Boston Scientific Neuromodulation PSC5210W Precision SCS System Remote Control User Manual II Patient Handbook
Boston Scientific Neuromodulation Corporation Precision SCS System Remote Control II Patient Handbook
Contents
Patient Handbook
Patient System Handbook
CAUTION:
Federal law restricts this device to sale, distribution and use by or on the order of a physician.
MP9055184 Rev A
DRAFT
Patient System Handbook
ii
Copyright
©2004 by Advanced Bionics Corporation. All Rights Reserved. Any copying, reproduction or
translation of all or part of the contents of this document without the express written permission of
Advanced Bionics Corporation is strictly forbidden by the provisions of the law of March 11th,
1957.
Guarantees
Advanced Bionics Corporation reserves the right to modify, without prior notice, information
relating to its products in order to improve their reliability or operating capacity.
Registered Trademarks
Vel c ro ® is a registered mark of Velcro Industries, Manchester, New Hampshire. Other brands and
their products are trademarks or registered trademarks of their respective holders and should be
noted as such.
Table of Contents
iii
Table of Contents
1 Introduction .......................................................................1
2 System Description ...........................................................3
3 Safety Information ............................................................7
Indications for Use ................................................................. 7
Precision System Clinical Summary .......................................... 7
Contraindications ................................................................. 16
Warnings ............................................................................ 16
Precautions .......................................................................... 19
Adverse Effects ..................................................................... 23
4 The Remote Control .......................................................27
Buttons and Basic Operation ................................................ 27
Stimulation On and Off ........................................................ 30
The Level Screen .................................................................. 30
Stimulation Level Control ....................................................... 33
Selecting Areas for Level Control ........................................... 34
Programs ............................................................................. 35
Selecting and Activating Programs ........................................ 36
Patient System Handbook
iv
Saving Program Changes ..................................................... 37
Options ............................................................................... 40
Understanding Battery Status Messages ................................ 46
Battery Replacement ............................................................. 50
5 Charging the Implant .....................................................51
Getting Started .................................................................... 53
Charging Your Implant ......................................................... 54
6 Help ..................................................................................59
Stimulation ........................................................................... 59
Remote Control Display Messages ........................................ 61
Accessories ......................................................................... 64
Contacting Advanced Bionics ............................................... 64
7 Limited Warranty ...........................................................65
Implanted Pulse Generator .................................................... 65
Externals .............................................................................. 67
Glossary ...........................................................................71
Index..................................................................................75

1
1Introduction
The Advanced Bionics® Precision™ SCS (Spinal
Cord Stimulation) system is prescribed for the
management of chronic pain. The system
electrically stimulates the spinal cord to alter the
perception of pain signals that move along the
nerve pathways on either side of the spine.
Paresthesia is the term that describes the light,
tingling sensation—the “feeling”—of spinal
cord stimulation.
Before receiving your new implant, you had the
opportunity to test stimulation therapy and
decide if it would work for you. By choosing to
have a stimulator surgically implanted, you
Patient System Handbook
2
confirmed that paresthesia is capable of providing you with good to excellent pain relief. As
you go forward with this therapy, your health professionals will work with you to find the
most comfortable level of paresthesia to cover the painful areas by adjusting your implant’s
settings. Although you may have pain areas that cannot be reached by spinal cord
stimulation, the goal is to bring you the most effective pain relief possible. The more you
help and work with your health professionals, the more likely you are to achieve the best
outcome possible from your new Precision system.
Advanced Bionics is an organization dedicated to helping you manage your pain. We will
help you make the most of this therapy for an improved quality of life.

3
2 System Description
The Precision system includes both implanted and external components: During your
surgery, one or more wires called leads were placed along your spinal cord where pain
signals to the brain can be intercepted. The lead was then attached to an implantable pulse
generator (IPG), also referred to as an implant. The IPG is commonly placed in the
abdomen, upper buttock, or subclavicular area. The implant sends a small electrical current
to a series of stimulating contacts, called electrodes, at the end of the lead. The battery-
powered implant is controlled by a hand-held programmer or Remote Control, and is
periodically recharged using a separate Charging System.
The Remote Control, the heart of the Precision system, is a powerful yet easy to use tool for
managing every aspect of your pain treatment—from controlling the level, or strength, of
stimulation to accessing special treatment programs and program options.
Patient System Handbook
4
To make the most of your Precision system, it’s important to learn:
1. what to be aware of for safety,
2. how to use the Remote Control, and
3. how to recharge the implant.
These subjects are covered on the following pages, and we encourage you to read this
manual entirely. If you have any questions, or need clarification of anything contained in
this manual, feel free to contact our Customer Service Department at (866) 360-4747.

System Description
5
Before reading more about the Precision System, first check that all of the following items
were included in your Patient Kit. (And check to be sure you have your Temporary Patient
Identification Card; keep it with you until you receive your permanent card.) If any item is
missing, please call our Customer Service department for a replacement.
(1) Remote Control
(1) Charger
(1) Charger Base Station
(1) Power Supply
(1) Remote Control Cover
(1) Velcro® Charging Belt
(1) Charger Adhesives (52 pieces)
(1) Remote Control Batteries (3)
(1) Carrying Case
Front
Permanent Patient Identification Card
Back
Patient System Handbook
6
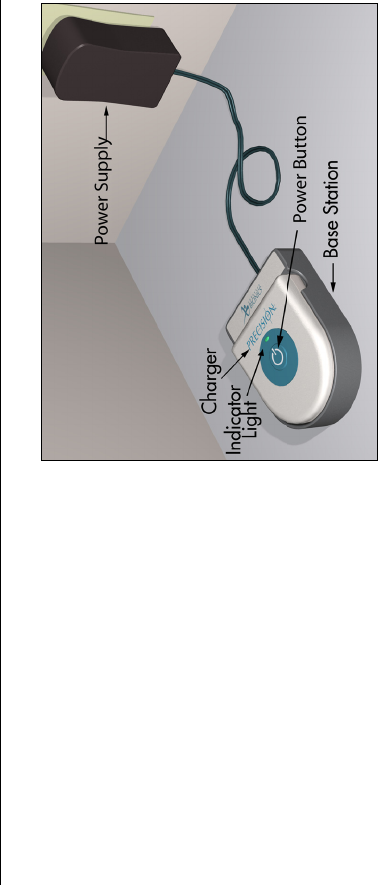
Find a convenient electrical outlet, one
that won’t expose the Charging System
parts to water or direct heat, and plug in
the Base Station Power Supply. Next,
connect the Power Supply to the Base
Station, and locate the Base Station on a
flat surface. Finally, place the Charger in
the Base Station with the stimulation on/
off button facing up.
For now, that’s all you need to do to get
started. For more information on the
Charging System and its use, see
“Charging the Implant” on page 51.

7
3 Safety Information
Indications for Use
The Advanced Bionics Precision™ Spinal Cord Stimulator System (Precision System) is
indicated as an aid in the management of chronic intractable pain of the trunk and/or limbs,
including unilateral or bilateral pain associated with the following: failed back surgery
syndrome, intractable low back pain and leg pain.
Precision System Clinical Summary
Determination of the safety and effectiveness of the PRECISION System was based on
available published clinical studies for similar implanted spinal cord stimulation systems.
The PRECISION System is similar to the SCS systems reported in published literature in
intended use, target patient population, technology, device design, and output
characteristics. Therefore, the clinical data from the published literature described below
represents evidence supporting the safety and effectiveness of the PRECISION System for
Patient System Handbook
8
the treatment chronic intractable pain of the trunk and/or limbs, including unilateral or
bilateral pain associated with the following: failed back surgery syndrome, intractable low
back and leg pain.
Efficacy Evaluation
Three (3) clinical literature studies were used to support the effectiveness of the
PRECISION System (Ohnmeiss et al. 1996, Villavincencio et al. 2000, Hassenbach SJ et al.
1995). The studies included a total of 116 patients that were implanted with an SCS system.
A total of approximately 3166 device months of experience was depicted from the
retrospective clinical evaluation. All three studies examined the effectiveness of SCS on
patients with chronic pain of the trunk and/or limbs including unilateral or bilateral pain
associated with the following: failed back surgery syndrome or intractable low back and leg
pain. In all studies, a totally implantable spinal cord stimulator was used in association with
a percutaneous and/or surgical lead. These studies provide the same diagnostic or
therapeutic intervention for the same disease/conditions and patient population as the
PRECISION System.
The prospective study by Ohnmeiss et al. 1996, examined the long-term effectiveness of
SCS in patients with intractable leg pain. Forty patients were implanted with SCS systems
and evaluated at 6 weeks, 12 months, and 24 months follow-up. Outcome measures
included the VAS, pain drawings, medication use, SIP (Sickness Impact Profile), isometric
Safety Information
9
lower extremity testing, and patient questionnaires. An intent-to-treat analysis was
performed. After patients had SCS for 24 months, leg pain, pain when walking, standing
pain, pain’s effect on overall lifestyle, and the total analog scale scores were significantly
improved from baseline. In this study, 25% of the implanted patients had greater than 50%
improvement in pain rating.
In addition, 3 patients from this study had their stimulators repositioned due to pain at the
original location. Three patients had reoperations to adjust lead position; 1 patient required 2
reoperations, 1 patient had the device removed due to infection and later to have a new
device implanted. A diabetic patient had skin problems which required device removal; a
new device was later implanted. Two patients had the device removed due to unsatisfactory
pain relief.
The prospective study performed by Villavicencio et al. 2000 included 41 patients with pain
of various etiologies. The majority of the patients, 24 (59%), had Failed Back Surgery
Syndrome (FBSS), 7 (17%) had Complex Regional Pain Syndrome (CRPS I and II), 4
(10%) had neuropathic pain syndrome, and 6 (15%) were diagnosed as stroke or other.
Patients underwent an initial trial period for SCS with temporary leads. If the trial resulted
in greater than 50% reduction in the patient’s pain, as measured by the VAS, the patient was
implanted with a SCS system. In this study, 27/41 patients, 66%, had permanent implants.
Patient System Handbook
10
All patients were examined after 6 weeks. Pain measurements were assessed at 3-6 month
intervals for the first year and annually thereafter. The median long-term follow-up was 34
months. A total of 24/27 (89%), reported greater than 50% reduction in pain. Since the
majority of the patients were treated for FBSS, this article supports the use of SCS for the
treatment of FBSS.
In this study, one patient required a revision because of electrode fracture. One patient
required removal of the system due to local infection. One patient required replacement of
the IPG due to mechanical failure. Overall, 16 of 27 (59%) patients required a total of 36
repositioning procedures.
A retrospective analysis performed by Hassenbusch SJ et al. 1995 included patients with
chronic lower body pain, predominately neuropathic pain and pain either midline lower
back and/or unilateral or bilateral leg pain treated over a 5 year period. The study was a
comparison of SCS to spinal infusion of opiods. For patients with radicular pain involving
one leg with or without unilateral buttock pain, a trial of SCS was recommended first. For
patients with midline back pain and /or bilateral leg pain, a trial of long-term spinal infusion
was recommended first. If the patients failed screening with either of these modalities, the
other was then tested. If the treatment reduced the pain by 50%, the systems were
internalized. A retrospective analysis of patients with unilateral leg and/or buttock pain
Safety Information
11
treated initially with SCS and bilateral leg or mainly low back pain treated initially with
spinal infusions of opioids was then done.
