St Jude Medical SJMRF Rf Implantable Medical Device User Manual Nuance Communications Inc
St. Jude Medical Rf Implantable Medical Device Nuance Communications Inc
Contents
- 1. User Manual
- 2. user manual for Ellipse devices (att1)
- 3. user manual (att1)
user manual (att1)

Ellipse™
Tiered-therapy Cardioverter/Defibrillator
Fortify Assura™
Tiered-therapy Cardioverter/Defibrillator
Quadra Assura™
Cardiac Resynchronization Device, Tiered-therapy Cardioverter/Defibrillator
Unify Assura™
Cardiac Resynchronization Device, Tiered-therapy Cardioverter/Defibrillator

Covered by one or more of the following US patents: 5,318,591
Proposition 65, a State of California voter initiative, requires the following notice:
WARNING: This product and its packaging have been sterilized with ethylene oxide. This packaging may expose
you to ethylene oxide, a chemical known to the state of California to cause cancer or birth defects or other
reproductive harm.
ST. JUDE MEDICAL, the nine-squares symbol, and MORE CONTROL. LESS RISK. are registered and
unregistered trademarks and service marks of St. Jude Medical, Inc. and its related companies.
CAUTION: Federal (USA) law restricts this device to sale by or on the order of a physician.
© 2012 St. Jude Medical Cardiac Rhythm Management Division. All Rights Reserved.
Unless otherwise noted, ® or ™ indicates that the name is a trademark of, or licensed to, St.
Jude Medical, Inc. or
its subsidiaries.
1
Device Description
This manual describes the following St. Jude Medical® pulse generators:
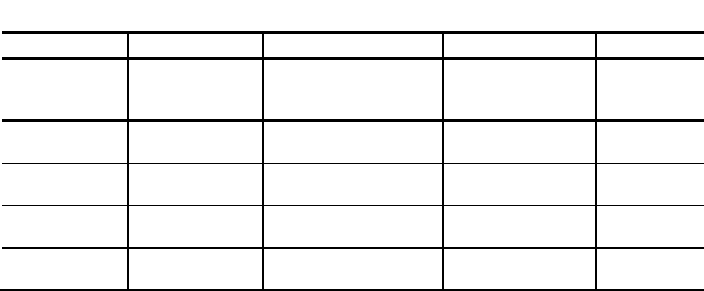
Table 1. Single-chamber pulse-generator descriptions
Name
Model Number
Description
Connector Type
Delivered
Energy
(approx.)
Ellipse VR
CD1275-36
Single-chamber ICD
with RF telemetry
DF-1/IS-1
36 J
Ellipse VR
CD1275-36Q
Single-chamber ICD
with RF telemetry
DF4-LLHH
36 J
Ellipse VR
CD1311-36
Single-chamber ICD
with RF telemetry
DF-1/IS-1
36 J
Ellipse VR
CD1311-36Q
Single-chamber ICD
with RF telemetry
DF4-LLHH
36 J
2
Table 1. Single-chamber pulse-generator descriptions
Fortify Assura
VR
CD1257-40 Single-chamber ICD
with RF telemetry
DF-1/IS-1 40 J
Fortify Assura
VR
CD1257-40Q
Single-chamber ICD
with RF telemetry
DF4-LLHH
40 J
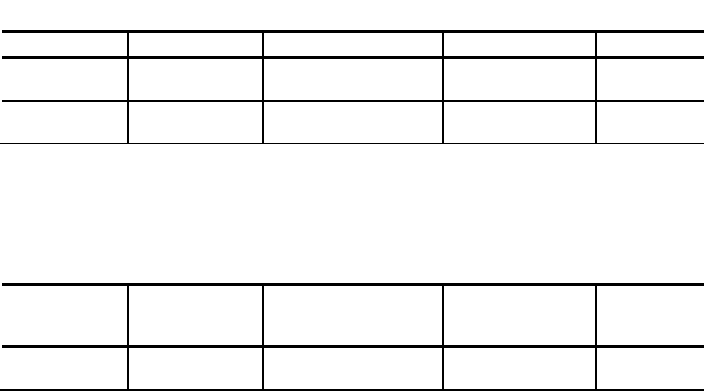
Table 2. Dual-chamber pulse-generator descriptions
Name
Model Number
Description
Connector Type
Delivered
Energy
(approx.)
Ellipse DR
CD2275-36
Dual-chamber ICD with
RF telemetry
DF-1/IS-1
36 J
3
Table 2. Dual-chamber pulse-generator descriptions
Name Model Number Description Connector Type Delivered
Energy
(approx.)
Ellipse DR
CD2275-36Q
Dual-chamber ICD with
RF telemetry
DF4-LLHH/
IS-1
36 J
Ellipse DR
CD2311-36
Dual-chamber ICD with
RF telemetry
DF-1/IS-1
36 J
Ellipse DR
CD2311-36Q
Dual-chamber ICD with
RF telemetry
DF4-LLHH/
IS-1
36 J
Fortify Assura
DR
CD2257-40
Dual-chamber ICD with
RF telemetry
DF-1/IS-1
40 J
Fortify Assura
DR
CD2257-40Q
Dual-chamber ICD with
RF telemetry
DF4-LLHH/
IS-1
40 J
4
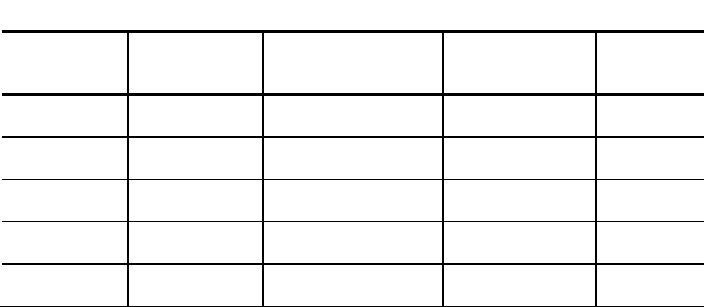
Table 3. CRT-D pulse-generator descriptions
Name Model Number Description Connector Type Delivered
Energy
(approx.)
Quadra Assura
CD3265-40
CRT-D with
RF telemetry
DF-1/IS-1/
IS4-LLLL
40 J
Quadra Assura
CD3265-40Q
CRT-D with
RF telemetry
DF4-LLHH/
IS4-LLLL/
IS-1
40 J
Unify Assura
CD3257-40
CRT-D with
RF telemetry
DF-1/IS-1
40 J
Unify Assura CD3257-40Q CRT-D with
RF telemetry DF4-LLHH/
IS-1 40 J
The pulse generator, along with compatible, commercially available leads, constitutes the
implantable portion of the ICD and CRT-D systems. The lead systems are implanted using either
transvenous or transthoracic techniques. The St. Jude Medical Merlin® Patient Care System (PCS)
with software model 3330 version 14.1 (or greater), a Merlin® Antenna (for devices with RF
communication), and a telemetry wand constitute the external portion of the ICD and CRT-D

