Drug 339
Performing Calculations for a Specific
Drug 339
Performing Drug Calculations 338
Performing In-Vivo Calibration 244, 247
Performing PiCCO C.O.
Measurements 201
Performing RH C.O. Measurements 205
Perfusion Change Indicator 171
Perfusion Numeric 171
Permanent Keys 26
Physical Specifications 395
Pleth Wave 171
Pop-Up Keys 29
Power Loss Tone 53
Power On/Power Off Behavior 44
Preparing to Measure Mainstream
CO2 215, 218
Preparing to Measure Microstream
CO2 221
Preparing to Measure NBP 175
Preparing to Measure Sidestream CO2 216
Preparing to Monitor with the M1011A
Narrow Module 246
Preparing to Monitor with the M1021A
Wide Module 242
Pressure INOPs 80
Previewing the Sepsis Management
Bundle 314
Printer Status Messages 331
Printing a Test Report 329
Printing an ST Map Report 149
Printing Hi-Res Trend Wave Reports 290
Printing Manually 331
Printing Patient Reports 325
Printing the 12-Lead ECG 124
Printing The QT Waves 152
Printout Location 325
ProtocolWatch 309
ProtocolWatch INOPs 92
Pulse Default Settings 438
Pulse INOPs 76
Q
QRS Tone 157
QT Alarms 152
QT Measurement Algorithm 149
QT View 151
Quick Admitting a Patient 96
Quickstarting Recordings 318
R
Radio-translucent Cables 371
Realtime Report 334
Rear of the Monitor 391
Recommended Cables 369
Recommended Separation Distance 426
Recommended separation distances from
portable and mobile RF communication
equipment 427
Recorded Waveforms 322
Recorder Accessories 386
Recorder Status Messages 323
Recording 317
Recording Priorities 321
Recording ST Segments 142
Recording Strip 321
Recording Strip Code 321
Recording The QT Waves 152
Recording Without a Template 318
Reference Method 174
Releasing Frozen Waves 39
Reloading Paper 323
Remembraning the tcGas Transducer 235
Removing Exhaust Gases from the
System 218, 222
Resetting Arrhythmia Alarm Timeouts 55
Resetting the Timeout Period 137
Resolving Label Conflicts 40
Resolving Patient Information
Mismatch 102
Resp Detection Modes and Cardiac
Overlay 161
Resp INOPs 77
Resp Safety Information 162
Respiration 408
Respiration Default Settings 439
Respiratory Loops 355
Restart time 428
Restarting Paused Alarms 55
Restarting the tcGas SiteTimer 234
Review Alarms Window 60
Reviewing Alarms 60
Reviewing Calculations 285
454
Rhythm Status Messages 133
Right side of the Monitor 392
Run Time 352
Running a Car Seat Assessment Record 297
S
Safety and Performance Tests 424
Sample Report Printouts 332
Saving and Calibrating PiCCO C.O.
Measurements 202
Screen Trends 279
ScvO2 Default Settings 446
Selecting a Measurement Label 242
Selecting a Pressure for Monitoring 184
Selecting a Temperature for
Monitoring 181
Selecting Leads for ST Analysis 140
Selecting Positions of Va and Vb Chest
Leads (for 6-lead placement) 116
Selecting Screen Elements 25
Selecting the Active Alarm Source
ECG or Pulse? 156
Selecting the Primary and Secondary ECG
Leads 112
Selecting The QT Leads 150
Selecting the tcGas HeatPowerDisplay
Mode 238
Sepsis Management Bundle 314
Sepsis Resuscitation Bundle 313
Set Combiners and Organizers 371, 372
Setting Measurement and Period for
Histograms 277
Setting SpO2/Pleth as Pulse Source 172
Setting the Computation Constant 205
Setting the Date and Time 43
Setting the Gas Compensation Mode 231
Setting the Horizon 281
Setting the Horizon Trend Scale 281
Setting the Paced Status (Pace Pulse
Rejection) 114
Setting the QRS Volume 172
Setting The QT Baseline 151
Setting the Screen Trend Time 279
Setting the tcGas Barometric Pressure 235
Setting the tcGas Sensor Temperature 233
Setting the tcGas Site Timer 234
Setting the Time Period for the Trend
Indicator Arrow 281
Setting Triggers and Notification for
Advanced Event Surveillance 297
Setting Triggers for NER and Basic Event
Surveillance 296
Setting up all CO2 Measurements 222
Setting Up Auto Reports 327
Setting up CO2 Corrections 222
Setting Up ECG Reports 327
Setting Up Individual Print Jobs 328
Setting Up Reports 327
Setting up RH C.O. Measurements 204
Setting Up Source Device 357
Setting up Spirometry 230
Setting Up the 12-Lead ECG 124
Setting Up the In-Vivo Calibration 244,
245
Setting up the Modules 44
Setting Up the PiCCO C.O.