In this study, 42 patients were screened; 26 (62%) patients received spinal stimulation; 16
(38%) received opioids via a spinal infusion pump. Five patients did not receive adequate
pain relief with SCS; 3 (7%) of these patients underwent trial spinal infusions and had
effective pain relief. There were 4 (10%) patients who underwent a trial of spinal infusion of
opioid but did not receive adequate pain relief; these patients were not tested with SCS. Pain
severity was rated using a verbal digital pain scale: “On a scale of 0 to 10 where 0 is no pain
and 10 is the worst pain you could ever imagine, what is your pain now?” 16/26 patients
(62%) had greater than 50% pain relief with SCS. In this study, 2/16 (13%) had greater than
50% pain relief with opioids. Mean follow-up was 2.1 + 0.3 years. This analysis supports
the use of SCS for intractable low back and leg pain.
In this study, 7 (17%) patients suffered complications after implantation of the device; 5
(12%) patients required repositioning of catheter type electrodes and 2 patients required
revision of the stimulator generator.
Safety Evaluation
Eleven studies were identified based on the detailed inclusion/exclusion criteria to
demonstrate the safety of the PRECISION System. The studies included a total of 1056
Patient System Handbook
12
patients that were trialed with SCS systems and 880 patients that received implants. The
table below depicts the number of patients, the number of events, and the percentage of
occurrences of each event compared to the total number of patients. It should be noted that
citations cover both IPG and RF Systems. The clinical experience reported in the literature
on RF systems is relevant to determining the safety of totally implantable IPG systems.
Table 1: Summary of Risks Identified in the Retrospective Clinical Studies
Risks
# Patients
With
Adverse
Event
Intent-to-
Treat Basis
N = 1056
Implanted
Patient
Basis
N = 880
Lead Migration 175 16.6% 19.9%
Infection 39 3.7% 4.4%
Epidural Hemorrhage 0 0% 0%
Seroma 0 0% 0%
Hematoma 1 0.1% 0.1%
Paralysis 0 0% 0%
CSF Leak 5 0.5% 0.6%
Safety Information
13
Clinical Experience-Safety
Clinical data has been collected during a clinical study of the PRECISION™ System. As of
January 15, 2004, 35 subjects were enrolled in the study at multiple sites and 26 subjects had
a successful trial stimulation period and were implanted with the PRECISION™ System.
Over/Under Stimula-
tion, Ineffective Pain
Control
46 4.4% 5.2%
Intermittent Stimula-
tion
00%0%
Pain Over Implant 16 1.5% 1.8%
Allergic Reaction 6 0.6% 0.7%
Skin Erosion 0 0% 0%
Lead Breakage 35 3.3% 4.0%
Hardware Malfunction 22 2.1% 2.5%
Loose Connection 0 0% 0%
Battery Failure 2 0.2% 0.2%
Other 45 4.3% 5.1%
Patient System Handbook
14
The follow-up period for the 26 implanted patients ranged from two weeks to six months.
The following major adverse events were reported.
Table 2: Clinical Experience Safety
Other minor adverse events reported by at least one patient included: receiver malfunction,
skin irritation, unpleasant stimulation, CSF leak, infection at implant site, lead migration,
and OR cable malfunction. Two of the subjects reported multiple events.
References
Burchiel, K.J., V.C. Anderson, F.D. Brown, R.G. Fessler, W.A. Friedman, S. Pelofsky, R.L. Weiner, J.
Oakley,and D. Shatin. “Prospective, Multicenter Study of Spinal Cord Stimulation for Relief of Chronic
Back and Extremity Pain.” Spine, 21:2786-2793, 1996.
Type Number of Patients Resolution
Lead Migration 1 Lead repositioning
and subsequent
replacement
Output malfunction 1 Device replaced
Infection 1 Infection treated
Pain 1 Lead explanted
Safety Information
15
Hassenbusch, S.J., M. Stanton-Hicks, E.C. Covington. “Spinal cord stimulation verses spinal infusion for low
back and leg pain”. Acta Neurochirgica, 64:109-115, 1995.
Kemler, M.A., G.A.M. Barendse, M. Van Kleef, H.C.W. De Vet, C.P.M. Rijks, C.A. Furnee and F.A.J.M. Van
den Wilderberg. “Spinal Cord Stimulation in Patients with Chronic Reflex Sympathetic Dystrophy.”
New England J of Medicine, 343: 618-24, 2000.
Kim S. H., R.R. Tasker, and M.Y. Oh. “Spinal Cord Stimulation for Nonspecific Limb Pain versus Neuropathic
Pain and Spontaneous versus Evoked Pain.” Neurosurgery, 48(5): 1056-1064, 2001.
Kumar, K., C. Toth, R. Nath, and P. Lang. “Epidural Spinal Cord Stimulation for Treatment of Chronic Pain-
Some Predictors of Success. A 15 year experience.” Surg Neurol, 50: 110-120, 1998.
Lang, P. “The Treatment of Chronic Pain by Epidural Spinal Cord Stimulation.” AXON, 18(4): 71-73, 1997.
Ohnmeiss, D., R. Rashbaum, M. Bogdanffy. Prospective Outcome Evaluation of Spinal Cord Stimulation in
Patients With Intractable Leg Pain. Spine, 21:1344-1351, 1996.
Rainov, N.G., V. Heidecke, and W. Burkert. “Short Test-Period Spinal Cord Stimulation for Failed Back
Surgery Syndrome.” Minim Invasive Neurosurg, 39(2):41-44, 1996.
Segal, R., B. Stacey, T. Rudy, S. Basser, J. Markham. “Spinal Cord Stimulation Revisited.” Neurological
Research, 20:391-396, 1998.
Patient System Handbook
16
Spieglemann, R. and W.A. Friedman. “Spinal Cord Stimulation: A Contemporary Series.” Neurosurg 28:65-
71, 1991.
Villavicencio, A.T., J.C. Leveque, L. Rubin, K. Bulsara, and J.P. Gorecki. “Laminectomy versus percutaneous
electrode placement for spinal cord stimulation.” Neurosurgery, 46:399-406, 2000.
Contraindications
Patients contraindicated for permanent SCS therapy are those who:
• are unable to operate the SCS system
• have failed trial stimulation by failing to receive effective pain relief
• are poor surgical risks
• are pregnant
Warnings
Magnetic Resonance Imaging (MRI). You should not be exposed to Magnetic Resonance
Imaging (MRI). Exposure to this diagnostic technology may result in dislodgement of your
IPG or lead(s), heating of the IPG, severe damage to the IPG electronics and/or increased
voltage through the leads or IPG which can cause an uncomfortable or “jolting” sensation.
Safety Information
17
Pediatric Use. The safety and effectiveness of spinal cord stimulation has not been
established for pediatric use.
Diathermy. As an SCS patient, you should not have any form of diathermy as either as
treatment for a medical condition or as part of a surgical procedure. The high energy and
heat generated by diathermy can be transferred through your stimulator system, causing
tissue damage at the lead site and, possibly, severe injury or death. The IPG, whether it is
turned on or off, may be damaged.
Cardiac Pacemakers. Spinal cord stimulators may interfere with the operation of
implanted sensing stimulators, such as pacemakers and implantable cardiac defibrillators
(ICDs). Be sure your physicians are aware of your spinal cord stimulator before going
forward with other implantable device therapies so that medical decisions can be made and
appropriate safety measures taken.
Implant Damage. Burns may result if the pulse generator case is ruptured or pierced and
patient tissue is exposed to battery chemicals. Do not implant the device if the case is
damaged.
Posture. Changes in posture or abrupt movements may cause decreases, or uncomfortable
or painful increases in the perceived stimulation level. Keep the Remote Control with you at
Patient System Handbook
18
all times, and turn the stimulation down or off before making posture changes. If unpleasant
sensations occur, the stimulation should be turned off immediately.
Electromagnetic Interference. Strong electromagnetic fields can potentially turn the
stimulator off, or cause uncomfortable or jolting stimulation. Avoid or exercise care around:
• Theft detectors or security screeners, such as those used at entrances/exits of
department stores, libraries, and other public establishments, and/or airport security
screening devices. It is recommended that you request assistance to bypass the device.
If you must proceed through the device, turn off the stimulator and proceed with
caution, and move through the center of the screener as quickly as possible.
• Power lines or power generators
• Electric steel furnaces and arc welder
• Large magnetized stereo speakers
As you approach these devices you may become aware of changing stimulation levels. In
rare instances, you could experience an increase in stimulation level to the point that the
sensation is uncomfortably strong or possibly “jolting.” If this happens, turn off the IPG. If
the IPG suddenly turns off by itself, first move away from the area. Next, check the implant
status with the Remote Control by pressing the Stimulation On/Off button and observing the
Safety Information
19
screen. The IPG may need to be recharged before stimulation can be re-started. (See
“Charging the Implant” on page 51 for additional information.)
Always be aware of your surroundings, particularly near theft detectors/security screeners.
Ask for assistance to go around these devices if you feel at all uncomfortable.
Precautions
Physician training is required.
Medical Devices/Therapies. The following medical therapies or procedures may turn
stimulation off or may cause permanent damage to the implant, particularly if used in close
proximity to the device:
• lithotripsy — high-output sound or shock waves often used to treat gall stones
and kidney stones
• electrocautery — the use of a heated electric probe to stop bleeding during
surgery
• external defibrillation — the use of electrically charged paddles to restart the
heart in an emergency
• radiation therapy — ionizing energy commonly used to treat cancer
Patient System Handbook
20
• ultrasonic scanning — very high frequency sound waves used to produce images
of internal organs or tissue for diagnostic purposes
• high-output ultrasound — high frequency sound waves which may be applied as
physical therapy to treat certain bone/muscle injuries, or for muscle stimulation,
or to improve blood flow
Before having procedures, medical therapies, or diagnostics, have your healthcare
professional call our Customer Service department at (866) 360-4747 for proper
instructions.
Automobiles and Other Equipment. Do not operate an automobile, other motorized
vehicle, or any potentially dangerous machinery/equipment with therapeutic stimulation
switched on. Turn off stimulation first. Sudden stimulation changes, if they occur, may
distract you from attentive operation of the vehicle or equipment.
Post Operative. During the two weeks following surgery, it is important to use extreme
care so that appropriate healing will secure the implanted components and close the surgical
incisions:
Safety Information
21
Do not exercise or attempt to move heavy objects, and avoid deep bending and stretching.
Temporarily, there may be some pain in the area of the implant as the incisions heal. If
discomfort continues beyond two weeks, contact your physician.
If you notice excessive redness around the wound areas during this time, contact your
physician to check for infection and administer proper treatment. In rare cases, adverse
tissue reaction to implanted materials can occur during this period.
Implant Location. Never attempt to change the orientation or “flip” the implant. Do not
“finger” or play with the implant. If the implant flips over in your body it cannot be charged.
If you know that the device has turned, or if stimulation cannot be turned on after charging,
contact your physician to arrange an evaluation of the system.