5
systems.
Models with the “Q” suffix” are functionally equivalent in all respects to the same model without the
“Q” suffix, except for the header. Models without the Q” suffix use DF-1 lead connectors for the
high-voltage leads, and models with the Q” suffix use a single DF4-LLHH lead connector for the
high-voltage leads and for the low voltage RV lead.
SJ4-LLHH is equivalent to DF4-LLHH. SJ4 and DF4 connectors comply with ISO
27186:2010(E).SJ4-LLLL is equivalent to IS4-LLLL. SJ4 and IS4 connectors comply with ISO
27186:2010(E).
Indications and Usage
St. Jude Medical® ICDs and CRT-Ds are intended to provide ventricular antitachycardia pacing and
ventricular defibrillation for automated treatment of life-threatening ventricular arrhythmias.
AF Suppression™ pacing is indicated for suppression of paroxysmal or persistent atrial fibrillation in
patients with the above ICD indication and sinus node dysfunction.
In patients indicated for an ICD, CRT-Ds are also intended:
to provide a reduction of the symptoms of moderate to severe heart failure (NYHA Functional
Class III or IV) in those patients who remain symptomatic despite stable, optimal medical

6
therapy (as defined in the clinical trials section included in the Merlin PCS on-screen help) and
have a left ventricular ejection fraction less than or equal to 35% and a prolonged QRS
duration
to maintain synchrony of the left and right ventricles in patients who have undergone an AV
nodal ablation for chronic (permanent) atrial fibrillation and have NYHA Class II or III heart
failure
Contraindications
Contraindications for use of the pulse generator system include ventricular tachyarrhythmias
resulting from transient or correctable factors such as drug toxicity, electrolyte imbalance, or acute
myocardial infarction.
Warnings and Precautions
Resuscitation Availability. Do not perform device testing unless an external defibrillator and
medical personnel skilled in cardiopulmonary resuscitation (CPR) are readily available.
Lead system. Do not use another manufacturer’s lead system without demonstrated compatibility
as undersensing cardiac activity and failure to deliver necessary therapy may result.
Avoiding shock during handling. Disable tachyarrhythmia therapy (Enable/ Disable Tachy
Therapy) or program tachyarrhythmia therapies Off during surgical implant and explant or post-