Measurement 200
Setting up the Pressure Measurement 183
Setting Up Timers 352
Setting Up Tone Modulation 172
Setting Up Trends 274
Setting Up Vital Signs and Graphic Trend
Reports 327
Severe Sepsis Screening 311
Short Range Radio Interface (MX600/700/
800 and 865244 Remote Control) 395
Showing/Hiding Loops 356
Shutting the iPC Down 47
Sidestream CO2 Accessories 382
Single- or Multi-lead ST Alarming 145
Skin Preparation for Electrode
Placement 111
SmartKeys 27
SO2 Accessories for M1011A 386
SO2 Accessories for M1021A 386
SO2 INOPs 83
Special Situations at Shutdown 47
Specifications 387
Spirometry 419
Spirometry Accessories 384
Spirometry Default Settings 444
Spirometry INOPs 89
Spirometry Values Window 230
SpO2 409
SpO2 Accessories 376
SpO2 Default Settings 439
SpO2 INOPs 79
SpO2 Sensors 165
SpO2 Signal Quality Indicator (Fast SpO2
only) 167
SSC Sepsis Protocol 309
ST Alarms 145
Standard 3-Lead Placement 118
Standard 5-Lead Placement 119
Standby Mode 31
Starting a Cyclic Impedance Check 260
Starting and Stopping Measurements 176
Starting and Stopping Recordings 317
Starting Monitoring 44
Starting Report Printouts 325
Starting the Different Types of Report 326
Starting the iPC 46
Sterilizing the Monitor 363
Stopping a Cyclic Impedance Check 260
Stopping Recordings 318
Stopping Reports Printouts 326
Storing and Sending the 12-Lead ECG 124
Storing tcGas Transducers 235
Supported Cables 371
Suppressing Sampling (not Mainstream
CO2) 223
Suppressing Zero Calibration 222
Suspending Telemetry Alarms 268
Suspending the Protocol for 24 Hours 311
SvO2 Default Settings 446
Swapping a Complete Profile 35
Swapping a Settings Block 35
Switching a Measurement On and Off 37
Switching All Yellow Arrhythmia Alarms
On or Off 136
Switching Arrhythmia Analysis On and
Off 130
Switching Between ST Map Views 148
Switching BIS and Individual Numerics On
and Off 262
Switching BIS Filters On or Off 262
Switching EEG Numerics On and Off 253
Switching Individual Arrhythmia Alarms
On and Off 136
Switching Individual QTc Alarms On and
Off 153
Switching Manually Entered Measurements
On and Off 42
Switching Numerics On and Off 37
Switching On 44
Switching Printers On Or Off for
Reports 329
Switching Pulse from NBP On/Off 179
Switching Pulse On and Off 156
Switching QT Monitoring On and Off 153
Switching ST On and Off 140
Switching to a Different Screen 32
Switching VueLink On and Off 349
Symbols 389
Synchronized Settings 269
455
System Pulse Source 155
T
Tabular View 280
tcGas 422
tcGas Accessories 385
TcGas Corrections 238
tcGas Default Settings 445
tcGas INOPs 86
Technical Alarm Messages (INOPs) 70
Telemetry Data Window 266
Telemetry INOPs 91
Temp 415
Temperature Accessories 380
Temperature Correction for tcpCO2 238
Temperature Default Settings 440
Temperature INOPs 78
Testing Alarms 62
The Events Database 298
Timer Counting Direction 353
Timer Label 352
Timer Setup Pop-up Keys 352
Timer Types 351
Timer Volume 353
To Change the Size of all the ECG
Waves 115
To Change the Size of an Individual ECG
Wave 115
To Discharge a Patient 97
To Pause All Alarms 54
To Switch All Alarms Off 54
To Switch Individual Measurement Alarms
On or Off 55
Trademark Acknowledgement 388
Traditional Audible Alarms (HP/Agilent/
Philips/Carenet) 51
Transferring a Centrally-Monitored
Patient 99
Transferring a Centrally-Monitored Patient
with X2 or MP5 100
Transferring a Centrally-Monitored Patient
with X2 or MP5 using IIT 100
Transferring a Patient with an X1 (no
Information Center) 101
Transferring a Patient with an X2 or MP5
(no Information Center) 101