In some cases, the skin over your implant may become very thin over time. If this occurs,
contact your physician.
Lead Location. In some instances a lead can move from its original location, and
stimulation at the intended pain site can be lost. If this occurs, consult your physician who
may able to restore stimulation by reprogramming the implant in the clinic or repositioning
the lead during another operation.
Patient System Handbook
22
Device Failure. Implants can fail at any time due to random component failure, loss of
battery functionality, or lead breakage. If the device stops working even after complete
charging (up to four hours), turn off stimulation and contact your physician so that the
system can be evaluated.
Storage. Do not expose the Remote Control or Charging System components to
excessively hot or cold conditions. Do not leave the devices in your car or outdoors for
extended periods of time. The sensitive electronics can be damaged by temperature
extremes, particularly high heat. If the Remote Control or the Charging System is to be
stored for a period of time, be careful that the storage temperature does not exceed -20–60
°C (-4–140 °F).
Handling. Handle the system components and accessories with care. Do not drop them or
submerge them in water. Avoid all sources of water that can come into contact with the
devices. Although reliability testing has been performed to ensure quality manufacturing
and performance, dropping the devices on hard surfaces or in water, or other rough
handling, can permanently damage the components. (See “Limited Warranty” on page 65.)
Component Disposal. Do not dispose of the Remote Control or Charger in fire. The battery
in these devices can explode in fire. Dispose of used batteries in accordance with local
Safety Information
23
regulations. The IPG should be explanted in the case of cremation, and returned to
Advanced Bionics.
Remote Control, Charging System Cleaning. The components can be cleaned using
alcohol or a mild detergent applied with a cloth or tissue. Residue from soapy detergents
should be removed with a damp cloth. Do not use abrasive cleansers for cleaning.
Cell Phones. While we don’t anticipate any interference with cell phones, the full effects of
interaction with cell phones are unknown at this time.
Adverse Effects
Potential risks are involved with any surgery. The possible risks of implanting a pulse
generator as part of a system to deliver spinal cord stimulation include:
• The lead(s) which deliver stimulation may move from their original implanted
location, resulting in undesireable changes in stimulation and subsequent
reduction in pain relief.
• System failure, which can occur at any time due to random failure(s) of the
components or the battery. These events, which may include battery leakage,
device failure, lead breakage, hardware malfunctions, loose connections,
Patient System Handbook
24
electrical shorts or open circuits and lead insulation breaches, can result in
ineffective pain control.
• Your body may react negatively to the materials used to manufacture the
stimulator or the leads. You may notice redness, warmth or swelling of the
implant area.
• The skin over your implant may become thin and increasingly tender over time.
A seroma may be formed.
• The most common surgical procedural risks are temporary pain at the implant
site and infection. However, since the leads are placed in the fluid surrounding
your spinal cord, there is a small risk that spinal fluid may leak from the lead
insertion site following surgery. Very rarely, you may develop an internal blood
clot (hematoma) or blister (seroma); or you may experience brain hemorrhage or
paralysis. Your spinal cord may become compressed.
• External sources of electromagnetic interference may cause the device to
malfunction and affect stimulation.
• MRI. Exposure to magnetic resonance imaging (MRI) can result in noticeable
heat near the implant or the leads; may distort or destroy the image needed for
diagnosis; and may produce enough electromagnetic interference (EMI) to erase
Safety Information
25
the implant programming, destroy the leads, or cause the leads to move from
their intended location.
• Undesirable stimulation may occur over time due to cellular changes in tissue
around the electrodes, changes in electrode position, loose electrical connections
and/or lead failure.
• You may experience painful electrical stimulation of your chest wall as a result
of stimulation of certain nerve roots several weeks after surgery.
• Over time, your implant may move from its original position.
• You may experience weakness, clumsiness, numbness or pain below the level of
implantation.
• You may experience persistent pain at the IPG or lead site.
Patient System Handbook
26
27
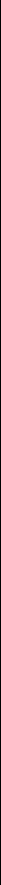
4 The Remote Control
Each button on the Remote Control activates one or more
of the stimulation functions which are described in detail
on the following pages of this section.
Buttons and Basic Operation
To use most Remote Control functions, you will simply
press a button as you would on a TV remote control.
Other functions require a “long press,” which is described
in “Selecting Options” on page 41.
Program Button
Area Button
Stimulation On/Off Button
Up/Activate
Down/Save
Patient System Handbook
28
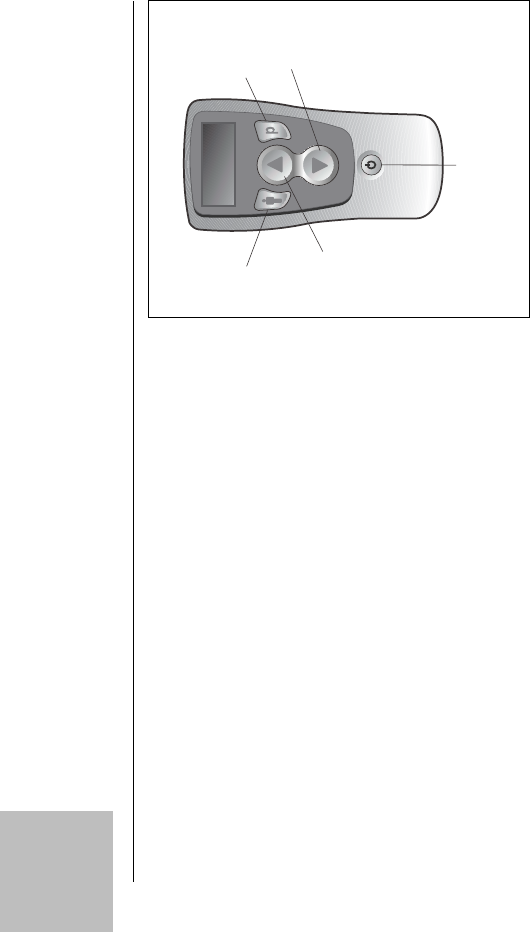
When it is not being used, the Remote Control sets
itself in a “sleep” or idle mode and the display screen
is blank. When you press any button except E
(stimulation on/off) during this sleep mode, the
Remote Control will “wake up” and display the
screen shown on the right. After you unlock the
buttons by pressing D, the remote will immediately
look for your implant and then connect with it,
allowing you to make adjustments to your
stimulation. When you are finished using it (no
buttons are being pressed), the remote will return to
the sleep mode within a minute or so.
P
Keys Locked
Press To
Unlock
The Remote Control
29
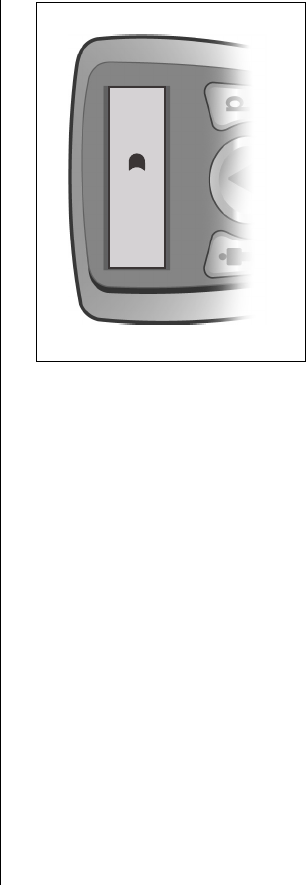
Good communication between your implant and the
Remote Control is very important. For that reason,
you will sometimes see the message “Connecting...”
while you are using the Remote Control because it is
always checking for the implant.
Note: If there is a problem communicating with the
implant, the message “No Response” will appear
on the Remote Control screen. See “Help” on
page 59 for more information.
The Remote Control unit is your direct link to
choices available for tailoring spinal cord stimulation
to suit your comfort and convenience requirements.
Keep the Remote Control with you at all times.
Patient System Handbook
30
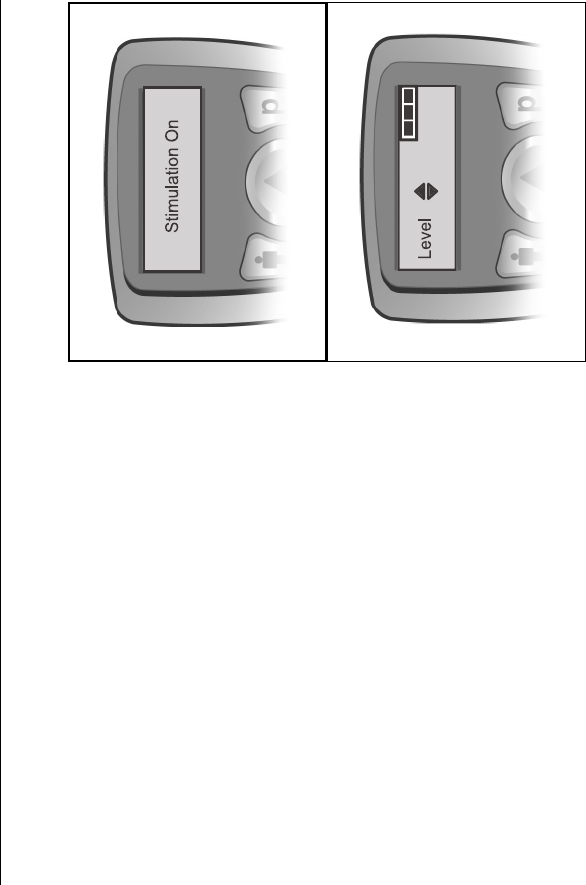
Stimulation On and Off
The Remote Control uses a “dedicated” stimulation
on/off switch.You may press E at any time—even
during the remote’s sleep or idle mode—to turn
stimulation on or off. The remote will briefly display
a message notifying you of the on or off status.
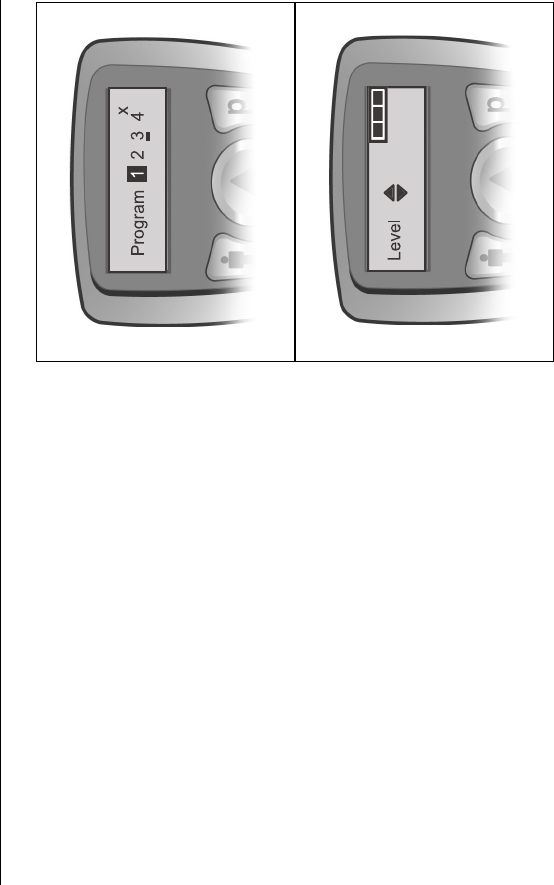
The Level Screen
Whenever stimulation is turned on, or after the
Remote Control is awakened from sleep/idle mode,
the remote display defaults to the Level screen.