7
mortem procedures as well as when disconnecting leads as the device can deliver a serious shock
if you touch the defibrillation terminals while the device is charged.
Additional pacemaker implanted. These devices provide bradycardia pacing. If another
pacemaker is used, it should have a bipolar pacing reset mode and be programmed for bipolar
pacing to minimize the possibility of the output pulses being detected by the device.
Modifying the device. This device has been tested for compliance to FCC regulations. Changes or
modifications of any kind not expressly approved by St. Jude Medical Inc. could void the user’s
authority to operate this device.
Suboptimal radio frequency (RF) communication. The Merlin PCS indicates the quality of the RF
communication by the telemetry strength indicator LEDs on both the Merlin PCS and the Merlin
Antenna. Below is a list of potential causes to suboptimal radio communication:
8
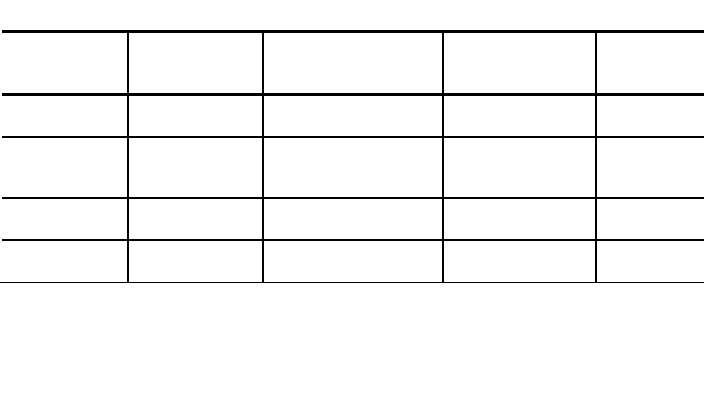
Table 4. Possible causes and solutions for suboptimal RF
communication
Possible Causes
Solutions
The Merlin Antenna
orientation/location is
suboptimal.
Move or reorient the Merlin
Antenna slightly. Make sure
that the front of the Merlin
Antenna faces the implantable
device.
People or objects interfere with
the communication between
the Merlin Antenna and the
device.
Make sure that the space
between the Merlin Antenna
and the device is free from
interfering objects/people.
The Merlin Antenna is too far
away from the device. Move the Merlin Antenna
closer to the device.
Someone is holding the Merlin
Antenna. Place the Merlin Antenna on a
flat surface. Do not hold the
Merlin Antenna.
9
Table 4. Possible causes and solutions for suboptimal RF
communication
Possible Causes
Solutions
Other products in the vicinity
are causing electromagnetic
interference (EMI).
Power off or remove
equipment that could cause
EMI.
The Merlin Antenna cable is
wound around the Merlin
Antenna.
Make sure the Merlin Antenna
cable is not wound around the
Merlin Antenna.
Sterilization, Storage and Handling
Resterilization. Do not resterilize and re-implant explanted pulse generators.
Use before date. Do not implant the device after the "use before" date because the battery may
have reduced longevity.
If package is damaged. Do not use the device or accessories if the packaging is wet, punctured,
opened or damaged because the integrity of the sterile packaging may be compromised. Return the
device to St. Jude Medical.

10
Device storage. Store the device in a clean area, away from magnets, kits containing magnets, and
sources of electromagnetic interference to avoid device damage. Store the device between 10° and
45°C because temperatures outside this range may damage the device.
Temperature Equilibration. After cold storage, allow the device to reach room temperature before
charging the capacitors, programming, or implanting the device because cold temperature may
affect initial device function.
Follow-up Testing
Ensure that an external defibrillator and medical personnel skilled in cardiopulmonary resuscitation
(CPR) are present during post-implant device testing should the patient require external rescue.
Be aware that the changes in the patient's condition, drug regimen, and other factors may change
the defibrillation threshold (DFT), which may result in nonconversion of the arrhythmia. Successful
conversion of ventricular fibrillation or ventricular tachycardia during arrhythmia conversion testing is
no assurance that conversion will occur post-operatively.
Implantation and Device Programming
Do not position a magnet over the device as that suspends detection and treatment (unless the
device has been programmed to ignore the magnet).
Replace the device when the battery reaches the elective replacement indicator (ERI).