Transferring Patients 98
Transferring Patients And Moving
Manually Between Phases 310
Trend Group 275
Trend Groups 275
Trend Interval 276
Trend Parameter Scales 276
Trend Priority 276
Trend Scales for Segment
Measurements 275
Trend View 147
Trending Multiple-Value
Measurements 279
Trends 271
Trends Databases 278
Trends Pop-Up Keys 272
Triggering Events Manually 297
Troubleshooting 367
Troubleshooting tcGas Calibration 237
Troubleshooting the Pressure
Calibration 190
Troubleshooting the Zero 186
Trunk Cables 369, 371
Two Or More Infection Signs Or
Symptoms Confirmed 312
U
Unavailable Printer
Re-routing Reports 330
Understanding Profiles 34
Understanding PVC-Related Alarms 139
Understanding Screens 32
Understanding Settings 36
Understanding SpO2 Alarms 168
Understanding the Arrhythmia
Display 132
Understanding the Care Group Overview
Bar 106
Understanding the ECG Display 112
Understanding the NBP Numerics 175
Understanding the Resp Display 160
Understanding the ST Display 141
Updating an ST Map Reference
Baseline 148
Updating ST Baseline Snippets 142
Updating The Frozen Wave 39
Use Models With Telemetry 269
Using a Mouse or Trackball 26
Using ECG Alarms 127
Using Input Devices with the iPC and
Monitor 47
Using Keys 26
Using Labels 39
Using Microstream Accessories 221
Using Pulse Alarms 156
Using Resp Alarms 162
Using Screens with External Device
Data 344
Using Standby 268
Using the C.O. Procedure Window 196
Using the Drug Calculator 337
Using the EEG Impedance/Montage
Window 250
Using the FilterLine and Airway
Adapter 221
Using the Integrated PC 46
Using the Loops Cursor 356
Using the On-Screen Calculator 31
Using the On-Screen Keyboard 30
Using the Remote Control 29
Using the Sidestream Sensor Holder 218
Using the SmartKeys Key 30
Using the tcGas Site Timer 234
Using the Titration Table 341
Using the Touchscreen 26
Using the Visitor Screen 34
Using the Wave Cursor 187
Using the X2 or MP5 with a Host
Monitor 47
Using the XDS Remote Display 34
Using the Zero Hardkey 186
Using Timers 351
Using VueLink Screens 349
V
Viewing All Alarm Limits 56
Viewing an ST Map 148
Viewing And Printing The Protocol
Log 316
Viewing and Silencing Telemetry Alarms at
the Bedside 267
Viewing Arrhythmia Waves 132
Viewing Calculations 284
Viewing Events 298
Viewing Graphic Trends 272
Viewing Histogram Trends 274
Viewing Individual Alarm Limits 56
Viewing Loops 355
Viewing Received Data 359
Viewing ST Maps 146
Viewing the Alarm Latching Settings 61
Viewing the IntelliBridge Device Data
Window 344
Viewing the iPC Desktop on the Monitor
Display 46
Viewing the My Care Group Window 107
Viewing the Other Bed Window 108
Viewing the Realtime 12-Lead ECG 123
Viewing the VueLink Device Data
Window 349
456
Viewing Timers 351
Viewing Trends 271
Viewing Vital Signs Trends 273
Visual Alarm Indicators 50
Visual Alarm Status Information in the
Other Bed Window 109
VueLink Default Settings 447
VueLink INOPs 90
VueLink Modules 347
W
Weight 206
What is a Timeout Period? 137
Where Can I Find More Information? 130,
150
While Alarms are Paused or Off 55
Working in the ST Map Task Window 148
X
X1 Connectors and Symbols 18
X1 Multi-Measurement Module
(M3001A) 17
X2 Controls and Indicators 20
X2 Left Side 21
X2 Multi-Measurement Module
(M3002A) 18
X2 Overview 19
X2 Patient Connectors, Right Side 21
Y
Yellow Arrhythmia Alarms 136
Z
Zero Calibration 228
Zeroing a Pressure Measurement 185
Zeroing All Pressures Simultaneously 186
Zeroing ICP (or IC1/IC2) 185
Zeroing the Pressure Transducer 184
Zeroing the tcGas Relative Heat Power 238