When you press the S or T button from this display,
you’re able to increase or decrease the stimulation
strength, or level, of all of your pain areas at once (if
your implant was programmed to treat more than one
The Remote Control
31
area). To learn about adjusting the stimulation of individual areas, please see “Selecting
Areas for Level Control” on page 34.
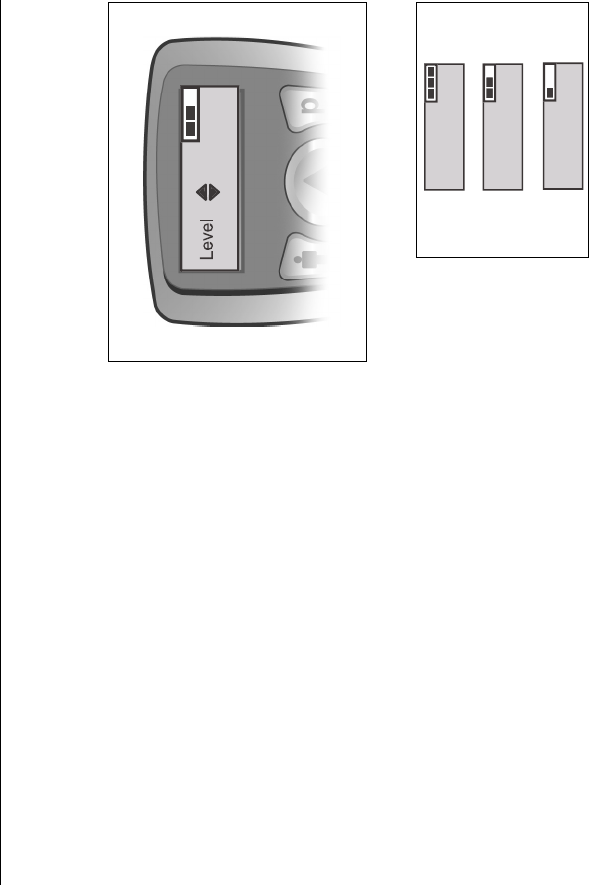
The Level screen also displays a bar graphic in the
upper right corner to indicate the battery charge level
of your implant. The graphic is very easy to
understand: Three filled-in bars means that your IPG
has a fully-charged battery. As the battery strength
wears down, depending on your stimulation settings
and usage, the bars will “empty” accordingly. For
complete information on maintaining your implant’s
battery for uninterrupted delivery of the therapy
prescribed for you, see “Charging the Implant” on
page 51.
OK
Full
Low
Patient System Handbook
32
Note: • Remember, the Level screen will remain on the display for approximately one minute if you
don’t press a button to perform an action with the Remote Control. After a minute, the
remote will go into idle mode and the display will go blank.
•Multiple area control is available only if your
system has been programmed to deliver stimula-
tion to separate areas. If you do not have sepa-
rate area control (for example, left leg vs. right
leg) but feel that separate control might improve
your therapy, contact your health professional to
determine what is possible.
The Remote Control
33
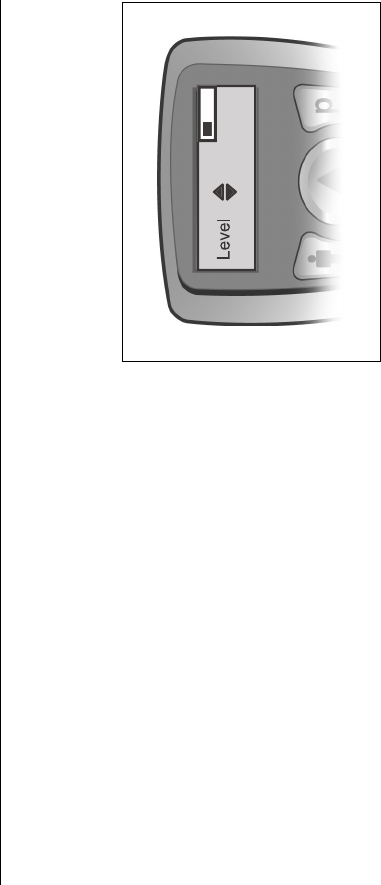
Stimulation Level Control
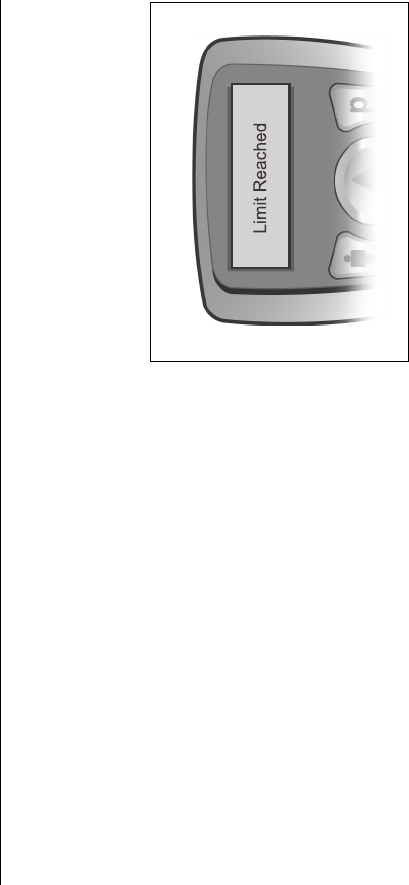
Occasionally, you may see one of the accompanying
messages on the Remote Control screen while
changing the stimulation level. These displays, and a
“beep” from the Remote Control, alert you that you
have reached either a maximum or a minimum level:
The bar replacing the up arrow means that you have
reached the maximum allowable level and can only
decrease the stimulation setting. The bar replacing
the down arrow means that you have reached the
minimum level and can only increase the stimulation
setting.
Patient System Handbook
34
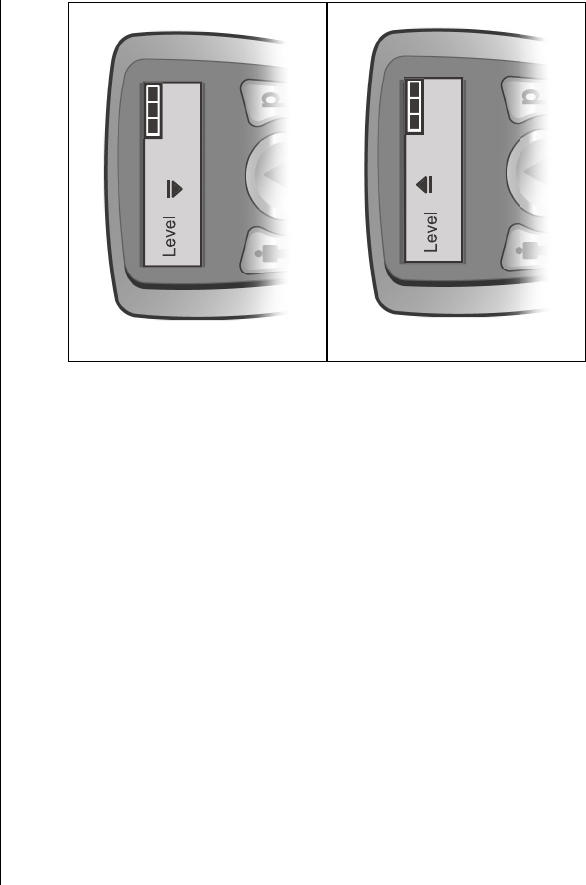
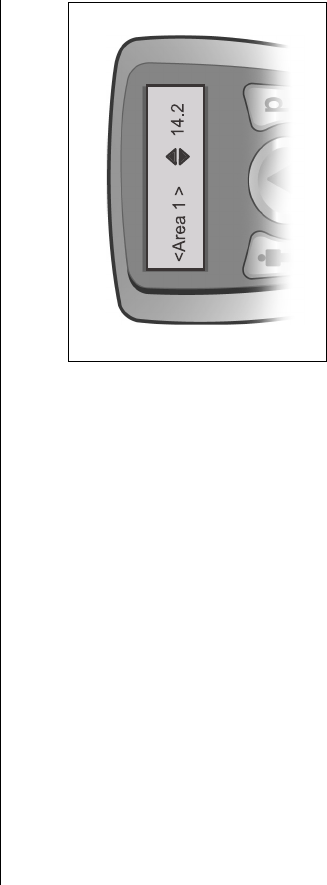
Selecting Areas for Level Control
Your Remote Control may have as many as four
therapy areas stored for your use. Each area will have
a name or a number (1 through 4) which was
assigned during your programming at the clinic.The
stimulation level for each of these areas is controlled
from an individual “area level” screen. To change the
stimulation strength of a single area:
1. From the main Level screen, press the Cbutton
as many times as necessary to cycle through your
programmed area Level screens.
Note: Button presses will move from one area to the next and will eventually return you to the Level
screen.
2. When the named or numbered area that you want to adjust is shown on the screen, press
S or T to change the stimulation level for that area.
When you’ve finished making your change, the Remote Control will return to the Level
screen.
The Remote Control
35
Programs
A stimulation program may provide paresthesia to cover a single pain area, or up to four
areas, depending on how the program was set up by your clinician. Your Remote Control
can store up to four programs—numbered 1 through 4—for you to select and activate at any
time. Often, the programs will have certain differences in the settings to allow you to vary
your stimulation in several ways. You may have been encouraged to try using specific
programs for different circumstances, or different body positions, or different times in your
daily routine. Programs and their flexibility give you and your healthcare professional a way
to continually “fine tune” your therapy.
Patient System Handbook
36
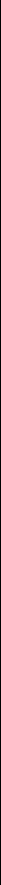
Selecting and Activating Programs
1. Press the Dbutton from the Level screen to go to
the Program screen.
From the Program screen, each additional
Dbutton press cycles you through the program
numbers. The black highlight box shows where
you are in the cycle. Pressing Dfrom program 4
returns you to the Level screen.
2. Press Duntil the program you want is
highlighted, then press S to activate the program.
The Remote Control
37
Note: • You might not have four programs saved in your
Remote Control. Empty program slots will have
an X beside the program number. If you try to
activate an empty program, nothing will happen.
•An underline beneath a program number means
that program was the most recently activated,
saved (see below), or restored (see page 44) pro-
gram.
Once you have selected and activated a program, the
Remote Control will return to the Level screen. Use
the S or T to adjust the stimulation level of the
program, if you wish.