11
Implant the pulse generator no deeper than 5 cm to ensure reliable data transmission. For patient
comfort, do not implant the pulse generator within 1.25 cm of bone unless you cannot avoid it.
Exercise caution when turning the setscrew, which may be backed out of the connector if turned
counterclockwise for more than two rotations.
Program the device parameters as specified in the Merlin® PCS on-screen help.
The results of the DAVID Study demonstrated that, for patients with standard indications for ICD
therapy, no indication for cardiac pacing and an EF < 40%, dual-chamber pacing offers no clinical
advantage over backup VVI pacing and may be associated with worsening heart failure.1 When
programming the device to dual-chamber pacing modes, give particular attention to setting the
pacing parameters (such as the A-V delay) to promote intrinsic conduction and minimize the amount
of ventricular pacing.
Pulse Generator Explant and Disposal
Interrogate the device and turn all therapies off before explanting, cleaning or shipping the device to
prevent unwanted shocks.
Return all explanted pulse generators and leads to St. Jude Medical.
Never incinerate the device because of the potential for explosion. Explant the device before
cremation.
1 Wilkoff BL, Cook JR, Epstein AE, Greene L, Hallstrom AP, Hsia H, Kutalek SP, Sharma A. Dual-Chamber Pacing or Ventricular
Backup Pacing in Patients With an Implantable Defibrillator: The Dual Chamber and VVI Implantable Defibrillator (DAVID) Trial.
JAMA. December 25, 2002; Vol 288, No. 24:3115-3123.

12
Environmental and Medical Therapy Hazards
Instruct patients to avoid devices which generate a strong electric or magnetic interference (EMI).
EMI could cause device malfunction or damage, resulting in non-detection or delivery of unneeded
therapy. Moving away from the source or turning it off will usually allow the pulse generator to return
to its normal mode of operation.
Hospital and Medical Environments
Electrosurgical cautery. Electrosurgical cautery could induce ventricular arrhythmias and/or
fibrillation, or may cause device malfunction or damage. If electrocautery is necessary, keep the
current path and groundplate as far away from the pulse generator and leads as possible.
External defibrillation. External defibrillation may damage the pulse generator or may result in
temporary and/or permanent myocardial damage at the electrode-tissue interface as well as
temporarily or permanently elevated pacing capture thresholds. Minimize current flowing through
the pulse generator and lead system by following these precautions when using external
defibrillation on a patient with a pulse generator:
Position defibrillation paddles as far from the pulse generator as possible (minimum of 13 cm)
Use the lowest clinically appropriate energy output
Confirm pulse generator function following any external defibrillation
High radiation sources. Do not direct high radiation sources such as cobalt 60 or gamma radiation

13
at the pulse generator. If a patient requires radiation therapy in the vicinity of the pulse generator,
place lead shielding over the device to prevent radiation damage and confirm its function after
treatment.
Lithotripsy. Lithotripsy may permanently damage the pulse generator. Avoid it unless the therapy
site is not near the pulse generator and leads.
Diathermy. Avoid diathermy, even if the device is programmed off, as it may damage tissue around
the implanted electrodes or may permanently damage the pulse generator.
Magnetic resonance imaging (MRI). MRI for patients with implantable pulse generators has been
contraindicated by MRI manufacturers. Clinicians should carefully weigh the decision to use MRI
with ICD/CRT-D patients. MRI may cause device malfunction or injury to the patient.
Ultrasound therapy. Diagnostic and therapeutic ultrasound treatment is not known to affect the
function of the pulse generator.
Transcutaneous Electrical Nerve Stimulation (TENS). TENS may interfere with device function.
To reduce interference, place the TENS electrodes close to one another and as far from the
device/lead system as possible. Monitor cardiac activity during TENS use.
Radiofrequency ablation. RF ablation in a patient with a pulse generator may cause device
malfunction or damage.
Minimize RF ablation risks by:
Programming all tachyarrhythmia therapies off
14
Avoiding direct contact between the ablation catheter and the implanted lead or pulse
generator
Positioning the groundplate so that the current pathway does not pass near the pulse
generator system, i.e., place the groundplate under the patient's buttocks or legs
Having external defibrillation equipment available.
RF Operating Frequencies. Nearby equipment emitting strong magnetic fields can interfere with
RF communication, even if the other equipment complies with CISPR emission requirements. The
operating characteristics are as follows:
MICS band: 402-405 MHz. The effective radiated power is below the limits as specified in:
Europe: EN ETSI 301 839-2
USA: FCC 47 CFR Part 95; 95.601-95.673 Subpart E, 95.1201-95.1221 Subpart I
FCC ID: RIASJMRF.
WARNING
This transmitter is authorized by rule under the Medical Device
Radiocommunication Service (in part 95 of the FCC Rules) and must not cause
harmful interference to stations operating in the 400.150–406.000 MHz band in the
Meteorological Aids (that is.,transmitters and receivers used to communicate
weather data), the Meteorological Satellite, or the Earth Exploration Satellite
Services and must accept interference that may be caused by such stations,

