St Jude Medical SJMRF Rf Implantable Medical Device User Manual Nuance Communications Inc
St. Jude Medical Rf Implantable Medical Device Nuance Communications Inc
Contents
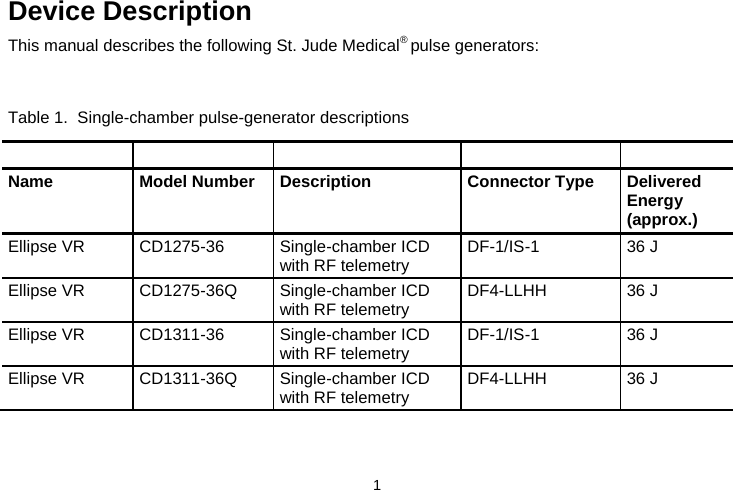
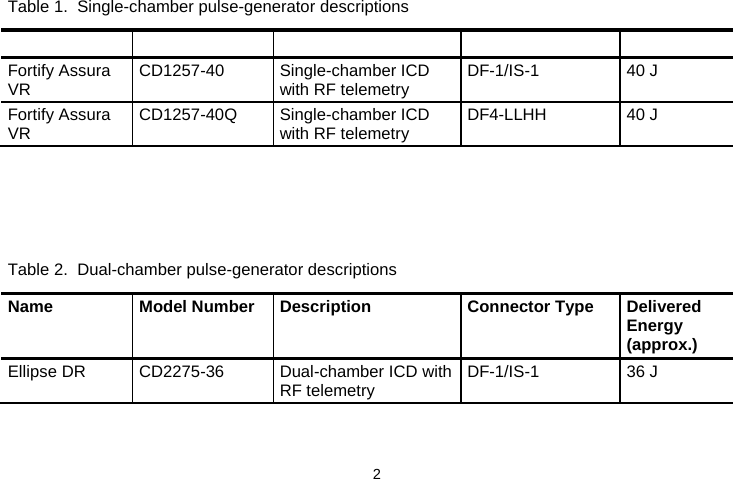
- 1. User Manual
- 2. user manual for Ellipse devices (att1)
- 3. user manual (att1)
user manual (att1)