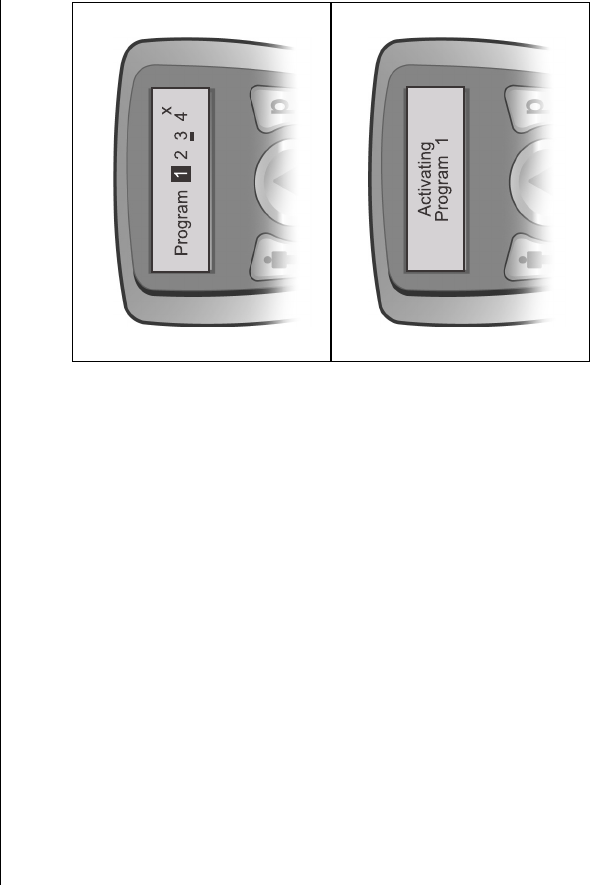
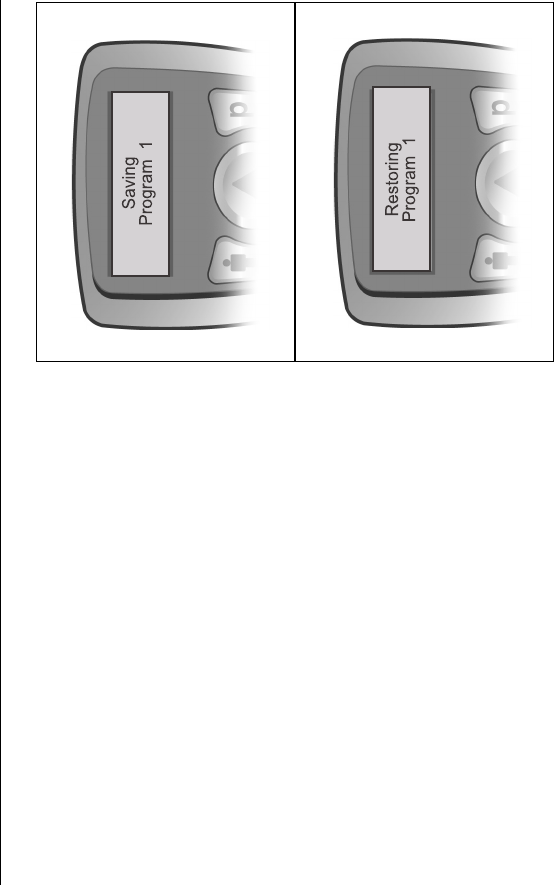
Saving Program Changes
If you do make a stimulation level adjustment and
decide that you prefer it to the original setting, you
can save the new level (or any other change) and
make it a permanent part of the program:
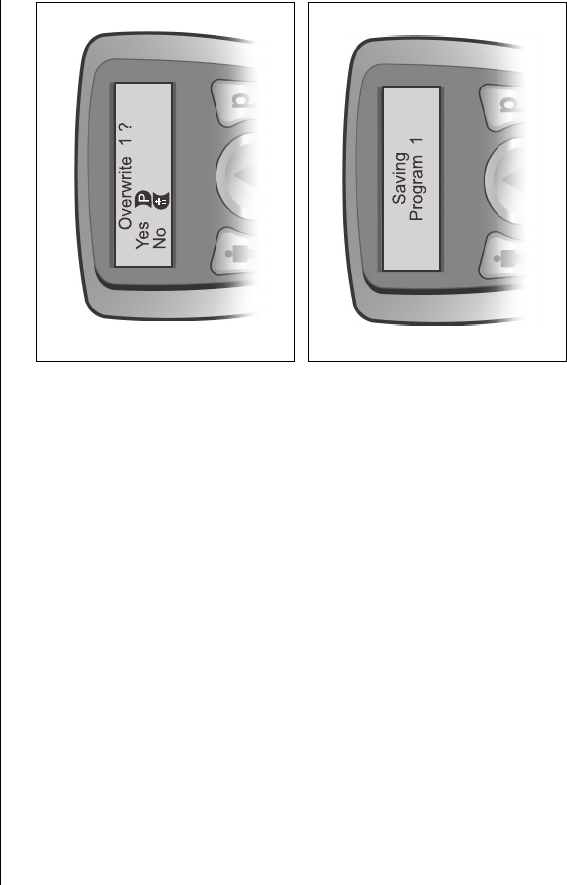
Patient System Handbook
38
1. After making a change to a program, press D
from any screen to return to the Program screen.
2. From the Program screen, press Das many times
as necessary to select the active program; that is,
the program that is currently running and the one
you’ve just changed.
3. With the active program selected, press T to save
the change in the remote’s memory.
The Remote Control will first ask you to confirm that
you want to “overwrite” the program; press the
appropriate button.
If you confirm the change (Yes, or D), the program
will be updated and saved. If you decide not to make
a permanent change, pressing Cwill return you to
the Program screen.
The Remote Control
39
You may also save a program change as a completely new program if an empty program slot
(X) is available: Simply select the empty slot using D and press T. After saving the new
program, the Remote Control will return to the Level screen.
Patient System Handbook
40
Options
Under some circumstances, and depending on your treatment prescription, your healthcare
provider may have given you therapy control beyond selectable programs by making special
options available to you. Program options make it possible for you to change certain preset
stimulation settings, and/or return changed programs to their original clinic settings. The
ability to go back to original settings allows you to change your mind... then change your
mind again... about how satisfied you are with your stimulation paresthesia.
If you’ve been told about program options and instructed in how to use them, you may
realize that you probably won’t “exercise” your option settings very often. However, if your
Remote Control has been set up to access options, please follow the steps detailed in
“Selecting Options” on page 41 to make adjustments.
The Remote Control
41
There are three possible options. One of these,
Restore, is not a stimulation setting but is similar to
an “undo” feature. It returns a changed program
back to its original settings. The other two options
are stimulation settings that can affect the overall
feeling of the stimulation you receive:
•Rate, or how many times-per-second your
implant sends a stimulation pulse, and
•Pulse Width, or how long each
stimulation pulse lasts.
Note: Restore is available to all patients. However, Rate and/or Pulse Width may not be available
to you. Their availability would have been discussed with you at your first programming
session.
Selecting Options
To access the options that may be available through your Remote Control, you will need to
use a “long” button press. This simply means that you will press and hold a button until a
Patient System Handbook
42
particular option screen is displayed. The action you take next depends on which option you
want to adjust. Follow the appropriate instructions below:
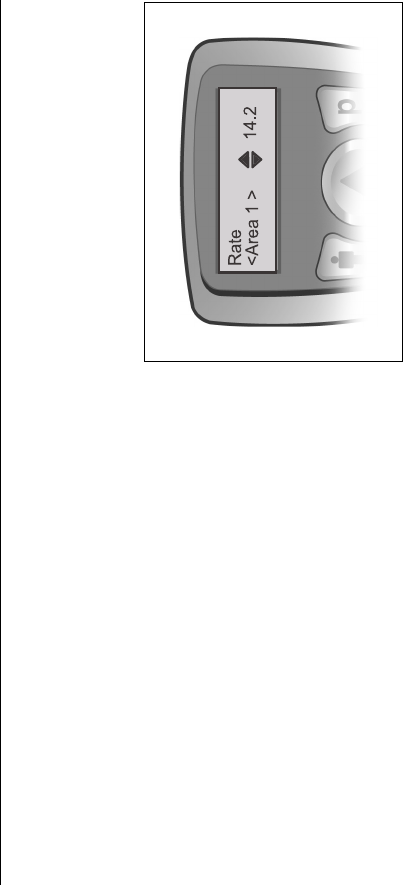
To Adjust Stimulation Rate:
1. From the Level screen, press and hold Cuntil
you see the Rate Area 1 screen. If this is the area
you want to adjust, press either S or T to
increase or decrease the Rate.
2. To move to another area, press Cbriefly (a
“normal” press) to cycle through your
programmed areas until you find the Rate Area
screen (2, 3 or 4) that you want.
3. Press either S or T to increase or decrease the
Rate.
Note: The Remote Control will beep to notify you if you reach a preset limit while increasing or
decreasing the Rate.
The Remote Control
43
To return to the Level screen from any Rate screen, press and hold Cuntil Pulse Width
Area 1 is displayed, then press and hold Cagain to see the Level screen. If you don’t have
access to the Pulse Width option, the Level screen will appear right away.
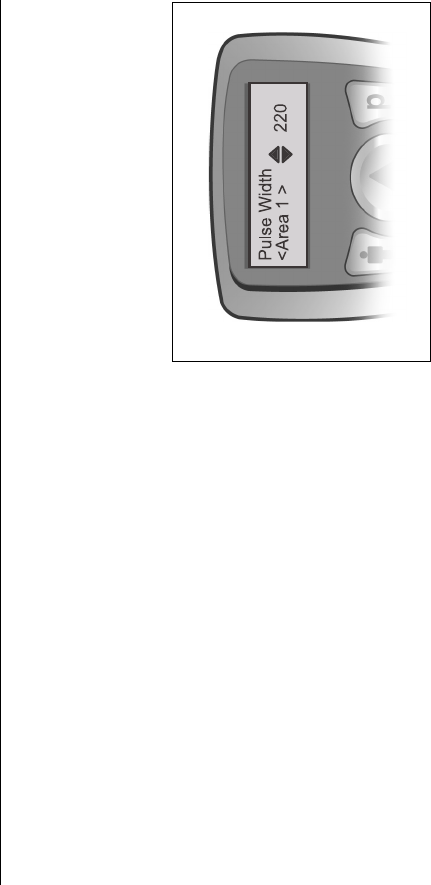
To Adjust Stimulation Pulse Width
1. From the Level screen make a long Cbutton
press to Rate Area 1.
Note: If you don’t have access to the Rate option, the long
press will take you directly to the Pulse Width Area
1 screen.
2. If the Rate Area 1 screen is displayed, make
another long Cbutton press to Pulse Width Area
1. If this is the area you want to adjust, press
either S or T to increase or decrease the Pulse
Width.
3. To move to another area, press Cbriefly (a “normal” press) to cycle through your
programmed areas until you find the Pulse Width Area screen (2, 3 or 4) that you want.
Patient System Handbook
44
4. Press either S or T to increase or decrease the Pulse Width.
Note: • You may also find Pulse Width Area 1 by making a long Cbutton press from any Rate
screen.
•The Remote Control will beep to notify you if you
reach a preset limit while increasing or decreas-
ing the Pulse Width.
To return to the Level screen from any Pulse Width
screen, press and hold C.