15
including interference that may cause undesired operation. This transmitter shall
be used only in accordance with the FCC Rules governing the Medical Device
Radiocommunication Service. Analog and digital voice communications are
prohibited. Although this transmitter has been approved by the Federal
Communications Commission, there is no guarantee that it will not receive
interference or that any particular transmission from this transmitter will be free
from interference.
The following is applicable to Canada only:
This device may not interfere with stations operating in the 400.150-406.000 MHz band in the
meteorological aids, meteorological-satellite, and earth exploration-satellite services and must
accept any interference received, including interference that may cause undesired operation.
Home and Occupational Environments
High-voltage power transmission lines. High-voltage power transmission lines may generate
enough EMI to interfere with pulse generator operation if approached too closely.
Communication equipment. Communication equipment such as microwave transmitters or high-
power amateur transmitters may generate enough EMI to interfere with pulse generator operation if
approached too closely.
16
Home appliances. Home appliances in good working order and properly grounded do not usually
produce enough EMI to interfere with pulse generator operation. There are reports of pulse
generator disturbances caused by electric hand tools or electric razors used directly over the pulse
generator implant site.
Industrial equipment. A variety of industrial equipment produce EMI of sufficient field strength and
modulation characteristics to interfere with proper operation of the pulse generator. These include,
but are not limited to: arc welders; induction furnaces; very large or defective electric motors; and
internal combustion engines with poorly shielded ignition systems.
Electronic Article Surveillance
Advise patients that the Electronic Article Surveillance/Anti-theft (EAS) systems such as those at the
point of sale and entrances/exits of stores, libraries, banks, etc., emit signals that may interact with
the device. It is very unlikely that these systems will interact with their device significantly. However,
to minimize the possibility of interaction, advise patients to simply walk through these areas at a
normal pace and avoid lingering near or leaning on these systems.
Metal Detectors
Advise patients that metal detector security systems such as those found in airports and
government buildings emit signals that may interact with ICDs and CRT-Ds. It is very unlikely that
these systems will interact with their device significantly. To minimize the possibility of interaction,

17
advise patients to simply walk through these areas at a normal pace and avoid lingering. Even so,
the ICD and CRT-D systems contain metal that may set off the airport security system alarm. If the
alarm does sound, the patient should present security personnel with their patient identification
card. If security personnel perform a search with a handheld wand, the patient should ask that they
perform the search quickly, stressing that they should avoid holding the wand over the device for a
prolonged period.
Cellular Phones
The pulse generator has been tested for compatibility with handheld wireless transmitters in
accordance with the requirements of AAMI PC69. This testing covered the operating frequencies
(450 MHz - 3 GHz) and pulsed modulation techniques of all of the digital cellular phone
technologies in worldwide use today. Based on the results of this testing, the pulse generator should
not be affected by the normal operation of cellular phones.
Potential Adverse Events
Possible adverse events (in alphabetical order) associated with the system, include, but are not
limited to the following:
Acceleration of arrhythmias (caused by device)
Air embolism
Allergic reaction

18
Bleeding
Cardiac tamponade
Chronic nerve damage
Death
Erosion
Exacerbation of heart failure
Excessive fibrotic tissue growth
Extracardiac stimulation (phrenic nerve, diaphragm, chest wall)
Extrusion
Fluid accumulation
Formation of hematomas or cysts
Inappropriate shocks
Infection
Keloid formation
Lead abrasion and discontinuity
Lead migration/dislodgment
Myocardial damage
Pneumothorax
Shunting current or insulating myocardium during defibrillation with internal or external paddles
19
Potential mortality due to inability to defibrillate or pace
Thromboemboli
Venous occlusion
Venous or cardiac perforation.
Patients susceptible to frequent shocks despite antiarrhythmic medical management may develop
psychological intolerance to an ICD or CRT-D system that may include the following:
Dependency
Depression
Fear of premature battery depletion
Fear of shocking while conscious
Fear of losing shock capability
Imagined shocking (phantom shock).
Clinician Use Information
WARNING
For devices without the Low Frequency Attenuation Filter, the default Atrial
Sensitivity setting and the lowest possible setting of Ventricular Sensitivity, 0.2 mV,
may be more susceptible to EMI, according to testing required by CENELEC
standard prEN45502-2-2. The devices comply with the electromagnetic