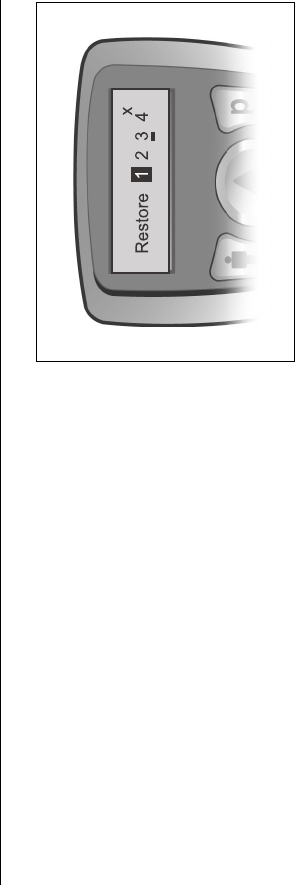
To Restore a Clinic Program
Over time, you may have made changes to one or
more of the programs originally saved to your
Remote Control. The Restore option allows you to
return to those original stimulation settings if ever you become dissatisfied with a changed
program.
The Remote Control
45
1. From the Level screen, press and hold Dto reach
the Restore screen. Program 1 will be
highlighted.
Note: The highlighted program is the current selection;
an underline indicates the last program saved,
activated, or restored; an X indicates an empty
program slot.
2. If necessary, press Dto cycle through the
program numbers to select the program you want
to restore. When the desired program is
highlighted, press S. The Remote Control will
briefly flash a message confirming the
restoration.
Patient System Handbook
46
Understanding Battery Status Messages
About the Remote Control Batteries
As an SCS patient, it’s essential that you appreciate the importance of battery power! The
replaceable batteries in your Remote Control and the rechargeable battery in your stimulator
work together to provide you with consistent, dependable parasthesia. Always pay close
attention to the battery status messages described in this section.
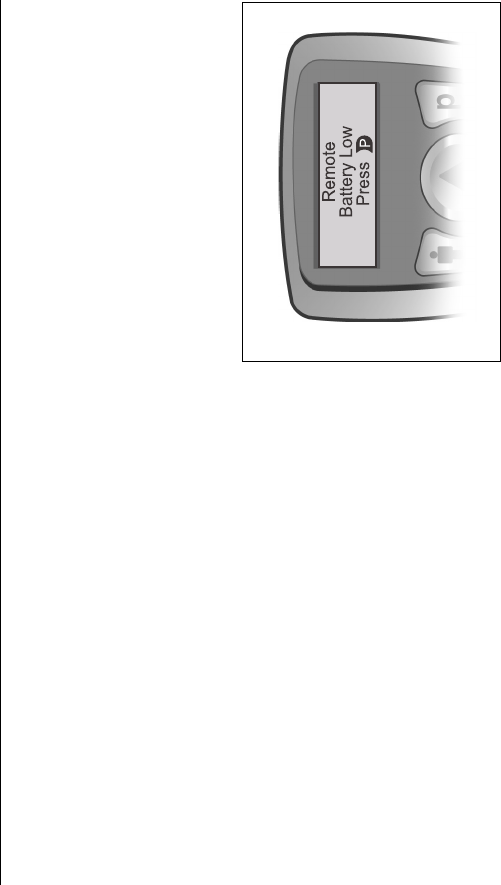
When the Remote Control batteries are at a low
power level, the battery message shown here will be
displayed. When you press the Dbutton from this
screen, the remote will make a check of your
implant’s battery status also.
If the implant battery is full or OK, the Remote
Control will return to the Level screen. To learn
about the messages you will see when the implant’s
battery is less than full, see page 48.
The Remote Control
47
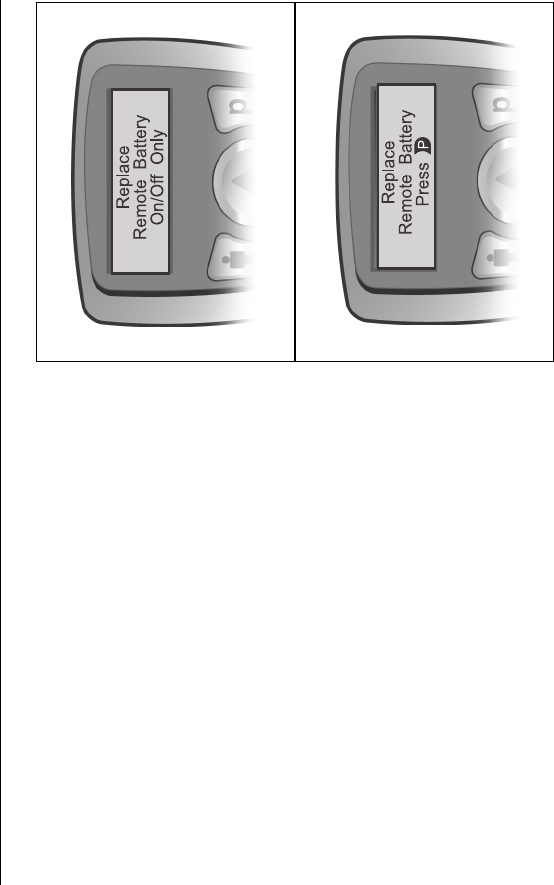
If you don’t respond to the Remote Battery Low
message in a timely manner, the batteries will
eventually drain to the point of not having enough
power to manage your stimulator.
First, you'd see a message meaning that (because of
its low-power condition) the Remote Control can't
send stimulation changes to your implant. You will
only able to turn stimulation on or off.
Next, you’d see the more urgent message shown
opposite. You must respond immediately! When you
press D, the remote will make another check of your
implant battery and may display one of the messages
shown on the following page.
Note: Make a habit of replacing the Remote Control
batteries when you first see the Remote Battery
Low message. See “Battery Replacement” on
page 50.
Patient System Handbook
48
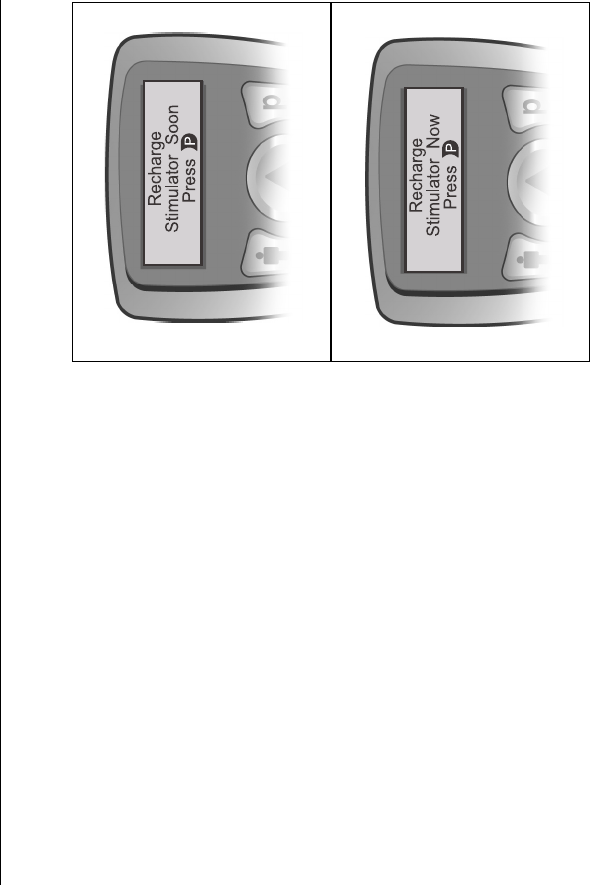
About Your Implant Battery
When the Remote Control checks the condition of
your implant battery, you may see one or more of the
following messages depending on the battery’s
charge level:
• If the implant battery is low, the Remote
Control will display the message shown
at right. Press Dto return to the Level
screen.
• If the implant battery is very low, the
remote will display this notice to recharge
the stimulator battery immediately.
Stimulation has most likely been turned
off automatically. Pressing Dfrom this
screen will prompt the message explained
on the following page.
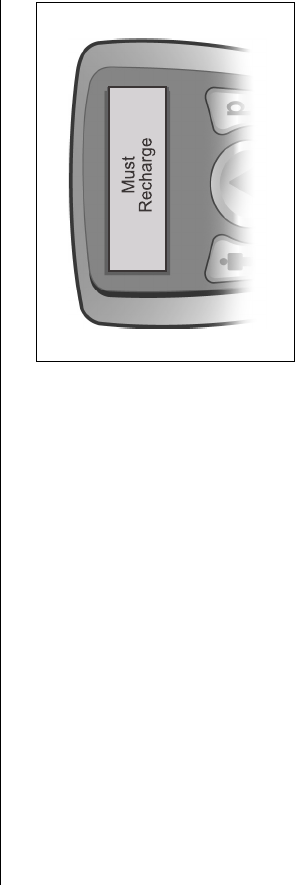
The Remote Control
49
The Must Recharge message means that your
implant has turned itself off and gone into a
“hibernation” mode. You may expect a three--four
hour charge period before you can resume your
therapy.
Patient System Handbook
50
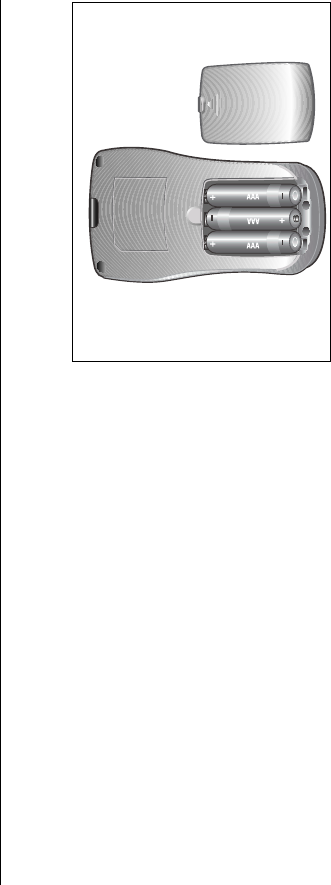
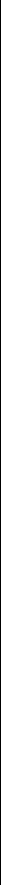
Battery Replacement
1. On the rear of the remote, push in slightly and
slide down the battery compartment cover.
2. Remove the old batteries.
3. Place the three new AAA batteries in the slots,
matching the positive (+) and negative (-)
markings.
4. Align the battery compartment cover on the case
and slide the cover into position until it snaps
closed.
The Remote Control will connect to the implant in approximately 30 seconds.

51
5 Charging the Implant
Your Precision implant uses a rechargeable battery to provide stimulation. The Precision
System’s programming software gives your healthcare provider recommendations for
recharging your implant, and you should be given guidelines on when to charge.
The Remote Control provides an easy-view implant battery charge status graphic on the
Level screen as well as messages to inform you of the battery’s condition. These messages
are explained beginning on page 48.
Based on your stimulation settings, you may charge:
• once a day
• every other day
• once or twice a week.
Patient System Handbook
52
Following the general recommendations made by your healthcare provider, you have the
freedom to establish the charging routine that suits you best. Keep in mind that if you do not
charge your implant before it reaches the very low/”hibernation” condition, stimulation will
eventually stop until you charge again. But charging the Precision is a such simple process,
requiring so little effort, that you should never have to experience an interruption of your
pain therapy.
Note: If the implant is not recharged as recommended, stimulation will stop due to a low battery. If
this happens, the implant must be recharged within three days from loss of stimulation. If
stimulation stops and you have lost or cannot get to your charger within five days, contact
Customer Service immediately at (866) 360-4747 for a new charger.
If discontinuing stimulation for an extended period of time, the implant should first be fully
charged. Additionally, the implant should be fully charged every month if stimulation is not
used.
Charging the Implant
53
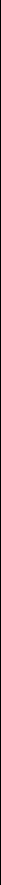
Getting Started
The Charging System for your implant consists of the Charger unit, a Base Station, and a
Power Supply. Power plug adaptors are also included for Charging System use in countries
other than U.S. The Base Station is designed to remain connected to a power outlet at all
times. When it is not being used, keep the Charger on the Base Station so that it is always
ready to deliver a charge.
1. Find a convenient place with a flat, clear surface to keep the Base Station plugged in.
2. Plug the Power Supply into a standard AC wall outlet, then plug the other end into the
Base Station connector.
3. Place the Charger in the Base Station.
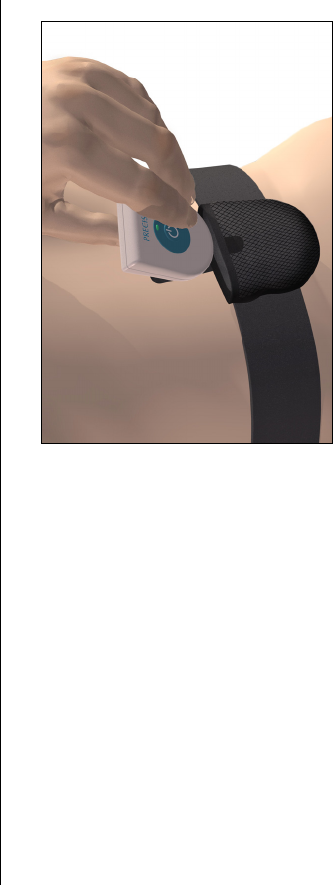
When charging, you can opt to use either a Velcro® belt or adhesive patches to hold the
Charger over the implant. Before using the Velcro® belt, you may cut it to a more
convenient size, but be careful not to cut too much. The patch adhesives are made of non-
reactive material suitable for most sensitive skin types.
Note: Advanced Bionics recommends the use of the Velcro® belt for charging.
Patient System Handbook
54
The Charger is completely ready and able
to fully charge your implant when the
indicator light is green. If the light is
amber-colored, the Charger can only
partially charge the implant. It may be
used, but it may not be able to return your
implant to a full charge (and you may
need to charge sooner than you normally
would).
Indicator Light Status:
• Green – ready for full charge
• Amber – partial charge
• Off – not ready for charging
Charging Your Implant
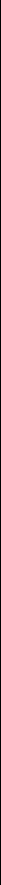
1. When the indicator light is green, remove the Charger from the Base Station. (The
indicator will go off, regardless of the ready status of the Charger.)
Charging the Implant
55
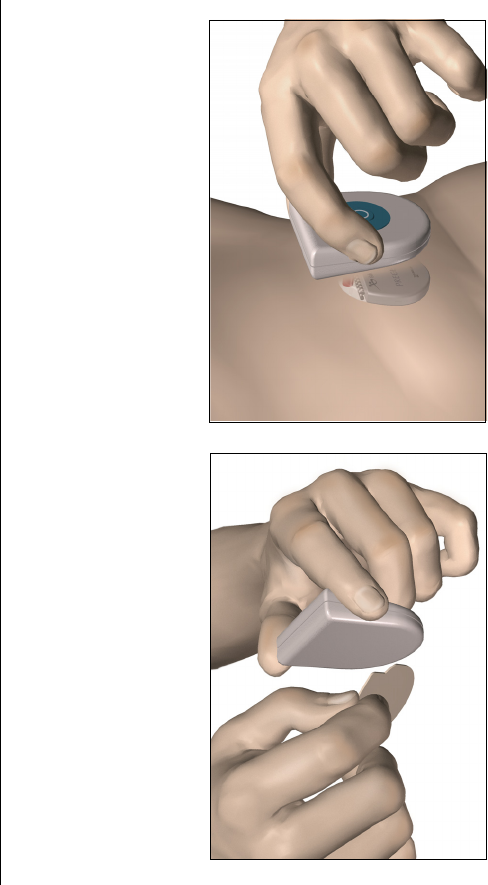
2. Using the Adhesive Patch: Apply the adhesive patch to the backside of the Charger
by peeling the clear liner from the patch. Remove the skin
side beige liner.
Using the Velcro® Belt: Place the Charger in the pocket with the power button fac-
ing out.
3. Press the power button. The indicator light will come on again, and the Charger will
begin beeping steadily to signal that it is searching for the implant.
Patient System Handbook
56
4. Locate the Charger over the implant. When the Charger is aligned with the implant, the
beeping will stop.
Secure the Charger over the implant either by pressing the adhesive side of the patch to
the location, or by attaching the Velcro® belt.
Note: If you accidentally locate the patch in the wrong place, or if the Velcro® belt moves out of
alignment, the Charger will start beeping again. Use a new adhesive patch or readjust the
belt to place the Charger back into position.
Charging the Implant
57
5. When the Charger emits a distinct
double beep, the implant is charged.
Switch off the Charger, remove the
adhesive patch or Velcro® belt, and
return the Charger to the Base Station.
Do not confuse the end of charge signal
(a distinct double beep) with the steady,
continuous misalignment signal.
Patient System Handbook
58
Note: • Depending on your program parameters, you may expect daily recharging times as low as
10 minutes up to four hours, or weekly recharging times from as low as one hour up to four
hours.
•The end of a charge signal is a distinct double beep, and the alignment indicator is a steady
continuous signal.
The rechargable implant battery should provide you with at least five years of service. Over
time and with repeated charging, the battery in your implant will lose the ability to recover
its full capacity. As a result, you may need to recharge your implant for longer periods and/
or more often after five years of service. Your implant will need replacement when
stimulation can no longer be maintained with routine charging.
59
6Help
Stimulation
No Stimulation
1. Toggle the Remote Control stimulation on/off
button to make sure that stimulation is ON. If the
Remote Control receives confirmation from the
implant, it will flash “Stimulation On.”
2. Turn up the level of stimulation from the main
screen or area screens.
3. Charge the implant. When the charge is
complete, try turning the stimulation on.
Patient System Handbook
60
4. Call our Customer Service Department at (866) 360-4747 if the above steps do not solve
the problem.
Stimulation Increases or Decreases on Its Own
1. Stimulation can change depending on body position (lying down, standing or bending).
2. Always keep the Remote Control with you, so that you can adjust your stimulation
levels as needed.
Stimulation Shuts Off
1. When the implant battery needs to be recharged, it will stop stimulating. Check the
battery status with the Remote Control and recharge if necessary, then turn stimulation
back on. If the implant regularly stops stimulating before you charge, you can charge
more often.
2. Although unlikely, anti-theft screeners can turn stimulation off. If you cannot turn the
stimulator back on with your Remote Control, you may need to charge the implant.
3. Large magnetized speakers or large power lines that emit interference may also turn off
stimulation. If you cannot turn the stimulator back on with your Remote Control, you
may need to charge the implant.
Help
61
Remote Control Display Messages
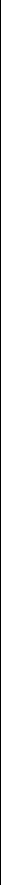
“Recharge Stimulator Now” and “Must Recharge” on the
Display
Stimulation has stopped if you see this message. You
will probably need to recharge your implant for as
long as 3–4 hours before stimulation resumes.
Patient System Handbook
62
Remote Battery Low” on the Display
The batteries in your Remote Control need to be
replaced with three fresh AAA batteries (refer to
“Battery Replacement” on page 50).
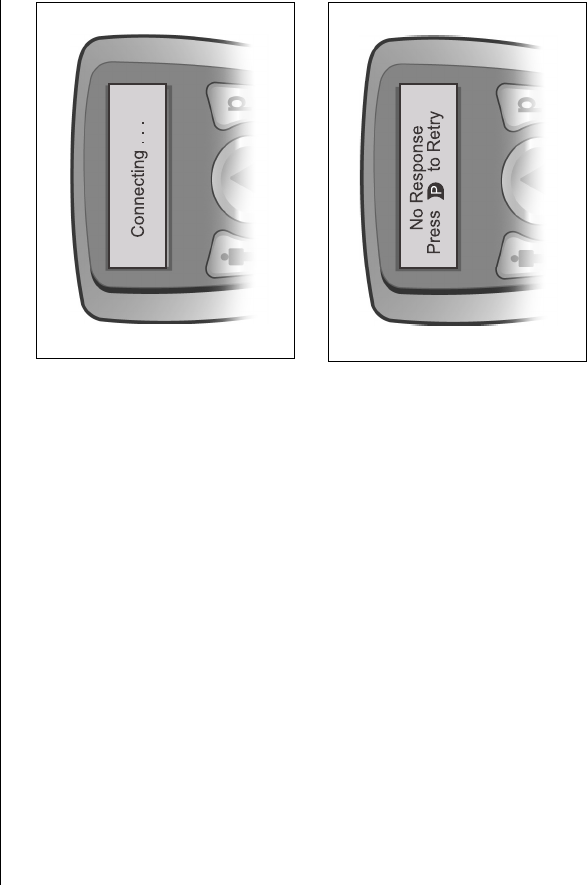
“No Response” on the Display
When the Remote Control displays “No Response,”
there is a communication problem between the
remote and the implant probably caused by a weak
implant battery. Press the Dbutton. If the Remote
Control is still not able to communicate with your
implant, the “No Response” message will appear
again; press D again. If the remote connects with
your implant, you will be returned to the display you
Help
63
were using before the problem began. If the problem cannot be corrected, the Remote
Control will go into sleep mode. Recharge the IPG and check to see if the problem is solved.
Occasionally, telemetry problems happen because the Remote Control cannot find the
implant because of orientation or interference. Move the remote closer and then press the
Dbutton.
Call our Customer Service Department at (866) 360-4747 if the problem continues.
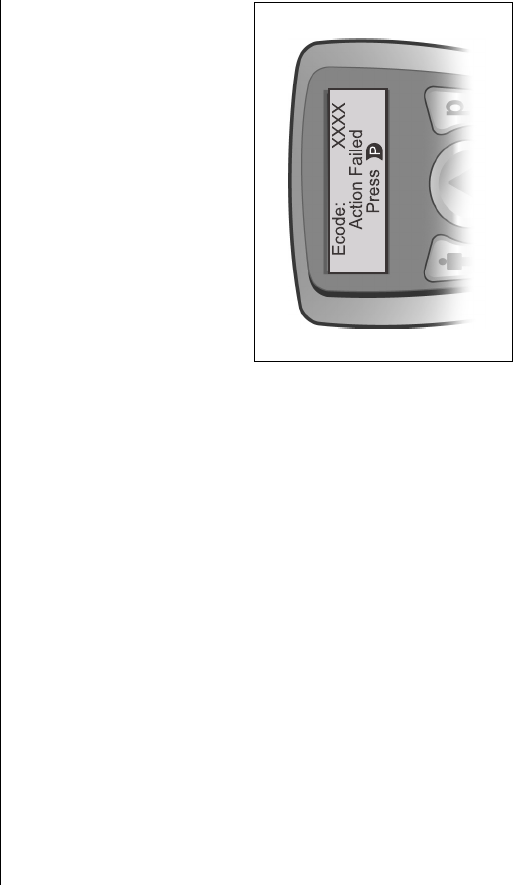
“Action Failed” on the Display
If the Remote Control displays the error screen
shown at right, try to make a note of the numbers (the
error code) on the top line. Then press D, wait a few
seconds, and try the action again.