20
compatibility requirements of CENELEC standard prEN45502-2-2 at atrial and
ventricular sensitivities of 0.3 mV and less sensitive settings.
For devices with the Low Frequency Attenuation Filter, the default Atrial Sensitivity
setting, the lowest possible setting of Ventricular Sensitivity, 0.2 mV, and the
Ventricular Sensitivity setting of 0.3 mV when the Low Frequency Attenuation Filter
is On, may be more susceptible to EMI, according to testing required by CENELEC
standard EN45502-2-2. The devices comply with the electromagnetic compatibility
requirements of CENELEC standard EN45502-2-2 at atrial sensitivities of 0.3 mV,
ventricular sensitivities of 0.3mV (Low Frequency Attenuation Filter OFF) or
ventricular sensitivities of 0.4 mV (Low Frequency Attenuation Filter On), and less
sensitive settings.
Physician Training
Physicians should be familiar with sterile pulse generator implant procedure and with follow-up
evaluation and management of patients with an ICD or CRT-D (or should refer the patient to such a
physician).

21
Maintaining Device Effectiveness
Device Storage
FOR SINGLE USE ONLY. Do not resterilize and re-implant explanted pulse generators.
St. Jude Medical has sterilized the pulse generator with ethylene oxide prior to shipment. Contact
St. Jude Medical if resterilization is necessary.
Do not implant the device when:
It has been dropped on a hard surface because this could have damaged pulse generator
components.
The sterility indicator within the inner package is purple, because it might not have been
sterilized.
Its storage package has been pierced or altered, because this could have rendered it non-
sterile.
It has been stored or transported outside the environmental temperature limits.
Storage limits: 10° to 45°C.
Transportation limits: -20° to 60°C.
An electrical reset condition may occur at temperatures below -20°C.
After cold storage, allow the device to reach room temperature before charging the capacitors,
programming, or implanting the device because cold temperature may affect initial device
function.

22
Its "use before" date has expired, because this can adversely affect pulse generator longevity
or device sterility.
Do not resterilize the pulse generator using an autoclave, gamma-irradiation, organic cleaning
agents (e.g., alcohol, acetone, etc.), or ultrasonic cleaners.
Sterilization Instructions
Contact St. Jude Medical if resterilization is necessary.
Directions for Use
Pulse generator operating characteristics should be verified at the time of implantation and recorded
in the patient file. Complete the Patient Registration Form and return it to St. Jude Medical as it
provides necessary information for warranty purposes and patient tracking.
Copies of this user's manual can be obtained by contacting your St. Jude Medical representative.
Radiopaque Identification
Each pulse generator has an X-ray absorptive marker for non-invasive identification. The marker
consists of the St. Jude Medical logo (SJM) and a two-letter model code.
23
Table 5. X-ray ID codes for the device models described in this manual
Device Model
X-ray ID Model
Code
CD1275-36/36Q, CD1311-36/36Q, CD2275-36/36Q, CD2311-
36/36Q
KF
CD1257-40/40Q, CD2257-40/40Q, CD3257-40/40Q, CD3265-
40/40Q KC
Package Contents
The pulse generator is supplied in a sterile tray for introduction into the operating field. The tray
contains:
One pulse generator (with all tachyarrhythmia therapies off) with pre-installed setscrews
Torque driver.
The outer box contains:
Literature.

24
Technical Support
St. Jude Medical Cardiac Rhythm Management Division maintains 24-hour phone lines for technical
questions and support:
1 818 362 6822
1 800 722 3774 (toll-free within North America)
+ 46 8 474 4147 (Sweden)
For additional assistance, call your local St. Jude Medical representative.
Additional Information
For additional information on this device, see the programmer's on-screen help.

Cardiac Rhythm Management Division
15900 Valley View Court
Sylmar, CA 91342 USA
+1 818 362 6822
Veddestavägen 19
SE-175 84 Järfälla
Sweden
+46 8 474 4000
sjm.com
April 2012
Art 60031731/B