Please call our Customer Service Department at your
earliest convenience to report the error code.
Note: The remote will go to idle mode when D is pressed,
or within fifteen seconds if D is not pressed.
Patient System Handbook
64
Accessories
Washing the Velcro® Belt
Wash the belt with mild soap and warm water.
Contacting Advanced Bionics
If you have any other questions, or need to contact Advanced Bionics for any reason, you
may do so in any of the following ways:
• Customer Service Phone: (866) 360-4747
• Customer Service Fax: (661) 362-1503
• Address: Advanced Bionics® Corporation
Pain Management Division
Mann Biomedical Park
25129 Rye Canyon Loop
Valencia CA 91355

65
7 Limited Warranty
Implanted Pulse Generator
Advanced Bionics® Corporation (hereinafter referred to as Advanced Bionics®) warrants
to the patient who receives a Precision™ System that the implanted pulse generator
(hereinafter referred to as the IPG), Model SC-1110, is free from defects in workmanship
and materials for a period of one (1) year from the date of surgical implant of the IPG. This
warranty only applies to the patient (recipient, hereinafter referred to as the patient), and no
other individual.
An IPG that fails to function within normal tolerances within (1) year from the date of
surgery is covered under this Limited Warranty. The liability of Advanced Bionics® under
this warranty shall be limited to: (a) replacement with a functionally equivalent IPG; or (b)
full credit equal to the original purchase price to be applied towards the purchase of a new
Patient System Handbook
66
IPG. Product claims under Advanced Bionics® Limited Warranty are subject to the
following conditions and limitations:
1. The product registration card must be completed and returned to Advanced Bionics®
within 30 days of surgery in order to obtain warranty rights.
2. The IPG must be returned to Advanced Bionics® (or authorized agent) within 30 days
of malfunction or discovery of defect, and shall be the property of Advanced Bionics®.
3. The IPG must be implanted prior to the “use before” date.
4. Failure of the IPG must be confirmed by Advanced Bionics®. This warranty specifically
excludes defects or malfunctions caused by: (a) fire, floods, lightning, natural disasters,
water damage and other calamities commonly defined as “Acts of God”; (b) accident,
misuse, abuse, negligence, or customer’s failure to operate the IPG in accordance with
manufacturer’s instructions; (c) unauthorized attempts to repair, maintain, or modify the
equipment by the customer or any unauthorized third party; or (d) attachment of any
equipment not supplied by Advanced Bionics® without prior approval.
This warranty does not include the leads, extensions or surgical accessories used with
the Precision™ IPG.
Limited Warranty
67
5. The decision as to product replacement or credit shall be made solely at the discretion of
Advanced Bionics®. For a replacement IPG, the warranty will run only to the end of the
warranty period for the original IPG that was replaced.
This warranty is in lieu of any other warranty, expressed or implied, including any warranty
of merchantability or fitness for intended use. Except as expressly provided by this Limited
Warranty, Advanced Bionics® shall not be responsible or liable for any direct,
consequential or incidental damages caused by device malfunction, failure or defect,
whether the claim is based on warranty, contract, tort or otherwise.
Externals
Advanced Bionics® warrants to the patient that the Remote Control device, Model
SC-5210, and Charger System (Charger, Model SC-5300, and/or Charger Base Station,
Model SC-5305) are free from defects in workmanship and materials for a period of one (1)
year from the date of purchase of a new Precision™ Patient Kit.
A Remote Control device or Charger or Charger Base Station component that fails to
function within normal tolerances within one (1) year from the date of surgery or purchase is
covered under this Limited Warranty. The liability of Advanced Bionics® under this
warranty shall be limited to: (a) replacement with a functionally equivalent component; or
Patient System Handbook
68
(b) full credit equal to the original purchase price to be applied towards the purchase of a
replacement device. Product claims under Advanced Bionics® Limited Warranty are
subject to the following conditions and limitations:
1. The product registration card must be completed and returned to Advanced Bionics®
within 30 days of surgery or receipt of product in order to obtain warranty rights.
2. The component must be returned to Advanced Bionics® (or authorized agent) within 30
days of malfunction or discovery of defect.
3. The component failure must be confirmed by Advanced Bionics®. This warranty
specifically excludes defects or malfunctions caused by: (a) fire, floods, lightning,
natural disasters, water damage and other calamities commonly defined as “Acts of
God”; (b) accident, misuse, abuse, negligence, or the customer’s failure to operate the
system and its components in accordance with manufacturer’s instructions; (c)
unauthorized attempts to repair, maintain, or modify the equipment by the customer or
any unauthorized third party; or (d) attachment of any equipment not supplied by
Advanced Bionics® without prior approval.
Limited Warranty
69
4. The decision as to product replacement or credit shall be made solely at the discretion of
Advanced Bionics®. For a replacement component, the warranty will run only to the
end of the warranty period for the original component that was replaced.
This warranty is in lieu of any other warranty, expressed or implied, including any warranty
of merchantability or fitness for intended use. Except as expressly provided by this Limited
Warranty, Advanced Bionics® shall not be responsible or liable for any direct,
consequential or incidental damages caused by device malfunction, failure or defect,
whether the claim is based on warranty, contract, tort or otherwise.
Patient System Handbook
70
Glossary
71
Glossary
C Area Button icon. This figure respresents the
area button on the Remote Control.
ADHESIVE PATCH. Non-reactive skin patch
designed to temporarily attach the Charger
to the skin over the IPG site.
ADVERSE EFFECT. Undesirable result.
AMPLITUDE. The measure-of-strength of
delivered stimulation. (See Level.).
AREA. A location on the body such as right
leg or left leg where stimulation will occur.
CARDIAC PACEMAKER. A small
implantable device used to control the
rhythm of the heart.
CHARGER. A portable device used to
recharge the battery of the implanted
stimulator.
CHARGER BASE STATION. A holder/
power supply that supports the Charger and
keeps it in a ready state for recharging the
implant.
CHARGING SYSTEM. The Charging
System consists of a Charger Base Station,
Charger, Power Supply, Velcro charging
belt and adhesive patches. The system is
used for recharging the implanted
stimulator.
CONTROL BUTTONS. Buttons located on
the Remote Control; used for adjusting
stimulation settings.
DIATHERMY. A therapeutic procedure used
to heat body tissue by high-frequency
electromagnetic currents.
Patient System Handbook
72
DISPLAY. The Remote Control screen.
ELECTRICAL PULSE GENERATOR. Also
called an implantable pulse generator
(IPG); used to send electrical pulses to the
spinal cord or other parts of the body.
ELECTRICAL STIMULATION.The energy
created by a pulse generator.
ELECTROMAGNETIC INTERFERENCE
(EMI). Electromagnetic signals that
interfere with a variety of electrical signals
including spinal cord stimulation.
IDLE MODE. A time-out period when the
Remote Control is not being used. Also
known as sleep mode.
IMPLANT. Small implantable electrical pulse
generator used to control stimulation.
INCISION. Small surgical cut or opening in
the skin.
INDICATOR. A signal light used on the Trial
Stimulator and the IPG Charger.
IPG. Implantable Pulse Generator.
LEAD MIGRATION. The movement of a
lead away from the spinal cord.
LEAD. A surgical wire that sends electrical
stimulation pulses from a pulse generator to
the spinal cord.
LEVEL. Term used on the Remote Control
screen to identify the amplitude or strength
of stimulation pulses.
LONG BUTTON PRESS. To press and hold a
button for about 3 seconds.
MRI. Magnetic Resonance Imaging; the use of
a nuclear magnetic resonance spectrometer
Glossary
73
to produce electronic images of tissues and
organs.
OPTIONS. Methods for adjusting stimulation
beyond amplitude, or level, using the
Remote Control. Your healthcare provider
may or may not provide you with all
available options.
D Program Button icon. This symbol
represents the Program button on the
remote control.
PARESTHESIA. Sensation produced by
electrical stimulation.
PATIENT IDENTIFICATION CARD. A
wallet size card that lists the patient and
physician names, and IPG model and serial
number.
PERMANENT IMPLANT. A stimulator
system, pulse generator and leads,
implanted in the body and maintained by a
pulse generator battery Charging System.
PRECAUTION. Generally, situations that you
should be aware of in order to avoid
potentially uncomfortable stimulation
sensations and/or damage to your
stimulation system.
PROGRAM. Combination of one or more
stimulation areas.
PULSE WIDTH. The length of time each
stimulation "spark" lasts. An option setting
available from the Remote Control.
RATE. The number of times–per-second
(speed) at which stimulation pulses are
delivered to the spinal cord. An option
setting available from the Remote Control.
Patient System Handbook
74
REMOTE CONTROL. A battery powered
hand-held computer used to adjust
stimulation.
SAVE. The Remote Control button command
used to store a newly created or modified
stimulation program.
SLEEP MODE. A time-out period when the
Remote Control is not being used. Also
known as idle mode.
SPINAL CORD STIMULATION (SCS). A
method of applying electrical pulses to the
spinal cord to block/mask pain signals to
the brain.
STIMULATION. When used as a therapy for
pain, an artificially applied, low-level,
pulsating electrical "shock" felt as a tingling
or pulsating sensation in the area of pain
and perceived enough to reduce the
awareness of pain.
STIMULATION COVERAGE. Area on the
body where stimulation occurs. (See Area.)
SUBCLAVICULAR. Under the collarbone.
SYSTEM FAILURE. Inability of spinal cord
stimulator system to deliver stimulation
therapy.
WARNING. Potential hazards that you must be
aware of to avoid serious situations that
may cause injury or death.
WIDTH. See Pulse Width.
Index
75
Index
A
Adhesive Patch ............................ 55, 71
amplitude ............................... 71, 72, 73
area ............................................... 71, 74
B
battery .......................................... 23, 62
C
charge indicator ............................ 54, 55
charge signal ...................................... 58
control buttons ................................... 71
D
diathermy ..................................... 17, 71
I
indicator ........................................54, 72
L
level ..............................................33, 72
M
MRI ..............................................18, 24
O
options ................................................73
P
paresthesia ......................................1, 73
Patient Identification Card ..............5, 73
Power Supply ...................................5, 6
program ..............................................73
Patient System Handbook
76
S
SAVE ................................................. 74
77
The following is federal government communications regulation information about the Pre-
cision™ System.
This device complies with part 15 of the FCC Rules. Operation is subject to the following
two conditions: (1) This device may not cause harmful interference, and (2) This device
must accept any interference received including interference that may cause undesired oper-
ation.
The Precision™ System components should only be serviced by Advanced Bionics. Do not
attempt to open or repair any of the components. Unauthorized opening of or attempts to
repair the components will void the warranty.
Changes of modifications to this product not authorized by Advanced Bionics Corporation
could void the FCC Certification and negate your authority to operate this product.
Patient System Handbook
78